2013 Poster Session Summaries - AAMC
2013 Poster Session Summaries - AAMC
2013 Poster Session Summaries - AAMC
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
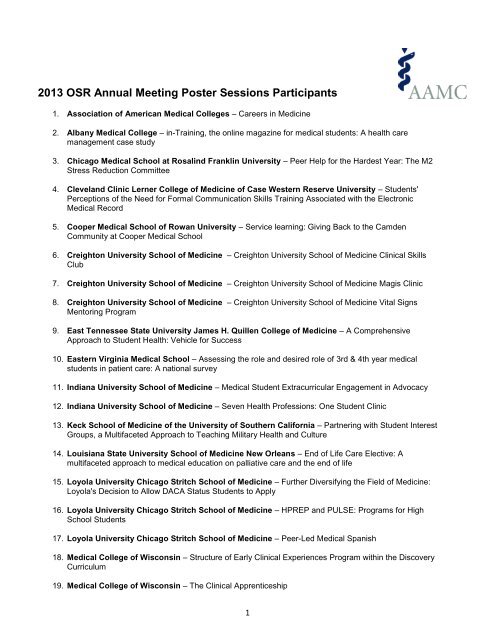
<strong>2013</strong> OSR Annual Meeting <strong>Poster</strong> <strong>Session</strong>s Participants<br />
1. Association of American Medical Colleges – Careers in Medicine<br />
2. Albany Medical College – in-Training, the online magazine for medical students: A health care<br />
management case study<br />
3. Chicago Medical School at Rosalind Franklin University – Peer Help for the Hardest Year: The M2<br />
Stress Reduction Committee<br />
4. Cleveland Clinic Lerner College of Medicine of Case Western Reserve University – Students'<br />
Perceptions of the Need for Formal Communication Skills Training Associated with the Electronic<br />
Medical Record<br />
5. Cooper Medical School of Rowan University – Service learning: Giving Back to the Camden<br />
Community at Cooper Medical School<br />
6. Creighton University School of Medicine – Creighton University School of Medicine Clinical Skills<br />
Club<br />
7. Creighton University School of Medicine – Creighton University School of Medicine Magis Clinic<br />
8. Creighton University School of Medicine – Creighton University School of Medicine Vital Signs<br />
Mentoring Program<br />
9. East Tennessee State University James H. Quillen College of Medicine – A Comprehensive<br />
Approach to Student Health: Vehicle for Success<br />
10. Eastern Virginia Medical School – Assessing the role and desired role of 3rd & 4th year medical<br />
students in patient care: A national survey<br />
11. Indiana University School of Medicine – Medical Student Extracurricular Engagement in Advocacy<br />
12. Indiana University School of Medicine – Seven Health Professions: One Student Clinic<br />
13. Keck School of Medicine of the University of Southern California – Partnering with Student Interest<br />
Groups, a Multifaceted Approach to Teaching Military Health and Culture<br />
14. Louisiana State University School of Medicine New Orleans – End of Life Care Elective: A<br />
multifaceted approach to medical education on palliative care and the end of life<br />
15. Loyola University Chicago Stritch School of Medicine – Further Diversifying the Field of Medicine:<br />
Loyola's Decision to Allow DACA Status Students to Apply<br />
16. Loyola University Chicago Stritch School of Medicine – HPREP and PULSE: Programs for High<br />
School Students<br />
17. Loyola University Chicago Stritch School of Medicine – Peer-Led Medical Spanish<br />
18. Medical College of Wisconsin – Structure of Early Clinical Experiences Program within the Discovery<br />
Curriculum<br />
19. Medical College of Wisconsin – The Clinical Apprenticeship<br />
1
20. Medical University of South Carolina College of Medicine – Enhancing Involvement in Research<br />
through the Medical Student Research Portal<br />
21. Medical University of South Carolina College of Medicine – The Role of Students in LCME<br />
Reaccreditation<br />
22. Michigan State University College of Human Medicine - Medical Business and Finance Elective<br />
23. Oakland University William Beaumont School of Medicine – Implementation of LGBT Safe Space<br />
Training in Medical Education<br />
24. Oakland University William Beaumont School of Medicine – Technology in Medical Education to<br />
Enhance Learning and Prepare Future Physicians for 21st Century Healthcare<br />
25. Perelman School of Medicine at the University of Pennsylvania – Factors Influencing the Intentions<br />
and Specialty Decisions of Physician-Scientist Trainees to Pursue Academic and Research Careers<br />
26. Perelman School of Medicine at the University of Pennsylvania – Training the Next Generation of<br />
Physician Educators through a Longitudinal Teaching Certificate Program<br />
27. Rush Medical College of Rush University Medical Center – Student Tutors in the Anatomy Lab<br />
28. Rush Medical College of Rush University Medical Center – Humanities in Medicine<br />
29. Saint Louis University School of Medicine – Curriculum changes to improve student wellness at SLU<br />
30. Texas A&M College of Medicine – M3/M4 Curricular Design at a Satellite Campus at Texas A&M COM<br />
31. Texas Tech University Health Sciences Center – Paul L. Foster School of Medicine – Integration of<br />
Medical Spanish Throughout Medical School Curriculum<br />
32. The University of Toledo College of Medicine – Pioneering Healthier Communities<br />
33. The University of Toledo College of Medicine – The University of Toledo Interprofessional Immersive<br />
Simulation Center and Medical Student Education<br />
34. Tulane University School of Medicine – Innovating a Curricular Quality Improvement Elective<br />
35. Universidad Central del Caribe – Advancing the Playing Field: A Look at How Technology and Play<br />
Can Change the Future of Medical Education<br />
36. Universidad Central del Caribe – Empowering Under-served Women Through Education Against<br />
Breast Cancer<br />
37. University of Arkansas for Medical Sciences College of Medicine – Student Opinion on the<br />
Effectiveness of a Student Curriculum Committee in the Era of Pre-Clinical Curriculum Change<br />
38. University of California, Irvine School of Medicine – Evaluating didactic methods for training medical<br />
students at The Faculty of Medicine in Transylvania, Romania in the use of bedside ultrasound for<br />
clinical practice<br />
39. University of Central Florida College of Medicine – Developing and Assessing the Efficacy of a<br />
Student Designed Summer Pre-Matriculation Program at the UCF College of Medicine<br />
40. University of Central Florida College of Medicine – Implementation and Assessment of an Effective<br />
Peer-Facilitated Transition-to-Clerkships (TTC) Program at the University of Central Florida College of<br />
Medicine (UCF COM)<br />
2
41. University of Central Florida College of Medicine – Peer Academic Coaching and its effect on<br />
academic performance at UCF College of Medicine<br />
42. University of Central Florida College of Medicine – Simulated Chaos: Adding Interactive Education to<br />
UCF COM’s Annual Global Health Conference<br />
43. University of Central Florida College of Medicine – UCF College of Medicine Global Health<br />
Conference "Emergency and Disaster Medicine"<br />
44. University of Colorado School of Medicine – Step 1 Pubquiz<br />
45. University of Florida College of Medicine – Journal Club in Preclinical Years: Five Easy Steps to<br />
Success<br />
46. University of Florida College of Medicine – Peer Academic Enrichment Program<br />
47. University of Illinois College of Medicine - Initiative to Increase Medical Student Awareness of LGBT<br />
Health Disparities<br />
48. University of Iowa Roy J. and Lucille A. Carver College of Medicine – Carver Rural Iowa Scholars<br />
Program (CRISP)<br />
49. University of Iowa Roy J. and Lucille A. Carver College of Medicine – Electronic Medical Records –<br />
Advanced Training for Medical Students<br />
50. University of Kentucky College of Medicine – Community Health Fair-Making Compassion our<br />
Tradition<br />
51. University of Miami Leonard M. Miller School of Medicine – DOCS Community Outreach Conference<br />
and Retreat<br />
52. University of Minnesota Medical School, Twin Cities – Phillips Neighborhood Clinic: Providing Health<br />
Care Access to the Underinsured<br />
53. University of Mississippi School of Medicine – Community Health Advocacy Project<br />
54. University of Mississippi School of Medicine – Dynamics of a Multidisciplinary Student Run Free<br />
Clinic<br />
55. University of Mississippi School of Medicine – Incorporating Business Medicine Preparedness in the<br />
Medical Curriculum<br />
56. University of Mississippi School of Medicine – Population Health Course at University of Mississippi<br />
57. University of Mississippi School of Medicine – Students Leading Students: A Model for Increasing<br />
Student Professionalism<br />
58. University of Mississippi School of Medicine – The Health Partnership Program: Affecting Healthy<br />
Change Using Motivational Interviewing<br />
59. University of North Dakota School of Medicine and Health Science – LCME Independent Student<br />
Analysis<br />
60. University of Oklahoma Health Sciences Center College of Medicine – Changing to a systemsbased<br />
curriculum: A four year retrospective<br />
61. University of South Florida Health Morsani College of Medicine – SuperUtilizer Project<br />
3
62. University of South Florida Health Morsani College of Medicine – USF Health Veterans Success<br />
Network<br />
63. University of Texas Southwestern Medical Center Southwestern Medical School – Innovating<br />
Healthcare Solutions (IHS) @ UT Southwestern<br />
64. University of Utah School of Medicine – Interprofessional Education in Health Sciences at the<br />
University of Utah<br />
65. University of Utah School of Medicine – Quantitative Analysis of Ophthalmological Surgical Education<br />
During Medical School and Residency<br />
66. University of Vermont College of Medicine – Rural Candidates Applications to Medical School<br />
67. Vanderbilt University School of Medicine – Medical Education in the Digital Age: A need for social<br />
media instruction<br />
68. Wake Forest School of Medicine – Emergency Medicine in the Third Year Curriculum<br />
69. Wayne State University School of Medicine – A Promising Pipeline to Medical Education: The Detroit<br />
Premedical Scholars Program<br />
70. Wayne State University School of Medicine – Health and Wellness Curriculum<br />
71. Yale University School of Medicine – Community-targeted Health Reform and ACA Implementation<br />
Education<br />
4
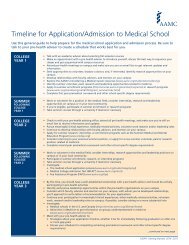
ASSOCIATION OF AMERICAN MEDICAL COLLEGES [Table # 1]<br />
Program/Project Title: Careers in Medicine<br />
Presenter(s): Jeanette Calli<br />
Email: jcalli@aamc.org<br />
Careers in Medicine (CiM) helps you explore your career options, choose a specialty, and apply to residency<br />
programs that meet your goals. CiM provides information, products, and services to support specialty choice<br />
activities throughout medical school. The core of the program is based on a career development process<br />
comprised of four phases: Understand Yourself, Explore Options, Choose a Specialty and Land a<br />
Residency. Resources include an extensive web site, self‐assessment tools, career information on more<br />
than 120 specialties and subspecialties, specialty choice and residency application information, and Choices,<br />
our quarterly newsletter. More information is available at www.aamc.org/cim.<br />
ALBANY MEDICAL COLLEGE [<strong>Poster</strong> # 2]<br />
Program/Project Title: in-Training, the online magazine for medical students: A health care<br />
management case study<br />
Presenter(s): Aleena Paul & Ajay Major<br />
Email: paula3@mail.amc.edu<br />
Research suggests that the socialized hierarchy and `hidden curriculum' of medical education promote<br />
student burnout and sap medical students of their optimism for the profession of medicine (Stewart 1995;<br />
Stewart 2000; Wear 1997). It is imperative that medical students become empowered to communicate with<br />
and seek support from their peers and to advocate for improvements in medical education. Historically, the<br />
geographic and ideological isolation of medical schools has made such communication unfeasible. To<br />
overcome these barriers, we created a dedicated student-written, peer-edited publication that promotes<br />
community building among medical students worldwide through self-reflection, communication and<br />
collaboration.<br />
in-Training is the online magazine for medical students, founded in April 2012 as a virtual community for<br />
students to reflect on their experiences and share their passions with their colleagues. In doing so, it helps<br />
students to cope with the rigors of medical education and to build a culture of open discourse among fellow<br />
physicians-in-training. To create a sustainable editorial process within this organizational culture, in-Training<br />
was founded on the core health care management principles of leadership development, governance<br />
modeling, and information management (Stefl 2008). We propose that this framework is optimal for the<br />
development of this niche as it promotes the authenticity and independence of the medical student voice. In<br />
14 months, 157 articles from 74 writers at 38 institutions across the United States, Canada and India have<br />
been published on in-Training. This is an indication that medical students are eager to share their<br />
experiences with the larger medical community in this previously unrealized forum. Topics include the<br />
patient-physician relationship, maintaining compassion during medical training, improving medical education,<br />
addressing health disparities, and refining the health care system. The distribution of writers for in-Training is<br />
representative of the medical student body; their pieces provide a snapshot of the opinions and passions of<br />
tomorrow's physicians, and indicate that medical students are cognizant of their roles in the evolving medical<br />
profession. Readership was steady at 800 unique visitors per month until March <strong>2013</strong>, when publication on<br />
the Scientific American Incubator blog caused a threefold increase to 2,200 unique visitors per month.<br />
Additional expansion was due to consistent presence on social media and strategic marketing targeted at<br />
academic deans nationwide.<br />
The use of in-Training provides for the development of connections between medical students with similar<br />
interests, and sets the stage for collaborations among medical students that surmount global boundaries.<br />
Reading and contributing to in-Training facilitates the spread of innovative ideas in improving both medical<br />
education and the health care system. Future goals for in-Training involve building partnerships with other<br />
medical student organizations and encouraging participation from the global medical student community. To<br />
ensure sustainability, organic enhancements will be made to the publication that reflect the evolving needs of<br />
the medical student body.<br />
5
CHICAGO MEDICAL SCHOOL AT ROSALIND FRANKLIN UNIVERSITY [<strong>Poster</strong> # 3]<br />
Program/Project Title: Peer Help for the Hardest Year: The M2 Stress Reduction Committee<br />
Presenter(s): Nick Hawley<br />
Email: Nicholas.hawley@my.rfums.org<br />
Stress is a significant concern among Medical students as they face an array of potential stressors including<br />
schoolwork, relationships, family issues, extracurricular activities, and USMLE exams. Students report that<br />
stress is worst during 2nd year while preparing for USMLE Step 1. The Chicago Medical School at Rosalind<br />
Franklin University noted its students’ stress levels and formed the M2 Stress Reduction Committee to<br />
address this problem. Comprised of fifteen students and an administrator, the committee’s primary goal is to<br />
investigate sources of student stress and plan ways to alleviate it all while fostering a supportive environment<br />
within the class. Its recommendations included various wellness-promoting activities and events,<br />
course/schedule changes, and education on stress and how to cope with it.<br />
During the year, the committee organized several student activities and wellness events. Most of the events<br />
required minimal or no cost and minimal planning beyond the committee members. They also took students<br />
concerns about courses and scheduling to identify areas where the administration could help minimize<br />
stress. Committee actions ranged from distributing candy before exams to having a potluck lunch to<br />
suggestions on semester schedules. The committee planned various events and activities, highlighting the<br />
importance of maintaining personal well-being.<br />
Student surveys will be conducted in March to gauge the effectiveness of the committee and better<br />
understand student stress. Data collected will be presented with the poster. We believe the stress reduction<br />
committee has helped raise awareness and lower stress within the class and created a platform for<br />
promoting student wellness.<br />
CLEVELAND CLINIC LERNER COLLEGE OF MEDICINE OF CASE WESTERN RESERVE UNIVERSITY<br />
[<strong>Poster</strong> # 4]<br />
Program/Project Title: Students' Perceptions of the Need for Formal Communication Skills Training<br />
Associated with the Electronic Medical Record<br />
Presenter(s): Daniel London<br />
Email: londond@ccf.org<br />
At the 2011 <strong>AAMC</strong> National Meeting joint regional session between the Central and Western regions, OSR<br />
representatives discussed the lack of educational opportunities focused on teaching medical students how to<br />
properly communicate with a patient while using the electronic medical record (EMR). Taking this idea back<br />
to our home institution, we began discussions on how to incorporate such training into our current<br />
communication skills curriculum. To garner institutional support for this innovation, however, we needed to<br />
obtain data demonstrating that this is a student need and want amongst our students.<br />
We performed a needs assessment survey of Cleveland Clinic Lerner College of Medicine (CCLCM) medical<br />
students to better understand their perspectives on the topic of how the EMR impacts patient-doctor<br />
communication and the potential utility of educational sessions. Students felt strongly that the EMR impacts<br />
communication with patients—positively in some aspects and negatively in others. By their second year of<br />
medical school, almost all students are using the EMR in patient interactions. Students have voiced a desire<br />
to be taught how to properly use the EMR when communicating with patients. This education would involve<br />
maximizing the positive aspects, such as educating the patient, acquiring the database, and performing<br />
health maintenance tasks, while limiting the negative aspects such as engaging in non-verbal<br />
communication, developing rapport, and demonstrating empathy. Students believe that this teaching should<br />
happen during second year, and that it should be done in a workshop setting such as communication skills<br />
with further reinforcement via longitudinal clinic experiences. As a result of our findings, two student driven<br />
educational projects have resulted: a book chapter and a revamped standardized patient encounter.<br />
6
COOPER MEDICAL SCHOOL OF ROWAN UNIVERSITY [<strong>Poster</strong> # 5]<br />
Program/Project Title: Service learning: Giving Back to the Camden Community at Cooper Medical<br />
School<br />
Presenter(s): Imoh Ikpot, Gita Byraiah & Rebecca Lee<br />
Email: ikpoti60@students.rowan.edu<br />
At Cooper Medical School of Rowan University, volunteerism is an integral part of the campus community.<br />
All students are required to engage in a service learning projects within the city of Camden. The outreach<br />
efforts are directed based on community needs as expressed through focus groups and at the<br />
recommendation of our Community Advisory Committee. This course was created to fulfill the philosophy<br />
that immersion of students provides a realistic view of the social, economic and cultural influences and<br />
barriers facing the underserved Camden community. Students have been involved with various activities<br />
including schools, homeless shelters, soup kitchens and churches. In aggregate, students view this as a<br />
favorable and beneficial experience.<br />
CREIGHTON UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 6]<br />
Program/Project Title: Creighton University School of Medicine Clinical Skills Club<br />
