Nursing Update 2007 - 2008 - Yale-New Haven Hospital
Nursing Update 2007 - 2008 - Yale-New Haven Hospital
Nursing Update 2007 - 2008 - Yale-New Haven Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
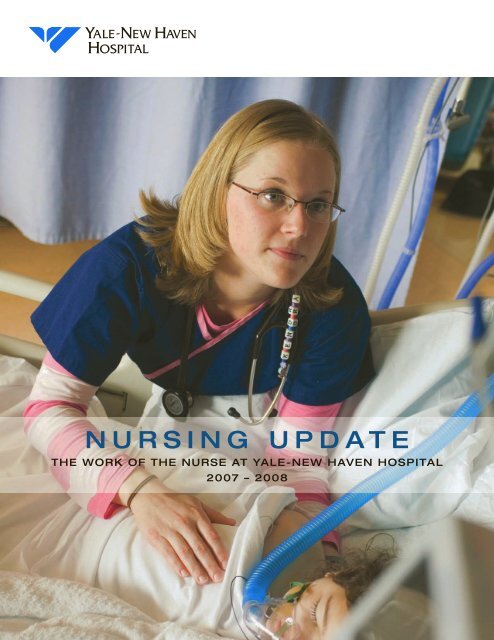
N U R S I N G U P D A T E<br />
THE WORK OF THE NURSE AT YALE-NEW HAVEN HOSPITAL<br />
<strong>2007</strong> – <strong>2008</strong>
conTEnTs<br />
1 leadership …2<br />
2 Evidence-based practice …6<br />
3 innovation …8<br />
4 community outreach …10<br />
5 research …12<br />
6 growth and development …14<br />
7 recognition …16<br />
Editorial Board: Sue Fitzsimons, R.N., Cathy Stevens, R.N.<br />
Editor: Leah Colihan<br />
Photography: Leah Colihan, Terry Dagradi, Jerry Domian, Ray Paige<br />
Writers: Leah Colihan, Katie Fischer, Kathy Katella<br />
Contributor: Bev DeCato<br />
Design: Jeanne Criscola | Criscola Design<br />
<strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> is an EEO/AAP employer<br />
© Spring <strong>2008</strong><br />
www.ynhh.org<br />
<strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong><br />
20 York Street<br />
<strong>New</strong> <strong>Haven</strong>, CT 06510-3202<br />
Recruitment and Staffing: (203) 688-5083
MAY <strong>2008</strong><br />
Dear Colleagues and Friends of <strong>Nursing</strong>:<br />
<strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> has a long tradition of nursing excellence and<br />
innovation. Our nursing model – founded on the principles espoused by<br />
Florence Nightingale and Virginia Henderson – provides the basis of this<br />
blend of caring and commitment to patient safety.<br />
Each day there is evidence that you – our nurses – find ways to make these<br />
concepts real. You do this through a commitment to research, a dedicated<br />
search for best practices and an appreciation for how innovation can help<br />
you deliver better, safer care to the almost 52,000 inpatients you cared for<br />
last year. You also delivered care to a record 536,500 outpatients.<br />
In this first <strong>Nursing</strong> <strong>Update</strong>, you will read about initiatives to improve<br />
how we care for our patients – from hourly rounding through the use<br />
of evidence to guide practice to the important work of the rapid<br />
response teams.<br />
Your work with patients and families is purposeful and aimed to achieve<br />
safe, efficient, effective and equitable care. It is my privilege to share just<br />
a few stories of your remarkable accomplishments with you and others<br />
interested in the work of the nurse at <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong>.<br />
I hope we convey our excitement as we continue to institute the changes<br />
that promote and elevate nursing practice in our fine institution.<br />
Sincerely,<br />
Sue Fitzsimons, R.N., Ph.D.<br />
Senior Vice President<br />
Patient Services
1<br />
Leadership<br />
Leadership is key to the success of any organization. In an academic medical center<br />
like <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong>, strong, confident nurse leaders impact the excellence of<br />
staff and the quality and safety of patient care. Nurses at all stages of their professional<br />
careers increasingly find opportunities to shape the future of nursing. The hospital’s<br />
embrace of collaborative governance will continue to ensure its reputation as a<br />
national employer of choice and a provider of choice for patients who choose YNHH<br />
for their care.<br />
2 N U R S I N G U P D A T E
Nurses create<br />
collaborative governance<br />
After a tradition of top-down nursing management,<br />
YNHH nursing leaders are implementing a<br />
collaborative governance structure in partnership<br />
with the nursing staff.<br />
Over the past year, a new model that will involve<br />
YNHH’s more than 2,000 clinical nurses has been<br />
initiated. This new professional model places<br />
accountability and authority for practice decisions<br />
at the level of the clinical nurse. It creates<br />
a framework that engages clinical nurses in decision-making<br />
and brings leaders organizationally<br />
closer to the nurses they manage.<br />
ABOVE Members of the <strong>Nursing</strong> Cabinet meet regularly and work closely with the Staff Nurse Council. Shown in the first row<br />
(l-r) are: Diane Vorio, R.N., vice president, Patient Services; Sue King, R.N., patient service manager, Critical Intervention Unit;<br />
Bertie Chuong, R.N., director of nursing, Temple Recovery Care Center; Sue Fitzsimons, R.N., Ph.D., senior vice president, Patient<br />
Services; Maribeth Hayes, R.N., coordinator, <strong>Nursing</strong> Performance Management; and Leslie O’Connor, A.P.R.N., administrative<br />
director, Psychiatry Services. In the second row (l-r) are: Francine LoRusso, R.N., director of nursing, Medicine; Stephanie Bilskis,<br />
R.N., practice administrator, Community Health; Catherine Stevens, R.N., director of nursing, Women’s and Infants Services; Cheryl<br />
Hoey, R.N., director of nursing, Pediatrics; Ena Williams, R.N., director of nursing, Perioperative Services; and Tahiry Sanchez, R.N.,<br />
director of nursing, Oncology. Missing from photo are: Mariane Carna, R.N., executive director, Heart and Vascular Center; Carol<br />
Just, R.N., director of nursing, Surgery; and Patricia Span, R.N., director, Professional Practice, Research and Education.<br />
<strong>Nursing</strong> Cabinet<br />
and Staff Nurse Council<br />
Evolving from “Striving for Excellence,” the<br />
first step in this model was the establishment<br />
of the <strong>Nursing</strong> Cabinet, whose membership<br />
includes all nursing directors within the<br />
YNHH network.<br />
The second phase was building the 14-member<br />
Staff Nurse Council. In the first year, the members<br />
were selected by managers based on criteria<br />
of leadership. In <strong>2008</strong>, nurses will nominate<br />
themselves to serve on this important body and<br />
the Staff Nurse Council will review nominations<br />
and choose their successors.<br />
The Staff Nurse Council is key to collaborative<br />
governance because it assures the nurse at<br />
the bedside a place at the decision-making<br />
table. In the past at <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong>, decisions<br />
were made by managers, policies and procedures<br />
were written by mid-level nurses, and<br />
staff nurses implemented decisions and processes<br />
that did not necessarily reflect their<br />
best thinking.<br />
Now, with a robust and vibrant Staff Nurse<br />
Council fully responsible for representing all<br />
nurses, ideas, questions, solutions and problems<br />
have a place to go – and that’s up. The goal is<br />
increased and productive communication that<br />
will further strengthen the delivery of safe, high<br />
quality care to <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> patients.<br />
Y A L E - N E W H A V E N H O S P I T A L 3
Cluster committees<br />
and standing committees<br />
In anticipation of the questions and issues they<br />
will work through, the <strong>Nursing</strong> Cabinet and the<br />
Staff Nurse Council have developed cluster committees<br />
in 11 areas, which will serve a valuable<br />
and efficient information-sharing function for<br />
groups of units. To date, the clusters represent<br />
pediatrics, medicine, surgery, heart, ambulatory,<br />
psychiatry, ambulatory services, women’s, adult<br />
ED, perioperative services and oncology.<br />
In addition to the <strong>Nursing</strong> Cabinet, Staff Nurse<br />
Council and cluster committees, standing committees<br />
deal with work directed from the Staff<br />
