Training Manual, part 4, sections 3 (126kb, pdf)
Training Manual, part 4, sections 3 (126kb, pdf)
Training Manual, part 4, sections 3 (126kb, pdf)
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
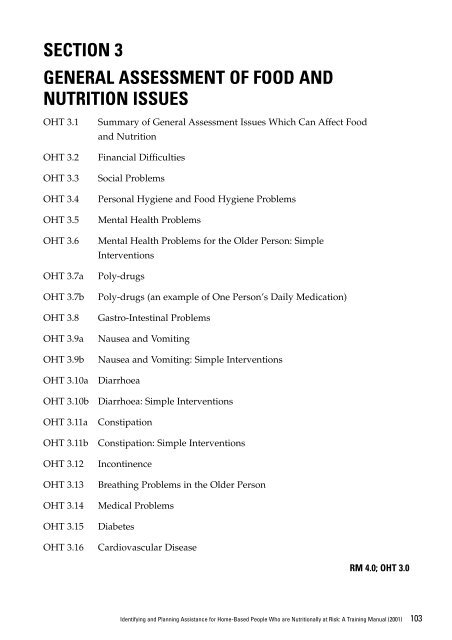
SECTION 3<br />
GENERAL ASSESSMENT OF FOOD AND<br />
NUTRITION ISSUES<br />
OHT 3.1<br />
OHT 3.2<br />
OHT 3.3<br />
OHT 3.4<br />
OHT 3.5<br />
OHT 3.6<br />
OHT 3.7a<br />
OHT 3.7b<br />
OHT 3.8<br />
OHT 3.9a<br />
OHT 3.9b<br />
OHT 3.10a<br />
OHT 3.10b<br />
OHT 3.11a<br />
OHT 3.11b<br />
OHT 3.12<br />
OHT 3.13<br />
OHT 3.14<br />
OHT 3.15<br />
OHT 3.16<br />
Summary of General Assessment Issues Which Can Affect Food<br />
and Nutrition<br />
Financial Difficulties<br />
Social Problems<br />
Personal Hygiene and Food Hygiene Problems<br />
Mental Health Problems<br />
Mental Health Problems for the Older Person: Simple<br />
Interventions<br />
Poly-drugs<br />
Poly-drugs (an example of One Person’s Daily Medication)<br />
Gastro-Intestinal Problems<br />
Nausea and Vomiting<br />
Nausea and Vomiting: Simple Interventions<br />
Diarrhoea<br />
Diarrhoea: Simple Interventions<br />
Constipation<br />
Constipation: Simple Interventions<br />
Incontinence<br />
Breathing Problems in the Older Person<br />
Medical Problems<br />
Diabetes<br />
Cardiovascular Disease<br />
RM 4.0; OHT 3.0<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
103
Summary of General Assessment Issues<br />
which can Affect Food and Nutrition<br />
Social Problems<br />
Financial Difficulties<br />
Household Management Problems<br />
Personal Hygiene and Food Hygiene Problems<br />
Mental Health Problems<br />
Poly-drugs<br />
(more than three types of medication daily)<br />
Gastro-intestinal problems<br />
• Nausea and vomiting<br />
• Diarrhoea<br />
• Constipation<br />
Incontinence<br />
Breathing problems<br />
Medical problems<br />
RM Section 4.1; OHT 3.1<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
105
Financial difficulties<br />
(I don’t always have enough money to buy food)<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
107<br />
• Possible restriction of the variety and amount of food bought<br />
• Possible restriction of nourishing foods which may be more expensive (for<br />
example meat, fresh fruit)<br />
• Vulnerable people may not spend enough on food, even when they have<br />
enough money<br />
• An adult person may not get enough nourishment, if this person spends less<br />
than $30 per week* on food for himself/herself every week<br />
* 1999 ($22 in 1995)<br />
This can result in poor nutrition, poor quality of life and poor health<br />
RM 4.2; OHT 3.2
Social problems<br />
(I eat alone most of the time)<br />
• Eating is usually a social activity<br />
• Reduced food intake is common in social isolation,<br />
bereavement and depression<br />
• The vulnerable person may be less motivated to<br />
eat and drink<br />
• Eating alone can lead to reduced interest in food<br />
and eating<br />
• Increased use of ready prepared snack foods<br />
rather than maintaining one’s cooking skills), may<br />
result from eating alone<br />
RM 4.3; OHT 3.3<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
109
Personal Hygiene and Food<br />
Hygiene Problems<br />
• Possible food contamination-possible client<br />
comments:<br />
-I have a stomach ache<br />
-I have diarrhoea<br />
-I am going to the toilet a lot today<br />
• Further questions:<br />
-Are you taking fluids?<br />
-What did you eat yesterday?<br />
-Where did you get this food?<br />
-What is the diarrhoea like (colour and texture)?<br />
