AUC Acknowledgements TAG Meeting Materials 07-29-10
AUC Acknowledgements TAG Meeting Materials 07-29-10
AUC Acknowledgements TAG Meeting Materials 07-29-10
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
<strong>Meeting</strong> <strong>Materials</strong><br />
<strong>Acknowledgements</strong> <strong>TAG</strong> <strong>Meeting</strong><br />
July <strong>29</strong>, 20<strong>10</strong><br />
1. Acknowledgments <strong>TAG</strong> <strong>07</strong>-<strong>29</strong>-<strong>10</strong> agenda<br />
2. Acknowledgement_<strong>TAG</strong>_Minutes<strong>07</strong>15<strong>10</strong><br />
3. Clarification Email Response From Code Committee<br />
4. Claim Category and Status Codes with homework changes 7-27-<strong>10</strong><br />
Page 1 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
<strong>AUC</strong> – Acknowledgments <strong>TAG</strong> Agenda<br />
July <strong>29</strong>, 20<strong>10</strong> (9:00-11:00 am, CDT)<br />
Minnesota Room at SOP<br />
Conference call number is: New call-in line: 213-289-0500 participant code: 337213<br />
WebEx Instructions--<br />
1. Click on this link: https://health-state-mnustraining.webex.com/mw0306l/mywebex/default.do?siteurl=health-state-mn-ustraining&service=7<br />
2. Click on the link to the <strong>AUC</strong> Acknowledgments <strong>TAG</strong> meeting.<br />
3. Type your name, email address and password into the prompt boxes. The password is: Ack20<strong>10</strong>!<br />
1. Minute Taker for Today –<br />
2. <strong>AUC</strong> Antitrust Statement<br />
3. Welcome and Introductions<br />
a. Take attendance for <strong>AUC</strong> member organizations<br />
4. ACTION ITEMS:<br />
a. Approve Minutes from July 15 meeting<br />
5. DISCUSSION ITEMS:<br />
a. Clarification on Claim Status Codes – see email<br />
b. Review HIR<br />
QUESTION:<br />
According to the note, the assigned value of zero or the sender assigned value would not<br />
be of value to the receiver of the 277CA if the original claim had multiple loops with the<br />
same billing provider. How does a zero or an assigned value inform the receiver of the<br />
277CA of where the error is?<br />
ANSWER:<br />
This issue is explicitly addressed in guide 0050<strong>10</strong>X214. The note on the 2200C loop TRN<br />
segment states "Because the TRN segment is syntactically required in order to use Loop<br />
2200C, TRN02 can either be a sender assigned value or a default value of zero (0)."<br />
The loop 2200C value in TRN02 is not intended to be of any help in identifying where an<br />
error is located. It is required syntactically in order to use other parts of the 2200C loop.<br />
Identification of the specific error, if there is an error, would be in the other parts of the<br />
2200C loop, like the STC segment, and would apply to all claims from that provider of<br />
service.<br />
i.<br />
c. Continue review of 277CA Status Code Usage<br />
Page 1 of 1<br />
Page 2 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
6. Other Business –<br />
a. Future meeting – Flows Best Practice<br />
7. Next <strong>Meeting</strong> Information:<br />
August 19, 9:00-11:00 am, Minnesota Dept of Health, Snelling Office Park, Minnesota<br />
Room<br />
Page 2 of 1<br />
Page 3 of 63
<strong>AUC</strong> Acknowledgement <strong>TAG</strong> Workgroup<br />
July 15, 20<strong>10</strong> 9:00 AM – 11:00 AM<br />
WEB EX and PHONE<br />
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
Minutes By: Patrice Kuppe<br />
DRAFT<br />
Agenda Item Discussion Action<br />
<strong>AUC</strong> Antitrust Reminded group we follow anit-trust. None<br />
Welcome and<br />
Introductions<br />
(attendance)<br />
Approve Minutes<br />
from June 15,<br />
20<strong>10</strong> <strong>Meeting</strong><br />
Review and<br />
approve 997<br />
statement for<br />
Approved the Approve Minutes from June 15 and July 8 meetings<br />
Approved 997 statement that <strong>AUC</strong> should recommend that MDH to not create guide based on X12<br />
interpretations and that Medicare does not use it.<br />
None<br />
Dave post to web.<br />
Patrice to send<br />
recommendation to<br />
Dave to get on <strong>AUC</strong><br />
Ops agenda.<br />
Continue review<br />
of 277CA Status<br />
Code Usage (see<br />
template)<br />
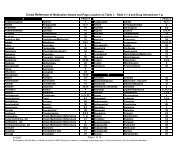
See spreadsheet<br />
We completed through status code 267.<br />
The group decided to share the burden and each of the following people took a set of codes. Each will research<br />
whether that data is reported in a claim (P, I, or D) and if so, recommend what category code(s) would be<br />
appropriate. The results will be sent to Patrice by 7/23 so she can incorporate into one spreadsheet for the group<br />
to review on 7/<strong>29</strong>.<br />
Person<br />
Numbers<br />
Chip Evelsizer 600 series<br />
Allan Klug 301 - 350<br />
Patrice Kuppe 268 - 300<br />
Faye Ostroot 700 -742<br />
Lisa Wichterman. 401- 450<br />
Steve Williams 451 - 500<br />
Brian Roy 501- 550<br />
Sherri Wilson 551-599<br />
Ed Stroot 351- 400<br />
<strong>TAG</strong> volunteers to<br />
complete assigned<br />
review and send to<br />
Patrice by 7/23.<br />
Page 4 of 63
Agenda Item Discussion Action<br />
Future meeting – Future meeting.<br />
Flows Best<br />
Practice<br />
Next <strong>Meeting</strong> July <strong>29</strong>, 20<strong>10</strong><br />
9:00 AM-12:00 AM<br />
MDH – Snelling Office Park, Minnesota Room<br />
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
Page 5 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
From: Cabral, Michael J. (CMS/OIS) [michael.cabral@cms.hhs.gov]<br />
Sent: Wednesday, July 14, 20<strong>10</strong> 6:21 AM<br />
To: Kuppe, Patrice M<br />
Cc: Stine, Merri-Lee; Debra Strickland<br />
Subject: Clarification on Claim Status Codes<br />
Patrice,<br />
Per our conversation of last week the two codes in question can fit into separate scenarios but<br />
the logic can be applied simply as follows:<br />
Claim Status Code:<br />
24 Entity not approved as an electronic submitter.<br />
Note: Changed as of 6/01<br />
One of the situations where this can be used is when a trading partner is attempting to send a<br />
transaction to another trading partner. e.g. Clearinghouse sending claims transactions to a<br />
payer. If the clearinghouse is approved to send a single form of the claim transaction (e.g.<br />
approved for institutional claims in production but not for professional claim submission in<br />
production). Using code 24 when the Professional claim transaction is submitted would indicate<br />
that the transaction is being rejected because the entity (trading Partner) is not approved as an<br />
electronic submitter.<br />
In the second scenario discussed a clearinghouse may be servicing several providers. Provider 1<br />
is approved and registered with the payer as is Provider 3. Provider 2 is not approved to bill the<br />
payer and the use of this code would require using the data element 98 in the composite data<br />
element of the STC segment in the 277, which would indicate that the Billing Provider is not<br />
approved. By indicating that all claims under Provider 2 are being rejected, the payer can<br />
accept and process claims for Provider 1 and Provider 3 per the payer’s adjudication processes<br />
without having to reject an entire transaction.<br />
25 Entity not approved. This change effective 11/1/20<strong>10</strong>: Entity not approved.<br />
Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Hope this helps to clarify our discussion.<br />
Michael J. Cabral<br />
Chair - Code Maintenance Committee<br />
Phone: (4<strong>10</strong>) 786-6168<br />
Email: michael.cabral@cms.hhs.gov<br />
From: wedi-acknowledgements-lists@lists.wedi.org [mailto:wedi-acknowledgementslists@lists.wedi.org]<br />
On Behalf Of Kuppe, Patrice M<br />
Sent: Tuesday, July 06, 20<strong>10</strong> <strong>10</strong>:49 AM<br />
To: WEDI-acknowledgements@lists.wedi.org<br />
Subject: Question for Claim ACK and Status Codes<br />
Page 6 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
Does anyone know if there is a way to get clarification from code committee?<br />
The MN <strong>AUC</strong> is hoping to get clarification on this:<br />
We want to understand how the codes below are expected to be used in a 999 or<br />
277CA?<br />
How would the electronic transaction ever get to someone if not approved?<br />
Also, what is the difference between electronic submitter approval versus entity not<br />
approved? Not approved for what? Thanks!<br />
Entity not approved as an electronic submitter. This change<br />
effective 11/1/20<strong>10</strong>: Entity not approved as an electronic submitter.<br />
Note: This code requires use of an Entity<br />
Code.<br />
Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity not approved. This change effective 11/1/20<strong>10</strong>: Entity not<br />
approved. Note: This code requires use of an Entity<br />
Code.<br />
Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Page 7 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
Claim Category Codes 05/<strong>10</strong>/20<strong>10</strong> - Check wpc-edi.com for current list<br />
Acknowledgement<br />
Pending<br />
Finalized<br />
Requests<br />
General Questions<br />
Response not possible<br />
Data Search Unsuccessful (Not for CA?)<br />
Correction required (Not for CA?)<br />
YES OR NO<br />
COMMENTS<br />
A0<br />
Acknowledgement/Forwarded-The claim/encounter has been forwarded to<br />
another entity. Start: 01/01/1995<br />
Y<br />
A1<br />
Acknowledgement/Receipt-The claim/encounter has been received. This does<br />
not mean that the claim has been accepted for adjudication.<br />
Start: 01/01/1995<br />
Y<br />
Allow for non-HIPAA covered entities<br />
A2<br />
Acknowledgement/Acceptance into adjudication system-The claim/encounter<br />
has been accepted into the adjudication system. Start: 01/01/1995<br />
Y<br />
A3<br />
Acknowledgement/Returned as unprocessable claim-The claim/encounter has<br />
been rejected and has not been entered into the adjudication system.<br />
Start: 01/01/1995<br />
Y<br />
Require Claim Status code<br />
A4<br />
Acknowledgement/Not Found-The claim/encounter can not be found in the<br />
adjudication system. Start: 01/01/1995<br />
N<br />
A5<br />
Acknowledgement/Split Claim-The claim/encounter has been split upon<br />
acceptance into the adjudication system. Start: 02/28/2002<br />
Y<br />
A6<br />
Acknowledgement/Rejected for Missing Information - The claim/encounter is<br />
missing the information specified in the Status details and has been rejected.<br />
Start: <strong>10</strong>/31/2002<br />
Y<br />
A7<br />
Acknowledgement/Rejected for Invalid Information - The claim/encounter has<br />
invalid information as specified in the Status details and has been rejected.<br />
Start: <strong>10</strong>/31/2002<br />
Y<br />
Page 8 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
A8<br />
P0<br />
P1<br />
P2<br />
Acknowledgement / Rejected for relational field in error. Start:<br />
<strong>10</strong>/31/2004<br />
Pending: Adjudication/Details-This is a generic message about a pended claim.<br />
A pended claim is one for which no remittance advice has been issued, or only<br />
part of the claim has been paid. Start: 01/01/1995<br />
Pending/In Process-The claim or encounter is in the adjudication system.<br />
Start: 01/01/1995<br />
Pending/Payer Review-The claim/encounter is suspended and is pending<br />
review (e.g. medical review, repricing, Third Party Administrator processing).<br />
Start: 01/01/1995 | Last Modified: 01/27/2008<br />
Y Example?<br />
N<br />
N<br />
N<br />
P3<br />
Pending/Provider Requested Information - The claim or encounter is waiting for<br />
information that has already been requested from the provider. (Note: A Claim<br />
Status Code identifying the type of information requested, must be reported)<br />
Start: 01/01/1995 | Last Modified: 01/27/2008<br />
N<br />
P4<br />
Pending/Patient Requested Information - The claim or encounter is waiting for<br />
information that has already been requested from the patient. (Note: A status<br />
code identifying the type of information requested must be sent)<br />
Start: 01/01/1995 | Last Modified: 01/27/2008<br />
N<br />
P5 Pending/Payer Administrative/System hold Start: <strong>10</strong>/31/2006 N<br />
F0<br />
Finalized-The claim/encounter has completed the adjudication cycle and no<br />
more action will be taken. Start: 01/01/1995<br />
F1 Finalized/Payment-The claim/line has been paid. Start: 01/01/1995 N<br />
F2 Finalized/Denial-The claim/line has been denied. Start: 01/01/1995 N<br />
N<br />
F3<br />
F3F<br />
Finalized/Revised - Adjudication information has been changed Start:<br />
02/28/2001<br />
Finalized/Forwarded-The claim/encounter processing has been completed. Any<br />
applicable payment has been made and the claim/encounter has been<br />
forwarded to a subsequent entity as identified on the original claim or in this<br />
payer's records. Start: 01/01/1995<br />
N<br />
N<br />
Page 9 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
F3N<br />
Finalized/Not Forwarded-The claim/encounter processing has been completed.<br />
Any applicable payment has been made. The claim/encounter has NOT been<br />
forwarded to any subsequent entity identified on the original claim.<br />
Start: 01/01/1995<br />
N<br />
F4<br />
R0<br />
R1<br />
R3<br />
R4<br />
Finalized/Adjudication Complete - No payment forthcoming-The<br />
claim/encounter has been adjudicated and no further payment is forthcoming.<br />
Start: 01/01/1995<br />
Requests for additional Information/General Requests-Requests that don't fall<br />
into other R-type categories. Start: 01/01/1995<br />
Requests for additional Information/Entity Requests-Requests for information<br />
about specific entities (subscribers, patients, various providers).<br />
Start: 01/01/1995<br />
Requests for additional Information/Claim/Line-Requests for information that<br />
could normally be submitted on a claim. Start: 01/01/1995 | Last<br />
Modified: 02/28/1998<br />
Requests for additional Information/Documentation-Requests for additional<br />
supporting documentation. Examples: certification, x-ray, notes.<br />
Start: 01/01/1995 | Last Modified: 02/28/1998<br />
N<br />
N<br />
N<br />
N<br />
N<br />
R5<br />
R6<br />
R7<br />
R8<br />
R9<br />
Request for additional information/more specific detail-Additional information<br />
as a follow up to a previous request is needed. The original information was<br />
received but is inadequate. More specific/detailed information is requested.<br />
Start: 01/01/1995 | Last Modified: 06/30/1998<br />
Requests for additional information - Regulatory requirements Start:<br />
02/28/20<strong>07</strong><br />
Requests for additional information - Confirm care is consistent with Health<br />
Plan policy coverage. Start: 02/28/20<strong>07</strong><br />
Requests for additional information - Confirm care is consistent with health<br />
plan coverage exceptions Start: 02/28/20<strong>07</strong><br />
Requests for additional information - Determination of medical necessity.<br />
Start: 02/28/20<strong>07</strong><br />
N<br />
N<br />
N<br />
N<br />
N<br />
Page <strong>10</strong> of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
R<strong>10</strong><br />
R11<br />
R12<br />
R13<br />
R14<br />
R15<br />
Requests for additional information - Support a filed grievance or appeal.<br />
Start: 02/28/20<strong>07</strong><br />
Requests for additional information - Pre-payment review of claims. Start:<br />
02/28/20<strong>07</strong><br />
Requests for additional information - Clarification or justification of use for<br />
specified procedure code Start: 02/28/20<strong>07</strong><br />
Requests for additional information - Original documents submitted are not<br />
readable. Used only for subsequent request(s). Start:<br />
02/28/20<strong>07</strong><br />
Requests for additional information - Original documents received are not what<br />
was requested. Used only for subsequent request(s). Start:<br />
02/28/20<strong>07</strong><br />
Requests for additional information - Workers Compensation coverage<br />
determination. Start: 02/28/20<strong>07</strong><br />
N<br />
N<br />
N<br />
N<br />
N<br />
N<br />
R16<br />
RQ<br />
E0<br />
Requests for additional information - Eligibility determination Start:<br />
02/28/20<strong>07</strong><br />
General Questions (Yes/No Responses)-Questions that may be answered by a<br />
simple 'yes' or 'no'. Start: 01/01/1995 | Last<br />
Modified: <strong>07</strong>/09/20<strong>07</strong> | Stop: 01/01/2008<br />
Response not possible - error on submitted request data. Start:<br />
01/01/1995 | Last Modified: 02/28/2002<br />
E1 Response not possible - System Status Start: 02/<strong>29</strong>/2000 N<br />
N<br />
N<br />
N should have denied on 999<br />
E2<br />
DO<br />
E3<br />
Information Holder is not responding; resubmit at a later time. Start:<br />
06/30/2003<br />
Data Search Unsuccessful - The payer is unable to return status on the<br />
requested claim(s) based on the submitted search criteria. Start:<br />
01/01/1995 | Last Modified: 09/20/2009<br />
Correction required - relational fields in error. Start:<br />
01/24/20<strong>10</strong><br />
N<br />
N<br />
N<br />
use A8 for acknowledgment<br />