Nurse Council. The four standing committees<br />
are: clinical quality, research, education, and<br />
nurse award and recognition.<br />
Succession planning<br />
Collaborative governance places responsibility<br />
on the staff nurse whose first job is caring for patients.<br />
Active participation in governing provides<br />
significant opportunity for nurses to learn about<br />
the working of a complex medical institution,<br />
gain exposure to nurses outside their area of<br />
practice, and improve or strengthen important<br />
communications skills.<br />
Over time, collaborative governance will give<br />
YNHH staff nurses the involvement they need to<br />
become tomorrow’s nurse leaders.<br />
ABOVE The Staff Nurse Council draws nurses from many practices who provide an important voice for the more than 2,000<br />
nurses who work at <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong>. Seated in the front row (l-r) are: Mary Weir, R.N., Perioperative Services; cochairs<br />
Rick O’Connor, R.N., Surgical Intensive Care Unit, and Nora O’Keefe, R.N., Diagnostic Radiology; and Jane Buglione,<br />
R.N., Pediatric Emergency Department. Standing (l-r) are: Sybil Shapiro, R.N., Temple Recovery; Kelly Baran, R.N., Gyn/<br />
Oncology; Erin Radocchia, R.N., Maternal Special Care; Melanie D’Amato, R.N., School-age/Adolescent; Mary Kelly O’Shea,<br />
R.N., Infants/Toddlers; and Kelly Poskus, R.N., Neuroscience. Missing from photo are: Shelley Harrigan, R.N., Primary Care<br />
Center; Heather Miska, R.N., Children’s Psychiatric Inpatient Service; and Jeramy Tabuzo, R.N., <strong>Hospital</strong> Research Unit.<br />
Collaborative governance is a history-altering<br />
departure for staff nurses at <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong>. The<br />
nurse at the bedside sees what works and what doesn’t,<br />
and we now have a system that examines practice so<br />
patient care is evidence-based.” “— Nora O’Keefe, R.N., Diagnostic Radiology and Staff Nurse Council Co-chair<br />
4 N U R S I N G U P D A T E
Y A L E - N E W H A V E N H O S P I T A L 5
2<br />
Evidence-based<br />
practice<br />
As nursing evolves with advances in knowledge and care protocols, nurses seek out<br />
ways to provide the most informed, thoughtful care for their patients. At YNHH,<br />
evidence-based practice is an increasingly important guide for clinical decision<br />
making. As nurses address each patient’s unique situation, they want to deliver the<br />
best practices based on the latest, most conclusive research.<br />
In <strong>2007</strong>, nurses at YNHH implemented new evidence-based practices in several areas<br />
as they worked to meet the specific needs of diverse patients and families. Their<br />
efforts have contributed to a carefully focused, assured level of nursing care. Three<br />
examples are nurse rounding, rapid response teams and new safety standards.<br />
6 N U R S I N G U P D A T E
Hourly rounding boosts<br />
satisfaction all around<br />
Last summer, YNHH began hourly rounding by<br />
nurses and patient care associates on pediatric<br />
and medical units.<br />
Marcelle Applewhaite, R.N., patient service manager<br />
for the Infants/Toddlers Unit, and Francine<br />
LoRusso, R.N., director of nursing, Medicine,<br />
spearheaded the effort after a presentation last<br />
summer by a nationally known healthcare consulting<br />
company. The Studer Group had studied<br />
hourly rounding in 14 hospitals across the country,<br />
and found the protocol reduced monthly<br />
call button use by 38 percent, patient falls by 50<br />
percent and skin breakdowns by 14 percent. At<br />
the same time, satisfaction scores soared.<br />
Studer Group staff instructed YNHH nurses in<br />
eight key behaviors, including making an initial<br />
introduction to a patient with a description of<br />
role and experience, and documenting each<br />
visit so patients who are sleeping will know the<br />
caregiver has been in the room. Each hour, nurses<br />
also ask their patients about the four P’s: pain,<br />
positioning, placement and personal needs.<br />
Patient satisfaction scores rose at YNHH last<br />
year, and LoRusso and Applewhaite believe the<br />
new hourly rounding initiative contributed.<br />
In fact, early results of hourly rounding are so<br />
promising that the practice is being implemented<br />
hospital-wide this year.<br />
Rapid response teams<br />
keep patients out of ICUs<br />
When a nurse at YNHH notes a trigger sign in<br />
a patient such as a drop in blood pressure or<br />
simply has a hunch that a patient is deteriorating,<br />
she or he may call in a rapid response<br />
team—essentially an “ICU at the bedside.”<br />
The team will arrive in less than ten minutes<br />
to stabilize the patient.<br />
Rapid response teams were among six evidence-based<br />
safety interventions included in<br />
the Institute of Healthcare Improvement<br />
(IHI)’s campaign to prevent 100,000 in-hospital<br />
deaths. In 2004, IHI recognized <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong><br />
Children’s <strong>Hospital</strong> as one of the first pediatric<br />
hospitals in the country to implement a rapid<br />
response team made up of critical care nurses<br />
and physicians. Use of the teams at YNHCH<br />
resulted in a dramatic decrease in cardio-respiratory<br />
arrests outside of the pediatric ICU.<br />
Adult units at YNHH began using rapid response<br />
teams, which consist of critical care nurses,<br />
physicians and respiratory therapists, to provide<br />
urgent and emergent care in 2006.<br />
For both adults and children, the teams have<br />
been so successful in identifying early warning<br />
signs, avoiding the ICU and saving lives that the<br />
hospital is now planning pilot programs that will<br />
allow families who sense a loved one is deteriorating<br />
to activate the teams directly.<br />
Nurses dedicated to safety<br />
set new standards<br />
YNHH actively protects its patients from preventable<br />
danger through the work of two <strong>Yale</strong>-<strong>New</strong><br />
<strong>Haven</strong> Health System patient safety registered<br />
nurses—one for obstetrics, one for Perioperative<br />
Services.<br />
Working under the umbrella of Performance<br />
Management, the safety nurses’ primary role is to<br />
educate peers about safety, explains Jean Zimkus,<br />
patient safety nurse for Perioperative Services.<br />
They review literature on safety topics, talk to<br />
physicians and staff about unique challenges<br />
at YNHH, and spearhead improvements. They<br />
collaborate with other healthcare professionals<br />
to promote communication such as briefings and<br />
“hand-off communication,” essentially memos for<br />
new caregivers with pertinent information about<br />
patients who have been transferred from other<br />
units. They installed white boards in surgery suites<br />
for practitioners to make checklists about such<br />
concerns as allergies and fetal heart rates before an<br />
operation begins.<br />
A safety attitude questionnaire conducted among<br />
OB staff in 2004 and 2006, and in Perioperative<br />
Services in 2006 and <strong>2007</strong>, showed a statistically<br />
significant improvement in attitude toward safety<br />
and teamwork since their safety nurse was hired.<br />
Patient safety nurses expect to see continued<br />
improvement when they analyze the results of a<br />
<strong>2007</strong> survey in both their departments.<br />
Our soon to be hospital-wide hourly rounding<br />
initiative is a perfect example of something we<br />
often find when we seek out the evidence and<br />
