“FEDERICO II” UNIVERSITY OF NAPLES PhD Program ... - FedOA
“FEDERICO II” UNIVERSITY OF NAPLES PhD Program ... - FedOA
“FEDERICO II” UNIVERSITY OF NAPLES PhD Program ... - FedOA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Martinelli et al<br />
Safety of embolization for ectopic pregnancy<br />
761<br />
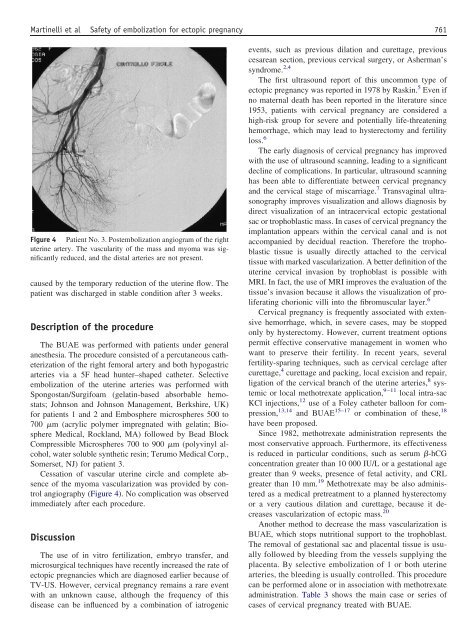
Figure 4 Patient No. 3. Postembolization angiogram of the right<br />
uterine artery. The vascularity of the mass and myoma was significantly<br />
reduced, and the distal arteries are not present.<br />
caused by the temporary reduction of the uterine flow. The<br />
patient was discharged in stable condition after 3 weeks.<br />
Description of the procedure<br />
The BUAE was performed with patients under general<br />
anesthesia. The procedure consisted of a percutaneous catheterization<br />
of the right femoral artery and both hypogastric<br />
arteries via a 5F head hunter–shaped catheter. Selective<br />
embolization of the uterine arteries was performed with<br />
Spongostan/Surgifoam (gelatin-based absorbable hemostats;<br />
Johnson and Johnson Management, Berkshire, UK)<br />
for patients 1 and 2 and Embosphere microspheres 500 to<br />
700 m (acrylic polymer impregnated with gelatin; Biosphere<br />
Medical, Rockland, MA) followed by Bead Block<br />
Compressible Microspheres 700 to 900 m (polyvinyl alcohol,<br />
water soluble synthetic resin; Terumo Medical Corp.,<br />
Somerset, NJ) for patient 3.<br />
Cessation of vascular uterine circle and complete absence<br />
of the myoma vascularization was provided by control<br />
angiography (Figure 4). No complication was observed<br />
immediately after each procedure.<br />
Discussion<br />
The use of in vitro fertilization, embryo transfer, and<br />
microsurgical techniques have recently increased the rate of<br />
ectopic pregnancies which are diagnosed earlier because of<br />
TV-US. However, cervical pregnancy remains a rare event<br />
with an unknown cause, although the frequency of this<br />
disease can be influenced by a combination of iatrogenic<br />
events, such as previous dilation and curettage, previous<br />
cesarean section, previous cervical surgery, or Asherman’s<br />
syndrome. 2,4<br />
The first ultrasound report of this uncommon type of<br />
ectopic pregnancy was reported in 1978 by Raskin. 5 Even if<br />
no maternal death has been reported in the literature since<br />
1953, patients with cervical pregnancy are considered a<br />
high-risk group for severe and potentially life-threatening<br />
hemorrhage, which may lead to hysterectomy and fertility<br />
loss. 6<br />
The early diagnosis of cervical pregnancy has improved<br />
with the use of ultrasound scanning, leading to a significant<br />
decline of complications. In particular, ultrasound scanning<br />
has been able to differentiate between cervical pregnancy<br />
and the cervical stage of miscarriage. 7 Transvaginal ultrasonography<br />
improves visualization and allows diagnosis by<br />
direct visualization of an intracervical ectopic gestational<br />
sac or trophoblastic mass. In cases of cervical pregnancy the<br />
implantation appears within the cervical canal and is not<br />
accompanied by decidual reaction. Therefore the trophoblastic<br />
tissue is usually directly attached to the cervical<br />
tissue with marked vascularization. A better definition of the<br />
uterine cervical invasion by trophoblast is possible with<br />
MRI. In fact, the use of MRI improves the evaluation of the<br />
tissue’s invasion because it allows the visualization of proliferating<br />
chorionic villi into the fibromuscular layer. 6<br />
Cervical pregnancy is frequently associated with extensive<br />
hemorrhage, which, in severe cases, may be stopped<br />
only by hysterectomy. However, current treatment options<br />
permit effective conservative management in women who<br />
want to preserve their fertility. In recent years, several<br />
fertility-sparing techniques, such as cervical cerclage after<br />
curettage, 4 curettage and packing, local excision and repair,<br />
ligation of the cervical branch of the uterine arteries, 8 systemic<br />
or local methotrexate application, 9–11 local intra-sac<br />
KCl injections, 12 use of a Foley catheter balloon for compression,<br />
13,14 and BUAE 15–17 or combination of these, 18<br />
have been proposed.<br />
Since 1982, methotrexate administration represents the<br />
most conservative approach. Furthermore, its effectiveness<br />
is reduced in particular conditions, such as serum -hCG<br />
concentration greater than 10 000 IU/L or a gestational age<br />
greater than 9 weeks, presence of fetal activity, and CRL<br />
greater than 10 mm. 19 Methotrexate may be also administered<br />
as a medical pretreatment to a planned hysterectomy<br />
or a very cautious dilation and curettage, because it decreases<br />
vascularization of ectopic mass. 20<br />
Another method to decrease the mass vascularization is<br />
BUAE, which stops nutritional support to the trophoblast.<br />
The removal of gestational sac and placental tissue is usually<br />
followed by bleeding from the vessels supplying the<br />
placenta. By selective embolization of 1 or both uterine<br />
arteries, the bleeding is usually controlled. This procedure<br />
can be performed alone or in association with methotrexate<br />
administration. Table 3 shows the main case or series of<br />
cases of cervical pregnancy treated with BUAE.