Presenter(s): Mayme Marshall<br />
Email: mem25750@creighton.edu<br />
This poster was created by the members of the student-run Clinical Skills Club at Creighton University<br />
School of Medicine and is designed to provide information about the organization as well as the monthly<br />
clinical workshops that are held in the Clinical Simulation and Education Center. The Clinical Skills Club was<br />
created by two medical students in 2011 who desired more opportunities for hands-on clinical practice in the<br />
first and second years of medical school. It has blossomed into an organization where upper class medical<br />
students (with faculty supervision) engage and educate first and second year medical students during clinical<br />
simulations.<br />
The clinical education is developed around the motto “See one, Do one, Teach one”. First the students “see”<br />
a short presentation of the clinical skill and its relevant background given by upperclassmen. Then, they “do<br />
one” and perform the skill using various simulators under the supervision of the upperclassmen, and in the<br />
later years they are invited back as upperclassmen to “Teach one”.<br />
CREIGHTON UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 7]<br />
Program/Project Title: Creighton University School of Medicine Magis Clinic<br />
Presenter(s): Laura Brannan<br />
Email: mem25750@creighton.edu<br />
The Magis Clinic began in 2004 when a group of Creighton medical students found there were few outpatient<br />
healthcare options available to disadvantaged men, women and children of the Omaha metropolitan area.<br />
The clinic is managed and staffed by Creighton medical students and overseen by a volunteer physician. In<br />
addition to providing valued medical care to our patients, Magis also provides a distinct and educational clinic<br />
experience for Creighton medical student volunteers. Another important facet of the Magis Clinic’s mission<br />
has been to foster in the medical student volunteers a lifelong commitment to service and learning and to<br />
serve as a site of teaching for our students. First- and second-year medical students are encouraged to push<br />
their limits and participate actively in patient interviews and physical exams. They are guided by<br />
upperclassmen volunteers, who work closely alongside them. This peer mentoring support is critical to<br />
facilitating an educational environment. The Magis Clinic’s attending physician is also available throughout<br />
clinic to answer questions, provide guidance, and educate students on diagnostic and treatment options, and<br />
while it is ultimately the attending physician’s treatment plan, medical students are encouraged to use their<br />
knowledge and skills to provide treatment options.<br />
7
CREIGHTON UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 8]<br />
Program/Project Title: Creighton University School of Medicine Vital Signs Mentoring Program<br />
Presenter(s): Laura Brannan<br />
Email: mem25750@creighton.edu<br />
In the complex world of healthcare and increasing pressures on healthcare professionals, medical students<br />
have a need for purposeful personal and professional development. The Vital Signs Mentoring Program has<br />
been created to provide structure and multiple opportunities for faculty, clinicians, students and alumni to<br />
interact and impact one another through mentoring relationships.<br />
EAST TENNESSEE STATE UNIVERSITY JAMES H. QUILLEN COLLEGE OF MEDICINE [<strong>Poster</strong> # 9]<br />
Program/Project Title: A Comprehensive Approach to Student Health: Vehicle for Success<br />
Presenter(s): Liane Gozmao & Kyle Owens<br />
Email: owensks@goldmail.etsu.edu<br />
The Quillen College of Medicine at East Tennessee State University strives to provide students with an<br />
atmosphere that not only supports academic achievement, but also personal well-being. Several programs<br />
have been implemented to support the overall health and wellness both inside and outside the classroom. A<br />
Student Study Center was constructed to provide a conducive environment for students to study, as well as<br />
an area for students to gather and build relationships outside of the classroom. In addition, a student led<br />
organization, Committee Supporting Student Health (CSSH), was implemented to support the total health of<br />
the student population, which includes support in dealing with stress, family crisis, mental illness and<br />
substance abuse. A mentorship program between incoming first year students and a second year provides<br />
each MS-1 with someone who can assist with navigating through the first year of medical school. Finally, one<br />
of the paramount components supporting the overall mental health of the student body is the Professional<br />
and Academic Resource Center (PARC). The PARC program provides psychological and psychiatric<br />
counseling to students and their families at no cost. Student feedback has shown that these programs have<br />
proven effective in strengthening the personal health of Quillen medical students. The Quillen College of<br />
Medicine is continuously seeking ways to further improve their programs.<br />
EASTERN VIRGINIA MEDICAL SCHOOL [<strong>Poster</strong> # 10]<br />
Program/Project Title: Assessing the role and desired role of 3rd & 4th year medical students in patient<br />
care: A national survey<br />
Presenter(s): Drew Bolton, Ed Nadimi, Jeff Goodwin, Brian Specht & Brian Pitts<br />
Email: bolton.drew@gmail.com<br />
In collaboration with the University of Colorado SOM and the Virginia Tech Carilion Clinic SOM, a brief<br />
survey was developed to determine the extent of involvement that third and fourth year medical students<br />
have in patient care. The goal was to determine what proportion of schools allow their third and fourth year<br />
students to write notes, write orders and answer pages. The survey also sought to solicit the opinion of each<br />
school's OSR on how to increase the role and responsibility of fourth year medical students in patient care.<br />
Ultimately, the objective was to perform a needs assessment to establish the foundation of a compelling<br />
argument for changing medical education. This change in medical education would seek to increase the<br />
capacity of fourth year students and improve the transition to intern year without compromising safe and<br />
quality patient care.<br />
This poster will highlight the literature regarding undergraduate medical education, with special attention<br />
given to the impact of Electronic Medical Records and note writing on preparing students for the intern year.<br />
The literature review will emphasize the clinical objectives of undergraduate medical education and the<br />
potential for EMRs to greatly improve students' capacity for effective communication and efficient patient<br />
care.<br />
8
INDIANA UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 11]<br />
Program/Project Title: Medical Student Extracurricular Engagement in Advocacy<br />
Presenter(s): Janice Farlow<br />
Email: JLLIN@IUPUI.EDU<br />
The <strong>AAMC</strong> has called for an increase in medical school enrollment to meet future projected physician<br />
shortages, but the number of residency positions has not increased proportionately. With traditional funding<br />
sources for Graduate Medical Education (GME) under threat, leaders in academic medicine, health care<br />
systems, and government will need to be engaged in proposing solutions to this predicament. Medical<br />
students, as future health professionals directly affected by the shortage of residency slots, should also be<br />
involved in the discussion. Furthermore, this presents a professional development opportunity for medical<br />
students, both in learning more about the country's health care system, and in building leadership skills<br />
through advocacy.<br />
Medical students at the Indiana University School of Medicine involved in the Medical Student Section (MSS)<br />
of the American Medical Association (AMA) have been actively monitoring the situation and engaging<br />
students across Indiana. Recently, the Indiana AMA-MSS proposed a resolution to study public/private<br />
partnerships as a mechanism for expanding residency training to meet the needs of the State of Indiana. The<br />
resolution was passed by the Indiana State Medical Association, and plans are underway for advancing the<br />
resolution to the national stage as well.<br />
The Indiana AMA-MSS has also facilitated programming to help students understand career planning in light<br />
of the concerning number of unmatched senior medical students. Other initiatives have included bringing<br />
speakers to campus to discuss recent health care policy changes and how students can get more involved in<br />
advocating for change. In this poster, these and other initiatives to get medical students engaged outside of<br />
the classroom in advocacy will be discussed.<br />
INDIANA UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 12]<br />
Program/Project Title: Seven Health Professions: One Student Clinic<br />
Presenter(s): Janice Farlow<br />
Email: JLLIN@IUPUI.EDU<br />
Organizations such as the <strong>AAMC</strong> and the Institute of Medicine have stressed the importance of<br />
interprofessional education. While student-run clinics have become a common vehicle for such<br />
collaborations across the country, the need still exists to provide meaningful interprofessional interaction at<br />
these clinics. The Indiana University Student Outreach Clinic (IU-SOC) not only represents a clinic with one<br />
of the most expansive lists of participating health professions in the country, but also is one of the few that<br />
boasts a student-driven, intentional interprofessional program to meet learning and clinical outcomes.<br />
Sponsored originally by the IU School of Medicine in 2009, the IU-SOC is a student-led service-learning<br />
collaborative that has grown to include formal partnerships with seven professional fields (Medicine,<br />
Pharmacy, Law, Dentistry, Social Work, Physical Therapy, Occupational Therapy) across three institutions<br />
(Indiana University, Butler University, University of Indianapolis), as well as informal partnerships with<br />
additional disciplines (public health, nonprofit management and business, and information technology, to<br />
name a few). The clinic has been recognized as an outstanding community-campus partnership locally by an<br />
Indianapolis City County Council Ordinance and as the recipient of the IUPUI Chancellor's Community Award<br />
for Excellence in Civic Engagement. Recently, the IU-SOC was also awarded the State of Indiana<br />
Governor's Service Award of Service-Learning. Student and faculty leaders from the IU-SOC have presented<br />
on the clinic's interprofessional model at local, regional, and national meetings.<br />
While exposure to each profession occurs naturally in the clinic space, the IU-SOC officers, made up of<br />
student leaders from each partner program, have developed a program to integrate each profession to<br />
provide comprehensive patient-centered care while also enhancing the interprofessional educational<br />
environment for volunteers. In addition to managing its discipline-specific operations, each partner school<br />
has a student position designated to coordinate efforts with other partner schools. A Partners Committee of<br />
these students, community representatives, and invited guests meets monthly to provide updates and<br />
discuss issues of general concern. Subcommittees of representatives holding analogous positions within<br />
each partner's student board convene separately to plan interdisciplinary efforts, such as patient education<br />
9
programs and community promotions. Student leaders from each school also participate in a biannual<br />
Partners Retreat that focuses on interdisciplinary long-term strategic planning.<br />
Additional interprofessional engagement opportunities exist for the volunteers, including an orientation held<br />
at the beginning of each clinic session to introduce all volunteers, explain the clinic's model, and emphasize<br />
the importance of interprofessional interactions. Medical school faculty can receive Continuing Medical<br />
Education credits for leading an interdisciplinary roundtable, where volunteers from each school discuss<br />
patient cases that required the cooperation of several disciplines that clinic day. There are interprofessional<br />
rounds, and students can also informally shadow volunteers of other schools to gain a more complete picture<br />
of their services.<br />
In focus groups and surveys conducted as part of an ongoing assessment of the learning environment of the<br />
IU-SOC, students have consistently identified the interprofessional nature of the clinic as a key reason for<br />
volunteering and as providing a unique and necessary component to their medical education. In this poster,<br />
we will share data collected, best practices learned, and ongoing endeavors to strengthen the IU-SOC's<br />
interprofessional program.<br />
KECK SCHOOL OF MEDICINE OF THE UNIVERSITY OF SOUTHERN CALIFORNIA [<strong>Poster</strong> # 13]<br />
Program/Project Title: Partnering with Student Interest Groups, a Multifaceted Approach to Teaching<br />
Military Health and Culture<br />
Presenter(s): Claire Sadler, Mariya Kalashnikova & Christos Theophanous<br />
Email: kalashni@usc.edu<br />
In alliance with the <strong>AAMC</strong>’s Joining Forces campaign we have developed and implemented a core<br />
curriculum for medical students at Keck that addresses the physical, social, psychological and spiritual needs<br />
of veterans and military- connected patients and their families. Previously Keck medical students had little<br />
exposure to military health issues due to a lack formal curriculum around military culture. We have partnered<br />
with specialty student interest groups (SIGs) to create a series of sessions that focus on military health<br />
issues in a variety of health care disciplines. This strategy generates peer involvement and engages students<br />
with a range of interests in the needs of military families and veterans. The proposed sessions are designed<br />
to introduce students to a broad spectrum of issues in military health care and increase both interest and<br />
awareness. Bypassing the formal curriculum allows us to introduce a large volume and range of content<br />
quickly, with flexibility to adjust sessions according to student feedback. Furthermore, by partnering with<br />
SIGs we hope to get “buy -in” from student leaders on campus, further widening the scope of the Joining<br />
Forces campaign at Keck. We propose a series of lunch time sessions as detailed below:<br />
- November 11, <strong>2013</strong> - Military SIG: Military culture in and outside the “fortress” – A primer on military<br />
culture, led by CPT Dustin Harris, LCSW, Behavioral Health Officer.<br />
- November 25, <strong>2013</strong> – Surgery SIG: Polytrauma in the military<br />
- TBD – Obstetrics and gynecology SIG: Sexual Assault in the Military<br />
- TBD – Pediatric SIG: The Military Child<br />
- TBD – Psychiatry SIG: Invisible Wounds – PTSD and TBI<br />
LOUISIANA STATE UNIVERSITY SCHOOL OF MEDICINE NEW ORLEANS [<strong>Poster</strong> # 14]<br />
Program/Project Title: End of Life Care Elective: A multifaceted approach to medical education on<br />
palliative care and the end of life<br />
Presenter(s): Laura Rachal & Abigail Freeman<br />
Email: lrach1@lsuhsc.edu<br />
The End-of-Life-Care Elective is a course designed for second year medical students to explore the issues<br />
surrounding patients facing terminally ill diseases. While the students participating in the course are in school<br />
to study health and illness, this course is primarily a lesson in the emotional, spiritual, and interpersonal<br />
relationships in the patient approaching end of life. The course emphasizes understanding the impact of<br />
terminal disease on a person's conscience and the provision of compassionate care. It has been part of the<br />
curriculum at LSUHSC New Orleans for almost 10 years.<br />
10
The course objectives are to develop a relationship with a dying patient; to identify some of the biopsychosocial<br />
issues faced by dying patients; to enhance student's communications skills with current and<br />
future patients; to witness treatment of terminally ill patients in modern health care systems; to identify some<br />
of the ethical principles pertinent to end-of-life-care; to better understand the role of hospice in the care of<br />
terminally ill patients and their families; and to learn about the interdisciplinary approach to end of life care.<br />
Each student in the course is required to attend at least one hospice team meeting, meet with their assigned<br />
patient along with a hospice team member, and have two additional meetings with their patient over the<br />
course of the semester. Interlaced with these patient visits are small-group session sled by third and/or<br />
fourth-year medical students and SOM faculty who will facilitate dialogue about the students' experiences.<br />
Students are evaluated by the SOM faculty on a Pass/Fail scale, on the basis of completion of all course<br />
responsibilities such as individual patient encounters and completion of reading assignments, and their level<br />
of engagement in small group sessions.<br />
LOYOLA UNIVERSITY CHICAGO STRITCH SCHOOL OF MEDICINE [<strong>Poster</strong> # 15]<br />
Program/Project Title: Further Diversifying the Field of Medicine: Loyola's Decision to Allow DACA<br />
Status Students to Apply<br />
Presenter(s): Mary Calderone, Sarah Hale, Isabel Malone, Andrew Tully<br />
Email: imalone1@luc.edu<br />
Starting in fall 2012, following the President’s speech announcing DACA (Deferred Action for Childhood<br />
Arrivals), Loyola University Chicago Stritch School of Medicine revised admissions standards to allow<br />
undocumented applicants to compete on their own merits for seats at Loyola. Loyola’s decision has been<br />
controversial nationwide. Some administrators fear these applicants may be unable to secure employment<br />
upon graduation. Although licensing boards in Illinois cannot inquire about immigration status, other states<br />
may. National work permits might not be renewed in an unstable political climate. And these applicants<br />
remain ineligible for most federal financial aid. Loyola’s administration is working to address these concerns.<br />
The university and the Illinois State legislature established a state loan program aimed at DACA medical<br />
school tuition relief. Loyola also gathered adequate institutional aid to make the financial burden comparable<br />
to other applicants. To the concern of political instability, Loyola sees this as an unacceptable excuse to<br />
continue to deny admittance to qualified applicants.<br />
In taking a positive stance that these applicants ought to be treated on their own merits, Loyola has already<br />
further solidified the DACA position. Secure in our Jesuit values of fostering social justice, extensive <strong>AAMC</strong><br />
research on the importance of a diversified physician workforce, and our fellow <strong>AAMC</strong> schools who share our<br />
mission, Loyola is honored to be the first and confident it will not be the last medical school to train these<br />
applicants as doctors for their country.<br />
LOYOLA UNIVERSITY CHICAGO STRITCH SCHOOL OF MEDICINE [<strong>Poster</strong> # 16]<br />
Program/Project Title: HPREP and PULSE: Programs for High School Students<br />
Presenter(s): Mary Calderone, Sarah Hale, Isabel Malone & Andrew Tully<br />
Email: imalone1@luc.edu<br />
