A New Beginning 2012-7 - UHSM
A New Beginning 2012-7 - UHSM
A New Beginning 2012-7 - UHSM
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Editorial board no. 1033/12<br />
Copyright University Hospital of South Manchester NHS Foundation Trust<br />
All rights reserved<br />
Issue Date : October <strong>2012</strong><br />
Review Date : October 2014
Foreword<br />
As a group of former heart patients, The Ticker Club, has been providing support for patients<br />
and their relatives since 1987, in the outpatient department and on the cardiac wards at<br />
Wythenshawe Hospital (<strong>UHSM</strong>). As part of this work, the Club has for some years now, been<br />
privileged to provide the funding that makes this booklet available to all the hospital’s cardiac<br />
patients.<br />
In our direct personal contact with patients, their relatives and friends - from diagnosis at the<br />
beginning of the “patient journey”, through the hospital stay and beyond - it is the feedback we<br />
receive from all concerned that has established beyond doubt the high value placed on this<br />
booklet and its contents.<br />
We have all found here, in this booklet, information and advice we can rely on to help us<br />
understand and benefit from the procedure we have undergone. At the same time it is clear this<br />
booklet has proved to be a valuable reference facility, not just for patients, but also for relatives,<br />
carers and supporters alike.<br />
As patient support providers we, in the Ticker Club, are pleased to help underpin the care and<br />
professionalism of all the Wythenshawe Hospital staff who will feature in your patient<br />
experience. We see this booklet as a key part of the support on offer. We hope you too will find it<br />
helpful.<br />
The Ticker Club<br />
Charity No. 519754<br />
The Ticker Club<br />
Founded 1987<br />
This booklet was produced by the Clinical Lead Physiotherapist for cardiac rehabilitation at<br />
Wythenshawe Hospital in 1992. The Cardiac Rehabilitation Team, along with colleagues from<br />
various wards and departments, has continued to write and develop this information, for<br />
patients undergoing heart surgery.<br />
For further information about cardiac rehabilitation, please contact the Wythenshawe Hospital<br />
Cardiac Rehabilitation Service on 0161 291 2177 or email us at cardiac.rehab@uhsm.nhs.uk<br />
We thank The Ticker Club for their continuing support in funding this booklet.<br />
Cardiac Rehabilitation Clinical Lead Physiotherapist/Team Manager
Weeks 8 – 10<br />
May be able to return to light or management types of work<br />
Wash and polish car, clean windows with regular rest breaks<br />
Gardening may include digging, hoeing, raking leaves, mowing the lawn (powered mower)<br />
If possible, use a hose, rather than a watering can<br />
Continue cardiac rehabilitation programme<br />
Daily brisk walk<br />
Week 12<br />
May be able to return to manual types of work<br />
D.I.Y. – decorating, painting with regular rest breaks<br />
Carpentry, moving furniture, trimming a hedge<br />
May start golf, badminton, tennis, jogging, and football<br />
Swimming (as long as wounds are completely healed)<br />
Daily brisk walk<br />
On completion of your cardiac rehabilitation programme, you may choose to be referred<br />
to a local exercise referral scheme or a local community-based exercise group.<br />
Alternatively, you will be advised to continue daily physical activity in the long-term and/or<br />
take up an exercise or hobby that you enjoy.<br />
Contents Page No.<br />
Section A - Your heart operation<br />
Introduction 5<br />
Patient Information Day 5<br />
Information about your admission 5<br />
How long will I be in hospital? 6<br />
What is Coronary Heart Disease? 6<br />
Coronary Artery Bypass Grafting 6<br />
What is heart valve disease? 8<br />
Heart valve surgery 9<br />
What will happen on the day of my operation? 10<br />
Cardiothoracic Critical Care Unit (CTCCU) 11<br />
• Pain 11<br />
• Intravenous infusions (drips) 11<br />
• Eating and drinking 12<br />
• Telephone enquiries and visiting arrangements 12<br />
Cardiothoracic Ward 12<br />
Section B - Your recovery<br />
Post-operative physiotherapy 13<br />
• Breathing exercises 13<br />
• Foot and leg exercises 13<br />
52<br />
1
• Arm and shoulder exercises 14<br />
• Moving about the bed 15<br />
• Positioning and posture 15<br />
Clothing advice 15<br />
Physical effects of surgery 15<br />
Psychological effects for you and your family 17<br />
Wound care, healing and bathing 17<br />
Going home 18<br />
Medication 18<br />
Your follow-up 22<br />
Advice about financial matters 22<br />
Section C - Your rehabilitation<br />
Cardiac rehabilitation 23<br />
First few days at home 24<br />
Sleep and rest 24<br />
Relaxation 25<br />
Physical activity 26<br />
Perceived exertion scale 28<br />
Walking 28<br />
Home exercises 30<br />
Household tasks and gardening 31<br />
2<br />
Summary: recovery and rehabilitation guide<br />
Below is a weekly guide intended to give you an overall picture of how you might hope to<br />
progress.<br />
Remember - it is only a guide. Everyone progresses at a different rate and a return to your<br />
normal daily activities should be determined by how you feel during each activity.<br />
Week 1<br />
Cardiothoracic Critical Care Unit (CTCCU) on day of operation<br />
CTCCU or ward (day one)<br />
Breathing exercises, begin foot, leg and arm exercises<br />
Return to ward, begin walking (day two)<br />
Progress walking gradually (days three to five), climb stairs if appropriate<br />
Week 2<br />
Return home<br />
Inform GP of your return home<br />
Home visit by district nurse (where appropriate)<br />
Rest and walk around your home and garden, climb stairs as necessary<br />
Continue arm and shoulder exercises<br />
Take things gently - read, listen to music, watch television<br />
Make yourself a light snack<br />
Week 3<br />
Continue arm and shoulder exercises<br />
Begin light activities, i.e. dusting, set the table, prepare light meals<br />
Short daily walk<br />
Week 4<br />
Continue arm and shoulder exercises<br />
Increase activities in the house<br />
Begin light activities (seated) outside<br />
Begin light social activities<br />
Sexual activity may be resumed<br />
May take a restful holiday in own country<br />
Daily walk<br />
Week 5<br />
Continue arm and shoulder exercises<br />
Increase activities to include machine washing, cooking and ironing<br />
Daily walk<br />
Weeks 6 - 7<br />
Continue arm and shoulder exercises. Add arm stretches (see page 14)<br />
May lie on stomach when sleeping<br />
May start walking a dog on a lead<br />
May start to lift weights exceeding 5 lbs (2.3 kg), carry shopping bags, push supermarket<br />
trolleys<br />
Increase activities to include sweeping, vacuuming, mopping floors<br />
May start driving a car<br />
Start the exercise component of your local cardiac rehabilitation programme<br />
May start cycling, bowling, dancing, putting for golf<br />
You should have had or received your appointment for your surgical outpatient<br />
follow-up<br />
Daily brisk walk<br />
51
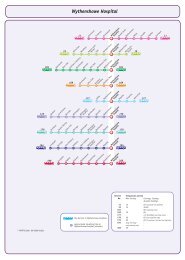
Wythenshawe Hospital (<strong>UHSM</strong>) contact numbers<br />
Contact Contact no.<br />
Cardiac Rehabilitation Secretary 0161 291 2177<br />
Cardiac Rehabilitation Physiotherapists 0161 291 2128<br />
Cardiac Rehabilitation Occupational Therapist 0161 291 2110<br />
Cardiothoracic Surgical Specialist Nurses 0161 291 5067<br />
Cardiology Liaison Nurses 0161 291 2679<br />
May be contacted by telephoning the hospital<br />
switch board on 0161 998 7070 and asking switch<br />
to air-call the cardiac rehabilitation specialist nurses<br />
Dietitian 0161 291 2701<br />
Pharmacist 0161 291 3331<br />
Smoking Cessation Service 0161 291 5030<br />
Waiting List Co-ordinator 0161 291 2463<br />
Cardiothoracic Critical Care Unit (CTCCU)<br />
Main reception 0161 291 4522<br />
Zone 1 Beds 1 - 6 0161 291 4833<br />
Zone 2 Beds 7 - 10, 17 - 20 0161 291 4836<br />
Zone 3 Beds 11 - 16 0161 291 4837<br />
Cubicles 1 - 2 0161 291 4536<br />
Cubicles 3 - 4 0161 291 4537<br />
Cubicles 5 - 6 0161 291 4538<br />
Ward F6 0161 291 2566<br />
Jim Quick Ward 0161 291 2204<br />
Active hobbies and sports 32<br />
Driving 33<br />
Returning to work 33<br />
Holidays and air travel 34<br />
Sexual intercourse 34<br />
Section D - Maintaining a healthy heart<br />
Risk factors associated with the development of 35<br />
coronary heart disease<br />
Modifiable risk factors 35<br />
• Smoking 35<br />
• Lack of physical activity 36<br />
• Poor diet 36<br />
• Being overweight 36<br />
• Alcohol 37<br />
• Stress 38<br />
• High blood pressure 38<br />
• High levels of fats in the blood (cholesterol) 40<br />
• Diabetes 41<br />
Non-modifiable risk factors 42<br />
• Family history 42<br />
• Age 42<br />
• Gender 42<br />
50<br />
3
• Ethnic background 42<br />
Healthy eating 43<br />
• Fats 43<br />
• Omega-3 (polyunsaturated fats) 44<br />
• Fruit and vegetables 45<br />
• Plant sterols and stanols 46<br />
• Salt 46<br />
• Watch your weight 47<br />
• Additional dietary information 47<br />
Support groups 48<br />
Useful addresses<br />
British Heart Foundation (BHF)<br />
Greater London House<br />
180 Hampstead Road<br />
London<br />
NW1 7AW<br />
Tel: 020 7554 0000<br />
Fax: 020 7554 0100<br />
Email: internet@bhf.org.uk www.bhf.org.uk<br />
Heart helpline 0300 330 3311 Monday – Friday 9am – 6pm<br />
The BHF produces a range of booklets and videos. The booklets are free of charge and can be<br />
ordered on line or by telephoning 0870 600 6566.<br />
Driver and Vehicle Licencing Agency (DVLA)<br />
Drivers Medical Group<br />
DVLA<br />
Swansea<br />
SA99 1TU<br />
Tel: 0300 790 6806 Monday – Friday 8am – 5.30pm, Saturday 8am – 1pm<br />
Fax: 0845 850 0095<br />
Email: eftd@dvla.gsi.gov.uk<br />
www.dvla.gov.uk<br />
• Ticker Club 48<br />
• Other support groups 48<br />
Useful addresses 49<br />
Wythenshawe Hospital (<strong>UHSM</strong>) contact numbers 50<br />
Summary: recovery and rehabilitation guide 51<br />
4<br />
49
Support groups<br />
Ticker Club<br />
Tel: 0161 291 2873<br />
tickerclub@uhsm.nhs.uk<br />
https://www.uhsm.nhs.uk/patients/tickerclub/pages/default.aspx<br />
The Ticker Club, a registered charity for Wythenshawe Hospital (<strong>UHSM</strong>) patients, was founded<br />
in 1987, by a group of patients who had recovered from open-heart surgery. It is a totally<br />
voluntary organisation open to all those who have undergone, or are about to undergo some<br />
form of cardiac or vascular procedure. It is also open to their families and to all who wish to<br />
support the aims and objectives of the Ticker Club.<br />
The Ticker Club raises money through subscriptions, donations, prize draws and other events.<br />
All funds raised are spent on facilities and equipment for the hospital's heart, vascular and<br />
cardiac rehabilitation units.<br />
Patient support volunteers visit the cardiac wards and clinics daily to offer practical advice and<br />
moral support to new patients, both before and after surgery. The Club also produces a<br />
quarterly <strong>New</strong>sletter with information on the Club’s activities.<br />
If you would like to join the Ticker Club, or require any further information about the work they<br />
do, please contact them on the above telephone number or email address.<br />
Other support groups<br />
If you wish to find out about the support or community based exercise groups available in your<br />
area, please contact your local cardiac rehabilitation co-ordinator. Alternatively, you may contact<br />
our cardiac rehabilitation secretary on 0161 291 2177.<br />
Section A - Your heart operation<br />
Introduction<br />
This booklet has been written to provide you and your family with information about your<br />
forthcoming operation. It will inform you how you are likely to progress afterwards and also<br />
inform you how to lead a healthier lifestyle in the future.<br />
You should bring this booklet into hospital when you come in for your operation so you may refer<br />
to it when the staff talk to you during your stay.<br />
An electronic version of this booklet and further information can be found at<br />
www.uhsm.uk/patients/cardiacs/pages/default.aspx<br />
You will have been given a free (returnable) copy of the DVD called ‘Hearts and Minds’ when<br />
you were listed for surgery. If you have not got a copy, you should contact your Cardiac Surgery<br />
Liaison Nurse or you can access the DVD on the internet by going to <strong>UHSM</strong> hearts and minds<br />
DVD.<br />
You can also access a presentation of the above DVD by logging onto the Hospedia television<br />
system by your bedside. Press the operator button. You will be asked for your name and<br />
postcode. You will have access to the DVD, all radio channels and 45 minutes of television<br />
from 9am - 9.45am. This service is available for free.<br />
Patient Information Day<br />
Approximately 1 or 2 weeks prior to your surgery you will be invited to attend a Patient<br />
Information Day on the Cardiothoracic Critical Care Unit (CTCCU ).This takes place on a Friday<br />
afternoon between 2.00 and 4.00pm.<br />
The purpose of the afternoon is to meet members of the team who will care for you during your<br />
stay in hospital and give you an insight into your journey from admission until discharge. The<br />
session allows for questions to be asked by patients and relatives.<br />
Information about your admission<br />
If you have a cough or flu, or if you are taking antibiotics, it is very important that you contact<br />
your Cardiac Surgery Liaison Nurse. Even if you think it is only something minor, please contact<br />
us for advice.<br />
Items to bring in on admission to the ward<br />
As we have limited amount of storage space we would appreciate it if you would only bring into<br />
hospital the suggested items below:<br />
Toiletries (denture pot if needed), towel<br />
Clean nightwear, slippers that are comfortable for walking and dressing gown<br />
Small amount of money if required for newspapers etc<br />
Book or magazine, glasses (if required)<br />
Comfortable clothes such as a T-shirt and tracksuit bottoms to wear after a few days.<br />
48<br />
On the day of admission you will need to telephone the ward before setting off to check there is<br />
a bed available. On arrival you will be asked to report to the admissions desk near the<br />
outpatients entrance before going to the ward.<br />
5
Once all your details have been checked you will be directed to a ward. You will be<br />
admitted to a cardiothoracic ward, normally F6. When you arrive on the ward you may<br />
have to wait in the dayroom until your bed is ready.<br />
When you are settled, the nursing staff will ask you some questions about your history and<br />