• Observations:<br />
-Try to identify the problem<br />
-Diarrhoea: what is the colour and texture like?<br />
-Check the food in the kitchen and rubbish<br />
This can be a client safety issue: If a number of<br />
clients have this problem, always report it<br />
RM 4.4; OHT 3.4<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
111
Mental Health Problems<br />
• Poor mental health can be related to alcoholism,<br />
dementia, depression, and other common medical<br />
problems affecting brain function<br />
(Parkinson’s disease, dementia, Alzheimer’s)<br />
• Severe micro-nutrient deficiencies (folate, Vitamin<br />
B-12, thiamin, niacin) and dehydration can cause<br />
mental problems<br />
• Memory problems or confusion, depression,<br />
anxiety, or nervousness may affect ability to<br />
organise nourishment<br />
• Poor mental health (sadness, grief, confusion,<br />
depression, memory loss) affects motivation and<br />
the ability to nurture self and general health<br />
RM 4.5; OHT 3.5<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
113
Mental Health Problems for the<br />
Older Person: Simple interventions<br />
Dementia<br />
• Avoid burns by not serving very hot foods<br />
• Reduce confusion with less food choice<br />
• Serve finger foods-if poor balance, coordination<br />
and reduced mobility<br />
Alzheimer’s disease<br />
Symptoms<br />
Agitation<br />
Loss of skills<br />
Confusion<br />
Medication effects<br />
Loss of memory Weight loss<br />
Depression<br />
Food strategies<br />
Reduce distractions Quiet, relaxing music<br />
Regular timed meals One course at a time<br />
Orient to food Time to eat<br />
Follow food habits Nourishing drinks<br />
RM 4.5; OHT 3.6<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
115
Poly-drugs<br />
(More than three types of medication daily)<br />
• Many medications have side-effects that reduce<br />
food intake<br />
• Taking more than three medications daily<br />
increases the chances of side effects and weight<br />
loss<br />
• Drug-nutrient and drug-drug interactions are<br />
exacerbated by poly-drugs, ageing, marginal food<br />
intakes or existing nutritional deficiencies<br />
• Medications can alter the body’s response to<br />
nourishment<br />
• Food itself can in turn alter the action of a drug or<br />
drugs that are taken<br />
• If the effect of drug therapy changes, always<br />
review whether there has been a recent diet<br />
change<br />
Possible referrals: pharmacist, doctor, dietitian<br />
RM 4.6; OHT 3.7a<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
117
Poly-drugs<br />
(An example of one older persons daily<br />
medication)<br />
Captopril<br />
Prazosin<br />
Diltiazen<br />
Lasix<br />
Slow K<br />
Prednisolone<br />
Pulmicort<br />
Atrovent<br />
Aspirin<br />
Nilstat<br />
Anginine<br />
Mianserin<br />
Coloxyl<br />
Panadol<br />
Eye drops<br />
bd<br />
bd<br />
tds<br />
mane<br />
mane<br />
mane<br />
bd<br />
bd<br />
mane<br />
qid<br />
prn<br />
nocte<br />
nocte<br />
prn<br />
qid<br />
RM 4.6; OHT 3.7b<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
119
Gastro-Intestinal Problems<br />
• Nausea and vomiting<br />
• Diarrhoea<br />
• Constipation<br />
RM 4.7-4.9; OHT 3.8<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
121
Nausea and Vomiting<br />
Nausea and vomiting can be caused by the<br />
following problems:<br />
• Poor personal hygiene<br />
• Poor food hygiene<br />
• Food contamination<br />
• Medication side effects<br />
• Illness<br />
Nausea and vomiting can lead to:<br />
• Dehydration<br />