Students at Loyola University Chicago School of Medicine are invested in ensuring that health care fields are<br />
diverse in future generations. Two programs focus on mentoring and encouraging students of color and<br />
economically disadvantaged students to pursue their dreams of becoming physicians, nurses, and other<br />
allied health care professionals - the Health Professions Education and Recruitment Program (HPREP) and<br />
PULSE.<br />
HPREP is a six-week program through the Students National Medical Association and Latino Student<br />
Medical Association for high school level students that want to pursue a health career. It was introduced last<br />
year with assistance from Chicago Schweitzer Fellowship Program, which continues to support the program.<br />
Students are introduced to a variety of fields, exposed to health disparities, and given the opportunity to<br />
engage with students and professionals from a variety of fields. At the end of the program students present<br />
their research to their families, faculty, and students. This year the program is expanding and adding a<br />
community service component in addition to interaction with pre-medical level students in order to complete<br />
the pre-health pipeline.<br />
11
PULSE is a year-long program that exposes students from Proviso Math and Science Academy in Maywood,<br />
IL to a variety of areas in the medical profession. Physicians and other medical professionals present<br />
aspects of their practice to students each month and assists the students as they attempt these clinical skills.<br />
Additionally, the students are grouped with current medical school students to foster a mentoring relationship<br />
that will hopefully pique and encourage their interest in medicine outside of what they learn in the classroom.<br />
Both programs seek to improve the representation of people of color in the health professions in order to<br />
address a diversifying and increasingly chronically ill population.<br />
LOYOLA UNIVERSITY CHICAGO STRITCH SCHOOL OF MEDICINE [<strong>Poster</strong> # 17]<br />
Program/Project Title: Peer-Led Medical Spanish<br />
Presenter(s): Mary Calderone, Sarah Hale, Isabel Malone & Andrew Tully<br />
Email: imalone1@luc.edu<br />
Peer-Led Medical Spanish is an elective course offered to Stritch medical students, Marcella Niehoff School<br />
of Nursing students, and interested faculty and administrators. First and second year medical students with<br />
an advanced or fluent knowledge of Spanish are able to earn a two week elective teaching credit by creating<br />
lesson plans, teaching classes on a weekly basis, compiling a portfolio of their work, and attending teaching<br />
seminars throughout the year. Classes themselves are offered at varying levels on a weekly basis. From<br />
complete beginners to native speakers, classes are designed to meet students at their level and provide<br />
language tools that will be invaluable skills for their current or future careers in healthcare.<br />
The number of Spanish-language speakers living in the United States has grown exponentially over the past<br />
decade, and that trend is projected to continue into the upcoming years as well. Therefore, as medical<br />
students dedicated to providing the best quality of patient care possible, we find it of the utmost importance<br />
that students are given an opportunity to learn, improve upon, and practice their Spanish communication<br />
skills, especially in a medical context. By attending classes, students learn essential medical vocabulary and<br />
are given the opportunity to practice patient interviews with their classmates and teachers in Spanish.<br />
Teachers are not only earning elective credit, but advancing their own skills and gaining valuable teaching<br />
skills to take into their careers. Since the program's initiative five years ago, classes have been growing in<br />
popularity, and have been widely attended by first and second year medical students.<br />
During the <strong>2013</strong>-2014 academic year, nursing students from Loyola University Marcella Niehoff School of<br />
Nursing will be collaborating with medical students and taking the same medical Spanish courses for the first<br />
time. We hope that this collaborative effort will continue to foster an environment of teamwork between all<br />
healthcare professionals. Finally, at the conclusion of their second year of medical school, advanced<br />
students are encouraged to take Loyola's Medical Spanish Certification exam. Upon passing this exam,<br />
students earn the legal right to translate for their Spanish-speaking patients during their third and fourth year<br />
clerkships. The Peer-Led Medical Spanish Program has been a tremendous success at Loyola Stritch<br />
School of Medicine, and we would love the opportunity to share this program with other interested schools.<br />
MEDICAL COLLEGE OF WISCONSIN [<strong>Poster</strong> # 18]<br />
Program/Project Title: Structure of Early Clinical Experiences Program within the Discovery<br />
Curriculum<br />
Presenter(s): Anish Patel & Melanie Bobbs<br />
Email: ahpatel@mcw.edu<br />
The Medical College of Wisconsin (MCW) debuted its new Discovery Curriculum in the fall of 2012. Among a<br />
host of updates to the preclinical curriculum was the introduction of several early clinical experiences. These<br />
experiences, which extend throughout the first two years of medical school, are designed to introduce<br />
students to clinical practice early on and prepare them for their clinical years. The structure of the Program<br />
begins with learning basic clinical competencies for working in the clinics during the first semester. For the<br />
next two semesters, students attend clinical apprenticeships one half day per week, where preceptors<br />
mentor students, observe respective levels of patient care and provide direct feedback. The final semester<br />
includes a Capstone project that allows students to hone the skills they have absorbed in the clinic with<br />
exposure to specialized and more complicated patient populations. While medical schools throughout the<br />
12
country are incorporating early clinical experiences into the preclinical curriculum, few programs, to our<br />
knowledge, are as extensive.<br />
MEDICAL COLLEGE OF WISCONSIN [<strong>Poster</strong> # 19]<br />
Program/Project Title: The Clinical Apprenticeship<br />
Presenter(s): Anish Patel & Melanie Bobbs<br />
Email: ahpatel@mcw.edu<br />
The Medical College of Wisconsin (MCW) debuted its Discovery Curriculum in the fall of 2012. Among a host<br />
of updates to the preclinical curriculum was the introduction of several early clinical experiences designed to<br />
introduce and familiarize M1 and M2 students with clinical medicine and patient care. Key among these new<br />
programs was the Clinical Apprenticeship, a longitudinal course where students spend one half-day per<br />
week working directly with clinical faculty. The Apprenticeship allows students to develop history and<br />
physical exam skills, gain familiarity with the clinical environment and more thoroughly explore a particular<br />
field of interest. Due to the significant time commitment and structure of the Apprenticeship, students have<br />
the opportunity to develop close relationships with their mentors and receive direct, personalized feedback.<br />
These experiences shorten the learning curve as students transition to the clerkships, and prepare them to<br />
be even more successful during their clinical years.<br />
MEDICAL UNIVERSITY OF SOUTH CAROLINA COLLEGE OF MEDICINE [<strong>Poster</strong> # 20]<br />
Program/Project Title: Enhancing Involvement in Research through the Medical Student Research<br />
Portal<br />
Presenter(s): Mallory Roberts, Daniel Weinberg & Arun Iyer<br />
Email: robertmn@musc.edu<br />
Research opportunities allow medical students to expand their understanding of evidence-based medicine<br />
and explore career options, but unfortunately there are several barriers to medical student involvement in<br />
research. LCME Standards suggest that a core function of undergraduate medical education is to remove<br />
some of these barriers: “The institution is expected to provide an appropriate number and variety of research<br />
opportunities,” and, “information about financial support for student research (e.g., stipends).” To this end,<br />
the Medical University of South Carolina created the Medical Student Research Portal (MSRP) in 2011. In an<br />
effort to pair interested medical students with research mentors both at home and at other institutions, the<br />
MSRP serves as an online hub where students can view research and funding opportunities and learn how<br />
to engage themselves in a research project. The MSRP includes links for internal and external research<br />
opportunities, funding options, departmental research contacts, important resources such as IRB and CITI<br />
training, FAQ about student research, and general information. Since the creation of the MSRP, our<br />
institution has increased the participation of first-year medical students in summer research projects two<br />
years in a row. Fourth year students have also shown increased participation in elective research and<br />
research for academic credit. Furthermore, the participation of minority students in research has increased.<br />
We plan to present data on this increased medical student involvement in research and discuss reasons for<br />
the success of the MSRP. Areas for further improvement will be noted, with an aim to show other medical<br />
universities how to integrate a system similar to the MSRP in to their online resources for medical students.<br />
MEDICAL UNIVERSITY OF SOUTH CAROLINA COLLEGE OF MEDICINE [<strong>Poster</strong> # 21]<br />
Program/Project Title: The Role of Students in LCME Reaccreditation<br />
Presenter(s): Daniel Weinberg, Arun Iyer & Mallory Roberts<br />
Email: weinber@musc.edu<br />
Since the revision of the LCME Standards in 2002, there has been a shift in the number of citations to reflect<br />
greater emphasis on the educational program and medical students. Such a shift reflects the importance of<br />
structuring a role for students throughout the accreditation process that not only allows for a successful<br />
LCME review, but also strengthens the foundation of the medical school. Unfortunately, outside of LCME<br />
publications, there remains a significant gap in the academic medical literature regarding specific roles of<br />
students in LCME review. With this presentation we hope to add to the resources for students and<br />
administration by providing a retrospective analysis of best practices and lessons learned from student<br />
involvement in preparing for LCME reaccreditation at the Medical University of South Carolina. We will<br />
13
discuss the process of the independent student analysis and how it led to beneficial changes in our own<br />
institution. We will also discuss strategies for engaging students in preparation for the site visit. Finally, we<br />
will demonstrate that by effectively incorporating students into LCME reaccreditation, not only will the<br />
reaccreditation process be successful, but an institution as a whole will become stronger.<br />
MICHIGAN STATE UNIVERSITY COLLEGE OF HUMAN MEDICINE [<strong>Poster</strong> # 22]<br />
Program/Project Title: Medical Business and Finance Elective<br />
Presenter(s): Joseph B. Meleca<br />
Email: melecajo@msu.edu<br />
The College of Human Medicine Medical Business & Finance (MBF) Elective in coordination with the Career<br />
Counseling and Development Program has for the past six months been planning an inaugural elective for<br />
medical students in the fall semester of <strong>2013</strong>. The MBF Elective has been newly established this year and is<br />
focused on providing students with a background in both medical business and finance. The goal of this<br />
elective is to expose students early on to the ever-changing aspects of insurance, reimbursement, contracts,<br />
investments, loans, and various other relevant topics. No longer are physicians exempt from needing to<br />
understand such things as insurance plans, billing standards, or how to run an office. We hope that this<br />
elective will educate young physicians-in-training to handle the business and finance side of medicine.<br />
The elective is well under way. We have been collecting data to see if students have enjoyed the course,<br />
find it relevant and necessary for their medical education, and feel that it has advanced their knowledge in<br />
both medical business and finance. This data would be presented on the poster.<br />
OAKLAND UNIVERSITY WILLIAM BEAUMONT SCHOOL OF MEDICINE [<strong>Poster</strong> # 23]<br />
Program/Project Title: Implementation of LGBT Safe Space Training in Medical Education<br />
Presenter(s): Florence Doo & Julian Thwainey<br />
Email: fxdoo@oakland.edu<br />
The Association of American Medical Colleges (<strong>AAMC</strong>) revealed in 2007 that lesbian, bisexual, gay, and<br />
transgender (LGBT) medical students experience discrimination throughout their educational and clinical<br />
training. In medical education, LGBT medical students may encounter faculty and staff with limited<br />
knowledge in LGBT topics, lack of LGBT topics in the medical curriculum, as well as derogatory comments in<br />
the classroom, on campus, and in clinical settings. Safe Space training is a program that promotes<br />
inclusivity and is primarily used to establish a network of LGBT allies. It is available on many college<br />
campuses, but implementation of Safe Space training in the medical school context has faced limited<br />
research and educational resources. Oakland University William Beaumont School of Medicine (OUWB) is<br />
working on developing a medically-relevant Safe Space training for medical school faculty and students. The<br />
design and implementation of a training model in a medical school setting will be discussed.<br />
OAKLAND UNIVERSITY WILLIAM BEAUMONT SCHOOL OF MEDICINE [<strong>Poster</strong> # 24]<br />
Program/Project Title: Technology in Medical Education to Enhance Learning and Prepare Future<br />
Physicians for 21st Century Healthcare<br />
Presenter(s): Julian Thwainey & Florence Doo<br />
Email: jgthwain@oakland.edu<br />
Indicated in our mission statement, Oakland University William Beaumont School of Medicine (OUWB) aims<br />
to develop a “technologically advanced learning community” to prepare tomorrow’s physicians. As medicine<br />
and technology continually advances, we believe medical education should keep up. This is why OUWB<br />
created an innovative curriculum that incorporates different technologies in order to not only better teach our<br />
medical students, but also to help our medical students become more technologically competent.<br />
Several journal articles outline the necessity of producing technologically competent physicians, as<br />
technology and computers are becoming part of our health care environment. OUWB integrates different<br />
teaching technologies in every aspect of our curriculum from basic lectures and anatomy lab to clinical skills<br />
and clerkships. All incoming medical students receive a Mac Book Pro 13” with preloaded concept-mapping<br />
software. Activities in our basic science courses help students use this software to learn. Our state-of-the-art<br />
14
anatomy lab gives students access to Mac computers located at each station during dissections. Cameras<br />
can relay video to station computers for better viewing of dissections. Lastly, M1s are introduced early to<br />
several types of advanced patient stimulations including Beaumont Hospital’s state-of-the-art Surgical Skills<br />
Center.<br />
In addition to utilizing technology in teaching medical students, the M1 and M2 curriculum integrates the<br />
teaching of using indispensable resources such as Pub Med, UpToDate, and even mobile software. OUWB<br />
continues to evaluate potentially useful technologies. We have setup an iPad Mini pilot program for use<br />
during clerkships. This showcase aims to show how OUWB uses different technologies to prepare its<br />
students for 21st century medicine.<br />
PERELMAN SCHOOL OF MEDICINE AT THE UNIVERSITY OF PENNSYLVANIA [<strong>Poster</strong> # 25]<br />
Program/Project Title: Factors Influencing the Intentions and Specialty Decisions of Physician-<br />
Scientist Trainees to Pursue Academic and Research Careers<br />
Presenter(s): Dania Daye<br />
Email: ddaye@mail.med.upenn.edu<br />
Physician-scientists dedicate their careers to advancing knowledge of human disease and in doing so enable<br />
development of new treatments and preventive measures to improve human health. Although the factors that<br />
influence the attrition of physician-scientist junior faculty have been studied extensively, the factors that<br />
influence the career decisions of medical students to pursue academic and research careers are less well<br />
characterized. Our student-led study aimed to assess the factors that influence the career decisions of<br />
physician- scientist trainees as well as the obstacles that they foresee as a future hindrance to their careers.<br />
Data was collected using an IRB-approved survey at 5 major US institutions with MSTP programs. The<br />
survey was distributed via email to all MD and MD/PhD trainees and garnered 1103 responses, a 40%<br />
response rate, representing all training stages. 20% of the respondents were MD/PhD trainees (n= 226).<br />
Using Chi-square and multivariate regression analyses, we found significant factors influencing trainee<br />
career decisions to enter academia and research and found statistically significant differences between the<br />
MD and MD/PhD trainee cohorts that responded to the survey. Compared to MD trainees, MD/PhD trainees<br />
were more likely to intend careers in academia (94% vs. 72%) and industry (25.6% vs. 9.7%) vs. private<br />
practice (17.7% vs. 51.3%) (p=0.001). MD/PhD trainees also value research as an important factor in their<br />
careers, favor different medical specialties such internal medicine, neurology, pathology over surgical<br />
specialties and anticipate obstacles such as lack of opportunity & funding (54.4% vs. 17.8%). This study is<br />
the basis for an ongoing national representative sample study and will play an important role in filling the<br />
data gap for current MD and MD/PhD trainee population in their career intentions and the perceptions and<br />
factors driving their decisions. Our study has identified statistically significant factors that influence the career<br />
decisions of our future physicians and physician scientists and thus, can provide insight into potential areas<br />
for intervention to maintain a strong interest in academic and research careers.<br />
Dania Daye 1,6 *, Jennifer M. Kwan 2,6 *, Mary Lou Schmidt 2 , Claudia Morrissey 3 , Hajwa Kim 2 , Bilwaj Gaonkar 1 , Megan<br />
Riddle 4 , Sharline Madera 4 , Kate Quinn 5<br />
1 Perelman School of Medicine at the University of Pennsylvania, 2 University of Illinois, Chicago College of Medicine,<br />
3 Save the Children DC, 4 Weill Cornell College of Medicine, 5 City University of Seattle, 6 American Physician Scientists<br />
Association.*authors contributed equally<br />
PERELMAN SCHOOL OF MEDICINE AT THE UNIVERSITY OF PENNSYLVANIA [<strong>Poster</strong> # 26]<br />
Program/Project Title: Training the Next Generation of Physician Educators through a Longitudinal<br />
Teaching Certificate Program<br />
Presenter(s): Dania Daye & Jonathan McNeill<br />
Email: ddaye@mail.med.upenn.edu<br />
A large number of medical students will have teaching responsibilities during residency and beyond. In an<br />
effort to promote better education of the next generation of physicians, we proposed adopting a formal<br />