will take your temperature, pulse and blood pressure. As part of your introduction to the<br />
ward, the nursing staff will discuss any support that you may require at home after your<br />
operation.<br />
The anaesthetist and the surgeon will visit you and talk to you about your operation. This<br />
will give you an opportunity to ask any remaining questions you may have before your<br />
operation.<br />
It may be necessary to remove any body hair from your chest, legs and forearms before<br />
you have your bath or shower. As shaving can increase the risk of infection, the hospital<br />
policy is to use clippers.<br />
How long will I be in hospital?<br />
You can usually expect to stay in hospital for 5 -10 days.<br />
Prior to your admission, every effort is made to ensure that a bed on the ward and the<br />
Cardiothoracic Critical Care Unit (CTCCU) is available for you. Sometimes, due to the<br />
pressure of emergencies, a bed may not be available on CTCCU. In this case, we will<br />
make every effort to ensure you can remain in hospital and reschedule your operation<br />
within the next day or two.<br />
What is Coronary Heart Disease?<br />
The coronary arteries supply blood and oxygen to the heart muscle. In people with<br />
Coronary (artery) Heart Disease (CHD), a fatty substance builds up in the walls of the<br />
arteries, causing narrowing or blockages inside the coronary arteries. When the arteries<br />
become narrowed the blood flow and amount of oxygen delivered to the heart muscle is<br />
reduced. This can cause chest pain (angina) or may lead to a heart attack (myocardial<br />
infarction).<br />
Coronary Artery Bypass Grafting<br />
The purpose of Coronary Artery Bypass Grafting (CABG) is to improve the flow of blood to<br />
the heart muscle. The surgeon may use sections of healthy vein or artery from the arm, leg<br />
or chest wall to ‘bypass’ these narrowed segment/s of coronary artery and provide new<br />
routes to restore normal blood flow to the heart.<br />
The internal mammary artery, an artery from the chest wall, is used as a bypass graft for<br />
the main branch of the left coronary artery whenever possible, as its life span has proved<br />
to be longer than that of a vein graft.<br />
In some instances, however, it is preferable to only use vein grafts, for example, in<br />
emergency surgery when time is important (removal of the internal mammary artery is a<br />
longer procedure). Your doctor, physiotherapist or nurse will tell you if the internal<br />
mammary artery was used for your operation.<br />
Part of a vein (the long saphenous vein) taken from the leg is used for your bypass graft<br />
which means you will have a leg wound. The position and length of the wound depends<br />
upon where your surgeon/surgical care practitioner can find the most suitable vein to use<br />
for the graft. Please refer to the ‘Vein Harvesting’ patient information leaflet that you will<br />
have been given at your out-patient clinic appointment.<br />
6<br />
Watch your weight<br />
If you are overweight, losing 5 -10% of your body weight can lower your risk factors of coronary<br />
heart disease and result in an improvement in your health. It is much better to lose weight slowly<br />
and consistently than to go on a crash diet. Studies have shown that it is also easier to maintain<br />
the loss if you lose it slowly (1 - 2lb per week).<br />
Waist circumference<br />
Evidence suggests that carrying too much weight around your middle<br />
increases your risk of heart disease more than a similar weight of fat<br />
deposited elsewhere in the body. You can’t choose your shape but if you<br />
are carrying extra weight around your waist, it is a greater strain on your<br />
heart. If you are “apple shaped” rather than “pear shaped”, make an effort<br />
to lose some of those extra inches.<br />
Men<br />
Below 94cm (37”) Normal<br />
94 – 100cm (37” – 40”) Increased risk<br />
Above 100cm (40”) High risk<br />
Women<br />
Below 80cm (31.5”) Normal<br />
80 – 87.9cm (31.5” – 34.5”) Increased risk<br />
Above 88cm (34.5”) High risk<br />
Recent evidence suggests that if you are from an Asian background you should aim for a weight<br />
in the lower half of the recommended range and a slightly lower waist measurement.<br />
If you have a poor appetite or have been losing weight unintentionally, ask one of the cardiac<br />
rehabilitation team or your doctor to refer you to a dietitian.<br />
Summary<br />
• Limit foods containing a lot of saturated salt, hydrogenated or trans-fats<br />
• Include one portion of oily fish per week<br />
• Aim for 5 portions of fruit and vegetable daily<br />
• Limit intake of salt<br />
• Check your weight and waist measurement<br />
Additional dietary information<br />
The British Heart Foundation produces various dietary information booklets and videos. Many are<br />
available in the hospital or you can contact them directly.<br />
If you have access to the internet, the following web addresses have useful dietary information:<br />
www.bhf.org.uk<br />
www.heartuk.org.uk www.foodstandards.gov.uk<br />
www.bda.uk.com www.nutrion.org.uk<br />
47
A guide to portion size:<br />
− pineapple or melon 1 large slice<br />
− grapefruit 1/2 fruit<br />
− apple, pear, orange, banana, peach 1 fruit<br />
− plums, kiwi, satsuma 2 fruits<br />
− berries, cherries or grapes 1 cupful<br />
− vegetables e.g. carrots, peas 3 large tablespoons<br />
− salad 1 small dessert<br />
bowl.<br />
Occasionally your surgeon will choose to use the radial artery in the arm as a graft. In this<br />
case, the incision is in the forearm, from elbow to wrist.<br />
Heart showing Coronary Artery Bypass Grafting<br />
Plant sterols and stanols<br />
Plant sterols and stanols which are added to some foods including spreads, soft cheeses, yogurts<br />
and yogurt style drinks may reduce cholesterol levels. However these products can be expensive<br />
and must be taken regularly. They may be helpful for people who cannot take<br />
cholesterol-lowering drugs or for those who have high cholesterol levels even after making<br />
changes to their diet. For further advice ask your doctor or dietitian.<br />
Salt<br />
Salt can raise your blood pressure. High blood pressure can increase your risk of developing<br />
heart disease and stroke.<br />
Limit salt to about 6g per day which is about one teaspoonful. This is not a large amount when<br />
you consider that around 75% of the salt we eat is in the food we buy.<br />
Foods which contain a lot of salt<br />
• Tinned/packet soup and gravy/stock cubes<br />
• Bacon and processed meats e.g. ham, sausages, pate<br />
• Crisps and salted nuts or crackers<br />
• Soya sauce, bottled sauces<br />
• Ready meals e.g. lasagne<br />
• Processed foods.<br />
A guide to reducing salt in your diet<br />
• Avoid adding salt at the table<br />
• Limit salt in cooking and gradually reduce. Use alternative flavourings e.g. pepper, herbs<br />
and spices<br />
• Avoid salty foods, choose fresh food where possible<br />
• Compare labels when you are shopping and choose the ones lower in salt. Be careful of<br />
other terms used for salt such as sodium, monosodium glutamate and sodium bicarbonate.<br />
To find out if a product has ‘a lot’ or ‘a little’ salt and sodium, look at the nutrition information label.<br />
Compare the ‘per 100g’ figures with the information below.<br />
This is a lot (per 100g of food) This is a little (per 100g of food)<br />
1.25g of salt or more 0.25g of salt or less<br />
0.5g of sodium or more 0.1g of sodium or less<br />
46<br />
Coronary artery bypass graft surgery may be performed using either of the following<br />
techniques:<br />
1. When using a heart-lung bypass machine, blood is diverted away from the heart and into<br />
the machine, allowing the surgeon to work on an ‘empty and dry’ heart. The heart-lung<br />
machine takes over the role of the heart and lungs during surgery.<br />
2. The ‘beating heart’ technique is where the heart is not stopped and the surgeon bypasses<br />
the blockages while the heart is still beating and working. This is called ‘off pump’ surgery.<br />
The decision regarding whether your operation requires the heart-lung bypass machine or<br />
not, will be made by your surgeon.<br />
Chest incision - In order to operate on the heart, an incision through the chest is necessary.<br />
This involves cutting through the breastbone lengthways. This is called a median sternotomy.<br />
Afterwards the bone is held together with about six stainless steel wires, which stay in place.<br />
They rarely need to be removed. The wound is approximately 30 cm (12 inches) long.<br />
What are the benefits of Coronary Artery Bypass Grafting?<br />
CABG can:<br />
• reduce angina and/or breathlessness<br />
• reduce the amount of medication you need to take<br />
• improve your quality of life<br />
• increase your chance of living longer.<br />
The benefits of CABG surgery vary for each person. Your surgeon will discuss the expected<br />
benefits for you, as an individual, at your out-patient clinic appointment.<br />
The benefits of CABG surgery vary for each person. Your surgeon will discuss the expected<br />
benefits for you, as an individual, at your out-patient clinic appointment.<br />
7
What are the risks and complications of Coronary Artery Bypass Grafting?<br />
You will have a chance to discuss your individual risk and possible complications with your<br />
surgeon. CABG surgery, like any other surgery, carries a risk of complications. The risk of<br />
complications varies for each person and will depend on several factors including:<br />
• your age and sex<br />
• whether you are having additional surgery at the same as your CABG<br />
• whether you have diabetes, lung problems, kidney damage or any significant problems<br />
with the circulation to your brain or legs<br />
• the urgency of the operation<br />
• your weight<br />
• whether you are a smoker and/or a heavy drinker.<br />
Your surgeon will take the above factors into account when assessing your individual risk.<br />
Possible complications<br />
• Bleeding – you may need to be taken back to theatre to treat excessive bleeding.<br />
• Infection – this may involve one of the wounds (chest, leg or arm), or the lungs, and will<br />
be treated with appropriate antibiotics depending on the severity of the infection.<br />
• Heart attack – on rare occasions during surgery the heart can suffer a heart attack.<br />
• Kidney problems. Bypass surgery can affect your kidney function. If you have any<br />
problems, you will be referred to a specialist.<br />
• Stroke – which may be temporary or permanent.<br />
A member of the surgical team will ask you to sign a written consent form for the operation to<br />
be carried out. Your surgeon will discuss the risks, benefits and alternatives for you as an<br />
individual. If you have any questions, please talk to the doctor before you sign the consent<br />
form.<br />
What is heart valve disease?<br />
Your heart has four valves. They ensure that blood is pumped in one direction only within the<br />
heart and towards the lungs and body. These valves can be damaged in many ways; for<br />
example be abnormal from birth, after rheumatic fever, from wear and tear or following a heart<br />
attack.<br />
There are two main types of valve problem:<br />
• the valve may become narrowed (called stenosis), which causes a block to normal<br />
blood flow<br />
• the valve may become leaky and allow blood to flow in the wrong direction called<br />
regurgitation.<br />
In both cases the heart has to work harder and eventually surgery may be necessary.<br />
The drainage of blood from the lungs to the heart may be affected. This will result in a build up<br />
of fluid on the lungs and cause breathlessness. The drainage of blood from the rest of the body<br />
to the heart may also be affected causing swollen ankles. Chest pain, palpitations and<br />
dizziness may also be experienced.<br />
How much omega-3 fats do I need to eat each week?<br />
• If you’ve had a heart attack aim for 2 - 3 large servings of oily fish per week<br />
• Everyone else should aim for one serving of oily fish and one serving of white fish per<br />
week<br />
• A serving is roughly 100 -150g (4 - 6oz) of fresh, frozen, or smoked fish<br />
• To help lower salt intake, keep smoked fish to no more than once a week.<br />
I do not eat fish, how do I get omega-3 fats?<br />
• Your body can convert a type of fat called alpha-linolenic acid (ALA), into small amounts of<br />
the more useful omega-3 found in oily fish.<br />
• To help your body convert as much omega-3 fats as possible from plants, it is important to<br />
eat a varied mixed diet with plant rich sources daily.<br />
−<br />
−<br />
−<br />
−<br />
−<br />
rapeseed, walnut, soya, flax or linseed oil<br />
ground or crushed linseeds, flax or pumpkin seeds<br />
unsalted nuts e.g. walnuts, pecans, peanuts, almonds<br />
soya beans and tofu<br />
dark green leafy vegetables, sweet potato and whole grains<br />
• Some foods have omega-3 added to them e.g. eggs, milk, yogurt and yogurt drinks.<br />
Omega-3 contents vary greatly, so check labels.<br />
Should I take omega-3 supplements?<br />
• If you eat oily fish you do not need to take a supplement.<br />
• If you have had a heart attack and do not eat oily fish either:<br />
− Take a prescribed or bought over the counter capsule containing 1.0g omega-3 (EPA<br />
and DHA) daily.<br />
Or<br />
−<br />
If you are unable to take fish oil capsules, try a supplement derived from algae (a good<br />
source of DHA).<br />
If using fish oil capsules, look at the label and check the content of omega-3 fats.<br />
These may be listed as EPA and DHA. Just add the total of both EPA and DHA together to find<br />
the total omega-3 fat content.<br />
Cholesterol<br />
Cholesterol (as discussed on page 40), is an important fatty substance found in every cell of the<br />
body. Too much cholesterol in your blood can increase your risk of heart disease. The most<br />
common cause of high cholesterol levels is eating total fat especially saturated fat.<br />
Fruit and vegetables<br />
Government agencies recommend that you aim to include five portions of fruit and vegetables a<br />
day because of the health benefits this brings. Fruit and vegetables contain vitamins and minerals<br />
and are low in fat. Aim to eat a variety to get the most benefit. These can be fresh, frozen,<br />
canned, dried or as a juice.<br />
8<br />
45
How to reduce saturated, hydrogenated and trans-fats<br />
• Choose lean cuts of meat, lean mince, low fat pate. Trim all visible fat and remove<br />
poultry skin.<br />
• Skim fat from gravy. Choose tomato-based sauces rather than<br />
cheesy or cream sauces.<br />
• Choose potato topped pies instead of pastry e.g. shepherd’s pie,<br />
fisherman’s pie.<br />
• Vegetarian options. Base meals on pulses, tofu, quorn, soya meats,<br />
nuts and seeds.<br />