take a hard look at how it fits with our needs<br />
at YNHH. Often a simple solution can bring<br />
greater rewards for less effort, and keep the<br />
focus where it matters most – on providing<br />
top-notch care for the patient.”<br />
— Francine LoRusso, R.N., Director of <strong>Nursing</strong>, Medicine<br />
Y A L E - N E W H A V E N H O S P I T A L 7
3<br />
Innovation<br />
<strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> continuously develops new ways to improve patient<br />
care, and nurses are a major factor in steering practice in positive new directions.<br />
Nurses may recommend an investment in a technology such as simulators that<br />
enhance the process of learning new practices, or they may develop a creative<br />
solution to a more organized medication delivery system.<br />
In the past few years, a number of innovations have significantly impacted<br />
patient care and patient safety, and resulted in changes in the way nurses care<br />
for patients.<br />
8 N U R S I N G U P D A T E
Pediatrics streamlines<br />
medication delivery<br />
One of the challenges for nurses caring for pediatric<br />
inpatients is to ensure that patients receive<br />
the correct medications they need in a timely<br />
manner. With a pharmacy department that fills<br />
3,800 orders a day, the staff wanted to make the<br />
process of medication dispensing and delivery as<br />
efficient and timely as possible.<br />
Kim Carter, R.N., patient service manager for<br />
the School-age/Adolescent Unit, formed a committee<br />
with Lorraine Lee, Pharmacy Services<br />
manager for medication safety and regulatory<br />
compliance, and members of both staffs. Last<br />
June, the group dedicated one week to pioneering<br />
a new medication delivery system using the<br />
“Lean” process improvement tools, a manufacturing<br />
process Toyota popularized and healthcare<br />
systems—including YNHH—have used to<br />
trim waste and inefficiencies in their processes.<br />
They developed eight interventions and<br />
launched them on the School-age/Adolescent<br />
Unit. They standardized time windows for delivery<br />
of various medications, now posted in the<br />
unit’s medication room, and created a dedicated<br />
area on the unit where all medications must be<br />
delivered. The committee also redesigned the<br />
medication room with a wall-mounted computer<br />
nearby so staff can easily look up information<br />
such as proper dosage and allergies.<br />
Due to the work of this unique collaborative<br />
committee, the School-age staff has seen<br />
significant benefits in accuracy and efficiency<br />
of medication delivery, and the new delivery<br />
system interventions are being implemented in<br />
all of YNHH’s pediatric units with eventual plans<br />
for the adult units as well.<br />
Simulators enhance<br />
nurses’ learning<br />
Since her arrival at the <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong><br />
Children’s <strong>Hospital</strong> last spring, Noelle has given<br />
birth hundreds of times. A life-size mannequin,<br />
Noelle can simulate the normal human birth<br />
process and be programmed to mimic birth<br />
complications. She comes complete with monitors<br />
that display maternal, fetal and newborn<br />
vital signs, and her simulation baby lets staff<br />
know its health status by its color: a healthy<br />
baby will be pink, while a baby experiencing<br />
oxygen deficiency will turn blue.<br />
“For nurses, the simulators are an excellent<br />
training tool,” Cheryl Raab, R.N., perinatal<br />
patient safety nurse, Performance Management,<br />
says. “Simulators give our nurses the<br />
opportunity to learn correct interventions in a<br />
risk-free environment, and provide them with<br />
information and feedback about their individual<br />
performance.”<br />
Raab is currently using Noelle to help train<br />
nurses, physicians, midwives and PCAs from both<br />
the Women’s Center and Labor and Birth, as well<br />
as medical and midwifery students. Meanwhile, in<br />
the Pediatric Emergency Department, SimBaby,<br />
<strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong>’s first interactive infant simulator,<br />
is used to train emergency healthcare professionals<br />
in the care of seriously ill infants.<br />
Simulation has become such an important training<br />
tool for nurses at YNHH that the hospital is<br />
looking at a future simulation center in partnership<br />
with <strong>Yale</strong> School of Medicine and <strong>Yale</strong><br />
School of <strong>Nursing</strong>.<br />
Wireless phone service<br />
speeds up care delivery<br />
When <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> equipped all<br />
of its nurses and patient care associates with<br />
“SpectraLink” wireless telephone service last<br />
year, telephone tag and noise from front-desk<br />
employees paging nurses became annoyances<br />
of the past, and patient satisfaction scores rose<br />
across the board.<br />
Every nurse and patient care associate (PCA)<br />
has a SpectraLink phone, which can be used<br />
for two-way communication throughout the<br />
hospital without the interference common with<br />
high-powered cellular phones. Patients may<br />
press the call button for assistance, or dial their<br />
nurse or PCA directly. The wireless phones also<br />
allow nurses to quickly connect with other staff<br />
to discuss pertinent information, treatment<br />
protocols, medication orders and time-sensitive<br />
information.<br />
“Equipping nurses and staff with wireless<br />
phones turned out to be a very positive innovation<br />
for caregivers,” said John Sward, R.N., patient<br />
service manager of the General Medicine<br />
Unit on 9-7, who trained nurses throughout<br />
YNHH in the use of the phones. Nurses hear<br />
about their patients’ needs more quickly and are<br />
better able to set priorities and serve them, he<br />
said. “The phones are speeding up the process<br />
of caregiving and make communication easier<br />
and quieter for everyone.”<br />
Innovations can change the way nurses practice<br />
in ways they don’t anticipate. For example,<br />
using wireless phones has made nursing more<br />
efficient in some ways. Now nurses don’t have<br />
to leave the bedside of one patient to take a<br />
phone call about another patient, and they<br />
are able to stay with a patient in crisis while<br />
communicating with the physician.”<br />
— Sue Arbo-Givens, R.N., Patient Service Manager, Orthopedics<br />
Y A L E - N E W H A V E N H O S P I T A L 9
4<br />
Community outreach<br />
Since its founding in 1826, one of YNHH’s most enduring missions has been its<br />
commitment to serving the community. This service takes many forms, including<br />
YNHH’s primary care, women’s and children’s centers and seven school-based clinics.<br />
Educating the public on health and nutrition, exposing high school students to careers<br />
in health care, and performing preventive screenings round out some of YNHH’s<br />
community efforts.<br />
Our nurses provide specialized care to the needy in our community. They are top-notch<br />
educators who are skilled at explaining complex medical conditions and role models for<br />
high school students interested in a nursing career.<br />
1 0 N U R S I N G U P D A T E
School-based nurses<br />
keep teens in the care loop<br />
Adolescents aren’t likely to go to the doctor<br />
on their own, and even parents who have<br />
insurance may be too busy to get them there.<br />
As a result, advanced practice nurses at seven<br />
YNHH school-based health centers (SBHC) in<br />
