InFocus Magazine 2007 - Hampshire Hospitals NHS Foundation Trust
InFocus Magazine 2007 - Hampshire Hospitals NHS Foundation Trust
InFocus Magazine 2007 - Hampshire Hospitals NHS Foundation Trust
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
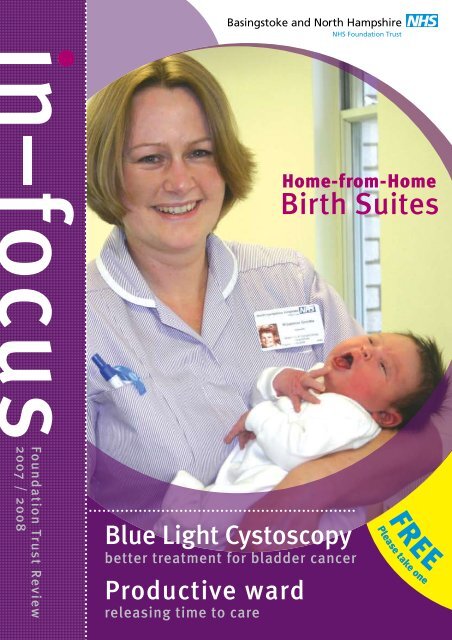
Basingstoke and North <strong>Hampshire</strong><br />
<strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong><br />
<strong>NHS</strong><br />
Home-from-Home<br />
Birth Suites<br />
<strong>Foundation</strong> <strong>Trust</strong> Review<br />
<strong>2007</strong> / 2008<br />
Blue Light Cystoscopy<br />
better treatment for bladder cancer<br />
Productive ward<br />
releasing time to care<br />
FREE<br />
Please take one
02<br />
Comments or suggestions?<br />
Please contact the communications<br />
team on (01256) 313062 or<br />
e-mail enquiries@bnhft.nhs.uk<br />
It’s been another great<br />
year for our <strong>Trust</strong>.<br />
Being authorised as<br />
a <strong>Foundation</strong> <strong>Trust</strong><br />
on 1 December was<br />
testament to the<br />
hard work of our<br />
staff members, who<br />
remain committed to<br />
our overarching aim:<br />
delivering high-quality<br />
services for our patients<br />
and their families.<br />
In this review we’d like to share<br />
some of the year’s achievements<br />
- from our refurbished maternity<br />
department, with more homely<br />
facilities, to the high-tech blue laser<br />
that makes it easier to identify bladder<br />
cancer. You can also read about some<br />
of the ways we’re working to improve<br />
the hospital – like our campaign<br />
to reduce hospital infections, and<br />
improvements to our nationallyacclaimed<br />
stroke service.<br />
But work at the <strong>Trust</strong> never stands<br />
still and, as we look forward to the<br />
next year, we’re planning exciting new<br />
developments. As a <strong>Foundation</strong> <strong>Trust</strong><br />
we’re now in a stronger position to<br />
develop locally-sensitive services. We’re<br />
relying on our members and governors<br />
to help us shape the future and deliver<br />
the best possible healthcare for the<br />
people of North <strong>Hampshire</strong>. We’re<br />
also relying on the local community<br />
to keep providing feedback and<br />
suggestions – we want to make<br />
our healthcare truly yours.<br />
Mary Edwards<br />
Chief executive<br />
Home-from-home Birth Suites<br />
even influence whether birth is normal or<br />
requires emergency surgery. Women giving<br />
birth in a homely environment are more<br />
relaxed and in control of their labour, which<br />
is more likely to result in a normal birth.<br />
Sofas, birth mats and en-suite<br />
bathrooms are just some of the<br />
facilities at our new, more homely<br />
maternity suites!<br />
The importance of homely surroundings<br />
In 2005 the National Childbirth <strong>Trust</strong> survey<br />
showed that comfortable surroundings can<br />
help to improve a woman’s birth experience.<br />
So when we redesigned our maternity units<br />
at Basingstoke and North <strong>Hampshire</strong> <strong>NHS</strong><br />
<strong>Foundation</strong> <strong>Trust</strong>, we incorporated two<br />
homely birth suites.<br />
The research showed that women believe<br />
their environment can affect their labour.<br />
The type and quality of birthing facilities could<br />
The new suites<br />
The Oasis and Orchid suites are designed<br />
to emulate a home environment. The large,<br />
en-suite rooms feature sofas, birthing balls<br />
and mats, and the Oasis suite also has a<br />
birthing pool. The philosophy behind the<br />
design focuses on promoting normal, active<br />
birth. The birthing balls and mats help<br />
women to remain active in labour. It has<br />
also been shown that women who choose<br />
to give birth in these environments use<br />
less traditional pain relief. The pool and<br />
additional facilities will provide ‘natural’<br />
pain relief options.<br />
Both rooms are available on a first come<br />
first served basis, and don’t need to be<br />
pre-booked - the decision to use a birthing<br />
suite can be made at any time leading<br />
up to the birth of the baby. For more<br />
information, contact the Maternity Unit or<br />
the community midwives.<br />
Nursing awards <strong>2007</strong><br />
Commitment to care, compassion and<br />
dedication are rewarded at our annual<br />
Director of Nursing awards.<br />
After announcing the award programme<br />
in April, we were inundated with nomination<br />
forms – more than 150 people wanted<br />
to commend nurses who had treated<br />
them with kindness and respect. In every<br />
category we were overwhelmed with the<br />
quality of submissions; individual nurses,<br />
midwives and teams have made a huge<br />
contribution to our hospital this year. In<br />
July Donna Green, our Director of Nursing,<br />
presented the awards at the Sherfield<br />
School in Basingstoke.