medical education certificate program for medical students at the Perelman School of Medicine at the<br />
University of Pennsylvania. The goal of the program would be to prepare students to become academic<br />
15
medical educators through: 1) training in the science of medical education, theoretical frameworks, and<br />
principles; 2) experiential learning through formal teaching experiences with reflection and feedback; 3)<br />
scholarship in medical education via curriculum development or medical education research; 4) mentorship<br />
by faculty with experience in medical education leadership or scholarship. The four components of the<br />
certificate program would be longitudinally integrated into the medical school curriculum through required<br />
workshop sessions, teaching experience, longitudinal mentoring and opportunities in medical education<br />
scholarship and research. Students also have the opportunity to enroll in a 2-week course, entitled Frontiers<br />
in Medical Education, to learn about the most recent scientific advances in medical education methodologies<br />
and research. Participants in the certificate program will be followed through residency and beyond to<br />
assess the effectiveness of this program and its contribution to their training and long term outcomes. It is<br />
expected that this program will provide medical students with much-needed training making them better<br />
educators, both as house officers and eventually as attending physicians.<br />
Dania Daye, MS4, Jonathan McNeill, MS4, Jennifer Kogan, M.D.<br />
Perelman School of Medicine at the University of Pennsylvania<br />
RUSH MEDICAL COLLEGE OF RUSH UNIVERSITY MEDICAL CENTER [<strong>Poster</strong> # 27]<br />
Program/Project Title: Student Tutors in the Anatomy Lab<br />
Presenter(s): Jennifer Olson<br />
Email: jlolson83@gmail.com<br />
While many schools employ students to tutor the classes below them, Rush has uniquely extended the<br />
program into the anatomy lab. Free tutoring is offered Monday through Thursday at two evening sessions or<br />
on Friday afternoon. Over thirty M2s volunteer to again don their scrubs and lead small group hands-on<br />
tutoring sessions. Students generally work in groups of two to four to divide that week’s anatomy curriculum.<br />
They arrive early to find an example cadaver, clean up the dissection, and then review structures and related<br />
information as the M1s rotate between tutors. They also organize a practice anatomy practical exam for<br />
every block which involves tagging structures and providing a key. <strong>Session</strong>s are well-attended with more<br />
than 90% of each class participating. Many cite the program’s value in that students can pass down memory<br />
tools and often-asked exam questions. It also eases anxiety about the practical exam and provides for<br />
mentorship opportunities by facilitating inter-class communication. The University organizes the paid<br />
employment of the students as tutors and announces its availability to the new class, but limits its<br />
involvement there. Tutors submit attendance sheets with participants’ signatures as time sheets which also<br />
functions as quality control as pupils will vote with their feet. Cost to the university is minimal, 20-30 tutors<br />
work 4-10 hours per month at $10/hour. The simple model of this program could be easily reproduced at<br />
other schools for the benefit of even more first year students.<br />
RUSH MEDICAL COLLEGE OF RUSH UNIVERSITY MEDICAL CENTER [<strong>Poster</strong> # 28]<br />
Program/Project Title: Humanities in Medicine<br />
Presenter(s): Jennifer Olson<br />
Email: Erica_J_Huelsmann@rush.edu<br />
At Rush Medical College, we recently integrated a unique “Humanities in Medicine” elective course for a<br />
small group of first year medical students. We would like to share the unique qualities of our program, the<br />
expected and unexpected responses of faculty and students, and future directions with others.<br />
General Course Description:<br />
This elective was an 18-session course that examined how empathy, observation and interpretation impact<br />
one’s experience of literature and the arts. Particular attention was paid to the ways in which observation<br />
and engagement with the arts parallels observation and engagement in patient care. Individual sessions<br />
focused on the role of temporal and professional perspective in describing medical events, differences and<br />
similarities in observational skills in the arts and medicine and the use of movement and drama exercises to<br />
examine how one experiences and is experienced by others. Course activities included museum visits,<br />
movement activities, acting exercises and reading and writing about selected works of literature.<br />
16
While many institutions have programs where students engage in observation of the fine arts, focus is placed<br />
mainly on increasing their own observational skills; our program is unique in that the focus is placed primarily<br />
on introspection and self-awareness as a mechanism to increase empathy.<br />
Reflection and Future Directions:<br />
Student and faculty responses were collected following each module and at the culmination of the course to<br />
examine the implementation of the course, how it was received, and what enhancements could be made for<br />
the future. Many replied that the course was "the best thing about this year", and requested for an additional<br />
version for second year medical students. Moreover, students requested the creation of an informal<br />
humanities club.<br />
As both faculty and students very well received this elective, we plan to continue offering this course to first<br />
year students. Our plans for the near future include expanding the course to allow participation of more<br />
students. Offering multiple sections of the course, not expanding the number of students in each section as<br />
the small group atmosphere was highly rated by students, will do this. Additionally, we hope to expand the<br />
target student body to include other colleges at Rush University (nursing, physician assistant, etc.). Finally,<br />
we would like to delineate a working conceptualization of physician empathy and describe an integrative<br />
approach to assessing physician empathy.<br />
SAINT LOUIS UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 29]<br />
Program/Project Title: Curriculum changes to improve student wellness at SLU<br />
Presenter(s): Divya Gumber, Brandon Beal & Kristin Pacl<br />
Email: dgumber@slu.edu<br />
Over the past year, several changes have been brought about in the curriculum at SLU School of Medicine in<br />
order to improve student wellness. We identify challenges faced by students in their preclinical as well as<br />
clinical years and the changes that are in motion to address these challenges.<br />
1. Subjectivity in third year grading system<br />
The grading system of core clerkships in third year is a source of significant anxiety among medical students.<br />
About 65% of the schools in US use some variation of the Honors/Pass/Fail system, where subjective<br />
evaluations by faculty and residents comprise the most significant proportion of the grade. 1 The inherent<br />
differences in the average grades awarded by different individuals put significant stress on medical students.<br />
Third year medical students feel that their grades in core clerkships are unduly affected by the evaluators<br />
they happen to work with. In order to address this issue, the OSR chapter at SLU has worked with the<br />
administration to provide evaluators with average scores awarded by other faculty members. This would<br />
allow evaluators to compare their evaluations with others’. We are also working on providing students a clear<br />
breakdown of how their evaluator form is used to arrive at a numerical score for their subjective evaluation.<br />
We believe that creating transparency regarding the clerkship grading system will help allay the anxiety that<br />
students feel.<br />
2. Computer based testing (CBT) for first year students<br />
During the first two years of medical school, students are traditionally tested with paper based examinations.<br />
This creates significant anxiety and apprehension for students when they have to take their NBME licensing<br />
exams - starting with Step 1- that are all electronic. 2 In order to facilitate this transition, SLU SOM is currently<br />
working on administering first year tests in an electronic format. Other advantages of CBT are easier editing<br />
of test items, enhancement of learning by using feedback from specific questions, and incorporation of<br />
multimedia into questions.<br />
3. Compressing preclinical curriculum<br />
Students at SLU have often expressed concern about not having enough time to do rotations in a variety of<br />
fields before applying for the match. The administration has now compressed the preclinical curriculum to<br />
give students two extra months in which to schedule electives in different fields before applying for the<br />
match. Picking a specialty is by far the most important and often the most difficult decision that medical<br />
students make, and we feel this change would allow them to make a well informed choice.<br />
17
References<br />
1. Takayama H, Grinsell R, Brock D et al. Is it appropriate to use core clerkship grades in the selection of<br />
residents? Curr Surg 2006; 63(6): 391-6.<br />
2. Hochlehnert A, Brass K, Moeltner A et al. Does medical student preferance of test format (computerbased<br />
Vs paper-based) have an influence on performance? BMC Medical Education 2011; 11: 89-92<br />
TEXAS A&M COLLEGE OF MEDICINE [<strong>Poster</strong> # 30]<br />
Program/Project Title: M3/M4 Curricular Design at a Satellite Campus at Texas A&M COM<br />
Presenter(s): Manik Aggarwal & Megan Ross<br />
Email: manik.aggarwal1@gmail.com<br />
At the Texas A&M College of Medicine, there are four clinical sites where students can complete their 3rd<br />
and 4th years of medical school. Although there is a minimum standard and expectation that the COM<br />
obliges by, each clinical campus has its own unique qualities and characteristics. This poster aims to<br />
highlight the clinical opportunities at the Dallas site at Baylor University Medical Center. This clinical site has<br />
been active for the last two years and continues to evolve to provide the best clinical experience and<br />
exposure to medical students. Briefly, here is a synopsis.<br />
M3 (limited flexibility, 48 academic weeks)<br />
1. Surgery (12 wks): 1 month with the overnight trauma service embedded with the resident teaching service<br />
(2 wks days, 2 wks nights); 1 month with the general service; 1 month on sub-specialty split into a pair of 2<br />
wks (ENT, urology, CT service, ortho, vascular)<br />
2. OB/GYN (6 wks): 2 wks inpatient gyn, 2 wks inpatient OB, 1 wk outpatient obgyn, 1 wk elective (MFM,<br />
ultrasound, fertility clinic); 5 total overnight calls during the rotation<br />
3. Pediatrics (6 wks): 3 wks outpatient, 2 wks inpatient, 1 wk nursery; admit patients daily while on inpatient<br />
service<br />
4. Family Medicine (6 wks): 5 wks outpatient, 1 wk inpatient; admit patients daily while on inpatient service<br />
5. Psychiatry (6 wks): 6 wks of outpatient and inpatient care; also have a simultaneous 2 wk alcohol and drug<br />
elective; admit patients once per week on inpatient service)<br />
6. Internal Medicine (12 wks): 8 wks inpatient, 3 wks outpatient, 1 wk assessment/examinations; admit<br />
patients while on call every fifth day during inpatient service<br />
M4 (significant flexibility, 40 academic weeks)<br />
1. Everyone (14 wks): Acting Internship (4 wks), ICU (4 wks), ED (4 wks), Professionalism (2 wks)<br />
2. 12 weeks pertinent to your specialty (ie 4 wks of HemeOnc, ID and Cardiology each)<br />
3. 14 weeks electives: clinical (any department), humanities or student self-initiated electives<br />
4. 8 weeks of vacation: utilized for Step 2, interview traveling and time off<br />
Equally important, the poster will highlight ways the poster will cover ways Texas A&M maintains equality<br />
across campuses—including student-attending interaction, clerkship goals and objectives, assessments,<br />
grading similarities.<br />
TEXAS TECH UNIVERSITY HEALTH SCIENCES CENTER - PAUL L. FOSTER SCHOOL OF MEDICINE<br />
[<strong>Poster</strong> # 31]<br />
Program/Project Title: Integration of Medical Spanish Throughout Medical School Curriculum<br />
Presenter(s): Huy Nguyen & James Showery<br />
Email: jennifer.pan@ttuhsc.edu<br />
To better train doctors for a growing Spanish-speaking population, the Paul L. Foster School of Medicine<br />
curriculum integrates medical Spanish and clinical sciences over a four-year period. Located in El Paso, TX,<br />
18
the Paul L. Foster School of Medicine at TTUHSC is the only four-year medical school on the U.S./Mexico<br />
border and provides medical students the unique opportunity to improve Spanish communication skills<br />
through a formal medical Spanish course and immersion experiences. In the medical Spanish course, first<br />
and second-year students expand their medical vocabularies by translating components of the medical/<br />
physical exam and practicing doctor-patient interactions with fluent or native speakers. The preclinical<br />
curriculum also offers Spanish language immersion experiences through required clinical rotations at<br />
community clinics and service learning activities in rural Hispanic communities. 3rd and 4th year students<br />
practice Spanish language skills in their clinical rotations, gaining proficiency by interacting with Spanishspeaking<br />
patients. With its integrated curriculum, TTUHSC PLFSOM hopes to graduate physicians who are<br />
capable of providing language-concordant clinical care in Spanish.<br />
THE UNIVERSITY OF TOLEDO COLLEGE OF MEDICINE [<strong>Poster</strong> # 32]<br />
Program/Project Title: Pioneering Healthier Communities<br />
Presenter(s): Frank Vento & James Whaley<br />
Email: stephen.schaaf@rockets.utoledo.edu<br />
The purpose of this program is to provide students a service learning opportunity. Service learning is defined<br />
as a learning experience that combines community service with preparation and reflection. The Pioneering<br />
Healthier Communities elective allow a first or second year medical student to volunteer at the South YMCA<br />
at the Morse Center. Students volunteer for programs that are already established as apart of the YMCA’s<br />
Pioneering Healthier Communities (PHC) program.<br />
Students participate in a service learning opportunity focused in the Lifestyle Eating, Activities, and Attitudes<br />
(LEAP) Program. Those who participate in LEAP are under the age of 21 and are referred by a physician.<br />
The program focuses on a multidisciplinary approach to maintaining an optimal weight and healthy lifestyle.<br />
Student volunteers in LEAP work as a health mentor responsible for assisting the children/young adults in a<br />
group or individualized exercise routine. In addition, students also will be able to teach classes advising the<br />
participants and their parents on proper nutrition.<br />
This elective is a great opportunity for the YMCA and JCC of Great Toledo and UTCOM to partner together<br />
to promote healthy living in the Toledo community. Students in this elective are able to see the importance<br />
that volunteer service can have in promoting healthy behaviors. In addition, students are able to use and<br />
strengthen their medical knowledge in order to promote healthy lifestyle changes for children/young adults.<br />
THE UNIVERSITY OF TOLEDO COLLEGE OF MEDICINE [<strong>Poster</strong> # 33]<br />
Program/Project Title: The University of Toledo Interprofessional Immersive Simulation Center and<br />
Medical Student Education<br />
Presenter(s): Frank Vento & James Whaley<br />
Email: james.whaley@rockets.utoledo.edu<br />
The University of Toledo Interprofessional Immersive Simulation Center (UT-IISC) aims to train health<br />
professional students prior to involvement in patient care through the use of a broad spectrum of “state-ofthe-art”<br />
clinical simulation and 3-D technologies. The UT-IISC will function as three separate, yet<br />
integrated centers - The Progressive Anatomy & Surgical Skills Center, an Advanced Clinical Simulation<br />
Center, and a Virtual Immersive Reality Center. With the combinational use of these centers, medical<br />
students will be able to practice surgical skills, train in interdisciplinary patient care activities, and be<br />
assessed for competency prior to involvement in patient care.<br />
TULANE UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 34]<br />
Program/Project Title: Innovating a Curricular Quality Improvement Elective<br />
Presenter(s): Justin Halls, Carlos Oronce<br />
Email: jhalls@tulane.edu<br />
This poster will showcase Tulane's new medical education elective (soon to be available to 3rd and 4th year<br />
students) that is designed to inspire academically minded research projects and school-wide introspection<br />
aimed at quality improvement.<br />
19
In order to provide an example of student activities, this poster will present a student led research project<br />
analyzing data from student feedback on Team Based Learning (TBL) activities at Tulane. The data being<br />
presented will utilize student survey questionnaire items to identify what correlates most strongly with overall<br />
high satisfaction scores and what items correlate most strongly with low satisfaction scores. The results are<br />
then discussed in the context of prominent papers and medical education literature on quality in TBL<br />
delivery.<br />
UNIVERSIDAD CENTRAL DEL CARIBE [<strong>Poster</strong> # 35]<br />
Program/Project Title: Advancing the Playing Field: A Look at How Technology and Play Can Change<br />
the Future of Medical Education<br />
Presenter(s): Jhonathan Duarte, José Vilaró, Cristina Villa, Wilson Veras & Elizabel De León<br />
Email: elizabel.deleon@uccaribe.edu<br />
Play combines all three aspects of learning: visual, auditory, and tactile/kinesthetic. An element of “play” is<br />
an essential component for perennial learning to occur in all individuals. In the case of learning medicine,<br />
lectures are commonly designed to favor one or maybe two types of learning styles, but seldom integrate all<br />
three. The question is, why not integrate all three aspects using play? By using the Microsoft Kinect<br />
gesture recognition device this project brings the element of play to the representation of fundamental<br />
anatomical concepts, and thus engages students more strongly in the learning process. The purpose of this<br />
project is to introduce the ludic andragogy, by using kinect interactive gaming sensor as a teaching tool in the<br />
anatomy laboratory. In addition, this study will assess the effectiveness of this interactive device on student<br />
performance.<br />
UNIVERSIDAD CENTRAL DEL CARIBE [<strong>Poster</strong> # 36]<br />
Program/Project Title: Empowering Under-served Women Through Education Against Breast Cancer<br />
Presenter(s): Claudia Rodríguez Miranda, Fiorella Reyes Báez, Verónica Díaz Vidal, Nicolle Canales Ramos<br />
& Ada Londoño Bello<br />
Email: elizabel.deleon@uccaribe.edu<br />
PINK (Professional women who Inspire, Nurture, and share their Knowledge with other women) is a studentgoverned<br />
coalition of women from three generations with the mission to create a forum where professional<br />
women serve as mentors and provide support, education, and outreach to the community by a two-step<br />
process. First, professional women pledge to share their expertise, gained through work and professional<br />
experience, with women who are in professional/graduate academic programs. Second, professional/<br />