the greater <strong>New</strong> <strong>Haven</strong> area provide on-site<br />
services, including primary health assessments<br />
as well as diagnosis and treatment of major and<br />
minor illnesses.<br />
In <strong>2007</strong>, the YNHH SBHCs treated nearly 9,000<br />
students in elementary, middle and high schools<br />
in Branford, Hamden and <strong>New</strong> <strong>Haven</strong>. Nurses<br />
may treat or advise students on diabetes, obesity,<br />
pregnancy and sexually transmitted diseases.<br />
Lynn Peckham, advanced practice registered<br />
nurse in <strong>New</strong> <strong>Haven</strong>’s Sheridan Middle School,<br />
said the most prevalent problem she sees among<br />
students is asthma. She explains that schoolbased<br />
nurses make an impact in helping students<br />
manage asthma so they can stay in school and<br />
out of the hospital. In addition, YNHH social<br />
workers work on-site at the SBHCs and help<br />
students with anger management, anxiety,<br />
depression and phobias.<br />
In addition to providing an important link<br />
between students and additional community<br />
services, school-based nurses establish YNHH as<br />
a medical home for those who don’t have one.<br />
They also provide health education that gives<br />
students a firm understanding of the importance<br />
of taking responsibility for their own<br />
health.<br />
Nurses help detect cancer<br />
early in the community<br />
If success means convincing women to take<br />
responsibility for their health, the Connecticut<br />
Breast and Cervical Cancer Early Detection<br />
Program for medically underserved women is<br />
making its mark. Working out of the YNHH<br />
Department of Community Health, the staff has<br />
always had to make multiple calls to get some<br />
patients in for screenings, but lately more women<br />
have been seeking out the program and making<br />
appointments themselves.<br />
Christine Galla, R.N., case manager, gives credit to<br />
media marketing efforts and vigorous outreach.<br />
YNHH, one of 18 sites in the state to offer cancer<br />
screening through this program, sends outreach<br />
workers to churches, hair salons and housing<br />
projects to educate women. The program provides<br />
Pap smears to women 19 to 64 years of age<br />
who have no insurance coverage or prohibitive<br />
deductibles, and mammograms to medically<br />
underserved women who are 40 and older.<br />
The program especially hopes to reach older<br />
women, who are likely to avoid mammograms;<br />
and African-American and Hispanic women,<br />
who have the highest mortality rate among all<br />
racial and ethnic groups.<br />
In the grant’s fiscal year that ended in June <strong>2007</strong>,<br />
the Early Detection Program made outreach visits<br />
to 902 women at 20 locations in the greater <strong>New</strong><br />
<strong>Haven</strong> area, and provided services to 251 women.<br />
Last July, YNHH launched a digital mammography<br />
van, the first in Connecticut, to provide mammograms<br />
to women where they live and work.<br />
Stroke team takes the<br />
offensive against brain attacks<br />
Since YNHH revamped its stroke program,<br />
nurses have played a key role in helping the<br />
hospital earn the distinction as a Joint Commission<br />
Primary Stroke Center, providing acute<br />
and recovery care for the more than 600 stroke<br />
patients the hospital admits each year.<br />
Karin Nyström, A.P.R.N., clinical coordinator,<br />
said the stroke program and neuroscience units<br />
at YNHH offer rich opportunities for nurses interested<br />
in research or clinical nursing. They can<br />
participate on multidisciplinary teams specially<br />
trained to evaluate and treat stroke and other<br />
cerebrovascular diseases. Nurses also collaborate<br />
with the YNHH Emergency Department to<br />
enhance the effective use of the clot-dissolving<br />
agent tPA.<br />
YNHH was the first hospital in southern Connecticut<br />
and the fourth in <strong>New</strong> England to<br />
become nationally certified as a Primary Stroke<br />
Center by The Joint Commission.<br />
In addition, YNHH nurses are actively involved<br />
with the program’s Stamp Out Stroke (S.O.S.)<br />
team, which educates people in the community<br />
to recognize symptoms of stroke and get to the<br />
hospital by calling 9-1-1 within the three-hour<br />
window when treatment is most successful.<br />
While the program has yet to measure the clinical<br />
outcomes of these efforts, Nystrom believes<br />
outreach, close teamwork and cutting-edge<br />
treatments are making a powerful impact in the<br />
diagnosis and treatment of stroke.<br />
Every woman in <strong>New</strong> <strong>Haven</strong> should make appointments for<br />
annual mammograms and cervical screenings. Unfortunately,<br />
needy women have incredibly difficult lives – they have to get<br />
past economic and transportation barriers, not to mention the<br />
fear barrier. At YNHH, we are reaching these women and letting<br />
them know we can help. Their health is important to us.”<br />
— Christine Galla, R.N., Case Manager, Connecticut Breast and Cervical Cancer<br />
Early Detection Program<br />
Y A L E - N E W H A V E N H O S P I T A L 1 1
5<br />
Research<br />
Nurses do their most important work at the patient’s bedside, and are often in the best<br />
position to question the many ways to care for patients – which approaches are working<br />
and which areas need closer scrutiny.<br />
At YNHH, research projects conducted by nurses have prompted changes that have<br />
raised the bar on patient care and improved patient outcomes. Through their<br />
questioning and analysis, nurses help the hospital develop more effective practices and<br />
procedures, control quality and improve patient satisfaction across the board.<br />
1 2 N U R S I N G U P D A T E
SICU nurses take evidencebased<br />
approach to care<br />
Surgical Intensive Care Unit (SICU) nurses are<br />
taking a fresh look at how they provide patient<br />
care with the help of an evidence-based practice<br />
committee. Quarterly, the committee analyzes<br />
the literature on topics selected by SICU nursing<br />
staff and then assists the staff in applying the<br />
findings to their practice.<br />
The SICU’s innovative approach has been so<br />
successful it earned SICU nurses Rick O’Connor,<br />
B.S.N., R.N., and Zachary Krom, B.S.N., R.N., the<br />
opportunity to present the results of the<br />
committee’s work at Sigma Theta Tau’s 18th<br />
International Conference in Vienna, Austria, last<br />
summer. More locally, they are expanding their<br />
important work into other YNHH intensive care<br />
units.<br />
The committee uses the hospital’s chosen model<br />
of incorporating research into practice, the Iowa<br />
Model, which provides a guide for clinical decision-making<br />
and details regarding implementation.<br />
The model includes both the practitioner<br />
and organizational perspectives.<br />
One significant result of the committee’s research<br />
in the SICU is further reinforcement of encouraging<br />
family visitation during resuscitative and<br />
invasive procedures, such as CPR and chest tube<br />
insertions. In cases where both caregivers and<br />
the family are comfortable, families are invited to<br />
stay in their loved one’s room as a nurse or social<br />
worker talks them through the experience. Krom<br />
and O’Connor’s research found that families who<br />
witness efforts to save a loved one’s life are appreciative<br />
to be part of the process. In addition, this<br />
practice can provide a greater sense of closure for<br />
those who are grieving.<br />