03<br />
New Cystic Fibrosis Screening<br />
Sexual health on schedule<br />
to meet 48-hour target<br />
Early detection of cystic fibrosis can lessen<br />
the risk of life-threatening complications, so<br />
our new testing will give many parents peace<br />
of mind. The cystic fibrosis test is now part<br />
of routine testing on the blood spot taken by<br />
our midwives on the 5th – 8th day after birth.<br />
This initial test is designed to identify ‘at risk’<br />
children, who can then go on for further testing<br />
and, if diagnosed with cystic fibrosis, can begin<br />
early treatment. Of course most tests will return<br />
with normal results, which are given to parents<br />
by the health visitor or GP. If the result gives<br />
cause for concern, the family will be contacted<br />
directly within two days. It’s important to note<br />
that although the test provides a good early<br />
indication of possible sufferers, it won’t pick<br />
up every case, and GPs are still on the alert for<br />
children with suspicious symptoms in their early<br />
months and years.<br />
Sexual Health Clinic: 01256 313333<br />
Our Sexual Health clinic is now offering 99% of new patients an appointment<br />
within 48 hours. This puts us firmly on-track for the Department of<br />
Health’s latest target. More than 6000 patients were seen at the<br />
clinic last year, of which 448 were diagnosed with Chlamydia<br />
– the more common infection in our area. The clinic is<br />
now working on ways to improve public awareness of<br />
this often-silent infection. Chlamydia doesn’t always<br />
show its symptoms. It can hide in the body for<br />
a number of years before causing any problems.<br />
However, once detected it can be treated<br />
with antibiotics, and it’s easily cleared.<br />
Developments in Cardiology<br />
With angioplasty and angiogram waiting lists<br />
at an all-time low and outpatients waiting less than<br />
7 weeks, our Cardiology division has streamlined<br />
its operations this year. Because of its excellent<br />
performance, the division has been selected to pilot<br />
a review designed to help achieve the government’s<br />
18-week waiting target (referral to treatment). The<br />
team will soon welcome a brand new laser treatment,<br />
to be offered as an alternative to angioplasty, as the<br />
latest addition to their pioneering developments.
04<br />
Assessing patient care at the Diagnosis and Treatment Centre<br />
On average our Diagnosis and Treatment<br />
Centre (DTC) sees up to 1000 patients<br />
every month. With such a high volume of<br />
patients coming and going, it would be<br />
easy to focus on the numbers and forget<br />
about the patient’s individual experience.<br />
So we’ve introduced a system of assessing<br />
the quality of care - by consulting directly<br />
with patients.<br />
The DTC sees a wide variety of patients<br />
- requiring a general anaesthetic, sedation<br />
or local anaesthetic – aged between<br />
12 months and 95 years! We cover most<br />
specialties - ear, nose and throat, general<br />
surgery, orthopaedics, gynaecology,<br />
endoscopy and urology, to name a few.<br />
Patient choice and opinion is very important<br />
here. The DTC team follows up every patient<br />
who has been anaesthetised or sedated,<br />
carrying out a telephone questionnaire to<br />
find out how they felt about the service they<br />
received in our care. These questionnaires<br />
are audited and the results used to improve<br />
patient service. If several patients highlight the<br />
same problem or issue, we won’t wait around<br />
- the issue will be immediately investigated<br />
and rectified. These questionnaires are<br />
also used to highlight areas in the DTC<br />
for further audit such as post-operative<br />
pain control. Telephoning the patient the<br />
following day also provides them with the<br />
opportunity to ask questions that may have<br />
arisen since discharge. If patients or their<br />
carers have comments while in our care,<br />
they can also write in the comment books<br />
in discharge areas and wards.<br />
Since introducing the questionnaires we’ve<br />
been able to make some positive changes<br />
that benefit patients. People frequently<br />
told us that they had forgotten the advice<br />
given to them on discharge, so we now<br />
give all patients their wound care advice<br />
in writing, with details about removing<br />
dressings or having sutures removed.<br />
We’ve also been prompted to investigate<br />
the amount of time patients can wait for<br />
certain procedures, particularly endoscopy.<br />
Our team is working out how staggered<br />
admission times can be improved to avoid<br />
patients’ long waits.<br />
For further information on the work of the<br />
DTC please contact Modern Matron, Kathy<br />
Barton or email kathy.barton@bnhft.nhs.uk<br />
Meet The School Nurse<br />
What does a School nurse do?<br />
We send nurses to schools for three important reasons:<br />
For many children, the school nurse is their<br />
first source of information about physical and<br />
emotional health. As well as organising events<br />
and promoting health messages, the school<br />
nurse does something very important: listening<br />
to children’s worries and concerns.<br />
To give confidential advice, care and treatment to children<br />
(and their parents or carers)<br />
To promote physical and emotional health and to help teachers<br />
understand what children need to be healthy<br />
To help protect and safeguard children from significant harm<br />
Why is this role important?<br />