• Reduced fluid intake<br />
• Reduced food intake<br />
• Weight loss<br />
After 24 hours, consider referral: doctor, trained<br />
nurse, dietitian<br />
RM 4.7; OHT 3.9a<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
123
Nausea and Vomiting:<br />
Simple Interventions<br />
• Ensure medication is correctly taken, perhaps after<br />
meals<br />
• Refer to Doctor immediately, if medication is<br />
suspected<br />
• Encourage 1/2 cup of fluid every hour or so (best<br />
tolerance is achieved by cold clear sweet fluids<br />
and then anything the client likes)<br />
• Then encourage small quantities of plain dry or<br />
sweet biscuits, dry bread, progressing through<br />
plain foods according to appetite<br />
• Recommend small frequent snacks throughout the<br />
day, building up to the usual pattern<br />
• Anti-nausea tablets (for example, Maxalon) may<br />
be used before food<br />
Monitoring: until nausea and vomiting cease<br />
Check outcomes: no further episodes?<br />
RM 4.7; OHT 3.9b<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
125
Diarrhoea<br />
Diarrohoea:<br />
• results from malabsorption of fluid and/or food<br />
(wasted food)<br />
• can cause abdominal discomfort, pain and<br />
distress, and reduced food and fluid intake<br />
• may be due to one or more possible reasons:<br />
-Poor personal hygiene<br />
-Contaminated food<br />
-Laxative abuse<br />
-Side effect of medication<br />
-Some sugar substitutes (sorbitol, fructose)<br />
-Stress<br />
-Lactose intolerance<br />
-Gastro-intestinal disease<br />
-Kidney disease<br />
RM 4.8; OHT 3.10a<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
127
Diarrhoea: Simple Interventions<br />
Acute diarrhoea<br />
• Clear sweet or other clear fluids (not fruit juices or<br />
milk) for 24 hours<br />
• Then introduce other fluids and foods-avoid<br />
rough fibrous foods and fatty foods<br />
• Continue until usual food pattern is restored<br />
Chronic diarrhoea<br />
• Ensure a nourishing diet is taken<br />
• Seek advice: doctor, dietitian, visiting nurse<br />
Monitoring: until diarrhoea ceases<br />
Check outcomes: no further episodes?<br />
RM 4.8; OHT 3.10b<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
129
Constipation<br />
Constipation can cause abdominal bloating and<br />
discomfort and reduced food intake<br />
Constipation may be due to one or more of the<br />
following reasons:<br />
• Reduced fluid intake<br />
• Reduced food intake<br />
• Low intake of dietary fibre-due to over-refined<br />
diet<br />
• Low activity level<br />
• Side-effect of medication<br />
• Laxative abuse<br />
RM 4.9; OHT 3.11a<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
131
Constipation: Simple Interventions<br />
• Review medications and use of laxatives<br />
• Recommend at least 6-8 cups of fluid daily<br />
• Recommend a slow but steady increase in dietary<br />
fibre:<br />
-Wholegrain cereals such as porridge, muesli,<br />
All-Bran, Fibre Plus, Just Right, Sultana Bran<br />
-Wholemeal breads or high fibre white bread<br />
-Fruits such as pineapple, apricots, fresh fruit<br />
-Fibrous vegetables, legumes<br />
• Offer hot tea and coffee (caffeine)<br />
• Recommend mobility and activity as tolerated<br />
• Recommend regular toileting<br />
Monitoring: daily fluid and fibre intake<br />
Check outcomes: gradual improvement in<br />
bowel actions (months)?<br />
RM 4.9; OHT 3.11b<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
133
Incontinence<br />
• Incontinence is very distressing and can lead to<br />
reduced fluid and food intake<br />
