Grand Rounds Archive - Otology/Neurotology - Famona Site
Grand Rounds Archive - Otology/Neurotology - Famona Site
Grand Rounds Archive - Otology/Neurotology - Famona Site
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
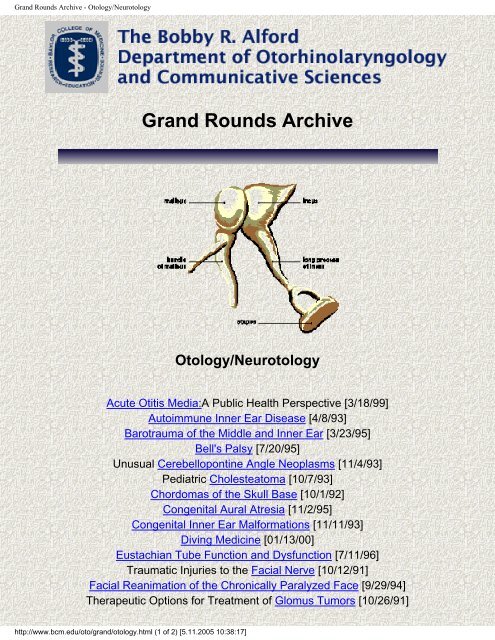
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> - <strong>Otology</strong>/<strong>Neurotology</strong><br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong><br />
<strong>Otology</strong>/<strong>Neurotology</strong><br />
Acute Otitis Media:A Public Health Perspective [3/18/99]<br />
Autoimmune Inner Ear Disease [4/8/93]<br />
Barotrauma of the Middle and Inner Ear [3/23/95]<br />
Bell's Palsy [7/20/95]<br />
Unusual Cerebellopontine Angle Neoplasms [11/4/93]<br />
Pediatric Cholesteatoma [10/7/93]<br />
Chordomas of the Skull Base [10/1/92]<br />
Congenital Aural Atresia [11/2/95]<br />
Congenital Inner Ear Malformations [11/11/93]<br />
Diving Medicine [01/13/00]<br />
Eustachian Tube Function and Dysfunction [7/11/96]<br />
Traumatic Injuries to the Facial Nerve [10/12/91]<br />
Facial Reanimation of the Chronically Paralyzed Face [9/29/94]<br />
Therapeutic Options for Treatment of Glomus Tumors [10/26/91]<br />
http://www.bcm.edu/oto/grand/otology.html (1 of 2) [5.11.2005 10:38:17]
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> - <strong>Otology</strong>/<strong>Neurotology</strong><br />
Considerations in the Evaluation of the Hearing Impaired Child [3/11/93]<br />
Update on Hearing Aids [6/3/93]<br />
Herpes Zoster Oticus [8/21/97]<br />
Neurotologic Manifestations Of HIV Infection [3/24/94]<br />
Infectious Intracranial Complications of Suppurative Ear Disease [3/18/93]<br />
Lateral Sinus Thrombosis [5/7/92]<br />
Acute Mastoiditis [2/3/94]<br />
Surgical Management Of Meniere's Syndrome [4/14/94]<br />
Myringoplasty and Tympanoplasty [2/16/95]<br />
Osteodystrophies of the Middle Ear and Temporal Bone [2/8/95]<br />
Ototoxicity [8/20/92]<br />
Ototoxicity [4/25/96]<br />
Otitis Externa [10/12/95]<br />
Pathology And Pathogenesis Of Otitis Media [4/21/94]<br />
The Diagnosis and Management of Perilymphatic Fistulas [10/21/93]<br />
Lesions of the Petrous Apex [8/4/94]<br />
Complications of Stapedectomy [11/11/99]<br />
Issues in Stapedectomy [2/6/92]<br />
Sudden Sensorineural Hearing Loss [3/5/92]<br />
Sudden Sensorineural Hearing Loss [11/18/93]<br />
Temporal Bone Fractures [4/2/92]<br />
Temporal Bone Gunshot Wounds: Evaluation and Management [8/5/93]<br />
Subjective Tinnitus [03/12/98]<br />
Tuberculous Otitis Media [11/22/92]<br />
Tympanostomy Tubes [2/23/95]<br />
Vestibular Adaptation and Rehabilitation [5/21/92]<br />
Vestibular Neuritis [7/14/94]<br />
Laryngology | Neoplasms | Pediatric | Plastics | Rhinology | Others | Main | Home<br />
©2001, The Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences,<br />
Baylor College of Medicine<br />
One Baylor Plaza, NA102, Houston, TX 77030 oto@bcm.tmc.edu<br />
URL: http://www.bcm.tmc.edu/oto (Modified: 12/12/01)<br />
http://www.bcm.edu/oto/grand/otology.html (2 of 2) [5.11.2005 10:38:17]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by<br />
doctors and other health care professionals. These documents were prepared by<br />
resident physicians for presentation and discussion at a conference held at The<br />
Baylor College of Medicine in Houston, Texas. No guarantees are made with<br />
respect to accuracy or timeliness of this material. This material should not be used<br />
as a basis for treatment decisions, and is not a substitute for professional<br />
consultation and/or peer-reviewed medical literature.<br />
Acute Otitis Media: A Public Health Perspective<br />
Derek Drummond, M.D.<br />
March 18, 1999<br />
Case Presentation<br />
J.D., a previously healthy girl, presented to her pediatrician at 6<br />
http://www.bcm.edu/oto/grand/031899.html (1 of 6) [5.11.2005 10:38:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
months of age with a 3-day history of increasing irritability and<br />
fevers. History revealed that she had upper respiratory tract<br />
symptoms for 3 days that included nasal congestion, rhinorrhea,<br />
dry cough, decreased appetite and low-grade fevers. The parents<br />
became concerned the night before presentation when she<br />
became very irritable, appeared to be in pain, and vomited once<br />
after bottle-feeding. The girl was seen pulling on her ears and<br />
was inconsolable prior to arrival at the pediatrician's office. She<br />
had no previous medical problems and was not taking any<br />
medication other than acetaminophen.<br />
Physical exam demonstrated a 6-month old girl who was crying<br />
in her mother's arms. She was alert but not cooperative. She had<br />
a temperature of 101.5 F. Examination of the ears revealed a<br />
right tympanic membrane that was bulging, erythematous, and<br />
didn't move with pneumotoscopy. The nasal mucosa was<br />
congested and the patient was mouth breathing. The remainder<br />
of the physical exam was unremarkable. She was diagnosed with<br />
acute otitis media and prescribed a 10-day course of amoxicillin<br />
at 40mg/kg/day. Within 24 hours, her symptoms were improving<br />
and she began to feed normally. Follow-up at 2 weeks revealed<br />
bilateral middle-ear effusions in a happy, asymptomatic child.<br />
The MEE would resolve spontaneously over the next 3 months.<br />
Bibliography<br />
Berman S. Otitis media in developing countries. Pediatrics 1995; 96:126-131.<br />
Berman S, Byrns PJ, Bondy J, Smith PJ, Lezotte D. Otitis media-related antibiotic prescribing<br />
patterns, outcomes, and expenditures in a pediatric medicaid population. Pediatrics 1996;100:585-<br />
592.<br />
Bluestone CD. Otitis media. In: Behrman RE, Vaughan RE, Nelson WE, editors. Nelson<br />
http://www.bcm.edu/oto/grand/031899.html (2 of 6) [5.11.2005 10:38:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Textbook of Pediatrics, 13th edition. Philadelphia: W.B. Saunders; 1987. pp. 880.<br />
Bluestone CD, Klein JO. Otitis media, atelectasis, and eustachian tube dysfunction. In: Bluestone<br />
CD, Stool SE, editors. Pediatric Otolaryngology, 3rd edition. Philadelphia: W.B. Saunders;1996.<br />
pp. 388-582.<br />
Bluestone CD, Stephenson JS, Martin LM. Ten-year review of otitis media pathogens. Pediatr<br />
Infect Dis J 1992;11:S7-S11.<br />
Blumer JL. Pharmacokinetics and pharmacodynamics of new and old antimicrobial agents for<br />
acute otitis media. Pediatr Infect Dis J 1998;17:1070-1075.<br />
Bottenfield GW, Burch DJ, Hedrick JA, Schaten R, Rowinski CA, Davies JT. Safety and<br />
tolerability of a new formulation (90 mg/kg/day divided every 12 h) of amoxicillin/clavulanate<br />
(Augmentin) in the empiric treatment of pediatric acute otitis media caused by drug-resistant<br />
Streptococcus pneumoniae. Pediatr Infect Dis J 1998;17:963-968.<br />
Boulesteix J, Dubreuil C, de La Roque F, Trinh A, Scheimberg A. Effects of cefixime or coamoxiclav<br />
treatment on nasopharyngeal carriage of Streptococcus pneumoniae and Haemophilus<br />
influenzae in children with acute otitis media: J Antimicrob Chemother 1998;41:253-258.<br />
Branthaver B, Greiner DL, Eichelberger R Determination of cost-effective treatment of acute<br />
otitis media from HMO records. Am J Health Syst Pharm 1997;54:2736-2740.<br />
Brown DH. Education of medical practitioners in otitis media management. J Otolaryngol 1998;<br />
2749-52.<br />
Canafax DM, Yuan Z, Chonmaitree T, Deka K, Russlie HQ, Giebink GS. Amoxicillin middle ear<br />
fluid penetration and pharmacokinetics in children with acute otitis media. Pediatr Infect Dis J<br />
1998;17:149-156.<br />
Casselbrant ML, Mandel EM, Kurs-Lasky M, Rockette HE, Bluestone CE. Otitis media in a<br />
population of black American and white American infants, 0-2 years of age. Int J Pediatr<br />
Otorhinolaryngol 1995;33:1-16.<br />
Clements DA, Langdon L, Bland C, Walter E. Influenza A vaccine decreases the incidence of<br />
otitis media in 6- to 30-month-old children in day care. Arch Pediatr Adolesc Med<br />
1995;149:1113-1117.<br />
Craig WA. Antimicrobial resistance issues of the future. Diagn Microbiol Infect Dis 1996;25:213-<br />
217.<br />
Culpepper L, From J. Routine antimicrobial treatment of otitis media: Is it necessary? JAMA<br />
1997;278:1643-1645.<br />
David CB, Hamrick HJ, Schwartz RJ. Follow-up after otitis media. N Engl J Med 1982;307:252.<br />
http://www.bcm.edu/oto/grand/031899.html (3 of 6) [5.11.2005 10:38:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
DeMaria TF, Prior RB, Briggs BR, Lim DJ, Birck HG. Endotoxin in middle-ear effusions from<br />
patients with chronic otitis media with effusion. J Clin Microbiol 1984;20:15-17.<br />
Dowell SF, Schwartz B. Resistant pneumococci: protecting patients through judicious use of<br />
antibiotics. Am Fam Phys 1997;55:1647-1654, 1657-1658.<br />
Gates G.A. Acute otitis media and otitis media with effusion. In: Cummings CE, Harker LE,<br />
editors. Otolaryngology, Head and Neck Surgery, 2nd edition. St. Louis: Mosby;1993. pp. 2808-<br />
2822.<br />
Gates G.A. Workshop on effects of otitis media on the child: socioeconomic impact of otitis<br />
media. Pediatrics 1983;71:639-652.<br />
Gehanno P, N'Guyen L, Derriennic M, Pichon F, Goehrs JM, Berche P. Pathogens isolated<br />
during treatment failures in otitis. Pediatr Infect Dis J 1998;17:885-890.<br />
Giebink GS. Vaccination against middle-ear bacterial and viral pathogens. Ann N Y Acad Sci<br />
1997; 830:330-352.<br />
Heikkinen T, Ruuskanen O. New prospects in the prevention of otitis media. Ann Med<br />
1996;28:23-30.<br />
Hoekelman RA. Infectious illness during the first year of life. Pediatrics 1977;59:119-121.<br />
Kaleida PH., Casselbrant ML, Rocket HE, Paradise JL, Bluestone CD, Blatter MM, Reisinger<br />
KS, Wald ER, Supance JS. Amoxicillin or myringotomy or both for acute otitis media. Results of<br />
a randomized clinical trial. Pediatrics 1991;87:466-474.<br />
Klein JO. Clinical implications of antibiotic resistance for management of acute otitis media.<br />
Pediatr Infect Dis J 1998;17:1084-1089.<br />
Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SE, Wincott JL, Sitar DS, Klassen TP, et al.<br />
Treatment of acute otitis media with a shortened course of antibiotics: a meta-analysis. JAMA<br />
1998;279:1736-1742.<br />
Klein JO, Teele DW, Masson R, Menyuk P, Rosner BA. Otitis media with effusion during the<br />
first three years of life and the development of speech and language. In: Lim DJ, Bluestone CD,<br />
Klein JO, Nelson DJ, editors. Recent Advances in Otitis Media With Effusion. Philapelphia, PA:<br />
BC Decker;1983. pp. 332-333.<br />
Ling D, McCoy RH, Levinson ED. The incidence of middle ear disease and its educational<br />
implications among Baffin Island Eskimo children. Can J Public Health 1969;60:385-390.<br />
Lister PD, Pong A, Chartrand SA, Sanders CC. Rationale behind high-dose amoxicillin therapy<br />
for acute otitis media due to penicillin-nonsusceptible pneumococci: support from in vitro<br />
http://www.bcm.edu/oto/grand/031899.html (4 of 6) [5.11.2005 10:38:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
pharmacodynamic studies. Antimicrob Agents Chemother 1997;41:1926-1932.<br />
Lynn GE, Benitez JT. Temporal bone preservation in a 2600-year-old Egyptian mummy. Science<br />
1974;183:200-202.<br />
Makela PH, Karma P, Leinonen MK. Pneumococcal vaccine and otitis media in infancy.<br />
Bull Eur Physiopathol Respir 1983;19:235-238.<br />
Mandel EM, Casselbrant ML, Rockette HE, Bluestone CD, Kurs-Lasky M. Efficacy of 20-<br />
versus 10-day antimicrobial treatment for acute otitis media. Pediatrics 1995;96:5-13.<br />
Nelson WL, Kennedy DL, Lao CS, Kuritsky JN. Outpatient systemic anti-infective use by<br />
children in the United States, 1977 to 1986. Pediatr Infect Dis J. 1988;7:505-509.<br />
Paradise JL: Controversies: Treatment of acute otitis media. JAMA 1998;279:1784-1785.<br />
Paradise JL. Managing otitis media: a time for change. Pediatrics 1995;96:712-715.<br />
Pean Y, Goldstein FW, Guerrier ML. Highlights of the French antimicrobial resistance<br />
surveillance project. French Study Group. Diagn Microbiol Infect Dis 1996;25:191-194.<br />
Population Estimates Program, Population Division, U.S. Bureau of the Census, Washington, DC<br />
Contact: Statistical Information Staff, Population Division, U.S. Bureau of the Census, 301-457-<br />
2422 Internet Release date: March 17, 1998. www.census.gov/population/estimates/county/co-97-<br />
1/97C1_48.txt<br />
Rathbun TA, Mallin R. Middle ear disease in a prehistoric Iranian population. Bull N Y Acad<br />
Med 1977;53:901-905.<br />
Rosenfeld RM. An evidence-based approach to treating otitis media. Pediatr Clin North Am<br />
1996;43:1165-1181.<br />
Rosenfeld RM, Vertrees JE, Carr J, Cipolle RJ, Uden DL, et al. Clinical efficacy of antimicrobial<br />
drugs for acute otitis media: meta-analysis of 5400 children from thirty-three randomized trials. J<br />
Pediatr 1994;124:355-367.<br />
Saainen UM. Prolonged breast feeding as prophylaxis for recurrent otitis media. Acta Paediatr<br />
Scand 1982;71:567-571.<br />
Schaefer O. Otitis media and bottle-feeding. An epidemiological study of infant feeding habits<br />
and incidence of recurrent and chronic middle ear disease in Canadian Eskimos. Can J Public<br />
Health 1971;62:478-489.<br />
Scheaffer RL, Mendelhall W, Ott L. Simple Random Sampling. In: Scheaffer RL, Mendelhall W,<br />
Ott L, editors. Elementary Survey Sampling, 5th edition. Wadsworth Publishing: Belmont,<br />
California, 1996. pp.79-124.<br />
http://www.bcm.edu/oto/grand/031899.html (5 of 6) [5.11.2005 10:38:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Schappert, SM. Office visits for otitis media, United States 1975-1990. Vital and Health Statistics<br />
of The Centers for Disease Control / National Center for Health Statistics. 1992;214:1.<br />
Schwartz RH, Rodriguez WJ, Hayden GF, Grundfast KM. The reevaluation visit for acute otitis<br />
media. J Fam Pract 1987;24:145-148.<br />
Teele DW, Kleine JO, Rosner B. et al. Middle ear disease and the practice of pediatrics. Burden<br />
during the first five years of life. JAMA 1983; 249:1026-1029.<br />
Teele DW, Kleine JO, Rosner B. Epidemiology of otitis media during the first seven years of life<br />
in children in greater Boston: a prospective cohort study. J Infect Dis 1989;160:83-94.<br />
Timmermans FJ, Gerson S. Chronic granulomatous otitis media in bottle-fed Inuit children. Can<br />
Med Assoc J 1980;122:545-547.<br />
White LL, Holimon TD, Tepedino JT, Portner TS, Wan JY, Thompson JW. Antimicrobials<br />
prescribed for otitis media in a pediatric Medicaid population. Am J Health Syst Pharm<br />
1996;53:2963-2969.<br />
Click here to view the slides from this presentation<br />
Return to the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCM Otolaryngology Home Page<br />
® Copyright, 1995-9. All Rights Reserved.<br />
Baylor College of Medicine. The Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/031899.html (6 of 6) [5.11.2005 10:38:33]
Acute Otitis Media<br />
Slide 1 of 62<br />
http://www.bcm.edu/oto/grand/03-18-99/sld001.htm [5.11.2005 10:39:23]
http://www.bcm.edu/oto/grand/4893.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
AUTOIMMUNE INNER EAR DISEASE<br />
Douglas D. Backous,, MD<br />
April 8, 1993<br />
The role of immunity in sensorineural hearing loss was first suggested in 1958 by Lenhart. Kikuchi, in<br />
1959, wrote of "sympathetic otitis" whereby surgery on one ear affected hearing in the other. He<br />
proposed an autoimmune phenomena as the etiology. In 1961 Beickert, and two years later, Terrayama<br />
presented data supporting autoimmunity in experimental guinea pig cochleas. McCabe described 18<br />
patients with bilateral asymmetric hearing loss progressing over weeks to months which responded to<br />
steroid therapy. His 1979 paper asserted the importance of a high index of suspicion in these patients<br />
since, if diagnosed early, they could be treated and their hearing preserved.<br />
Humoral and cell mediated immunity, the lymphocyte-macrophage system, and the complement cascade<br />
work in homeostatic harmony to provide immune protection to the host. B cells are produced in the bone<br />
http://www.bcm.edu/oto/grand/4893.html (1 of 5) [5.11.2005 10:39:37]
http://www.bcm.edu/oto/grand/4893.html<br />
marrow and, through antigen stimulation and differentiation into plasma cells, produce specific<br />
antibodies. T cells are derived in the thymus and provide regulatory function for B cells, cytotoxic<br />
activity, and generate lymphokines. B and T cells also form immunologic memory. Cells of the<br />
lymphocyte-macrophage system phagocytose foreign cellular components, process antigen, and produce<br />
interferons. The complement cascade amplifies antigen antibody reactions. Chemotactic, anaphylotoxic,<br />
opsoninization, and immune adherence functions arise from the complement system. Kinin-like<br />
substances are also complement generated.<br />
The inner ear is immunologically active. The endolymphatic sac acts as the afferent limb of inner ear<br />
immunity since it can concentrate and primarily synthesize antibody. IgG is the most common antibody<br />
produced with IgM, IgA, and secretory component being present in lower concentrations. The distal<br />
endolymphatic sac is the site of immunologic activity due to extensive perisaccular lymphatics. Antibody<br />
production is independent of serum or cerebrospinal fluid levels. Secondary exposure to antigen in the<br />
inner ear induces a more intense response than primary exposure to antigen.<br />
Autoimmunity occurs with loss of homeostatic control in the immune system. Host tissues become<br />
recognized as foreign and induce damaging vasculitis and fibrosis. Veldman described a continuum of<br />
autoimmunity. On one end, organ specific responses with organ specific autoantibodies and T cells<br />
produce tissue alteration (i.e. Hashimoto's thyroiditis). On the opposite end of the spectrum is non-organ<br />
specific diseases with circulating non-specific autoantibodies (i.e. systemic lupus erythematosus). In<br />
between is organ specific disease with non-specific autoantibodies (ie primary biliary cirrhosis).<br />
Patients with idiopathic autoimmune sensorineural hearing loss present most commonly with bilateral<br />
progressive hearing loss. Fifty percent have vestibular signs, and symptomatically progress over weeks to<br />
months. Females between the ages of 17 to 42 years represent 65% of the cases reported by Hughes.<br />
Twenty percent of Hughes' study later manifested signs of systemic autoimmune disease.<br />
McCabe proposed using ESR, ANA, RF, complement levels, and quantitative immunoglobulin levels as<br />
a screening panel for autoimmune inner ear disease in high risk patients. Positive values in any of the<br />
screening tests would warrant leukocyte inhibition testing. Hughes classified patients as high risk if they<br />
had bilateral and progressive sensorineural hearing loss, no response to conventional therapy,<br />
concomitant immune disorders, abnormal screening tests or improvement of hearing with steroid therapy.<br />
Treatment goals in autoimmune inner ear disease include improving speech thresholds to levels treatable<br />
with hearing aids in severely affected patients and recovery of hearing to near normal levels in those with<br />
mild to moderate losses. Steroids, cytoxan, and plasmapheresis compose the available therapeutic<br />
modalities. Hughes advocates high dose (prednisone 20 mg four times daily for 10 days then 10 mg<br />
every other day for 3-6 months) steroids as initial treatment. Patients are tapered slowly and restarted if<br />
symptoms recur. As initial therapy, McCabe recommends cytoxan (2mg/kg twice daily) combined with<br />
steroids (prednisone 30 mg every other day) for 3 weeks. If speech discrimination scores increase by<br />
20% or pure tone average improves by 15 dB, therapy is continued for 3 months. Cyclophosphamide is<br />
tapered first followed by steroids. If symptoms recur both drugs are restarted. Three month cycles are<br />
http://www.bcm.edu/oto/grand/4893.html (2 of 5) [5.11.2005 10:39:37]
http://www.bcm.edu/oto/grand/4893.html<br />
continued until patients can be weaned. No patient required more than 24 months of treatment in<br />
McCabe's study. Hughes advises plasmapheresis for those patients unresponsive to steroids and cytoxan<br />
after 6 to 8 weeks at the above stated doses. Plasmapheresis theoretically removes unwanted humoral and<br />
cellular elements. Treatments are given three times weekly for 2 weeks followed by once weekly for 4<br />
additional weeks.<br />
In summary, otolaryngologists need a high index of suspicion for autoimmune etiologies in patients with<br />
sensorineural hearing loss. Ophthalmologic, neurologic and rheumatologic consultations are useful in<br />
ruling out systemic vasculitic diseases. Steroids and cyclophosphamide remain the cornerstones of<br />
treatment in autoimmune inner ear disease, with reservation of plasmapheresis for refractory cases. If<br />
caught early, and with aggressive medical management, hearing stabilization and possible improvement<br />
are feasible.<br />
Case Presentation<br />
A 53-year-old white woman was first seen in November 1991 by a private MD, for sore throat, otalgia,<br />
scleritis, and temporal headaches. ANA, RF, RPR, and VDRL were all negative at that time. Her ESR<br />
was mildly elevated to 56. Magnetic resonance imaging of the head and neck was read as normal. She<br />
was treated unsuccessfully for occipital nerve impingement with local steroid injection. Systemic steroids<br />
relieved all symptoms until attempted taper when the headaches returned. In December 1991 she was<br />
admitted to the Neurology service at The Methodist Hospital with a diagnosis of temporal artery<br />
headaches. Further past medical history revealed an episode of temporal headache and pleuritic chest<br />
pain 6 months prior to her workup in Beaumont. Neurological and ophthalmologic evaluations revealed<br />
no specific anomalies. Lumbar puncture and temporal artery biopsy were without pathological change.<br />
VDRL was nonreactive. RF, ANA, and HIV testing were all negative. She had improvement of her<br />
headaches with systemic steroids. She was readmitted to Hospital in January 1992 with new onset<br />
nausea, vomiting, and sudden hearing loss in her left ear. ESR on admission was 37, urinalysis clear, and<br />
blood hematologic assessment showed a very mild iron deficiency anemia. C3, C4, RPR, FTA:ABS,<br />
SSA, SSB, RF, ANA, and antineutrophil cytoplasmic antibody were all within normal values. ACE<br />
inhibitor level was 8.4 (1.8 to 6.2). Serum protein electrophoresis was consistent with an acute phase<br />
response to inflammation. Chest x-ray was normal. Repeat MRI was remarkable only for left middle ear<br />
inflammation. Gallium scan showed increased uptake in the auricular region. Electronystagmography<br />
was consistent with a left peripheral (nerve or end organ) deficit. Lip biopsy was negative for<br />
inflammatory changes. Mastoid and middle ear biopsies obtained after complete mastoidectomy showed<br />
no pathologic abnormality. She has been managed with long-term steroid therapy with good control of<br />
her vestibular symptoms.<br />
http://www.bcm.edu/oto/grand/4893.html (3 of 5) [5.11.2005 10:39:37]
http://www.bcm.edu/oto/grand/4893.html<br />
Bibliography<br />
Arnold W, Pfaltz R, Altermatt H-J. Evidence of serum antibodies against inner ear tissues in the blood of patients with<br />
certain sensorineural hearing disorders. Acta Otolaryngol 1985;99:437-444.<br />
Bauwens LJJM, Veldman JE, Huizing EG. Progress in temporal bone histopathology. III. An improved technique for<br />
immunohistochemical investigation of the adult human inner ear. Acta Otolaryngol Suppl 1990;470:34-39.<br />
Berlinger NT. Immunobiology. In: Paparella MM, Shumrick DA, Gluckman JL, Meyerhoff WL, editors. Otolaryngology.<br />
Volume I. Basic sciences and related principles. 3rd edition. Philadelphia: WB Saunders, 1991:725-737.<br />
Harris JP. Autoimmunity of the inner ear. Am J Otol 1989;10:193-195.<br />
Harris JP. Immunology of the inner ear: evidence of local antibody production. Ann Otol Rhinol Laryngol 1984;93:157-<br />
162.<br />
Harris JP. Immunology of the inner ear: response of the inner ear to antigen challenge. Otolaryngol Head Neck Surg<br />
1983;91:18-23.<br />
Hughes GB, Barna BP, Kinney SE, Calabrese LH, Nalepa NJ. Clinical diagnosis of immune inner-ear disease.<br />
Laryngoscope 1988;98:251-253.<br />
Hughes GB, Barna BP, Kinney SE, Calabrese LH, Nalepa NL. Predictive value of laboratory tests in "autoimmune" inner<br />
ear disease: preliminary report. Laryngoscope 1986;96:502-505.<br />
Hughes GB, Kinney SE, Barna BP, Calabrese LH. Practical versus theoretical management of autoimmune inner ear<br />
disease. Laryngoscope 1984;94:758-767.<br />
Kanzaki J, O-Uchi T. Circulating immune complexes in steroid-responsive sensorineural hearing loss and the long-term<br />
observation. Acta Otolaryngol Suppl 1983;393:77-84.<br />
McCabe BF. Autoimmune inner ear disease: therapy. Am J Otol 1989;10:196-197.<br />
]McCabe BF. Autoimmune sensorineural hearing loss. Ann Otol 1979;88:585-589.<br />
McCabe BF, McCormick KJ. Tests for autoimmune disease in otology. Am J Otol 1984;5:447-449.<br />
Mogi G, Lim DJ, Watanabe N. Immunologic study on the inner ear. Arch Otolaryngol 1982;108:270-275.<br />
Mogi G, Maeda S, Watanabe N. The development of mucosal immunity in guinea pig middle ears. Internatl J Pediatr<br />
Otorhinolaryngol 1980;1:331-349.<br />
Musiek FE, Morgan GJ. The use of central auditory tests in a case of vasculitis. Ear Hear 1981;2:100-102.<br />
Plester D, Soliman AM. Autoimmune hearing loss. Am J Otol 1989;10:188-192.<br />
http://www.bcm.edu/oto/grand/4893.html (4 of 5) [5.11.2005 10:39:37]
http://www.bcm.edu/oto/grand/4893.html<br />
Quick CA. Antigenic causes of hearing loss. Otolaryngol Clin North Am 1975;8:385-394.<br />
Rask-Andersen H, Stahle J. Immunodefence of the inner ear? Lymphocyte-macrophage interaction in the endolymphatic<br />
sac. Acta Otolaryngol 1980;89:283-294.<br />
Ryan AF, Cleveland PH, Hartman MT, Catanzaro A. Humoral and cell-mediated immunity in peripheral blood following<br />
introduction of antigen into the middle ear. Ann Otol 1982;91:70-75.<br />
Stephens SDG, Luxon L, Hinchcliffe R. immunological disorders and auditory lesions. Audiology 1982;21:128-148.<br />
Veldman JE, Cochlear and retrocochlear immune-mediated inner ear disorders. Pathogenetic mechanisms and diagnostic<br />
tools. Ann Otol Rhinol Laryngol 1986;95:535-540.<br />
Veldman JE. The immune system in hearing disorders. Acta Otolaryngol Supple 1988;458:67-75.<br />
Veldman JE. Immunology of hearing: experiments of nature. Am J Otol 1989;10:183-187.<br />
Veldman JE, Roord JJ, O'Connor AF, Shea JJ. Autoimmunity and inner ear disorders: an immune-complex mediated<br />
sensorineural hearing loss. Laryngoscope 1984;94:501-507.<br />
Yoo TJ, Stuart JM, Kang AH, Townes AS, Tomoda K, Dixit S. Type Ii collagen autoimmunity in otosclerosis and<br />
Meniere's disease. Science 1982;217:1153-1155.<br />
Yoo TJ, Tomoda K, Stuart JM, Cremer MA, Townes AS, Kang AH. Type II collagen-induced autoimmune sensorineural<br />
hearing loss and vestibular dysfunction in rats. Ann Otol Rhinol Laryngol 1983;92:267-271.<br />
Yoo TJ, Tomoda K, Stuart JM, Kang AH, Townes AS. Type II collagen-induced autoimmune otospongiosis. A<br />
preliminary report. Ann Otol Rhinol Laryngol 1983;92:103-108.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/4893.html (5 of 5) [5.11.2005 10:39:37]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by<br />
doctors and other health care professionals. These documents were prepared by<br />
resident physicians for presentation and discussion at a conference held at The Baylor<br />
College of Medicine in Houston, Texas. No guarantees are made with respect to<br />
accuracy or timeliness of this material. This material should not be used as a basis for<br />
treatment decisions, and is not a substitute for professional consultation and/or peerreviewed<br />
medical literature.<br />
BAROTRAUMA OF THE MIDDLE AND INNER EAR<br />
March 23, 1995<br />
Willard C. Harrill, M.D.<br />
The most common causes of barotrauma today are from the use of the Self-Contained<br />
Underwater Breathing Apparatus (i.e. SCUBA gear), commercial air travel, and from<br />
hyperbaric oxygen chambers. In fact, hyperbaric oxygen therapy has been found to<br />
produce over a 50% incidence of barotrauma. Well over 50% of the medical problems<br />
that are related to barotrauma are referred to an Otolaryngologist. Over 90% of these<br />
complaints involve the ear.<br />
The noncompressible middle ear cavity makes the ear susceptible to damage from these<br />
ambient pressure changes. Middle ear pressure is governed by a law of physics known<br />
as Boyle's Law, which states that at a constant temperature, the volume of a body of gas<br />
http://www.bcm.edu/oto/grand/32395.html (1 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
is inversely related to the pressure to which it is subjected. Applying this law to diving,<br />
demonstrates that if a diver descends 33 feet (or the equivalent of 1 atmosphere of<br />
pressure), the ambient pressure will double from 1 atmosphere to 2 atmospheres. This<br />
will cause the volume of gas to be cut in half in the middle ear, resulting in a 50%<br />
increase in negative middle ear pressure if the eustachian tube is closed. The first 33 feet<br />
of descent represents the largest change in the volume of the middle ear while diving or<br />
during hyperbaric decompression. A diver must dive to greater than 150 feet in depth to<br />
equal the total volume change produced during the first 33 feet. This explains why the<br />
majority of otologic diving and hyperbaric injuries occur during shallow dives and not<br />
during deep water dives as one might expect. In fact, MEBT and IEBT have been<br />
reported to occur in as little as 8 ft of water.<br />
The pressure experienced during air travel is closely regulated by artificial means<br />
through the use of pressurized cabins. Commercial air lines maintain a constant pressure<br />
differential in the cabin of 8.5 psi above the changing ambient pressure outside the<br />
plane. At an altitude of 18,000 feet above sea level, a person in an unpressurized cabin<br />
would equilibrate the middle ear to an ambient pressure of 1/2 an atmosphere.<br />
Regulating cabin pressure at 8.5 psi above the changing ambient pressures, a passenger<br />
will experience a cabin pressure equal to that at sea level (i.e., 1 Atmosphere) while<br />
flying at an altitude of 16,000 feet and will require minimal middle ear equilibration. At<br />
40,000 feet, the passenger will have a cabin pressure equal to 7000 feet above sea level.<br />
This pressurization is beneficial when a plane descends from a cruising altitude of<br />
40,000 feet to land at sea level. The ambient pressure change experienced by the<br />
passenger is decreased by 2/3 since the passenger will be actually experiencing a<br />
descent equivalent to a 7000 foot descent. Although pressurized air travel has reduced<br />
the potential risks of barotrauma, it is important to keep in mind that only a pressure<br />
differential of 80mm Hg is required to close the eustachian tube in normal individuals.<br />
A descent from 37,000 ft to 27,000 feet cruising altitude will result in a cabin gauge<br />
pressure change equal to 80mm hg, resulting in difficulty with clearing the middle ear.<br />
In order to fully understand the effects that Boyle's Law has on Eustachian tube<br />
function, we will briefly review the normal anatomy and function of the eustachian tube.<br />
In the resting state, the eustachian tube is closed. A positive pressure within the<br />
nasopharynx, or a contraction of the tensor veli palatini, levator palatini, or the<br />
salpingopharyngeus is required to open the eustachian tube when middle ear pressure<br />
equalization is attempted. There are three common maneuvers which can be used to aid<br />
in middle ear pressure equalization. These are the Valsalva maneuver, the Frenzel<br />
maneuver, and the Toynbee maneuver. The Valsalva maneuver opens the eustachian<br />
tube by increasing the nasopharyngeal pressure above the middle ear pressure as a result<br />
of closing the naries and glottis while increasing intrathoracic and intra-abdominal<br />
pressure. This maneuver is the most common cause of barotrauma to the ear if<br />
performed too forcefully. The Frenzel maneuver is performed with a low pressure<br />
valsalva while contracting the muscles of the pharynx. This forces air into the<br />
http://www.bcm.edu/oto/grand/32395.html (2 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
eustachian tube without increasing the total intrathoracic pressure. Finally the Toynbee<br />
maneuver involves swallowing while pinching the nose, thus creating a negative<br />
nasopharyngeal pressure which can force the eustachian tube open. By far, the Frenzel<br />
and Toynbee maneuvers are the safest to perform during eustachian tube dysfunction as<br />
neither have been associated with barotrauma. .<br />
To date, there is no readily available test to identify patients with eustachian tube<br />
dysfunction other than a history of difficulty with clearing the middle ear. Factors which<br />
would lead to a decrease in eustachian tube function include recent upper respiratory<br />
infections, uncontrolled nasal allergy, nasal polyposis, and deviated nasal septum.<br />
The differential diagnosis of the disorders related to barotrauma are damage to the<br />
middle and inner ear, inner ear decompression sickness, and alternobaric vertigo.<br />
Middle ear barotrauma, also known as aerotitis media, is due to an inability to<br />
equilibrate to ambient pressure changes. The etiology can be located either in the middle<br />
ear or external ear. This process also occurs most commonly during the descent as a<br />
forced valsalva is attempted, increasing the middle ear pressure and allowing for<br />
damage of the tympanic membrane to occur. This process can also occur during ascent<br />
if eustachian tube dysfunction causes air trapping, otherwise known as "reverse<br />
Squeeze."<br />
The external ear canal can also be a source of middle ear barotrauma if a closed space is<br />
created between the outer rim of the concha bowl and the tympanic membrane. The<br />
closed space may be due to either a cerumen impaction, ear plugs, or external otitis. As<br />
a diver descends, ambient pressure will increase, causing a net negative pressure<br />
gradient between the external ear canal obstruction and the tympanic membrane. The<br />
obstructing plug is then forced deeper into the external ear, resulting in a tympanic<br />
hemorrhage or perforation. The patient typically experiences extreme pain as the<br />
descent phase of the dive begins, despite an ability to clear the middle ear.<br />
Edmonds et al from the Australian Diving Medical Center, devised a grading system for<br />
middle ear barotrauma. The grading scale is from zero to five. Grade 0 is when a patient<br />
experiences symptoms of middle ear barotrauma and no physical findings are present.<br />
Grade I is when the presence of tympanic membrane injection can be seen. Grade II has<br />
injection as well as hemorrhage within the tympanic membrane. Grade III includes<br />
gross hemorrhage and Grade IV includes gross hemotympanum. Grade V includes the<br />
presence of a tympanic perforation.<br />
There are three common forms of IEBT: Cochlear Damage resulting in intracochlear<br />
and intralabyrinthine hemorrhage, perilymphatic fistula formation, and IEDS secondary<br />
to the formation of gas bubbles beneath the round window.<br />
http://www.bcm.edu/oto/grand/32395.html (3 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
IEBT usually occurs with MEBT, although the absence of MEBT cannot exclude the<br />
presence of IEBT. The symptoms of sensory neural hearing loss, vertigo, and or tinnitus<br />
should indicate the presence of possible IEBT. The etiology of IEBT has been proposed<br />
by Goodhill et al to be secondary to implosive or explosive forces within the cochlea.<br />
Goodhill proposed that forces exerted on the cochlea during a forced Valsalva have<br />
different effects depending on the patency of the eustachian tube. When the eustachian<br />
tube is forced open suddenly, an acute rise in middle ear pressure will result causing an<br />
inward bulge of the round window and an outward bulge of the stapes foot plate. If the<br />
force is strong enough, implosion of the round window and a secondary outward pull on<br />
the stapes footplate may occur.<br />
If the eustachian tube is blocked, a valsalva maneuver will cause an elevation of CSF<br />
pressure which will be transmitted through a patent cochlear aqueduct or internal<br />
auditory canal causing a rise in the intracochlear pressure. If the difference between the<br />
perilymphatic space is sufficiently greater than the middle ear pressure, an explosive<br />
rupture of the round or oval window ligament will occur.<br />
Both the implosive and explosive forces generated by a force valsalva are theorized to<br />
cause a perilymphatic fistulae or dislocation and rupture of Reissner's membrane, as<br />
well as the basilar membrane, the saccule, the utricle, or the semicircular canals.<br />
Antonelli and Paparella have studied the temporal bone pathology in scuba diving<br />
deaths and confirmed the presence of these pathologic findings. Simmons et al have<br />
demonstrated through experimental models that pressure differentials of less than 2 cm<br />
of water can cause labyrinthine ruptures.<br />
IEBT secondary to cochlear damage will present with nonfluctuating high frequency<br />
sensorineural or mixed hearing loss with or without tinnitus or vertigo. There is<br />
typically no progression of symptoms. The treatment of IEBT secondary to damage to<br />
the membranous labyrinth and cochlea includes bed rest with head elevation, the use of<br />
vasodilators, steroids, histamine, and carbogen, in an effort to decrease inflammatory<br />
changes and increase the delivery of oxygen. Parell et al have shown that if proper<br />
precautions are taken to maintain proper eustachian tube function, no further<br />
deterioration takes place in hearing if a patient returns to diving after experiencing<br />
cochlear IEBT.<br />
IEBT secondary to a perilymphatic fistulae typically presents with fluctuating<br />
sensorineural or mixed hearing loss, as well as vertigo exacerbated with positional<br />
changes, and a sense of constant disequilibrium. On physical exam, a positive<br />
Hennebert's sign (the presence of nystagmus when positive and negative pressure is<br />
applied to the EAC in the presence of an intact tympanic membrane) has been cited by<br />
Thompson and Kohut as a strong positive indicator of a perilymphatic fistula in patients<br />
with or without the presence of hearing loss. Healy et al have indicated that a positive<br />
http://www.bcm.edu/oto/grand/32395.html (4 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Romberg sign and the presence of positional nystagmus are consistent with the presence<br />
of a perilymphatic fistula.<br />
When present, the most common location of the perilymphatic fistula has been<br />
demonstrated by Goodhill et al to be at the anterior rim of the oval window in the area<br />
of the fistula ante fenestram, which is one of the weakest areas of the otic capsule. The<br />
management of patients suspected of having a perilymphatic fistula includes bed rest<br />
with head elevation and avoidance of increased intracranial pressure for a variable<br />
period of days, with intermittent regular audiograms.<br />
The length of time a patient should be observed before an exploratory tympanotomy is<br />
performed is very controversial. In a study by Paparella et al, it was shown that in<br />
chinchillas suffering a traumatic round window perforation, all perforations had<br />
partially healed after 3 days, and all were completely healed after 9 days. The results of<br />
this study form the basis for conservative management of perilymphatic fistulas.<br />
Simmons et al recommend that if hearing loss or vestibular symptoms are progressive,<br />
or if after 10 days any vestibular symptoms remain, an exploratory tympanotomy should<br />
be performed. Parell and Becker also advocate this 10 day observation period. Singleton<br />
and Kohut are proponents of a 5 day observation period. Goodhill et al suggest a 48<br />
hour observation period. Pullen et al suggest that the shape of the audiogram should<br />
indicate if an exploratory tympanotomy should be performed. He advocates immediate<br />
surgery if an audiogram demonstrates a flat shaped total or near total SNHL in the<br />
presence of a history of diving or air travel within the past 72 hours. However, he states<br />
that if the hearing loss is limited to only the high frequencies, a down-sloping<br />
audiogram, a closure of a perilymphatic fistula has not been shown to improve hearing<br />
and, thus, surgery is contraindicated unless vertigo is present.<br />
Inner ear decompression sickness (IEDS) is a form of nontraumatic cochlear damage<br />
and is the result of gas bubble formations within the inner ear. It is commonly seen after<br />
dives to extreme depths using a Helium oxygen mixture as a substitute for nitrogen<br />
oxygen mixture, in order to minimize the narcotic effects of nitrogen. IEDS occurs as a<br />
diver returns to the surface and, in an attempt to accelerate helium elimination from the<br />
tissues, changes from an oxygen-helium mixture to an air mixture. McCormick et al<br />
demonstrated that if rapid decompression occurs, inert gas bubbles of helium will form<br />
within the microvessels and otic fluids, causing a blockage of the microcirculation and<br />
resulting ischemia of the stria vascularis, spiral ligament and semicircular canals. A<br />
hypercoagulable state is produced secondary to the activation of factor XII, resulting in<br />
further vascular occlusion. As previously stated, the treatment of this disorder is<br />
immediate recompression to approximately three atmospheres deeper than the depth at<br />
which the symptoms began to occur. Farmer et al have demonstrated a near total return<br />
to baseline hearing if recompression is initiated immediately. Proper diagnosis is<br />
crucial, as the hyperbaric chamber recompression will aggravate inner ear damage due<br />
to perilymphatic fistulas and cochlear barotrauma.<br />
http://www.bcm.edu/oto/grand/32395.html (5 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
The differentiation between IEDS and IEBT can be made based on the following<br />
criteria.<br />
●<br />
●<br />
●<br />
●<br />
Dive profile:<br />
1. IEDS is rare in shallow water (only 3 cases reported in less than 100 feet<br />
of water),<br />
2. diving to a depth that is near the limits of the nodecompression zone and<br />
not undergoing decompression,<br />
3. using a HE-02 gas mixture (IEDS),<br />
4. h/o rapid ascent. (IEBT associated with rapid descent);<br />
Time of symptom onset:<br />
1. During descent (IEBT),<br />
2. During ascent (IEDS),<br />
3. Shortly after decompression (IEDS);<br />
Associated symptoms:<br />
1. the presence of decompression sickness (only 6 cases in literature of IEDS<br />
without systemic decompression sickness),<br />
2. h/o difficulties in clearing the ear (IEBT),<br />
3. h/o nasal or sinus problems (IEBT);<br />
Physical findings:<br />
1. MEB (IEBT),<br />
2. Central neurologic signs (IEDS).<br />
The last disorder related to barotrauma is the phenomenon known as alternobaric<br />
vertigo. This is a syndrome first described by Lundgren in 1965 as vertigo occurring<br />
during ascent due to unequal pressure in the right and left middle ear. The duration of<br />
the vertigo is usually from a few seconds to minutes and is not associated with hearing<br />
loss. In his review of 2053 Swedish divers, Lundgren found a 16.7% incidence of<br />
alternobaric vertigo. A review of 526 Australian naval divers by Bayliss cited a 0.4%<br />
incidence. Although this process is self-limiting, a diver experiencing alternobaric<br />
vertigo while attempting a valsalva maneuver at the surface, should not undergo a dive<br />
or air travel.<br />
As people become more active in both air travel and recreational water sports, education<br />
regarding the hazards of extreme middle ear pressure changes should be expanded.<br />
Patients who are more susceptible to aural barotrauma, either due to lifestyle, upper<br />
respiratory infections, or after ear surgery, should take extra precautions to guard against<br />
eustachian tube function during air travel or underwater sports or simply avoid these<br />
activities when the risks of barotrauma are the greatest.<br />
http://www.bcm.edu/oto/grand/32395.html (6 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Case Presentation<br />
A 36-year-old man experienced difficulty clearing his left ear while snorkeling to a<br />
depth of 35 feet in Cozumel, Mexico. After attempting a forced valsalva maneuver, the<br />
patient reported sudden hearing loss and tinnitus in his left ear that continued to persist.<br />
He denied any sensation of dysequilibrium or vertigo. A history of a previous high<br />
frequency SNHL was noted before the diving incident. No other past history of middle<br />
or inner ear disorders was noted. No history of a recent URI, nasal obstruction, or recent<br />
eustachian tube dysfunction was reported. Physical exam demonstrated a Grade III<br />
tympanic membrane hemorrhage with an intact drum. The right ear canal, tympanic<br />
membrane, and middle ear appeared normal. The Weber exam lateralized to the right<br />
ear and ear conduction was greater than bone conduction in the left ear. No evidence of<br />
spontaneous nystagmus was noted. Hennebert's sign and Rhomberg sign were negative.<br />
Fistula test was negative. An audiogram was obtained demonstrating an 80 dB SNHL on<br />
the left and no change in the high frequency loss on the right. An MRI scan<br />
demonstrated no abnormalities. The patient was placed on steroids and antibiotics.<br />
Carbogen therapy was initiated and two stellate ganglion blocks were performed. A<br />
repeat audiogram was obtained one week later that demonstrated improvement in the<br />
left SNHL. The patient continued to report no dizziness. The patient was advised to<br />
refrain from exertion for 1 month and schedule a follow-up audiogram in six months.<br />
Bibliography<br />
Anson B, Caldwell DW, Bast TH. The fissula ante fenestram of the human otic capsule. Ann Otol<br />
Rhinol Laryngol 1948;57:103-128.<br />
Antonelli PJ, Parell GJ, Becker GD, Paparella MM. Temporal bone pathology in scuba diving deaths.<br />
Otolaryngol Head Neck Surg 1993;109:514-521.<br />
Bayliss GJA. Aural barotrauma in naval divers. Arch Otolaryngol 1968;88:141-147.<br />
Becker GD, Parell GJ. Otolaryngologic aspects of scuba diving. Otolaryngol Head Neck Surg<br />
1979;87:569-571.<br />
Caparosa RJ, Shamblin JD, Junter CW. Stapedectomy-fistula repair. Laryngoscope 1977;87:1373-<br />
1377.<br />
Caruso VG, Winkelmann PE, Correia MJ, et al. Otologic and otoneurologic injures in divers: clinical<br />
studies on nine commercial and two sport divers. Laryngoscope 1977;87:508-512.<br />
http://www.bcm.edu/oto/grand/32395.html (7 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Eichel BS, Landes BS. Sensorineural hearing loss caused by skin diving. Arch Otolaryngol<br />
1970;92:315-319.<br />
Farmer JC, Thomas WG, Youngblood DB, et al. Inner ear decompression sickness. Laryngoscope<br />
1976;86:1315-1327.<br />
Farmer JC. Diving injuries to the inner ear. Ann Otol Rhinol Laryngol 1977;86:1-20.<br />
Freeman P, Edmonds C. Inner ear barotrauma. Arch Otolaryngol 1972;95:556-563.<br />
Goodhill V. Sudden deafness and round window rupture. Laryngoscope 1971;81:1462-1474.<br />
Goodhill V. Leaking labyrinth lesions, deafness, tinnitus and dizziness. Ann Otol Rhinol Laryngol<br />
1981;90:99-106.<br />
Goodhill V. The conductive loss phenomenon in post stapedectomy perilymphatic fistulas.<br />
Laryngoscope 1967;77:1179-1190.<br />
Green SM, Rothrock SG, Green EA. Tympanometric evaluation of middle ear barotrauma during<br />
recreational scuba diving. Int J Sports Med 1993;14:411-415.<br />
Head PW. Decompression injuries in the temporal bone. J Laryngol Otol 1980;94:111-116.<br />
Healy GB, Friedman J, Strong MS. Vestibular and auditory findings of perilymphatic fistulas: a review<br />
of 40 cases. Trans Am Acad Ophthalmol Otolaryngol 1976;82:44-49.<br />
House HP. The fistula problem in otosclerosis surgery. Laryngoscope 1967;77:1410-1426.<br />
Igarashi Y, Watanabe Y, Mizukoshi K. Middle ear barotrauma associated with hyperbaric oxygen<br />
treatment. Acta Otolaryngol Suppl 1993;504:143-145.<br />
Love JT Jr, Caruso VG. Civilian air travel and the otolaryngologist. Laryngoscope 1978;88:1732-1742.<br />
McCormick JG, Philbrick T, Holland W, Harrill JA. Diving induced sensorineural deafness:<br />
prophylactic use of heparin and preliminary histopathology results. Laryngoscope 1973;63:1483-1501.<br />
McNicoll WD. Eustachian tube dysfunction in submariners and divers. Arch Otolaryngol<br />
1982;108:279-283.<br />
Molvaer OI, Natrud E. Ear damage due to diving. Acta Otolaryngol Suppl 1979;360:187-189.<br />
Money KE, Buckingham IP, Calder IM, Johnson WH, King KD, Landolf JP, et al. Damage to the<br />
middle ear and the inner ear in underwater divers. Undersea Biomed Res 1985;12:77-84.<br />
Neblett LM. Otolaryngology and sport scuba diving: update and guidelines. Ann Otol Rhinol Laryngol<br />
http://www.bcm.edu/oto/grand/32395.html (8 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
1985;94:1-12.<br />
Novotny GM. Cochlear bends. J Otolaryngol 1980;9:395-398.<br />
Parell GJ, Becher GD. Conservative management of inner ear barotrauma resulting from scuba diving.<br />
Otolaryngol Head Neck Surg 1985;93:393-397.<br />
Parell GJ, Becker GD. Inner ear barotrauma in scuba divers. A long-term follow-up after continued<br />
diving. Arch Otolaryngol Head Neck Surg 1993;119:455-457.<br />
Pullen FW 2d. Perilymphatic fistula induced by barotrauma. Am J Otol 1992;13:270-272.<br />
Reuter SH. Underwater medicine: otolaryngologic considerations of the skin and scuba diver. In:<br />
Paparella MM, Shumrick DA, editors. Otolaryngology. Volume IV: Plastic and Reconstructive<br />
Surgery and Interrelated Disciplines, 3rd ed. Philadelphia: Saunders, 1991:3231-3257.<br />
Schuchman G, Joachims HZ. Tympanometric assessment of eustachian tube function of divers. Ear<br />
Hear 1985;6:325-328.<br />
Seltzer S, McCabe BF. Perilymph fistula: the Iowa experience. Laryngoscope 1986;94:37-46.<br />
Shupak A, Sharoni Z, Ostfeld E, Doweck I. Pressure chamber tympanometry in diving candidates.<br />
Laryngoscope 1991;101:173-179.<br />
Simmons FB. The double membrane break syndrome in sudden hearing loss. Laryngoscope<br />
1979;89:59-66.<br />
Simmons FB. Theory of membrane breaks in the sudden hearing loss. Arch Otolaryngol 1968;88:41-<br />
48.<br />
Singleton GT, Karlan MS, Posh KN, Bock DG. Perilymph fistulas: diagnostic criteria and therapy.<br />
Ann Otol Rhinol Laryngol 1978;87:797-803.<br />
Talmi YP, Finkelstein Y, Zohar Y. Barotrauma-induced hearing loss. Scand Audiol 1991;20:1-9.<br />
Talmi YP, Finkelstein Y, Zohar Y. Decompression sickness induced hearing loss. A review. audiol<br />
1991;20:25-28.<br />
Thompson JN, Kohut RI. Perilymph fistulae: variability of symptoms and results of surgery.<br />
Otolaryngol Head Neck Surg 1979;87:898-903.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
http://www.bcm.edu/oto/grand/32395.html (9 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/32395.html (10 of 10) [5.11.2005 10:39:56]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by<br />
doctors and other health care professionals. These documents were prepared by<br />
resident physicians for presentation and discussion at a conference held at The<br />
Baylor College of Medicine in Houston, Texas. No guarantees are made with<br />
respect to accuracy or timeliness of this material. This material should not be used<br />
as a basis for treatment decisions, and is not a substitute for professional<br />
consultation and/or peer-reviewed medical literature.<br />
BELL'S PALSY<br />
July 20, 1995<br />
S. Mark Overholt, M.D.<br />
Bell's palsy is synonymous with idiopathic facial paralysis. It is the most common<br />
cause of an acute facial paralysis, and accounts for 75 to 80 percent of all cases.<br />
The annual incidence is 20 to 30 per 100,000. It's name is derived from Sir Charles<br />
Bell, a surgeon and accomplished artist from Edinburgh, Scotland who lived from<br />
1774 to 1842. In 1821, he published his anatomic diagrams of the course of the<br />
facial nerve and its innervation of the facial musculature.<br />
Early treatment strategies for Bell's palsy were primarily surgical. In the 1930's<br />
Balance and Duel described decompression of the distal one centimeter of the<br />
facial nerve at the stylomastoid foramen. Tumarkin felt that decompression of the<br />
http://www.bcm.edu/oto/grand/72095.html (1 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
stylomastoid artery was necessary to adequately treat Bell's palsy. By the 1940's the<br />
main treatment modality was facial nerve decompression in the mastoid segments.<br />
In the 1960's electrical testing allowed refinement of the indications for surgery.<br />
Jongkees proposed decompression of the nerve when a difference of greater than<br />
3.5 mAmps was noted by nerve excitability testing when comparing the unaffected<br />
to the affected side. Alford further delineated indications and discussed the<br />
importance of associated symptoms, the cause of the paralysis, and the experience<br />
of the surgeon in deciding to proceed with decompression. Important surgical<br />
advances were also developed in the 1960's. These include the middle cranial fossa<br />
approach which was initially described by House in 1961, and the total facial nerve<br />
decompression described by Pulec in 1966. The 1970's was a transition period for<br />
the theoretical treatment approach to a patient with Bell's palsy. With the<br />
refinement of electrical testing and the use of steroids, a trend had begun away<br />
from surgery. Adour was one of the first neurotologists to state that surgery might<br />
not be beneficial. In 1985 May discussed the failure of transmastoid decompression<br />
to improve outcome. However, Fisch and Esslen found good results after combined<br />
middle cranial fossa and mastoid decompression of the facial nerve in 11 out of 12<br />
patients with Bell's Palsy. The role of surgery remains controversial and indication<br />
will be discussed later. By the 1980's and 1990's the treatment had changed to<br />
being primarily medical. Coker additionally demonstrated that the electrical<br />
evidence of a degenerating facial nerve on electroneuronography was reliable and<br />
correlated with histologic evidence of neuronal degeneration.<br />
Several theories exist regarding the cause of Bell's palsy. Most favor a viral inciting<br />
event that triggers edema and inflammation in the nerve leading to infarction and<br />
nerve damage. Many viruses have been implicated but there is mounting evidence<br />
supporting the herpes simplex virus serotype 1 as the etiologic culprit.<br />
Mechanical entrapment in the fallopian canal is the cause of the ischemic injury to<br />
the facial nerve. In 1981 Fisch described the "physiologic bottleneck" at the meatal<br />
foramen. In his comparative study of adult temporal bone specimens, the average<br />
diameter of the fallopian canal was found to be 1.02 to 1.53 mm, except at the<br />
meatal foramen where it was 0.68 mm. Histologic examinations have demonstrated<br />
hemorrhage and edema in the nerve at this site. Additionally, intraoperative<br />
stimulation blockage has been documented to occur in this narrow segment with<br />
intact stimulation distally.<br />
Nerve injury is classified according to the schema of Sunderland. This system<br />
describes progressively worsening injury to the nerve starting with a neuropraxic<br />
injury and ending in neuronotmesis or nerve transection. Five grades of injury are<br />
described. The grade of the injury correlates to the final functional recovery of the<br />
facial nerve. Clinically facial nerve injury is classified using the House-Brackmann<br />
system. Grade I is normal function. Grade II shows slight weakness but no<br />
http://www.bcm.edu/oto/grand/72095.html (2 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
synkinesis. Grade III shows obvious weakness with some mass movement. Grade<br />
IV has inability to elevate the brow, significant synkinesis, and obvious weakness.<br />
Grade V has barely perceptible motion, and grade VI has no movement.<br />
The differential diagnosis for facial paralysis is broad and must include<br />
inflammatory causes such as herpes zoster oticus or sarcoidosis, traumatic injuries<br />
such as temporal bone fractures, mastoiditis, cholesteatomas, the Melkersson-<br />
Rosenthal syndrome, and primary or metastatic neoplasms of the temporal bone.<br />
By far though, idiopathic facial paralysis predominates. It accounts for almost 80 %<br />
of all cases of facial palsy.<br />
The epidemiology of Bell's palsy is best described in Peitersen's monograph from<br />
the Copenhagen facial nerve study. In over 1000 patients he found there to be no<br />
sex predilection. A broad age range was noted, typically from 15 to 60 years old.<br />
Rarely did he note bell's palsy in patients less than 15 years of age. Patients<br />
presented with a classic constellation of symptoms. There is usually a prodrome of<br />
periauricular pain that heralds the onset of facial palsy within 24 hours. The palsy<br />
is unilateral and involves all muscle groups. In order to make the diagnosis of Bell's<br />
palsy the evaluating clinician must exclude the following: concurrent CNS disease,<br />
otologic infection, auricular blebs suggesting the Ramsey-Hunt syndrome, parotid<br />
masses, and an occult neoplasm such as a facial neuroma in a patients who has a<br />
recurrent palsy.<br />
There is no consensus regarding the work up of a patient with Bell's palsy. Most<br />
would include a routine basic audiogram in order to rule out an asymmetric hearing<br />
loss, which might suggest another process. Topognostic tests, which include the<br />
Schirmer's test of tearing, the salivary flow test popularized by May, and the<br />
acoustic reflex test are of historic interest only. While once felt to assist in<br />
localizing the nerve injury, we know now that the injury occurs at the meatal<br />
foramen. Additionally, they do not offer prognostically valuable information.<br />
Radiographic imaging is reserved for those who have no improvement in there<br />
palsy within 6 months and for those who a have recurrent palsy. The MRI is the<br />
best study to image the facial nerve. In patients with Bell's palsy gadolinium MRI<br />
enhancement of the perigeniculate region is prominent. However, as Schwaber<br />
pointed out in 1990, this enhancement does not correlate with outcome.<br />
Furthermore, Gribarski showed that 76% of normal subjects will show<br />
enhancement of the perigeniculate region with gadolinium.<br />
Electrodiagnostic test are reserved for patients with complete facial paralysis.<br />
Available tests include the nerve excitability test(NET), maximal stimulation<br />
test(MST), electroneuronography (ENog), and electromyography. The latter is<br />
http://www.bcm.edu/oto/grand/72095.html (3 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
appropriate when the paralysis has been present for several weeks. In the acute<br />
period the first three are most appropriate. NET and the MST are both performed<br />
using the Hilger stimulator. The first is a threshold test and the second a<br />
supramaximal stimulation test. A criticism of these two tests is that the grading of<br />
the response to the stimulus is subjective, and thus may not reliably predict<br />
denervation. However, Coker and Fordice demonstrated that a greater than 3.5<br />
mAmp difference side-to-side on NET correlated closely with objective ENog data<br />
showing greater than 90% degeneration of the nerve. May showed that in patients<br />
who did not have a response to the MST for 10 days, over 85% did not fully<br />
recover. Those who did have a response to MST within the first 10 days had<br />
excellent recovery. Enog is the most widely used test to evaluate an acute complete<br />
facial paralysis. It is an objective reliable test that compares the difference in the<br />
amplitude of the compound action potential of the unaffected to affected side of the<br />
face. Fisch and Esslen found that when the amplitude of the affected side is less<br />
than 10% of the unaffected side the prognosis is poor. Coker correlated the<br />
evidence of electrical degeneration with histologic evidence of nerve degeneration.<br />
Treatment of an acute facial paralysis is initially medical. The regimen currently<br />
used by most otologists is prednisone 1mg/kg/day tapered over a 10 day period.<br />
With the mounting evidence implicating the herpes virus, many additionally<br />
recommend acyclovir 800 mg three times a day for 10 days.<br />
Indications for surgery are controversial, but most neurotologists feel that electrical<br />
evidence of greater than 90% degeneration or a difference of 3.5mAmp from sideto-side<br />
is sufficient to proceed with a decompression. Surgery must be performed<br />
as early as possible. After 21 days there is probably no benefit. The decompressive<br />
surgery must focus on the meatal foramen. May found that transmastoid<br />
decompression alone did not improve outcome, whereas when combining<br />
transmastoid and middle cranial fossa decompression Fisch found good outcome in<br />
11 of 12 patients .<br />
Good prognostic variables include presentation with an incomplete palsy, onset o f<br />
return of facial function within three weeks, and age below 60 years. Peitersen<br />
found that 94% of patients who presented with an incomplete palsy progressed to<br />
full recovery. If return of facial function was within one week almost 90% fully<br />
recovered Return of function in the second and third weeks yielded full recovery in<br />
83% and 60% respectively. Overall, 85% of patients with Bell's palsy will recover<br />
to normal function.<br />
In conclusion, Bell's palsy is the most common cause of an acute facial palsy. It is<br />
unilateral and sudden in onset, often with a prodrome of auricular pain. After<br />
excluding other potential causes of a facial paralysis, treatment is with prednisone<br />
and acyclovir. Surgery is reserved for those who meet electrodiagnostic criteria or<br />
http://www.bcm.edu/oto/grand/72095.html (4 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
are worsening on medical treatment. Decompression must include the site of<br />
pathologic compression of the facial nerve, the meatal foramen. Finally, fortunately<br />
85% of patients with Bell's palsy have full return of facial function.<br />
Case Presentation<br />
A white female initially presented at the age of 29, with a 16-day history of a<br />
complete right-sided facial paralysis. Complicating this problem was the fact that<br />
she was also 34 weeks pregnant. No complaints of associated dizziness or changes<br />
in her hearing were reported, but she did note some facial dysesthesias in the<br />
distribution of the mandibular branch of the trigeminal nerve. There was no history<br />
of recurrent facial edema or a fissured tongue. Physical exam did not show any<br />
auricular blebs or parotid masses. An audiogram was normal with the exception of<br />
absent right-sided acoustic reflexes. Nerve excitability testing showed a good<br />
response at 3.0 milliamps on the unaffected side and no response at 7.0 milliamps<br />
on the right. Because of her pregnancy and late presentation she was not offered<br />
further treatment. Her recovery was incomplete. In May, she began to notice some<br />
unusual movements and spasms in her face. Final recovery left her with good<br />
symmetry at rest and excellent eye closure, but she had mild brow ptosis,<br />
synkinesis, and gustatory tearing. She was graded according to the House-<br />
Brackmann scale as a III out of VI. She subsequently did well with some<br />
intermittent dysesthesias of the right face until age 36 when she suffered an attack<br />
of Bell's Palsy on the left side of her face. She was treated with prednisone and<br />
acyclovir and eventually fully recovered. Approximately two years later she<br />
experienced two recurrences of her right-sided facial paralysis. Both episodes were<br />
treated with prednisone and acyclovir with recovery to her baseline grade III<br />
deficit. She is currently being followed by the neurotology service at The<br />
Methodist Hospital to monitor any further recurrence.<br />
Bibliography<br />
Abraham-Inpijn L, Oosting J, Hart AAM. Bell's palsy: factors affecting the prognosis in 200<br />
patients with reference to hypertension and diabetes mellitus. Clin Otolaryngol 1987;12:349-355.<br />
Adour KK. Medical management of idiopathic (Bell's) palsy. Proc R Soc Med 1973;66:554-556.<br />
Adour KK, Bell DN, Hilsinger RL Jr. Herpes simplex virus in idiopathic facial paralysis (Bell's<br />
palsy). JAMA 1975;233:527-530.<br />
http://www.bcm.edu/oto/grand/72095.html (5 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Adour KK, Byl FM, Hilsinger RL Jr, Kahn ZM, Sheldon MI. The true nature of Bell's palsy:<br />
analysis of 1000 consecutive patients. Laryngoscope 1978;88:787-801.<br />
Adour KK, Hissinger RL Jr., Callan EJ. Facial paralysis and Bell's palsy: a protocol for<br />
differential diagnosis. Am J Otol Suppl 1985:68-73.<br />
Adour KK, Sheldon MI, Kahn ZM. Maximal nerve excitability testing versus neuromyography:<br />
prognostic value in patients with facial paralysis. Laryngoscope 1980;90:1540-1547.<br />
Adour KK, Wingerd J. Idiopathic facial paralysis (Bell's palsy): factors affecting severity and<br />
outcome in 446 patients. Neurology 1974;24:1112-1116.<br />
Adour KK, Wingerd J, Bell DN, Manning JJ, Hurley JP. Prednisone treatment for idiopathic<br />
facial paralysis (Bell's palsy). N Engl J Med 1972;287:1268-1272.<br />
Alford BR. Electrodiagnostic studies in facial paralysis. Arch Otolaryngol 1967;85:259-264.<br />
Alford BR. Facial nerve grafting. Laryngoscope 1976;86:257-258.<br />
Alford BR, Ickey JR, Pratt FE. Management of facial paralysis. Tex Med 1966;62:56-60.<br />
Alford BR, Jerger JF, Coats AC, Peterson CR, Weber SC. Neurophysiology of facial nerve<br />
testing. Arch Otolaryngol 1973;97:214-219.<br />
Alford BR, Jerger JF, Coats AC, Peterson CR, Weber SC. Diagnostic tests of facial nerve<br />
function. Otolaryngol Clin North Am 1974;7:331-342.<br />
Alford BR, Sessions RB, Weber SC. Indications for surgical decompression of the facial nerve.<br />
Laryngoscope 1971;81;620-635.<br />
Alford BR, Weber SC, Sessions RB. Neurodiagnostic studies in facial paralysis. Ann Otol Rhinol<br />
Laryngol 1970;79:227-233.<br />
Austin, JR., Peskind SP, Austin SG, Rice DH. Idiopathic facial nerve paralysis: a randomized<br />
double blind controlled study of placebo versus prednisone. Laryngoscope 1993;103:1326-1333.<br />
Balkany T, Fradis M, Jafek BW, Rucker NC. Intrinsic vasculature of the labyrinthine segment of<br />
the facial nerve--implications for site of lesion in Bell's palsy. Otolaryngol Head Neck Surg<br />
1991;104:20-23.<br />
Brackmann DE. Bell's palsy: incidence, etiology, and results of medical treatment. Otolaryngol<br />
Clin North Am 1974;7:357-368.<br />
Brandt TW, Jenkins HA, Coker NJ. Facial paralysis as the initial presentation of an internal<br />
http://www.bcm.edu/oto/grand/72095.html (6 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
carotid artery aneurysm. Arch Otolaryngol Head Neck Surg 1986;112:198-202.<br />
Burgess RC, Michaels L, Bale JF Jr, Smith RJ. Polymerse chain reaction amplification of herpes<br />
simplex viral DNA from the geniculate ganglion of a patient with Bell's palsy. Ann Otol Rhinol<br />
Laryngol 1994;103:775-779.<br />
Cawthorne T, Haynes DR. Facial palsy. Br Med J 1956;2:1197-2000.<br />
Coker NJ. Facial electroneurography: analysis of techniques and correlation with degenerating<br />
motorneurons. Laryngoscope 1992;102:747-759.<br />
Coker NJ. Facial nerve disorders. Otolaryngol Head Neck Surg 1992;106:8-9.<br />
Coker NJ. Minutes of the annual meeting of the Facial Nerve Study Group September 1992. Am<br />
J Otol 1994;15:114-116.<br />
Coker NJ, Fordice JO, Moore S. Correlation of the nerve excitability test and electroneurography<br />
in acute facial paralysis. Am J Otol 1992;13:127-33.<br />
Coker NJ, Kendall KA, Jenkins HA, Alford BR. Traumatic intratemporal facial nerve injury:<br />
management rationale for preservation of function. Otolaryngol Head Neck Surg 1987;97:262-<br />
269.<br />
Coker NJ, Salzer TA. The use of masseter electromyography with electro-neurography in the<br />
evaluation of facial paralysis. Otolaryngol Head Neck Surg 1990;103:391-395.<br />
Danielides V, Skevas A, Kastanioudakis I. Assimakopoulos D. Comparative study of evoked<br />
electromyography and facial nerve latency test in the prognosis of idiopathic facial nerve palsy in<br />
childhood. Childs Nerv Syst 1994;10:122-125.<br />
Danielides VG, Skevas AT, Panagopoulos K, Kastanioudakis I. Value of the facial nerve latency<br />
test in the prognosis of childhood Bell's palsy. Childs Nerv Syst 1992;8:126-128.<br />
Devriese PP. Prednisone in idiopathic facial paralysis (Bell's palsy). ORL J Otorhinolaryngol<br />
Relat Spec 1977;39:257-271.<br />
Eicher SA, Coker NJ, Alford BR, Igarashi M, Smith RJ. A comparative study of the fallopian<br />
canal at the meatal foramen and labyrinth segment in young children and adults. Arch<br />
Otolaryngol Head Neck Surg 1990;116:1030-1035.<br />
Engström M, Thuomas KA, Naeser P, Stålberg E, Jonsson L. Facial nerve enhancement in Bell's<br />
palsy demonstrated by different gadolinium-enhanced magnetic resonance imaging techniques.<br />
Arch Otolaryngol Head Neck Surg 1993;119:221-225.<br />
Fisch U. Surgery for Bell's palsy. Arch Otolaryngol 1981;107:1-11.<br />
http://www.bcm.edu/oto/grand/72095.html (7 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Fisch U, Esslen E. Total intratemporal exposure of the facial nerve. Arch Otolaryngol<br />
1972;95:335-341.<br />
Fisch U, Felix H. On the pathogenesis of Bell's palsy. Acta Otolaryngol 1983;95:532-538.<br />
Fitzgerald DC. Role of electrical stimulation therapy for Bell's palsy. Am J Otol 1993;14:413-<br />
414.<br />
Frach JP, Osterbauer PJ, Fuhr AW. Treatment of Bell's palsy by mechanical force, manually<br />
assisted chiropractic adjusting and high-voltage electrotherapy. J Manipulative Physio Ther<br />
1992;15:596-598.<br />
Gantz BJ, Gmür A, Fisch U. Intraoperative evoked electromyography in Bell's palsy. Am J<br />
Otolaryngol 1982;3:273-278.<br />
Glasscock ME, 3d, House WF, Alford BR. Middle fossa facial nerve decompression. Ann Otol<br />
Rhinol Laryngol 1970;79:234-240.<br />
Gontier J, Fisch U. Shirmer's test: its normal values and clinical significance. ORL J<br />
Otorhinolaryngol Relat Spec 1976;38:1-10.<br />
Gorodezky C, Carranza JM, Bustamante A, Yescas P, Martinez A, Alonso Vilatela ME. The<br />
HLA system and T-cell subsets in Bell's palsy. Acta Otolaryngol 1991;1111:1070-1074.<br />
Halvorson DJ, Coker NJ, Wang-Bennett LT. Histologic correlation of the degenerating facial<br />
nerve with electroneurography. Laryngoscope 1993;103:178-184.<br />
Honda H, Takahashi A. Virus-associated demyelination in the pathogenesis of Bell's palsy. Intern<br />
Med 1992;31:1250-1256.<br />
Hyden D, Roberg M, Forsberg P, Fridell E, Fryden A, Linde A, Odkvist L. Acute "idiopathic"<br />
peripheral facial palsy: clinical, serological, and cerebrospinal fluid finding and effects of<br />
corticosteriods. Am J Otolaryngol 1993;114:179-186.<br />
Ivarsson S, Andreasson L, Ahlfors K. Acyclovir treatment in a case of facial paralysis caused by<br />
herpes zoster. Pediatr Infect Dis 1987;6:84.<br />
Jenkins HA, Herzog JA, Coker NJ. Bell's palsy in children. Cases of progressive facial nerve<br />
degeneration. Ann Otol Rhinol Laryngol 1985;94:331-336.<br />
Jongkees LBW. On the histology of Bell's palsy. Acta Otolaryngol 1954;44:336-343.<br />
Jonsson L, Alm G, Thomander L. Elevated serum interferon levels in patients with Bell's palsy.<br />
Arch Otolaryngol Head Neck Surg 1989;115:37-40.<br />
http://www.bcm.edu/oto/grand/72095.html (8 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Jonsson L, Larsson A, Thomander L. Immune complexes and complement components in Bell's<br />
palsy. ORL J Otorhinolaryngol Relat Spec 1987;49:294-301.<br />
Katusic SK, Beard CM, Wiederholt WC, Bergstralh EH, Kurland LT. Incidence, clinical features,<br />
and prognosis in Bell's palsy. Rochester, Minnesota, 1968-1982. Ann Neurol 1986;20:622-627.<br />
Kohsyu H, Aoyagi M, Tojima H, Tada Y, Inamura H, Ikarashi T, Koike Y. Facial nerve<br />
enhancement in Gd-MRI in patients with Bell's palsy. Acta Otolaryngol Suppl 1994;511:165-<br />
169.<br />
Lipkin AF, Coker NJ, Jenkins HA, Alford BR. Intracranial and intratemporal facial neuroma.<br />
Otolaryngol Head Neck Surg 1987;96:71-79.<br />
Magielski JE, Blatt IM. Submaxillary salivary flow: a test of chorda tympani nerve function as an<br />
aid in diagnosis and prognosis of facial nerve paralysis. Laryngoscope 1958;68:1770-1789.<br />
Marsh MA, Coker NJ. Surgical decompression of idiopathic facial palsy. Otolaryngol Clin North<br />
Am 1991;24:675-689.<br />
May M, Harvey JE, Marovitz WF, Stroud M. The prognostic accuracy of the maximal<br />
stimulation test compared with that of the nerve excitability test in Bell's palsy. Laryngoscope<br />
1971;81:931-938.<br />
May M, Klein SR. Differential diagnosis of facial nerve palsy. Otolaryngol Clin North Am<br />
1991;24:613-645.<br />
May M, Klein SR, Taylor FH. Indications for surgery for Bell's palsy. Am J Otol 1984;5:503-<br />
512.<br />
McCormick DP. Herpes-simplex virus as a cause of Bell's palsy. Lancet 1972;1:937-939.<br />
McGovern FH, Estevez J, Jackson R. Immunological concept for Bell's palsy. Ann Otol Rhinol<br />
Laryngol 1977;86:300-305.<br />
Michaels L. Histopathological changes in the temporal bone in Bell's palsy. Acta Otolaryngol<br />
Suppl 1990;470:114-117<br />
Murphy TP, Teller DC. Magnetic resonance imaging of the facial nerve during Bell's palsy.<br />
Otolaryngol Head Neck Surg 1991;105:667-674.<br />
Murr AH, Benecke JE Jr. Association of facial paralysis with HIV positivity. Am J Otol<br />
1991;12:450-451.<br />
Neely JG, Alford BR. Facial nerve neuromas. Arch Otolaryngol 1974;100:298-301.<br />
Njoo FL, Wertheim-van Dillen P, Devriese PP. Serology in facial paralysis caused be clinically<br />
http://www.bcm.edu/oto/grand/72095.html (9 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
presumed herpes zoster infection. Arch Otorhinolaryngol 1988;245:230-233.<br />
Palva T, Hortling L, Ylikoski J, Collan Y. Viral culture and electron microscopy of ganglion cells<br />
in Meniere's disease and Bell's palsy. Acta Otolaryngol 1978;86:269-275.<br />
Peitersen E. The natural history of Bell's palsy. Am J Otol 1982;4:107-111.<br />
Peitersen E. Natural history of Bell's palsy. Acta Otolaryngol Suppl 1992;492:122-124.<br />
Rosenberg JJ, Alford BR. Experimentally controlled facial nerve injuries. Arch Otolarryngol<br />
1966;84:337-342.<br />
Ruboyianes JM, Adour KK, Santos DQ, Van Doersten PG. The maximal stimulation and facial<br />
nerve conduction latency tests: predicting the outcome of Bell's Palsy. Laryngoscope 1994;104:1-<br />
6.<br />
Saito O, Aoyagi M, Tojima H, Koike Y. Diagnosis and treatment for Bell's palsy associated with<br />
diabetes mellitus. Acta Otolaryngol Suppl 1994;511:153-155.<br />
Salzer TA, Coker NJ, Wang-Bennett LT. Stimulation variables in electroneurography of the<br />
facial nerve. Arch Otolaryngol Head Neck Surg 1990;116:1036-1040.<br />
Schwaber MK, Larson TC 3d, Zealer DL, Creasy J. Gadolinium-enhanced magnetic resonance<br />
imaging in Bell's palsy. Laryngoscope 1990;100:1264-1269.<br />
Shafshak TS, Essa AY, Bakey FA. The possible contributing factors for the success of steroid<br />
therapy in Bell's palsy: a clinical and electrophysiological study. J Laryngol Otol 1994;108:940-<br />
943.<br />
Sillman JS, Niparko JK, Lee SS, Kileny PR. Prognostic value of evoked and standard<br />
electromyography in acute facial paralysis. Otolaryngol Head Neck Surg 1992;107:377-381.<br />
Smith IM, Cull RE. Bell's palsy--which factors determine final recovery? Clin Otolaryngol<br />
1994;19:465-466.<br />
Smith IM, Maynard C, Mountain RE, Barr-Hamilton R, Armstrong M, Murray JA. The<br />
prognostic value of facial electroneurography in Bell's palsy. Clin Otolaryngol 1994;19:201-203.<br />
Stankiewicz JA. A review of the published data on steroids and idiopathic facial paralysis.<br />
Otolaryngol Head Neck Surg 1987;97:481-486.<br />
Tojima H, Aoyagi M, Inamura H, Koike Y. Clinical advantages of electroneurography in patients<br />
with Bell's palsy within two weeks after onset. Acta Otolaryngol Suppl 1994;511:147-149.<br />
Vahlne A, Edstrom S, Arstila P, Beran M, Ejnell H, Nylen O, et al. Bell's palsy and herpes<br />
http://www.bcm.edu/oto/grand/72095.html (10 of 11) [5.11.2005 10:40:15]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
simplex virus. Arch Otolaryngol 1981;107:79-81.<br />
Welkoborsky HJ, Amedee RG, Elkhatieb A, Mann WJ. Auditory-evoked brain-stem responses<br />
and auditory disorders in patients with Bell's palsy. Eur Arch Otorhinolaryngol 1991;248:417-<br />
419.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1995-7. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/72095.html (11 of 11) [5.11.2005 10:40:15]
http://www.bcm.edu/oto/grand/110493.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
UNUSUAL CEREBELLOPONTINE ANGLE NEOPLASMS<br />
Glenn W. Knox, MD<br />
November 4, 1993<br />
Cerebellopontine angle lesions are the predominant skull base neoplasms that affect the posterior fossa.<br />
Although vestibular schwannomas account for the majority of primary neoplasms, a wide array of other<br />
lesions must also be considered in the differential diagnosis. In Brackmann and Bartels' series of CPA<br />
neoplasms, vestibular schwannoma accounted for over 90%. The remaining primary tumors were<br />
meningiomas (3.1%), primary cholesteatomas (2.4%), facial nerve schwannomas (1.2%), other<br />
schwannomas (0.2%), and other tumors (1.9%).<br />
Meningiomas represent up to 18% of all intracranial tumors and approximately 3% of CPA tumors. The<br />
cells lining the arachnoid villae are the cells of origin. These cells are distributed throughout the<br />
intracranial space predominantly in relation to veins and dural sinuses. Meningiomas are benign but<br />
http://www.bcm.edu/oto/grand/110493.html (1 of 6) [5.11.2005 10:40:24]
http://www.bcm.edu/oto/grand/110493.html<br />
locally aggressive tumors which occur at different anatomic sites in the following order of frequency:<br />
parasaggital, falx, convexity, olfactory groove, tuberculum sellae, sphenoid ridge, CPA, tentorium,<br />
lateral ventricle, clivus. The gross appearance is typically a globular mass that is firmly adherent to the<br />
dura mater, with characteristic speckles scattered throughout the tumor that correspond to the<br />
microscopic psammoma bodies. The tumor displaces but does not invade adjacent neural tissue.<br />
Case Presentation<br />
A 51-year-old white man noted the onset of vertigo in 1980. This resolved, but returned in the late 1980s,<br />
reaching a peak in 1988. His vertigo symptoms had improved since then. He also complained of a multiyear<br />
history of mild right-sided tinnitus, which had been variable but more noticeable this year. He<br />
complained of a two-year history of mild right-sided hearing loss which had also been more noticeable<br />
this year. His major complaint was a sense of fullness in the right ear which he had noticed in January of<br />
1993, which did not improve with medical treatment. Past medical history was noncontributory. Physical<br />
examination was unremarkable. A recent audiogram showed a right-sided 40 dB high frequency<br />
sensorineural hearing loss with a PB max of 96%. Tympanograms were type A. MRI revealed an<br />
intracanalicular mass.<br />
The patient was admitted to TMH and underwent a right excision of cerebellopontine angle mass via the<br />
midfossa approach. During surgery, the tumor appeared to be associated with the superior vestibular<br />
nerve. The tumor was noted to be tightly adherent to the surrounding structures, was rubbery in<br />
consistency, and contained several apparent venous sinuses. The patient recovered uneventfully with<br />
useful hearing preserved. Pathology revealed benign fibrous tissue with abundant vessels, consistent with<br />
a benign vascular tumor.<br />
Bibliography<br />
Arriaga MA, Brackmann DE, Hitselberger WE. Extended middle fossa resection of petroclival and cavernous sinus<br />
neoplasms. Laryngoscope 1993;103:693-698.<br />
Balkany T, Fradis M, Jafek BW, Rucker NC. Hemangioma of the facial nerve: role of the geniculate capillary plexus. Skull<br />
Base Surg 1991;1:59-63.<br />
Batsakis JG. Tumors of the Head and Neck, 2nd ed. Baltimore: Williams & Wilkins, 1979.<br />
Beatty CW, Ebersold MJ, Harner SG. Residual and recurrent acoustic neuromas. Laryngoscope 1987;97:1168-1171.<br />
Bellet PS, Benton C Jr, Matt BH, Myer CM 3d. The evaluation of ear canal, middle ear, temporal bone, and<br />
cerebellopontine angle masses in infants, children, and adolescents. Adv Pediatr 1992;39:167-205.<br />
http://www.bcm.edu/oto/grand/110493.html (2 of 6) [5.11.2005 10:40:24]
http://www.bcm.edu/oto/grand/110493.html<br />
Bourgouin PM, Tampiere D, Robitaille Y, Robert F, Bergeron D, del Carpio R, et al. Low-grade myxoid chondrosarcoma<br />
of the base of the skull: CT, MR, and histopathology. J Comput Assist Tomogr 1992;16:268-273.<br />
Brackmann DE, Anderson RG. Cholesteatomas of the cerebellopontine angle. In: Silverstein H, Norrell H, editors.<br />
Neurological Surgery of the Ear. Birmingham: Aesculapius, 1979.<br />
Brackmann DE, Bartels LJ. Rare tumors of the cerebellopontine angle. Otolaryngol Head Neck Surg 1980;88:555-559.<br />
Brackman DE, Gherini SE. Differential diagnosis of skull base neoplasms involving the posterior fossa. In: Cummings<br />
CW, Harker MD, editors. Otolaryngology - Head and Neck Surgery IV. St. Louis: Mosby, 1986:3421-3436.<br />
Brackmann DE, Kwartler JA. A review of acoustic tumors: 1983-1988. Am J Otol 1990;11:216-232.<br />
Bushe KA, Naumann M, Warmuth-Metz M, Meizensberger J, Muller J. Maffucci's syndrome with bilateral cartilaginous<br />
tumors of the cerebellopontine angle. Neurosurgery 1990;27:625-628.<br />
O'Keefe LJ, Ramsden RT, Birzgalis AR. Cerebellopontine angle lipoma. J Laryngol Otol 1993;107:553-555.<br />
Cosnard G, Galidie G, Cordoliani YS, Le Gall R. Rare tumors of the cerebellopontine angle. Ann Radiol (Paris)<br />
1992;35:36-43.<br />
Dort JC, Fisch U. Facial nerve schwannomas. Skull Base Surg 1991;1:51-56.<br />
Elster AD, Challa VR, Gilbert TH, Richardson DM. Meningiomas: MR and histopathologic features. Radiology<br />
1989;179:857-862.<br />
Gao PY, Osborn AG, Smirniotopoulos JG, Harris CP. Radiologic-pathologic correlation: epidermoid tumor of the<br />
cerebellopontine angle. AJNR Am J Neuroradiol 1992;13:863-872.<br />
Garcia CA, McGarry PA, Rodriguez F. Primary intracranial squamous cell carcinoma of the right cerebellopontine angle. J<br />
Neurosurg 1981;54:824-828.<br />
Giddings NA, Brackmann DE, Kwartler JA. Transcanal infracochlear approach to the petrous apex. Otolaryngol Head<br />
Neck Surg 1991;104:29-36.<br />
Haberkamp TJ, Monsell EM, House WF, Levine SC, Piazza L. Diagnosis and treatment of arachnoid cysts of the posterior<br />
fossa. Otolaryngol Head Neck Surg 1990;103:610-614.<br />
Hamann G, Bier B, Schimrigk K. Basilar aneurysm in the cerebello-pontine angle. Case report with review of the<br />
literature. Nervenarzt 1992;63:113-115.<br />
Iplikcioglu AC, Ozer F, Benli K, Bertan V, Ruacan S. Malignant teratoma of the cerebellopontine angle: case report.<br />
Neurosurgery 1990;27:137-139.<br />
http://www.bcm.edu/oto/grand/110493.html (3 of 6) [5.11.2005 10:40:24]
http://www.bcm.edu/oto/grand/110493.html<br />
Jackler RK, Shapiro MS, Dillon WP, Pitts L, Lanser MJ. Gadolinium-DTPA enhanced magnetic resonance imaging in<br />
acoustic neuroma. Otolaryngol Head Neck Surg 1990;102:670-677.<br />
Jamjoom A, Jamjoom ZA, Griffiths D, Moss T, Coakham H. Cerebellopontine angle epithelial cyst. A case report.<br />
Neurosurg Rev 1993;16:67-70.<br />
Janecka IP, Sekhar LN, Horton JA, Yonas H. General blood flow evaluation. In: Cummings CW, et al. Otolaryngology -<br />
Head and Neck Surgery Update II. St. Louis: Mosby, 1990:54-63.<br />
Jenkins HA. Hearing preservation in acoustic neuroma surgery. Laryngoscope 1992;102:125-128.<br />
Jerger J, Oliver TA, Jenkins H. Suprathreshold abnormalities of the stapedius reflex in acoustic tumors: a series of case<br />
reports. Ear Hear 1987;8:131-139.<br />
Johnson EW. Results of auditory tests in acoustic tumor patients. In: House WF, Luetje CM, editors. Acoustic Tumors.<br />
Baltimore: University Park Press, 1979.<br />
Kartush JM, Niparko JK, Graham MD, Kemink JL. Electroneurography: preoperative facial nerve assessment for tumors<br />
of the temporal bone. Otolaryngol Head Neck Surg 1987;97:257-261.<br />
Kasantikul V, Netsky MG, Glasscock ME 3d. Acoustic neurilemmoma: clinicoanatomical study of 103 patients. J<br />
Neurosurg 1980;52:28-35.<br />
Kitamura K, Futaki T, Miyoshi S. Fluctuating hearing loss in lipoma of the cerebellopontine angle. ORL J<br />
Otorhinolaryngol Relat Spec 1990;52:335-339.<br />
Knorr JR, Ragland RL, Smith TW, Davidson RI, Keller JD. Squamous carcinoma arising in a cerebellopontine angle<br />
epidermoid: CT and MR findings. AJNR Am J Neuroradiol 1991;12:1182-1184.<br />
Koci TM, Chiang F, Mehringer CM, Yuh WT, Mayr NA, Itabashi H, et al. Adult cerebellar medulloblastoma: imaging<br />
features with emphasis on MR findings. AJNR Am J Neuroradiol 1993;14:929-939.<br />
Lalwani AK. Meningiomas, epidermoids, and other nonacoustic tumors of the cerebellopontine angle. Otolaryngol Clin<br />
North Am 1992;25:707-728.<br />
Lalwani AK, Jackler RK. Preoperative differentiation between meningioma of the cerebellopontine angle and acoustic<br />
neuroma using MRI. Otolaryngol Head Neck Surg 1993;109:88-95.<br />
Langman AW, Jackler RK, Althaus SR. Meningioma of the internal auditory canal. Am J Otol 1990;11:201-204.<br />
Le-Marc Hadour F, Mouret P, Bost F, Pasquier D, Pasquier B, Charachon R. Lipoma of the internal auditory canal: an<br />
anatomo-clinical case study and review of the literature about cranial nerve lipomas. Arch Anat Cytol Pathol 1991;39:147-<br />
150.<br />
Linthicum FH Jr , Waldorf R, Luxford WM, Caltogirone S. Infrared/video ENG recording of eye movements to evaluate<br />
the inferior vestibular nerve using the minimal caloric test. Otolaryngol Head Neck Surg 1988;98:207-210.<br />
http://www.bcm.edu/oto/grand/110493.html (4 of 6) [5.11.2005 10:40:24]
http://www.bcm.edu/oto/grand/110493.html<br />
Lipper MH, Cail WS. Chordoma of the petrous bone. South Med J 1991;84:629-631.<br />
Lo WW. Tumors of the temporal bone and cerebellopontine angle. In: Som PM, Bergeron RT, editors. Head and Neck<br />
Imaging, 2nd ed. St. Louis: Mosby, 1991:1046-1108.<br />
Lunardi P, Missori P, Salvati M, Licastro G. Cholesterol granuloma of the cerebello-pontine angle. Clin Neurol Neurosurg<br />
1992;94:265-268.<br />
Martuza RL, Eldridge R. Neurofibromatosis 2 (bilateral acoustic neurofibromatosis). N Engl J Med 1988;318:684-688.<br />
McCormick PC, Bello JA, Post KD. Trigeminal schwannoma: surgical series of 14 cases with review of the literature. J<br />
Neurosurg 1988;69:850-860.<br />
Mohsenipour I, Deusch E, Ortler M, Pallua A. Meningiomas of the cerebellopontine angle. Neurochirugia 1993;36:90-92.<br />
Pappas DG, Brackmann DE. Arachnoid cysts of the posterior fossa. Otolaryngol Head Neck Surg 1981;89:328-332.<br />
Pappas DG, Schneiderman TS, Brackmann DE, Simpson LC, Chandra Sekar B, Sofferman RA. Cavernous hemangiomas<br />
of the internal auditory canal. Otolaryngol Head Neck Surg 1989;101:27-32.<br />
Parnes LS, Lee DH, Peerless SJ. Magnetic resonance imaging of facial nerve neuromas. Laryngoscope 1991;101:31-35.<br />
Press GA, Hesselink JR. MR imaging of cerebellopontine angle and internal auditory canal lesions at 1.5T. AJR Am J<br />
Roentgenol 1988;150:1371-1381.<br />
Rubenstein LI. Tumors of the central nervous system. In: Firminger HI, editor. Atlas of Tumor Pathology, Second series,<br />
fascicle 6. Washington, D.C.: Armed Forces Institute of Pathology, 1972.<br />
Russell DS, Rubenstein LJ. Pathology of Tumors of the Nervous System, 4th ed. Edinburgh: T & A Constable, 1977.<br />
Sataloff RT, Davies B, Myers DL. Acoustic neuromas presenting as sudden deafness. Am J Otol 1985;6:349-352.<br />
Saunders JE, Kwartler JA, Wolf HK, Brackmann DE, McElveen JT Jr. Lipomas of the internal auditory canal.<br />
Laryngoscope 1991;101:1031-1037.<br />
Segall HD, Zee CS, Naidich TP, Ahmadi J, Becker TS. Computed tomography in neoplasms of the posterior fossa in<br />
children. Radiol Clin North Am 1982;20:237-253.<br />
Sekhar LN, Jannetta PJ. Cerebellopontine angle meningiomas: microsurgical excision and follow-up results. J Neurosurg<br />
1984;60:500-505.<br />
Selters WA, Brackmann DE. Acoustic tumor detection with brainstem electric response audiometry. Arch Otolaryngol<br />
1977;103:181-187.<br />
http://www.bcm.edu/oto/grand/110493.html (5 of 6) [5.11.2005 10:40:24]
http://www.bcm.edu/oto/grand/110493.html<br />
Shinozaki N, Sekiya T, Suzuki S, Iwabuchi T, Suzuki M. Five cases of intracranial lipoma; CT and magnetic resonance<br />
images. No Shinkei Geka 1992;20:289-293.<br />
Spector GJ, Wobol S, Thawley SE, Maisel RH, Ogura JH. Glomus jugulare tumors of the temporal bone: patterns of<br />
invasion of the temporal bone. Laryngoscope 1979;89:1628-1639.<br />
Tekkok IH, Suzer T, Erbengi A. Non-acoustic tumors of the cerebellopontine angle. Neurosurg Rev 1992;117-123.<br />
Valvanis A, et al. Clinical Imaging of the Cerebellopontine Angle. Berlin: Springer-Verlag, 1986.<br />
Weber AL. Magnetic resonance imaging and computed tomography of the internal auditory canal and cerebellopontine<br />
angle. Isr J Med Sci 1992;28:173-182.<br />
Westra I, Drummond GT. Occult pontine glioma in a patient with hemifacial spasm. Can J Ophthalmol 1991;26:148-151.<br />
Wilms G, Plets C, Boossens L, Goffin J, Vanwambeke K. The radiological differentiation of acoustic neuronoma and<br />
meningioma occurring together in the cerebellopontine angle. Neurosurgery 1992;30:443-5, 445-6.<br />
Yokota J, Imai H, Okuda O, Sato K. Inverted Bruns' nystagmus in arachnoid cysts of the cerebellopontine angle. Eur<br />
Neurol 1993;33:62-64.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/110493.html (6 of 6) [5.11.2005 10:40:24]
http://www.bcm.edu/oto/grand/10793.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
PEDIATRIC CHOLESTEATOMA<br />
A. Paul Vastola, MD<br />
October 7, 1993<br />
The term cholesteatoma is actually a misnomer coined by Johannes Muller in 1838. He described "a<br />
layered pearly tumor of fat which was distinguished from other fat tumors by the presence of biliary fat or<br />
cholestrin that is interspersed among sheets of polyhedral cells." Aural cholesteatomas are best thought of<br />
as skin growing in the middle ear space. Cholesteatomas actually do not contain fat but are composed of<br />
an outer matrix which surrounds layers of desquamated epithelium. The matrix is comprised of fully<br />
