Tool and Resource Evaluation Template - Department of Health
Tool and Resource Evaluation Template - Department of Health
Tool and Resource Evaluation Template - Department of Health
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
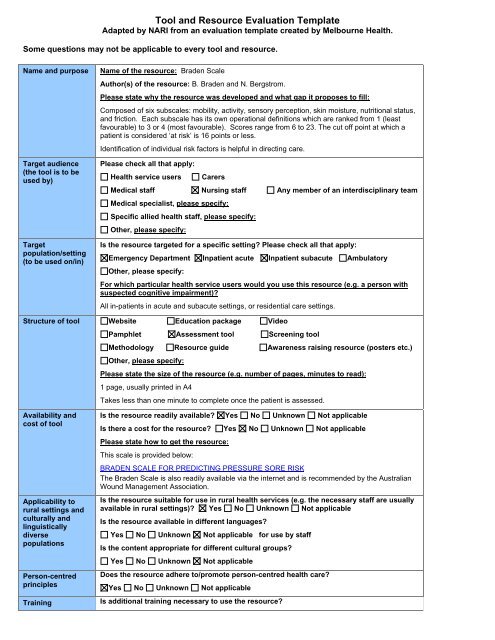
<strong>Tool</strong> <strong>and</strong> <strong>Resource</strong> <strong>Evaluation</strong> <strong>Template</strong><br />
Adapted by NARI from an evaluation template created by Melbourne <strong>Health</strong>.<br />
Some questions may not be applicable to every tool <strong>and</strong> resource.<br />
Name <strong>and</strong> purpose<br />
Target audience<br />
(the tool is to be<br />
used by)<br />
Target<br />
population/setting<br />
(to be used on/in)<br />
Name <strong>of</strong> the resource: Braden Scale<br />
Author(s) <strong>of</strong> the resource: B. Braden <strong>and</strong> N. Bergstrom.<br />
Please state why the resource was developed <strong>and</strong> what gap it proposes to fill:<br />
Composed <strong>of</strong> six subscales: mobility, activity, sensory perception, skin moisture, nutritional status,<br />
<strong>and</strong> friction. Each subscale has its own operational definitions which are ranked from 1 (least<br />
favourable) to 3 or 4 (most favourable). Scores range from 6 to 23. The cut <strong>of</strong>f point at which a<br />
patient is considered ‘at risk’ is 16 points or less.<br />
Identification <strong>of</strong> individual risk factors is helpful in directing care.<br />
Please check all that apply:<br />
<strong>Health</strong> service users<br />
Carers<br />
Medical staff Nursing staff Any member <strong>of</strong> an interdisciplinary team<br />
Medical specialist, please specify:<br />
Specific allied health staff, please specify:<br />
Other, please specify:<br />
Is the resource targeted for a specific setting? Please check all that apply:<br />
Emergency <strong>Department</strong> Inpatient acute Inpatient subacute Ambulatory<br />
Other, please specify:<br />
For which particular health service users would you use this resource (e.g. a person with<br />
suspected cognitive impairment)?<br />
All in-patients in acute <strong>and</strong> subacute settings, or residential care settings.<br />
Structure <strong>of</strong> tool Website Education package Video<br />
Pamphlet Assessment tool Screening tool<br />
Methodology <strong>Resource</strong> guide Awareness raising resource (posters etc.)<br />
Other, please specify:<br />
Please state the size <strong>of</strong> the resource (e.g. number <strong>of</strong> pages, minutes to read):<br />
1 page, usually printed in A4<br />
Takes less than one minute to complete once the patient is assessed.<br />
Availability <strong>and</strong><br />
cost <strong>of</strong> tool<br />
Applicability to<br />
rural settings <strong>and</strong><br />
culturally <strong>and</strong><br />
linguistically<br />
diverse<br />
populations<br />
Person-centred<br />
principles<br />
Training<br />
Is the resource readily available? Yes No Unknown Not applicable<br />
Is there a cost for the resource? Yes No Unknown Not applicable<br />
Please state how to get the resource:<br />
This scale is provided below:<br />
BRADEN SCALE FOR PREDICTING PRESSURE SORE RISK<br />
The Braden Scale is also readily available via the internet <strong>and</strong> is recommended by the Australian<br />
Wound Management Association.<br />
Is the resource suitable for use in rural health services (e.g. the necessary staff are usually<br />
available in rural settings)? Yes No Unknown Not applicable<br />
Is the resource available in different languages?<br />
Yes No Unknown Not applicable for use by staff<br />
Is the content appropriate for different cultural groups?<br />
Yes No Unknown Not applicable<br />
Does the resource adhere to/promote person-centred health care?<br />
Yes No Unknown Not applicable<br />
Is additional training necessary to use the resource?