Page 11 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
Health Care Claim Status Codes 5/<strong>10</strong>/20<strong>10</strong> (see WPC-EDI.com for current list)<br />
Health Care Claim Status Codes convey the status of an entire claim or a specific service line<br />
(A) Acknowledgement<br />
(P) Pending<br />
(F) Finalized<br />
(R)Requests<br />
(G) General Questions<br />
(NP) Response not possible<br />
4 levels needed? (Patrice has notes)<br />
Add defn of A0. etc.<br />
Additional notes<br />
Claim<br />
Status<br />
Code<br />
Claim Status Code Description<br />
Claim Cateory<br />
Codes: A0, A1,<br />
A2, A3, A5, A6,<br />
A7, A8 or NA<br />
COMMENTS<br />
Entity Codes<br />
0 Cannot provide further status electronically. Start: 01/01/1995 NA<br />
1<br />
For more detailed information, see remittance advice.<br />
Start: 01/01/1995<br />
NA<br />
2 More detailed information in letter. Start: 01/01/1995 NA<br />
3<br />
Claim has been adjudicated and is awaiting payment cycle.<br />
Start: 01/01/1995<br />
NA<br />
6 Balance due from the subscriber. Start: 01/01/1995 NA<br />
12<br />
One or more originally submitted procedure codes have been combined.<br />
Start: 01/01/1995 | Last Modified: 06/30/2001<br />
NA<br />
shouldn't be using codes for<br />
ajudication<br />
15<br />
One or more originally submitted procedure code have been modified.<br />
Start: 01/01/1995 | Last Modified: 06/30/2001<br />
NA<br />
16<br />
Claim/encounter has been forwarded to entity. This change effective 11/1/20<strong>10</strong>:<br />
Claim/encounter has been forwarded to entity. Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
A0<br />
requires use of<br />
entity code -- add<br />
later<br />
17<br />
Claim/encounter has been forwarded by third party entity to entity. This change<br />
effective 11/1/20<strong>10</strong>: Claim/encounter has been forwarded by third party entity to<br />
entity. Note: This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
A0<br />
requires use of<br />
entity code -- add<br />
later<br />
18<br />
Entity received claim/encounter, but returned invalid status. This change effective<br />
11/1/20<strong>10</strong>: Entity received claim/encounter, but returned invalid status. Note: This<br />
code requires use of an Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
NA<br />
19<br />
Entity acknowledges receipt of claim/encounter. This change effective 11/1/20<strong>10</strong>:<br />
Entity acknowledges receipt of claim/encounter. Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
NA<br />
20<br />
Accepted for processing. Start: 01/01/1995 |<br />
Last Modified: 06/30/2001<br />
A2<br />
21<br />
Missing or invalid information. Note: At least one other status code is required to<br />
identify the missing or invalid information. Start:<br />
01/01/1995 | Last Modified: <strong>07</strong>/09/20<strong>07</strong><br />
???<br />
how does this add value if we have<br />
to add another reason?<br />
Page 12 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
23<br />
24<br />
25<br />
26<br />
Returned to Entity. This change effective 11/1/20<strong>10</strong>: Returned to Entity. Note: This<br />
code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Entity not approved as an electronic submitter. This change effective 11/1/20<strong>10</strong>:<br />
Entity not approved as an electronic submitter. Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity not approved. This change effective 11/1/20<strong>10</strong>: Entity not approved. Note:<br />
This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Entity not found. This change effective 11/1/20<strong>10</strong>: Entity not found. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
27 Policy canceled. Start: 01/01/1995 | Last Modified: 06/30/2001 A3<br />
<strong>29</strong><br />
Subscriber and policy number/contract number mismatched.<br />
Start: 01/01/1995<br />
30 Subscriber and subscriber id mismatched. Start: 01/01/1995 A3<br />
31 Subscriber and policyholder name mismatched. Start: 01/01/1995 A3<br />
32<br />
Subscriber and policy number/contract number not found.<br />
Start: 01/01/1995<br />
33 Subscriber and subscriber id not found. Start: 01/01/1995 A3<br />
34 Subscriber and policyholder name not found. Start: 01/01/1995 NA<br />
35 Claim/encounter not found. Start: 01/01/1995 NA<br />
37<br />
Predetermination is on file, awaiting completion of services.<br />
Start: 01/01/1995<br />
38 Awaiting next periodic adjudication cycle. Start: 01/01/1995 NA<br />
39 Charges for pregnancy deferred until delivery. Start: 01/01/1995 NA<br />
A3<br />
???<br />
???<br />
???<br />
??<br />
NA<br />
NA<br />
Patrice to follow up with claims<br />
status code committee -- 7-8-<strong>10</strong><br />
PK rec'd verbal response -- written<br />
response soon. Diff between #24<br />
and #25? 25 is for entity not<br />
enrolled. Patrice to email response<br />
to <strong>TAG</strong><br />
Patrice to follow up with claims<br />
status code committee<br />
what entities would this apply to?<br />
Includes use by non-HIPAA<br />
covered entities Also for level<br />
discussion--<br />
If policy/contract not required on<br />
claim, would this be used?<br />
Patrice to follow up with claims<br />
status code committee re category<br />
code A8<br />
If policy/contract not required on<br />
claim, would this be used?<br />
requires use of<br />
entity code -- add<br />
later<br />
requires use of<br />
entity code -- add<br />
later<br />
HK<br />
40 Waiting for final approval. Start: 01/01/1995 NA<br />
41 Special handling required at payer site. Start: 01/01/1995 NA<br />
42 Awaiting related charges. Start: 01/01/1995 NA<br />
44 Charges pending provider audit. Start: 01/01/1995 NA<br />
45 Awaiting benefit determination. Start: 01/01/1995 NA<br />
46 Internal review/audit. Start: 01/01/1995 NA<br />
47 Internal review/audit - partial payment made. Start: 01/01/1995 NA<br />
Perhaps used by non-HIPAA<br />
covered entities<br />
48<br />
Referral/authorization. Start: 01/01/1995 |<br />
Last Modified: 02/28/2001<br />
A6, A7, A8<br />
Page 13 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
49 Pending provider accreditation review. Start: 01/01/1995 NA Not for pending<br />
50 Claim waiting for internal provider verification. Start: 01/01/1995 NA Not for pending<br />
51 Investigating occupational illness/accident. Start: 01/01/1995 A1<br />
52<br />
53<br />
Investigating existence of other insurance coverage. Start:<br />
01/01/1995<br />
Claim being researched for Insured ID/Group Policy Number error. Start:<br />
01/01/1995<br />
NA<br />
NA<br />
Providers should research 51 --<br />
does it help to know that non-<br />
HIPAA covered payer took in and<br />
is pended until investigation<br />
completed<br />
54 Duplicate of a previously processed claim/line. Start: 01/01/1995 A3<br />
55 Claim assigned to an approver/analyst. Start: 01/01/1995 NA<br />
56 Awaiting eligibility determination. Start: 01/01/1995 NA<br />
57 Pending COBRA information requested. Start: 01/01/1995 NA<br />
59 Non-electronic request for information. Start: 01/01/1995 NA<br />
60 Electronic request for information. Start: 01/01/1995 NA<br />
61 Eligibility for extended benefits. Start: 01/01/1995 NA<br />
64 Re-pricing information. Start: 01/01/1995 NA<br />
65 Claim/line has been paid. Start: 01/01/1995 NA<br />
66<br />
Payment reflects usual and customary charges. Start:<br />
01/01/1995<br />
NA<br />
72 Claim contains split payment. Start: 01/01/1995 NA<br />
73<br />
Payment made to entity, assignment of benefits not on file. This change effective<br />
11/1/20<strong>10</strong>: Payment made to entity, assignment of benefits not on file. Note: This<br />
code requires use of an Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
NA<br />
78 Duplicate of an existing claim/line, awaiting processing. Start: 01/01/1995 A3<br />
81<br />
Contract/plan does not cover pre-existing conditions. Start:<br />
01/01/1995<br />
NA<br />
83 No coverage for newborns. Start: 01/01/1995 NA<br />
84 Service not authorized. Start: 01/01/1995 NA<br />
85<br />
Entity not primary. This change effective 11/1/20<strong>10</strong>: Entity not primary. Note: This<br />
code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
A0<br />
86<br />
Diagnosis and patient gender mismatch. Start: 01/01/1995<br />
| Last Modified: 02/28/2000<br />
A3<br />
88<br />
Entity not eligible for benefits for submitted dates of service. This change effective<br />
11/1/20<strong>10</strong>: Entity not eligible for benefits for submitted dates of service. Note: This<br />
code requires use of an Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
A3<br />
82, 85<br />
Page 14 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
89<br />
Entity not eligible for dental benefits for submitted dates of service. This change<br />
effective 11/1/20<strong>10</strong>: Entity not eligible for dental benefits for submitted dates of<br />
service. Note: This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
A3<br />
90<br />
Entity not eligible for medical benefits for submitted dates of service. This change<br />
effective 11/1/20<strong>10</strong>: Entity not eligible for medical benefits for submitted dates of<br />
service. Note: This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
A3<br />
91<br />
Entity not eligible/not approved for dates of service. This change effective<br />
11/1/20<strong>10</strong>: Entity not eligible/not approved for dates of service. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
A3<br />
92<br />
Entity does not meet dependent or student qualification. This change effective<br />
11/1/20<strong>10</strong>: Entity does not meet dependent or student qualification. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
A3<br />
93<br />
Entity is not selected primary care provider. This change effective 11/1/20<strong>10</strong>: Entity<br />
is not selected primary care provider. Note: This code requires use of an Entity<br />
Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
A3<br />
94<br />
Entity not referred by selected primary care provider. This change effective<br />
11/1/20<strong>10</strong>: Entity not referred by selected primary care provider. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
A3<br />
95<br />
Requested additional information not received. Start: 01/01/1995<br />
| Last Modified: <strong>07</strong>/09/20<strong>07</strong><br />
Notes: If known, the payer must report a second claim status code identifying the<br />
requested information.<br />
NA<br />
if asking for addl info, claim must<br />
have already been taken in<br />
96<br />
No agreement with entity. This change effective 11/1/20<strong>10</strong>: No agreement with<br />
entity. Note: This code requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
A3<br />
97<br />
Patient eligibility not found with entity. This change effective 11/1/20<strong>10</strong>: Patient<br />
eligibility not found with entity. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
A3<br />
Examples of entity codes? One<br />
example -- medical home (health<br />
care home)<br />
98 Charges applied to deductible. Start: 01/01/1995 NA<br />
99 Pre-treatment review. Start: 01/01/1995 NA<br />
<strong>10</strong>0 Pre-certification penalty taken. Start: 01/01/1995 NA<br />
<strong>10</strong>1<br />
<strong>10</strong>2<br />
Claim was processed as adjustment to previous claim. Start:<br />
01/01/1995<br />
Newborn's charges processed on mother's claim. Start:<br />
01/01/1995<br />
NA<br />
NA<br />
<strong>10</strong>3 Claim combined with other claim(s). Start: 01/01/1995 NA<br />
<strong>10</strong>4<br />
Processed according to plan provisions (Plan refers to provisions that exist<br />
between the Health Plan and the Consumer or Patient) Start:<br />
01/01/1995 | Last Modified: 06/01/2008<br />
NA<br />
<strong>10</strong>5 Claim/line is capitated. Start: 01/01/1995 NA<br />
Page 15 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
<strong>10</strong>6<br />
1<strong>07</strong><br />
<strong>10</strong>9<br />
This amount is not entity's responsibility. This change effective 11/1/20<strong>10</strong>: This<br />
amount is not entity's responsibility. Note: This code requires use of an Entity<br />
Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Processed according to contract provisions (Contract refers to provisions that<br />
exist between the Health Plan and a Provider of Health Care Services)<br />
Start: 01/01/1995 | Last Modified: 06/01/2008<br />
Entity not eligible. This change effective 11/1/20<strong>10</strong>: Entity not eligible. Note: This<br />
code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
NA<br />
NA<br />
A3<br />
1<strong>10</strong> Claim requires pricing information. Start: 01/01/1995 A6<br />
111<br />
At the policyholder's request these claims cannot be submitted electronically.<br />
Start: 01/01/1995<br />
NA<br />
114<br />
Claim/service should be processed by entity. This change effective 11/1/20<strong>10</strong>:<br />
Claim/service should be processed by entity. Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
NA<br />
Use number 16 above<br />
116 Claim submitted to incorrect payer. Start: 01/01/1995 A3<br />
117 Claim requires signature-on-file indicator. Start: 01/01/1995 A3<br />
121<br />
123<br />
124<br />
125<br />
126<br />
127<br />
128<br />
1<strong>29</strong><br />
130<br />
131<br />
Service line number greater than maximum allowable for payer.<br />
Start: 01/01/1995<br />
Additional information requested from entity. This change effective 11/1/20<strong>10</strong>:<br />
Additional information requested from entity. Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity's name, address, phone and id number. This change effective 11/1/20<strong>10</strong>:<br />
Entity's name, address, phone and id number. Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity's name. This change effective 11/1/20<strong>10</strong>: Entity's name. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's address. This change effective 11/1/20<strong>10</strong>: Entity's address. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's phone number. This change to be effective 7/1/20<strong>10</strong>: Entity's<br />
Communication Number. This change effective 11/1/20<strong>10</strong>: Entity's Communication<br />
Number. Note: This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Entity's tax id. This change effective 11/1/20<strong>10</strong>: Entity's tax id. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's Blue Cross provider id. This change effective 11/1/20<strong>10</strong>: Entity's Blue Cross<br />
provider id. Note: This code requires use of an Entity Code. Start: 01/01/1995<br />
| Last Modified: 02/11/20<strong>10</strong><br />
Entity's Blue Shield provider id. This change effective 11/1/20<strong>10</strong>: Entity's Blue<br />
Shield provider id. Note: This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Entity's Medicare provider id. This change effective 11/1/20<strong>10</strong>: Entity's Medicare<br />
provider id. Note: This code requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
NA<br />
A3 or A6<br />
A3 or A6<br />
A3 or A6<br />
A3 or A6<br />
A3 or A6<br />
NA<br />
NA<br />
NA<br />
When using A3 have to use in<br />
combination with another claims<br />
status code<br />
When using A3 have to use in<br />
combination with another claims<br />
status code<br />
When using A3 have to use in<br />
combination with another claims<br />
status code<br />
When using A3 have to use in<br />
combination with another claims<br />
status code<br />
When using A3 have to use in<br />
combination with another claims<br />
status code<br />
Page 16 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
132<br />
133<br />
Entity's Medicaid provider id. This change effective 11/1/20<strong>10</strong>: Entity's Medicaid<br />
provider id. Note: This code requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
Entity's UPIN. This change effective 11/1/20<strong>10</strong>: Entity's UPIN. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
Entity's CHAMPUS provider id. This change effective 11/1/20<strong>10</strong>: Entity's CHAMPUS<br />
provider id. Note: This code requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
A3 or A6<br />
NA<br />
When using A3 have to use in<br />
combination with another claims<br />
status code (should only be used<br />
for atypical providers) 82, 85<br />
134<br />
NA<br />
135<br />
136<br />
Entity's commercial provider id. This change effective 11/1/20<strong>10</strong>: Entity's<br />
commercial provider id. Note: This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Entity's health industry id number. This change effective 11/1/20<strong>10</strong>: Entity's health<br />
industry id number. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Entity's plan network id. This change effective 11/1/20<strong>10</strong>: Entity's plan network id.<br />
Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's site id . This change effective 11/1/20<strong>10</strong>: Entity's site id . Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's health maintenance provider id (HMO). This change effective 11/1/20<strong>10</strong>:<br />
Entity's health maintenance provider id (HMO). Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity's preferred provider organization id (PPO). This change effective 11/1/20<strong>10</strong>:<br />