differentiated keratinizing squamous epithelium resting on a collagenous perimatrix. Various theories<br />
have been advanced to account for the destructive bone resorption seen commonly with these lesions.<br />
These include activation of osteoclastic bone destruction, mechanical pressure necrosis and bone<br />
degradation by enzymes such as collagenases and lysozymes.<br />
http://www.bcm.edu/oto/grand/10793.html (1 of 6) [5.11.2005 10:40:33]
http://www.bcm.edu/oto/grand/10793.html<br />
Cholesteatomas may be classified as either congenital or acquired. Congenital cholesteatomas develop<br />
behind an intact tympanic membrane; according to the classic teachings of Derlacki and Clemis there<br />
must be no antecedent history of infection or breach of the tympanic membrane. This definition has<br />
recently been challenged by Friedman et al who note that approximately 70% of children will have had at<br />
least one episode of otitis media. There is little doubt that patients with epidermal rests of cells in the<br />
protympanum may also have episodes of AOM. The acquired form of cholesteatoma is much more<br />
common. Primary acquired disease arises from a skin lined retraction pocket within which retained<br />
keratin debris accumulates. Primary acquired cholesteatoma occurs most commonly in the posteriorsuperior<br />
quadrant of the pars tensa and in the pars flaccida. Secondary acquired cholesteatoma develops<br />
from an ingrowth of skin through a tympanic membrane perforation that is then retained within the<br />
middle ear, mastoid or both.<br />
The pathogenesis of cholesteatoma growth is still poorly understood as evidenced by the multiple theories<br />
currently found in the literature. However, a common denominator appears to be eustachian tubal<br />
dysfunction. Bluestone proposes that patients with acquired cholesteatoma have a functional obstruction<br />
of the eustachian tube and are thus predisposed to high negative middle ear pressures. The areas of the<br />
tympanic membrane most susceptible to these forces are the pars flaccida and posterior-superior regions.<br />
The expansion or growth of cholesteatomas are channeled along well defined pathways determined by<br />
ligaments and folds. Review of embryologic development is helpful in understanding these pathways.<br />
Between the 3rd and 7th months of development the gelatinous tissue of the middle ear space is absorbed.<br />
A primitive tympanic cavity develops by growth of an endothelium lined pouch extending from the<br />
eustachian tube to the middle ear cleft. Four primary sacs then bud into the cleft. The remnants of these<br />
sacs direct the growth of cholesteatoma along predictable pathways in the middle ear. Prussaks space is<br />
commonly thought of as the most common point of invasion for primary acquired cholesteatomas. From<br />
this space cholesteatomas expand in one of three directions: the posterior route is most commonly seen,<br />
and follows the superior incudal space above the incus into the epitympanum. The inferior route follows<br />
the inferior incudal space into the mesotympanum. The anterior route from Prussaks space is the route<br />
least frequently travelled. The anterior pouch of von Trolsch serves as the avenue for spread into the<br />
protympanum.<br />
The presence of cholesteatoma requires surgical intervention unless underlying medical problems<br />
contraindicate exposure to general anesthesia. Most cholesteatomas are asymptomatic in their early<br />
development; children may come to medical attention with otorrhea but will rarely complain of decreased<br />
hearing. Microscopic examination of the ear is imperative in identifying and delineating cholesteatoma.<br />
Audiometric evaluation is part of the standard preoperative workup. Computerized tomography may be<br />
used to delineate the extent of disease, check the aeration of the mastoid and to help rule out<br />
intratemporal and /or intracranial complications.<br />
The primary surgical goal is to achieve a safe, dry ear by removing disease with the preservation of<br />
normal anatomy. Improving hearing is a secondary goal. The principles of surgical management are based<br />
on the extent of the disease and the presence of complications arising from cholesteatoma. Much debate<br />
has emerged in the literature concerning canal wall up procedures vs canal wall down approaches. It is<br />
clear that the consensus among otologists over the last several years has been that canal wall up<br />
http://www.bcm.edu/oto/grand/10793.html (2 of 6) [5.11.2005 10:40:33]
http://www.bcm.edu/oto/grand/10793.html<br />
procedures are indicated in patients with well pneumatized mastoids and adequate middle ear clefts with<br />
cholesteatoma limited to the middle ear space or mastoid. Relative contraindications to canal wall up<br />
procedures include a sclerotic mastoid, a fistula, an only hearing ear and poor eustachian tubal function.<br />
There is no objective measurement of eustachian tubal function though several clinical observations can<br />
help predict the ability of the middle ear to ventilate itself. According to Parisier et al the appearance of<br />
the pars tensa, the amount of mastoid cellular development and the appearance of middle ear mucosa will<br />
reflect the eustachian tubal function and guide the surgical approach. The success of any given approach<br />
may be measured in terms of the rate of recidivism. Originally a term applied to criminal behavior,<br />
recidivism is the measurement of residual disease plus recurrent cholesteatoma.<br />
Cholesteatoma in children is widely considered to be a more aggressive disease than in the adult<br />
population for two major reasons. First, very extensive disease is found more frequently in children<br />
compared to adults and second, higher rates of residual and recurrent disease have been documented in<br />
the pediatric population. Of note however is the observation that the incidence of complications arising<br />
from cholesteatoma is directly related to the duration of the disease and, as such, adults tended to have<br />
higher complication rates.<br />
Glasscock in 1981 published a retrospective review of charts comparing rates of recidivism in patients<br />
less than 16 years old to those older than 16. Almost 90% of both groups had a canal wall up approach<br />
regardless of initial findings. Rates of recidivism were compared and it was found that patients less than<br />
16 had an almost two-fold higher rate and a much shorter interval to recurrence. Based on these findings<br />
Glasscock concluded that pediatric cholesteatoma is more aggressive than that seen in adults. There was<br />
no statistical analysis presented and no criteria were set forth regarding canal wall up vs canal wall down<br />
approaches.<br />
In 1977 Palva published a retrospective evaluation of 65 pediatric patients (
http://www.bcm.edu/oto/grand/10793.html<br />
A preliminary evaluation of the Baylor experience with pediatric cholesteatoma was performed. There<br />
were 26 patients (19 males and 7 females) for a total of 27 operated ears. The age at presentation<br />
averaged 8 years (range 2-15 years) with an average follow-up of 4 years (range 3 months to 15 years).<br />
The most common presenting symptoms were otorrhea (11/26), hearing loss (4/26) and tympanic<br />
membrane perforation (3/26). Five patients had congenital cholesteatoma. Pre-operative and postoperative<br />
audiograms were performed in all patients and there was no significant difference in pure tone<br />
averages (30dB pre-op compared with 27dB post-op). Fifty-four percent of patients had canal wall up<br />
procedures while 27% had canal wall down procedures. Nineteen percent of patients had a tympanotomy<br />
approach. Planned second look surgery was performed in 16 of 27 ears. Two patients underwent primary<br />
ossicular reconstruction while 9 patients had a secondary ossicular reconstruction. The rate of residual<br />
disease was 4/27 (15%) while the rate of recurrent disease was 3/27 (11%) for a recidivism rate of 26%.<br />
In conclusion there remain many questions concerning the pathophysiology of cholesteatoma; whether or<br />
not the disease differs in children and adults is still a matter of debate. The next area of inquiry will be on<br />
a cellular level. It is clear however, from the above data, that a reasoned individualized approach to<br />
cholesteatoma is the best way to achieve low rates of recidivism.<br />
Case Presentations<br />
An eight-year-old white female child presented with a history of chronic eustachian tube dysfunction,<br />
numerous episodes of acute otitis media and recent bloody otorrhea from the left ear. Her otologic history<br />
dates to the age of three when she had an episode of acute otitis media which was treated with antibiotics<br />
and decongestants. The patient subsequently failed a school audiogram and continued to require<br />
intermittent courses of oral antibiotics. Subsequent school audiogram failures were attributed to "fluid in<br />
the ears." There was no history of facial nerve palsy, vertigo or otologic surgery.<br />
Physical exam was significant for a white mass behind the posterior half of the right tympanic membrane<br />
and a central posterior, superior perforation of the left tympanic membrane. There was no evidence of<br />
keratin debris although the drum was severely retracted over the malleus. Audiometric evaluation of the<br />
right ear demonstrated a slight loss over the lower frequencies and a type C tympanogram. CTT of the<br />
temporal bones revealed a soft tissue mass involving the tympanic membrane extending toward the<br />
epitympanum without erosion of the scutum.<br />
The child was brought to the operating room where a right tympanomastoidectomy (canal wall up) was<br />
performed. Cholesteatoma was found involving the posterior half of the eardrum, extending towards the<br />
epitympanum and antrum. The ossicular mechanism was noted to be intact although there was some<br />
attenuation of the incudostapedial joint. The cholesteatoma was excised completely, leaving the ossicles<br />
intact. A medial graft was incorporated. The patient has done well postoperatively.<br />
http://www.bcm.edu/oto/grand/10793.html (4 of 6) [5.11.2005 10:40:33]
http://www.bcm.edu/oto/grand/10793.html<br />
Bibliography<br />
Abramson M, Lachenbruch PA, Press BA, McCabe BF. Results of conservative surgery for middle ear cholesteatoma.<br />
Laryngoscope 1977;87:1281-1286.<br />
Derlacki EL, Clemis JD. Congenital cholesteatoma of the middle ear and mastoid. Ann Otol Rhinol Laryngol 1965;74:706-<br />
727.<br />
Edelstein DR, Parisier SC. Surgical techniques and recidivism in cholesteatoma. Otolaryngol Clin North Am 1989;22:1029-<br />
1040.<br />
Edelstein DR, Parisier SC, Ahuja GS, Jurabe C, Clute P, Wenig S, et al. Cholesteatoma in the pediatric age group. Ann<br />
Otol Rhinol Laryngol 1988;97:23-29.<br />
Edelstein DR, Parisier SC, Han JC. Acquired cholesteatoma in the pediatric age group. Otolaryngol Clin North Am<br />
1989;22:955-965.<br />
Glasscock ME III, Dickins JRE, Wiet R. Cholesteatoma in children. Laryngoscope 1981;91:1743-1753.<br />
Jackson DG, Glasscock ME III, Nissen AJ, Schwaber MK, Bojrab DI. Open mastoid procedures: contemporary indications<br />
and surgical technique. Laryngoscope 1985;95:1037-1043.<br />
Jahn AF. Cholesteatoma: What is it, how did it get there, and how do we get rid of it? Otolaryngol Clin North Am<br />
1989;22:847-857.<br />
Jansen C. Cholesteatoma in children. Clin Otolaryngol 1978;3:349-352.<br />
McGill TJ, Merchant S, Healy GB, Friedman EM. Congenital cholesteatoma of the middle ear in children: a clinical and<br />
histopathological report. Laryngoscope 1991;101:606-613.<br />
Nadol JB Jr. Causes of failure of mastoidectomy for chronic otitis media. Laryngoscope 1985;95:410-413.<br />
Palva A, Karma P, Kärjä J. Cholesteatoma in children. Arch Otolaryngol 1977;103:74-77.<br />
Schmid H, Dort JC, Fisch U. Long-term results of treatment for children's cholesteatoma. Am J Otol 1991;12:83-87.<br />
Schulerati N, Bluestone CD. Pathogenesis of cholesteatoma. Otolaryngol Clin North Am 1989;22:859-881.<br />
Sheehy JL. Cholesteatoma surgery in children. Am J Otol 1985;6:170-172.<br />
Sheehy JL. Cholesteatoma surgery: canal wall down procedures. Ann Otol Rhinol Laryngol 1988;97:30-35.<br />
http://www.bcm.edu/oto/grand/10793.html (5 of 6) [5.11.2005 10:40:33]
http://www.bcm.edu/oto/grand/10793.html<br />
Sheehy JL, Patterson ME. Intact canal wall tympanoplasty with mastoidectomy: a review of eight years' experience.<br />
Laryngoscope 1967;77:1502-1542.<br />
Sismanis A, Hutchinson L, Abedi E. Chronic otitis media: surgical failures and management. Am J Otol 1989;10:460-465.<br />
Stern SJ, Fazekas-May M. Cholesteatoma in the pediatric population: prognostic indicators for surgical decision making.<br />
Laryngoscope 1992;102:1349-1352.<br />
Toner JG, Smyth GDL. Surgical treatment of cholesteatoma: a comparison of three techniques. Am J Otol 1990;11:247-<br />
249.<br />
Tos M. Treatment of cholesteatoma in children: a long-term study of results. Am J Otol 1983;4:189-197.<br />
Vartiainen E, Nuutinen J. Long-term results of surgical treatment in different cholesteatoma types. Am J Otol 1993;14:507-<br />
511.<br />
Weiss MG, Parisier SC, Han JC, Edelstein DR. Surgery for recurrent and residual cholesteatoma. Laryngoscope<br />
1992;102:145-151.<br />
Wullstein SR. Cholesteatoma in children: is the disease different in childhood? Clin Otolaryngol 1978;3:353-362.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/10793.html (6 of 6) [5.11.2005 10:40:33]
http://www.bcm.edu/oto/grand/10192.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
CHORDOMAS OF THE SKULL BASE<br />
Carla M. Giannoni, MD<br />
October 1, 1992<br />
Chordomas are relatively rare neoplasm arising from embryonic notochordal remnants and comprise less<br />
than 1% of intracranial neoplasms. They typically occur along the neuraxis, especially at the<br />
developmentally more active cranial and caudal ends, notably in the spheno-occipital, sacrococcygeal,<br />
and vertebral locations. Twenty-five percent to 40% of chordomas occur in the speno-occipital or skull<br />
base region. These tumors occur predominately in the 30 to 50 year old age range and show a slight<br />
predominance in men.<br />
These tumors can occur extra-axially, in unusual locations, and are then termed primary. They probably<br />
arise from ectopic notochordal elements. Chordomas have been described in the nasopharynx, mandible,<br />
maxillary sinus, frontal sinus, and, as in our case report, in the petrous apex of the temporal bone.<br />
http://www.bcm.edu/oto/grand/10192.html (1 of 7) [5.11.2005 10:40:41]
http://www.bcm.edu/oto/grand/10192.html<br />
In 1856 Luschke, working in Virchow's lab, described jelly-like tumors in the region of the clivus of<br />
Blumenbach. In 1857 Virchow also examined these tumors and named them "ecchondrosis<br />
physaliphora." He believed they arose from the spheno-occipital synchondrosis and were of cartilaginous<br />
origin. Muller, in 1858, examined embryonic tissues and, after noting their histologic similarities,<br />
postulated these tumors derived from embryonic notochord. In 1895 Ribbert demonstrated the origin of<br />
these tumors when he pierced the nucleus pulposus of the vertebral column and found that similar tumors<br />
developed. He applied the term "chordoma" to these tumors.<br />
The embryonic development of the notochord is important in understanding the anatomic distribution of<br />
these tumors. The primitive streak forms in the third week of fetal development and forms the notochord.<br />
During the fifth week of life, it extends from the coccyx cephalad to the skull base, where it courses<br />
through the odontoid process, the posterior sphenooccipital plate and ends at Rathke's pouch. The<br />
notochord becomes surrounded by mesodermal tissue which then forms the vertebral column. Ultimately<br />
the notochord disappears, but remnants persist in the nucleus pulposus of the intervertebral discs.<br />
Binkhorst et al described seven points of origin of craniocervical chordomas: the dorsum sellae, the<br />
Blumenbach's clivus, retropharyngeal region, squama occipalis, nuclei pulposi of cervical vertebrae, and<br />
the ligament of the dens.<br />
SYMPTOMS<br />
The clinical presentation depends on the origin and extension of each particular tumor. Delay in<br />
diagnosis is common, secondary to the occult nature of the disease and poorly localizing signs and<br />
symptoms. A headache arising in the vertex, ipsi-parietal, orbital, or frontal regions is a typical early<br />
symptom. This is due to stretching of middle fossa dura and is often severe. Patients may also present<br />
with paresthesias or anesthesia of the jaw region, serous otitis media, hearing loss, nasal<br />
obstruction/anosmia, syncope and, rarely, vertigo. Recurrent meningitis has also been noted in these<br />
patients.<br />
The late symptoms generally depend on the direction of tumor extension. Anterior extension leads to<br />
diplopia and ophthalmoplegia, or both. Posterior extension presents as facial or other lower cranial nerve<br />
neuropathies.<br />
RADIOGRAPHIC FEATURES<br />
CT findings of an expansile, destructive, lytic lesion with associated soft tissue mass are characteristic of<br />
chordomas. However, they are also seen with chondrosarcomas and other similar lesions. Foci of<br />
calcification may also be seen. The CT scan is useful in defining the anatomy of bone destruction.<br />
MRI is better than CT for defining the limits of a lesion and any vascular relationships, especially on the<br />
T2-weighted images. MRI of chordomas show hyperintensity in T2 and hypointensity in the T1-weighted<br />
http://www.bcm.edu/oto/grand/10192.html (2 of 7) [5.11.2005 10:40:41]
http://www.bcm.edu/oto/grand/10192.html<br />
images. The T1 images are especially useful in defining any tumor-SCF interfaces.<br />
On arteriogram, an avascular may be seen displacing the basilar artery. Radiographic studies cannot<br />
reliably distinguish chordomas from chondrosarcomas and other similar lesions, but can help eliminate<br />
other possible diagnoses.<br />
DIFFERENTIAL DIAGNOSIS<br />
Benign lesions most frequently occurring at the skull base include: meningiomas,<br />
neuromas/schwannomas, glomus tumors, vascular anomalies (e.g., internal carotid aneurysms),<br />
congenital cholesteatoma, mucocele, osteomyelitis, eosinophilic granuloma, and cholesterol cysts.<br />
Malignant lesions of this location include primary carcinoma (squamous-, adeno-, acinic, adenoid cystic),<br />
metastatic carcinoma (breast, prostatic, renal cell, bronchogenic), rhabdomyosarcoma, nasopharyngeal<br />
cancer, lymphoma and chordoma, and other mesenchymal tumors (chondroma, chondrosarcoma, and<br />
osteoclastoma).<br />
HISTOPATHOLOGY<br />
Four criteria have been used in the histologic diagnosis of chordoma: 1) a lobular arrangement of cells;<br />
2) a tendency of the cells to grow in cords, irregular bands, or pseudoacinar forms; 3) production of<br />
abundant intercellular mucinous matrix; and 4) the presence of large physaliphorous cells. A<br />
microscopically mixed population of cell types exist: stellate or primordial cells, intermediate cells and<br />
the physaliphorous cells. The stellate cell is the only actively proliferating cell. Chordoma cells then<br />
proceed through a stage of vacuolization until they reach the characteristic physaliphorous appearance.<br />
The cells then progress to destruction and rupture, completing their life cycle.<br />
Immunohistochemical tests have been developed in an effort to aid in the differentiation of these lesions.<br />
Chordomas are frequently positive for epithelial antigens - cytokeratin (CK) and epithelial membrane<br />
antigen (EMA), and negative for vimentin.<br />
A subtype of chordoma, chondroid chordoma, deserves special mention. Histologically these tumors are<br />
a mixture of chordoma, chondroma, and chondrosarcoma.<br />
PROGNOSIS AND TREATMENT<br />
The reported average survival for chordomas of the skull base is 4.1 years. There appears to be a better<br />
prognosis for chordomas of the nasopharynx and paranasal sinuses. Notably, chondroid chordomas have<br />
a reported 15.8 years average survival. The best treatment for these lesions is total surgical excision.<br />
Recurrence is the rule and metastases are extremely uncommon; patients usually succumb to local<br />
disease.<br />
http://www.bcm.edu/oto/grand/10192.html (3 of 7) [5.11.2005 10:40:41]
http://www.bcm.edu/oto/grand/10192.html<br />
Radiation therapy has been used in the postoperative care of these patients because of the tumor's usual<br />
relentless course to local recurrence and death with current conventional treatments. Fractionated proton<br />
radiation therapy is currently advocated for the treatment of chordomas. Because of its higher biological<br />
effectiveness, patients can be treated with a higher total equivalent radiation dose.<br />
Case Presentation<br />
A 57-year-old white female presented with a six- to nine-month history of intermittent left temporal<br />
headaches. They occurred monthly and usually lasted three days. She had no complaints of visual<br />
difficulties, hearing loss, vertigo, hoarseness, or dysphagia. Her past medical, surgical, and family<br />
histories were unremarkable. On physical exam she was found to be healthy. All cranial nerves were<br />
functionally intact.<br />
An MRI of the brain was done and revealed a signal abnormality of the left petrous apex and adjacent<br />
basiocciput with associated enhancement. A CT scan of the head and cervical spine showed a<br />
destructive, lytic lesion of the left basiocciput just anterior to the jugular foramen and anterolateral to the<br />
foramen magnum with probable erosion of the carotid canal.<br />
A full metastatic workup ensued including routine laboratory work, chest x-ray, mammogram, CT of the<br />
abdomen and pelvis, thyroid ultrasound, and serum protein electrophoresis. No significant abnormalities<br />
were found. A radionucleotide bone scan showed no additional bony lesions. Four vessel cerebral<br />
angiogram was negative for vascular abnormality. Three months later a follow-up CT scan of the head<br />
with thin cuts of the temporal bone showed a 1.5 X 2 X 1 cm lytic lesion corresponding with the<br />
previously identified lesion, but slightly increased in size. The bony margins of the lesions were irregular<br />
and suggestive of an aggressive process. She was then referred for surgical evaluation.<br />
She underwent a joint neurotologic and neurosurgical procedure comprised of a combination left type B<br />
infratemporal fossa and temporal fossa approach with biopsy and removal of the tumor. Frozen section<br />
revealed the tumor to be a chordoma. The patient tolerated the procedure well and had an uneventful<br />
postoperative course. The patient has been referred to Boston for fractionated proton radiation therapy.<br />
Bibliography<br />
Austin-Seymour M, Munzenrider J, Boitein M, Verhey L, Urie M, Gentry R, et al. Fractionated proton radiation therapy of<br />
chordoma and low-grade chondrosarcoma of the base of the skull. J Neurosurg 1989;70:13-17.<br />
Batsakis JG. The pathology of head and neck tumors: neoplasms of cartilage, bone and the notochord. Head Neck Surg<br />
http://www.bcm.edu/oto/grand/10192.html (4 of 7) [5.11.2005 10:40:41]
http://www.bcm.edu/oto/grand/10192.html<br />
1980;3:43-57.<br />
Batsakis JG. Tumors of the head and neck. Baltimore: Williams and Wilkins, 1979.<br />
Batsakis JG, Kittleson AC. Chordomas. Otorhinolaryngologic presentation and diagnosis. Arch Otolaryngol 1963;78:168-<br />
175.<br />
Brooks JJ, LiVolsi VA, Trojanowski JQ. Does chondroid chordoma exist? Acta Neuropathol 1987;72:229-235.<br />
Carlson BM. Patten's foundations of embryology, 5th edition. New York: McGraw-Hill, 1988.<br />
Crown RV, Sage MR, Brophy BP. CT and MR findings in patients with chordomas of the petrous apex. AJNR Am J<br />
Neuroradiol 1990;11:121-124.<br />
Crumley RL, Butin PH. Surgical access for clivus chordoma. The University of California, San Francisco, experience.<br />
Arch Otolaryngol Head Neck Surg 1989;115:295-300.<br />
Dahlin DC, MacCarty CS. Chordoma. A study of fifty-nine cases. Cancer 1952;5:1170-1178.<br />
Fisch U. Infratemporal fossa approach to tumors of the temporal bone and base of skull. J Laryngol Otol 1978;92:969-977.<br />
Fisch U, Pillsbury HC. Intratemporal approach to lesions in the temporal bone and base of skull. Arch Otolaryngol<br />
1979;105:99-107.<br />
Flood LM, Kemink JL. Surgery in lesions of the petrous apex. Otolaryngol Clin North Am 1984;17:565-75.<br />
Gacek RR. Diagnosis and management of primary tumors of the petrous apex. Ann Otol Rhinol Laryngol 1975;84(Suppl<br />
18):1-20.<br />
Glasscock ME III, Gulya AJ, Pensak ML. Surgery of the posterior fossa. Otolaryngol Clin North Am 1984;17:483-497.<br />
Glasscock, ME III, Miller GW, Drake FD, Kanok MM. Surgery of the skull base. Laryngoscope 1978;88:905-923.<br />
Heffelfinger MJ, Dahlin DC, MacCarty CS, Beabout JW. Chordomas and cartilaginous tumors at the skull base. Cancer<br />
1973;32:410-420.<br />
House WF. Middle cranial fossa approach to the petrous pyramid. Arch Otolaryngol 1963;78:460-469.<br />
House WF, DeLaCruz A, Hitselberger WE. Surgery of the skull base; transcochlear approach to the petrous apex and<br />
clivus. Otolaryngology 1978;86:770-779.<br />
Jenkins HA, Franklin DJ. Infratemporal approaches to the skull base. In: Jackson CG, editor. Surgery of skull base tumors.<br />
New York: Churchill Livingstone, 1991:121-139.<br />
Kaneko Y, Sato Y, Iwaki T, Shin RW, Tateishi J, Fukui M. Chordoma in early childhood: a clinicopathological study.<br />
http://www.bcm.edu/oto/grand/10192.html (5 of 7) [5.11.2005 10:40:41]
http://www.bcm.edu/oto/grand/10192.html<br />
Neurosurgery 1991;29:442-446.<br />
Kendal BE, Lee BCP. Cranial chordomas. Br J Radiol 1977;50:687-698.<br />
Kondziolka D, Lunsford LD, Flickinger JC. The role of radiosurgery in the management of chordoma and chondrosarcoma<br />
of the cranial base. Neurosurgery 1991;29:38-46.<br />
Krespi YP, Levine TM, Oppenheimer R. Skull base chordomas. Otolaryngol Clin North Am 1986;19:797-804.<br />
Kumar PP, Good RR, Skultety FM, Leibrock LG. Local control of recurrent clival and sacral chordoma after interstitial<br />
irradiation with iodine 125: new techniques for treatment of recurrent or unresectable chordomas. Neurosurgery<br />
1988;22:478-483.<br />
Lipper MH, Cail WS. Chordoma of the petrous bone. South Med J 1991;84:629-631.<br />
Lushka H. Cited by: Windeyer BW. Chordoma. Proc R Soc Med 1959;52:1088-1100.<br />
Meis JM, Giraldo AA. Chordoma. An immunohistochemical study of 20 cases. Arch Pathol Lab Med 1988;112:553-556.<br />
Miller RH, Woodson GE, Neely JG, Murphy EC. A surgical approach to chordomas at the base of the skull. Otolaryngol<br />
Head Neck Surg 1982;90:251-255.<br />
Muller H. Cited by: Windeyer BW. Chordoma. Proc R Soc Med 1959;52:1088-1100.<br />
Pile RF, Melville GE, New PF, Austin-Seymour M, Munzenrider J, Pile-Spellman J, et al. The role of MR and CT in<br />
evaluating clival chordomas and chondrosarcoms. AJR AM J Roentgenol 1988;151:567-575.<br />
Ribbert H. Cited by: Windeyer BW. Chordoma. Proc R Soc Med 1959;52:1088-1100.<br />
Rupa V, Rajshekhar V, Bhanu TS, Chandi SM. Primary chondroid chordoma of the base of the petrous temporal bone. J<br />
Laryngol Otol 1989;103:771-773.<br />
Salisbury JR. Demonstration of cytokeratins and an epithelial membrane antigen in chondroid chordoma. J Pathol<br />
1987;153:37-40.<br />
Sen CN, Sekhar LN, Schramm VL, Janecka IP. Chordoma and chondrosarcoma of the cranial base: an 8-year experience.<br />
Neurosurgery 1989;25:931-941.<br />
Shugar JMA, Som PM, Krepsi UP, Arnold LM, Som ML. Primary chordoma of the maxillary sinus. Laryngoscope<br />
1980;90:1825-1830.<br />
Spoden JE, Bumsted RM, Warner ED. Chondroid chordoma, case report and literature review. Ann Otol Rhinol Laryngol<br />
1980;89:279-285.<br />
Virchow R. Cited by: Windeyer BW. Chordoma. Proc R Soc Med 1959;52:1088-1100.<br />
http://www.bcm.edu/oto/grand/10192.html (6 of 7) [5.11.2005 10:40:41]
http://www.bcm.edu/oto/grand/10192.html<br />
Wright D. Nasopharyngeal and cervical chordoma. Some aspects of their development and treatment. J Laryngol Otol<br />
1967;81:1337-1355.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/10192.html (7 of 7) [5.11.2005 10:40:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
CONGENITAL AURAL ATRESIA<br />
January 12, 1995<br />
Alberto D. Fernandez, M.D.<br />
The first mention of attempts to surgically correct congenital aural atresia was made by Thomson in 1843<br />
in England. Although 2 out of the three cases were aborted when a thick atresia plate was encountered, a<br />
third record documented what was presumably a tympanic membrane, although it appears that stenosis<br />
became a problem postoperatively. In 1883, Kiesselbach attempted an atresia repair on a child that<br />
resulted in facial paralysis. It was not until 1947 and the work of Pattee and Ombredonne that a<br />
significant improvement in hearing could be obtained with surgery. Pattee reported that fixation of the<br />
stapes via the lateral chain to the atresia plate was responsible for these patients' deficits. Ombredonne<br />
devised an approach through the mastoid in order to fenestrate the lateral semicircular canal, with<br />
reportedly good hearing results.<br />
http://www.bcm.edu/oto/grand/11295.html (1 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Using Wullstein and Zollner's tympanoplasty techniques, Bellucci reported a 30 decibel gain in hearing<br />
level in 50% of his cases. Shambaugh, in 1967, recommended surgery in unilateral cases only if the<br />
cochlear reserve allowed hearing improvement to approach that of the normal ear by 25dB. Several<br />
studies by Gill, Naumann and Schuknecht reported their individual experiences adding minor variations<br />
to the basic transmastoid approach. With the advent of polytomography and subsequently, computed<br />
tomography, finer detail of middle and inner ear structures could be obtained and used to select patients<br />
for surgery. Jahrsdoerfer, in 1978, reported the first large series using the anterior approach for<br />
congenital aural atresia repair, whereby the middle ear cavity was entered directly via a newly-created<br />
external canal without performing a mastoidectomy.<br />
An appreciation of the events that occur during embryogenesis with regard to the inner, middle and<br />
external ear is requisite to understanding the trends that occur in atresia.<br />
The inner ear, including all of the components of the membranous labyrinth, develops from an<br />
invagination of ectoderm, the otic placode, at approximately 3 week's gestation, and achieves adult<br />
dimensions at midterm. Further elaboration on inner ear development and abnormality is the subject of<br />
Congenital Sensorineural Hearing Loss.<br />
The middle ear space, including the mastoid air cell system, the Eustachian tube and the inner surface of<br />
the tympanic membrane derive from endoderm of the first pharyngeal pouch. Most of these elements<br />
complete their development by the 30th week, excepting the mastoid system in which pneumatization<br />
can progress well into adulthood. Due to the late development of the mastoid system, several authors<br />
have pointed out that patients with atresia who maintain a well-developed mastoid generally manifest<br />
greater development of their middle ear space and ossicles, thus making them better surgical candidates.<br />
Ossicular development, which progresses from the 8th through the 26th week, derives from the<br />
mesoderm of the first and second branchial arches. The malleus head and body and the short process of<br />
the incus arise from the first branchial arch (Meckel's) cartilages. Second branchial (Hyoid) arch<br />
derivatives include the manubrium of the malleus, the long process of the incus and the stapes<br />
superstructure. The footplate derives from both the second arch and the lamina stapedialis of the otic<br />
capsule. Ossification occurs through endochondral bone growth. Release of the ossicles except at their<br />
ligamentous attachments occurs by endodermal resorption as it gives rise to the tympanic cavity.<br />
Ectoderm of the first branchial cleft gives rise to the external auditory canal, which develops as an<br />
invagination at the site of the future auricle at the fourth gestational week. By the eighth week, a solid<br />
core of epithelium arises and extends to the area of the middle ear space, separated from it by a thin layer<br />
of mesoderm. At approximately 28 weeks, this core begins to recanalize from medial to lateral until the<br />
surface ectoderm is reached giving rise to the external auditory canal. At its medial extent, ectoderm<br />
persists as the outermost layer of the TM, with the mesodermal layer reduced to a fibrous sheet<br />
interposed between outer ectoderm and inner cuboidal endoderm.<br />
Mesoderm from the tympanic ring serves as the primary impetus for the formation of the tympanic bone<br />
http://www.bcm.edu/oto/grand/11295.html (2 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
and the osseous portion of the external auditory canal, starting at about the 12th week. Finally, the auricle<br />
is the result of the fusion of six hillocks (His) from the first and second branchial arches, which is usually<br />
complete by the 12th week as well. Malformations are graded I through III, with Grade I manifesting as a<br />
small, but well-formed auricle; Grade II representing a recognizable auricle with varying degrees of<br />
anomaly; and Grade III, which describes a rudimentary appendage or none at all. Auricular anomalies are<br />
the subject of Microtia.<br />
Congenital aural atresia has a reported incidence that varies between 1 in 10 to 1 in 20,000. Congenital<br />
aural atresia is usually found in isolation and in these instances patterns of inheritance have not been<br />
seen. Its association with several known craniofacial syndromes is well known. Aural atresia has been<br />
found in association with 22 of the 71 known craniofacial syndromes. The most common of these are<br />
Treacher-Collins (mandibulofacial dysostosis), Nager (acrofacial dysostosis), Crouzon's (craniofacial<br />
dysostosis), hemifacial microsomia, and the first and second branchial arch syndromes including<br />
Goldenhar's (oculoauriculovertebral dysplasia). In unilateral cases, Jafek et al and others have cited an<br />
increased incidence of atresia on the right. Bilateral atresia has been reported to occur in approximately<br />
30% of cases.<br />
Establishing a classification system of the congenital ear malformations has been almost as difficult as<br />
the operative procedures themselves. Several schemes have been proposed over time, one the first being<br />
that proposed by Marx in 1926 for auricular anomalies, which were graded I - III for mild to severe<br />
deformities. Altmann in 1955 proposed the first schema based on the temporal bone itself, looking at the<br />
status of the canal, tympanic bone, drum and ossicles. Lapchenko in 1967 and Gill in 1969 both set up a<br />
four tier scale, examining the degree of middle ear and external canal development, and the presence of<br />
ossicular abnormality. Additionally, Gill incorporated into his system, the degree of pneumatization of<br />
the mastoid, as this seemed to predict the relative success of operative interventions. Ombredonne and<br />
Nager and Colman each tried to establish simplified and clinically practical systems based on Altmann's<br />
original scheme, but these were inconsistent at predicting outcome in those cases of major aplasia or<br />
group II anomalies. Jahrsdoerfer in 1992 established not so much a classification system, but rather a<br />
grading scale as a means selecting patients that would most likely benefit from attempts at repair of their<br />
atresias.<br />
This system of grading allows for a quantitative analysis of the temporal bone and those structures that<br />
are considered vital to the success of an operation. Whereas prior systems were excellent descriptions of<br />
surgical and anatomical findings, they lacked predictive power and were subject to interobserver bias.<br />
This scale, which is based on temporal bone CT findings, assesses nine different parameters that are used<br />
in making the determination of candidacy for surgery. Of note, the stapes and oval window complex<br />
account for 3 out of the 10 points possible in the scale. Other parameters include the middle ear cleft,<br />
facial nerve position, status of the ossicles and round window, and pneumatization of the mastoid. Scores<br />
of 6 through 10 range from marginal to excellent candidates for surgery while a score of 5 or less usually<br />
anticipates a poor outcome.<br />
In general, patients with congenital aural atresia are seen in referral from neonatologists in those cases<br />
where gross craniofacial anomalies are present. However, many cases of isolated atresia or even those<br />
http://www.bcm.edu/oto/grand/11295.html (3 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
with very mild head and neck syndromes may be delayed until later in development and may be referred<br />
by pediatricians for either atresia or for problems relating to a stenotic canal. As is usual, a thorough<br />
history is important in the initial evaluation of these patients, including questions relating to the gestation<br />
of the infant. Specifically, issues of drug utilization, toxic exposures, prior family history of hearing<br />
impairment and developmental craniofacial disorders and maternal infections should be probed as<br />
possible etiologies.<br />
A thorough physical exam of the head and neck as well as of other organ systems should be performed,<br />
especially the spine, extremities and genitourinary systems as these develop concurrently with those of<br />
the head and neck. Associated anomalies of the midface and mandible should be noted. Position of the<br />
auricle and the degree of external canal development should be checked. The degree of mastoid<br />
prominence should be noted as this may give an early insight to the operative potential of the patient.<br />
Cranial nerve function, especially that of the facial nerve should be assessed.<br />
An audiologic evaluation is essential in the initial assessment of these patients. A screening ABR should<br />
be obtained for several reasons. The first is to establish the presence of a functional inner ear. In very<br />
young patients this is accomplished with multichannel air and bone conduction ABR. In cases of bilateral<br />
atresia, this form of ABR will also allow one to establish with greater certainty the ear with greater<br />
cochlear function by examining the response obtained in wave I, which is indicative of ipsilateral<br />
cochlear status only. The second reason for early ABR is that if an intact inner ear is present, the child<br />
can be fitted early on with a bone-conducting device. The usual finding is that of moderate to maximal<br />
conductive loss, although mild conductive losses are sometimes seen in cases with membranous atresia.<br />
A third reason for early ABR is to assess the functional status of the contralateral ear in unilateral<br />
atresias. Several cases of sensorineural or mixed losses in the contralateral, normal-appearing ear have<br />
been reported and should be ruled out. Having ascertained the functional status of the inner ear,<br />
diagnostic imaging is used to assess the degree and nature of the temporal bone deformity.<br />
With CT scanning, an assessment of the ossicular mass, the nature of the atretic plate (whether bony or<br />
soft), the position and course of the facial nerve, the degree of external canal development and mastoid<br />
pneumatization is possible. The presence of a cholesteatoma, which has a slight predilection for stenotic<br />
ears, can also be ruled out. Current recommendations for the timing of CT scan is at approximately 4<br />
years when mastoid pneumatization is most complete. A review of the literature by Cressman et al has<br />
shown that approximately 50% of patients seen for this condition are ultimately found to be candidates<br />
for reconstruction based on CT scan findings.<br />
The current consensus among those who undertake these procedures is that surgery on cases of either<br />
bilateral or unilateral atresia should be deferred until the patient is at least 4 to 6 years of age, with an<br />
additional delay to consenting age espoused by others for those cases of unilateral atresia. The need to<br />
foster continued mental development and the evolution of speech skills requires that interim bone<br />
conducting appliances be provided for these patients with bilateral atresias that have documented<br />
cochlear function on ABR. Unilateral atresia patients usually do not require any intervention as long as<br />
normal hearing is present in the contralateral ear.<br />
http://www.bcm.edu/oto/grand/11295.html (4 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Once the decision to proceed with surgery has been made, a consideration of both the functional and<br />
cosmetic aspects of the operation needs to be taken together. Close coordination with the plastic surgeon<br />
reconstructing the auricle is needed and usually takes place as a multi-staged procedure. Because of<br />
problems relating to healing in a fibrotic, previously-operated area, current practice is to allow the plastic<br />
surgeon to operate first with the implantation of an auricular framework of autogenous rib graft in a<br />
subcutaneous pocket. Stage II consists of lobule transposition and remnant excision. Correction of the<br />
atresia with the creation of a new external meatus, canal, drum and conducting mechanism in continuity<br />
with the stapes and inner ear is completed in Stage III along with alignment of the new auricle to the<br />
meatus. Stages IV and V usually consist of the creation of a new tragus and the elevation of the auricle<br />
off the post-auricular skin.<br />
Contrary to the standard practice of operating on the poorer hearing ear first, as is the case with chronic<br />
ear infection, cholesteatoma and otosclerosis, the better hearing ear is operated on first in CAA as this<br />
will afford the best chance for an optimal outcome. Two general approaches to the repair of atresia are<br />
currently described, both of which commence with postauricular incisions. The first of these is the<br />
transmastoid approach that makes use of the familiar landmarks of the tegmen and sinodural angle to<br />
approach the mastoid antrum and the bony atresia plate. This dissection is conducted with the aid of a<br />
facial nerve monitor, as the course of this nerve is commonly aberrant owing to the anomalous<br />
development of the tympanic bone and mastoid. Some surgeons opt to perform incudostapedial<br />
dislocation if this is feasible in order to prevent transmitted acoustic trauma to the inner ear with resultant<br />
sensorineural loss. Once the plate is removed, a canal wall down mastoidectomy is completed leaving an<br />
open cavity.<br />
A second, newer, approach described by Jahrsdoerfer and known as the Anterior Approach involves<br />
exposure of the tympanum and ossicular mass by directly removing bone from lateral to medial between<br />
the glenoid fossa and the middle cranial fossa dura. Drilling begins just posterior to the condyle, and<br />
proceeds medially using the middle fossa dura as a superior guide. An anterior and superior approach<br />
presents the least risk in injuring an anomalous facial nerve. This usually leads to an ossicular mass<br />
consisting of a fused incus and malleus attached to the atretic plate. Once identified, the atretic plate can<br />
be taken down with diamond burrs and curettes, taking care to avoid contact with the ossicular mass.<br />
Mobility of the stapes and the status of the oval and round windows is checked. Middle ear<br />
reconstruction with a prosthesis is performed if necessary. Otherwise, temporalis fascia and splitthickness<br />
skin grafting is performed to create a new eardrum and line the newly-created canal. A<br />
meatoplasty completes the procedure and places the canal in continuity with the auricular meatus.<br />
Modification of this approach has been described including a canal wall-up approach that allows the<br />
surgeon to identify the nerve and atresia plate prior to opening a canal.<br />
The goal of attaining hearing improvement in an ear with a previously moderate to maximal conductive<br />
loss varies from persistent maximal conductive loss to cases of near-total closure of the air-bone gap.<br />
Although different parameters for successful improvement in hearing have been reported, according to<br />
Cressman et al, if one chooses a speech reception threshold of 25 decibels or less, then anywhere from 20<br />
to 80% of patients will have a successful operation. Much of this range hinges on patient selection,<br />
http://www.bcm.edu/oto/grand/11295.html (5 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
experience and technique. Crabtree, de la Cruz and Glasscock have each reported varying degrees of<br />
success with this operation. However, this may reflect the utilization of different parameters and<br />
definitions by each of these authors. Jahrsdoerfer reported in 1992 on his results based on patients<br />
selected using a 10-point grading system. He reported achieving speech reception thresholds of 25<br />
decibels or less in 75% of 86 cases operated on. Several authors have noted that cases requiring a<br />
prosthesis for ossicular reconstruction tend to have greater air-bone gaps postoperatively than those<br />
receiving grafts over a mobile ossicular mass.<br />
Complications relating to CAA repair can be divided into intraoperative and postoperative categories.<br />
Intraoperative complications include facial nerve injury, sensorineural deafness, and perilymph fistula.<br />
Although cited as a potential complication, permanent facial paralysis is exceedingly rare despite its<br />
aberrant course through atretic temporal bones. High frequency sensorineural loss secondary to<br />
transmitted vibrations has been reported with both approaches. Postoperative or delayed complications<br />
for the most part include stenosis and chronic drainage, more common with the transmastoid approach,<br />
and graft lateralization that plagues both approaches as well. This can be prevented by the creation of a<br />
bony ledge medial to the ossicular mass wherein the graft can be placed, or through the use of a silastic<br />
button just lateral to the graft.<br />
Bilateral atresia patients that are either unable or unwilling to undergo surgery have the option of being<br />
fitted with a bone-conducting hearing appliance. Both percutaneous and transcutaneous devices have<br />
been developed; however, only the transcutaneous version is FDA approved. Older devices that are held<br />
to the head by a tight-fitting headband are unsightly and uncomfortable.<br />
Despite the advances that have been made in technique and imaging over the past twenty years, several<br />
issues regarding the timing of surgery in general, when to operate on cases of unilateral atresia, and the<br />
operability of cases with severe craniofacial malformations remain difficult questions. The issue of when<br />
to operate on these patients is a difficult one because many surgeons with considerable experience in this<br />
area maintain such varied opinions. Generally speaking, most would agree that the earliest age at which<br />
to proceed is at 4 to 5 years of age, thereby allowing time for adequate mastoid and middle ear<br />
pneumatization and increasing patient compliance with the postoperative care that is required. Also, most<br />
authors state that in cases of unilateral atresia with evidence of cholesteatoma, infection or with very thin<br />
atresia plates, surgery should be undertaken earlier. However, there are differing opinions regarding<br />
cases of grade II and III unilateral atresia in patients with normal hearing in the other ear. Jahrsdoerfer<br />
finds that the benefit of binaural hearing far exceeds the risk of facial nerve injury and other<br />
complications. De la Cruz also favors operating earlier on unilateral atresias if a good outcome can be<br />
expected based on CT findings. Others, including Crabtree, Bellucci, Glasscock and Fisch, favor waiting<br />
until the patient is of consenting age at which point an individually informed decision can be made. All<br />
points considered, the decision to proceed with early intervention ultimately depends on the experience<br />
of the surgeon and the relative degree of malformation that the individual patient has and with which the<br />
surgeon is comfortable.<br />
In summary, congenital aural atresia is a congenital developmental anomaly of the middle ear that<br />
manifests with varying degrees of external auditory canal stenosis or atresia, ossicular derangements,<br />
http://www.bcm.edu/oto/grand/11295.html (6 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
poorly developed mastoid and tympanic cavities and is characterized by a conductive hearing loss that is<br />
of a moderate to maximal degree. Heritable forms of CAA are found in association with many of the<br />
craniofacial syndromes, but nonheritable, isolated CAA is more frequent. History and physical exam<br />
findings are important in the early identification of the problem complemented by audiometric/ABR<br />
evaluation in order to allow speech development. CT scanning to assess operative potential is then<br />
performed at about 4 years of age, with an approximate yield of 50%. Grading of the patient based on CT<br />
findings has been shown to be predictive of outcome. Success rates of as high as 75% have been reported<br />
with speech reception thresholds of 25dB or less. Historically, a transmastoid approach has been used,<br />
but the problems of stenosis, drainage and long-term care of a mastoid cavity have favored the anterior<br />
approach. Issues regarding the timing of unilateral cases are complex and the decision to operate early on<br />
in these cases ultimately depends on the experience of the surgeon and the degree of malformation<br />
present.<br />
Case Presentation<br />
A 2-year and 9-months-old male, former 36-week premature infant that at birth was noted to have<br />
midfacial and mandibular hypoplasia consistent with the diagnosis of Treacher-Collins Syndrome. The<br />
family history was negative for relatives with craniofacial or auricular malformations. His past medical<br />
history was notable for uncomplicated neonatal jaundice. Medical work-up for congenital cardiac and<br />
renal anomalies was negative. On exam, the patient is noted to have malar hypoplasia, absent zygomatic<br />
arches, hypoplasia of the mandible with Class III occlusion, and bilateral Grade III microtia with aural<br />
atresia. The mastoids, however, are well developed bilaterally. A tracheotomy is present in the neck. The<br />
remainder of the physical exam was unremarkable. Upper airway obstruction secondary to severe<br />
mandibular hypoplasia necessitated elective tracheotomy in the first week of life. A gastrostomy tube<br />
was placed secondary to poor oral intake. At two months of age, he underwent audiometric evaluation<br />
consisting of air and bone conduction multichannel ABR. The patient was fitted with a bone-conducting<br />
type hearing aid at age four months.<br />
Subsequently, the patient underwent repair of his palatal defect at age two, and most recently underwent<br />
bilateral Ilizarov mandibular distraction procedures. After more than two years with his bone-conducting<br />
aids, he has acquired comprehensible speech and a vocabulary comparable to that of children with<br />
normal hearing.<br />
Bibliography<br />
Andrews JC, Anzai Y, Mankovich NJ, Favilli M, Lufkin RB, Jabour B. Three-dimensional CT scan reconstruction for the<br />
assessment of congenital aural atresia. Am J Otol 1992;13:236-240.<br />
http://www.bcm.edu/oto/grand/11295.html (7 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Chang SO, Min YG, Kim CS, Koh TY. Surgical management of congenital aural atresia. Laryngoscope 1994;104:606-<br />
611.<br />
Cole, RR. The "buttock sign" in congenital aural atresia. Otolaryngol Head Neck Surg 1993;109:140-141.<br />
Cole RR, Jahrsdoerfer RA. The risk of cholesteatoma in congenital aural stenosis. Laryngoscope 1990;100:576-578.<br />
Cole RR, Jahrsdoerfer RA. Congenital aural atresia. Clin Plast Surg 1990;17:367-371.<br />
Cressman WR, Pensak ML. Surgical aspects of congenital aural atresia. Otolaryngol Clin North Am 1994;27:621-633.<br />
Fuente del Campo A, Elizondo MM, Arnaud E. Treacher Collins syndrome (mandibulofacial dysostosis). Clin Plast Surg<br />
1994;21:613-623.<br />
Glasscock MR, Jackson CG, Nissen AJ, Schwaber MK. Management of congenital ear malformations. Ann Otol Rhinol<br />
Laryngol 1983;92:504-509.<br />
Granstrom G, Bergstrom K, Tjellstrom A. The bone-anchored hearing aid and bone-anchored epithesis for congenital ear<br />
malformations. Otolaryngol Head Neck Surg 1993;109:46-53.<br />
Hall JW, Morgan SH, Aguilar EA, Mackey J, Jahrsdoerfer RA. Neuro-otologic applications of simultaneous multi-channel<br />
auditory evoked response recordings. Laryngoscope 1994;94:883-889.<br />
Hayes D. Hearing loss in infants with craniofacial anomalies. Otolaryngol Head Neck Surg 1994; 110:39-45.<br />
Jahrsdoefer RA, Hall JW. Congenital malformations of the ear. Am J Otol 1986;7:267-269.<br />
Jahrsdoerfer RA, Garcia ET, Yeakley JW, Jacobson JT. Surface contour three-dimensional imaging in congenital aural<br />
atresia. Arch Otolaryngol Head Neck Surg 1993;119:95-99.<br />
Jahrsdoerfer RA, Worth JW, Aguilar EA, Cole RR, Gray LC. Grading system for the selection of patients with congenital<br />
aural atresia. Am J Otol 1992;13:6-12.<br />
Jahrsdoerfer RA. Congenital atresia of the ear. Laryngoscope 1978;88:1-49.<br />
Jones RL. Smith's Recognizable Patterns of Human Malformation, 4th ed. Philadelphia: Saunders, 1988:709.<br />
Lambert PR. Congenital Aural Atresia. In: Bailey BJ., et al. Head and Neck Surgery - Otolaryngology. Philadelphia, .<br />
Lippincott, 1993:1579-1591.<br />
Mattox DE. Fisch U. Surgical correction of congenital aural atresia of the ear. Otolaryngol Head Neck Surg 1986;94:574-<br />
577.<br />
Molony TB, De la Cruz A. Surgical approaches to congenital atresia of the external auditory canal. Otolaryngol Head<br />
http://www.bcm.edu/oto/grand/11295.html (8 of 9) [5.11.2005 10:40:53]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Neck Surg 1990;103:991-1001.<br />
Pattee GL. An operation to improve hearing in cases of congenital atresia of the external auditory meatus. Arch<br />
Otolaryngol 1947;46:568-580.<br />
Patten BM. Human Embryology. New York: McGraw-Hill, 1968:335-344.<br />
Schuknecht HF. Congenital aural atresia. Laryngoscope 1989;99:908-917.<br />
Shambaugh GE. Surgery of the Ear. Philadelphia: Saunders, 1959:493-523.<br />
Shih L, Crabtree JA. Long-term surgical results for congenital aural atresia. Laryngoscope 1993; 103:1097-1102.<br />
Swartz JD, Harnsberger HR. Imaging of the Temporal Bone. New York: Thieme Medical Publishers, 1992:20.<br />
Portmann M, Guillen G, Richards AE. The Ear and Temporal Bone. New York: Masson, 1979:382-384.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/11295.html (9 of 9) [5.11.2005 10:40:53]
http://www.bcm.edu/oto/grand/111193.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
CONGENITAL INNER EAR MALFORMATIONS<br />
H. Jeff Kim, MD<br />
November 11, 1993<br />
The reported incidence of significant sensorineural hearing loss in young children varies from 1:1000 to<br />
1:2000 depending on the population studies. Approximately 20% of patients with congenital<br />
sensorineural hearing loss have radiographic anomalies of the inner ear.<br />
The structure of the inner ear consists of a membranous labyrinth surrounded by a bony labyrinth within<br />
the petrous temporal bone. The primordium of the membranous labyrinth, which is referred to as the otic<br />
placodes, appears in the third week of gestation as thickened planes of surface ectoderm on either side of<br />
the developing hindbrain. It differentiates into the otic pit and then fuses to become the otic vesicles, or<br />
otocyst, by the fifth week. The otocyst subdivides into two pouches. The ventral portion develops into the<br />
cochlear duct and saccule. The dorsal segment is transformed into the endolymphatic sac and duct,<br />
http://www.bcm.edu/oto/grand/111193.html (1 of 6) [5.11.2005 10:41:02]
http://www.bcm.edu/oto/grand/111193.html<br />
utricle, and semicircular canals. By the 10th week, the adult membranous labyrinth is recognized, and<br />
completely developed by week 26. The bony semicircular canals began at the sixth week and are<br />
complete by week 22. The superior semicircular canals are completed first, followed by the posterior and<br />
finally the lateral. The bony labyrinthine begins in the fourth week as a condensation of mesenchyme and<br />
forms a cartilage capsule around the developing membranous labyrinth. Its ossification begins at week 14<br />
and is completed by week 23. Congenital ear malformation results from a defect in the development of<br />
the membranous labyrinthine, the osseous labyrinthine, or both.<br />
The malformations limiting the membranous labyrinthine cannot be detected radiographically. Complete<br />
labyrinthine dysplasia is very rare, and was first described by Bing and Siebenmann in 1907. It has been<br />
associated with Jervell-Lange Nielson and Usher's syndromes. Cochleosaccular dysplasia was first<br />
described by Schiebe in 1892. It is characterized by a collapse of the cochlear duct and saccule. It is<br />
probably the most common form of inner ear pathology in patients with congenital deafness. The<br />
Alexander's ear deformity, or the cochlear base turn dysplasia, is related to familial high frequency<br />
sensorineural hearing loss.<br />
Jackler has classified cochlear anomalies based on inner ear embryogenesis. The complete labyrinthine<br />
aplasia, known as Michel's deformity, represents an early failure in development correlating to the third<br />
week of gestation. It is extremely rare. The common cavity deformity represents developmental arrest at<br />
the fourth week, and a common cavity of the cochlea and vestibule is formed with internal architecture.<br />
Cochlear aplasia results from the arrested development of the cochlea during the fifth week. The cochlea<br />
fails to form and appears as a single cavity. The vestibule and semicircular canals may be normal or<br />
malformed. Cochlear hypoplasia displays a small, rudimentary cochlea but is associated with a normal or<br />
malformed vestibule and semicircular canals. This lesion is due to an arrest at the sixth week of gestation.<br />
Incomplete partition deformity, also well known as Mondini's deformity, represents a small cochlea with<br />
incomplete or no intrascalar septa. The cochlea is usually flat and has one and one-half turns instead of<br />
the normal two and one-half turns. Arrest of maturation at the gestational seventh week may result in the<br />
Mondini deformity.<br />
The internal auditory canal (IAC) may be enlarged or stenosed. The narrow IAC can be associated with a<br />
failure of the 8th nerve development. Patients with the wide IAC may be predisposed to cerebral spinal<br />
fluid (CSF) leaks, resulting in recurrent meningitis.<br />
Patients with the Mondini deformity and other congenital inner ear malformations are at an increased risk<br />
for developing recurrent meningitis or perilymphatic fistula. They are predisposed to develop a CSF leak<br />
due to the enlarged cochlear aqueduct or an abnormal connection between the internal auditory canal and<br />
the membranous labyrinth.<br />
A thorough clinical, audiological and radiological evaluation should be made of all patients suspected of<br />
having these deformities. Clinical history should include possible exposure to teratogen during<br />
pregnancy, family history of hearing impairment, progression and/fluctuation of the hearing loss, and<br />
associated vestibular symptom. A routine audiologic evaluation is required. Work-ups can be helpful in<br />
determining possible etiology. These include TORCH titers, FTA-ABS, urinalysis, and thyroid function<br />
http://www.bcm.edu/oto/grand/111193.html (2 of 6) [5.11.2005 10:41:02]
http://www.bcm.edu/oto/grand/111193.html<br />
tests. High resolution, computed tomography provides excellent visualization of the bony labyrinthine of<br />
the inner ear.<br />
Patients are advised to avoid contact sports because of the increased risk of CSF leak following minor<br />
head injury. Middle ear infections are treated aggressively because of the increased risk for meningitis.<br />
Genetic counseling is provided after a careful analysis of the family history. Hearing rehabilitation,<br />
including amplification and especially educational efforts, are also indicated.<br />
Currently, cochlear implantation is indicated for bilaterally profound sensorineural hearing loss without<br />
speech discrimination using hearing aids. It is contraindicated in the patient with complete cochlear<br />
aplasia and narrow IAC since neural elements for stimulation would be absent. Further study is required<br />
to evaluate the long-term benefits of cochlear implantation in the congenital inner malformation.<br />
Case Presentation<br />
A patient was referred to Texas Children's Hospital at eight months of age with a history of<br />
developmental delay and no perception to auditory stimuli. She was a term infant, weighing 7 lbs 11 oz<br />
when delivered by Caesarean section due to breech presentation. Her postnatal care was uncomplicated.<br />
The pregnancy was only complicated by a urinary tract infection and hypertension during the third<br />
trimester. She was recently diagnosed with congenital hypotonia, but was otherwise healthy without any<br />
previous ear problems. An ABR demonstrated no response to air or bone conduction click stimuli.<br />
Her family history was only significant for a maternal grandmother with a hearing loss. Physical<br />
examination was unremarkable. Titers were negative for cytomegalovirus, rubella, toxoplasma, and<br />
herpes simples virus. Thyroid function tests were within normal limits. A high resolution temporal bone<br />
CT scan revealed cochlear common cavity deformity.<br />
She was fitted with bilateral behind-the-ear (BTE) hearing aids. Repeat audiogram demonstrated her<br />
aided speech detection threshold to be 60 dB, and a 1000 Hz warble tone at 70 dB. She has been involved<br />
in a total communication program. Her parents noted significant differences in her sound perception with<br />
hearing aids. Currently she has been using a five-word vocabulary.<br />
Bibliography<br />
Brookhouser PE. Sensorineural hearing loss in children. In: Cummings CW, Harker LA, editors. Otolaryngology - Head<br />
and Neck Surgery, 2nd ed. St. Louis: Mosby, 1993:3080-3102.<br />
http://www.bcm.edu/oto/grand/111193.html (3 of 6) [5.11.2005 10:41:02]
http://www.bcm.edu/oto/grand/111193.html<br />
Clarós P, Guirado C, Clarós C, Clarós A Jr, Clavería T, Wienberg P. Association of spontaneous anterior fossa CSF<br />
rhinorrhea and congenital perilymphatic fistula in a patient with recurrent meningitis. Internatl J Pediatr Otorhinolaryngol<br />
1993;27:65-71.<br />
Emmett JR. The large vestibular aqueduct syndrome. Am J Otol 1985;6:387-415.<br />
Gussen R. Middle and inner ear changes in congenital rubella. Am J Otolaryngol 1961;2:314-320<br />
Ilium P. The Mondini type of cochlear malformation: a survey of the literature. Arch Otolaryngol 1972;96:305-311.<br />
Jackler RK, Luxford WM, Brackmann DE, Monsell EM. Endolymphatic sac surgery in congenital malformations of the<br />
inner ear. Laryngoscope 1988;98:698-704.<br />
Jackler RK, Luxford WM, House WF. Congenital malformations of the inner ear: a classification based on embryogenesis.<br />
Laryngoscope 1987;97(Suppl 40):2-14.<br />
Jackler RK, Luxford WM, House WF. Sound detection with the cochlear implant in five ears of four children with<br />
congenital malformations of the cochlea. Laryngoscope 1987;97(Suppl):15-17.<br />
Johnsson L-G, Hawkins JE Jr, Rouse RC, Kingsley TC. Four variations of the Mondini inner ear malformations as seen in<br />
microdissections. Am J Otolaryngol 1984;5:242-257.<br />
Jorgensen MB, Kristensen HK, Buch NH. Thalidomide-induced aplasia of the inner ear. J Laryngol Otol 1964;78:1095-<br />
1101.<br />
Lindsay JR. Profound childhood deafness: inner ear pathology. Ann Otol Rhinol Laryngol 1973;82(Suppl 5):1-73.<br />
Makishima K, Snow JB Jr. Pathologic features of the inner ear in congenital deafness. Arch Otolaryngol 1975;101;600-<br />
604.<br />
Mangabeira-Alberrnaz PL. The Mondini dysplasia - from early diagnosis to cochlear implant. Acta Otolaryngol<br />
1983;95:627-631.<br />
Mangabeira-Albernaz PL, Fukuka Y, Chammas F, Ganança MM. The Mondini dysplasia - a clinical study. ORL J<br />
Otorhinolaryngol Relat Spec 1981;43:131-152.<br />
Mitchell DP, Rubin AM. Mondini dysplasia - late complications. J Otolaryngol 1985;265-267.<br />
Miyamoto RT, McConkey Robbins AJ, Myres WA, Pope ML. Cochlear implantation in the Mondini inner ear<br />
malformation. Am J Otol 1986;7:258-261.<br />
Molter DW, Pate BR Jr, McElvenn JT Jr. Cochlear implantation in the congenitally malformed ear. Otolaryngol Head Neck<br />
Surg 1993;108:174-177.<br />
Murakami Y, Schuknecht HF. Unusual congenital anomalies of the inner ear. Arch Otolaryngol 1968;87:335-349.<br />
http://www.bcm.edu/oto/grand/111193.html (4 of 6) [5.11.2005 10:41:02]
http://www.bcm.edu/oto/grand/111193.html<br />
Nadol JB Jr. Histological considerations in implant patients. Arch Otolaryngol 1984;110:160-163.<br />
Nadol JB Jr, Young Y-S, Glynn RJ. Survival of spiral ganglion cells in profound sensorineural hearing loss: implications<br />
for cochlear implantation. Ann Otol Rhinol Laryngol 1989;98:411-416.<br />
Ohlms LA, Edwards MS, Mason EO, Igarashi M, Alford BR, Smith RJH. Recurrent meningitis and Mondini dysplasia.<br />
Arch Otolaryngol Head Neck Surg 1990;116:608-612.<br />
Otte J, Schuknecht HF, Kerr AG. Ganglion cell populations in normal and pathological human cochleae: implications for<br />
cochlear implantation. Laryngoscope 1978;88:1231-1246.<br />
Paparella MM. Mondini's deafness: a review of histopathology. Ann Otol Rhinol Laryngol 1980;89(Suppl 65):1-23.<br />
Phelps PD. Cochlear implants for congenital deformities. J Laryngol Otol 1992;106:967-970.<br />
Phelps PD. Congenital lesions of the inner ear, demonstrated by tomography: a retrospective study of 34 cases with special<br />
reference to the lateral semicircular canal. Arch Otolaryngol 1974;100:11-18.<br />
Reilly JS. Congenital perilymphatic fistula: a prospective study in infants and children. Laryngoscope 1989;99:393-397.<br />
Sando I, Takahara T, Ogawa A. Congenital anomalies of the inner ear. Ann Otol Rhinol Laryngol 1984;93:(Suppl 112):110-<br />
118.<br />
Schmidt JM. Cochlear neuronal populations in developmental defects of the inner ear. Acta Otolaryngol 1985;99:14-20.<br />
Schuknecht HF. Mondini dysplasia: a clinical and pathological study. Ann Otol Rhinol Laryngol 1980;89:3-23.<br />
Shelton C, Luxford WM, Tonokawa LL, Lo WW, House WF. The narrow internal auditory canal in children: a<br />
contraindication to cochlear implants. Otolaryngol Head Neck Surg 1989;100:227.<br />
Suehiro S, Sando I. Congenital anomalies of the inner ear: introducing a new classification of labyrinthine anomalies. Ann<br />
Otol Rhinol Laryngol 1979;88:2-24.<br />
Supance JS, Bluestone CD. Perilymph fistulas in infants and children. Otolaryngol Head Neck Surg 1983;91:663-671.<br />
Swartz JD, Harnsberger HR. Imaging of the Temporal Bone, 2nd ed. NY: Thieme, 1992;192-246.<br />
Tom LW, Bilaniuk L, Roa RA, Potsic WP. Recurrent meningitis and a congenital perilymph fistula. Ear Nose Throat J<br />
1992;71:287-290.<br />
Tsuzuki T, Kaga K. The relation between motor function development and vestibular function tests in four children with<br />
inner ear anomaly. Acta Otolaryngol 1991;481:443-446.<br />
Wetmore SJ, Herrmann P, Fisch U. Spontaneous cerebrospinal fluid otorrhea. Am J Otol 1987;8:96-102.<br />
http://www.bcm.edu/oto/grand/111193.html (5 of 6) [5.11.2005 10:41:02]
http://www.bcm.edu/oto/grand/111193.html<br />
Zalzal GH, Shott SR, Towbin R, Cotton RT. Value of CT scan in the diagnosis of temporal diseases in children.<br />
Laryngoscope 1986;96:27-32.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/111193.html (6 of 6) [5.11.2005 10:41:02]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for<br />
use by doctors and other health care professionals. These documents were<br />
prepared by resident physicians for presentation and discussion at a<br />
conference held at The Baylor College of Medicine in Houston, Texas. No<br />
guarantees are made with respect to accuracy or timeliness of this material.<br />
This material should not be used as a basis for treatment decisions,<br />
and is not a substitute for professional consultation and/or peerreviewed<br />
medical literature.<br />
Diving Medicine<br />
Brian H. Weeks, M.D.<br />
January 13, 2000<br />
There are about 3.4 million certified scuba divers in the United States. And<br />
about 300,000 become certified per year. About one-third of all divers<br />
experience some diving related medical problem in their careers. The<br />
important thing to remember is that even in healthy divers with safe diving<br />
profiles, there is a 1% to 5% incidence of decompression sickness, which<br />
can be an extremely serious problem.<br />
http://www.bcm.edu/oto/grand/011300.html (1 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
The most common diving related injury involves middle ear barotrauma.<br />
The incidence of vestibular symptoms reaches about 20% among divers in<br />
some studies. Most importantly for this talk, as an otolaryngologist we are<br />
considered the diving experts. So it is quite probable that sometime in our<br />
career we will all see a patient who is a scuba diver.<br />
In literature there are many referrals to breath-hold divers used by kings to<br />
recover treasures for their wealth and fame. In the 17th century an open<br />
diving bell was documented, which was an air-holding chamber that<br />
prolonged possible diving times. In 1810 a copper helmet was designed,<br />
which was sealed to a watertight canvas. This allowed air to be pumped<br />
down from the surface. Today we have a modification of this original design<br />
for very deep hard-hat diving.<br />
In early 1940 Jacques Cousteu designed what was then referred to as the<br />
aqua-lung. Today it is known as the scuba device. Scuba is an acronym for<br />
self-contained underwater breathing apparatus. These were actually initially<br />
used in World War II, but because of their relatively low cost and their<br />
reliability, the apparatus was made available to the everyday diver and for<br />
recreational purposes.<br />
For those unfamiliar with scuba diving, the basic set up involves a tank,<br />
which the diver wears on his back, that delivers pressurized air via a hose<br />
and a mouthpiece, which is known as a regulator. The pressure is<br />
comparable to the aquatic depth that the diver obtains. A demand regulator<br />
either at the tank or at the mouthpiece controls the differential on the<br />
pressure from the tank air to the ambient pressure. The duration of the dive<br />
is limited to the amount of air in the tank as well as to the physiology of the<br />
diver.<br />
The weight of the air at sea level is one atmosphere, so atmospheric<br />
pressure is sea level, which is described as one square inch of air for as far<br />
as the atmosphere extends. Atmospheric pressure is also recorded as 14.7<br />
lb. per square inch or 760 tore. One atmosphere under water is 33 feet of<br />
seawater, which is the equivalent of 34 feet of fresh water. So, there is onefoot<br />
difference in the amount of an atmospheric pressure. Probably the<br />
most important concept to understand is that when a body is submerged in<br />
water, it not only experiences the pressure from the water, but it also<br />
experiences the pressure from the air, which is called absolute pressure -<br />
atmospheric plus water pressure.<br />
As divers, we refer to the gauge pressure, which is really the pressure that<br />
http://www.bcm.edu/oto/grand/011300.html (2 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
is important to us and is the pressure that is exerted by the water alone.<br />
Just for comparison, 18,000 feet into the atmosphere in an airplane is the<br />
equivalent of a half of atmosphere. This gives a perspective as to what we<br />
are looking at from a diving standpoint. As you descend to deeper depths,<br />
33 feet, 66 feet, your absolute pressure is the air pressure plus the water<br />
pressure.<br />
Basic laws govern scuba diving. Probably the most important law to us as<br />
otolaryngologists and divers is Boyle's Law. This law says that at constant<br />
temperature, volume and pressure are inversely related. Since we deal with<br />
air-filled cavities, this is clearly the most common law relating to us as<br />
otolaryngologists. Remember that soft tissue is mostly made of water and is<br />
relatively incompressible compared to air-filled spaces. However the<br />
sinuses and the middle ears are all affected by pressure changes.<br />
Again, a scuba diver breathes air through his tank, through his glottis, which<br />
is delivered to him at one atmosphere pressure. As the diver descends<br />
deeper into the ocean, the pressure increases but the lung volume remains<br />
constant. However, even at deeper depths, inspiration becomes more<br />
difficult because as the density of the molecules changes, it becomes more<br />
difficult to breathe the air. As the diver descends, the pressure increases in<br />
the lungs because depth pressure increases. However, the volume stays<br />
the same. The volume is constant, the density changes and the pressure<br />
changes. The fact that the lung volume stays the same is what protects the<br />
lungs while we are diving.<br />
Breath-hold diving or free diving is a very common sport especially in<br />
Hawaii and along the West Coast. Even snorkeling involves diving using<br />
only mask, fins, and a snorkel. Most of these divers are limited to 1-2<br />
atmospheres of gauge pressure in their depth. Again the thing to remember<br />
with these divers is that their lung volumes will be changing because they<br />
are not using a scuba apparatus to equalize their pressures. At one<br />
atmosphere, the lung volume goes down by ½ and at two atmospheres<br />
their lung volume is reduced by 1/3 again. Those are important concepts to<br />
remember.<br />
The second law is Dalton's Law, which basically says that in a gas mixture,<br />
pressure exerted by each gas is the same as it would exert if it alone<br />
occupied the same volume. So, as you increase the total pressure, the<br />
relative contributions of each gas in the mixture remain the same. If oxygen<br />
is one-third of the mixture at sea level, even if you decrease or descend to<br />
three atmospheres pressure, it still would have an equal contribution. The<br />
contribution of oxygen triples to the total mixture. This is extremely<br />
http://www.bcm.edu/oto/grand/011300.html (3 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
important with the biological effects of gas. The partial pressures of each<br />
individual gas in the tank determine the tissue diffusion and the amount of<br />
gas that is ultimately dissolved in the body tissues and in the blood stream.<br />
Remember that oxygen delivery depends on PO2 and not on total gas<br />
pressure. A good example to illustrate this is that at sea level the PO2 is 16<br />
tore, which is 21% of 760 tore. At 132 feet of seawater, which is four<br />
atmospheres, the PO2 is equivalent to breathing 100% air at sea level. This<br />
shows that even though it has the same amount of concentration at that<br />
depth and the relative contribution is the same, because the pressure is so<br />
much greater, the effects are quite different. This can lead to oxygen<br />
toxicity, because breathing the equivalent of 100% oxygen is very difficult<br />
and very damaging to the body over long periods of time.<br />
The last law of Physics to consider is Henry's Law, which basically says<br />
that given temperature, the mass of the gases dissolved, and the given<br />
volume of solvent is proportional to the pressure of the gas with which it is<br />
at equilibrium. Basically, this law dictates how much of a gas is absorbed at<br />
a given pressure. This is important when we discuss things like nitrogen<br />
narcosis and decompression sickness. Again, this is most important when<br />
applied with nitrogen solubility in the body tissues during descent and then<br />
the relative insolubility when ascent is performed.<br />
Nitrogen narcosis is often called The Rapture of the Deep." And was first<br />
described by Captain Albert Binky, a seaman. He learned that nitrogen<br />
under pressure acts as an anesthetic. At greater depths, there is a greater<br />
force driving nitrogen into the tissues. This is an application of Henry's Law.<br />
Divers themselves refer to another law: Martini's Law. This law states for<br />
every 50 feet of descent, a diver breathing tank air experiences the<br />
equivalent of drinking one martini on an empty stomach. At dives of 100<br />
feet of seawater, or even down to close to 150 feet of seawater, the effect<br />
can be like drinking three mixed drinks with no food in your stomach. This<br />
can become extremely dangerous especially when the diver needs to make<br />
quick decisions and needs to determine exactly what his dive bottom times<br />
should be. Commercial divers who dive much deeper than recreational<br />
divers, often substitute helium in their gas mixtures for nitrogen in order to<br />
limit the anesthetic effect and to allow them to dive deeper without<br />
intoxicating effects.<br />
Ears, sinuses, and the neighboring structures are all susceptible to injury<br />
during diving. The ear and the Eustachian tube are considered to be the<br />
weak links in our body's ability to tolerate diving situations. The<br />
nasopharyngeal opening of the Eustachian tube is usually closed. As we all<br />
know, it opens with positive nasopharyngeal pressure or by contracture of a<br />
http://www.bcm.edu/oto/grand/011300.html (4 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
number of muscles: tensor vallee palantini, lavatar palantini, and the palato<br />
pharyngeus muscles contract and open the nasopharyngeal orifice of the<br />
Eustachian tubes.<br />
In 1937 Armstrong and his colleagues did a very interesting study of<br />
something that is probably obvious to us now. Upon descent with divers he<br />
found that the Eustachian tube acts as a flutter valve and actually is closed<br />
and only opens if the diver equalizes. The Eustachian tube will not open on<br />
its own under these pressures to equalize middle ear pressure. It has to be<br />
reflexive or voluntary, an act made by the diver himself to ensure that his<br />
middle ear pressure is equalized throughout his dive. If pressure is not<br />
equalized, the diver experiences what is commonly called a middle ear<br />
squeeze, which refers to barotrauma of the middle ear. A Valsalva, which<br />
involves holding the nose, closing the mouth and exhaling against a closed<br />
glottis, is one of the techniques used to re-inflate or auto-inflate the middle<br />
ear and equalize the pressures. If divers have upper respiratory infections,<br />
allergies, nasal polyposis or septal deviation, they increase their risk of<br />
middle ear squeeze because of their inability to equalize their pressures.<br />
The most common or simple problem that can occur is occlusion of the<br />
EAC, which can be related to cerumen, ear plugs, or a hood used in cold<br />
water diving. The diver experiences pain during descent because of the<br />
pressure build-up due to the occlusion. On examination of these patients,<br />
we see congestion of the external auditory canal skin and often of the TM<br />
as well, with edema in the canal. There may be rupture of the skin and even<br />
a tympanic membrane perforation from this problem, which will cause<br />
hemorrhage and severe, severe pain. Treatment is conservative: stay out of<br />
the water and do not scuba dive until the area is completely healed.<br />
Probably the most common problem involving the EAC with scuba divers is<br />
otitis externa. This is often due to the water exposure or divers drying their<br />
ears excessively with cotton after a dive. It is a fairly simple problem, and<br />
for a mild case, the patient should use acidified alcohol solution after dives,<br />
often called Swim Ear. There are also silicone oil sprays that divers can<br />
apply to the EAC skin before dives, providing a protective coat.<br />
The most common problem in the middle ear is barotrauma, also known as<br />
aerotitis media or middle ear squeeze. When scuba divers make their<br />
descent, the most critical time is within the first atmosphere. It is most<br />
important that pressure is equalized properly. If pressures are not<br />
equalized, the diver will experience severe otalgia. This can lead to<br />
subsequent tympanic membrane rupture. This can actually occur at even<br />
just a few feet of water and in pressure differences as low as 5 pounds per<br />
http://www.bcm.edu/oto/grand/011300.html (5 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
square inch. With a tympanic membrane rupture, there is often otorrhea<br />
and the diver frequently experiences dizziness and some form of a mild<br />
hearing loss. At surface pressure all pressures are equalized. As a diver<br />
descends, the ambient pressure increases and the pressure in the middle<br />
ear should be equalized through the Eustachian tubes. However, if there is<br />
a block in the Eustachian tubes, the diver can no longer equalize his<br />
pressures. If he continues to submerge or to descend, this pressure will<br />
increase and eventually the weak link in the system will give, which means<br />
that the tympanic membrane will likely rupture. If the diver chooses to return<br />
to the surface he can do so. However, he will continue to experience the<br />
problem and the situation is often even worsened because small amounts<br />
of oxygen are actually absorbed through the middle ear, further increasing<br />
the negative pressure differential in the middle ear and causing further<br />
pressure. Mucosa edema of the middle ear occurs and there is hemorrhage<br />
into the small capillaries. Treatment involves the use of systemic<br />
decongestants and mucolytic agents plus or minus an antihistamine for<br />
patients experiencing allergy. The otolaryngologist should also instruct the<br />
diver to perform periodic auto-inflation if he is not having pain without<br />
movement. If continued pain occurs, it usually indicates a middle ear<br />
infection. At that time, a decision needs to be made whether the patient<br />
would benefit from a myringotomy or PE tube and certainly antibiotics. With<br />
a tympanic membrane perforation, the original treatment is the same as<br />
always: with oral hygiene and ototopical agents, these usually close nonsurgically.<br />
However, tympanoplasty is indicated for persistent perforation.<br />
Divers should be encouraged to concentrate on prevention of these injuries.<br />
A nasal decongestant before a dive can help prevent this sort of problem.<br />
When these medicines are applied to the nose, the position of the head is<br />
very important. The diver should actually have his head down so that the<br />
medicine can reach the Eeustachian tube ostium more easily. Some divers<br />
use systemic decongestants, such as Sudafed, and often add an<br />
antihistamine for allergy. It is very important to remember that these should<br />
be non-sedating medicines and that no new medicines should be given<br />
before a dive unless that have already been tried on the surface.<br />
And, as we have all seen before, Afrin can even have rebound hypercongestion,<br />
which can lead to nasal obstruction. Because this is a delayed<br />
phenomenon, it can happen at depths of maybe 60 or 70 feet below the<br />
surface in the middle of the dive. This can lead to what is known as a<br />
reverse squeeze. That is expansion of the middle ear air, which can lead to<br />
TM distention and perforation, but through the opposite direction - an<br />
increase in the middle ear pressure.<br />
Some divers begin Valsalva and auto-inflation in the middle ear before they<br />
http://www.bcm.edu/oto/grand/011300.html (6 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
even begin their dive. With a very forceful Valsalva, a diver can experience<br />
barotrauma. This is related to an increased intrathoracic and abdominal<br />
pressure, which ultimately increases the CSF pressure via engorged spinal<br />
veins, which can be transmitted to the endolymph, the cochlea, perilymph,<br />
and eventually to the round window and oval window membranes. This<br />
leads to tinnitus and usually a unilateral high frequency hearing loss.<br />
Another preventative measure is the Frenzel maneuver, which involves<br />
holding the nose, closing the glottis and contracting the pharyngeal<br />
muscles. This also forces air into the Eustachian tubes. Some people are<br />
able to perform this to equalize pressure and don't have to use a Valsalva<br />
technique. Other preventive measures include using a feet-first descent.<br />
Multiple studies have shown that it is easier to inflate the middle ear with<br />
the head up, as this causes less hyperemia of the Eustachian tubes and<br />
mucosa. The diver is also less distracted with his head up, and it may help<br />
him to remember to continuously auto-inflate his middle ear every 2-3 feet<br />
as he makes his descent. An anchor line on the boat should also be used to<br />
verify exactly how deep the diver is. If a diver experiences middle ear<br />
squeeze, he should ascend a few feet and attempt to auto-inflate, and then<br />
begin the redescent. It is also important to have a form-fitting mask, so that<br />
nasal compression is easier to perform. Jaw and head movements from<br />
side to side are often used to facilitate middle ear inflation.<br />
One of the more uncommon problems seen in divers is what is known as<br />
ultinebaric facial paralysis. This is extremely uncommon. This is due to<br />
dehiscent portions of the facial nerve, which are vulnerable to barometric<br />
trauma. It is usually seen in normal people who descend during a dive, but<br />
when they ascend and get to the surface, they have a facial paralysis. This<br />
is almost always a transient paralysis and is related to barotrauma. These<br />
divers almost always resume normal function of the facial nerve over time.<br />
Inner ear problems in divers are usually related to middle ear barotrauma.<br />
As we have discussed, middle ear negative pressure causes a depression<br />
of the tympanic membrane. This can be transmitted to the ossicle of the<br />
stapes and cause significant and rapid foot plate depression, which can<br />
tear the sensitive inner ear membranes and lead to the types of hearing<br />
losses we have discussed. The second thing that can occur in the inner ear<br />
is sudden pressure equalization, which can cause a rush of air up the<br />
Eustachian tube, putting an outward force on the tympanic membranes and<br />
the ossicles and pulling the stapes footplate up. This can cause a pressure<br />
wave in the inner ear and distort the inner ear membranes. All these<br />
membranes are extremely fragile. There are multiple theories as to how the<br />
trauma occurs. But it is thought that either Ricener's membrane or the<br />
http://www.bcm.edu/oto/grand/011300.html (7 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
basilar membranes are involved or the vestibule and semi-circular canals<br />
are involved. The shearing force of this rapid fluid movement is transmitted<br />
to the labyrinth and cochlea and can cause tears in the membranes and<br />
hemorrhage from the small torn vessels.<br />
Round window implosion is a well-described problem in the literature from<br />
inner ear trauma during diving. This involves a pull on the stapes footplate<br />
and a shock wave through the scala vestibuli to the scala tympani. It<br />
causes a bulging inward from a rapid pull on the stapes footplate and it<br />
causes an inward pull on the round window membrane, which causes an<br />
implosion injury and the leakage of perilymph into the middle ear. A sudden<br />
pull on the stapes footplate can also lead to a tear of the annular ligament<br />
of the oval window, leading to a crack in the footplate and also leakage.<br />
Frequently when divers are having a difficult time auto-inflating, their first<br />
inclination is to try harder to equalize the pressure. This can lead to the<br />
elevation of the CSF pressure that can be transmitted directly through a<br />
patent cochlear aqueduct into the internal meatus, raising intracochlear<br />
pressure to dangerous levels. The difference between the middle ear and<br />
the perilymph space can cause an explosive outward rupture of the round<br />
window membranes. It is the opposite of the implosion injury, an outward<br />
injury, which can cause perilymph leakage and a perilymph fistula.<br />
Dr. Healy and his colleagues did a study that looked at 40 cases of<br />
perilymph fistula in divers. The patients' chief complaints with this problem<br />
were episodic positional vertigo. They did not have as many complaints of<br />
hearing loss or tinnitus. These patients all underwent surgical exploration.<br />
At exploration, 31 out of 40 of these patients (75% of them) had oval<br />
window leaks, 5 of them had round window leaks, and 4 of them had both<br />
oval window and round window leaks. None of these patients had a hearing<br />
loss for longer than 3 weeks. They regained any significant hearing in those<br />
ears. If the suspicion is high for a perilymph fistula, early exploration leads<br />
to the best hearing restoration. Healy felt that the most important factors<br />
during these procedures were proper magnification, and patience. He<br />
commented that after blotting in the middle ear, it often took 5 to 10 minutes<br />
for perilymph to build back up or for a leak to be revisualized. In two<br />
patients he had to perform bilateral jugular vein compression to enhance<br />
the perilymph leakage.<br />
To summarize, hearing loss and dizziness are indicative of inner ear<br />
barotrauma and require immediate treatment. Depending on the etiology, or<br />
presumed etiology, treatment involves strict bedrest and convalescence, no<br />
coughing, no sneezing, auto inflating or straining. These patients all<br />
deserve an audiogram to determine whether this is a middle ear or an inner<br />
http://www.bcm.edu/oto/grand/011300.html (8 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
ear problem. With inner ear problems with a cochlear etiology, you will see<br />
a non-progressive centrally neural hearing loss. And, as I said, with a<br />
perilymph fistula one way to distinguish it is that there is often a progressive<br />
and fluctuating hearing loss. In the study by Healy, he also found that<br />
posturography with EAC pressure changes have a 97% sensitivity for<br />
diagnosing a perilymph fistula.<br />
Antonelli and his colleagues did a study looking at 18 temporal bones<br />