In practice, a school nurse has a very diverse role. School nurses act<br />
as a link between school and other organisations, like children’s<br />
services and the police. They organise immunisation programmes<br />
and help teachers with their personal and social health education<br />
lessons. It’s important that teachers themselves understand how to<br />
deal with health issues such as allergies, epilepsy, and asthma, and<br />
the school nurse can help train teaching staff in this respect.<br />
But the school nurse is also available whenever children need<br />
confidential, independent advice. Children and young people<br />
can see a school nurse in school for lots of different reasons –<br />
for instance:<br />
To talk about their health or worries in confidence<br />
To get emotional support, for example if they have problems<br />
with friends or at home<br />
To assess for any health problems and refer to somebody else<br />
who can help, for example, a doctor<br />
To give advice on smoking, relationships or sexual health
05<br />
Advances in stroke care<br />
and rehabilitation<br />
The Oakley Stroke and Rehabilitation Unit is a national centre of excellence,<br />
committed to improving the standards of modern stroke care.<br />
“Gone are the days when a stroke would leave patients and<br />
clinicians alike powerless,” says Consultant Stroke Physician,<br />
Dr Elio Giallombardo. “These days nurses, doctors and therapists<br />
have the evidence and the equipment to save lives and restore<br />
an increasing proportion of patients to their previous lifestyle.”<br />
Reducing waiting times<br />
“By 2008, no one will have to wait longer than<br />
18 weeks from GP referral to hospital treatment”<br />
<strong>NHS</strong> Improvement Plan, June 2004<br />
The stroke pathway<br />
Every patient admitted with a stroke diagnosis is assessed by<br />
our specialist team. Most patients are transferred to the Oakley<br />
Stroke and Rehabilitation Unit at the earliest opportunity. If there<br />
are any delays in transfer, the team will visit the patient on the<br />
admission ward, ensuring all the correct support is in place.<br />
This year the national audit of stroke care showed that 80%<br />
of our stroke patients are treated in our own stroke and<br />
rehabilitation unit, against a 62% national average. We’d like<br />
to get that figure closer to 100%, and have opened more beds<br />
at Alton Community Hospital for the purposes of rehabilitation.<br />
This ensures that patients with ongoing rehabilitation needs<br />
continue to receive the care they need, and frees up beds for<br />
the acute patients to be cared for in the right place.<br />
A model of good practice<br />
Getting patients treated in a place like our Stroke and<br />
Rehabilitation Unit, where the most experienced clinicians<br />
can work together, is key to success. Our good work did not<br />
escape the attention of the <strong>NHS</strong> Institute for Innovation and<br />
Improvement and we were one of five acute trusts invited to<br />
share our experience on caring for stroke patients. This led to the<br />
development of a Stroke Care Pathway to be piloted in a number<br />
of hospitals across the country.<br />
Preparing for the future<br />
We plan to maintain our reputation as a centre of excellence.<br />
We’re anticipating an exciting new option – clot-busting<br />
treatment – for certain stroke patients. It’s extremely effective<br />
in preventing disability, but to work must be started within<br />
3 hours of the onset of symptoms. “Stroke will continue to<br />
be a devastating illness for a proportion of patients and their<br />
families,” says Dr Giallombardo, “but the days of general<br />
hopelessness and despair are truly gone.”<br />
Time is Brain<br />
THE 18-WEEK TARGET is one of the most ambitious access<br />
targets the <strong>NHS</strong> will ever have delivered. For the first time in the<br />
history of the <strong>NHS</strong>, patient journey time will be measured from<br />
start to finish – including the times between diagnostic and<br />
outpatient appointments, which are mostly unmeasured.<br />
When it’s achieved, the 18-week target will enormously improve<br />
the experience of every patient in <strong>NHS</strong> care.<br />
Basingstoke and North <strong>Hampshire</strong> <strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong> has<br />
been declared an ‘Early Achiever’ which means that, in certain<br />
departments, we will be meeting the 18-week target one year<br />
early (December <strong>2007</strong>). We are currently piloting it in four<br />
specialties: Cardiology, Orthopaedics, Gynaecology and Urology.<br />
By March next year, we will extend the programme to every<br />
specialty in the hospital.<br />
The target demands a united approach from all our staff and<br />
clinical teams. To achieve it, we will be modernising services,<br />
implementing new technology, hiring and allocating new staff,<br />
ensuring faster access to diagnostics, assessing whether there are<br />
enough staff and making sure there are appointments and clinics<br />
available to see, diagnose and treat patients quickly.<br />
We will need to accurately record how long each patient’s<br />
journey takes. We know that, in many cases, patients are already<br />
seen, diagnosed and treated within 18 weeks, but this is not<br />
recorded yet. We are now working with clinicians and admin<br />
staff to monitor and assess every patient journey. By 2008, the<br />
patient journey should be as smooth and efficient as it’s ever<br />
been – and we’ll be right on target.
