A BROADER VIEWOF HEALTH: - UCLA School of Public Health
A BROADER VIEWOF HEALTH: - UCLA School of Public Health
A BROADER VIEWOF HEALTH: - UCLA School of Public Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
U C L A<br />
PUBLIC <strong>HEALTH</strong><br />
NOVEMBER 2010<br />
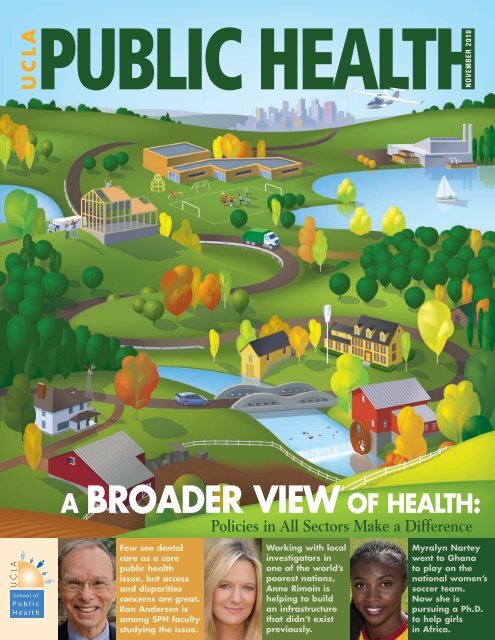
A <strong>BROADER</strong> VIEW OF <strong>HEALTH</strong>:<br />
Policies in All Sectors Make a Difference<br />
<strong>UCLA</strong><br />
<strong>School</strong> <strong>of</strong><br />
<strong>Public</strong><br />
<strong>Health</strong><br />
Few see dental<br />
care as a core<br />
public health<br />
issue, but access<br />
and disparities<br />
concerns are great.<br />
Ron Andersen is<br />
among SPH faculty<br />
studying the issue.<br />
Working with local<br />
investigators in<br />
one <strong>of</strong> the world’s<br />
poorest nations,<br />
Anne Rimoin is<br />
helping to build<br />
an infrastructure<br />
that didn’t exist<br />
previously.<br />
Myralyn Nartey<br />
went to Ghana<br />
to play on the<br />
national women’s<br />
soccer team.<br />
Now she is<br />
pursuing a Ph.D.<br />
to help girls<br />
in Africa.
PUBLIC <strong>HEALTH</strong><br />
<strong>UCLA</strong><br />
U C L A<br />
Gene Block, Ph.D.<br />
Chancellor<br />
Linda Rosenstock, M.D., M.P.H.<br />
Dean,<strong>UCLA</strong> <strong>School</strong><strong>of</strong><strong>Public</strong><strong>Health</strong><br />
Sarah Anderson<br />
AssistantDeanforCommunications<br />
John Sonego<br />
AssistantDeanforDevelopment<br />
andAlumniRelations<br />
Dan Gordon<br />
EditorandWriter<br />
Martha Widmann<br />
ArtDirector<br />
E D I TO R I A L B OA R D<br />
Richard Ambrose, Ph.D.<br />
Pr<strong>of</strong>essor,Environmental<strong>Health</strong>Sciences<br />
Roshan Bastani, Ph.D.<br />
Pr<strong>of</strong>essor,<strong>Health</strong>Services<br />
AssociateDeanforResearch<br />
Thomas R. Belin, Ph.D.<br />
Pr<strong>of</strong>essor,Biostatistics<br />
Pamina Gorbach, Dr.P.H.<br />
AssociatePr<strong>of</strong>essor,Epidemiology<br />
F. A. Hagigi, Dr.P.H., M.B.A.<br />
Pr<strong>of</strong>essor,<strong>Health</strong>Services<br />
Moira Inkelas, Ph.D.<br />
AssistantPr<strong>of</strong>essor,<strong>Health</strong>Services<br />
Richard Jackson, M.D., M.P.H.<br />
Pr<strong>of</strong>essorandChair,<br />
Environmental<strong>Health</strong>Sciences<br />
Michael Prelip, D.P.A.<br />
AssociatePr<strong>of</strong>essor,<br />
Community<strong>Health</strong>Sciences<br />
Andrew Tsui and Tarah Griep<br />
Co-Presidents,<strong>Public</strong><strong>Health</strong>StudentAssociation<br />
Christopher Mardesich, J.D., M.P.H. ’98<br />
President,AlumniAssociation<br />
features<br />
4<br />
WISDOM ON TEETH:<br />
A Growing Focus on<br />
Dental Care Needs<br />
Poor oral health has been called a “silent<br />
epidemic,” with disparities and access problems<br />
calling for more attention from public health.<br />
8<br />
ANNE RIMOIN:<br />
Bringing<br />
Emerging<br />
Diseases Above<br />
the Radar<br />
She is working with the<br />
Congolese to build a disease<br />
surveillance system that<br />
has already revealed the<br />
surprisingly dramatic growth<br />
<strong>of</strong> human monkeypox.<br />
1<br />
