NETWORK - Ubhonline.com
NETWORK - Ubhonline.com
NETWORK - Ubhonline.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
SPRING 2003<br />
Level of Care Guidelines and<br />
Care Authorization Decisions<br />
USBHPC psychologists and psychiatrists make authorization and denial decisions<br />
on the basis of the member’s clinical information and the USBHPC Level of Care<br />
(LOC) Guidelines. The LOC Guidelines have been developed to produce optimal<br />
clinical out<strong>com</strong>es and consistency in the authorization process. To assist with<br />
the finalization of these guidelines, input was obtained from providers representing<br />
all disciplines and from a wide geographic distribution.<br />
Level of Care authorization decisions require agreement between the provider and<br />
USBHPC regarding the appropriateness of the proposed treatment plan. Our care<br />
management process offers every practitioner the opportunity to discuss a medical<br />
necessity denial with an appropriate peer reviewer at USBHPC during the<br />
authorization process before a final denial determination is made. Then, if a denial<br />
determination has been made, you have the opportunity to appeal the decision<br />
by following our Appeal process outlined in the USBHPC Provider Manual.<br />
Both the USBHPC Level of Care Guidelines and the USBHPC Provider Manual can<br />
be found on the USBHPC website, www.ubhonline.<strong>com</strong> or may be obtained<br />
through the mail by calling Provider Services at 1-800-798-3053, ext. 2058.<br />
USBHPC does not <strong>com</strong>pensate employees, appeal reviewers or providers for<br />
denials of coverage or service. There are no financial incentives for utilization<br />
management decision-makers to encourage denial of benefits.<br />
PRESORTED<br />
STANDARD CLASS<br />
U.S. POSTAGE<br />
PAID<br />
SAN LEANDRO CA<br />
PERMIT NO. 311<br />
Preventive Health<br />
Programs<br />
In 2003, USBHPC will be working on some<br />
behavioral health preventive health programs.<br />
We will be looking to the provider <strong>com</strong>munity<br />
for input and advice regarding these programs,<br />
so if you have information or ideas that might be<br />
useful, please contact our Senior Director of<br />
Network Management, Kimberly Davis, at<br />
1-800-798-3053, ext. 6605.<br />
Providers are responsible for discussing<br />
treatment options with patients. However, not<br />
all options will necessarily be covered benefits.<br />
Therefore, please verify the member's eligibility<br />
through the USBHPC Intake Department before<br />
indicating to the member that the services are<br />
covered benefits.<br />
The Intake Department can be reached at<br />
1-800-798-3053, ext. 6920.<br />
CM325E:00<br />
<strong>NETWORK</strong>notes<br />
new Spring edition!!<br />
in this<br />
issue<br />
<br />
<br />
<br />
<br />
<br />
U.S. BEHAVIORAL HEALTH PLAN CA<br />
Billing Issues<br />
Access<br />
Standards<br />
Provider<br />
Satisfaction<br />
Survey<br />
SM<br />
Lifepath<br />
Advisors Program<br />
Communicating<br />
with PCP’s<br />
HIPAA<br />
The Health Insurance Portability and<br />
Accountability Act of 1996 ("HIPAA") became<br />
a reality for the health care industry on April 14,<br />
2003. HIPAA is a federal law enacted to ensure<br />
privacy and security of a consumer’s Protected<br />
Health Information ("PHI"). PHI is basically<br />
defined as individually identifiable health<br />
information that is transmitted by or maintained<br />
in any form or medium. A few examples of PHI<br />
include an individual’s name, social security<br />
number or member identification number,<br />
address, and date of birth. HIPAA is changing<br />
the way that health care plans conduct business<br />
with their membership, providers, partners and<br />
contractors.<br />
U.S. Behavioral Health Plan, California<br />
("USBHPC") has been working diligently for over<br />
a year to ensure all aspects of our operations<br />
are <strong>com</strong>pliant with the required HIPAA privacy<br />
practices by April 14, 2003. USBHPC would<br />
like to take this opportunity to share with you<br />
some important aspects of our privacy practices<br />
under HIPAA.<br />
Uses and Disclosures of PHI — USBHPC has<br />
established policies relating to requests for and<br />
disclosure of PHI in accordance with HIPAA<br />
and other applicable federal and state laws.<br />
These policies ensure that only the minimum<br />
amount of information necessary is exchanged<br />
to ac<strong>com</strong>plish the purpose of the disclosure<br />
or request.<br />
Use of Release of Information — It is USBHPC<br />
policy to release PHI about Individuals only to<br />