Entity's preferred provider organization id (PPO). Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity's administrative services organization id (ASO). This change effective<br />
11/1/20<strong>10</strong>: Entity's administrative services organization id (ASO). Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
A3 or A6<br />
NA<br />
When using A3 have to use in<br />
combination with another claims<br />
status code (should only be used<br />
for atypical providers)<br />
82, 85, DQ<br />
137<br />
NA<br />
138<br />
NA<br />
139<br />
NA<br />
140<br />
NA<br />
141<br />
NA<br />
142<br />
Entity's license/certification number. This change effective 11/1/20<strong>10</strong>: Entity's<br />
license/certification number. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
143<br />
Entity's state license number. This change effective 11/1/20<strong>10</strong>: Entity's state license<br />
number. Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's specialty license number. This change effective 11/1/20<strong>10</strong>: Entity's specialty<br />
license number. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
144<br />
NA<br />
145<br />
Entity's specialty/taxonomy code. This change effective 11/1/20<strong>10</strong>: Entity's<br />
specialty/taxonomy code. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
A3 or A6<br />
When using A3 have to use in<br />
combination with another claims<br />
status code Invalid Taxonomy<br />
Code 82, 85<br />
146<br />
Entity's anesthesia license number. This change effective 11/1/20<strong>10</strong>: Entity's<br />
anesthesia license number. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
Page 17 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
147<br />
148<br />
149<br />
150<br />
Entity's qualification degree/designation. (e.g. RN,PhD,MD) This change effective<br />
11/1/20<strong>10</strong>: Entity's qualification degree/designation (e.g. RN,PhD,MD). Note: This<br />
code requires use of an Entity Code. Start: 02/28/1997 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity's social security number. This change effective 11/1/20<strong>10</strong>: Entity's social<br />
security number. Note: This code requires use of an Entity Code. Start:<br />
01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
Entity's employer id. This change effective 11/1/20<strong>10</strong>: Entity's employer id. Note:<br />
This code requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
Entity's drug enforcement agency (DEA) number. This change effective 11/1/20<strong>10</strong>:<br />
Entity's drug enforcement agency (DEA) number. Note: This code requires use of<br />
an Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
NA<br />
NA<br />
NA<br />
NA<br />
152 Pharmacy processor number. Start: 01/01/1995 NA<br />
153<br />
Entity's id number. This change effective 11/1/20<strong>10</strong>: Entity's id number. Note: This<br />
code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
NA<br />
154 Relationship of surgeon & assistant surgeon. Start: 01/01/1995 NA<br />
155<br />
Entity's relationship to patient. This change effective 11/1/20<strong>10</strong>: Entity's relationship<br />
to patient. Note: This code requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
156 Patient relationship to subscriber. Start: 01/01/1995 A6 or A7<br />
Use with entity codes (find element<br />
number for patient relationship in<br />
837) --stopping point on 7-8-<strong>10</strong> --<br />
Patrice to fill in through end of<br />
spreadsheet, to be emailed to<br />
<strong>TAG</strong> for review prior to next<br />
Thursday<br />
157<br />
158<br />
159<br />
160<br />
161<br />
162<br />
163<br />
Entity's Gender. This change effective 11/1/20<strong>10</strong>: Entity's Gender. Note: This code<br />
requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's date of birth. This change effective 11/1/20<strong>10</strong>: Entity's date of birth. Note:<br />
This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's date of death. This change effective 11/1/20<strong>10</strong>: Entity's date of death. Note:<br />
This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's marital status. This change effective 11/1/20<strong>10</strong>: Entity's marital status. Note:<br />
This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's employment status. This change effective 11/1/20<strong>10</strong>: Entity's employment<br />
status. Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's health insurance claim number (HICN). This change effective 11/1/20<strong>10</strong>:<br />
Entity's health insurance claim number (HICN). Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity's policy number. This change effective 11/1/20<strong>10</strong>: Entity's policy number.<br />
Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
A7<br />
A7 or A8<br />
A7<br />
NA<br />
NA<br />
A6 or A7 or A8<br />
A6 or A7 or A8<br />
statement dates must be equal to<br />
or greater than patient's date of<br />
birth.<br />
QC<br />
When CLM Freq Type Cd (CLM05-<br />
3) indicates claim is a replacement<br />
or cancel, then this REF segment<br />
must contain the original payer<br />
claim number. 85<br />
20<strong>10</strong> BB of 837 SBR03 names this<br />
equal to group no.<br />
Page 18 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
164<br />
Entity's contract/member number. This change effective 11/1/20<strong>10</strong>: Entity's<br />
contract/member number. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
A8<br />
check MN companion guide<br />
165<br />
Entity's employer name, address and phone. This change effective 11/1/20<strong>10</strong>:<br />
Entity's employer name, address and phone. Note: This code requires use of an<br />
Entity Code. Start: 01/01/1995 | Last Modified:<br />
02/11/20<strong>10</strong><br />
NA<br />
166<br />
Entity's employer name. This change effective 11/1/20<strong>10</strong>: Entity's employer name.<br />
Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
NA<br />
167<br />
Entity's employer address. This change effective 11/1/20<strong>10</strong>: Entity's employer<br />
address. Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
NA<br />
168<br />
Entity's employer phone number. This change effective 11/1/20<strong>10</strong>: Entity's employer<br />
phone number. Note: This code requires use of an Entity Code.<br />
Start: 01/01/1995 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
170<br />
Entity's employee id. This change effective 11/1/20<strong>10</strong>: Entity's employee id. Note:<br />
This code requires use of an Entity Code. Start: 01/01/1995 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
171<br />
Other insurance coverage information (health, liability, auto, etc.). Start:<br />
01/01/1995<br />
A6 or A7<br />
172 Other employer name, address and telephone number. Start: 01/01/1995 NA<br />
173<br />
174<br />
175<br />
176<br />
177<br />
Entity's name, address, phone, gender, DOB, marital status, employment status and<br />
relation to subscriber. This change effective 11/1/20<strong>10</strong>: Entity's name, address,<br />
phone, gender, DOB, marital status, employment status and relation to subscriber.<br />
Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's student status. This change effective 11/1/20<strong>10</strong>: Entity's student status.<br />
Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's school name. This change effective 11/1/20<strong>10</strong>: Entity's school name. Note:<br />
This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's school address. This change effective 11/1/20<strong>10</strong>: Entity's school address.<br />
Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Transplant recipient's name, date of birth, gender, relationship to insured.<br />
Start: 01/01/1995 | Last Modified: 02/28/2000<br />
NA<br />
NA<br />
NA<br />
NA<br />
NA<br />
178 Submitted charges. Start: 01/01/1995 A6 or A7<br />
179 Outside lab charges. Start: 01/01/1995 follow -- check to see if in 50<strong>10</strong><br />
180 Hospital s semi-private room rate. Start: 01/01/1995 NA<br />
181 Hospital s room rate. Start: 01/01/1995 NA<br />
182<br />
Allowable/paid from primary coverage. This change to be effective 11/1/20<strong>10</strong>:<br />
Allowable/paid from other entities coverage NOTE: This code requires the use of an<br />
entity code. Start: 01/01/1995 | Last Modified:<br />
01/24/20<strong>10</strong><br />
A6 or A7<br />
for secondary claims<br />
183<br />
Amount entity has paid. This change effective 11/1/20<strong>10</strong>: Amount entity has paid.<br />
Note: This code requires use of an Entity Code. Start: 01/01/1995 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
A6 or A7<br />
patient paid amount must be<br />
positive value and cannot exceed<br />
total claim charge amount.<br />
QC<br />
Page 19 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
184<br />
Purchase price for the rented durable medical equipment. Start:<br />
01/01/1995<br />
A6 or A7<br />
185 Rental price for durable medical equipment. Start: 01/01/1995 A6 or A7<br />
186<br />
Purchase and rental price of durable medical equipment. Start:<br />
01/01/1995<br />
187 Date(s) of service. Start: 01/01/1995 A6 or A7 or A8<br />
188 Statement from-through dates. Start: 01/01/1995 A6 or A7 or A8<br />
189 Facility admission date. Start: 01/01/1995 | Last Modified: <strong>10</strong>/31/2006 A6 or A7 or A8<br />
190 Facility discharge date. Start: 01/01/1995 | Last Modified: <strong>10</strong>/31/2006 A6 or A7 or A8<br />
191 Date of Last Menstrual Period (LMP) Start: 02/28/1997 A6 or A7 or A8<br />
192<br />
Date of first service for current series/symptom/illness. Start:<br />
01/01/1995<br />
NA<br />
ending date of service must be<br />
greater than or equal to the<br />
beginning date of service AND<br />
service line date must be within<br />
statement date range. (may also<br />
get this status code when date is<br />
tied to another reject reason. This<br />
would always be the second code<br />
in this case.)<br />
statement end date must be<br />
greater than or eequal to statement<br />
start date. Statement start date<br />
must be equal to or before<br />
statement dates. (may also get this<br />
status code when date is tied to<br />
another reject reason. This would<br />
always be the second code in this<br />
case.)<br />
Admission date must be equal to or<br />
before statement dates.<br />
LMP date can not be greater than<br />
receipt date. In 837p not in 837I<br />
NA check to see if in 50<strong>10</strong><br />
193 First consultation/evaluation date. Start: 02/28/1997 check to see if in 50<strong>10</strong><br />
194 Confinement dates. Start: 01/01/1995 NA<br />
195<br />
Unable to work dates. This change to be effective 7/1/20<strong>10</strong>: Unable to work<br />
dates/Disability Dates. Start: 01/01/1995 |<br />
Last Modified: 09/20/2009<br />
A6 or A7 or A8<br />
196 Return to work dates. Start: 01/01/1995 A6 or A7 or A8<br />
197 Effective coverage date(s). Start: 01/01/1995 A3 This is patient's coverage<br />
198 Medicare effective date. Start: 01/01/1995 A3 This is patient's coverage<br />
199 Date of conception and expected date of delivery. Start: 01/01/1995 NA<br />
200 Date of equipment return. Start: 01/01/1995 NA<br />
201 Date of dental appliance prior placement. Start: 01/01/1995 A6 or A7 or A8<br />
202<br />
Date of dental prior replacement/reason for replacement. Start:<br />
01/01/1995<br />
A6 or A7 or A8<br />
203 Date of dental appliance placed. Start: 01/01/1995 A6 or A7 or A8<br />
Page 20 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
204<br />
205<br />
206<br />
Date dental canal(s) opened and date service completed. Start:<br />
01/01/1995<br />
Date(s) dental root canal therapy previously performed. Start:<br />
01/01/1995<br />
Most recent date of curettage, root planing, or periodontal surgery. Start:<br />
01/01/1995<br />
NA<br />
NA<br />
NA<br />
2<strong>07</strong> Dental impression and seating date. Start: 01/01/1995 NA<br />
208 Most recent date pacemaker was implanted. Start: 01/01/1995 NA no field<br />
209 Most recent pacemaker battery change date. Start: 01/01/1995 NA<br />
2<strong>10</strong> Date of the last x-ray. Start: 01/01/1995 A6 or A7 or A8<br />
211 Date(s) of dialysis training provided to patient. Start: 01/01/1995 NA<br />
212 Date of last routine dialysis. Start: 01/01/1995 check<br />
213 Date of first routine dialysis. Start: 01/01/1995 check<br />
214 Original date of prescription/orders/referral. Start: 02/28/1997 NA<br />
215 Date of tooth extraction/evolution. Start: 01/01/1995 A6 or A7 or A8<br />
216 Drug information. Start: 01/01/1995 A6 missing NDC segment<br />
217 Drug name, strength and dosage form. Start: 01/01/1995 NA<br />
218 NDC number. Start: 01/01/1995 A6 or A7 or A8<br />
219 Prescription number. Start: 01/01/1995 A6 or A7 24<strong>10</strong> ref segment<br />
220 Drug product id number. Start: 01/01/1995 NA<br />
221<br />
222<br />
Drug days supply and dosage. Start: 01/01/1995<br />
Last Modified: 01/24/20<strong>10</strong> | Stop: 01/01/2012<br />
Drug dispensing units and average wholesale price (AWP). Start:<br />
01/01/1995<br />
| Discontinued 01- check<br />
01-12<br />
check<br />
223 Route of drug/myelogram administration. Start: 01/01/1995 NA<br />
224 Anatomical location for joint injection. Start: 01/01/1995 NA<br />
225 Anatomical location. Start: 01/01/1995 NA<br />
226 Joint injection site. Start: 01/01/1995 NA<br />
227 Hospital information. Start: 01/01/1995 NA<br />
228<br />
Type of bill for UB claim Start: 01/01/1995 |<br />
Last Modified: <strong>10</strong>/31/2006<br />
A6 or A7 or A8<br />
Invalid type of bill (3 digit<br />
combination of CLM05-1 and<br />
CLM05-3)<br />
2<strong>29</strong> Hospital admission source. Start: 01/01/1995 A6 or A7 or A8<br />
230 Hospital admission hour. Start: 01/01/1995 A6 or A7 or A8<br />
Page 21 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
231 Hospital admission type. Start: 01/01/1995 A6 or A7 or A8<br />
232 Admitting diagnosis. Start: 01/01/1995 A6 or A7 or A8<br />
233 Hospital discharge hour. Start: 01/01/1995 A6 or A7 or A8<br />
234 Patient discharge status. Start: 01/01/1995 A6 or A7 or A8<br />
235 Units of blood furnished. Start: 01/01/1995 NA<br />
236 Units of blood replaced. Start: 01/01/1995 NA<br />
237 Units of deductible blood. Start: 01/01/1995 NA<br />
Admitting diagnosis must be<br />
present. Admitting diagnosis must<br />
be a valid value for the admit date,<br />
dates of service and statement<br />
from dates submitted.<br />
238 Separate claim for mother/baby charges. Start: 01/01/1995 A3<br />
239 Dental information. Start: 01/01/1995 NA<br />
To be used if mother and baby<br />
charges are in one claim<br />
240 Tooth surface(s) involved. Start: 01/01/1995 A6 or A7 or A8<br />
241 List of all missing teeth (upper and lower). Start: 01/01/1995 NA check<br />
242<br />
Tooth numbers, surfaces, and/or quadrants involved. Start:<br />
01/01/1995<br />
A6 or A7 or A8<br />
243 Months of dental treatment remaining. Start: 01/01/1995 A6 or A7 or A8<br />
244 Tooth number or letter. Start: 01/01/1995 A6 or A7<br />
245 Dental quadrant/arch. Start: 01/01/1995 A6 or A7<br />
246<br />
Total orthodontic service fee, initial appliance fee, monthly fee, length of service.<br />
Start: 01/01/1995<br />
NA<br />
247 Line information. Start: 01/01/1995 NA<br />
248<br />
Accident date, state, description and cause. Start:<br />
01/01/1995 | Last Modified: 01/24/20<strong>10</strong> | Stop: 01/01/2012<br />
249 Place of service. Start: 01/01/1995 A6 or A7 or A8<br />
250 Type of service. Start: 01/01/1995 NA<br />
Discontinued 01- check for separate versions of 248<br />
01-12<br />
251 Total anesthesia minutes. Start: 01/01/1995 A6 or A7 this is for units<br />
252 Authorization/certification number. Start: 01/01/1995 A6 or A7<br />
254 Primary diagnosis code. Start: 01/01/1995 A6 or A7<br />
255 Diagnosis code. Start: 01/01/1995 A7<br />
256 DRG code(s). Start: 01/01/1995 A6 or A7<br />
Diagnosis code must be a valid<br />
ICD-9-CM Code.<br />
257 ADSM-III-R code for services rendered. Start: 01/01/1995 NA<br />
Page 22 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
258 Days/units for procedure/revenue code. Start: 01/01/1995 A6 or A7 or A8<br />
259 Frequency of service. Start: 01/01/1995 A6 or A7 or A8<br />
260 Length of medical necessity, including begin date. Start: 02/28/1997 NA<br />
261 Obesity measurements. Start: 01/01/1995 NA<br />
262<br />
Type of surgery/service for which anesthesia was administered. Start:<br />
01/01/1995<br />
263 Length of time for services rendered. Start: 01/01/1995 NA check<br />
264<br />
Number of liters/minute & total hours/day for respiratory support. Start:<br />
01/01/1995<br />
265 Number of lesions excised. Start: 01/01/1995 NA<br />
266 Facility point of origin and destination - ambulance. Start: 01/01/1995 A3 or A8<br />
267 Number of miles patient was transported. Start: 01/01/1995 A6 or A7 or A8<br />
NA<br />
NA<br />
Unit value billed is inconsistent with<br />
procedure code.<br />
CR1 segment is missing or is<br />
relational to the procedure<br />
ending point on 7-15-<strong>10</strong> -- see<br />
assignments for individual followup<br />