examined from 11 divers who died from complications during diving, either<br />
from rapid ascent or drowning. He found that bleeding into the middle ear<br />
and mastoid air cells was nearly universal in all these divers. The most<br />
common damage seen was bleeding around Ricener's membrane and the<br />
round window membrane. He also found that a number of these divers,<br />
usually the ones who had rapid ascent injuries, had rupture of both the<br />
utricle and saccule and that tympanic membrane rupture from rapid ascent<br />
was far more common in people who dive than had been presumed. The<br />
other interesting point was that most of the inner ear damage was not<br />
surgically treatable. Other than for the perilymph fistula, most of these<br />
injuries do not have surgical treatments.<br />
Lastly, Zannini and his colleagues followed 160 professional divers with<br />
serial audiograms. He found that these 160 divers had significantly worse<br />
hearing than control divers. The greatest loss was in the group with the<br />
longest diving times. He found that their hearing losses were in the highest<br />
frequencies, usually in the 8 kilohertz. Divers who reported difficulty auto<br />
inflating their middle ears had even worse hearing or the most central<br />
hearing loss. Zannini also commented that perilymph fistula demands early<br />
surgical exploration and that inner ear barotrauma is managed medically<br />
with vasodilators, steroids, histamines, and Carbogen.<br />
There is a different set of problems that divers can experience during<br />
descent which involve the sinuses. This is called aerosinusitis or sinus<br />
squeeze and involves osteomuculuson and pressure equalization. It is<br />
really infrequently an issue in the sinuses but if you have a demitasse<br />
mucosa with an upper respiratory infection, an allergy, a polyp occluding<br />
the ostium or a septal deviation, this can cause a problem and mimic what<br />
happens in the middle ear. You get a negative pressure in the sinuses<br />
because of the inability for the pressures to equalize. This causes a<br />
vacuum, which can lead to mucosal edema, hemorrhage and severe pain.<br />
Management includes sinus irrigation and either endoscopic sinus surgery,<br />
if it is a polyp, or septoplasty to straighten the septum.<br />
Tooth squeeze or aerodontalgia is a very uncommon problem. The most<br />
http://www.bcm.edu/oto/grand/011300.html (9 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
common cause of tooth pain in the diver is from aerosinusitis. But<br />
aerodontalgia can be caused by an air pocket underneath the tooth cap or<br />
filling. It causes severe pain when the diver descends and the pressure<br />
changes. To treat this condition, dental work should be done and the filling<br />
or cap should be replaced.<br />
Facemask squeeze is failure to equalize pressure changes in the facemask.<br />
It can lead to tissue damage from the pressure differential in the mask<br />
along the soft tissues. The most common areas of injury are around the<br />
eyeball and the lining of the eyelids where the mucosa is quite sensitive.<br />
Exhaling through the nose and into the facemask and equalizing the<br />
pressure that way easily prevents facemask squeeze.<br />
Epistaxis is bleeding from the nose into the mask underwater. It is a very<br />
common problem. The bleeding is due to pressure changes on<br />
Keisselbach's plexus. Oftentimes the diver will not even recognize that he<br />
has had a nosebleed. As you move underwater, the selective absorption of<br />
color by the blue green seawater makes blood appear blue green. So<br />
oftentimes the diver will ascend to the surface and then realize that his<br />
mask is full of blood. There is no treatment required. Almost all of these<br />
invariably resolve within minutes of reaching the surface just through<br />
external compression on the nose.<br />
Alternobaric vertigo is another problem seen in divers. This is transient<br />
vestibular dyfunction due to dysequilibrium of pressures in the two middle<br />
ears. It can lead to vertiginous feeling and has been seen in up to 15% to<br />
16% of divers in some series. When you are underwater, any sort of<br />
incoordination or change in equilibrium can be extremely dangerous. These<br />
patients usually have poor auto-inflation and don't usually have any hearing<br />
loss or tinnitus. To correct this problem, the diver should reverse the<br />
direction of movement, allowing the vestibular system to equilibrate.<br />
Another way to correct this involves auto-inflating the middle ear to equalize<br />
the pressures.<br />
Finally, unequal caloric stimulation vertigo is a problem seen when cold<br />
water enters only one ear (due to either an external canal obstruction or a<br />
hood). It is like a caloric stimulation test. The best way to treat this is by<br />
removing the obstruction so that both of the ears are sensing the cold water<br />
at the same time.<br />
Anxiety is the most common cause of dizziness in the diver. It is actually not<br />
due to the vestibular system. There are multiple studies that say that<br />
http://www.bcm.edu/oto/grand/011300.html (10 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
greater than 50% of all scuba deaths are due to panic or anxiety in the<br />
diver. Treatment would include educating yourself properly before you<br />
scuba dive. Go through proper certification and never dive alone.<br />
TMJ syndrome is caused by forcefully biting down on the regulator. This is<br />
frequently seen in novice divers who become anxious and excited and then<br />
bite down. It is treated just like any other treatment of TMJ, with<br />
reassurance, heat, NSAIDS and a soft diet<br />
There are other problems that divers may encounter that are associated<br />
with ascent. These are pulmonary rather than pressure accidents and these<br />
are very serious problems. These are all caused by holding of the breath<br />
during ascent and can be predisposed in patients with obstructive lung<br />
disease. At the surface, the pressures are all equal. As we descend, the<br />
ambient pressure increases and the lung pressure increases as well. As we<br />
are breathing, the pressures all stay equal because of our scuba apparatus.<br />
However, if we don't breath during the ascent, the pressure in the lungs<br />
stays high and the pressure on the outside stays low. The lung pressures<br />
are higher than ambient pressure and this pressure has to go somewhere.<br />
The first one is mediastinal emphysema, which is caused by local air<br />
trapping with escaping alveolar air dissecting along the bronchi into the<br />
mediastinum. This can lead to neck and chest discomfort, and shortness of<br />
breath. We have all seen what subcutaneous emphysema looks like in the<br />
soft tissues of the neck. The treatment for this is 100% oxygen, expectant<br />
management and, if the airway becomes an issue, that needs to be treated<br />
emergently.<br />
The second thing is pneumothorax, which is caused by air from alveoli<br />
rupturing into the pleural cavity. It is sudden and rapid and causes<br />
shortness of breath and labored breathing and can actually be lifethreatening<br />
underwater. The treatment is a chest tube. On a boat, or out in<br />
the water when a chest tube is not available, a large bore needle with a<br />
condom or a piece of plastic can substitute as a one way air valve to<br />
ventilate the air pressures. These patients need to be put on 100% oxygen<br />
immediately and, for this type of pneumothorax, patients should undergo<br />
chamber recompression.<br />
The most serious problem that occurs in diving is an air embolism, a<br />
devastating problem that can lead to neurologic complications. This occurs<br />
when alveoli and pulmonary blood vessels rupture and air bubbles get to<br />
the blood stream and then track to the body. If these end up in the cerebral<br />
http://www.bcm.edu/oto/grand/011300.html (11 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
circulation they can coalesce to form larger bubbles and actually entirely<br />
block the cerebral circulation. These divers usually experience loss of<br />
consciousness after surfacing. Frequently, while still in the water, they have<br />
frothy, bloody sputum and complain of chest pain, confusion, and blurry<br />
vision. These patients need to be transferred immediately to recompression<br />
chambers and frequently need treatment in these chambers intermittently<br />
for up to 2 weeks. If you are ever with a diver and suspect air embolism, the<br />
diver needs to be transported in the left lateral decubitus position. Air rises,<br />
so we want them in the left lateral decubitus to prevent a bubble from<br />
blocking the left ventricular outflow track. They also need 100% oxygen.<br />
Another issue is air evacuation, since flying in an airplane or at elevation<br />
can cause an increased bubble formation in the body. However, if the issue<br />
is getting the patient to a recompression chamber as quickly as possible,<br />
then the risk is usually warranted, as opposed to taking them by ground.<br />
Not holding the breath, and just breathing normally as the ascent is made<br />
will prevent air embolism. Also, make sure that patients with obstructive<br />
lung disease do not scuba dive.<br />
Case Presentation<br />
The patient is a 25-year-old male with extensive SCUBA diving experience<br />
who was on a dive with friends. The patient was nearing the end of his dive<br />
and noted his gauge air pressure to be at 500 psi. He began to surface<br />
when, at 50 fsw depth, he begun to breathe 'heavy air', indicating a lack of<br />
adequate remaining air in his scuba tank. He emergently descended to his<br />
dive buddy at 80 fsw depth and began to share his companion's air. During<br />
his emergent re-descent, he noted severe otalgia while failing to equalize<br />
his middle ear pressure. Upon reaching the surface, the patient noted leftsided<br />
bloody otorrhea and rhinorrhea. He also experienced mild dizziness.<br />
On subsequent otolaryngologic exam, the patient had a 25% left tympanic<br />
membrane perforation. His dizziness had completely resolved. He was<br />
treated with ototopic agents and aural hygiene, and had complete closure<br />
of his perforation on 1-month follow-up.<br />
Bibliography<br />
Antonelli PJ, Adamczyk M, Appleton CM, Parell GJ. Inner ear barotrauma after<br />
stapedectomy in the guinea pig. Laryngoscope 1999;109:1991-1995.<br />
Antonelli PJ, Parell GJ, Becker GD, Paparella MM. Temporal bone pathology in scuba<br />
diving deaths. Otolaryngol Head Neck Surg 1993;109:514-521.<br />
http://www.bcm.edu/oto/grand/011300.html (12 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
Arthur DC, Margulies RA. A short course in diving medicine. Ann Emerg Med<br />
1987;16:689-701.<br />
Becker GD, Parell GJ. Medical examination of the sport scuba diver. Otolaryngol Head<br />
Neck Surg 1983;91:246-250.<br />
Becker GD, Parell GJ. Otolaryngologic aspects of scuba diving. Otolaryngol Head Neck<br />
Surg 1979;87:569-571.<br />
Camporesi EM. Diving and pregnancy. Semin Perinatol 1996;20:292-302.<br />
Crockett AT, Pauley SM, Zehl DN, Pilmanis AA, Cockett WS. Pathology of the bends<br />
and decompression sickness. Arch Surg 1979;114:296-301.<br />
Edge CJ, Grieve AP, Gibbons N, O'Sullivan F, Bryson P. Control of blood glucose in a<br />
group of diabetic scuba divers. Undersea Hyperb Med 1997;24:201-207.<br />
Eichel BS, Landes BS. Sensorineural hearing loss caused by skin diving. Arch<br />
Otolaryngol 1970;92:128-131.<br />
Fields JA. Skin diving: its physiological and otolaryngological aspects. Arch Otolaryngol<br />
1958;86:531-541.<br />
Harrill WC, Jenkins HA, Coker NC. Barotrauma after stapes surgery: a survey of<br />
recommended restrictions and clinical experiences. Am J Otol 1996;17:835-845.<br />
Miller JM, Axelsson A, Potter W. Chronic effects of phasic middle ear pressure changes.<br />
Ann Otol Rhinol Laryngol 1981;90:281-286.<br />
Parell GJ, Becker GD. Conservative management of inner ear barotrauma resulting from<br />
scuba diving. Otolaryngol Head Neck Surg 1985;93:393-397.<br />
Reuter SH. "No decompression" dive tables explained. Undersea J 1971;5:6-9.<br />
Reuter SH. Dive table rearrangement and simplification. Third International Conference<br />
on Underwater Education. Nation Association of Underwater Instructors, Dallas, TX,<br />
September 1971.<br />
Reuter SH. Medical management of near-drowning victims. Physician's Newsletter, St.<br />
Joseph Hospital. August 1982.<br />
Reuter SH. Ninety-five percent of divers' ear problems start in the Eustachian tube. Clin<br />
Trends Ophthalmol Allergy. 1971;10:8.<br />
Reuter SH. Scuba diving and respiratory problems. McGovern Allery Clinic Newsletter.<br />
http://www.bcm.edu/oto/grand/011300.html (13 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
Summer 1988.<br />
Reuter SH. Three means of preventing barotrauma of the ear in scuba divers. Med<br />
Tribune Med New 1971;12:23.<br />
Reuter SH. Underwater medicine: otolaryngologic considerations of the skin and scuba<br />
diver. In: Paparella MM, editor. Otolaryngology, 3rd ed. Philadelphia: Saunders; 1991.<br />
Pp. 3231-3257.<br />
Simmons FB. Theory of membrane breaks in the sudden hearing loss. Arch Otolaryngol<br />
1968;99:41-48.<br />
Strauss RH, ed. Diving Medicine. New York: Grune & Stratton; 1976.<br />
Taylor GD. The otolaryngologic aspects of skin and scuba diving. Laryngoscope<br />
1959;69:829-858.<br />
Tirpitz D, Schipke JD. Delayed recompression after SCUBA diving-induced barotrauma:<br />
a case report. Aviat Space Environ Med 1996;67:266-267.<br />
Wilson HL. Otolaryngologic complications of skin and scuba diving. Their causes and<br />
treatment. Trans Pac Coast Otoophthalmol Soc Annu Meet 1974;55:61-76.<br />
Wolf SL, Twarog F, Weiler JM, Barron RJ, Lang DM, Wells JH, et al. Discussion of risk<br />
of scuba diving in individuals with allergic and respiratory diseases: SCUBA<br />
Subcommittee. J Allergy Clin Immunol 1995;96:871-873.<br />
Zannini D, Odalglia G, Sperati G. Audiographic changes in professional divers.<br />
Proceedings of the Fifth Symposium on Underwater Physiology. Freeport, British<br />
Bahamas;August 1972.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCM Otolaryngology Home Page<br />
©2001, The Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences,<br />
Baylor College of Medicine<br />
http://www.bcm.edu/oto/grand/011300.html (14 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor: Allergic Rhinitis<br />
One Baylor Plaza, NA102, Houston, TX 77030 oto@bcm.tmc.edu<br />
URL: http://www.bcm.tmc.edu/oto (Modified: 12/11/01)<br />
http://www.bcm.edu/oto/grand/011300.html (15 of 15) [5.11.2005 10:41:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by<br />
doctors and other health care professionals. These documents were prepared by<br />
resident physicians for presentation and discussion at a conference held at The<br />
Baylor College of Medicine in Houston, Texas. No guarantees are made with<br />
respect to accuracy or timeliness of this material. This material should not be used<br />
as a basis for treatment decisions, and is not a substitute for professional<br />
consultation and/or peer-reviewed medical literature.<br />
Eustachian Tube Function and Dysfunction<br />
July 11, 1996<br />
Ronald B. Kuppersmith, M.D.<br />
The eustachian tube is an 3-4 cm tubular structure which links two of the major<br />
areas of interest in our specialty, the nose and the ear. Dysfunction of the<br />
eustachian tube causes many common symptoms that present to our clinics, and<br />
may have important management implications. This presentation will consists of a<br />
review of the history, anatomy and physiology of the eustachian tube, and the role<br />
of the eustachian tube in clinical situations.<br />
History<br />
The first description of the eustachian tube is attributed to Alcmaceon of Sparta in<br />
http://www.bcm.edu/oto/grand/71196.html (1 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
400 BC. It was his belief that the eustachian tube allowed goats to breath through<br />
their ears as well as their noses.<br />
In 1562, Bartolomeus Eustachius, the Chair of Anatomy in Rome, published the<br />
first detailed description in his thesis Epistola de Auditus organis, accurately<br />
describing the structure, course, and relations eustachian tube.<br />
Antonio Valsalva, Professor of Anatomy at Bologna, applied the name "Eustachian<br />
Tube" to the pharyngotympanic tube, which was described by Eustachius.<br />
In 1724, around the time of Valsalva, Edme-Gilles Guyot, a postmaster at<br />
Versailles, described the technique of eustachian tube catheterization. He<br />
succeeded in relieving his own deafness by passing a curved pewter tube through<br />
his mouth into the opening.<br />
Since that time many noted otolaryngologists, including Drs. Politzer, Bezold, and<br />
Bluestone, have contributed significantly to our understanding of the intricacies of<br />
eustachian tube anatomy and function, and management of the various disorders<br />
that it is embroiled in.<br />
Development and Anatomy<br />
Understanding the development and anatomy of the eustachian tube provides<br />
insight into its role in several pathologic processes.The eustachian tube develops as<br />
a persistence of the first pharyngeal pouch. At 10 weeks post conception only the<br />
epithelial lining of the lumen has differentiated. Between the 10th and 12th weeks<br />
post conception the levator veli palatini and tensor veli palatini muscles develop.<br />
At 14 weeks the tensor tympani muscle becomes apparent, cartilage differentiation<br />
begins and rugae begin to develop within the tube.<br />
The tube increases in length from 1 mm at 10 weeks post conception to 13 mm at<br />
birth. Also, the angle between the eustachian tube and the skull base is 10 degrees<br />
at birth.<br />
This is in contrast to the adult length of 35 mm and angle of 45 degrees in adults.<br />
Vertical development of the skull, and increases in the angle of the skull base,<br />
allow the eustachian tube to reach its adult length and angle by age 7.<br />
Basic Anatomy<br />
In the adult, the eustachian tube can be visualized as two truncated cones attached<br />
at their narrowed ends. It runs from the middle ear to the nasopharynx and is<br />
http://www.bcm.edu/oto/grand/71196.html (2 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
approximately 31-38 mm in length. Its lumen is roughly triangular and has average<br />
diameter of 2-3 mm. The lumen is lined by ciliated psuedostratified, columnar<br />
epithelium, which sweeps material from the middle ear to the nasopharynx.<br />
Mucous glands predominate near the pharyngeal orifice, and there is a gradual<br />
change to a mixture of goblet, columnar, and ciliated cells as the middle ear is<br />
approached.<br />
The eustachian tube is composed of an osseous and a cartilaginous portion. The<br />
osseous eustachian tube or protympanum measures 11 to 14 mm and extends from<br />
the anterior and medial portion of the petrous temporal bone. Its orifice is oval<br />
shaped, measures 5 x 2 mm and is located above the floor of the middle ear space.<br />
When healthly, the osseous portion of the eustachian tube is always patent. The<br />
cartilaginous portion measures 20-25 mm and opens into the nasopharynx<br />
approximately 10 mm above the plane of the hard palate. The cartilage protrudes<br />
into the nasopharynx, and the protruding portion is known as the torus tubarius.<br />
The fossa of Rosenmuller is this area in the nasopharynx superior to the torus<br />
tubaris.<br />
The cartilaginous portion is composed of one main piece of cartilage and can be<br />
accompanied by several accessory cartilages. Its composition and elasticity is<br />
similar to that found in the pinna and nose. It is attached at the sphenoid sulcus on<br />
the base of skull superiorly and its anteriomedial end is attached to a small tubercle<br />
on the posterior edge of the medial pterygoid plate.<br />
Blood Supply and Innervation<br />
The blood supply to the eustachian tube is from branches of the internal maxillary<br />
artery, ascending pharyngeal artery, and the ascending palatine artery. Sensory and<br />
motor innervation of the eustachian tube is provided by a branch from the otic<br />
ganglion, sphenopalatine nerve, and the pharyngeal plexus, predominately through<br />
branches of the glossopharyngeal nerve. Sympathetic branches reach the eustachian<br />
tube from the sphenopalatine ganglion, otic ganglion, glossopharyngeal nerve,<br />
petrosal nerves, and the carticotympanic nerve. Parasympathetic innervation is<br />
from the tympanic branch of the glossopharyngeal nerve. The multiple nerves<br />
innervating the eustachian tube, may be a source for referred pain to other anatomic<br />
regions of the head and neck.<br />
Muscles of the Eustachian Tube<br />
There are four muscles associated with the eustachian tube. These include the<br />
tensor veli palatini, levator veli palatini, salpingopharyngeus, and the tensor<br />
tympani.<br />
http://www.bcm.edu/oto/grand/71196.html (3 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
The tensor veli palatini is composed of two distinct bundles of muscle fibers<br />
mediolateral to the tube. The lateral bundle takes its origin from the scaphoid fossa,<br />
and the lateral osseous ridge of the sulcus tubae for the course of the eustachian<br />
tube. It descends anteriorly and lateral and inferiorly, to converge in a tendon<br />
which passes around the hamulus and inserts on the posterior border of the<br />
horizontal process of the palatine bone and into the palatine aponeurosis of the<br />
velum.<br />
The medial most portion of the tensor veli palatini originates on the lateral<br />
membranous wall of the eustachian tube and blends with the lateral bundle of the<br />
tensor veli palatini. This medial portion of the tensor veli palatini, referred to as the<br />
dilator tubae muscle, is probably responsible for active dilation of the eustachian<br />
tube by inferolateral displacement of the membranous wall.<br />
The levator veli palatini arises from the inferior aspect of the petrous apex, passes<br />
inferomedially, paralleling the tubal cartilage, and attaches to the dorsal surface of<br />
the soft palate. It is thought to assist in active dilation and provide support.<br />
The salpingopharyngeus arises from the medial and inferior portion of the<br />
eustachian tube and descends posterior and inferior to blend with the<br />
palatopharyngeus muscle. Its physiologic function is undefined.<br />
The tensor tympani muscle arises from fibers common to the tensor veli palatini.<br />
The tendon of the tensor tympani rounds the cochleaform process and inserts into<br />
the manubrium of the malleus. It is not thought to play a role in eustachian tube<br />
function.<br />
Normal Function<br />
The normal eustachian tube is functionally collapsed at rest, with slight negative<br />
pressure present in the middle ear. It opens during swallowing, sneezing, and<br />
yawning. The eustachian tube is thought to close through passive reapproximation<br />
of the tubal walls by extrinsic forces and recoil of the elastic fibers.<br />
The eustachian tube has three functions: ventilation, drainage, and protection.<br />
When the eustachian tube is patent it allows ventilation of the middle ear and<br />
equalization of middle ear and atmospheric pressure. It also allows the middle ear<br />
to clear unwanted secretions. By staying physiologically obstructed, it protects the<br />
middle ear from nasopharyngeal secretions and sound.<br />
Conditions interfering with normal eustachian tube function cover the pathologic<br />
spectrum from benign to malignant. Resultant middle ear complications can be the<br />
http://www.bcm.edu/oto/grand/71196.html (4 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
primary condition that the clinician needs to address, may be a sign of something<br />
more serious, or may have implications that will affect the outcome of surgical<br />
interventions.<br />
Eustachian Tube Dysfunction<br />
Bluestone has classified eustachian tube disorders into obstructive disorders, and<br />
disorders of abnormal patency.<br />
Obstructive disorders can be mechanical or functional. Mechanical obstruction can<br />
be intrinsic due to intraluminal factors such as mucosal inflammation due to allergy<br />
or infection, or extrinsic obstruction resulting in compromise of the lumen.<br />
Extrinsic obstruction can be physiologic such as when the patient is supine, or may<br />
be caused by a mass lesion such as a neoplasm or an adenoidal mass.<br />
Functional obstruction results from persistent collapse of the eustachian tube due to<br />
increased tubal compliance, an abnormal opening mechanism, or both. Functional<br />
obstruction is more common in infants and young children, and in many cases can<br />
be related to normal or abnormal developmental factors.<br />
Evaluating Eustachian Tube Function<br />
There are many methods for evaluating the condition of the eustachian tube, which<br />
reflect its deep location and complex physiology.<br />
IN THE CLINIC<br />
During the physical examination, otoscopy, pneumatic otoscopy, indirect<br />
nasopharyngoscopy, and endoscopy of the nasopharynx can provide clues to the<br />
condition of the eustachian tube.<br />
Several maneuvers can be easily performed in clinic that may indicate patency of<br />
the eustachian tube. These include the Valsalva test, the Toynbee test, the Politzer<br />
test, and eustachian tube catheterization.<br />
The Valsalva test is performed by visual inspection of the tympanic membrane<br />
while the eustachian tube and middle ear are inflated by a forced expiration with<br />
the mouth closed and the nose occluded by the thumb and forefinger. The test is<br />
positive when an intact tympanic membrane is observed moving, or by air heard<br />
through a perforated TM. A positive valsalva test only indicates an anatomically<br />
patent and probably distensible eustachian tube.<br />
http://www.bcm.edu/oto/grand/71196.html (5 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
The Politzer test is performed by visual inspection of the tympanic membrane<br />
while compressing one naris into which the end of a rubber tube attached to an air<br />
bag has been inserted while the opposite naris is compressed with digital pressure.<br />
The patient is asked to repeat the letter K or to swallow while air is injected into the<br />
nasal cavity. When positive, the overpressure that develops in the nasopharynx is<br />
transmitted to the middle ear, and only indicates an anatomically patent ET tube.<br />
Both the Politzer and Valsalva test may be beneficial as a temporary treatment of<br />
effusion or high negative middle ear pressure.<br />
The Toynbee Test is performed by visual inspection of the tympanic membrane<br />
while the patient swallows with their nose manually occluded. This generates a<br />
positive pressure within the nasopharynx, followed by a negative pressure phase<br />
and is considered positive when there is an alteration in middle-ear pressure as<br />
assessed by pneumatic otoscopy before and after the maneuver. Negative middleear<br />
pressure or temporary negative middle ear pressure followed by return to<br />
ambient pressure after the Toynbee test usually is indicative of normal eustachian<br />
tube function. This is in contrast to the Politzer and Valsalva tests which only test<br />
patency. The results of this maneuver can often be equivocal, since several studies<br />
have shown that a significant portion of normal adults and children can not open<br />
their eustachian tubes with this maneuver, and patients with patulous eustachian<br />
tube often can not maintain a negative pressure within their middle ears.<br />
Eustachian tube catheterization can be performed, and also can indicate eustachian<br />
tube patency.<br />
Radiographic evaluation includes computed tomography, and magnetic resonance<br />
imaging. The use of contrast materials to evaluate patency has been described in<br />
the past, but is infrequently used today.<br />
IN THE LAB<br />
There are several more complex methods of evaluating eustachian tube function<br />
that have been described and most involve the use of manometry, sonometry, of<br />
tympanometry. Besides tympanometry most of these tests require complex<br />
equipment, and are mainly used in a research setting.<br />
Non-intact Tympanic Membrane Tests<br />
●<br />
●<br />
●<br />
The Inflation-Deflation test<br />
Forced Response test<br />
clearance test<br />
http://www.bcm.edu/oto/grand/71196.html (6 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Intact Tympanic membrane tests<br />
●<br />
●<br />
●<br />
pressure chamber technique<br />
sonometry<br />
tympanometry<br />
Clinical Examples Of Eustachian Tube Dysfunction<br />
Here are a small sample of the clinical scenarios where eustachian tube dysfunction<br />
is important:<br />
OTITIS MEDIA WITH EFFUSION<br />
Obstruction may result in persistent high negative middle-ear pressure. If pressure<br />
equalization does not occur, atelectasis of the tympanic membrane-middle ear,<br />
sterile otitis media with effusion, or both can occur. If the negative pressure is<br />
overcome, it can aspirate secretions from the nasopharynx resulting in an acute<br />
otitis media.<br />
Serous otitis media with effusion can result from either inadequate ventilation of<br />
the middle ear or from reflux of unwanted nasopharyngeal secretions into the<br />
middle ear. Both types of eustachian tube dysfunction can result in otitis media,<br />
abnormal patency and obstruction.<br />
This is common in children and infants probably due to the configuration of their<br />
eustachian tube, shorter length, and lower efficiency of their tensor veli palantini.<br />
While serous otitis media is something that many of us treat on a daily basis, Dr.<br />
Gacek of Syracuse reminds us, in an article entitled "A Differential Diagnosis of<br />
Unilateral Serous Otitis Media", of the potentially serious nature of this condition.<br />
Clinicians need to maintain a high index of suspicion, particularly in adults, in<br />
unilateral cases, and in persistent or recurrent cases. From Dr. Gacek's article, it is<br />
important to remember:<br />
1. The eustachian tube lumen can be obstructed and this is usually from<br />
inflammatory, allergic or functional disorders.<br />
2. The nasopharynx is usually obstructed by adenoid hypertrophy, but<br />
extensive nasal polyposis, benign neoplasms, and malignant neoplasms also<br />
may present in this location.<br />
3. Obstruction may occur from laterally in the infratemporal fossa, by<br />
parapharyngeal space masses and neoplasms, or skull base lesions.<br />
http://www.bcm.edu/oto/grand/71196.html (7 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
4. Medial obstruction from the petrous apex may be caused by solid or cystic<br />
lesions, including congenital epidermoids, cholesterol granulomas,<br />
neurofibromas, internal carotid artery aneurysms and other rare petrous apex<br />
lesions.<br />
5. Effusion of CSF from the middle ear and mastoid caused by temporal bone<br />
trauma, surgery, or congenital defects may mimic otitis media with effusion<br />
and must be remembered as part of the differential diagnosis.<br />
Dr. Gacek reinforces the importance of a thorough head and neck examination<br />
including the nasopharynx, CT scan of the head including the neck, and<br />
myringotomy as the minimal workup in any pediatric or adult patient with<br />
unilateral recurrent or persistent serous otitis media without an obvious explanation<br />
for eustachian tube obstruction.<br />
He also emphasizes that in pediatric patients, the eustachian tube lumen and<br />
nasopharynx are the anatomic locations most frequently responsible, but congenital<br />
CSF leaks should be suspected in patients with a history of meningitis, or if the<br />
fluid after myringotomy resembles CSF.<br />
In adults, all levels should be suspected.<br />
NASOPHARYNGEAL CARCINOMA<br />
Patients with nasopharyngeal carcinoma frequently have complications that relate<br />
to their eustachian tube. The frequently present with serous otitis media. Also, highdose<br />
radiation therapy, the treatment for nasopharyngeal carcinoma, causes edema,<br />
vasodilation, mucosal damage, and fibrosis of the eustachian tube and middle ear<br />
resulting in damage to the middle ear contents and poor middle ear ventilation.<br />
While it seems intuitive that serous otitis media with effusion in patients with<br />
nasopharyngeal carcinoma would be caused by mechanical obstruction of the<br />
pharyngeal orifice of the eustachian tube, several studies question whether<br />
nasopharyngeal tumors, actually obstruct the lumen of the eustachian tube, and<br />
instead propose that eustachian tube dysfunction and resulting otitis media with<br />
effusion is caused by infiltration of the tensor veli palatini muscle.<br />
With regard to patients after radiation, a study by Hsu, et al, in 1995, showed that<br />
95% of 38 eustachian tubes were patent prior to radiotherapy, 34% where patent at<br />
6 months after radiotherapy, and 60% were patent at 5 years after radiotherapy<br />
using the passive opening test. They also showed decreased dynamic function and<br />
clearance at six months after radiotherapy and improved at 5 years. They attributed<br />
these findings to inflammation caused by radiation rather than tumor obstruction.<br />
http://www.bcm.edu/oto/grand/71196.html (8 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Electromyographic evaluation of the tensor veli palatini in patients with<br />
nasopharyngeal carcinoma status post radiation indicated neurogenic paralysis.<br />
These authors have also found that in patients treated with ventilation tube insertion<br />
for post-irradiation OME tend to develop a chronic draining ear, and deterioration<br />
of hearing. They suggest myringotomy, avoidance of ventilating tubes, and<br />
frequent local treatment of infections of the nose, sinuses, and nasopharynx to<br />
avoid this outcome.<br />
PATULOUS EUSTACHIAN TUBE<br />
Patulous eustachian tubes often present a frustrating problem for patients and<br />
clinicians.The incidence is reported to be between 0.3-6.6% of the general<br />
population.<br />
Patients with patulous eustachian tubes complain of aural fullness, humming<br />
tinnitus, and autophony. They also may hear their own breath sounds, which is<br />
known as tympanophonia. The sound is synchronous with nasal respiration and<br />
resolves when the patient is supine or when upper respiratory tract inflammation<br />
occurs. The sounds may be aggravated by mastication.<br />
Symptoms are usually absent when the patient is supine or relieved when the<br />
patient bends forward with the head between the knees. For this reason, patients<br />
should not be examined in a supine position. Physical examination may reveal a<br />
tympanic membrane that moves during forced breathing through one nostril, and an<br />
amorphic sound may be heard using a diagnostic tube in the patient's ear.<br />
The eustachian tube is usually closed, and closure is maintained by the elasticity of<br />
its cartilage, mucosal lining, surrounding muscles and fat. Alteration of any of<br />
these anatomic components may cause patulous eustachian tubes.<br />
Conditions associated with patulous eustachian tubes include: radiation therapy,<br />
hormonal therapy, pregnancy, nasal decongestants, fatigue, stress, and weight loss.<br />
Patulous eustachian tubes in the most severe form may be patent at all times,<br />
whereas a less severe form has been reported, where the tube is anatomically closed<br />
at rest, but may open easily during exercises or in association with a decrease in<br />
peritubal extracellular fluid.<br />
Many patients can be treated with simple reassurance after a thorough history and<br />
physical examination. Treatment or removal of underlying factors may reverse the<br />
problem. Such as weight gain by patients who have lost weight.<br />
http://www.bcm.edu/oto/grand/71196.html (9 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Many medical regimens have been described including agents which produce<br />
intraluminal and extraluminal swelling, including: insufflation of boric acid and<br />
salicylate powder as described by Bezold, application of nitric acid and phenol, oral<br />
administration of saturated solution of potassium iodide (10 drops in juice TID),<br />
premarin nasal spray (25 mg in 30 cc NS).<br />
New medications are currently under investigation including a herbal combination<br />
being evaluated in Japan, and a medication reported Dr. DiBartolomeo of Santa<br />
Barbara, California that is composed of chlorobutanol, benzyl alcohol, diluted<br />
hydrochloric acid, and propylene glycol. In the initial report, complete elimination<br />
of symptoms was reported by 8 of 10 patients. This formulation was derived from<br />
chlorinated pool water based on the observation that several patients had eustachian<br />
tube congestion proportional to the frequency of time they spent in a public pool. In<br />
letter to the editor in American Journal of <strong>Otology</strong>, Dr. DiBartolomeo indicated<br />
that the medication was held up with the FDA.<br />
In patients who do not improve with medical therapy and who want further<br />
treatment, several surgical interventions have been used including<br />
electrocauterization of the eustachian tube orifice, peritubal injection with gelfoam,<br />
paraffin, avitene, or teflon paste, transposition of the tensor veli palatini muscle<br />
medial to the pterygoid hamulus, myringotomy with ventilation tube placement,<br />
and insertion of an indwelling catheter and subsequent ventilation tube placement.<br />
Catheter placement is through either an anterior tympanomeatal flap or through a<br />
myringotomy.<br />
The close anatomic relationship of the eustachian tube and the carotid artery should<br />
be noted by clinicians who plan inject materials into the eustachian tube orifice, as<br />
injection of telfon paste into the carotid artery has been reported.<br />
HYPERBARIC OXYGEN THERAPY<br />
Another clinical situation where proper eustachian tube function is important is in<br />
the use of hyperbaric oxygen therapy, particularly in patients who require multiple<br />
sessions.<br />
Hyperbaric oxygen therapy involves intermittent inhalation of 100% oxygen under<br />
greater than 1 atmosphere of pressure and is being used increasingly in patients<br />
with decompression sickness, osteomyelitis, carbon monoxide poisoning, crush<br />
injuries, radiation necrosis, and poorly healing wounds. Many of these patients<br />
develop otalgia and aural fullness that may be long-standing. Reports in the<br />
literature indicate that the incidence of middle ear barotrauma ranges from 5% to<br />
http://www.bcm.edu/oto/grand/71196.html (10 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
28% of all patients.<br />
Fernau, et al suggest patients should be taught clearing techniques such as the<br />
Valsalva or Politzer maneuver, supplemented with topical and/or systemic<br />
decongestants, subjected to slower compression rates, or possibly have ventilation<br />
tubes placed.<br />
In a study of 33 patients undergoing hyperbaric oxygen therapy by Fernau, et al. in<br />
1992, 82% of patients developed fullness in their ears, 52% developed serous otitis<br />
media, and 21% developed otalgia requiring ventilation tubes. Of 11 patients<br />
managed with decongestants,10 patients resolved their effusion and pain and did<br />
not require further therapy. 45% of 33 patients had evidence of pre-existing<br />
eustachian tube dysfunction using the inflation-deflation test. Of these patients<br />
100% developed aural fullness, 87% developed serous otitis media, and 47%<br />
required tympanostomy tubes. Fernau, et al, identified a history of eustachian tube<br />
dysfunction as a risk factor for serous otitis media in patients undergoing<br />
hyperbaric oxygen therapy.<br />
An article by Presswood, et al, points out that the middle ear complication rate in<br />
intubated patients receiving hyperbaric oxygen therapy is 94% compared to 46% of<br />
non-intubated patients. (Hemotympanum and otalgia) They state that the use of<br />
nasal decongestants in this population is controversial, and probably of no value in<br />
patients who are intubated. They recommend ventilation tubes should be placed in<br />
their ears prophylactically.<br />
OTHER CLINICAL SITUATIONS<br />
Obviously, there are many more clinical situations that the role of eustachian tube<br />
dysfunction is important. Disorders of the eustachian tube present important issues<br />
that in diagnosis and management that are faced in daily clinical practice. Despite<br />
the large volume of literature on eustachian tube dysfunction, the lack of welldesigned<br />
prospective studies make the literature difficult to decipher, and these<br />
disorders continue to represent some of the most challenging management<br />
problems we face as otolaryngologists.<br />
Summary<br />
The eustachian tube is an important anatomic structure that ventilates, protects, and<br />
drains the middle ear.<br />
During development the eustachian tube lengthens and the angle between it and the<br />
skull base increases from 10 degrees in infancy to 45 degrees in adulthood.<br />
http://www.bcm.edu/oto/grand/71196.html (11 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Eustachian tube dysfunction can be caused by mechanical obstruction, which may<br />
be intrinsic or extrinsic, by functional obstruction, or by the presence of patulous<br />
eustachian tubes.<br />
Otitis media with effusion is a common sequalae of eustachian tube dysfunction,<br />
but a high index of suspicion must be maintained in adults, in unilateral cases, and<br />
in patients with recurrent or persistent disease without an obvious explanation.<br />
Case Presentation<br />
A 54-year-old male was referred to the Bobby R. Alford Department of<br />
Otorhinolaryngology and Communicative Sciences for evaluation and management<br />
of a right patulous eustachian tube. The patient had previously undergone a right<br />
myringotomy and ventilation tube placement without resolution of his symptoms.<br />
He complained of right aural pressure and autophony for over one year. The<br />
autophony was particularly bothersome while singing. The patient had a history of<br />
high pitched noise exposure while in the military, and wears ear protection while at<br />
work. He denied headaches, nausea, vomiting, vertigo, otorrhea, otalgia, ear<br />
trauma, or ear surgery. He had no history of recent weight loss, and the remainder<br />
of his medical history was unremarkable.<br />
Physical examination revealed his left tympanic membrane to be clear, intact, and<br />
mobile. The right tympanic membrane had a scar in the anterior inferior quadrant,<br />
but was otherwise unremarkable. The right tympanic membrane did not move with<br />
swallowing or Valsalva maneuver. There were no masses noted in the<br />
nasopharynx. The rest of physical examination was unremarkable.<br />
The patient had an audiogram which was remarkable for symmetric severe<br />
sensorineural hearing loss above 2000 hertz bilaterally. He had Type A<br />
tympanograms bilaterally.<br />
The patient was reassured of his condition and Premarin nose drops were started,<br />
but the patient failed to respond. The patient was given the option of surgical<br />
intervention, and has noted an improvement in symptoms 2 weeks status post<br />
eustachian tube obliteration and ventilating tube placement.<br />
http://www.bcm.edu/oto/grand/71196.html (12 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Bibliography<br />
Bluestone CD. Current concepts in eustachian tube function as related to otitis media. Auris<br />
Nasus Larynx 1985, 12 (Suppl 1): S1-S4.<br />
Bluestone CD. Eustachian tube obstruction in the infant cleft palate. Ann Otol Rhinol Laryngol<br />
1971, 80: 1-30.<br />
Deron P, Clement PA, Derde MP. Septal surgery and tubal function. Rhinology 1995, 33: 7-9.<br />
DiBartolomeo JR, Henry DF. A new medication to control patulous eustachian tube disorders.<br />
Am J Otol 1992, 13: 323-327.<br />
Dyer RK, McElveen JT. The patulous eustachian tube: management option. Otolaryngology<br />
Head Neck Surg 1991, 105: 832-835.<br />
Fernau JL, Hirsch BE, Derkay C, Ramasastry S, Schaefer SE. Hyperbaric oxygen therapy: effect<br />
on middle ear and eustachian tube function. Laryngoscope 1992, 102: 48-52.<br />
Gacek RR. A differential diagnosis of unilateral serous otitis media. Laryngoscope 1992, 102:<br />
461-468.<br />
Halsted TH. Pathology and surgery of the eustachian tube. Arch Otolaryngol 1926, 4: 189-195.<br />
Henry DF, DiBartolomeo JR. Patulous eustachian tube identification using tympanometry. J Am<br />
Acad Audiol 1993, 4: 53-57.<br />
Holborow C. Eustachian tubal function: changes throughout childhood and neuromuscular<br />
control. J Laryngol Otol 1975, 89:47.<br />
Hsu MM, Young YH, Lin KL. Eustachian tube function of patients with nasopharyngeal<br />
carcinoma. Ann Otol Rhinol Laryngol 1995, 104: 453-455.<br />
Iwano T, Kinoshita T, Hamada E, Doi T, Ushiro K, Kumazawa T. Otitis media with effustion and<br />
eustachian tube dysfunction in adults and children. Acta Otolaryngol 1993, Suppl 500, 66-69.<br />
Presswood G, Zamboni WA, Stephenson LL, Santos P. Effect of artificial airway on ear<br />
complications from hyperbaric oxygen. Laryngoscope 1994, 104: 1383-1384.<br />
Proctor B. Embryology and anatomy of the eustachian tube. Arch Otolaryngol 1967, 86: 503-<br />
514.<br />
Sade J. The nasopharynx, eustachian tube and otitis media. J Laryngol Otol 1994, 108: 105-110.<br />
http://www.bcm.edu/oto/grand/71196.html (13 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Sakakihara J, Honjo I, Fujita A, Kurata K, Takahashi. Eustachian tube compliance in sniffinduced<br />
otitis media with effusion. Acta Otolaryngol 1993, 113: 187-190.<br />
Sakikawa Y, Kobayashi H, Normura Y. Changes in middle ear pressure in daily life.<br />
Laryngoscope 1995, 105:1353-1357.<br />
Shambaugh GE. Continuously open eustachian tube. Arch Otolaryngol 1938, 27: 420-425.<br />
Young Y, Lin KL, Ko JY. Otitis media with effusion in patients with nasopharyngeal carcinoma,<br />
postirradiation. Arch Otolaryngol 1995, 121: 765-768.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1995-7. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/71196.html (14 of 14) [5.11.2005 10:41:28]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
TRAUMATIC INJURIES TO THE FACIAL NERVE<br />
October 12, 1991<br />
Randall S. Zane, M.D.<br />
Traumatic injuries to the facial nerve can be classified by site (extracranial, intratemporal, intracranial)<br />
and by the type of trauma (penetrating, non-penetrating, or iatrogenic). The general principles of<br />
management remain the same regardless of the location of the injury, but the details vary and will be<br />
presented by location.<br />
Blunt trauma to the face rarely causes significant extracranial facial nerve injury. An example is birth<br />
trauma, most often the result of a forceps delivery where the exposed facial nerve is compressed against<br />
the rigid cervical spine. Penetrating lesions of the facial nerve distal to the parotid gland and medial to<br />
the lateral canthus of the eye rarely result in severe disfigurement and most often do not require repair.<br />
Repair of the cervical or platysmal division is also usually unnecessary because of the minimal functional<br />
http://www.bcm.edu/oto/grand/101291.html (1 of 7) [5.11.2005 10:41:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
loss that results from transection. Lesions of the main trunk or the temporozygomatic or cervicofacial<br />
divisions should be repaired or a major deficit in facial movement will persist. Clean facial lacerations<br />
with immediate onset of facial paralysis should be promptly explored. After three days, the severed<br />
branch loses its excitability, and that can make its identification tedious and uncertain. If there is gross<br />
contamination of the wound requiring debridement, other life threatening injuries where it is not<br />
advisable to prolong anesthesia, or if there is a lack of equipment or expertise, an attempt should be made<br />
to identify the severed nerve endings and to tag them for later identification. Whenever possible, primary<br />
end-to-end anastomosis is ideal and allows the greatest functional return. Interpositional grafting is<br />
second best, but a certain percentage of regenerating axons are lost across each anastomosis. For<br />
interposition grafting, the greater auricular and sural nerves are popular largely because of the ease in<br />
which these sensory nerves are harvested.<br />
Iatrogenic injuries occur most often with extirpation of parotid malignancy where the facial nerve passes<br />
through the tumor and must be removed. In this instance, interpositional grafting is the usual procedure.<br />
Even when there is a question as to the adequacy of resection, potential long-term survival or the need<br />
for postoperative radiotherapy, grafting should be undertaken since it adds only a short time to the<br />
operation. The psychological<br />
advantages of even incomplete return of function as soon as possible after surgery should not be<br />
underestimated. In more routine parotid surgery, the facial nerve should be stimulated near the<br />
stylomastoid foramen before wound closure. If brisk facial movement occurs, subsequent facial motion<br />
will be satisfactory, even if there is paresis immediately postop. If movement does not occur in all major<br />
muscle groups, the nerve should be inspected carefully under magnification for evidence of injury, for<br />
example, ligature on the nerve, crush injury, and the like. If a crush injury is suspected it may be<br />
necessary to split the sheath to ascertain whether the fascicles are in continuity. If they are not, excision<br />
of the damaged segment and repair may be the best course of action.<br />
Temporal bone fractures are a unique form of non-penetrating injury that can cause significant damage to<br />
the intratemporal facial nerve. They may be classified as longitudinal or transverse according to the<br />
orientation of the fracture planes on high resolution CT scanning, and they may occur in a mixed form.<br />
Facial nerve injuries are more common with transverse fractures, but because the incidence of<br />
longitudinal fractures is higher, they are seen more frequently as a result of longitudinal fractures.<br />
With longitudinal fractures where the associated hearing loss is conductive in nature, exploration of the<br />
geniculate ganglion should be carried out via a middle cranial fossa approach, followed by transmastoid<br />
exploration of the tympanic and vertical segments for the occasional injury caused by fractures through<br />
the osseous canal. Transverse fractures, by virtue of the associated severe sensorineural hearing loss are<br />
explored through transmastoid and translabyrinthine approaches. Injuries in the tympanic and<br />
labyrinthine segments are easily accessible for repair via this approach. Lesions including edema,<br />
hemorrhage, contusion, and impacted bony spicules are best managed by decompression of the nerve in<br />
the fallopian canal. Transection of more than 50% of the nerve requires an interpositional graft to ensure<br />
regeneration of an adequate number of motoneurons.<br />
http://www.bcm.edu/oto/grand/101291.html (2 of 7) [5.11.2005 10:41:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Penetrating injuries of the temporal bone are most often caused by gunshot wounds but can be the result<br />
of some stab wounds. If there is any suspicion of a vascular injury of the sigmoid or lateral sinus, jugular<br />
vein or carotid system, carotid arteriography is indicated. When surgery is indicated, most can be<br />
explored through standard transmastoid approaches. Primary reanastomosis of a severed nerve in the<br />
fallopian canal is rarely encountered as an option to restore continuity - Interpositional grafts are<br />
frequently necessary using the nerve's natural self-adhesiveness without the use of suture, and this may<br />
be enhanced by the application of autologous fibrin glue. The fallopian canal can be used as a sort of<br />
stent to hold the graft in place.<br />
The most common sites of inadvertent injury to the nerve in tympanomastoid surgery are in the middle<br />
ear where the tympanic segment of the nerve above the oval window is occasionally dehiscent, and in the<br />
mastoid at the second genu where it is susceptible to injury during antrotomy if the usual landmarks<br />
including the lateral semicircular canal are distorted or not recognized. If a postoperative paralysis<br />
occurs, sufficient time must elapse<br />
to ensure that the effects of any local anesthesia have worn off. If the surgeon did not identify the nerve<br />
during the operation, exploration is mandatory. If the nerve was identified and the surgeon knows it to be<br />
intact, the patient should be followed with electrodiagnostic testing. If only postoperative paresis is<br />
evident, the patient is followed closely by examination, and if the palsy becomes complete the patient<br />
should undergo electrodiagnostic testing.<br />
Injury to the intracranial segment of the facial nerve is usually iatrogenic, secondary to tumor removal,<br />
but infrequently can result from penetrating injuries or medial transverse temporal bone fracture.<br />
Collagen splints have been used for grafting in this location, but results are poor.<br />
As the quality of radiographic studies, primarily high resolution CT scan, has improved, the importance<br />
of topognostic testing has fallen off. However, although it is sometimes inaccurate and has not been<br />
shown to be of prognostic significance, they can be helpful in determining the proximal extent of injury<br />
and should not be forgotten.<br />
In the past, decisions as to surgery traditionally were based on the time of onset of complete paralysis,<br />
such that patients with immediate onset following trauma were explored and those with delayed onset<br />
were managed conservatively. Electrophysiologic testing has changed the scene quite a bit, since cases of<br />
paralysis with an immediate onset have been monitored and have had good spontaneous return of<br />
function, while delayed onset has been monitored to progress and lead to suboptimal results. In the first<br />
three days, electrical testing takes a back seat to clinical evaluation including the physical examination.<br />
Between three days and three weeks, if the patient has visible facial motion, electrical testing is not<br />
needed and will be normal if obtained. If there is paralysis, early screening with a Hilger nerve stimulator<br />
is used. If the threshold on the involved side stays less than 3.5 mAmps above the normal side, no further<br />
testing is necessary. If the threshold difference goes above 3.5 mAmps, some authors recommend<br />
exploration. However, if ENoG is available to you, it is recommended that serial examinations be<br />
performed every one or two days to follow the course of degeneration. Fisch has set up guidelines such<br />
http://www.bcm.edu/oto/grand/101291.html (3 of 7) [5.11.2005 10:41:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
that should degeneration, to greater than 90% of nerve fibers as calculated by ENoG, take place in the<br />
first three weeks, the prognosis is poor for spontaneous recovery and that patient should be explored.<br />
Anytime after three weeks, there is some controversy regarding the decision to explore, primarily<br />
because some nonpenetrating injuries can show spontaneous recovery. Dr. Coker and Dr. Jenkins feel<br />
that all penetrating and iatrogenic injuries with evidence of complete degeneration need exploration to<br />
document location and cause of the problem. The intact nerve can then be left alone and observed, while<br />
the severed nerve is appropriately managed. All blunt injuries outside the stylomastoid foramen can be<br />
observed for six to twelve months before intervention.<br />
The most controversy is generated over late exploration for temporal bone fractures with complete<br />
paralysis. This is because the natural course of recovery has not been established.<br />
Except by perceptible facial movement or EMG activity, there is no way of knowing whether or not<br />
regeneration is occurring across the injury site and that with time facial function<br />
could be acceptable. Some argue that bony fragments and fibrosis can impede the spontaneous<br />
regeneration at the injury site and that exploration can enhance the opportunity for regeneration. This is a<br />
difficult problem to reconcile and should be approached on a case-by-case basis with careful counseling<br />
of the patient. Should there be no return of function by twelve to eighteen months post temporal bone<br />
fracture, there is little argument that the nerve should be explored with interpositional grafting at the site<br />
of injury.<br />
The following management rationale for injuries to the facial nerve is reproduced (by permission) from<br />
the award-winning scientific exhibit presented by Dr. Newton Coker and Dr. Herman Jenkins at the 1990<br />
American Academy of Otolaryngology - Head and Neck Surgery meeting in San Diego.<br />
Case Presentation<br />
A 54 year old black male was assaulted and stabbed multiple times in the back, shoulders and right face.<br />
The single facial wound was one centimeter in length and was vertically oriented 1.5 centimeters anterior<br />
to the tragus. Examination revealed complete right peripheral facial paralysis without significant edema<br />
or hematoma. Clear saliva was easily expressed from Stenson's duct. On the third day post injury, after<br />
stabilization and complete evaluation of his other injuries, he was taken to the operating room for right<br />
facial nerve exploration. The main trunk of the facial nerve was identified and found to be transected just<br />
proximal to the pes anserinus. All branches of the nerve were distally intact as demonstrated by electrical<br />
stimulation of the distal cut edge. A primary neurorrhaphy was carried out under no tension with 10-0<br />
Prolene suture using a perineural technique.<br />
http://www.bcm.edu/oto/grand/101291.html (4 of 7) [5.11.2005 10:41:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Bibliography<br />
Adkins WY, Osguthorpe JD: Management of trauma of the facial nerve. Otolaryngol Clin North Am 24:587-611, 1991.<br />
Adour KK, Bayajian JA, Kahn ZM, Schneider GS: Surgical and nonsurgical management of facial paralysis following<br />
closed head injury. Laryngoscope 87:380-90, 1977.<br />
Aguilar EA, Yeakley JW, Ghorayeb BY, Hauser M, Cabrera J, Jahrsdoerfer RA: High resolution CT scan of temporal<br />
bone fractures: Association of facial nerve paralysis with temporal bone fractures. Head Neck Surg 9:162-66, 1987.<br />
Alford BR: Electordiagnostic studies in facial paralysis. Arch Otolaryngol 85:259-64, 1967.<br />
Alford BR, Jerger JF, Coats AC, Peterson CR, Weber SC: Diagnostic tests of facial nerve function. Otolaryngol Clin<br />
North Am 7:331-42, 1974.<br />
Alford BR, Sessions RB, Weber SC: Indications for surgical decompression of the facial nerve. Laryngoscope 81:620-35,<br />
1971.<br />
Alford BR, Weber SC, Sessions RB: Neurodiagnostic studies in facial paralysis. Ann Otol Rhinol Laryngol, 79:227-33,<br />
1970.<br />
Babin RW: Topognostic and prognostic evaluation of traumatic facial nerve injuries. Otolaryngol Head Neck Surg 90:610-<br />
11, 1982.<br />
Baker DC, Conley J; Facial nerve grafting: A thirty year retrospective review. Clin Plast Surg 6:343-60, 1979.<br />
Cannon CR, Jahrsdoerfer RA: Temporal bone fractures. Arch Otolaryngol 109:285-88, 1983.<br />
Coker NJ, Jenkins HA, Psifidis A: Electrophysiologic prognostication of acute facial nerve trauma, in Fisch U, Valavanis<br />
A, and Yasargil MG (eds): Neurological Surgery of the Ear and the Skull Base: Proceedings of the Sixth international<br />
Symposium. Amsterdam, Kugler and Ghedini, 1989.<br />
Coker, NJ, Kendall KA, Jenkins HA, Alford BR: Traumatic intratemporal facial nerve injury: Management rationale for<br />
preservation of function. Otolaryngol Head Neck Surg 97:262-69, 1987.<br />
Dott NM: Facial nerve reconstruction by graft bypassing the petrous bone. Arch Otolaryngol 78:426-28, 1983.<br />
Duncan NO, Coker NJ, Jenkins HA: Gunshot injuries of the temporal bone. Otolaryngol Head Neck Surg 94:47-55, 1986.<br />
Fisch U: Facial nerve grafting. Otolaryngol Clin North Am 24:691-708, 1991.<br />
Fisch U: Facial paralysis in fractures of the petrous bone. Laryngoscope 84:2141-54, 1974.<br />
Fisch U: Prognostic value of electrical tests in acute facial paralysis. Am J Otol 5:494-98, 1984.<br />
http://www.bcm.edu/oto/grand/101291.html (5 of 7) [5.11.2005 10:41:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Glasscock ME, House WF, Alford BR: Middle fossa facial nerve decompression. Laryngoscope 79:234-40, 1969.<br />
Grobman LR, Pollak A, Fisch U: Entrapment injury of the facial nerve resulting from fracture of the temporal bone.<br />
Otolaryngol Head Neck Surg 101:404-08, 1989.<br />
Guilford FR: Surgical consideration in disorders of the horizontal and vertical portions of the facial nerve. Ann Otol Rhinol<br />
Laryngol 79:241-51, 1970.<br />
Harker LA, McCabe BF: Temporal bone fractures and facial nerve injury. Otolaryngol Clin North Am 7:425-31, 1974.<br />
Hasso AN, Ledington JA: Traumatic injuries of the temporal bone. Otolaryngol Clin North Am 21:295-316, 1988.<br />
Johns ME, Crumley RL: Facial nerve injury, repair and rehabilitation (SIPac). Alexandria, VA, American Academy of<br />
Otolaryngology, 1979.<br />
Kamerer DB: Intratemporal facial nerve injuries. Otolaryngol Head Neck Surg 90:612-15, 1982.<br />
Lambert PR, Brackmann DE: Facial paralysis in longitudinal temporal bone fractures: A review of 26 cases. Laryngoscope<br />
94:1022-26, 1984.<br />
May M: Total facial nerve exploration: Transmastoid, extralabyrinthine, and subtemporal indications and results.<br />
Laryngoscope 89:906-17, 1979.<br />
May M, Klein SR: Differential diagnosis of facial nerve palsy. Otolaryngol Clin North Am 24:613-45, 1991.<br />
Miehlke A: Extratemporal injury and repair of the facial nerve. Otolaryngol Clin North Am 7:467-92, 1974.<br />
Millen SJ, Daniels D, Meyer G: Gadolinium-enhanced magnetic resonance imaging in facial nerve lesions. Otolaryngol<br />
Head Neck Surg 102:26-33, 1990.<br />
Pillsbury HC, Fisch U: Extratemporal facial nerve grafting and radiotherapy. Arch Otolaryngol 105:441-46, 1979.<br />
Pulec JL: Total decompression of the facial nerve. Laryngoscope 75:1015-28, 1966.<br />
Schwaber MK, Zealear D, Netterville JL, Seshul M, Ossoff RH: The use of magnetic resonance imaging with highresolution<br />
CT scan in the evaluation of facial paralysis. Otolaryngol Head Neck Surg 101:449-58, 1989.<br />
Sunderland S: Some anatomical and pathophysiological data relevant to facial nerve injury and repair, in: Facial Nerve<br />
Surgery. New York, Aesculapius Publishing, 1977.<br />
Tucker HM: The management of facial paralysis due to extracranial injuries. Laryngoscope 88:348-54, 1978.<br />
Wiet RJ: Iatrogenic facial paralysis. Otolaryngol Clin North Am 15:773-80, 1982.<br />
http://www.bcm.edu/oto/grand/101291.html (6 of 7) [5.11.2005 10:41:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Yanagihara N: Transmastoid decompression of the facial nerve in temporal bone fracture. Otolaryngol Head Neck Surg<br />
90:616-21, 1982.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/101291.html (7 of 7) [5.11.2005 10:41:41]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
FACIAL REANIMATION OF THE CHRONICALLY PARALYZED FACE<br />
September 28, 1994<br />
Amy Y. Chen, M.D.<br />
Facial nerve paralysis is a devastating injury that can result in blindness, oral incontinence and social<br />
handicaps. The muscles of the face are exquisitely designed for both voluntary and involuntary<br />
expression.<br />
The facial nerve emerges from the brainstem via the internal auditory canal and exits the brain through the<br />
stylomastoid foremen. At this point, the nerve travels a short distance to the pes where it divides into five<br />
motor branches--the temporal, zygomatic, buccal, mandibular and cervical branches.<br />
The nerve is responsible for orchestrating an intimately designed facial musculature system. The facial<br />
musculature is capable of maintaining tone as well as expressing both voluntary and involuntary<br />
http://www.bcm.edu/oto/grand/92994.html (1 of 6) [5.11.2005 10:41:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
emotions.<br />
First, we will discuss the importance of eye protection and methods used to achieve a healthy eye.<br />
Paralysis of orbicularis oculi results not only in drying of the cornea but also in poor distribution of tears.<br />
The lower lid is not able to contract and disperse the tears across the eye. Furthermore, loss of<br />
parasympathetic innervation can result in decreased tear production. This can result in keratitis and rarely,<br />
corneal ulceration and cataract formation. Therefore, the primary objective of the surgeon is to protect the<br />
eye via surgical and/or nonsurgical methods.<br />
Surgical methods may involve both upper lid procedures such as tarsorraphy, gold weights, and palpebral<br />
springs as well as lower lid procedures.<br />
Muscle transposition can be utilized to reanimate the face. Two muscles primarily used are the masseter<br />
and the temporalis. The patient must have an intact V for these procedures. Movement of the face can be<br />
achieved by instructing the patient to clench the teeth.<br />
Masseter muscle transposition involves harvesting two anterior slips of masseter muscle and transposing<br />
it to the upper and lower lip. Advantages include supplementing other reanimation techniques such as XII-<br />
VII or temporalis sling and providing static tone for the face. However, a downwards vector may cause<br />
the lip to droop.<br />
Temporalis muscle transposition is also commonly used. This muscle is used primarily to reanimate the<br />
mouth and lower aspect of the face. The temporalis muscle is harvested and sewn to upper lip,<br />
commissure and lower lip. The key to success is to ensure overcorrection and exaggeration of the lip.<br />
Goretex strips can be used to lengthen the muscle so that it can reach the mouth. The defect in the<br />
temporalis can be corrected with synthetic insert or a temporoparietal fascial flap. May & Drucker in 1993<br />
reported that the success of temporalis muscle transfer to restore a smile was 80% and to improve mouth<br />
function was 96%.<br />
Various neural methods have also been employed to attempt facial reanimation. Primary anastomosis can<br />
be utilized effectively in the acute injury. But in the chronic palsy, primarily three techniques are<br />
currently used--XII-VII traditional, XII-VII jump, and VII-VII cross face graft. 4-6 months usually pass<br />
before the facial muscles begin to show signs of recovery.<br />
The XII-VII traditional anastomosis was first performed in 1903 by Korte. Indications for this procedure<br />
include an intact peripheral facial nerve and a nonatrophic facial musculature. However, if the patient has<br />
injured the peripheral facial nerve or has atrophied muscles, or if other cranial nerve palsies exist, this<br />
procedure is to be avoided. The patient must learn to push his tongue against the teeth when he wishes to<br />
smile. Advantages of the procedure are that majority of patients has good movement. However, some<br />
patients can develop synkinesis and mass motion as well as atrophy of the tongue.<br />
Another method of XII-VII anastomosis is that of placing an interposition graft between the two, thus<br />
http://www.bcm.edu/oto/grand/92994.html (2 of 6) [5.11.2005 10:41:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
"jumping" from XII-VII. This procedure involves partially severing the XII nerve. One usually uses either<br />
the greater auricular nerve or the sural nerve as grafts. The former is preferred since it does not involve<br />
another operative exposure. However, the sural nerve can be advantageous for it provides a longer graft as<br />
well as larger diameter graft.<br />
For best results, the anastomoses should be performed within one year of surgery. This jump graft<br />
procedure can diminish the incidence of tongue atrophy, the problems with synkinesis and mass motion<br />
and those with swallowing, mastication and speech. However, patients can have weak facial contractures.<br />
Another disadvantage is that the procedure involves two anastomoses rather than one as in the traditional<br />
XII-VII.<br />
The incidences of swallowing deficiencies, mastication problems and speech difficulty are greater for XII-<br />
VII traditional grafts as compared to XII-VII jump. However, the results of achieving symmetry and<br />
excellent facial movement are similar between the two. One is able to reduce the incidence of mass<br />
movement with a jump graft.<br />
VII -VII cross face grafts have also been used. Scaramella first described the procedure in 1970. It<br />
involves grafting VII from the functional side of the face to the stump on the paralyzed side. Obvious<br />
disadvantages include long operative time involving two anastomoses and surgical intrusion of the<br />
functional side of the face. Synkinesis and low grade neural input can result in less forceful contracture of<br />
the face. This procedure is often used in conjunction with free muscle transfers.<br />
With the advent of microsurgery, it is also possible to transpose free flaps. Harii et al in 1975 were the<br />
first to transfer free muscle tissue for facial reanimation. Free muscle transfer provides soft tissue<br />
coverage of a defect as well as the opportunity for one to develop voluntary control of the face. This is<br />
usually a two stage procedure. The first stage involves anastomosing the nerve graft, usually a cross face<br />
graft. 6-12 months later, the free flap is harvested and anastamosed to the site. Commonly used donor<br />
sites include the gracilis, serratus anterior, latissimi dorsi, and rectus abdominis. The recipient vessels are<br />
typically facial artery and common facial vein.<br />
In summary, the management of the permanently paralyzed face is threefold. First, one must provide<br />
protection of the eye. Second, muscle transposition is performed to restore tone to the patient's face.<br />
Third, efforts are made to restore facial movement that automatically reflects the breadth and depth of<br />
human expression. It is this last goal that remains elusive. However, with these methods, a patient can use<br />
the restored movement to express human emotion by practice and adaptation.<br />
Case Presentation<br />
A 65-year-old black woman presented with a long history of right-sided hearing loss. Over the past few<br />
months, she has had dizziness and unsteadiness in her gait. Past medical history was significant for<br />
http://www.bcm.edu/oto/grand/92994.html (3 of 6) [5.11.2005 10:41:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
diabetes and hypertension. A hysterectomy was her only surgical history.<br />
Imaging studies revealed a large 5 cm tumor in the cerebellopontine angle consistent with a vestibular<br />
schwannoma. Audiogram revealed a profound right sensorineural hearing loss.<br />
Excision of the tumor was performed via a transotic and translabyrinthine approach. The VII nerve was<br />
not preserved and therefore the patient developed a right facial paralysis. She did not have other cranial<br />
nerve deficits.<br />
Approximately 6 weeks after the initial surgery, the patient was evaluated for facial reanimation. At this<br />
time, gold weights were implanted in the right eyelid and a XII-VII hypoglossal-facial nerve<br />
interpositional-jump graft procedure was performed. The patient had an uneventful postoperative course<br />
and was discharged home two days after surgery.<br />
Bibliography<br />
Anderl H. Cross-face nerve transplant. Clin Plast Surg 1989;6:433-449.<br />
Aviv JE, Urken ML. Management of the paralyzed face with microneurovascular free muscle transfer. Arch Otolaryngol<br />
Head Neck Surg 1992;118:909-912.<br />
Baker DC, Conley J. Facial nerve grafting: a thirty year retrospective review. Clin Plast Surg 1979;6:343-360.<br />
Baker DC, Conley J. Regional muscle transposition for rehabilitation of the paralyzed face. Clin Plast Surg 1979;6:317-<br />
331.<br />
Conley J. Myths and misconceptions in the rehabilitation of facial paralysis. Plast Reconstr Surg 1983;71:538-539.<br />
Harii K, Ohmori K, Torii S. Free gracilis muscle transplantation, with microneurovascular anastomoses for the treatment of<br />
facial paralysis. Plast Reconstr Surg 1976;57:133-143.<br />
Hata Y, Yano K, Matsuka K, Ito O, Matsuda H, Hosokawa K. Treatment of chronic facial palsy by transplantation of the<br />
neurovascularized free rectus abdominis muscle. Plast Reconstr Surg 1990;86:1178-1179.<br />
Kartush JM, Linstrom CJ, McCann PM, Graham MD. Early gold weight eyelid implantation for facial paralysis.<br />
Otolaryngol Head Neck Surg 1990;103:1016-1023.<br />
Levine RE. Reanimation of paralyzed eyelids. Facial Plast Surg 1992;8:121-126.<br />
May M, Sobol SM, Mester SJ. Hypoglossal-facial nerve interpositional-jump graft for facial reanimation without tongue<br />
atrophy. Otolaryngol Head Neck Surg 1991;104:818-825.<br />
http://www.bcm.edu/oto/grand/92994.html (4 of 6) [5.11.2005 10:41:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
May M. Gold weight and wire spring implants as alternatives to tarsorraphy. Arch Otolaryngol Head Neck Surg<br />
1987;113:656-660.<br />
May M. Paralyzed eyelids reanimated with a closed-eyelid spring. Laryngoscope 1988;98:382-385.<br />
May M, Hoffmann DF. Buerger GF, Soll DB. Management of the paralyzed lower eyelid by implanting auricular cartilage.<br />
Arch Otolaryngol Head Neck Surg 1990;116:786-788.<br />
May M, Drucker C. Temporalis muscle for facial reanimation: a 13-year experience with 224 procedures. Arch Otolaryngol<br />
Head Neck Surg 1993;119:378-382.<br />
May M. Muscle transposition for facial reanimation: indications and results. Arch Otolaryngol 1984;110:184-189.<br />
May M. Muscle transposition for facial reanimation. Facial Plast Surg 1992;8:115-120.<br />
May M, Sobol SM, Brackmann DE. Facial reanimation: the temporalis muscle and middle fossa surgery. Laryngoscope<br />
1991;101:430-432.<br />
O'Brien BM, Franklin JD, Morrison WA. Cross-facial nerve grafts and microneurovascular free muscle transfer for long<br />
established facial palsy. Br J Plast Surg 1980;33:202-215.<br />
O'Brien BM, Pederson WC, Khazanchi RK, Morrison WA, MacLeod AM, Kumar V. Results of management of facial<br />
palsy with microvascular free-muscle transfer. Plast Reconstr Surg 1990;86:12-22.<br />
Mackinnon SE, Dellon AL. Technical considerations of the latissimus dorsi muscle flap: a segmentally innervated muscle<br />
transfer for facial reanimation. Microsurg 1988;(;36-45.<br />
Neuman AR, Weinberg A, Sela M, Peled IJ, Wexler MR. The correction of seventh nerve palsy lagophthalmos with gold<br />
lid load (16 years experience). Ann Plast Surg 1989;22:142-145.<br />
O'Connell JE, Robin PE. Eyelid gold weights in the management of facial palsy. J Laryngol Otol 1991;105:471-474.<br />
Rosenwasser RH, Liebman EM, Jimenez DF, Buchheit WA, Andrews DW. Neurosurg 1991;29:568-574.<br />
Scaramella LF. Anastomosis between the two facial nerves. Laryngoscope 1975;85:1359-1366.<br />
Seiff SR, Chang J. Management of ophthalmic complications of facial nerve palsy. Otolaryngol Clin North Am<br />
1992;25:669-690.<br />
Wells MD, Manktelow RT. Surgical management of facial palsy. Otolaryngol Clin North Am 1990;17:645-653.<br />
Whitney TM, Buncke JH, Alpert BS, Buncke GM, Lineaweaver WC. The serratus anterior free-muscle flap: experience<br />
with 100 consecutive cases. Plast Reconstr Surg 1990;86:481-490.<br />
http://www.bcm.edu/oto/grand/92994.html (5 of 6) [5.11.2005 10:41:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/92994.html (6 of 6) [5.11.2005 10:41:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
THERAPEUTIC OPTIONS FOR TREATMENT<br />
OF GLOMUS TUMORS OF THE TEMPORAL BONE<br />
October 26, 1991<br />
Judith J. Owens, M.D.<br />
Glomus tumors arise from paraganglionic chemoreceptor cells and are part of the APUD system of cells<br />
of neural crest origin. Paragangliomas of the jugular-tympanic area are the most common tumors<br />
involving the middle ear. In 1941, Guild described the distribution of normal glomus bodies within the<br />
temporal bone. Then in 1945, Rosenwasser correctly recognized and reported the first case of a tumor<br />
arising from these cells. After this report, many new cases were reported and many older cases were<br />
reclassified as true glomus tumors.<br />
These neoplasms can occur at any age but the peak incidence is in the fifth decade. Glomus tumors occur<br />
four to five times as often in women as in men and there is a predilection for them in the Caucasian race.<br />
http://www.bcm.edu/oto/grand/102691.html (1 of 7) [5.11.2005 10:41:59]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
The majority of these tumors arise from along the jugular bulb or Jacobson's nerve (85%), while 12%<br />
arise from glomus bodies overlying the promontory and three percent have their origin attributed to<br />
Arnold's nerve. The most common presenting symptoms include conductive hearing loss and pulsatile<br />
tinnitus. Other symptoms may include aural hemorrhage or otorrhea, otalgia and facial palsy. When the<br />
tumors enlarge within the jugular foramen neuropathies of IX, X, XI and XII occur. Anterior expansion<br />
toward the clivus may produce abducens and trigeminal palsies. Aquino's sign is blanching of the<br />
tympanic mass with gentle pressure on the carotid artery. The sign of Brown is the pulsation sign elicited<br />
by pneumatic compression and abolished with further compression. These tumors may be multicentric.<br />
Association of these tumors with other tumors arising from cells of neural crest origin (MEN I and<br />
pheochromocytoma) is not uncommon. This must be considered to avoid the devastating consequences of<br />
inducing general anesthesia in a patient with an unrecognized pheochromocytoma. Malignancy occurs in<br />
one to three percent of these tumors.<br />
Evaluation includes a careful history and physical examination. High resolution computed tomography<br />
provides accurate information about bony destruction and the extent of the disease. Arteriography<br />
remains the most useful radiologic modality available for the assess-ment of a glomus tumor. Prior to<br />
angiography, serum catacholamines and urinary vanillylmandelic acid (VMA) levels should be obtained<br />
to screen for tumors which secrete these vasoactive compounds.<br />
Therapeutic options for glomus tumors of the temporal bone include surgical excision, radiotherapy,<br />
combined therapy and in selected cases observation. Surgical excision offers the only chance for total<br />
tumor eradication. Gary Jackson writes that "...surgical management is curative and the treatment of<br />
choice." Proponents of radiotherapy argue that radiation provides for the amelioration of symptoms and<br />
arrests the progression of the glomus tumors providing a safe and efficacious modality of therapy.<br />
Many surgical approaches have been proposed for the resection of these tumors (see bibliography). No<br />
single approach is optimal for all tumors. Jackson and Glasscock proposed guidelines for a planned<br />
excision of these tumors. They suggest approaching type I glomus tympanicum tumors via a transcanal<br />
approach, and an extended facial recess approach for type II-IV glomus tympanicum tumors. Type I and<br />
II glomus jugulare lesions are treated by standard skull base techniques. Type III and IV tumors require<br />
an infratemporal fossa approach. The infratemporal fossa as described by Fisch provides for direct<br />
surgical access to the entire length of the intratemporal carotid artery and for control of the great venous<br />
sinuses. These infratemporal fossa approaches provide access as follows: Type A provides access to the<br />
temporal bone in its infralabyrinthine and apical compartments and its inferior surface. Type B provides<br />
access to the clivus and type C provides access to the parasellar region and nasopharynx. Utilizing these<br />
skull base approaches it is now possible to perform total extirpation of tumors that were previously<br />
considered unresectable. Skull base surgery is not undertaken without certain risks. Mortality rates range<br />
from four to seven percent. Reported complications include CSF leaks, new cranial nerve palsies, wound<br />
infections, and deafness. The risks of surgery are balanced out by the chance for total tumor eradication.<br />
The reported rate of local control for glomus tumors of the temporal bone with surgical treatment from<br />
several studies is shown in Table 4.<br />
Although radiotherapy is unable to provide complete tumor eradication, the success of radiotherapy in<br />
http://www.bcm.edu/oto/grand/102691.html (2 of 7) [5.11.2005 10:41:59]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
controlling the progression of symptoms is quite high. The reported rate of local control with radiation<br />
therapy for glomus tumors of the temporal bone from several studies is shown in Table 5. Complications<br />
of radiotherapy include osteoradionecrosis, brain necrosis, abscess formation, and radiation induced<br />
malignancies.<br />
Case Presentation<br />
A 69-year-old black female had initially sought assistance from a hearing aid dispenser after<br />
experiencing several years of slow, progressive left-sided hearing loss. However, a medical referral was<br />
made when the presence of a unilateral conductive hearing loss and pulsatile mass on the tympanic<br />
membrane were discovered. CT examination of the temporal bones demonstrated an opacification of the<br />
left mastoid air cells and middle ear cavity.<br />
She was then referred to Baylor College of Medicine for further evaluation and treatment. Upon<br />
questioning, she reported that she could appreciate a rhythmic sound in her left ear that was synchronous<br />
with her heart rate. Examination revealed a pulsating tympanic membrane with dilated vasculature that<br />
extended onto the skin of the external canal. The sign of Aquino was negative and the Weber lateralized<br />
to the left. There were no cranial nerve deficits. Arteriography was obtained. This demonstrated a<br />
vascular mass of the left temporal bone supplied by the penetrating vessels of the external carotid artery.<br />
These findings were consistent with a glomus tympanicum. The options of surgical resection,<br />
radiotherapy and observation were explained to the patient. It was elected to observe the tumor for the<br />
time being and to offer her radiotherapy should the tumor enlarge or become symptomatic.<br />
Bibliography<br />
Alford BR, Guilford FR: A comprehensive study of tumors of the glomus jugulare. Laryngoscope 72:765-787, 1962.<br />
Aquino J: Glomus jugulare tumors. Arch Otolaryngol 65:263-268, 1957.<br />
Bartels LJ, Gurucharri M: Pediatric glomus tumors. Otolaryngol Head Neck Surg 98:392-395, 1988.<br />
Bataini J, Pontvert D, Jaulerry C, et al: Tumeurs du glomus jugulaire. Neurochirurgie 31:377-380, 1985.<br />
Bojrab DI, Glasscock ME, Roland PS, et al: Glomus tumors of the temporal bone. Washington DC: AAO-HNS, 1988.<br />
Boyle, JO, Shimm DS, Coulthard SW: Radiation therapy for paragangliomas of the temporal bone. Laryngoscope 100:896-<br />
901, 1990.<br />
http://www.bcm.edu/oto/grand/102691.html (3 of 7) [5.11.2005 10:41:59]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Brackmann DE, Hitseleberger WE: Retrolabyrinthine approach technique and newer indications. Laryngoscope 88:286-<br />
297, 1978.<br />
Brandt TW, Jenkins HA, Coker NA: Facial paralysis as the initial presentation of an internal carotid artery aneurysm. Arch<br />
Otolaryngol Head Neck Surg 112:198-202, 1986.<br />
Brismar J, Cronqvist: Therapeutic embolization in the external carotid artery region. Radiologica Diagnosis 19:713-731,<br />
1978.<br />
Brown, LA: Glomus jugulare tumor of the middle ear clinical aspects. Laryngoscope 53:281292, 1953.<br />
Bundgaard T, Tandrup O, Elbrond O, et al: Treatment of glomus tumours. A retrospective survey. Clin Otolaryngol<br />
14:155-160, 1989.<br />
Cece JA, Lawson W, Biller HF: Complications in the management of large glomus jugulare tumors. Laryngoscope 97:152-<br />
157, 1987.<br />
Cole JM: Glomus jugulare tumor. Laryngoscope 87:1244-55, 1977.<br />
Conley JJ: Multiple paragangliomas in the head and neck. Ann Otol Rhinol Laryngol 65:356-360, 1956.<br />
Cummings BJ, Beale FA, Garrett PG: The treatment of glomus tumors in the temporal bone by megavoltage radiation.<br />
Cancer 53:2635-2640, 1984.<br />
Dawes PJ, Filippou M, Welch AR, et al: The management of glomus jugulare tumours. Clin Otolaryngol 12:15-24, 1987.<br />
Dayal VS, Hinojosa R, Amenta CA: Surgical inferences from study of temporal bones with glomus jugulare tumor.<br />
Otolaryngol Head Neck Surg 102:690-697, 1990.<br />
Dickens JW, Million RR, Singleton GT, et al: Chemodectomas arising in temporal bone structures. Laryngoscope 92:188-<br />
191, 1982.<br />
Ferrara P, Cimino A, Tortorici M: Role of radiation therapy in glomus tumor. Am J Otol 8:390-395, 1987.<br />
Fisch U: Infratemporal fossa approach for extensive tumors of the temporal bone and base of the skull, in Silverstein H,<br />
Norrell H (eds): Neurological Surgery of the Ear. Birmingham, Ala., Aesculapius, 1977.<br />
Fisch U: Infratemporal fossa approach for glomas tumors of the temporal bone. Ann Otol Rhinol Laryngol 92:474-479,<br />
1982.<br />
Fisch U: La voie d'abord infratemporale pour les tumeurs du glomus jugulaire. Neurochirurgie 31:367-376, 1985.<br />
Fisch U, Fagan P, Valavanis A: The infratemporal fossa approach for the lateral skull base. Otolaryngol Clin North Am<br />
17:513-552, 1984.<br />
http://www.bcm.edu/oto/grand/102691.html (4 of 7) [5.11.2005 10:41:59]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Franklin DJ, Jenkins HA, Horowitz, BL: Management of petrous apex lesions. Arch Otolaryngol 115:1121-1125, 1989.<br />
Fuller AM, Brown HA, Harrison, EG: Chemodectomas of the glomus jugulare tumors. Laryngoscope 77:218-238, 1967.<br />
Gardner G, Cocke EW, Robertson, JT et al: Glomus jugulare tumours - combined treatment. J Laryngol Otol 95:437-580,<br />
1981.<br />
Glasscock ME, Harris PF, Newsome G: Glomus tumors: Diagnosis and treatment. Laryngoscope 84:2006-2032, 1974.<br />
Glassock ME, Smith PG, Bond AG: Management of aneurysms of the petrous portion of the internal carotid artery by<br />
resection and primary anastomosis. Laryngoscope 93:1445-1453, 1983.<br />
Guild SR: The glomus jugulare, a nonchromaffin paraganglion, in man. Ann Otol Rhinol Laryngol 62:1045-1071, 1953.<br />
Gulya AJ, Glasscock ME, Jackson CG, et al: Skull-base surgery: Operative refinements. Otolaryngol Head Neck Surg<br />
94:315-320, 1986.<br />
Hatfield PM, James AE, Schulz MD: Chemodectomas of the glomus jugulare. Cancer 30:1164-1168, 1972.<br />
House, WF: Surgical exposure of the internal auditory canal and its contents through the middle cranial fossa.<br />
Laryngoscope 71:1363-1385, 1961.<br />
House WF, Glasscock ME: Glomus tympanicum tumors. Arch Otolaryngol 87:124-128, 1968.<br />
House WF, Hitselberger WE: The transcochlear approach to the skull base. Arch Otolaryngol 102:334-342, 1976.<br />
Hudgins PT: Radiotherapy for extensive glomus. Radiology 103:427-429, 1972.<br />
Hurst WB: Glomus jugulare tumours. J Laryngol Otol 95:581-588, 1981.<br />
Iaccarino V, Sodano A, Belfiore G, et al: Embolization of glomus tumors of the carotid: Temporary or definitive?<br />
Cardiovasc Intervent Radiol 8:206-210, 1985.<br />
Jackson CG: Skull base surgery. Am J Otol 3:161-171, 1981.<br />
Jackson CG, Glasscock ME, Harris PF: Glomus tumors: Diagnosis, classification, and management of large lesions.<br />
Otolaryngol 108:401-406, 1982.<br />
Jackson CG, Glasscock ME, Nissen AJ: Glomus tumor surgery: The approach, results, and problems. Otolaryngologic<br />
Clin North Am 15:897-902, 1982.<br />
Jackson CG, Glasscock ME, McKennan KX: The surgical treatment of skull-base tumors with intracranial extension.<br />
Otolaryngol Head Neck Surg 96:175-185, 1987.<br />
Jackson CG, Welling DB, Chironis P: Glomus tympanicum tumors: Contemporary concepts in conservation surgery.<br />
http://www.bcm.edu/oto/grand/102691.html (5 of 7) [5.11.2005 10:41:59]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Laryngoscope 99:875-916, 1989.<br />
Jenkins HA, Fisch U: Glomus tumors of the temporal region. Otolaryngol 107:209-214, 1981.<br />
Kennedy DW, Nager GT: Glomus tumor and multiple endocrine neoplasia. Otolaryngol Head Neck Surg 94:644-648,<br />
1986.<br />
Kim J, Elkon D, Lim M, et al: Optimum dose of radiotherapy for chemodectomas of the middle ear. Int J Radiation<br />
Oncology Biol Phys 6:815-819, 1980.<br />
Makek M, Franklin DJ, Zhao J, et al: Neural infiltration of glomus temporale tumors. Am J Otol 11:1-5, 1990.<br />
Marsh MA, Jenkins HA, Coker NJ: Extended lateral cranial base surgery, in Cummings DW, et al: Otolaryngology - Head<br />
and Neck Surgery. St. Louis: Mosby, in press.<br />
McCabe B, Flether M: Selection of therapy of glomus jugulare tumors. Arch Otolaryngol 89:182-185, 1969.<br />
Moffat DA, Hardy DG: Surgical management of large glomus jugulare tumours: Infra-and trans-temporal approach. J<br />
Laryngol Otol 103:1167-1180, 1989.<br />
Murphy TP, Brackmann DE: Effects of preoperative embolization on glomus jugulare tumors. Laryngoscope 99:1244-<br />
1247, 1989.<br />
Ossama A, Kersh JE, Routh A, et al: The long-term side effects of radiation therapy for benign brain tumors in adults. J<br />
Neurosurg 73:502-512, 1990.<br />
Pellet W, Cannoni M, Pech A: The widened transcochlear approach to jugular foramen tumors. J Neurosurg 69:887-894,<br />
1988.<br />
Pilepich MV, Konefal JB, Perez CA, et al: Radiation therapy in the treatment of chemodectomas. Laryngoscope 97:1331-<br />
1338, 1987.<br />
Pryzant RM, Chou JL, Easley JD: Twenty year experience with radiation therapy for temporal bone chemodectomas. Int J<br />
Radiation Oncology Biol Phys 17:1303-1307, 1989.<br />
Rosenwasser H: Carotid body tumor of the middle ear and mastoid. Arch Otolaryngol 41:64-7, 1945.<br />
Rosenwasser H: Current management glomus jugulare tumors. Ann Otol Rhinol Laryngol 76:603-10, 1967.<br />
Rosenwasser H: Glomus jugulare tumors. Arch Otolaryngol 88:37-77, 1968.<br />
Rosenwasser H: Glomus jugulare tumors. Arch Otolaryngol 89:186-192, 1969.<br />
Rosenwasser H: Metastasis from glomus jugulare tumors. Arch Otolaryngol 67:197-203, 1957.<br />
http://www.bcm.edu/oto/grand/102691.html (6 of 7) [5.11.2005 10:41:59]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Schwaber MK, Glasscock ME, Nissen AJ, et al: Diagnosis and management of catecholamine secreting glomus tumors.<br />
Laryngoscope 94:1008-1015, 1984.<br />
Shambraugh GE: Surgical approach for so-called glomus jugulare tumors of the middle ear. Laryngoscope 65:185-198,<br />
1955.<br />
Shapiro MJ, Neues DK: Technique for removal of glomus jugulare tumors. Arch Otolaryngol 79:219-224, 1961.<br />
Sharma D, Johnson AP, Whitton AC: Radiotherapy for jugulo-tympanic paragangliomas. J Laryngol Otol 98:621-629,<br />
1984.<br />
Simpson GT, Konrad HR, Takahashi M, et al: Immediate postembolization excision of glomus jugulare tumors.<br />