the Individual themselves or to other parties<br />
designated in writing by the Individual, unless<br />
otherwise required or allowed by law. For each<br />
party that the Individual designates to access<br />
their PHI, he or she must sign and date a Release<br />
of Information specifying what information may<br />
be disclosed, to whom, and during what period<br />
of time. This policy is not applicable to PHI<br />
being exchanged with a USBHPC provider or<br />
other entity designated by HIPAA for the<br />
purposes of Treatment, Payment, or Health<br />
Care Operations. 1<br />
Identification and Authentication — USBHPC<br />
requires that anyone requesting access to PHI<br />
be appropriately identified and authenticated.<br />
Members and personal representatives are<br />
required to provide the member identification<br />
number or subscriber number and the member<br />
or subscriber date of birth in the regular<br />
identification and authentication process.<br />
Providers or provider’s staff are identified and<br />
authenticated by giving the provider’s federal<br />
tax identification number or physical address.<br />
This information will be required for each and<br />
every request for access or disclosure of PHI<br />
Internal Protection of Oral, Written, and<br />
Electronic PHI — USBHPC works with<br />
UnitedHealth Group, USBHPC’s grandparent<br />
organization, to ensure that all physical and<br />
logical safeguards are in place to protect against<br />
the unauthorized use, disclosure, modification<br />
and destruction of PHI across all media.<br />
All employees of USBHPC receive training<br />
and are familiar with the HIPAA privacy practices<br />
relevant to their job duties and responsibilities.<br />
www.ubhonline.<strong>com</strong><br />
continued
USBHPC Preferred<br />
Practice Guidelines<br />
USBHPC’s Preferred Practice Guidelines are treatment protocols<br />
for specific clinical conditions. These guidelines are developed<br />
by USBHPC on the basis of extensive literature review, scientific<br />
evidence and expert consensus. The guidelines are intended<br />
for Care Management staff and network providers to consider<br />
during the treatment review process. While they identify and<br />
describe generally re<strong>com</strong>mended courses of intervention, they<br />
are not intended to be a substitute for professional judgment<br />
during the review of an individual patient's treatment and<br />
situation. They simply provide you with supplemental clinical<br />
information to support your own treatment practices.<br />
USBHPC’s Preferred Practice Guidelines are available on our<br />
website, www.ubhonline.<strong>com</strong>. If you would like to request a<br />
copy by mail, please contact us at 1-800-798-3053.<br />
Availability Standards<br />
USBHPC is <strong>com</strong>mitted to ensuring that its members have the availability of behavioral health care providers to meet their mental health and<br />
substance abuse needs. USBHPC has established standards for the numbers and types of providers, as well as for their geographic distribution.<br />
The following standards are monitored semi-annually:<br />
Provider Type Standard Goal 2002 Results<br />
Physician Estimated 30 Miles 95% 93.9%<br />
Doctoral-Level Psychologist Estimated 30 Miles 95% 99.0%<br />
Masters-Level Clinician Estimated 30 Miles 95% 99.5%<br />
Practitioner without Regard to Licensure Type Estimated 30 Miles 95% 99.6%<br />
Behavioral Health Care Facilities and Programs Estimated 60 Miles 85% 96.9%<br />
USBHPC collects and analyzes this data to ensure performance against these standards and implements interventions to improve performance<br />
when barriers are identified. During 2003, USBHPC will be working on focused recruiting efforts in specific geographic areas to<br />
ensure that we are providing the number and types of providers that our members need to ensure high quality care.<br />
Access Standards<br />
USBHPC wants to ensure that members have access to appropriate treatment as needed and, therefore, adheres to NCQA standards for<br />
member accessibility to services. These standards require our network of physicians and other health care providers to see members within<br />
the following time limits:<br />
• Emergency — immediate access<br />
• Non-life threatening emergency — within 6 hours<br />
• Urgent — within 48 hours<br />
• Routine — within 10 business days<br />
Annually USBHPC collects and analyzes data to measure performance against these standards and implements interventions to improve<br />
performance when barriers are identified. For 2002, USBHPC reports the following results:<br />
Appointment Type<br />
Emergency<br />
Non-Life threatening Emergency<br />
Urgent<br />