KUPPE 268 - 300<br />
This is not a clear<br />
enough reason -<br />
do not use<br />
268 Location of durable medical equipment use. Start: 01/01/1995 NA Currently, this is<br />
not sent<br />
269 Length/size of laceration/tumor. Start: 01/01/1995 NA Currently, this is<br />
not sent<br />
270 Subluxation location. Start: 01/01/1995 NA Currently, this is<br />
not sent<br />
271 Number of spine segments. Start: 01/01/1995 NA Currently, this is<br />
not sent<br />
272 Oxygen contents for oxygen system rental. Start: 01/01/1995 NA<br />
273 Weight. Start: 01/01/1995 NA Currently, this is<br />
not sent<br />
274 Height. Start: 01/01/1995 NA Currently, this is<br />
not sent<br />
275 Claim. Start: 01/01/1995 NA<br />
276<br />
UB04/HCFA-1450/1500 claim form Start: 01/01/1995<br />
| Last Modified: <strong>10</strong>/31/2006<br />
277 Paper claim. Start: 01/01/1995 NA<br />
278 Signed claim form. Start: 01/01/1995 NA<br />
NA<br />
85<br />
Not clear<br />
279 Itemized claim. Start: 01/01/1995<br />
PWK Attachment<br />
Page 23 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
280 Itemized claim by provider. Start: 01/01/1995<br />
281 Related confinement claim. Start: 01/01/1995<br />
282 Copy of prescription. Start: 01/01/1995 NA<br />
PWK Attachment<br />
PWK Attachment<br />
283<br />
Medicare entitlement information is required to determine primary coverage<br />
Start: 01/01/1995 | Last Modified: 01/27/2008<br />
NA<br />
PWK Attachment<br />
284 Copy of Medicare ID card. Start: 01/01/1995 NA<br />
PWK Attachment<br />
285 Vouchers/explanation of benefits (EOB). Start: 01/01/1995 NA<br />
286<br />
Other payer's Explanation of Benefits/payment information. Start:<br />
01/01/1995<br />
A6<br />
If report type cd (PWK01) = EB<br />
(EOB) then PWK02 (transmission<br />
code) must not =AA (available at<br />
provider's site).<br />
see 286<br />
PWK Attachment<br />
287 Medical necessity for service. Start: 01/01/1995 NA Currently, this is<br />
not sent<br />
288 Reason for late hospital charges. Start: 01/01/1995<br />
289 Reason for late discharge. Start: 01/01/1995<br />
NA for PB<br />
NA for PB<br />
<strong>29</strong>0 Pre-existing information. Start: 01/01/1995 Currently, this is<br />
not sent<br />
<strong>29</strong>1 Reason for termination of pregnancy. Start: 01/01/1995 Currently, this is<br />
not sent<br />
<strong>29</strong>2 Purpose of family conference/therapy. Start: 01/01/1995 Currently, this is<br />
not sent<br />
<strong>29</strong>3 Reason for physical therapy. Start: 01/01/1995 Currently, this is<br />
not sent<br />
<strong>29</strong>4 Supporting documentation. Start: 01/01/1995<br />
<strong>29</strong>5 Attending physician report. Start: 01/01/1995<br />
<strong>29</strong>6 Nurse's notes. Start: 01/01/1995<br />
<strong>29</strong>7 Medical notes/report. Start: 02/28/1997<br />
<strong>29</strong>8 Operative report. Start: 01/01/1995<br />
PWK Attachment<br />
PWK Attachment<br />
PWK Attachment<br />
PWK Attachment<br />
PWK Attachment<br />
Page 24 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
<strong>29</strong>9 Emergency room notes/report. Start: 01/01/1995<br />
PWK Attachment<br />
300 Lab/test report/notes/results. Start: 02/28/1997<br />
PWK Attachment<br />
KLUG 301 - 350 837P 837I Support<br />
301 MRI report. Start: 01/01/1995<br />
304 Reports for service. Start: 01/01/1995<br />
305 X-ray reports/interpretation. Start: 01/01/1995<br />
306 Detailed description of service. Start: 01/01/1995<br />
3<strong>07</strong> Narrative with pocket depth chart. Start: 01/01/1995<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
? No 837D<br />
available<br />
308 Discharge summary. Start: 01/01/1995<br />
3<strong>10</strong><br />
NA PWK*DS PWK*DS<br />
Progress notes for the six months prior to statement date. Start:<br />
01/01/1995 NA ‐ ‐<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
311 Pathology notes/report. Start: 01/01/1995<br />
312 Dental charting. Start: 01/01/1995<br />
313 Bridgework information. Start: 01/01/1995<br />
314 Dental records for this service. Start: 01/01/1995<br />
315 Past perio treatment history. Start: 01/01/1995<br />
NA PWK*P4 PWK*P4<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
? No 837D<br />
available<br />
316 Complete medical history. Start: 01/01/1995<br />
NA PWK*P5 PWK*P5<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
Page 25 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
317 Patient's medical records. Start: 01/01/1995<br />
NA PWK*M1 PWK*M1<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
318 X-rays. Start: 01/01/1995<br />
NA PWK*MT PWK*MT<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
319 Pre/post-operative x-rays/photographs. Start: 02/28/1997<br />
320 Study models. Start: 01/01/1995<br />
NA PWK*XP PWK*XP<br />
NA ‐ ‐<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
321 Radiographs or models. Start: 01/01/1995<br />
322 Recent fm x-rays. Start: 01/01/1995<br />
323 Study models, x-rays, and/or narrative. Start: 01/01/1995<br />
324 Recent x-ray of treatment area and/or narrative. Start: 01/01/1995<br />
325 Recent fm x-rays and/or narrative. Start: 01/01/1995<br />
326 Copy of transplant acquisition invoice. Start: 01/01/1995<br />
NA PWK*MT PWK*MT<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
Page 26 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
327<br />
Periodontal case type diagnosis and recent pocket depth chart with narrative.<br />
Start: 01/01/1995<br />
NA ‐ ‐<br />
3<strong>29</strong> Exercise notes. Start: 01/01/1995<br />
330 Occupational notes. Start: 01/01/1995<br />
331 History and physical. Start: 01/01/1995 | Last Modified: 08/01/20<strong>07</strong><br />
333 Patient release of information authorization. Start: 01/01/1995<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
A6/A7 CLM09 CLM09<br />
334 Oxygen certification. Start: 01/01/1995<br />
335 Durable medical equipment certification. Start: 01/01/1995<br />
NA PWK*OX PWK*OX<br />
A6/A7 PWK*CT ‐<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
336 Chiropractic certification. Start: 01/01/1995<br />
337 Ambulance certification/documentation. Start: 01/01/1995<br />
NA/A6/A7 CR2 CR2<br />
NA/A6/A7 CRC CRC<br />
Required on<br />
chiropractic claims<br />
involving spinal<br />
manipulation<br />
when the<br />
information is<br />
known to impact<br />
the payer’s<br />
adjudication<br />
process. If not<br />
required by this<br />
implementation<br />
guide, do not<br />
send.<br />
the claim involves<br />
ambulance<br />
339 Enteral/parenteral certification. Start: 01/01/1995<br />
NA PWK*PE PWK*PE<br />
NA‐Best practice<br />
for PWK indicate 3<br />
days. <strong>TAG</strong> agreed<br />
277CA returned<br />
within 24 hours of<br />
receipt from<br />
provider<br />
Page 27 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
340 Pacemaker certification. Start: 01/01/1995<br />
341 Private duty nursing certification. Start: 01/01/1995<br />
342 Podiatric certification. Start: 01/01/1995<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
343<br />
344<br />
Documentation that facility is state licensed and Medicare approved as a surgical<br />
facility. Start: 01/01/1995<br />
Documentation that provider of physical therapy is Medicare Part B approved.<br />
Start: 01/01/1995<br />
NA ‐ ‐<br />
NA ‐ ‐<br />
345 Treatment plan for service/diagnosis Start: 01/01/1995<br />
NA ‐ ‐<br />
346 Proposed treatment plan for next 6 months. Start: 01/01/1995<br />
STROOT 351 - 400<br />
352 Duration of treatment plan. Start: 01/01/1995 A6,<br />
353 Orthodontics treatment plan. Start: 01/01/1995 A6,<br />
354<br />
Treatment plan for replacement of remaining missing teeth. Start:<br />
01/01/1995<br />
355 Has claim been paid? Start: 01/01/1995 NA<br />
356 Was blood furnished? Start: 01/01/1995 NA<br />
357 Has or will blood be replaced? Start: 01/01/1995 NA<br />
358 Does provider accept assignment of benefits? Start: 01/01/1995 NA<br />
359 Is there a release of information signature on file? Start: 01/01/1995 NA<br />
NA ‐ ‐<br />
NA<br />
DN1 segment - Treatment months<br />
could be missing<br />
DN1 segment - Treatment months,<br />
or DN1-04 could be missing.<br />
360<br />
Is there an assignment of benefits signature on file? Start:<br />
01/01/1995<br />
361 Is there other insurance? Start: 01/01/1995 NA<br />
362 Is the dental patient covered by medical insurance? Start: 01/01/1995 NA<br />
363<br />
364<br />
Will worker's compensation cover submitted charges? Start:<br />
01/01/1995<br />
Is accident/illness/condition employment related? Start:<br />
01/01/1995<br />
365 Is service the result of an accident? Start: 01/01/1995 NA<br />
366 Is injury due to auto accident? Start: 01/01/1995 NA<br />
367<br />
Is service performed for a recurring condition or new condition? Start:<br />
01/01/1995<br />
NA<br />
NA<br />
NA<br />
NA<br />
Could this be "A6" missing COB<br />
information?<br />
Could this be "A6" missing<br />
condition information (HI<br />
segment)?<br />
Could this be "A6" missing<br />
condition information (HI<br />
segment)?<br />
Could this be "A6" missing<br />
condition information (HI<br />
segment)?<br />
368<br />
Is medical doctor (MD) or doctor of osteopath (DO) on staff of this facility?<br />
Start: 01/01/1995<br />
NA<br />
Page 28 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
369<br />
Does patient condition preclude use of ordinary bed? Start:<br />
01/01/1995<br />
370 Can patient operate controls of bed? Start: 01/01/1995 NA<br />
371 Is patient confined to room? Start: 01/01/1995 NA<br />
372 Is patient confined to bed? Start: 01/01/1995 NA<br />
373 Is patient an insulin diabetic? Start: 01/01/1995 NA<br />
374 Is prescribed lenses a result of cataract surgery? Start: 01/01/1995 NA<br />
375 Was refraction performed? Start: 01/01/1995 NA<br />
NA<br />
376 Was charge for ambulance for a round-trip? Start: 01/01/1995 NA<br />
377<br />
Was durable medical equipment purchased new or used? Start:<br />
01/01/1995<br />
378 Is pacemaker temporary or permanent? Start: 01/01/1995 NA<br />
NA<br />
Could this be "A6" missing CR1-09<br />
information?<br />
379<br />
380<br />
Were services performed supervised by a physician? Start:<br />
01/01/1995<br />
Were services performed by a CRNA under appropriate medical direction?<br />
Start: 01/01/1995 | Last Modified: <strong>10</strong>/31/1999<br />
NA<br />
NA<br />
381 Is drug generic? Start: 01/01/1995 NA<br />
382<br />
383<br />
384<br />
Did provider authorize generic or brand name dispensing? Start:<br />
01/01/1995<br />
Was nerve block used for surgical procedure or pain management? Start:<br />
01/01/1995<br />
Is prosthesis/crown/inlay placement an initial placement or a replacement?<br />
Start: 01/01/1995<br />
NA<br />
NA<br />
NA<br />
385<br />
Is appliance upper or lower arch & is appliance fixed or removable? Start:<br />
01/01/1995<br />
386 Is service for orthodontic purposes? Start: 01/01/1995 NA<br />
387<br />
Date patient last examined by entity. This change effective 11/1/20<strong>10</strong>: Date patient<br />
last examined by entity. Note: This code requires use of an Entity Code.<br />
Start: 02/28/1997 | Last Modified: 02/11/20<strong>10</strong><br />
388 Date post-operative care assumed. Start: 02/28/1997 A8<br />
389 Date post-operative care relinquished. Start: 02/28/1997 A8<br />
390<br />
Date of most recent medical event necessitating service(s). Start:<br />
02/28/1997<br />
391 Date(s) dialysis conducted. Start: 02/28/1997 NA<br />
392 Date(s) of blood transfusion(s) Start: 02/28/1997 NA<br />
393 Date of previous pacemaker check. Start: 02/28/1997 NA<br />
NA<br />
A6, A8 DTP*304 (Last Seen Date)<br />
??<br />
Assume care date may not be<br />
greater than receipt date.<br />
Relinquish care date cannot be<br />
greater than receipt date.<br />
Is this the same as code 397<br />
below?<br />
394<br />
Date(s) of most recent hospitalization related to service. Start:<br />
02/28/1997<br />
NA<br />
Page <strong>29</strong> of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
395<br />
Date entity signed certification/recertification This change effective 11/1/20<strong>10</strong>: Date<br />
entity signed certification/recertification Note: This code requires use of an Entity<br />
Code. Start: 02/28/1997 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
396 Date home dialysis began. Start: 02/28/1997 NA<br />
397 Date of onset/exacerbation of illness/condition. Start: 02/28/1997 A8<br />
Onset date of current<br />
illness/symptom cannot be greater<br />
than receipt date.<br />
398 Visual field test results. Start: 02/28/1997 NA<br />
399<br />
Report of prior testing related to this service, including dates Start:<br />
02/28/1997<br />
NA<br />
400 Claim is out of balance. Start: 02/28/1997<br />
WICHTERMAN 401 - 450<br />
401 Source of payment is not valid. Start: 02/28/1997 NA<br />
402<br />
Amount must be greater than zero. Note: At least one other status code is required<br />
to identify which amount element is in error. Start: 02/28/1997 | Last<br />
Modified: 09/20/2009<br />
A3 A6 A7<br />
403 Entity referral notes/orders/prescription. Start: 02/28/1997 A6 A7<br />
404<br />
Specific findings, complaints, or symptoms necessitating service. Start:<br />
02/28/1997<br />
A6<br />
405 Summary of services. Start: 02/28/1997 A6<br />
406 Brief medical history as related to service(s). Start: 02/28/1997 NA<br />
4<strong>07</strong> Complications/mitigating circumstances. Start: 02/28/1997 NA<br />
408 Initial certification. Start: 02/28/1997 A6<br />
409<br />
4<strong>10</strong><br />
Medication logs/records (including medication therapy). Start:<br />
02/28/1997<br />
Explain differences between treatment plan and patient's condition. Start:<br />
02/28/1997<br />
NA<br />
NA<br />
411 Medical necessity for non-routine service(s). Start: 02/28/1997 A6<br />
412<br />
413<br />
Medical records to substantiate decision of non-coverage. Start:<br />
02/28/1997<br />
Explain/justify differences between treatment plan and services rendered.<br />
Start: 02/28/1997<br />
NA<br />
NA<br />
414 Need for more than one physician to treat patient. Start: 02/28/1997 A6<br />
415 Justify services outside composite rate. Start: 02/28/1997 A6<br />
416<br />
417<br />
Verification of patient's ability to retain and use information. Start:<br />
02/28/1997<br />
Prior testing, including result(s) and date(s) as related to service(s). Start:<br />
02/28/1997<br />
NA<br />
A6<br />
418 Indicating why medications cannot be taken orally. Start: 02/28/1997 A6<br />
419<br />
Individual test(s) comprising the panel and the charges for each test. Start:<br />
02/28/1997<br />
A6<br />
Page 30 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
420<br />
421<br />
Name, dosage and medical justification of contrast material used for radiology<br />
procedure Start: 02/28/1997<br />
Medical review attachment/information for service(s). Start:<br />
02/28/1997<br />
A6<br />
A6<br />
422 Homebound status. Start: 02/28/1997 NA<br />
424 Statement of non-coverage including itemized bill. Start: 02/28/1997 A6<br />
425 Itemize non-covered services. Start: 02/28/1997 A6<br />
426 All current diagnoses Start: 02/28/1997 A6<br />
427 Emergency care provided during transport. Start: 02/28/1997 A6<br />
428 Reason for transport by ambulance. Start: 02/28/1997 A6<br />
4<strong>29</strong><br />
Loaded miles and charges for transport to nearest facility with appropriate<br />
services. Start: 02/28/1997<br />
A6<br />
430 Nearest appropriate facility. Start: 02/28/1997 A6<br />
431<br />
Provide condition/functional status at time of service. Start:<br />
02/28/1997<br />
A6<br />
432 Date benefits exhausted. Start: 02/28/1997 A6<br />
433 Copy of patient revocation of hospice benefits. Start: 02/28/1997 A6<br />
434<br />
Reasons for more than one transfer per entitlement period Start:<br />
02/28/1997<br />
A6<br />
435 Notice of Admission. Start: 02/28/1997 A6<br />
436 Short term goals. Start: 02/28/1997 A6<br />
437 Long term goals. Start: 02/28/1997 A6<br />
438 Number of patients attending session. Start: 02/28/1997 A6<br />
439 Size, depth, amount, and type of drainage wounds. Start: 02/28/1997 NA<br />
440<br />
Why non-skilled caregiver has not been taught procedure. Start:<br />
02/28/1997<br />
NA<br />
441 Entity professional qualification for service(s). Start: 02/28/1997 A6<br />
442 Modalities of service. Start: 02/28/1997 A6<br />
443 Initial evaluation report. Start: 02/28/1997 A6<br />
444 Method used to obtain test sample. Start: 02/28/1997 NA<br />
445<br />
446<br />
Explain why hearing loss not correctable by hearing aid. Start:<br />
02/28/1997<br />
Documentation from prior claim(s) related to service(s). Start:<br />
02/28/1997<br />
NA<br />
NA<br />
447 Plan of teaching. Start: 02/28/1997 NA<br />
Page 31 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
448<br />
Invalid billing combination. See STC12 for details. This code should only be used to<br />
indicate an inconsistency between two or more data elements on the claim. A<br />
detailed explanation is required in STC12 when this code is used.<br />
Start: 02/28/1997 | Last Modified: 01/24/20<strong>10</strong> | Stop: 01/01/2012<br />
Discontinued 01-<br />
01-12<br />
449 Projected date to discontinue service(s). Start: 02/28/1997 A6<br />
450 Awaiting spend down determination. Start: 02/28/1997 NA<br />