• Use rapeseed oil, olive oil, sunflower oil instead of lard, ghee, suet, vegetable suet.<br />
Avoid deep-frying or re-using oil. Use olive spread, sunflower spread, low fat spread<br />
instead of butter or ordinary margarines.<br />
• Choose fat-reduced cheese and limit quantity to 110g (4oz) per week. Spread this out<br />
over three meals. Avoid eating cheese as a snack unless it is very low-fat such as<br />
cottage cheese.<br />
• Choose semi-skimmed (in moderation), skimmed milk, low fat yogurt, low fat fromage<br />
frais. (If you have diabetes or wish to lose weight, choose healthy eating or diet yogurts<br />
as these are low in fat and low in sugar).<br />
• Desserts. Fresh or frozen fruit, tinned fruit, low fat custard or milk pudding, jelly,<br />
meringue, low fat ice cream or frozen yogurt, trifle sponge cakes, sponge flan are lower<br />
fat options.<br />
• Cakes and biscuits. Malt loaf, garibaldi, ginger nuts, fig rolls, marie biscuits, rice cakes,<br />
oatcakes are better choices but remember to limit the quantity eaten. Once you have<br />
reached your target weight, you could try making your own biscuits or cake using<br />
suitable fats and oils.<br />
The most common valves, which require surgery, are the mitral and aortic valves (see<br />
picture). They are found in the left side of the heart.<br />
Surgical treatment has a very good success rate for severe valve disease and is the<br />
treatment of choice. However, alternatives to valve surgery, including other medical<br />
treatments, may have already been discussed with you by your cardiologist and surgeon.<br />
Check food labels<br />
To find out if a product has ‘a lot’ or ‘a little’ fat and saturated fat, look at the nutrition information<br />
label. Compare the ‘per 100g’ figures with the information below.<br />
This is a lot (per 100g of food) This is a little (per 100g of food)<br />
20g of fat or more 3g of fat or less<br />
5g of saturated fat or more 1g of saturated fat or less<br />
Omega-3 (polyunsaturated fats)<br />
Omega-3 fats are healthy fats which help to protect your heart by:<br />
• helping the heart to beat more regularly<br />
• reducing the stickiness of blood, making it less likely to clot<br />
• helping to keep arteries smooth and supple.<br />
Omega-3 fats are also known as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).<br />
Sources of omega-3 fats<br />
• Oily fish<br />
• Other sources are rapeseed (or canola) oil, nuts and dark green leafy vegetables.<br />
Examples of oily fish:<br />
mackerel kippers pilchards<br />
fresh tuna trout salmon<br />
sardines herring sild.<br />
44<br />
Heart valve surgery<br />
Heart showing valves and chambers<br />
There are two types of valve surgery. The damaged valve can either be repaired or<br />
replaced. A replacement valve can either be mechanical (metal or plastic) or tissue<br />
(obtained from an animal, usually a pig or cow).<br />
• Mechanical valves are longer lasting, but you will need to take anti-coagulant drugs<br />
(those which thin the blood) for the rest of your life (see page 20).<br />
• Tissue valves do not last indefinitely, but you are less likely to require<br />
anti-coagulant drugs.<br />
Your surgeon will discuss with you the most suitable valve in your case.<br />
All valve operations are performed using the heart-lung bypass machine.<br />
What are the benefits of valve surgery?<br />
The benefits of valve surgery vary for each person. The benefits for you will depend on<br />
your particular symptoms before the operation. You can expect to see an improvement in<br />
your symptoms. The surgery will also help to prevent your heart valves from deteriorating<br />
further.<br />
9
What are the risks of valve surgery?<br />
Valve surgery, like any other surgery, carries a risk of complications. The risk of complications<br />
varies for each person and will depend on several factors including:<br />
• your age and sex<br />
• which valve is being operated on, and the extent of valve and heart muscle disease<br />
• whether you are having a coronary artery bypass graft at the same time as your<br />
valve surgery<br />
• whether you have diabetes, lung problems, kidney damage or any significant problems<br />
with the circulation to your brain or legs<br />
• the urgency of the operation.<br />
Your surgeon will take the above factors into account when assessing your individual risk.<br />
Possible complications are:<br />
• wound or chest infection<br />
• ongoing risk of infection (endocarditis). To reduce this risk all patients should have<br />
regular dental checks<br />
• irregular heart beat<br />
• blood clots can form, mostly on mechanical valves<br />
• wear or damage to valves - this is more common with tissue valves<br />
• stroke - there is always a very small risk of stroke with valve surgery.<br />
Consent for your operation<br />
A member of the surgical team will ask you to sign a written consent form for the operation to<br />
be carried out. Your surgeon will discuss the risks, benefits and alternatives for you as an<br />
individual. If you have any questions, please talk to the doctor before you sign the consent form.<br />
What will happen on the day of my operation?<br />
On the day of your operation the anaesthetist will have prescribed for you a ‘premedication’ to<br />
be given a few hours before your operation. This will involve you being given some tablets or an<br />
injection and possibly some of your normal medication. The premedication will help you relax<br />
and may make you drowsy. You will be taken to theatre on your bed.<br />
In the anaesthetic room the anaesthetist will put a drip into the back of your hand and give you<br />
the anaesthetic injection. Whilst you are asleep the anaesthetist will put a tube down your throat,<br />
into your windpipe and connect you to a ventilator (breathing machine). This tube stays in place<br />
throughout your operation. It is needed because during the operation it is necessary for your<br />
body temperature to be lowered to rest your heart and lungs and allow their function to be taken<br />
over by the “bypass and breathing machine”. Whilst the thought of having this tube in your<br />
windpipe is not pleasant, please remember that you will be asleep and therefore not aware<br />
of its presence.<br />
After your operation you will be transferred into the CTCCU whilst still under the anaesthetic. It is<br />
important for us to monitor your heart rate, breathing and blood pressure. Your sedation will be<br />
reduced once you are stable. The tube in your windpipe will be removed when your lungs are<br />
strong enough for you to breathe properly.<br />
10<br />
Healthy eating<br />
Research has shown that by making changes to your diet you can reduce your risk of recurrent<br />
heart problems.<br />
You should aim to achieve this by:<br />
Fats<br />
• reducing your saturated fat intake<br />
• including omega-3 fats weekly<br />
• having at least five portions of fruit and vegetables per day<br />
• reducing your salt intake<br />
• maintaining a healthy weight<br />
All fats and oils contain a mixture of saturated fats and unsaturated fats in different proportions.<br />
Unsaturated fats are either mono-unsaturated or poly-unsaturated.<br />
Saturated fats<br />
Too much saturated fat causes the level of cholesterol in your blood to increase.<br />
Therefore you should reduce your intake of saturated fat.<br />
Saturated fats are mainly found in:<br />
• butter, lard, suet, ghee, coconut oil, palm oil, and any products made using these, for<br />
example pastry, pies, cakes, biscuits<br />
• fat on meat, processed meats such as sausages, beef burgers, salami, corned beef<br />
• full-fat dairy products such as full-cream milk, cream, cheese, full-fat yogurt<br />
• manufactured foods such as chocolate, mayonnaise, cream substitutes.<br />
Unsaturated fats<br />
As part of a healthy diet you could replace foods that contain saturated fats with foods that<br />
contain unsaturated fats. Unsaturated fats can be good for our hearts.<br />
Some foods that could replace products high in saturated fats include:<br />
• oily fish<br />
• nuts and seeds<br />
• olives and olive oil<br />
• sunflower and rapeseed oil<br />
• avocado.<br />
Trans-fats and hydrogenated fats<br />
These fats are formed during food processing when they are subjected to high temperatures.<br />
They are mainly found in deep fried foods, shop bought cakes, biscuits, confectionery and crisps.<br />
It is important to eat as little trans-fats and hydrogenated fat as possible, because they cause<br />
your blood cholesterol to increase.<br />
43
Non-modifiable risk factors<br />
Family history<br />
Coronary heart disease runs in families. Your own risk of developing<br />
coronary heart disease is increased if your father or brother was<br />
diagnosed with the disease under the age of 55, or your mother or<br />
sister was diagnosed under the age of 65. Other conditions which<br />
can run in families include high cholesterol levels, diabetes and<br />
hypertension. It is important that family members are aware of their<br />
own risk factors and take steps to prevent heart disease.<br />
Age<br />
The older you are the more likely you are to develop coronary heart disease.<br />
Gender<br />
Men are much more likely to develop coronary heart disease at a younger age than women.<br />
Women appear to be protected by their hormones until the menopause, after which their risk of<br />
heart disease increases.<br />
Ethnic background<br />
People from Afro-Caribbean backgrounds and South Asians are at a higher risk of developing<br />
coronary heart disease.<br />
Cardiothoracic Critical Care Unit (CTCCU)<br />
The amount of time spent recovering on CTCCU can vary from one individual to another.<br />
Patients will stay on CTCCU until they are fit to be cared for on the ward.<br />
The morning following your operation the consultant and anaesthetist will visit you. They will<br />
review your condition and decide whether you are to stay on CTCCU or be transferred to the<br />
ward.<br />
In general most patients are transferred between 12 to 36 hours after their operation. The nurse<br />
who is looking after you will keep you fully informed about your transfer.<br />
Your nurse will monitor your condition and assess when you are ready to begin breathing<br />
unassisted again. As you start to wake up your nurse will tell you that you are back on the<br />
CTCCU and that your operation is over. To check that you have woken up properly your nurse<br />
will ask you to move your toes and squeeze their hand. This helps them to assess how awake<br />
you are. You will still be very sleepy at this stage and you may become aware of the tube in<br />
your throat and windpipe. If, at this stage, your condition is considered stable the nurse will<br />
remove the tube in your throat. If not, the sedation will be topped up until you are ready for<br />
the tube to be removed. It is important to remember that whilst the tube remains in your throat<br />
you will be unable to talk. Do not be alarmed – your voice will return once the tube is removed.<br />
As your nurse will be monitoring your breathing very closely they will be with you all the time.<br />
They will ask you to communicate with them by nodding or shaking your head or by squeezing<br />
their hand.<br />
Some patients who have existing lung disease, for example asthma or chronic bronchitis, may<br />
need more assistance with their breathing. The consultant anaesthetist who speaks to you<br />
before the operation will tell you if they consider that this will be the case.<br />
Once you are off the ventilator and the tube is removed you will need extra oxygen via a<br />
facemask for approximately the next two days. The mask should remain in place for most of the<br />
time, but you can take it off in order to eat or drink.<br />
Pain<br />
Your comfort is very important to us. When you are pain-free it will improve your breathing and<br />
help your physiotherapy (see page 13). We will give you painkillers through one of your drips<br />
and gradually replace this with tablets as you recover sufficiently to be able to eat and drink<br />
again. It is important that you let us know if you are experiencing any discomfort so that we can<br />
adjust your painkillers to suit your need.<br />
Intravenous infusions (drips)<br />
Whilst you are sedated you will have several drips inserted. Some of these will be in your hand,<br />
others in your neck or shoulder. Most of these will be removed on the CTCCU before your<br />
transfer to the ward. You will be left with one drip in your hand and possibly one in a neck vein.<br />
Whilst you are under the anaesthetic, a tube (catheter) will have been put into your bladder.<br />
This will drain your urine whilst you are asleep and for a short time afterwards. The catheter<br />
may be removed during your stay on CTCCU or on the ward.<br />
42<br />
11
Eating and drinking<br />
Soon after the tube in your throat has been removed you will be able to drink again. Most people<br />
are ready to eat again on the evening of the first day after the operation. You will be offered light<br />
meals to start with.<br />
Telephone enquiries and visiting arrangements<br />
A member of staff will telephone your next of kin (within the hour) when you have been<br />
transferred from the theatre and arrived on CTCCU.<br />
Telephone enquiries are welcome at any time of the day or night. In order to help the nursing<br />
staff who are caring for you, we ask that only one or two family members ring the unit. They<br />
can then pass on the information to other family members. We understand that relatives are<br />
anxious to enquire but each time the nurse has to answer the phone they are taken away from<br />
caring for you.<br />
Visiting on the CTCCU is restricted to immediate family only. On the day of your operation we do<br />
not encourage relatives to visit. Nevertheless we realise that this day will be an anxious time for<br />
your family and in some instances visiting may be possible. Please ask members of your family<br />
to contact the CTCCU and speak to the nurse who is looking after you. He/she will make<br />
arrangements for them. Normal visiting arrangements can be resumed on the first day after your<br />
surgery. Before visiting, your family should contact the CTCCU by telephone to check whether<br />
you have been transferred to another ward. Visiting times on CTCCU are 2 - 4.30pm and<br />
6 - 8pm. This is to allow protected meal times for patients and also to provide rest time for<br />
patients. Unfortunately due to health and safety reasons and also infection control, flowers are<br />
not allowed on the unit or wards.<br />
Mobile phones and camera attachments are not to be used on the CTCCU.<br />
Cardiothoracic Ward<br />
When you are transferred off the CTCCU, it is likely you will move to Ward F6 (or to Jim Quick<br />