Routine<br />
2002 Appointment Access Results<br />
100% immediate access<br />
100% access within 6 hours<br />
83% access within 48 hours<br />
90% kept within 10 business days for<br />
PhDs and Master’s Level Clinicians*<br />
*Access for MDs is measured on an annual basis and 2002 results showed that only 75% of appointments were kept within 10 business days.<br />
During 2003, USBHPC will continue to identify opportunities to improve our performance for urgent and routine appointments. Some of<br />
these activities include educating providers regarding the access standards and recruitment of MDs in geographic areas that have been<br />
identified as problematic.<br />
In addition, the current access standards require you to return member calls within 24 hours. If you are unable to accept new patients into your<br />
practice at this time, please contact our Provider Services Line at 1-800-798-3053, ext. 2058 so that we may temporarily suspend new referrals.<br />
Provider Satisfaction<br />
Survey<br />
The 2001 Provider Satisfaction Survey for California providers<br />
was <strong>com</strong>pleted in August of 2002. 519 USBHPC providers<br />
were surveyed with a response rate of 36%. This survey was<br />
developed to assess our providers’ level of satisfaction with<br />
various aspects of USBHPC’s operation.<br />
There was a dramatic decrease in satisfaction in responses to<br />
the 2001 survey <strong>com</strong>pared to 2000. Intake, Care Management,<br />
Provider Services and Claims departments all showed a<br />
decrease in the level of provider satisfaction with "overall<br />
satisfaction" dropping from 87% in 2000 to 80% in 2001.<br />
After analyzing the survey results, USBHPC has been able to<br />
identify many opportunities for improvement. We are<br />
enhancing our initial and on-going staff training programs<br />
and developing new and improved technological systems<br />
that will make it easier for providers to obtain authorizations<br />
and will improve our claims processes. Many other initiatives<br />
are also underway, including improved <strong>com</strong>munication with<br />
our providers via this newsletter, mailings, the provider<br />
website, www.ubhonline.<strong>com</strong>, and a planned revision of<br />
the Provider Manual.<br />
USBHPC would like to thank all providers who participated in<br />
the survey. This feedback is an invaluable tool in finding ways<br />
to improve service to our network providers.<br />
www.ubhonline.<strong>com</strong><br />
<strong>NETWORK</strong>notes
continued<br />
Disclosure to Plan Sponsors or Employers —<br />
Summary health information is released to a Plan<br />
Sponsor 2 without the authorization of the affected<br />
Individual, as long as the Plan Sponsor needs the<br />
information for the purpose of obtaining premium bids<br />
or modifying, amending, or terminating the Group Health<br />
Plan; or for providing access to employees of an employer<br />
or Plan Sponsor to carry out administrative duties of<br />
a Health Plan related to Treatment, Payment or Health<br />
Care Operations.<br />
USBHPC subscribers and/or members will receive Privacy<br />
Notices outlining the uses and disclosures of their PHI<br />
and their rights under HIPAA, as well as the legal duties<br />
of their health plan to ensure protection of their PHI<br />
under HIPAA. A copy of the USBHPC Privacy Notice<br />
will be posted on the UBH provider website<br />
www.ubhonline.<strong>com</strong> and will also be available in hard<br />
copy by contacting the USBHPC Provider Line toll free at<br />
1-800-798-3053, ext. 2058. For access to the <strong>com</strong>plete<br />
text of the HIPAA rules and regulations, please visit the<br />
U.S. Department of Health and Human Services ("HHS")<br />
website www.hhs.gov/ocr/hipaa/ or contact HHS Privacy<br />
Hotline toll free at 1-866-627-7748.<br />
1 ”Treatment, Payment, or Health Care Operations” as defined by HIPAA include:<br />
1) Treatment – Coordination or management of health care and related services;<br />
2) Payment purposes – The activities of a health plan to obtain premiums or fulfill<br />
responsibility for coverage and provision of benefits under the health plan; and<br />
3) Health Care Operations – The activities of a health plan such as quality review,<br />
business management, customer service, and claims processing<br />
2 "Plan Sponsor" as defined in ERISA, means the employer in the case of a Group Health<br />
Plan maintained by a single employer, the employee organization in the case of a plan<br />
maintained by such organization, or the <strong>com</strong>mittee or similar group or representatives<br />
in the case of a plan maintained by two or more employers jointly by one or more<br />