equirements Yes No Unknown Not applicable<br />
Administration<br />
details<br />
If applicable, please state how extensive any training is, <strong>and</strong> what resources are required:<br />
How long does the resource take to use? 0-5 mins 5-15 mins 15-25mins 25mins +<br />
Can the resource be used as a st<strong>and</strong>alone, or must it be used in conjunction with other<br />
tools, resources, <strong>and</strong> procedures?<br />
St<strong>and</strong>alone<br />
Must be used with other resources, please specify:<br />
Can be used with other tools, please specify:<br />
Data collection <strong>and</strong><br />
analysis<br />
Are additional resources required to collect <strong>and</strong> analyse data from the resource?<br />
Yes No Unknown Not applicable<br />
If applicable, please state any special resources required (e.g. computer s<strong>of</strong>tware):<br />
Sensitivity <strong>and</strong><br />
specificity<br />
Sensitivity is the proportion <strong>of</strong> people that will be correctly identified by the tool.<br />
Specificity is the probability that an individual who does not have the condition being tested<br />
for will be correctly identified as negative.<br />
Has the sensitivity <strong>and</strong> specificity <strong>of</strong> the resource been reported?<br />
Yes No Unknown Not applicable<br />
If applicable, please state what has been reported:<br />
Initial studies reported 83 - 100% sensitivity <strong>and</strong> 64-90% specificity. In subsequent studies,<br />
sensitivity has ranged from 22 – 89% <strong>and</strong> specificity has ranged from 56 – 100% (Defloor &<br />
Grypdonck, 2004).<br />
Face Validity<br />
Reliability<br />
Does the resource appear to meet the intended purpose?<br />
Yes No Unknown Not applicable<br />
Reliability is the extent to which the tool’s measurements remain consistent over repeated<br />
tests <strong>of</strong> the same subject under identical conditions. Inter-rater reliability measures<br />
whether independent assessors will give similar scores under similar conditions.<br />
Has the reliability <strong>of</strong> the resource been reported?<br />
Yes No Unknown Not applicable<br />
If applicable, please state what has been reported:<br />
Percentage agreement <strong>of</strong> up to 88% was achieved <strong>and</strong> correlational measures <strong>of</strong> reliability were<br />
excellent when used by a registered nurse (r = 0.99). However, Raycr<strong>of</strong>t-Malone (2000) argues<br />
that the reliability has not been properly assessed. Bergstrom <strong>and</strong> Braden recommended that that<br />
registered nurses use the tool. Scores less reliable when the tool was used by less qualified staff.<br />
Strengths<br />
What are the strengths <strong>of</strong> the resource? Is the resource easy to underst<strong>and</strong> <strong>and</strong> use? Are<br />
instructions provided on how to use the resource? Is the resource visually well presented<br />
(images, colour, font type/ size)? Does the resource use older friendly terminology (where<br />
relevant), avoiding jargon?<br />
Please state any other known strengths, using dot points:<br />
• User friendly <strong>and</strong> quick.<br />
• Reliable when used by nursing staff.<br />
• In common usage in Australia <strong>and</strong> USA.<br />
• Validity compares well with Norton <strong>and</strong> Waterlow scales.<br />
Limitations<br />
What are the limitations <strong>of</strong> the tool/resource? Is the tool/resource difficult to underst<strong>and</strong><br />
<strong>and</strong> use? Are instructions provided on how to use the tool/resource? Is the tool/resource<br />
poorly presented (images, colour, font type/ size)? Does the tool/resource use difficult to<br />