<strong>School</strong> <strong>of</strong><br />
<strong>Public</strong><br />
<strong>Health</strong>
A <strong>BROADER</strong><br />
VIEW OF<br />
<strong>HEALTH</strong>:<br />
Policies in<br />
All Sectors Make<br />
a Difference<br />
HIGHER<br />
EDUCATION:<br />
New Strategies for<br />
Promoting <strong>Health</strong><br />
in every issue<br />
0<br />
As momentum builds for considering the<br />
public health effects <strong>of</strong> decisions outside<br />
health’s traditional purview, SPH faculty<br />
are leading the way.<br />
16<br />
With the one-size-fits-all approach a distant<br />
memory, efforts to change health behaviors are<br />
relying on better-targeted messages delivered in<br />
proactive and innovative ways.<br />
23<br />
28<br />
30<br />
32<br />
RESEARCH<br />
Monkeypox rising in<br />
Africa…children not getting<br />
dental care…insurance<br />
inequities for same-sex<br />
couples…dangerous<br />
nanoparticles…home<br />
kitchens not making<br />
grade…centralized health<br />
care fares well.<br />
STUDENTS<br />
FACULTY<br />
NEWS BRIEFS<br />
ON THE COVER<br />
A broader view <strong>of</strong> health takes into account that policies in a wide variety <strong>of</strong> sectors can directly<br />
or indirectly influence the health <strong>of</strong> populations. Matt LeBarre © 2010<br />
PHOTOGRAPHY<br />
Reed Hutchinson / Cover: Nartey; pp. 28-29<br />
Sandra Shagat, <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> Dentistry / TOC: dentistry; p. 6<br />
Todd Cheney, AS<strong>UCLA</strong> / p. 7: Westwood Predoctoral Dental Clinic<br />
J. Rose Photography by Jessica Williams / p. 7: toothbrush learning station<br />
Matt LeBarre / Cover: Broader View; TOC: Broader View; pp. 11-12, 14-15<br />
Shoshee Jau, Daily Bruin / p. 32<br />
Courtesy <strong>of</strong> Anne Rimoin / Cover: Rimoin; TOC: Faculty Pr<strong>of</strong>ile; pp. 8, 23<br />
Courtesy <strong>of</strong> Beatriz Solis / p.16: Solis<br />
Courtesy <strong>of</strong> Philip Massey / pp. 16-17<br />
Courtesy <strong>of</strong> David Gere / TOC: Higher Education; pp. 18-19<br />
Courtesy <strong>of</strong> Antronette Yancey / p. 20<br />
Courtesy <strong>of</strong> Roshan Bastani / p. 21<br />
Courtesy <strong>of</strong> <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> / Cover: Andersen; TOC: Dentistry; p. 2; p. 4: Andersen; pp. 5-6;<br />
p. 7: dentist cleaning teeth; p. 10: Fielding; p. 11: Guerrero;<br />
p. 12: Jackson; p. 19: Yancey; pp. 31, 33; back cover<br />
iStockphoto © 2010 / Cover; p. 4: teeth; p. 22; pp. 25-26<br />
<strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> Home Page: www.ph.ucla.edu<br />
E-mail for Application Requests: info@ph.ucla.edu<br />
<strong>UCLA</strong> <strong>Public</strong> <strong>Health</strong> Magazine is published by the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> for the alumni, faculty,<br />
students, staff and friends <strong>of</strong> the school. Copyright 2010 by The Regents <strong>of</strong> the University <strong>of</strong> California.<br />
Permission to reprint any portion must be obtained from the editor. Contact Editor, <strong>UCLA</strong> <strong>Public</strong> <strong>Health</strong><br />
Magazine, Box 951772, Los Angeles, CA 90095-1772. Phone: (310) 825-6381.