employers and employee organizations.<br />
www.ubhonline.<strong>com</strong><br />
Billing Issues<br />
U.S. Behavioral Health Plan, CA is aware that, on occasion,<br />
you may experience difficulties with billing issues related<br />
to services rendered to USBHPC members. We encourage<br />
you to contact us at the toll-free number listed on the<br />
back of the member’s identification card if you have<br />
questions regarding a member’s benefits.<br />
Our members report that billing issues may occur when<br />
a provider charges up front for the entire cost of services<br />
rendered instead of the co-pay/deductible, as outlined in<br />
the member’s benefit contract, or if services are rendered<br />
without the required pre-certification.<br />
Please remember that requesting payment beyond a<br />
member’s co-pay, applicable coinsurance and/or deductible<br />
is not allowed and is in breach of your agreement with<br />
USBHPC. To obtain more information related to billing/<br />
claims guidelines, log on to the USBHPC provider website,<br />
www.ubhonline.<strong>com</strong> or contact us at 1-800-798-3053.<br />
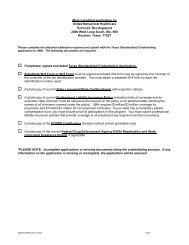
Demographic Changes<br />
In order to ensure ongoing participating status and minimize<br />
problems with claims submission and payment, you must<br />
contact USBHPC Provider Services for demographic<br />
changes, practice changes, or when utilizing a different<br />
tax ID number. Failure to provide timely notification of<br />
these changes may negatively impact claims processing<br />
and can even lead to termination. Please do not put a<br />
new address or tax ID on a claim form. Claim information<br />
is <strong>com</strong>pared to the provider database and, if the information<br />
does not match, the claim cannot be processed.<br />
It is also necessary to notify USBHPC to change your status<br />
to unavailable if you are temporarily unable to accept<br />
referrals (e.g. vacation, illness, lack of available appointments).<br />
Please contact Provider Services at 1-800-798-3053,<br />
ext. 2058 or send notification to:<br />
United Behavioral Health<br />
Provider Database Specialists<br />
P. O. Box 1459<br />
Mail Route MN010-S155<br />
Minneapolis, MN 55440-1459<br />
Address and contact changes may also be requested<br />
online if you are a registered user of ubhonline, our<br />
Provider Services’ website (www.ubhonline.<strong>com</strong>). To<br />
register and obtain an ID and password for ubhonline,<br />
call 1- 866-209-9320.<br />
Communication<br />
with PCPs<br />
It is very important that behavioral health clinicians<br />
<strong>com</strong>municate with their patients’ PCPs. Please help your<br />
patients get the optimum care they deserve by sending their<br />
PCPs a brief update on diagnosis, status, prognosis, and most<br />
importantly, psychotropic medications the patient has been<br />
prescribed. It is not necessary to do this every time you see<br />
the patient, but routine updates can mean a big difference<br />
in the health out<strong>com</strong>e of the patient.<br />
Members Identify<br />
Education as a Primary<br />
Consideration<br />
Each year, USBHPC surveys its membership for satisfaction<br />
with its operations. The results of each year’s survey are<br />
<strong>com</strong>pared to the previous year’s to identify significant changes<br />
in satisfaction for those services surveyed. We are happy to<br />
report that the latest Member Satisfaction Survey showed a<br />
significant improvement in the overall satisfaction score when<br />
<strong>com</strong>pared to the prior year’s survey. Specifically, the overall<br />
satisfaction score was 89% for the 2002 survey on services<br />
rendered in the last quarter of 2001 <strong>com</strong>pared to 82% for the<br />
2001 survey on services rendered in the last quarter of 2000.<br />
This was noted to exceed our goal of 83% overall satisfaction<br />
by a statistically significant margin.<br />
Despite this notable success, the Member Satisfaction Survey<br />
also demonstrated that members were relatively dissatisfied<br />
with the information received about medications being<br />
prescribed. It was specifically noted that satisfaction dropped<br />
from 87% in 2000 to 70% in 2001. USBHPC revealed these<br />
results, for purposes of discussion, at the December 5, 2002<br />
USBHPC Clinical Advisory Board meeting. The Clinical<br />
Advisory Board re<strong>com</strong>mended that providers utilize any and<br />
all appropriate and accurate sources of information available<br />
regarding medication education, including that information<br />
provided by USBHPC.<br />
For psychiatrists, the use of medications in the management<br />