Study examines charge nurse<br />
and decision-making<br />
The personality traits of charge nurses do not<br />
always mix with those of physicians – in fact,<br />
the two can be polar opposites, according to a<br />
study conducted by Victoria Dahl Vickers, R.N.,<br />
M.B.A., who was recently named coordinator of<br />
regulatory readiness, and Eija Faulkner, learning<br />
and development consultant in the hospital’s<br />
Institute for Excellence. They presented their<br />
findings last year at the National <strong>Nursing</strong> Staff<br />
Development Organization’s annual convention<br />
in Atlanta.<br />
Vickers and Faulkner assessed nurses at <strong>Yale</strong>-<br />
<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> with the help of the<br />
Myers-Briggs personality model, typically used<br />
by career counselors. Out of 149 nurses who<br />
participated, 98 identified “feeling” as their<br />
decision-making preference mode, which is the<br />
opposite of physicians, who tend to use a “thinking”<br />
mode to make decisions, Vickers explained.<br />
The second part of the survey dealt with conflict<br />
resolution, using the Thomas Kilman Conflict<br />
Mode Instrument, a leading instrument used to<br />
assess conflict-handling styles. Asked to describe<br />
their conflict resolution style, most nurses expressed<br />
a preference for avoiding conflict.<br />
Vickers and Faulkner, who are using their findings<br />
in training sessions for nurses, say awareness<br />
of how nurses relate to colleagues is useful<br />
because it can help them make adjustments and<br />
perform more efficiently when working as part<br />
of a team.<br />
Nurses play key role<br />
on successful diabetes team<br />
For patients with diabetes, the evidence is<br />
increasingly clear that aggressive management<br />
of blood glucose can reduce complications<br />
from illness or surgery, lower rates of infection<br />
and shorten hospital stays. At <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong>,<br />
nurses on Connecticut’s first full-time multidisciplinary<br />
diabetes team play a key role in keeping<br />
glucose levels down.<br />
The team—a joint effort between YNHH and<br />
<strong>Yale</strong> School of Medicine—includes physicians<br />
and caregivers collaborating with primary care<br />
teams to control blood sugar and educate patients<br />
about their diabetes before discharge.<br />
Last year, the team presented 11 months of data<br />
on its work and earned the top prize in research<br />
for <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> at the annual <strong>2007</strong><br />
Joseph A. Zaccagnino Patient Safety and Clinical<br />
Quality Conference.<br />
Among the team’s findings: Glucose is better<br />
controlled when patients receive either a continuous<br />
insulin infusion with frequent monitoring,<br />
or a basal bolus correction regimen, an<br />
approach that imitates normal physiology by<br />
using a fast-acting (bolus) insulin with each meal<br />
and a long-acting (basal) insulin once or twice a<br />
day. Two nurses, Helen Psarakis, A.P.R.N., and<br />
Gael Ulisse, A.P.R.N., contributed to the project<br />
team’s findings and success.<br />
We developed our evidence-based practice committee because<br />
we want nurses to keep searching for the best ways to care<br />
for patients. Research turns up new information all the time,<br />
and nurses need to have this information available to them.<br />
With more data and research behind their practice, nurses can<br />
make better choices and that improves care overall.”<br />
— Zachary Krom, R.N., Surgical Intensive Care Unit<br />
Y A L E - N E W H A V E N H O S P I T A L 1 3
6<br />
Growth and<br />
development<br />
Professional development for nurses at <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> begins on the first<br />
day of employment and spans their careers. As part of their orientation, nurses receive<br />
intensive training that continues through their first year of service. Nurses at YNHH<br />
also have opportunities for career development as the hospital introduces the latest<br />
cutting-edge treatments for improved patient care and safety.<br />
As a result, patients who come to YNHH can expect not only the utmost sensitivity and<br />
warmth in their care, but also some of the most knowledgeable nurses in their fields.<br />
1 4 N U R S I N G U P D A T E
Nurses improve practice<br />
through transplant<br />
certification<br />
With the recent appointment of Sukru Emre,<br />
M.D., an internationally known transplant<br />
surgeon, the <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> Transplantation<br />
Center has witnessed a growing patient volume,<br />
and cutting-edge surgeries such as the first split<br />
liver and living donor liver transplant performed<br />
in Connecticut. Last year, nurses expanded their<br />
knowledge about transplantation in a study<br />
group for a new Certified Clinical Transplant<br />
Nurse (CCTN) credential exam developed by the<br />
American Board of Transplant Certification.<br />
Rick O’Connor, R.N., SICU, who led the study<br />
group and was the first nurse to take the exam,<br />
said research shows nurse certification improves<br />
outcomes for transplant patients. The CCTN<br />
exam covers heart, liver, kidney and pancreas<br />
transplants, in addition to lung and small bowel<br />
transplants. The certification also covers a<br />
variety of nursing concerns and topics, including<br />
vascular complications, infection control and<br />
drugs that prevent rejection.<br />
This year, three more YNHH nurses are planning<br />
to take the rigorous test. Meanwhile, O’Connor<br />
plans to begin a new study group and is targeting<br />
all surgical ICU nurses to participate to<br />
prepare for next year’s test.<br />
Nurses standardize the<br />
language of fetal monitoring<br />
Families who decide to have babies at <strong>Yale</strong>-<strong>New</strong><br />
<strong>Haven</strong> <strong>Hospital</strong> can feel especially confident that<br />
they will have a successful experience thanks to<br />
an emphasis on safety in labor and delivery. A<br />
perinatal patient safety nurse has instituted some<br />
30 new evidence-based clinical guidelines, and<br />
trained all perinatal teams in the proper use and<br />
interpretation of fetal monitoring tests.<br />
Her work has resulted in a 30-40 percent reduction<br />
in adverse events in obstetrics, including<br />
stillbirths, birth injuries and low Apgar scores<br />
for newborns.<br />
Training and certification in the use of fetal<br />
monitoring alone made an especially significant<br />
impact in the department. “Historically, doctors<br />
and nurses trained separately in fetal monitoring,<br />
and learned different terminologies,” said<br />
Cheryl Raab, R.N., the perinatal safety nurse.<br />
In the late ’90s, standard terminology was developed<br />
to provide a common language pertaining<br />
to variability and rates of acceleration and<br />
deceleration of fetal heart rate.<br />
Staff members on units that perform fetal monitoring<br />
have taken and passed the fetal monitoring<br />
training. Raab said the 223 obstetricians,<br />
nurses and midwives who trained at YNHH<br />
and took a national certification test had an<br />
initial 99 percent pass rate, compared with a<br />
national 87 percent pass rate.<br />
Residency provides<br />
support for new nurses<br />
The hospital’s Post-Baccalaureate Nurse Residency<br />
Program provides important support for<br />
new nurses as they make the transition from<br />
nursing students to acute-care professionals.<br />
