Endoscopic Ultrasound–Guided Fine Needle Aspiration Cytology of ...
Endoscopic Ultrasound–Guided Fine Needle Aspiration Cytology of ...
Endoscopic Ultrasound–Guided Fine Needle Aspiration Cytology of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
AJG – September, 2003<br />
EUS-FNA <strong>Cytology</strong> <strong>of</strong> Solid Liver Lesions<br />
1977<br />
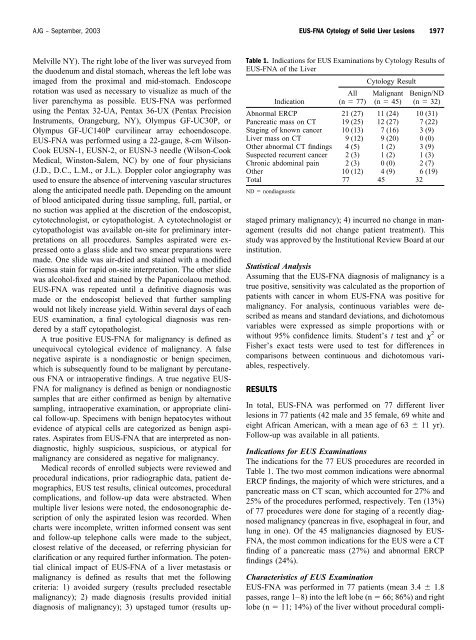
Table 1. Indications for EUS Examinations by <strong>Cytology</strong> Results <strong>of</strong><br />
EUS-FNA <strong>of</strong> the Liver<br />
Melville NY). The right lobe <strong>of</strong> the liver was surveyed from<br />
the duodenum and distal stomach, whereas the left lobe was<br />
imaged from the proximal and mid-stomach. Endoscope<br />
rotation was used as necessary to visualize as much <strong>of</strong> the<br />
liver parenchyma as possible. EUS-FNA was performed<br />
using the Pentax 32-UA, Pentax 36-UX (Pentax Precision<br />
Instruments, Orangeburg, NY), Olympus GF-UC30P, or<br />
Olympus GF-UC140P curvilinear array echoendoscope.<br />
EUS-FNA was performed using a 22-gauge, 8-cm Wilson-<br />
Cook EUSN-1, EUSN-2, or EUSN-3 needle (Wilson-Cook<br />
Medical, Winston-Salem, NC) by one <strong>of</strong> four physicians<br />
(J.D., D.C., L.M., or J.L.). Doppler color angiography was<br />
used to ensure the absence <strong>of</strong> intervening vascular structures<br />
along the anticipated needle path. Depending on the amount<br />
<strong>of</strong> blood anticipated during tissue sampling, full, partial, or<br />
no suction was applied at the discretion <strong>of</strong> the endoscopist,<br />
cytotechnologist, or cytopathologist. A cytotechnologist or<br />
cytopathologist was available on-site for preliminary interpretations<br />
on all procedures. Samples aspirated were expressed<br />
onto a glass slide and two smear preparations were<br />
made. One slide was air-dried and stained with a modified<br />
Giemsa stain for rapid on-site interpretation. The other slide<br />
was alcohol-fixed and stained by the Papanicolaou method.<br />
EUS-FNA was repeated until a definitive diagnosis was<br />
made or the endoscopist believed that further sampling<br />
would not likely increase yield. Within several days <strong>of</strong> each<br />
EUS examination, a final cytological diagnosis was rendered<br />
by a staff cytopathologist.<br />
A true positive EUS-FNA for malignancy is defined as<br />
unequivocal cytological evidence <strong>of</strong> malignancy. A false<br />
negative aspirate is a nondiagnostic or benign specimen,<br />
which is subsequently found to be malignant by percutaneous<br />
FNA or intraoperative findings. A true negative EUS-<br />
FNA for malignancy is defined as benign or nondiagnostic<br />
samples that are either confirmed as benign by alternative<br />
sampling, intraoperative examination, or appropriate clinical<br />
follow-up. Specimens with benign hepatocytes without<br />
evidence <strong>of</strong> atypical cells are categorized as benign aspirates.<br />
Aspirates from EUS-FNA that are interpreted as nondiagnostic,<br />
highly suspicious, suspicious, or atypical for<br />
malignancy are considered as negative for malignancy.<br />
Medical records <strong>of</strong> enrolled subjects were reviewed and<br />
procedural indications, prior radiographic data, patient demographics,<br />
EUS test results, clinical outcomes, procedural<br />
complications, and follow-up data were abstracted. When<br />