• Always seek expert advice from a continence<br />
adviser, doctor, visiting nurse, dietitian<br />
• Incontinence can be caused by one or more of<br />
the following:<br />
-Constipation<br />
-Weak anal sphincter<br />
-Poor mobility<br />
-Use of medications<br />
Bowel hydrating agents (lactulose, sorbilax)<br />
Diuretics, sedatives, anti-cholinergic agents,<br />
sleeping tablets<br />
-Medical problems<br />
Diabetes, urinary tract infection, obesity,<br />
stroke<br />
Parkinson’s disease, multiple sclerosis<br />
-Too much alcohol<br />
-Not enough dietary fibre<br />
Constipation<br />
-Insufficient fluid intake<br />
Constipation, decreased bladder capacity<br />
RM 4.10; OHT 3.12<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
135
Breathing Problems in the Older Person<br />
• The extra effort of breathing uses up a lot more<br />
energy than normal breathing<br />
• One and a half times more food energy is required<br />
• It is difficult to take sufficient food energy to<br />
achieve a good body weight<br />
• Fat metabolism results in less carbon dioxide<br />
produced by the body to be expired<br />
• Increased fat intake will improve food energy and<br />
assist breathing<br />
Consider specialist referral: dietitian<br />
RM 4.11; OHT 3.13<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
137
Medical problems<br />
• Medical problems which reduce ability to access<br />
and eat enough food and fluids<br />
-Decreased mobility<br />
-Breathing difficulty<br />
-Weight loss<br />
• Medical problems which increase the need for<br />
energy and nutrients<br />
-High body temperature, fever<br />
-Infection, impaired wound healing<br />
• Major medical disorders which change the need<br />
for nourishment and can cause feeding problems<br />
-Metabolic disorders<br />
-Cancer<br />
-Gastro-intestinal disorders<br />
RM 4.12; OHT 3.14<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
139
Diabetes<br />
• Simple diabetes-treated by diet only<br />
• Moderate diabetes-treated by diet and tablets<br />
• Complex diabetes-treated by diet and insulin<br />
injections<br />
Simple interventions-it is best for the client to:<br />
• Keep a good weight<br />
• Be as active as possible without overdoing it<br />
• Take regular meals and snacks, and nourishing<br />
foods<br />
• Have assistance from the visiting nurse<br />
• Have the best and latest information to keep well<br />
Monitoring:<br />
• Regular medical check, thorough yearly review<br />
• Regular dietary check, thorough yearly review of<br />
dietary treatment with a dietitian<br />
• Referral to a diabetic educator if appropriate.<br />
Referral for <strong>part</strong>icular advice: doctor, dietitian<br />
RM 4.12.1; OHT 3.15<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
141
Cardiovascular disease<br />
Frail older adults:<br />
• Risk factors not so important as prevention of<br />
weight loss and frailty<br />
Active adults:<br />
• Reduction of risk factors and prevention of<br />
problem development more important<br />
Younger high dependency adults:<br />
• Risk factors not so important as prevention of<br />
weight loss and frailty<br />
Monitoring:<br />
• Body weight in normal range for age<br />
• Yearly review of blood cholesterol and blood fats<br />
(if the client is on a modified fat diet)<br />
Referral for <strong>part</strong>icular advice: doctor, dietitian<br />
RM 4.12.2; OHT 3.16<br />
Identifying and Planning Assistance for Home-Based People Who are Nutritionally at Risk: A <strong>Training</strong> <strong>Manual</strong> (2001)<br />
143