That support—unique among hospitals in <strong>New</strong><br />
England—has also become a draw for nurses<br />
who choose to start their careers at YNHH.<br />
In three years, 137 new nurses have completed<br />
the year-long program developed by the<br />
University Health System Consortium and the<br />
American Association of Colleges of <strong>Nursing</strong>.<br />
Residents cover such topics as clinical judgment<br />
and leadership development. They meet monthly<br />
in small groups with a resident facilitator<br />
who may be from Southern Connecticut State<br />
University, <strong>Yale</strong> School of <strong>Nursing</strong> or <strong>Yale</strong>-<strong>New</strong><br />
<strong>Haven</strong> <strong>Hospital</strong>.<br />
In addition, 29 new associate degree and<br />
diploma nurses have completed the <strong>New</strong> Graduate<br />
Associate and Diploma Nurses First Year<br />
Development Program, a parallel program to<br />
the Nurse Residency Program.<br />
Every new graduate nurse at YNHH is required<br />
to participate in one of the two programs.<br />
Graduates report that the programs gave them<br />
the direction and support they need at a critical<br />
time in their careers, giving them confidence and<br />
introducing them to nurses who address their<br />
questions in an encouraging environment.<br />
“<br />
Critical care nurses are feeling the impact of<br />
the increased volume of transplant patients,<br />
so it is becoming increasingly important for<br />
us to enhance our knowledge as we set up<br />
nursing guidelines and follow these special<br />
patients through their ICU course. Advances<br />
in medicine at YNHH are challenging nurses<br />
to challenge themselves to keep improving<br />
upon the way they provide care.”<br />
— Rick O’Connor, R.N., Surgical Intensive Care Unit<br />
and Staff Nurse Council Co-Chair<br />
Y A L E - N E W H A V E N H O S P I T A L 1 5
7<br />
Recognition<br />
In a busy environment that operates 24 hours a day, seven days a week and<br />
365 days a year, it is sometimes easy to forget to take a step back and recognize the<br />
extraordinary women and men who are direct care givers to the tens of thousands<br />
of patients who choose YNHH for their care.<br />
While its nurses have historically been highly regarded in Connecticut and beyond,<br />
the hospital has intensified its effort to develop opportunities to find and honor its<br />
finest nurses. Below are just a few of the ways in which YNHH nurses have been<br />
honored for their contributions to patient care.<br />
1 6 N U R S I N G U P D A T E
YNHH named 12<br />
Nightingales in <strong>2007</strong><br />
Each year, <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> nominates nurses<br />
for the Nightingale Award, an award the honors<br />
nurses from greater <strong>New</strong> <strong>Haven</strong> area hospitals<br />
and healthcare institutions for commitment to<br />
excellence in their nursing practice. The Visiting<br />
Nurse Association of South Central Connecticut,<br />
the <strong>Hospital</strong> of St. Raphael, the Community<br />
Foundation for Greater <strong>New</strong> <strong>Haven</strong> and<br />
YNHH are founding sponsors of the Nightingales<br />
program which raises awareness of the<br />
contributions nurses make.<br />
The 12 <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> nurses honored as<br />
Nightingales in <strong>2007</strong> were:<br />
ABOVE Nine of the Nightingales honored in <strong>2007</strong> met in the Atrium for their “class” photo with Sue Fitzsimons (right). Shown are<br />
(l-r): Gloria Wallace, Elizabeth Miller, Joan Workman, Jill Jolley, Barbara Ackerman, Deirdre Lonergan, Gerri Slowikowski, Millicent<br />
Gershon and Earl Hapgood.<br />
Five nurse leaders honored<br />
At the <strong>2007</strong> Nurse of the Year ceremony,<br />
five nurses were honored with four nurse<br />
leadership awards. Shown (below) in Harkness<br />
Hall, where the ceremony was held, are (l-r):<br />
Surgical Intensive Care Unit nurses Zach Krom<br />
and Rick O’Connor, who received the award for<br />
research; Shelley Harrigan, Adult Primary Care<br />
Center, for practice; Sue Fitzsimons, senior vice<br />
president, Patient Services; Karen Camp,<br />
retired nurse manager for whom the management<br />
award is named; and Marie Devlin, R.N.,<br />
patient service manager, SICU, who received<br />
the Karen L. Camp Award for Management.<br />
Unable to attend the ceremony was Ann Marie<br />
Rausch, R.N., Surgery (6-5), who earned the<br />
education award.<br />
Barbara Ackerman (in memoriam)<br />
<strong>New</strong>born Special Care Unit<br />
Jeannine Bradley<br />
Pediatric Emergency Department<br />
Laurie Finta<br />
Ambulatory Surgery<br />
Millicent Gershon<br />
Diagnostic Radiology<br />
Earl Hapgood<br />
Adult and Pediatric Post-Anesthesia Care Units<br />
Jill Jolley<br />
School-age/Adolescent Unit<br />
Mengqing Lai<br />
Winchester Chest Clinic<br />
Deirdre Lonergan<br />
Orthopedics<br />
Elizabeth Miller<br />
Maternal Special Care<br />
Gerri Slowikowski<br />
Surgical Intensive Care Unit<br />
Gloria Wallace<br />
Acute Care for the Elderly<br />
Joan Workman<br />
Adult Inpatient, <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong><br />
Psychiatric <strong>Hospital</strong><br />
Y A L E - N E W H A V E N H O S P I T A L 1 7
Nurse of the Year <strong>2007</strong><br />
Each year during National Nurse Week, <strong>Yale</strong>-<br />
<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> takes the opportunity to<br />
recognize its nurses in a variety of ways. Each<br />
unit nominates a nurse for her or his commitment<br />
to patient care. The following nurses were<br />
honored as Nurse of the Year from their units.<br />
Jeff Agli<br />
Diagnostic Radiology<br />
Deanna Arizzi<br />
Medical Oncology/Bone Marrow Transplant<br />
Ann Marie Bautz<br />
Cardiac Medical Units (5-2/3)<br />
Nadine Bruder<br />
School-age/Adolescent<br />
Pat Capone<br />
Acute Care for the Elderly<br />
Pam Cohane<br />
Pediatric Specialty Center<br />
Amanda Coppola<br />
Infant/Toddler<br />
Sherry Coyle<br />
South Pavilion Operating Room<br />
Christine Danilowicz<br />
General Medicine (9-7)<br />
Chris DeFrancesco<br />
Adult Emergency Department<br />
Kate Delossantos<br />
Adult Resource Support Unit<br />
Diane Dirzius<br />
Medical Oncology Clinic<br />
Marcie Durso<br />
Pediatric Primary Care Center<br />
Stacy Farago<br />
General Medicine (5-7)<br />
Allison Febbroriello<br />
Maternal Special Care<br />
Ellen Ferraro<br />
Surgery (6-5)<br />
Tracey Frith<br />
Obstetrics (WP 11)<br />
Toni Frizinia<br />
Cardiac Medical Units (5-2/3)<br />
David Gauley<br />
Adult Diagnostic Radiology<br />
Megan Gnidula<br />
Pediatric Catheter Laboratory<br />
Joanne Gorman<br />
Women’s Primary Care Center<br />
Jill Grillo<br />
Cardiothoracic Intensive Care Unit<br />
Michael Hayes<br />
Surgery (6-7)<br />
Betsy Hine<br />
Cardiac Intensive Care Unit<br />
Deb Hollaway<br />
Shoreline Medical Center ED<br />
Lynn Irons<br />
Adult Primary Care Center<br />
Terri Johnson<br />
Shoreline Medical Center Post-Anesthesia Care Unit<br />
(PACU)<br />
Susanne Koshis<br />
GI Procedure Center<br />
Debbie Krista<br />
Pediatric PACU<br />
Roman Kudrycki<br />
Adolescent Unit YNHPH<br />
Kimberly La Pia<br />
Breast Center<br />
Sandy Lee<br />
Medical Intensive Care Unit<br />
Annelie Lindvall<br />
Dual Diagnosis YNHPH<br />
Li-Ping Liu<br />
Neuroscience Intensive Care Unit<br />
Deirdre Lonergan<br />
Orthopedics<br />
Jennifer Maddern<br />
Surgery (6-4)<br />
Katie Mannochi<br />
PACU<br />
Susan Marchini<br />