graduate female students pledge to provide psychological support, education, and outreach to at-risk<br />
adolescent girls and under-served women through a mentoring program, and serve as positive role models<br />
for them.<br />
According to The Cancer Journal of Clinicians, the mortality in women beginning at age 40 with breast<br />
cancer is reduced by 44% if early detected. PINK recognizes that education is crucial, especially for the<br />
people who have limited access to health services. As part of our mission, PINK participated in a health fair<br />
in the Dominican Republic last May <strong>2013</strong> to attend the needs of under-served women and assess their<br />
knowledge about breast cancer and self-examinations. They were given a pre-test before the educative<br />
session and a post-test afterwards. The results of both tests were sorted and analyzed. Breast examinations<br />
were performed under the supervision of an OB/GYN and patients that needed further exams were advised<br />
to visit their primary physician. PINK advocated the importance of monthly self-examinations in order to<br />
detect breast tissue anomalies, and fomented yearly mammograms for women after the age of 40. The data<br />
collected demonstrated that, even if the women knew about breast cancer, they actively learned more<br />
information after the session. Ultimately, educating women about their health and possible risks empowers<br />
them to prevent future progression of breast diseases.<br />
20
UNIVERSITY OF ARKANSAS FOR MEDICAL SCIENCES COLLEGE OF MEDICINE [<strong>Poster</strong> # 37]<br />
Program/Project Title: Student Opinion on the Effectiveness of a Student Curriculum Committee in the<br />
Era of Pre-Clinical Curriculum Change<br />
Presenter(s): Parth Shah<br />
Email: shahp.123@gmail.com<br />
With the pre-clinical curriculum overhaul that the University of Arkansas for Medical Sciences – College of<br />
Medicine (UAMS-COM) has undergone, along with changes that medical schools across the nation are<br />
experiencing or have already undergone, it is imperative that student opinion regarding these changes be<br />
heard. The purpose of this study was to measure the effectiveness and opinion of a Student Liaison<br />
Curriculum Committee (SLCC), defined as an organization besides the class executives that acts solely to<br />
provide communication/feedback between the student body and the faculty regarding changes in the<br />
curriculum. It surveyed students who only had the old curriculum for their entire pre-clinical years (Seniors),<br />
students who had half of the old curriculum and half of the new curriculum (Juniors), a slightly modified<br />
version of the new curriculum (Sophomores), and then the completely redesigned curriculum (Freshman).<br />
The methods in which data was collected were through an eighteen-question survey. Statistical analysis was<br />
done to show the change in opinion across the four classes. The data will be used to further modulate, guide,<br />
and mold the pre-clinical curriculum in order to provide the best education possible to the students.<br />
UNIVERSITY OF CALIFORNIA, IRVINE SCHOOL OF MEDICINE [<strong>Poster</strong> # 38]<br />
Program/Project Title: Evaluating didactic methods for training medical students at The Faculty of<br />
Medicine in Transylvania, Romania in the use of bedside ultrasound for clinical practice<br />
Presenter(s): Cosmin Florescu<br />
Email: florescu@uci.edu<br />
Medical students' time is a precious commodity and learning activities should maximize time efficiency and<br />
the amount of useful material that is learned. The purpose of this research project was to help the research<br />
team and Dr. Chris Fox from UC Irvine School of Medicine determine whether podcasts or live-class<br />
teaching best augments hands-on ultrasound teaching. O'Bannon et al. found that there was no significant<br />
difference between using traditional lecture and podcast modalities in the realm of students seeking a<br />
teaching credential. The research team wanted to see if this is the case for teaching bedside<br />
ultrasonography to medical students (O'Bannon, 2011). The hypothesis was that the best method of teaching<br />
ultrasound includes a combination of podcasts describing the anatomy, pathology, and sonography of organ<br />
systems and hands-on sessions with the ultrasound machine.<br />
The training was done in an international setting at the Faculty of Medicine at Transilvania University of<br />
Brasov in Romania. Medical students were randomly assigned to one of three different study groups.<br />
Students assigned to the first group watched a 50-minute live lecture and attended a 50-minute hands-on<br />
bedside ultrasound training session. Students assigned to the second group watched a podcast that covered<br />
the same material as the live lecture and attended a 50-minute hands-on bedside ultrasound training<br />
session. Students assigned to the third group did not attend a lecture or watch a podcast but attended a 50-<br />
minute bedside ultrasound training session. Each day, a different topic was covered; these were 1)<br />
Introduction to ultrasound & knobology, 2) Pulmonary ultrasound, 3) Cardiac ultrasound, 4) Focused<br />
Assessment with Sonography for Trauma (FAST) exam, and 5) Hepatobiliary ultrasound. Pre- and posttraining<br />
evaluations were conducted to compare the three study groups. On the first day of the program,<br />
students were randomly assigned an ID number and asked to complete a 20-question pre-training quiz that<br />
covered basic ultrasound principles and the FAST exam. At the end of the ultrasound course, the students<br />
completed a post-training quiz and the FAST exam for their practical test. Students' pre- to post-training quiz<br />
scores in the lecture group increased from 33.6% to 72.6% correct, while those in the podcast group<br />
increased from 40.7% to 75.5% correct, and the control group increased from 37.8% to 70%. Data analysis<br />
(one-way ANOVA) showed that there were no statistically significant differences in quiz score improvement<br />
among the three study groups. Similar analysis for the practical exam showed no statistically significant<br />
differences among the three study groups. These results suggest that all three methods are equally effective<br />
at improving student comprehension of bedside ultrasound and that faculty have the flexibility to use the one<br />
that best suits their institution and student learning style.<br />
O'Bannon, B.W., Lubke, J.K., Beard, J.L., and Britt, V.G. (2011), Using podcasts to replace lectures: Effects on student<br />
achievement. 57; 1885-1892. Doi:10.1016/j.compedu.2011.04.0 0<br />
21
UNIVERSITY OF CENTRAL FLORIDA COLLEGE OF MEDICINE [<strong>Poster</strong> # 39]<br />
Program/Project Title: Developing and Assessing the Efficacy of a Student Designed Summer Pre-<br />
Matriculation Program at the UCF College of Medicine<br />
Presenter(s): Bassam Ayoub & Elizabeth John<br />
Email: Sayoub@knights.ucf.edu<br />
Many medical students encounter transitional challenges at the start of their medical school careers.<br />
Historically, these challenges are faced by both traditional students and non-traditional students, defined in<br />
this study as students who have taken time away from academia or those who lacked previous exposure to<br />
the medical sciences in their undergraduate careers. Faculty-led pre-matriculation programs have been<br />
previously used at other institutions to address these challenges, with the majority being targeted towards<br />
non-traditional students.<br />
In this study, a novel online summer pre-matriculation program was developed and made available to all<br />
incoming UCF 1st year medical students. This program consisted of six online Self Learning Modules (SLMs)<br />
that highlighted the most important concepts of the first module of the UCF curriculum. There were two<br />
components of this study that were of particular interest - students' academic performances and their<br />
perceptions on how the pre-matriculation program prepared them for the beginning of medical school. First,<br />
the students’ mastery of the content knowledge was gauged by administering a Pre- and Post-test. Results<br />
demonstrated that a student-led program is an effective means of instruction, as evidenced by the<br />
significantly better scores on the Post-test (n = 25, mean = 61.8%; SE = 3.7%) as compared to the Pre-test<br />
(n = 25, mean = 37.0%; SE = 2.9%; p < 0.001). Furthermore, the performances of traditional and nontraditional<br />
students were compared, and no significant differences were found between the two groups’<br />
mastery of knowledge.<br />
An additional component of the study included gauging the students’ perceptions of this pre-matriculation<br />
program before the start of start of the academic year and after completion of the first module of the UCF<br />
curriculum. It was found that 88% of participants found the instructional content of this program to be<br />
organized and accurate. Moreover, 88% of participants believed that the continuation of this program would<br />
be beneficial for future classes at the UCF College of Medicine. Finally, 62.5% of participants reported that<br />
participation in this program had eased their transition into medical school and raised their awareness of<br />
which specific concepts they will encounter at the start of their medical school experience. The data garnered<br />
from this study is important because of the program’s unique ability to provide tutelage to all students in a<br />
cost-effective manner. This study should be re-run on a larger sample size for more telling findings.<br />
UNIVERSITY OF CENTRAL FLORIDA COLLEGE OF MEDICINE [<strong>Poster</strong> # 40]<br />
Program/Project Title: Implementation and Assessment of an Effective Peer-Facilitated Transition-to-<br />
Clerkships (TTC) Program at the University of Central Florida College of Medicine (UCF COM)<br />
Presenter(s): Rabia Zafar<br />
Email: rabiazafar@gmail.com<br />
Rabia Zafar, Ph.D.; Lori Boardman, M.D., MSc; Marcy Verduin, M.D.<br />
University of Central Florida College of Medicine, 6850 Lake Nona Blvd. Orlando, FL 32827<br />
The majority of U.S. medical schools largely follow a curriculum constituting two years of basic science<br />
education preceding two years of clinical clerkships. Many students find themselves ill-prepared when<br />
entering the clinical realm of medical education due to the vastly different learning environments of both<br />
phases. To bridge this transition from pre-clinical to clinical years, several medical schools have introduced a<br />
“transition course” prior to beginning clerkships. Existing transition courses, although partially successful,<br />
have failed to fully mitigate the deficiency in clinical readiness due to their pedagogical approach. The<br />
optimum transition course should be designed to cater to the unique needs of a student body, keeping in<br />
mind the demands of their specific clerkship sites. As a new medical school, UCF COM is well-suited for the<br />
implementation of such a program. In this study, we proposed to develop a peer-facilitated transition-toclerkships<br />
program for rising third year students. We initially identified the unique needs of our students by<br />
surveying charter class (class of <strong>2013</strong>) students. Feedback from this survey was used to design an<br />
interactive program to prepare rising third years in procedural skills, clinical infrastructure and student wellbeing.<br />
Lastly, the effectiveness of this program was evaluated by surveying both students and clerkship<br />
directors for perceived and actual readiness, respectively. There was a significant improvement in the mean<br />
22
ating of the program for class of 2014 (mean = 6) compared to class of <strong>2013</strong> (mean = 4.2), who were<br />
offered a more general orientation. Clerkship directors rated student performance for class of 2014 at a<br />
mean of 7.8 out of 10. Although we were successful in preparing students to handle the responsibilities of<br />
student clerks, as assessed by self- and mentor-evaluation, we plan to continue to collect feedback and<br />
outcome data in order to further improve student readiness for clinical training.<br />
UNIVERSITY OF CENTRAL FLORIDA COLLEGE OF MEDICINE [<strong>Poster</strong> # 41]<br />
Program/Project Title: Peer Academic Coaching and its effect on academic performance at UCF<br />
College of Medicine<br />
Presenter(s): Jennifer Bazemore & Omar Shakeel<br />
Email: jbazemore@knights.ucf.edu<br />
The Student Academic Support Services at the University of Central Florida College of Medicine (UCF COM)<br />
offers a variety of resources to help students learn as efficiently and effectively as possible. The Peer<br />
Academic Coaching (PAC) program was a student-driven initiative that was created to support fellow<br />
students as they adapt their study skills, test taking strategies, and personal habits to the demands of<br />
medical education.<br />
As part of our program, we developed several large group sessions including study skills sessions, test<br />
review sessions, and Step 1 board review sessions. Additionally, several small group sessions were<br />
facilitated and delivered. Student coaches also participated in individual coaching with other medical<br />
students.<br />
In this presentation, we will review the impact the PAC program has had on academics at UCF COM. We<br />
will present student perception of the PAC program and its effect on academic improvement, including an<br />
increase in USMLE Step 1 scores since the PAC program was implemented. Our goal is to convey that nearpeer<br />
teaching is a powerful study tool to utilize in the medical curriculum.<br />
UNIVERSITY OF CENTRAL FLORIDA COLLEGE OF MEDICINE [<strong>Poster</strong> # 42]<br />
Program/Project Title: Simulated Chaos: Adding Interactive Education to UCF COM’s Annual Global<br />
Health Conference<br />
Presenter(s): Erin Kane, Daniel Carlyle, Jennifer Bazemore & Omar Shakeel<br />
Email: ekane@knights.ucf.edu<br />
Purpose<br />
The second annual Global Health Conference sponsored by MedPACt (Medical Students Providing Across<br />
Continents) focused on disaster preparedness and emergency medicine, highlighted by a half day of<br />
interactive simulations. Participants engaged in six different simulations designed with specific learning<br />
objectives in mind to further the participant's knowledge of various maladies and situational decision-making<br />
skills. Following each set of learning objectives, individual simulations were designed to include a short<br />
briefing by student and physician instructors, a 15-20 minute simulated experience, and a debrief including<br />
instructor feedback and participant Q&A. Simulations included a mass casualty scenario with rapid triage,<br />
life-saving intervention with limited supplies (featuring interactive mannequins), grief counseling, burn<br />
treatment, and patient stabilization and evacuation both with and without standard medical supplies. Three of<br />
the scenarios followed a longitudinal story of one patient from the mass casualty scene through life-saving<br />
treatment and culminating with counseling.<br />
Players<br />
Participation included UCF faculty, community physicians, local EMS crews, and students from universities<br />
and medical schools across Florida. The simulations were designed and implemented by medical students.<br />
Two Directors of Simulations designed and implemented the scenarios, including creation of learning<br />
objectives, community contact, and participant training. Participation from the student body included Student<br />
Instructors who were paired with physicians to lead simulations, voice actors to give life to the SimMann 3G<br />
computerized mannequins, and moulaged triage and burn victims who brought varying degrees of life and<br />
theatrical presence to their simulations. UCF COM faculty and community physicians led and participated in<br />
five of the simulations, providing representation from several fields and areas of disaster response<br />
experience. The Clinical Simulations Department provided training, supervision, and use of the computerized<br />
23
mannequins. Professional make-up artists brought movie magic to the triage scenario. Two community<br />
members accustomed to working with our Clinical Skills Department volunteered their services as<br />
standardized patients for grief counseling, bringing their theatrical skills and tears. Orange County Fire<br />
Rescue provided a six person educational team to help students walk in the shoes of rescue personnel.<br />
When not sounding the sirens to start the mass casualty scenario, the ALS team gave tours of the<br />
ambulance during breaks. Last, but not least, the American Red Cross donated one of their refrigerated<br />
trucks to help keep cold water and snacks readily available due to the hot Florida sun.<br />
Program Impact<br />
Ultimately, the coordination of the Central Florida medical community with student leadership provided a<br />
unique, interactive learning experience for students from five Florida universities, including students from<br />
medical, nursing, undergraduate, and graduate schools. The simulation format was developed to be<br />
sustainable for future annual conferences and long-lasting community relationships.<br />
UNIVERSITY OF CENTRAL FLORIDA COLLEGE OF MEDICINE [<strong>Poster</strong> # 43]<br />
Program/Project Title: UCF College of Medicine Global Health Conference "Emergency and Disaster<br />
Medicine"<br />
Presenter(s): Daniel Carlyle<br />
Email: dcarlyle@knights.ucf.edu<br />
The University Of Central Florida College Of Medicine's MedPACt (Medical Students Providing Across<br />
Continents) organization is dedicated to providing education and mentoring for students to become actively<br />
engaged within communities of need both locally and abroad, and to promote awareness and participation in<br />
improving the health-related needs of people throughout the world. Our school holds a unique two day<br />
conference each year that encourages collaboration between medical students across the state in order to<br />
learn and share new initiatives in global health. This year, the conference theme was "Emergency and<br />
Disaster Medicine" held on January 12th-13th, <strong>2013</strong>. The conference featured Dr. Erik Noji, emergency<br />
medicine attending and full time faculty at Johns Hopkins University School of Medicine, who coordinated<br />
Domestic and International response at the CDC and Director of WHO's Collaborating Center for Disaster<br />
Preparedness. Additionally, the conference featured speakers Anne Cummings, International Branch Chief in<br />
the U.S. Department of Health and Human Services Office of Preparedness and Emergency Operations, and<br />
Dr. Luis Vasquez who is champion of the Yantalo Foundation, a medical humanitarian aid to the people of<br />
Peru. The conference also featured spectacular simulations placing students in real emergency situations<br />
including triage, counseling, burns, rapid extractions, and more. Small group workshops allowed students to<br />
interact and discuss about their experience during the conference with groups and speakers such as Medical<br />
Reserve Corps, American Red Cross, Solving Mass Toxicity in Bangladesh, Emergency Communication<br />
Networks, and Wilderness Medicine Workshop. Medical schools across Florida attended annually. Overall<br />
the conference increased awareness of the major players and roles of the medical profession in Emergency<br />
and Disaster Medicine.<br />
UNIVERSITY OF COLORADO SCHOOL OF MEDICINE [<strong>Poster</strong> # 44]<br />
Program/Project Title: Step 1 Pubquiz<br />