Ward). It is recommended that the number of visitors to the ward is restricted to a maximum of<br />
three visitors per patient. Children under the age of 12 are discouraged from visiting the ward.<br />
Permission for children to visit should be obtained beforehand from the nurse in charge. Visiting<br />
times on Ward F6 are 2 - 4pm and 6 - 8pm. Out of hours visiting will need prior arrangements<br />
with the ward sister.<br />
Diabetes<br />
Diabetes occurs when the glucose level in the blood is too high. Glucose is a sugar that the body<br />
makes mainly from the starches and sugars (carbohydrates) in food. The blood carries glucose<br />
to all the cells in the body, where it is used to produce energy. However, the cells cannot just<br />
take the glucose out of the blood; to do this, they need a hormone called insulin. Insulin is made<br />
in the pancreas – (a large gland that lies behind the stomach), and is carried in the blood. Insulin<br />
allows the glucose to move from the blood and into the cells, therefore enabling the glucose level<br />
in the blood to fall.<br />
There are two types of diabetes:<br />
Type 1 – when the body does not produce any insulin<br />
Type 2 – when the body does not produce enough insulin, or the cells of the body are<br />
unable to use insulin effectively.<br />
In diabetes, glucose levels in the blood rise because glucose cannot move from the blood into<br />
the cells due to a lack of insulin. The cells become starved of glucose (fuel) which leads to<br />
symptoms of diabetes. Diabetes increases the risk of coronary heart disease and can cause<br />
other serious health problems. Diabetes damages the heart in several ways.<br />
• High glucose levels in the blood affect the walls of the arteries, making them more<br />
likely to develop atheroma (plaque).<br />
• Platelets stick together more easily.<br />
• Diabetes increases the damage done by the major coronary heart disease risk factors<br />
of smoking, high blood pressure and high blood cholesterol.<br />
• Diabetes can affect the heart muscle itself, making it a less efficient pump.<br />
• People with Type 2 diabetes often have lower levels of HDL cholesterol.<br />
• Diabetes can affect the nerves to the heart so that the symptoms of heart disease<br />
are not felt in the usual way.<br />
If you have this condition we will give you more information and, if necessary, you may be<br />
referred to a Diabetic Nurse whilst you are in hospital.<br />
A normal blood sugar is between 4 - 9 mmols. If your blood sugar is consistently higher than this<br />
your medication (either insulin or tablets) may need adjusting. You should contact your practice<br />
nurse, district nurse, GP or Diabetes Nurse Specialist. You should attend your GP surgery for<br />
regular diabetic check ups, which include a blood test which tests your long-term blood sugars<br />
(HbA1c).<br />
12<br />
41
High levels of fats in the blood (cholesterol)<br />
Cholesterol is a word you may well have heard, but never understood. Cholesterol is the best<br />
known of a group of fat-like substances in the body called lipids. The liver makes cholesterol from<br />
the saturated fats we eat. A certain amount of cholesterol is essential for life and it is present in<br />
every cell in the body and also in the blood. When people have an excess of fats in their blood,<br />
the body is unable to break these down and may therefore be deposited in the artery wall. These<br />
affected areas are known as atheroma or atherosclerotic plaques. Over time these get bigger<br />
and can spread into the centre of the artery, making the artery smaller. This may cause the<br />
symptoms of angina or more seriously lead to a heart attack.<br />
This is a normal Here atherosclerotic<br />
artery wall plaques are beginning<br />
to develop<br />
Atherosclerotic<br />
plaques<br />
• Cholesterol is carried around the blood in different forms<br />
• The two main forms are high density lipid (HDL) cholesterol and low density lipid (LDL)<br />
cholesterol<br />
• HDL is sometimes known as ‘good cholesterol’ because it carries the cholesterol away from<br />
your arteries back to your liver<br />
• LDL is sometimes referred to as ‘bad cholesterol’ because it carries the cholesterol to your<br />
arteries where it can contribute to the build up of fatty deposits (atheroma), in your artery<br />
walls.<br />
If you have high total cholesterol or a high LDL cholesterol and low HDL cholesterol you are more<br />
at risk of a heart attack.<br />
A high level of cholesterol may be inherited (a condition called familial hyperlipidaemia or<br />
hypercholesterolaemia) or it may be affected by diet and lifestyle.<br />
If you are known to have a heart problem, you should try to lower your cholesterol. The best way<br />
is to cut down on saturated fats in your diet, have moderate alcohol intake and take regular<br />
exercise.<br />
For many people these natural ways are not enough on their own. In this case, research has<br />
shown that the need for tablets is essential (see page 19). The test for cholesterol is often done<br />
as a fasting test which means you will be asked not to eat or drink anything other than water for<br />
12 hours before the test.<br />
My cholesterol result was:<br />
Total cholesterol (T.C.)………….. mmol/l (recommended less than 4mmol/l)<br />
HDL ……………………………….. mmol/l (recommended greater than 1mmol/l)<br />
LDL ……………………………….. mmol/l (recommended less than 2mmol/l)<br />
Triglycerides ………………………<br />
Ratio ……………………………….<br />
Section B – Your recovery<br />
Post-operative physiotherapy<br />
Physiotherapy is a very important part of the recovery process after your operation. You will be<br />
assessed by a physiotherapist the day after your operation and treated either once or twice a<br />
day whilst you are in hospital. They will encourage you to do breathing exercises and will help<br />
you to get back on your feet.<br />
Breathing exercises<br />
After your operation, breathing exercises help to prevent the development of chest infections.<br />
Breathing exercises are important because the anaesthetic (used during the operation) can<br />
cause sputum (phlegm) to collect on your chest. You do not breathe as deeply when in bed as<br />
you do when you are up and about which can mean that the bottom parts of your lungs don’t<br />
fully expand in the early post-operative period. Many patients are also reluctant to take deep<br />
breaths and cough because of their wound, pain and drains.<br />
After your operation until you are discharged or advised by your physiotherapist you should carry<br />
out the following deep breathing exercises:<br />
• take a slow deep breath in, trying to fill your lungs as much as you can, hold it for three<br />
seconds and then breathe out<br />
• repeat this three times<br />
• perform a ‘huff’. This is a short sharp breath out with your mouth open<br />
• cough.<br />
Repeat the cycle again.<br />
To reduce any discomfort when huffing or coughing you can support your chest with your hands<br />
or you may be given a rolled up towel. You should expect some discomfort when carrying out<br />
the breathing exercises but if the pain is stopping you from doing them effectively you must<br />
inform your physiotherapist or nurse. Your painkillers will then be reviewed. You may be given<br />
an incentive spirometer to encourage you to breathe deeply. This device helps to exercise your<br />
lungs to improve their function and measure how well your lungs fill up with each breath.<br />
Foot and leg exercises<br />
Your physiotherapist will also teach you how to do the foot and leg exercises (pictured below)<br />
regularly. These will help reduce the risk of blood clots forming and reduce swelling in your leg<br />
and ankle. Early movement of your leg will also help to reduce tightness and pain of the leg<br />
wound. You can help to reduce swelling in the leg by sitting with your leg up, knee fully<br />
supported by a pillow or chair, so that your foot is higher than your hip. This helps the fluid to<br />
drain away more easily. Also, do not sit with your legs crossed as this reduces the normal<br />
flow of blood in the veins.<br />
1. Lying on your back or sitting,<br />
bend and straighten your ankles quickly.<br />
Repeat 10 times.<br />
Date taken…………………………<br />
I need to get my cholesterol re-checked in three months time on ……………………………at the<br />
GP surgery.<br />
40<br />
13
2. Sitting up in bed, bend<br />
your hip and knee upwards.<br />
Repeat 10 times.<br />
On the second day after your operation, you are likely to start walking with help from your<br />
physiotherapist. If necessary, you can be given a walking aid to assist with your walking. Between<br />
the third and fourth day after your operation you will be encouraged to walk without supervision<br />
around the ward. Before you go home, if appropriate, your physiotherapist will make sure you can<br />
climb the stairs safely.<br />
Arm and shoulder exercises<br />
In order to prevent stiffness in your shoulder joints and to stretch the scar tissue over your<br />
breastbone, your physiotherapist will teach you to do arm exercises. They should be carried out<br />
five times each, three times a day, until full pain-free movement is gained.<br />
From day 1 after your operation:<br />
1. Lying on your bed or sitting<br />
raise one arm out in front and then up<br />
above the head. Progress to raising both<br />
arms together.<br />
You have probably heard the doctor or nurse say something like, ‘the BP is 140 over 80’. Blood<br />
pressure is measured in millimeters of mercury. This is usually written down as mmHg. The top<br />
number (140) is the pressure that your heart is pumping at (systolic). The lower number (80) is<br />
the pressure between heart beats when the heart relaxes (diastolic).<br />
High blood pressure is often unrecognised as there are no obvious symptoms. This is why<br />
hypertension is particularly dangerous. If left untreated, it can cause damage to many parts of<br />
the body including blood vessels, the heart, the kidneys and the eyes. It is a major risk factor for<br />
hardening of the arteries, heart attack, stroke, heart failure, kidney failure and sight loss.<br />
You should have regular blood pressure checks at your GP surgery. A small reduction in blood<br />
pressure can help protect your heart. You can help by:<br />
• not smoking<br />
• reducing your weight by eating healthily<br />
• using less salt when cooking or on your food<br />
• reducing your alcohol intake<br />
• becoming more active and taking regular exercise<br />
• taking your prescribed medications<br />
• avoiding stressful situations<br />
• practicing relaxation and using other stress management techniques.<br />
My blood pressure is:……………………………………………….mmHg<br />
Once at home include:<br />
2. Standing - raise both arms out to the side,<br />
then up above the head.<br />
At six weeks after the operation include:<br />
3. Standing or sitting - stretch both arms<br />
back. Hold each stretch for 10 seconds.<br />
14<br />
39
Stress<br />
Research evidence has shown that, for some people at least, stress may contribute towards<br />
coronary heart disease. Stress is hard to measure but it is known that stress increases the<br />
production of cortisol and adrenaline which prepares the body to react to a new challenge or to<br />
cope with danger or emergencies. These hormones can increase blood pressure and encourage<br />
clotting in the arteries.<br />
Stress can also affect how you feel psychologically and change the way you respond in situations<br />
that you perceive as challenging. We all experience stress in different ways and have good stress<br />
and bad stress. Too much bad stress over a long period of time can have a negative effect on<br />
your health and wellbeing. It is important to be able to recognize when stress is affecting you and<br />
identify the things that are causing you stress.<br />
Stress can make you rely on short term fixes rather than taking long term action to deal with<br />
stress. It can encourage less healthy behaviours such as overeating, drinking too much alcohol or<br />
smoking rather than spending time on healthy behaviours such as relaxation or physical activity.<br />
Take time to look at the kind of things that are stressful to you. By identifying the sources of<br />
stress, you can start to think about how you can deal with them. Try to reduce the source of<br />
stress if you can. Even if you cannot change a situation, it may help to talk to someone about it.<br />
Using relaxation techniques as described earlier in the booklet can help to reduce your stress<br />
levels. Also your cardiac rehabilitation may have a stress management programme you can<br />
attend during your rehab period or after.<br />
There are many things you can do to manage stress or anxiety.<br />
• Avoid stressful situations at home or work if you can.<br />
• Learn to say no to people when you feel overburdened.<br />
• Learn different techniques for managing stress.<br />
• Talk to family or friends or find out about support groups.<br />
• Learn to relax. There are many different ways of relaxing<br />
such as physical activity, yoga or relaxation techniques.<br />
• Making changes to your lifestyle such as taking more<br />
exercise, healthy eating, cutting down on alcohol and<br />
giving up smoking.<br />
• Making more time for yourself and enjoying activities<br />
that make you feel good.<br />
High blood pressure (hypertension)<br />
Blood pressure (BP) is the pressure in the arteries as the heart pumps blood around the body.<br />
Ideally your blood pressure at rest should be no more than 140/85 (or 130/80 if you are diabetic).<br />
It is normal for your blood pressure to rise and fall depending on your activity.<br />
High blood pressure happens if the walls of the larger arteries lose their natural elasticity and<br />
become rigid, and the smaller arteries or vessels constrict (become narrower).<br />
As we get older, we often need a ‘higher pressure’ to force the blood through vessels that have<br />
‘stiffened’ with age.<br />
So, what might be a high reading for a young person can be perfectly normal for someone older.<br />
Your doctor or nurse will tell you the correct reading for you.<br />
38<br />
Moving about the bed<br />
We encourage patients to be independent in moving about and getting on and off the bed and<br />
chair as early as possible. You will find it less painful to move up and down the bed by shuffling<br />
your bottom from side to side. When getting off the bed it is easier to roll onto your side first,<br />
swing your legs over the edge of the bed and then push up with your arms. Do the same in<br />
reverse for getting into the bed. It is important in the early stages not to put too much pressure<br />
through your arms. You will be advised how to do this correctly by your physiotherapist.<br />