underst<strong>and</strong> jargon?<br />
Please state any other known limitations, using dot points:<br />
• Reliability is reduced when not used by nursing staff.<br />
• Experienced nurses should conduct the risk assessment (Papanikolaou et al., 2007).<br />
• Critical cut-<strong>of</strong>f score is disputable (Papanikolaou et al., 2007).<br />
References <strong>and</strong><br />
further reading<br />
Supporting references <strong>and</strong> associated reading.<br />
1. Australian Wound Management Association Clinical Practice Guidelines for the prediction
<strong>and</strong> prevention <strong>of</strong> pressure ulcers. Available at:<br />
http://www.awma.com.au/publications/2007/cpgpppu_v_full.pdf<br />
2. <strong>Health</strong> Services Technology Assessment Test - National Library <strong>of</strong> Medicine.<br />
http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat2.chapter.4409<br />
3. Braden B & Bergstrom N. A conceptual scheme for the study <strong>of</strong> etiology <strong>of</strong> pressure<br />
sores. Rehabilitation Nursing. 1987;12:8-16.<br />
4. Defloor T & Grypdonck M. Validation <strong>of</strong> pressure ulcer risk assessment scales: a critique.<br />
Journal <strong>of</strong> Advanced Nursing. 2004;48:613-621.<br />
5. Papanikolaou P, Lyne P & Anthony D. Risk assessment scales for pressure ulcers: A<br />
methodological review. International Journal <strong>of</strong> Nursing Studies, 2007;44:285-296.<br />
6. Raycr<strong>of</strong>t-Malone J. Pressure ulcer risk assessment <strong>and</strong> prevention. Technical reporting.<br />
2000 RCN Publishing, London.
BRADEN SCALE FOR PREDICTING PRESSURE SORE RISK<br />
Patient=s Name _____________________________________ Evaluator=s Name________________________________ Date <strong>of</strong> Assessment<br />
SENSORY PERCEPTION<br />
ability to respond meaningfully<br />
to pressure-related<br />
discomfort<br />
1. Completely Limited<br />
Unresponsive (does not moan,<br />
flinch, or grasp) to painful<br />
stimuli, due to diminished level <strong>of</strong><br />
con-sciousness or sedation.<br />
OR<br />
limited ability to feel<br />
pain over most <strong>of</strong> body<br />
2. Very Limited<br />
Responds only to painful<br />
stimuli. Cannot communicate<br />
discomfort except by moaning<br />
or restlessness<br />
OR<br />
has a sensory impairment which<br />
limits the ability to feel pain or<br />
discomfort over 2 <strong>of</strong> body.<br />
3. Slightly Limited<br />
Responds to verbal comm<strong>and</strong>s,<br />
but cannot always<br />
communicate discomfort or the<br />
need to be turned.<br />
OR<br />
has some sensory impairment<br />
which limits ability to feel pain<br />
or discomfort in 1 or 2 extremities.<br />
4. No Impairment<br />
Responds to verbal<br />
comm<strong>and</strong>s. Has no<br />
sensory deficit which would<br />
limit ability to feel or voice<br />
pain or discomfort..<br />
MOISTURE<br />
degree to which skin is<br />
exposed to moisture<br />
1. Constantly Moist<br />
Skin is kept moist almost<br />
constantly by perspiration, urine,<br />
etc. Dampness is detected<br />
every time patient is moved or<br />
turned.<br />
2. Very Moist<br />
Skin is <strong>of</strong>ten, but not always moist.<br />
Linen must be changed at least<br />
once a shift.<br />
3. Occasionally Moist:<br />
Skin is occasionally moist, requiring<br />
an extra linen change approximately<br />
once a day.<br />
4. Rarely Moist<br />
Skin is usually dry, linen<br />
only requires changing at<br />
routine intervals.<br />
ACTIVITY<br />
degree <strong>of</strong> physical activity<br />
1. Bedfast<br />
Confined to bed.<br />
2. Chairfast<br />
Ability to walk severely limited or<br />
non-existent. Cannot bear own<br />