multiple liver lesions were noted, the endosonographic description<br />
<strong>of</strong> only the aspirated lesion was recorded. When<br />
charts were incomplete, written informed consent was sent<br />
and follow-up telephone calls were made to the subject,<br />
closest relative <strong>of</strong> the deceased, or referring physician for<br />
clarification or any required further information. The potential<br />
clinical impact <strong>of</strong> EUS-FNA <strong>of</strong> a liver metastasis or<br />
malignancy is defined as results that met the following<br />
criteria: 1) avoided surgery (results precluded resectable<br />
malignancy); 2) made diagnosis (results provided initial<br />
diagnosis <strong>of</strong> malignancy); 3) upstaged tumor (results upstaged<br />
primary malignancy); 4) incurred no change in management<br />
(results did not change patient treatment). This<br />
study was approved by the Institutional Review Board at our<br />
institution.<br />
Statistical Analysis<br />
Assuming that the EUS-FNA diagnosis <strong>of</strong> malignancy is a<br />
true positive, sensitivity was calculated as the proportion <strong>of</strong><br />
patients with cancer in whom EUS-FNA was positive for<br />
malignancy. For analysis, continuous variables were described<br />
as means and standard deviations, and dichotomous<br />
variables were expressed as simple proportions with or<br />
without 95% confidence limits. Student’s t test and 2 or<br />
Fisher’s exact tests were used to test for differences in<br />
comparisons between continuous and dichotomous variables,<br />
respectively.<br />
RESULTS<br />
Indication<br />
All<br />
(n 77)<br />
<strong>Cytology</strong> Result<br />
Malignant<br />
(n 45)<br />
Benign/ND<br />
(n 32)<br />
Abnormal ERCP 21 (27) 11 (24) 10 (31)<br />
Pancreatic mass on CT 19 (25) 12 (27) 7 (22)<br />
Staging <strong>of</strong> known cancer 10 (13) 7 (16) 3 (9)<br />
Liver mass on CT 9 (12) 9 (20) 0 (0)<br />
Other abnormal CT findings 4 (5) 1 (2) 3 (9)<br />
Suspected recurrent cancer 2 (3) 1 (2) 1 (3)<br />
Chronic abdominal pain 2 (3) 0 (0) 2 (7)<br />
Other 10 (12) 4 (9) 6 (19)<br />
Total 77 45 32<br />
ND nondiagnostic<br />
In total, EUS-FNA was performed on 77 different liver<br />
lesions in 77 patients (42 male and 35 female, 69 white and<br />
eight African American, with a mean age <strong>of</strong> 63 11 yr).<br />
Follow-up was available in all patients.<br />
Indications for EUS Examinations<br />
The indications for the 77 EUS procedures are recorded in<br />
Table 1. The two most common indications were abnormal<br />
ERCP findings, the majority <strong>of</strong> which were strictures, and a<br />
pancreatic mass on CT scan, which accounted for 27% and<br />
25% <strong>of</strong> the procedures performed, respectively. Ten (13%)<br />
<strong>of</strong> 77 procedures were done for staging <strong>of</strong> a recently diagnosed<br />
malignancy (pancreas in five, esophageal in four, and<br />
lung in one). Of the 45 malignancies diagnosed by EUS-<br />
FNA, the most common indications for the EUS were a CT<br />
finding <strong>of</strong> a pancreatic mass (27%) and abnormal ERCP<br />
findings (24%).<br />
Characteristics <strong>of</strong> EUS Examination<br />
EUS-FNA was performed in 77 patients (mean 3.4 1.8<br />
passes, range 1–8) into the left lobe (n 66; 86%) and right<br />
lobe (n 11; 14%) <strong>of</strong> the liver without procedural compli-