06<br />
Productive ward<br />
releasing time to care<br />
The premise is simple:<br />
To review working practices and give<br />
nursing staff more time to spend with<br />
patients. Using knowledge from the<br />
commercial and business worlds, we can<br />
tighten efficiency to release more time.<br />
In conjunction with the <strong>NHS</strong> Institute<br />
for Innovation and Improvement, our<br />
hospital has embarked on a project<br />
designed to conserve the time of<br />
nursing staff.<br />
Our nursing team on C3 are closely<br />
involved in the project, helping to<br />
determine areas of need. For example,<br />
the nurses are frequently interrupted<br />
by visitors who are looking for patients.<br />
These interruptions can take nurses’<br />
attention away from important or<br />
urgent tasks. Nurses, medical staff<br />
and patients discussed this problem<br />
and came up with the ‘patient location<br />
board’. This displays the ward layout<br />
with each patient’s name in their<br />
allocated bed space. It enables visitors<br />
to see at a glance where the patient<br />
is and therefore nurses are not<br />
interrupted as frequently.<br />
Stock cupboards on each ward<br />
have also been reorganised. These<br />
cupboards – one per ward – contain<br />
all the frequently-used items that<br />
may be needed when patients<br />
suddenly feel unwell. They were not<br />
regularly stocked and were mostly<br />
in disarray, making it difficult to<br />
quickly access equipment. There was<br />
no consistency in their layout or<br />
contents. Nursing staff agreed to<br />
rationalise the contents, stick to one<br />
layout and designate someone to<br />
top up stock on a daily basis. Now a<br />
cupboard in bay 3 and a cupboard<br />
in bay 5 are arranged in the same<br />
orderly fashion, making them quicker<br />
for nurses to access.<br />
Plenty of other measures have been<br />
identified to free up time: a redesign<br />
of the nurses’ station, rationalisation<br />
of stock in the sub-pharmacy area<br />
(saving almost £1,000), an information<br />
leaflet for patients on the ward<br />
routine and the trial of equipment<br />
that will automate the management<br />
of supplies.<br />
This ongoing project has already<br />
brought many positive outcomes.<br />
Staff members have embraced the<br />
opportunity to foster a culture of<br />
change, nurses and patients have<br />
engaged in decisions affecting their<br />
environment and visitor feedback<br />
has also been positive. As a result of<br />
this project’s success, it will soon be<br />
adapted by other departments in the<br />
<strong>Trust</strong>, freeing up time and improving<br />
patient care right across the hospital.<br />
Two Week Rule and the Breast Symptomatic Service<br />
When cancer is suspected, early diagnosis and swift treatment<br />
are vital. The government has installed a number of targets to<br />
make sure this happens, and the ‘Two Week Rule’ (TWR)<br />
is one of these. Current guidelines say that patients<br />
referred with suspected breast cancer should be offered<br />
an appointment within two weeks; and all cancer patients<br />
should be offered treatment within 31 days of referral.<br />
To reach these targets this year, our breast cancer team<br />
has continued to make some great improvements to their<br />
service. Patients with suspected breast cancer can take<br />
advantage of our one-stop service, where they will have a<br />
clinical consultation, mammogram, ultrasound and/or needle<br />
and core biopsy at one appointment. As well as being far<br />
more convenient for patients, this speeds up the diagnosis<br />
process. It’s also enabled us to meet all cancer-related targets<br />
This year we have seen:<br />
374 TWR referrals<br />
168 new patients with primary breast cancer<br />
And we have recorded the following average times:<br />
Time from TWR referral to treatment: 35 days<br />
Time from ‘Decision to Treat’ to treatment: 14 days<br />
These figures meet all of our targets, ensuring that all<br />
cancer TWR patients are treated within 62 days of referral<br />
and that all cancer patients receive their first treatment<br />
within 31 days of deciding which treatment is appropriate.<br />
This is down to a dedicated multi-disciplinary team working<br />
hard to ensure all cancer patients receive the best possible<br />
care in a timely manner.