Otolaryngol 106:1979.<br />
Spector GJ, Maisel RH, Ogura JH: Glomus tumors in the middle ear. I. An analysis of 46 patients. Laryngoscope 83:1652-<br />
1672, 1973.<br />
Spector GJ, Maisel RH, Ogura JH: Glomus jugulare tumors II. a clinicopathologic analysis of the effects of radiotherapy.<br />
Ann Otol 83:26-36, 1974.<br />
Spector GJ, Compagno J, Perez CA: Glomus jugulare tumors: Effects of radiotherapy. Cancer 35:1316-1321, 1975.<br />
Spector GJ, Sobol S: Surgery for glomus tumors at the skull base. Otolaryngol Head Neck Surg 88:524-530, 1980.<br />
Springate SC, Weichselbaum RR: Radiation or surgery for chemodectoma of the temporal bone: A review of local control<br />
and complications. Head Neck Surg 303-307, 1990.<br />
Taylor DM, Alford BR, Greenberg SD: Metastases of glomus jugulare tumors. Arch Otolaryngol 82:5-13, 1965.<br />
Tidwell TJ, Montague ED: Chemodectomas involving the temporal bone. Radiology 118:147-149, 1975.<br />
Wang M, Hussey DH, Doornbos JF: Chemodectoma of the temporal bone: A comparison of surgical and radiotherapeutic<br />
results. Int J Radiation Oncology Biol Phys 14:643-648, 1988.<br />
Zinreich ES, Lee D: Radiotherapy for the treatment of paragangiomas in the temporal bone. Ear Nose Throat J 65:181-4,<br />
1986.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/102691.html (7 of 7) [5.11.2005 10:41:59]
http://www.bcm.edu/oto/grand/31193.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
CONSIDERATIONS IN THE EVALUATION OF THE HEARING<br />
IMPAIRED CHILD<br />
Judith J. Owens, MD<br />
March 11, 1993<br />
Approximately 5,000 children are born every year in the United States who will be found to have a<br />
significant hearing impairment. The hearing loss may be secondary to congenital or postnatally acquired<br />
conditions. Congenital hearing loss is attributed to a defect that the child is born with, either an inherited<br />
genetic defect or the result of a prenatally acquired condition. The important non-hereditary causes of<br />
congenital hearing loss include drug exposure, prenatal infections (TORCH) and erythroblastosis fetalis.<br />
Three-quarters of childhood hearing impairment is postnatally acquired. Infections, drugs,<br />
hyperbilirubinemia, noise exposure, and trauma have all been implicated in contributing to postnatally<br />
http://www.bcm.edu/oto/grand/31193.html (1 of 6) [5.11.2005 10:42:07]
http://www.bcm.edu/oto/grand/31193.html<br />
acquired hearing loss. In addition to meningitis and sepsis, the important infectious diseases associated<br />
with postnatally acquired hearing loss include adenovirus, mumps, chicken pox, hepatitis, EBV, and<br />
influenza. Hyperbilirubinemia when greater than 20 mg % will result in damage to the cochlear nucleus.<br />
Although most hereditary disorders appear to follow the rules of Mendelian inheritance, marked<br />
variability of gene expression and incomplete penetrance may confound the diagnosis and clinical<br />
recognition of many of these disorders. A complete family history is essential to uncover these types of<br />
hearing loss. This is especially true for nonsyndromic inherited hearing loss. The hearing loss may be<br />
present at birth or may develop later in life. All forms of inheritance, autosomal dominant, autosomal<br />
recessive, and X-linked, have been documented in families with nonsyndromal hereditary hearing<br />
impairment (HHI).<br />
Hearing loss is a component of over 200 inherited syndromes. Many syndromes in which hearing loss is<br />
a significant component were reviewed for this presentation. The major features of some of these<br />
syndromes will be reviewed in this abstract.<br />
For convenience these syndromes can be categorized by the association with other morphologic<br />
abnormalities. Important syndromes where deafness is associated with craniofacial abnormalities include<br />
Treacher-Collins, Goldenhar's, Crouzon's, and Apert's syndromes. All except Goldenhar's (AR) are<br />
inherited in an autosomal dominant fashion. Hearing loss in these syndromes is mixed or conductive and<br />
may be surgically correctable.<br />
Hearing loss in association with visual loss is a particularly devastating combination. There are four<br />
important syndromes with this combination: Usher's, Alstrom's, Cockayne's and Refsum's disease. All<br />
are inherited in an autosomal recessive fashion. Retinitis pigmentosa is associated with all except for<br />
Cockayne's syndrome. There are four types of Usher's syndrome. Type I is the most severe and is<br />
associated with vestibular dysfunction<br />
Apert's syndrome consists of progressive renal insufficiency, progressive sensorineural hearing loss and<br />
various ocular abnormalities. This syndrome demonstrates X-linked dominant inheritance: males are<br />
more severely affected and females may have a variable course to their disease because of random X<br />
chromosome inactivation.<br />
Jervell and Lange-Nielsen syndrome is the most common syndrome with cardiac dysfunction and<br />
hearing loss. There is a conduction defect resulting in a prolonged QT interval on electrocardiogram, and<br />
clinically with fainting spells or sudden death. Jervell and Lange-Nielsen is inherited in an autosomal<br />
recessive manner.<br />
Pendred's syndrome is the most frequently occurring example of associated deafness and endocrine<br />
dysfunction. This disorder results from an error in thyroxin metabolism. A goiter may be clinically<br />
palpable and profound sensorineural hearing loss is usually present.<br />
http://www.bcm.edu/oto/grand/31193.html (2 of 6) [5.11.2005 10:42:07]
http://www.bcm.edu/oto/grand/31193.html<br />
Dermal abnormalities and deafness characterize Waardenburg's syndrome and the LEOPARD syndrome.<br />
Clinical features of Waardenburg's include dystopia canthorum, deafness, a high broad nasal root,<br />
synophrys, heterochromia irides, and early graying. There are two types of this syndrome characterized<br />
by the presence or absence of dystopia canthorum. When dystopia canthorum is absent, but the other<br />
features of the syndrome are present, there is a higher incidence of deafness.<br />
Metabolic syndromes, especially the mucopolysaccharidoses, are frequently associated with conductive<br />
or mixed hearing loss. Chromosomal abnormalities, specifically trisomy 13 and 18 are often associated<br />
with deafness. Because these conditions are lethal in early infancy the deafness is of relatively minor<br />
significance. Down's syndrome is often associated with a mixed hearing loss.<br />
Early identification of hearing loss is desirable to optimize rehabilitation. Identification of hearing loss in<br />
young children is facilitated by a clinician who looks carefully for a family history of early hearing loss,<br />
and who is attuned to the many syndromes associated with hearing impairment. Complete otologic and<br />
auditory evaluation of these children is essential.<br />
Case Presentation<br />
An eight-month-old child presented to Texas Children's Hospital for an otologic evaluation. The child<br />
was born full term via an uncomplicated vaginal delivery. There was no history of infections, drug or<br />
alcohol use during the pregnancy. Both parents are hearing- impaired. The mother reported the etiology<br />
of her deafness as "tonsillitis" and the etiology of her husband's hearing loss as "high fever." On physical<br />
examination the child demonstrated multiple stigmata of Waardenburg syndrome including dystopia<br />
cantorum, heterochromia irides, a broad nasal root, and synophrys or confluence of the eyebrows. The<br />
mother has similar features and in addition has a white forelock that is also associated with this<br />
syndrome.<br />
Audiologic evaluation revealed no responses to speech, warble tones, or narrow band noise in the sound<br />
room. Auditory brainstem response audiometry showed no response to air or bone conducted clicks at<br />
equipment levels in either ear. In light of her significant sensitivity loss she was referred for hearing aid<br />
evaluation.<br />
Despite the fact that both parents are hearing-impaired and communicate through signing, they were<br />
anxious to have the child fitted with hearing aids. The parents were referred for genetic counselling to<br />
provide them with a better understanding of the full implications of this disease.<br />
Bibliography<br />
http://www.bcm.edu/oto/grand/31193.html (3 of 6) [5.11.2005 10:42:07]
http://www.bcm.edu/oto/grand/31193.html<br />
Considerations in the Evaluation of the Hearing-Impaired Child<br />
Alford BR. Rubella - la bête noire de la médecine. Laryngoscope 1968;78:1623-1659.<br />
Alport AC. Hereditary familial congenital haemorrhagic nephritis. Br Med J 1927;1:504-506.<br />
Anagnostakis D, Petmezakis J, Papazissis G, Messaritakis J, Matsaniotis N. Hearing loss in low-birth-weight infants. Am J<br />
Dis Child 1982;136:602-607.<br />
Andreoli SP, Deaton M. Alport's syndrome. Ear Nose Throat J 1992;71:508-511.<br />
Batsakis JG, Nishiyama RH. Deafness with sporadic goiter: Penred's syndrome. Arch Otolaryngol 1962;76:401-406.<br />
Cockayne EA. Dwarfism with retinal atrophy and deafness. Arch Dis Child 1936;11:1-8.<br />
Crysdale WE. Otorhinolaryngologic problems in patients with craniofacial anomalies. Otolaryngol Clin North Am<br />
1981;14:145-155.<br />
d'Avignon M, Barr B. Ear abnormalities and cranial nerve palsies in thalidomide children. Arch Otolaryngol 1964;80:136-<br />
140.<br />
Dimitrius A, Petmezakes J, Papazesses G, et al. Hearing loss in low birth weight infants. Am J Dis Child 1982;136:602-<br />
604.<br />
Dodge PR, Hallowell D, Feigin RD, Holmes SJ, Kaplan SL, Jubelirer DP, et al. Prospective evaluation of hearing<br />
impairment as a sequela of acute bacterial meningitis. N Engl J Med 1984;311:869-874.<br />
Everberg G. Deafness following mumps. Acta Otolaryngol 1957;48:397-403.<br />
Feinmesser M, Landau J. Deafness in toxoplasmosis. J Laryngol 1961;75:171-174.<br />
Fisch L. Deafness as part of an hereditary syndrome. J Laryngol Otol 1959;73:355=82.<br />
Fraser GR. The causes of profound deafness in childhood. Baltimore: Johns Hopkins University Press, 1976:11-48.<br />
Fraser GR. Profound childhood deafness. J Med Genet 1964;1:118-151.<br />
Friedmann I, Fraser GR, Froggatt P. Pathology of the ear in the cardio-auditory syndrome of Jervell and Lange-Nielsen<br />
(recessive deafness with electrocardiographic abnormalities). J Laryngol Otol 1966;80:451-470.<br />
Gorlin RJ, Cohen MM, Levin LS. Syndromes of the head and neck, 3rd edition. NY: OUP, 1990.<br />
Grundfast KM, Lalwani AK. Practical approach to diagnosis and management of hereditary hearing impairment (HHI).<br />
http://www.bcm.edu/oto/grand/31193.html (4 of 6) [5.11.2005 10:42:07]
http://www.bcm.edu/oto/grand/31193.html<br />
Ear Nose Throat J 1992;71:479-493.<br />
Hageman MJ, Delleman JW. Heterogeneity in Waardenburg syndrome. Am J Hum Genet 1977;29:468-485.<br />
Hanshaw JB. Congenital cytomegalovirus infection: a fifteen year perspective. J Infect Dis 1971;123:555-561.<br />
Jackler RK, Luxford WM, House WF. Congenital malformations of the inner ear: a classification based on embryogenesis.<br />
Laryngoscope 1987;97(Suppl 40):2-14.<br />
Jervell A, Lange-Nielsen F. Congenital deaf-mutism, functional heart disease with prolongation of the Q-T interval, and<br />
sudden death. Am Heart J 1957;54:59-68.<br />
Johnsen T, Larsen C, Friis J, Hougaard-Hensen F. Pendred's syndrome: acoustic, vestibular and radiological findings in 17<br />
unrelated patients. J Laryngol Otol 1987;101:1187-1192.<br />
Kelemen G. Hurler's syndrome and the hearing organ. J Laryngol Otol 1966;80:791-803.<br />
Kloepfer HW, Laguaite JK. The hereditary syndrome of congenital deafness and retinitis pigmentosa (Usher's syndrome).<br />
Laryngoscope 1966;76:850-862.<br />
Konigsmark BW. Hereditary congenital severe deafness syndromes. Ann Otol Rhinol Laryngol 1981;80:269-288.<br />
Konigsmark BW. Hereditary deafness in man. N Engl J Med 1969;281:713-720,774-778,827-832.<br />
Konigsmark BW, Gorlin RJ. Genetic and metabolic deafness. New York: WB Saunders, 1976.<br />
Kos AO, Schuknecht HF, Singer JD. Temporal bone studies in 13-15 and 18 trisomy syndromes. Arch Otolaryngol<br />
1966;83:439-445.<br />
MacDonald WB, Firch KD, Lewis IC. Cockayne's syndrome. Pediatr 1960;25:997-999.<br />
Matthews NL. Lentigo and electrocardiographic changes. N Engl J Med 1968;278:780-781.<br />
McLay K, Maran AGD. Deafness and the Klippel-Feil syndrome. J Laryngol Otol 1969;83:175-184.<br />
Nance WE, Setleff RC, McLeod A, et al. X-linked mixed deafness with congenital fixation of the stapedial footplate and<br />
perilymphatic gusher. Birth Defects 1971;7:64-69.<br />
Paparella MM, Fox RY, Schachern PA. Diagnosis and treatment of sensorineural hearing loss in children. Otolaryngol<br />
Clin North Am 1989;22:51-74.<br />
Pass RF, Stagno S, Myers GJ, Alford CA. Outcome of symptomatic congenital cytomegalovirus infection: results of longterm<br />
longitudinal follow-up. Pediatr 1980;66:758-762.<br />
Peckham CS, Stark O, Dudgeon JA, et al. Congenital cytomegalovirus infection: a cause of sensorineural hearing loss.<br />
http://www.bcm.edu/oto/grand/31193.html (5 of 6) [5.11.2005 10:42:07]
http://www.bcm.edu/oto/grand/31193.html<br />
Arch Dis Child 1987;62:1233-1237.<br />
Pendred V. Deaf-mutism and goitre. Lancet 1896;2:532.<br />
Preus M, Fraser FC. Genetics of hereditary nephropathy with deafness (Alport's disease). Clin Genet 1971;2:331-337.<br />
Quisling RW, et al. Osteogenesis imperfecta. A study of 160 family members. Arch Otolaryngol 1979;105:207-211.<br />
Refsum S. Heredopathia atactica polyneuritis formis. Acta Psychiatr Scand 1946;38:1-303.<br />
Reynolds DW, Stagno S, Stubbs G, Dahle AJ, Livingston MM, Saxon SS, et al. Inapparent congenital cytomegalovirus<br />
infection with elevated cord IgM levels. N Engl J Med 1974;290:291-296.<br />
Richards BW, Runderl AT. A familial hormonal disorder associated with mental deficiency, deaf-mutism, and ataxia. J<br />
Ment Defic Res 1959;3:33-55.<br />
Robinson GC, Cambon KG. Hearing loss in infants of tuberculous mothers treated with streptomycin during pregnancy. N<br />
Engl J Med 1964;271:949-953.<br />
Scheibe A. A case of deaf-mutism, with auditory atrophy and anomalies of development in the membranous labyrinth of<br />
both ears. Arch Otolaryngol 1892;21:120-122.<br />
Shiller JG. Craniofacial dysostosis of Crouzon. Pediatr 1959;23:107-112.<br />
Schuknecht HF. Pathology of the ear. Cambridge, MA: Harvard University Press, 1974;165-209.<br />
Smith RJH. Medical diagnosis and treatment of hearing loss in children. In: Cummings CW, Harker LA, editors.<br />
Otolaryngology - Head and Neck Surgery. St. Louis: CV Mosby, 1986;3225-3246.<br />
Smith RJH. A DNA linkage study of Usher's syndrome excluding much of chromosome 4. Laryngoscope 1989;99:940-<br />
949.<br />
Waardenburg PJ. A new syndrome combining developmental anomalies of the eyelids, eyebrows and nose root with<br />
pigmentary defects of the iris and head hair and with congenital deafness. Am J Hum Genet 1951;3:195-253.<br />
Wahl RA. Dick M. Congenital deafness with cardiac arrhythmias: the Jervell and Lange-Nielsen syndrome. Am Ann Deaf<br />
1980;125:34-37.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/31193.html (6 of 6) [5.11.2005 10:42:07]
http://www.bcm.edu/oto/grand/6393.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
UPDATE ON HEARING AIDS<br />
Michael G. Stewart, MD<br />
June 3, 1993<br />
Approximately 22 million Americans have some degree of hearing loss.<br />
Currently, patients with sensorineural hearing loss represent approximately 90%<br />
of hearing aid users. The sales of hearing aids in the United States have grown<br />
steadily, from 830,000 units in 1981 to 1,780,000 units in 1992. Behind-the-ear<br />
(BTE) aids represent 18.5% of this total, with body and eyeglass aids accounting<br />
for only 0.4%; the remaining 81.1% sold are in-the-ear (ITE) aids. This is a<br />
distinct change from only ten years ago, when ITE and BTE aids each represented<br />
http://www.bcm.edu/oto/grand/6393.html (1 of 7) [5.11.2005 10:42:11]
http://www.bcm.edu/oto/grand/6393.html<br />
about 50% of the market.<br />
Electronic hearing aids consist of a microphone, an amplifier, and a receiver. The<br />
microphone transduces sound into an electrical signal and sends it to the<br />
amplifier. The amplifier increases the amplitude of the electrical signal, and the<br />
signal may be further modified by filters and volume or tone controls. The<br />
amplified signal is transmitted to the receiver, where it is transduced into sound.<br />
When the amount of amplification is expressed in decibels, it is called the gain of<br />
the aid.<br />
One complaint of most patients with cochlear loss is a decrease in dynamic range,<br />
also called cochlear recruitment. This is because the loudest sounds are still<br />
perceived with the same intensity, whereas patients with cochlear loss are unable<br />
to hear quiet sounds. Therefore the range between comfortable listening and<br />
uncomfortable loudness is much smaller than in normal subjects. Aids must then<br />
be able to supply adequate gain to the user without creating sounds which are too<br />
loud. Most aids sold today use linear amplifiers, which increase the signal<br />
amplitude by a constant amount, regardless of input level. These aids then require<br />
some kind of output limiting - such as peak clipping or compression amplification<br />
- to differentially amplify soft sounds more than loud sounds.<br />
Earmold design is an important factor in aid design. With BTE type aids, a<br />
silicone earmold is used to deliver sound to the ear. With ITE type aids, the aid<br />
itself fits into the EAC. In both cases, the aid potentially acts as an earplug and<br />
creates the so-called "occlusion effect." Completely blocking the canal results in<br />
an increased amplification and perception of low frequencies, especially in the<br />
sound of the wearer's own voice. One solution to this problem is venting, or<br />
making an opening in the earmold or aid, which attenuates (or decreases) the<br />
amplification of low frequencies. However, venting may create a problem of its<br />
own: feedback. Feedback occurs when a microphone is placed very near a<br />
speaker. The microphone picks up the speaker output, which is amplified and sent<br />
to the speaker, which is picked up by the microphone and amplified again, etc.<br />
The capacity of the amplifier is quickly overloaded, and the high-pitched sound<br />
called feedback results. Feedback is an inherent problem with ITE aids because<br />
http://www.bcm.edu/oto/grand/6393.html (2 of 7) [5.11.2005 10:42:11]
http://www.bcm.edu/oto/grand/6393.html<br />
the microphone and speaker are on the same piece of equipment. Venting may<br />
further decrease the amount of gain possible before the microphone picks up the<br />
speaker output and feedback results. Feedback is a less significant problem in<br />
BTE aids because the microphone and speaker are physically separated.<br />
There are several types of aids available. Body aids are seldom used today, but<br />
have very high gain possible because of the separation of microphone and<br />
speaker. Body aids are still used for some patients with profound hearing gloss.<br />
Eyeglass aids allow the fitting of CROS and BICROS hearing aids. CROS aids<br />
are helpful for patients with unaidable loss in one ear only, and BICROS aids are<br />
used for a combination of unaidable loss in one ear and aidable loss in the other.<br />
In BTE aids, the controls, microphone and amplifier are in the body, and sound is<br />
transduced through an earmold. There are three varieties of ITE aids: the fullconcha<br />
aid, the half-concha aid, and the canal aid. Typically ITE and BTE aids<br />
have 65 to 75 dB of gain, and body aids may have 80 dB or higher gain.<br />
The latest technology in hearing aids is the digital aid. In the past, electronic aids<br />
have all used analog circuitry, where the sound is transformed into an electrical<br />
signal and then further modified. There are natural limitations in the amplifier's<br />
ability to amplify the signal without exceeding power limitations or introducing<br />
distortion. In digital technology, the electrical waveform is converted into a<br />
digital code of a series of ones and zeros. This digital signal is then modified by<br />
computer, and transformed back into an electrical signal and sent to the speaker.<br />
The advantage of digital processing is that flexibility is much greater. The digital<br />
waveform can be transformed in complex ways without loss of precision, and the<br />
natural limitations of electronic equipment are not imposed. Specifically, the<br />
frequency response can be adjusted more accurately, the output can be limited at<br />
any frequency to prevent uncomfortable sound levels, filtering is more accurate,<br />
noise is not introduced, and acoustic feedback can be controlled. These<br />
modifications result in the more "natural" sound of digital aids, according to<br />
many aid users.<br />
Although hearing aids are tested and have published specifications, these are<br />
obtained by placing the aid in a standardized device called a 2 cm coupler, and<br />
http://www.bcm.edu/oto/grand/6393.html (3 of 7) [5.11.2005 10:42:11]
http://www.bcm.edu/oto/grand/6393.html<br />
measuring performance. Real ear testing involves the placement of a tiny probe in<br />
the patient's ear canal. The frequency response of the unaided ear canal is<br />
measured, then the aid is placed, and the aided frequency response is measured<br />
using different sound inputs.<br />
ASSISTIVE LISTENING DEVICES<br />
Many patients have a mild to moderate hearing loss or a narrow band of<br />
frequency loss (especially high-frequency loss) that makes hearing aid use<br />
difficult. In addition, some patients do not have the manual or mental dexterity to<br />
use hearing aids. Assistive listening devices are designed to improve hearing<br />
ability in special listening situations - especially if background noise, multiple<br />
talkers or large distances are a problem. There are several types of assistive<br />
devices.<br />
A hard-wired device uses a microphone close to the source which is directly<br />
connected to an amplifier and earphone that the patient wears. The AM radio<br />
signal has been used as a wireless system to transmit sound from the source to<br />
individual receivers. However, AM signal is limited in power and range, and is<br />
very sensitive to electrical disturbances and electronic equipment. Wireless FM<br />
systems are much more popular because FM provides a clear signal that is almost<br />
immune to outside interference. Finally, infrared light has been used as a signal<br />
carrier. Infrared light is invisible, but requires an unobstructed view to the<br />
receiver, and is interfered with by some other sources of light.<br />
These assistive listening devices (ALDs) are all based on the principle of<br />
improving signal to noise ratio (SN ratio), which means that the desired sound is<br />
amplified with respect to surrounding noise. This is very useful for hearingimpaired<br />
persons in lecture halls, school, or church, or for such activities as TV<br />
viewing with a large group of people. ALDs may also be used in conjunction with<br />
a hearing aid.<br />
http://www.bcm.edu/oto/grand/6393.html (4 of 7) [5.11.2005 10:42:11]
http://www.bcm.edu/oto/grand/6393.html<br />
Case Presentation<br />
A 48-year-old male veteran suffered noise exposure while in the service. He was<br />
fitted with a right-side monaural behind-the-ear aid in 1965 while in the military.<br />
He has been followed at the Houston Veterans Affairs Medical Center Audiology<br />
Clinic since 1972, preferring right ear only hearing aid use. His most recent<br />
audiogram shows a stable bilateral moderate to severe sensorineural hearing loss<br />
from low to high frequencies. His discrimination was 80% in the right ear, and<br />
70% in the left. Acoustic reflex thresholds were elevated, but consistent with the<br />
extent of the sensitivity loss, and tympanometry revealed Type A tympanograms.<br />
The patient was recently fitted with bilateral in-the-ear hearing aids, which the<br />
patient uses regularly with good results. His real ear testing reveals excellent<br />
tuning to the computer-simulated parameters.<br />
Bibliography<br />
Berger KW. History and development of hearing aids. In: Pollack MC, editor. Amplification for the Hearing Impaired, 3rd<br />
ed. Orlando: Grune & Stratton, 1988:1-20.<br />
Byrne D. Key issues in hearing aid selection and evaluation. J Am Acad Audiol 1992;3:67-80.<br />
Carver WF. Development of the hearing aid and the hearing aid industry. In: Hodgson WR, Skinner PH, editors. Hearing<br />
Aid Assessment and Use in Audiologic Habilitation. Baltimore: Williams and Wilkins, 1977:5-16.<br />
Cheple M. Hearing aids. In: Paparella MM, et al. Otolaryngology, 3rd ed. Philadelphia: W.B. Saunders, 1991:1017-1024.<br />
Cole WA. Current design options and criteria for hearing aids. JSLPA Monograph 1993;Suppl 1:7-14.<br />
Cranmer-Briskey KS. 1992 Hearing Instruments dispenser survey results. Hear Instrum 1992;(12)43:8-15.<br />
Elfenbein JL, Bentler RA, Davis JM, Niebuhr DP. Status of school children's hearing aids relative to monitoring practices.<br />
Ear Hear 1988;9:212-217.<br />
Gelfand SA, Silman S. Usage of CROS and IROS hearing aids by patients with bilateral high-frequency hearing loss. Ear<br />
Hear 1981;3:24-29.<br />
Harris RW, Brey RH, Chang Y-S, Soria BD, Hilton LM. The effects of digital quantization error on speech intelligibility<br />
and perceived speech quality. J Speech Hear Res 1991;34:189-196.<br />
http://www.bcm.edu/oto/grand/6393.html (5 of 7) [5.11.2005 10:42:11]
http://www.bcm.edu/oto/grand/6393.html<br />
Hecox KE. Digital hearing aid technology: medical perspective. Otolaryngol Clin North Am 1989;22:129-142.<br />
Hecox KE, Punch JL. The impact of digital technology on the selection and fitting of hearing aids. Am J Otol 1988;9:77-<br />
85.<br />
Jerger J, Speaks C, Malmquist C. Hearing-aid performance and hearing-aid selection. J Speech Hear Res 1966;9:136-149.<br />
Jerger J, Malmquist C, Speaks C. Comparison of some speech intelligibility tests in the evaluation of hearing aid<br />
performance. J Speech Hear Res 1966;9:253-258.<br />
Jerger J, Silman S, Lew HL, Chmiel R. Case studies in binaural interference: converging evidence from behavioral and<br />
electrophysiologic measures. J Am Acad Audiol 1993;4:122-131.<br />
Kirkwood DH. 1992 U.S. hearing aid sales: latest HIA reports show lull in market growth. Hear J 1992;45(12):7-15.<br />
Kuk FK. Amplification devices for the hearing-impaired individual. In: Cummings CW, et al. Otolaryngology--Head and<br />
Neck Surgery, 2nd ed. St. Louis: C.V. Mosby, 1993:3127-3141.<br />
Letowski TR, Richards WD, Burchfield SB. Transmission of sound, vibration through earmold materials. Hear Instrum<br />
1992;43(12):11-15.<br />
Levitt H. Future directions in signal processing hearing aids. Ear Hear 1991;12(6 suppl):125S-130S.<br />
Murray DJ, Hanson JV. Application of digital signal processing to hearing aids: a critical survey. J Am Acad Audiol<br />
1992;3:145-152.<br />
Pehringer JL: Assistive devices: technology to improve communication. Otolaryngol Clin North Am 1989;22:143-174.<br />
Pehringer JL, Schirber CM: Assistive devices: new opportunities for rehabilitating hearing impairment. In: Paparella MM,<br />
et al. Otolaryngology, 3rd ed. Philadelphia: W.B. Saunders, 1991:1025-1035.<br />
Podoshin L, Kremer M, Fradis M, Heiglin H. Effect of hearing aids on hearing. Laryngoscope 1984;94:113-117.<br />
Revit LJ. Two techniques for dealing with the occlusion effect. Hear Instrum 1992;43(12):16-18.<br />
Sammeth CA, Ochs MT. A review of current "noise reduction" hearing aids: rationale, assumptions, and efficacy. Ear<br />
Hear 1991; 12(6 suppl):116S-124S.<br />
Skinner MW. Recent advances in hearing aid selection and adjustment. Ann Otol Rhinol Laryngol 1984;93:569-575.<br />
Smriga DJ, Huber TP, Paparella MM. Developments in hearing aid fitting and delivery: a decade of revolution.<br />
Otolaryngol Clin North Am 1989;22:105-127.<br />
Stach BA, Loiselle LH, Jerger JF. Special hearing aid considerations in elderly patients with auditory processing disorders.<br />
http://www.bcm.edu/oto/grand/6393.html (6 of 7) [5.11.2005 10:42:11]
http://www.bcm.edu/oto/grand/6393.html<br />
Ear Hear 1991;12(6 suppl):131S-138S.<br />
Surr RK, Montgomery AA, Mueller HG. Effect of amplification on tinnitus among new hearing aid users. Ear Hear<br />
1985;6:71-75.<br />
Tecca JE. Further investigation of ITE vent effects. Hear Instrum 1992;43(12):8-10.<br />
Tyler RS. What can we learn about hearing aids from cochlear implants? Ear Hear 1991;12(6 suppl):177S-186S.<br />
Vernon J, Griest S, Press L. Attributes of tinnitus and the acceptance of masking. Am J Otolaryngol 1990;11:44-50.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCM Otolaryngology Home Page<br />
® Copyright, 1995-7. All Rights Reserved. Last modified: July 28, 2000 (ASM)<br />
Baylor College of Medicine. The Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/6393.html (7 of 7) [5.11.2005 10:42:11]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for<br />
use by doctors and other health care professionals. These documents were<br />
prepared by resident physicians for presentation and discussion at a<br />
conference held at The Baylor College of Medicine in Houston, Texas. No<br />
guarantees are made with respect to accuracy or timeliness of this material.<br />
This material should not be used as a basis for treatment decisions,<br />
and is not a substitute for professional consultation and/or peerreviewed<br />
medical literature.<br />
Herpes Zoster Oticus<br />
August 21, 1997<br />
F. Christopher Holsinger, M.D.<br />
History<br />
Herpes zoster has been known since antiquity. Herpes is derived from the<br />
Greek meaning “to creep” and zoster “sword belt or girdle.” The Greeks<br />
called it “zona” and for centuries thereafter the disease was thought of as a<br />
cutaneous process. By the nineteenth century, physicians had begun to<br />
question this understanding.<br />
http://www.bcm.edu/oto/grand/082197.html (1 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Bright (1831) and Henley (1840) first suggested that herpes zoster<br />
represented a cutaneous manifestation of a nerve disease involving the<br />
sensory portion of the spinal nerves. Dr. von Barensprung (1861)<br />
demonstrated definitely at autopsy inflammatory lesions at the posterior root<br />
ganglion in a patient with herpes zoster.<br />
Numerous observers described cases of herpetic eruption at the cephalic<br />
extremity due to herpetic infections involving the various cranial nerve<br />
ganglia or the upper cervical spinal root ganglia. Tryde gave the first<br />
description of cases of herpes zoster associated with facial palsy in 1872.<br />
Head and Campbell published their landmark study in 1900. By correlating<br />
autopsy findings and careful, detailed clinical descriptions, these<br />
investigators mapped the sensory dermatomes defined by the dorsal root<br />
ganglia. Their work laid the foundation for future work and focused the<br />
energy and interest of others in this area.<br />
Koerner, writing in the 1904, coined the term “herpes oticus” designating a<br />
syndrome that consists of the triad: blisters at the auricle, facial paralysis,<br />
and inner ear disturbances.<br />
In 1907, Dr. Hunt, chief of Neurological Sciences at the Cornell University<br />
Medical Center, published his hypothesis regarding the etiology of herpes<br />
zoster oticus. Rather than presenting a new theoretic construct for disease,<br />
Dr. Hunt’s theory advanced the work begun by Drs. Head and Campbell<br />
and accurately classified herpes zoster of the head and neck. His paper<br />
represented the capstone of nearly a century of medical research and<br />
debate in this area. Hunt felt that herpetic eruption and associated<br />
symptoms (a viral prodrome, severe otalgia, facial nerve dysfunction,<br />
vesicular eruption involving the pinna, and occasionally vestibulocochlear<br />
symptoms), which he was the first to describe together as part of a clinical<br />
syndrome, were actually the result of, in his words, geniculate ganglionitis.<br />
Hunt analyzed the sensory innervation of the ear and described the “zoster<br />
zone” for the geniculate ganglion as comprising a portion of the tympanic<br />
membrane, the external auditory canal, the tragus, antitragus, concha, a<br />
part of the helix, and a strip of the lobule. Here the typical herpetic lesions<br />
of geniculate zoster are most commonly found. The geniculate zone of the<br />
auricle is bounded anteriorly by the gasserian zone and posteriorly by the<br />
cervical zone, with some overlapping. Hunt classified herpes zoster at the<br />
cephalic extremity according to the sensory ganglion involved and the site<br />
of the rash into the following groups: (1) geniculate herpes zoster (herpes<br />
http://www.bcm.edu/oto/grand/082197.html (2 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
oticus), (2) gasserian herpes zoster (herpes facialis), and (3) cervical<br />
herpes zoster (herpes occipito-collaris)<br />
Hunt then further classified the herpes zoster oticus syndrome according to<br />
severity of symptoms and the degree of extension: (1) herpes zoster<br />
auricularis without neurological signs, (2) herpes zoster oticus with facial<br />
palsy, (3) herpes zoster oticus with facial palsy and mild acoustic symptoms<br />
(diminished hearing and tinnitus), and (4) herpes zoster oticus with facial<br />
palsy and Ménière’s syndrome complex (deafness, tinnitus, vertigo,<br />
nystagmus, nausea, and vomiting). Ramsay Hunt described not so much a<br />
discrete clinical syndrome but rather a spectrum of herpetic disease,<br />
involving the ear and cranial nerves VII and VIII.<br />
To support this classification scheme, he postulated that the major site of<br />
the pathologic lesion in herpes zoster oticus was the geniculate ganglion of<br />
the facial nerve. Increased pressure of the swollen ganglion on the facial<br />
nerve resulted in facial palsy. He further postulated that the etiology of the<br />
Ménière’s syndrome complex was either the simultaneous infection of the<br />
adjacent ganglions of the eighth nerve or the extension of the inflammatory<br />
process from the facial to the auditory nerve by means of nerve fibers that<br />
communicate between the two. He believed that this clinical syndrome<br />
represented “geniculate ganglionitis.” Unfortunately, he was not able to<br />
provide evidence for his theory. With histopathologic studies of autopsy<br />
speciments, subsequent investigators demonstrated little, if any, ganglion<br />
involvement.<br />
Denny-Brown and his colleagues in 1944 were the first to challenge Hunt’s<br />
theory. They examined histopathologic specimens from a patient with<br />
auricular and occipital herpes zoster and facial palsy. At autopsy, they<br />
found no changes in the geniculate ganglion, but were able to demonstrate<br />
other significant findings: a necrotizing ganglionitis of the second cervical<br />
ganglion and a patchy motor neuritis of the facial nerve. They concluded<br />
“the evidence for geniculate ganglionitis in the Ramsay Hunt syndrome is<br />
invalid.”<br />
In time, virology research further clarified these questions. Tissue culture<br />
studies published by Drs. Weller and Coons in 1954 confirmed the theory<br />
that the virus that causes varicella and herpes zoster is one in the same. In<br />
1965, Hope-Simpson’s novel hypothesis unified thinking on herpes zoster<br />
and has laid the foundation for our current understanding. He suggested<br />
that the varicella virus lies dormant in the sensory ganglion after the initial<br />
infection. In a patient with low circulating antibodies, the virus would<br />
reactivate and infection would then manifest itself as herpes zoster,<br />
http://www.bcm.edu/oto/grand/082197.html (3 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
anywhere along the distribution supplied by that particular ganglion. Indeed,<br />
the facial nerve may be affected at any site from the brainstem to the<br />
periphery by the herpes virus. What is still not known is what activates the<br />
virus after it has lain dormant for so long.<br />
In 1967, Blackley presented histologic evidence to support this emerging<br />
notion. He found extensive lymphocytic infiltration along the course of the<br />
facial nerve, as well as divisions of the VIII cranial nerve including vestibular<br />
and cochlear ganglia. Massive lymphocytic infiltration of the right facial<br />
nerve was seen. In addition, there was collapse and disruption of<br />
Reissner’s membrane, an increase of round cells in the stria vascularis, and<br />
destruction of the organ of Corti near the apical turn. Broad perivascular<br />
cuffing of several vessels is seen and marked atrophy of spiral neurones.<br />
Epidemiology<br />
A Mayo clinic study estimated the annual incidence of herpes zoster,<br />
regardless of site, as 130 cases per 100,000. The attack rate increased<br />
dramatically over the age of 60, and 10% this population had identifiable<br />
risk factors for decreased cell-mediated immunity including carcinoma,<br />
trauma, radiation therapy, or chemotherapy. The increased incidence in the<br />
elderly population is explained by a decrease in cellular immune response<br />
to varicella-zoster virus with age.<br />
Adour reported the incidence as 5 per 100,000 a year, or one case every<br />
52 minutes. These age-adjusted incidence figures for VZV cranial neuritis<br />
with facial paralysis parallel those Hope-Simpson estimated for VZV in the<br />
general population in 1965. These figures compare with those for Bell’s<br />
palsy: 20 per 100,000 per year. Few studies outside J.R. Hunt’s own<br />
assess the incidence of herpes zoster oticus in the population.<br />
Microbiology: The Herpesvirus family<br />
Members of the family herpesviridae are found in a wide range of host<br />
systems. To date, at least seven different species are known to infect man,<br />
including herpes simplex virus (HSV); cytomegalovirus (CMV), Epstein Barr<br />
virus (EBV), and varicella zoster (VZV).<br />
Nomenclature is critical. It is important to distinguish VZV as a member of<br />
the greater family of herpes viruses. But it is distinct from herpes simplex.<br />
This is a common point of confusion.<br />
http://www.bcm.edu/oto/grand/082197.html (4 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
The varicella-zoster virus (VZV) belongs to the herpes family. It is a doublestranded<br />
DNA virus that causes chicken pox (varicella) and zoster<br />
infections. Again what distinguishes Varicella from Zoster is the time of<br />
presentation. Reactivation of virus stored in sensory ganglia from previous<br />
varicella infection results in zoster.<br />
Herpes viruses have an envelope surrounding an icosahedral capsid,<br />
approximately 100nm in diameter, which contains the dsDNA genome.<br />
When the envelope breaks and collapses away from the capsid, negatively<br />
stained virions have a typical "fried-egg" appearance.<br />
Work Up and Evaluation<br />
A thorough history and physical examination, a fundamental axiom in<br />
medicine, is the most crucial element of the work-up. Diagnosis still hinges<br />
on the clinical findings described in Hunt's classification scheme.<br />
Clinical Presentation<br />
Frequently, the first symptom is a deep, burning pain in the region of the<br />
ear. This is shortly followed in 1 to 4 days by a vesicular eruption of the<br />
EAC and concha, or, less frequently, of the face, neck, trunk, palate or<br />
fauces. The distribution of the vesicles depends on which sensory afferent<br />
fibers are involved by the viral eruption, but all the fibers may be involved,<br />
including cranial nerves V, IX, X and the cervical plexus arising from<br />
cervical roots II, III, IV. Cranial nerves VII and VIII are almost always both<br />
involved. During the acute illness, a varicelliform rash often accompanies<br />
the painful vesicular eruption. Facial nerve paralysis, vertigo, and hearing<br />
loss are commonly seen.<br />
Natural History<br />
The natural history of herpes zoster oticus differs from that of Bell’s palsy in<br />
several ways, perhaps reflecting the difference in the behavior of herpes<br />
simplex type I and VZV. Bell’s palsy recurs in 10% -12% of cases, but<br />
herpes zoster oticus rarely recurs. In addition, the acute phase of the<br />
infection, as measured by electrical response and progression, peaks in 5<br />
to 10 days with Bell’s palsy, whereas herpes zoster oticus peaks in days 10<br />
to 14. Finally, 84% of individuals with Bell’s palsy have a satisfactory<br />
recovery of function, but only 60% of patients with herpes zoster oticus<br />
recover function.<br />
http://www.bcm.edu/oto/grand/082197.html (5 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Crabtree (1968) was among the first to suggest that complete facial nerve<br />
recovery is less likely following herpes zoster oticus than in other cases of<br />
idiopathic facial palsy—despite treatment with high-dose steroids. Ten<br />
percent of patients with total facial nerve paralysis and 66 percent of those<br />
with partial paralysis recover completely. Recovery is better in those cases<br />
in which vesicles appear prior to nerve paralysis. Two percent of patients<br />
over age 50 will have severe, while nine percent will have moderate, post<br />
herpetic neuralgia.<br />
The timing of the appearance of the vesicular eruption may have prognostic<br />
significance. In most cases, eruption and paralysis occur simultaneously. In<br />
approximately 25% of cases, the eruption precedes the paralysis, and the<br />
likelihood of recovery is higher in this group (Devriese and Moesker, 1988).<br />
Diagnosis<br />
The Tzanck prep, which is useful with herpes zoster, located on the truck in<br />
more peripheral nerve distribution areas, required toluidine blue staining a<br />
scraping from the blister. Occasionally, these blisters are located medially in<br />
the ear canal, andl are quite small. So, often it is difficult to obtain adequate<br />
specimens for the prep. A positive prep demonstrates multinucleated giant<br />
cells. Vesicular fluid, when present, can be cultured with human diploid<br />
fibroblasts and after 3-5 days multinucleated giant cells within the fibroblast<br />
population can confirm clinical diagnosis. These studies, however, require<br />
five days or more to produce results. Laboratory confirmation of the<br />
diagnosis is based on increasing antibody titers in repeated complement<br />
fixation tests. Immunofluorescence of varicella antigen obtained from<br />
exfoliated cells from lesions can provide a more expedient verification of<br />
clinical suspicion. Often, diagnosis rests alone on the clinical criteria,<br />
defined by Dr. Hunt<br />
Diagnosis: Immunological Evaluation<br />
Clinical diagnosis can be confirmed by either viral culture or fluorescence<br />
antibody testing using VZV identification reagent (Fluorescein<br />
isothiocyanate-conjugated monoclonal anti-VZV; Ortho Diagnostic<br />
Systems).<br />
Hadar and colleagues from the Tel-Aviv University Medical Centers<br />
designed and tested VZV-specific IgG and IgA antibody titers in serial<br />
serum samples of 23 patients with Ramsay Hunt using immunoperoxidase<br />
assay. They demonstrated that all patients had VZV-specific IgG<br />
http://www.bcm.edu/oto/grand/082197.html (6 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
antibodies, but IgA can be a useful marker in confirming early diagnosis of<br />
the disease.<br />
The mechanism of reactivation of VZV in herpes zoster oticus has not been<br />
clarified. Although the mechanism involved in general herpes zoster is also<br />
unclear, deterioration of cell-mediated immunity is thought to play a specific<br />
role as the “trigger” in reactivating the virus. The term "cellular immunity"<br />
colloquially refers to the T cell system. In fact, cell-mediated immunity is<br />
initiated by lymphokines produced by activated CD4+ T cells, activate<br />
macrophages and the precursors of CD8+ cytotoxic T cells. These effector<br />
cells then cause cell-mediated immune responses such as delayed- types<br />
hypersensitivity and cell-mediated cytotoxicity.<br />
Nucleic acid hybridization and more recently polymerase chain reaction<br />
technology have confirmed VZV latency in human sensory dorsal root<br />
ganglia.<br />
Diagnosis: Audiological Evaluation<br />
In 1976, Byl and Adour were the first to thoroughly review the auditory<br />
symptoms and audiological data associated with herpes zoster oticus. They<br />
compared auditory symptoms in patient’s with Bell’s palsy and herpes<br />
zoster oticus. of 1080 patients with idiopathic facial paralysis, 29% of<br />
patients had auditory symptoms, while 37% of 172 patients with HZO had<br />
these symptoms. In their series of 1252 patients, 377 patients with facial<br />
paralysis had auditory symptoms. However, in only 11 of these 377 patients<br />
were abnormal cause-related sensorineural hearing loss documented with<br />
audiological testing. All of these patients had been diagnosed with HZO.<br />
These authors were the first to recommend a diagnosis in patients with<br />
idiopathic facial nerve paralysis and hearing loss—even when the<br />
characteristic vesicular eruption was absent. In their series, when recovery<br />
of auditory function occurs, a high-frequency sensorineural loss may<br />
persist, except in younger patients. Factors that appeared favorable for the<br />
recovery of hearing include not being older than 64 years, a mild initial<br />
hearing loss, a cochlear pattern of hearing loss, and absence of vertigo.<br />
Wayman et al in 1990 retrospectively reviewed the audiological<br />
manifestations of herpes zoster oticus in 186 patients. In their study, active<br />
herpes zoster infection was confirmed by a four-fold increase between<br />
acute and convalescent complement fixation serum titres of VZV.<br />
Audiograms were performed on 152 patients, 82%, not all of whom had<br />
auditory symptoms at the time. Seven of these underwent more extensive<br />
http://www.bcm.edu/oto/grand/082197.html (7 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
evaluation to determine a cochlear or retrocochlear pattern of hearing loss.<br />
Patients with a demonstrated cause-related hearing loss were treated with<br />
oral prednisone, 60mg/day for six days, then gradually tapered. Of the 152<br />
initial audiograms, 93 or 61% were normal, 29 or 19% were cause-related<br />
abnormal, and 30 or 20% were unrelated abnormal examinations. This final<br />
group was excluded from their analysis. Vertigo was documented in 8 of 29<br />
of the cause-related hearing loss patients and in only 5 of 93 (5%) of<br />
normal hearing patients [p=0.002]. Vertigo was more likely with increased<br />
severity of hearing loss in the isolated high-frequency hearing loss group.<br />
Of the seven patients who underwent more extensive audiological work-up,<br />
six had findings consistent with cochlear pathology: elevated SISI, ABLB<br />
recruitment pattern, type II Bekesy tracing, with no evidence of tone delay.<br />
The seventh patient had severe speech-frequency hearing loss with a<br />
speech discrimination score of 18%, type IV Bekesy tracing, evidence of<br />
tone delay, and grossly abnormal brainstem evoked response with marked<br />
delay or wave V latency, all suggestive of retrocochlear hearing loss. No<br />
correlation was demonstrated between severity of facial paralysis and<br />
presence of any hearing loss. The incidence of incomplete paralysis was<br />
68% in the normal hearing and 62% in the cause-related abnormal hearing<br />
group. Extrapolating their clinical data to the previous histopathologic<br />
findings, especially of Blackley et al., these investigators suggested that a<br />
cochlear pattern represents inflammation confined to the cochlea while the<br />
retrocochlear pattern represents a more profound change involving the<br />
entire nerve.<br />
Diagnosis: Radiological Evaluation<br />
Magnetic resonance imaging has added a new dimension to the research<br />
of herpes zoster oticus and confirmed the histopathologic findings of early<br />
investigators. Images are taken with and without the paramagnetic agent<br />
Gadolinium as a contrast medium. Gadolinium does not normally cross the<br />
blood-brain barrier but this barrier is broken down in the presence of<br />
inflammation or edema. This results in increased signal density and<br />
enhancement in these areas. Another reason suggested for abnormal<br />
enhancement in these situations is venous congestion in the epineurium<br />
and perineurium. There is little dispute that the facial nerve enhances on<br />
MRI in the majority of patients with acute facial palsy, but the role of MRI in<br />
differential diagnosis and prognostic determination is not entirely clear. The<br />
majority of published studies refer to MRI of the facial nerve in idiopathic<br />
Bell’s facial palsy. It has been shown that even the normal facial nerve<br />
shows some mild to moderate enhancement of the geniculate ganglion and<br />
the tympanic-mastoid segment. Nearly twenty studies of the use of MRI in<br />
evaluation have been published. All the papers reported enhancement of<br />
http://www.bcm.edu/oto/grand/082197.html (8 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
the facial nerve on MRI scanning in the majority of patients with facial palsy<br />
but only three papers suggested that the degree of enhancement or the<br />
anatomical level of the facial nerve enhancement had any prognostic<br />
significance. Brugel et al (1993) concluded that moderate enhancement in<br />
the geniculate ganglion as well as in the labyrinthine segment correlated<br />
with a good prognosis with respect to restoration of facial movement while<br />
an increased enhancement correlated with poor prognosis. Yanagida et al<br />
in 1993 noted that in subjects with Ramsay Hunt syndrome who experience<br />
internal auditory symptoms such as vertigo and tinnitus, enhancement was<br />
not only in the facial nerve but also in the vestibular and cochlear nerves.<br />
Treatment: Medical Management<br />
Introduced in 1977, the antiviral agent acyclovir has dramatically improved<br />
the treatment of herpesviridae infections. In the treatment of herpes zoster<br />
oticus, acyclovir therapy can be expected to produce House-Brackmann<br />
grade I-III recovery in most cases. Consequently, the success of antiviral<br />
therapy has greatly diminished enthusiasm for surgical decompression in<br />
cases of herpes zoster oticus with facial nerve paralysis.<br />
Acyclovir remains the most widely prescribed and clinically effective<br />
antiviral drug available. It is 9-(2-hydroxy-methyl) guanine and a selective<br />
inhibitor of the replication of varicella-zoster and both herpes simplex types<br />
1 and 2. It is converted by virus-encoded thymidine kinase to its<br />
monophosphate derivative, an event that does not occur to any substantial<br />
extent in uninfected cells. Subsequent disphosphorylation and<br />
triphosphorylation are then catalyzed by cellular enzymes resulting in<br />
acyclovir triphosphate concentrations that are 40 to 100 times higher in VZVinfected<br />
cells than uninfected cells. Acyclovir triphosphate inhibits viral DNA<br />
synthesis by competing with deoxyguanosine triphosphate as a substrate<br />
for viral DNA polymerase. Because acyclovir triphosphate lacks the 3’-<br />
hydroxyl group required to elongate the DNA chain, the synthesis of viral<br />
DNA is terminated. Furthermore, the viral DNA polymerase is tightly<br />
associated with the terminated DNA chain and is functionally inactivated.<br />
Viral polymerase has greater affinity for acyclovir triphosphate than does<br />
cellular DNA polymerase, resulting in little incorporation of acyclovir into<br />
cellular DNA. In vitro, acyclovir is most active against HSV-1, HSV-2, and<br />
VZV (average median effective concentrations 0.04, 0.10, and 0.50 µg per<br />
mL respectively.) Higher concentrations are required to inhibit replication of<br />
the Epstein Barr virus. Cytomegalovirus, which lacks a virus-specific<br />
thymidine kinase, is resistant.<br />
Absorption from the GI tract is only 15% - 25% of the ingested dose. In<br />
http://www.bcm.edu/oto/grand/082197.html (9 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
addition, the blood-brain barrier results in a 50% reduction of circulating<br />
acyclovir into cerebrospinal fluid. Thymidine kinase found in VZV has<br />
diminished affinity for acyclovir than TK found in HSV. For these reasons,<br />
the oral dose is more substantial than the recommended dose for herpes<br />
simplex.<br />
A recent randomized prospective clinical study in the NEJM compared 7-<br />
day treatment of acyclovir to two other treatment arms: 21-day course of<br />
acyclovir with and without prednisone. Neither additional treatment reduced<br />
the frequency of post-herpetic neuralgia.<br />
HSV can develop resistance to acyclovir through mutations in the viral gene<br />
encoding thymidine kinase, through the generation of thymidine-kinase<br />
deficient mutants or through the selection of mutants possessing a<br />
thymidine kinase that is unable to phosphorylate acyclovir.<br />
Acyclovir-resistant isolates of VZV have been identified much less<br />
frequently than acyclovir-resistant HSV, but they have recently been<br />
recovered from bone-marrow transplant patients and AIDS patients. The<br />
acyclovir-resistant isolates all had altered or absent thymidine kinase<br />
function but remained susceptible to vidarabine and foscarnet. Acyclovir<br />
therapy has been associated with very few adverse effects. Renal<br />
dysfunction has been reported, especially in patients given large doses of<br />
acyclovir by rapid intravenous infusion. This appears to be an uncommon<br />
finding and usually reversible. Administering the drug in a slow infusion and<br />
ensuring adequate hydration can minimize the risk of administering<br />
acyclovir. On the other hand, oral acyclovir even at doses of 800mg five<br />
times daily has not been associated with renal dysfunction.<br />
Several limited retrospective studies have been done to examine<br />
specifically the role of acyclovir in herpes zoster oticus.<br />
Hall and Kerr from the Royal Victoria Hospital in Belfast reported in a 1985<br />
edition of the Lancet the first use of acyclovir for herpes zoster oticus. They<br />
treated seven patients with HZO with a parenteral dose of 5 mg/kg three<br />
times per day. Within 3 days these investigators noted a striking<br />
improvement in the toxemia associated with this condition. Of the six<br />
patients who had total facial paralysis, four recovered completely, one<br />
partially recovered, and one patient had no recovery.<br />
Stafford and Welch reported a year later from Newcastle upon Tyne<br />
another small series of only 5 patients. Each patient received intravenous<br />
http://www.bcm.edu/oto/grand/082197.html (10 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
administration of acyclovir (5mg/kg) TID for a minimum of three days,<br />
followed by a two-week course of oral acyclovir. High-dose oral steroids<br />
(20mg PO QID in four cases; 10mg IVSS dexamethasone QID x 3 days)<br />
were prescribed for 5 days in full dosage, tapered gradually over another<br />
week. Each patient made a “satisfactory” recovery (4 patients with complete<br />
recovery by six months; one with partial recovery).<br />
Dickens et al published their results in 1988. All patients received<br />
intravenous acyclovir 10mg/kg every 8 hours over a 7-day hospitalization<br />
period. Five of seven patients showed some return of facial function at the<br />
time of discharge. Their study suggests that prognosis depends on<br />
immediate initiation of therapy, and that multiple cranial nerve involvement<br />
did not appear to be a negative prognostic indicator.<br />
Newer antiviral agents are available now for the treatment of herpes zoster.<br />
Valaciclovir and Famciclovir are both available in oral preparations and in<br />
more convenient thrice-daily dosing regimen.<br />
Valaciclovir is the l-valine ester of acyclovir and essentially an acyclovir<br />
prodrug. It is rapidly and almost completely converted to acyclovir in vivo.<br />
Valaciclovir requires less frequent dosing than acyclovir due to its superior<br />
bioavailability over acyclovir. Acyclovir bioavailability is 3—5 times greater<br />
when administered as valaciclovir compared to 800 mg oral doses of<br />
acyclovir. Major adverse reactions include nausea (16%-19%), headache<br />
(11%-14%), vomiting (4%-9%), diarrhea (4%-6%).<br />
Famciclovir is an oral prodrug for penciclovir and acts through a mechanism<br />
that is similar to that of acyclovir. Recommended dose for herpes zoster is<br />
500mg PO TID for 7 days. It also is reported to diminish post-herpetic<br />
neuralgias.<br />
Oral steroids have been used in zoster infections since the early 1950's.<br />
Some studies advocate the use of steroids along with acyclovir to reduce<br />
the incidence of post herpetic neuralgia and to enhance facial nerve<br />
recovery. Recovery of labyrinthine dysfunction after pharmacological<br />
therapy is not delineated in the current literature.<br />
Case Presentation<br />
http://www.bcm.edu/oto/grand/082197.html (11 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
A 62-year-old white male presented for consultation to the VAMC<br />
Otolaryngology—Head and Neck Surgery service. The patient reported a 3-<br />
day history of left facial weakness, left otalgia, and left hearing loss. There<br />
was no vertigo, nausea or vomiting, no recent otologic infection, and no<br />
recent trauma to the head and neck. On physical examination, a vesicular<br />
eruption was noted over the left concha and extending into the left external<br />
auditory canal. Grade IV House-Brackmann facial nerve weakness was<br />
noted. There was numbness and vesicular eruption along the V2 trigeminal<br />
nerve distribution. No nystagmus was elicited. Cranial nerves I-VI, IX, X, XI,<br />
XII were grossly intact. A diagnosis of herpes zoster oticus was made.<br />
Treatment was begun with oral regimen of acyclovir 800mg five doses per<br />
day. Oral prednisone (20mg PO TID) for 5 days was begun and gradually<br />
tapered over the next week. The patient was instructed in the use of<br />
artificial tears, lacrilube, and nightly application of a left eyepatch. At 3-<br />
month follow-up, the vesicular eruption had completely resolved and facial<br />
nerve function had returned to normal (House-Brackmann Grade I). There<br />
was no post-herpetic neuralgia.<br />
Bibliography<br />
Aleksic SN, Budzilovich GN, Lieberman AN. Herpes zoster oticus and facial paralysis<br />
(Ramsay Hunt Syndrome). J Neurol Sci 1973;20:149-159.<br />
Anderson RE, Laskoff JM. Ramsay Hunt syndrome mimicking intracanalicular acoustic<br />
neuroma on contrast-enhanced MR. Am J Neuroradiol 1990;11:409.<br />
Aono T, Murakami S, Yanagihara N, Yamanishi K. Detection of human alphaherpesvirus<br />
DNA using consensus primers and specific probes. Acta Otolaryngol Suppl<br />
1994;514:132-134.<br />
Berg R, Forsgren M, Schiratzki H. Acute facial palsy. Acta Otolaryngol 1976;81:462-467.<br />
Brandle P, Satoretti-Schefer S, Bohmer A, Wichmann W, Fisch U. Correlation of MRI,<br />
clinical, and electroneuronographic findings in acute facial nerve palsy. Am J Otol<br />
1996;17:154-161.<br />
Beutner KR, Friedman DJ, Forszpaniak C, Andersen PL, Wood MJ. Valaciclovir<br />
compared with acyclovir for improved therapy for herpes zoster in immunocompetent<br />
adults. Antimicrob Agents Chemother 1995;39:1546-1553.<br />
http://www.bcm.edu/oto/grand/082197.html (12 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Blackley B, Friedmann I, Wright I. Herpes zoster auris associated with facial nerve palsy<br />
and auditory nerve symptoms: a case report with histopathological findings. Acta<br />
Otolaryngol 1967;63:533-550.<br />
Burgoon CF, Burgoon JS, Baldridge GD. The natural history of herpes zoster. JAMA<br />
1957;164:265-268.<br />
Byl FM, Adour KK. Auditory symptoms associated with herpes zoster or idiopathic facial<br />
paralysis. Laryngoscope 1977;87:372-379.<br />
Carroll SM, Mastaglia FL. Optic neuropathy and ophthalmoplegia in herpes zoster<br />
oticus. Neurol 1979;29:726-729. Crabtree JA. Herpes zoster oticus. Laryngoscope<br />
1968;78:1853-1878.<br />
Crabtree JA. Herpes zoster and facial paralysis. Otolaryngol Clin North Am 1974;7:369-<br />
373.<br />
Crumpacker C . The pharmacological profile of famciclovir. Sem Dermatol<br />
1996;15(Suppl 1):14-26, 1996. Daniels DL, Czervionke LF, Millen SJ. MR findings in the<br />
Ramsay Hunt syndrome. Am J Neuroradiol 1988;9:609.<br />
Denny-Brown D, Adams RD, Fitzgerald PJ. Pathologic features of herpes zoster. Arch<br />
Neurol Psychiatr 1944;51:216.<br />
Devriese PP, Moesker WH. The natural history of facial paralysis in herpes zoster. Clin<br />
Otolaryngol 1988;13:289-298.<br />
Dickins JRE, Smith JT, Graham SS. Herpes zoster oticus: treatment with intravenous<br />
acyclovir. Laryngoscope 1988;98:776-779.<br />
Downie AC, Howlett DC, Koefman RJ, Banerjee AK, Tonge KA . Case report: prolonged<br />
contrast enhancement of the inner ear on magnetic resonance imaging in Ramsay Hunt<br />
syndrome. Br J Radiol 1994;67:819-821.<br />
Djupesland G, Degre M, Stien R, Skrede S. Acute peripheral facial palsy. Arch<br />
Otolaryngol 1977;103:641-644.<br />
Fisch U. Surgery for Bell's palsy. Arch Otolaryngol 1981;107:1-11.<br />
Gelfand ML. Treatment of herpes zoster with cortisone. JAMA 1954;154:911-912.<br />
Goldsmith P, Zammit-Maempel I, Meikle D. Ramsay Hunt syndrome mimicking acoustic<br />
neuroma on MRI. J Laryngol Otol 1995;109:1013-1015.<br />
Hall SJ, Kerr AG. Acyclovir in herpes zoster oticus. Lancet 1985;1(8437):1103.<br />
http://www.bcm.edu/oto/grand/082197.html (13 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Harner SG, Heiny BA, Newell RC. Herpes zoster. Arch Otolaryngol 1970;92:632-635.<br />
Head H, Campbell AW. The pathology of herpes zoster: a long-term study and a new<br />
hypothesis. Brain 1900;23:353.<br />
Hope-Simpson RE. The nature of herpes zoster: a long-term study and a new<br />
hypothesis. Proc Royal Soc Med 1965;58:9-20.<br />
House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg<br />
1985;93:146-147.<br />
Huff JC, Bean B, Balfour HH Jr, Laskin OL, Connor JD, Corey L, et al. Therapy of<br />
herpes zoster with oral acyclovir. Am J Med 1988;85:84-89.<br />
Hunt JR. Herpetic inflammations of the geniculate ganglion. A new syndrome and its<br />
complications. J Nerv Ment Dis 1907;34:73-96.<br />
Ikeda M, Hiroshige K, Abiko Y, Onoda K. Impaired specific cellular immunity to the<br />
varicella-zoster virus in patients with herpes zoster oticus. J Laryngol Otol 1996;110:918-<br />
921.<br />
Inamura H, Aoyagi M, Tojima H, Koike Y. Viral infection in acute peripheral facial palsy:<br />
investigation in Yamagata prefecture. Acta Otolaryngol Suppl 1988;446:23-26.<br />
Johnson L, Zonderman B. Herpes zoster oticus (“Ramsay Hunt Syndrome”): a report of<br />
a case. Arch Otolaryngol 1948;48:1-8.<br />
Jonsson L, Tien R, Engstrom M, Thuomas KA. Gd-DPTA enhanced MRI in Bell's palsy<br />
and herpes zoster oticus: an overview and implications for future studies. Acta<br />
Otolaryngol 1995;115:577-584.<br />
Kanzaki J. Electrodiagnostic findings in the early stages of Bell's palsy and Ramsay-<br />
Hunt's syndrome. Acta Otolaryngol Suppl 1985;446:42-46.<br />
Keane JR. Delayed trochlear nerve palsy in a case of zoster oticus. Arch Ophthalmol<br />
1975;93:382-383.<br />
Korzec K, Sobol SM, Kubal W, Mester SJ, Winzelberg G, May M. Gadolinium-enhanced<br />
magnetic resonance imaging of the facial nerve in herpes zoster oticus and Bell's palsy:<br />
clinical implications. Am J Otol 1991;12:163-168.<br />
Kukimoto N, Ikeda M, Yamada K, Tanaka M, Tsurumachi M. Tomita H. Viral infections in<br />
acute peripheral facial paralysis: nationwide analysis centering on CF. Acta Otolaryngol<br />
Suppl 1988;446:17-22.<br />
Kuo MJ, Drago PC, Proops DW, Chavda SV. Early diagnosis and treatment of Ramsay<br />
http://www.bcm.edu/oto/grand/082197.html (14 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Hunt syndrome: the role of magnetic resonance imaging. J Laryngol Otol 1995;109:777-<br />
780.<br />
LaBagnara J, Jahn AF, Habif DV, Solomon EM. MRI findings in two cases of acute facial<br />
paralysis. Otolaryngol Head Neck Surg 1989;101:562-565.<br />
Lee D, Belmont M, Lucente FE. Pathologic quiz case 2. Bilateral herpes zoster oticus.<br />
Arch Otolaryngol Head Neck Surg 1996;122:195,197-198.<br />
May M, Schlaepfer WW. Bell's palsy and the chorda tympani nerve: a clinical and<br />
electron microscopic study. Laryngoscope 1975;85:1957-1975.<br />
May M, Shambaugh GE Jr. Facial nerve paralysis. In: Paparella MM, Shumrick DA,<br />
Gluckman JL, Meyerhoff WL, editors. Otolaryngology, 3rd ed. Philadelphia: Saunders;<br />
1991. pp.1123-1124.<br />
Neely JG, Joaquin AH, Kohn LA, Cheung JY. Quantitative assessment of the variation<br />
within grades of facial paralysis. Laryngoscope 1996;106:438-442.<br />
Obituary: JR Hunt. J Nerv Disorders Ment Dis 1938;87:394-402.<br />
Osumi A, Tien RD. MR findings in a patient with Ramsay-Hunt syndrome. J CompAssist<br />
Tomogr 1990;14:991-993<br />
Peterslund NA, Seyer-Hansen K, Ipsen J, Esmann V, Schonheyder H, Juhl H. Acyclovir<br />
in herpes zoster. Lancet 1981;2(8251):827-830.<br />
Proctor L, Lindsay J, Perlman H, Matz G. Acute vestibular paralysis in herpes zoster<br />
oticus. Ann Otol Rhinol Laryngol 1979;88:303-309.<br />
Ragozzino MW, Melton LJ 3d, Kurland LT, Chu CP, Perry HO. Population-based study<br />
of herpes zoster and its sequelae. Medicine 1982;61:310-316.<br />
Rathore MH, Friedman AD, Barton LL, Dunkle LM. Herpes zoster oticus. Am J Dis Child<br />
1991;45:722-723.<br />
Robillard RB, Hilsinger RL, Adour KK. Ramsay Hunt facial paralysis: clinical analyses of<br />
185 patients. Otolaryngol Head Neck Surg 1986;95:292-297.<br />
Sartoretti-Schefer S, Wichmann W, Valavanis A. Idiopathic, herpetic, and HIVassociated<br />
facial nerve palsies: abnormal MR enhancement patterns. Am J Neuroradiol<br />
1994;15:479-485.<br />
Schuknecht HF. Pathology of the Ear, 2nd ed. Boston: Harvard University Press; 1993.<br />
pp. 236-237.<br />
http://www.bcm.edu/oto/grand/082197.html (15 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Stafford FW, Welch AR. The use of acyclovir in Ramsay Hunt syndrome. J Laryngol Otol<br />
1986;100:337-340.<br />
Tien R, Dillon WP, Jackler RK. Contrast-enhanced MR imaging of the facial nerve in 11<br />
patients with Bell's palsy. Am J Neuroradiol 1990;11:735-741.<br />
Tschiassny K. The site of facial nerve lesion in cases of Ramsay Hunt’s syndrome. Ann<br />
Otol Rhinol Laryngol 1946;55:152-174.<br />
Uri N, Meyer W, Greenberg E, Kitzes-Cohen R. Herpes zoster oticus: treatment with<br />
Acyclovir. Ann Otol Rhinol Laryngol 1992;101:161-162.<br />
Wayman DM, Pham HN, Byl FM, Adour KK. Audiological manifestations of Ramsay<br />
Hunt syndrome. J Laryngol Otol 1990;104:104-108.<br />
Weller S, Blum MR, Doucette M, Burnette T, Cederberg DM, de Miranda P, et al.<br />
Pharmacokinetics of the acyclovir pro-drug valaciclovir after escalating single- and<br />
multiple-dose administration to normal volunteers. Clin Pharmacol Therap 1993;54:595-<br />
605.<br />
Weller TH.,Coons AH. Fluorescent antibody studies with agents of varicella and herpes<br />
zoster propagated in vitro. Proc Soc Exper Biol 1954;86:789.<br />
Wilson WR. The relationship of herpesvirus family to sudden hearing loss: a prospective<br />
clinical study and literature review. Laryngoscope 1986;96:870-877.<br />
Whitley RJ, Gnann JW Jr. Acyclovir: a decade later. N Engl J Med 1992;327:782-789.<br />
Wood MJ, Johnson RW, McKendrick MW, Taylor J, Mandal BK, Crooks J. A randomized<br />
trial of acyclovir for 7 days or 21 days with and without prednisone for treatment of acute<br />
herpes zoster. N Engl J Med 1994;330:896-900.<br />
Yanagida M, Ushiro K, Yamashita T, Kumazaqa T, Katoh T. Enhanced MRI in patients<br />
with Ramsay Hunt’s Syndrome. Acta Otolaryngol Suppl 1993;500:58-61.<br />
Zajtchuk JT, Matz GJ, Lindsay JR. Temporal bone pathology in herpes oticus. Ann Otol<br />
Rhinol Laryngol 1972;81:331-338.<br />
Zammit-Maempel I, Campbell RSD. Prolonged contrast enhancement of the inner ear<br />
on MRI in Ramsay Hunt syndrome. Br J Radiol 1995;68:334-335<br />
http://www.bcm.edu/oto/grand/082197.html (16 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCM Otolaryngology Home Page<br />
©2001, The Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences,<br />
Baylor College of Medicine<br />
One Baylor Plaza, NA102, Houston, TX 77030 oto@bcm.tmc.edu<br />
URL: http://www.bcm.tmc.edu/oto (Modified: 10/02/01)<br />
http://www.bcm.edu/oto/grand/082197.html (17 of 17) [5.11.2005 10:42:23]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
NEUROTOLOGIC MANIFESTATIONS OF HIV INFECTION<br />
March 24, 1994<br />
Thomas A. Salzer, M.D.<br />
As health care providers we are faced with the prospect of caring for an increasing number of AIDS<br />
patients. The disease is no longer limited to specific populations and nearly everyone is at risk.<br />
Familiarity with the protean manifestations of AIDS is important for early diagnosis and treatment. AIDS<br />
is of particular interest to the Otolaryngologist-Head and Neck surgeon since 40-84% of patients have a<br />
symptom or physical finding in the head and neck region at initial presentation. Early diagnosis is<br />
essential because prompt initiation of treatment significantly diminishes morbidity and improves both<br />
quality and length of life in affected individuals. We will briefly review current statistics relevant to the<br />
AIDS epidemic, discuss the classification of HIV associated diseases and review in detail the<br />
neurotologic manifestations of HIV infection.<br />
http://www.bcm.edu/oto/grand/32494.html (1 of 8) [5.11.2005 10:42:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
The causative agent for AIDS, HIV, is a retrovirus of the subfamily Lentovirinae. The term retrovirus is<br />
used because the virus contains the enzyme reverse trancriptase, with transcribes viral RNA to DNA- the<br />
reverse of other viral genetic transcription. HIV appears to be neurotropic and lymphotrophic and<br />
preferencially attacks T-helper cells, which are central to the function of the human cell-mediated<br />
immune system. Impairment of this system renders the host susceptible to numerous opportunistic<br />
infections from viruses, fungi, and protozoas, many of which are native to the oral cavity, pharynx and<br />
larynx. Aside from infectious consequences, HIV is also associated with malignancy, degenerative<br />
diseases and autoimmune sequelae.<br />
OTOLOGIC-NEUROTOLOGIC MANIFESTATIONS<br />
Otologic complaints are common in AIDS patients and include: hearing loss (62%), otalgia (50%),<br />
otorrhea (31%), vertigo (15%) and tinnitus (15%). It is not known if the neurotologic effects seen in<br />
AIDS is the effect of HIV alone or a combination of the effects of HIV infection coupled with<br />
opportunistic infections and/or possible toxic effects of certain therapeutic agents. The brain may be the<br />
site of tumors such as lymphoma or metastatic Kaposi's sarcoma. The HIV itself may cause aseptic<br />
meningitis, subacute encephalitis and isolated cranial nerve neuropathy. The following case reports<br />
associate HIV infection with otologic diagnoses:<br />
RAMSAY HUNT SYNDROME<br />
Mishell and Applebaum 1990, reported a case of a 29 y/o homosexual male who was HIV+ with Ramsay<br />
Hunt syndrome associated with facial nerve palsy. The patient was treated with intravenous nafcillin and<br />
acyclovir.<br />
HERPES ZOSTER MYRINGITIS<br />
Kohan et al 1988 reported two cases of Herpes zoster myringitis which were successfully treated with<br />
acyclovir.<br />
KAPOSI'S SARCOMA<br />
KS is a slowly progressive, malignant mesenchymal tumor characterized clinically by red-purple plaques<br />
and nodules that may be seen externally or internally. Proliferation of atypical spindle cells within<br />
vascular channels is seen on histopathology. KS has been reported to involve the mastoid (Linstrom<br />
1993) and external ear (Morris 1990).<br />
GRADENIGO'S SYNDROME<br />
Linstrom et al 1993 reported a 28 year old male IVDA with otalgia, purulent otorrhea, and sixth and<br />
seventh cranial nerve palsy secondary to petrous apicitis due to Aspergillus infection<br />
PROGRESSIVE MULTIFOCAL LEUKENCEPHALOPATHY<br />
Langford and Kuntz 1988 presented two adult patients with AIDS who had multiple cranial neuropathies<br />
resulting from progressive multifocal leukencephalopathy. Clinical symptoms included facial paralysis,<br />
trigeminal hypaesthesia, hemianopsia, and deafness. Cranial MRI in both patients showed progressive<br />
PML, an unusual demyelinating disease seen in AIDS patients and thought to result from a direct effect<br />
http://www.bcm.edu/oto/grand/32494.html (2 of 8) [5.11.2005 10:42:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
of HIV in the cerebral white matter.<br />
PNEUMOCYSTIS CARINII OTITIS / MASTOIDITIS<br />
Pseudomonas carinii is the most common opportunistic pathogen infecting persons with HIV infection,<br />
affecting nearly 85% patients at some point of the illness. Otic Pneumocystis typically presents as a<br />
unilateral polypoid mass associated with otalgia, hearing loss and occasionally otorrhea. Pneumocystis<br />
carinii otitis media and mastoiditis have been. Pneumocystis carinii recovered from aural polyps is<br />
occasionally the initial manifestation of HIV infection in patients presenting to otologists for evaluation<br />
of otorrhea, otalgia and hearing loss. Pneumocystis carinii of the external canal has been effectively<br />
treated with local debridement and a 3- week course of Bactrim.<br />
OPPORTUNISTIC INFECTIONS<br />
Toxoplasmosis is the most common opportunistic infection to effect the CNS (Real, 1988). Kohan<br />
reported two such patients which presented with bilateral SNHL. Cryptococcal meningitis is known to be<br />
associated with SNHL in up to 25% cases (Real, 1987). Tuberculous meningitis is not infrequent in<br />
AIDS patients and is known to be associated with hearing loss.<br />
OTOSYPHILIS<br />
Otosyphilis must always be considered and investigated in a patient with fluctuating, asymmetric or<br />
sudden hearing loss. The diagnosis and treatment of syphilitic cochleovestibular dysfunction remains<br />
controversial, however the presumptive diagnosis is made in patients with cochleovestibular dysfunction,<br />
positive serology for syphilis and no other known etiology for the inner ear disturbance.. Smith and<br />
Canalis, 1989 found otosyphilis to develop at an accelerated rate from primary syphilis in AIDS patients.<br />
All cases arose in patients previously treated for primary syphilis (latent syphilis). They propose that the<br />
HIV somehow hastens the development of otosyphilis effectively activating the disease.. Furthermore<br />
they propose that all patients with otosyphilis should have an HIV test.<br />
The index of suspicion should be high in the homosexual population because of the high incidence of<br />
syphilis in this group. 35-55% patients with AIDS have a past history of other sexually transmitted<br />
diseases including syphilis. Otosyphilis is well recognized as a cause of otologic disease in patients with<br />
AIDS (Morris and Prasad, 1990).<br />
Gleich et al identified three factors associated with hearing improvement in patients with otosyphilis<br />
treated with intravenous penicillin and corticosteroids. In there study 31% patients with otosyphilis<br />
experienced hearing improvement, tinnitus decreased in 85% and vertigo improved in 86% . Specific<br />
factors associated with hearing improvement include: hearing loss present less than 5 years, fluctuating<br />
hearing, and age less than 60 years. Improvement was unrelated to the severity of the loss or previous<br />
treatment.<br />
CENTRAL NERVOUS SYSTEM<br />
HIV is frequently accompanied by neurological complications which are observed in 40% to 75% of<br />
patients during the course of the disease. De la Monte discovered CNS involvement in more than 90% of<br />
http://www.bcm.edu/oto/grand/32494.html (3 of 8) [5.11.2005 10:42:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
HIV infected patients at autopsy. Neurological findings are detectable in approximately one third of<br />
AIDS patients. At autopsy however, up to of 75% subjects reveal neuropathological changes related to<br />
HIV infection. The most common neurologic syndrome seen in AIDS patients is subacute encephalitis.<br />
Early stages are characterized by subtle cognitive changes that may progress to dementia in several<br />
weeks or months. The HIV appears to be directly involved in both clinical and pathological changes in<br />
the CNS. Neurotologic workup may reveal central vestibular and auditory dysfunction. ENG findings<br />
show ataxic pursuit and optikinetic nystagmus with total loss of caloric excitability. ABR indicate<br />
absolute and interpeak latencies and synthetic sentence identification test yield reduced scores. At<br />
autopsy the AIDS virus was found in mononuclear and multinuclear giant cells in the cortical and<br />
subcortical gray matter, cerebral and cerebellar white matter and through out the brain stem.<br />
Hausler compared the incidence of peripheral and central auditory and vestibular disorders occurring in<br />
different stages of HIV infection. The results of audiological, vestibular and electrophysiologic tests<br />
performed on symptomatic and asymptomatic HIV-positive homosexual males with age matched<br />
seronegative homosexual males were compared. 57% of symptomatic and 45% off asymptomatic HIV<br />
positive patients had substantial abnormalities in comparison to minor abnormalities detected in 12%<br />
seronegative patients. The results suggested a high incidence of neurotologic disorders in HIV positive<br />
patients and that subclinical involvement of the auditory and vestibular system is common.<br />
The frequency of electrophysiologic abnormalities in asymptomatic patients indicates subclinical<br />
involvement of the Central nervous system.<br />
SENSORINEURAL HEARING LOSS<br />
The incidence of SNHL in patients with HIV ranges from 23 - 49% . Kohan reported seven patients with<br />
persistent SNHL. In three instances the hearing loss could be traced to the use of well-known ototoxic<br />
drugs used in the treatment of AIDS. The remaining four patients were divided among CNS<br />
toxoplasmosis and cryptococcal meningitis, CNS toxoplasmosis alone, tuberculous meningitis and leutic<br />
otitis. For example, acyclovir may cause vertigo, trimethoprim-sulfamethoxazole may cause vertigo and<br />
tinnitus, and azidothymidine may lead to vertigo and hearing loss.<br />
The characteristics of the SNHL in patients with HIV are not uniformly defined. The degree of hearing<br />
loss, range of loss and even incidence appear variable. Hearing loss in the high frequencies is more<br />
commonly reported than in the low frequencies. Delayed latencies of brainstem auditory-evoked<br />
responses have been observed in patients with HIV, suggesting neuropathies of the central auditory and<br />
vestibular region.<br />
Boccellari found an association between immune suppression in HIV patients and neurophysiologic<br />
measures. Asymptomatic subjects without evidence of immune suppression do not appear to be at greater<br />
risk for neurophysiological impairment than HIV-negative subjects. The HIV-positive individuals with<br />
evidence of immunosuppression, however, appear to have an increased likelihood of central conduction<br />
time slowing. In contrast, studies by Pagano suggest that subclinical involvement of the upper brain stem<br />
occurs in HIV infection and that brainstem auditory evoked potential abnormalities could be the direct<br />
http://www.bcm.edu/oto/grand/32494.html (4 of 8) [5.11.2005 10:42:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
result of the HIV effect on central nervous system structures.<br />
Case Presentation<br />
A 35-year-old man with human immunodeficiency virus infection diagnosed seven years ago was<br />
hospitalized for disseminated histoplasmosis which served as his AIDS-defining illness. During that<br />
admission he was also found to have Mycobacterium avium-intracellulare septicemia and bilateral<br />
external otitis secondary to Pseudomonas aeruginosa. CT scan of the temporal bones and gallium scan<br />
failed to reveal bony involvement. The otitis externa was treated with local debridement, culture specific<br />
intravenous antibiotics and otic drops. The patient experienced near total resolution of his symptoms with<br />
decreased otalgia, erythema and edema. Post treatment cultures were negative. Two months later he<br />
presented to the Otolaryngology service for evaluation and treatment of recurrent otitis externa which<br />
had progressed despite oral ciprofloxacin and Cortisporin otic drops. Examination revealed severe<br />
external otitis with erythema, edema and ulceration limited to the concha cavum and a right paranasal<br />
ulcer. The possibility of drug reaction was entertained and initial improvement was seen with withdrawal<br />
of the otic drops, however symptoms worsened thereafter prompting tissue biopsy of the ear and<br />
paranasal region for histology and culture. Histologic evaluation revealed multiple rrport inclusion<br />
bodies consistent with Herpes simplex infection. Audiometric evaluation was normal. The patient's<br />
condition improved dramatically on intravenous acyclovir.<br />
Bibliography<br />
Barzan L, Carbone A, Tirelli U, Crosato IM, Vaccher E, Volpe R, et al. Nasopharyngeal lymphatic tissue in patients<br />
infected with human immunodeficiency virus. A prospective clinicopathologic study. Arch Otolaryngol Head Neck Surg<br />
1990;116:928-931.<br />
Barzan L, Tavio M, Tirelli U, Comoretto R. Head and neck manifestations during HIV infection. J Laryngol Otol<br />
1993;107:133-136.<br />
Birdsall HH, Ozluoglu LN, Lew HL, Trial J, Brown DP, Wofford MJ, et al. Auditory P300 abnormalities and leukocyte<br />
activation in HIV infection. Otolaryngol Head Neck Surg 1994;110:53-59.<br />
Boccellari AA, Dilley JW, Yingling CD, Chambers DB, Tauber MA, Moss AR, et al. Relationship of CD4 counts to<br />
neurophysiological function in HIV-1--infected homosexual men. Arch Neurol 1993;50:517-521.<br />
Breda SD, Hammerschlag PE, Gigliotti F, Schinella R. Pneumocystis carinii in the temporal bone as a primary<br />
manifestation of the acquired immunodeficiency syndrome. Ann Otol Rhinol Laryngol 1988;97:427-431.<br />
http://www.bcm.edu/oto/grand/32494.html (5 of 8) [5.11.2005 10:42:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Chandrasekhar SS, Siverls V, Sekhar HK. Histopathologic and ultrastructural changes in the temporal bones of HIVinfected<br />
human adults. Am J Otol 1992;13:207-214.<br />
Chilla R, Booken G, Rasche H. Bell's palsy as the initial symptom of HIV infection. Laryngol Rhinol Otol 1987;66:629-<br />
630.<br />
Chow JH, Stern JC, Kaul A, Pincus RL, Gromisch DS. Head and neck manifestations of the acquired immunodeficiency<br />
syndrome in children. Ear Nose Throat J 1990;69:416-9, 422-3.<br />
Gleich LL, Linstrom CJ, Kimmelman CP. Otosyphilis: a diagnostic and therapeutic dilemma. Laryngoscope<br />
1992;102:1255-1259.<br />
Hart CW, Cokely CG, Schupbach J, Dal Canto MC, Coppleson LW. Neurotologic findings of a patient with acquired<br />
immune deficiency syndrome. Ear Hear 1989;10:68-76.<br />
Hausler R, Vibert D, Koralnik IJ, Hirschel B. Neuro-otological manifestations in different stages of HIV infection. Acta<br />
Otolaryngol Suppl 1991;481:515-521.<br />
Kohan D, Hammerschlag PE, Holliday RA. Otologic disease in AIDS patients: CT correlation. Laryngoscope<br />
1990;100:1326-1330.<br />
Kohan D, Rothstein SG, Cohen NL. Otologic disease in patients with acquired immunodeficiency syndrome. Ann Otol<br />
Rhinol Laryngol 1988;97:636-640.<br />
Lannigan FJ, Jones NS, von Schoenberg MV. An avoidable occupational hazard during mastoid surgery. J Laryngol Otol<br />
1989;103:566.<br />
Linstrom CJ, Pincus RL, Leavitt EB, Urbina MC. Otologic neurotologic manifestations of HIV-related disease.<br />
Otolaryngol Head Neck Surg 1993;108:680-687.<br />
Lucente FE. Impact of the acquired immunodeficiency syndrome epidemic on the practice of laryngology. Ann Otol<br />
Rhinol Laryngol Suppl 1993;161:1-24.<br />
Mishell JH, Applebaum EL. Ramsay-Hunt syndrome in a patient with HIV infection. Otolaryngol Head Neck Surg<br />
1990;102:177-179.<br />
Morrison GA, Butler P, Booth JB. AIDS to the post nasal space. J Laryngol Otol 1989;103:1091-1092.<br />
Murr AH, Benecke JE,Jr. Association of facial paralysis with HIV positivity. Am J Otol 1991;12:450-451.<br />
Northfelt DW, Clement MJ, Safrin S. Extrapulmonary pneumocystosis: clinical features in human immunodeficiency virus<br />
infection. Medicine 1990;69:392-398.<br />
Pagano MA, Cahn PE, Garau ML, Mangone CA, Figini HA, Yorio AA, et al. Brain-stem auditory evoked potentials in<br />
human immunodeficiency virus-seropositive patients with and without acquired immunodeficiency syndrome. Arch<br />
Neurol 1992;49:166-169.<br />
http://www.bcm.edu/oto/grand/32494.html (6 of 8) [5.11.2005 10:42:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Paller AS, Sahn EE, Garen PD, Dobson RL, Chadwick EG. Pyoderma gangrenosum in pediatric acquired<br />
immunodeficiency syndrome. J Pediatr 1990;117:63-66.<br />
Park S, Wunderlich H, Goldenberg RA, Marshall M. Pneumocystis carinii infection in the middle ear. Arch Otolaryngol<br />
Head Neck Surg 1992;118:269-270.<br />
Rarey KE. Otologic pathophysiology in patients with human immunodeficiency virus. Am J Otolaryngol 1990;11:366-<br />
369.<br />
Real R, Thomas M, Gerwin JM. Sudden hearing loss and acquired immunodeficiency syndrome. Otolaryngol Head Neck<br />
Surg 1987;97:409-412.<br />
Rowe Jones JM, Pringle MB. Prevention of occupational transmission of HIV in the ENT clinic. Ann R Coll Surg Engl<br />
1992;74:5-8.<br />
Sandler ED, Sandler JM, LeBoit PE, Wenig BM, Mortensen N. Pneumocystis carinii otitis media in AIDS: a case report<br />
and review of the literature regarding extrapulmonary pneumocystosis. Otolaryngol Head Neck Surg 1990;103:817-821.<br />
Shapiro AL, Shechtman FG, Guida RA, Kimmelman CP. Head and neck lymphoma in patients with the acquired immune<br />
deficiency syndrome. Otolaryngol Head Neck Surg 1992;106:258-260.<br />
Strauss M, Fine E. Aspergillus otomastoiditis in acquired immunodeficiency syndrome. Am J Otol 1991;12:49-53.<br />
Taylor DN, Wallace JG, Masdeu JC. Perception of different frequencies of cranial transcutaneous electrical nerve<br />
stimulation in normal and HIV-positive individuals. Percept Mot Skills 1992;74:259-264.<br />
Timon CI, Walsh MA. Sudden sensorineural hearing loss as a presentation of HIV infection. J Laryngol Otol<br />
1989;103:1071-1072.<br />
Tosti A, Gaddoni G, Peluso AM, Misciali C, Piraccini BM, Menni B. Acquired hairy pinnae in a patient infected with the<br />
human immunodeficiency virus. J Am Acad Dermatol 1993;28:513.<br />
Wasserman L, Haghighi P. Otic and ophthalmic pneumocystosis in acquired immunodeficiency syndrome. Report of a<br />
case and review of the literature. Arch Pathol Lab Med 1992;116:500-503.<br />
Welkoborsky HJ, Lowitzsch K. Auditory brain stem responses in patients with human immunotropic virus infection of<br />
different stages. Ear Hear 1992;13:55-57.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/32494.html (7 of 8) [5.11.2005 10:42:33]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/32494.html (8 of 8) [5.11.2005 10:42:33]
http://www.bcm.edu/oto/grand/31893.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
INFECTIOUS INTRACRANIAL COMPLICATIONS OF SUPPURATIVE<br />
EAR DISEASE<br />
Andrew L. de Jong, MD<br />
March 18, 1993<br />
The existence and treatment of the intracranial complications of suppurative ear disease can be traced to<br />
the European Neolithic period. It is well-known that prehistoric man performed trephining, or the<br />
surgical opening of the skull with primitive instruments, for such infections. Until the 1940s the outlook<br />
for these patients remained grim, with a mortality of 75%. However, the introduction of penicillin by<br />
Fleming drastically changed this, decreasing mortality to 10%.<br />
There are four well-known infectious otitic intracranial complications:<br />
http://www.bcm.edu/oto/grand/31893.html (1 of 5) [5.11.2005 10:42:38]
http://www.bcm.edu/oto/grand/31893.html<br />
1. Epidural abscess<br />
2. Subdural abscess<br />
3. Meningitis<br />
4. Brain abscess<br />
The signs and symptoms of these complications can often be difficult to detect initially. Impending<br />
complications should be suspected when: 1) otologic infection recurs two to three weeks after initial<br />
treatment; 2) fetid aural discharge is present; 3) headache or subtle mental status changes in the presence<br />
of otologic disease; and 4) otalgia in the setting of chronic ear disease. These warning signs should<br />
prompt further investigation.<br />
The most useful initial study is computerized tomography (CT) with contrast. If the CD findings are<br />
equivocal and the index of suspicion remians high, this should be followed by magnetic resonance<br />
imaging (MRI) with and without contrast. Therapy is tailored to each specific complication but should<br />
include intravenous antibiotics, medical management of elevated cerebrospinal fluid pressure, and<br />
neurosurgical consultation. Once the patient is neurologically stable, attention should be focused on<br />
definitive otologic intervention.<br />
The pathogenesis, microbiology, and treatment of each otitic intracranial complication were discussed in<br />
detail.<br />
Case Presentation<br />
A 20-year-old white woman with an extensive otologic history including left mastoidectomy in 1984<br />
with revision in 1991, presented to another hospital with a five-day history of right-sided fetid aural<br />
discharge, otalgia, headache, and fever. She had been placed on oral antibiotics three days earlier by a<br />
private physician. On admission she was noted to be lethargic with neck rigidity, vomiting, and<br />
photophobia. Her aural exam was significant for the discharge and a posterior, superior deep retraction<br />
pocket. CT scanning revealed right mastoiditis and probable posterior fossa bony erosion. A lumbar<br />
puncture was consistent with meningitis, with the CSF fluid growing staphylococcus, proteus, and<br />
pseudomonas species.<br />
The patient was transferred to BTGH on broad spectrum antibiotics. A right modified radical<br />
mastoidectomy with removal of a cholesteatoma was performed. A bony defect was found over the<br />
lateral sinus, but the sinus was patent. Postoperatively, DM had persistent headaches and neck pain. She<br />
developed somnolence, ataxia, and dysdiadochokinesia. CT and MRI imaging showed an infratentorial<br />
subdural empyema. A suboccipital craniotomy was performed by the neurosurgical team with removal of<br />
a sterile empyema. DM then made steady progress with only mild residual ataxia.<br />
http://www.bcm.edu/oto/grand/31893.html (2 of 5) [5.11.2005 10:42:38]
http://www.bcm.edu/oto/grand/31893.html<br />
Bibliography<br />
Alford BR, Cohn AM. Complications of suppurative otitis media and mastoiditis. In: Paparella MM, Shumrick DA,<br />