weight <strong>and</strong>/or must be assisted into<br />
chair or wheelchair.<br />
3. Walks Occasionally<br />
Walks occasionally during day, but<br />
for very short distances, with or<br />
without assistance. Spends<br />
majority <strong>of</strong> each shift in bed or chair<br />
4. Walks Frequently<br />
Walks outside room at least<br />
twice a day <strong>and</strong> inside room<br />
at least once every two<br />
hours during waking hours<br />
MOBILITY<br />
ability to change <strong>and</strong> control<br />
body position<br />
1. Completely Immobile<br />
Does not make even slight<br />
changes in body or extremity<br />
position without assistance<br />
2. Very Limited<br />
Makes occasional slight changes in<br />
body or extremity position but<br />
unable to make frequent or<br />
significant changes independently.<br />
3. Slightly Limited<br />
Makes frequent though slight<br />
changes in body or extremity<br />
position independently.<br />
4. No Limitation<br />
Makes major <strong>and</strong> frequent<br />
changes in position without<br />
assistance.<br />
NUTRITION<br />
usual food intake pattern<br />
1. Very Poor<br />
Never eats a complete meal.<br />
Rarely eats more than a <strong>of</strong> any<br />
food <strong>of</strong>fered. Eats 2 servings or<br />
less <strong>of</strong> protein (meat or dairy<br />
products) per day. Takes fluids<br />
poorly. Does not take a liquid<br />
dietary supplement<br />
OR<br />
is NPO <strong>and</strong>/or maintained on<br />
clear liquids or IV=s for more<br />
than 5 days.<br />
2. Probably Inadequate<br />
Rarely eats a complete meal <strong>and</strong><br />
generally eats only about 2 <strong>of</strong> any<br />
food <strong>of</strong>fered. Protein intake<br />
includes only 3 servings <strong>of</strong> meat or<br />
dairy products per day.<br />
Occasionally will take a dietary<br />
supplement.<br />
OR<br />
receives less than optimum amount<br />
<strong>of</strong> liquid diet or tube feeding<br />
3. Adequate<br />
Eats over half <strong>of</strong> most meals. Eats<br />
a total <strong>of</strong> 4 servings <strong>of</strong> protein<br />
(meat, dairy products per day.<br />
Occasionally will refuse a meal, but<br />
will usually take a supplement when<br />
<strong>of</strong>fered<br />
OR<br />
is on a tube feeding or TPN<br />
regimen which probably meets<br />
most <strong>of</strong> nutritional needs<br />
4. Excellent<br />
Eats most <strong>of</strong> every meal.<br />
Never refuses a meal.<br />
Usually eats a total <strong>of</strong> 4 or<br />
more servings <strong>of</strong> meat <strong>and</strong><br />
dairy products.<br />
Occasionally eats between<br />
meals. Does not require<br />
supplementation.<br />
FRICTION & SHEAR<br />
1. Problem<br />
Requires moderate to maximum<br />
assistance in moving. Complete<br />
lifting without sliding against<br />
sheets is impossible. Frequently<br />
slides down in bed or chair,<br />
requiring frequent repositioning<br />
with maximum assistance.<br />
Spasticity, contractures or<br />
agitation leads to almost<br />
constant friction<br />
2. Potential Problem<br />
Moves feebly or requires minimum<br />
assistance. During a move skin<br />
probably slides to some extent<br />
against sheets, chair, restraints or<br />
other devices. Maintains relatively<br />
good position in chair or bed most<br />
<strong>of</strong> the time but occasionally slides<br />
down.<br />
3. No Apparent Problem<br />
Moves in bed <strong>and</strong> in chair<br />
independently <strong>and</strong> has sufficient<br />
muscle strength to lift up<br />
completely during move. Maintains<br />
good position in bed or chair.<br />
8 Copyright Barbara Braden <strong>and</strong> Nancy Bergstrom, 1988 All rights reserved Total Score