Positioning and Posture<br />
When you are in bed or sitting in a chair it is important to be as upright as possible, with your<br />
head supported and your shoulders relaxed. This will help you with your breathing and also help<br />
to relieve tension in your muscles. Also remember not to allow yourself to become round<br />
shouldered or 'stooped'. This could lead to poor long-term posture and discomfort.<br />
Clothing Advice<br />
Please wear underpants as soon as possible if you have any groin surgical wounds. If you are<br />
female, please wear a bra as soon as you can (unless you have pacemaker wires or ECG wires<br />
etc). Wearing a bra whenever possible will help reduce pressure on the chest wound. A surgical<br />
pad or some gauze can be fitted under the bra to minimize discomfort across the wound.<br />
Physical effects of surgery<br />
Below are some common immediate post-operative problems. They can be attributed to<br />
the surgery, the effects of the heart/lung bypass machine or the anaesthetic used during<br />
the operation. Most of these problems should settle during the first few weeks after your<br />
operation.<br />
• Tiredness. This is very common and may last for up to six weeks. Ensure you pace<br />
yourself with any activities you may do.<br />
• Sore throat and hoarse voice. Due to bruising of tissues by the tube in your mouth.<br />
• Sweatiness. Suddenly feeling hot and cold and having night sweats is normal. It is<br />
due to the temperature regulation of your body settling down again.<br />
• Change in sense of smell. This should soon return to normal.<br />
• Reduced sense of taste for a short time only. Many people have a metallic taste in<br />
their mouths or find that all food tastes the same or is tasteless.<br />
• Poor appetite. Try to eat something at each meal time and eat a small snack between<br />
meals. This is important for both nutrition and wound healing.<br />
• Indigestion and constipation. This is also common, as normal function of the gut<br />
slows down during surgery. Inform your nurse if you have a problem so they may give<br />
you something to help.<br />
• Visual disturbances. You may have blurred vision, spots before your eyes and visual<br />
hallucinations. It is advisable to wait about three months before having your eyes<br />
tested.<br />
15
• Vivid dreams. These are commonly experienced during the early days.<br />
• Thumping sensations. Many patients experience a thumping noise in their ears or at<br />
the back of the head when lying flat or on their left side. If this occurs, change your<br />
position. It will settle after a few weeks.<br />
• Fast Heart Rate. You may feel your heart beating fast, irregularly or missing a beat,<br />
especially at night. This is very common after heart surgery and is a reaction to the<br />
heart being handled during surgery. You should inform a member of staff. You may<br />
be attached to a monitor for a short time and will need to carry a portable transmitter<br />
with you. A fast heart rate is easily treated with medication (see page 19).<br />
• Discomfort. It is quite common after major chest surgery to have aches and pains in<br />
your back, neck, shoulders and in the front of your chest. This discomfort is due to<br />
stiffness in the muscles and ligaments that have been stretched during the operation.<br />
Do not confuse this with angina, which you may have had before the operation. The<br />
degree of pain is extremely variable and is often worse in the morning after waking,<br />
late at night and when moving arms and shoulders. It will improve with time, but may<br />
take up to three months or even longer. It is important that you take adequate pain<br />
relief.<br />
• 'Clicking' of breastbone. It is not unusual to feel the edges of the breastbone 'grate'<br />
together for the first few weeks. However, frequent 'grating' or 'clicking' when moving,<br />
coughing or sneezing should be reported to a member of staff on the ward or your GP.<br />
• Lump or swelling at the top of the chest wound. This should gradually disappear<br />
over several weeks.<br />
• Ache or stabbing pain inside the chest. This is common when the internal mammary<br />
artery is used especially when moving (see page 6). It tends to occur in the same place<br />
each time. You may be aware of an area of numbness, tingling or discomfort on the<br />
outside of your chest, which can be temporary or remain permanent for some people.<br />
Leg incision - there are three main after effects:<br />
• Pain. It is common to experience pain along the wound site, particularly if the wound<br />
crosses the knee joint or extends to the groin area. Gentle movement of the leg will<br />
help to ease this pain.<br />
• Numbness. It is common to experience unusual sensations (pins and needles and<br />
numbness) along the leg wound. At the lower end of the wound there may be a small<br />
area which feels numb. This is because a small nerve, which runs to this area of the<br />
foot and ankle, lies very near the veins and it often stops working after being disturbed.<br />
These sensations are likely to improve after a few months.<br />
• Swelling. It is normal for swelling to occur in the ankle and leg from which the vein<br />
was removed. It is often present for about three months, until the other veins have<br />
taken over the job of the missing vein. Wearing compression (also called anti-embolitic<br />
or thrombo-embolus deterrent -TED) stockings can help to prevent fluid from<br />
accumulating in the tissues and reduce the risk of you developing a blood clot<br />
immediately after your surgery.<br />
16<br />
You can do this in three ways:<br />
• by eating and drinking fewer calories<br />
• using more calories by becoming more active<br />
• a combination of both the above.<br />
Most people find that doing both achieves the best results.<br />
In order to determine if someone is a healthy weight it is important to consider both the Body<br />
Mass Index (BMI) i.e. height in relation to weight and waist circumference. Ask the nurses on the<br />
ward or the cardiac rehabilitation team in hospital to measure these to see how much weight you<br />
need to lose. Please see page 47 for further information.<br />
Alcohol<br />
Many people enjoy a drink and alcohol in moderation is fine. It is thought that a small amount of<br />
alcohol may actually protect the heart from coronary heart disease. However an increased intake<br />
of alcohol may result in high blood pressure. All alcoholic drinks contain calories but little else of<br />
nutritional value. If you are trying to lose weight you should reduce your intake of alcohol to below<br />
recommended levels or less. It is also recommended you have two alcohol free days in the week.<br />
Current advice:<br />
Men:<br />
3 - 4 units per day, 21 units in total for the week<br />
Women: 2 - 3 units per day, 14 units in total for the week<br />
These guidelines apply whether you drink everyday, once or twice a week or occasionally.<br />
It is not accurate to say one glass of wine is one unit. How many units a drink contains depends<br />
on the strength of the drink (%ABV) and the volume of liquid. In order to work it out you multiply<br />
the volume of drink by %ABV, and then divide by 1000.<br />
e.g. 175ml glass of 14% wine = 175 x 14 ÷ 1000 = 2.45 (2.5 units)<br />
A small glass of wine A large glass of wine 1bottle of alcopop<br />
1.5 units 3.5 units 1.7 units<br />
Double measure of spirits A pint of strong lager A pint of strong cider<br />
3 units 5 units 4.5 units<br />
My alcohol consumption in one week is:…………………………………………..<br />
37
Studies show that benefits of using NRT to quit smoking outweigh any risks there may be with<br />
NRT. There are six different products available including: patches, inhalator, gum, lozenge, micro<br />
tab and nasal spray and also two medication products which can be prescribed by your doctor or<br />
smoking cessation clinic.<br />
The nicotine replacement therapy I have chosen is……………………………………………….<br />
…………………………………………………………………………………………………….........<br />
If you require further help or advice on NRT whilst you are in hospital we can refer you to the<br />
smoking cessation nurses (0161 291 5030) who can offer you support in stopping smoking.<br />
You can also obtain help from:<br />
• National NHS Quit line 0800 169 0169<br />
• Manchester Stop Smoking Service 0161 205 5998<br />
www.stopsmokingmanchester.co.uk - www.gosmokefree.co.uk<br />
• Practice nurse at your GP practice.<br />
Lack of physical activity<br />
Before coming into hospital for surgery you may have been<br />
limited as to the amount of activity you could do. Following<br />
your operation you should now find that you are able to do a<br />
great deal more. It is important to take some form of exercise<br />
as a non-active lifestyle can be considered another risk factor.<br />
It has been shown that inactive people have twice the risk of<br />
developing coronary heart disease compared with active<br />
people.<br />
Your local cardiac rehabilitation team will advise you regarding<br />
appropriate exercise. Physical activity and the heart are<br />
discussed on page 26.<br />
Poor diet<br />
Eating should be a pleasure. A healthy diet does not mean eating things you do not like. There is<br />
no such thing as bad or good foods. The key to a healthy diet is to have a balanced diet so you<br />
get all the nutrients you need.<br />
Dietary advice is discussed in detail on pages 43 - 47<br />
Being overweight<br />
Being overweight can make you more at risk of developing<br />
conditions such as high blood pressure, diabetes, osteoarthritis<br />
and coronary heart disease. Losing weight has many health<br />
benefits as well as making you feel more energetic and<br />
increasing your confidence. To lose weight you need to use<br />
up more energy (calories or joules) than your body takes in<br />
from food and drink.<br />
36<br />
The nursing staff on the ward will advise, as appropriate, on:<br />
• the need to wear compression stockings (for you as an individual)<br />
• the need to take them off every day to wash your legs and check the condition of<br />
your skin<br />
• the need to change and wash them regularly<br />
• the length of time your consultant has asked for you to continue wearing them<br />
post surgery<br />
• how to ensure they are pulled up correctly as areas where the stockings ‘bunch<br />
up’ will put pressure on your legs and may cause an indentation (sunken ridge)<br />
where they put pressure on the soft tissues.<br />
Psychological effects for you and your family<br />
• Lack of concentration and memory lapses. Many people find it difficult to<br />
concentrate when reading and often find they cannot remember simple things,<br />
for example their own telephone number. This should improve over the first few<br />
weeks, but you may continue to be affected for 6 -12 months, when you are tired<br />
or under stress.<br />
• Change in mood or emotion. Immediately following a major operation it is<br />
perfectly normal to have days when you feel down, depressed, more emotional<br />
than usual and even tearful. On other days you may feel on top of the world. It is<br />
possible for these feelings to recur now and again over the next 12 months. They<br />
will go with time, as you become stronger and more confident.<br />
• Anxiety. This is quite common following major surgery. This may result in<br />
feelings of irritability, tension, poor sleep, lack of energy and anxieties about<br />
minor aches and pains. There is also fear and frustration that you might not be<br />
making sufficient progress and a tendency to compare yourself with someone<br />
else. Try to avoid making comparisons as everyone is different and recovers at a<br />
different pace. It is important to think positively and remember that the aim of the<br />
operation is to improve your quality of life.<br />
• Your family may also have worries about your discharge from hospital. We would<br />
encourage you to talk about the written and verbal information you have been<br />
given. Try and explain how you feel to help your family understand. It is also<br />
important for the person looking after you to have a break during the day.<br />
Wound care, healing and bathing<br />
Your wound dressings will normally be removed 48 hours after your operation; if your<br />
wounds are clean and dry they will be left uncovered. If they are oozing, another dressing<br />
will be applied.<br />
Most of the wounds are sewn together using dissolvable stitches which cannot be seen<br />
when the dressing is removed. Occasionally stronger stitches are used in addition to the<br />
dissolving sutures. These are usually removed 10 days after surgery, either in hospital or at<br />
home by the district nurse. Very occasionally, a piece of ‘stitch’ remains beneath the skin<br />
and looks as though it has come out of the wound. If it becomes troublesome, arrange to<br />
see your GP.<br />
17
The skin layers will begin to heal very quickly and top layers are usually healed sufficiently within<br />
48 hours. They will continue to heal across the full depth of the wound for at least a further six<br />
weeks or more. As the wound heals, the scar shrinks to a thin white line. Occasionally it can<br />
remain red for a long time.<br />
It is vitally important that you look after your surgical wounds once you get home. You should<br />
report immediately, to your nurse or GP, if you notice any of the following symptoms:<br />
• increased pain – as the wounds heal the pain should decrease steadily<br />
• discharge (leakage)<br />
• increased redness/tenderness – the skin around the wound edges should be healthy<br />
in appearance<br />
• swelling<br />
• itching.<br />
At first we will help you to wash yourself but you will be encouraged to become independent as<br />
soon as possible. It is important to keep your wounds clean. A warm daily bath or shower will<br />
keep your wounds clean and encourage healing. Avoid strong perfumed soaps as they can<br />
cause irritation. Do not use flannels on wounds as they can harbour bacteria and can actually<br />
infect wounds. Use either your hand or a disposable cloth to wash the wound. If you need to<br />
touch your wounds make sure you wash your hands first and then afterwards to avoid<br />
contamination with unseen germs.<br />
Going home<br />
You will be able to go home when the doctor thinks you are medically fit.<br />
When you go home, a relative or friend should collect you from the ward. The nursing staff can<br />
give you a sickness certificate covering your stay in hospital.<br />
In most modern day cars, front airbags are standard. In the event of an accident, activation of an<br />
airbag could cause considerable harm to your chest. It is therefore not advisable to sit in the<br />
front passenger seat for the first six weeks.<br />