General Medicine (10-7)<br />
Marilou Masocol<br />
Adult Unit YNHPH<br />
Allyson McManama<br />
Temple Recovery Care Center<br />
Sherry Molaskey-Jones<br />
Perinatal Maternal-Fetal Medicine<br />
Shanda Nardelli<br />
Gyn/Oncology Unit<br />
Peggie O’Donnell<br />
Apheresis/Transfusion Service<br />
Jillian Orlando<br />
Pediatric Oncology/Respiratory Care Unit<br />
Paula Pastore<br />
Children’s Psychiatric Inpatient Service<br />
Carol Penta<br />
Radiation Therapy<br />
Melissa Rafael<br />
Surgical Intensive Care Unit<br />
Judy Rodriguez<br />
Neuro Medicine and Surgery<br />
Jerrilyn Rosa<br />
Express Admission Service/Pre-Admission Testing<br />
Joyce Russell<br />
General Clinical Research Center<br />
Marjorie Russell<br />
General Medicine (5-5)<br />
Rowena Saga-Abrina<br />
Cardiac Surgery<br />
Aida Santiago<br />
Ambulatory PACU<br />
Jenny Scholl<br />
Pediatric Emergency Department<br />
Jackie Selly<br />
Surgery (7-5)<br />
Diane Smart-Greene<br />
General Medicine (9-5)<br />
Mary Ellen Smith<br />
<strong>New</strong>born Special Care Unit<br />
Nancy Smith<br />
Obstetrics (WP 10)<br />
Joy Southard<br />
Pediatric Resource Support Unit<br />
Wynnett Stewart<br />
Nathan Smith Clinic<br />
Sheila Stranz<br />
Temple Surgical PACU<br />
Christine Suntheimer<br />
Perinatal Maternal-Fetal Medicine<br />
Jaime Swartz<br />
Children’s Research/Oncology<br />
Dennis Uy<br />
Ambulatory OR<br />
Sally Varghese<br />
Pediatric Intensive Care Unit<br />
Lori Vogt<br />
Labor and Birth<br />
ABOVE RIGHT Last year, YNHH president and CEO Marna P. Borgstrom (left) personally<br />
congratulated each of the 16 employees who were named “I am <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong>”<br />
Service Excellence Heroes. Here she is shown with Anne Summach, R.N.,<br />
Neuroscience Unit.<br />
RIGHT Richard D’Aquila, executive vice president and COO, regularly rounds on patient<br />
care units. Nurses take the opportunity to discuss issues with him when he visits. On<br />
a recent visit to General Surgery (6-7), D’Aquila meets (l-r): Linda Russell, R.N., Terri<br />
Wusterbarth, R.N., and Nancy Hoey, R.N., patient service manager.<br />
1 8 N U R S I N G U P D A T E
Service Excellence<br />
Heroes for <strong>2007</strong><br />
Sixteen <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> employees<br />
were named “I am <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong>” Service<br />
Excellence Heroes. Five nurses were among<br />
the first 16 employees to be honored with this<br />
significant hospital award. They are:<br />
Nicole Buxton, R.N.<br />
Post-Partum (WP 11)<br />
Earl Hapgood, R.N.<br />
Nurse Educator, Adult and Pediatric Post-Anesthesia<br />
Care Units<br />
Larry Richardson, R.N.<br />
Coordinator of Transplant Services,<br />
Perioperative Services<br />
Anne Summach, R.N.<br />
Neuroscience/Acute Care Unit<br />
Ena Williams, R.N.<br />
<strong>Nursing</strong> Director, Perioperative Services<br />
Recognition and Clinical<br />
Advancement Program<br />
In 1991, <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> <strong>Hospital</strong> introduced<br />
an internal clinical ladder called the Recognition<br />
and Clinical Advancement Program (RCAP), and<br />
more than 2,000 nurses have advanced on it.<br />
RCAP has three rungs – Clinical Nurse II, III and<br />
IV – and managers consistently encourage nurses<br />
to climb the ladder through a rigorous program<br />
in which nurses, working with a preceptor, record<br />
their experiences with patients in a portfolio<br />
of exemplars. Nurses who advance are recognized<br />
at a quarterly ceremony. The following<br />
nurses advanced to levels II and III in <strong>2007</strong>.<br />
Clinical Nurse III<br />
Evelyn Afriyie<br />
Post-Anesthesia Care Unit<br />
Jill Azzarone<br />
Oncology/Pediatric Respiratory Care Unit<br />
Twila Balint<br />
Occupational Health Services<br />
Melissa Barre<br />
Surgical Intensive Care Unit<br />
Janet Battaglia<br />
Express Admissions<br />
Michelle Bosley<br />
Surgery Unit (7-5)<br />
Nicole Buxton<br />
Maternity (WP 11)<br />
Kathy Caliendo<br />
Surgery Unit (4-7)<br />
Erin Cavanaugh<br />
Labor and Birth<br />
Christopher DeFrancesco<br />
Adult Emergency Department<br />
Laurie Devin<br />
Resource Support Unit<br />
Janina Dziurzynski<br />
GI Procedure Clinic<br />
Tamar Edelkind<br />
<strong>New</strong>born Special Care Unit<br />
Pam Fleming<br />
Surgery Unit (4-7)<br />
Elizabeth Flynn<br />
Temple Recovery Care Center<br />
Cindy Fusco<br />
Surgery Unit (7-5)<br />
Patricia Gray<br />
Oncology/Pediatric Respiratory Care Unit<br />
Daniel Hartmann<br />
Adult Emergency Department<br />
ABOVE Nurses attend the Recognition and Clinical Advancement<br />
Program to celebrate the advancement of their colleagues<br />
on the three-rung clinical ladder. The three nurses who<br />
attained Level III and senior managers are shown (l-r): Chong<br />
Jumarito-Panaguiton, R.N., CTICU; Sue Fitzsimons, senior<br />
vice president, Patient Services; Debbie DiMarco, R.N.,<br />
Perioperative Services; Leslie O’Connor, A.P.R.N., clinical<br />
director, <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong> Psychiatric <strong>Hospital</strong>; Kevin Myatt,<br />
senior vice president, Human Resources; and Alison Lucibello,<br />
R.N., CICU.<br />
Theresa Hyland<br />
Labor and Birth<br />
Katherine Mannochi<br />
South Pavilion Post-Anesthesia Care Unit (PACU)<br />
Staci McNeil<br />
Adult Primary Care Center<br />
Phyllis Murphy<br />
Medical Intensive Care Unit<br />
Eleanor Myers-Brown<br />
South Pavilion PACU<br />
Laetitia Nakaar<br />
Gyn/Oncology Unit<br />
Carol Nockunas<br />
GI Procedure Clinic<br />
Megan Nolan<br />
Labor and Birth<br />
Anne H. O’Connor<br />
<strong>Hospital</strong> Research Unit<br />
Danielle Orfitelli<br />
Adult Emergency Department<br />
Victoria Parker Orkins<br />
Cardiothoracic Intensive Care Unit<br />
Jillian Orlando<br />
Oncology/Pediatric Respiratory Care Unit<br />
Alaire Perazella<br />
Maternal-Fetal Medicine Unit<br />
Stephanie Piscitelli<br />
Oncology/Pediatric Respiratory Care Unit<br />
Annalisa Porter<br />
Surgical Intensive Care Unit<br />
Carey Ranz<br />
Surgery Unit (4-7)<br />
Kelley Reddington<br />
Labor and Birth<br />
Y A L E - N E W H A V E N H O S P I T A L 1 9
Rowena Saga-Abrina<br />
Surgery Unit (4-7)<br />
Cristina Santiago<br />
Diagnostic Radiology<br />
John Strathy<br />
Surgical Intensive Care Unit<br />
Tracy Sturrock<br />
Medicine Unit (6-5)<br />
Jeramy Tabuzo<br />
<strong>Hospital</strong> Research Unit<br />
Carolyn Thompson<br />
Gyn/Oncology Unit<br />
Clinical Nurse II<br />
Roxanne Amato<br />
Adult Emergency Department<br />
Deanna Arizzi<br />
Medical Oncology<br />
Annette Avallone<br />
Acute Care for the Elderly<br />
Frank Balisciano<br />
Ambulatory Surgery<br />
Samantha Bean<br />
Maternal Special Care Unit<br />
Lisa Berardi<br />
Temple Surgical Recovery<br />
Filjah Bernardo<br />
Acute Care for the Elderly<br />
Deborah Bok<br />
Temple Endoscopy Center<br />
Elizabeth Borges<br />
Acute Care for the Elderly<br />
Peggy Bouchard<br />
Cardiothoracic Intensive Care Unit<br />
Jessica Boughton<br />
School-age/Adolescent Unit<br />
R. Titlope Boyejo<br />
Women’s Center<br />
Donna Brester<br />
Pediatric Intensive Care Unit<br />
Erin Brown<br />
Medicine Unit (5-5)<br />
Maureen Bruce<br />
Surgery Unit (6-7)<br />
Nadine Bruder<br />
School-age/Adolescent Unit<br />
Carly Brueggestrat<br />
Cardiothoracic Intensive Care Unit<br />
Shayleen Brueggestrat<br />
Surgery Unit (6-4)<br />
Starley Buchanan<br />
School-age/Adolescent Unit<br />
Heather Bugay<br />
Medical Intensive Care Unit<br />