Presenter(s): Regina Kwon<br />
Email: regina.kwon@ucdenver.edu<br />
The summertime Step 1 Pubquiz was begun at the University of Colorado School of Medicine as a relaxing,<br />
collegial way to review the material learned in the first year of classes. This event was designed with multiple<br />
objectives:<br />
(a) to offer students a non-threatening way to start preparing for USMLE Step 1;<br />
(b) to encourage socializing for students who, without classes, might isolate themselves; and<br />
(c) to promote retention of first-year material using testing rather than rereading questions and self-score<br />
their results.<br />
The Step 1 Pubquiz was a well-received, low-cost method of supporting student learning. We believe that<br />
this program can easily be replicated at other schools. To facilitate this, we have created a customizable<br />
24
toolkit that includes all materials needed plus a brief guide for setting up a Step 1 Pubquiz, and this toolkit will<br />
be provided to any interested attendees.<br />
UNIVERSITY OF FLORIDA COLLEGE OF MEDICINE [<strong>Poster</strong> # 45]<br />
Program/Project Title: Journal Club in Preclinical Years: Five Easy Steps to Success<br />
Presenter(s): Samuel Lipten & John Lindsey<br />
Email: samlipten@ufl.edu<br />
While journal clubs are common among graduate students and medical residents, they are rare among preclinical<br />
medical students. We started an informal journal club, with discussion of both a clinical case and an<br />
original research article led by a rotating presenter. Our objectives were threefold: to improve clinical acumen<br />
in a low-stress environment, to learn practical biostatistics, and to provide a forum for curiosity and wonder in<br />
the first two years of medical school. In our poster we will describe the history and importance of journal<br />
clubs in medical education, the lessons we've learned through starting our own journal club, and five key<br />
pieces of advice for medical students wishing to found clubs at their own institution.<br />
UNIVERSITY OF FLORIDA COLLEGE OF MEDICINE [<strong>Poster</strong> # 46]<br />
Program/Project Title: Peer Academic Enrichment Program<br />
Presenter(s): Tene Sablo & Ella Uwaibi<br />
Email: tsablo@ufl.edu<br />
Starting medical school can be a difficult transition for students. They can struggle with academic<br />
performance, developing effective study methods, adjusting to the rigorous pace, and dealing with the<br />
psychological pressures of medical school. In order to help alleviate some of these difficulties, several<br />
medical schools have developed pre-matriculation programs. Historically, pre-matriculation programs have<br />
been residential summer programs that targeted students under-represented in medicine, non-traditional<br />
students, and non-science majors.<br />
A needs assessment for the University of Florida College of Medicine (UF COM) was conducted by<br />
implementing focus groups comprised of students from the UF COM Class of 2016. Students were asked<br />
questions about their experiences and opinions regarding their transition into their first year of medical<br />
school. An analysis of the transcriptions of the focus groups suggested several common themes, including:<br />
difficulties establishing studying techniques; struggles with finding a study group, and the need for academic<br />
mentorship from upperclassmen. Results of the analysis also indicated that UF COM students would<br />
recommend a longitudinal program over a traditional pre-matriculation program.<br />
Therefore, in August <strong>2013</strong> we developed an optional on-campus Peer Academic Enrichment Program<br />
(PAEP), which was made available to all incoming first year UF COM students. The Peer Academic<br />
Enrichment Program is comprised of two components: (1) peer-led academic support workshops to teach<br />
incoming students the study skills needed to foster success in the medical school curriculum; (2) a peer<br />
mentorship component to provide incoming students with social/emotional support, encouragement, and<br />
guidance.<br />
On August 12, <strong>2013</strong> an academic skills workshop was offered to students in the UF COM Class of 2017.<br />
Approximately 40 students attended. The first hour entailed a study skills lecture given by fourth year<br />
students. During the second hour, the first year students had the opportunity to attend a small group session<br />
based on their learning style. We have designed future academic support workshops that will be held at<br />
several key academic transition points during the first year curriculum.<br />
The peer mentorship component was designed to function as a support group for students. Approximately<br />
70 second, third, and forth year students volunteered to participate in this program. These students were<br />
asked to respond to biography questions, complete a learning style assessment, and also identify what<br />
specialty areas they were interested in. The student mentors were then divided in to 16 teams. This<br />
information was provided to the first year students in the class of 2017 so that they could choose the team<br />
that they felt would best suit their needs. These teams will meet a minimum of four times during the school<br />
year to discuss topics such as: (1) adjustment to medical school; (2) difficulty with coursework; (3) balancing<br />
school with your personal life; (4) stress reduction.<br />
25
The participants evaluated the first session by rating several descriptive statements on a scale of 1-5 (1-<br />
Strongly Disagree, 5-Strongly Agree). The means for all evaluation categories were greater than 4.4, which<br />
indicated that the UF COM Peer Academic Enrichment Program was helpful in assisting students with their<br />
transition to medical school.<br />
UNIVERSITY OF ILLINOIS COLLEGE OF MEDICINE [<strong>Poster</strong> # 47]<br />
Program/Project Title: Initiative to Increase Medical Student Awareness of LGBT Health Disparities<br />
Presenter(s): Marcus Gustafsson<br />
Email: gustafssonbm@gmail.com<br />
The <strong>AAMC</strong> Group on Diversity and Inclusion has made a call for inclusion of LGBT medical education in<br />
undergraduate and graduate medical education. The goal is to address health disparities and discrimination<br />
in the LGBT patient population. Faculty and students at UIC-COM have made a commitment to answer this<br />
call through curricular revision and student driven initiatives. A great majority of medical students feel<br />
unprepared to work with LGBT patients and are unfamiliar with LGBT issues.<br />
Curriculum integration examples:<br />
• Core clinical preparation course includes a session dedicated to LGBT education and an interactive<br />
panel where students hear from LGBT patients about their health care experience.<br />
• The Patient Centered Medicine program available to interested students includes a track focused on<br />
HIV/AIDS.<br />
Student initiatives examples:<br />
• The student council at UIC-COM approved and added the Diversity in Healthcare track to the Leadership<br />
Certificate program with a focus on health disparities in minority populations, including LGBT.<br />
• Student organizations collaborated to hold a series of events themed "The LGBT patient."<br />
• "Big sib" mentor program pairs incoming LGBT students with current LGBT student.<br />
The effort includes further integration in clinical years and residency programs and more changes are<br />
planned due to positive student on current initiatives.<br />
UNIVERSITY OF IOWA ROY J. AND LUCILLE A. CARVER COLLEGE OF MEDICINE [<strong>Poster</strong> # 48]<br />
Program/Project Title: Carver Rural Iowa Scholars Program (CRISP)<br />
Presenter(s): Timothy Bahr, Anne Thompson & Tyler Bertroche<br />
Email: joseph-bertroche@uiowa.edu<br />
In order to address the growing shortage of rural physicians, the Carver College of Medicine created the<br />
Carver Rural Iowa Scholars Program (CRISP) in 2012. This is a comprehensive program that provides<br />
individualized learning opportunities and financial incentives ($80-100,000 in loan repayment) for medical<br />
students to pursue careers in rural medicine. Graduates of the program are expected to practice in an<br />
eligible community (population 20 miles from a city with a population >50,000) for<br />
a minimum of five years after they complete a residency in pediatrics, family medicine, internal medicine,<br />
general surgery, or psychiatry. Acceptance to the program is competitive and is currently limited to Iowa<br />
residents. Applicants from Iowa accepted to the Carver College of Medicine for fall matriculation may apply<br />
to the program in March. Each year, four applicants are selected.<br />
Students begin the program in the summer prior to matriculation by shadowing a rural physician for at least 1<br />
week. In the M1 year, students are required to shadow a rural physician and begin monthly interactions with<br />
a physician mentor. Following the M1 year, students participate in a Medical Education in Community<br />
Orientation program for 4-12 weeks. This program provides a stipend for students to observe and work with<br />
physicians in rural settings. Students also participate in a 3-day field experience in rural medicine that covers<br />
relevant public health concerns. In the pre-clinical curriculum, CRISP students are placed in small groups<br />
with faculty interested in rural medicine as part of the Foundations of Clinical Practice courses. Students in<br />
the program also complete a Rural Health and Agricultural Medicine course in their M2 year. A seminar<br />
series offered by the Rural Medicine Interest Group offers additional enrichment four times each year.<br />
CRISP students begin a community-based research project in their M2 year and present a Rural Capstone<br />
26
project before graduation. In the clinical years, CRISP participants are required to complete continuity of<br />
care experiences at a rural site, participate in a telemedicine elective, and attend a state or national<br />
conference in rural medicine.<br />
UNIVERSITY OF IOWA ROY J. AND LUCILLE A. CARVER COLLEGE OF MEDICINE [<strong>Poster</strong> # 49]<br />
Program/Project Title: Electronic Medical Records – Advanced Training for Medical Students<br />
Presenter(s): Tyler Bertroche<br />
Email: joseph-bertroche@uiowa.edu<br />
Over the past several years, there has been a large push to train medical students in the use of electronic<br />
medical records (EMR). The Carver College of Medicine recognized this need, and recently started a<br />
program to better prepare our students for the use of EMR. The goal of this project is to: (1) ensure students<br />
become proficient in the use of EMR, (2) allow students to contribute to the documentation of patient care<br />
during their clinical years, and (3) facilitate an easy transition for students to use electronic records in<br />
residency programs.<br />
Beginning in the fall of <strong>2013</strong>, medical students are introduced to the use of EMR during their first-year<br />
courses. Case-based learning sessions have provided an ideal, small-group environment to teach the use of<br />
EMR. In the past, these sessions relied solely on paper copies of our simulated cases. These cases now<br />
exist as simulated patients using the actual electronic record program used by University of Iowa Hospitals<br />
and Clinics. Students learn to access a patient’s prior and current medical history, interpret lab values, order<br />
tests, and view radiographs. These learning sessions span the pre-clinical years and allow students to<br />
become more proficient at using the electronic record. Third and fourth year students receive additional<br />
training for the use of EMR. Students are allowed and expected to access patient information, document<br />
clinic and consult notes, and help manage patient care using electronic records during their clinical rotations.<br />
The EMR program has been designed to forward all student-written notes to the faculty for review and<br />
feedback. In this way, students learn how to write comprehensive clinical notes under the guidance of staff<br />
physicians.<br />
Through these programs, the Carver College of Medicine has allowed students to learn how to use EMR in<br />
both simulated and real-life settings. Students have responded positively to these changes, and the<br />
opportunity to improve their skills in documenting patient care. The University will continue to monitor student<br />
progress in developing EMR proficiency and solicit feedback from students and faculty.<br />
UNIVERSITY OF KENTUCKY COLLEGE OF MEDICINE [<strong>Poster</strong> # 50]<br />
Program/Project Title: Community Health Fair- Making Compassion our Tradition<br />
Presenter(s): Kristina Pescosolido<br />
Email: raevti.bole@uky.edu<br />
The poster describes a brief history of the University of Kentucky College of Medicine's community health<br />
fair. The fair has undergone over a decade of student lead transformation. A comparison between the<br />
demographics from this year's fair and those from socio-economically targeted Lexington zip codes was<br />
made in order to assess our effectiveness at reaching out to those medically under-served in our community.<br />
Interviews from health fair participants gave insight into their immediate health concerns. The goal of this<br />
poster is to highlight the Fair's most utilized services including the student run clinic, women's health<br />
screenings, nutrition counseling, and dental screening, among many others. Equipped with this information<br />
we hope that future classes will expand upon and continually improve the effectiveness of the fair.<br />
UNIVERSITY OF MIAMI LEONARD M. MILLER SCHOOL OF MEDICINE [<strong>Poster</strong> # 51]<br />
Program/Project Title: DOCS Community Outreach Conference and Retreat<br />
Presenter(s): Danielle Neuman, Nicole Stanford & Rimsky Denis<br />
Email: drneuman@med.miami.edu<br />
The Department of Community Service (DOCS) is a student run, non-profit organization of the University of<br />
Miami Miller School of Medicine. DOCS develops, coordinates, and aids in the implementation of student-run<br />
community health initiatives including nine health fairs, two weekly free clinics, and one community outreach<br />
conference.<br />
27
The DOCS Community Outreach Conference and Florida Keys Retreat is an opportunity for student leaders<br />
from different medical schools across the country to share their models of student-run community service<br />
organizations, discuss some of the biggest challenges student-run organizations face, and get hands-on<br />
experience at the University of Miami Miller School of Medicine’s biggest health fair of the year in the Florida<br />
Keys.<br />
Through the DOCS Community Outreach Conference and Retreat, attendees have the opportunity to<br />
discuss common challenges that medical student organizations across the nation face in planning and<br />
implementing community health projects. This is accomplished through power-point presentations given by<br />
each participating school, problem-solving breakout sessions, and interactive discussions. The large group<br />
wrap-up allows all of the retreat attendees to gather at the end of the day to discuss the problems brought up<br />
in each problem solving session and to collectively brainstorm solutions for these challenges. The attendees<br />
also learn how they can implement the DOCS model to help strengthen their own medical schools’<br />
community service efforts.<br />
The Retreat also provides hands-on experience as attendees are paired-up with a DOCS student leader<br />
while they volunteer at the DOCS Florida Keys Health Fairs. Retreat attendees are assigned to health fair<br />
sites in Key West or Big Pine Key, where they volunteer at two different health stations. This experience will<br />
demonstrate the ability of a comprehensive community screening health fair to deliver valuable care and<br />
education to underserved communities and provide attendees with the opportunity to see the DOCS model<br />
of community service in action while working closely with patients and faculty.<br />
Thus far, forty-six students, representing twenty-one medical schools across the country and Canada, have<br />
attended the DOCS Community Outreach Conference and Retreat. After the weekend, we hope that our<br />
attendees find themselves empowered to implement the key concepts they learned at the conference in<br />
order to make impactful changes at their respective schools and communities.<br />
UNIVERSITY OF MINNESOTA MEDICAL SCHOOL, TWIN CITIES [<strong>Poster</strong> # 52]<br />
Program/Project Title: Phillips Neighborhood Clinic: Providing Health Care Access to the Underinsured<br />
Presenter(s): Joseph Valentin<br />
Email: valen243@umn.edu<br />
The Phillips Neighborhood Clinic (PNC) is a free clinic located in Minneapolis, Minnesota. There are two<br />
objectives in the clinic’s mission: to provide health care access for the underinsured population in the<br />
Minneapolis area and to offer University of Minnesota health professional students the skills and experience<br />
to serve patients who are in need of medical access. PNC operates on Mondays and Wednesdays during<br />
the evenings, it is ran by a team of volunteer students and professionals from the schools of Medicine,<br />
Physical Therapy, Pharmacy, Nursing and Public Health. Together all of these volunteers, with the<br />
supervision of licensed clinicians, are able to provide clinical services such as: blood pressure monitoring,<br />
mental health, women’ health, pediatrics, physical exams, laboratory testing and many others. The clinic<br />
opened its doors in 2003, operating one night per week. However, in 2009 PNC started providing service two<br />
nights per week serving around 1000 patients per year. This clinic is especially important for the Hispanic<br />
community living in Minneapolis since for many of them English is not their native language, therefore PNC<br />
provides Spanish interpreters to many of these immigrants so they can feel that language is not a barrier for<br />
health care access. Phillips Neighborhood Clinic has had a tremendous impact on the underinsured<br />
Minneapolis community, especially the Latino population, for the past 10 years. It is my goal to highlight<br />
PNC’s impact for its patients, how its model has succeeded and can be used in other parts of the country to<br />
serve those in need of accessible and appropriate free health care services.<br />
UNIVERSITY OF MISSISSIPPI SCHOOL OF MEDICINE [<strong>Poster</strong> # 53]<br />
Program/Project Title: Community Health Advocacy Project<br />
Presenter(s): Wilfreda J. Lindsey<br />
Email: wlindsey@umc.edu<br />
INTRODUCTION. Mississippi leads the nation in many chronic diseases. The limited number of primary care<br />
providers coupled with low health literacy in many regions in the state exacerbates this issue. The<br />
community health advocacy (CHA) project was begun to reduce health disparities in the state of Mississippi<br />
28
y empowering the community and by partnering with academic medical centers and faith-based<br />
communities. The goal of community health advocacy is to train individuals who will increase health<br />
awareness and literacy leading to the improved health status of individuals within the community. Students<br />
were given basic clinical training such as taking blood pressure, blood glucose levels, and calculating body<br />
mass index. Students were also given skills in areas such as addressing health literacy, learning to read<br />
prescriptions, planning healthy and balanced meal portions, and helping individuals gain access to health<br />
care. The ultimate goal of the CHA program is to enable the students to be able to train others to serve as<br />