Medication<br />
A pharmacist or pharmacy technician will sort through any medication you bring into hospital.<br />
When you leave hospital you will be given at least one week’s supply of medication to take<br />
home. Your nurse or pharmacist will explain how and why to take your tablets before you are<br />
discharged. You will be given a copy of the discharge prescription for your own records. Your<br />
GP will prescribe your medication from there on. Continue to take your prescribed medication<br />
until you are told not to, either at the out-patient clinic, or by your GP. If you have supplies of<br />
your medication at home and are unsure whether you are still to take them, ask your GP or local<br />
pharmacist (chemist).<br />
Following surgery, you will find that your medication will be altered. Angina medication such as<br />
Isosorbide Mononitrate, and Nicorandil (Ikorel) will be stopped. However, medicines for other<br />
medical conditions you have will normally be restarted following your operation. The doses of<br />
these medicines might have changed so please check carefully.<br />
18<br />
Section D – Maintaining a healthy heart<br />
Risk factors associated with the development of coronary<br />
heart disease<br />
In Britain today we continue to have one of the highest rates of heart disease known in the<br />
western world. Although no single reason has been shown to cause coronary heart disease,<br />
research has shown that certain factors in a person’s lifestyle can increase the risk of getting<br />
coronary heart disease. These factors contribute to narrowing of the arteries surrounding the<br />
heart, which leads to coronary heart disease.<br />
These factors are called risk factors and generally fall into two categories; modifiable and<br />
non-modifiable. Modifiable means you can do something about them. Non-modifiable means you<br />
cannot change them. Many non-modifiable risk factors can be controlled and their effect reduced<br />
by making changes to your lifestyle.<br />
It is important to remember that some people may have many risk factors and others may have<br />
none.<br />
Modifiable risk factors<br />
Smoking<br />
Major studies show that smoking is the most significant preventable risk<br />
factor. People who smoke tobacco have twice the risk of developing<br />
coronary heart disease as those who do not. People who do not smoke<br />
but have to inhale the smoke from others (passive smoking) are also at<br />
risk of heart disease.<br />
Smoking affects the heart in many ways: There are more than 4000<br />
chemicals contained in tobacco smoke, many of which are harmful<br />
when inhaled by smokers and those around them. Smoking just three<br />
cigarettes a day doubles the risk of having a heart attack. Other main<br />
components include;<br />
Carbon monoxide. This is a poisonous, invisible gas with no smell. It is found in car exhausts,<br />
leaking gas heaters and burning cigarettes. It is carried around the body in the blood. To try and<br />
get more oxygen in, the heart beats faster and more red blood cells are produced. The heart has<br />
to work harder which increases the risk of heart attack or heart failure.<br />
Nicotine. This is the drug that causes addiction. It is very powerful and fast acting, hitting the brain<br />
in seven seconds after each drag. Nicotine appears to have minimal long term effects on health. In<br />
the short term it causes stimulation of the nervous system and an increase in blood pressure and<br />
heart rate. These return to normal after about 20 minutes (Manchester Stop Smoking Service 2007).<br />
Even if you have tried to give up before, it is worth another try. Stopping smoking dramatically<br />
reduces your risk of a heart attack and stroke. Did you know that former smokers live longer than<br />
continuing smokers, no matter what age they stop smoking, so whatever age you are, it is never<br />
too late to stop. Your chances of a heart attack or stroke reduce with every day you continue not to<br />
smoke.<br />
Nicotine Replacement Therapy (NRT) helps by providing the body with nicotine. The purpose of<br />
NRT is to take the edge off withdrawal symptoms. The nicotine provided from NRT is clean i.e. it<br />
does not contain the other 3999 chemicals found in cigarette smoke. Consequently it can now be<br />
used by smokers with cardiovascular disease. Stopping smoking is critical for those with heart<br />
disease as it can slow the progression of the disease down.<br />
35
Generally you may return to:<br />
Light occupations from 8 weeks after your operation<br />
Management type work 10 weeks after your operation<br />
(if stressful, you should<br />
look into ways to modify it)<br />
Manual work 3 - 4 months after your operation<br />
(including lifting weights<br />
- you should build up to this<br />
kind of work gradually)<br />
Holidays and air travel<br />
A restful holiday in this country may be taken after the first couple of weeks at home, as long as<br />
you are well and able to cope with the travelling. During a long journey, you should have frequent<br />
breaks and get out of the car to stretch your legs.<br />
After heart surgery there are usually no restrictions placed on air travel. If it is vital that you fly<br />
before your clinic appointment (usually about 6 - 8 weeks after your operation), discuss this with<br />
your doctor prior to discharge. Otherwise delay a holiday abroad until you are feeling stronger and<br />
more able to cope with a change in climate. During a long flight you should walk up and down the<br />
aisle of the aircraft every half hour or so. Avoid lifting and carrying very heavy luggage for long<br />
distances. Make use of the baggage trolleys wherever possible.<br />
Make sure that you have adequate health insurance. Check your policy carefully. If you go<br />
somewhere very hot protect your scar with a sun block. In hot weather you will tire more easily so<br />
reduce the intensity of your daily exercise.<br />
For more information please contact the British Heart Foundation or visit www.bhf.org.uk<br />
Sexual intercourse<br />
Sexual activity may be resumed after about four weeks, but be guided by how you are coping<br />
with other physical activities. It is normal to feel anxious about resuming your sex life so start<br />
when you feel ready and ensure you and your partner talk about your feelings. Cuddling,<br />
touching and caressing are good ways to build up self-confidence and may help you both to<br />
resume your normal relationship.<br />
It may be helpful to keep the room and bed at a relaxing temperature. Choose a position which<br />
is comfortable and does not place a strain on your chest. It is sensible to wait a few hours<br />
following a meal or after drinking alcohol. Ask your partner to play a more active role.<br />
Emotional stress and some of the tablets that people take for their heart condition can cause<br />
problems for a very small number of people. Men may experience problems with their erections;<br />
women may lose their desire to make love. Talk to your doctor or nurse about it; don’t be shy.<br />
A simple change of medication may be all you need.<br />
Pain killers<br />
e.g. Paracetamol, Dihydrocodeine, Codeine, Tramadol<br />
Take your painkillers regularly as prescribed by your doctor, for as long as you have pain.<br />
This will help you to breathe deeply, cough, sleep, move around more comfortably and<br />
exercise. Dihydrocodeine (and Codeine) commonly cause constipation. You can take<br />
regular laxatives to prevent and treat this.<br />
Aspirin<br />
Aspirin will normally be restarted following surgery, although your dose may have changed.<br />
If you cannot take aspirin you will be prescribed Clopidogrel (Plavix). These medicines<br />
reduce the ‘stickiness’ of your blood and reduce the risk of clots forming in the new grafts.<br />
Lipid lowering medication<br />
e.g. Simvastatin (Zocor), Pravastatin (Lipostat), Atorvastatin (Lipitor)<br />
These medicines will normally be restarted following surgery. They help reduce the<br />
likelihood of your grafts becoming narrowed or blocked, due to fatty deposits. Occasionally,<br />
the dose may be increased in order to achieve a lower cholesterol level. We recommend<br />
that you take them in the evening as this is when your body produces the most cholesterol<br />
and the level in your body is the highest.<br />
Blood pressure lowering medication<br />
e.g. Bendrofluazide, Bisoprolol, Ramipril, Doxazosin, Amlodipine<br />
These medicines may or may not be restarted in hospital after your operation. This will<br />
depend on your blood pressure. If they are restarted then this is frequently at a lower dose<br />
than before your heart surgery. Once you return home, your GP or practice nurse should<br />
check your blood pressure regularly. It may then be necessary for the GP to gradually<br />
increase the dose again.<br />
Angiotensin-converting enzyme (ACE) inhibitors<br />
e.g. Ramipril, Lisinopril, Perindopril<br />
ACE inhibitors work in a complex way by stopping certain enzymes working within the body.<br />
They are used to help the heart pump blood around the body, if you suffer from heart failure<br />
and are also used to treat high blood pressure.<br />
After surgery, using an ACE inhibitor can prevent your heart from weakening further and<br />
has been shown to reduce the risk of you suffering a heart attack, whether or not you suffer<br />
from high blood pressure.<br />
After starting on an ACE inhibitor some patients complain of a dry tickling cough. This is a<br />
possible side effect of the drug. We advise patients that they should continue taking the<br />
tablets. However if the cough becomes troublesome your doctor may reduce the dose or<br />
stop the tablets and prescribe a suitable alternative.<br />
34<br />
19
Medication to control heart rhythm<br />
e.g. Bisoprolol, Amiodarone, Digoxin<br />
It is possible that you may be started on a medicine to correct an irregular/fast heart beat, which<br />
sometimes occurs after this type of surgery (see page 16).<br />
Medication to reduce amount of acid in the stomach<br />
e.g. Lansoprazole, Omeprazole, Ranitidine<br />
These are commonly started after surgery to protect your stomach. If you were not on this type of<br />
medication before your operation, it is normally stopped shortly after discharge.<br />
Medication to remove extra fluid from your body (water tablets)<br />
e.g. Furosemide, Bumetanide, Co-Amilofruse (Frumil)<br />
After surgery you may be started on a water tablet if you have any extra fluid in your body. This<br />
may only be for a short while and the tablets will be stopped before you go home. Sometimes the<br />
doctors will send you home on these drugs if they think that the fluid will return if you stop taking<br />
them or if you are still retaining excess fluid. Water tablets should be taken in the morning. If you<br />
have to take them more than once a day, you should take the second dose before tea-time or you<br />
may find that you are waking up in the middle of the night to go to the toilet.<br />
Anticoagulants<br />
This information applies to all patients who have a mechanical valve and in a few circumstances<br />
to some patients with a tissue valve or who have had coronary artery bypass grafts.<br />
The most common anti-coagulant treatment is called warfarin. Warfarin slows the clotting of the<br />
blood and so prevents clots forming on the new valve. The clotting or ‘thinness’ of your blood is<br />
measured by a blood test. This is called the International Normalised Ratio (INR). The higher the<br />
INR the ‘thinner’ the blood. The doctors will decide what the Target INR should be, for each<br />
patient, receiving warfarin. The dose of warfarin may change from day to day, but this is quite<br />
normal. You will only be allowed to go home when your blood is ‘thin enough’ and the desired INR<br />
has been achieved.<br />
The hospital normally supplies 1mg (brown) warfarin tablets. The doctors will prescribe your daily<br />
dose of warfarin in milligrams (mg). For example, 4mg of warfarin is four brown warfarin tablets.<br />
This should be written in your yellow anticoagulant book. There is some important information in<br />
the front of the anticoagulant book that you must read. We recommend you carry your<br />
anticoagulant book with you. You must inform doctors, dentists, and pharmacists about your<br />
anticoagulant treatment.<br />
It is best to take your warfarin at the same time each day, at tea-time. If you forget to take your<br />
warfarin at the usual time, but remember later the same day, you can take your dose.<br />
However, if you remember the following day, do not take the dose you have missed, but do take<br />
the dose for that day as prescribed. Please make a note of any missed doses in your<br />
anticoagulant book.<br />
20<br />
• if you are feeling tired<br />
• if you are unwell with a virus, cold or stomach bug. Wait until at least two days after the<br />
symptoms have disappeared.<br />
If you or your relatives have worries about you starting or progressing physical exercise, please<br />
contact the cardiac rehabilitation physiotherapists on 0161 291 2177 or<br />
cardiac.rehab@uhsm.nhs.uk<br />
Driving<br />
Although the Driver and Vehicle Licencing Agency (DVLA) say you may start driving at one month<br />
after your operation, we prefer you to wait at least six weeks. It is essential that you do not drive<br />
until the healing process is sufficiently advanced to allow you to cope with sudden movements. As<br />
the recovery process varies from person to person, it is advisable to check with your doctor first.<br />
It is advisable to inform your car insurance company of the operation you have had or you may<br />
invalidate your insurance. If you decide you would like to change your insurance company, the<br />
British Heart Foundation provide a list of current companies who do not raise their premiums for<br />
people after heart surgery. If your insurance company insists on a fitness to drive certificate your<br />
GP should issue this. You do not need to inform the DVLA of your operation unless you have<br />
recurrent angina, attacks of dizziness, palpitations or are diagnosed with diabetes.<br />
You are not exempt from wearing a seat belt. Try placing a small flat cushion between the belt<br />
and your chest for protection. If necessary, you can purchase a plastic product from shops which<br />
relieves the tension from the seat belt. It eases any discomfort caused by the seat belt rubbing<br />
across your chest and shoulders but it allows the seat belt to work normally in an emergency. You<br />
should avoid driving in heavy traffic at first, as this can be very stressful. Increase driving<br />
gradually in the same way as physical exercise starting with a short, quiet drive with a friend or<br />