editors. Otolaryngology, Volume II. Philadelphia: WB Saunders, 1980;1490-1509.<br />
Alford BR, Pratt FE. Intracranial complications from otitis media. Tex Med 1966;62:66-70.<br />
Chole RA. Osteoclasts in chronic otitis media, cholesteatoma, and otosclerosis. Ann Otol Rhinol Laryngol 1988;97:661-<br />
666.<br />
Friedman EM, McGill TJ, Healy GB. Central nervous system complications associated with acute otitis media in children.<br />
Laryngoscope 1990;100:149-151.<br />
Froeschner EH. Two examples of ancient skull surgery. J Neurosurg 1992;76:559-562.<br />
Glasscock ME, Shambaugh GE. Surgery of the Ear, 4th edition. Philadelphia: WB Saunders, 1990:249-275.<br />
Gower D, McGuirt WF. Intracranial complications of acute and chronic infectious ear disease: a problem still with us.<br />
Laryngoscope 1983;93:1028-1033.<br />
Grossman RG, editor. Principles of Neurosurgery. NY: Raven Press, 1991:179-190.<br />
Holt GR, Gates GA. Masked mastoiditis. Laryngoscope 1983;93:1034-1037.<br />
Hoyt DJ, Fisher SR. Otolaryngolgic management of patients with subdural empyema. Laryngoscope 1991;101:20-24.<br />
Jahn AF. Chronic otitis media; diagnosis and treatment. Med Clin North Am 1991;75:1277-1291.<br />
Keet PC. Cranial intradural abscess management of 641 patients during the 35 years from 1952 to 1986. Br J Neurosurg<br />
1990;4:273-278.<br />
Koltai PJ, Eames FA, Parnes SM, Wood GW, Bie B. Comparison of computed tomography and magnetic resonance<br />
imaging in chronic otitis media with cholesteatoma. Arch Otolaryngol Head Neck Surg 1989;115:1231-1233.<br />
Kurihara A, Toshima M, Yuasa R, Takasaka T. Bone destruction mechanisms in chronic otitis media with cholesteatoma:<br />
specific production by cholesteatoma tissue in culture of bone-resorbing activity attributable to interleukin-1 alpha. Ann<br />
Otol Rhinol Laryngol 1991;100:989-998.<br />
Martin-Hirsch DP, Habashi S, Page R, Hinton AE. Latent mastoiditis: no room for complacency. J Laryngol Otol<br />
1991;105:767-768.<br />
Mathews TJ, Marus G. Otogenic intradural complications: a review of 37 patients. J Laryngol Otol 1988;102:121-124.<br />
McLaurin RL, editor. Pediatric Neurosurgery, 2nd edition. Philadelphia: WB Saunders, 1989:479-489.<br />
http://www.bcm.edu/oto/grand/31893.html (3 of 5) [5.11.2005 10:42:38]
http://www.bcm.edu/oto/grand/31893.html<br />
Munz M, Farmer JP, Auger L, O'Gorman AM, Schloss MD. Otitis media and CNS complications. J Otolaryngol<br />
1992;21:224-246.<br />
Murthy PS, Sukumar R, Hazarika P, Rao AD, Raja M, Raja A. Otogenic brain abscess in childhood. Int J Pediatr<br />
Otorhinolaryngol 1991;22:9-17.<br />
Nalbone VP, Kuruvilla A, Gacek RR. Otogenic brain abscess; the Syracuse experience. Ear Nose Throat J 1992;71:238-<br />
242.<br />
Neely JG. Complications of Suppurative Otitis Media. Part 2: Intracranial Complications.<br />
Washington D.C.: AAO-HNS, 1979.<br />
Neely JG. Complications of temporal bone infection. In: Cummings CW, Harker LA, editors. Otolaryngology - Head and<br />
Neck Surgery, Volume 4, 2nd edition. St. Louis: Mosby, 1992:2840-2864.<br />
Nunez DA, Browning GG. Risks of developing an otogenic intracranial abscess. J Laryngol Otol 1990; 104:468-472.<br />
Ponka A, Ojala K, Teppo AM, Weber TH. The differential diagnosis of bacterial and aseptic meningitis using<br />
cerebrospinal fluid laboratory tests. Infection 1983;11:129-131.<br />
Rupa V, Raman R. Chronic suppurative otitis media: complicated versus uncomplicated disease. Acta Otolaryngol<br />
1991;111:530-535.<br />
Schmidek HH, editor. Operative Neurosurgical Techniques: Indications, Methods, and Results, 2nd edition. Philadelphia:<br />
WB Saunders, 1988:490-495.<br />
Schwaber MK, Pensak ML, Bartels LJ. The early signs and symptoms of neurotologic complications of chronic<br />
suppurative otitis media. Laryngoscope 1989;99:373-375.<br />
Stevensen RS, Guthrie D. A History of Oto-Laryngology. Edinburgh: Livingstone, 1949;112-118.<br />
Wackym PA, Canalis RF, Feuerman T. Subdural empyema of otorhinological origin. J Laryngol Otol 1990;104:118-122.<br />
Weingarten K, Zimmerman RD, Becker RD, Heier LA, Haines AB, Beck MD. Subdural and epidural empyemas: MR<br />
imaging. AJR Am J Roentgen 1989;152:615-621.<br />
Yaniv E, Pocock R. Complications of ear disease. Clin Otolaryngol 1988;13:357-361.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
http://www.bcm.edu/oto/grand/31893.html (4 of 5) [5.11.2005 10:42:38]
http://www.bcm.edu/oto/grand/31893.html<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/31893.html (5 of 5) [5.11.2005 10:42:38]
http://www.bcm.edu/oto/grand/5792.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
LATERAL SINUS THROMBOSIS<br />
Judith J. Owens, MD<br />
May 7, 1992<br />
Although seldom encountered in the practice of modern otology, lateral sinus thrombosis (LST) and<br />
other intracranial complications of otitis media still occur. The classic picture of this disease is often<br />
modified by prior antibiotic treatment, making the diagnosis and management difficult.<br />
Infective thrombosis of the lateral sinus was first described in 1826 by Hooper. This disease was<br />
universally fatal until surgical intervention was established in 1888 by Lane. Despite later advances in<br />
surgical techniques mortality remained at nearly 50% until the introduction of antibiotics. Prior to the<br />
advent of antibiotic therapy, the mortality of all intracranial complications was extraordinarily high. In a<br />
study of autopsy statistics at LA County Hospital, it was found that before the introduction of antibiotics<br />
approximately 25:1,000 deaths were due to an intracranial complication of otitis media. The death rate<br />
http://www.bcm.edu/oto/grand/5792.html (1 of 6) [5.11.2005 10:42:45]
http://www.bcm.edu/oto/grand/5792.html<br />
from these complications dropped 90% after the introduction of antibiotics.<br />
The intracranial complications of otitis media include purulent meningitis, extradural or peridural<br />
abscess, LST, brain abscess and otitic hydrocephalus. Respiratory mucosa, intact boney walls and<br />
protective granulations provide natural defense barriers within the middle ear; complications occur when<br />
these are overcome. The spread of infection through the natural defenses can occur by osteothrombosis,<br />
bone erosion and when present along preformed pathways.<br />
Classic symptoms of LST include a "picket fence" fever pattern; chills; progressive anemia (especially<br />
with beta-hemolytic strep); and, symptoms of septic emboli, headache and papilledema may indicate<br />
extension to involve the cavernous sinus. The Toby-Ayer test is measured by monitoring the CSF<br />
pressure during a lumbar puncture. No increase in CSF pressure during external compression of the<br />
internal jugular vein on the affected side, and an exaggerated response on the patent side, is suggestive of<br />
LST.<br />
Since the introduction of antibiotics, some authors have noted that a high percentage of cases are due to<br />
chronic rather than acute cases of otitis media; however this finding has not been consistent in all reports.<br />
Teenagers and young adults are more commonly affected in modern reports whereas younger children<br />
were reported in higher numbers in earlier series. In the pre-antibiotic era streptococcus and<br />
staphylococcus were reported as causing the majority of cases of LST, recent reports have included<br />
anaerobic and gram negative organisms as well.<br />
The diagnostic procedure of choice is MRI with MR angiography. The thrombus can be identified by its<br />
signal intensity on MRI and the flow void in the affected sinus is clearly documented on MR<br />
angiography.<br />
Treatment is always surgical removal of the infected thrombosis in addition to broad spectrum antibiotic<br />
coverage. Once a highly controversial issue, ligation of the internal jugular vein is seldom necessary. In<br />
the majority of recent cases, anticoagulation has not been found to be necessary. However, it has been<br />
advocated by Shambaugh and may be indicated in selected cases.<br />
Case Presentation<br />
A 6-year-old Hispanic male presentedwith no prior history of systemic illness or otologic disease. He<br />
was seen at Ben Taub General Hospital with a five day history of upper respiratory infection, headache,<br />
and bilateral otorrhea. Two days earlier swelling and tenderness had developed along the left<br />
sternocleidomastoid muscle. On arrival, his temperature was 101°F and white blood cell count was<br />
18,300; he was alert and appropriate, but irritable and uncooperative. A CT scan was obtained that<br />
showed bilateral opacification of the mastoid air cells, and an abscess in the left upper neck. That night<br />
he was taken to the OR for incision and drainage of the neck abscess and complete otologic examination.<br />
http://www.bcm.edu/oto/grand/5792.html (2 of 6) [5.11.2005 10:42:45]
http://www.bcm.edu/oto/grand/5792.html<br />
There was marked swelling of the left external auditory canal which precluded visualization of the left<br />
tympanic membrane. The right external auditory canal was also swollen, but the tympanic membrane<br />
could be visualized. The tympanic membrane was found to be thickened, a myringotomy was performed,<br />
purulent fluid was aspirated from the middle ear cleft and a ventilating tube was left in place. He was<br />
initially treated with Ceftriaxone (Rocephin) and Cortisporin otic drops. Cultures obtained from the right<br />
tympanic aspiration and the left neck abscess grew Streptococcus pneumonia and a Pseudomonas grew<br />
from the left external canal specimen. Antibiotic therapy was changed to ticarcillin and clavulanate<br />
(Timentin). However, despite this, he continued to spike fevers to 101 and 102° F. On April 2, 1992 a<br />
second CT scan with thin cuts through the temporal bones was then obtained. This study suggested<br />
thrombosis of the left lateral sinus. While arrangements were being made for surgical decompression, an<br />
MR angiogram was performed. This confirmed vascular flow through the right sigmoid sinus and jugular<br />
vein, but no flow through the left lateral sinus or jugular vein. A few hours later, he underwent a left<br />
complete mastoidectomy with incision of the lateral sinus and removal of an obstructing thrombus.<br />
Postoperatively, his antibiotics were changed to Ceftazidime (Fortaz), Amikacin and Penicillin G.<br />
Anticoagulation therapy was instituted for two weeks following surgical decompression. Subsequent<br />
MRA studies showed the development of collateral flow around the left sigmoid sinus and internal<br />
jugular vein. Additionally, reduced flow in the right system persisted. On April 21, 1992, he underwent<br />
right mastoidectomy. An MRA obtained on April 30, 1992 demonstrated unobstructed flow through the<br />
right venous system and no evidence of recanalization through the left sigmoid sinus or jugular vein.<br />
Bibliography<br />
Albert DM, Williams SR. Clinical and anatomical considerations of the TobeyAyer test in lateral sinus thrombosis. J<br />
Laryngol Otol 1986;100:13111313.<br />
Alford BR, Pratt FE. Intracranial complications for otitis media. Texas Med 1966;62:66-70.<br />
Amirmajdi NM. Sigmoid sinus involvement in middleear infection. Laryngoscope 1988;98:310-312.<br />
Coates GM, Ersner MS, Persky AH. Lateral sinus thrombosis with a review of the literature. Ann Otol Rhinol Laryngol<br />
1934;43:419-440.<br />
Cody CC. Thrombosis of the lateral sinus. Arch Otolaryngol 1939;29:674-680.<br />
Courville CB. Intracranial complications of otitis media and mastoiditis in the antibiotic ear. I. Modification of the<br />
pathology of otitic intracranial lesions by antibiotic preparations. Laryngoscope 1955;65:31-46.<br />
Einhaupl KM, Villringer A, Meister W, Mehraein S, Garner C, Pellkofer M, et al. Heparin treatment in sinus venous<br />
thrombosis. Lancet 1991;338:597-600.<br />
http://www.bcm.edu/oto/grand/5792.html (3 of 6) [5.11.2005 10:42:45]
http://www.bcm.edu/oto/grand/5792.html<br />
Erbguth F, Brenner P, Schuierer G, Druschky KF, Neundorfer B. Diagnosis and treatment of deep cerebral vein<br />
thrombosis. Neurosurg Rev 1991;14:145-148.<br />
Goldenberg RA. Lateral sinus thrombosis: medical or surgical treatment? Arch Otolaryngol 1985;111:5658.<br />
Gower D, McGuirt WF. Intracranial complications of acute and chronic infectious ear disease: a problem still with us.<br />
Laryngoscope 1983;93:1028-1033.<br />
Habib RG, Girgis NI, Abu El Ella AH, Farid Z, Woody J. The treatment of outcome of intracranial infections of otogenic<br />
origin. J Trop Med Hyg 1988;91:83-86.<br />
Hawkins DB. Lateral sinus thrombosis: a sometimes unexpected diagnosis. Laryngoscope 1985;95:674-677.<br />
Holmes FA, Obbens EAMT, Griffin E, Lee YY. Cerebral venous sinus thrombosis in a patient receiving adjuvant<br />
chemotherapy for stage II breast cancer through an implanted central venous catheter. Am J Clin Oncol 1987;10:362-366.<br />
Holt GR, Gates GA. Masked mastoiditis. Laryngoscope 1983;93:1034-1038.<br />
Irving RM, Jones NS, HallCraggs MA, Kendall B. View from within: radiology in focus. CT and MR imaging in lateral<br />
sinus thrombosis. J Laryngol Otol 1991;105:693-695.<br />
Jackson CG, Dickens JRE. Lateral sinus thrombosis. Am J Otolaryngol 1979;1:4951.<br />
Jahrsdoerfer RA, FitzHugh GS. Lateral sinus thrombosis. South Med J 1968;61:1271-1275.<br />
Jensen AM. Sinus thrombosis and otogene sepsis. Acta Otolaryngol 1962;55:237-244.<br />
Kelly KE, Jackler RK. Diagnosis of septic sigmoid sinus thrombosis with magnetic resonance imaging. Otolaryngol Head<br />
Neck Surg 1991;106:617-624.<br />
Kopetzky SJ. Acute and chronic otitis media, sinus thrombosis and suppuration of the petrous pyramid. Arch Otolaryngol<br />
1936;24:505-526.<br />
Kraus M, Tovi F. CNS complications of ear, nose and throat infections: an analysis of 50 consecutive cases. J Otolaryngol<br />
1991;20:329-335.<br />
Lane WA. Five cases of complicated disease of the middle ear. Tr Clin Soc London 1889;22:255-265.<br />
Lund WS. A review of 50 cases of intracranial complications from otogenic infection between 1961 and 1977. Clin<br />
Otolaryngol 1978;3:495-501.<br />
Mas JL, Meder JF, Meary E, Bousser MG. Magnetic resonance imaging in lateral sinus hypoplasia and thrombosis. Stroke<br />
1990;21:1350-1356.<br />
Mathews TJ. Lateral sinus pathology (22 cases managed at Groote Schuur Hospital). J Laryngol Otol 1988;102:118-120.<br />
http://www.bcm.edu/oto/grand/5792.html (4 of 6) [5.11.2005 10:42:45]
http://www.bcm.edu/oto/grand/5792.html<br />
Meltzer PE. Treatment of thrombosis of the lateral sinus: a summary of the results obtained during twelve years at the<br />
Massachusetts Eye and Ear Infirmary. Arch Otolaryngol 1935;22:131-142.<br />
O'Connell JE. Lateral sinus thrombosis: a problem still with us. J Laryngol Otol 1990;104:949-951.<br />
Pennybacker J, Dixon SW, Fulton CJ. Discussion on intracranial complications of otogenic origin. Proc Roy Soc Med<br />
1961;54:309-320.<br />
Persson L, Lilja A. Extensive dural sinus thrombosis treatment by surgical removal and local streptokinase infusion.<br />
Neurosurgery 1990;26:117-121.<br />
Proctor CA. Intracranial complications of otitic origin. Laryngoscope 1966;76:288-308.<br />
Purvin V, Dunn DW, Edwards M. MRI and cerebral venous thrombosis. Comput Radiol 1987;11:7579.<br />
Samuel J, Fernandes CMC. Lateral sinus thrombosis (A review of 45 cases). J Laryngol Otol 1987;101:1227-1229.<br />
Scott JA, Pascuzzi RM, Hall PV, Becker GJ. Treatment of dural sinus thrombosis with local urokinase infusion : case<br />
report. J Neurosurg 1988;68:284-287.<br />
Seid AB, Sellars SL. Management of otogenic lateral sinus disease at Groote Schuur Hospital. Laryngoscope 1973;83:397-<br />
403.<br />
Shambaugh GE, Glasscock ME. Surgery of the ear. 3rd ed. Philadelphia:W.B. Saunders, 1980:288-315.<br />
Sneed WF. Lateral sinus thrombosis. Am J Otol 1983;4:258-262.<br />
Teichgraeber JF, PerLee JH, Turner JS. Lateral sinus thrombosis: a modern perspective. Laryngoscope 1982;92:744-751.<br />
Tovi F, Hirsch M, Gatot A. Superior vena cava syndrome: presenting symptom of silent otitis media. J Laryngol Otol<br />
1988;102:623-625.<br />
Tveteras K, Dristensen S, Dommerby H. Septic cavernous and lateral sinus thrombosis: modern diagnostic and therapeutic<br />
principles. J Laryngol Otol 1988;102:877-882.<br />
Vidalihet M, Piette JC, Wechsler B, Bousser MG, Brunet P. Cerebral venous thrombosis in systemic lupus erythematosus.<br />
Stroke 1990;21:1226-1231.<br />
Whitaker CW. Intracranial complications of ear, nose, and throat infections. Laryngoscope 1971;81:1375-1380.<br />
Woflowitz BL. Otogenic intracranial complications. Arch Otolaryngol 1972;96:220-222.<br />
Wright JLW, Grimaldi PMGB. Otogenic intracranial complications. J Laryngol Otol 1973;87:1085-1096.<br />
http://www.bcm.edu/oto/grand/5792.html (5 of 6) [5.11.2005 10:42:45]
http://www.bcm.edu/oto/grand/5792.html<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/5792.html (6 of 6) [5.11.2005 10:42:45]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
ACUTE MASTOIDITIS<br />
February 3, 1994<br />
Jennifer L. Parker, M.D.<br />
Acute mastoiditis is rarely seen today. Prior to the discovery of antibiotics, acute mastoiditis was the<br />
most common complication of acute otitis media and often resulted in death. The incidence has dropped<br />
significantly with the advent of antibiotics. Likewise, the frequency of mastoidectomy for this condition<br />
has decreased ten fold, down from 20% in 1938 to 2.8% in 1948 with a 90% decrease in mortality rate.<br />
Acute mastoiditis is a natural extension of acute otitis media. At the onset of infection, acute<br />
inflammation of the middle ear also involves inflammation of the mastoid air cells, which is not<br />
associated with bony resorption and must be differentiated from clinically significant mastoiditis.<br />
Temporal bone development is integral in the ability to develop this disease. The degree of<br />
pneumatization varies greatly in temporal bones. Infection, heredity, ventilation, environment, and<br />
http://www.bcm.edu/oto/grand/2394.html (1 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
nutrition all play a role in the pneumatization process. Inflammation that develops is easily passed<br />
through these contiguous pneumatized regions. Not only can inflammation spread to these pneumatized<br />
regions, but it can spread to adjacent areas.<br />
The evolution of acute mastoiditis begins when the mucosal lining of the pneumatized cells become<br />
inflamed and produce an exudate. Serosanguinous fluid eventually becomes mucopurulent. Spontaneous<br />
perforation of the tympanic membrane or myringotomy would halt the process at this point. However, 1-<br />
5% of these cases go on to the next phase. The cellular walls of the pneumatized cells then become<br />
demineralized due to: increased osteoclastic activity, pressure of the purulent exudate on the thin bony<br />
septae, and ischemia of the septae secondary to reduced blood flow. As the bony septae breakdown small<br />
abscess cavities form leading to coalescence. Finally the coalescent cells form an empyema, or pus under<br />
pressure, which then escapes to surrounding areas. Treatment of acute mastoiditis depends on the<br />
pathologic stage at which it is encountered.<br />
The bacteriology of acute mastoiditis surprisingly differs from that of acute otitis media. The causative<br />
organism in acute otitis media are usually S Pneumo or H Flu. However, acute mastoiditis is more<br />
commonly due to Group A Beta-Hemolytic Strep and S Pneumo with rare involvement by H. Flu.<br />
Subacute and chronic disease is usually attributed to S. Aureus and gram negative rods such as E. Coli,<br />
Proteus and Pseudomonas.<br />
The signs and symptoms of acute mastoiditis mimic severe acute suppurative otitis media; the disease<br />
entities are distinguished by the duration of symptoms. When the symptoms persist or recur after several<br />
weeks of acute otitis media, they point toward development of a coalescent process within the mastoid.<br />
The most common symptoms are otorrhea and otalgia. Subperiosteal abscess is noted by a fluctuant mass<br />
with overlying edema and erythema. This process produces displacement of the ear downward, outward,<br />
and forward. Sagging of the posterosuperior meatal wall occurs secondary to thickening of the<br />
periosteum overlying the bone in the area of the antrum. The tympanic membrane can simply appear<br />
normal, thickened or can demonstrate a small central perforation. Neurologic changes may be seen with<br />
intracranial complications. Perforation of the mastoid tip along the medial aspect of the SCM through the<br />
incisura mastoidea produces a deep abscess in the neck known as a Bezold's abscess.<br />
Acute mastoiditis is one of the 10 basic complications of acute otitis media. Some worth noting are listed<br />
here. Petrositis is indicated by Gradenigo triad -- acute or subacute otitis media, retro-orbital pain and<br />
abducens palsy. Labyrinthitis due to suppurative ear disease is potentially fatal with spread to the<br />
cerebrospinal fluid producing meningitis. Presence of an extradural abscess is best evaluated by CT scan<br />
but must be excluded intraoperatively by visualizing normal dura through thin intact bone. Sigmoid sinus<br />
thrombosis may be asymptomatic or associated with toxemia or septic emboli. Griesinger's sign may be<br />
encountered and is noted by the presence of edema erythema of the posterior aspect of the mastoid<br />
process associated with mastoid emissary vein thrombosis. The Tobey - Ayer or Queckenstedt test is<br />
usually of historic significance and shows a rise in CSF pressure with occlusion of the normal IJ and NO<br />
change in CSF pressure with occlusion of the thrombosed vein. Brain abscess formation begins with<br />
cerebritis and should be closely monitored if suspected with CT scan every 1-2 weeks.<br />
http://www.bcm.edu/oto/grand/2394.html (2 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Evaluation of the patient with acute mastoiditis begins with the history and physical examination. The<br />
majority of the diagnosis is based on clinical judgment. Laboratory evaluation reveals a leukocytosis and<br />
elevated erythrocyte sedimentation rate. Mastoid radiographs are characteristic and will show cloudiness<br />
of the mastoid air cells associated with fuzziness of the bony partitions. Although helpful in the<br />
diagnosis, most agree that mastoid x-rays are not helpful in determining whether mastoid surgery is<br />
necessary. CT scan of the temporal bones is helpful in evaluation of concomitant intracranial<br />
complications as well as discerning any anatomical variations preoperatively. Chest x-ray is useful to rule<br />
out infiltrates in patients with septicemia and possible embolic phenomena secondary to lateral sinus<br />
thrombosis. Tympanocentesis is performed for guidance of antibiotic therapy.<br />
Acute mastoiditis may be associated with periostitis, osteitis, or may be masked. This differentiation is<br />
key in the management of the patient. Acute mastoiditis with periostitis can be described as infection in<br />
the mastoid air cells which spreads to cause inflammation of the overlying periosteum. The route of<br />
infection may be through direct spread through a defect in the mastoid cortex or more commonly through<br />
venous channels, a.k.a. mastoid emissary veins. Periostitis should not be confused with subperiosteal<br />
abscess which requires surgical intervention.<br />
Acute mastoiditis with osteitis is also known as coalescent mastoiditis. Less than 15% of patients with<br />
periostitis will progress to coalescence. This coalescence may spread in several directions. The spread of<br />
the pus anteriorly to the middle ear via the aditus ad antrum producing spontaneous resolution. If the pus<br />
spreads to the soft tissues lying anteromedially a Bezold's abscess may form. The infection may also<br />
spread lateral to produce a subperiosteal abscess. The spread of pus medially to the petrous air cells<br />
causes petrositis. Posterior spread to the occipital bone may result in osteomyelitis of the calvarium a.k.a.<br />
Citelli abscess.<br />
Masked mastoiditis has an insidious course, owing to the use of broad spectrum antibiotics to treat<br />
middle ear disease. The apparent resolution of symptoms of acute otitis media "masks" the development<br />
of mastoiditis and leads to the presentation with intracranial complications. The presence of pathology<br />
may only be apparent on careful neurologic examination. Diagnosis is usually made on CT of the<br />
temporal bones which demonstrates temporal bone pathology in conjunction with the accompanying<br />
intracranial complication.<br />
Acute mastoiditis can also occur in conjunction with chronic ear disease. It has been the teaching in the<br />
past that acute mastoiditis only occurred in well pneumatized mastoids in which the thin bony trabeculae<br />
are easily broken down. Chronic ear disease has long been associated with a sclerotic "cue - ball" like<br />
mastoid which is less susceptible to demineralization. However, several studies note the presence of<br />
cholesteatoma in patients with acute mastoiditis.<br />
Antibiotic therapy is guided by the patients history. If the history is otherwise uncomplicated by ear<br />
disease or protracted episode of otitis media, the infecting organism is probably S. pneumo or S.<br />
pyogenes which is best treated by ampicillin. If the patient has a protracted course of otitis media then<br />
coverage for S. Aureus and gram negative organisms is necessary with a penicillinase resistant penicillin<br />
http://www.bcm.edu/oto/grand/2394.html (3 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
and an aminoglycoside or single antibiotic coverage with a cephalosporin. Anaerobic coverage should be<br />
added to the above therapy when suspected.<br />
There exists controversy over the management of this disease. All studies on acute mastoiditis are<br />
retrospective and conclusions drawn regarding therapy are limited. There have been no prospective or<br />
controlled studies on the surgical and medical management of the disease. This is limited by the relative<br />
rarity of the disease in the current day. Options for treatment are antibiotics alone, antibiotics plus<br />
myringotomy, Incision and drainage of abscess, and mastoidectomy. If periostitis is present<br />
tympanocentesis followed by myringotomy should be performed with placement on intravenous<br />
antibiotics directed toward gram stain results. It is preferable to insert pressure equalization tubes for<br />
drainage over a longer period of time. This periosteal involvement usually resolves within 24 to 48 hours<br />
after initiation of therapy. If clinical deterioration occurs, manifest by persistent fever and otalgia, or<br />
development of subperiosteal abscess, then further surgical intervention is indicated. Analysis of the<br />
literature reveals approximately 57% of cases are able to be treated in this manner.<br />
Indications for surgery include acute mastoiditis with subperiosteal abscess, acute mastoiditis not<br />
responsive after 24 to 48 hours of intravenous antibiotics and myringotomy, and intracranial<br />
complications with evidence of mastoid coalescence. These indications were derived from the current<br />
literature.<br />
Some have managed the disease with simple I & D of the abscess which does not afford decompression<br />
and drainage of the underlying mastoid. There have been no studies to evaluate the efficacy of this mode<br />
of therapy versus mastoidectomy. Most reported cases of simple I & D have been anecdotal. 60% of the<br />
cases reported in the literature have come to mastoidectomy after I & D.<br />
The procedure of choice is a complete simple mastoidectomy. Simple mastoidectomy is an emergency<br />
procedure and should be performed on a clinically stable patient with control of sepsis before undergoing<br />
anesthesia. Mastoidectomy may be performed at a later date if the patient is unstable after drainage of<br />
intracranial process. The goal of surgery is to effect drainage. Establishment of good communication<br />
between the middle ear and mastoid is achieved by removing the edema and granulation in the aditus ad<br />
antrum. External drainage is necessary with a drain in the mastoid cavity to drain the antrum, and a<br />
pressure equalization tube inserted to ventilate the middle ear space.<br />
In conclusion, acute mastoiditis is a diagnosis based on clinical acumen. When acute mastoiditis is<br />
suspected a careful history and physical examination should be ascertained to evaluate for intratemporal<br />
or intracranial complications. The presence of acute mastoiditis does not exclude the presence of<br />
underlying chronic ear disease, and should be taken into account in the evaluation and treatment of the<br />
patient. The presence of subperiosteal abscess or progression of symptoms on the above therapy warrants<br />
surgical intervention. Simple mastoidectomy is the surgery of choice. Prospective controlled studies are<br />
necessary to firmly identify indications for medical versus surgical therapy.<br />
http://www.bcm.edu/oto/grand/2394.html (4 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Case Presentation<br />
An 11-year-old boy with a history of chronic otitis media with effusion presented with a 10-day history<br />
of fever, right otalgia, and a right, dull occipital headache. The headache was not associated with<br />
photophobia. A CT scan of the head revealed a right parieto-occipital epidural abscess.. Physical<br />
examination revealed a young, alert boy with a temperature of 102øF. Examination of his right ear<br />
revealed a thickened, but intact tympanic membrane and middle ear effusion. Postauricular edema,<br />
erythema, tenderness, and fluctuance was evident. The remainder of the physical examination, including<br />
a neurological exam, was normal. White blood cell count was 18.7 cells/mm3 with a left shift. CT scan<br />
of the temporal bones revealed soft tissue changes within the middle ear and mastoid and an overlying<br />
subperiosteal abscess and possible lateral sinus thrombosis.<br />
The patient was taken to the operating room and underwent bur hole drainage and irrigation of a right<br />
parieto-occipital epidural abscess by the neurosurgical team followed by a right simple mastoidectomy,<br />
exploration of the lateral sinus, insertion of a pressure equalization tube, and Penrose drainage of the<br />
mastoid cavity. Findings included coalescent mastoiditis and no evidence of lateral sinus thrombus.<br />
Intraoperative cultures grew microaerophilic streptococcus; the antibiotic regimen was changed to<br />
Cefotaxime and Penicillin G. The right temporoparietal cerebritis showed no progression to brain abscess<br />
and no neurologic sequelae. Drains were discontinued when drainage decreased. The patient was<br />
discharged on the thirteenth postoperative day in good condition to continue intravenous antibiotics for a<br />
total course of 6 weeks. Weekly CT scan of the head demonstrated slow resolve of the cerebritis. The<br />
patient has had no further episodes of otitis media and is currently doing well in the sixth grade.<br />
Bibliography<br />
Alford BR, Pratt FE. Intracranial complications from otitis media. Texas Med 1966;62:66-70.<br />
Allam AF. Pneumatization of the temporal bone. Ann Otol Rhinol Laryngol 1969;78:49-64.<br />
Allam AF, Schuknecht HF. Pathology of petrositis. Laryngoscope 1968;78:1813-1832.<br />
Arcand P, Cerat J, Spenard JR. Acute otomastoiditis in the leukemic child. J Otolaryngol 1989;18:380-383.<br />
Bluestone CD, Klein JO. Otitis Media in Infants and Children. Philadelphia: WB Saunders, 1988.<br />
Davison FW. Otitis media - then and now. Laryngoscope 1955;65:142-151.<br />
Dolowitz DA, Wakefield RH. A case of mastoiditis without apparent otitis media. Ann Otol Rhinol Laryngol 1949;58:512-<br />
516.<br />
http://www.bcm.edu/oto/grand/2394.html (5 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Eby TL, Nadol BJ Jr. Postnatal growth of the human temporal bone: implications for cochlear implants in children. Ann<br />
Otol Rhinol Laryngol 1986;95:356-364.<br />
Faye-Lund H. Acute and latent mastoiditis. J Laryngol Otol 1989;103:1158-1160.<br />
Ginsburg CM, Rudoy R, Nelson JD. Acute mastoiditis in infants and children. Clin Pediatr 1980;19:549-553.<br />
Glasscock ME III, Shambaugh GE Jr. Surgery of the Ear, 4th ed. Philadelphia: WB Saunders, 1990.<br />
Goodwin MR. Acute mastoiditis and acute labyrinthitis without mastoidectomy. Laryngoscope 1968;78:227-235.<br />
Goodwin MR. Complicated acute mastoiditis treated conservatively. N Y State J Med 1969;69:594-598.<br />
Hawkins DB, Dru D. Mastoid subperiosteal abscess. Arch Otolaryngol 1983;109:369-371.<br />
Hawkins DB, Dru D, House JW, Clark RW. Acute mastoiditis in children: a review of 54 cases. Laryngoscope<br />
1983;93:568-572.<br />
Holt GR, Gates GA. Masked mastoiditis. Laryngoscope 1983;93:1034-1037.<br />
Holt GR, Young WC. Acute coalescent mastoiditis. Otolaryngol Head Neck Surg 1981;89:317-321.<br />
Jazrawy H, Wortzman G, Kassel EE, Noyek AM. Computed tomography of the temporal bone. J Otolaryngol 1983;12:37-<br />
44.<br />
Juselius H, Kaltiokallio K. Complications of acute and chronic otitis media in the antibiotic era. Acta Otolaryngol<br />
1972;74:445-450.<br />
Lim DJ, DeMaria TF. Pathogenesis of otitis media. Bacteriology and immunology. Laryngoscope 1982;92:278-287.<br />
Maharaj D, Jadwat A, Fernandes CM, Williams B. Bacteriology in acute mastoiditis. Arch Otolaryngol Head Neck Surg<br />
1987;113:514-515.<br />
Mathews TJ. Acute and acute-on-chronic mastoiditis (a five-year experience at Groote Schuur Hospital). J Laryngol Otol<br />
1988;102:115-117.<br />
McKenzie W. The Schwartze mastoidectomy, its value at the present time. Arch Otolaryngol 1958;67:417-423.<br />
Meyerhoff WL, Giebink GS, Shea DA, Le CT. Effect of tympanostomy tubes on the pathogenesis of acute otitis media.<br />
Am J Otolaryngol 1982;3:189-195.<br />
Meyerhoff WL, Gates GA, Montalbo PJ. Pseudomonas mastoiditis. Laryngoscope 1977;87:483-492.<br />
Milstein S. The history of mastoid surgery. Am J Otol 1980;1:174-178.<br />
http://www.bcm.edu/oto/grand/2394.html (6 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Neely JG: Complications of suppurative otitis media, Part 1: Aural complications. American Academy of Otolaryngology<br />
Self-Instruction Package 78300. Rochester, 1978.<br />
Nielsen JM. Intracranial complications of otitis media and mastoiditis in the antibiotic era. II. Intracranial complications of<br />
otitis media as modified by sulfa drugs and antibiotics - clinical aspects. Laryngoscope 1955;65:47-52.<br />
Ogle JW, Lauer BA. Acute mastoiditis: diagnosis and complications. Am J Dis Child 1986;1178-1182.<br />
Palva T, Virtanen H, Makinen J. Acute and latent mastoiditis in children. J Laryngol Otol 1985;99:127-136.<br />
Palva T, Pulkkinen K. Mastoiditis. J Laryngol Otol 1959;78:573-588.<br />
Palva T. Mastoiditis in children. Laryngoscope 1962;72:353-360.<br />
Paparella MM, Meyerhoff WL, Oliviera CA. Mastoiditis and brain hernia (mastoiditis cerebri). Laryngoscope<br />
1978;88:1097-1106.<br />
Pfaltz CR, Griesemer C. Complications of acute middle ear infections. Ann Otol Rhinol Laryngol Suppl 1984;112:133-<br />
137.<br />
Ronis BJ, Ronis ML, Liebman EP. Acute mastoiditis as seen today. Eye Ear Nose Throat 1968;47:502-507.<br />
Rosen A, Ophir D, Marshak G. Acute mastoiditis: a review of 69 cases. Ann Otol Rhinol Laryngol 1986;95:222-224.<br />
Rubin JS, Wei WI. Acute mastoiditis: a review of 34 patients. Laryngoscope 1985;95:963-965.<br />
Samuel J, Fernandes CM. Otogenic complications with an intact tympanic membrane. Laryngoscope 1985;95:1387-1390.<br />
Scheibel WR, Urtes MA. Mastoiditis. Am Fam Physician 1987;35:123-127.<br />
Scott TA, Jackler RK. Acute mastoiditis in infancy: a sequela of unrecognized acute otitis media. Otolaryngol Head Neck<br />
Surg 1989;101:683-687.<br />
Shaffer HL, Gates GA, Meyerhoff WL. Acute mastoiditis and cholesteatoma. Otolaryngol 1978;86:ORL394-399.<br />
Smouha EE, Levenson MJ, Anand VK, Parisier SC. Modern presentations of Bezold's abscess. Arch Otolaryngol Head<br />
Neck Surg 1989;115:1126-1129.<br />
Sorensen H. Antibiotics in suppurative otitis media. Otolaryngol Clin North Am 1977;10:45-50.<br />
Venezio FR, Naidich TP, Shulman ST. Complications of mastoiditis with special emphasis on venous sinus thrombosis. J<br />
Pediatr 1982;101:509-513.<br />
http://www.bcm.edu/oto/grand/2394.html (7 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/2394.html (8 of 8) [5.11.2005 10:43:06]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
SURGICAL MANAGEMENT OF MENIERE'S SYNDROME<br />
April 14, 1994<br />
Glenn Knox, M.D.<br />
Although the underlying etiology of Meniere's syndrome is unknown, a consistent histopathologic finding<br />
is hydrops (dilatation) of the endolymphatic spaces. The hydrops presumably results from a malfunction<br />
of the resorptive function of the endolymphatic sac. The classic constellation of symptoms includes:<br />
fluctuating hearing loss, episodic vertigo, tinnitus, and a sensation of fullness in the ear. These symptoms,<br />
however, do not necessarily develop simultaneously and many patients do not develop them at all.<br />
Subcategories of Meniere's syndrome describe these other conditions; for instance, cochlear hydrops<br />
(fluctuating hearing loss alone) or vestibular hydrops (vestibular symptoms without hearing loss).<br />
In most patients, Meniere's syndrome is ultimately self-limited; over time the patient suffers deterioration<br />
of hearing and a gradual subsiding of the episodic dizzy spells. This evolution, however, may require 1 to<br />
http://www.bcm.edu/oto/grand/41494.html (1 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
2 decades. In the interim, the patient's lifestyle may be severely impaired.<br />
A few patients cannot be adequately managed by medical means alone and surgical intervention must be<br />
considered. The surgical procedures for Meniere's disease may be categorized as those designed to alter<br />
the function of the vestibular system and those that ablate the vestibular system either with or without<br />
preservation of hearing.<br />
Case Presentation<br />
A 58-year-old white female noted the onset of fluctuating right hearing loss, right tinnitus and vertigo<br />
eight years prior to presentation. For the first 5 years her symptoms were controlled with sodium<br />
restriction and diuretics. Three years prior to presentation she began to experience intense episodic<br />
vertigo associated with nausea and vomiting. Two years prior to presentation she underwent a right<br />
endolymphatic shunt procedure with some relief of her symptoms. After a 6-month period the vertigo and<br />
dizziness returned. She underwent a revision of the endolymphatic shunt 1 year prior to presentation,<br />
again followed by initial relief and then recurrence of symptoms. She was referred to The Methodist<br />
Hospital for further evaluation. Preoperative evaluation showed predominantly low-frequency<br />
sensorineural hearing loss in the right ear, with a PTA of 45 and a PBmax of 40%. Left ear showed a PTA<br />
of 10 and PBmax of 100%. ENG showed right unilateral weakness. ABR was normal bilaterally. The<br />
patient underwent a right middle cranial fossa vestibular nerve section. Postoperatively the patient did<br />
well and has been free of vertiginous episodes<br />
Bibliography<br />
Amedee RG, Norris CH, Risey JA. Selective chemical vestibulectomy: preliminary results with human application.<br />
Otolaryngol Head Neck Surg 1991;105:107-112.<br />
Andrews JC, Ator GA, Honrubia V. The exacerbation of symptoms in Meniere's disease during the premenstrual period.<br />
Arch Otolaryngol Head Neck Surg 1992;118:74-78.<br />
Austin DF. Class A results in Meniere's disease. Am J Otol 1991;12:317-322.<br />
Barun V, Richter HP. Results of 100 consecutively operated patients with acoustic neuroma. Nervenarzt 1993;64:238-243.<br />
Bohmer A, Fisch U. Bilateral vestibular neurectomy for treatment of vertigo. Otolaryngol Head Neck Surg1993;109:101-<br />
107.<br />
Boles R, Rice DH, Hybels R, Work WP. Conservative management of Meniere's disease: Furstenberg regimen revisited.<br />
http://www.bcm.edu/oto/grand/41494.html (2 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Ann Otol Rhinol Laryngol 1975;84:513-517.<br />
Brackmann DE. Surgical treatment of vertigo. J Laryngol Otol 1990;104:849-859.<br />
Cass SP, Kartush JM, Graham MD. Clinical assessment of postural stability following vestibular nerve section.<br />
Laryngoscope 1991;101:1056-1059.<br />
Cass SP, Kartush JM, Graham MD. Patterns of vestibular function following vestibular nerve section. Laryngoscope<br />
1992;102:388-394.<br />
Cody DT. The tack operation for endolymphatic hydrops. Laryngoscope 1969;79:1737-1744.<br />
Colebatch JG, Halmagyi GM. Vestibular evoked potentials in human neck muscles before and after unilateral vestibular<br />
deafferentation. Neurology 1992;42:1635-1636.<br />
Curthoys IS, Dai MJ, Halmagyi GM. Human ocular torsional position before and after unilateral vestibular neurectomy.<br />
Exp Brain Res 1991;85:218-225.<br />
Debruyne F. Clinical observations on the on-off effect of the acoustic stapedius reflex. Clin Otolaryngol 1992;17:10-12.<br />
Derebery MJ, Valenzuela S. Meniere's syndrome and allergy. Otolaryngol Clin North Am 1992;25:213-224.<br />
Fick IA. Decompression of the labyrinth: a new surgical procedure for Meniere's disease. Arch Otolaryngol 1964;79:447-<br />
458.<br />
Furman JM, Schor RH, Kamerer DB. Off-vertical axis rotational responses in patients with unilateral peripheral vestibular<br />
lesions. Ann Otol Rhinol Laryngol 1993;102:137-143.<br />
Gibson WP. The use of intraoperative electrocochleography in Meniere's surgery. Acta Otolaryngol Suppl 1991;485:65-73.<br />
Giddings NA, Shelton C, O'Leary MJ, Brackmann DE. Ocohleosacculotomy revisited: long-term results poorer than<br />
expected. Arch Otolaryngol Head Neck Surg 1991;117:1150- 1152.<br />
Goin DW, Mischke RE, Esses BA, Young D, Priest EA, Whitmoyer-Goin V. Hearing results from endolymphatic sac<br />
surgery. Am J Otol 1992;13:393-397.<br />
Graham MD. Transmastoid labyrinthectomy: further experience with the indications, complications and early postoperative<br />
results. J Laryngol Otol 1981;95:1205-1211.<br />
Graham MD, Colton JJ. Transmastoid labyrinthectomy: indications, technique and early postoperative results.<br />
Laryngoscope 1980;90:1253-1263.<br />
Green JD Jr, Blum DJ, Harner SG. Longitudinal follow-up of patients with Meniere's disease. Otolaryngol Head Neck Surg<br />
1991;104:783-788.<br />
http://www.bcm.edu/oto/grand/41494.html (3 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Halmagyi GM, Curthoys IS, Todd MJ, D'Cruz DM, Cremer PD, Henderson CJ, Staples MJ. Unilateral vestibular<br />
neurectomy in man causes a severe permanent horizontal vestibulo- ocular reflex deficit in response to high-acceleration<br />
ampullofugal stimulation. Acta Otolaryngol Suppl 1991;481:411-414.<br />
Hausler R, Kasper A, Demierre B. Intraoperative electrically evoked vestibular potentials in humans. Acta Otolaryngol<br />
1992;112:180-185.<br />
Heermann J. Predominance of left ear in Meniere's disease, sudden deafness, inner ear damage, tinnitus and abnormally<br />
patent Eustachian tube. Ear Nose Throat J 1993;72:205- 208.<br />
Hickey SA, O'Commor AF. Measurement of drill-generated noise levels during ear surgery. J Laryngol Otol 1991;105:732-<br />
735.<br />
Huang TS, Lin CC. Endolymphatic sac surgery for refractory luetic vertigo. Am J Otol 1991;12:184-187.<br />
Huang TS, Lin CC. Revision endolymphatic sac surgery for recurrent Meniere's disease. Acta Otolaryngol Suppl<br />
199;485:131-144.<br />
Huang TS, Linn C. Surgical treatment of chronic otitis media and Meniere's syndrome. Laryngoscope 1991;101:900-904.<br />
Huang TS, Lin CC, Chang YL. Endolymphatic sac surgery for Meniere's disease: a cumulative study of twelve years'<br />
experience. Acta Otolaryngol Suppl 1991;485:145-154.<br />
Hughes GB, et al. Autoimmune reactivity in Meniere's disease: a preliminary report. Laryngoscope 1983;93:410-417.<br />
Itoh A, Sakata E. Treatment of vestibular disorders. Acta Otolaryngol Suppl 1991;481:617- 623.<br />
Jackson CG, personal communication.<br />
Karmody CS, Schuknecht HF. Deafness in congenital syphilis. Arch Otolaryngol 1966;83:18- 27.<br />
Kemink JL, Telian SA, Graham MD, et al. Transmastoid labyrinthectomy: reliable surgical management of vertigo.<br />
Otolaryngol Head Neck Surg 1989;101:5-10.<br />
Li CW, Cousins V, Hooper R. Vestibulo-ocular compensation following unilateral vestibular deafferentation. Ann Otol<br />
Rhinol Laryngol 1992;101:525-529.<br />
Linstrom CJ, Stockwell CW. Clinical evaluation of the monothermal caloric test. Otolaryngol Head Neck Surg<br />
1993;108:27-35.<br />
Love JT. Basilar artery migraine presenting as fluctuating hearing loss and vertigo. Otolaryngol Head Neck Surg<br />
1978;86:450-458.<br />
Luetje CM. Hearing results following posterior semicircular canal injury during antesigmoid retrolabyrinthine selective<br />
vestibular nerve section. Am J Otol 1992;13:600-602.<br />
http://www.bcm.edu/oto/grand/41494.html (4 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
McCabe B. Autoimmune sensorineural hearing loss. Ann Otol Rhinol Laryngol 1979;88:585- 589.<br />
Maddox D, personal communication.<br />
Magliulo G, Vingolo GM, Petti R, de Vincentiis M. Vestibular neurectomy by the infralabyrinthine approach. J Laryngol<br />
Otol 1992;106:780-782.<br />
Magnan J, Bremond G, Chays A, Gignac D, Florence A. Vestibular neurotomy by retrosigmoid approach: technique,<br />
indications, and results. Am J Otol 1991;12:101-104.<br />
Moffat DA, Baguley DM, Harries ML, Atlas M, Lynch CA. Bilateral electrocochleographic findings in unilateral Meniere's<br />
disease. Otolaryngol Head Neck Surg 1992;107:370-373.<br />
Moffat DA, Toner JG, Baguley DM, Hardy DG. Posterior fossa vestibular neurectomy. J Laryngol Otol 1991;105:1002-<br />
1003.<br />
Monsell EM, Shelton C. Labyrinthotomy with streptomycin infusion: early results of a multicenter study. The LSI<br />
Multicenter Study Group. Am J Otol 1992;13:416-425.<br />
Nedzelski JM, Schessel DA, Bryce GE, Pfleiderer AG. Chemical labyrinthectomy: local application of gentamicin for the<br />
treatment of unilateral Meniere's disease. Am J Otol 1992;13:18-22.<br />
Nguyen CD, Brackmann DE, Crane RT, Linthicum FH Jr, Hitselberger WE. Retrolabyrinthine vestibular nerve section:<br />
evaluation of technical modification in 143 cases. Am J Otol 1992;13:328-332.<br />
Nomura Y, Okuno T, Hara M, Young YH. "Floating" labyrinth: pathophysiology and treatment of perilymph fistula. Acta<br />
Otolaryngol 1992;112:186-191.<br />
Ohlms LA, Lonsbury-Martin BL, Martin GK. The clinical applications of acoustic distortion products. Otolaryngol Head<br />
Neck Surg 1990;103:52-59.<br />
Paparella MM, DaCosta SS, Fox R, Yoon TH. Meniere's disease and other labyrinthine diseases. In: Paparella MM,<br />
Shumrick DA, Gluckman JL, Meyerhoff WL, eds. Otolaryngology. Philadelphia: WB Saunders, 1991:1689-1714.<br />
Parnes LS, Campbell KC. Chronic perilymph fistula in the guinea pig with implications in the human. Ann Otol Rhinol<br />
Laryngol 1992;101:176-182.<br />
Pulec JL. Meniere's disease: results of two and a half years' study of etiology, natural history and results of treatment.<br />
Laryngoscope 1972;82:1703-1715.<br />
Pulec JL. The otic-periotic shunt. Otolaryngol Clin North Am 1968;1:643-648.<br />
Pulec JL. The surgical treatment of vertigo. Laryngoscope 1979;79:1783-1822.<br />
Ramsden RT, Timms MS. Promontory stimulation following labyrinthectomy. J Laryngol Otol 1991;105:729-731.<br />
http://www.bcm.edu/oto/grand/41494.html (5 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Rassekh CH, Harker LA. The prevalence of migraine in Meniere's disease. Laryngoscope 1992;102:135-138.<br />
Report of the Committee on Hearing and Equilibrium. Trans Am Acad Ophthalmol Otolaryngol 1972;76:1462-1464.<br />
Rosenberg S, Silverstein H, Flanzer J, Wanamaker H. Bilateral Meniere's disease in surgical versus nonsurgical patients.<br />
Am J Otol 1991;12:336-340.<br />
Ruth RA. Trends in electrocochleography. J Am Acad Audiol 1990;1:134-137.<br />
Schuknecht HF. Cochleosacculotomy for Meniere's disease: internal endolymphatic shunt. Oper Tech Otolaryngol<br />
1991;2:35-37.<br />
Schuknecht HF. Myths in neurotology. Am J Otol 1992;13:124-136.<br />
Schuknecht HF. Pathology of Meniere's disease as it relates to the sac and tack procedures. Ann Otol Rhinol Laryngol<br />
1977;86:677-682.<br />
Schuknecht HF. Pathology of the Ear. Cambridge, MA: Harvard Univ Press, 1974.<br />
Schuknecht HF. Transcanal labyrinthectomy. Oper Tech Otolaryngol 1991;2:17-19.<br />
Schwaber MK, Kveton J. Transmastoid labyrinthectomy. Oper Tech Otolaryngol 1991;2:20- 22.<br />
Schwaber MK, Whetsell WO. Cochleovestibular nerve compression syndrome. II. Vestibular nerve histopathology and<br />
theory of pathophysiology. Laryngoscope 1992;102:1030-1036.<br />
Shambaugh GE Jr. Decompression of the endolymphatic sac for hydrops. Otolaryngol Clin North Am 1968;1:613-621.<br />
Shea JJ. Medical and surgical treatment of Meniere's disease. Ann Acad Med Singapore 1991;20:686-689.<br />
Shea JJ, Norris CH. Streptomycin perfusion of the labyrinth. Acta Otolaryngol Suppl 1991;485:123-130.<br />
Shotton JC, Gresty MG, Ludman H, Metcalfe T. Clinical and vestibulometric status following labyrinthectomy or<br />
vestibular nerve section for Meniere's disease. Clin Otolaryngol 1992;17:332-336.<br />
Silverstein H, Norrell H. Retrolabyrinthine vestibular neurectomy. Otolaryngol Head Neck Surg 1982;90:778-782.<br />
Silverstein H, Wanamaker H, Flanzer J, Rosenberg S. Vestibular neurectomy in the United States - 1990. Am J Otol<br />
1992;13:23-30.<br />
Sperling NM, Paparella MM, Yoon TH, Zelterman D. Symptomatic versus asymptomatic endolymphatic hydrops: a<br />
histopathologic comparison. Laryngoscope 1993;103:277-285.<br />
Spindler J. Negative relationships between responses from head-shake and caloric tests. Ann NY Acad Sci 1992;656:892-<br />
http://www.bcm.edu/oto/grand/41494.html (6 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
894.<br />
Stouffer JL, Tyler RS, Kileny PR, Dalzell LE. Tinnitus as a function of duration and etiology: counselling implications.<br />
Am J Otol 1991;12:188-194.<br />
Suzuki M, Kitahara M. Immunologic abnormality in Meniere's disease. Otolaryngol Head Neck Surg 1992;107:57-62.<br />
Teixido M, Wiet RJ. Hearing results in retrolabyrinthine vestibular neurectomy. Laryngoscope 1992;102:33-38.<br />
Telischi FF, Luxford WM. Long-term efficacy of endolymphatic sac surgery for vertigo in Meniere's disease. Otolaryngol<br />
Head Neck Surg 193;109:83-87.<br />
Thomsen J, Bretlau P, Tos M, Johnsen NJ. Endolymphatic sac - mastoid shunt surgery: a nonspecific treatment modality?<br />
Ann Otol Rhinol Laryngol 1986;95:32-35.<br />
Thomsen J, Bretlau P, Tos M, Johnsen NJ. Placebo effect in surgery for Meniere's disease. Arch Otolaryngol 1981;107:271-<br />
277.<br />
Uemura K. Some neurosurgical and clinical neurophysiological notes on selected neurootological problem, with special<br />
reference to acoustic neurinoma, brain death and NVC. Acta Otolaryngol Suppl 1993;503:174-187.<br />
Viscomi GJ, Bojrab DI. Use of electrocochleography to monitor antigenic challenge in Meniere's disease. Otolaryngol<br />
Head Neck Surg 1992;107:733-737.<br />
Wackym PA, Storper IS, Fu YS, House WF, Ward PH. Differential diagnosis of virus-like particles in the human inner ear.<br />
Am J Otol 1992;13:431-437.<br />
Wolf SR, Christ P, Haid CT. Patient use of telemetric ENG to register nystagmus in the private sphere. Laryngoscope<br />
1993;103:704-707.<br />
Wolf SR, Christ P, Haid CT. "Telemetric" electronystagmography: a new method for examination of nystagmus outside the<br />
clinic. Acta Otolaryngol Suppl 1991;481:374-381.<br />
Wolfe GI, Taylor CL, Flamm ES, Gray LG, Raps EC, Galetta SL. Ocular tilt reaction resulting from vetibuloacoustic nerve<br />
surgery. Neurosurgery 1993;32:417-421.<br />
Yoo TJ, et al. Type II collagen autoimmunity in otosclerosis and Meniere's disease. Science 1982;217:115301155.<br />
Yoshida GY, Woods TR, Barrs DM. Mastoid pneumatocele: unusual complication after transmastoid translabyrinthine<br />
labyrinthectomy. Otolaryngol Head Neck Surg 1991;105:877- 880.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
http://www.bcm.edu/oto/grand/41494.html (7 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/41494.html (8 of 8) [5.11.2005 10:43:16]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
Introduction<br />
MYRINGOPLASTY AND TYMPANOPLASTY<br />
February 16, 1995<br />
Rance W. Raney, M.D.<br />
Tympanoplasty without mastoidectomy is performed to control infection through eradication of disease<br />
and to reconstruct the sound conducting mechanism. Tympanic membrane grafting may or may not be<br />
required. This presentation focuses on tympanoplasty types I through III and ossiculoplasty. It is not a<br />
detailed discussion of otitis media, mastoidectomy or stapedectomy.<br />
Anatomy<br />
Horst Wullstein (1956) said, "The tympanic membrane has two functions, sound pressure transformation<br />
http://www.bcm.edu/oto/grand/21695.html (1 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
for the oval window and sound protection of the round window." The outer ear functions to capture air<br />
pressure waves. The middle ear functions to convert air pressure waves efficiently into endolymphatic<br />
fluid waves, and the inner ear (cochlea) serves to convert fluid waves into nerve impulses. This soundtransforming<br />
mechanism includes the ossicles whose lever action adds 3 dB to the sound level at the oval<br />
window. The hydraulic principle explains how the difference in the surface area of the tympanic<br />
membrane and the stapedial footplate increases the hearing level by 27 dB. The tympanic membrane also<br />
serves to protect the round window from sound by efficiently conducting the pressure waves to the oval<br />
window and delaying the arrival of pressure waves to the round window.<br />
Middle ear pathology associated with perforation or a conductive deficit includes otitis media, otitis<br />
externa, granulation tissue and trauma including myringotomy. Other disorders can interfere with the<br />
ventilatory or conducting function of the middle ear without producing perforations. These include<br />
tympanosclerosis, otosclerosis, congenital cholesteatoma, and Eustachian tube dysfunction.<br />
The Eustachian tube, or pharyngotympanic tube, originates in the middle ear and extends into the<br />
nasopharynx. It is normally closed, but opens for 0.1 to 0.2 seconds during swallowing to allow air to<br />
move between the nasopharynx and middle ear to equalize the pressure across the tympanic membrane.<br />
There is no doubt that Eustachian tube dysfunction can lead to negative pressure in the middle ear and<br />
retraction of the tympanic membrane. But, we cannot distinguish which patients have retractions from<br />
previous tubal dysfunction and which patients have persistent tubal dysfunction and will tend to reform<br />
retractions after surgery.<br />
Preoperative Evaluation<br />
The examiner should make note of otorrhea, hearing loss, otalgia, vertigo and facial weakness when<br />
evaluating a patient with middle ear pathology. A hearing loss of 30 dB or more may represent ossicular<br />
disruption. Progressive loss with no obvious middle ear pathology on exam may represent<br />
tympanosclerosis or otosclerosis.<br />
A microscopic exam should be performed and pneumatic otoscopy used to assess the mobility of the<br />
tympanic membrane and the malleus. A Fistula Test can be performed if there is a history of dizziness or<br />
a marginal perforation.<br />
Surgical Technique<br />
The particular technique that will best repair the tympanic membrane is impossible to determine<br />
preoperatively with confidence. The final decision regarding medial or lateral placement of the graft or<br />
the ossiculoplasty to be performed must be reserved until the ear has been examined under anesthesia.<br />
Wullstein created a classification scheme in 1956 identifying five basic types of tympanoplasty. Type I is<br />
myringoplasty. The Type II tympanoplasty is for tympanic membrane perforations with erosion of the<br />
malleus. It involves grafting on to the incus or the remains of the malleus. The Type III tympanoplasty is<br />
http://www.bcm.edu/oto/grand/21695.html (2 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
indicated for destruction of the lateral ossicles, but with an intact and mobile stapes. It involves placing a<br />
graft onto the stapes and providing protection for the round window. The Type IV tympanoplasty is used<br />
for ossicular destruction including destruction of all or part of the stapes arch. It involves placing a graft<br />
onto or around a mobile stapes footplate. The resulting middle ear consists of the hypotympanum and the<br />
Eustachian tube orifice only. The impedance matching system is abandoned. The Type V tympanoplasty<br />
is used when the footplate of the stapes is fixed. The Paparella modification Type Va with fenestration of<br />
the horizontal canal, has largely been abandoned in favor of Type Vb with stapedectomy. Farrior (1971)<br />
proposed subclassifications based on the resultant ossicular/ prosthesis arrangement.<br />
There are two basic approaches to tympanoplasty without mastoidectomy. The retroauricular and the<br />
transaural approaches are equally successful, but most surgeons choose a retroauricular approach to<br />
anterior perforations.<br />
Tympanic membrane grafting can be accomplished by medial or lateral grafting. Medial grafting, also<br />
known as the underlay technique, involves creating a tympanomeatal flap via a canal incision and<br />
elevation of the annulus and tympanic membrane. Graft material is then secured between the tympanic<br />
membrane and a bed of Gelfoam placed in the middle ear. Lateral grafting can be performed with a<br />
variety of materials. One technique uses an overlay graft of temporalis fascia and free canal skin. This<br />
produces a thick, well-vascularized graft that will clean itself by epithelial migration, but care must be<br />
taken to maintain the acute angle between the drum and the canal anteriorly, which is essential for a good<br />
hearing result. Recurrent retraction pockets can be prevented for the most part, by cartilage grafting and<br />
scutumplasty.<br />
Graft Materials<br />
Materials used for tympanic membrane repair include autologous grafts (from the same person),<br />
homografts (from other humans), xenografts (from animals), or allografts (synthetic materials). Rambo<br />
(1958) described the use of autologous muscle in a procedure he called a musculoplasty. Fat patch<br />
myringoplasty is an autologous tissue technique. Autologous temporalis fascia and canal skin are used<br />
for medial and lateral grafting. Replacing the tympanic membrane with cartilage prevents subsequent<br />
retractions, but obviously shielding large portions of the drum with cartilage causes a substantial hearing<br />
loss. A composite cartilage-perichondrium graft taken from the tragus was evaluated by Poe and Gadre<br />
(1993), who found that reinforcing the posterior quadrants and pars flaccida with cartilage did prevent<br />
retractions.<br />
Homograph materials used in tympanoplasty have included dura, tympanic membranes, ossicles, corneas<br />
and banked cadaveric materials such as tympanic membranes with attached mallei, including sclera,<br />
infant dura, and nasal septal cartilage. One potential drawback of homografts is the theoretical risk of<br />
transmitting pathogens such as HIV. The fixation process inactivates viral particles and the remaining<br />
material is organic but non-viable. The grafts are implants not transplants. Yet, the fear of litigation has<br />
decreased the number of hospitals willing to bank organic materials. Other potential disadvantages<br />
include the additional time required to sculpt and the cost of tissue banking.<br />
http://www.bcm.edu/oto/grand/21695.html (3 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Allograft membranes incorporating wire, metal, ceramic, and plastic, have been largely unsuccessful<br />
according to Campbell (1990). The disadvantage of using allografts is their tendency for extrusion.<br />
Ossiculoplasty<br />
The ossicles may become fixed or lose continuity. They may be eroded by a mass or inflammatory<br />
process, or they may be congenitally malformed. Any of these can prevent the transmission of sound to<br />
the inner ear.<br />
Austin, in 1971, devised a system for classifying ossicular defects. He reasoned that loss of the malleus<br />
head or neck was not important to reconstruction, and that the incus would be mobilized for<br />
reconstruction. So, the condition of the handle of the malleus and the stapes superstructure is the relevant<br />
issuein ossiculoplasty. He classified the four possible defects as types A through D, and noted that most<br />
commonly both the incus and stapes are present. The next most common situation is to have an isolated<br />
defect in the stapes arch. This scheme can aid in planning reconstruction.<br />
Since 1964, homograft ossicles have been used to reconstruct the ME mechanism. The incus could be<br />
prepared in two ways. The notched incus with short process can connect the malleus to the capitulum of<br />
the stapes. The notched incus with long process can connect the malleus to the stapes footplate when the<br />
stapes superstructure was missing or removed. In 1986, hydroxylapatite prostheses became available in<br />
two lengths as an incus or incus-stapes substitute.<br />
Several maneuvers are key to the success of an ossiculoplasty. Special attention should be given to<br />
dislocating the incudostapedial joint, ensuring mobility of the footplate, removing mucosa from the<br />
malleus handle, and popping the prosthesis in place. Malleus head fixation is addressed by dislocation of<br />
the I-S joint followed by dislocation of the I-M joint and removal of the malleus head. Erosion of the<br />
manubrium of the malleus can be addressed by reconstruction with a homograft tympanic membrane and<br />
malleus or use of a PORP (malleus-incus) prosthesis. If the malleus handle and the stapes arch are<br />
absent, a TORP (malleus-incus-stapes) can be used.<br />
There are a wide variety of prostheses available to the surgeon. The stapes prostheses are either wire<br />
loops or pistons. Some of the pistons have a cup rather than a crook to hold the incus. The incus<br />
prostheses come as struts or struts with side arms. Incus-stapes prostheses come in more than 9 types.<br />
They are struts or pistons of stainless steel alone or together with a polymer.<br />
PORP's (partial ossicular reconstruction prostheses) are for lateral chain reconstruction in the absence of<br />
the malleus handle. They have a broad lateral platform designed to minimize point pressure on the TM to<br />
resist extrusion. There are 13 TORP's (total ossicular reconstruction prostheses), available for use as<br />
malleus-incus-stapes substitutes. Ossicular prostheses range in price from about $39.00 to $263.00, and<br />
are constructed of stainless steel, platinum, tantalum, polyethylene, Plasti-pore, fluoroplastic, and<br />
hydroxylapatite.<br />
http://www.bcm.edu/oto/grand/21695.html (4 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Staging Tympanoplasty<br />
In 1991, James Sheehy reviewed the current thinking regarding staging of tympanoplasty in badly<br />
diseased ears. Staged operations have been preferred since the mid-1960's at the House Institute and<br />
elsewhere. The first operation would eliminate disease and aerate the middle ear cleft, and the second<br />
would reconstruct the sound pressure transfer mechanism. There are three requirements for a successful<br />
functional result in tympanoplasty: 1) a tympanic membrane; 2) an air-filled, mucosa-lined middle ear<br />
space; and, 3) a secure connection between the vibrating tympanic membrane and the inner ear fluids.<br />
The need for staging is determined in part, by the second of these: a mucosa lined middle ear space. If<br />
there is minimal mucosal disease at the time of the initial operation, there is no need for staging and the<br />
conductive mechanism may be reconstructed immediately. Often large areas of mucosa are diseased.<br />
Infection must be controlled before healthy mucosa can regenerate. Edematous mucosa and uninfected<br />
granulations are reversible. Mucosa should not be stripped if there is any possibility of rejuvenation,<br />
because denuded areas are prone to formation of synechiae or adhesions, scarring or granulation. Such<br />
scarring can impair drum and ossicular mobility. Another obstacle to the regeneration of the mucosal<br />
lining is the presence of residual squamous epithelium in the middle ear. Remnants from a cholesteatoma<br />
or epithelium migrating medially through a perforation may take root on denuded bone in the middle ear.<br />
If removal of the middle ear disease denudes large areas of the medial wall, staging is necessary to<br />
prevent fibrosis of the middle ear cleft. Staging may also enhance the hearing result by allowing the new<br />
drumhead to "settle" before ossiculoplasty, thereby reducing the risk of lateralization (Donaldson and<br />
Snow, 1992).<br />
Some believe that although staged procedures may produce slightly better hearing result, they are often<br />
unnecessary. This is because many patients with extensive middle ear disease heal amazingly well after<br />
the first procedure. The inability to predict who will heal well leads some to reconstruct the conductive<br />
mechanism in a single procedure hoping for a good result. In this way, those who do well are spared a<br />
second operation (Wehrs, Schuknecht, Austin, Gacek, Jansen, and Shea).<br />
Middle Ear Stents<br />
Exogenous and synthetic materials have been used to prevent adhesions within the middle ear after<br />
resection of mucosa for disease. Rambo (1961) recognized this problem and began filling the middle ear<br />
cleft with paraffin. In the mid-1960's, thin plastic sheets of polyethylene, Teflon and silicone rubber<br />
(silastic) were used. Occasionally, this sheeting was pushed laterally by a bed of scar tissue and extruded.<br />
This led to the use of thicker pieces of 0.04 inch silicone rubber or 0.3mm Supramid.<br />
More recently, biodegradable substances such as Gelfilm and Gelfoam (purified gelatin matrix) have<br />
been used. They do not require removal at a later time and will not extrude. The disadvantage comes<br />
when the material is absorbed and no longer stents the middle ear. Some do not stent the middle ear<br />
space at all, but rather avoid adhesions by leaving the perforation ungrafted until the second stage<br />
http://www.bcm.edu/oto/grand/21695.html (5 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
procedure.<br />
Donaldson and Snow (1992), in a prospective study of 71 patients found a better long-term hearing result<br />
in patients who had mastoidectomies and silastic implants as a part of their first stage procedure. Some<br />
suggest that these measures improve middle ear ventilation by increasing the "air-cushion" available to<br />
resist eustachian reflux.<br />
Surgical Indications and Contraindications<br />
The indications for surgery are conductive hearing loss due to TM perforation or ossicular dysfunction;<br />
chronic or recurrent otitis media and recurrent otitis media due to contamination through a perforated<br />
tympanic membrane; progressive hearing loss due to chronic ME pathology; perforation or hearing loss<br />
persistent for more than three months due to trauma, infection or surgery; and, the inability to bathe or<br />
participate in water sports safely due to perforation of the TM. Normal hearing is not a contraindication<br />
to surgery in the presence of disease, because secretions and granulations may close a perforation or<br />
protect the round window thus improving a conductive deficit, or a cholesteatoma might conduct sound<br />
as a functional portion of the ossicular chain.<br />
Glasscock (1976) listed four absolute contraindications and seven relative contraindications to<br />
tympanoplasty. Absolute contraindications are uncontrolled cholesteatoma, malignant tumors, unusual<br />
infections, and complications of chronic ear disease such as meningitis, brain abscess or sinus<br />
thrombosis. The relative contraindications include Eustachian tube insufficiency, uncooperative patients,<br />
a dead ear, a better hearing or only hearing ear, elderly patients, young children and cases of repeated<br />
failure.<br />
He stated that the factors considered in the surgeon's decision to close the ear or leave it open constitute<br />
the indications or contraindications for tympanoplasty. He stressed that tympanoplasty has been<br />
controversial from the start because filling an infected cavity with foreign material and then closing it off<br />
to the outside, flies in the face of classical surgical training.<br />
Much has been made of the presence or absence of discharge in the ear at the time of surgery. Several<br />
studies found that the secretion type (dry vs. mucoid or purulent) in the middle ear at the time of surgery<br />
had no effect on the final success rate for myringoplasty. Poor eustachian function as evidenced by<br />
contralateral effusion or atelectasis predicts poorer results (60% success).<br />
Post-Operative Care<br />
One goal of post-operative care is to keep the patient comfortable. Infection is generally prevented by<br />
antibiotic-soaked canal and middle ear packing and host defenses. In order for the graft to heal it must<br />
remain in contact with organic matrix or stroma, be free from infection, and not experience shearing<br />
forces or excessive tension. Aural hygiene is aimed at achieving this environment. Maneuvers that<br />
change the transtympanic pressure are forbidden, such as sneezing with the mouth shut, using a straw to<br />
http://www.bcm.edu/oto/grand/21695.html (6 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
drink, valsalva or heavy lifting or nose blowing.<br />
Complications<br />
Possible complications of tympanoplasty include: failure of the graft to heal resulting in residual or<br />
recurrent perforation, lateralization of a graft, canal stenosis, scarring or adhesions in the middle ear,<br />
perilymph fistula and hearing loss, erosion or extrusion of a prosthesis, dislocation of a prosthesis, facial<br />
nerve or chorda tympani injury.<br />
Other problems may or may not be surgical complications, such as recurrence of cholesteatoma or<br />
atelectasis of the middle ear space with retraction of the TM. The patient should be informed of these<br />
preoperatively, and understand the importance of aural hygiene and follow-up care.<br />
Pediatric Tympanoplasty<br />
Timing of repair in the pediatric population is very controversial. Glasscock (1976) gave young age as a<br />
relative contraindication to tympanoplasty because children under three or four are prone to upper<br />
respiratory infections and otitis media. Koch et al (1990) reported an 81% success rate for children age 8<br />
and older, but only a 30% success rate in younger patients. They concluded that tympanoplasty before<br />
age 8 results in a high rate of failure because of poor Eustachian tube function and frequent URI's. Smyth<br />
(1992) agreed, noting that patients less than 10 years old had a higher failure rate for myringoplasty than<br />
older children. This was independent of secretion type, perforation site, and graft material.<br />
Yet, others such as Lau and Tos (1986) found no significant difference in outcome between the 2 to 7 age<br />
group and those children ages 8 to 14. They suggested that early operation may prevent progression of<br />
ossicular chain resorption. Ophir et al (1987) reported a 79% overall success rate, and their success in<br />
younger children (5-8) was comparable to the rate for older children. They concluded that myringoplasty<br />
had a good chance of success at any age. Kessler et al (1994) reviewed the results of 209 myringoplasties<br />
and concluded that even in young patients (2-6 years) myringoplasty has a high success rate (75-94%),<br />
and that age alone could not be considered a contraindication to surgery.<br />
Surgical Outcome<br />
In his 1992 Toynbee Memorial Lecture, Gordon Smyth of Belfast stated that any hope for cost-effective<br />
health care reform required urgent self-audit and the provision of more realistic advice to patients. He<br />
took exception to the generally quoted success rate for myringoplasty of 90%. When the success rate is<br />
corrected for the length of follow-up, using Survival Life-table Analysis, the success rate for maintaining<br />
a healed TM diminished to 81% at 11 years. He also suggested that the success of ossiculoplasty should<br />
be measured as the effect on binaural hearing, rather than the air-bone gap on the operated side. This is<br />
because the operated ear must reach an air conduction level of 30 dB at speech frequencies or be within<br />
15 dB of the other ear for the patient to benefit (Belfast rule of thumb) (Smyth and Peterson, 1985).<br />
Smyth warned that, "Fiction and fact need untangling, otherwise surgeons are little better than gossips."<br />
http://www.bcm.edu/oto/grand/21695.html (7 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Summary<br />
In summary, tympanoplasty without mastoidectomy is performed to eradicate middle ear disease and<br />
reconstruct the conductive hearing mechanism. Priorities in tympanoplasty are to prevent recurrence, to<br />
improve hearing and to minimize ear after care.<br />
Though most would agree that myringoplasty has a high success rate and that staged operations optimize<br />
the hearing result, controversy abounds in other areas. Specifically we need to standardize outcome<br />
measures. To say that a tympanoplasty failed or succeeded in a given case is meaningless if our criteria<br />
are different. 1) It seems reasonable to use post-operative sensorineural hearing level rather than the preoperative<br />
level to calculate closure of the "air-bone gap." 2) When reporting pure tone average, "air-bone<br />
gaps," these results should be tabulated in increments of 5 dB. 3) We should agree to report effusions or<br />
retractions as numbers without lumping them into surgical failures.<br />
We need studies with longer follow-up times. This is difficult for three reasons. 1) The population is<br />
highly mobile in this country. 2) Patients no longer choose which specialist they will see or when they<br />
will see him. Attempts to control medical costs may arbitrarily limit follow-up for asymptomatic<br />
individuals. 3) Patients who are doing well may not see the benefit of follow-up, and conversely, patients<br />
with poor results may blame their surgeon and seek referral to a different otolaryngologist. The solution<br />
to this problem lies in improved physician to physician communication. Pre-operative patient counseling<br />
that stresses the importance of follow-up may help as well.<br />
We need more studies that limit the variability of the population by focusing on a single type of<br />
procedure or pathology. The solution to this problem lies in cooperative studies to increase the<br />
population in each study.<br />
Finally, we need improved means of measuring Eustachian tube function. It may be necessary to measure<br />
small gradual pressure changes on an ambulatory basis, like esophageal pH monitoring, in order to gain<br />
clinically relevant information.<br />
Case Presentation<br />
A 20-year-old man with a history of chronic otitis media as a child, requiring the placement of<br />
tympanostomy tubes on three separate occasions, presented with a left myringotomy that failed to heal<br />
after the last set of tympanostomy tubes. He developed a chronic perforation but rejected surgical repair<br />
in favor of expectant management and meticulous aural hygiene. He has had no ear infections in the last<br />
year. He has no complaints of decreased hearing, otorrhea, tinnitus, dizziness, or ear pain.<br />
Recently, he returned for follow-up examination and requested a tympanoplasty so that he could swim,<br />
http://www.bcm.edu/oto/grand/21695.html (8 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
bathe and exercise without concern for ear protection.<br />
He has no family history of chronic middle ear disease. He has seasonal allergies, but otherwise has no<br />
medical problems. He takes no medications and has no drug allergies.<br />
On physical examination he has a 3cm x 3cm hemangioma of the soft palate on the right. Examination of<br />
the left ear reveals a normal external auditory canal; the tympanic membrane has a 30% posterior<br />
marginal perforation with ragged edges and an adjacent posterior-central monomer. The middle ear<br />
mucosa appears normal. The long process of the incus and stapes appear normal.<br />
He underwent left lateral graft tympanoplasty via a retroauricular approach. The middle ear exploration<br />
revealed no pathology. A type I tympanoplasty was performed using a temporalis fascia and free canal<br />
skin overlay technique.<br />
Bibliography<br />
Alford BR, McFarlane JR, Neely JG. Homograft replacement of the tympanic membrane. Laryngoscope 1976;86:199-208.<br />
Austin DF. Ossicular reconstruction. Arch Otolaryngol 1971;94: 525-535.<br />
Austin DF. Reporting results in tympanoplasty. Am J Otol 1985;6:85-88.<br />
Bellucci RJ. Dual classification of tympanoplasty. Laryngoscope 1973;83:1754-1758.<br />
Black B. A universal ossicular replacement prosthesis: Clinical trials of 152 cases. Otolaryngol Head Neck Surg<br />
1991;104:210-218.<br />
Bluestone CD, Cantekin EI, Douglas GS. Eustachian tube function related to the results of tympanoplasty in children.<br />
Laryngoscope 1979;89:450-458.<br />
Brackman DE, Sheehy JL, Luxford WM. TORPS and PORPS in tympanoplasty: a review of 1042 operations. Otolaryngol<br />
Head Neck Surg 1984;92:32-37.<br />
Campbell EE. Homograft tympanoplasty: a long-term review of 477 ears. Am J Otol 1990;11:66-70.<br />
Chalet NI. Tympanic membrane transplant. Harper Hosp Bull 1964;22:27-34.<br />
Cohen AM, Schwaber MK, Anthony LS, Jerger JF. Eustachian tube function and tympanoplasty. Ann Otol Rhinol<br />
Laryngol 1979;88:339-347.<br />
Committee on conservation of hearing of the American Academy of Ophthalmology and Otolaryngology. Standard<br />
http://www.bcm.edu/oto/grand/21695.html (9 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
classification for surgery of chronic ear disease. Arch Otolaryngol 1965;81:204-205.<br />
Deguine C. Staging in cholesteatoma surgery. Ear Nose Throat J 1993;72:197-200.<br />
Donaldson I, Snow DG. A five year follow up of incus transposition in relation to the first stage tympanoplasty technique.<br />
J Laryngol Otol 1992;106:607-609.<br />
Frootko NJ. Reconstruction of the ear. In: Booth JB, Kerr AG, eds. Scott-Brown's Otolaryngology, 5th ed, Vol. 3. The Ear.<br />
London: Butterworth, 1987:238-263.<br />
Glasscock ME 3d. Contraindications to tympanoplasty II: an exercise in clinical judgment. Laryngoscope 1976;86:70-76.<br />
Glasscock ME 3d. Ossicular chain reconstruction. Laryngoscope 1976;86:211-1221.<br />
Green JD, Shelton C, Brackmann DE. Iatrogenic facial nerve injury during otologic surgery. Laryngoscope 1994;104:922-<br />
926.<br />
Gyo K, Hinohira Y, Hirata Y, Yanagihara N. Incidence of attic retraction after staged intact canal wall tympanoplasty for<br />
middle ear cholesteatoma. Auris Nasus Larynx 1992;19:75-82.<br />
Halik JL, Smith GDL. Long term results of tympanic membrane repair. Otolaryngol Head Neck Surg 1988;98:162-169.<br />
House WF, Patterson ME, Linthicum FH. Incus homografts in chronic ear surgery. Arch Otolaryngol 1966;84:148-153.<br />
Igarashi M, Konishi S, Alford BR, Guilford FR. The pathology of tympanosclerosis. Laryngoscope 1970;80:233-243.<br />
Kaddour HS. Myringoplasty under local anaesthesia: day case surgery. Clin Otolaryngol 1992;17:567-568.<br />
Kessler A, Potsic WP, Marsh RR. Type 1 tympanoplasty in children. Arch Otolaryngol Head Neck Surg 1994;120:487-<br />
490.<br />
Koch WM, Friedman EM, McGill TJI, Healy GB. Tympanoplasty in children: The Boston Children's Hospital experience.<br />
Arch Otolaryngol Head Neck Surg 1990;116:35-40.<br />
Lau T, Tos M. Tympanoplasty in children: an analysis of late results. Am J Otol 1986;7:55-59.<br />
Levenson MJ, Michaels L, Parisier SC. Congenital cholesteatomas of the middle ear in children: origin and management.<br />
Otolaryngol Clin North Am 1989;22:941-954.<br />
Levinson RM. Cartilage-perichondrial composite graft tympanoplasty in the treatment of posterior marginal and attic<br />
retraction pockets. Laryngoscope 1987;97:1069-1074.<br />
Matt BH, Miller RP, Meyers RM, Campbell JM, Cotton RT. Incidence of perforation with Goode T-tube. Int J Pediatr<br />
Otolaryngol 1991;21:1-6.<br />
http://www.bcm.edu/oto/grand/21695.html (10 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Ophir D, Porat M, Marshak G. Myringoplasty in the pediatric population. Arch Otolaryngol Head Neck Surg<br />
1987;113:1288-1290.<br />
Parisier SC, Weiss MH. Recidivism in congenial cholesteatoma surgery. Ear Nose Throat J 1991;70:362-364.<br />
Poe DS, Gadre AK. Cartilage tympanoplasty for management of retraction pockets and cholesteatomas. Laryngoscope<br />
1993;103:614-618.<br />
Rambo JHT. Musculoplasty: a new operation for suppurative middle ear deafness. Trans Am Acad Ophthalmol<br />
Otolaryngol 1958;62:166-177.<br />
Rambo JHT. The use of paraffin to create a middle ear space in musculoplasty. Laryngoscope 1961;71:612-619.<br />
Sheehy JL, Shelton C. Tympanoplasty: To stage or not to stage. Otolaryngol Head Neck Surg 1991;104:399-407.<br />
Smyth GDL. Toynbee Memorial Lecture 1992: facts and fantasies in modern otology: the ear doctor's dilemma. J Laryngol<br />
Otol 1992;106:591-596.<br />
Silverstein H, McDaniel AB, Lichtenstein R. A comparison of TORP, PORP, and incus homograft for ossicular<br />
reconstruction in chronic ear surgery. Laryngoscope 1986;96:159-165.<br />
Stewart MG, Troendle-Atkins J, Starke JR, Coker NJ. Nontuberculous mycobacterial mastoiditis. Arch Otolaryngol Head<br />
Neck Surg 1995;121:225-228.<br />
Tos M, Lau T. Stability of tympanoplasty in children. Otolaryngol Clin North Am 1989;22:15-28.<br />
Vartiainen E. Results of surgical treatment for chronic noncholesteatomatous otitis media in the pediatric population. Int J<br />
Pediatr Otolaryngol 1992;24:209-216.<br />
Vartiainen E. Findings in revision myringoplasty. Ear Nose Throat J 1993;72:201-204.<br />
Wehrs RE. Homograft ossicles in middle ear surgery. Am J Otol 1985;6:33-34.<br />
Wullstein H. Theory and practice of tympanoplasty. Laryngoscope 1956;66:1076-1095.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/21695.html (11 of 11) [5.11.2005 10:43:24]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
OSTEODYSTROPHIES OF THE MIDDLE EAR AND TEMPORAL BONE<br />
February 9, 1995<br />
Carla M. Giannoni, M.D.<br />
Five major osteodystrophies that affect the middle ear and temporal bone are presented: Paget's Disease,<br />
Osteogenesis Imperfecta, Osteopetrosis, Fibrous Dysplasia, and Osteitis Fibrosa Cystica. The<br />
epidemiology, pathophysiology, clinical features, histopathology, diagnosis, treatment and prognosis of<br />
these five disorders are discussed.<br />
Paget's Disease<br />
The classic description of a patient with Paget's disease is that of a deaf old man with a bent back, bowed<br />
legs, curved tibia, a large skull and a wobbling gait. However, these advanced changes are not frequently<br />
seen. Czerny (1873) was first to describe this disease, but it was Sir James Paget (1877) who correlated<br />
http://www.bcm.edu/oto/grand/2895.html (1 of 6) [5.11.2005 10:43:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
and described the clinical and pathological features of this disease. Paget's disease is a chronic,<br />
progressive disorder and is believed to be AD or X-linked. The disease primarily affects older people and<br />
commonly presents in 6th decade. There is evidence for a viral etiology, possibly a slow virus. Diagnosis<br />
is based on history, exam, radiographic and laboratory findings. Frequently, the alkaline phosphatase is<br />
often grossly increased; the acid phosphatase is often elevated - prostate cancer should be ruled out. The<br />
calcium is usually normal. Demineralization of bone is seen radiographically, such as the well-known<br />
osteoporosis circumscripta and cotton-wool patches of the skull. The histology characteristically shows<br />
osteoclastic bone resorption and a mosaic pattern of new, lamellar bone interspersed with marrow spaces<br />
that become obliterated with fibrous tissue. Typically, pagetoid bone and microfractures are seen in the<br />
temporal bone.<br />
Symptoms are mainly due to the excess osteoid and resulting soft, easily deformed bones. Hearing loss<br />
occurs in 5% - 44%: mixed, CHL or SNHL. CHL component is very rare due to ossicular fixation and<br />
surgery is not recommended. Treatment consists of symptomatic relief. Salmon calcitonin can promote<br />
healing of osteolytic lesions, and stabilize hearing. Prognosis is generally good; however, there is a 20-<br />
fold risk for developing osteosarcoma in the pagetoid lesions and these malignancies are very aggressive<br />
lesions and portend a poor prognosis.<br />
Osteogenesis Imperfecta<br />
Osteogenesis Imperfecta results from a defect in the biosynthesis of the alpha 1 or alpha 2 chains of type<br />
I collagen. This results in bone fragility with multiple fractures, bone deformities, thin skin, and capillary<br />
fragility with increased bleeding tendency. Histopathologically, those with the most severe form possess<br />
thin, immature cortical bone with small, irregular spicules of bone, decreased osteoid matrix and<br />
increased fibrous tissue and vascular spaces. A thin, fragile stapes is typical. Those with less severe<br />
forms have hypercellular, nonlamellar (immature) bone which fails to mature; there are large remnants of<br />
cartilage in the endochondral bone and delay in ossification of the endochondral layer. Radiographically<br />
this disorder appears similar to osteoporosis with demineralization / deossification of bone and<br />
sometimes with bowing of long bones, thinning of the cortices and exuberant calus formation at<br />
fractures. In the skull, embryonic microfusion lines or "wormian bone" is seen. A "halo sign" of<br />
demineralization of the otic capsule, similar to otosclerosis, may be found.<br />
Previously in two groups (congenita and tarda), they are now grouped in four main categories: 1. blue<br />
sclera and an associated CHL; 2. most severe form; 3. blue sclera and an associated CHL, more severe<br />
than 1, and associated with skeletal deformities; and, 4. similar to 1, but associated with grey sclera and<br />
normal hearing or SNHL. Severe SNHL occurs in 40% of cases and correlates with gray or normal<br />
sclera. CHL reflects structural changes in the ossicles and usually correlates with patient with blue sclera.<br />
The CHL may be due to soft or missing stapes crural arch, due to otosclerosis or due to a combination of<br />
the two. Otosclerosis commonly occurs in association with OI and the histologic independence of these<br />
two disorders has been clearly demonstrated. Otosclerosis in these patients tends to be more aggressive<br />
and there is a higher incidence of SNHL and window obliteration. Medical treatment with calcium,<br />
vitamin D, calcitonin, and anabolic steroids have not been shown to be helpful. Treatment is aimed at<br />
function; bracing and orthopedic stabilization is provided as needed, and physical therapy to maintain<br />
http://www.bcm.edu/oto/grand/2895.html (2 of 6) [5.11.2005 10:43:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
good range of motion and muscular tone (e.g. swimming) is encouraged. Stapedectomy may yield good<br />
results for CHL.<br />
Osteopetrosis<br />
Osteopetrosis is due to defective osteoclast function with failure of normal bone resorption, while normal<br />
osteoblastic bone formation continues with excess deposition of mineralized osteoid and cartilage and<br />
displacement of marrow spaces. Radiographically, one sees increased density of all bones with loss of<br />
marrow spaces and obliteration of mastoid air cells and paranasal sinuses. Later, the periosteal bone<br />
becomes sclerotic without marrow spaces, resulting in dense, brittle bones and anemia. In infants, the<br />
temporal bone is primarily dense, calcified cartilage; the stapes exists in fetal form; dehiscence of VII is a<br />
consistent finding.<br />
Patients with the "tarda" form may be asymptomatic or they may have syndactyly, easy fracturing of<br />
bones, bone pain, osteomyelitis, and skull thickening, and, possibly, narrowing of foramina of optic,<br />
trigeminal, facial, and auditory cranial nerves. CHL is due to encroachment of bone on the middle ear<br />
space with entrapment or ankylosis of the ossicles. Those with the congenital form die at an early age<br />
from anemia or sepsis (none live more than 20 years). Bone marrow transplantation from HLA-identical<br />
sibs has been used successfully with reversal of anemia & osteosclerosis.<br />
Fibrous Dysplasia<br />
Fibrous dysplasia usually presents in the 2nd or 3rd decades and is a chronic, slowly progressive, but not<br />
self-limiting disease of unknown cause and without a known genetic predisposition. It is pathologically<br />
and radiologically similar to osteitis fibrosa cystic. Monostic, polyostic and syndromal (Mc-Cune -<br />
Albright) types are described. Histopathology shows replacement of normal cancellous bone by a fibrous<br />
stroma arranged in a whorled pattern with "C or Y shapes" of immature, woven bone with scattered<br />
islands of cartilage. The marrow is replaced with fibrous tissue. There is active simultaneous osteoblastic<br />
and osteoclastic activity. Radiographic studies show thickening +/- sclerosis of bones, especially of the<br />
femur, tibia, ribs, jaw and skull; the paranasal sinuses may be obliterated. Variable amounts of the<br />
irregularly arranged spicules of bone lead to the "ground glass" appearance on x-ray. The typically<br />
unilateral distribution may resemble malignant growth and biopsy may be indicated for confirmation of<br />
the diagnosis. Temporal bone involvement is unusual, but it can cause SNHL, vertigo & VII palsy due to<br />
erosion. CHL due to EAC stenosis or cholesteatoma can also occur.<br />
Major otologic findings include: unilateral CHL; swelling of mastoid or temporal regions; SNHL<br />
(erosion otic capsule); stenosis of EAC; cholesteatoma due to stenosis; pain (associated with<br />
cholesteatoma); vertigo (erosion otic capsule) or VII paralysis (erosion fallopian canal). Partial surgical<br />
removal can be performed for functionally or cosmetically deforming masses. XRT is contraindicated in<br />
the treatment of FD because a 0.4% transformation rate to osteo-, chondro-, or fibro-sarcomas (400 time<br />
the de novo risk) has been observed.<br />
http://www.bcm.edu/oto/grand/2895.html (3 of 6) [5.11.2005 10:43:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Osteitis Fibrosa Cystica (von Recklinghausen's disease)<br />
This disease is due to hyperparathyroidism and the resultant hypercalcemia and loss of bone calcium.<br />
Elevated calcium (96% of patient) and elevated radioimmunoassay for iPTH (carboxyl end) provide the<br />