WILLIAMS 451 - 450<br />
451 Preoperative and post-operative diagnosis. Start: 02/28/1997 NA<br />
452<br />
Total visits in total number of hours/day and total number of hours/week.<br />
Start: 02/28/1997<br />
453 Procedure Code Modifier(s) for Service(s) Rendered. Start: 02/28/1997 A6, A7<br />
454 Procedure code for services rendered. Start: 02/28/1997 A6, A7<br />
455 Revenue code for services rendered. Start: 02/28/1997 A6, A7<br />
456 Covered Day(s) Start: 02/28/1997 A7<br />
457 Non-Covered Day(s) Start: 02/28/1997 NA<br />
458 Coinsurance Day(s) Start: 02/28/1997 NA<br />
459 Lifetime Reserve Day(s) Start: 02/28/1997 NA<br />
460 NUBC Condition Code(s) Start: 02/28/1997 A7<br />
461<br />
462<br />
463<br />
464<br />
NUBC Occurrence Code(s) and Date(s) Start:<br />
02/28/1997 | Last Modified: 01/24/20<strong>10</strong> | Stop: 01/01/2012<br />
NUBC Occurrence Span Code(s) and Date(s) Start:<br />
02/28/1997 | Last Modified: 01/24/20<strong>10</strong> | Stop: 01/01/2012<br />
NUBC Value Code(s) and/or Amount(s) Start: 02/28/1997<br />
| Last Modified: 01/24/20<strong>10</strong> | Stop: 01/01/2012<br />
Payer Assigned Claim Control Number Start: 02/28/1997<br />
| Last Modified: <strong>10</strong>/31/2004<br />
NA<br />
Discontinued 01-<br />
01-12<br />
Discontinued 01-<br />
01-12<br />
Discontinued 01-<br />
01-12<br />
465 Principal Procedure Code for Service(s) Rendered Start: 02/28/1997 A7, A8<br />
466<br />
467<br />
Entities Original Signature. This change effective 11/1/20<strong>10</strong>: Entities Original<br />
Signature. Note: This code requires use of an Entity Code. Start: 02/28/1997 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity Signature Date. This change effective 11/1/20<strong>10</strong>: Entity Signature Date. Note:<br />
This code requires use of an Entity Code. Start: 02/28/1997 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
468 Patient Signature Source. Start: 02/28/1997 NA<br />
469 Purchase Service Charge. Start: 02/28/1997<br />
NA<br />
NA<br />
NA<br />
If principal procedure code is<br />
present then this date is required<br />
(A8).<br />
470<br />
Was service purchased from another entity? This change effective 11/1/20<strong>10</strong>: Was<br />
service purchased from another entity? Note: This code requires use of an Entity<br />
Code. Start: 02/28/1997 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
Page 32 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
471 Were services related to an emergency? Start: 02/28/1997 NA<br />
472 Ambulance Run Sheet. Start: 02/28/1997 NA<br />
473 Missing or invalid lab indicator. Start: 06/30/1998 A7, A8<br />
474<br />
475<br />
Procedure code and patient gender mismatch. Start: 06/30/1998<br />
| Last Modified: 02/<strong>29</strong>/2000<br />
Procedure code not valid for patient age Start:<br />
06/30/1998 | Last Modified: 02/<strong>29</strong>/2000<br />
476 Missing or invalid units of service. Start: 06/30/1998 A7<br />
477 Diagnosis code pointer is missing or invalid. Start: 06/30/1998 A8<br />
478<br />
Claim submitter's identifier (patient account number) is missing. This change to be<br />
effective 11/1/20<strong>10</strong> - Claim submitter's identifier. Start: 06/30/1998 | Last<br />
Modified: 01/24/20<strong>10</strong><br />
479 Other Carrier payer ID is missing or invalid. Start: 06/30/1998 A6<br />
A8<br />
A8<br />
A6<br />
Number of services cannot be zero<br />
or a negative value.<br />
First diagnosis pointer cannot point<br />
to "E" diagnosis.<br />
480<br />
Other Carrier Claim filing indicator is missing or invalid. Start:<br />
06/30/1998<br />
481 Claim/submission format is invalid. Start: <strong>10</strong>/31/1998 A3<br />
482<br />
483<br />
Date Error, Century Missing. Start: 02/28/1999 |<br />
Last Modified: 09/20/2009 | Stop: <strong>10</strong>/01/20<strong>10</strong><br />
Maximum coverage amount met or exceeded for benefit period. Start:<br />
06/30/1999<br />
484 Business Application Currently Not Available. Start: 02/<strong>29</strong>/2000 NA<br />
A6, A7<br />
A6, A7<br />
NA<br />
85<br />
485<br />
More information available than can be returned in real time mode. Narrow your<br />
current search criteria. Start: 02/28/2001<br />
NA<br />
486<br />
Principal Procedure Date. Start: <strong>10</strong>/31/2001 |<br />
Last Modified: <strong>07</strong>/01/2009<br />
A8<br />
If principal procedure code is<br />
present then this date is required.<br />
487<br />
Claim not found, claim should have been submitted to/through 'entity'. This change<br />
effective 11/1/20<strong>10</strong>: Claim not found, claim should have been submitted to/through<br />
'entity'. Note: This code requires use of an Entity Code. Start:<br />
02/28/2002 | Last Modified: 02/11/20<strong>10</strong><br />
A3<br />
488 Diagnosis code(s) for the services rendered. Start: 06/30/2002 A6, A7<br />
489 Attachment Control Number. Start: <strong>10</strong>/31/2002 A8<br />
490 Other Procedure Code for Service(s) Rendered. Start: 02/28/2003 A7<br />
491<br />
Entity not eligible for encounter submission. This change effective 11/1/20<strong>10</strong>: Entity<br />
not eligible for encounter submission. Note: This code requires use of an Entity<br />
Code. Start: 02/28/2003 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
492 Other Procedure Date. Start: 02/28/2003 A8<br />
If other procedure code is present,<br />
then this date is required.<br />
493<br />
Version/Release/Industry ID code not currently supported by information holder.<br />
Start: 02/28/2003<br />
A3<br />
Page 33 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
494<br />
495<br />
Real-Time requests not supported by the information holder, resubmit as batch<br />
request. Start: 02/28/2003<br />
Requests for re-adjudication must reference the newly assigned payer claim control<br />
number for this previously adjusted claim. Correct the payer claim control number<br />
and re-submit. Start: <strong>10</strong>/31/2003<br />
NA<br />
A8<br />
496<br />
Submitter not approved for electronic claim submissions on behalf of this entity.<br />
This change effective 11/1/20<strong>10</strong>: Submitter not approved for electronic claim<br />
submissions on behalf of this entity. Note: This code requires use of an Entity<br />
Code. Start: 02/<strong>29</strong>/2004 | Last Modified: 02/11/20<strong>10</strong><br />
A3<br />
497 Sales tax not paid. Start: 06/30/2004 NA<br />
498 Maximum leave days exhausted. Start: 06/30/2004 NA<br />
499<br />
500<br />
501<br />
502<br />
503<br />
504<br />
505<br />
No rate on file with the payer for this service for this entity This change effective<br />
11/1/20<strong>10</strong>: No rate on file with the payer for this service for this entity Note: This<br />
code requires use of an Entity Code. Start: 06/30/2004 | Last Modified:<br />
02/11/20<strong>10</strong><br />
Entity's Postal/Zip Code. This change effective 11/1/20<strong>10</strong>: Entity's Postal/Zip Code.<br />
Note: This code requires use of an Entity Code. Start: 06/30/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
ROY 501 - 550<br />
Entity's State/Province. This change effective 11/1/20<strong>10</strong>: Entity's State/Province.<br />
Note: This code requires use of an Entity Code. Start: 06/30/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's City. This change effective 11/1/20<strong>10</strong>: Entity's City. Note: This code requires<br />
use of an Entity Code. Start: 06/30/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's Street Address. This change effective 11/1/20<strong>10</strong>: Entity's Street Address.<br />
Note: This code requires use of an Entity Code. Start: 06/30/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's Last Name. This change effective 11/1/20<strong>10</strong>: Entity's Last Name. Note: This<br />
code requires use of an Entity Code. Start: 06/30/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's First Name. This change effective 11/1/20<strong>10</strong>: Entity's First Name. Note: This<br />
code requires use of an Entity Code. Start: 06/30/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
NA<br />
A7<br />
A7<br />
77, 85, 87, DK, GB,<br />
HK, PR, QC, SEP<br />
77, 85, 87, DK, GB,<br />
HK, PR, QC<br />
506<br />
Entity is changing processor/clearinghouse. This claim must be submitted to the<br />
new processor/clearinghouse. This change effective 11/1/20<strong>10</strong>: Entity is changing<br />
processor/clearinghouse. This claim must be submitted to the new<br />
processor/clearinghouse. Note: This code requires use of an Entity Code.<br />
Start: 06/30/2004 | Last Modified: 02/11/20<strong>10</strong><br />
NA<br />
5<strong>07</strong> HCPCS Start: <strong>10</strong>/31/2004<br />
508<br />
ICD9 NOTE: At least one other status code is required to identify the related<br />
procedure code or diagnosis code. Start: <strong>10</strong>/31/2004 | Last<br />
Modified: <strong>07</strong>/01/2009<br />
509 E-Code Start: <strong>10</strong>/31/2004 A7, A8<br />
5<strong>10</strong><br />
Future date. This change to be effective 7/1/20<strong>10</strong>: Future date. Note: At least one<br />
other status code is required to identify the data element in error.<br />
Start: <strong>10</strong>/31/2004 | Last Modified: 09/20/2009<br />
???<br />
A8<br />
Similar to code 21, questioning<br />
value if another more specific code<br />
is needed.<br />
First diagnosis pointer cannot point<br />
to "E" diagnosis (A8).<br />
LMP date can not be greater than<br />
receipt date.<br />
Page 34 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
511<br />
512<br />
Invalid character. This change to be effective 7/1/20<strong>10</strong>: Invalid character. Note: At<br />
least one other status code is required to identify the data element in error.<br />
Start: <strong>10</strong>/31/2004 | Last Modified: 09/20/2009<br />
Length invalid for receiver's application system. This change to be effective<br />
7/1/20<strong>10</strong>: Length invalid for receiver's application system. Note: At least one other<br />
status code is required to identify the data element in error.<br />
Start: <strong>10</strong>/31/2004 | Last Modified: 09/20/2009<br />
513 HIPPS Rate Code for services Rendered Start: <strong>10</strong>/31/2004 A7<br />
514<br />
Entities Middle Name This change effective 11/1/20<strong>10</strong>: Entities Middle Name Note:<br />
This code requires use of an Entity Code. Start: <strong>10</strong>/31/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Product or service ID qualifier must<br />
equal HC or ZZ.<br />
515 Managed Care review Start: <strong>10</strong>/31/2004<br />
516<br />
Adjudication or Payment Date. This change to be effective 7/1/20<strong>10</strong>: Other Entity's<br />
Adjudication or Payment/Remittance Date. Note: An Entity code is required to<br />
identify the Other Payer Entity, i.e. primary, secondary. Start:<br />
<strong>10</strong>/31/2004 | Last Modified: 11/<strong>29</strong>/2009<br />
517 Adjusted Repriced Claim Reference Number Start: <strong>10</strong>/31/2004<br />
518 Adjusted Repriced Line item Reference Number Start: <strong>10</strong>/31/2004<br />
519 Adjustment Amount Start: <strong>10</strong>/31/2004<br />
520 Adjustment Quantity Start: <strong>10</strong>/31/2004<br />
521 Adjustment Reason Code Start: <strong>10</strong>/31/2004 A7<br />
522 Anesthesia Modifying Units Start: <strong>10</strong>/31/2004<br />
523 Anesthesia Unit Count Start: <strong>10</strong>/31/2004<br />
524 Arterial Blood Gas Quantity Start: <strong>10</strong>/31/2004<br />
525 Begin Therapy Date Start: <strong>10</strong>/31/2004<br />
526 Bundled or Unbundled Line Number Start: <strong>10</strong>/31/2004<br />
527 Certification Condition Indicator Start: <strong>10</strong>/31/2004<br />
528 Certification Period Projected Visit Count Start: <strong>10</strong>/31/2004<br />
5<strong>29</strong> Certification Revision Date Start: <strong>10</strong>/31/2004<br />
530 Claim Adjustment Indicator Start: <strong>10</strong>/31/2004 A8<br />
When CLM Freq Type Cd (CLM05-<br />
3) indicates claim is a replacement<br />
or cancel, then this REF segment<br />
must contain the original payer<br />
claim number. 85<br />
531 Claim Disproportinate Share Amount Start: <strong>10</strong>/31/2004<br />
532 Claim DRG Amount Start: <strong>10</strong>/31/2004<br />
Page 35 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
533 Claim DRG Outlier Amount Start: <strong>10</strong>/31/2004<br />
534 Claim ESRD Payment Amount Start: <strong>10</strong>/31/2004<br />
535 Claim Frequency Code Start: <strong>10</strong>/31/2004 A3, A7<br />
A3 used when<br />
original claim is<br />
medicare crossover<br />
to indicate that<br />
Medicare must be<br />
replaced or<br />
cancelled first. A7<br />
is used when the<br />
value submitted is<br />
not valid.<br />
536 Claim Indirect Teaching Amount Start: <strong>10</strong>/31/2004<br />
537 Claim MSP Pass-through Amount Start: <strong>10</strong>/31/2004<br />
538 Claim or Encounter Identifier Start: <strong>10</strong>/31/2004<br />
539 Claim PPS Capital Amount Start: <strong>10</strong>/31/2004<br />
540 Claim PPS Capital Outlier Amount Start: <strong>10</strong>/31/2004<br />
541 Claim Submission Reason Code Start: <strong>10</strong>/31/2004<br />
542 Claim Total Denied Charge Amount Start: <strong>10</strong>/31/2004<br />
543 Clearinghouse or Value Added Network Trace Start: <strong>10</strong>/31/2004<br />
544 Clinical Laboratory Improvement Amendment Start: <strong>10</strong>/31/2004<br />
545 Contract Amount Start: <strong>10</strong>/31/2004<br />
546 Contract Code Start: <strong>10</strong>/31/2004<br />
547 Contract Percentage Start: <strong>10</strong>/31/2004<br />
548 Contract Type Code Start: <strong>10</strong>/31/2004<br />
549 Contract Version Identifier Start: <strong>10</strong>/31/2004<br />
550 Coordination of Benefits Code Start: <strong>10</strong>/31/2004<br />
WILSON 551 - 600<br />
551 Coordination of Benefits Total Submitted Charge Start: <strong>10</strong>/31/2004 A6,A7 ??? Not is 50<strong>10</strong> 837<br />
Additiona 837 l<br />
Comments<br />
Page 36 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
552 Cost Report Day Count Start: <strong>10</strong>/31/2004 A6<br />
553 Covered Amount Start: <strong>10</strong>/31/2004 A6<br />
554 Date Claim Paid Start: <strong>10</strong>/31/2004 A6, A7<br />
555 Delay Reason Code Start: <strong>10</strong>/31/2004 A6<br />
556 Demonstration Project Identifier Start: <strong>10</strong>/31/2004 A6<br />
837I only: Cost Report Day Count<br />
is missing (A6)<br />
????? 837 only references the noncovered<br />
amount<br />
837 P,I, D: Date Claim Paid is<br />
missing (A6) Or invalid (A7)<br />
837 P,I D: Delay Reason Code is<br />
Missing (A6)<br />
837 P,& I Demonstration Project<br />
Identifier is missing (A6)<br />
CMS Situtiational<br />
Rule: Required<br />
when inpatient<br />
adjudication<br />
information is<br />
reported in the<br />
remittance<br />
advice.OR<br />
Required when it<br />
is necessary to<br />
report remark<br />
codes.<br />
2330B DTP*573<br />
Situational Rules:<br />
Required when the<br />
claim is submitted<br />
late (past<br />
contracted date of<br />
filing<br />
limitations).2300<br />
CLM20<br />
Stiuational<br />
Rule:Required<br />
when it is<br />
necessary to<br />
identify claims<br />
which are atypical<br />
in ways such as<br />
content, purpose,<br />
and/or payment,<br />
as could be the<br />
case for a<br />
demonstration or<br />
other special<br />
project, or a<br />
clinical trial:.<br />
Page 37 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
557 Diagnosis Date Start: <strong>10</strong>/31/2004 A6,A7<br />
Required for Home HealthCare<br />
billling. Date of Onset or<br />
Exacerbation of Principal<br />
Diagnosis: Diagnosis Date is<br />
missing (A6) OR invalid (A7)<br />
Most of the Home<br />
HealthCare<br />
segments have<br />
been removed in<br />
50<strong>10</strong>. 837i, Home<br />
HealthCare<br />
Information,<br />
primary is CR605,<br />
secondary diag 1<br />
is CR618, diag 2 is<br />
CR619, diag 3 is<br />
CR620, diag 4 is<br />
CR621<br />
558 Discount Amount Start: <strong>10</strong>/31/2004 A6,A7<br />
837P & D 50<strong>10</strong> -Discount Amount<br />
Section Removed. 837I references<br />
the term "Discount Percentage ???<br />
Discount Percentage Amount is<br />
missing (A6) OR invalid (A7)<br />
837 I Terms<br />
Discount Percent :<br />
Terms discount<br />
percentage,<br />
expressed as a<br />
percent, available<br />
to the purchaser if<br />
an invoice is paid<br />
on or before the<br />
Terms Discount<br />
Due Date<br />
SITUATIONAL<br />
RULE: Required<br />
when the provider<br />
is required by<br />
contract<br />
to supply this<br />
information on the<br />
claim.<br />
IMPLEMENTATIO<br />
N NAME: Terms<br />
Discount<br />
Percentage<br />
Page 38 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
559 Document Control Identifier Start: <strong>10</strong>/31/2004 A6, A7<br />
837 P&I: Payer document Control<br />
Number Identifier is missing (A6)<br />
OR invalid (A7)<br />
837 P, I: Required<br />
when CLM05-3<br />
(Claim Frequency<br />
Code) indicates<br />
this claim is a<br />
replacement or<br />
void to a<br />
previously<br />
adjudicated claim .<br />
TR3 Note: This<br />
information is<br />