community health advocates throughout the state so that lay community health advocates can work with<br />
health care professionals on health literacy. These trained lay community advocates will be able to perform<br />
health screenings for obesity, diabetes, hypertension, and blood fat abnormalities and will be able to refer<br />
those patients requiring healthcare to accessible facilities. One hundred and thirty-five medical students have<br />
been trained and over ten community sessions have been scheduled.<br />
METHODS. Students attended two lectures detailing the aspects of the community health advocacy program<br />
before receiving hands on training. Clinical skills were practiced on other medical students. Students took<br />
each other’s’ blood pressure, blood glucose, and body mass index. Students also received nutrition training<br />
and received community health advocate certificates after demonstrating mastery of the assigned tasks.<br />
RESULTS. At the completion of the course, medical students were trained community health advocates with<br />
an increased knowledge of the state's chief disease processes as well as the disease's epidemiology.<br />
CONCLUSION. Medical students attended detailed lectures and received hands-on training to become<br />
Community Health Advocates. Upon successful completion of the Community Health Advocacy program,<br />
students were equipped to measure blood pressure, blood glucose levels, and body mass index, as well as<br />
give nutritional counsel. Students are now in the process of getting trained to lead community sessions that<br />
will improve health literacy and address health disparities throughout Mississippi.<br />
UNIVERSITY OF MISSISSIPPI SCHOOL OF MEDICINE [<strong>Poster</strong> # 54]<br />
Program/Project Title: Dynamics of a Multidisciplinary Student Run Free Clinic<br />
Presenter(s): Clark Walker<br />
Email: cwalker2@umc.edu<br />
The Jackson Free Clinic is a 501(c)(3) non-profit corporation operated by 18 medical students of the<br />
University of Mississippi Medical Center School of Medicine, along with volunteer physicians from the local<br />
community. The student-run Jackson Free Clinic was created to increase access to health care and assist in<br />
restoring health to an underserved population. A little over one year ago the 18 medical students who made<br />
up the board of directors of the JFC had a vision to expand not only the physical structure of the free clinic,<br />
but also the services provided. After launching a capital campaign to renovate and expand the clinic and<br />
raising over $300,000, the board of directors set their sights on further meeting the needs of their patient<br />
population by incorporating the Schools of Dentistry, Nursing, Pharmacy, and School of Health Related<br />
Professions (PT/OT) into the board of directors and as a part of the services provided at the Jackson Free<br />
Clinic. As of today, the Jackson Free Clinic has student representatives from the Schools of Dentistry,<br />
Nursing, Pharmacy, and Health Related Professions who are a part of the board of directors and volunteer<br />
weekly. Patients of the JFC now have access to a multitude of medical services all provided free of charge<br />
by students and local community physicians who volunteer each week. The original vision of the 18 medical<br />
student board members to broaden the scope of healthcare services provided at the JFC has been<br />
implemented and will continue to grow as the current board pursues the incorporation of even more<br />
healthcare disciplines into the Jackson Free Clinic to further serve their patients.<br />
UNIVERSITY OF MISSISSIPPI MEDICAL CENTER [<strong>Poster</strong> # 55]<br />
Program/Project Title: Incorporating Business Medicine Preparedness in the Medical Curriculum<br />
Presenter(s): Megan Storm<br />
Email: Mstorm@umc.edu<br />
Incorporating Business Medicine Preparedness into the Medical Curriculum<br />
Storm, MV; Husband, LD.<br />
29
Problem:<br />
Most medical school curriculums only provide basic science and clinical education, without formal exposure<br />
to practical business elements relevant to medicine (e.g., billing, reimbursement payment models, or practice<br />
management and expenses). 1 Not understanding medical business allows inappropriate financial planning<br />
and decreased efficiency, which ultimately increases patient care costs. 2<br />
Objective:<br />
The University of Mississippi Medical Center’s (UMMC) Department of Family Medicine’s business in<br />
medicine workshop provides every UMMC medical student exposure to the interplay between insurance,<br />
coding, and patient care costs as well as the basics of practice management.<br />
Program Description:<br />
Starting in 2002, UMMC’s Department of Family Medicine implemented a business in medicine workshop as<br />
part of the clerkship orientation. The workshop involves lectures, problem-based learning, and scenariobased<br />
learning.<br />
The business in medicine workshop starts with an introduction to International Classifications of Diseases-<br />
9th Revision (ICD-9) and Current Procedural Terminology coding systems and their use in patient<br />
documentation and reimbursement. Students then learn the basic billing process by discussing allowable<br />
charges, non-allowable amount, and contractual adjustments. A hypothetical patient bill with different<br />
insurance companies (i.e. Medicaid, Medicare, BCBS, United HC, Cigna, Uninsured) is used to enrich<br />
discussion and demonstrate how insurance impacts business and patients. Students learn why CPT code<br />
reimbursement varies between companies. An overview of insurance negotiations helps students understand<br />
how to tailor these negotiations to their future practices, when to charge more or less for procedures, and<br />
how cash discounts can legally help the uninsured. These discussions are reinforced through Excel<br />
examples calculating sample payouts from different companies. Discussion on payment models including fee<br />
for service, diagnosis related groups, value based payment modifier, and the Accountable Care Act help<br />
students learn incentives, costs, advantages and disadvantages for different models. They receive an<br />
overview of payer classes and how percentages of charge payer mix predict expected income, serve as a<br />
model for budgeting expenses, as well as how to recognize problems if not receiving expected amounts.<br />
Excel examples are applied to convey the importance of payer mix analysis. Students receive an overview of<br />
expected expenses of running a practice and what percent of income should be spent on human resources,<br />
facilities, insurance and marketing. Students learn how efficiency and work flow in a clinic can reduce overall<br />
costs, the importance of quality staff members, which staff members qualify for hourly wage vs. exempt<br />
employees, how to manage overtime pay, and how nurse practitioners are utilized in practice.<br />
After learning the elements of the business-side of medicine students are introduced to the basics of medical<br />
billing. A certified medical coder discusses the purpose of medical coding, the importance of documentation,<br />
and how the coding process functions. Students receive a sample doctor’s note and instructions on how to<br />
extract information from the note to determine the appropriate level of service for the visit. Afterwards,<br />
students create their own note based on a hypothetical patient visit. Students code the note individually, then<br />
as a group to see how leaving out details could change the level of service. The coding exercises culminate<br />
when students are given another note and asked to quickly assess the level of service based on their current<br />
knowledge.<br />
Once coding is complete, students apply their knowledge to a hypothetical patient. Small groups are formed,<br />
and each is provided with an imaginary $3500, list of procedure and laboratory costs, patient age, and chief<br />
complaint. Groups develop a differential diagnosis, a plan, and decide which tests to order ranging from<br />
history, physical exam, x-rays, CT scans, various blood work and laboratory tests. Students are encouraged<br />
to think about which tests are most appropriate given the patient information and your differential diagnoses.<br />
Conclusion:<br />
Through various learning methods and activities, students are exposed to basic business elements they<br />
need in the medical field. Students have a broader understanding of aspects of medical billing,<br />
reimbursement, payment models and healthcare policy, payer mix analysis, expenses and budgeting,<br />
organizing a practice, the importance of documentation, and overall costs of patient care.<br />
30
References:<br />
1.(<strong>2013</strong>) Medical School Graduation Questionnaire <strong>2013</strong> All Schools Summary Report. <strong>AAMC</strong>. Retrieved<br />
September 16, <strong>2013</strong> from<br />
https://www.aamc.org/download/350998/data/<strong>2013</strong>gqallschoolssummaryreport.pdf. July <strong>2013</strong>.<br />
2.Kim, J. (2012, May/June) Teaching Medical Students about Management, Business, and Leadership. PEJ<br />
May/June 2012. Retrieved September 16, <strong>2013</strong> from http://www.physicianleaders.org/<br />
UNIVERSITY OF MISSISSIPPI SCHOOL OF MEDICINE [<strong>Poster</strong> # 56]<br />
Program/Project Title: Population Health Course at University of Mississippi<br />
Presenter(s): Turner Brown<br />
Email: jtbrown@umc.edu<br />
Physicians with a population health perspective are able not only to diagnose and treat illness but also to act<br />
on opportunities to prevent disease and promote health in their patients and to protect the health of the<br />
public. “Population Health, Disease Prevention and Health Promotion” is a one-semester course designed to<br />
achieve this by informing first year students of the unique challenges facing Mississippi and equip them to<br />
better serve the state as “population health-minded” clinicians. The course has three components:<br />
1. Self-guided learning – Students work through twelve self-study modules. Each module addresses<br />
diseases, conditions or health risk behaviors of public health importance in Mississippi and the U.S. Students<br />
must access online journal articles and reports, state health department websites, and online data sources to<br />
answer questions and complete each module.<br />
2. Integrative Case – Small mixed groups of medical and pharmacy students are allocated a topic of public<br />
health importance and are required to meet with faculty, do background research, and prepare a poster for<br />
presentation. The aim of this component is to use a clinical case to illustrate the interrelatedness of<br />
preclinical, clinical and public health knowledge and practice – in particular, the relevance of public health<br />
and epidemiology to clinical practice. This activity links students with mentors from different areas<br />
(preclinical, clinical, and public health). Additionally, the case gives students experience in presentation skills<br />
and inter-professional communication.<br />
3. Community Health Advocacy (CHA) Training – CHA training is a practical component that teaches<br />
students how to conduct basic health screening tests for obesity, diabetes, hypertension and blood lipid<br />
abnormalities, and refer those patients requiring health care to accessible health facilities. Students learn to<br />
check blood pressure, perform blood glucose tests, measure BMI, and how to give general nutrition advice.<br />
Following course completion, students are certified to participate in one (or more) of the various health fairs<br />
in the local area and teach health advocacy courses in the community.<br />
Traditionally, medical school teaches students how to diagnose and treat illness in individual patients. This<br />
course adds a population health perspective and “plants the seed” of disease prevention and health<br />
promotion. By introducing students to public health programs, resources and data, students are better<br />
equipped to interact with public health agencies and become involved with programs and interventions that<br />
address the important public health issues in the state. Additionally, CHA training provides students a<br />
patient-centered, practical experience prior to clinical rotations. Finally, interaction with physician mentors<br />
and practice with group presentation encourages professionalism and communication.<br />
UNIVERSITY OF MISSISSIPPI SCHOOL OF MEDICINE [<strong>Poster</strong> # 57]<br />
Program/Project Title: Students Leading Students: A Model for Increasing Student Professionalism<br />
Presenter(s): Summer Bailey (with help from Dr. Peggy Davis)<br />
Email: ssbailey@umc.edu<br />
In 2005, the University of Mississippi Medical Center established a Professionalism subcommittee, as a part<br />
of the School of Medicine Curriculum Committee, with the charge of organizing and promoting<br />
professionalism throughout the medical school curriculum. In 2008, a medical student was appointed to the<br />
committee. The value of this student’s insight was quickly recognized. The following year another medical<br />
31
student who expressed interest in professionalism and leadership was invited to join. This student’s work<br />
resulted in establishment of the Student Professionalism Project (SPP) for M1 students with a goal to help<br />
ease the M1 transition into the demanding environment of professional school. Fueled by positive student<br />
response, especially regarding peer leadership, the decision was made to add more student members to the<br />
Professionalism subcommittee. All student members have a role in teaching and participation in some<br />
capacity. We believe that increasing student participation in professionalism activities has brought new<br />
energy and vigor to the cause of professionalism. The Student Professionalism Project, in which student<br />
leaders model and teach professional behavior, is now an established part of the M1 curriculum. Student<br />
interest in participating in other professionalism activities, such as the institution’s Quality Enhancement<br />
Program which also has an emphasis on professionalism is also on the upswing.<br />
In conclusion, the Student Professionalism Project has evolved from the work of an individual student to an<br />
established student group with responsibility for part of the M1 curriculum. Encouraging student leaders to<br />
teach and exemplify professional behavior among peers has brought about a positive momentum, evidenced<br />
by increased interest in participation among freshmen medical students. This perpetuation of student<br />
professionalism will continue to foster the objectives and goals of the Professionalism Project over the years<br />
to come.<br />
UNIVERSITY OF MISSISSIPPI SCHOOL OF MEDICINE [<strong>Poster</strong> # 58]<br />
Program/Project Title: The Health Partnership Program: Affecting Healthy Change Using Motivational<br />
Interviewing<br />
Presenter(s): Hal Flowers & Elliott Welford<br />
Email: rhflowers@umc.edu, ewelford@umc.edu<br />
As the obesity epidemic grows in our country, primary care clinics will continue to be at the forefront of<br />
prevention and treatment of obesity and its associated chronic diseases. Experimentally validated methods<br />
to help patients create healthy change in their lives, such as Motivational Interviewing (MI), will be most<br />
useful in helping patients in these settings. In this context, students of the University of Mississippi Medical<br />
Center (UMMC) have established the Health Partnership Program, which has two components: a nine-hour<br />
Motivational Interviewing course for students, and a 10-session partnership program that pairs student and<br />
patient. MI is a patient-centered counseling approach that is particularly useful for medical students, whose<br />
clinic knowledge may be limited by lack of experience but whose empathy and desire to affect change is<br />
fresh and abundant. The patients that our students pair with are from the Jackson Free Clinic, run by<br />
students from UMMC. This partnership component of the program consists of ten counseling sessions, both<br />
over the phone and in the clinic, at regular intervals over six months, and it seeks to empower patients to be<br />
the agents of healthy changes in their lives. Empirical measures of the program’s efficacy will be weight and<br />
waist circumference, with the prediction that decreases in all measures will be seen after the six-month<br />
program. This presentation will focus on the program’s implementation, successes, obstacles, and future.<br />
UNIVERSITY OF NORTH DAKOTA SCHOOL OF MEDICINE AND HEALTH SCIENCE [<strong>Poster</strong> # 59]<br />
Program/Project Title: LCME Independent Student Analysis<br />
Presenter(s): Craig Meiers, Anna Cymbaluk, Andrew Mills, Michael Jordan & Kenneth Ruit<br />
Email: craig.meiers@my.und.edu<br />
An Independent Student Analysis for our upcoming LCME accreditation visit displaying how the students<br />
organized themselves as well as the required steps and successful implementation of the student survey,<br />
data analysis, and ISA report development. This is important information for students who are about to enter<br />
into this process.<br />
UNIVERSITY OF OKLAHOMA HEALTH SCIENCES CENTER COLLEGE OF MEDICINE [<strong>Poster</strong> # 60]<br />
Program/Project Title: Changing to a systems-based curriculum: A four year retrospective<br />
Presenter(s): Ryan Makipour, Phillip Bonney & Bahar Malakouti<br />
Email: ryan-makipour@ouhsc.edu<br />
In 2009 the University of Oklahoma Health Sciences Center College of Medicine (OUCOM) changed its<br />
curriculum to systems-based curriculum. This year, OUCOM will be graduating its first class to complete their<br />
medical education under the new systems-based curriculum. Changes to the curriculum included: 1) the<br />
32
eplacement of semester long courses with the introduction of 4- to 10-week systems courses, 2) switching<br />
to a pass/fail/honors grading system for preclinical courses, 3) the addition of National Board of Medical<br />
Examiners (NBME) finals for each systems-based course, and 4) the addition of a 10-week capstone course<br />
with a Cumulative Basic Sciences Exam (CBSE) final exam to conclude preclinical courses. After the initial<br />
curriculum change, adjustments included increasing the number of NBME finals for systems based courses,<br />
resulting in the class of 2016 taking a NBME final for every systems-based course. Increases in average<br />
USMLE Step 1 scores and pass rates (when compared to the six-year average of the traditional curriculum)<br />
were seen after the implementation of the new curriculum. The USMLE Step 1 data for Classes of 2014 and<br />
2015 exhibit the implementation of the systems based curriculum, as compared to the six-year average for<br />
the Classes of 2007-<strong>2013</strong>. Among first time test takers, the Classes of 2014 and 2015 saw a 5% and 7%,<br />
increase in average USMLE Step 1 score compared to the six-year OUCOM score, respectively. Pass rate<br />
jumped from 91% (traditional curriculum) to 96% and 98% (systems-based curriculum). The data illustrates<br />
the greatest increase the year after initial implementation of the new curriculum; furthermore, progress was<br />
made in the subsequent year due to adjustments to the curriculum.<br />
UNIVERSITY OF SOUTH FLORIDA HEALTH MORSANI COLLEGE OF MEDICINE [<strong>Poster</strong> # 61]<br />
Program/Project Title: SuperUtilizer Project<br />
Presenter(s): Alexandra Printz<br />
Email: aprintz@health.usf.edu<br />
Working with administration, several students created a `Superutilizer Project' added to the 3rd year<br />