partner to help you regain your confidence.<br />
Large goods and public carrying vehicle licences<br />
If your job requires that you hold a large goods vehicle (LGV) or passenger carrying vehicle<br />
(PCV) licence, you must inform the DVLA of your medical condition. You can also visit<br />
www.direct.gov.uk or contact the DVLA on their direct line for HGV/PCV enquiries on<br />
0870 241 1879 to speak to staff with additional training regarding Group 2 guidelines. Under the<br />
medical conditions and disabilities section you should download, fill in and return questionnaire<br />
VOCH1 to tell the DVLA about your medical condition. Re-licensing will be considered after a<br />
successful exercise test result and a satisfactory report from your cardiologist.<br />
Returning to work<br />
Most patients who want to return to work will be able to return to their previous occupations.<br />
Where possible, you should leave the decision of when and whether to return to work until you<br />
feel able to cope with considering all the options open to you. When you return, will depend on<br />
the type of work you do and the amount of physical or emotional stress involved. Discuss your<br />
individual circumstances with your consultant or GP and your employers.<br />
Attending your local cardiac rehabilitation programme can help you in your return to work by<br />
discussing your progress week by week and reviewing your exercise programme. Ideally you<br />
should begin working on a part-time basis and gradually increase the hours worked. Your<br />
employer may be willing to give you lighter duties when you first go back. If a change of<br />
employment is suggested, the Disability Employment Adviser (DEA) at the Job Centre is available<br />
to help you find a suitable new occupation.<br />
33
Active hobbies and sports<br />
In most cases you may return to activities you previously enjoyed. If you were not physically<br />
active before your illness you may now decide to take up a new enjoyable activity. When<br />
undertaking any activity always start gently and gradually build up. If one particular activity<br />
causes discomfort, it should be discontinued and replaced with another.<br />
It is important to remember that each person’s progress with an activity will be different. It may<br />
depend upon whether it is a new activity or sport for you, your rate of recovery after your<br />
operation and your previous level of fitness.<br />
At six weeks after your operation it is recommended that you attend a cardiac rehabilitation<br />
programme in your local area (see page 23) to improve your fitness. You will obtain guidance<br />
regarding the sports and activities you may do and at what stage they may be undertaken.<br />
You will need to attend the anticoagulant clinic at your local hospital for regular blood tests. The<br />
staff on the ward will give you details of your first appointment. Your anticoagulant clinic<br />
appointments will be quite often to begin with. Once your dose is stabilised, your appointments<br />
will become less frequent. It is useful if you take a list of your medicines (such as a copy of the<br />
take home prescription) with you to the clinic, especially on your first visit.<br />
Many medicines will interact with warfarin. They can increase its effect, making the blood even<br />
thinner or work against it and lead to a thickening of the blood (both of these things can have<br />
serious implications). For this reason, ALWAYS check first with a doctor or pharmacist before<br />
deciding to take any medicines that are not part of your usual regimen, such as those you may<br />
have purchased over the counter. Despite the cautions highlighted, warfarin is an extremely<br />
valuable medicine for certain heart patients.<br />
Medication list<br />
• Cycling - start with short periods on the flat, preferably not in heavy traffic. Increase the<br />
distance, speed and include hills when you feel able, in the same way as with your<br />
walking programme.<br />
• Static cycling - may be started slightly earlier but do not put too much weight through<br />
your arms as your breastbone will still be healing.<br />
• Bowling - you can start playing using light wood bowls. Practice gently swinging your<br />
arm before you play. Gradually increase to playing with your usual weight of wood and<br />
to a full game.<br />
You can list all your heart tablets below<br />
Name of tablet What is the dose? How often<br />
you take it?<br />
What are they for?<br />
• Dancing - this is an excellent exercise and also a very sociable one. You may return to<br />
ballroom dancing once you can hold your arms up for a period of time.<br />
• Golf - start by walking the course and putting the ball but wait 8 -12 weeks before<br />
starting the full swing. It may be useful practicing on the driving range before attempting<br />
a full game of golf. Ensure you do not carry your golf clubs. You should make use of a<br />
trolley, preferably a powered one.<br />
At 12 weeks after your operation you may consider one of the activities below.<br />
• Swimming - if you are a keen swimmer and wish to return, make sure your wounds are<br />
fully healed before you go for a swim. Start by swimming widths in the shallow end<br />
before you progress to swimming lengths. If you have not previously been a regular<br />
swimmer, the cardiac rehabilitation team may advise that at first it may be more<br />
preferable to take up a different activity.<br />
• Tennis and badminton - avoid a high level of competition for up to six months.<br />
• Fishing, jogging, football - be guided by your cardiac rehabilitation team member.<br />
Avoid sports which are highly competitive or of high intensity, which impose sudden severe loads<br />
on the heart, such as squash, scuba driving, water skiing or weight lifting. If you want to start<br />
contact sports, such as rugby, discuss this with your GP or cardiac rehabilitation team member<br />
before beginning.<br />
Avoid sports and activities in the following circumstances:<br />
• extremes of temperature<br />
• for two hours after eating a large meal<br />
32<br />
21
Your follow up<br />
• By General Practitioner<br />
You will be given a discharge summary with details of your operation and discharge medication.<br />
You should inform your GP practice when you arrive home and give them a copy of the discharge<br />
summary. The information of your operation, recovery and the medication you are on will also be<br />
faxed to your GP after discharge.<br />
You should contact your GP if you feel unwell or if you have any worries about your recovery.<br />
• Surgical out-patient appointment<br />
About 6 - 8 weeks after you go home from hospital you will see your surgeon for a check up at<br />
either the centre where you had your operation or at your local hospital. If you have not<br />
received your appointment by six weeks, please contact your surgeon’s secretary.<br />
Advice about financial matters<br />
Having heart surgery can lead to concerns about managing financial matters. There are agencies<br />
who offer free, confidential and independent advice on benefits, rent or mortgage arrears and<br />
possible rebates. Please inform the nursing staff as soon as possible if you would like to see the<br />
Welfare Rights Adviser whilst you are on the ward.<br />
Additionally there are people known as money advisers who offer advice on problems paying<br />
debts and negotiating repayments. Your local Citizens Advice Bureau will have the number of<br />
your local Welfare Rights Adviser and money advisers.<br />
Household tasks and gardening<br />
Everyone will progress at a different rate. It can depend upon your level of fitness and severity<br />
of your illness before your surgery, the nature of your surgery and your age. During activities it<br />
is important to take regular rest breaks, even when you do not feel tired.<br />
Activities should be restricted for approximately six weeks after your operation to allow time for<br />
the breastbone (sternum) to knit together and become stronger.<br />
Up to six weeks after your operation avoid activities which require pulling, pushing or a sudden<br />
burst of energy. Avoid carrying heavy shopping bags, pushing supermarket trolleys or lifting<br />
babies/toddlers. Do not lift anything heavier than about 5lbs (2.3 kg) in weight.<br />
Some people will see caring for the household and the family as mainly their responsibility. This<br />
can lead to them starting heavier household tasks sooner than they should. It is important not to<br />
feel guilty about leaving the housework for a while and letting others help.<br />
Remember the following information should only be used as a guide for returning to normal daily<br />
activities.<br />
Up to 2 weeks Take things gently. Read, listen to music or watch television.<br />
Make yourself a light snack.<br />
Week 3 Begin light activities, i.e. dusting, set the table, prepare<br />
simple meals, washing and drying dishes and tending indoor plants.<br />
Week 4 Increase activities to include light hand washing, ironing small items,<br />
changing the bed linen (do not pull the bed out).<br />
Begin activities outside (seated), such as light cutting and weeding.<br />
Begin light social activities i.e. visiting friends or going out for a meal<br />
when you feel ready.<br />
Week 5 Increase activities to include machine washing, cooking and ironing.<br />
Week 6 - 7 Increase activities to include sweeping, vacuuming, mopping floors, food<br />
shopping with trolley.<br />
Weeks 8 - 10 Wash and polish car, cleaning windows with regular rest breaks.<br />
Gardening may include digging, hoeing, raking leaves, mowing the lawn<br />
(powered mower). If possible, use a hose, rather than a watering can.<br />
Week 12 D.I.Y. – decorating, painting with regular rest breaks. Carpentry, moving<br />
furniture, trimming a hedge.<br />
Limit the amount of sustained work that you do with your arms above shoulder height as this can<br />
increase the workload of the heart.<br />
In the long term, certain activities including lifting or pushing heavy weights require a degree of<br />
caution. If you are keen to undertake these activities you can discuss this when you attend your<br />
cardiac rehabilitation programme.<br />
22<br />
31
Home exercises<br />
The following exercises should be carried out if you are unable to go for your daily walk due to<br />
bad weather:<br />
1. Standing 2. Step-ups<br />
Hold on to a stable object.<br />
Stand 10 inches away from the<br />
Push up on your toes. step. Step up with right leg for 15<br />
Hold for 10 seconds. Rest.<br />
seconds and then change to lead<br />
Repeat 10 times.<br />
with left leg for 15 seconds.<br />
Section C – Your rehabilitation<br />
What is cardiac rehabilitation<br />
Cardiac rehabilitation is a specialist service, usually delivered by a team of healthcare<br />
professionals in a hospital, community or home-based setting.<br />
We will support you and your family in helping you return to the best possible health and<br />
well-being following your operation.<br />
When do I start cardiac rehabilitation?<br />
Cardiac rehabilitation normally starts when you are in hospital. A cardiology liaison nurse will<br />
visit you on the ward to provide you with cardiac rehabilitation and give you advice to prepare<br />
you for home. As well as discussing the information in this booklet, you will have the opportunity<br />
to discuss any individual concerns about getting back to your usual activities. You will be<br />
informed of your nearest available programme and given their contact details. The <strong>UHSM</strong><br />
cardiology liaison nurse team may be contacted on 0161 291 2679.<br />
3. Walk on the spot 4. Sitting to standing<br />
Walk or march on the spot<br />
Sit on a dining room chair and<br />
at a comfortable pace for<br />
push up with one hand. Progress<br />
30 seconds. to standing up with arms crossed.<br />
Stand up and sit down 5 - 10 times.<br />
Once you are discharged, your details will be sent to your local cardiac rehabilitation<br />
programme. You should be contacted at home within one week of discharge. If you are not<br />
contacted, please call your local programme to confirm that they have received your referral. In<br />
some areas you may be contacted and/or visited by a member of staff soon after you arrive<br />
home.<br />
Depending on your individual case, you may start the exercise sessions, as part of the cardiac<br />
rehabilitation programme from 6 weeks after your heart operation.<br />
What are the aims of cardiac rehabilitation?<br />
• To give information on heart disease and its causes.<br />
• To improve your awareness and understanding of coronary heart disease.<br />
• To develop an individual plan to help you to make positive lifestyle changes.<br />
• To restore your confidence to be physically active and to exercise regularly and<br />
independently to improve your physical fitness.<br />
• To discuss physical activity and exercise opportunities for you in the future.<br />
• To reduce the risks of further cardiac problems and improve your quality of life.<br />
What do cardiac rehabilitation programmes provide?<br />
Try to begin with the time or number of repetitions suggested above.<br />
When you are able to cope comfortably with the above exercises, you may slowly progress by<br />
increasing the time or number of repetitions, for instance 30 seconds to 40 seconds, 10<br />
repetitions to 12 repetitions and so on. Refer to the scale on page 28 and do not allow yourself<br />
to become uncomfortably breathless.<br />
These programmes are available all over the country. If you have access to the Internet, you can<br />
locate your nearest programme on the website www.cardiac-rehabilitation.net The actual<br />
content varies depending upon local resources and the staffing levels available . Your spouse or<br />
partner is usually encouraged to attend with you.<br />
The main areas of provision included in any cardiac rehabilitation programme are:<br />
• Initial assessment of your individual patient needs<br />
- to discuss any concerns<br />
- to tell you about the various options within the local programme<br />
- to refer you for appropriate interventions<br />
30<br />
23
• Exercise classes<br />
- usually in a group setting, usually lasting between 6 to12 weeks.<br />
- exercises are adapted to you and you are encouraged to increase activity<br />
gradually under supervision.<br />
• Risk factor management (see page 35) and lifestyle behaviour change.<br />
• Education topics often included:<br />
- benefits and effects of physical activity and exercise<br />
- healthy eating<br />
- medication<br />
- risk factors of Coronary Heart Disease (CHD)<br />
- relaxation<br />
- emotions and feelings about CHD<br />
- recommendations for long-term physical activity and healthy lifestyle<br />