diagnosis. The cause is usually a parathyroid adenoma (85-90% cases), occasionally associated with<br />
MEN I syndrome. It may also be due to chief cell hyperplasia. (MEN I or Wermer's syndrome consists of<br />
hyperparathyroidism, pancreatic islet cell tumors and pituitary tumors.) The hypercalcemia caused by<br />
parathryoid hormone influenced release of calcium from bone causes a clinical symptom complex of<br />
"Bones, Stones, Moans, Groans, and Hypertones." This refers to the complications of hypercalcimia that<br />
are observed: skeletal deformities; muscle weakness and wasting; bone pain and fractures; anemia; renal<br />
stones (nephrocalcinosis); abdominal pain, ulcer disease and pancreatitis; and impaired mentation,<br />
depression, hyperreflexia, and rarely coma.<br />
Histopathology shows tongues of fibrous tissue with leading osteoclasts; the resulting abnormal bone is<br />
demineralized and made up of loosely arranged trabeculae of varying sizes interspersed with marrow<br />
spaces containing fibrous tissue. Cystic degeneration of fibrous tissue may occur and lead to the<br />
formation of brown tumors. Temporal bone shows similar changes and some cases of SNHL have been<br />
observed. Radiographic studies show subperiosteal erosions ("pepper-pot skull"), chondrocalcinosis and<br />
nephrocalcinosis. Neck exploration are generally curative with restoration of normal calcium balance.<br />
Surgery should be entertained especially in those patients that exhibit one of the following five criteria:<br />
Ca >11.0, x-ray evidence for metabolic bone disease, presence of a complication of hypercalcemia,<br />
active nephrolithiasis, or decreasing renal function.<br />
Case Presentation<br />
A 72-year-old Hispanic man presented in April 1992 with right hip and back pain. A routine lumbarspine<br />
series revealed marked degenerative changes of the lumbar spine with narrowing of the intervertebral<br />
spaces and some increased bone densities of the right ilium and lumbar spine. The findings were<br />
consistent with degenerative change of the spine or possibly Paget's disease. Further evaluation was<br />
significant for an elevated alkaline phosphatase and normal levels of calcium, ionized calcium,<br />
phosphorous, magnesium and PSA. A 24-hour urine calcium collection was significantly elevated (416<br />
mg/24 hr). He was seen by the Endocrinology service and started on Indomethacin and Didronel with<br />
partial pain relief; salmon calcitonin was then begun with good alleviation of his symptoms. With<br />
treatment, his alkaline phosphatase levels decreased to the high normal range. He did well, and in May of<br />
1993 a taper of his calcitonin was commenced. Unfortunately, in November 1993 he re-presented with a<br />
compression fracture of L5. He was restarted on calcitonin with good response and subsequently retapered<br />
off calcitonin over six months.<br />
The patient was referred to the Otolaryngology service in September 1994 with a complaint of hearing<br />
loss of several years' duration. The loss was greater in the left ear than the right. He also noted mild<br />
http://www.bcm.edu/oto/grand/2895.html (4 of 6) [5.11.2005 10:43:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
episodic dizziness over the previous two months. Routine audiometric evaluation revealed a right downsloping<br />
sensorineural hearing loss and a left mixed hearing loss with a significant conductive component.<br />
Tympanograms were normal. Laboratory evaluation showed an alkaline phosphatase again elevated<br />
(115) and he was restarted on calcitonin with relief of his pain and dizziness. The patient has been<br />
referred for amplification and is currently doing well on a tapering dose of calcitonin.<br />
Bibliography<br />
Andreoli TE, ed. Cecil Essentials of Medicine, 3rd ed. Philadelphia: Saunders, 1993:1415-1468.<br />
Armstrong BW. Stapes in patients with osteogenesis imperfecta. Ann Otol Rhinol Laryngol 1984;93:634-636.<br />
Berger G, Hawke M, Johnson A, Proops D. Histopathology of the temporal bone in osteogenesis imperfecta congenita - a<br />
report of 5 cases. Laryngoscope 1985;95:193-199.<br />
Coccia PF, Krivit W, Cervenka J, Clawson C, Kersey JH, Kim TH. Successful bone-marrow transplantation for infantile<br />
malignant osteopetrosis. N Engl J Med 1980;302:701-708.<br />
Davies DG. Paget's disease of the temporal bone, a clinical and histopathological survey. Acta Otolaryngol Suppl<br />
1968;242:1-47.<br />
Edeiken J, Dalinka M, Karasick D. Edeiken's Roentgen Diagnosis of Diseases of the Bone, 4th ed, vol. 2. Baltimore:<br />
Williams & Wilkins, 1990.<br />
Harersma H. Total decompression of the facial nerve in osteopetrosis. ORL J Otorhinolaryngol Relat Spec 1973;36:21-25.<br />
Hawke M, Jahn AF, Bailey D. Osteopetrosis of the temporal bone. Arch Otolaryngol 1981;107:278-282.<br />
Khetarpal U, Schuknecht HF. In search of pathologic correlates of hearing loss and vertigo in Paget's disease, a clinical<br />
and histopathologic study of 26 temporal bones. Ann Otol Rhinol Laryngol Suppl 1990;145:1-16.<br />
Kritzinger EE, Wright BE. Color Atlas of the Eye and Systemic Disease. Chicago: Year Book Medical Publishers, 1984.<br />
Lindsay JR, Suga F. Sensorineural deafness due to osteitis fibrosa. Arch Otolaryngol 1976;102:37-42.<br />
Marcover RC, Arlen M. Atlas of Bone Pathology with Clinical and Radiographic Correlations. Philadelphia: Lippincott,<br />
1992.<br />
Mills BG, Singer FR. Nuclear incisions in Paget's disease of bone. Science 1976;194:201-202.<br />
Milroy CM, Michaels L. Temporal bone pathology of adult type osteopetrosis. Arch Otolaryngol Head Neck Surg<br />
http://www.bcm.edu/oto/grand/2895.html (5 of 6) [5.11.2005 10:43:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
1990;116:79-84.<br />
Mirra JM. Pathogenesis of Paget's disease based on viral etiology. Clin Orthop 1987;217:162-170.<br />
Myers EN, Stool S. The temporal bone in osteopetrosis. Arch Otolaryngol 1969;89:460-469.<br />
Nadol JB Jr, Merchant SN. Systemic disease manifestations in the middle ear and temporal bone. In: Cummings, CW,<br />
Harker LA, editors. Otolaryngology - Head and Neck Surgery, 2nd ed, vol 4. St Louis: Mosby, 1993:2906-2925.<br />
Nager GT. Osteogenesis imperfecta of the temporal bone and its relation to otosclerosis. Ann Otol Rhinol Laryngol<br />
1988;97:585-593.<br />
Nager GT, Holliday MJ. Fibrous dysplasia of the temporal bone: update with case reports. Ann Otol Rhinol Laryngol<br />
1983;93:630-633.<br />
Parons V. Color Atlas of Bone Disease. Chicago: Year Book Medical Publishers, 1980.<br />
Patterson CN, Stone HB 3d. Stapedectomy in van der Hoeve's syndrome. Laryngoscope 1970;80:544-558.<br />
Sando I, Myers D, Harada T, Hinojosa R, Myers E. Osteogenesis imperfecta tarda and otosclerosis: a temporal bone<br />
histopathology report. Ann Otol Rhinol Laryngol 1981;90:199-203.<br />
Schuknecht H. Pathology of the Ear, 2nd ed. Philadelphia: Lea & Febiger, 1993:365-414.<br />
Schwartz DT, Alpert M. The malignant transformation of fibrous dysplasia. Am J Med Sci 1964;247:1-.<br />
Spranger JW, Langer LO, Wiedemann H-R. Bone Dysplasias: An Atlas of Constitutional Disorders of Skeletal<br />
Development. Philadelphia: Saunders, 1974.<br />
Suga F, Lindsay JR. Temporal bone histopathology of osteopetrosis. Ann Otol Rhinol Laryngol 1976;85:15-29.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/2895.html (6 of 6) [5.11.2005 10:43:32]
http://www.bcm.edu/oto/grand/82092.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
OTOTOXICITY<br />
Andrew T. Lyos, MD<br />
August 20, 1992<br />
Ototoxicity is defined as the tendency of certain therapeutic agents to cause functional impairment and<br />
cellular degeneration of the inner ear and of the eighth cranial nerve. Ototoxicity may be reversible or<br />
irreversible. Ototoxicity is differentiated from neurotoxicity where the site of action is central to the<br />
eighth cranial nerve.<br />
The aminoglycosides are a class of broad-spectrum antibiotics capable of producing profound,<br />
irreversible sensorineural hearing loss (SNHL). Morphologic studies demonstrate that the inner row of<br />
outer hair cells (OHCs) of the basal turn of the cochlea are affected first, followed by the other two rows<br />
of OHCs and the inner hair cells. Prospective studies demonstrate an incidence ranging from 4% to 24%.<br />
Clinically, patients frequently develop symptoms following the cessation of therapy. SNHL is primarily<br />
http://www.bcm.edu/oto/grand/82092.html (1 of 6) [5.11.2005 10:43:38]
http://www.bcm.edu/oto/grand/82092.html<br />
high frequency and may be unilateral. Risk factors for aminoglycoside ototoxicity include: therapy<br />
lasting more than seven days, elevated serum levels, prior exposure to aminoglycosides, noise exposure,<br />
high daily dose, and use in neonates.<br />
Loop diuretics, including furosemide and ethacrynic acid, are capable of producing SNHL which is<br />
frequently reversible. The site of action is thought to be the stria vascularis, with inhibition of potassium<br />
chloride co-transport. Risk factors include renal insufficiency, use in neonates, intravenous<br />
administration, and co-administration with aminoglycosides.<br />
Cis-platinum is a relatively new cytoreductive agent used to treat a variety of malignancies. The<br />
mechanism of ototoxic action is uncertain; however, it produces a loss of OHCs in the basal turn of the<br />
cochlea in a fashion similar to the aminoglycosides. Morphological changes have not been noted in the<br />
vestibular organs. Clinical studies demonstrate an irreversible ototoxicity incidence ranging from 9% to<br />
91%, depending on the criteria used and the cumulative dose. Symptoms are frequently present at the<br />
onset of measurable hearing loss. Risk factors for ototoxicity include renal insufficiency, intravenous<br />
bolus, co-administration with aminoglycosides, and increased cumulative doses. An audiogram should be<br />
obtained at the onset of therapy, before each successive dose, and with the onset of symptoms.<br />
Salycilates have been used for more than 100 years and have long been known to produce reversible<br />
hearing loss associated with tinnitus. The mechanism of action is thought to involve vasoconstriction of<br />
capillaries in the stria vascularis. Symptoms typically resolve within 24 hours following cessation of<br />
therapy; however, cases of irreversible SNHL and tinnitus have been reported.<br />
Following a single dose in sensitive individuals or, more typically, after a prolonged course, the<br />
antimalarial agent quinine can produce the symptom complex of hearing loss, tinnitus, vertigo, nausea,<br />
and vomiting (cinchonism). Symptoms resolve following cessation of therapy. However, several cases of<br />
irreversible SNHL and tinnitus have been reported.<br />
Monitoring for ototoxicity should be individualized to the drug and to the patient. The early symptoms<br />
seen with some drugs, such as the salycilates and quinine, obviate the need for formal monitoring. The<br />
profound, irreversible effects seen with drugs such as the aminoglycosides and cis-platinum require much<br />
more formal monitoring.<br />
Case Presentation<br />
A 64-year-old man was initially referred to the Otolaryngology service for evaluation prior to initiation<br />
of aminoglycoside therapy. He had no prior otologic history, including surgery, noise exposure, or<br />
ototoxic drugs. Past medical history was significant for a right total knee replacement seven months prior<br />
to consultation. His postoperative course was complicated by wound dehiscence and osteomyelitis. He<br />
underwent removal of the hardware and debridement. Cultures grew Serratia marcescens. The Infectious<br />
http://www.bcm.edu/oto/grand/82092.html (2 of 6) [5.11.2005 10:43:38]
http://www.bcm.edu/oto/grand/82092.html<br />
Disease service was consulted and a six-week course of gentamycin was initiated.<br />
A baseline audiogram was obtained which demonstrated a mild sensitivity loss on the right with normal<br />
sensitivity on the left to 1 kHz, at which point he had a severe sensorineural loss. An audiogram<br />
performed eight days later demonstrated no change in sensitivity; however, the PB performance dropped<br />
from 95% to 76% on the right, and from 70% to 28% on the left. The patient denied symptoms of hearing<br />
loss, tinnitus, or vertigo at that time. However, he noticed progressive difficulty understanding speech<br />
during the next several days. On physical examination, the tympanic membranes were clear and there<br />
was no evidence of nystagmus.<br />
The dose of gentamycin was decreased and serum levels were monitored closely. He completed five<br />
weeks of therapy prior to discontinuation due to elevation of his blood urea nitrogen and creatinine.<br />
Serial audiograms performed weekly during the course of therapy, as well as those performed during the<br />
following five years, have failed to demonstrate any changes in sensitivity or speech understanding.<br />
Bibliography<br />
Bernard PA. Freedom from ototoxicity in aminoglycoside treated neonates: a mistaken notion. Laryngoscope<br />
1981;91:1985-1994.<br />
Bernstein J, Weiss A. Further observations on salicylate oto-toxicity. J Laryngol Otol 2967;82:915-927.<br />
Brown RD, Henley CM, Penny JE, Rupetz S. Link between functional and morphological changes in the inner ear -<br />
functional changes produced by ototoxic agents and their interaction. Arch Toxicol Suppl 1985;8:240-250.<br />
Fausti SA, Rappaport BZ, Schechter MA, Frey RH, Wart TT, Brummett RE. Detection of aminoglycoside ototoxicity by<br />
high-frequency auditory evaluation: selected case studies. Am J Otolaryngol 1984;5:177-182.<br />
Fee WE Jr. Aminoglycoside ototoxicity in the human. Laryngoscope 1980;90(Suppl 24):1-19.<br />
Fowler EP Jr, Seligman E. Otic complications of streptomycin therapy. JAMA 1947;133:87-91.<br />
Gallagher KI, Jones JK. Furosemide-induced ototoxicity. Ann Int Med 1979;91:744-745.<br />
Goycoolea MV, Paparella MM, Goldberg B, Carpenter AM. Permeability of the round window membranae in otitis media.<br />
Arch Otolaryngol 1964;206:430-433.<br />
Hart CW, Naunton RG. Ototoxicity of chloroquine phosphate. Arch Otolaryngol 1964;80:407-412.<br />
Hawkins JR Jr. Drug ototoxicity. In: Keidel WD, Neff WD, editors. Handbook of sensory physiology. Volume V, Auditory<br />
system. Berlin: Springer-Verlag, 1976:707-748.<br />
http://www.bcm.edu/oto/grand/82092.html (3 of 6) [5.11.2005 10:43:38]
http://www.bcm.edu/oto/grand/82092.html<br />
Hawkins JR Jr, Lurie MH. The ototoxicity of streptomycin. Ann Otol 1952;61:789-806.<br />
Henley CM. Postnatal developmental changes in inner ear ornithine decarboxylase (ODC). Hear Res 1991;55:45-49.<br />
Henley CM, Schacht J. Pharmacokinetics of aminoglycoside antibiotics in blood, inner ear fluids and tissues and their<br />
relationship to ototoxicity. Audiology 1988;27:136-146.<br />
Henley CM, Rybak LP. Ototoxicity in developing mammals. (Manuscript in preparation)<br />
Hinshaw HC, Feldman WH. Streptomycin in the treatment of clinical tuberculosis: a preliminary report. Proc Mayo Clin<br />
1945;20:313-318.<br />
Jackson GG, Arcieri G. Ototoxicity of gentamicin in man: a survey and controlled analysis of clinical experience in the<br />
United States. J Inf Dis 1971;124(Suppl):130-137.<br />
Johnsson LG, Hawkins JE Jr, Kingsley TC, Black FO, Matz GJ. Aminoglycoside-induced cochlear pathology in man. Acta<br />
Otolaryngol Suppl 1981;383:1-19.<br />
Kapur YP. Ototoxicity of acetylsalicylic acid. Arch Otolaryngol 1965;81:134-138.<br />
Karmody CA, Weinstein L. Reversible sensorineural hearing loss with intravenous erythromycin lactobionate. Ann Otol<br />
Rhinol Laryngol 1977;86:9-11.<br />
Koegel L Jr. Ototoxicity: a contemporary review of aminoglycosides, loop diuretics, quinine, erythromycin, and cisplatinum.<br />
Am J Otol 1985;6:190-199.<br />
Komune S, Asakuma S, Snow JB. Pathophysiology of the ototoxicity of cis-diamminedichloroplatinum. Otolaryngol Head<br />
Neck Surg 1981;89:275-282.<br />
Lenoir M, Marot M, Uziel A. Comparative ototoxicity of four aminoglycoside antibiotics during the critical period of<br />
cochlear development in the rat. Acta Otolaryngol Suppl 1983;405:1-16.<br />
Lerner SA, Matz GJ. Aminoglycoside ototoxicity. Am J Otolaryngol 1980;1:169-179.<br />
Lerner SA, Reyes MP, Cone LA et al. Randomized, controlled trial of the comparative efficacy, auditory toxicity, and<br />
nephrotoxicity of tobramycin and netilmicin. Lancet 1983;1:1123-1126.<br />
Lerner SA, Matz GH, Hawkins JE Jr. Aminoglycoside ototoxicity. Boston: Little, Brown, 1981.<br />
Lerner SA, Seligshon R, Matz GH. Comparative clinical studies of ototoxicity and nephrotoxicity of amikacin and<br />
gentamicin. Am J Med 1977;62:919-923.<br />
Lim DJ. Effects of noise and ototoxic drugs at the cellular level in the cochlea: a review. Am J Otolaryngol 1986;7:117-<br />
119.<br />
http://www.bcm.edu/oto/grand/82092.html (4 of 6) [5.11.2005 10:43:38]
http://www.bcm.edu/oto/grand/82092.html<br />
Marot M, Uziel A, Romand R. Ototoxicity of kanamycin in developing rats: relationship with the onset of auditory<br />
function. Hear Res 1990;2:111-113.<br />
Meyerhoff WL, Morizono T, Wright CG, Shaddock LC, Shea DA, Sikora MA. Tympanostomy tubes and otic drops.<br />
Laryngoscope 1983;93:1022-1027.<br />
New HC, Bendush CL. Ototoxicity of tobramycin: a clinical overview. J Inf Dis 1976;134(Suppl):5206-5218.<br />
Paloheimo JA, Thalmann R. Influence of "loop" diuretics upon Na-K-ATPase and adenylate cyclase of the stria vascularis.<br />
Arch Otorhinolaryngol 1977;217:347-359.<br />
Pujol R. Periods of sensitivity to antibiotic treatment. Acta Otolaryngol 1986;249:29-33.<br />
Reddel RR, Kefford RF, Grant JM, Coates AS, Fox RM, Tattersall MH. Ototoxicity in patients receiving cis-platin:<br />
importance of dose and method of drug administration. Cancer Treat Rep 1982;66:19-23.<br />
Rybak LP. Cis-platinum associated hearing loss. J Laryngol Otol 1981;95:745-747.<br />
Rybak LP. Drug ototoxicity. Ann Rev Pharmacol Toxicol 1986;26:79-99.<br />
Rybak LP. Pathophysiology of furosemide ototoxicity. J Otolaryngol 1982;11:127-133.<br />
Rybak LP, Whitworth C, Scott V, Weberg A. Ototoxicity of furosemide drug development. Laryngoscope 1991;101:1167-<br />
1174.<br />
Schacht J. Molecular mechanisms of drug-induced hearing loss. Hear Res 1986;22:297-304.<br />
Silverstein J, Bernstein J, Davies DG. Salicylate ototoxicity: a biochemical and electrophysiological study. Ann Otol<br />
Rhinol Laryngol 1967;76:118-128.<br />
Smith BM, Myers MG. The penetration of gentamicin and neomycin into perilymph across the round window membrane.<br />
Head Neck Surg 1979;87:888-891.<br />
Strauss M, Towfighi J, Lord S, Lipton A, Brown HA. Cis-platinum ototoxicity: clinical experience and temporal bone<br />
histopathology. Laryngoscope 1983;93:1554-1559.<br />
Stupp H, Kupper K, Lagler F et al. Inner ear concentration and ototoxicity of different antibiotics in local and systemic<br />
application. Audiology 1973;12:350-363.<br />
Tange RA, Dreschler WA, van der Hulst RJAM. The importance of high-tone audiometry in monitoring for ototoxicity.<br />
Arch Otorhinolaryngol 1985;242:77-81.<br />
Toone EC Jr, Hayden GD, Ellmann HM. Ototoxicity of chloroquine. Arthritis Rheum 1965;8:475-476.<br />
http://www.bcm.edu/oto/grand/82092.html (5 of 6) [5.11.2005 10:43:38]
http://www.bcm.edu/oto/grand/82092.html<br />
Weatherly RA, Owens JJ, Catlin FI, Mahoney DH. Cis-platinum ototoxicity in children. Laryngoscope 1991;101:917-924.<br />
Wright CG, Meyerhoff WL. Ototoxicity of otic drops applied to the middle ear in the chinchilla. Am J Otolaryngol<br />
1984;5:166-176.<br />
Wright DB, Schaefer SD. Inner ear histopathology in patients treated with cis-platinum. Laryngoscope 1982;92:1408-<br />
1413.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/82092.html (6 of 6) [5.11.2005 10:43:38]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by<br />
doctors and other health care professionals. These documents were prepared by<br />
resident physicians for presentation and discussion at a conference held at The<br />
Baylor College of Medicine in Houston, Texas. No guarantees are made with<br />
respect to accuracy or timeliness of this material. This material should not be used<br />
as a basis for treatment decisions, and is not a substitute for professional<br />
consultation and/or peer-reviewed medical literature.<br />
OTOTOXICITY<br />
April 25, 1996<br />
John S. Oghalai, M.D.<br />
Aminoglycoside ototoxicity is associated with the total daily dose, duration of<br />
treatment, previous treatment with aminoglycosides, and renal disease. The<br />
ototoxicity has a delayed onset (months to years later). Aminoglycosides enter the<br />
fluids of the inner ear via the bloodstream or via the round window with topical<br />
application. The drug is cleared more slowly from perilymph and endolymph than<br />
from serum, hence the once-daily dosing theory to reduce ototoxicity. A review of<br />
29 clinical trials (Barclay et al, 1994) found that if the same total daily dose of drug<br />
is given with a once-daily regimen as opposed to the traditional 2-4 doses/day, the<br />
efficacy of antibiotic activity was the same, but there tended to be less ototoxicity.<br />
http://www.bcm.edu/oto/grand/42596.html (1 of 6) [5.11.2005 10:43:44]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Symptoms of aminoglycoside ototoxicity include irreversible high-frequency<br />
sensorineural hearing loss, decreased otoacoustic emissions, and disequilibrium.<br />
With further toxicity, this can lead to complete deafness and/or oscillopsia. Studies<br />
of the organ of corti reveal widespread loss of outer hair cells. Potential<br />
mechanisms of toxicity include:<br />
1. Aminoglycosides binding to the cell membrane and blocking<br />
transmembrane signaling systems.<br />
2. Inhibition of the enzyme, ornithine decarboxylase, leading to decreased<br />
polyamine synthesis (Henley, 1994).<br />
3. An unknown drug metabolite may be responsible for the ototoxicity.<br />
(Schacht, 1993).<br />
Briefly stated, topical antimicrobials (particularly Cortisporin) are severely ototoxic<br />
in guinea pigs (Barlow et al, 1994). However, there is no evidence for toxicity of<br />
topical agents in humans. There has never been a controlled study that<br />
demonstrates hearing loss, and there has never even been a case report of hearing<br />
loss after treatment with a topical antimicrobial.<br />
Salicylates and NSAID's cause reversible tinnitus and hearing loss. Also decreased<br />
otoacoustic emissions have been noted. Theories of salicylate ototoxicity include:<br />
1. Vasoconstriction of vessels in stria vascularis, leading to decreased cochlear<br />
blood flow (Didier et al, 1993).<br />
2. Reversible ultrastructural changes in outer hair cells that correlate with<br />
decreased electromotility (Dieler et al, 1991).<br />
In summary, aminoglycosides cause permanent structural damage to hair cells, and<br />
lead to permanent hearing loss and disequilibrium. Salicylates cause reversible<br />
changes in hair cells or the cochlea, and lead to reversible symptoms.<br />
Case Presentation<br />
A 41-year-old female presented with complaints of high-pitched ringing in her ears<br />
for one week. She stated the sound was worse in quiet environments, and was<br />
particularly noticeable when trying to fall asleep. She had no complaints of hearing<br />
loss, aural fullness, unsteadiness, or vertiginous symptoms. She had no history of<br />
ear infections or ear surgery. Family history was negative. There was no history of<br />
autoimmune disease, skin rashes, or arthritis. The patient denied use of diuretics,<br />
intravenous antibiotics, or chemotherapy medications. She did state that she had<br />
http://www.bcm.edu/oto/grand/42596.html (2 of 6) [5.11.2005 10:43:44]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
been taking 3 aspirin tablets 3 to 4 times per day for stress headaches recently.<br />
Physical examination, including complete neuro-otologic exam, was unremarkable.<br />
A preliminary diagnosis of salicylate ototoxicity was made, and discontinuing the<br />
use of aspirin was recommended to see if her tinnitus resolved. In addition, a<br />
neurology appointment was made for evaluation of her headaches. After one week<br />
the patient returned for follow-up and stated that her tinnitus, as well as her<br />
headache, had resolved. She had no further complaints and was discharged from<br />
clinic.<br />
Bibliography<br />
Aran JM. Current perspectives on inner ear toxicity. Otolaryngol Head Neck Surg 1995;112:133-<br />
144.<br />
Aran JM, Hiel H, Hayashida T, et al. Noise, aminoglycosides, and diuretics. In: Dancer A,<br />
Henderson D, Salvi RJ, Hamemik RP, eds. Noise Induced Hearing Loss. Philadelphia: B.C.<br />
Decker, 1991:188-195.<br />
Barclay ML, Begg EJ. Aminoglycoside toxicity and relation to dose regimen. Adverse Drug<br />
Reactions & Toxicological Reviews 1994;13:207-234.<br />
Barclay ML, Begg EJ, Hickling KG. What is the evidence for once-daily aminoglycoside<br />
therapy? Clin Pharmacokinetics 1994;27:32-48.<br />
Barlow DW, Duckert LG, Kreig CS, Gates GA. Ototoxicity of topical otomicrobial agents. Acta<br />
Otolaryngol 1994;115:231-235.<br />
Barlow DW, Duckert LG, Kreig CS, Gates GA. Ototoxicity of topical otomicrobial agents. Acta<br />
Oto-Laryngologica 1995;115:231-235.<br />
Brown AM, Williams DM, Gaskill SA. The effect of aspirin on cochlear mechanical tuning. J<br />
Acoust Soc Am 1993;93:3298-3307.<br />
Brownlee RE, Hulka GF, Prazma J, Pillsbury HC, 3d. Ciprofloxacin. Use as a topical otic<br />
preparation. Arch Otolaryngol Head Neck Surg 1992;118:392-396.<br />
Didier A, Miller JM, Nuttall AL. The vascular component of sodium salicylate ototoxicity in the<br />
guinea pig. Hear Res 1993;69:199-206.<br />
Dieler R, Shehata-Dieler WE, Brownell WE. Concomitant salicylate-induced alterations of outer<br />
hair cell subsurface cisternae and electromotility. J Neurocytol 1991;20:637-653.<br />
http://www.bcm.edu/oto/grand/42596.html (3 of 6) [5.11.2005 10:43:44]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Dieler R, Shehata-Dieler WE, Richter CP, Klinke R. Effects of endolymphatic and perilymphatic<br />
application of salicylate in the pigeon. II: Fine structure of auditory hair cells. Hear Res<br />
1994;74:85-98.<br />
Duckert LG, Rubel EW. Morphological correlates of functional recovery in the chicken inner ear<br />
after gentamycin treatment. J Comp Neurol 1993;331:75-96.<br />
Ernst A, Reuter G, Zimmermann U, Zenner HP. Acute gentamicin ototoxicity in cochlear outer<br />
hair cells of the guinea pig. Brain Res 1994;636:153-156.<br />
Fitzgerald JJ, Robertson D, Johnstone BM. Effects of intra-cochlear perfusion of salicylates on<br />
cochlear microphonic and other auditory responses in the guinea pig. Hear Res 1993;67:147-156.<br />
Forge A, Li L, Corwin JT, Nevill G. Ultrastructural evidence for hair cell regeneration in the<br />
mammalian inner ear. Science 1993;259:1616-1619.<br />
Garetz SL, Altschuler RA, Schacht J. Attenuation of gentamicin ototoxicity by glutathione in the<br />
guinea pig in vivo. Hear Res 1994;77:81-87.<br />
Garetz SL, Rhee DJ, Schacht J. Sulfhydryl compounds and antioxidants inhibit cytotoxicity to<br />
outer hair cells of a gentamicin metabolite in vitro. Hear Res 1994;77:75-80.<br />
Hawkins JE. Drug Ototoxicity. In: Anonymous Handbook of Sensory Physiology, 1st ed. Berlin:<br />
Springer-Verlag, 1976:707-739.<br />
Henley CH. Kanamycin depletes cochlear polyamines in the developing rat. Otolaryngol Head<br />
Neck Surg 1994;110:103-109.<br />
Henley CM, Rybak LP. Developmental ototoxicity. Otolaryngologic Clin North Am 1993;26:857-<br />
871.<br />
Henley CM, Rybak LP. Ototoxicity in developing mammals. Brain Res 1995;20:68-90.<br />
Hiel H, Erre JP, Aurousseau C, Bouali R, Dulon D, Aran JM. Gentamicin uptake by cochlear hair<br />
cells precedes hearing impairment during chronic treatment. Audiology 1993;32:78-87.<br />
Hotz MA, Harris FP, Probst R. Otoacoustic emissions: an approach for monitoring<br />
aminoglycoside-induced ototoxicity. Laryngoscope 1994;104:1130-1134.<br />
Hutchin T, Cortopassi G. Proposed molecular and cellular mechanism for aminoglycoside<br />
ototoxicity. Antimicrobial Agents & Chemotherapy 1994;38:2517-2520.<br />
Hyde GE, Rubel EW. Mitochondrial role in hair cell survival after injury. Otolaryngol Head<br />
Neck Surg 1995;113:530-540.<br />
http://www.bcm.edu/oto/grand/42596.html (4 of 6) [5.11.2005 10:43:44]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Jung TT, Miller SK, Rozehnal S, Woo HY, Park YM, Baer W. Effect of round window<br />
membrane application of salicylate and indomethacin on hearing and levels of arachidonic acid<br />
metabolites in perilymph. Acta Otolaryngol Suppl 1992;493:81-87.<br />
Jung TT, Rhee CK, Lee CS, Park YS, Choi DC. Ototoxicity of salicylate, nonsteroidal<br />
antiinflammatory drugs, and quinine. Otolaryngologic Clin North Am 1993;26:791-810.<br />
Matz GJ. Aminoglycoside cochlear ototoxicity. Otolaryngol Clin North Am 1993;26:705-712.<br />
Meiteles LZ, Raphael Y. Scar formation in the vestibular sensory epithelium after<br />
aminoglycoside toxicity. Hear Res 1994;79:26-38.<br />
Mukhopadhyay S, Baer S, Blanshard J, Coleman M, Carswell F. Assessment of potential<br />
ototoxicity following high-dose nebulized tobramycin in patients with cystic fibrosis. J<br />
Antimicrob Chemother 1993;31:429-436.<br />
Pollice PA, Brownell WE. Characterization of the outer hair cell's lateral wall membranes. Hear<br />
Res 1993;70:187-196.<br />
Schacht J. Biochemical basis of aminoglycoside ototoxicity. Otolaryngol Clin North Am<br />
1993;26:845-856.<br />
Schuknecht HF. Pathology of the Ear,2nd ed. Philadelphia: Lea & Febiger, 1993.<br />
Shehata-Dieler WE, Richter CP, Dieler R, Klinke R. Effects of endolymphatic and perilymphatic<br />
application of salicylate in the pigeon. I: Single fiber activity and cochlear potentials. Hear Res<br />
1994;74:77-84.<br />
Spongr VP, Boettcher FA, Saunders SS, Salvi RJ. Effects of noise and salicylate on hair cell loss<br />
in the chinchilla cochlea. Arch Otolaryngol Head Neck Surg 1992;118:157-164.<br />
Tunstall MJ, Gale JE, Ashmore JF. Action of salicylate on membrane capacitance of outer hair<br />
cells from the guinea-pig cochlea. J Physiol 1995;485:739-752.<br />
Warchol ME, Lambert PR, Goldstein BJ, Forge A, Corwin JT. Regenerative proliferation in inner<br />
ear sensory epithelia from adult guinea pigs and humans. Science 1993;259:1619-1622.<br />
Weisleder P, Rubel EW. Hair cell regeneration after streptomycin toxicity in the avian vestibular<br />
epithelium. J Comp Neurol 1993;331:97-110.<br />
Wersall J. Ototoxic antibiotics: a review. Acta Otolaryngol Suppl 1995;519:26-29.<br />
http://www.bcm.edu/oto/grand/42596.html (5 of 6) [5.11.2005 10:43:44]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1995-7. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/42596.html (6 of 6) [5.11.2005 10:43:44]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by<br />
doctors and other health care professionals. These documents were prepared by<br />
resident physicians for presentation and discussion at a conference held at The<br />
Baylor College of Medicine in Houston, Texas. No guarantees are made with<br />
respect to accuracy or timeliness of this material. This material should not be used<br />
as a basis for treatment decisions, and is not a substitute for professional<br />
consultation and/or peer-reviewed medical literature.<br />
OTITIS EXTERNA<br />
October 12, 1995<br />
John S. Oghalai, MD<br />
Acute Otitis Externa is an infection of the skin of the cartilaginous portion of the<br />
ear canal. Contributing factors include moisture, canal occlusion, local trauma, and<br />
allergic disease. These factors lead to a loss of the protective wax layer, causing<br />
edema of the squamous epithelium with plugging of the glandular secretory ducts.<br />
Consequent scratching induces local trauma, allowing bacteria to invade through<br />
the skin, leading to inflammation and production of exudate.<br />
The pathogens in acute otitis externa are pseudomonas (41%), peptostreptococcus<br />
(22%), Staph. aureus (15%), and Bacteroides (11%). The differential diagnosis<br />
includes malignant external otitis, chronic external otitis, furunculosis, otomycosis,<br />
http://www.bcm.edu/oto/grand/101295.html (1 of 6) [5.11.2005 10:43:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
herpes zoster oticus, bullous external otitis, granular external otitis, chondritis,<br />
cellulitis, and eczematoid dermatitis.<br />
Malignant external otitis is a complication of acute otitis externa. The disease starts<br />
as a local infection of the external auditory canal and spreads through the fissures<br />
of Santorini (in cartilage of ear canal) towards the parotid gland and mastoid. This<br />
can lead to facial nerve paralysis. As the disease progresses, there is spread along<br />
the skull base to the jugular foramen (paralysis of CN IX, X, and XI), and finally to<br />
the hypoglossal canal (paralysis of CN XII).<br />
Symptoms are similar to acute otitis externa, however, the main difference is that<br />
the disease is not responsive to several weeks of conventional local therapy. On<br />
physical exam, there may be granulation tissue present in the ear canal, cranial<br />
nerve dysfunction, or a palpable bony defect in the anterior wall of the ear canal.<br />
Risk factors include diabetes, elderly, and immunocompromised status. The<br />
pathogen in malignant external otitis is nearly always Pseudomonas (99.2%).<br />
Relevant laboratory studies include an erythrocyte sedimentation rate (ESR) and a<br />
fasting glucose level. A bone scan is important to demonstrate osteomyelitis. It will<br />
remain positive for years after a full recovery, so it is not useful in following<br />
response to therapy. A gallium scan will demonstrate active inflammation in either<br />
soft tissue or bone, and it will return to normal if the disease is effectively treated.<br />
A CT scan is useful to determine bony erosion and soft tissue involvement,<br />
however its sensitivity for detecting osteomyelitis is low (30%).<br />
Therapy for malignant external otitis includes meticulous control of blood glucose,<br />
local debridement of granulation tissue, and possibly hyperbaric oxygen (Davis et<br />
al., 1992). Traditional antibiotic therapy is 6-8 weeks of IV drugs (usually an antipseudomonal<br />
penicillin or cephalosporin, and an aminoglycoside). Recent studies<br />
have demonstrated that oral ciprofloxacin has been 96.4% successful in treating<br />
mild to moderate malignant external otitis (Gehanno, 1994). In severe disease, IV<br />
therapy is recommended initially, and then a long course of oral ciprofloxacin is<br />
needed. Therapy is continued until the gallium scan is clear.<br />
Case Presentation<br />
A 59-year-old female was referred from the General Medicine Clinic for a 1 month<br />
history of bilateral ear pain and otorrhea. She had been treated with Cortisporin otic<br />
drops without benefit for several weeks. Her past history was unremarkable. She<br />
had no history of diabetes or immunosuppressed states. Physical exam revealed the<br />
http://www.bcm.edu/oto/grand/101295.html (2 of 6) [5.11.2005 10:43:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
left ear canal to be erythematous and tender. There was scant mucoid discharge and<br />
no granulations. The right ear canal was also erythematous, swollen, and tender.<br />
There was abundant mucoid discharge, and granulation tissue was present at the<br />
cartilaginous/bony junction posteriorly. Both tympanic membranes were normal.<br />
The rest of the exam was unremarkable. Laboratory studies revealed a slightly<br />
elevated WBC of 12.7, a greatly elevated ESR of 92, a normal random blood<br />
glucose of 100, and a slightly elevated glycosylated Hgb of 7.4.<br />
The patient was admitted to the hospital with the diagnosis of malignant external<br />
otitis. Her ears were debrided and cultures were sent, which eventually grew<br />
Pseudomonas aeruginosa. A CT scan done on admission showed soft tissue<br />
thickening around the ear canals, but was otherwise normal. A technetium bone<br />
scan was negative, and a gallium scan was positive for bilateral temporal<br />
inflammation. The patient was placed on ceftazidime and gentamicin otic drops.<br />
Her ear canals were regularly debrided. Twice daily blood glucose checks during<br />
hospitalization were all normal. After 10 days, her ear canals had no granulation<br />
tissue or discharge, and she was discharged to home on ciprofloxacin. In follow-up,<br />
she has been seen in at 2 weeks and 4 weeks post-discharge and has a normal<br />
exam. She is still taking ciprofloxacin.<br />
Bibliography<br />
Agius AM, Reid AP, Hamilton C. Patient compliance with short-term topical aural antibiotic<br />
therapy. Clin Otolaryngol 1994;19:138-141.<br />
Barrow HN, Levenson MJ. Necrotizing 'malignant' external otitis caused by Staphylococcus<br />
epidermidis. Arch Otolaryngol Head Neck Surg 1992;118:94-96.<br />
Benecke JE Jr. Management of osteomyelitis of the skull base. Laryngoscope 1989;99:1220-<br />
1223.<br />
Brody T, Pensak ML. The fluoroquinolones. Am J Otol 1991;12:477-479.<br />
Brook I, Coolbaugh JC. Changes in the bacterial flora of the external ear canal from the wearing<br />
of occlusive equipment. Laryngoscope 1984;94:963-965.<br />
Brook I, Frazier EH, Thompson DH. Aerobic and anaerobic microbiology of external otitis. Clin<br />
Infect Dis 1992;15:955-958.<br />
Chandler JR. Malignant external otitis and osteomyelitis of the base of the skull. Am J Otol.<br />
1909;10:108-110.<br />
http://www.bcm.edu/oto/grand/101295.html (3 of 6) [5.11.2005 10:43:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Cohen D, Friedman P. The diagnostic criteria of malignant external otitis. J Laryngol Otol<br />
1987;101:216-221.<br />
Cohen D, Friedman P, Eilon A. Malignant external otitis versus acute external otitis. J Laryngol<br />
Otol 1987;101:211-215.<br />
Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Schuller DE. Otolaryngology - Head<br />
and Neck Surgery. St Louis: Mosby, 1993.<br />
Davis JC, Gates GA, Lerner C, Davis MG Jr, Mader JT, Dinesman A. Adjuvant hyperbaric<br />
oxygen in malignant external otitis. Arch Otolaryngol Head Neck Surg 1992;118:89-93.<br />
Dekker PJ. Alternative method of application of topical preparations in otitis externa. J Laryngol<br />
Otol 191;105:842-843.<br />
Dingle AF. Fistula between the external auditory canal and the temporomandibular joint: a rare<br />
complication of otitis externa. J Laryngol Otol 1992;106:994-995.<br />
Driscoll PV, Ramachandrula A, Drezner DA, Hicks TA, Schaffer SR. Characteristics of cerumen<br />
in diabetic patients: a key to understanding malignant external otitis? Otolaryngol Head Neck<br />
Surg 1993;109:676-679.<br />
el-Silimy O, Sharnuby M. Malignant external otitis: management policy. J Laryngol Otol<br />
1992;106:5-6.<br />
Farrior J. Osteomyelitis of the skull base. South Med J 1989;82:719-722.<br />
Gehanno P. Ciprofloxacin in the treatment of malignant external otitis. Chemotherapy<br />
1994;40(Suppl 1):35-40.<br />
Gherini SG, Brackmann DE, Bradley WG. Magnetic resonance imaging and computerized<br />
tomography in malignant external otitis. Laryngoscope 1986;96:542-548.<br />
Giamarellou H. Malignant otitis externa: the therapeutic evolution of a lethal infection J<br />
Antimicrob Chemother 1992;30:745-751.<br />
Gordon G, Giddings NA. Invasive otitis externa due to Aspergillus species: case report and<br />
review. Clin Infect Dis 1994;19:866-870.<br />
Guy RL, Wylie E, Hickey A, Tonge KA. Computed tomography in malignant external otitis. Clin<br />
Radiol 1991;43:166-170.<br />
Hickey SA, Ford GR, O'Connor AF, Eykyn SJ. Sonksen PH. Treating malignant otitis with oral<br />
ciprofloxacin. BMJ 1989;299:550-551.<br />
http://www.bcm.edu/oto/grand/101295.html (4 of 6) [5.11.2005 10:43:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Hirsch BE. Infections of the external ear. Am J Otolaryngol 1992;13:154-155.<br />
Hunsaker DH. Conchomeatoplasty for chronic otitis externa. Arch Otolaryngol Head Neck Surg<br />
1988;114:395-398.<br />
Koriwchak M. Temporal bone cancer. Am J Otol 1993;14:623-626.<br />
Kraus DH, Rehm SJ, Kinney SE. The evolving treatment of necrotizing external otitis.<br />
Laryngoscope 1988;98:934-939.<br />
Levenson MJ, Parisier SC, Dolitsky J, Bindra G. Ciprofloxacin: drug of choice in the treatment<br />
of malignant external otitis (MEO). Laryngoscope 1991;101:821-824.<br />
Lucente FE. Fungal infections of the external ear. Otolaryngol Clin North Am 1993;26:995-1006.<br />
Lucente FE, Parisier SC, Som PM. Complications of the treatment of malignant external otitis<br />
Laryngoscope 1983;93:279-281.<br />
Martin-Hirsch DP, Smelt GJ. Conchal flap meatoplasty. J Laryngol Otol 1993;107:1029-1031.<br />
Murray ME, Britton J. Osteomyelitis of the skull base: the role of high resolution CT in<br />
diagnosis. Clin Radiol 1994;49:408-411.<br />
Ostfeld EJ, Kupferberg A. Biocompatible implantable antimicrobial release for necrotizing<br />
external otitis. J Laryngol Otol 1991;105:252-256.<br />
Raza SA, Denholm SW, Wong JC. An audit of the management of acute otitis externa in an ENT<br />
casualty clinic. J Laryngol Otol 1995;109:130-133.<br />
Rubin J, Curtin HD, Yu VL, Kamerer DB. Malignant external otitis: utility of CT in diagnosis<br />
and follow-up. Radiology 1990;174:391-394.<br />
Rubin J, Yu VL. Malignant external otitis: insights into pathogenesis, clinical manifestations,<br />
diagnosis, and therapy. Am J Med 1988;85:391-398.<br />
Rubin J, Yu VL, Kamerer DB, Wagener M. Aural irrigation with water: a potential pathogenic<br />
mechanism for inducing malignant external otitis? Ann Otol Rhinol Laryngol 1990;99:117-119.<br />
Russell JD, Donnelly M, McShane DP, Alun-Jones T, Walsh M. What causes acute otitis<br />
externa? J Laryngol Otol 1993;107:898-901.<br />
Senturia BH, Marcus MD, Lucente FE. Diseases of the External Ear. New York: Grune and<br />
Stratton, 1980.<br />
Shpitzer T, Stern Y, Cohen O, Levy R, Segal K, Feinmesser R. Malignant external otitis in<br />
http://www.bcm.edu/oto/grand/101295.html (5 of 6) [5.11.2005 10:43:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
nondiabetic patients. Ann Otol Rhinol Laryngol 1993;102:870-872.<br />
Strashun AM, Nejatheim M, Goldsmith SJ. Malignant external otitis: early scintigraphic<br />
detection Radiology 1984;150:541-545.<br />
Strauss M. Current therapy of malignant external otitis. Otolaryngol Head Neck Surg<br />
1990;102:174-176.<br />
Swartz JD, Harnsberger HR. Imaging of the Temporal Bone. New York: Thieme Medical, 1992.<br />
Uri N, Gips S, Front A, Meyer SW, Hardoff R. Quantitative bone and 67Ga scintigraphy in the<br />
differentiation of necrotizing external otitis from severe external otitis. Arch Otolaryngol Head<br />
Neck Surg 1991;117:623-626.<br />
Weinroth SE, Schessel D, Tuazon CU. Malignant otitis externa in AIDS patients: case report and<br />
review of the literature. Ear Nose Throat J 1994;73:772-778.<br />
Wilde AD, England J, Jones AS. An alternative to regular dressings for otitis externa and chronic<br />
supperative otitis media? J Laryngol Otol 1995;109:101-103.<br />
Wormald PJ. Surgical management of benign necrotizing otitis externa. J Laryngol Otol<br />
1994;108:101-105.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1995-7. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/101295.html (6 of 6) [5.11.2005 10:43:50]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
Pathology<br />
PATHOLOGY AND PATHOGENESIS OF OTITIS MEDIA<br />
April 21, 1994<br />
Philip A. Matorin, M.D.<br />
Understanding the pathology and pathogenesis of otitis media (OM) is important in predicting the<br />
prognosis and sequelae of the disease. In this way treatment can be tailored to individual needs.<br />
There have been several attempts to gain a consensus definition of OM. In 1980, the Ad Hoc Committee<br />
on the Classification of Otitis Media defined OM based on the temporal sequence: Acute < 3 weeks;<br />
Subacute 4-8 weeks; Chronic >9 weeks. In 1989, the Task Force of the 4th International Symposium on<br />
Otitis Media published a working classification. Acute Suppurative OM refers to an identifiable infection<br />
of the middle ear of short duration and sudden onset. Secretory OM refers to the presence of a middle ear<br />
http://www.bcm.edu/oto/grand/42194.html (1 of 6) [5.11.2005 10:44:00]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
effusion without acute signs or symptoms. Chronic Suppurative OM refers to a chronic middle ear<br />
discharge through a perforated tympanic membrane.<br />
Much of our understanding of the pathology of OM comes from experimental animal models and from<br />
temporal bone preparations. After Eustachian tube obstruction in the cat and chinchilla, edema<br />
hyperemia, subepithelial hemorrhage with PMN infiltration are noted, modeling acute Suppurative OM.<br />
In addition mucoperiosteal thickening and osteitis can be seen. Mild metaplasia from squamous to<br />
cuboidal epithelium is noted.<br />
Continued Eustachian tube obstruction models secretory OM. Early transudation of serum into the<br />
subepithelial space is seen within 18-24 hours. More metaplasia is seen with increased numbers of<br />
pseudostratified, ciliated columnar epithelial cells, and goblet cells. Resorption of water is thought to<br />
promote thickening of the effusion converting thin serous fluid into a thick mucoid effusion. In temporal<br />
bone preparations, thickening and fibrosis of the tensor tympanic is seen. This is felt to be important in<br />
the development of spasm and contracture of the muscle resulting in retraction and fixation of the<br />
tympanic membrane.<br />
In chronic OM models, columnar metaplasia is greatest. fibroblastic density is increased. A lymphoid<br />
infiltrate is noted with polypoid changes present in the mucosa. Osteitis and osteoneogenesis are also<br />
commonly noted. Friable immature granulation tissue with neovascularization and fibroblastic<br />
proliferation is seen. Mature granulation with subepithelial fibrosis and decreased vascularity are found<br />
in long standing disease. The sequelae of COM including tympanosclerosis, cholesterol granuloma, and<br />
cholesteatoma can also be encountered.<br />
Paparella's group has proposed that OM exists as a continuum of mucoperiosteal disease. Epidemiologic<br />
evidence comes from studies showing the overlap and progression of disease from acute suppurative OM<br />
to secretory OM or chronic OM. One out of 5 cases of Acute OM is superimposed on a chronic mucoid<br />
OM. Temporal bone histology also demonstrates the continuum of mucosal disease. Lastly, experimental<br />
animal models of Eustachian tube obstruction followed longitudinally have demonstrated the gradual<br />
change from suppurative, to secretary, to chronic histopathology.<br />
Pathogenesis<br />
Since the time of Politzer, the Eustachian tube has been identified as central to the pathogenesis of OM.<br />
For OM to occur, three conditions must be met. Bacteria must adhere to the nasopharyngeal mucosa. The<br />
bacteria must the enter the Eustachian tube and finally, the bacteria must be able to multiply in the<br />
middle ear environment.<br />
Pathogenic bacteria bind to cell surface receptors in a highly specific fashion. The adhesin receptor<br />
binding mechanism prevents colonizing bacteria from being swept away by the mechanical cleansing<br />
action in the nasopharynx. Adhesion through a receptor mechanism is suggested by the fact that<br />
adherence can be saturated by an increase in bacterial concentration. In general, the more adherent an<br />
http://www.bcm.edu/oto/grand/42194.html (2 of 6) [5.11.2005 10:44:00]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
organism is to the nasopharyngeal mucosa, the more likely it will be a successful pathogen. In children,<br />
the adenoid bed is an important source of pathogenic bacteria. In addition, Influenza A can cause<br />
destruction of the normal tubal mucosa promoting bacterial entry. One study showed a 5-fold increase in<br />
the rate of pneumococcal OM in chinchillas infected with the virus.<br />
The Eustachian tube itself is cartilaginous in its lower 2/3 portion. It is normally in the closed position.<br />
The main dialator of the tube is the tensor veli palatini innervated by the mandibular division of the<br />
trigeminal nerve. Comparing the infant to the adult tube, the Eustachian tube is shorter (13mm vs 31-<br />
38mm), shallower (10 deg. vs 45 deg from horizontal), and has abundant goblet cells. These anatomic<br />
features make the pediatric Eustachian tube much more likely to become dysfunctional.<br />
Eustachian tube function can be divided into ventilation, drainage, and protection from nasopharyngeal<br />
secretions. Bluestone has described 4 functional abnormalities radiographically by instilling contrast<br />
material into the nasopharynx. The abnormalities include retrograde obstruction, abnormal distensibility,<br />
middle ear reflux, and retrograde obstruction with abnormal distensibility. The patulous Eustachian tube<br />
predisposes to middle ear reflux. The abnormally compliant Eustachian tube could result in middle ear<br />
reflux with slight increases in nasopharyngeal pressure. On the other hand, rapid changes in pressure<br />
could cause locking of the tube and functional obstruction.<br />
The ventilatory function of the Eustachian tube is also affected by the gaseous equilibrium of the middle<br />
ear space. Large rapid changes can occur because the middle ear space is a relatively small pocket of gas<br />
surrounded by vascular mucosa. Gas is exchanged between the middle ear cavity and the mucosa. Recent<br />
evidence suggests that the diffusion gradient is due to the nitrogen partial pressure gradient.<br />
Anatomically, neoplasms, cleft palate, and large adenoids can cause obstruction of the Eustachian tube.<br />
In children, it appears that adenoid size does not correlate with the incidence of OM. Adenoids act as a<br />
source of pathogenic bacteria rather than anatomic obstruction in the pathogenesis of OM.<br />
The final stage in the development of OM is bacterial replication in the middle ear space. Therefore, the<br />
immunology of OM has generated great interest. In human studies, IgG is the predominant<br />
immunoglobulin involved. Several clinical series have shown lower levels of IgG2 in otitis prone<br />
children. These children have greater susceptibility to non-typeable H.Flu. Higher levels of interleukin-1<br />
have been found in both younger children and those with cleft palate with Eustachian tube dysfunction<br />
and OM. Increased levels of specific hydrolase activity and higher levels of lipoxygenase products have<br />
also been found in otitis media effusions.<br />
Case Presentation<br />
An 11-month-old full term white male child presented with a history of otitis media for the past 5<br />
months. He completed six courses of several different antibiotics without resolution. Physical exam<br />
http://www.bcm.edu/oto/grand/42194.html (3 of 6) [5.11.2005 10:44:00]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
showed dull, slightly retracted tympanic membranes and no other abnormalities. Visual reinforcement<br />
audiometry showed normal sensitivity for age. Acoustic immittance measurements showed type C<br />
tympanograms. In view of the persistence of the effusion, the patient underwent bilateral myringotomy<br />
and placement of pressure equalization tubes. Thin viscous fluid was aspirated from both middle ear<br />
cavities. One month postoperative assessment revealed that the child was doing fine with well-placed,<br />
patent PE tubes.<br />
Bibliography<br />
Beachey EH, Courtney SH. Bacterial adherence: attachment of group A streptococci to mucosal surfaces. In: Lim DJ, ed.<br />
Proceedings of the Fourth International Symposium Recent Advances in Otitis Media, June 1-4, 1987, Bal Harbour,<br />
Florida. Toronto: B.C. Decker, 1988:291-296.<br />
Bernstein JM. Immunologic reactivity in the middle ear in otitis media with effusion. Otolaryngol Clin North Am<br />
1991;24:845-858.<br />
Biegink GS, Ripley-Petzoldt ML, Juhn SK, Aeppli D, Tomasz A, Tuomanen E. Contribution of pneumococcal cell wall to<br />
experimental otitis media pathogenesis. Ann Otol Rhinol Laryngol 1988;97:28-30.<br />
Bluestone CD, Paradise JL, Beery QC. Physiology of the eustachian tube in the pathogenesis and management of middle<br />
ear effusion. Laryngoscope 1972;82:1654-1670.<br />
Bluestone CD, Rood SR, Swarts JD. Anatomy and physiology of the eustachian tube. In: Cummings, DW, Harker LA, eds.<br />
Otolaryngology -Head and Neck Surgery, Volume 4, 2nd ed. St. Louis: Mosby, 1993:2548-2565.<br />
Cantekin EI, Casselbrant ML, Doyle WJ, Brostoff LM. Eustachian tube function: prospective study of eustachian tube<br />
function and otitis media. In: Lim DJ, ed. Proceedings of the Fourth International Symposium Recent Advances in Otitis<br />
Media, June 1-4, 1987, Bal Harbour, Florida. Toronto: B.C. Decker, 1988:58-60.<br />
Collins ME, Coker NJ, Igarashi M. Inflammatory disease of the anterior epitympanum. Am J Otol 1991;12:11-15.<br />
Diven WF, Doyle WJ, Vietmeier B. Hydrolytic enzymes in otitis media pathogenesis. Ann Otol Rhinol Laryngol<br />
1988;97:6-9.<br />
Diven WF, Doyle WJ, Vietmeier BN. Studies in otitis media, Pittsburgh Otitis Media Research Center. Progress report<br />
1988: Hydrolase activity in experimental middle ear effusion. Ann Otol Rhinol Laryngol Suppl 1988;133:26-27.<br />
Diven WF, LaMarco KL, Doyle WJ, Glew RH. Studies in otitis media, Pittsburgh Otitis Media Research Center. Progress<br />
report 1988: Role of bacterial hydrolases in the pathologic changes caused by otitis media. Ann Otol Rhinol Laryngol<br />
Suppl 1988;133:23-24.<br />
Diven WF, Scanlon KL, Glew RH. Studies in otitis media, Pittsburgh Otitis Media Research Center. Progress report 1988:<br />
http://www.bcm.edu/oto/grand/42194.html (4 of 6) [5.11.2005 10:44:00]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Purification and properties of a neuraminidase from streptococcus pneumoniae culture filtrates. Ann Otol Rhinol Laryngol<br />
Suppl 1988;133:24-25.<br />
Diven WF, Vietmeier BN. Studies in otitis media, Pittsburgh Otitis Media Research Center. Progress report 1988: Isolation<br />
and characterization of chinchilla a1-antitrypsin. Ann Otol Rhinol Laryngol Suppl 1988;133:24.<br />
Gates GA, Muntz HR, Gaylis B. Adenoidectomy and otitis media. Ann Otol Rhinol Laryngol Suppl 1992;155:24-32.<br />
Giebink GS. Otitis media update: pathogenesis and treatment. Ann Otol Rhinol Laryngol 1992;101:21-23.<br />
Goycoolea MV, Buah DB, Bequer N. General surgical approach based on pathogenesis: an overall approach. Otolaryngol<br />
Clin North Am 1991;24:957-966.<br />
Goycoolea MV, Hueb MM, Ruah C. Definitions and terminology. Otolaryngol Clin North Am 1991;24:757-761.<br />
Goycoolea MV, Nuchow DC, Goycoolea HG. Otitis media: 16 years of pathogenesis approach. Otolaryngol Clin North<br />
Am 1991;24:967-980.<br />
Hellström S, Goldie P. Mechanisms of otitis medial development: involvement of neurogenic inflammation. Otolaryngol<br />
Clin North Am 1991;24:829-834.<br />
Johnson MD, Fitzgerald JE, Leonard G, Burleson JA, Dreutzer DL. Cytokines in experimental otitis media with effusion.<br />
Laryngoscope 1994:104:191-196.<br />
Juhn SK, Tolan CJ, Antonelli PJ, Giebink GS, Goycoolea MV. The significance of experimental animal studies in otitis<br />
media. Otolaryngol Clin North Am 1991;24:813-827.<br />
Jung TT. Arachidonic acid metabolites in otitis media pathogenesis. Ann Otol Rhinol Laryngol 1988;97:14-17.<br />
Jung TT, Park YM, Schlund D, Weeks D, Miller S, Wong O, et al. Effect of prostaglandin, leukotriene,m and arachidonic<br />
acid on experimental otitis media with effusion in chinchillas. Ann Otol Rhinol Laryngol 1990;99:28-32.<br />
Kenna MA. Etiology and pathogenesis of chronic suppurative otitis media. Ann Otol Rhinol Laryngol Suppl 1988;131:16-<br />
24.<br />
Klein JO, Naunton RF, Tos M, Ohyama M, Hussl B, van Cauwenberge PB. Recent advances in otitis media: definition and<br />
classification. Ann Otol Rhinol Laryngol Suppl 1989;139:10.<br />
Lim DJ, Demaria TF, Bakaletz LO. Current concepts of pathogenesis of otitis media: a review. Acta Otolaryngol Suppl<br />
1988;458:174-180.<br />
Meyerhoff WL, Biegink GS. Pathology and microbiology of otitis media. Laryngoscope 1982;92:273-277.<br />
Meyerhoff WL, Shea DA, Giebink GS. Experimental pneumococcal otitis media: a histopathologic study. Otolaryngol<br />
Head Neck Surg 1980;88:606-612.<br />
http://www.bcm.edu/oto/grand/42194.html (5 of 6) [5.11.2005 10:44:00]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Morizono T, Tono T. Middle ear inflammatory mediators and cochlear function. Otolaryngol Clin North Am 1991;24:824-<br />
852.<br />
Paparella MM, Schachern PA, Yoon TH, Abdelhammid MM, Sahni R, da Costa SS. Otopathologic correlates of the<br />
continuum of otitis media. Ann Otol Rhinol Laryngol 1990;99:17-22.<br />
Senturia BH, Paparella MM, Lowery HN, Klein JO, Arnold WJ, Lim DJ, et al. Report of Research Conference. Recent<br />
Advances in Otitis Media with Effusion: Modified report of the ad hoc committee on definition and classification of otitis<br />
media. Ann Otol Rhinol Laryngol Suppl 1980;69:6.<br />
Sando I, Takahashi H. Otitis media in association with various congenital diseases: preliminary study. Ann Otol Rhinol<br />
Laryngol 1990;99:13-16.<br />
Schachern P, Paparella MM, Sano S, Lamey S, Guo Y. A histopathological study of the relationship between otitis media<br />
and mastoiditis. Laryngoscope 1991;101:1050-1055.<br />
Schuknecht H. Pathology of the Ear, 2nd ed. Philadelphia: Lea and Febiger, 1993.<br />
Weir N. Otolaryngology: An Illustrated History. London: Butterworths, 1990: 14, 18, 42, 81, 206, 211-212, 218.<br />
Yoon TH, Paparella MM, Schachern PA, Lindgren BR. Morphometric studies of the continuum of otitis media. Ann Otol<br />
Rhinol Laryngol 1990;99:23-27.<br />
Yoon TH, Schachern PA, Paparella MM, Aeppli DM. Pathology and pathogenesis of tympanic membrane retraction. Am J<br />
Otol 1990;11:10-17.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/42194.html (6 of 6) [5.11.2005 10:44:00]
http://www.bcm.edu/oto/grand/102193.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
THE DIAGNOSIS AND MANAGEMENT OF PERILYMPHATIC<br />
FISTULAS<br />
Troy A. Callender, MD<br />
October 21, 1993<br />
A perilymphatic fistula is an abnormal communication between the inner ear fluids and the middle ear.<br />
Perilymphatic fistulas can be classified into four broad categories: iatrogenic, traumatic, spontaneous, and<br />
congenital. Symptoms of perilymphatic fistula are variable and include sensorineural hearing loss,<br />
vertigo, dysequilibrium, unsteadiness, motion intolerance, tinnitus and aural fullness. Simmons in 1968<br />
first postulated that sensorineural hearing loss could result from intracochlear membrane breaks. In 1971<br />
Goodhill stated that the labyrinth is hydrostatically loaded with intimate relations to hydrodynamic forces<br />
in the carotid arterial system, intracranial venous-sinus systems and the CSF pressure gradients in the<br />
subarachnoid space. He proposed that the membranous labyrinth could be ruptured by an explosive route<br />
via the external auditory canal and eustachian tube and concluded that membrane ruptures could occur<br />
http://www.bcm.edu/oto/grand/102193.html (1 of 7) [5.11.2005 10:44:09]
http://www.bcm.edu/oto/grand/102193.html<br />
throughout the membranous labyrinth with both acoustic and/or vestibular system sequelae. Simmons<br />
later expounded on his original theory and proposed the "double membrane break theory" in the<br />
development of sensorineural hearing loss. In this theory he postulated that the second membrane break<br />
was the result of a pressure gradient created by the first break, profound sensorineural hearing loss<br />
resulted from the mixing of perilymph and endolymph, healing of intracochlear breaks halts the mixing of<br />
fluid and the widespread hearing loss disappears resulting in hearing loss at the specific site where local<br />
tissue damage occurred along the membrane.<br />
The diagnosis of perilymphatic fistula is very difficult to make since there is no diagnostic test for this<br />
disorder. The diagnosis depends upon a high degree of clinical suspicion and ruling out other possible<br />
causes for the symptoms. In addition to the hearing loss, vestibular dysfunction, tinnitus and aural<br />
fullness, patients may also have recruitment, the Tullio phenomenon and a positive fistula test. Evaluation<br />
of these patients should include a careful history and physical examination, audiogram,<br />
electronystagmography, fistula test, imaging to rule out an intracranial tumor and exclusion of other<br />
possible causes for the symptoms (i.e., autoimmune diseases, vascular diseases, infectious diseases and<br />
endolymphatic hydrops).<br />
The treatment of suspected perilymphatic fistulas is controversial as are most aspects of this disorder and<br />
consists of conservative medical therapy or surgical exploration and closure of the fistula. Medical<br />
therapy consists of strict bed rest, head elevation, and refraining from all strenuous activity. Some authors<br />
advocate this treatment for all cases of suspected perilymphatic fistula if the patient presents early in the<br />
course of the disease, whereas others use it to treat patients with symptoms consistent with a<br />
perilymphatic fistula but no antecedent history of trauma or surgery. After 5 to 7 days, the patients are reevaluated<br />
and if symptoms persist, surgical exploration is undertaken. Surgical treatment consists of a<br />
middle ear exploration and careful examination of the oval and round window niches, looking for crystal<br />
clear fluid that persistently wells up after careful suctioning. Special maneuvers such as trendelenburg,<br />
internal jugular vein compression and valsalva may be required to adequately visualize a fistula. In<br />
addition to fistulas of the oval and round windows, fistulas can also develop from microfissures around<br />
the oval and round windows as well as from Hyrtl's fissure and the fissula ante fenestram. Most authors<br />
agree that whether a fistula is found or not, a tissue seal with fat, fascia, perichondrium or loose areolar<br />
tissue should be made around both the oval and round windows since there is a possibility that the fistula<br />
is only intermittently patent or is too small to be visualized. Some authors feel that surgery as an initial<br />
form of therapy is indicated in all patients with symptoms for greater than one month, whereas others<br />
would proceed only if there is a clear antecedent history of trauma or surgery associated with the typical<br />
symptoms of perilymphatic fistula. There are several large studies reporting the results of surgical<br />
treatment of perilymphatic fistulas. The percentage of patients with fistulas found surgically ranges from<br />
24% to 93%. Vestibular symptoms had the best response to surgical treatment, with 60% to 90% of cases<br />
improving. Hearing loss responded much less favorably except in fluctuating or progressive sensorineural<br />
hearing loss in which case surgery would often stabilize or slightly improve the hearing. Postoperative<br />
management consists of bed rest, head elevation and no straining for the first 5 days, followed by 4 to 6<br />
weeks of light, non-strenuous activity. The objective assessment of treatment results awaits the<br />
development of an objective test for diagnosing perilymphatic fistulas.<br />
http://www.bcm.edu/oto/grand/102193.html (2 of 7) [5.11.2005 10:44:09]
http://www.bcm.edu/oto/grand/102193.html<br />
Case Presentation<br />
A 59-year-old white man presented to the VAMC Otolaryngology Clinic 4 days after he developed<br />
sudden right hearing loss. The hearing loss developed shortly after he sneezed and was associated with a<br />
headache. He denied vestibular symptoms, otalgia, fever or a history of otologic surgery. His past medical<br />
history was unremarkable except for left hearing loss of probable sudden onset in 1976 for which he was<br />
extensively evaluated while in the Navy. Physical examination was unremarkable and significant<br />
laboratory findings included a ESR of 3 mm/hr, rheumatoid factor < 30, negative ANA, nonreactive RPR<br />
and mildly elevated liver function tests. Audiogram obtained on admission revealed a profound SNHL on<br />
the left with no word discrimination and moderate to severe mixed hearing loss on the right with 35%<br />
word discrimination. Tympanograms were type A.<br />
The patient was admitted to the VAMC hospital for bed rest and treated with carbogen, intravenous<br />
steroids and diuretics. MRI scan of the brain, posturography, and fistula test were all negative. Because<br />
the patient's history was suggestive for a perilymphatic fistula, exploratory tympanotomy was performed<br />
on the second hospital day. At surgery, clear fluid was noted to collect around the oval window niche<br />
consistent with a perilymphatic fistula. Both windows were sealed with loose areolar tissue and the<br />
patient recovered unremarkably. A repeat audiogram obtained 2 months after surgery revealed a 10 dB<br />
improvement in the PTA and a 10% improvement in speech discrimination score on the right side.<br />
Bibliography<br />
Allen GW. Fluid flow in the cochlear aqueduct and cochlea - hydrodynamic considerations in perilymph fistula, stapes<br />
gusher, and secondary endolymphatic hydrops. Am J Otol 1987;8:319-322.<br />
Althaus SR. Perilymph fistulas. Laryngoscope 1981;91:538-562.<br />
Althaus SR, House HP. Long-term results of perilymph fistula repair. Laryngoscope 1973;83:1502-1509.<br />
Althaus SR. Spontaneous and traumatic perilymph fistulas. Laryngoscope 1977;87:364-371.<br />
Bassiouny B, Hirsch BE, Kelly RH, Kamerer DB, Cass SP. Beta2 transferrin application in otology. Am J Otol<br />
1992;13:552-555.<br />
Black FO, Lilly DJ, Nashner LM, Peterka RJ, Pesznecker SL. Quantitative diagnostic test for perilymph fistulas.<br />
Otolaryngol Head Neck Surg 1987;96:125-134.<br />
Black FO, Pesznecker S, Norton T, Fowler L, Lilly DJ, Shupert C, Hemenway WG, et al. Surgical management of<br />
http://www.bcm.edu/oto/grand/102193.html (3 of 7) [5.11.2005 10:44:09]
http://www.bcm.edu/oto/grand/102193.html<br />
perilymphatic fistulas: a Portland experience. Am J Otol 1992;13:254-262.<br />
Böhmer A. On the pathomechanism of cochlear dysfunction in experimental perilymph fistulas. Laryngoscope<br />
1991;191:1307-1312.<br />
Bojrab DI, Shansali SA. Fluorescein use in the detection of perilymphatic fistula: a study in cats. Otolaryngol Head Neck<br />
Surg 1993;103:348-355.<br />
Campbell KC, Savage MM. Electrocochleographic recordings in acute and healed peilymphatic fistula. Arch Otolaryngol<br />
Head Neck Surg 1992;118:301-304.<br />
Daspit CP, Churchill D, Linthicum FH Jr. Diagnosis of perilymph fistula using ENG and impedance. Laryngoscope<br />
1980;90:217-223.<br />
Davis RE. Diagnosis and management of perilymph fistula: the University of North Carolina approach. Am J Otol<br />
1992;13:85-89.<br />
Fee GA. Traumatic perilymphatic fistulas. Arch Otolaryngol 1968;88:477-480.<br />
Flint P, Duckert LG, Dobie RA, Rubel EW. Chronic perilymphatic fistula: experimental model in the guinea pig.<br />
Otolaryngol Head Neck Surg 1988;99:380-388,<br />
Flood LM, Fraser JG, Hazell WP, Rothera MP. Perilymph fistula: four year experience with a new audiometric test. J<br />
Laryngol Otol 1985;99:671-676.<br />
Glasscock ME III, McKennan KX, Levine SC. Persistent traumatic perilymph fistulas. Laryngoscope 1987;97:860-864.<br />
Glasscock ME III, Hart MJ, Rosdeutscher JD, Bhansali SA. Traumatic perilymphatic fistula: how long can symptoms<br />
presist? A follow-up report. Am J Otol 1992;13:333-338.<br />
Glasscock ME III. The stapes gusher. Arch Otolaryngol 1973;98:82-91.<br />
Goodhill V. Leaking labyrinth lesions, deafness, tinnitus and dizziness. Ann Otol Rhinol Layrngol 1981;90:99-106.<br />
Goodhill V. Sudden deafness and round window rupture. Laryngoscope 1971;81:1462-1474.<br />
Goodhill V. The conductive loss phenomenon in post-stapedectomy perilymphatic fistulas. Laryngoscope 1967;77:1179-<br />
1190.<br />
Goodhill V. Traumatic fistulae. J Laryngol Otol 1980;94:123-128.<br />
Grundfast KM, Bluestone CD. Sudden or fluctuating hearing loss and vertigo in children due to perilymph fistula. Ann Otol<br />
Rhinol Laryngol 1978;87:761-771.<br />
Harris I. Sudden hearing loss: membrane rupture. Am J Otol 1984;6:484-487.<br />
http://www.bcm.edu/oto/grand/102193.html (4 of 7) [5.11.2005 10:44:09]
http://www.bcm.edu/oto/grand/102193.html<br />
Harrison WH, Shambaugh GE, Derlacki EL, Clemis JD. Perilymph fistula in stapes surgery. Laryngoscope 1967;77:836-<br />
849.<br />
Hazell JW, Fraser JG, Robinson PJ. Positional audiometry in the diagnosis of perilymphatic fistula. Am J Otol 1992;13:263-<br />
269.<br />
House HP. The fistula problem in otosclerosis surgery. Laryngoscope 1967;77:1410-1426.<br />
Hughes GB, Sismanis A. Is there consensus in perilymph fistula management? Otolaryngol Head Neck Surg 1990;102:111-<br />
117.<br />
Jackler RK, Hwang PH. Enlargement of the cochlear aqueduct: fact or fiction? Otolaryngol Head Neck Surg 1993;109:14-<br />
25.<br />
Kamerer DB, Sando I, Hirsch B, Takagi A. Perilymph fistula resulting from microfissures. Am J Otol 1987;8:489-494.<br />
Kaseki Y, Nakashima T, Fukuta S, Suzuki T, Yanagit N. Effects of persistent perilymph fistula on the inner ear.<br />
Laryngoscope 1991;101:1085-1090.<br />
Kohut RI, Hinojosa R, Budetti JA. Perilymphatic fistula: a histopathologic study. Ann Otol Rhinol Laryngol 1986;95:466-<br />
471.<br />
Kohut RI. Perilymph fistulas: clinical criteria. Arch Otolaryngol Head Neck Surg 1992;118:687-692.<br />
Kohut RI. Peilymphatic fistulae: more than a century of notions, conjectures, and critical studies. Am J Otol 1982;13:38-40.<br />
Kohut RI, Waldorf RA, Haenel JL, Thompson JN. Minute perilymph fistulas: vertigo and Hennebert's sign without hearing<br />
loss. Ann Otol Rhinol Laryngol 1979;88:153-159.<br />
Lehrer JF, Poole DC, Sigal B. Use of the glycerin test in the diagnosis of post-traumatic perilymphatic fistulas. Am J<br />
Otolaryngol 1980;1:207-210.<br />
Luntz M, Frank I, Yurovitzki I, Berger G, Sadé J. Large perilymph fistulas. Am J Otol 1986;7:282-286.<br />
Meyerhoff WL, Pollock KJ. A patient-oriented approach to perilymph fistula. Arch Otolaryngol Head Neck Surg<br />
1990;116:1317-1319.<br />
Meyerhoff WL, Yellin MW. Summating potential/action potential ratio in perilymph fistula. Otolaryngol Head Neck Surg<br />
1990;102:678-682.<br />
Narula A, Marks NJ. Acoustic trauma and perilymph fistula. J Laryngol Otol 1985;99:909-911.<br />
Nomura Y, Hara M, Young Y-H, Okuno T. Inner ear morphology of experimental perilymphatic fistula. Am J Otol<br />
1992;13:32-37.<br />
http://www.bcm.edu/oto/grand/102193.html (5 of 7) [5.11.2005 10:44:09]
http://www.bcm.edu/oto/grand/102193.html<br />
Parell GJ, Becker GD. Results of surgical repair of inapparent perilymph fistulas. Otolaryngol Head Neck Surg<br />
1986;95:344-346.<br />
Petroff MA, Simmons FB, Winzelberg J. Two emerging perilymph fistula "syndromes" in children. Laryngoscope<br />
1986;96:498-501.<br />
Pillsbury HC III, Postma DS. The Tullio phenomenon, fistula test, and Hennebert's sign: clinical significance. Otolaryngol<br />
Clin North Am 1983;16:205-207.<br />
Poe DW, Gadre AK, Rebeiz EE, Pankratov MM. Intravenous fluorescein for detection of perilymphatic fistulas. Am J Otol<br />
1993;14:51-54.<br />
Poe DS, Rebeiz EE, Pankratov MM. Evaluation of perilymphatic fistulas by middle ear endoscopy. Am J Otol 1992;13:529-<br />
533.<br />
Pullen FW II. Perilymphatic fistula induced by barotrauma. Am J Otol 1992;13:270-272.<br />
Pyykkö I, Ishizaki H, Aalto H, Starck J. Relevance of the Tullio phenomenon in assessing perilymphatic leak in vertiginous<br />
patients. Am J Otol 1992;13:339-342.<br />
Rizer FM, House JW. Perilymph fistulas: the House Ear Clinic experience. Otolaryngol Head Neck Surg 1991;104:239-<br />
243.<br />
Schuknecht HF, Witt RL. Suppressed sneezing as a cause of hearing loss and vertigo. Am J Otolaryngol 1985;6:468-470.<br />
Seltzer S, McCabe BF. Perilymph fistula: the Iowa experience. Laryngoscope 1986;94:37-49.<br />
Shea JJ. The myth of spontaneous perilymph fistula. Otolaryngol Head Neck Surg 1992;107:613-616.<br />
Shelton C, Simmons FB. Perilymph fistula: the Stanford experience. Ann Otol Rhinol Laryngol 1988;97:105-108.<br />
Shepard NT, Telian SA, Niparko JK, Kemink JL, Fujita S. Platform pressure test in identification of perilymphatic fistula.<br />
Am J Otol 1992;13:49-54.<br />
Silverstein H. Rapid protein test for perilymph fistula. Otolaryngol Head Neck Surg 1991;105:422-426.<br />
Simmons FB. Theory of membrane breaks in sudden hearing loss. Arch Otolaryngol 1968;88:67-74.<br />
Simmons FB. Fluid dynamics in sudden sensorineural hearing loss. Otolaryngol Clin North Am 1978;11:55-61.<br />
Singleton GT. Diagnosis and treatment of perilymph fistulas without hearing loss. Otolaryngol Head Neck Surg<br />
1986;94:426-429.<br />
Singleton GT, Post KN, Karlan MS, Bock DG. Perilymph fistulas: diagnostic criteria and therapy. Ann Otol Rhinol<br />
Laryngol 1978;87:797-803.<br />
http://www.bcm.edu/oto/grand/102193.html (6 of 7) [5.11.2005 10:44:09]
http://www.bcm.edu/oto/grand/102193.html<br />
Stroud MH, Calcaterra TC. Spontaneous perilymph fistulas. Laryngoscope 1970;80:479-487.<br />
Supance JS, Bluestone CD. Perilymph fistulas in infants and children. Otolaryngol Head Neck Surg 1983;91:663-671.<br />
Thompson JN, Kohut RI. Perilymph fistulae: variability of symptoms and results of surgery. Otolaryngol Head Neck Surg<br />
1979;87:898-903.<br />
Weider DJ. Treatment and management of perilymphatic fistula: a New Hampshire experience. Am J Otol 1992;13:158-<br />
166.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/102193.html (7 of 7) [5.11.2005 10:44:09]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
LESIONS OF THE PETROUS APEX<br />
August 4, 1994<br />
Philip A. Matorin, M.D.<br />
The petrous apex is the most inaccessible portion of the temporal bone. The petrous apex can be involved<br />
in congenital, infectious, inflammatory, and neoplastic processes. Since direct examination is not<br />
possible, careful attention to the often subtle signs and symptoms, as well as keeping a high index of<br />
suspicion, is necessary to diagnose these entities. The true incidence of these rare lesions is difficult to<br />
estimate, but the House group has reported that acoustic neuromas are about 30 times more common in<br />
their practice.<br />
The petrous apex is a truncated pyramid forming the medial portion of the temporal bone. The base is<br />
bounded by the bony labyrinth and the carotid artery anteriorly. The superior surface is the middle cranial<br />
fossa, Meckel's Cave, and the ascending carotid artery. The posterior surface is the posterior cranial fossa<br />
http://www.bcm.edu/oto/grand/8494.html (1 of 6) [5.11.2005 10:44:18]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
and Dorello's canal transmitting CNVI. The inferior surface is the jugular bulb and the inferior petrosal<br />
sinus. The petrous apex is marrow filled in 84%, pneumatized in 9%, and sclerotic in 7%.<br />
Clinical presentations can range from subtle to dramatic. Involvement of the Eustachian tube can result in<br />
aural fullness or otitis media. Compression at the foramen ovale can cause V3 paresthesia or numbness.<br />
Stretching of the dura can cause headache of eye pain. In addition, ophthalmoplegia, tinnitus, vertigo,<br />
hearing loss, and facial paralysis can occur.<br />
CT and MRI have revolutionized the preoperative work-up of petrous apex lesions. An accurate<br />
differential diagnosis is critical in that it may influence the surgical approach for specific lesions. The two<br />
modalities may provide complimentary information based on density, bone erosion, contrast<br />
enhancement, and imaging characteristics with T1 and T2 weighting.<br />
Several benign anatomic variants may produce radiographic abnormalities that can mimic pathologic<br />
conditions. Thirty to thirty-five percent of petrous apices are pneumatized and 6.8% may have<br />
asymmetric pneumatization that can be demonstrated by CT. On MRI, the less pneumatized, marrowfilled<br />
apex would appear bright on T1 and T2, mimicking a lesion. A giant petrous air cell can cause<br />
distortion of the IAC appearing similar to an expansile lesion. Lastly, simple effusions, mucoceles, and<br />
mucus retention cysts of the petrous apex appear as soft tissue density with preservation of the air cell<br />
septae. Expansile mucoceles may have eroded margins. On MRI, these appear low on T1 and bright on<br />
T2.<br />
Cholesterol granuloma is the most common lesion of the petrous apex. It is approximately 10 times more<br />
common than cholesteatoma and 40 times more common than mucocele. The cyst wall lacks the<br />
keratinizing squamous epithelium of cholesteatoma. On CT, the lesion appears as a homogeneous soft<br />
tissue ovoid lesion posterior to the horizontal carotid canal. On MRI, it appears bright on T1 and T2<br />
without enhancement with gadolinium. The surgical treatment is re-establishment of aeration of the apex<br />
by using a silicone drain into the middle ear or mastoid.<br />
Cholesteatoma of the petrous apex can be congenital or acquired. Acquired cholesteatomas are rare and<br />
occur by extension from the middle ear space along the supralabyrinthian air cell system along the<br />
anterior epitympanic space. Facial nerve dysfunction occurs in 20% - 50% of cases. On CT,<br />
cholesteatoma appears as a smooth, expansile lesion hypodense to brain without contrast enhancement.<br />
On MRI, it appears as low intensity on T1 and hyperintense on T2, similar to CSF. The translabyrinthiantranscochlear<br />
and the middle fossa approaches are used most often for extirpation of these lesions.<br />
Metastatic lesions of the temporal bone are uncommon. However, the petrous apex and clivus are two of<br />
the most common sites for metastasis in the head and neck. The most common primary sites are the<br />
breast, lung, kidney, stomach, prostate, and larynx. Metastases to the skull base in isolation are<br />
uncommon and infraclavicular metastases are usually present. A bone scan should be performed when<br />
metastasis is suspected. Most tumors are erosive, but some stimulate sclerosis from osteoblastic activity.<br />
The MRI appearance is variable depending on the type of lesion.<br />
http://www.bcm.edu/oto/grand/8494.html (2 of 6) [5.11.2005 10:44:18]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Other lesions of the petrous apex that should be in the differential include: petrous apicitis usually due to<br />
pseudomonas and rarely TB; intrapetrous carotid artery aneurysm, chondroma/chondrosarcoma,<br />
meningioma, schwannoma, and chordoma.<br />
Case Presentation<br />
A 64-year-old white lady presented with a nine-month history of asymmetric left-sided hearing loss of<br />
sudden onset. The hearing loss was accompanied by tinnitus. She denied headache, vertigo, and otalgia.<br />
She denied any significant medical or surgical history and had no history of otologic disease, nor previous<br />
otologic surgery. She did have a history of left Bell's Palsy one year before presentation, which had<br />
resolved completely. She admitted having a 75 pack/year smoking history. Audiometry revealed an<br />
asymmetric, moderate to profound, left sensorineural hearing loss, absent acoustic reflexes and<br />
significantly depressed speech audiometry. CT scanning of the temporal bones showed a well defined,<br />
lobulated, expansile lesion of the left petrous apex. By MRI, the lesion was bright on T1 and T2. CT<br />
scanning of the chest and a screening mammogram were negative. The petrous apex was entered after<br />
complete mastoidectomy via the retrofacial air cell tract. A cyst filled with a brown exudate consistent<br />
with a cholesterol granuloma was drained into the mastoid using a pediatric feeding tube. Two months<br />
post operatively, she was asymptomatic, doing well, and had minimal change in her hearing.<br />
Bibliography<br />
Appling D, Jenkins HA, Patton GA. Eosinophilic granuloma in the temporal bone and skull. Otolaryngol Head Neck Surg<br />
1983;91:358-364.<br />
Arriaga MA, Brackmann DE. Differential diagnosis of primary petrous apex lesions. Am J Otol 1991;12:470-474.<br />
Atlas MD, Moffat DA, Hardy DG. Petrous apex cholesteatoma: diagnostic and treatment dilemmas. Laryngoscope<br />
1992;102:1363-1368.<br />
Benecke EE, Kuczer A, Cooper MH. Anatomic importance of the retrofacial air tract. Am J Otol 1992;13:499-500.<br />
Behnke EE, Schindler RA. Dermoid of the petrous apex . Laryngoscope 1984;94:779-782.<br />
Brown RV, Sage MR, Brophy BP. CT and MR findings in patients with chordomas of the petrous apex. AJNR Am J<br />
Neuroradiol 1990;11:121-124.<br />
Charachon R, Crouzet G, Vasdev A, Gratacap B. Tumours of the petrous apex: a clinical series. J Neuroradiol 1988;15:186-<br />
201.<br />
http://www.bcm.edu/oto/grand/8494.html (3 of 6) [5.11.2005 10:44:18]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Chole RA. Petrous apicitis: surgical anatomy. Ann Otol Rhinol Laryngol 1985;94:251-256.<br />
Dalley RW, Robertson WD, Nugent RA. Computed tomography of calvarial and petrous bone sarcoidosis. J Comput Assist<br />
Tomogr 1987;11:884-886.<br />
Davis AE, Robin PE. Transpalatal approach to the petrous apex. J Laryngol Otol 1989;103:94-96.<br />
DeLozier HL, Parkins CW, Gacek RR. J Laryngol Otol 1979;93:177-180.<br />
Franklin DJ, Jenkins HA, Horowitz BL, Coker NJ. Management of petrous apex lesions. Arch Otolaryngol Head Neck<br />
Surg 1989;115:1121-1125.<br />
Frates MC, Oates E. Petrous apicitis: evaluation by bone SPECT and magnetic resonance imaging. Clin Nucl Med<br />
1990;15:293-294.<br />
Gacek RR. Diagnosis and management of primary tumors of the petrous apex. Ann Otol Rhinol Laryngol Suppl 1975;18:1-<br />
20.<br />
Gacek RR. Evaluation and management of primary petrous apex cholesteatoma. Otolaryngol Head Neck Surg 1980;88:519-<br />
523.<br />
Gates GA. The lateral facial approach to the nasopharynx and infratemporal fossa. Otolaryngol Head Neck Surg<br />
1988;99:321-325.<br />
Gherini SG, Brackmann DE, Lo WW, Solti-Bohman LG. Cholesterol granuloma of the petrous apex. Laryngoscope<br />
1985;95:659-664.<br />
Ghorayeb BY, Jahrsdoerfer RA. Subcochlear approach for cholesterol granulomas of the inferior petrous apex. Otolaryngol<br />
Head Neck Surg 1990;103:60-65.<br />
Giddings NA, Brackmann DE, Kwartler JA. Transcanal infracochlear approach to the petrous apex. Otolaryngol Head<br />
Neck Surg 1991;104:29-36.<br />
Glasscock ME 3d, Woods CI, Poe DS, Patterson AK, Welling DB. Petrous apex cholesteatoma. Otolaryngol Clin North<br />
Am 1989;22:981-999.<br />
Goin DW. Surgical management of petrous apex meningioma. Laryngoscope 1979;89:204-213.<br />
Goldsmith AJ, Myssiorek D, Valderrama E, Patel M. Unifocal Langerhans' cell histiocytosis (eosinophilic granuloma) of<br />
the petrous apex. Arch Otolaryngol Head Neck Surg 1993;119:113-116.<br />
Heinrich DE, Gantz BJ, Moore SA, Schubkegel AJ. Undifferentiated small-cell neoplasm of the petrous apex: a case report.<br />
Arch Otolaryngol Head Neck Surg 1992;118:767-770.<br />
Hendershot EL, Wood JW, Bennhoff D. The middle cranial fossa approach to the petrous apex. Laryngoscope 1976;86:658-<br />
http://www.bcm.edu/oto/grand/8494.html (4 of 6) [5.11.2005 10:44:18]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
663.<br />
Horn KL, Hankinson HL, Erasmus MD, Beauparalant PA. The modified transcochlear approach to the cerebellopontine<br />
angle. Otolaryngol Head Neck Surg 1991;104:37-41.<br />
Jackler RK, Parker DA. radiographic differential diagnosis of petrous apex lesions. Am J Otol 1992;13:561-574.<br />
Jahn AF, Farkashidy J, Berman JM. Metastatic tumors in the temporal bone - a pathophysiologic study. J Otolaryngol<br />
1979;8:85-94.<br />
Kearns DB, Coker NJ, Pitcock JK, Jenkins HA. Tuberculous petrous apicitis. Arch Otolaryngol 1985;111:406-408.<br />
Lempert J. Complete apicectomy (mastoidotympano-apicectomy): a new technique for the complete exenteration of the<br />
apical carotid portion of the petrous pyramid. Arch Otolaryngol 1937;25:144-177.<br />
Lipkin AF, Coker NJ, Jenkins HA, Alford BR. Intracranial and intratemporal facial neuroma. Otolaryngol Head Neck Surg<br />
1987;96:11-77.<br />
Montgomery WW. Cystic lesions of the petrous apex: transsphenoid approach. Ann Otol Rhinol Laryngol 1977;86:429-<br />
435.<br />
Prasad S, Janecka IP. Efficacy of surgical treatments for squamous cell carcinoma of the temporal bone: a literature review.<br />
Otolaryngol Head Neck Surg 1994;110:270-280.<br />
Roland PS, Meyerhoff WL, Judge LO, Mickey BE. Asymmetric pneumatization of the petrous apex. Otolaryngol Head<br />
Neck Surg 1990;103:80-88.<br />
Samy LL, Girgis IH. Transzygomatic approach to the petrous apex with a record of three cases. J Laryngol Otol<br />
1967;81:277-289.<br />
Smith PG, Leonetti JP, Kletzker GR. Differential clinical and radiographic features of cholesterol granulomas and<br />
cholesteatomas of the petrous apex. Ann Otol Rhinol Laryngol 1988;97:599-604.<br />
Solodnik P, Som PM, Shugar JM, Sachdev VP, Sacher M, Lanzieri CF, et al. Intraosseous petrous apex neuroma: CT<br />
findings. J Comput Assist Tomogr 1986;10:1027-1029.<br />
Thedinger BA, Nadol JB Jr, Montgomery WW, Thedinger BS, Greenberg JJ. Radiographic diagnosis, surgical treatment<br />
and long-term follow-up of cholesterol granulomas of the petrous apex. Laryngoscope 1989;99:896-906.<br />
Umansky F, Valarezo A, Elidan J. The microsurgical anatomy of the abducens nerve in its intracranial course.<br />
Laryngoscope 1992;102:1285-1292.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
http://www.bcm.edu/oto/grand/8494.html (5 of 6) [5.11.2005 10:44:18]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/8494.html (6 of 6) [5.11.2005 10:44:18]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for<br />
use by doctors and other health care professionals. These documents were<br />
prepared by resident physicians for presentation and discussion at a<br />
conference held at The Baylor College of Medicine in Houston, Texas. No<br />
guarantees are made with respect to accuracy or timeliness of this material.<br />
This material should not be used as a basis for treatment decisions,<br />
and is not a substitute for professional consultation and/or peerreviewed<br />
medical literature.<br />
Causes of Failure and Complication in Surgery for<br />
Otosclerosis<br />
Mas Takashima, M.D.<br />
November 11, 1999<br />
The restoration of hearing in patients with conductive hearing loss secondary to<br />
otosclerosis has, as some may say, been the most important development in<br />
otology. A number of techniques for opening the oval window and reconstructing<br />
http://www.bcm.edu/oto/grand/111199.htm (1 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
the ossicular chain have been developed since Rosen first mobilized the stapes in<br />
1953. Excellent hearing improvement is possible with most of the techniques in use<br />
today. However, a significant number of complications or failures continue to<br />
compromise the expected hearing results and necessitate revision surgery. The best<br />
chance of success is at the time of the initial procedure, with revision surgery<br />
successful in less than 80% of cases. It is the purpose of this grand rounds to<br />
review the most common pitfalls incurred in stapedectomy, as well as to report<br />
surgical complications of this procedure.<br />
The pertinent anatomy includes the tympanic membrane, the anterior and posterior<br />
crus of the stapes, the capitulum, the long process of the incus, the tendon and<br />
stapedius muscle, the footplate of the stapes, the tympanic segment of the facial<br />
nerve, the cochlea, and the labyrinth.<br />
The earliest surgical attempts to improve hearing loss associated with stapes<br />
fixation was by Kessler in 1876. In this procedure, he incised the posterior portion<br />
of the tympanic membrane, separated the incus stapedial joint, removed the bony<br />
canal wall when necessary and attempted to mobilize the stapes by applying<br />
pressure to the capitulum in various directions. If the stapes could not be mobilized,<br />
it was removed. The interest in stapes surgery abruptly stopped in 1900 when at the<br />
International Congress, Politzer and Sutton and other prominent otologists declared<br />
these operations were useless and dangerous. It is surmised that this statement was<br />
prompted by large numbers of complications that had gone unreported.<br />
Next, the area of surgical fistulization began with the work of Barany and<br />
Holmgren. They fistulized the superior semicircular canal in otosclerotic ears,<br />
allowing the dura to rest against the membranous labyrinth. Hearing improvement<br />
was fruitfully noted with this procedure. Sordell studied with Holmgren and<br />
devised a three-stage operation in which the skin-covered horizontal canal fistula<br />
was used to improve hearing. In 1938, Lempert simplified this to a one-stage<br />
operation. After being modified in 1945, this operation became the standard for the<br />
next seven years. The next major advancement occurred in 1952 when Rosen<br />
accidentally mobilized the stapes during palpation on the ossicular chain in a<br />
fenestration operation. The patient noticed remarkable, immediate hearing<br />
improvement, which lasted for years. One year later, when mobilization had<br />
become the standard of care, Rosen reported hearing improvement to at least the 30<br />
decibel level in 22% of 211 operations he performed. In 1954, Shambaugh applied<br />
the operating microscope to stapes mobilization. This paved the way for Shea to<br />
revive the stapedectomy with the modifications of an intact ossicular chain in a<br />
covered oval window. To date, multiple modifications of this procedure have been<br />
performed using various types of prostheses and grafts.<br />
Otosclerosis is the primary focal spongiform disease of the labyrinthine capsule.<br />
http://www.bcm.edu/oto/grand/111199.htm (2 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Valsalva first described this pathologic process underlying otosclerosis in 1735,<br />
from the autopsy of a deaf patient. Today, there is still some controversy regarding<br />
the etiology and pathogenesis of otosclerosis. Briefly, otosclerosis, otherwise<br />
known as otospongiosis, is thought to be a familial autosomal dominant disorder<br />
with a variable penetrance of 25% to 40%. The mechanism has recently been<br />
suggested to be an autoimmune reaction to cartilaginous remnants and collagen<br />
fiber type II. This is thought to stimulate an inflammatory reaction in lysosomal<br />
proteases in and around the otospongiotic foci.<br />
For a successful surgical outcome, one must begin planning treatment with the<br />
initial physical examination. This begins with an overall observation of the patient.<br />
The age of the patient alone should not be a contraindication to performing surgery.<br />
In patients less than 16 years of age, there is a greater chance that the conductive<br />
impairment is secondary to congenital anomalies rather than otosclerosis. Likewise,<br />
very active diffuse obliterative otosclerosis may be found in a young patient,<br />
predisposing to a higher incidence of complications. Yet surgery should be<br />
considered in the young because hearing acuity is essential during the formative<br />
years of development. Patients older than 75 years are still surgical candidates if<br />
they are in good health. Hearing acuity becomes more important as other senses<br />