Longitudinal Primary Care Clerkship curriculum. The objective of this project was for students to identify a<br />
`superutilizer' at their family practice. Patients were identified based on the Camden Coalition criteria, which<br />
include multiple chronic conditions and more than 3 ER visits or inpatient admissions in the past 6 months.<br />
Students then perform a home visit, working with nurses and social workers to assess the patient's needs<br />
and limitations in accessing care. If the patient is interested, the team enrolls them in the Camden Coalition<br />
project and begins to provide them with the resources they need to improve their health and lower their<br />
healthcare utilization.<br />
For students who are interested in being more involved, an option was created to have students spend 50%<br />
of their Longitudinal Family Practice experience with the `Superutilizer Project'. This allows those students to<br />
work more closely with the project's interdisciplinary team, and serve as a `health coach' for patients. In this<br />
role students perform weekly home visits, accompany patients to appointments, and help them navigate their<br />
health.<br />
By the end of the year we will have brought the `Hot Spotter' model to over a dozen providers in the<br />
community, and had students work one on one with over 20 patients living with chronic disease. Meanwhile,<br />
student leaders work to collect data to measure the impact of the project on the healthcare utilization of our<br />
`superutilizers'.<br />
Our poster will include on overview of the concept of 'Hot Spotters', and a step-by-step of how we<br />
implemented the program.<br />
UNIVERSITY OF SOUTH FLORIDA HEALTH MORSANI COLLEGE OF MEDICINE [<strong>Poster</strong> # 62]<br />
Program/Project Title: USF Health Veterans Success Network<br />
Presenter(s): Tom Fowler, Josiah Hill & Anthony Desantis<br />
Email: tfowler2@health.usf.edu<br />
The Tillman Military Scholars at USF Morsani College of Medicine (MCOM) saw a need to 1) increase<br />
education about veterans’ health issues among health professions students 2) increase educational avenues<br />
for veterans desiring a career in healthcare and 3) create a veteran-focused professional development<br />
community. Working off of the <strong>AAMC</strong>'s collaboration with the Joining Forces Initiative, we are creating a<br />
program that will strategically ease the transition of veterans into a healthcare career. Called the USF Health<br />
Veterans Success Network, the program has formalized partnerships with the Department of Veterans<br />
Affairs, the Pat Tillman Foundation, and the Got Your 6 Foundation. We plan to launch the initiative in<br />
November on Veterans Day weekend.<br />
33
Through education, interpersonal engagement, and mentorship, the USF Health Veterans Success Network<br />
will enhance the academic journey of healthcare professions students and faculty, helping us provide<br />
enhanced care to the community of veterans which we have the honor to serve.<br />
UNIVERSITY OF TEXAS SOUTHWESTERN MEDICAL CENTER SOUTHWESTERN MEDICAL SCHOOL<br />
[<strong>Poster</strong> # 63]<br />
Program/Project Title: Innovating Healthcare Solutions (IHS) @ UT Southwestern<br />
Presenter(s): Anu Atluru<br />
Email: a.atluru@gmail.com<br />
Academic and extracurricular opportunities in healthcare innovation at UTSW have expanded rapidly,<br />
supporting the strong interest from students and the need for physician-innovators in the evolving U.S.<br />
healthcare system. The Innovating Healthcare Solutions program (IHS) is a year-long, experiential program,<br />
medical and graduate students at UTSW acquire the skills and mindset required to accurately assess<br />
problems and develop feasible solutions in a team based environment. Using these skills and the aid of<br />
course facilitators and faculty advisors, students tackle real world healthcare challenges locally and abroad<br />
by designing products (Product Track) or implementing community-based initiatives (Initiative Track). The<br />
program has formal partnerships with the Office of Global Health, Community Action & Research, Office of<br />
Quality Improvement, and the Dallas BioCenter, as well as UT Arlington Engineering and UT Dallas<br />
Business, allowing the creation of truly multi-disciplinary project teams. By formalizing and broadening<br />
access to institutional and industry support, the impact of experiential education and the likelihood of success<br />
for teams is enhanced. A new elective, Clinical Needs-Finding, was piloted this summer and serves two<br />
roles. First, medical students learn to effectively identify, understand, and evaluate unmet clinical needs<br />
during an immersive clinical experience (volunteering at the ER, medical service trips, clinical rotations),<br />
allowing them to, at the very least, develop an innovative mindset that stays with them throughout their<br />
residencies and practice as physicians. The unmet needs generated through the elective also provide a<br />
continuous pipeline of challenges to be tackled by the students themselves and/or teams in the IHS course.<br />
Currently, IHS projects are often continued as capstone projects for the existing M.D. distinction programs in<br />
Global Health and Community Action & Research. By 2016, we aim to grow the suite of healthcare<br />
innovation courses offered at UTSW and to enable establishment of a separate, one of a kind M.D.<br />
distinction program in Clinical Innovation.<br />
UNIVERSITY OF UTAH SCHOOL OF MEDICINE [<strong>Poster</strong> # 64]<br />
Program/Project Title: Interprofessional Education in Health Sciences at the University of Utah<br />
Presenter(s): Matt Lamont & Erin Anstadt<br />
Email: m.lamont@hsc.utah.edu<br />
At the University of Utah, a program has been implemented among health sciences to promote<br />
interprofessional learning and teamwork. Interprofessional Education (IPE), is a required course that offers<br />
collaborative experiences during each of the four years of medical school. During these experiences, we<br />
work with students from nursing, PA, pharmacy, PT, and OT. We gain better insight into their roles, and<br />
learn how to better serve patients as a team. Recently, a new clinic has been established by University of<br />
Utah Healthcare, which offers care to underserved members of our community. This clinic is partially staffed<br />
by students from the varied health sciences. This offers a chance for students to apply the skills acquired in<br />
IPE. The goal for IPE is to educate future health professionals in order to improve quality of care by utilizing<br />
the collective skills of the entire health care team.<br />
UNIVERSITY OF UTAH SCHOOL OF MEDICINE [<strong>Poster</strong> # 65]<br />
Program/Project Title: Quantitative Analysis of Ophthalmological Surgical Education During Medical<br />
School and Residency<br />
Presenter(s): Maximilian Padilla, Sam Francis, Dustin Nash, Adam Bracken, Matt Lamont & Erin Anstadt<br />
Email: maximilianrpadilla413@gmail.com<br />
Exposure to the operating room during 3rd and 4th year of medical school can be widely variable between<br />
surgical subspecialities. The first goal of this project was to quantify the amount of time that students spend<br />
in the operating room during Ophthalmology rotations, and other surgical subspecialty rotations.<br />
34
There is also a great deal of variability in the length of medical school and residencies in other countries.<br />
The amount of time that students spend in the Operating room, as well as the amount of surgical cases that<br />
are performed during a residency can be very different. We compared the length and scope of medical<br />
school and residency training in Ophthalmology in the United States compared to nine other countries. To<br />
do this we focused on training in Ophthalmology and compare the length and depth of clinical and surgical<br />
education in the United States to that of prospective Ophthalmologists in the many different parts of the<br />
world.<br />
UNIVERSITY OF VERMONT COLLEGE OF MEDICINE [<strong>Poster</strong> # 66]<br />
Program/Project Title: Rural Candidates Applications to Medical School<br />
Presenter(s): Peter Wingfield & Priyanka Chilakamarri<br />
Email: peter.wingfield@med.uvm.edu<br />
The <strong>AAMC</strong> has drawn attention to the significant problem of finding physicians who want to practice in rural<br />
areas of the US. Research has previously shown that students who come from rural areas are more likely to<br />
return and practice in rural areas after becoming physicians than are students from urban areas. The state of<br />
Vermont has a large rural population. The University of Vermont medical college offers approximately 25-<br />
30% of its medical college places to "In-State" applicants. This project looks at whether the student body at<br />
UVM medical college has a higher proportion of "rural" applicants than the national average, and also at<br />
whether these students have a higher likelihood of acceptance into the program.<br />
VANDERBILT UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 67]<br />
Program/Project Title: Medical Education in the Digital Age: A need for social media instruction<br />
Presenter(s): Vanessa Kennedy & Shannon Koh<br />
Email: vanessa.e.kennedy@vanderbilt.edu<br />
Background:<br />
In the last several years, social media platforms, featuring user-created content and communication, have<br />
experienced dramatic expansion. Recently, the American College of Physicians released a position paper<br />
describing the role of social media in the public perception of physician behavior, and provided<br />
recommendations on how social media may be used professionally. However, there is limited understanding<br />
on how social media reflects on the professionalism of medical students, and no official policy on what<br />
constitutes professional conduct for a medical student in the digital environment.<br />
Methods:<br />
We distributed surveys regarding social media, medical education, and professionalism to both residency<br />
program directors and medical students and Vanderbilt University School of Medicine. 56 residency program<br />
directors responded, and 184 medical responded (20.7% MS1, 26.2% MS2, 23.4% MS3, 25% MS4, 4.9%<br />
other).<br />
Results:<br />
Medical students are active participants in social media. 95.1% (175/184) of medical students report having a<br />
social media profile, and 85.3% (157/184) are active on social media at least once per day. At Vanderbilt,<br />
16.1% (9/56) of residency program directors reported looking up applicants on social media. Of these, 44.4%<br />
(4/9) reported that their decision was influenced by the applicant’s social media activity. 50% (2/4) reported a<br />
negative influence, while 50% (2/4) reported a positive influence. Overall, 82.1% (46/56) of program directors<br />
feel that social media is a reflection of professionalism, compared to only 50.5% (93/184) of medical<br />
students. Interestingly, the degree to which students consider social media presence a reflection of<br />
professionalism appears to decrease with training. 58.1% (50/86) of pre-clinical (MS1, MS2) students<br />
reported that social media presence reflects professionalism, compared to 42.7% (38/89) of clinical (MS3,<br />
MS4) students. Most medical students appear to manage their social media professionalism profiles by<br />
restricting content; 70.1% (129/194) reported that they will delete or alter their profiles when applying to<br />
residency programs. Overall, 68.5% (126/184) of medical students and 83.9% (47/56) of program directors<br />
believe that medical students should be instructed on how to use social media professionally.<br />
35
Conclusion:<br />
As social media is becoming an increasingly common avenue of communication and personal expression,<br />
medical educators must recognize that it does and will continue to reflect on an applicant’s professionalism.<br />
This does not, however, imply that medical students should avoid social media altogether—as shown in the<br />
above data, a student’s social media presence has the potential to reflect positively on their professionalism.<br />
Instead, instruction should be given to medical students on how to shape a professional social media<br />
presence, much in the way instruction would be given on how to prepare a professional CV. Currently, there<br />
are no established guidelines regarding social media presence and medical education. As part of educating<br />
medical students on digital professionalism, a unified consensus should be reached regarding what is and is<br />
not appropriate for medical trainees to communicate through social media.<br />
WAKE FOREST SCHOOL OF MEDICINE [<strong>Poster</strong> # 68]<br />
Program/Project Title: Emergency Medicine in the Third Year Curriculum<br />
Presenter(s): Daniel Oldroyd & Charlie Pitts<br />
Email: doldroyd@wakehealth.edu<br />
An Emergency Medicine curriculum in the third year of medical school serves to benefit the student, staff,<br />
faculty, and institution as a whole. In the Emergency Department, students are given the unique opportunity<br />
to approach patients with general complaints and broad differential diagnoses in an acute care setting.<br />
While inpatient medicine grants daily opportunities to manage patients’ problems, the primary care setting of<br />
the emergency department allows students to triage patients, make new diagnoses, and to manage these<br />
new diagnoses. In the ED, students gain unique exposure to procedures, treatment algorithms,<br />
interdisciplinary teams, cost conscious decision making, and some health policies. Students' presence<br />
encourages an education-oriented atmosphere, and provides faculty and staff additional leadership and<br />
teaching opportunities. Currently, about 33% of US allopathic medical schools have a required third year<br />
rotation in Emergency Medicine. Given the advantages mentioned above, we believe this rotation to be<br />
greatly beneficial to our students and institution. For our poster, we plan to outline the recommendations as<br />
given in current literature on the subject, and compare those recommendations to the current curriculum that<br />
is in place at the Wake Forest School of Medicine. By doing so, we hope to share the potential benefits of<br />
implementing such a curriculum at other institutions, as well as some logistical information in regard to the<br />
implementation of our EM curriculum.<br />
WAYNE STATE UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 69]<br />
Program/Project Title: A Promising Pipeline to Medical Education: The Detroit Premedical Scholars<br />
Program<br />
Presenter(s): Osamuedemen Iyoha, Robert Guglielmo & Tahsin Khundkar<br />
Email: oiyoha@med.wayne.edu<br />
Increasing the number of underrepresented minorities in medical education is of critical importance, as this<br />
directly and positively impacts the quality of patient care, health outcomes, and health disparities. Through its<br />
many pipeline programs, the Office of Diversity and Inclusion (ODI) at Wayne State University School of<br />
Medicine is helping to increase the number of students who represent the diversity of our global community.<br />
The Detroit Premedical Scholars Program (DPSP) is a 6 week long summer enrichment program for rising<br />
high school seniors within the Detroit Public School system. This program, whose purpose is to introduce<br />
interested students from the inner city to the various clinical aspects of medicine as well as helping them to<br />
navigate the pathway towards a career in medicine. Student participants receive a summer stipend to assist<br />
with their food and transportation needs throughout the program. Post-program follow up is done to track<br />
student progress and provide additional resources as needed.<br />
We believe that this program is a noteworthy initiative for other institutions to implement because it<br />
addresses a major concern in medical education and is reproducible. While the hardest part of implementing<br />
this initiative is finding funding, the ODI have successfully secured funding through support from various<br />
community foundations including the Detroit Public Schools Foundation and the Sinai Grace Foundation.<br />
Plans are currently underway to duplicate this model in other counties of Southeastern Michigan in the<br />
future. A pipeline program such as this one not only provides productive resources for the youth of a<br />
36
community, it also makes the pathway to medicine more accessible to underrepresented minorities who<br />
otherwise would not pursue a career a medicine.<br />
WAYNE STATE UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 70]<br />
Program/Project Title: Health and Wellness Curriculum<br />
Presenter(s): Tahsin Khundkar, Robert Guglielmo, Osamuedemen Iyoha<br />
Email: tkhundka@med.wayne.edu<br />
The Health and Wellness Program with the motto “feel well, do well,” aims that each student optimizes<br />
healthy coping strategies, finds good balance and achieves academic success throughout medical school.<br />
The wellness program is divided into five sections: Physical, Psychological, Academic, Social and<br />
Community. Student representatives, elected by the general student senate, participate on the planning<br />
committee for the wellness program and assist in the coordination of social events, workshops, speakers and<br />
other relevant activities. Furthermore, this committee has planned a Wellness Week for January, where there<br />
will be multiple events everyday ranging from yoga classes to lectures on mindfulness and ending with a<br />
“wellness fair” as a finale. In addition, the wellness program presents on important wellness topics and<br />
facilitates fitness classes throughout the year. For student convenience, the Campus Counseling and<br />
Psychological services are hosted on the medical campus as part of the “Let’s Talk” program and students<br />
are encouraged to just drop in.<br />
There is a school-wide push to participate in these wellness activities and there is a considerable positive<br />
shift in culture. Students are encouraged to become a “Health and Wellness Ambassador” by attending 15<br />
seminars over 4 years. This accomplishment is to be recognized at the annual Medical Student Recognition<br />
Program. The School of Medicine Co-Curricular Program also gives credit for some of these activities.<br />
In the last <strong>AAMC</strong> national meeting, OSR representatives gathered what other schools are doing to ensure<br />
and promote student wellness. Since then, our office of student affairs has set in place a robust Health and<br />
Wellness curriculum and we are excited to share our progress with other schools at this year’s <strong>AAMC</strong><br />
national meeting.<br />
YALE UNIVERSITY SCHOOL OF MEDICINE [<strong>Poster</strong> # 71]<br />
Program/Project Title: Community-targeted Health Reform and ACA Implementation Education<br />
Presenter(s): Lorenzo R. Sewanan, Matthew L. Meizlish, Priscilla Wang & Ankit Kansal<br />
Email: lorenzo.sewanan@yale.edu<br />
On October 1, millions of people can have access to health insurance through the implemented ACA health<br />
insurance exchange marketplace, but only if they know about it. Over the past year, we’ve developed a<br />
campaign “Students for a Better Healthcare System” at Yale to bring short, accessible, understandable<br />
presentations to the New Haven community about how the health care system works, the changes with<br />
health reform, and the practical impact on their access to insurance. We hope to expand our efforts and find<br />
partner schools who can carry out this vital work in their communities.<br />
37