07<br />
Blue Light Cystoscopy<br />
better treatment for bladder cancer<br />
Patients from North <strong>Hampshire</strong> have become<br />
some of the first in the country to be offered<br />
Blue Light Cystoscopy. This brilliant new<br />
technique is reducing the likelihood of cancer<br />
recurrence from 35% to 10%.<br />
12,000 patients a year are diagnosed with<br />
bladder cancer, making it the 5th most<br />
common cancer in the UK. 4,000 of these<br />
patients will die of the disease. In its earliest<br />
stages, bladder cancer is treated by ‘resecting’<br />
the tumour off the bladder wall using a<br />
telescope (Cystoscopy) under anaesthetic.<br />
However, even after this treatment tumours<br />
can recur for 35% of patients. This means<br />
that patients have to come back for frequent<br />
Cystoscopy of their bladder to detect and<br />
treat any tumours at an early stage. This isn’t<br />
just expensive for the health system but very<br />
unsettling for patients too.<br />
One of the main reasons so many patients get<br />
a recurrence is that most tumours are invisible<br />
to the naked eye under normal ‘white light’<br />
(see picture 1). It can be difficult, after surgery,<br />
to be sure that all of the tumour has been removed.<br />
Blue Light Cystoscopy addresses this problem.<br />
1. White Light Cystoscopy<br />
2. Blue Light Cystoscopy<br />
What is Blue Light Cystoscopy?<br />
Used with the fluorescent dye Hexvix, the Blue<br />
Light Cystoscopy reveals tumours with better<br />
clarity. Hexvix is instilled into the bladder an<br />
hour before Cystoscopy, where it is selectively<br />
taken up (absorbed) by the bladder tumours.<br />
When blue light is shone onto the area, these<br />
tumours reflect fluorescent light (see picture 2<br />
- same as picture 1 but with ‘blue light’). This<br />
technique is called photodynamic diagnosis,<br />
or PDD.<br />
Better results<br />
This new technique is exciting because it<br />
makes removal and detection of bladder<br />
tumours much easier. A medical trial showed<br />
that Blue Light Cystoscopy reduces the<br />
recurrence rate of bladder cancer from 35%<br />
to just 10%. Last year, about 100 bladder<br />
resections were carried out at Basingstoke<br />
and North <strong>Hampshire</strong> Hospital. With current<br />
techniques, we would expect about 35 of<br />
these to recur. With Blue Light Cystoscopy, we<br />
can expect just 10 recurrences – that means<br />
25 more patients would be permanently<br />
cancer-free.<br />
Liver Surgery at Basingstoke<br />
More than 100 patients had liver surgery at Basingstoke and<br />
North <strong>Hampshire</strong> Hospital last year – referred from all over south<br />
England and Wales. Although their condition is relatively rare, new<br />
treatments and techniques are developing all the time, and our<br />
team is at the forefront of modern science.<br />
The current surgical team – Myrddin Rees, Tim John and Fenella<br />
Welsh – carries out liver surgery for malignant disease, removing<br />
either primary or metastatic (secondary) liver cancers. Before<br />
booking patients in for surgery, an MRI scan is used to make sure<br />
the tumours are removable in a way that will preserve enough<br />
functioning liver. Surgery – which at Basingstoke is usually keyhole<br />
surgery – offers 30% of patients a long-term cure.<br />
For many patients, though, surgery isn’t appropriate, and other<br />
options will be suggested. Radio Frequency Ablution is often<br />
recommended. This is a method of “cooking” small tumours<br />
which is carried out in the x-ray department. Fenella Welsh is also<br />
developing intraoperative microwave ablation, an exciting new<br />
technique that we hope to offer in the near future. The increased<br />
capacity for chemotherapy at our hospital gives many more patients<br />
the opportunity to receive effective treatment.