decline with age. In order to prepare for surgery and to prevent failures and<br />
complications, infections and anatomic variations must also be considered. The<br />
otologic evaluation may reveal dermatological conditions of the external ear canal<br />
that will predispose to postoperative infections. These include chronic external<br />
otitis, trauma from hearing aides or self-inflicted injury with cotton-tipped swabs.<br />
Likewise, one may see a small, crooked stenotic ear canal that, until corrected, will<br />
restrict surgical movement. Small exostosis usually does not impair access to the<br />
mesotympanum and may be left untouched. Even larger exostosis, which is limited<br />
to the anterior canal wall, usually does not interfere with the surgical approach.<br />
When the removal of the large posterior exostosis is necessary, it may be<br />
impossible to preserve a satisfactory tympanomeatal skin flap. In such cases, it is<br />
best to remove the exostosis first and delay the stapedectomy.<br />
Brahe Pedersen and Felding have postulated a connection between the influenza<br />
viral infection and unexplained sensorineural hearing loss immediately after stapes<br />
surgery. Although without evidence, this cannot be proven, it would seem prudent<br />
to avoid operation when respiratory viral infections are prevalent, especially in the<br />
patient, the patient's family or the surgeon.<br />
The diagnosis of otosclerosis should be confirmed only after other reasons for<br />
progressive hearing loss have been ruled out. The most common differential<br />
diagnoses of conductive losses are malleus fixation, serous otitis media, ankylosis<br />
of the malleus incus joint, Waardenburg's syndrome, Paget's disease,<br />
tympanosclerosis and progressive lysis to the long process of the incus.<br />
http://www.bcm.edu/oto/grand/111199.htm (3 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Tympanometry provides the most useful method to exclude most of these cases,<br />
particularly serous otitis media and ossicular fixation. Clinical history is of special<br />
value to rule out systemic disease such as Paget's disease, osteogenesis imperfecta<br />
or ankylosing rheumatoid arthritis.<br />
Many of the common anatomic variations, congenital anomalies and pathologic<br />
conditions are not known until seen during surgery. The surgeon must be well<br />
trained and experienced, first in recognizing these malformations, and second, in<br />
skillfully correcting them. A systematic examination of the unusual should be done.<br />
A superiorly located jugular bulb may come into juxtaposition with a tympanic<br />
annulus and in this position is vulnerable to injury during elevation of the tympanic<br />
meatal flap. For this reason, the elevation of the tympanic annulus inferiorly should<br />
not be performed with both strobes of the elevator. Tears of the jugular bulb, of<br />
course, result in profuse bleeding and constitute an alarming, although not serious,<br />
complication. Elevating the head of the operating room table and packing the area<br />
with Gelfoam may control the bleeding. If the bleeding is readily controlled, the<br />
operation may be completed. If the tear is large and the bleeding is difficult to<br />
control, the procedure should be terminated.<br />
The location of the facial nerve should be determined before proceeding with<br />
removal of the stapes. Usually, the facial nerve lies superior to the oval window,<br />
which permits the surgeon to acquire a complete view of the footplate. In this<br />
position, the lateral surface of the nerve is usually covered by bone, although the<br />
inferior surface may be partially dehiscent. When the nerve overhangs the<br />
footplate, there is frequently a lateral as well as an inferior dehiscence to the<br />
fallopian aqueduct. Dehiscence of the facial nerve is not uncommon, and in about<br />
0.5% of middle ears there is a sizable dehiscence, so that the nerve bulges down<br />
and obscures the arch and footplate. Even in these cases, for the experienced<br />
surgeon, it is often possible to remove the footplate, although somewhat blindly,<br />
and the prosthesis can be contoured so as to adapt to the overhanging facial nerve.<br />
Otosclerosis of the round window niche is of no significance unless the round<br />
window opened is completely closed. When obliteration of the niche is severe, only<br />
a dimple may mark its location. From a retrospective study of 30,567<br />
stapedectomies, this has been shown to occur in 300 patients or 1% of cases. In this<br />
situation, the mucosa should be elevated in an attempt to determine that the closure<br />
is complete. When it is not possible to determine with certainly whether the<br />
window is blocked, the stapedectomy should be performed. Patients with round<br />
window closure tend to have an early onset of hearing loss, frequently beginning in<br />
childhood or in adolescence, similar to the hearing losses associated with<br />
obliterative otosclerosis. However, these patients develop a more severe mixed<br />
hearing loss than those patients with disease limited to the oval window. A family<br />
history can be obtained from 50% of the patients with otosclerosis. Shea's series<br />
http://www.bcm.edu/oto/grand/111199.htm (4 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
showed 78% of patients who developed round window closure had a strong family<br />
history consistent with otosclerosis.<br />
The stapedial artery, which is present in the early stage of embryonic life and<br />
persists in many lower animals, is usually absent in the human ear. A pulsating<br />
vessel nearly filling the crural arch will identify a persistent stapedial artery. In<br />
some cases, the stapes can be removed and the prosthesis introduced, but in 0.2%<br />
of the operations it is not feasible to proceed with the surgery. Rupture of the vessel<br />
could result in profuse hemorrhage and is to be meticulously avoided. A small<br />
artery on the footplate is a consistent finding and is not to be confused with the<br />
persistent stapedial artery.<br />
Until the advent of stapedectomy surgery, the high incidence of malleus ankylosis<br />
had not been recognized. Malleus ankylosis occurs with a disease entity unrelated<br />
to, but sometimes associated with, otosclerosis of the oval window. A bridge of<br />
lamellar bone extending from the anterior part of the head of the malleus to the<br />
anterior epitympanic wall fixes the head of the malleus. Presumably, this bridge of<br />
bone results from failure of the malleus to completely separate from the<br />
epitympanic wall during embryonic development. The otologic history, often<br />
secured in retrospect, usually reveals hearing loss in childhood that becomes worse<br />
in adult life. Such cases represent malleus ankylosis with subsequent development<br />
of otosclerosis. When there is a history of hearing loss since early childhood<br />
without progression, the case may represent pure malleus fixation without oval<br />
window otosclerosis. If there is a history of hearing loss dating from childhood or if<br />
the hearing loss is unilateral, the preoperative evaluation could certainly include<br />
tests for malleus mobility. Should examination with the pneumatic otoscope be<br />
inconclusive, mobility should be determined with direct instrumental manipulation<br />
with the aid of magnification. If there is fixation, it is necessary to perform an<br />
atticotomy and widely expose the head of the malleus and the body of the incus.<br />
Proper treatment will consist of amputation of the head of the malleus followed by<br />
ossicular reconstruction.<br />
Congenital anomalies of the stapes and incus are usually suspected because of a<br />
history of hearing problems from early childhood. The anomalies may range from<br />
simple fixation of the footplate due to incomplete resolution of the mesenchymal<br />
tissue during embryologic development, to the absence of the stapes in infancy.<br />
The stapes may be small and articulate with a short, underdeveloped long process<br />
of the incus. The crural arch may contain bone or may be replaced by a single bony<br />
strut. The floor of the oval window niche may consist of a solid layer of bone<br />
without evidence of a footplate or the oval window niche may be completely<br />
missing. The correction of simple congenital stapes fixation may be the same as for<br />
fixation due to otosclerosis. Corrective surgery for anomalies is attended with a<br />
higher incidence of injury to the inner ear because of frequent associations of<br />
http://www.bcm.edu/oto/grand/111199.htm (5 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
anomalies to the membranous labyrinth. For example, the utriculosaccular deck<br />
may be located in the oval window area and may be vulnerable to injury. These<br />
patients should be counseled regarding the greater risk of sensorineural hearing<br />
loss. In very rare cases, the otosclerotic foci may not only obliterate the oval<br />
window niche, but may also extend into the vestibule. This has been shown to<br />
occur in 7%-11% of the cases in which stapedectomies failed. When removing the<br />
bone, the surgeon will find that the growth extends into the vestibule beyond the<br />
footplate level. This is best managed using a slow rotation per minute microdrill to<br />
create a 0.8-mm diameter cylinder. In this situation, laser creates a potential risk to<br />
the patient because of heat transfer to the perilymph of the vestibule and<br />
subsequently to the utriculosaccular.<br />
The gusher is a dramatic complication to stapes surgery. The smallest control hole<br />
in the footplate can produce a perilymph leak so profuse that it fills the middle ear<br />
and internal auditory canal within seconds. The existence of this abnormality is<br />
suggested by an upward sloping air conduction audiogram with best responses at 2<br />
kilohertz. This complication is more common in ears with congenital fixation of the<br />
footplate. Management of the stapes gusher is the same as management for a CSF<br />
leak. Once the surgeon notes the onset of fluid leaking from the aperture in the<br />
stapes footplate, leakage may be controlled with a small piece of Surgicel. A graft<br />
should be placed over the leaking footplate with the completion of the<br />
stapedectomy. A lumbar drain will now effect a diversion of the CSF thereby<br />
decreasing the pressure of the purulence. The head of the patient's bed is elevated<br />
and daily fluid intake is restricted. The flow of CSF may last for several days and a<br />
sensorineural hearing loss is likely to occur. Clearly, if such ears can be identified,<br />
the operation is contraindicated.<br />
Next, we will move on to surgical trauma. Tears of the tympanic meatal flap that<br />
may occur in the following locations. First, a linear tear or buttonhole perforation<br />
may occur in the skin flap. Usually, these tears require no repair. However, when<br />
replacing a flap at the completion of the procedure, care must be taken to avoid<br />
enfolding the margins of the tear. The skin flap may separate from the tympanic<br />
annulus as well. This usually occurs in an inferior location and is due to failure to<br />
elevate the tympanic annulus from the sulcus. Another cause of a tear of this type is<br />
failure to achieve total elevation of skin flap from incision-to-incision. Usually no<br />
repair is required if separation occurs inferiorly. However, if it occurs superiorly,<br />
grafting may be necessary.<br />
Subluxation and luxation of the incus consists of a tear in the capsule of the<br />
incudomalleolar joint, but with a sufficiently intact capsule to maintain the incus in<br />
its normal anatomical position. Although the long process of the incus will be<br />
excessively mobile, the operation may be completed and functional results may be<br />
satisfactory. Luxation of the incus is due to a complete disruption of the<br />
http://www.bcm.edu/oto/grand/111199.htm (6 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
incudomalleolar joint and demands that the removal of the incus and the use of a<br />
malleus over-window prosthesis. Attempts to replace and maintain the incus in its<br />
original position are usually not successful. The incus may be accidentally<br />
dislocating during curetting of the bony annulus and during manipulations of the<br />
oval window. The long process of the incus may be accidentally displaced when<br />
withdrawing the instrument from the oval window niche. Fractures of the long<br />
process of the incus are an unusual complication, but may happen during the wire<br />
tightening procedure. If the fracture appears near the tip of the long process, the<br />
wire may still be placed on the stump. If this is not possible, the procedure must be<br />
altered.<br />
Injury to the facial nerve during stapedectomy is uncommon, but there may be a<br />
direct injury to the nerve in the facial canal by careless use of the instruments,<br />
touching with the drill or heating by a drill if the tip is not cool. An interesting<br />
remark made by Schuknecht states that direct instrumental injury to the facial nerve<br />
is extremely rare and has only occurred once during his numerous stapedectomies.<br />
Since the risk to the facial nerve injury is almost nil, Schuknecht considered that<br />
the possibility of its occurrence need not be mentioned to the patient before<br />
operation.<br />
During a stapedectomy operation, it is frequently necessary to displace the chorda<br />
tympani nerve to gain adequate exposure. There is controversy concerning the<br />
advisability of stretching the nerve or cutting it. Approximately one-fourth of<br />
patients complain of ageusia in the postoperative period. Chorda tympani nerve<br />
dysfunction is usually transient and fewer than 5% of patients experience<br />
permanent deficits. It should be appreciated that if the nerve is cut, it will produce<br />
permanent loss of sensation of taste on the anterior two-thirds of the tongue on the<br />
same side. No reinnervation of the taste buds can take place, either from the chorda<br />
tympani nerve on the opposite side or the posterior third of the tongue supplied by<br />
the glossopharyngeal nerve. Permanent loss of the chorda tympani innervation<br />
results in atrophy of the taste receptors. The dorsum of the tongue becomes smooth<br />
and pale. The patient may not complain of the loss of taste if one nerve is cut, as<br />
long as the tongue retains sensation for 66% of the surface. If the nerve is stretched<br />
during operation, a persistent abnormal sensation in the tongue may occur,<br />
described by the patient as salty or metallic. Bilateral loss of the chorda tympani<br />
nerve produces marked symptoms in the majority of patients. In addition to the loss<br />
of taste, there is loss of secretum motor supply to the submandibular and sublingual<br />
glands that produces an uncomfortably dry mouth. Deficits include a diminution of<br />
taste sensation or a dry mouth. Revision causes cases to deserve special attention.<br />
Sensorineural hearing loss is perhaps the most disappointing and devastating<br />
complication for both the surgeon and patient. Complete sensorineural hearing loss<br />
can occur even in the most meticulously and appropriately performed stapes<br />
http://www.bcm.edu/oto/grand/111199.htm (7 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
procedure. Most commonly, however, are complications due to surgical trauma.<br />
Intraoperative studies performed in stapedectomy indicate that acoustic trauma in<br />
drilling, excessive movement of the stapes producing a hydraulic effect, rupture of<br />
the membranous inner ear, rapid loss in perilymph that may lead to damage at the<br />
membranous structures in the vestibule, footplate fragments or bone death in the<br />
vestibule, and the floating footplate are the great offenders for vestibular and<br />
presumably cochlear damage. The reported incidence of dead ears after operation<br />
varies from 0.5% to 4%. It is important to appreciate that these are figures from a<br />
series of operations performed by expert surgeons with a special interest in<br />
stapedectomy. Results achieved by the occasional operator are not reported and it is<br />
likely that the incidence of cochlear damage is much higher. Mawson has shown<br />
that in a series of 1000 operations, there was a hearing loss at 4% in the first 50<br />
operations, 2% hearing loss after the next 50 operations, no loss in the next 500 and<br />
0.25% of the remaining 400 operations.<br />
An attempt at removal of the floating footplate may result in a dead ear and if this<br />
complication is encountered it must be dealt with correctly. If the footplate is<br />
visible, it may be possible to remove it by manipulation and extraction with a fine<br />
hook, or a small drill hole may be made at the margin of the oval window and a<br />
fine hook used to remove it. If the footplate cannot be removed without excessive<br />
manipulation, it should be left in place and a soft tissue graft placed over the oval<br />
window and the operation abandoned.<br />
The depressed footplate may result from incorrect attempts to remove a floating<br />
footplate or may occur during attempts to carry out a total stapedectomy. Causse<br />
documented this at an incidence of 0.16%. No attempt should be made to retrieve<br />
the submerged footplate by instrument as this may cause severe cochlear damage.<br />
Roche et al have described a method of dealing with this complication that is not<br />
damaging to the contents of the vestibule. Drops of blood are poured laterally into<br />
the vestibule and when the vestibule is full of blood and a clot is formed, the clot is<br />
removed by a lateral application of the sucker and the footplate coated with the clot<br />
is usually removed from the oval window. It is of paramount importance for the<br />
surgeon to understand the relationship of the stapes footplate to the vestibular<br />
contents. Almost all patients have a minimal safe distance of approximately 1-mm<br />
between the medial surface of the footplate and the utricle and saccule. Penetration<br />
of the vestibule by more than 1 mm with the footplate instruments or prosthesis<br />
may perforate the utricle and saccule inducing sensorineural hearing loss, vertigo or<br />
both. In patients with endolymphatic hydrops the saccule may extend to contact the<br />
medial surface of the footplate, thereby placing these patients at a higher risk for<br />
complications from this procedure.<br />
Concerning postoperative complications, prosthesis displacement is the most<br />
common postoperative complication, accounting for 50-70% of revision surgeries.<br />
The hearing deterioration may be acute, as the prosthesis becomes dislodged or<br />
http://www.bcm.edu/oto/grand/111199.htm (8 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
chronic as it gradually displaces out of position. This complication may be<br />
encountered many years after stapes surgery. The diagnosis is definitely made at<br />
reoperation, but may be suspected based on tuning fork and audiometric tests.<br />
Prosthesis loosening due to erosion or notching of the incus and prosthesis<br />
displacement due to necrosis of the incus also occurs. With removal of the stapes<br />
arch, the blood supply to the long process of the incus is divided as it courses over<br />
the incudostapedial joint. Collateral vessels exist from the body of the incus and<br />
maintain the viability of the remaining bone. Circumferential overtightening of the<br />
prosthesis can remove the blood supply to the tip of the incus.<br />
The signs and symptoms of perilymphatic fistula were first described by Lewis in<br />
1961, and this complication, which at one time was thought be unusual, is now<br />
accepted as being one of the more common complications of stapedectomy. The<br />
surgeon creates a fistula at every stapedectomy operation and relies on the natural<br />
process of healing or in some techniques a graft of soft tissue, to seal the opening<br />
that has been made. In most operations, there is enough surgical trauma to the oval<br />
window mucoperiosteum to lead to the production of an inflammatory repair<br />
envelope around the prosthesis, sealing the opening into the oval window. With<br />
symptoms of a perilymphatic fistula or fluctuating hearing loss, tinnitus, a feeling<br />
of fullness in the ear and vertigo, there is no doubt that a small fistula remained<br />
after many stapedectomy operations with incomplete closure of air bone gap, but<br />
the hearing result may be acceptable to the patient. Although a perilymph fistula<br />
usually leads to sensorineural hearing loss, this is not always the case and a<br />
persistent conductive loss after an operation should warn the surgeon that there<br />
might be a fistula. A revision operation to close it would be the best line of<br />
treatment. The fistula may be primary, dating from the time of operation when<br />
there is a failure of the oval window to seal, or it may be secondary, where it can<br />
appear many months or even years after the original operation. Hearing tests<br />
carried out soon after the onset of fistula will show findings similar to those seen in<br />
labyrinthine hydrops. For example, puretone sensorineural hearing loss and low<br />
frequency initially, followed by a flat loss that fluctuates. There may be recruitment<br />
as well. Vestibular tests such as the Hallpike caloric test, EMG, and fistula test with<br />
a pneumatic otoscope may all be helpful, but have been found to be negative in<br />
20% of the cases. Welder described a newer technique, diagnosis by radioactive<br />
Indian-111 that is injected into the lumbar subarachnoid space. The demonstration<br />
of an increased radioactivity in the nasopharyngeal secretions strongly supports the<br />
diagnosis of a fistula.<br />
The treatment of a perilymphatic fistula is a tympanotomy at the earliest possible<br />
moment with an attempt to close the fistula. When the leak is detected, the fistulous<br />
track is excised and the prosthesis removed with great care. The opening of the<br />
vestibule is covered with a soft tissue graft that is held in place by another<br />
http://www.bcm.edu/oto/grand/111199.htm (9 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
prosthesis. Unless early treatment is instituted, the chances of restoration or<br />
improvement of hearing are small. In some cases troublesome dysequilibrium may<br />
remain. It is imperative that the surgeon is fully aware of these complications and<br />
realizes that some techniques are safer than others. The use of Gelfoam to seal the<br />
oval window in stapedectomy produces a very thin membrane and has caused the<br />
highest incidence of fistula formation. The perilymphatic fistula is the only<br />
complication of stapedectomy that is dangerous, and although the risk of meningitis<br />
is small, death from meningitis after this operation has been reported.<br />
As with the perilymphatic fistula, postoperative granulomas can also be a cause of<br />
dysequilibrium, vertigo or progressive sensorineural hearing loss. Granuloma<br />
formation is seen in approximately 1:100 cases of revision stapedectomy. Foreign<br />
body reaction is a suspected etiology of postoperative granuloma formation. Glove,<br />
starch and Teflon have all been implicated. For this reason, direct pullout prosthesis<br />
contact should be avoided. It may also be prudent to rinse the prosthesis prior to its<br />
insertion. The condition usually manifests between the 5th and 15th postoperative<br />
day and is characterized symptomatically by hearing loss after an initial hearing<br />
gain or a sensation of unsteadiness. Associated with the hearing loss are loss of<br />
speech discrimination and a sensation of fullness in the ear. Examination reveals an<br />
edematous, thickened and hypervascular skin flap as well as dullness and reddening<br />
at the posterior part of the tympanic membrane. Audiometric studies show a<br />
combined sensorineural and conductive hearing loss that is worse in the higher<br />
frequency that is also associated with decreased speech discrimination. High-dose<br />
steroids may decrease the inflammatory response and its effects on the inner ear.<br />
Emergency surgical intervention is imperative. Surgical exploration reveals a<br />
granulomatous mass extending from the oval window niche to completely envelop<br />
the prosthesis and the long process of the incus. In about half of the cases the<br />
granuloma extends into the vestibule. The granuloma, including the portion within<br />
the vestibule, must be removed in its entirety along with the prosthesis. They may<br />
also be vaporized with laser after the prosthesis has been removed.<br />
Cholesteatoma following stapedectomy is a rare complication. Mawson reported<br />
only one post-stapedectomy cholesteatoma in a review of nearly 2000 cases. Only<br />
five other cases have been previously reported in the literature. Proposed<br />
mechanisms for formation include prosthesis extrusion, the presence of a squamous<br />
epithelium in the fascial graft, inversion of the tympanomeatal flap and a marginal<br />
perforation associated with a disruptive annulus.<br />
Diplacusis occurs in approximately one-third of the patients. There may be a<br />
variation of distortion of sound, especially music and the human voice, of which<br />
patients frequently complain. For the first few weeks after the operation most<br />
people complain of pure tones appearing higher in pitch when compared with the<br />
unoperated side. It is seldom problematic and usually fades by six weeks<br />
http://www.bcm.edu/oto/grand/111199.htm (10 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
postoperatively. Almost all patients have some degree of phonophobia<br />
postoperatively as well. Reassurance is adequate treatment. A subset of this has<br />
been documented as an abnormal, emotional response. In a 1993 article in<br />
Laryngoscope, Lloyd Stores describes such a case:<br />
"This is the most curious and unexpected phenomena that I have ever encountered.<br />
They brought this girl in that I had performed the stapedectomy a few days prior.<br />
Honestly, her mouth was open and fixed and she had a glassy stare. From the<br />
history, it turns out that her symptoms developed almost immediately after I took<br />
the first packing out of her ear canal. The mother-in-law was a talker and she<br />
continued to talk about how useless her daughter-in-law was. The daughter-in-law,<br />
my patient, had not been hearing all of this for years and she went into a catatonic<br />
trance that was unbelievable. She really freaked."<br />
In conclusion, we have come a long way from the original attempts at mobilization<br />
of the stapes by Kessel, as resurrected by Rosen, which led to the modern day<br />
stapedectomy performed by Shea. A survey of articles in the last 30 years<br />
concerning the complications of stapedectomy indicates that although there are<br />
some differences over the relative importance attributed to a certain problem, there<br />
is general agreement about the direction in which new research should be directed.<br />
The situation is well summarized by Dr. Shea in his 40-year report on over 14,449<br />
stapedectomies, where he makes the observation that although the original<br />
objections to stapedectomy have all but disappeared, it is now increasingly<br />
necessarily to concentrate on the problems arising from the operation itself.<br />
Case Report<br />
I.K. is a 36-year-old Indian male who presents to the BTGH clinic with a several<br />
year history of progressively worsening hearing loss in his left ear. The patient has<br />
previously undergone an unknown middle ear procedure on the right ear,<br />
performed in another state for hearing loss. Of note is that the patient's mother and<br />
father also have had some degree of hearing loss. An audiogram obtained on March<br />
23, 1999 revealed a 40-50 decibel conductive hearing loss in the left ear with a pure<br />
tone average of 67 decibels. On physical exam, the patient had an unremarkable<br />
head and neck examination except for his conductive hearing loss. The patient was<br />
taken to the operating room on April 13, 1999. Upon elevation of the patient's<br />
tympanomeatal flap, there was a narrowed oval window niche. The facial nerve<br />
was in the fallopian canal without dehiscence. The stapes was fixed with diffuse<br />
otosclerosis of the footplate. A 0.8 mm diamond drill was then used to thin the<br />
thickened footplate. The footplate was then perforated and a 4.0 mm Fisch stapes<br />
piston was placed.<br />
http://www.bcm.edu/oto/grand/111199.htm (11 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Postoperatively, the patient did well, and during the first 15 days, he stated that his<br />
hearing was markedly improved. On post operative day 16, the patient experienced<br />
a sudden decrease of hearing in that ear. There were no associated symptoms of<br />
vertigo, otorrhea or ear pain. A repeat audiogram was performed which revealed<br />
similar results as the preoperative test. The patient was thus taken to the operating<br />
room again on June 17, 1999, for a middle ear exploration, where it was noticed<br />
that the oval window was once again obliterated. It was demonstrated that the<br />
prosthesis was no longer sitting in the oval window, but was surrounded and riding<br />
on top of a thickened and obliterated footplate. A re-drill out of the oval window<br />
was performed, and the vestibule was entered carefully with a sharp pick. A longer<br />
4.5mm Fisch prosthesis was then used. Postoperatively, the patient was started on<br />
sodium fluoride. Unfortunately, the patient never returned for a postoperative visit.<br />
Bibliography<br />
Backous DD, Coker NJ, Jenkins HA. Prospective study of resident-performed stapedectomy. Am<br />
J Otol 1993;14:451-454.<br />
Beales PH. Otosclerosis. Triangle West, Bristol: John Wright & Sons; 1981. pp 85-185.<br />
Belal A Jr, Ylikoski J. Poststapedectomy dizziness. A histopathologic report. Am J Otol<br />
1982;3:187-191.<br />
Bhardwaj BK, Kacker SK. Revision stapes surgery. J Laryngol Otol 1988;102:20-24.<br />
Bracewell A. Diplacusis binauralis--a complication of stapedectomy. J Laryngol Otol 1966;80:55-<br />
60.<br />
Brackmann DE. Otologic surgery. Philadelphia: Saunders; 1994. pp 347-384.<br />
Burnam JA, Lazar L, Pickard RE. Cholesteatoma: A complication of stapedectomy. Eye Ear<br />
Nose Throat 1971;50:324-326.<br />
Causse J, Causse JB. Eighteen years report on stapedectomy: Problems of fixation. Clin<br />
Otolaryngol 1980;5:49-59.<br />
Clairmont AA, Nicholson WL, Turner JS. Pseudomonas aeruginosa meningitis following<br />
stapedectomy. Laryngoscope 1975;85:1076-1083.<br />
Coker NJ, Duncan NO, Wright GL, Jenkins HA, Alford BR. Stapedectomy trends for the<br />
resident. Ann Otol Rhinol Laryngol 1988;97:109-113.<br />
http://www.bcm.edu/oto/grand/111199.htm (12 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Cremers CW, Hombergen GC, Wentges RT. Perilymphatic gusher and stapes surgery. A<br />
predictable complication? Clin Otolaryngol 1983;8:235-240.<br />
Derlacki EL. Revision stapes surgery: Problems with some solutions. Laryngoscope<br />
1985;95:1047-1053.<br />
Dornhoffer JL, Bailey HA, Jr., Graham SS. Long-term hearing results following stapedotomy.<br />
Am J Otol 1994;15:674-678.<br />
Doyle PJ, Woodham J. Results of stapes surgery - subjective and objective. J Otolaryngol<br />
1980;9:381-386.<br />
Fenton JE, Turner J, Shirazi A, Fagan PA. Post-stapedectomy reparative granuloma: A<br />
misnomer. J Laryngol Otol 1996;110:185-188.<br />
Ferguson BJ, Gillespie CA, Kenan PD, Farmer JC Jr. Mechanisms of cholesteatoma formation<br />
following stapedectomy. Am J Otol 1986;7:420-424.<br />
Flood LM, Kemink JL, Kartush JM. Pneumocephalus following treatment of a stapes gusher. Am<br />
J Otol 1985;6:508-511.<br />
Franklin DJ, Pollak A, Fisch U. Meniere's symptoms resulting from bilateral otosclerotic<br />
occlusion of the endolymphatic duct: An analysis of a causal relationship between otosclerosis<br />
and Meniere's disease. Am J Otol 1990;11:135-140.<br />
Freeman J. Failures in surgery for stapedial otosclerosis. Laryngoscope 1981;91:1245-1258.<br />
Hammerschlag PE, Fishman A, Scheer AA. A review of 308 cases of revision stapedectomy.<br />
Laryngoscope 1998;108:1794-1800.<br />
Horn KL. Surgical management of otosclerosis: Primary stapes surgery. Oper Tech Otolaryngol<br />
Head Neck Surg1998;9:1-12.<br />
Gibb AG, Pang YT. Surgical treatment of tympanosclerosis. Eur Arch Otorhinolaryngol<br />
1995;252:1-10.<br />
Glasscock ME 3rd, Storper IS, Haynes DS, Bohrer PS. Twenty-five years of experience with<br />
stapedectomy. Laryngoscope 1995;105:899-904.<br />
Hough JV, Dyer RK Jr. Stapedectomy. Causes of failure and revision surgery in otosclerosis.<br />
Otolaryngol Clin North Am 1993;26:453-470.<br />
Krieger LW, Lippy WH, Schuring AG, Rizer FM. Revision stapedectomy for incus erosion:<br />
Long term hearing. Otolaryngol Head Neck Surg 1998;119:370-373.<br />
http://www.bcm.edu/oto/grand/111199.htm (13 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Krmpotic-Nemanic J, Draf W, Helms J. Surgical Anatomy of the Head and Neck. Berlin,<br />
Germany: Springer Verlag, 1985.<br />
Langman AW, Lindeman RC. Revision stapedectomy. Laryngoscope 1993;103:954-958.<br />
Leighton SE, Robson AK, Freeland AP. Audit of stapedectomy results in a teaching hospital.<br />
Clin Otolaryngol 1991;16:488-492.<br />
Man A, Segal S. Serous otitis media as a complication of stapedectomy. Ear Nose Throat J<br />
1980;59:510-513.<br />
Mann WJ, Amedee RG, Fuerst G, Tabb HG. Hearing loss as a complication of stapes surgery.<br />
Otolaryngol Head Neck Surg 1996;115:324-328.<br />
Mawson SR. Management of complication of stapdectomy. J Laryngol Otol 1975;89:145-149.<br />
Merifield DO. Epithelial cyst as a complication of stapedectomy: A case report. Laryngoscope<br />
1965;75:1893-1896.<br />
Meyer SE. The effect of stapes surgery on high frequency hearing in patients with otosclerosis.<br />
Am J Otol 1999;20:36-40.<br />
Miglets AW, Paparella MM, Saunders WH. Atlas of Ear Surgery. St. Louis, MO: Mosby; 1986.<br />
Millman B, Giddings NA, Cole JM. Long-term follow-up of stapedectomy in children and<br />
adolescents. Otolaryngol Head Neck Surg 1996;115:78-81.<br />
Milstein S. Otosclerosis. Am J Otol 1981;2:283-285.<br />
Morrison AW. Otosclerosis. Br Med J 1962;1:1804.<br />
Parnes LS, Wong L. Pneumo-membranous labyrinth: An unusual complication of a<br />
stapedectomy. Ann Otol Rhinol Laryngol 1998;107:359-361.<br />
Pedersen CB. Revision surgery in otosclerosis--an investigation of the factors which influence<br />
the hearing result. Clin Otolaryngol 1996;21:385-388.<br />
Portmann M, Portmann D. Otologic Surgery: Manual of Oto-surgical Techniques, 2nd ed. San<br />
Diego, CA: Singular Publishing Group; 1998. pp 32-38.<br />
Schuknecht HF. Stapedectomy. Boston, MA: Little Brown; 1971.<br />
Schuknecht HF, Jones DD. Stapedectomy post-mortem findings. Ann Otol Rhinol Laryngol<br />
1979;88:1-43.<br />
http://www.bcm.edu/oto/grand/111199.htm (14 of 15) [5.11.2005 10:44:32]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Shapira A, Ophir D, Marshak G. Success of stapedectomy performed by residents. Am J<br />
Otolaryngol 1985;6:388-391.<br />
Shea JJ. Stapedectomy - long-term report. Ann Otol Rhinol Laryngol 1982;91:516-520.<br />
Shea JJ, Farrior JB. Stapedectomy and round window closure. Laryngoscope 1987;97:10-12.<br />
Shea JJ Jr. Forty years of stapes surgery. Am J Otol 1998;19:52-55.<br />
Shea JJ Jr. A personal history of stapedectomy. Am J Otol 1998;19:S2-S12.<br />
Sheehy JL, Nelson RA, House HP. Revision stapedectomy: A review of 258 cases. Laryngoscope<br />
1981;91:43-51.<br />
Silverstein H. Laser stapedotomy minus prosthesis (laser STAMP): A minimally invasive<br />
procedure. Am J Otol 1998;19:277-282.<br />
Slattery WH 3rd, House JW. Prostheses for stapes surgery. Otolaryngol Clin North Am<br />
1995;28:253-264.<br />
Smyth GD, Hassard TH. Eighteen years experience in stapedectomy. The case for the small<br />
fenestra operation. Ann Otol Rhinol Laryngol Suppl 1978;87:3-36.<br />
Storrs LA. Complications after surgery for otosclerosis. Laryngoscope 1983;93:265-267.<br />
Wiet RJ, Raslan W, Shambaugh GE Jr. Otosclerosis 1981 to 1985. Our four-year review and<br />
current perspective. Am J Otol 1986;7:221-228.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCM Otolaryngology Home Page<br />
©2001, The Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences,<br />
Baylor College of Medicine<br />
One Baylor Plaza, NA102, Houston, TX 77030 oto@bcm.tmc.edu<br />
URL: http://www.bcm.tmc.edu/oto (Modified: 11/08/01)<br />
http://www.bcm.edu/oto/grand/111199.htm (15 of 15) [5.11.2005 10:44:32]
http://www.bcm.edu/oto/grand/2692.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
ISSUES IN STAPEDECTOMY<br />
Douglas D. Backous, MD<br />
February 6, 1992<br />
The history of stapedectomy is one of near discovery, condemnation, reintroduction and refinement.<br />
Prior to the twentieth century poor lighting and magnification, nonstandardized audiometry, and a lack of<br />
understanding of the middle ear conduction mechanism plagued early researchers. Procedures<br />
concentrated on either partial or total removal of the tympanic membrane and ossicles. Mobilization of<br />
the stapes, described by Miot and later by Blake, would eventually be condemned by the otologic world.<br />
Siebenmann, in 1900, capped the early era of stapes surgery by stating, "Clinical experience teaches that<br />
all endeavors at mobilization of the stapes in otosclerosis are not only useless but often harmful."<br />
Between 1900 and 1952 attempts at fenestration of the horizontal semicircular canal came to the<br />
spotlight. Results were reported as excellent but temporary. Microscopy and rotating drills were<br />
http://www.bcm.edu/oto/grand/2692.html (1 of 5) [5.11.2005 10:44:37]
http://www.bcm.edu/oto/grand/2692.html<br />
introduced. In 1929 the American Otologic Society commissioned a committee to compile a resume of<br />
all literature concerning otosclerosis up to 1928. The result included a 700 page, two volume document<br />
covering histology of the otic capsule, heredity, audiology, and treatment of otosclerosis.<br />
Successful surgery for hearing restoration truly began with Lempert's fenestration operation. Rosen, a<br />
student of Lempert, serendipitously discovered that footplate mobilization improved hearing immediately<br />
in a patient with otosclerosis. He continued to refine his mobilization procedure until Shea, his student,<br />
reopened the era of stapedectomy in 1956. Shea developed the modern technique of footplate<br />
mobilization, soft tissue grafting of the oval window, and ossicular replacement.<br />
Shea is also credited with the first stapedotomy, performed on a young girl in 1960. A 6 millimeter<br />
stapedotomy with piston insertion and soft tissue packing provides equally improved hearing with less<br />
risk for damage to inner ear structures. Higher frequency hearing is preserved better with stapedotomy.<br />
Robinson summed up the stapedectomy/stapedotomy debate best by declaring the "best" procedure is the<br />
operation which provides the individual surgeon with a predictable and safe outcome along with<br />
improved hearing to levels consistent with current otologic standards.<br />
Depletion of the pool of patients with otosclerosis occurred during the "golden age" of stapes surgery<br />
throughout the sixty's and early seventies. Increased numbers of trained otolaryngologists and improved<br />
hearing amplification further contribute to an overall limited exposure in modern practice and residency.<br />
Stapedectomy is the second least performed procedure in American residency, as shown by Harris and<br />
Osborne in 1990.<br />
The issue of training residents to do successful stapedectomy first appeared in the literature in 1983.<br />
Chandler and Rodriguez-Torro revealed a 62% closure of the air-bone gap to within 10 dB in resident<br />
cases, well below the 90-95% standard expected of practicing otologists. Five studies of results from<br />
training programs have since revealed results ranging from 64%-82% closure to within 10 Db in training<br />
programs. Of interest are the results of Shapira, et al. Their residents, in Israel, did stapedectomy in all<br />
four years of training. Results during the first two years of residency compared with American programs.<br />
During the second two years, however, results approached and often equaled those of staff. These<br />
findings further emphasized the critical importance of adequate numbers of procedures to insure<br />
acquisition of competence.<br />
Solutions to the problem of numbers of cases include increased observation of otologic procedures with<br />
correlation in the temporal bone laboratory. Residents should display competence in surgery for chronic<br />
middle ear disease prior to attempting stapedectomy. Finally, all procedures should be supervised by<br />
senior otologic staff and one consistent technique used. For physicians in practice, batching<br />
stapedectomies into groups with review of needed skills in the temporal bone lab followed by<br />
consecutive case completion and review of results could provide valuable feedback in regard to outcome<br />
and maintenance of required skills.<br />
In summary, stapedectomy has a fascinating history. Had Rosen not been open-minded to his first<br />
http://www.bcm.edu/oto/grand/2692.html (2 of 5) [5.11.2005 10:44:37]
http://www.bcm.edu/oto/grand/2692.html<br />
accidental mobilization, more delay in technique development was inevitable. The best procedure is<br />
surgeon dependent varying with individual skills and experience. Otosclerosis is now at a steady<br />
incidence making increased work in the temporal bone laboratory mandatory for both the acquisition and<br />
maintenance of required skills in footplate manipulation.<br />
Case Presentation<br />
A 68-year-old white male presented with a fifteen year history of progressive hearing loss. He had the<br />
most difficulty hearing in small group conversations. He denied tinnitus, dizziness, otalgia, or chronic<br />
middle ear infections. He did admit to a long history of loud noise exposure. Past surgical and medical<br />
histories were unremarkable. Weber exam showed localization to the right. Audiometry revealed normal<br />
to moderate sensorineural and severe to moderate conductive loss in the right ear with absence of<br />
acoustic reflexes. The left ear had mild to moderate sensorineural loss with normal acoustic immittance<br />
measures. Speech intelligibility scores were within the normal range bilaterally. The patient underwent<br />
right middle ear exploration, stapedectomy, with perichondrial grafting over the oval window and<br />
insertion of a standard well Robinson prosthesis.<br />
Bibliography<br />
Alford BR. Residency program length and structure. Otolaryngol Head Neck Surg 1983;91:1228-230.<br />
Alford BR. Chance favors the prepared mind. The Crowe Lecture, Johns Hopkins School of Medicine, October 2, 1986.<br />
Bailey HA, Pappas JJ, Graham SS. Small fenestra stapedectomy technique: reducing risk and improving hearing.<br />
Otolaryngol Head Neck Surg 1983;91:516-519.<br />
Benecke JE. Editorial. Am J Otol 1990;11:78.<br />
Chandler JR, Rodriguez-Torro OE. Changing patterns of otosclerosis surgery in teaching institutions. Otolaryngol Head<br />
Neck Surg 1983;91:239-245.<br />
Coker NJ, Duncan NO, Wright GL, Jenkins HA, Alford BR. Stapedectomy trends for the resident. Ann Otol Rhinol<br />
Laryngol 1988;97:109-113.<br />
Conrad GJ. Collective stapedectomy (an approach to the numbers problem). J Laryngol Oto 1990;104:390-393.<br />
Cummings CW, Fredrickson JM, Harker LA, et al. Otolaryngology-Head and Neck Surgery, Vol. IV. St Louis, Toronto:<br />
C. V. Mosby Company, 1986:1095-3113.<br />
http://www.bcm.edu/oto/grand/2692.html (3 of 5) [5.11.2005 10:44:37]
http://www.bcm.edu/oto/grand/2692.html<br />
Engel TL, Schindler RA. Stapedectomy in residency training. Laryngoscope 1984;94:768-771.<br />
Farrior B. Contraindication to the small hole stapedectomy. Ann Otol 1981;90:636-639.<br />
Farrior JB. Stapedectomy for the home temporal bone dissection laboratory. Otolaryngol Head Neck Surg 1986;94:521-<br />
525.<br />
Fisch U. Stapedotomy versus stapedectomy. Am J Otol 1982;4:112-117.<br />
Fisch U. Tympanoplasty and Stapedectomy. New York: Theime-Skatton Inc. 1980:57-67.<br />
Glasscock MF, Shambaugh GE. Surgery of The Ear, 4th ed. Philadelphia: WB Saunders, Co., 1980:389-418.<br />
Gristwood RE. The surgical concept for otosclerosis. Adv Oto-Rhino-Laryngol 1988;39:52-64.<br />
Jerger SJ, Jerger JJ. Auditory Disorders: A Manual for Clinical Disorders. Boston: Little, Brown and Company, 1981:131-<br />
136.<br />
Handley GH, Hicks JN. Stapedectomy in residency - the UAB experience. Am J Otol 1990;11:128-130.<br />
Harris JP, Osborne E. A surgery of otologic training in US residency programs. Arch Otolaryngol Head Neck Surg<br />
1990;116:342-344.<br />
Hillel AD. History of stapedectomy. Am J Otolaryngol 1983;4:131-140.<br />
Hughes GB. The learning curve in stapes surgery. Laryngoscope 1991;101:1280-1284.<br />
Igarashi M, Guilford R, Alford BR. Bilateral vein graft stapedectomy. Acta Otolaryngol 1970;69:9499.<br />
Rosen S. The Autobiography of Dr. Samuel Rosen. New York: Knopf, 1980:48-68.<br />
Levin G, Fabian P, Stahle J. Incidence of otosclerosis. Am J Otol 1988;9:299-301.<br />
Levenson MJ, Bellucci RJ, Grimes C, et al. Otosclerosis surgery in a resident training program. Arch Otolaryngol Head<br />
Neck Surg 1987;113:29-31.<br />
Levy R, Shvero J, Hadar T. Stapedotomy technique and results: ten years' experience and comparative study with<br />
stapedectomy. Laryngoscope 1990;100:1097-1099.<br />
McGee TM. Comparison of small fenestra and total stapedectomy. Ann Otol 1981;90:633-635.<br />
Manu P, Lane TJ, Matthews DA. How much practice makes perfect? A quantitative measure of the experience needed to<br />
achieve procedural competence. Med Teacher 1990;12:367-369.<br />
http://www.bcm.edu/oto/grand/2692.html (4 of 5) [5.11.2005 10:44:37]
http://www.bcm.edu/oto/grand/2692.html<br />
Marquet J, Creten WL, Van Camp KJ. Considerations about the surgical approach in stapedectomy. Acta Otolaryngol<br />
1972;74:406-410.<br />
Moon CN. Stapedectomy, connective tissue graft and stainless steel prosthesis. Laryngoscope 1968;78:798-807.<br />
Murrant NJ, Gatland DJ. Temporal bone laboratory training for stapedectomy. J Laryngol Otol 1989;103:833-834.<br />
Robinson M. Panel on stapes surgery - total footplate extraction in stapedectomy. Ann Otol 1981;90:630-632.<br />
Robinson M. Is there a "best" stapedectomy technique for the general otolaryngologist? Ear Nose Throat J 1989;68:221-<br />
224.<br />
Rosen S. Palpation of the stapes for fixation. Arch Otolaryngol 1952;56:610-5.<br />
Shapira A, Ophir D, Marshak G. Success of stapedectomy performed by residents. Am J Otolaryngol 1985;6:388-391.<br />
Shea JJ. Fenestration of the oval window. Ann Otol Rhinol Laryngol 1958;67:932-51.<br />
Shea JJ. Thirty years of stapes surgery. J Laryngol Otol 1988;102:14-19.<br />
Schuknecht HF. Editorial-Training in otolaryngology. Arch Otolaryngol 1979;105:57.<br />
Smyth GDL, Hassard TH. Eighteen years experience in stapedectomy-the case for the small fenestra operation. Ann Otol<br />
Rhinol Laryngol 1978;87:3-36.<br />
Vernick DM. Stapedectomy results in a residency training program. Ann Otol Rhinol Laryngol 1986;95:477-479.<br />
Vernick DM. Who operated on Max? Ear Nose Throat 1988;67:125.<br />
Weir N. Otolaryngology: An Illustrated History. London: Butterworth, 1990:203-212.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/2692.html (5 of 5) [5.11.2005 10:44:37]
http://www.bcm.edu/oto/grand/3592.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
SUDDEN SENSORINEURAL HEARING LOSS<br />
Randall S. Zane, MD<br />
March 5, 1992<br />
Sudden sensorineural hearing loss is a confusing and controversial issue in otolaryngology that most of<br />
us will encounter in our practice. The impact of the loss of hearing on the patient can be catastrophic and<br />
most physicians consider it a medical emergency. On the other hand, it usually becomes frustrating for<br />
the physician, as the cause is most often not obvious and the treatment empiric and poorly understood.<br />
There is no accepted definition of the problem, no standard method for evaluating these patients, no<br />
agreement on what the usual etiology is, no easy way to stage the loss and no clearly effective treatment.<br />
Some authors feel strongly that sudden sensorineural hearing loss is just a symptom and not a disease<br />
entity. The most useful definition of sudden sensorineural hearing loss is an idiopathic loss greater than<br />
30 Db in three contiguous frequencies and that occurs in less than 3 days. Most sudden losses occur<br />
http://www.bcm.edu/oto/grand/3592.html (1 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/3592.html<br />
within minutes to several hours, and about 1/3 of these patients awaken in the morning with a hearing<br />
loss. Approximately 1/2 note imbalance or vertigo and the intensity of vertigo correlates in general with<br />
the degree of hearing loss. Byl reported an incidence of between 5-20 cases per 100,000 population per<br />
year.<br />
Doug Mattox and Blair Simmons at Stanford reported a 5 year prospective study involving 166 patients,<br />
looking at the natural history of the process. They found that males and females were equally affected<br />
with a mean age of 46 years. There was no seasonal or geographic clustering. They noted that 65% of<br />
patients showed some degree of recovery without any medical or surgical intervention at all. The<br />
likelihood of recovery was influenced by the shape of the audiogram - all but one patient with an upward<br />
sloping audiogram had complete or good recovery and all but two patients with a severely downsloping<br />
audiogram had a fair or poor recovery. Other poor prognostic indicators that are generally agreed upon in<br />
the literature include sensitivity loss greater than 90 Db in the mid-frequencies, advanced age, and the<br />
presence of vertigo. In his triologic thesis, Dr. Frederick Byl compiled data from 225 patients over an<br />
eight year period forming a prognostic table. He also noted the direct relationship between the severity of<br />
the initial hearing loss and potential recovery and recorded several modifying factors. The study<br />
confirmed that the sooner a patient is seen, the better the prognosis for recovery.<br />
Unfortunately, there is no better understanding of the etiology of sudden sensorineural hearing loss than<br />
there was 1 or 2 decades ago. It is certain that there is no single etiology -the loss of hearing is just the<br />
final outcome for many potential insults to the inner ear. The four most accepted hypothetical etiologies<br />
are viral infections, vascular insult, labyrinthine membrane rupture, and autoimmune disease.<br />
Although viral infection of the inner ear is an attractive theoretical explanation for sudden hearing loss,<br />
the supporting evidence is not conclusive and consists of 4 types:<br />
1) coincident symptoms suggesting coincident viral infection;<br />
2) serological data showing coincident viral infection;<br />
3) histopathological studies showing similarities between known viral infections and cases of sudden<br />
hearing loss;<br />
4) extrapolations from the degeneration of the inner ear seen in viral disease such as the prenatal rubella<br />
syndrome.<br />
Uncontrolled studies from Van Dishoeck, Jaffe, and Schuknecht reported "flu-like" symptoms in 20 -<br />
60% of patients suffering idiopathic sudden sensorineural hearing loss. However, a study by Rowson and<br />
Hinchcliffe in 1975 found the same symptoms of upper respiratory tract infection to be present in<br />
approximately 40% of the general population. Veltri et al looked at 77 unmatched patients with sudden<br />
sensorineural hearing loss and found a conversion rate of 65%. Multiple viruses were implicated<br />
including influenza A and B, rubeola, rubella, mumps, herpes simplex, and CMV. Wilson and coworkers<br />
http://www.bcm.edu/oto/grand/3592.html (2 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/3592.html<br />
studied 122 patients, 63% of whom seroconverted compared with 40% of controls. Other studies from<br />
Morrison and Booth as well as Rowson and Hinchcliffe failed to demonstrate a viral titer rise in sudden<br />
hearing loss patients. The most consistent evidence supporting viral etiology is the histopathologic<br />
findings of varying degrees of atrophy of the organ of Corti, stria vascularis, and tectorial membrane with<br />
variable loss of the neuronal population as shown by Schuknecht and others. Perhaps the strongest<br />
evidence for the involvement of viruses in hearing loss comes from the use of immunofluorescent antigen<br />
studies such as those performed by Davis and Johnson, demonstrating the ability of rubeola and mumps<br />
to infect the inner ears of animal models.<br />
A vascular cause for sudden hearing loss is attractive because it is logically consistent with immediate<br />
onset of symptoms and because there are established models of acute hearing loss secondary to vascular<br />
occlusion in hypercoagulable states such as leukemia and sickle cell disease. However, most of the<br />
experimental and clinical evidence casts serious doubt on a vascular etiology. One would expect that<br />
older patients with known peripheral vascular disease would be the ones most often afflicted, but in fact,<br />
most patients are younger and have no stigmata of systemic vascular disease. Perlman and other<br />
investigators have demonstrated permanent loss of the cochlear microphonic and action potential occurs<br />
after only 30 minutes of ischemia. The histopathology of ears affected by sudden hearing loss also differs<br />
significantly from temporal bones examined after experimental vascular occlusion. Permanent<br />
obstruction leads to marked degeneration of the neurons followed by fibrous and osseous proliferation<br />
within the inner ear, changes that are not seen typically in sudden sensorineural hearing loss.<br />
Intracochlear membrane breaks were proposed as a cause of sudden hearing loss by Simmons in 1968,<br />
but the evidence is only coincidental. Schuknecht and Donovan studied 12 temporal bones of patients<br />
afflicted with sudden sensorineural hearing loss, and found no evidence of Reissner's or basilar<br />
membrane rupture.<br />
There are several known autoimmune diseases that are epidemiologically associated with sudden<br />
sensorineural hearing loss, including Cogan's syndrome, systemic lupus erythematosus, and temporal<br />
arteritis. Some of the most convincing evidence has come out of the University of Tennessee by Yoo and<br />
coworkers who showed that monoclonal antibodies specific for type II collagen can activate an<br />
immunologic response in the inner ear of the rat leading to sensorineural hearing loss as documented by<br />
ABR testing. They were able to demonstrate perivascular inflammation and fibrosis and degeneration of<br />
the spiral ganglion on histopathology, and using immunofluorescent techniques they saw immune<br />
complexes in the otic capsule.<br />
Unfortunately, the lack of scientific understanding of the etiology or etiologies of the problem limits its<br />
treatment to simple empiricism. Every proposed treatment has study to support it, but corroborative data<br />
from independent researchers is usually lacking. Perhaps the fatal flaw in most of those studies is that a<br />
single treatment is applied to a symptom that undoubtedly has multiple etiologies.<br />
Wilson and his colleagues did a double blind study of 67 patients with sudden sensorineural hearing loss.<br />
33 were treated with oral steroids and 34 received placebo. 52 additional subjects served as controls. 76%<br />
http://www.bcm.edu/oto/grand/3592.html (3 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/3592.html<br />
of patients who had hearing loss greater than 90 Db failed to recover regardless of whether or not they<br />
received steroids. 78% of the steroid treated patients with hearing loss less than 90 Db improved,<br />
compared with only 38% of matched untreated patients. There have been a few other studies supporting<br />
these findings. However, Dr. Wilson returned to his lab and several years later published a report failing<br />
to demonstrate improved recoveries in patients with proven viral antibody seroconversions treated with<br />
steroids.<br />
The use of diuretics is sort of borrowed from their use in the treatment of Meniere's disease. The use of<br />
heparin and warfarin is borrowed from their use in cerebral vascular occlusion in which they seem to<br />
promote better collateral circulation. Dextran is an example of an effective plasma expander that is useful<br />
in reducing red cell sludging and improving microcirculation. Stellate ganglion blocks produce Horner's<br />
syndrome with vasodilation and increased blood flow and is done by making an injection lateral and<br />
inferior to the thyroid gland to the C-7 vertebra, and then backing off slightly to the area of the ganglion<br />
and injecting Lidocaine. Haug, Draper and Haug demonstrated a 70% chance for a patient to recover a 10<br />
Db pure tone gain and 10 dB discrimination improvement with this procedure compared to a 20% chance<br />
of a similar gain if not treated with stellate ganglion blocks. They also noted that the most successful<br />
cases were treated in the first 20 weeks after symptoms appeared. Some of the vasodilators commonly<br />
employed include nylidrin hydrochloride, papaverine hydrochloride, nicotinic acid, histamine, atropine,<br />
and carbogen. Despite the many studies over the years looking at various vasodilators, there has been no<br />
adequately controlled study that supports the use of vasodilators in sudden hearing loss. Suga and Snow<br />
in their 1969 report actually demonstrated experimentally that vasodilators could in fact reduce cochlear<br />
blood flow by causing shunting. Professor Fisch performed several elegant studies and concluded that<br />
carbogen was the safest and most effective.<br />
"Shotgun" therapy includes as many potentially helpful treatment regimens as can be safely combined.<br />
However, there are very few studies looking at the efficacy of shotgun therapy and those that do exist<br />
obviously have so many variables that they are impossible to control for.<br />
The workup and shotgun regimen recommended by the faculty here at Baylor is attached. This treatment<br />
protocol was put together based in part on the experience of the faculty and in part on the information<br />
available in the literature, but again there is no scientific data to show that it is any more effective than<br />
other treatment protocols or even expectant observation.<br />
In summary, sudden sensorineural hearing loss remains a poorly understood and frustrating problem for<br />
the otolaryngologist. More rational treatment will probably only follow the elucidation of the specific<br />
cause or causes of this disease process.<br />
Case Presentation<br />
A 55-year-old healthy white male smoker with no previous otologic history, noted the acute loss of<br />
http://www.bcm.edu/oto/grand/3592.html (4 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/3592.html<br />
hearing in his right ear during his usual morning activities. He denied strenuous activity stating that he<br />
had finished brushing his teeth and began to put on his clothes when he suddenly noted a crescendo high<br />
pitched tone in his right ear and inability to hear. There were no other associated symptoms of dizziness<br />
or visual change. After several hours without improvement, he presented to the emergency room and an<br />
otorhinolaryngology consult was obtained. Head and neck examination including otoscopy was<br />
completely normal. An audiogram revealed a severe primarily sensorineural sensitivity loss on the right.<br />
Laboratory studies including SMA-20, CBC, thyroid function tests, and urinalysis were within normal<br />
limits. Syphilis serology was non-reactive and erythrocyte sedimentation rate was minimally elevated at<br />
15 mm/hr. The veteran was admitted and placed on the Baylor sudden sensorineural hearing loss protocol<br />
which will be described.<br />
Bibliography<br />
Alford BR, Shaver EF, Rosenberg JJ, Guildford FR. Physiologic and histopathologic effects of microembolization of the<br />
internal auditory artery. Ann Otol Rhinol Laryngol 1965;74:728748.<br />
Anderson RG, Meyerhoff WI. Sudden sensorineural hearing loss. Otolaryngol Clin N Am 1981;16:189195.<br />
Beal DD, Hemenway WG, Lindsay JR. Inner ear pathology of sudden deafness: the histopathology of acquired deafness in<br />
the adult coincident with viral infection. Arch Otolaryngol 1967;85:591598.<br />
Belal A, Jr. Pathology of vascular sensorineural hearing impairment. Laryngoscope 1980;90:18311839.<br />
Bredenkamp JK, Shelton C. Sudden hearing loss: determining the specific cause and the most appropriate treatment.<br />
Postgrad Med 1989;86:125132.<br />
Byl FM. Seventysix cases of presumed sudden hearing loss occurring in 1973: prognosis and incidence. Laryngoscope<br />
1977;87:817825.<br />
Byl FM. Sudden hearing loss: eight years experience and suggested prognostic table. Laryngoscope 1984;94:647661.<br />
Cole RR, Jahrsdoerfer RA. Sudden hearing loss: an update. Am J Otol 1988;9:211215.<br />
DeKleyn A. Sudden complete or partial loss of function in the octavus system in apparently normal persons. Acta<br />
Otolaryngol 1944;32:407425.<br />
Donaldson JA. Heparin therapy of sudden sensorineural hearing loss. Arch Otolaryngol 1979;105:351352.<br />
Fisch U. Management of sudden deafness. Otolaryngol Head Neck Surg 1983;91:38.<br />
Fowler E. Sudden deafness. Ann Otol Rhinol Laryngol 1950;59:980987.<br />
http://www.bcm.edu/oto/grand/3592.html (5 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/3592.html<br />
Goodhill W. The "idiopathic group" and the "labyrinthine window rupture group" approaches to sudden sensorineural<br />
hearing loss. In: Snow JB,Jr., editor. Controversy in Otolaryngology. Philadelphia: Saunders, 1980:1220.<br />
Gussen R. Sudden hearing loss associated with vascular origins: a temporal bone study. Ann Otol Rhinol Laryngol<br />
1976;85:94100.<br />
Hallberg O. Sudden deafness of obscure origin. Laryngoscope 1956;66:12371267.<br />
Haug O, Draper L, Haug SA. Stellate ganglion block for idiopathic sensorineural hearing loss. Arch Otolaryngol<br />
1976;102:58.<br />
Igarashi M, Alford BR, Konishi S, Shaver EF, Guilford FR. Functional and histopathological correlates after<br />
microembolization of the peripheral labyrinthine artery in the dog. Laryngoscope 1969;79:602623.<br />
Igarashi M, Card G, Johnson PE, Alford BR. Bilateral sudden hearing loss and metastatic pancreatic adenocarcinoma.<br />
Arch Otolaryngol 1979;105:196199.<br />
Jaffe BF. Sudden deafness: an otologic emergency. Arch Otolaryngol 1967;86:8186.<br />
Jaffe BF. Sudden deafness a local manifestation of systemic disorders: fat emboli, hypercoagulation, and infection.<br />
Laryngoscope 1970;80:788801.<br />
Jaffe BF. Hypercoagulation and other causes of sudden hearing loss. Otolaryngol Clin N Am 1975;8:395403.<br />
Jaffe BF. Clinical studies in sudden deafness. Adv Otorhinolaryngol 1978;20:221228.<br />
Jaffe BF, Maasab HF. Sudden deafness associated with adenovirus infection. N Engl J Med 1967;276:14061409.<br />
Jenkins HA, Pollack AM, Fisch U. Polyarteritis nodosa as a cause of sudden deafness. Am J Otolaryngol 1981;2:99107.<br />
Jerger J, Allen G, Robertson D, Harford E. Hearing loss of sudden onset. Arch Otolaryngol 1961;73:350357.<br />
Kaplan SL, Catlin FI, Weaver T, Feigin RD. Onset of hearing loss in children associated with bacterial meningitis.<br />
Pediatrics 1984;73:575578.<br />
Lipkin AF, Jenkins HA, Coker NJ. Migraine and sudden sensorineural hearing loss. Arch Otolaryngol Head Neck Surg<br />
1987;113:325326.<br />
McCabe BF. Autoimmune sensorineural hearing loss. Ann Otol 1979;88:585-589.<br />
Mattox DE, Lyles CA. Idiopathic sudden sensorineural hearing loss. Am J Otol 1989;10:242247.<br />
Mattox DE, Simmons FB. Natural history of sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol<br />
1977;86:463480.<br />
http://www.bcm.edu/oto/grand/3592.html (6 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/3592.html<br />
Meyerhoff WL. The management of sudden deafness. Laryngoscope 1979;89:18671868.<br />
Meyerhoff WL, Paparella MM. Medical therapy of sudden hearing loss. In: Snow JB, Jr., editor. Controversy in<br />
Otolaryngology. Philadelphia: Saunders, 1980:311.<br />
Nadol J, Wilson W. Treatment of sudden hearing loss is illogical. In: Snow JB, Jr., editor. Controversy in Otolaryngology.<br />
Philadelphia: Saunders, 1980:2332.<br />
Noury KA, Katsarkas A. Sudden unilateral sensorineural hearing loss: a syndrome or a symptom. J Otolaryngol<br />
1989;18:274278.<br />
Ohlms LA, LonsburyMartin BL, Martin GK. Acousticdistortion products: separation of sensory from neural dysfunction in<br />
sensorineural hearing loss in human beings and rabbits. Otolaryngol Head Neck Surg 1991;104:159174.<br />
Rowson K, Hinchicliffe R. A virological and epidemiological study of patients with acute hearing loss. Lancet 1975;1:471-<br />
474.<br />
Schuknecht HF, Benitez J, Beekhuis J, Igarashi M, Singleton G, Ruedi L. The pathology of sudden deafness.<br />
Laryngoscope 1962;72:11421157.<br />
Schuknecht HF, Donovan ED. The pathology of idiopathic sudden sensorineural hearing loss. Arch Otorhinolaryngol<br />
1986;243:115.<br />
Shaia FT, Sheehy JL. Sudden sensorineural hearing impairment: a report of 1220 cases. Laryngoscope 1976;86:389398.<br />
Shikowitz MJ. Sudden sensorineural hearing loss. Med Clin North Am 1991;75:12391250.<br />
Siegel LG. The treatment of idiopathic sudden sensorineural hearing loss. Otolaryngol Clin N Am 1975;8:467473.<br />
Simmons FB. Theory of membrane breaks in sudden hearing loss. Arch Otolaryngol 1968;88:4148.<br />
Singleton G. Cervical sympathetic chain block in sudden deafness. Laryngoscope 1971;81:734.<br />
Suga F, Preston J, Snow JB, Jr. Experimental microembolization of cochlear vessels. Arch Otolaryngol 1970;92:213220.<br />
Suga F, Snow JB, Jr. Cochlear blood flow in response to vasodilating drugs and some related agents. Laryngoscope<br />
1969;79:19561979.<br />
Van Dishoeck H, Bierman T. Sudden perceptive deafness and viral infection. Ann Otol Rhinol Laryngol 1957;66:963980.<br />
Veltri RW, Wilson WR, Sprinkle RM, Rodman SM, Kavesh DA. The implication of viruses in idiopathic sudden hearing<br />
loss: primary infection or reactivation of latent viruses? Otolaryngol Head Neck Surg 1981;89:137141.<br />
Weber RS, Jenkins HA, Coker NJ. Sensorineural hearing loss associated with ulcerative colitis: a case report. <strong>Archive</strong>s Oto<br />
http://www.bcm.edu/oto/grand/3592.html (7 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/3592.html<br />
Laryngol 1984;110:810-812.<br />
Wilkins SA, Jr., Mattox DE, Lyles A. Evaluation of a "shotgun" regimen for sudden hearing loss. Otolaryngol Head Neck<br />
Surg 1987;97:474480.<br />
Wilson WR. Why treat sudden hearing loss? Am J Otol 1984;5:481483.<br />
Wilson WR, Byl FM, Larid N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss: a double blind<br />
clinical trial. Arch Otolaryngol 1980;106:772776.<br />
Yoo TJ, Tomoda K, Stuart JM, Cremer MA, Townes AS, Kang AH. Type II collagen induced autoimmune sensorineural<br />
hearing loss and vestibular dysfunction in rats. Ann Otol Rhinol Laryngol 1983;92:267-271.<br />
Yoon TH, Paparella MM, Schachern PA, Alleva M. Histopathology of sudden hearing loss. Laryngoscope<br />
1990;100:707715.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/3592.html (8 of 8) [5.11.2005 10:44:45]
http://www.bcm.edu/oto/grand/111893.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
SUDDEN SENSORINEURAL HEARING LOSS<br />
James O. Fordice, MD<br />
November 18, 1993<br />
Sudden sensorineural hearing loss (SHL) is one of the most perplexing and controversial unsolved<br />
mysteries in otolaryngology. SHL has no universally accepted definition, but one useful definition is an<br />
idiopathic hearing loss of sensorineural origin, greater than 30 dB in three contiguous frequencies that<br />
occurs in less than three days. Most patients report onset of hearing loss within minutes to several hours.<br />
About one-third of patients will awaken with the loss; others may discover the problem when they try to<br />
use the telephone, or may describe a brief period of fluctuating hearing before the loss. About 50% of<br />
patients complain of concomitant unsteadiness or vertigo.<br />
Most studies find no seasonal, geographic, ethnic, racial or sexual predilection for SHL. The right and<br />
left ears appear equally vulnerable. In a series of 225 cases, Byl in 1984 noted bilateral SHL in 2% of<br />
http://www.bcm.edu/oto/grand/111893.html (1 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
patients. Reported overall incidence of SHL ranges from 5% to 20% per 100,000 persons per year. The<br />
mean overall age for SHL is 46 years, according to a large series by Mattox and Simmons.<br />
Sudden hearing loss is most likely a symptom rather than a discrete disease, merely representing the end<br />
result of many insults to the inner ear. Known etiologies of sudden hearing loss include multiple<br />
sclerosis, Cogan's syndrome, Buerger's disease, macroglobulinemia, leukemia, sickle cell disease,<br />
polycythemia, syphilis, bacterial infection, mumps, ototoxic drugs, metastatic tumors, trauma, and lupus.<br />
Ten percent of patients with Meniere's disease and up to 10% of acoustic neuroma patients will present<br />
with sudden hearing loss. In patients with sudden hearing loss, all of these known etiologies should be<br />
considered and ruled out before the most common "diagnosis" - idiopathic sudden hearing loss (SHL) - is<br />
accepted. Among patients with SHL, four etiologic theories remain pre-eminent: viral, vascular,<br />
membrane rupture, and auto-immune.<br />
Viruses have long been suspected as etiologic agents in SHL. Wilson et al, in 1983, studied 122 patients<br />
with SHL in the Boston area, and documented 63% viral seroconversion, compared with 40% of<br />
controls. Conversion rates were statistically significantly higher for mumps, rubeola, varicella-zoster,<br />
influenza, and CMV. Mumps virus was cultured from the perilymph of a patient with SHL by Westmore<br />
in 1979, and CMV has been cultured from the perilymph of a congenitally infected infant. Davis, Davis<br />
and Johnston, and Shimokata et al documented viral infection of the inner ear in animal models with<br />
CMV, mumps, and rubeola, respectively. However, SHL has not successfully been induced in an animal<br />
model using viruses. Schuknecht and Donovan in 1986 studied the temporal bone pathology in twelve<br />
ears with SHL and reviewed the literature for ten others; comparing the histopathologic findings in these<br />
SHL patients with findings from patients with known viral labyrinthitis, they found similar degenerative<br />
changes: atrophy of the organ of Corti, tectorial membrane, and stria vascularis in most cases. They<br />
concluded that viral cochleitis was the most probable cause of SHL.<br />
Simmons in 1968 proposed a double membrane break theory for SHL. Goodhill et al in 1973 discovered<br />
perilymph fistulas in three patients with sudden hearing loss, thus establishing round and oval window<br />
breaks as accepted etiologies for sudden hearing loss. Intracochlear membrane breaks, with and without<br />
round or oval window breaks, as a cause for SHL, have been poorly supported clinically and<br />
histopathologically. Most patients with SHL do not provide a history suggestive of implosive or<br />
explosive forces on the membranous labyrinth; Schuknecht and Donovan found no active or healed<br />
membrane breaks in the twelve temporal bones they examined.<br />
A vascular etiology for SHL is logically appealing, since sudden onset is suggestive of a vascular event.<br />
Sudden hearing loss has been observed in patients with vascular or coagulatory defects. However,<br />
histopathologic findings after permanent occlusion of the labyrinthine vasculature include necrosis of the<br />
membranous labyrinth followed by ossification and fibrosis - these findings are not consistent with those<br />
seen in most cases of SHL. Furthermore, temporary occlusion of the internal auditory artery was studied<br />
by Perlman et al in 1959, and these workers found irreversible loss of cochlear function after about one<br />
hour. They found that the hair cells, ganglion cells, and spiral limbus were the structures most frequently<br />
affected. These histopathologic findings are at odds with those from SHL ears studied. The irreversibility<br />
of the loss is also inconsistent with the reversibility of SHL in most cases. Finally, SHL typically strikes<br />
http://www.bcm.edu/oto/grand/111893.html (2 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
relatively young patients without systemic manifestation of vascular disease. This population seems<br />
unlikely to suffer isolated labyrinthine vascular compromise.<br />
In recent years autoimmune ear disease has been added to the theoretical etiologic triad of vascular, viral,<br />
and membrane rupture. Lehnhardt in 1958 first theorized that bilateral hearing disorders could result<br />
from autoimmune reactions directed against inner ear antigens. McCabe in 1979 first proposed the<br />
clinical entity of autoimmune sensorineural hearing loss. Yoo et al in 1983 induced autoimmune<br />
sensorineural hearing loss in rats by immunization with type II collagen, and demonstrated the presence<br />
of monoclonal antibody to type II collagen within the otic capsule. Harris in 1983 demonstrated the full<br />
competence of an independent inner ear immune system, capable of producing its own antibodies. In<br />
further work reported this year, Drs. Yamanobe and Harris isolated five autoantibodies to inner earspecific<br />
antigens in patients with idiopathic sensorineural hearing loss. No study has yet detected inner<br />
ear-specific autoantibodies in SHL, and no study has proven the development of SHL in animal models<br />
using such antibodies. The role of autoimmunity in SHL has yet to be clarified.<br />
Given the lack of understanding of the etiology or etiologies of SHL, treatment regimens have of<br />
necessity been empirical. One of the most commonly used treatments is vasodilator therapy. Many agents<br />
have been tried, but one of the most popular has been carbogen, which is a gaseous mixture of 5% CO2<br />
in 95% O2. Ugo Fisch in 1983 compared carbogen therapy with papaverine and low molecular weight<br />
dextran therapy in SHL patients. He found no significant short term difference in hearing results, but<br />
discovered significantly better hearing in carbogen-treated SHL patients after one year.<br />
Wilson et al in 1980 reported a double-blinded study of 67 SHL patients treated with steroids or placebo,<br />
and included an additional 52 controls who received no treatment. They found that patients with isolated<br />
midfrequency losses recovered without regard to therapy, and that 76% of patients with losses greater<br />
than 90 dB failed to recover regardless of therapy. However, in 74 patients with hearing loss less than 90<br />
Db not limited to the midfrequencies, 78% treated with steroids improved, compared with 38% of<br />
untreated patients. Subsequent studies have confirmed the benefit of steroids in selected patients. This is<br />
the only controlled study showing conclusive superiority of any treatment for SHL over no treatment.<br />
Other treatment regimens have included diuretics, anticoagulants, plasma expanders, and diatrizoate<br />
meglumine, or Hypaque, an intravenous contrast dye. Controlled studies have not been performed to<br />
show a benefit from any of them. Stellate ganglion block is an invasive technique used in SHL therapy.<br />
Ganglion block causes vasodilation and subsequent increased blood flow through sympathetic blockade.<br />
Haug et al from Houston reported in 1976 that 70% of 56 patients with SHL treated by a series of blocks<br />
experienced greater than or equal to 10 dB pure tone average improvement and over 10% gain in speech<br />
discrimination scores, versus only 20% of 20 patients treated by other means. Because this procedure<br />
involves deep injection of anesthetic in the low neck, it carries obvious risk of lung injury and injury to<br />
vital neural and vascular structures. Many centers, including Baylor, use a so-called "shotgun" approach<br />
to SHL treatment, in an attempt to address all theoretical etiologies. Wilkins et al in 1987 evaluated one<br />
exhaustive shotgun regimen of dextran, histamine, Hypaque, diuretics, steroids, vasodilators, and<br />
carbogen, but found the results no different from those for no treatment.<br />
http://www.bcm.edu/oto/grand/111893.html (3 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
It is generally agreed that spontaneous recovery is common in SHL, usually occurring within two weeks<br />
of onset. Mattox and Simmons stated that 65% of all SHL patients will have spontaneous recovery of<br />
functional hearing without treatment. Others have estimated that about one-third have spontaneous return<br />
to normal hearing, and another one-third have return to functional hearing with a residual deficit.<br />
Obviously, the ideal treatment protocol would improve on these numbers. Only steroid treatment, as<br />
evaluated by Wilson et al, in 1980, has been proven superior to no treatment, and this success came only<br />
in patients with moderate loss across many frequencies. Byl in 1984 reported a prospective study of 225<br />
SHL patients. He found the most important factors influencing recovery to be severity of initial loss,<br />
degree of vertigo, and time from onset to initial visit. All of these factors were inversely related to degree<br />
of recovery. Other facts identified by Byl and others include patient age, shape of initial audiogram, and<br />
ESR. Byl found that patients under 15 years of age and over 60 recovered less well than their<br />
counterparts within these two age limits. Most researchers agree that SHL patients with upsloping and<br />
midfrequency loss audiograms recover the best, while those with downsloping initial audiograms fare the<br />
worst. Elevated ESR has been shown to be a negative prognostic sign. Tinnitus, present in 70% to 85%<br />
of SHL patients, has no prognostic value.<br />
Sudden sensorineural hearing loss remains a poorly understood and maddening problem for the<br />
otolaryngologist. Prognostic predictors include audiogram shape, severity of loss, patient age, presence<br />
of vestibular symptoms, and duration of symptoms. Viral and autoimmune mechanisms are currently the<br />
best etiologic candidates, but the heterogeneity of patients and findings makes the discovery of a single<br />
pathologic pathway for all SHL unlikely.<br />
Case Presentation<br />
A fifty-two-year-old Latin American man presented to Ben Taub General Hospital with a twelve hour<br />
history of sudden hearing loss in the left ear. The patient had been watching television when he felt a pop<br />
in his left ear, followed by tinnitus and subjective hearing loss. He denied dizziness, vertigo, nausea, or<br />
vomiting, and gave no history of straining, trauma, or barotrauma. He also denied any history of ototoxic<br />
drugs or otologic surgery. Hearing was subjectively normal bilaterally prior to this episode. Past medical<br />
history was remarkable only for insulin-dependent diabetes mellitus, and social history was negative for<br />
drinking, smoking, and drug use. Physical examination was unremarkable except for tuning fork tests<br />
indicating a left sensorineural hearing loss. The patient had a negative fistula test and no spontaneous<br />
nystagmus. Laboratory studies were all within normal limits, including an ESR of 2 and negative syphilis<br />
serologies. Admission audiogram showed a pure tone average of 73 dB on the left and 8 dB on the right,<br />
and speech understanding depressed to 32% on the left, normal on the right. Tympanograms were Type<br />
A bilaterally. The patient was admitted and put to bedrest with a low salt diet. He underwent stellate<br />
ganglion blocks times three, and was started on a prednisone taper from 80 mg and given carbogen<br />
treatments. He experienced subjective improvement in his hearing on day three, and repeat audiogram on<br />
day four showed pure tone average of 42 on the left, with speech discrimination of 60%. The patient was<br />
discharged on day 5 on prednisone taper and low salt ADA diet, with light activity. Outpatient MRI of<br />
http://www.bcm.edu/oto/grand/111893.html (4 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
the head was normal. At follow-up two months later, the patient reported subjective return of normal<br />
hearing. Audiogram showed pure tone average of 12 dB on the left, 8 dB on the right, with 100% speech<br />
discrimination bilaterally.<br />
Bibliography<br />
Alford BR, Shaver EF, Rosenberg JJ, Guildford FR. Physiologic and histopathologic effects of microembolization of the<br />
internal auditory artery. Ann Otol Rhinol Laryngol 1965;74:728-748.<br />
Anderson RG, Meyerhoff WI. Sudden sensorineural hearing loss. Otolaryngol Clin N Am 1983;16:189-195.<br />
Beal DD, Hemenway WG, Lindsay JR. Inner ear pathology of sudden deafness: the histopathology of acquired deafness in<br />
the adult coincident with viral infection. Arch Otolaryngol 1967;85:591-598.<br />
Belal A, Jr. Pathology of vascular sensorineural hearing impairment. Laryngoscope 1980;90:1831-1839.<br />
Bredenkamp JK, Shelton C. Sudden hearing loss: determining the specific cause and the most appropriate treatment.<br />
Postgrad Med 1989;86:125-132.<br />
Byl FM. Seventysix cases of presumed sudden hearing loss occurring in 1973: prognosis and incidence. Laryngoscope<br />
1977;87:817-825.<br />
Byl FM. Sudden hearing loss: eight years experience and suggested prognostic table. Laryngoscope 1984;94:647-661.<br />
Cole RR, Jahrsdoerfer RA. Sudden hearing loss: an update. Am J Otol 1988;9:211-215.<br />
DeKleyn A. Sudden complete or partial loss of function in the octavus system in apparently normal persons. Acta<br />
Otolaryngol 1944;32:407-425.<br />
Donaldson JA. Heparin therapy of sudden sensorineural hearing loss. Arch Otolaryngol 1979;105:351-352.<br />
Fisch U. Management of sudden deafness. Otolaryngol Head Neck Surg 1983;91:38.<br />
Fowler E. Sudden deafness. Ann Otol Rhinol Laryngol 1950;59:980-987.<br />
Goodhill W. The "idiopathic group" and the "labyrinthine window rupture group" approaches to sudden sensorineural<br />
hearing loss. In: Snow JB Jr, editor. Controversy in Otolaryngology. Philadelphia: Saunders, 1980:12-20.<br />
<strong>Grand</strong>is JR, Hirsch BE, Wagener MM. Treatment of idiopathic sudden sensorineural hearing loss. Am J Otol 1993;14:183-<br />
5.<br />
Gussen R. Sudden hearing loss associated with vascular origins: a temporal bone study. Ann Otol Rhinol Laryngol<br />
http://www.bcm.edu/oto/grand/111893.html (5 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
1976;85:94-100.<br />
Hallberg O. Sudden deafness of obscure origin. Laryngoscope 1956;66:1237-1267.<br />
Harris I. Sudden hearing loss: membrane rupture. Am J Otol 1984;5:484-7.<br />
Harris JP. Immunology of the inner ear: response of the inner ear to antigen challenge. Otolaryngol Head Neck Surg<br />
1983;91:18-23.<br />
Harris JP. Experimental immunology of the inner ear. Adv Otorhinolaryngol 1991;46:26-33.<br />
Harris JP. Autoimmunity of the inner ear. Am J Otol 1989;10:193-5.<br />
Harris JP, Tomiyama S. Experimental immune system of the inner ear. J Otorhinolaryngol -Relat-Spec 1987;49:225-33.<br />
Harris JP, Sharp PA. Inner ear autoantibodies in patients with rapidly progressive sensorineural hearing loss.<br />
Laryngoscope 1993;100:516-24.<br />
Haug O, Draper L, Haug SA. Stellate ganglion block for idiopathic sensorineural hearing loss. Arch Otolaryngol<br />
1976;102:58.<br />
Igarashi M, Alford BR, Konishi S, Shaver EF, Guilford FR. Functional and histopathological correlates after<br />
microembolization of the peripheral labyrinthine artery in the dog. Laryngoscope 1969;79:602-623.<br />
Igarashi M, Card G, Johnson PE, Alford BR. Bilateral sudden hearing loss and metastatic pancreatic adenocarcinoma.<br />
Arch Otolaryngol 1979;105:196-199.<br />
Jaffe BF. Sudden deafness: an otologic emergency. Arch Otolaryngol 1967;86:81-86.<br />
Jaffe BF. Sudden deafness a local manifestation of systemic disorders: fat emboli, hypercoagulation, and infection.<br />
Laryngoscope 1970;80:788-801.<br />
Jaffe BF. Hypercoagulation and other causes of sudden hearing loss. Otolaryngol Clin North Am 1975;8:395-403.<br />
Jaffe BF. Viral causes of sudden inner ear deafness. Otolaryngol Clin North Am 1978;10:63-9.<br />
Jaffe BF. Clinical studies in sudden deafness. Adv Otorhinolaryngol 1978;20:221-228.<br />
Jaffe BF, Maasab HF. Sudden deafness associated with adenovirus infection. N Engl J Med 1967;276:1406-1409.<br />
Jenkins HA, Pollack AM, Fisch U. Polyarteritis nodosa as a cause of sudden deafness. Am J Otolaryngol 1981;2:99-107.<br />
Jerger J, Allen G, Robertson D, Harford E. Hearing loss of sudden onset. Arch Otolaryngol 1961;73:350-357.<br />
http://www.bcm.edu/oto/grand/111893.html (6 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
Kaplan SL, Catlin FI, Weaver T, Feigin RD. Onset of hearing loss in children associated with bacterial meningitis.<br />
Pediatrics 1984;73:575-578.<br />
Kronenberg J, Almagor M, Bendet E, Kushnir D. Vasoactive therapy versus placebo in the treatment of sudden hearing<br />
loss: a double-blind clinical study. Laryngoscope 1992;102: 65-8.<br />
Lipkin AF, Jenkins HA, Coker NJ. Migraine and sudden sensorineural hearing loss. Arch Otolaryngol Head Neck Surg<br />
1987;113:325-326.<br />
McCabe BF. Autoimmune sensorineural hearing loss. Ann Otol Rhinol Laryngol 1979;88:585-589.<br />
McCabe BF. Autoimmune inner ear disease:therapy. Am J Otol 1989;10:196-7.<br />
Mattox DE, Lyles CA. Idiopathic sudden sensorineural hearing loss. Am J Otol 1989;10:242-247.<br />
Mattox DE, Simmons FB. Natural history of sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol 1977;86:463-<br />
480.<br />
Meyerhoff WL. The management of sudden deafness. Laryngoscope 1979;89:1867-1868.<br />
Meyerhoff WL, Paparella MM. Medical therapy of sudden hearing loss. In: Snow JB Jr, editor. Controversy in<br />
Otolaryngology. Philadelphia: Saunders, 1980:311.<br />
Nadol J, Wilson W. Treatment of sudden hearing loss is illogical. In: Snow JB Jr, editor. Controversy in Otolaryngology.<br />
Philadelphia: Saunders, 1980:23-32.<br />
Noury KA, Katsarkas A. Sudden unilateral sensorineural hearing loss: a syndrome or a symptom. J Otolaryngol<br />
1989;18:274-278.<br />
Ohlms LA, LonsburyMartin BL, Martin GK. Acousticdistortion products: separation of sensory from neural dysfunction in<br />
sensorineural hearing loss in human beings and rabbits. Otolaryngol Head Neck Surg 1991;104:159-174.<br />
Rowson K, Hinchicliffe R. A virological and epidemiological study of patients with acute hearing loss. Lancet 1975;1:471-<br />
474.<br />
Schuknecht HF, Benitez J, Beekhuis J, Igarashi M, Singleton G, Ruedi L. The pathology of sudden deafness.<br />
Laryngoscope 1962;72:1142-1157.<br />
Schuknecht HF, Donovan ED. The pathology of idiopathic sudden sensorineural hearing loss. Arch Otorhinolaryngol<br />
1986;243:1-15.<br />
Shaia FT, Sheehy JL. Sudden sensorineural hearing impairment: a report of 1220 cases. Laryngoscope 1976;86:389-398.<br />
Shikowitz MJ. Sudden sensorineural hearing loss. Med Clin North Am 1991;75:1239-1250.<br />
http://www.bcm.edu/oto/grand/111893.html (7 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
Siegel LG. The treatment of idiopathic sudden sensorineural hearing loss. Otolaryngol Clin N Am 1975;8:467-473.<br />
Simmons FB. Theory of membrane breaks in sudden hearing loss. Arch Otolaryngol 1968;88:41-48.<br />
Simmons FB. Fluid dynamics in sudden sensorineural hearing loss. Otolaryngol Clin North Am 1978;11:55-61.<br />
Singleton G. Cervical sympathetic chain block in sudden deafness. Laryngoscope 1971;81:7-34.<br />
Suga F, Preston J, Snow JB Jr. Experimental microembolization of cochlear vessels. Arch Otolaryngol 1970;92:213-220.<br />
Suga F, Snow JB Jr. Cochlear blood flow in response to vasodilating drugs and some related agents. Laryngoscope<br />
1969;79:1956-1979.<br />
Van Dishoeck H, Bierman T. Sudden perceptive deafness and viral infection. Ann Otol Rhinol Laryngol 1957;66:963-980.<br />
Veldman JE, Hanada T, Meeuwsen F. Diagnostic and therapeutic dilemmas in rapidly progressive sensorineural hearing<br />
loss and sudden deafness. Acta Otolaryngol 1993; 113:303-6.<br />
Veltri RW, Wilson WR, Sprinkle RM, Rodman SM, Kavesh DA. The implication of viruses in idiopathic sudden hearing<br />
loss: primary infection or reactivation of latent viruses? Otolaryngol Head Neck Surg 1981;89:137-141.<br />
Weber RS, Jenkins HA, Coker NJ. Sensorineural hearing loss associated with ulcerative colitis: a case report. Arch<br />
Otolaryngol 1984;110:810-812.<br />
Wilkins SA Jr, Mattox DE, Lyles A. Evaluation of a "shotgun" regimen for sudden hearing loss. Otolaryngol Head Neck<br />
Surg 1987;97:474-480.<br />
Wilson WR. Why treat sudden hearing loss? Am J Otol 1984;5:481-483.<br />
Wilson WR, Byl FM, Larid N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss: a double blind<br />
clinical trial. Arch Otolaryngol 1980;106:772-776.<br />
Yamanobe S, Harris JP. Inner ear-specific autoantibodies. Laryngoscope 1993;103:319-25.<br />
Yoo TJ, Tomoda K, Stuart JM, Cremer MA, Townes AS, Kang AH. Type II collagen induced autoimmune sensorineural<br />
hearing loss and vestibular dysfunction in rats. Ann Otol Rhinol Laryngol 1983;92:267-271.<br />
Yoon TH, Paparella MM, Schachern PA, Alleva M. Histopathology of sudden hearing loss. Laryngoscope 1990;100:707-<br />
715.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
http://www.bcm.edu/oto/grand/111893.html (8 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/111893.html<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/111893.html (9 of 9) [5.11.2005 10:45:02]
http://www.bcm.edu/oto/grand/4292.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
TEMPORAL BONE FRACTURES<br />
Warren E. Morgan, MD<br />
April 2, 1992<br />
Temporal bone fractures may cause a variety of signs and symptoms. These include hearing loss, vertigo,<br />
facial paralysis, cerebrospinal fluid (CSF) otorhinorrhea, tympanic membrane (TM) perforation,<br />
hemotympanum, canal wall laceration, and Battle's sign. Adults and children are similarly affected but<br />
several series have found that the complication rate is lower in children.<br />
Fractures of the temporal bone are commonly classified based on the relationship of the fracture line to<br />
the long axis of the temporal bone. Longitudinal fractures are the most common accounting for 80% of<br />
the temporal bone fractures. This fracture extends along the length of the temporal bone. Transverse<br />
fractures extend directly across the petrous bone and make up about 10% of temporal bone fractures.<br />
Mixed fractures display some characteristics of each.<br />
http://www.bcm.edu/oto/grand/4292.html (1 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
Longitudinal fractures usually present with classic findings of laceration of the ear canal, tympanic<br />