of the major mental disorders is considered to be a primary<br />
intervention in the treatment of these disorders. Success<br />
in the treatment of these major mental disorders is significantly<br />
determined by <strong>com</strong>pliance with medication regimen.<br />
Compliance with taking prescribed medication is certainly<br />
influenced by the quality of the collaboration between the<br />
prescribing physician and the patient. Medication education<br />
is a central part of achieving success in the medication<br />
management of the major mental disorders. There is no<br />
question that the use of printed material in support of<br />
medication education further reinforces what has been<br />
discussed during the course of appointments.<br />
USBHPC is in the process of assessing ways in which it can<br />
further support its provider network in the effort to educate<br />
the membership about prescribed medications. One approach<br />
will be the availability of "tip sheets" for behavioral health<br />
clinicians. These "tip sheets" describe various classes of<br />
psychotropic drugs and their actions and side effects, etc.<br />
and are meant to be given to patients. These same "tip sheets"<br />
were offered to PCPs in 2002 with great success. Other<br />
approaches may include information posted on web sites and<br />
in member newsletters.<br />
Please take the time to educate and collaborate with<br />
your patients regarding the use of medications.<br />
Quality Improvement/<br />
Utilization Management<br />
Programs<br />
As a contracted provider, you have the right to request<br />
information at any time regarding USBHPC’s Quality<br />
Improvement and Utilization Management Programs.<br />
Here are just a few things that were done in 2002 to<br />
improve our internal processes and to improve patient care:<br />
• Routine phone and/or letter follow-up with every patient<br />
being discharged from an acute care psychiatric facility to<br />
check on availability of timely outpatient appointments<br />
and general well being of the patient. As a result, the<br />
number of patients who keep an outpatient appointment<br />
within seven and thirty days following discharge has<br />
steadily risen throughout the year. We are close to the<br />
80% mark for the thirty-day follow-up.<br />
• Identification and stratification of Blue Shield patients<br />
with a co-morbid Axis III condition who are being<br />
treated in an inpatient psychiatric setting. This has<br />
resulted in being able to identify those patients who have<br />
serious medical conditions as well as serious mental<br />
health conditions, and co-manage them with Blue Shield<br />
of California medical case managers.<br />
• Successful recruitment efforts have grown our total provider<br />
network by 5.7% over 2001, and our psychiatrist network<br />
has grown by 12%.<br />
For more information about our Quality Improvement or<br />
Utilization Management programs, please contact us at<br />
1-800-798-3053.<br />
<strong>NETWORK</strong>notes
SM<br />
Lifepath Advisers Program<br />
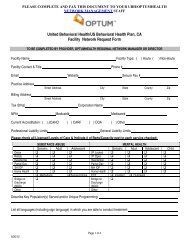
Blue Shield of California (BSC) recently launched a new program of services called Lifepath Advisers (LPA). BSC members who have their<br />
mental health and substance abuse benefits managed by U.S. Behavioral Health Plan, California (USBHPC) will be eligible for LPA.<br />
This new benefit is an assessment and referral service, similar to an EAP benefit, integrated with work-life and nurse line services. It is<br />
delivered through a single toll free number, 1-866-Lifepath (1-866-543-3728), 24 hours a day, 7 days a week. Members can also register<br />
with mylifepath.<strong>com</strong> to access information about the program, request a phone consultation online, and find additional resources.<br />
The Work/Life service through LPA offers resource specialists who can assist members with <strong>com</strong>plex issues regarding aging, chronic illness,<br />
child development and parenting concerns. The resource counselors can also help members find local resources for child and elder care,<br />
legal or financial needs.<br />
Lifepath Advisers nurse advice line provides 24 hour phone access to registered nurses. BSC members can call this line for answers to<br />
medical questions and for help in deciding how to handle minor illnesses, injuries or other health care issues.<br />
BSC refers to the EAP portion of LPA as a “Personal Consultation” benefit in their <strong>com</strong>munication materials. BSC is not marketing this service<br />
as an EAP benefit. Members may have up to three face-to-face assessment visits, using a network provider, when clinically appropriate.<br />