specific to the<br />
destination payer<br />
reported in Loop<br />
ID-20<strong>10</strong>BB.<br />
560<br />
Entity's Additional/Secondary Identifier. This change effective 11/1/20<strong>10</strong>: Entity's<br />
Additional/Secondary Identifier. Note: This code requires use of an Entity Code.<br />
Start: <strong>10</strong>/31/2004 | Last Modified: 02/11/20<strong>10</strong><br />
A6,A7<br />
837 P,I D : Missing required<br />
secondary identifier (A6) OR<br />
Invalid secondary identifier (A7)<br />
41, FA,HK,82,85,<br />
DN, 71, 72, DQ,<br />
73,DD,,DK, PR<br />
561<br />
562<br />
Entity's Contact Name. This change effective 11/1/20<strong>10</strong>: Entity's Contact Name.<br />
Note: This code requires use of an Entity Code. Start: <strong>10</strong>/31/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
Entity's National Provider Identifier (NPI). This change effective 11/1/20<strong>10</strong>: Entity's<br />
National Provider Identifier (NPI). Note: This code requires use of an Entity Code.<br />
Start: <strong>10</strong>/31/2004 | Last Modified: 02/11/20<strong>10</strong><br />
A6, A7<br />
A3, A6, A7, A8<br />
837 P, I, D: Submitter or Billing<br />
Provider Contact Name is missing (<br />
A6) OR Invalid ( A7)<br />
837 P,I,D: NPI has not been<br />
reported to the payer (A3). OR NPI<br />
is missing and provider is not<br />
atypical (A6) OR NPI is invalid<br />
(A7). OR multiple provider type<br />
identifiers are not allowed on the<br />
same claim (A8).<br />
85 Billing Provider<br />
41 Submitter<br />
41, FA,HK,82,85,<br />
DN, 71, 72, DQ,<br />
73,DD,DK, PR<br />
Page 39 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
563<br />
Entity's Tax Amount. This change effective 11/1/20<strong>10</strong>: Entity's Tax Amount. Note:<br />
This code requires use of an Entity Code. Start: <strong>10</strong>/31/2004 |<br />
Last Modified: 02/11/20<strong>10</strong><br />
A6<br />
837, P, I, D : Sales Tax amount is<br />
missing (A6)<br />
85 Billing Provider<br />
Situational<br />
Rule:Required<br />
when sales tax<br />
applies to the<br />
service line and<br />
the submitter is<br />
required to report<br />
that information to<br />
the receiver. If not<br />
required by this<br />
implementation<br />
guide, do not<br />
send. TR3<br />
Note:When<br />
reporting the Sales<br />
Tax Amount<br />
(AMT02), the<br />
amount reported<br />
in the Line Item<br />
Charge Amount<br />
(SV<strong>10</strong>2) for this<br />
service line must<br />
include the<br />
amount reported in<br />
the Sales Tax<br />
Amount.<br />
564 EPSDT Indicator Start: <strong>10</strong>/31/2004 A6 A7<br />
837 P, I , D: EPSDT Indicator is<br />
missing (A6) OR invalid (A7)<br />
565 Estimated Claim Due Amount Start: <strong>10</strong>/31/2004 A6,A7<br />
837 I: Required when the Patient<br />
Responsibility Amount is applicable<br />
to this claim. Estimated Claim Due<br />
Amount is missing (A6) OR invalid<br />
(A7)<br />
QC<br />
837i only. The<br />
payer Estimated<br />
Claim Due Amount<br />
was removed in<br />
50<strong>10</strong>. Only the<br />
patient claim due<br />
amount remains.<br />
2300 loop AMT*F3<br />
566 Exception Code Start: <strong>10</strong>/31/2004 A6 A7<br />
937 P,I, D: Required when this<br />
information is deemed necessary<br />
by the repricer. The segment is not<br />
completed by providers. The<br />
information is completed by<br />
repricers only. Exception Code is<br />
missing (A6) OR invalid (A7)<br />
The only<br />
esxception code I<br />
could find, other<br />
that the service<br />
authorization<br />
exception code, is<br />
th one use in the<br />
HCP reprising<br />
information<br />
segment. 2300<br />
and 2400 loops in<br />
HCP15<br />
Page 40 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
567 Facility Code Qualifier Start: <strong>10</strong>/31/2004 A6, A7<br />
568 Family Planning Indicator Start: <strong>10</strong>/31/2004 A6, A7<br />
569 Fixed Format Information Start: <strong>10</strong>/31/2004 A6<br />
837 P, I , D. :Facility Code<br />
Quallifier is missing (A6) OR<br />
invalid (A7)<br />
837 P & I: Required when<br />
applicable for Medicaid claims;<br />
Family Planning Indicator is<br />
missing (A6) OR invalid (A7)<br />
837 P, I , D: See TR3 Notes: If K3<br />
segment is approved for use by<br />
X12, then the following would<br />
apply: Fixed Format Informatiion<br />
missing (A6)<br />
In 40<strong>10</strong> this was<br />
"NOT USED" in<br />
the 837p. 2300<br />
loop CLM05-2<br />
2400 loop SV112<br />
TR3 Notes:At the<br />
time of publication<br />
of this<br />
implementation,<br />
K3 segments have<br />
no specific use.<br />
The K3 segment is<br />
expected to be<br />
used only when<br />
necessary to meet<br />
the unexpected<br />
data requirement<br />
of a legislative<br />
authority. Before<br />
this segment can<br />
be used :<br />
- The X12N Health<br />
Care Claim<br />
workgroup must<br />
conclude there is<br />
no<br />
other available<br />
option in the<br />
implementation<br />
guide to meet the<br />
emergency<br />
legislative<br />
requirement.<br />
- The requestor<br />
must submit a<br />
proposal for<br />
approval<br />
accompanied by<br />
Page 41 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
570 Free Form Message Text Start: <strong>10</strong>/31/2004 ????<br />
571 Frequency Count Start: <strong>10</strong>/31/2004 ???<br />
572 Frequency Period Start: <strong>10</strong>/31/2004 ????<br />
573 Functional Limitation Code Start: <strong>10</strong>/31/2004 A6 A7<br />
574 HCPCS Payable Amount Home Health Start: <strong>10</strong>/31/2004 ???<br />
837 P, I. D: If NTE Segment is<br />
used, then NTE03 is required.<br />
Free Form Message Text is<br />
missing ( A6)OR invalid (A7)<br />
Formerly in the Home HealthCare<br />
HSD segment. No longer used in<br />
50<strong>10</strong>. HSD04<br />
Formerly in the Home HealthCare<br />
HSD segment. No longer used in<br />
50<strong>10</strong>. HSD03<br />
837 P: Functional Limitation Code<br />
is missing (A6) OR invalid (A7)<br />
837P & I : Cannot find specifc to<br />
home heatlh??<br />
Situational Rule: to<br />
substantiate the<br />
medical treatment<br />
and is not<br />
supported<br />
elsewhere<br />
within the claim<br />
data set. OR<br />
Required when in<br />
the judgment of<br />
the provider,<br />
narrative<br />
information from<br />
the forms “Home<br />
Health<br />
Certification and<br />
Plan of Treatment”<br />
or “Medical<br />
Update and<br />
Patient<br />
Information” is<br />
needed to<br />
substantiate home<br />
health<br />
services. If not<br />
required by this<br />
implementation<br />
guide, do not<br />
send.<br />
206 TR3 Notes: 1.<br />
The developers of<br />
this<br />
implementation<br />
The only functional<br />
limitation<br />
reference is the<br />
CRC*75 segment<br />
in the 837p. Not<br />
sure what the<br />
code would be.<br />
Does not<br />
specifically state<br />
home health…just<br />
HCPCS Montary<br />
Amt. (2320<br />
HCPCS Payable<br />
Amount in<br />
MOA02)<br />
Page 42 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
575 Homebound Indicator Start: <strong>10</strong>/31/2004 A6 A7<br />
576 Immunization Batch Number Start: <strong>10</strong>/31/2004 A6<br />
577 Industry Code Start: <strong>10</strong>/31/2004 A6 A7<br />
578 Insurance Type Code Start: <strong>10</strong>/31/2004 A6 A7<br />
579 Investigational Device Exemption Identifier Start: <strong>10</strong>/31/2004 A6 A7<br />
580 Last Certification Date Start: <strong>10</strong>/31/2004<br />
581 Last Worked Date Start: <strong>10</strong>/31/2004 A6<br />
582 Lifetime Psychiatric Days Count Start: <strong>10</strong>/31/2004 A6<br />
583 Line Item Charge Amount Start: <strong>10</strong>/31/2004 A3 A6<br />
837 P& I :Homebound Indicator is<br />
missing (A6) OR invalid (A7)<br />
837P: Immunization Batch Number<br />
missing (A6)<br />
837 P,I, D : Industry Code missing<br />
(A6) OR invalid ( A7)<br />
837 P , I , D: Insurance Type Code<br />
missing (A6) OR invalid ( A7)<br />
837 P & I : Investigational Device<br />
Exemption Identifier is missing (<br />
A6) OR invalid ( A7)<br />
837P: Last Certification Date is<br />
missing (A6) OR invalid (A7)<br />
837 P: Last Worked Date is<br />
missing (A6)<br />
837I : Lifetime Psychiatric Days<br />
Count missing ( A6)<br />
837 P, I, D : Line Item Charge<br />
Amount was not submitted to the<br />
payer (A3) OR missing (A6)<br />
Required for<br />
Medicare claims<br />
when an<br />
independent<br />
laboratory renders<br />
an<br />
EKG tracing or<br />
obtains a<br />
specimen from a<br />
homebound or<br />
institutionalized<br />
patient. 2300 loop<br />
CRC*75 field<br />
CRC03<br />
Sum of service<br />
line charges must<br />
equal the Total<br />
Claim Charge<br />
Amount in Loop<br />
2300 CLM02<br />
Page 43 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
584 Line Item Control Number Start: <strong>10</strong>/31/2004 A6<br />
837P,I,D: Line Item Control<br />
Number is missing (A6)<br />
TR3 NoteS:The<br />
line item control<br />
number must be<br />
unique within a<br />
patient control<br />
number (CLM01).<br />
Payers are<br />
required to return<br />
this number in the<br />
remittance advice<br />
transaction (835) if<br />
the provider sends<br />
it to them in<br />
the 837 and<br />
adjudication is<br />
based upon line<br />
item detail<br />
regardless of<br />
whether bundling<br />
or unbundling has<br />
occurred. 2400<br />
loop REF*6R<br />
585<br />
Denied Charge or Non-covered Charge Start: <strong>10</strong>/31/2004<br />
| Last Modified: <strong>07</strong>/09/20<strong>07</strong><br />
586 Line Note Text Start: <strong>10</strong>/31/2004 A6 A7<br />
587 Measurement Reference Identification Code Start: <strong>10</strong>/31/2004 ?? Cannot find<br />
588 Medical Record Number Start: <strong>10</strong>/31/2004 A6 A7<br />
A6<br />
837 P I D: Non Covered Charges<br />
missing (A6)<br />
837 P & I: If NTE segment is used<br />
then NTE02 is required. Line Note<br />
Text is missing (A6)<br />
837 P & I : Medical Record Number<br />
is missing (A6) OR invalid (A7)<br />
For an 837i,<br />
Required when the<br />
TPO/repricer<br />
needs to forward<br />
additional<br />
information to the<br />
payer. This<br />
segment is not<br />
completed by<br />
providers<br />
Could not find a<br />
reference to this<br />
name<br />
589 Medicare Assignment Code Start: <strong>10</strong>/31/2004 A6<br />
837 P&I Provider Accept<br />
Assignment Code: Medicare<br />
Assignement Code is missing (A6)<br />
2300 CLM<strong>07</strong><br />
Page 44 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
590 Medicare Coverage Indicator Start: <strong>10</strong>/31/2004 A6,A7 ???<br />
591 Medicare Paid at <strong>10</strong>0% Amount Start: <strong>10</strong>/31/2004 NA<br />
592 Medicare Paid at 80% Amount Start: <strong>10</strong>/31/2004 NA<br />
593 Medicare Section 4081 Indicator Start: <strong>10</strong>/31/2004 A6,A7<br />
Required when the submitter is<br />
Medicare and the claim is a<br />
Medigap or COB crossover claim.<br />
I am going to<br />
guess that this is<br />
SBR09. If the<br />
destination payer<br />
in loop 20<strong>10</strong>BB is<br />
Medicare the<br />
claim filing<br />
indicator should<br />
indicate the proper<br />
Medicare<br />
coverage.<br />
I am thinking that<br />
these are 276<br />
responces as to<br />
what adjudication<br />
was used<br />
I am thinking that<br />
these are 276<br />
responces as to<br />
what adjudication<br />
was used<br />
2300 REF*F5<br />
594 Mental Status Code Start: <strong>10</strong>/31/2004 A6,A7<br />
595 Monthly Treatment Count Start: <strong>10</strong>/31/2004 ??<br />
596 Non-covered Charge Amount Start: <strong>10</strong>/31/2004 A6 A7<br />
597 Non-payable Professional Component Amount Start: <strong>10</strong>/31/2004 ??<br />
This segment is required to convey<br />
Home Health Plan of Treatment<br />
information when applicable.<br />
837 P, I, D: Non-covered charge<br />
amount cannot be greater than<br />
service line charge amount. Non<br />
Covered Charge Amount is missing<br />
(A6) OR invalid<br />
Most of the Home<br />
HealthCare<br />
segments have<br />
been removed in<br />
50<strong>10</strong>. 837i, 2300<br />
CRC*77<br />
could not find a<br />
reference to this<br />
added to 837p in<br />
50<strong>10</strong><br />
I could only find<br />
the professional<br />
component<br />
BILLED amount<br />
Page 45 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
598<br />
Non-payable Professional Component Billed Amount Start:<br />
<strong>10</strong>/31/2004<br />
A7 ?????<br />
Used when there<br />
was a prior<br />
payment and<br />
required when<br />
returned in the<br />
prior remittance<br />
advice. 2320<br />
MOA09 and in<br />
837i 2320 loop<br />
MIA19<br />
599 Note Reference Code Start: <strong>10</strong>/31/2004 A6,A7<br />
EVELSIZER 601 - 700<br />
837 P I D: If NTESegment is used<br />
then NTE01 is required . Note<br />
Reference Code is missing (A6)<br />
OR invalid (A7)<br />
0040<strong>10</strong>X098A1 CR511 - Entire<br />
CR5 segment removed in<br />
0050<strong>10</strong>X222A1<br />
2300 and 2400<br />
loops NTE01<br />
600 Oxygen Saturation Qty Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
0050<strong>10</strong>X223A1 may carry percent<br />
value using Value Code 59 -<br />
covered under error code 726 (nonspecific)<br />
601 Oxygen Test Condition Code Start: <strong>10</strong>/31/2004<br />
602 Oxygen Test Date Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
A3 or A7?<br />
999 will report<br />
50<strong>10</strong> standard allows CR511<br />
If element is sent, 277CA with error<br />
code 684 and A3 may be returned.<br />
0040<strong>10</strong>X098A1 CR512 - Entire<br />
CR5 segment removed in<br />
0050<strong>10</strong>X222A1<br />
0040<strong>10</strong>X098A1 DTP with DTP01<br />
481 removed in 0050<strong>10</strong>X222A1<br />
http://ushik.ahrq.g<br />
ov/dr.ui.drData_Pa<br />
ge?system=mdr&<br />
Search=xxKEYIDx<br />
x&KeyOrgID=18&<br />
KeyRID=2662300<br />
0&Referer=DataEl<br />
ement<br />
Page 46 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
603 Old Capital Amount Start: <strong>10</strong>/31/2004 A7<br />
604 Originator Application Transaction Identifier Start: <strong>10</strong>/31/2004 A6<br />
0050<strong>10</strong>X223A1 MIA12 - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
Destination Payer may not be able<br />
to determine when this value is<br />
required. If present must be valid<br />
monetary amount. No known<br />
crossedit against other data.<br />
0050<strong>10</strong>X222A1 BHT03 required<br />
0050<strong>10</strong>X223A1 BHT03 required<br />
g<br />
ov/dr.ui.drData_Pa<br />
ge?System=mdr&<br />
CallingRoutine=&<br />
ResponsibleOrgan<br />
ization=&Submittin<br />
gOrganization=&R<br />
egistrationAuthorit<br />
y=&Administrative<br />
Status=&Registrati<br />
onStatus=&Criteri<br />
aDataType=&Com<br />
ponentName=&Da<br />
taAgreementID=&<br />
DefinitionSearchT<br />
ype=&DefinitionSe<br />
arch=&valueMeani<br />
ngSearchType=$v<br />
alueMeaningSearc<br />
hType$&valueMea<br />
ningSearch=$valu<br />
eMeaningSearch$<br />
&valueSearch=$v<br />
alueSearch$&Nam<br />
eSearchType=&Se<br />
arch=O&ModelOrg<br />
ID=&ModelRegID=<br />
&InitiativeOrgID=&<br />
InitiativeRegID=&<br />
KeyOrgID=3&Key<br />
RID=26453000&O<br />
rgID=&DataCollect<br />
ionID=&RecordOff<br />
605 Orthodontic Treatment Months Count Start: <strong>10</strong>/31/2004 A7 or A8<br />
606 Paid From Part A Medicare Trust Fund Amount Start: <strong>10</strong>/31/2004<br />
6<strong>07</strong> Paid From Part B Medicare Trust Fund Amount Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
A3 or A7?<br />
999 will report<br />
0050<strong>10</strong>X224A1 BHT03 required<br />
0050<strong>10</strong>X224A1 DN<strong>10</strong>2 sit required<br />
0040<strong>10</strong>X096A1 AMT segment<br />
removed in 0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows AMT<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0040<strong>10</strong>X096A1 AMT segment<br />
removed in 0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows AMT<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
Page 47 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
608 Paid Service Unit Count Start: <strong>10</strong>/31/2004 A6 or A7<br />
609 Participation Agreement Start: <strong>10</strong>/31/2004 A7<br />
0050<strong>10</strong>X222A1 SVD05<br />
0050<strong>10</strong>X223A1 SVD05<br />
0050<strong>10</strong>X224A1 SVD05<br />
No known crossedit against other<br />
data.<br />
0050<strong>10</strong>X222A1 CLM<strong>07</strong><br />
0050<strong>10</strong>X223A1 CLM<strong>07</strong><br />
0050<strong>10</strong>X224A1 CLM<strong>07</strong><br />
If CLM<strong>07</strong> is not 'A', then an error<br />
may be returned if a Participation<br />
Agreement exists<br />
6<strong>10</strong> Patient Discharge Facility Type Code Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
0040<strong>10</strong>X096A1 CR617 - Entire<br />
CR6 segment removed in<br />
0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows CR617<br />
If element is sent, 277CA with error<br />
code 684 and A3 may be returned.<br />
611 Peer Review Authorization Number Start: <strong>10</strong>/31/2004 A6 or A7<br />