membrane perforation, ossicular disruption, facial paralysis, and hearing loss. The hearing loss is<br />
predominately conductive but may have a sensorineural component as well. Facial paralysis occurs in<br />
about 10-20% of longitudinal fractures. These fractures result from trauma directed laterally over the<br />
temporal area. Conversely, transverse fractures of the temporal bone show hearing loss, hemotympanum,<br />
facial paralysis, and vertigo. Facial nerve paralysis occurs about 50% of the time. Transverse fractures<br />
result from trauma to the anterior and posterior aspects of the head.<br />
Recently a new classification system was proposed by Ghorayeb and Yeakley at The University of<br />
Texas, Houston. They studied 150 temporal bone fractures radiographically using CT scan with threedimensional<br />
reconstruction. Based on their findings they proposed a new classification system. They<br />
identified an oblique fracture type that had originally been described by Voss. In their review this was the<br />
most common fracture type, occurring in 74.7% of the temporal bone fractures in this series. Other<br />
fracture types encountered in this series include transverse, mixed, longitudinal, and fractures confined to<br />
the petrous apex. They differentiate the oblique and longitudinal fractures based on the orientation of the<br />
fracture line on the external aspect of the temporal bone. The oblique fracture crosses the external canal<br />
in a horizontal plane and then extends upward obliquely toward the middle fossa. The fracture misses the<br />
otic capsule and may extend toward the petrous apex where the fracture line may extend to the foramen<br />
lacerum. Conversely, the longitudinal fracture line is oriented in a more vertical plane.<br />
Histopathologic examination of temporal bone fractures reveals several patterns of injury. As previously<br />
mentioned, longitudinal fractures extend anterior to the otic capsule and do not cause direct injury to the<br />
otic capsule. In transverse fractures the otic capsule may be completely disrupted leading to complete<br />
loss of audiovestibular function. Fractures of the otic capsule do not heal, but may have fibrous union<br />
and new bone formation. This lack of healing may lead to infectious complications and the development<br />
of labyrinthitis ossificans. This is an important consideration because of the potential for cochlear<br />
implantation in patients with bilateral temporal bone fractures and profound deafness. Loss of<br />
audiovestibular function results from concussion of the inner ear as well. This may occur in patients with<br />
longitudinal fractures or may occur in patients without a temporal bone fracture. As demonstrated<br />
experimentally in cats by Schuknecht, high frequency hearing loss may occur from the transfer of<br />
vibratory energy to the cochlea. Lindsay described the changes noted in concussion and found the<br />
predominate injury to be hemorrhage into the audiovestibular elements. It is thought that hemorrhage<br />
induces a hyperplastic inflammatory response which may lead to degeneration of neural elements,<br />
fibrosis, and eventual ossification.<br />
The examination of a patient with suspected temporal bone fracture begins with a history and physical<br />
exam. Often times the initial assessment occurs in the emergency room where the patient is also being<br />
evaluated for other more life threatening injuries as well. History about the mechanism of injury should<br />
be obtained along with any audiovestibular symptoms. The physical exam begins with a general<br />
examination of the patient. The head and neck should be examined carefully, looking for the signs and<br />
symptoms of temporal bone fractures. The facial nerve should be carefully examined and any evidence of<br />
weakness documented. When the patient's condition improves audiogram and CT scan of the temporal<br />
http://www.bcm.edu/oto/grand/4292.html (2 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
bones should be performed with further workup directed by any subsequent complications. These<br />
complications include hearing loss, vertigo, facial nerve injury, and cerebrospinal fluid otorrhea.<br />
Conductive and sensorineural hearing loss can result from temporal bone fractures. Classically,<br />
conductive loss is associated with longitudinal fractures, and sensorineural loss with transverse fractures.<br />
But each may have components of both. The etiology of the conductive hearing loss may result from<br />
tympanic membrane perforation, hemotympanum, and ossicular disruption. Persistent conductive hearing<br />
loss suggests an ossicular disruption. Middle ear injury with ossicular derangement was initially reported<br />
at the time of autopsy by Keleman, and was noted by Thornburn in 1956. Shortly thereafter Hough<br />
described this<br />
as well, and later published his experience with 31 patients. He found that the most commonly damaged<br />
ossicle is the incus. This is thought to result from its relative lack of support compared to the other<br />
ossicles; and its location between the other two ossicles, which subjects it to torsional forces. Treatment<br />
of these injuries requires middle ear exploration and appropriate ossicular reconstruction.<br />
Sensorineural hearing loss may result from disruption of the membranous labyrinth or concussion.<br />
Treatment options for traumatic sensorineural hearing loss are limited. For the majority of patients the<br />
only option is rehabilitative. This consists of hearing aids and cochlear implantation for patients with<br />
profound bilateral hearing loss.<br />
Another sequelae of temporal bone fractures is vertigo. The incidence varies between different studies<br />
with a incidence of 78% by Tuohimaa, while Griffiths reports only 24%. The mechanism of the vertigo<br />
may vary and can result from a variety of causes which may be central or peripheral. Central causes are<br />
related to injury to the brainstem and result from dysfunction of the vestibular nuclei. There are a number<br />
of peripheral causes, the most common being benign positional vertigo. Patients that have associated<br />
vertigo with a fluctuating hearing loss should be suspected of having a perilymph fistula. Disruption of<br />
the labyrinth may lead to a unilateral weakness that causes vertigo. Another cause of vertigo that has<br />
been reported is endolymphatic hydrops. Rivzi describes a patient who sustained a transverse temporal<br />
bone fracture that left the otic capsule intact. This patient developed Meniere's-type symptoms and<br />
several months later died of unrelated causes. On examination of the temporal bones the fracture line was<br />
noted to cross the vestibular aqueduct. Since the majority of these patients' symptoms resolve within 12<br />
months, initial treatment is conservative. Patients who have persistent incapacitating symptoms may<br />
require vestibular nerve section or labyrinthectomy.<br />
Temporal bone fractures may result in facial nerve paralysis. Approximately 20% of longitudinal<br />
fractures and 50% of transverse fractures result in a facial palsy. This derives from edema, intraneural<br />
hemorrhage, bony fragment impingement and dehiscence of the nerve. In a review of 15 cases of<br />
longitudinal temporal bone fractures at Baylor, Coker et al found the perigeniculate region to be the most<br />
common site of injury. This injury occurred there about 93.3% of the time. Surgical findings noted neural<br />
edema present in 93%, intraneural hemorrhage in 40%, bony fragment impingement in 33%, and one<br />
patient with dehiscent geniculate ganglion and dehiscent proximal tympanic segment. In this same<br />
http://www.bcm.edu/oto/grand/4292.html (3 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
review, three patients with transverse temporal bone fractures underwent surgical exploration and they<br />
were noted to have injury to the labyrinthine and tympanic segments of the facial nerve.<br />
The evaluation of patients' facial paralysis from temporal bone fractures begins with early diagnosis.<br />
Patients with complete paralysis should be followed up with electrical testing. Several tests are available,<br />
with nerve excitability test, ENOG, and EMG being the most commonly used. Audiogram is also<br />
important since hearing status influences the choice of surgical approach. Initial treatment is<br />
conservative, consisting of eye protection and steroids. Facial nerve exploration and decompression is<br />
indicated for patients who show significant neural degeneration. For patients with serviceable hearing,<br />
decompression by a middle cranial fossa/transmastoid approach is best. For those without hearing a<br />
translabyrinthine/transmastoid approach is used.<br />
CSF otorrhea may result from temporal bone fractures, although the incidence is relatively low. In a<br />
review of 1,185 patients with skull fractures Raaf found that 3.6% presented with CSF otorrhea. Of these,<br />
97% closed spontaneously. Of the patients with otorrhea 7.8% developed meningitis, with one patient<br />
dying. Patients with longitudinal fractures usually develop CSF leaks from the tegmen where the fracture<br />
line perforates the dura. Transverse fractures are more likely to cross the vestibule and leakage may<br />
occur through the defect. Also, since the TM may be intact they are more likely to present with CSF<br />
otorhinorrhea. In most cases identification of the fluid is obvious. In questionable cases the most specific<br />
test available is electrophoretic identification of the B2 fraction of transferrin, which is specific for CSF.<br />
For persistent leaks localization may be attempted with CT scan with metrizamide.<br />
Since the majority of these leaks close spontaneously management is conservative. Several studies have<br />
failed to show any benefit from prophylactic antibiotics, and, while it remains controversial, they are<br />
probably not indicated. Initial management includes elevating the head and avoiding elevations of<br />
intracranial pressure. If this fails to resolve the leak the next step in management is insertion of lumbar<br />
drain. Leaks that persist, despite these measures, require surgical closure. While the period of waiting is<br />
controversial, surgical closure should be considered for leaks that have persisted for two weeks despite<br />
conservative therapy. The surgical approach is based on the suspected location and status of hearing. If<br />
the patient has good hearing and the defect is suspected in the tegmen, a middle fossa approach may be<br />
used. For patients with no hearing, obliteration via a translabyrinthine approach may be used.<br />
In a review of 82 temporal bone fractures in 75 patients Ghorayeb et al presented several other more<br />
unusual complications of temporal bone fractures. These include abducens nerve palsy which may be<br />
bilateral or unilateral, trigeminal paralysis, and aseptic sigmoid sinus thrombosis. In their review the<br />
incidence of abducens palsy was 6.67%. The abducens nerve has the longest intracranial course of any<br />
cranial nerve and is intimately associated with the facial nerve and the trigeminal nerve. It appears the<br />
nerve is most vulnerable as it enters Dorello's canal at the end of the petrous apex. Because of the<br />
complex anatomy of this nerve the exact mechanism of injury is unclear and may result from stretching<br />
and contusion alone. Patients present with an inability to abduct the eye. Many of these injuries are<br />
partial and may recover. Treatment consists of alternately patching one eye and if the injury fails to<br />
recover, corrective surgery may be attempted.<br />
http://www.bcm.edu/oto/grand/4292.html (4 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
Ghorayeb et al found an incidence of trigeminal paralysis in 2.67% of the cases. This injury also occurs<br />
near the end of the petrous apex where the trigeminal ganglion sits in Meckel's Cave. Patients present<br />
with hypesthesias and paresthesia in the trigeminal distribution. They may also have weakness of the<br />
muscles of mastication. No therapy is available for this injury.<br />
Sigmoid sinus thrombosis was found in one patient in this series. Patients may be asymptomatic or<br />
symptoms of increased intracranial pressure may occur. These include headache and retinal changes. The<br />
diagnosis is made with CT scan which shows occlusion of the sigmoid sinus with soft tissue. Clinically<br />
the diagnosis is made with the Tobey-Ayer Test, which consists of measuring changes in the CSF<br />
pressure with compression and release of the jugular veins. For septic sigmoid thrombophlebitis the<br />
treatment of choice is exploration of the sinus via a mastoid approach. For aseptic sigmoid sinus<br />
thrombosis Ghorayeb et al caution against exploration in debilitated patients, but advocate exploration as<br />
part of any other ear procedure. The patient presented in this review underwent facial nerve<br />
decompression and at that time the sinus was explored.<br />
Another rare complication of temporal bone fractures is cholesteatoma formation. This occurs in<br />
fractures that involve the external canal. With the disruption of the bony external canal small amounts of<br />
epithelium may be trapped. Many years later these patients may present with large and extensive<br />
cholesteatomas.<br />
Due to the complex anatomy, temporal bone fractures may cause a variety of disorders. Often the<br />
patients have sustained other more life threatening injuries that take precedence over the evaluation of<br />
temporal bone fracture. Early identification of the fracture, along with careful observation in the recovery<br />
period, is necessary for proper treatment.<br />
Case Presentation<br />
A 21-year-old black male presented to the Emergency Room after suffering blunt trauma to the head. He<br />
reportedly was hit with a vase in the right temporal area and lost consciousness at the scene. He<br />
complained of decreased hearing and bleeding from the right ear, but denied any vertigo. Physical exam<br />
of the right ear revealed a posterior external canal wall laceration and a hemotympanum. The facial nerve<br />
was intact. CT scan of the head and temporal bone was obtained which revealed a longitudinal fracture of<br />
the right temporal bone. He was admitted to the Neurosurgery Service for observation. On the second<br />
day of hospitalization he developed a complete right facial paralysis and he was transferred to the<br />
Otolaryngology Service. Audiogram showed a mild conductive hearing loss in the right ear, and acoustic<br />
reflexes showed a probe effect in the right ear. He was started on steroids and received local care for the<br />
right eye. He was followed daily with nerve excitability tests with the side to side difference remaining<br />
less than 2mA. On the seventh day after the onset of the paralysis, nerve excitability testing revealed a<br />
greater than 3.5 mA difference between sides. ENOG revealed greater than 95% degeneration of the<br />
facial nerve. He subsequently underwent a combined middle cranial fossa/transmastoid exploration and<br />
http://www.bcm.edu/oto/grand/4292.html (5 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
decompression of the facial nerve. At the time of surgery a bony spicule was found impinging on the<br />
facial nerve at the geniculate ganglion. The facial nerve was intact but edematous in the labyrinthine and<br />
tympanic segments. The postoperative course was uneventful and the patient was discharged to home on<br />
the sixth postoperative day.<br />
Bibliography<br />
Aguilar EA, III, Yeakley JW, Ghorayeb BY, Hauser M, Cabrera J, Jahrsdoerfer RA. High resolution CT scan of temporal<br />
bone fractures: association of facial nerve paralysis with temporal bone fractures. Head Neck Surg 1987;9:162-166.<br />
Alford BR, Sessions RB, Weber SC. Indications for surgical decompression of the facial nerve. Laryngoscope<br />
1971;81:620-635.<br />
Babin RW. Topognostic and prognostic evaluation of traumatic facial nerve injuries. Otolaryngol Head Neck Surg<br />
1982;90:610-611.<br />
Barber HO. Head injury: audiological and vestibular findings. Ann Otol Rhinol Laryngol 1969;78:239-252.<br />
Battle WH. Three lectures on some points relating to injuries to the head. Lancet 1890;1:57-63.<br />
Bellucci RJ. Traumatic injuries of the middle ear. Otolaryngol Clin North Am 1983;16:633-650.<br />
Benitez JT, Bouchard KR, LaneSzopo D. Pathology of deafness and disequilibrium in head injury: a human temporal bone<br />
study. Am J Otol 1980;1:163-167.<br />
Bottrill ID. Posttraumatic cholesteatoma. J Laryngol Otol 1991;105:367-369.<br />
Brodsky L, Eviatar A, Daniller A. Posttraumatic facial nerve paralysis: three cases of delayed temporal bone exploration<br />
with recovery. Laryngoscope 1983;93:1560-1565.<br />
Brookes GB, Graham MD. Posttraumatic cholesteatoma of the external auditory canal. Laryngoscope 1984;94:667-670.<br />
Cannon CR, Jahrsdoerfer RA. Temporal bone fractures. Review of 90 cases. Arch Otolaryngol 1983;109:285-288.<br />
Coker NJ. Management of traumatic injuries to the facial nerve. Otolaryngol Clin North Am 1991;24:215-227.<br />
Coker NJ, Kendall KA, Jenkins HA, Alford BR. Traumatic intratemporal facial nerve injury: management rationale for<br />
preservation of function. Otolaryngol Head Neck Surg 1987;97:262-269.<br />
Eby TL, Pollak A, Fisch U. Histopathology of the facial nerve after longitudinal temporal bone fracture. Laryngoscope<br />
1988;98:717-720.<br />
http://www.bcm.edu/oto/grand/4292.html (6 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
Eby TL, Pollak A, Fisch U. Intratemporal facial nerve anastomosis: a temporal bone study. Laryngoscope 1990;100:623-<br />
626.<br />
Fisch U. Current surgical treatment of intratemporal facial palsy. Clin Plast Surg 1979;6:377-388.<br />
Fisch U. Management of intratemporal facial nerve injuries. J Laryngol Otol 1980;94:129-134.<br />
Fredrickson JM, Griffith AW, Lindsay JR. Transverse fracture of the temporal bone: a clinical and histopathologic study.<br />
Arch Otolaryngol Head Neck Surg 1963;78:770-784.<br />
Freeman J. Temporal bone fractures and cholesteatoma. Ann Otol Rhinol Laryngol 1983;92:558-560.<br />
Ghorayeb BY, Yeakley JW, Hall JW, III, Jones BE. Unusual complications of temporal bone fractures. Arch Otolaryngol<br />
Head Neck Surg 1987;113:749-753.<br />
Glasscock ME, III, House WF, Alford BR. Middle fossa facial nerve decompression. Ann Otol Rhinol Laryngol<br />
1970;79:234-240.<br />
Glasscock ME, III, Wiet RJ, Jackson CG, Dickins JR. Rehabilitation of the face following traumatic injury to the facial<br />
nerve. Laryngoscope 1979;89:1389-1404.<br />
Goodwin WJ, Jr. Temporal bone fractures. Otolaryngol Clin North Am 1983;16:651-659.<br />
Griffin JE, Altenau MM, Schaefer SD. Bilateral longitudinal temporal bone fractures: a retrospective review of seventeen<br />
cases. Laryngoscope 1979;89:1432-1435.<br />
Grobman LR, Pollak A, Fisch U. Entrapment injury of the facial nerve resulting from longitudinal fracture of the temporal<br />
bone. Otolaryngol Head Neck Surg 1989;101:404-408.<br />
Hallpike CS. On a case of deafmutism of traumatic origin. J Laryngol Otol 1937;52:661-674.<br />
Harris JP, Butler D. Recognition of malleus handle fracture in the differential diagnosis of otologic trauma. Laryngoscope<br />
1985;95:665-670.<br />
Hicks GW, Wright JW, Jr., Wright JW, III. Cerebrospinal fluid otorrhea. Laryngoscope 1980;90:125.<br />
Hough JV. Restoration of hearing loss after head trauma. Ann Otol Rhinol Laryngol 1969;78:210-226.<br />
Hough JV. Surgical aspects of temporal bone fractures. Proc R Soc Med 1970;63:245-252.<br />
Hough JVD, Stuart WD. Middle ear injuries in skull trauma. Laryngoscope 1968;78:899-937.<br />
Kamerer DB. Intratemporal facial nerve injuries. Otolaryngol Head Neck Surg 1982;90:612-615.<br />
http://www.bcm.edu/oto/grand/4292.html (7 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
Kelemen G. Fractures of the temporal bone. Arch Otolaryngol Head Neck Surg 1944;40:333-373.<br />
Khan AA, Marion M, Hinojosa R. Temporal bone fractures: a histopathologic study. Otolaryngol Head Neck Surg<br />
1985;93:177-186.<br />
KoefoedNielsen B, Tos M. Posttraumatic sensorineural hearing loss: a prospective long-term study. ORL J<br />
Otorhinolaryngol Relat Spec 1982;44:206-215.<br />
Kveton JF. Obliteration of mastoid and middle ear for severe trauma to the temporal bone. Laryngoscope 1987;97:1385-<br />
1387.<br />
Lambert PR, Brackmann DE. Facial paralysis in longitudinal temporal bone fractures: a review of 26 cases. Laryngoscope<br />
1984;94:1022-1026.<br />
Lindsay JR, Zajtchuk J. Concussion of the inner ear. Ann Otol Rhinol Laryngol 1970;79:699-709.<br />
May M. Trauma to the facial nerve. Otolaryngol Clin North Am 1983;16:661-670.<br />
Millen SJ. Excellent spontaneous recovery following temporal bone fracture with loss of nerve excitability. Am J Otol<br />
1991;12:235-236.<br />
Millen SJ. Spontaneous recovery following temporal bone fracture in spite of loss of nerve excitability. Am J Otol<br />
1990;11:459-460.<br />
Perlman HG. Process of healing in injuries to the capsule of the labyrinth. Arch Otolaryngol Head Neck Surg 1939;29:287-<br />
305.<br />
Podoshin L, Pradis M. Hearing loss after head injury. Arch Otolaryngol Head Neck Surg 1975;101:1518.<br />
Rizvi SS, Gibbin KP. Effect of transverse temporal bone fracture on the fluid compartment of the inner ear. Ann Otol<br />
Rhinol Laryngol 1979;88:741-748.<br />
Rohrt T. Fracture of temporal bone, early or retrospective diagnosis, and surgical hearing reconstruction. Acta Otolaryngol<br />
1973;75:355-356.<br />
Schneider RC, Boles R. Combined neurootologic and neurosurgical problems in head trauma. Laryngoscope 1968;78:955-<br />
972.<br />
Schuknecht HF. A clinical study of auditory damage following trauma to the head. Ann Otolaryngol Chir Cervicofac<br />
1950;59:331-358.<br />
Schuknecht HF. Mechanism of inner ear injury from blows to the head. Ann Otol Rhinol Laryngol 1969;78:253-262.<br />
Schuknecht HF, Neff WD, Perlman HB. An experimental study of auditory damage following blows to the head. Ann Otol<br />
Rhinol Laryngol 1951;60:273-289.<br />
http://www.bcm.edu/oto/grand/4292.html (8 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/4292.html<br />
Shapiro RS. Temporal bone fractures in children. Otolaryngol Head Neck Surg 1979;87:323-329.<br />
Vartiainen E, Karjalainen S, Karja J. Auditory disorders following head injury in children. Acta Otolaryngol 1985;99:529-<br />
536.<br />
Ward PH. The histopathology of auditory and vestibular disorders in head trauma. Ann Otol Rhinol Laryngol 1969;78:227-<br />
238.<br />
Wennmo C, Svensson C. Temporal bone fractures. Vestibular and other related ear sequelae. Acta Otolaryngol Suppl<br />
1989;468:379-383.<br />
Wiet RJ, Valvassori GE, Kotsanis CA, Parahy C. Temporal bone fractures. State of the art review. Am J Otol 1985;6:207-<br />
215.<br />
Yanagihara N. Transmastoid decompression of the facial nerve in temporal bone fracture. Otolaryngol Head Neck Surg<br />
1982;90:616-621.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/4292.html (9 of 9) [5.11.2005 10:45:18]
http://www.bcm.edu/oto/grand/8593.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
TEMPORAL BONE GUNSHOT WOUNDS:<br />
EVALUATION AND MANAGEMENT<br />
Douglas D. Backous, MD<br />
August 5, 1993<br />
With the significant increase in handgun availability since the 1960s, treatment of gunshot injuries is no<br />
longer limited to major trauma centers. Five thousand Americans under the age of 20 die annually from<br />
gunshot wounds in the United States alone, with many more victims surviving with significant injury.<br />
The easy availability of guns is seen in rural as well as in metropolitan areas across the country.<br />
Wound ballistics is the study of the effects of missiles striking tissues. Kinetic energy is directly<br />
proportional to the mass of the projectile and proportional to the square of the velocity at which the bullet<br />
is traveling. The most efficient missile enters tissues and imparts the majority of its kinetic energy to<br />
http://www.bcm.edu/oto/grand/8593.html (1 of 5) [5.11.2005 10:45:25]
http://www.bcm.edu/oto/grand/8593.html<br />
surrounding structures without exiting the victim. Traditionally, gunshot injuries could be classified as<br />
civilian or military. Civilian injuries were inflicted with low velocity weapons (90-210 m/sec) while<br />
military wounds typically were caused by high velocity weapons (610 m/sec and up). Due to medium to<br />
high velocity weapons appearing on the streets, more civilians are suffering from military-type injuries.<br />
Gunshot injuries to the temporal bone affect intracranial, vascular, middle or inner ear, cranial nerve, and<br />
external canal structures. Being the toughest bone in the body, the temporal bone deflects missles, often<br />
resulting in hidden injuries. Early intracranial injuries include skull fractures, subdural hematoma,<br />
foreign bodies, pneumocephalus and cerebrospinal fluid leaks. Temporal lobe abscess, meningitis,<br />
aphasia, hemianopsia, and hemiplegia are late intracranial complications. Venous injuries to the<br />
transverse and sigmoid sinuses, jugular system and cavernous sinus have been reported. Acute<br />
transection of internal or external carotid arteries is usually obvious while pseudoaneurysms and carotidcavernous<br />
fistulae can develop later during the recovery period. Tympanic membrane perforations,<br />
ossicular disruption, labyrinthine destruction, and mixed longitudinal and transverse temporal bone<br />
fractures are the most commonly associated middle ear injuries. The majority of victims suffer acoustic<br />
injury inflicted either by direct damage from the bullet path or, more commonly, from blast effects. Fifty<br />
percent of victims will have facial nerve involvement with transections by far outweighing contusions.<br />
The vagus, hypoglossal, and abducens nerves are the next most frequently damaged cranial nerves. Bony<br />
and cartilaginous fractures, cicatricial scarring, temporomandibular joint displacement, canal<br />
cholesteatoma, and chronic bony infections can occur after gunshot injury involving the external auditory<br />
canal.<br />
Initial assessment includes a standard trauma workup with attention directed to life-threatening problems<br />
first. General and neurosurgical clearance is mandatory prior to thorough head and neck and otologic<br />
examination. Evaluation of the ear should be done with sterile instruments to avoid further soft tissue<br />
contamination. Computed tomography of the temporal bones is ordered once the patient is stable. Carotid<br />
and vertebral arteriograms should be obtained at the slightest suspicion of potential vascular<br />
involvement. Venous phases of these studies are important. Audiometric testing documents hearing at<br />
baseline and prior to any surgical manipulation of the otic structures and aids in selecting approaches to<br />
the middle ear and facial nerve. Vestibular testing may be obtained to document the nature and location<br />
of lesions in symptomatic patients and is useful to follow vestibular compensation.<br />
Patients are first stabilized from life-threatening injuries. Acute care for intracranial injuries includes<br />
intravenous steroids and osmotic diuretics. Antibiotic prophylaxis is key, especially if dural injury is<br />
suspected. Lumbar drainage and craniotomy should be employed as indicated. Embolization, packing at<br />
the skull base, and vessel ligation in the neck are options for vascular injuries. Mastoidectomy and<br />
tympanoplasty should be considered whenever remaining anatomy permits and residual hearing is<br />
documented. Debridement of the external auditory canal, labyrinthectomy and temporal bone obliteration<br />
should be used depending on the extent of destruction within the temporal bone and depending on the<br />
status of remaining critical structures.<br />
Presentation with a complete facial nerve paralysis signals a transection and should be managed<br />
aggressively. Exploration of the wound to localize damaged nerve endings is best done before 72 hours<br />
http://www.bcm.edu/oto/grand/8593.html (2 of 5) [5.11.2005 10:45:25]
http://www.bcm.edu/oto/grand/8593.html<br />
when distal nerve segments have not undergone degeneration. Exploration is often delayed while other<br />
injuries are treated. Exploration is then best completed in the subsequent 6 to 12 months. The best results<br />
are accomplished with end-to-end anastomosis. Due to local destruction from blast effects, end-to-end<br />
anastomosis is frequently not feasible mandating interposition grafting techniques. The great auricular<br />
nerve provides 5 cm to 7 cm of graft material while the sural nerve affords up to 30 cm of donor tissue.<br />
Delayed loss of facial nerve function most likely results from nerve edema or contusion and<br />
decompression suffices as definitive operative management. House-Brackmann grade 4 recovery or<br />
worse is expected with interposition grafting while up to grade 3 recovery has been documented from<br />
decompressions. Local eye care is mandatory to avoid exposure keratitis while nerve recovery<br />
progresses. Other cranial nerve injuries are managed symptomatically. Long-term follow-up is required<br />
since many of these patients will need secondary facial reanimation procedures.<br />
In conclusion, multispecialty assessment is required for patients with gunshot wounds involving the<br />
temporal bone. Life-threatening injuries are addressed first, followed by a thorough head and neck<br />
workup. Care must be taken to avoid missing hidden injuries induced secondary to blast effects or due to<br />
deflection of the missile off of the otic capsule. Indications for surgical exploration of the temporal bone<br />
include facial nerve paralysis, vascular injury, cerebrospinal leakage, chronic otitis media, conductive<br />
hearing loss and to debride necrotic tissue.<br />
Case Presentations<br />
A 44-year-old black male presented to the shock room at Ben Taub General Hospital with a single<br />
gunshot wound to the left preauricular area. On admission, he was awake and alert, with a complete left<br />
facial nerve paralysis. He had significant tissue loss on the left side of his face and in the left tonsillar<br />
area. After airway stabilization by endotracheal intubation, emergent computerized tomographic<br />
scanning of the head was negative for intracranial pathology and four vessel arteriograms showed no<br />
vascular injury. A barium swallow revealed no extravasation into the pharynx or esophagus. He was<br />
extubated after 48 hours. The left external auditory canal was remarkable for bloody discharge and<br />
squamous debris, with the Weber lateralizing to the right. The remaining cranial nerves were intact. No<br />
other injuries were found after thorough physical examination. The patient had swallowed the bullet that<br />
was originally presumed to be resting in his posterior oropharynx. Temporal bone CT scans revealed a<br />
comminuted left mastoid tip and fractured external auditory canal and temporomandibular joint.<br />
Audiogram showed no responses in the left ear and a moderate sensorineural loss on the right. No<br />
response could be elicited by nerve excitability testing on the left side. The patient was discharged after<br />
11 days in the hospital. He was readmitted seven days later, at which time he underwent left radical<br />
mastoidectomy, complete facial nerve decompression, sural nerve grafting and meatoplasty. The patient<br />
did well postoperatively and has been followed regularly in clinic. He has a House-Brackmann grade VI<br />
recovery and is now, at two years postrepair, being considered for a secondary procedure to improve his<br />
facial tone and to gain left eye closure.<br />
http://www.bcm.edu/oto/grand/8593.html (3 of 5) [5.11.2005 10:45:25]
http://www.bcm.edu/oto/grand/8593.html<br />
Bibliography<br />
Brookes GB. Post-traumatic cholesteatoma. Clin Otolaryngol 1983;8:31-38.<br />
Byrnes DP, Crockard HA, Gordon DS, Gleadhill CA. Penetrating craniocerebral missile injuries in the civil disturbances<br />
in Northern Ireland. Br J Surg 1974;61:169-176.<br />
Coker NJ. Management of traumatic injuries to the facial nerve. Otolaryngol Clin North Am 1991;24:215-227.<br />
Coker NJ, Jenkins HA. Traumatic injury to the facial nerve. Exhibit Handout 1990.<br />
Coker NJ, Kendall KA, Jenkins HA, Alford BR. Traumatic intratemporal facial nerve injury: management and rationale<br />
for preservation of function. Otolaryngol Head Neck Surg 1987;97:262-269.<br />
Cushing H. A study of a series of wounds involving the brain and its enclosing structures. Br J Surg 1918;5:558-684.<br />
du Trevou M, Teasdale RB, Quin RO. False aneurysms of the carotid tree due to unsuspected penetrating injury of the<br />
head and neck. Br J Accident Surg 1991;22:237-239.<br />
Duncan NO, Coker NJ, Jenkins HA, Canalis RF. Gunshot injuries to the temporal bone. Otolaryngol Head Neck Surg<br />
1986;94:4755.<br />
Hagan WE, Tabb HG, Cox RH, Travis LW. Gunshot injuries to the temporal bone: an analysis of thirtyfive cases.<br />
Laryngoscope 1979;89:1258-1272.<br />
Holt GR, Kostohryz G. Wound ballistics of gunshot injuries to the head and neck. Arch Otolaryngol 1983;109:313-318.<br />
House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg 1988;93:146-147.<br />
Kerr AG. Gunshot injury of the temporal bone a histological report. J Irish Med Assn 1967;110(366):446-448.<br />
Kinney SE. Trauma to the middle ear and temporal bone. In: Cummings CW, Fredrickson JM, Harker LA, Krause CJ,<br />
Schuller DE, editors. Otolaryngology Head and Neck Surgery. 2nd ed. St. Louis: Mosby, 1993:2873-2884.<br />
Mahmoud NA. Traumatic aneurysm of the internal carotid artery and epistaxis. J Laryngol Otol 1979;93:629-656.<br />
Singh SP, Adeloye A. Hearing loss in missile head injuries. J Laryngol Otol 1971;85:1183-1187.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
http://www.bcm.edu/oto/grand/8593.html (4 of 5) [5.11.2005 10:45:25]
http://www.bcm.edu/oto/grand/8593.html<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/8593.html (5 of 5) [5.11.2005 10:45:25]
http://www.bcm.edu/oto/grand/111292.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
TUBERCULOUS OTITIS MEDIA<br />
Troy Callender, MD<br />
November 12, 1992<br />
Despite tremendous advances in the treatment and prevention of tuberculosis (TB) it remains one of the<br />
most common, lethal infectious diseases in the United States. Worldwide, TB is the single most important<br />
bacterial infection, with more than 7 million active cases. Fortunately the ear is rarely infected by<br />
mycobacterium tuberculosis; current incidence is estimated to be between 0.9% and 0.04%. The tubercle<br />
bacillus can spread to the middle ear by several routes. The most common route is hematogenous. Other<br />
routes of infection include regurgitation of the tubercle bacillus through the eustachian tube, through<br />
previously existing tympanic membrane perforations; and by direct extension from a nasopharyngeal site<br />
of infection. TB can also be transmitted congenitally and is associated with a high incidence of ear<br />
involvement. However, congenital TB is extremely rare and hardly ever presents with isolated ear<br />
involvement.<br />
http://www.bcm.edu/oto/grand/111292.html (1 of 5) [5.11.2005 10:45:30]
http://www.bcm.edu/oto/grand/111292.html<br />
Classically, tuberculous otitis media is described as having an insidious onset with painless otorrhea,<br />
multiple tympanic membrane perforations, abundant pale granulation tissue in the middle ear, early<br />
severe hearing loss out of proportion to clinical findings, and bone necrosis. However, the current<br />
literature indicates most patients actually present with a single perforation. Indications of tuberculous<br />
otitis media include hearing loss out of proportion to clinical findings, failure to respond to the usual<br />
medical therapy, post-mastoidectomy recurrence of granulation tissue, slow wound healing, persistent<br />
otorrhea, and the formation of bony sequestra.<br />
The evaluation of these patients should include a history of contact to active tuberculosis, placement of a<br />
PPD skin test with control, culture and stain of ear drainage for AFB, biopsy of granulation tissue for<br />
histology and culture, and evaluation of the immune system if indicated. All patients should be evaluated<br />
with a chest x-ray, urinalysis, sputum for AFB culture and smear, gastric aspirates in children, and lumbar<br />
puncture if CNS involvement is suspected or if the patient has miliary TB. On examination of the ear, the<br />
tympanic membrane will appear dull and thickened with dilated vessels on the surface early and will later<br />
develop perforations from liquification of caseous tubercles. There will also be abundant granulation<br />
tissue in the middle ear. Late complications include facial paralysis, labyrinthitis, postauricular fistulae,<br />
subperiosteal abscess, petrous apicitis, and intracranial extension of infection. Radiologic evaluation of<br />
the temporal bone cannot differentiate TB from non-specific infections. A well-pneumatized mastoid<br />
with chronic otitis media is suggestive of tuberculous otitis media but not diagnostic, as these cases can<br />
also have sclerotic and destructive mastoid lesions.<br />
The differential diagnosis of tuberculous otitis media includes fungal infections, Wegener's<br />
granulomatosis, midline granuloma, sarcoidosis, syphilis, necrotizing otitis externa, atypical<br />
mycobacterial infections, and histiocytosis X.<br />
The treatment of tuberculous otitis media is primarily medical and should include a 6- to 9-month course<br />
of Isoniazid, Rifampin, and Pyrazinamide. Indications for surgical intervention include the late<br />
complications of tuberculous otitis media; cases unresponsive to medical therapy; extensive disease with<br />
bone sequestra or necrotic bone; and reconstruction of the tympanic membrane and ossicular chain after<br />
the middle ear disease has been eradicated.<br />
Case Presentation<br />
A 10-month-old black female, developed persistent otitis media at 4 months, which failed to respond to<br />
multiple courses of antibiotics. On referral to the Pediatric Otolaryngology Service, examination was<br />
remarkable for bilateral dull, thickened, erythematous tympanic membranes with poor mobility on<br />
insufflation. Myringotomy on June 22, 1992 revealed granulation tissue filling the middle ear cleft<br />
bilaterally. Post-operatively she was improved but had persistent scant otorrhea in spite of outpatient<br />
medical therapy. A CT scan of the temporal bones was obtained and showed opacification but no<br />
destructive lesions. The patient was returned to the OR on September 23, 1992. Middle ear tissue was<br />
http://www.bcm.edu/oto/grand/111292.html (2 of 5) [5.11.2005 10:45:30]
http://www.bcm.edu/oto/grand/111292.html<br />
obtained for routine AFB, fungal cultures, and histologic examination, and her ventilation tubes were<br />
replaced. She was admitted and a pediatric infectious disease consultation was obtained.<br />
Additional historical data obtained at that time revealed the patient to have had close contact with a<br />
relative with active tuberculosis. Complete evaluation during this admission was remarkable for elevated<br />
total IgG and IgG1, + ELISA HIV with an indeterminate western blot, miliary CXR pattern consistent<br />
with TB, CSF analysis showing 62 WBC's, 2 RBC's, 82% monos, a glucose of 36 mg/dl and protein of 38<br />
mg/dl consistent with tuberculous meningitis. A CT scan of the brain revealed tuberculomas in the<br />
posterior fossa and a PPD skin test was positive with 19 mm to 20 mm of induration. ABR was<br />
compatible with a mild conductive loss.<br />
Treatment was instituted with isoniazid, rifampin, pyrazinamide, and kanamycin. She was also treated<br />
with oral prednisone. She had a dramatic otologic response with resolution of granulation tissue over 2 to<br />
3 weeks. Except for occasional fever she was otherwise well. She was kept in the hospital for 4 weeks to<br />
insure compliant therapy and is being closely followed as an outpatient. Final cultures at eight weeks<br />
show no AFB growth.<br />
Bibliography<br />
Austin WK, Lockey MW. Mycobacterium fortuitum mastoiditis. Arch Otolaryngol 1976;102:558-560.<br />
Bate TWP, Sinclair RE, Robinson MJ. Neonatal tuberculosis. Arch Dis Child 1986;61:738-740.<br />
Cunningham MJ, Curtin HD, Jaffe R, Stool SE. Otologic manifestations of Langerhans' cell histiocytosis. Arch<br />
Otolaryngol Head Neck Surg 1989;115:807-813.<br />
Davidson S, Creter D, Leventon G, Katznelson K. Tuberculosis of the middle ear in an infant. Arch Otolaryngol Head<br />
Neck Surg 1989;115:876-877.<br />
Glover SC, Tranter RMD, Innes JA. Tuberculous otitis media - a reminder. J Laryngol Otol 1981;95:1261-1264.<br />
Grabscheid E. Tuberculosis of the petrous apex. Report of a case. Arch Otolaryngol 1937;25:11-16.<br />
Harbert F, Riordan D. Tuberculosis of the middle ear. Laryngoscope 1984;74:198-204.<br />
Jeang TK, Fletcher EC. Tuberculosis otitis media. JAMA 1983;249:2231-2232.<br />
Kinsella JP, Grossman M, Black S. Otomastoiditis caused by Mycobacterium avium-intracellulare. Pediatr Infect Dis<br />
1986;5:704-706.<br />
Lederer E. Diseases of the Ear, Nose and Throat. Philadelphia: Davis, 1953:216-223.<br />
http://www.bcm.edu/oto/grand/111292.html (3 of 5) [5.11.2005 10:45:30]
http://www.bcm.edu/oto/grand/111292.html<br />
Li CK, Chan Y-F, Har CMY. Congenital tuberculosis. Aust Paediatr J 1989;25:366-3677.<br />
Lowry WP, Jarvis WR, Oberle AD, Bland LA, Silberman R, Bocchini JA Jr, et al. Mycobacterium chelonae causing otitis<br />
media in an ear-nose-and-throat practice. New Engl J Med 1988;319:978-982.<br />
Lucente FE, Tobias GW, Parisier SC, Som PM. Tuberculous otitis media. Laryngoscope 1987;88:1107-1115.<br />
Lyons AS, Petrocelli RJ. Medicine. An Illustrated History. NY: Abradale Press, 1978:559,590.<br />
Ma KH, Tang PSO, Chan KW. Aural tuberculosis. Am J Otol 1990;11:174-177.<br />
Munzel MA. Tympanoplasty and tuberculosis of the middle ear. Clin Otolaryngol 1978;3:311-313.<br />
Neitch SM, Bydnor JB, Schleupner CJ. Mycobacterium fortuitum as a cause of mastoiditis and wound infection. Arch<br />
Otolaryngol 1982;108:11-14.<br />
Palva T, Palva A, Kärjä J. Tuberculous otitis media. J Laryngol Otol 1973;87:253-261.<br />
Plester D, Pusalkar A, Steinbach E. Middle ear tuberculosis. J Laryngol Otol 1980;94:1415-1421.<br />
Ramages LJ, Gertler R. Aural tuberculosis: a series of 25 patients. J Laryngol Otol 1985;99:1073-1080.<br />
Sahn SA, Davidson PT. Mycobacterium tuberculosis infection of the middle ear. Chest 1974;66:104-106.<br />
Scully RE, Mark EJ, McNeely WF, McNeely BU. Case records of the Massachusetts General Hospital. Case 21-1991. New<br />
Engl J Med 1991;324:1489-1495.<br />
Shambaugh GE, Glasscock ME. Surgery of the Ear, 3rd edition. Philadelphia: WB Saunders, 1980:208-210.<br />
Slonik PR, Nadol JB Jr, Baker AS. Tuberculosis of the middle ear: review of the literature with an instructive case report.<br />
Rev Infect Dis 1986;8:403-461.<br />
Snider DE, Rieder HL, Combs D, Bloch AB, Hayden CH, Smith MHD. Tuberculosis in children. Pediatr Infect Dis J<br />
1988;7:271-278.<br />
Summary of notifiable diseases, United States 1991. MMWR 1991;40(53):3-63.<br />
Turner AL, Fraser JS. Tuberculosis of the middle ear cleft in children: a clinical and pathological study. J Laryngol Otol<br />
1915;6:207-247.<br />
Vomero E, Ratner SJ. Diagnosis of miliary tuberculosis by examination of middle ear discharge. Arch Otolaryngol Head<br />
Neck Surg 1988;114:1029-1030.<br />
Wallner LJ. Tuberculous otitis media. Laryngoscope 1953;63:1058-1077.<br />
http://www.bcm.edu/oto/grand/111292.html (4 of 5) [5.11.2005 10:45:30]
http://www.bcm.edu/oto/grand/111292.html<br />
Wardrop PE, Pillsbury HC III. Mycobacterium avium acute mastoiditis. Arch Otolaryngol 1984;110:686-687.<br />
Windle-Taylor PC, Bailey CM. Tuberculous otitis media: a series of 22 patients. Laryngoscope 1980;90:1039-1044.<br />
Wolfowitz BL. Tuberculous mastoiditis. Arch Otolaryngol 1982;95:109-113.<br />
Yaniv E. Tuberculous otitis media: a clinical record. Laryngoscope 1987;97:1303-1306.<br />
Yaniv E, Traub P, Conradie R. Middle ear tuberculosis - a series of 24 patients. Int J Pediatr Otorhinolaryngol 1986;12:59-<br />
63.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/111292.html (5 of 5) [5.11.2005 10:45:30]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
TYMPANOSTOMY TUBES<br />
February 23, 1995<br />
Warren Morgan, M.D.<br />
Otitis media is the most common diagnosis in children, affecting two thirds of all children by the age of<br />
two years. Recurrent otitis media or otitis media with effusion may be treated with tympanostomy tubes,<br />
and approximately 700,000 children undergo this procedure each year. In an article that appeared in<br />
JAMA, Kleinman and colleagues studied the medical appropriateness of tympanostomy tube insertion in<br />
children under the age of 16. After developing clinical indicators, they retrospectively reviewed a large<br />
group of patients. They felt that preoperative indicators for tympanostomy insertion were inappropriate<br />
for 25% and equivocal for 33% of the patients reviewed. Despite several biases in the study, this paper<br />
received a lot of national attention, increasing parental concern about tympanostomy tubes. In addition,<br />
the increase in cost concerns related to health care reform has lead to increased scrutiny as well.<br />
http://www.bcm.edu/oto/grand/22395.html (1 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Tympanostomy tubes are indicated for chronic otitis media with effusion, recurrent acute otitis media,<br />
tympanic membrane atelectasis, and complications of acute otitis media in children. A recent health care<br />
panel convened by the US government recommended tympanostomy tubes as a treatment option for otitis<br />
media with effusion that persists for three months with associated hearing loss. If the effusion persists<br />
four to six months despite other treatments, then tympanostomy tubes should be inserted at that time.<br />
Recurrent acute otitis media (5-6 episodes/year) with persistent middle ear effusion is best treated with<br />
tympanostomy tubes. Children with recurrent otitis media without persistent effusion may be treated with<br />
antibiotic prophylaxis or tympanostomy tubes. Children who fail antibiotic prophylaxis are candidates for<br />
tympanostomy tubes.<br />
No guidelines exist for preoperative audiologic testing in normal children undergoing tympanostomy tube<br />
insertion. Preoperative testing may identify undetected hearing loss and document hearing for<br />
medicolegal reasons. Manning et al reviewed the audiologic results of 600 children undergoing<br />
preoperative audiologic testing prior to tympanostomy tube insertion at Children's Medical Center in<br />
Dallas, Texas.<br />
They identified 6 patients (1%) with previously undetected sensorineural hearing loss. Each patient in this<br />
group had risk factors for hearing loss. Also, because the study was done in a tertiary children's hospital,<br />
the rate of hearing loss was higher than in the community. Despite these factors, they still recommended<br />
screening of all patients.<br />
A vast array of tympanostomy tubes have been designed. Tympanostomy tubes have been made out of<br />
Teflon, silicone, polyethylene, stainless steel, titanium, and even gold plated steel. Karlan et al performed<br />
a laboratory and clinical study comparing silicone and Teflon tubes and found the Teflon to be superior.<br />
Metal compounds such as stainless steel, titanium, and gold have been considered good compounds for<br />
tympanostomy tube construction. Several studies have failed to show a significant advantage over<br />
synthetic tubes.<br />
The shape and design of the tympanostomy tube is more important in determining its function. Large<br />
inner flanges increase the duration of middle ear ventilation. Tympanostomy tubes with a large inner<br />
diameter and short length are less likely to occlude but may allow easier passage of water. These<br />
characteristics must be considered during the selection of tympanostomy tubes.<br />
Tympanostomy tubes may be arbitrarily divided based on the duration of ventilation. Short term tubes are<br />
shaped like grommets or bobbins and have and the average duration of intubation is about 10 months. The<br />
tubes are easy to insert, have a low rate of obstruction, and low rate of permanent perforation. Long term<br />
ventilation tubes are typically T-shaped and have the opposite characteristics. The average duration of<br />
ventilation is around 30 months. Both groups of tubes have been modified to provide intermediate<br />
characteristics.<br />
Other operative factors may be important in tympanostomy tube insertion. In the past, several authors<br />
have felt that ear canal preparation was important prior to tympanostomy tube insertion. But Baldwin and<br />
Aland found no advantage with iodine preparation of the external canal prior to tympansotomy tube<br />
http://www.bcm.edu/oto/grand/22395.html (2 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
insertion. Myringotomy direction and location have been thought to influence the duration of middle ear<br />
ventilation and subsequent healing of the tympanic membrane. Although some authors have reported that<br />
intubation is longer when the tube is inserted in the anterior superior quadrant, a study by April et al<br />
found no difference between the anterior superior and anterior inferior quadrants. Likewise, myringotomy<br />
direction had no effect in a study by Guttenplan et al.<br />
Tympanostomy tubes may be inserted under local or general anesthesia. Some otolaryngologists have<br />
reported successful tympanostomy tube insertion using iontophoresis for local anesthesia in cooperative<br />
children over the age of six. Summerfield and White described insertion of tympanostomy tubes in 103<br />
patients with an age range of 3-12 years using EMLA cream for local anesthesia. EMLA is a mixture of<br />
lignocaine and prilocaine in a high concentration that is absorbed across the epidermis providing local<br />
anesthesia. They were successful in 93.2% of the patients, with all failures occurring in children less than<br />
four years. Many children undergo the tympanostomy tube insertion under general anesthesia. Markowitz-<br />
Spence et al reviewed the anesthetic complications in a series of 510 children undergoing general<br />
anesthesia for tympanostomy tubes at the Children's Hospital of Buffalo. No complications were reported<br />
in 423 (82.3%). Minor complications without long-term sequelae occurred in the other patients.<br />
Postoperative topical antibiotic prophylaxis after tympanostomy tubes remains controversial. Many<br />
otolaryngologists use otic drops to prevent blockage of the tube by blood or discharge and to prevent<br />
postoperative otorrhea, despite the theoretical risk of ototoxicity. Garcia et al performed a meta analysis<br />
of the five previous studies on the use of antibiotic drops and found a reduction in otorrhea by 85 %. They<br />
recommend continued use of topical antimicrobial prophylaxis in high risk cases with mucoid or purulent<br />
effusions. For routine cases without effusion and normal middle ear mucosa, they do not advocate routine<br />
use.<br />
Water may pass through a tympanostomy tube and cause a middle ear infection. Consequently, most<br />
otolaryngologists instruct parents to take precautions to avoid water exposure. This usually includes the<br />
use of ear plugs during bathing or water sports, while others forbid water sports. Paradoxically, children<br />
with ear tubes who swim do not have an increased rate of otorrhea, as shown in nine different studies.<br />
For middle ear contamination to occur through a tympanostomy tube, water must reach the tympanic<br />
membrane and then cross the tympanostomy tube into the middle ear. Middle ear contamination with bath<br />
water is much more irritating than other solutions. Studies suggest that middle ear contamination without<br />
immersion underware occurs rarely.<br />
Occasionally, a tympanostomy tube will persistent beyond the desired period of middle ear ventilation.<br />
The otolaryngologist must then decide at what time to remove the tube. Based on an increased rate of<br />
complications in tubes that persist for three years or longer, most tubes are removed at 2-3 years. No other<br />
tests or criteria exist to determine when they should be removed.<br />
Tympanostomy tubes may have significant complications. Meclelland reviewed his series of 307 patients<br />
under the age of 10 years who had been treated with tympanostomy tubes and followed for a minimum of<br />
1 year. The most common complication was otorrhea in 34.5% of patients. This include postoperative and<br />
http://www.bcm.edu/oto/grand/22395.html (3 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
delayed otorrhea with chronic otorrhea occurring in 5.5% of patients. Tympanic membrane perforation<br />
occurred in 6.2% of patients, but only 2.8% had chronic perforation that required surgical closure.<br />
Persistent tympanostomy tube and cholesteatoma occurred in 0.2 % of patients. Several other studies have<br />
been done on the overall rate of complications, showing similar rates.<br />
Long term complications following myringotomy and tubes was reported by Ben-Ami et al for Afula,<br />
Israel. They retrospectively reviewed and examined 64 patients 10 years after having myringotomy and<br />
tubes. In their review, 77.9% of patients were treated with one procedure, and the remainder required<br />
multiple procedures. Two patients had perforations on follow-up. Myringosclerosis was found in 42.3%<br />
of tympanic membranes with only 17.8% of the patients having myringosclerosis in the area of the<br />
previous tympanostomy tube. Only two patients (1.9%) developed long term otorrhea.<br />
Otorrhea, the most common complication, occurs in around 20% of all patients with tympanostomy tubes.<br />
Postoperative otorrhea is most likely related to the presence of purulent fluid or inflamed middle ear<br />
mucosa. Delayed otorrhea occurs due to another episode of acute otitis media, which may result from<br />
either external contamination through the tube or from nasopharyngeal reflux. Management of post<br />
tympanostomy otorrhea usually begins with ototopical agents and antibiotics. If this fails to clear the<br />
infection, then a culture is taken to identify any resistant organisms and guide further therapy. Sometimes<br />
if all therapy fails, removal of the tympanostomy tube is required.<br />
Chronic tympanic membrane perforation remains problematic with tympanostomy tubes. The rate of<br />
perforation varies widely in reported series and is heavily influenced by tympanostomy tube type and<br />
duration of intubation. In a number of studies, the rate of chronic perforation with short term grommet<br />
type tube is less than 5%, while with long term tympanostomy tubes the rate of perforation is around 15-<br />
20%. The longer the period of intubation, the greater the risk of persistent perforation. This factor should<br />
be considered during selection of tympanostomy tubes.<br />
Tympanosclerosis, or more accurately myringosclerosis, occurs in around 40-50% of children with<br />
tympanostomy tubes. The incidence of tympanosclerosis in chronic otitis media not treated with<br />
tympanostomy tubes is around 10%. The etiology of the tympanosclerosis is unclear and is related to both<br />
the disease process and the tympanostomy tube. In several studies the myringosclerosis does not cause an<br />
appreciable difference in hearing.<br />
The development of cholesteatoma with tympanostomy tubes is a relatively rare occurrence, reported in<br />
less than 1% in most series. Cholesteatoma may result from squamous debris being trapped in the middle<br />
ear around the tympanostomy tube. In some series, patients developed cholesteatoma in the attic area<br />
away from the tube site.<br />
In conclusion, tympanostomy tubes are an important tool in the treatment of chronic otitis media in<br />
children. Successful management requires the use of appropriate indications and the proper selection of<br />
tube type.<br />
http://www.bcm.edu/oto/grand/22395.html (4 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Case Presentation<br />
A 10-month-old female infant was referred to the Otolaryngology Clinic for recurrent otitis media for<br />
which she had been treated six times with antibiotics. Each episode responded to antibiotics, but she<br />
would develop another episode shortly after completion of antibiotic therapy. She was not routinely<br />
exposed to cigarette smoke, and was not in day care. The remainder of her history was normal. Her<br />
physical examination was remarkable for bilateral middle ear effusions. After discussing treatment<br />
options with the family, they elected to proceed with insertion of tympanostomy tubes. Preoperative<br />
audiologic evaluation was normal. She underwent bilateral myringotomies with tympanostomy tube<br />
insertion under general anesthesia. At the time of surgery she had thick middle ear effusions.<br />
Postoperatively she received a 3-day course of Cortisporin otic solution. She recovered well and has had<br />
no further episodes of otitis media.<br />
Bibliography<br />
April MM, Portella RR, Orobello PW Jr. Tympanostomy tube insertion: anterosuperior vs. anteroinferior quadrant.<br />
Otolaryngol Head Neck Surg 1992;106:241-242.<br />
Arcand P, Gauthier P, Bilodeau G, Chapados G, Abela A, Desjardins R, et al. Post-myringotomy care: a prospective study.<br />
J Otolaryngol 1984;13:305-308.<br />
Armstrong BW. A new treatment for chronic secretory otitis media. Arch Otolaryngol 1954;59:653-654.<br />
Avraham S, Luntz M, Sade J. The influence of ventilating tubes on the surgical treatment of atelectatic ears. Eur Arch<br />
Otorhinolaryngol 1991;248:259-261.<br />
Baldwin RL, Aland J. The effects of povidone-iodine preparation on the incidence of post-tympanostomy otorrhea.<br />
Otolaryngol Head Neck Surg 1990;102:631-634.<br />
Balkany TJ, Arenberg IK, Steenerson RL. Ventilation tube surgery and middle ear irrigation. Laryngoscope 1986;96:529-<br />
532.<br />
Becker GD, Eckberg TJ, Goldware RR. Swimming and tympanostomy tubes: a prospective study. Laryngoscope<br />
1987;97:740-741.<br />
Ben-Ami M, Rosen G, Shlezinger T, Konack S, Ben-Ami M. Otitis media with effusion - complications after treatment. J<br />
Laryngol Otol 1983;97:1091-1094.<br />
Bhatnagar RK. Critical evaluation of Per-Lee tube sin children. J Laryngol Otol 1990;104:112-113.<br />
http://www.bcm.edu/oto/grand/22395.html (5 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Bright RA, Moore RM, Jeng LL, Sharkness CM, Hamburger SE, Hamilton PM. The prevalence of tympanostomy tubes in<br />
children in the United States, 1988. Am J Public Health 1993;83:1026-1028.<br />
Bulkley WJ, Bowes AK, Marlowe JF. Complications following ventilation of the middle ear using Good T tubes. Arch<br />
Otolaryngol Head Neck Surg 1991;117:895-898.<br />
Dingle AF, Flood LM, Kumar BU, Hampal S. The mini-grommet and tympanosclerosis: results at two years. J Laryngol<br />
Otol 1993;107:108-110.<br />
Fior R, Veljak C. Late results and complications of tympanostomy tube insertion for prophylaxis of recurrent purulent otitis<br />
media in pediatric age. Int J Pediatr Otorhinolaryngol 1984;8:139-146.<br />
Garcia P, Gates GA, Schechtman KB. Does topical antibiotic prophylaxis reduce post-tympanostomy tube otorrhea? A<br />
meta-analysis. Ann Otol Rhinol Laryngol 1994;103:54-58.<br />
Gates GA, Avery C, Prihoda TJ, Holt GR. Delayed onset post-tympanotomy otorrhea. Otolaryngol Head Neck Surg<br />
1988;98:111-115.<br />
Gates GA, Avery C, Prihoda TJ, Holt GR. Delayed onset post-tympanotomy otorrhea. Otolaryngol Head Neck Surg<br />
1988;98:111-115.<br />
Gates GA, Avery C, Prihoda TJ, Holt BR. Post-tympanostomy otorrhea. Laryngoscope 1986;96:630-634.<br />
Giebink GS, Kaly K, Buran DJ, Satz M, Ayre T. Predictors for postoperative otorrhea following tympanostomy tube<br />
insertion. Arch Otolaryngol Head Neck Surg 1992;118:491-494.<br />
Guttenplan MD, Tom LWC, DeVito MA, Handler SD, Wetmore RF, Potsic WP. Radial versus circumferential incision in<br />
myringotomy and tube placement. Int J Pediatr Otorhinolaryngol 1991;21:211-215.<br />
Handler SD, Miller L, Potsic WP, Wetmore RF, Marsh RR. A controlled study of a 'new' ventilating tube. The gold<br />
standard? Int J Pediatr Otorhinolaryngol 1986;12:33-38.<br />
Handler SD, Miller L, Potsic WP, Wetmore RF, Marsh RR. A prospective study of titanium ventilation tubes. Int J Pediatr<br />
Otorhinolaryngol 1988;16:55-60.<br />
Hughes LA, Warder FR, Hudson WR. Complications of tympanostomy tubes. Arch Otolaryngol 1974;100:151-154.<br />
Hunter LL, Margolis RH, Giebink GS. Identification of hearing loss in children with otitis media. Ann Otol Rhinol<br />
Laryngol 1994;103:59-61.<br />
Jurgens GL, Paparella MM. Three new middle ear ventilation tubes. Trans Am Acad Ophthalmol Otolaryngol<br />
1968;76:1017-1019.<br />
Karlan MS, Skobel B, Grizzard M, Cassisi NJ, Singleton GT, Buscemi P, et al. Myringotomy tube materials: bacterial<br />
adhesion and infection. Otolaryngol Head Neck Surg 1980;88:783-795.<br />
http://www.bcm.edu/oto/grand/22395.html (6 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Kleinman LC, Kosecoff J, Dubois RW, Brook RH. The medical appropriateness of tympanostomy tubes proposed for<br />
children younger than 16 years in the United States. JAMA 1994;271:1250-1255.<br />
Kobayashi H, Zusho H. When to remove the ventilation tube - judgment using t-tube on the time to remove the tube. Auris<br />
Nasus Larynx 1985;12(Suppl I):S247-S248.<br />
Le CT, Freeman DW, Fireman BH. Evaluation of ventilating tubes and myringotomy in the treatment of recurrent or<br />
persistent otitis media. Pediatr Infect Dis J 1991;10:2-11.<br />
Levine S, Daly K, Gieink GS. Tympanic membrane perforations and tympanostomy tubes. Ann Otol Rhinol Laryngol<br />
1994;103:27-33.<br />
Levinson SR, Gill AJ. Middle ear semipermeable membrane tubes for prolonged retention. Otolaryngol Head Neck Surg<br />
1986;94:438-440.<br />
Luotonen J, Laitaraki K, Karjalainen H, Jokinen K. EMLA in local anesthesia of the tympanic membrane. Acta Otolaryngol<br />
Suppl 1992;492:63-67.<br />
Luxford WM, Sheehy JL. Myringotomy and ventilation tubes: a report of 1,568 ears. Laryngoscope 1982;92:1293-1297.<br />
Mangat KS, Morrison GAJ, Ganniwalla TM. T-tubes: a retrospective review of 1274 insertions over a 4-year period. Int J<br />
Pediatr Otorhinolaryngol 1993;25:119-125.<br />
Mangat KS, Morrison GAJ, Ganniwalla TM. T-tubes: a retrospective review of 1274 insertions over a 4-year period. Int J<br />
Pediatr Otorhinolaryngol 1993;25:119-125.<br />
Manning SC, Brown OE, Roland PS, Phillips DL. Incidence of sensorineural hearing loss in patients evaluated for<br />
tympanostomy tubes. Arch Otolaryngol Head Neck Surg 1994;120:881-884.<br />
Markowitz-Spence L, Brodsky L, Syed N, Stanievich J, Volk M. Anesthetic complications of tympanotomy tube placement<br />
in children. Arch Otolaryngol Head Neck Surg 1990;116:809-812.<br />
Matt BH, Miller RP, Meyers RM, Campbell JM, Cotton RT. Incidence of perforation with Goode T-tube. Int J Pediatr<br />
Otorhinolaryngol 1991;21:1-6.<br />
Maws AR. Development of tympanosclerosis in children with otitis media with effusion and ventilation tubes. J Laryngol<br />
Otol 1991;105:614-617.<br />
McLelland CA. Incidence of complications from use of tympanostomy tubes. Arch Otolaryngol 1980;106:97-99.<br />
Meyerhoff WL, Morizono T, Wright CG, Shaddock LC, Shea DA, Sikora MA. Tympanostomy tubes and otic drops.<br />
Laryngoscope 1983;93:1022-1027.<br />
Moore PJ. Ventilation tube duration versus design. Ann Otol Rhinol Laryngol 1990;99:722-723.<br />
http://www.bcm.edu/oto/grand/22395.html (7 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Morgan NJ. Penetration of water down the external auditory meatus to the tympanic membrane. J Laryngol Otol<br />
1987;101:536-537.<br />
Pappas JJ. Middle ear ventilation tubes. Laryngoscope 1974;84:1098-1117.<br />
Pashley NRT, Scholl PD. Tympanostomy tubes and liquids - an in vitro study. J Otolaryngol 1984;13:296-298.<br />
Per-Lee JH. A wide flanged middle ear ventilation tube. Trans Am Acad Ophthalmol Otolaryngol 1967;71:358-359.<br />
Prichard AJN, Marshall J, Skinner DW, Narula AA. Long-term results of Good's tympanostomy tubes in children. Int J<br />
Pediatr Otorhinolaryngol 1992;24:227-233.<br />
Pringle MB. Grommets, swimming and otorrhoea - a review. J Laryngol Otol 1993;107:190-194.<br />
Rothera MP, Grant HR. Long-term ventilation of the middle ear using the Goode T-tube. J Laryngol Otol 1985;99:335-337.<br />
Silverstein H. Malleus clip tube for long-term equalization of middle ear pressure. Trans Am Acad Ophthalmol Otolaryngol<br />
1966;70:640-642.<br />
Smelt GJ, Monkhouse WS. The effect of bath water, sea water and swimming pool water on the guinea pig middle ear. J<br />
Laryngol Otol 1985;99:1209-1216.<br />
Summerfield MJ, White PS. Ventilation tube insertion using topical anaesthesia in children. J Laryngol Otol 1992;106:427-<br />
428.<br />
Tami TA, Kennedy KS, Harley E. A clinical evaluation of gold-plated tubes for middle-ear ventilation. Arch Otolaryngol<br />
Head Neck Surg 1987;113:979-980.<br />
Tavin ME, Gordon M, Ruben RJ. Hearing results with the use of different tympanostomy tubes: a prospective study. Int J<br />
Pediatr Otorhinolaryngol 1988;15:39-50.<br />
Tos M, Stanger S-E. Hearing loss in tympanosclerosis caused by grommets. Arch Otolaryngol Head Neck Surg<br />
1989;115:931-935.<br />
Weigel MT, Parker MY, Goldsmith MM, Postma DS, Pillsbury HC. A prospective randomized study of four commonly<br />
used tympanostomy tubes. Laryngoscope 1989;99:252-256.<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
http://www.bcm.edu/oto/grand/22395.html (8 of 9) [5.11.2005 10:45:40]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/22395.html (9 of 9) [5.11.2005 10:45:40]
http://www.bcm.edu/oto/grand/52192.html<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
VESTIBULAR ADAPTATION AND REHABILITATION<br />
Greg Ator, MD<br />
May 21, 1992<br />
A patient presenting with vague disequilibrium and occasional episodic vertigo is a common occurrence<br />
in the general otolaryngology clinic. Typical etiologies include status post head injury and the<br />
vestibulopathy of the elderly. These patients often have mild progressive symptoms without spontaneous<br />
resolution. Many patients, over time, will have resolution of their symptoms, but for the patient who<br />
continues to have symptoms, treatment is frequently required. Traditional treatment methods have relied<br />
upon medication such as Antivert® and Valium® and perhaps Cawthorne type exercises in an attempt to<br />
encourage central nervous system adaptation and rehabilitation. I will briefly describe vestibular<br />
physiology, as it relates to compensation, and discuss the design and efficacy of a program of vestibular<br />
rehabilitation.<br />
http://www.bcm.edu/oto/grand/52192.html (1 of 6) [5.11.2005 10:45:54]
http://www.bcm.edu/oto/grand/52192.html<br />
The function of the vestibular system is to transduce head acceleration into a signal the brain can<br />
interpret. This information is used by the central nervous system (CNS) for gaze stabilization on the<br />
retina and posture control. Transduction is performed for rotational motion by the semicircular canals<br />
and for linear motion by the otolith organs. A spontaneous discharge rate is present in the nerve fibers<br />
arising from these sense organs and rotation or displacement is excitatory in one direction and inhibitory<br />
in the opposite direction. Any difference between the discharge rates of the bilateral symmetrical<br />
vestibular apparatus is perceived as motion.<br />
After a unilateral vestibular insult, there is persistent asymmetry in the vestibular nerve discharge rates<br />
leading to the incorrect sensation of vertigo and motion. These static symptoms, present in the absence of<br />
motion, quickly resolve with restoration of symmetrical discharge rates in the vestibular nuclei.<br />
Symptoms brought about by head motion (dynamic) take longer to compensate and the remaining<br />
vestibular organ as well as the visual system and the somatosensory network work in concert to maintain<br />
posture and balance. In most cases by reliance on these and other inputs the CNS can adapt to the<br />
unilateral loss of input and near normal function in all aspects of daily living can be attained. The<br />
mechanisms for the static and dynamic aspects of vestibular compensation to a peripheral deficit are<br />
largely unknown. Several mechanisms have been proposed: commissural pathways between nuclei of the<br />
vestibular system, reactive synaptogenesis, cerebellum nuclei modifications, and denervation<br />
supersensitivity. The most likely mechanism for resolution of static symptoms is, however, that neurons<br />
of the vestibular nuclei have a spontaneous pacemaker activity which takes over after input is eliminated<br />
from the peripheral organ. The compensation mechanism is affected by external manipulations which are<br />
of therapeutic value. It is known that sedative medications may prolong the time course and decrease the<br />
extent of compensation while stimulants such as amphetamines accelerate compensation. Other external<br />
factors can also influence the compensation process. Visual input is important in dynamic compensation<br />
and animals deprived of visual input do not manifest dynamic compensation although this has no effect<br />
on static deficits. Somatosensory and visual dysfunction impair dynamic compensation. The best<br />
example is the diabetic with retinal and somatosensory disease who suffers a new onset vestibular deficit.<br />
Because of the existence of dysfunction in all three limbs of the posture and balance system,<br />
compensation will likely be very minimal. Exercise is important in vestibular compensation in that<br />
immobility has been demonstrated to prevent dynamic compensation from occurring.<br />
The importance of exercise in vestibular rehabilitation is not new, having first been described by<br />
Cawthorne and Cooksey in 1946. They noted that patients who exercised early after a unilateral ablation<br />
did better and they did so faster than patients who did not exercise. This clinical observation in support of<br />
modern experimental evidence provides the basis for rehabilitation; CNS compensation is facilitated by<br />
exercises with visual and somatosensory stimulation. The first step in a rehabilitation program is an<br />
assessment which is typically performed by a physical or occupational therapist. The patient is<br />
questioned about symptoms and a objective clinical assessment of vestibular function is made by<br />
physical examination, rotatory function, and posturography. A specific, tailored program is developed to<br />
address the particular deficits. The treatment strategy relies on the following factors: balance retraining<br />
for postural control mechanisms; eye and head coordination with progressively more difficult visual<br />
tracking tests; habituation therapy; and a general conditioning program. Indications for rehabilitation<br />
therapy include patients with: movement induced dizziness or poor compensation after a unilateral<br />
http://www.bcm.edu/oto/grand/52192.html (2 of 6) [5.11.2005 10:45:54]
http://www.bcm.edu/oto/grand/52192.html<br />
vestibular injury; status post head injury; the elderly patient with vague disequilibrium; and poor<br />
compensation or recurrent symptoms after surgery.<br />
Several large series have been published recently detailing results from vestibular rehabilitation<br />
programs. Horak and Shemway reported a prospective study of twentyfive subjects with a peripheral<br />
vestibular disorder and symptoms greater than six months duration. These patients were divided into<br />
three treatment groups. The first group underwent a tailored program of twice weekly outpatient<br />
exercises. The second group was given a regiment of general (Cawthorne) exercises. Finally, a third<br />
group was given medications such as Antivert® and Valium® only. The results are encouraging in that<br />
the<br />
patients who were on medication alone showed no objective improvement on posturography scores, but<br />
in the patients who had a tailored vestibular exercise regiment, there was a statistically significant<br />
increase in the posturography scores indicating improvement in compensation. A subjective dizziness<br />
index also showed significant improvement with the vestibular exercise program while no improvement<br />
was seen with the general exercise program and approximately 50% improvement with the medication<br />
alone group.<br />
A prospective study from Shepard et al at the University of Michigan of 98 patients with diagnoses<br />
including peripheral, central, and mixed etiologies. These patients participated in a tailored program with<br />
twice daily home therapy lasting ten to fifteen weeks. Results showed a reduction in symptoms scores in<br />
87% with complete resolution of symptoms in 36%. Patients with head injury accompanied by postural<br />
problems, but with normal visual and somatosensory systems, and those with secondary gain did the<br />
worst. Patients with episodic motion dysfunction had the best prognosis for improvement with this<br />
protocol.<br />
In summary, vestibular rehabilitation is a important treatment modality for patients with vestibular<br />
dysfunction who are not surgical candidates. An increasing proportion of our society, the elderly, are<br />
often prime candidates for vestibular rehabilitation therapy. It appears that patients with peripheral<br />
vertigo with classical symptoms, especially of an episodic variety will definitely benefit from a vestibular<br />
rehabilitation program but also patients with a vague disequilibrium and probable central etiology for this<br />
condition may also benefit from vestibular rehabilitation therapy.<br />
Case Presentation<br />
A 39-year-old female had benign paroxysmal positional nystagmus, vertigo, and imbalance secondary to<br />
a mild blow to the head. She fell while downhill ski racing and hit her head (no loss of consciousness)<br />
but was able to continue her activities within several minutes. She was previously healthy, with no<br />
significant medical problems, led an active life, and continued employment as a nurse. Symptoms of<br />
vertigo, nausea, and disequilibrium progressed over two weeks post-injury and persisted for ten months.<br />
http://www.bcm.edu/oto/grand/52192.html (3 of 6) [5.11.2005 10:45:54]
http://www.bcm.edu/oto/grand/52192.html<br />
Neurologic examination was normal; CT and MRI were negative. Tests of horizontal vestibulo-ocular<br />
reflex control (caloric and rotary chair) were within normal limits. On ENG testing, the patient<br />
demonstrated a directionally fixed vertical oblique nystagmus and vertigo in the right Hallpike position.<br />
All other positional tests were normal. Symptoms progressed to the point of interfering with her work<br />
and she sought medical treatment. She received outpatient therapy twice a week for six weeks, and twice<br />
daily performed home exercises targeted at a variety of postural, gaze, and motion perception disabilities.<br />
In addition, she participated in a low-impact aerobics program several times a week. After six weeks of<br />
therapy, repeat platform posturography revealed that she had normal body sway during all six of the<br />
sensory organization tests and her complaints of dizziness had significantly decreased. She still had mild<br />
complaints (intensity two on a scale of zero to ten) in 12 positions. She continued with her exercises, and<br />
within six months she was vertigo-free in all positions and has remained so.<br />
Bibliography<br />
Baloh RW, Honrubia V. Clinical neurophysiology of the vestibular system. 2nd ed. Philadelphia: F. A. Davis, 1989.<br />
Cawthorne T. Vestibular injuries. Proc R Soc Med 1946;39:270-272.<br />
Cohen B. Erasmus Darwin's observations on rotation and vertigo. Human Neurobiol 1984;3:121-128.<br />
Cooksey FS. Rehabilitation in vestibular injuries. Proc R Soc Med 1946;39:273-275.<br />
Galiana HL, Flohr H, Jones GM. A reevaluation of intervestibular nuclear coupling: its role in vestibular compensation. J<br />
Neurophysiol 1984;51:242-259.<br />
Galiana HL, Outerbridge JS. A bilateral model for central neural pathways in vestibulo-ocular reflex. J Neurophysiol<br />
1984;51:211-241.<br />
Grusser OJ. J. E. Purkyne's contributions to the physiology of the visual, the vestibular and the oculomotor systems.<br />
Human Neurobiol 1984;3:129-144.<br />
Hecker HC, Haug CO, Herndon JW. Treatment of the vertiginous patient using Cawthorne's vestibular exercises.<br />
Laryngoscope 1974;84:2065-2072.<br />
Henn V. E. Mach on the analysis of motion sensation. Human Neurobiol 1984;3:145-148.<br />
Herdman SJ. Exercise strategies for vestibular disorders. Ear Nose Throat J 1989;68:961-964.<br />
Horak FB, JonesRycewicz C, Black FO, ShumwayCook A. Effects of vestibular rehabilitation on dizziness and imbalance.<br />
Otolaryngol Head Neck Surg 1992;106:175-180.<br />
http://www.bcm.edu/oto/grand/52192.html (4 of 6) [5.11.2005 10:45:54]
http://www.bcm.edu/oto/grand/52192.html<br />
Igarashi M. Vestibular compensation: An overview. Acta Otolaryngol 1984;(Suppl 406):78-82.<br />
Igarashi M, Alford BR, Kato Y, Levy JK. Effect of physical exercise upon nystagmus and locomotor dysequilibrium after<br />
labyrinthectomy in experimental primates. Acta Otolaryngol 1975;79:214-220.<br />
Igarashi M, Ishikawa K, Ishii M, Schmidt KA. Effect of ACTH(410) on equilibrium compensation after unilateral<br />
labyrinthectomy in the squirrel monkey. Eur J Pharmacol 1985;19:239-242.<br />
Igarashi M, Levy JK, OUchi T, Reschke MF. Further study of physical exercise and locomotor balance compensation after<br />
unilateral labyrinthectomy in squirrel monkeys. Acta Otolaryngol 1981;92:101-105.<br />
Ito M. Longterm depression. Ann Rev Neurosci 1989;12:85-102.<br />
Leigh DS, Zee DS. The neurology of eye movements, 2nd ed. Philadelphia: F. A. Davis, 1991<br />
Lowenstein O. Fifty years of vestibular science. In: Dawson WW, Enoch JM, editors. Foundations of Sensory Science.<br />
Berlin: SpringerVerlag, 1984: 513-551.<br />
Norre ME, Forrez GHJ, Beckers AM. Vestibular compensation evaluated by rotation tests and posturography. Arch Otol<br />
Head Neck Surg 1987;113:533-535.<br />
Peppard SB. Effect of drug therapy on compensation from vestibular injury. Laryngoscope 1986;96:878-898.<br />
Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol 1988;42:290-293.<br />
Shepard NT, Telian SA, SmithWheelock M. Habituation and balance retraining therapy. Neurol Clin 1990;8:459-475.<br />
ShumwayCook A, Horak FH. Rehabilitation strategies for patients with vestibular deficits. Neurol Clin 1990;8:441-457.<br />
Smith PF, Curthoys IS. Mechanisms of recovery following unilateral labyrinthectomy. Brain Res Rev 1989;14:155-180.<br />
Smith PF, Darlington CL. Neurochemical mechanisms of recovery from peripheral vestibular lesions (vestibular<br />
compensation. Brain Res Rev 1991;16:117-133.<br />
SmithWheelock M, Shepard NT, Telian SA. Physical therapy program for vestibular rehabilitation. Am J Otol<br />
1991;12:218-225.<br />
Thach WT, Goodkin HP, Keating JG. The cerebellum and the adaptive coordination of movement. Annu Rev Neurosci<br />
1992;15:403-442.<br />
Westheimer G. Helmholtz on eye movements. Human Neurobiol 1984;3:149-152.<br />
Zee DS. Adaptation to vestibular disturbances: some clinical implications. Acta Neurol Belg 1991;91:97-104.<br />
http://www.bcm.edu/oto/grand/52192.html (5 of 6) [5.11.2005 10:45:54]
http://www.bcm.edu/oto/grand/52192.html<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
http://www.bcm.edu/oto/grand/52192.html (6 of 6) [5.11.2005 10:45:54]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
<strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong>s<br />
**** DISCLAIMER ****<br />
The information contained within the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> is intended for use by doctors and other<br />
health care professionals. These documents were prepared by resident physicians for presentation and<br />
discussion at a conference held at The Baylor College of Medicine in Houston, Texas. No guarantees are<br />
made with respect to accuracy or timeliness of this material. This material should not be used as a basis<br />
for treatment decisions, and is not a substitute for professional consultation and/or peer-reviewed<br />
medical literature.<br />
VESTIBULAR NEURITIS<br />
July 14, 1994<br />
Douglas D. Backous, M.D.<br />
Vestibular neuritis refers to a disorder of the vestibular system without an associated auditory deficit or<br />
other disease of the central nervous system. It is a unilateral peripheral disorder, primarily affecting<br />
patients in their third and fourth decades, which is associated with ipsilateral caloric weakness. Except<br />
for persistent unsteadiness, symptoms usually resolve by 3-6 months. The episode of vertigo usually<br />
consists of a series of attacks within a 10 day period. Of the patients in Coats' series, 38.2% had an<br />
antecedent infection, 20% with sinusitis, and 61% had spontaneous nystagmus. Besides the unilateral<br />
caloric weakness, electronystagmography reveals a directional preponderance and beating nystagmus<br />
away from the affected side. Vestibular neuritis has also been referred to in the literature as vestibular<br />
neuronitis, epidemic vertigo, acute labyrinthitis, vestibular paralysis, and vestibular neuropathy.<br />
http://www.bcm.edu/oto/grand/71494.html (1 of 5) [5.11.2005 10:46:09]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
A multiple attack variant of vestibular neuritis occurs in a younger age group and consists of recurrent<br />
attacks over months to years. Symptoms of unsteadiness and disequilibrium have shorter duration, and<br />
patients have less severe caloric weakness. Preceding upper respiratory illness is more commonly<br />
reported in this subset of patients.<br />
The differential diagnosis of vestibular neuritis includes Meniere's disease, vestibular schwannoma,<br />
perilymphatic fistula, cerebellar infarction, multiple sclerosis, disequilibrium of aging, basilar artery<br />
insufficiency, vestibular atelectasis, and metastatic carcinoma. Meniere's disease (endolymphatic<br />
hydrops) patients describe tinnitus, fluctuating hearing loss, and frequent episodes of vertigo of duration<br />
limited to hours. Caloric responses are normal early in the course of endolymphatic hydrops. Tinnitus<br />
and hearing losses are much more common in the presentation of vestibular schwannoma than is vertigo.<br />
Patients can have signs of brainstem compression and often have other deficits in cranial nerves,<br />
primarily V and VII. The majority of perilymphatic fistula patients describe "popping" while straining as<br />
a precipitating event to their symptoms. Vertigo is often positional with fluctuating hearing loss and<br />
normal caloric testing. Cerebellar infarction can be caused by hemorrhagic or ischemic events in the<br />
distribution of the anterior inferior or posterior inferior cerebellar arteries. These patients report<br />
symptoms consistent with the single attack variant of vestibular neuritis. Multiple sclerosis is a<br />
demyelinating disease of mainly white matter. Early symptoms include blurred vision, vertigo, cranial<br />
nerve palsies, and awkward extremity use. Nystagmus, scanning speech, and intention tremors occur<br />
later. There is no sex predilection and patients are typically in their third to fourth decades of life when<br />
diagnosed. This disease has an average duration of 20 years from discovery until eventual death.<br />
Findings of oligoclonal banding in CSF and white matter plaques on MRI scanning help establish the<br />
diagnosis. Disequilibrium of aging is due to degenerative changes seen in the vestibular labyrinth and to<br />
interference with fluid motion within labyrinthine sense organs. Sudden head movements exacerbate the<br />
vertigo. Basilar artery insufficiency is caused by occlusion of the vestibular branch of the internal<br />
auditory artery. This most often occurs in an older age group of people who also have high frequency<br />
hearing loss. Additional neurotologic findings are not uncommon. Collapse of vestibular membranous<br />
structures either primarily or as a component of another process such as endolymphatic hydrops is<br />
described as vestibular atelectasis. The most likely etiologies include viral and degenerative changes seen<br />
in aging patients. The principle symptom is unsteadiness with head movement that is not amenable to<br />
medical management but is not severe enough to warrant surgical therapy. The symptoms associated<br />
with metastatic carcinoma to the temporal bone depend on where the metastasis occurs and can include<br />
vertigo or unsteadiness.<br />
Work-up of patients with vestibular neuritis begins with thorough history and physical examination.<br />
Audiometry and vestibular testing are the cornerstones to diagnosis with imaging and laboratory studies<br />
being guided by findings on examination. Bedside examination includes Doll's eye test, head shaking<br />
nystagmus, dynamic visual acuity, caloric testing, rotational testing, past pointing, Romberg and Fukuda<br />
tests, and tandem walking.<br />
Treatment is primarily supportive with reassurance that symptoms will resolve in most cases. Vestibular<br />
suppressants are reserved for patients with severe symptomatology. Medical labyrinthine ablation or<br />
surgical therapy are rarely indicated.<br />
http://www.bcm.edu/oto/grand/71494.html (2 of 5) [5.11.2005 10:46:09]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
In conclusion, the characteristic symptom complex of unilateral vestibular weakness without auditory or<br />
other central nervous system pathology comprises vestibular neuritis. Vestibular nerve atrophy or<br />
degeneration may occur but vascular etiologies are unlikely. Treatment is primarily conservative and the<br />
majority of patients will recover in 3-6 months. Refractory cases should be investigated for other<br />
etiologies.<br />
Case Presentation<br />
A 65-year-old white man presented to the Otolaryngology clinic with a three-day history of severe<br />
vertigo. He reported nausea and vomiting for the first two days of his illness but successfully ate<br />
breakfast on the day he was seen in clinic. He denied hearing loss and tinnitus. His past medical and<br />
surgical histories were unremarkable. He had no previous exposure to ototoxic drugs and denied further<br />
neurologic symptoms. Physical examination revealed an obviously uncomfortable white male in a<br />
wheelchair. Otologic examination was without abnormality. Weber testing with a 512 hz tuning fork was<br />
to midline. Romberg and Fukuda testing indicated right-sided pathology. Other than a crisp left beating<br />
nystagmus, cranial nerve examination was normal. In light of the nystagmus and severe vertigo, the Dix-<br />
Hallpike maneuver was not done. Audiometry revealed a symmetrical mild-to-moderate high frequency<br />
hearing loss. Acoustic reflexes were mildly elevated bilaterally with adequate speech understanding.<br />
Type A tympanograms were present bilaterally. The patient was treated with valium, m q 8 hours. He<br />
returned to the clinic 7 days later, able to walk and with persistent unsteadiness. Electronystagmography<br />
performed one week later revealed 30% unilateral weakness on the right with a 55% directional<br />
preponderance to the right. Rotatory testing revealed a right peripheral disorder. On return clinic followup<br />
he had a residual feeling of unsteadiness but no vertigo.<br />
Bibliography<br />
Adour KK, Sprague MA, Hilsinger RL Jr. Vestibular vertigo: a form of polyneuritis? JAMA 1981;246:1564-1567.<br />
Baloh FW, Honrubia V. Clinical Neurophysiology of the Vestibular System, ed. 2. Philadelphia: F.A. Davis, 1990.<br />
Baloh RW, Jacobson K, Honrubia V. Idiopathic bilateral vestibulopathy. Neurology 1989;39:272-275.<br />
Brandt T, Dieterich M. Vestibular falls. J Vestibular Res 1993;3:3-14.<br />
Brantberg K, Magnusson M. The dynamics of the vestibulo-ocular reflex in patients with vestibular neuritis. Am J<br />
Otolaryngol 1990;11:345-351.<br />
http://www.bcm.edu/oto/grand/71494.html (3 of 5) [5.11.2005 10:46:09]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Coats AC. Vestibular neuronitis. Tran Am Acad Ophthalmol Otolaryngol 1969;73:395-408.<br />
Davis LE. Infections of the labyrinth. In: Cummings CW, Harker LA, eds. Otolaryngology - Head and Neck Surgery, Vol.<br />
4. St. Louis: Mosby, 1993:2795-2807.<br />
Davis LE, Shurin S, Johnson RT. Experimental viral labyrinthitis. Nature 1975;254:329-331.<br />
Davis LE. Comparative experimental viral labyrinthitis. Am J Otolaryngol 1990;11:382-388.<br />
Disher MJ, Telian SA, Kemink JL. Evaluation of acute vertigo: unusual lesions imitating vestibular neuritis. Am J Otol<br />
1991;12:227-231.<br />
Fluur E. Interaction between the utricles and the horizontal semicircular canals. IV. Tilting of human patients with acute<br />
unilateral vestibular neuritis. Acta Otolaryngol 1973;76:349-352.<br />
Gagey PM, Toupet M. Orthostatic postural control in vestibular neuritis: a stabilometric analysis. Ann Otol Rhinol<br />
Laryngol 1991;100:971-975.<br />
Karmody CS. Viral labyrinthitis: early pathology in the human. Laryngoscope 1983;93:1527-1533.<br />
Kemink JL, Telian SA, El-Kashlan H, Langman AW. Retrolabyrinthine vestibular nerve section: efficacy in disorders<br />
other than Meniere's disease. Laryngoscope 1991;101:523-528.<br />
Lachman J, Stahle J. Vestibular neuritis: a clinical and electronystagmographic study. Neurology 1967;17:376-380.<br />
Lindsay JR, Vital labyrinthitis - histopathologic characteristics. Acta Otolaryngol 1967;63:138-143.<br />
Magnusson M, Brantberg K, Pyykkö, Schalén L. Reduction of the time constant in the VOR as a protective mechanism in<br />
acute vestibular lesions. Acta Otolaryngol Suppl 1989;468:329-332.<br />
Montandon PB, Häusler R. Relevance of otopathological findings in the treatment of dizzy patients. Ann Otol Rhinol<br />
Laryngol Suppl 1984;112:12-16.<br />
Pfaltz CR. Vestibular compensation: physiological and clinical aspects. Acta Otolaryngol 1983;95:402-406.<br />
Rahko T, Karma P. New clinical finding in vestibular neuritis: high-frequency audiometry hearing loss in the affected ear.<br />
Laryngoscope 1986;96:198-199.<br />
Schuknecht HF, Kitamura K., Vestibular neuritis. Ann Otol Rhinol Laryngol Suppl 1981;78:1-19.<br />
Schuknecht HF, Witt RL. Acute bilateral sequential vestibular neuritis. Am J Otolaryngol 1985;6:255-257.<br />
Yoneda S, Tokumasu K. Frequency analysis of body sway in the upright posture: statistical study in cases of peripheral<br />
vestibular disease. Acta Otolaryngol 1986;102:87-92.<br />
http://www.bcm.edu/oto/grand/71494.html (4 of 5) [5.11.2005 10:46:09]
From the <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> at Baylor<br />
Return <strong>Grand</strong> <strong>Rounds</strong> <strong>Archive</strong> Index<br />
Return to BCOM Otolaryngology Home Page<br />
® Copyright, 1996. All Rights Reserved.<br />
Baylor College of Medicine. Bobby R. Alford Department of Otorhinolaryngology and Communicative Sciences.<br />
http://www.bcm.edu/oto/grand/71494.html (5 of 5) [5.11.2005 10:46:09]