When a BSC member receives authorization over the telephone for the 3 face-to-face visits, an authorization letter, along with the appropriate<br />
EAP claim form, is mailed to provider. Providers with questions regarding an authorization may contact an EAP counselor at 866-543-3728.<br />
SM<br />
Treatment Record Documentation<br />
Appropriate and thorough documentation of a patient’s clinical history, presenting symptoms and treatment interventions are key to ensuring<br />
appropriate patient management and continuity of care. We have developed treatment record documentation and maintenance standards,<br />
outlined in the USBHPC Provider Manual. We expect that our panel providers and facilities will maintain their treatment records in accordance<br />
with these standards. We would also like you to maintain an organized treatment record keeping system, as well as procedures for the<br />
availability of patient records, appropriate to your practice site. Treatment records must be stored in a secure area and your practice site must<br />
have an established procedure to maintain the confidentiality of treatment records in accordance with any applicable statutes and regulations.<br />
USBHPC may review your records during a scheduled site audit. A site audit can occur for a number of reasons including: pre-credentialing<br />
visits of potential high volume providers, reviews of facilities without national accreditation, and audits concerning quality of care issues<br />
brought to USBHPC’s attention. The audits focus on the <strong>com</strong>pleteness and quality of documentation within treatment records. USBHPC<br />
has established a performance goal of 85%. For those reviews that don’t meet the performance goal, USBHPC requests a plan for corrective<br />
action and/or a re-audit within six (6) months.<br />
You can find the USBHPC Provider Manual containing the documentation requirements, conveniently located on the USBHPC Internet site,<br />
www.ubhonline.<strong>com</strong>. You may also request that a copy be sent to you by contacting Provider Services at 1-800-798-3053, ext. 2058.<br />
Online EAP claims submission for Lifepath Advisers office visits is available via our provider Internet site, ubhonline (www.ubhonline.<strong>com</strong>).<br />
Online EAP claims submission speeds up turn-around time and ensures greater accuracy. This website allows you to verify the status of an<br />
EAP claim, and enables you to view and submit changes to your physical and billing addresses. All EAP claims for Lifepath Advisers<br />
visits not submitted online should be submitted, on the EAP claim form to:<br />
United Behavioral Health<br />
P.O. Box 744925<br />
Houston, Texas 77274-4925<br />
1-800-333-8724 (for EAP claims questions)<br />
If the BSC member requests or requires services that are covered under their Mental Health/Substance Abuse (MH/SA) benefits,<br />
the Lifepath Advisor would refer the member to USBHPC for benefit information and appropriate authorization of services.<br />
For members who have received services covered by their MH/SA benefits through USBHPC, claims should be submitted to:<br />
USBHPC Claims<br />
P.O. Box 880639<br />
San Diego, CA 92168<br />
877-263-9952<br />
Members wanting additional information regarding the Lifepath Advisers program should be directed to call 1-866-Lifepath (1-866-543-3728).<br />
ubhonline.<strong>com</strong> – A Hit with Providers<br />
United Behavioral Health’s provider web site, www.ubhonline.<strong>com</strong>, also serves U.S. Behavioral Health Plan, California (USBHPC) providers.<br />
ubhonline is helping providers to manage their patients and their practices. Many of you are logging on to ubhonline to submit<br />
behavioral health and EAP claims, check on service authorizations, and review claims status. Since the new ubhonline was launched<br />
in April 2002, the growth of transactions performed at the site has been tremendous.<br />
• Over 21,000 confidential transactions came through ubhonline in October 2002.<br />
• User logons have increased nearly 600% since year-end, 2001.<br />
• First pass adjudication rates for claims submitted online exceeds 90%.<br />
If you haven’t had a chance to try ubhonline, logon today and see what you’ve been missing. In addition to claims information,<br />
you can find –<br />
• Network management contact information,<br />
• Level of Care Guidelines<br />
• Preferred Practice Guidelines<br />
• Provider Manual<br />
• Patient Education and more.<br />
Our ubhonline Support Center is available at 1-866-209-9320 from 8:00 AM to 8:00 PM Eastern Standard Time to help you with any<br />
questions or to request a user ID.<br />
www.ubhonline.<strong>com</strong><br />
<strong>NETWORK</strong>notes