0050<strong>10</strong>X223A1 REF01 = G4<br />
Crosscheck against REF01 if<br />
REF02 is blank considered A6<br />
612 Per Day Limit Amount Start: <strong>10</strong>/31/2004<br />
613 Physician Contact Date Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
A3 or A7?<br />
999 will report<br />
0040<strong>10</strong>X096A1 AMT - AMT01 =<br />
DY segment removed in<br />
0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows AMT<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0040<strong>10</strong>X096A1 CR614 - Entire<br />
CR6 segment removed in<br />
0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows CR614<br />
If element is sent, 277CA with error<br />
code 684 and A3 may be returned.<br />
614 Physician Order Date Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
615 Policy Compliance Code Start: <strong>10</strong>/31/2004 A3 or A7<br />
0040<strong>10</strong>X096A1 CR612 - Entire<br />
CR6 segment removed in<br />
0050<strong>10</strong>X223A1<br />
0050<strong>10</strong>X222A1 HCP14<br />
0050<strong>10</strong>X223A1 HCP14<br />
0050<strong>10</strong>X224A1 HCP14<br />
Note: this entire segment, including<br />
this element is not expected in the<br />
837 for a provider to payer<br />
exchange. If received by<br />
destination payer, rejection may<br />
occur. (A3)<br />
Page 48 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
616 Policy Name Start: <strong>10</strong>/31/2004 N/A<br />
617 Postage Claimed Amount Start: <strong>10</strong>/31/2004 A7 or A8<br />
618 PPS-Capital DSH DRG Amount Start: <strong>10</strong>/31/2004 A7<br />
619 PPS-Capital Exception Amount Start: <strong>10</strong>/31/2004 A7<br />
620 PPS-Capital FSP DRG Amount Start: <strong>10</strong>/31/2004 A7<br />
621 PPS-Capital HSP DRG Amount Start: <strong>10</strong>/31/2004 A7<br />
622 PPS-Capital IME Amount Start: <strong>10</strong>/31/2004 A7<br />
623 PPS-Operating Federal Specific DRG Amount Start: <strong>10</strong>/31/2004 A7<br />
624 PPS-Operating Hospital Specific DRG Amount Start: <strong>10</strong>/31/2004 A7<br />
625 Predetermination of Benefits Identifier Start: <strong>10</strong>/31/2004 A3<br />
626 Pregnancy Indicator Start: <strong>10</strong>/31/2004 A7<br />
Possible SBR04 Group Plan<br />
Name. Policy Name listed as<br />
present in 0050<strong>10</strong>X224A1 in<br />
reference material, but not found.<br />
0050<strong>10</strong>X222A1 AMT - AMT01 =<br />
F4<br />
Crosscheck against service line<br />
charge.<br />
0050<strong>10</strong>X223A1 MIA11 - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
0050<strong>10</strong>X223A1 MIA24 - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
0050<strong>10</strong>X223A1 MIA09 - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
0050<strong>10</strong>X223A1 MIA<strong>10</strong> - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
0050<strong>10</strong>X223A1 MIA13 - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
0050<strong>10</strong>X223A1 MIA16 - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
0050<strong>10</strong>X223A1 MIA14 - Sit rule<br />
Required when returned in the<br />
remittance advice<br />
predetermination of benefit<br />
inquiries cannot be submitted<br />
electronically using the 837<br />
transaction for this payer.<br />
0050<strong>10</strong>X223A1 2000B, 2000C<br />
PAT09 - Sit rule Required when<br />
mandated by law.<br />
http://ushik.ahrq.g<br />
ov/dr.ui.drData_Pa<br />
ge?system=mdr&<br />
KeyRID=2687800<br />
0&Referer=DataEl<br />
ement<br />
627 Pre-Tax Claim Amount Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
0040<strong>10</strong>X098A1 2320 AMT - Entire<br />
AMT qualifier T2 segment removed<br />
in 0050<strong>10</strong>X222A1<br />
50<strong>10</strong> standard allows AMT<br />
If segment T2 is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
Page 49 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
0050<strong>10</strong>X222A1 2300, 2400 HCP01<br />
0050<strong>10</strong>X223A1 2300, 2400 HCP01<br />
0050<strong>10</strong>X224A1 2300, 2400 HCP01<br />
628 Pricing Methodology Start: <strong>10</strong>/31/2004 A3 or A7<br />
Note: this entire segment, including<br />
this element is not expected in the<br />
837 for a provider to payer<br />
exchange. Repricers only. If<br />
received by destination payer,<br />
rejection may occur. (A3)<br />
6<strong>29</strong> Property Casualty Claim Number Start: <strong>10</strong>/31/2004<br />
A3 or A6 or<br />
A7 or A8<br />
630 Referring CLIA Number Start: <strong>10</strong>/31/2004 A6<br />
631 Reimbursement Rate Start: <strong>10</strong>/31/2004 A7<br />
0050<strong>10</strong>X222A1 20<strong>10</strong>BA, 20<strong>10</strong>CA<br />
REF01 = Y4<br />
0050<strong>10</strong>X223A1 20<strong>10</strong>BA, 20<strong>10</strong>CA<br />
REF01 = Y4<br />
0050<strong>10</strong>X224A1 20<strong>10</strong>BA, 20<strong>10</strong>CA<br />
REF01 = Y4<br />
Crosschecks against CLM11,<br />
SBR09, PER Property and<br />
Casualty Patient Contact<br />
Information, PER Property and<br />
Casualty Subscriber Contact<br />
Information, Occurrance codes,<br />
Condition codes, etc.<br />
0050<strong>10</strong>X222A1 2400 REF01 = F4<br />
Crosscheck against REF01 if<br />
REF02 is blank considered A6<br />
0050<strong>10</strong>X222A1 2320 MOA01<br />
0050<strong>10</strong>X223A1 2320 MOA01<br />
0050<strong>10</strong>X224A1 2320 MOA01<br />
Sit rule - required when returned in<br />
the remittance advice<br />
632 Reject Reason Code Start: <strong>10</strong>/31/2004 A3 or A6 or A7<br />
0050<strong>10</strong>X222A1 2300, 2400 HCP13<br />
0050<strong>10</strong>X223A1 2300, 2400 HCP13<br />
0050<strong>10</strong>X224A1 2300, 2400 HCP13<br />
Syntax crosscheck - HCP01 or<br />
HCP13 must be present (A6)<br />
Note: this entire segment, including<br />
this element is not expected in the<br />
837 for a provider to payer<br />
exchange. Repricers only. If<br />
received by destination payer,<br />
rejection may occur. (A3)<br />
Page 50 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
633 Related Causes Code Start: <strong>10</strong>/31/2004 A3 or A7 or A8<br />
0050<strong>10</strong>X222A1 2300 CLM11<br />
0050<strong>10</strong>X224A1 2300 CLM11<br />
Crosscheck with Date Accident - if<br />
present CLM11 required<br />
0050<strong>10</strong>X223A1 2300 CLM11 Not<br />
used<br />
50<strong>10</strong> standard allows CLM11<br />
If element is sent, 277CA with error<br />
code 684 and A3 may be returned.<br />
634 Remark Code Start: <strong>10</strong>/31/2004 A7<br />
0050<strong>10</strong>X222A1 2300 MOA03-<strong>07</strong><br />
0050<strong>10</strong>X223A1 2300 MOA03-<strong>07</strong><br />
MIA05<br />
MIA20-23<br />
0050<strong>10</strong>X224A1 2300 MOA03-<strong>07</strong><br />
Invalid remittance advice remark<br />
code.<br />
0050<strong>10</strong>X222A1 2300, 2400 HCP06<br />
0050<strong>10</strong>X223A1 2300, 2400 HCP06<br />
0050<strong>10</strong>X224A1 2300, 2400 HCP06<br />
635<br />
Repriced Ambulatory Patient Group. This change effective 11/1/20<strong>10</strong>: Repriced<br />
Ambulatory Patient Group Code Start: <strong>10</strong>/31/2004<br />
A3<br />
Note: this entire segment, including<br />
this element is not expected in the<br />
837 for a provider to payer<br />
exchange. Repricers only. If<br />
received by destination payer,<br />
rejection may occur. (A3)<br />
0050<strong>10</strong>X222A1 2400 REF-1 = 9B<br />
0050<strong>10</strong>X223A1 2400 REF-1 = 9B<br />
636 Repriced Line Item Reference Number Start: <strong>10</strong>/31/2004 A3 or A6<br />
Note: this entire segment, including<br />
this element is not expected in the<br />
837 for a provider to payer<br />
exchange. Repricers only. If<br />
received by destination payer,<br />
rejection may occur. (A3)<br />
0050<strong>10</strong>X224A1 2400 REF-1 = 9B<br />
Not Used<br />
50<strong>10</strong> standard allows 2400 REF<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
Page 51 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
0050<strong>10</strong>X222A1 2300, 2400 HCP02<br />
0050<strong>10</strong>X223A1 2300, 2400 HCP02<br />
0050<strong>10</strong>X224A1 2300, 2400 HCP02<br />
637 Repriced Saving Amount Start: <strong>10</strong>/31/2004 A3 or A7<br />
Note: this entire segment, including<br />
this element is not expected in the<br />
837 for a provider to payer<br />
exchange. Repricers only. If<br />
received by destination payer,<br />
rejection may occur. (A3)<br />
0050<strong>10</strong>X222A1 2300, 2400 HCP05<br />
0050<strong>10</strong>X223A1 2300, 2400 HCP05<br />
0050<strong>10</strong>X224A1 2300, 2400 HCP05<br />
638 Repricing Per Diem or Flat Rate Amount Start: <strong>10</strong>/31/2004 A3 or A7<br />
Note: this entire segment, including<br />
this element is not expected in the<br />
837 for a provider to payer<br />
exchange. Repricers only. If<br />
received by destination payer,<br />
rejection may occur. (A3)<br />
Assume this represents the Patient<br />
Responsibility Amount Prof/Dental<br />
and Patient Estimated Amount Due<br />
Inst<br />
639 Responsibility Amount Start: <strong>10</strong>/31/2004 A3 or A6 or A7<br />
0050<strong>10</strong>X223A1 2300 AMT01 = F3<br />
Patient Estimated Amount Due<br />
0050<strong>10</strong>X224A1 2300 AMT01 =<br />
EAF<br />
Remaining Patient Liability<br />
0040<strong>10</strong>X098A1 2320 AMT01 = F2<br />
Entire Patient Responsibility AMT<br />
segment removed in<br />
0050<strong>10</strong>X222A1<br />
50<strong>10</strong> standard allows 2320 AMT<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
Page 52 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
640 Sales Tax Amount Start: <strong>10</strong>/31/2004 A6 or A7<br />
0050<strong>10</strong>X222A1 2400 AMT01 = T<br />
or 2400 SV<strong>10</strong>2 when SV<strong>10</strong>1-2 =<br />
S9999<br />
0050<strong>10</strong>X224A1 2400 AMT01 = T<br />
Note: ADA procedure codes do not<br />
have a specific value for Sales Tax<br />
amount.<br />
0050<strong>10</strong>X223A1 does not contain<br />
an AMT where AMT01 = T. There<br />
is no specific value to represent<br />
Sales Tax. 2400 SV203 when<br />
SV202-2 = S9999<br />
641<br />
Service Adjudication or Payment Date. Note: Use code 516. Start:<br />
<strong>10</strong>/31/2004 | Last Modified: 09/20/2009 | Stop: <strong>10</strong>/01/20<strong>10</strong><br />
N/A<br />
(see code 516<br />
rules)<br />
0050<strong>10</strong>X222A1 2330B, 2430<br />
DTP01 = 573<br />
0050<strong>10</strong>X223A1 2330B, 2430<br />
DTP01 = 573<br />
0050<strong>10</strong>X224A1 2330B, 2430<br />
DTP01 = 573<br />
642 Service Authorization Exception Code Start: <strong>10</strong>/31/2004 A6 or A7<br />
0050<strong>10</strong>X222A1 2300 REF01 = 4N<br />
0050<strong>10</strong>X223A1 2300 REF01 = 4N<br />
0050<strong>10</strong>X224A1 2300 REF01 = 4N<br />
Sit rule for segment - Required<br />
when mandated by government law<br />
or regulation<br />
643 Service Line Paid Amount Start: <strong>10</strong>/31/2004 A6 or A7 or A8<br />
0050<strong>10</strong>X222A1 2400 SVD02<br />
0050<strong>10</strong>X223A1 2400 SVD02<br />
0050<strong>10</strong>X224A1 2400 SVD02<br />
Sit rule for segment - Required<br />
when claim has been previously<br />
adjudicated by payer in loop 2330B<br />
Crosscheck against other payer<br />
2330B Other Payer Name<br />
644 Service Line Rate Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
0040<strong>10</strong>X098A1 2400 SV206<br />
0050<strong>10</strong>X223A1 2400 SV206 not<br />
used<br />
645 Service Tax Amount Start: <strong>10</strong>/31/2004 A7<br />
0050<strong>10</strong>X223A1 2400 AMT01 = GT<br />
(Note: X12 N TG2 WG2 could not<br />
define what tax amount would be<br />
carried in this data element)<br />
Page 53 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
646 Ship, Delivery or Calendar Pattern Code Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
0040<strong>10</strong>X098A1 2305, 2400 HSD<strong>07</strong><br />
- Entire HSD qualifier VS segment<br />
removed in 0050<strong>10</strong>X222A1<br />
0040<strong>10</strong>X096A1 2305 HSD<strong>07</strong> -<br />
Entire HSD qualifier VS segment<br />
removed in 0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows HSD<strong>07</strong><br />
If element is sent, 277CA with error<br />
code 684 and A3 may be returned.<br />
647 Shipped Date Start: <strong>10</strong>/31/2004 A7<br />
0050<strong>10</strong>X222A1 2400 DTP01 = 011<br />
date value in DTP03<br />
648 Similar Illness or Symptom Date Start: <strong>10</strong>/31/2004<br />
649 Skilled Nursing Facility Indicator Start: <strong>10</strong>/31/2004<br />
A3 or A7?<br />
999 will report<br />
A3 or A7?<br />
999 will report<br />
0040<strong>10</strong>X098A1 2300 DTP - Entire<br />
DTP qualifier 438 segment<br />
removed in 0050<strong>10</strong>X222A1<br />
50<strong>10</strong> standard allows DTP<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0040<strong>10</strong>X096A1 2300 CR606<br />
Entire CR6 segment removed in<br />
0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows CR6<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0050<strong>10</strong>X222A1 2300 CLM12<br />
0050<strong>10</strong>X224A1 2300 CLM12<br />
650 Special Program Indicator Start: <strong>10</strong>/31/2004 A3 or A7<br />
0050<strong>10</strong>X223A1 2300 CLM12 not<br />
used<br />
50<strong>10</strong> standard allows CLM12<br />
If element is sent, 277CA with error<br />
code 684 and A3 may be returned.<br />
Page 54 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
0040<strong>10</strong>X098A1 Multiple REF<br />
segments - Qualifier X5 no longer<br />
included in any REF segment in<br />
0050<strong>10</strong>X222A1<br />
0040<strong>10</strong>X096A1 Multiple REF<br />
segments - Qualifier X5 no longer<br />
included in any REF segment in<br />
0050<strong>10</strong>X223A1<br />
651 State Industrial Accident Provider Number Start: <strong>10</strong>/31/2004 A3<br />
652 Terms Discount Percentage Start: <strong>10</strong>/31/2004 A3 or A7<br />
0040<strong>10</strong>X097A1 Multiple REF<br />
segments - Qualifier X5 no longer<br />
included in any REF segment in<br />
0050<strong>10</strong>X224A1<br />
50<strong>10</strong> standard allows REF01<br />
qualifier of X5<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0050<strong>10</strong>X222A1 2300, 2400 CN<strong>10</strong>5<br />
0050<strong>10</strong>X223A1 2300 CN<strong>10</strong>5<br />
0050<strong>10</strong>X224A1 2300, 2400 CN<strong>10</strong>5<br />
CN1 segment is deemed non<br />
HIPAA use and for post<br />
adjudicated claims only<br />
653 Test Performed Date Start: <strong>10</strong>/31/2004 A3 or A6 or A7<br />
0050<strong>10</strong>X222A1 2400 DTP01 =<br />
738, 739<br />
50<strong>10</strong> standard allows DTP<br />
If segment is sent with qualifiers<br />
not allowed by guide, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0040<strong>10</strong>X096A1 AMT01 = YT -<br />
Segment AMT - Qualifier YT no<br />
longer included in any REF<br />
segment in 0050<strong>10</strong>X223A1<br />
654 Total Denied Charge Amount Start: <strong>10</strong>/31/2004 A3<br />
50<strong>10</strong> standard allows AMT qual YT<br />
If segment is sent with qualifiers<br />
not allowed by guide, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
Page 55 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
0040<strong>10</strong>X096A1 AMT01 = N1 -<br />
Segment AMT - Qualifier N1 no<br />
longer included in any REF<br />
segment in 0050<strong>10</strong>X223A1<br />
655 Total Medicare Paid Amount Start: <strong>10</strong>/31/2004 A3<br />
50<strong>10</strong> standard allows AMT qual N1<br />
If segment is sent with qualifiers<br />
not allowed by guide, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0040<strong>10</strong>X098A1 CR703 -<br />
Segment CR7 no longer included<br />
in 0050<strong>10</strong>X222A1<br />
656 Total Visits Projected This Certification Count Start: <strong>10</strong>/31/2004 A3<br />
0040<strong>10</strong>X096A1 CR703 -<br />
Segment CR7 no longer included<br />
in 0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows CR7<br />
segment<br />
If segment is sent and not allowed<br />
by guide, 277CA with error code<br />
684 and A3 may be returned.<br />
0040<strong>10</strong>X098A1 CR702 -<br />
Segment CR7 no longer included<br />
in 0050<strong>10</strong>X222A1<br />
657 Total Visits Rendered Count Start: <strong>10</strong>/31/2004 A3<br />
658 Treatment Code Start: <strong>10</strong>/31/2004 A7<br />
659 Unit or Basis for Measurement Code Start: <strong>10</strong>/31/2004<br />
A3 or A6 or<br />
A7 or A8<br />
50<strong>10</strong> standard allows CR7<br />
segment<br />
If segment is sent and not allowed<br />
by guide, 277CA with error code<br />
684 and A3 may be returned.<br />
0040<strong>10</strong>X096A1 2300 HI##-01 = TC<br />
-<br />
Value in HI##-02<br />
Invalid treatment code.<br />
Code source 359<br />
Various segments may contain<br />
D.E. Number 355<br />
Some segments required<br />
Some segment sit required<br />
Some segments not used<br />
Page 56 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
0040<strong>10</strong>X098A1 2400 REF01 = OZ,<br />
VP -<br />
Segment REF with qualifier OZ, VP<br />
no longer included in<br />
0050<strong>10</strong>X222A1<br />
660 Universal Product Number Start: <strong>10</strong>/31/2004 A3<br />