flat and a multifunctional ‘quiet room’ that opens onto a patio<br />
garden with table, chairs and a water feature.<br />
Who Works here?<br />
The Neonatal Unit requires the input of many professionals,<br />
ranging from paediatric consultants to nursery nurses.<br />
The nursing team is specially trained in the intensive<br />
care of newborns, with individual specialisms like infant<br />
feeding. Other team members who attend the unit<br />
include physiotherapy staff, an ophthalmologist, health<br />
visitors, midwives, social workers and staff from the<br />
Drug Advisory Centre.<br />
How are you making a difference?<br />
Sick or premature babies have a wide and diverse range of<br />
healthcare needs. It’s crucial that we keep our equipment<br />
maintained and replaced, and this year we’ve had two new<br />
incubators, which have been a great asset for the babies.<br />
Parents at the Neonatal Unit receive plenty of support, too.<br />
Many babies can spend several weeks in the unit until they have<br />
established feeding, gained weight and are able to maintain their<br />
temperature. Our nursing and support staff offer parentcraft<br />
training to help parents manage their newborn.<br />
08<br />
What happens here?<br />
The Neonatal Unit is part of the Maternal and Child Health Division,<br />
and is situated on the ground floor of the Sherborne building.<br />
Here we care for newborn babies who are ill or premature.<br />
As well as fourteen cots (divided between intensive and high<br />
care) there are also parents’ facilities – an expressing room for<br />
breastfeeding mothers, a milk kitchen, a pay-phone, a self-contained<br />
We think a comfortable environment is important – and this year we<br />
commissioned several bright, nursery-style murals all around the unit.<br />
How many admissions?<br />
Last year we admitted 248 babies (from 2,592 total deliveries).<br />
Reasons for admission include prematurity, difficult birth, congenital<br />
abnormalities, neonatal abstinence syndrome and jaundice. We also<br />
admit babies for adoption or whose parents are unable to care for<br />
them and infants who may have child protection issues.<br />
Orthopaedic Trauma Ward<br />
If you are injured in a Road<br />
Traffic Accident (RTA),<br />
have a fall, a significant<br />
sports injury or require<br />
complex surgery to<br />
realign bones you may<br />
find yourself in our<br />
Orthopaedic Trauma Unit.<br />
Our dedicated team of surgeons,<br />
doctors, nurses, physiotherapists<br />
and occupational therapists are<br />
supported by many other health<br />
professionals to deliver the<br />
optimum care to our patients<br />
on the ward.<br />
They will also ensure that the<br />
follow-up rehabilitation is<br />
carried out in the most suitable<br />
manner liaising with any<br />
outside agencies to facilitate<br />
this happening. Our team of<br />
domestics and housekeeping<br />
staff are responsible for<br />
delivering a clean and safe<br />
environment, supporting health<br />
professionals to maintain<br />
our low infection rates. For<br />
example in the recently reported<br />
‘National Site Surveillance’<br />
statistics, which reviews wound<br />
infections; the Orthopaedic<br />
Trauma Unit had a rate of 0%<br />
compared to a national<br />
rate of 4.3%.<br />
Last year there were 1,350<br />
admissions to the ward and<br />
the injuries varied from broken<br />
ankles and wrists to serious neck<br />
and back injuries with a length<br />
of stay ranging from a few hours<br />
to many months.
09<br />
Rachael Hartley, Occupational Therapist<br />
Working jointly with other members of the team (doctors,<br />
nurses, physiotherapists, speech and language therapists and<br />
social workers), attending meetings and case conferences.<br />
Completing projects such as audits, service development and<br />
presenting at groups (like the pulmonary rehabilitation group).<br />
Why did you decide to become an Occupational Therapist?<br />
I first discovered occupational therapy when a family member<br />
became ill and received input from an occupational therapist (OT).<br />
Seeing the positive outcomes made me interested to explore the<br />
profession further, but it was later that I realised it fulfilled all of<br />
my criteria. We help people realise functional independence and<br />
promote a better quality of life. They can work in a variety of<br />
settings including mental health the community or paediatrics.<br />
In the hospital there is the opportunity to work in a number of<br />
specialist areas depending on your interests.<br />
What does your job entail?<br />
The main aim of occupational therapy at the hospital is to<br />
provide a safe and rapid discharge. We work closely with<br />
medics, nurses, physiotherapists and social workers to achieve<br />
this. I’m called on to provide:<br />
Assessments of daily living (washing and dressing, meal<br />
preparation) and transfer assessments (getting from A to B)<br />
Cognitive assessments (assessing the functions of the brain)<br />
Wheelchair and seating assessments<br />
Assessment for and provision of equipment<br />
Assessment for minor house adaptation – rails, raising<br />
chairs/beds etc<br />
Home assessments<br />
Education and advice to family and carers about things<br />
like hoisting patients who are no longer able to transfer<br />
independently or safely.<br />
What is the best part of your job?<br />
It’s difficult to pick just one thing as there are so many aspects<br />
of the job that I enjoy! The most rewarding part of the job<br />
is contributing to an individual’s progress or achievement. It<br />
takes time but your time, patience and effort as a therapist<br />
allows many patients to achieve their goal(s). These goals might<br />
be things like walking again, being able to prepare a meal<br />
independently, or returning home safely. I also enjoy spending<br />
time with the patient to find out what difficulties they are<br />
experiencing, discuss any concerns, and try to understand how<br />
this impacts on their life. I do a lot of problem-solving, which<br />
keeps me on my feet!<br />
What is the most challenging part of your job?<br />
The most challenging part of the job is often the pace and<br />
constant demand for hospital beds which can become quite<br />
tiring! I think it’s important to have a healthy work/life balance<br />
and remember why you initially became an OT.<br />
What are your plans for the future?<br />
I want to develop my knowledge on a specific interest area of<br />
multiple sclerosis. I also hope to become accredited as a practice<br />
educator for students. Long-term, I want to take a more senior<br />
role within OT, which would involve greater responsibilities<br />
within the team, taking on a more managerial and operational<br />
role whilst continuing with a clinical caseload. OT is becoming<br />
more and more recognised and I would encourage people to<br />
consider it as a career path that can present many opportunities<br />
and be very rewarding.<br />
Occupational Therapist<br />
What is a typical day like?<br />
There is no typical day in acute medicine! I enjoy the<br />
challenge of prioritising my day, which can often change<br />
quite rapidly, so you have to remain quite flexible. Jobs<br />
on my daily schedule might include:<br />
Patient contact – completing assessments, carrying<br />
out treatment interventions, monitoring progress,<br />
providing training, information and advice and<br />
facilitating a safe discharge from hospital.
