16th Annual Scientific Meeting - Heart Failure Society of America
16th Annual Scientific Meeting - Heart Failure Society of America
16th Annual Scientific Meeting - Heart Failure Society of America
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
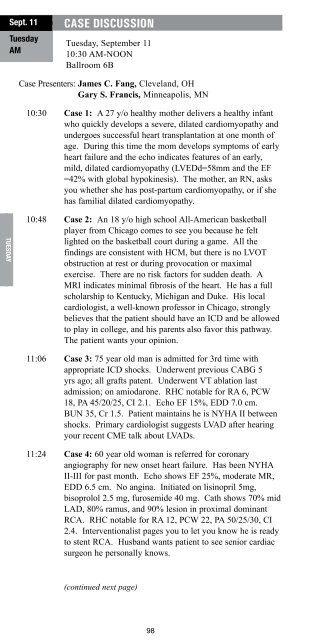
Sept. 11<br />
Tuesday<br />
AM<br />
Tuesday<br />
CASE DISCUSSION<br />
Tuesday, September 11<br />
10:30 AM-NOON<br />
Ballroom 6B<br />
Case Presenters: James C. Fang, Cleveland, OH<br />
Gary S. Francis, Minneapolis, MN<br />
10:30 Case 1: A 27 y/o healthy mother delivers a healthy infant<br />
who quickly develops a severe, dilated cardiomyopathy and<br />
undergoes successful heart transplantation at one month <strong>of</strong><br />
age. During this time the mom develops symptoms <strong>of</strong> early<br />
heart failure and the echo indicates features <strong>of</strong> an early,<br />
mild, dilated cardiomyopathy (LVEDd=58mm and the EF<br />
=42% with global hypokinesis). The mother, an RN, asks<br />
you whether she has post-partum cardiomyopathy, or if she<br />
has familial dilated cardiomyopathy.<br />
10:48 Case 2: An 18 y/o high school All-<strong>America</strong>n basketball<br />
player from Chicago comes to see you because he felt<br />
lighted on the basketball court during a game. All the<br />
findings are consistent with HCM, but there is no LVOT<br />
obstruction at rest or during provocation or maximal<br />
exercise. There are no risk factors for sudden death. A<br />
MRI indicates minimal fibrosis <strong>of</strong> the heart. He has a full<br />
scholarship to Kentucky, Michigan and Duke. His local<br />
cardiologist, a well-known pr<strong>of</strong>essor in Chicago, strongly<br />
believes that the patient should have an ICD and be allowed<br />
to play in college, and his parents also favor this pathway.<br />
The patient wants your opinion.<br />
11:06 Case 3: 75 year old man is admitted for 3rd time with<br />
appropriate ICD shocks. Underwent previous CABG 5<br />
yrs ago; all grafts patent. Underwent VT ablation last<br />
admission; on amiodarone. RHC notable for RA 6, PCW<br />
18, PA 45/20/25, CI 2.1. Echo EF 15%, EDD 7.0 cm.<br />
BUN 35, Cr 1.5. Patient maintains he is NYHA II between<br />
shocks. Primary cardiologist suggests LVAD after hearing<br />
your recent CME talk about LVADs.<br />
CASE DISCUSSION<br />
11:42 Case 5: A 37 y/o woman blood type O with advanced<br />
dilated cardiomyopathy (EF=22%, NYHA Class III) is<br />
referred to you for management. There are two issues that<br />
the referring physician wants you to clarify: The patient<br />
has a dilated LV with an LVIDd <strong>of</strong> 64 mm, and severe<br />
4+ MR with restricted mitral valve leaflet motion. The<br />
PVR, TPG and PA pressure indicate she is an acceptable<br />
transplant candidate. Can or should the MV be considered<br />
for repair? The other problem is that she is not tolerating<br />
her medications (carvedilol, lisinopril, spironolactone and<br />
furosemide) very well due to symptomatic hypotension.<br />
These are being down-titrated. How does one down-titrate?<br />
He asks you “is it time for an LVAD, or even MV repair and<br />
then an LVAD”? He is from the University <strong>of</strong> Michigan<br />
where MV repair for severe MR and a low EF is frequently<br />
performed.<br />
Panelists:<br />
Michele A. Hamilton, Los Angeles, CA<br />
Soon Park, Rochester, MN<br />
Patricia A. Uber, Baltimore, MD<br />
Sarah C. Paul, Hickory, NC<br />
Mario Talajic, Montreal, QC Canada<br />
Learning Objective: Using practice guidelines, research<br />
findings and clinical experience, make decisions about the<br />
management <strong>of</strong> difficult cases in heart failure.<br />
Sept. 11<br />
Tuesday<br />
AM<br />
Tuesday<br />
11:24 Case 4: 60 year old woman is referred for coronary<br />
angiography for new onset heart failure. Has been NYHA<br />
II-III for past month. Echo shows EF 25%, moderate MR,<br />
EDD 6.5 cm. No angina. Initiated on lisinopril 5mg,<br />
bisoprolol 2.5 mg, furosemide 40 mg. Cath shows 70% mid<br />
LAD, 80% ramus, and 90% lesion in proximal dominant<br />
RCA. RHC notable for RA 12, PCW 22, PA 50/25/30, CI<br />
2.4. Interventionalist pages you to let you know he is ready<br />
to stent RCA. Husband wants patient to see senior cardiac<br />
surgeon he personally knows.<br />
(continued next page)<br />
98 99