50<strong>10</strong> standard allows REF01<br />
qualifier value of OZ or VP<br />
If segment is sent and not allowed<br />
by guide, 277CA with error code<br />
684 and A3 may be returned.<br />
0040<strong>10</strong>X096A1 CR702 -<br />
Segment CR7 no longer included<br />
in 0050<strong>10</strong>X223A1<br />
661 Visits Prior to Recertification Date Count CR702 Start: <strong>10</strong>/31/2004 A3<br />
50<strong>10</strong> standard allows CR7<br />
segment<br />
If segment is sent and not allowed<br />
by guide, 277CA with error code<br />
684 and A3 may be returned.<br />
0040<strong>10</strong>X098A1 2400 CR212 -<br />
Element CR212 Spinal<br />
Manipulation not used in<br />
0050<strong>10</strong>X222A1<br />
662 X-ray Availability Indicator Start: <strong>10</strong>/31/2004 A3<br />
50<strong>10</strong> standard allows CR212<br />
element<br />
If element is sent and not allowed<br />
by guide, 277CA with error code<br />
684 and A3 may be returned.<br />
663<br />
Entity's Group Name. This change effective 11/1/20<strong>10</strong>: Entity's Group Name. Note:<br />
This code requires use of an Entity Code. Start: <strong>10</strong>/31/2004 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
N/A<br />
0050<strong>10</strong>X222A1 2000B, 2320<br />
SBR04<br />
0050<strong>10</strong>X223A1 2000B, 2320<br />
SBR04<br />
0050<strong>10</strong>X224A1 2000B, 2320<br />
SBR04<br />
Sit rule for segment - Required<br />
when SBR03 is not used and the<br />
group name is available. (External<br />
condition)<br />
664 Orthodontic Banding Date Start: <strong>10</strong>/31/2004 A6 or A7<br />
0050<strong>10</strong>X224A1 2300, 2400 DTP01<br />
= 452<br />
Page 57 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
0040<strong>10</strong>X096A1 2300 CR609<br />
Entire CR6 segment removed in<br />
0050<strong>10</strong>X223A1<br />
656 Surgery Date Start: <strong>10</strong>/31/2004 A3<br />
666 Surgical Procedure Code Start: <strong>10</strong>/31/2004 A3<br />
667<br />
668<br />
Real-Time requests not supported by the information holder, do not resubmit<br />
Start: 02/28/2005<br />
Missing Endodontics treatment history and prognosis Start:<br />
06/30/2005<br />
669 Dental service narrative needed. Start: <strong>10</strong>/31/2005 N/A<br />
670<br />
Funds applied from a consumer spending account such as consumer<br />
directed/driven health plan (CDHP), Health savings account (H S A) and or other<br />
similar accounts Start: 06/30/2006 | Last Modified: 02/28/20<strong>07</strong><br />
A3<br />
N/A<br />
N/A<br />
50<strong>10</strong> standard allows CR6<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
0040<strong>10</strong>X096A1 2300 CR611<br />
Entire CR6 segment removed in<br />
0050<strong>10</strong>X223A1<br />
50<strong>10</strong> standard allows CR6<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
Coordinate with error code 494<br />
Possible PWK not present - Not<br />
related to data within 837<br />
transaction<br />
0050<strong>10</strong>X224A1 2300 NTE -<br />
missing<br />
Possible PWK not present<br />
671<br />
Funds may be available from a consumer spending account such as consumer<br />
directed/driven health plan (CDHP), Health savings account (H S A) and or other<br />
similar accounts. Start: 06/30/2006 | Last Modified:<br />
02/28/20<strong>07</strong><br />
N/A<br />
0050<strong>10</strong>X222A1 2320, 2430<br />
CAS03,06,09,12,15,18<br />
SVD02<br />
AMT02<br />
672<br />
Other Payer's payment information is out of balance. Start:<br />
<strong>10</strong>/31/2006<br />
A8<br />
0050<strong>10</strong>X223A1 2320, 2430<br />
CAS03,06,09,12,15,18<br />
SVD02<br />
AMT02<br />
0050<strong>10</strong>X224A1 2320, 2430<br />
CAS03,06,09,12,15,18<br />
SVD02<br />
AMT02<br />
Crosscheck amounts<br />
Page 58 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
673 Patient Reason for Visit Start: <strong>10</strong>/31/2006 A6 or A7 or A8<br />
674 Authorization exceeded Start: <strong>10</strong>/31/2006 N/A<br />
0050<strong>10</strong>X223A1 2300 HI01-01 =<br />
PR, APR<br />
Sit rule - Required when claim<br />
involves outpatient visits.<br />
Crosscheck CLM05-01 Facility<br />
Type<br />
0050<strong>10</strong>X222A1 2300 DTP01 = 435<br />
DTP01 = 096<br />
0050<strong>10</strong>X222A1 2300 DTP01 = 434<br />
or HI##-01 = BH and HI##-02<br />
Occurrence code 42 (discharge)<br />
675 Facility admission through discharge dates. Start: <strong>10</strong>/31/2006<br />
A3 or A6 or<br />
A7 or A8<br />
0040<strong>10</strong>X096A1 2300 DTP01 = 435<br />
DTP01 = 096 -<br />
Segments with DTP01 values 435<br />
and 096 have been removed from<br />
0050<strong>10</strong>X222A1<br />
676<br />
677<br />
Entity possibly compensated by facility. This change effective 11/1/20<strong>10</strong>: Entity<br />
possibly compensated by facility. Note: This code requires use of an Entity Code.<br />
Start: <strong>10</strong>/31/2006 | Last Modified: 02/11/20<strong>10</strong><br />
Entity not affiliated. This change effective 11/1/20<strong>10</strong>: Entity not affiliated. Note: This<br />
code requires use of an Entity Code. Start: <strong>10</strong>/31/2006 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
678 Revenue code and patient gender mismatch. Start: <strong>10</strong>/31/2006 A8<br />
N/A<br />
A3<br />
50<strong>10</strong> standard allows DTP01 435<br />
and 096<br />
If qualifier is sent and not allowed<br />
by guide, 277CA with error code<br />
684 and A3 may be returned.<br />
Not related to data contained in<br />
837 requires use of<br />
entity code -- add<br />
later<br />
Blues use this to indicate that the<br />
claim must be submitted to the<br />
local Blue Plan<br />
0050<strong>10</strong>X223A1 20<strong>10</strong>BA, 20<strong>10</strong>CA<br />
DMG03<br />
2400 SV201<br />
Crosscheck SV201 against DMG03<br />
679 Submit newborn services on mother's claim Start: <strong>10</strong>/31/2006 A3<br />
680<br />
Entity's Country. This change effective 11/1/20<strong>10</strong>: Entity's Country. Note: This code<br />
requires use of an Entity Code. Start: <strong>10</strong>/31/2006 | Last<br />
Modified: 02/11/20<strong>10</strong><br />
681 Claim currency not supported Start: <strong>10</strong>/31/2006 A7<br />
682 Cosmetic procedure Start: 02/28/20<strong>07</strong> A3<br />
683 Awaiting Associated Hospital Claims Start: 02/28/20<strong>07</strong> P1 or P5<br />
A7<br />
Possible CL<strong>10</strong>1, Value code 54,<br />
Revenue Code 017 1-4, DMG02<br />
0050<strong>10</strong>X222A1 N404<br />
0050<strong>10</strong>X223A1 N404<br />
0050<strong>10</strong>X224A1 N404<br />
Validate against Codesource 5<br />
0050<strong>10</strong>X222A1 2000A CUR02<br />
0050<strong>10</strong>X223A1 2000A CUR02<br />
0050<strong>10</strong>X224A1 2000A CUR02<br />
0050<strong>10</strong>X222A1 2400 SV<strong>10</strong>1-02<br />
0050<strong>10</strong>X223A1 2400 SV202-02<br />
0050<strong>10</strong>X224A1 2400 SV301-02<br />
requires use of<br />
entity code -- add<br />
later<br />
Page 59 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
684<br />
685<br />
Rejected. Syntax error noted for this claim/service/inquiry. See Functional or<br />
Implementation Acknowledgement for details. (Note: Only for use to reject claims or<br />
status requests in transactions that were 'accepted with errors' on a 997 or 999<br />
Acknowledgement.) Start: 11/05/20<strong>07</strong><br />
Claim could not complete adjudication in real time. Claim will continue processing<br />
in a batch mode. Do not resubmit. Start: 01/27/2008<br />
N/A or A3<br />
A3<br />
Only use 684 when transaction has<br />
been accepted with syntax errors.<br />
The syntax errors will be reported<br />
in 277CA instead of using the 999.<br />
Optionally, the 999 could be used<br />
to report the syntax errors and no<br />
277CA would be returned, thus<br />
N/A.<br />
Coordinate with error code 494<br />
ISA transaction id is assumed to<br />
indicate batch or real time<br />
submission.<br />
686<br />
The claim/ encounter has completed the adjudication cycle and the entire claim has<br />
been voided. Start: 01/27/2008<br />
F0<br />
Not related to data contained in<br />
837<br />
687<br />
688<br />
Claim estimation can not be completed in real time. Do not resubmit. Start:<br />
01/27/2008<br />
Present on Admission Indicator for reported diagnosis code(s). Start:<br />
01/27/2008<br />
A3<br />
A6 or A7<br />
Coordinate with error code 494<br />
0050<strong>10</strong>X223A1 2300 HI##-09<br />
Sit rule - Required as directed by<br />
the NUBC manual<br />
689<br />
690<br />
691<br />
692<br />
Entity was unable to respond within the expected time frame. This change effective<br />
11/1/20<strong>10</strong>: Entity was unable to respond within the expected time frame. Note: This<br />
code requires use of an Entity Code. Start: 06/01/2008 | Last Modified: 02/11/20<strong>10</strong><br />
Multiple claims or estimate requests cannot be processed in real time. Start:<br />
06/01/2008<br />
Multiple claim status requests cannot be processed in real time. Start:<br />
06/01/2008<br />
Contracted funding agreement-Subscriber is employed by the provider of services.<br />
Start: 09/21/2008<br />
A3<br />
A3<br />
N/A<br />
??<br />
Not related to data contained in<br />
837 requires use of<br />
entity code -- add<br />
later<br />
Coordinate with error code 494<br />
Used for 276/277 Claim Status<br />
Request<br />
Crosscheck Subscriber data with<br />
contract data - external to 837<br />
693<br />
Amount must be greater than or equal to zero. Note: At least one other status code<br />
is required to identify which amount element is in error. Start: 01/25/2009<br />
A8<br />
Patient paid amount must be<br />
positive value and can not exceed<br />
total claim charge amount.<br />
694<br />
695<br />
Amount must not be equal to zero. Note: At least one other status code is required<br />
to identify which amount element is in error. Start: 01/25/2009<br />
Entity's Country Subdivision Code. This change effective 11/1/20<strong>10</strong>: Entity's<br />
Country Subdivision Code. Note: This code requires use of an Entity Code.<br />
Start: 01/25/2009 | Last Modified: 02/11/20<strong>10</strong><br />
A7<br />
A7<br />
Any amount included in 837 that is<br />
deemed by payer to be<br />
inappropriate as zero (defined by<br />
guide notes or business practice<br />
per payer)<br />
0050<strong>10</strong>X222A1 N4<strong>07</strong><br />
0050<strong>10</strong>X223A1 N4<strong>07</strong><br />
0050<strong>10</strong>X224A1 N4<strong>07</strong><br />
Validate against Part 2 of ISO 3166<br />
696 Claim Adjustment Group Code. Start: 01/25/2009 A6 or A7<br />
0050<strong>10</strong>X222A1 2320, 2430 CAS01<br />
0050<strong>10</strong>X223A1 2320, 2430 CAS01<br />
0050<strong>10</strong>X224A1 2320, 2430 CAS01<br />
Page 60 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
697<br />
Invalid Decimal Precision. Note: At least one other status code is required to<br />
identify the data element in error. Start: <strong>07</strong>/01/2009<br />
A7<br />
Relates to any integer defined data<br />
element (example: monetary<br />
amounts)<br />
0050<strong>10</strong>X222A1 2440 LQ02<br />
(assumed location)<br />
698 Form Type Identification Start: <strong>07</strong>/01/2009 A6 or A7<br />
0050<strong>10</strong>X223A1 2440 LQ02 not<br />
included<br />
0050<strong>10</strong>X224A1 2440 LQ02 not<br />
included<br />
50<strong>10</strong> standard allows LQ02<br />
If segment is sent, 277CA with<br />
error code 684 and A3 may be<br />
returned.<br />
699<br />
Question/Response from Supporting Documentation Form. Start:<br />
<strong>07</strong>/01/2009<br />
A6 or A7<br />
0050<strong>10</strong>X222A1 2440 FRM03,04,05<br />
FRM02 = Freeform text format (A6)<br />
FRM03 = Date format (A6 or A7)<br />
FRM04 = Percent decimal format<br />
(A6 or A7)<br />
700<br />
ICD<strong>10</strong>. Note: At least one other status code is required to identify the related<br />
procedure code or diagnosis code. Start: <strong>07</strong>/01/2009<br />
OSTROOT 701 - 742<br />
A6, A7 or A8<br />
HI<br />
Same as 508 only this code for<br />
ICD<strong>10</strong><br />
701 Initial Treatment Date Start: <strong>07</strong>/01/2009 A6, A7 or A8 DTP<br />
702 Repriced Claim Reference Number. Start: 11/01/2009 A6, A7 or A8 REF<br />
703 Advanced Billing Concepts (ABC) code. Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
704 Claim Note Text Start: 01/24/20<strong>10</strong> A7<br />
SV<strong>10</strong>1-1 (qualifier WK) and SV<strong>10</strong>1-<br />
2<br />
NTE - invalid characters, payer can<br />
not require NTE submission.<br />
705 Repriced Allowed Amount. Start: 01/24/20<strong>10</strong> A6, A7 or A8 HCP02<br />
706 Repriced Approved Amount. Start: 01/24/20<strong>10</strong> A6, A7 or A8 HCP04<br />
7<strong>07</strong><br />
Repriced Approved Ambulatory Patient Group Amount. Start:<br />
01/24/20<strong>10</strong><br />
A6, A7 or A8 HCP<strong>07</strong><br />
708 Repriced Approved Revenue Code. Start: 01/24/20<strong>10</strong> A6, A7 or A8 HCP08<br />
709 Repriced Approved Service Unit Count. Start: 01/24/20<strong>10</strong> A6, A7 or A8 HCP12<br />
7<strong>10</strong><br />
Line Adjudication Information. Note: At least one other status code is required to<br />
identify the data element in error. Start: 01/24/20<strong>10</strong><br />
A6, A7 or A8 SVD<br />
711 Stretcher purpose Start: 01/24/20<strong>10</strong> A6, A7 or A8 CR1<strong>10</strong><br />
Page 61 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
712 Obstetric Additional Units Start: 01/24/20<strong>10</strong> A6, A7 or A8 QTY02<br />
713 Patient Condition Description Start: 01/24/20<strong>10</strong> A6, A7 or A8 CR2<strong>10</strong> and CR211<br />
714 Care Plan Oversight Number Start: 01/24/20<strong>10</strong> A6, A7 or A8 REF<br />
715 Acute Manifestation Date Start: 01/24/20<strong>10</strong> A6, A7 or A8 DTP<br />
716 Repriced Approved DRG Code Start: 01/24/20<strong>10</strong> A6, A7 or A8 HCP06<br />
717 This claim has been split for processing. Start: 01/24/20<strong>10</strong> A5<br />
718<br />
Claim/service not submitted within the required timeframe (timely filing).<br />
Start: 01/24/20<strong>10</strong><br />
719 NUBC Occurrence Code(s) Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
A3<br />
HI-OCCURRENCE INFORMATION<br />
461 DEACTIVATED<br />
720 NUBC Occurrence Code Date(s) Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
721 NUBC Occurrence Span Code(s) Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
722 NUBC Occurrence Span Code Date(s) Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
723 Drug days supply Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
724 Drug dosage Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
725 NUBC Value Code(s) Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
726 NUBC Value Code Amount(s) Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
727 Accident date Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
728 Accident state Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
7<strong>29</strong> Accident description Start: 01/24/20<strong>10</strong> NA<br />
730 Accident cause Start: 01/24/20<strong>10</strong> A6, A7 or A8<br />
HI-OCCURRENCE INFORMATION<br />
461 DEACTIVATED<br />
HI-OCCURRENCE SPAN<br />
INFORMATION<br />
462 DEACTIVATED<br />
HI-OCCURRENCE SPAN<br />
INFORMATION<br />
462 DEACTIVATED<br />
NCPDP<br />
221 DEACTIVATED<br />
NCPDP<br />
221 DEACTIVATED<br />
HI-VALUE INFORMATION<br />
463 DEACTIVATED<br />
HI-VALUE INFORMATION<br />
463 DEACTIVATED<br />
DTP<br />
248 DEACTIVATED<br />
REF<br />
248 DEACTIVATED<br />
CLM11<br />
248 DEACTIVATED<br />
731 Measurement value/test result Start: 01/24/20<strong>10</strong> A6, A7 or A8 MEA03<br />
732<br />
Information submitted inconsistent with billing guidelines. Note: At least one other<br />
status code is required to identify the inconsistent information.<br />
Start: 01/24/20<strong>10</strong><br />
A3,A6, A7 or A8<br />
dependant upon second status<br />
733 Prefix for entity's contract/member number. Start: 01/24/20<strong>10</strong> A6 or A7 NM<strong>10</strong>8 subscriber loop<br />
734 Verifying premium payment NA adjudication related<br />
735 This service/claim is included in the allowance for another service or claim NA adjudication related<br />
736 A related or qualifying service/claim has not been received/adjudicated NA adjudication related<br />
737 Current Dental Terminology (CDT) code A6 or A7 SV301<br />
738<br />
Institutional-SV2 or SVD<br />
Home Infusion EDI Coalition (HIEC) Product/Service Code<br />
A6 or A7 professional-SV1 or SVD<br />
HK<br />
Page 62 of 63
Preliminary Discussion Draft–For <strong>Acknowledgements</strong> <strong>TAG</strong> Review 7-<strong>29</strong>-<strong>10</strong><br />
739<br />
740<br />
741<br />
742<br />
Jurisdiction Specific Procedure and Supply Code<br />
drop off location<br />
entity must be a person<br />
payer responsibility sequence number code<br />
A6 or A7<br />
A6 or A7 or A8<br />
A3<br />
A6 or A7 or A8<br />
Institutional-SV2 or SVD<br />
professional-SV1 or SVD<br />
NM1-AMBULANCE DROP OFF<br />
LOCATION<br />
Loop 20<strong>10</strong>BA NM<strong>10</strong>2 to qualify<br />
subscribers as people<br />
pertains to elements SBR01 and<br />
SBR02<br />
Page 63 of 63