Lois Caldrello<br />
Cardiothoracic Intensive Care Unit<br />
Arturo Capiral<br />
Perioperative Services<br />
Tracey Cassese<br />
Pediatric Emergency Department<br />
Tammy Ciuci<br />
Surgery Unit (6-4)<br />
Maria Lourdes Co<br />
Medical Oncology Unit<br />
Sheryl Combs<br />
Pediatric Resource Pool<br />
Daniel Coraluzzi<br />
Temple Surgical<br />
Robin Corcoran<br />
Shoreline Surgery/Endoscopy<br />
Denise Corso<br />
<strong>New</strong>born Special Care Unit<br />
Janice Cossette<br />
Shoreline Surgery/Endoscopy<br />
Valerie Curbow<br />
Adult Emergency Department<br />
Jeffrey Curran<br />
Surgery Unit (7-5)<br />
Amy Cusano<br />
Medical Oncology Unit<br />
Heather Daigle<br />
<strong>New</strong>born Special Care Unit<br />
Melanie D’Amato<br />
School-age/Adolescent Unit<br />
Debbie Debiase<br />
Surgery Unit (6-4)<br />
Amy Degray<br />
Maternal Special Care Unit<br />
Roselyn Desiree<br />
Medicine Unit (9-7)<br />
Donna D’Eugenio<br />
<strong>Hospital</strong> Research Unit<br />
Kathryn Dias<br />
Surgical Intensive Care Unit<br />
Joan Ecklund<br />
Orthopedics Unit<br />
Tricia Eddy<br />
Perioperative Services<br />
Etsuko Elmammann<br />
Orthopedics Unit<br />
Samantha Emerling<br />
Medicine Unit (9-7)<br />
Dolores Errity<br />
Temple Surgical Recovery<br />
Carlotta Evans<br />
Surgery Unit (6-4)<br />
Martha Ferreira<br />
Surgery Unit (6-4)<br />
M. Michele Flowers<br />
South Pavilion Operating Rooms<br />
Autumn Foshee<br />
Maternity (WP 11)<br />
Jill Franco<br />
Labor and Birth<br />
Tracey Frith<br />
Maternity (WP 11)<br />
Heather Gainer<br />
Medicine Unit (9-5)<br />
Mary Catherine Gannon<br />
Surgery Unit (7-5)<br />
Elizabeth Gernat<br />
Maternity (WP 11)<br />
Cecilyn Glorioso<br />
Medicine Unit (9-7)<br />
Kevin Gonzalez<br />
Medical Intensive Care Unit<br />
Erwille Joy Gurdek<br />
Labor and Birth<br />
Carrie Guttman<br />
Gyn/Oncology Unit<br />
Katarzyna Haley<br />
Orthopedics Unit<br />
Lois Hawken<br />
Resource Support Unit<br />
Stephanie Hays<br />
Neuro Intensive Care Unit<br />
Robyn Hewitt<br />
Adult Emergency Department<br />
Stephanie Hinchliff<br />
Surgical Intensive Care Unit<br />
Deborah Hollaway<br />
Shoreline Emergency Department<br />
Jessica Holmes<br />
Maternity Unit (WP 11)<br />
Megan Homes<br />
Medical Oncology Unit<br />
Chelsea Howell<br />
Medical Oncology Unit<br />
Marie Gael Husmalaga<br />
Medicine Unit (9-7)<br />
Danielle Innis<br />
Medicine Unit (9-5)<br />
Kenneth Jacobs<br />
Shoreline Emergency Department<br />
Nataliya Jatsiv<br />
Surgery Unit (6-5)<br />
Elizabeth Jobbagy<br />
Surgical Intensive Care Unit<br />
Cheryl Jones<br />
South Pavilion Post-Anesthesia Care Unit<br />
Lisa Jones<br />
Medicine Units (10-7/8)<br />
Lida Jureczko-Russell<br />
Urology/General Surgery Unit<br />
Kristine Keller<br />
Adult Emergency Department<br />
20 nursing uPDATE
Carol Kennedy<br />
Oncology/Pediatric Respiratory Care Unit<br />
Shawn King<br />
Cardiothoracic Intensive Care Unit<br />
Linda Koch<br />
Radiation Therapy<br />
Maria Koursaris<br />
Neuro Intensive Care Unit<br />
Hope Lamberson<br />
Surgery Unit (7-5)<br />
Jay Lano<br />
Medicine Unit (5-7)<br />
Sara Lantowski<br />
Gyn/Oncology Unit<br />
Liliana Lara<br />
Maternity (WP 11)<br />
Elpidio Latorilla<br />
Temple Surgical<br />
Tracy Lee<br />
Medicine Unit (5-7)<br />
Carolyn Levy<br />
Labor and Birth<br />
Tawnia Lewis<br />
<strong>New</strong>born Special Care Unit<br />
Alison Linske<br />
Surgery Unit (6-4)<br />
Virach Lotharakphong<br />
Cardiothoracic Intensive Care Unit<br />
Robyn Lussier<br />
Temple Surgical Recovery<br />
Dawn Lyder<br />
Labor and Birth<br />
Brittany Lyhus<br />
Pediatric Intensive Care Unit<br />
Jennifer Maddern<br />
Surgery Unit (6-4)<br />
Jena Malchiodi<br />
Apheresis<br />
Mary Manseau<br />
Surgery Unit (6-7)<br />
Destiny Massaro<br />
Adult Emergency Department<br />
Stella Mateo<br />
Maternity (WP 11)<br />
Tracy Mazzella<br />
Surgery Unit (6-4)<br />
Christina McCann<br />
Acute Care for the Elderly<br />
Diane McQueeney<br />
Temple Surgical<br />
Stacy Mehmet<br />
Medicine Unit (5-5)<br />
Alexandra Mena Hertado<br />
Medical Oncology Unit<br />
Felice Mennone<br />
Maternal Special Care Unit<br />
Sami Merit<br />
Neuro Intensive Care Unit<br />
Shandi Montiel<br />
Pediatric Emergency Department<br />
Diana Moore<br />
Maternity (WP 11)<br />
Jennifer Morgan<br />
Surgical Intensive Care Unit<br />
Sandra Morgan<br />
Temple Recovery Care<br />
Deann Morin<br />
School-age/Adolescent Unit<br />
Krystal Mozny<br />
Pediatric Emergency Department<br />
Catherine Mulvey<br />
Shoreline Emergency Department<br />
Kathleen Murphy<br />
Temple Endoscopy Center<br />
Lindsay Neptune<br />
Infants and Toddlers Unit<br />
Melane Ninonuevo<br />
Labor and Birth<br />
Vicki Ogbejesi<br />
Resource Support Unit<br />
Mary Okwusosu-Osakwe<br />
Medical Oncology Unit<br />
Elaine Ovecka<br />
Medical Intensive Care Unit<br />
Maria Paterno<br />
South Pavilion Operating Rooms<br />
Erin Patton<br />
Pediatric Intensive Care Unit<br />
Alisha Pearson<br />
Adult Emergency Department<br />
Jennifer Pelletier<br />
Oncology/Pediatric Respiratory Care Unit<br />
Melanie Pipping<br />
South Pavilion Operating Rooms<br />
Doreen Prentise<br />
Perioperative Services<br />
Marian Quitain<br />
Adolescent/Geriatric Unit YNHPH<br />
Cathy Rafalowski<br />
Acute Care for the Elderly<br />
Meighann Recile<br />
Medicine Unit (9-5)<br />
Wayne Rollins<br />
Medical Oncology Unit<br />
Jasmine Rosales-Anchetta<br />
Medicine Unit (9-7)<br />
Heather Rosario<br />
Ambulatory Surgicenter<br />
Lorien Sargolini<br />
<strong>Hospital</strong> Research Unit<br />
Jaime Sawyer<br />
Medicine Unit (5-5)<br />
Susan Shaw<br />
Labor and Birth<br />
Rachael Soyka<br />
Adult Emergency Department<br />
Kathryn Standish<br />
Medicine Unit (5-5)<br />
Marina Syrax<br />
Medicine Unit (9-7)<br />
Cindy Taylor<br />
South Pavilion PACU<br />
Alyssa Wanat<br />
Medicine Unit (5-5)<br />
Louise Ward<br />
Labor and Birth<br />
Ilene (Dee) Zimmerman<br />
Radiation Therapy<br />
Daniel Zweeres<br />
Medicine Unit (5-5)<br />
AONE taps three nurses<br />
for its prestigious fellowship<br />
In <strong>2007</strong>, the American Organization of Nurse<br />
Executives (AONE) chose three <strong>Yale</strong>-<strong>New</strong> <strong>Haven</strong><br />
nurse leaders for its prestigious <strong>2008</strong> nurse manager<br />
fellowship. They are (below): Denine Baxter,<br />
R.N., patient service manager, Pediatric ED;<br />
Marie Devlin, R.N., patient service manager, SICU<br />
and Stepdown and General Trauma Unit; and<br />
Sandra Watcke, R.N., patient service manager,<br />
Medical Oncology Treatment Center.<br />
The AONE Nurse Manager Fellowship is a yearlong<br />
professional development program designed<br />
to provide in-depth education and development<br />
through four fellowship retreats, by applying<br />
classroom learning in the workplace and through<br />
electronic communications with expert faculty<br />
and other fellows. The goal of the program is to<br />
ensure the vitality of strong nursing leadership<br />
within American healthcare organizations.<br />
a b o v e The three YNHH nurse managers chosen for AONE<br />
fellowships meet with Sue Fitzsimons. Shown (l-r) are: Denine<br />
Baxter; Sandra Watcke; Sue Fitzsimons, R.N., Ph.D., senior vice<br />
president, Patient Services; and Marie Devlin.<br />
YAlE-nEw hAvEn hosPiTAl 21
N U R S I N G<br />
U P D A T E


![Annual Report Donor Listings [pdf] - Yale-New Haven Hospital](https://img.yumpu.com/49673575/1/190x245/annual-report-donor-listings-pdf-yale-new-haven-hospital.jpg?quality=85)