10<br />
Haematology<br />
Nurse Practitioner -<br />
Loraine Lloyd<br />
What’s your job description?<br />
My remit is to improve outcomes for haematology patients in line<br />
with the recently published NICE guidance ‘Improving outcomes<br />
in Haematological Cancers.’ [2003]. One of the key features of<br />
my role is to simply ‘be there’ to provide information, advice and<br />
support for all patients with a haematological condition, from their<br />
initial visit to see the haematologist and then throughout their<br />
cancer treatment.<br />
So how do you achieve this?<br />
All patients, and their relatives or carers, are encouraged to phone<br />
or call in and see me if they have any worries or concerns related<br />
to their disease or treatment. As a nurse practitioner much of my<br />
working day is spent undertaking clinical procedures. I perform<br />
most of the bone marrow procedures, venesections and specialist<br />
PICC [peripherally inserted central venous catheter] line insertions.<br />
I also provide support, leadership and education to other healthcare<br />
professionals, including our community-based nurses. Behind the<br />
scenes, I help facilitate change, develop new services and set<br />
evidence-based standards, policies and protocols with colleagues.<br />
As a senior nurse within the Haematology team I can help to focus<br />
clinical decision-making on the needs, values and priorities of<br />
individual patients, giving them a voice where it counts.<br />
How has your role improved the service?<br />
Setting up nurse-led clinics to handle most of the procedures means<br />
that patients can now choose a date and time convenient for them<br />
to come in. The new PICC line insertion service has dramatically<br />
improved the patient’s experience and outcome. Patients no longer<br />
have to go to theatre or radiology but can stay on the ward for<br />
this much less invasive procedure. Removal of the line is relatively<br />
quick and painless, and the lines are associated with a far lower<br />
complication rate, reduced chance of infection and lower expense.<br />
What do you most enjoy about your role?<br />
I am passionate about nursing research and audit as a means of<br />
improving the patient’s experience. In July <strong>2007</strong> I won Basingstoke<br />
and North <strong>Hampshire</strong> <strong>NHS</strong> <strong>Foundation</strong> <strong>Trust</strong> ‘Researcher of the year’<br />
prize for research into the pain experienced by patients during their<br />
bone marrow procedure. My study looked at how we could help to<br />
reduce the pain experienced by our patients when they were having<br />
this diagnostic test performed. As a result of the study patients<br />
are now offered an innovative way to help relieve the pain they<br />
experience during this procedure.<br />
Instant x-rays save time and money<br />
Since purchasing PACS – our Picture Archive Computer<br />
System, for digital x-rays – and all the work it involved<br />
to set up, our investment has been more than<br />
repaid. Today doctors can view x-rays before their<br />
patient has walked back from the department.<br />
Every single x-ray image is stored safely and is<br />
easy to access (no more film archives). The new<br />
system has saved all the expenses of processing,<br />
printing and transporting x-ray images. Even<br />
more importantly, it has supported us to<br />
reduce waiting lists. We don’t know how<br />
we ever managed without it!