- cardiopulmonary resuscitation (basic life support).<br />
• Other possible services are:<br />
- stress awareness, stress management, and other psychological support<br />
- smoking cessation<br />
- diet and weight management.<br />
For further information about cardiac rehabilitation, please contact the Wythenshawe Hospital<br />
Cardiac Rehabilitation Service on 0161 291 2177 or email us at cardiac.rehab@uhsm.nhs.uk<br />
Alternatively you can visit the web page<br />
http//www.uhsm.nhs.uk/patients/cardiacrehab/pages/defalt.aspx<br />
First few days at home<br />
For the first few days at home, you should rest, following the same routine as in hospital. You<br />
may walk around the house and up and down stairs as necessary.<br />
During this time it is quite common for you to only want to see close friends and family. As<br />
receiving visitors can be very tiring, ask them to stay for a short period only so you can enjoy<br />
their company without getting over-tired. It is advisable to have no more than two visitors a day<br />
for the first two weeks.<br />
For the first few days it is advisable to have someone with you at all times if possible. You may<br />
get out and about and be driven to places as soon as you feel able.<br />
Sleep and rest<br />
It is normal to feel tired in the first few weeks after leaving hospital. During this time it is<br />
important that you get adequate sleep and rest, as there is still a lot of healing taking place.<br />
Take a rest as necessary. It is sensible to rest for at least ten minutes after a meal or after<br />
having a shower.<br />
It can take a few weeks to settle back into your normal sleep pattern. You can help yourself by<br />
going to bed at your usual time and making yourself as comfortable as possible. Use as many<br />
pillows as you need and sleep in your normal position. Avoid lying on your stomach for the first<br />
six weeks due to the healing of the breastbone. If you wake in the night, try getting up and<br />
moving around before settling back down again.<br />
24<br />
You should always be able to walk and talk at the same time. Feeling slightly short of breath<br />
whilst exercising is normal, but you should not feel exhausted.<br />
If you do too much one day, rest the following day and then continue at a reduced level the<br />
next day until you feel happy to increase it. Listen to your body and on days when you feel<br />
less energetic, reduce the amount you do or walk at a slower speed. Be careful if walking a<br />
dog on a lead as the dog may pull too much or want to walk at a faster pace.<br />
Below is intended as a guide to the amount of walking you may undertake:<br />
Stage of recovery<br />
(approximate)<br />
Week 1<br />
Week 2<br />
Week 3<br />
Week 4<br />
Weeks 5 - 6<br />
Target<br />
It is better to go for your walk in the day time, preferably the morning. Do not leave it until the<br />
evening when you are likely to be tired. Do not go for a walk sooner than one hour following<br />
a meal. In cold or windy weather, wear a hat, scarf and gloves, as the heart has to work<br />
much harder in these conditions.<br />
Gradually progress by:<br />
Length of walk (in minutes)<br />
Gradually increase the time you spend walking as<br />
you feel ready<br />
5 minutes, several times a day as a stroll<br />
10 minutes, twice a day, leisurely pace<br />
15 minutes daily, leisurely pace<br />
20 minutes daily, moderate pace<br />
25 - 30 minutes daily, moderate/brisk pace<br />
At least 30 - 40 minutes daily, brisk pace<br />
• increasing the distance or time of your walk (as above). If you find a week difficult,<br />
repeat the week (rather than increasing) until you are able to progress comfortably.<br />
• increasing the speed of your walk – start by strolling at a leisurely pace, then walk<br />
at a moderate pace and aim to walk at a brisker pace by six weeks.<br />
• going up and down slopes or hills in your walk. If possible walk uphill on the way<br />
out and downhill on the way home. If you live in a hilly area, it is best if you are<br />
taken by car to a flat park with level ground, for the first few weeks.<br />
It is very important to gradually build up the pace during the first few minutes of the walk,<br />
(warming up), to ensure your body and particularly your heart has a chance to adapt to the<br />
increase in physical activity. Likewise, it is important to gradually slow down your pace during<br />
the last part of your walk rather than suddenly stopping when you reach home.<br />
You should aim to go walking at least five times a week, gradually building up to a brisk pace<br />
for at least 30 minutes. If you find it difficult to fit in a 30 minute continuous walk, then try<br />
doing three walks of 10 minutes during the day.<br />
If you have not been used to walking regularly before your operation or suffer from other<br />
restricting conditions, the above programme may be too strenuous for you. Your cardiac<br />
rehabilitation physiotherapist will discuss your specific needs. If you are used to regular<br />
waling or other types of exercise you may find you progress more quickly than suggested.<br />
29
Perceived exertion scale<br />
When carrying out physical activity, the scale below can be used to help ensure you are working<br />
at the correct level of intensity of effort. The perception depends mainly on the strain and fatigue in<br />
your muscles and on your feeling of breathlessness or aches in the chest. This scale will be<br />
explained in more detail when you attend your cardiac rehabilitation programme.<br />
The correct guidelines are given below:<br />
No. Intensity of effort experienced Perception of how strenuous the activity feels to you<br />
0 Nothing at all No exertion at all<br />
0.5 Extremely weak Just noticeable<br />
1 Very weak No problem<br />
2 Weak Light/very easy to continue<br />
3 Moderate Comfortable to continue<br />
4 <strong>Beginning</strong> to feel puffed<br />
5 Strong Heavy/feeling a bit puffed<br />
6 Feeling puffed<br />
7 Very strong Tiring/You have to push yourself to continue<br />
8 Very tiring<br />
9 Out of breath/shattered<br />
10 Extremely strong Maximum - think of the hardest thing you have ever done<br />
and you could only sustain for 1 - 2 minutes<br />
When you first leave hospital, only carry out activities which are very easy (i.e. up to 2 on the<br />
above scale) for you to continue. Once you start the exercises in the cardiac rehabilitation<br />
programme the intensity will be increased gradually to a more moderate level (i.e. 3 - 4) as appropriate<br />
for you as an individual. It is not advisable ever to push yourself to continue activity<br />
where you feel very tired and out of breath (i.e. 7 -10 ).<br />
Never continue to carry on with physical activity if you have any of the following symptoms:<br />
• chest discomfort or pain<br />
• dizziness<br />
• nausea<br />
• excessive shortness of breath<br />
• palpitations<br />
• muscle cramps<br />
• extreme or unusual fatigue.<br />
Walking<br />
Regular walking is recommended as the main physical activity to regain or improve fitness during<br />
the initial weeks before you start the exercise sessions in the cardiac rehabilitation programme. It<br />
is also a good choice of exercise to help maintain your fitness in the future.<br />
At first, try to walk with a relative or friend at a steady pace on the flat. This will help with your<br />
confidence and is also more fun. You should feel warm and be breathing slightly heavier than<br />
normal.<br />
28<br />
Relaxation<br />
It is important that you spend time relaxing after your operation. Relaxation benefits the heart as<br />
it can help to lower your blood pressure, heart rate and possibly your cholesterol. Relaxation can<br />
be learnt by anyone and with practice you should be able to relax almost anywhere.<br />
Five minute relaxation<br />
• Find a quiet room and make sure you are warm.<br />
• Wear loose clothing and remove any spectacles.<br />
• You may relax either lying down or sitting in a chair.<br />
• If you are sitting make sure your head, thighs and back are well supported (use a<br />
cushion in the small of the back if it helps).<br />
• Place your hands on your lap.<br />
• Close your eyes. If you are uncomfortable with your eyes closed, keep your eyes<br />
focused on one point ahead of you throughout the session.<br />
Spend a short time each day practising the following technique. If possible ask someone<br />
to read out the below instructions.<br />
Begin by breathing out:<br />
Then breathe in steadily, just as much as you need.<br />
Now breathe out slowly, with a slight sigh, like a balloon slowly deflating.<br />
Do this once more, slowly breathing in….breathe out sigh….as you breathe out feel the tension<br />
begin to drain away. Then go back to your ordinary breathing, even, quiet, and steady.<br />
Now direct your thoughts to each part of your body in turn, to the muscles and joints. Think first<br />
about your left foot. Your toes are still. Your foot feels heavy on the floor. Let your foot and toes<br />
start to feel completely relaxed.<br />
Now think about your right foot….toes….ankle….they are resting heavily on the floor. Let both<br />
your feet, your toes and ankle start to relax.<br />
Now think about your legs. Let your legs feel completely relaxed and heavy on the chair or floor.<br />
Your thighs and your knees roll outwards when they relax, so let them go.<br />
Think now about your back. Let your back relax into the chair and let the tension drain away from<br />
your back. Follow your breathing, and each time you breathe out, relax your back and spine a<br />
little more.<br />
Now to your abdominal muscles. Let them become soft and loose. There is no need to hold your<br />
stomach in tight, it rises and falls as you breathe quietly. Feel that your stomach is completely<br />
relaxed.<br />
Without tension in your chest, let your breathing be slow and easy, and each time you breathe<br />
out, let go a little more.<br />
Think now about the fingers of your left hand – are they curved, limp and quite still?<br />
Now think about the fingers of your right hand – are they relaxed, soft and still?<br />
Let this feeling of relaxation spread up your arms….feel the heaviness in your arms – up to your<br />
shoulders. Let your shoulders relax, let them drop easily….and then let them drop even further<br />
than you thought they could.<br />
25
Think about your neck. Feel the tension melt away from your neck and shoulders. Each time you<br />
breathe out, relax your neck a little more.<br />
Now before you move on, just check to see if all these parts of your body are still relaxed - your<br />
feet, legs, back, tummy, hands, arms, neck and shoulders. Keep your breathing gentle and easy.<br />
Every time you breathe out relax a little more and let all the tensions ease away from your body.<br />
No tensions - just enjoy this feeling of relaxation.<br />
Now think about your face. Let your whole face relax. Smooth out your brow and let your<br />
forehead feel wide and relaxed. Let your eyebrows drop gently. There’s no tension round your<br />
eyes - your eyes are still. Let your jaw relax with your teeth slightly apart.<br />
Feel the relief of letting go of any tension.<br />
Now think about your tongue and throat. Let your tongue drop down to the bottom of your mouth<br />
and relax completely. Relax your tongue and throat and your lips…. lips lightly together, no<br />
pressure between them.<br />
Let all the muscles in your face relax so there is no tension in your face, just let it relax more and<br />
more.<br />
Now, instead of thinking about yourself in parts, feel the all over sensation of letting go, think of<br />
quiet and of rest. Check to see if you are still relaxed. Clear your mind of thoughts by<br />
concentrating on this relaxed sensation, as this time is for relaxing not thinking. Stay like this for<br />
a few moments, and listen to your breathing….in….and out…. Let your body become looser<br />
and heavier each time you breathe out.<br />
Now continue for a little longer, and enjoy this time for relaxation.<br />
Coming back - slowly, wiggle your hands a little, and your feet. When you are ready, open your<br />
eyes and sit quietly for a while, stretch, if you want to, or yawn, and slowly start to move again.<br />
The heart is a muscle, and like any other muscle, it needs physical activity to stay healthy.<br />
Regular physical activity will improve the blood flow to the heart muscle and will help your heart<br />
to become stronger and more efficient. The type of exercise that is most beneficial for your heart<br />
is called aerobic or cardiovascular activity. This is any repetitive, rhythmic activity, involving the<br />
large muscle groups in your body such as the legs, shoulders and arms. Examples of aerobic<br />
activity include walking, cycling and dancing. This type of activity increases the body’s demand<br />
for oxygen and adds to the workload of the heart and lungs. This makes the heart and circulation<br />
more efficient, and helps to develop your stamina.<br />
You should aim for 30 minutes a day of moderate activity, such as brisk walking. It is better to<br />
take regular exercise, rather than isolated sessions. With any activity it is important to begin<br />
slowly and to build up gradually.<br />
Other activities are good for improving flexibility and mobility. Keeping your body supple and<br />
flexible will help you keep a full range of movement and stay independent as you get older.<br />
Examples are gardening and yoga.<br />
Strengthen your muscles and bones with strength-type activities. These will help give you good<br />
balance, good posture and bone strength. Examples are climbing the stairs and digging the<br />
garden.<br />
Normal response to exercise:<br />
• faster and stronger heart beat (pulse rate)<br />
• slight breathlessness<br />
• slight sweating<br />
• slight muscle ache approximately 36 hours after exercising<br />
• start to get warm and flushed.<br />
If you have any questions about the above, or would like details of where to obtain relaxation<br />
CDs, please contact the cardiac rehabilitation team on 0161 291 2177.<br />
Physical activity<br />
The convenience of modern life is making us increasingly inactive and this is proving hazardous<br />
to our health. Inactive people have twice the risk of developing coronary heart disease compared<br />
with active people. Inactivity increases the risk of coronary heart disease as much as smoking<br />
does.<br />
Physical activity:<br />
• halves the risk of developing coronary heart disease<br />
• reduces the risk of having a stroke<br />
• lowers blood pressure<br />
• reduces the chance of developing diabetes and helps control diabetes<br />
• helps you to lose weight<br />
• relieves stress<br />
• makes you feel more energetic<br />
• improves your blood cholesterol levels.<br />
26<br />
27