11<br />
Increasing the chemotherapy capacity<br />
More beds, better treatment options, and more hours of care: after a thorough<br />
assessment of the Basing Unit, we’ve made some changes to improve the patient<br />
experience. With improved chemotherapy drugs, more patients are being offered<br />
chemotherapy as a treatment option. As a result we had to assess the capacity in<br />
the Unit, making sure that patients get enough time with nursing staff and – equally<br />
important – that staff aren’t overworked. We’ve also reviewed the booking and<br />
administrative processes to make them more efficient, as well as increasing bed<br />
capacity and keeping a bed free every day for unplanned inpatients. This is just one<br />
example of where we have reviewed our processes to give patients a quicker, more<br />
efficient route from diagnosis to discharge.<br />
Questions, comments, or complaints?<br />
PALS is the patient advice and liaison service. It’s<br />
available to:<br />
Help resolve concerns<br />
Provide information<br />
You can contact PALS:<br />
At Basingstoke and North <strong>Hampshire</strong> Hospital<br />
Tel: 01256 486766 / Email: pals@bnhft.nhs.uk<br />
FIRVALE, our respite unit for children with special needs, is a<br />
warm and friendly place where parents and children interact,<br />
get out and about and generally have a great time!<br />
Children with special needs require long-term, permanent<br />
care solutions, and Firvale is the perfect way for children to<br />
receive special attention and learn social skills at the same<br />
time. Staff members from the unit liaise with families,<br />
school and healthcare professionals to ensure the best<br />
care and continuity at all times.<br />
Gaining confidence and independence is an<br />
important part of Firvale, so the older children<br />
often go on organised trips to the cinema,<br />
bowling, seaside and the Watercress Line - always<br />
lots of fun. During the summer holidays we<br />
organised trips to Longleat, Chessington and<br />
Paultons Park.<br />
For younger children, Firvale hosts ‘Treetots’ – a<br />
mother and toddler group for ages 0-5. This weekly<br />
group allows families to meet and discuss issues<br />
around their special needs.<br />
Firvale - our respite unit for children
12<br />
Our Infection Control team is stepping up work<br />
on its ‘Clean your Hands’ campaign. The team<br />
has already met government targets to reduce<br />
hospital infections, and is now planning the<br />
next stages of its campaign.<br />
The <strong>Trust</strong> has worked hard over the last<br />
year to reduce the rate of MRSA infections.<br />
Government targets required the <strong>Trust</strong> to<br />
report less than 12 bacteraemias by March<br />
2008. From April 06 to March 07 the <strong>Trust</strong><br />
only had 6 MRSA bacteraemias. This great<br />
result is largely due to the hard work of<br />
all our staff to reduce infections – but we<br />
cannot become complacent and must work<br />
hard to stay on target.<br />
Better hand-washing<br />
This year, the Infection Control team is overseeing<br />
a more hard-hitting campaign. Their aim is for every<br />
single person who enters the hospital to understand the<br />
importance of hand-washing to patient safety. All staff, patients<br />
and visitors are asked to decontaminate their hands on entry and<br />
before entering any clinical area. We’ve introduced the latest alcohol gel<br />
(Spirigel), which is designed to safely disinfect skin. It’s available at all hospital<br />
and ward entrances and beside all bed spaces.<br />
Communicating<br />
with your <strong>Trust</strong><br />
New targets<br />
Another government target (April <strong>2007</strong>) has been set for Clostridium difficile<br />
infections – no more than 10 infections per month. To achieve this, clinical staff<br />
members must ensure that they isolate any patient with unexplained diarrhoea<br />
until a diagnosis can be found or the patient has no further symptoms for<br />
48 hours. Staff must also ensure that the correct antibiotics are prescribed to<br />
try to reduce occurrence of this infection.<br />
Are you a member yet?<br />
As a <strong>Foundation</strong> <strong>Trust</strong> we are answerable to the<br />
local community. If you have a voice, we want to<br />
hear it – and membership is one of the best ways<br />
to become involved in shaping your health service.<br />
Membership is completely free and you can do as<br />
much or as little as you want to participate.<br />
We currently have around 4,500 members – but<br />
we’re looking for more! As a member you’ll receive<br />
free newsletters and invitations to members’ events.<br />
For an application form:<br />
Telephone 01256 313601<br />
print the form from<br />
www.northhampshire.nhs.uk<br />
Contacting Governors<br />
Our Council of Governors is 27 strong. 14 are elected from constituencies in<br />
and around Basingstoke, North and East <strong>Hampshire</strong> and West Berkshire and the<br />
rest represent our business partners – local authorities, the business community<br />
and the voluntary sector. The Council of Governors has three main areas of<br />
responsibility:<br />
Advising the <strong>Trust</strong> to make sure its business decisions match the needs of<br />
members and the wider community.<br />
Guardianship of the <strong>Trust</strong>, ensuring it operates in a way that fits with its<br />
statement of purpose.<br />
Strategic direction for the <strong>Trust</strong>’s planning so that the Board of Directors can<br />
effectively determine its policies.<br />
If you want to find out about the next public meeting or see who your local<br />
Governor is, just visit our website at www.northhampshire.nhs.uk. To contact<br />
your Governor, e-mail <strong>Foundation</strong>@bnhft.nhs.uk or telephone 01256 313601.