2<br />
dean’s message<br />
PUBLIC <strong>HEALTH</strong> HAS LONG ESPOUSED the role <strong>of</strong> many factors<br />
– such as education, housing, employment and the environment – contributing<br />
to overall health status. There is a growing movement to take this broader view<br />
<strong>of</strong> health into all aspects <strong>of</strong> society. As a result, with leadership from several<br />
faculty members at our school, there is a push for policy and decision-makers<br />
to utilize the <strong>Health</strong> Impact Assessment (HIA) when making decisions in<br />
any sector.<br />
Our cover story takes a look at this innovative approach and how, in<br />
addition to our faculty, our students and alumni are working to encourage the<br />
use <strong>of</strong> HIA to evaluate objectively the potential health effects <strong>of</strong> a project<br />
(e.g., a light rail system) or policy (e.g., curbing diesel emissions) before it is<br />
built or implemented. They are applying one <strong>of</strong> the tenets <strong>of</strong> public health –<br />
prevention – not just to individual and community health, but to the policymaking<br />
process.<br />
We are also taking a broader view when it comes to global health. In<br />
addition to activities at the school, faculty and students in a number <strong>of</strong> <strong>UCLA</strong><br />
schools and colleges are participating in active global health programs. Crosscampus<br />
collaborations in global health are emerging, representing a new frontier<br />
<strong>of</strong> academic opportunity. In order to capitalize on this opportunity the campus<br />
is launching a <strong>UCLA</strong>-wide Global <strong>Health</strong> Initiative; I have been asked to chair<br />
the steering committee.<br />
To support the campus-wide effort, in which I expect our school to play a<br />
central role, and to further implement one <strong>of</strong> our school’s strategic goals to build<br />
a world-class global health presence, I am pleased to announce the appointment<br />
<strong>of</strong> Dr. Onyebuchi Arah, associate pr<strong>of</strong>essor in the Department <strong>of</strong> Epidemiology,<br />
as the first associate dean for global health. You can read more about Dr. Arah’s<br />
appointment on page 33.<br />
Finally, I’m pleased to share that we have an exciting year ahead <strong>of</strong> us.<br />
In 2011, the <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> celebrates its 50th. We plan to spend the<br />
year celebrating our past, present and future.<br />
Many <strong>of</strong> us have a vague recollection <strong>of</strong> what life was like in the early<br />
1960s, and for those who don’t, the TV show Mad Men reminds us <strong>of</strong> a few<br />
critical changes we’ve seen since the school was founded in 1961. Long gone<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
2 0 0 9 - 1 0 D E A N ’ S<br />
A DV I S O RY B OA R D<br />
3<br />
are the days <strong>of</strong> the three-martini lunch, smoke-filled <strong>of</strong>fice and advertising<br />
campaigns to convince smokers to keep on puffing. Fifty years ago cars were<br />
not required to have seat belts and the notion <strong>of</strong> a child restraint system was<br />
your mother’s arm flung across your chest. It would be 20 years until the first<br />
positive case <strong>of</strong> HIV/AIDS in the United States was reported to the Centers for<br />
Disease Control.<br />
It was into this environment that the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> was<br />
born. As part <strong>of</strong> an institution consistently rated among the top schools <strong>of</strong><br />
public health in the country, our faculty, students and alumni have led the way<br />
in improving the quality <strong>of</strong> life and longevity for people across the globe.<br />
I would like to personally invite all <strong>of</strong> you – our alumni, friends, faculty,<br />
staff and students – to join us in celebrating the enormous contribution we have<br />
made, as well as our potential for even greater contributions in the years ahead.<br />
Whether you join us online for our new webinar series (see page 32), join us<br />
at the 50th Anniversary Gala, or simply provide your updated information for<br />
the alumni directory, let us hear from you this year. You are the reason for our<br />
success, and the key to our ability to continue to make a difference in the health<br />
<strong>of</strong> populations locally and globally. Thank you for being part <strong>of</strong> something great.<br />
Ira R. Alpert *<br />
Lester Breslow<br />
Sanford R. Climan<br />
Edward A. Dauer<br />
Deborah Kazenelson Deane*<br />
Michele DiLorenzo<br />
Samuel Downing*<br />
Robert J. Drabkin<br />
Gerald Factor (Vice Chair)<br />
Jonathan Fielding<br />
Dean Hansell (Chair)<br />
Cindy Harrell Horn<br />
Stephen W. Kahane *<br />
Carolyn Katzin *<br />
Carolbeth Korn *<br />
Jacqueline B. Kosec<strong>of</strong>f<br />
Kenneth E. Lee *<br />
Edward J. O’Neill *<br />
Thomas Priselac<br />
Monica Salinas<br />
Fred W. Wasserman *<br />
Pamela K. Wasserman *<br />
Thomas Weinberger<br />
Cynthia Sikes Yorkin<br />
*SPH Alumni<br />
Linda Rosenstock, M.D., M.P.H.<br />
Dean<br />
TOTAL REVENUES<br />
Grants and Contracts<br />
State-Generated Funds<br />
Gifts and Other<br />
Fiscal Year 09-10<br />
$70.5 million<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
4<br />
POOR ORAL<br />
<strong>HEALTH</strong> HAS BEEN<br />
CALLED A “SILENT<br />
EPIDEMIC,” WITH<br />
DISPARITIES AND<br />
ACCESS PROBLEMS<br />
CALLING FOR MORE<br />
ATTENTION FROM<br />
PUBLIC <strong>HEALTH</strong>.<br />
WISDOM ON TEETH:<br />
A Growing Focus<br />
on Dental Care Needs<br />
Few public health issues have received<br />
more attention in recent years than lack <strong>of</strong> access to essential medical services<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
“Oral health<br />
issues fit so<br />
closely with<br />
public health’s<br />
mission, and<br />
through efforts<br />
aimed at prevention, education and<br />
addressing access issues, we have<br />
the potential to get more in return<br />
from our investment than from<br />
many other investments.”<br />
—Dr. Ronald Andersen<br />
and its disproportionate effect on certain population groups. Meanwhile, a parallel<br />
issue has gone relatively unnoticed.<br />
“Access problems appear to be considerably greater with respect to oral<br />
health services than general health services, and the disparities by income and<br />
minority status are probably larger,” says Dr. Ronald Andersen, pr<strong>of</strong>essor <strong>of</strong> health<br />
services at the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>. “But because dental care isn’t<br />
associated with saving lives, it hasn’t been emphasized in public health to the<br />
extent that it should be.”<br />
Overall, oral health has improved dramatically in the United States over<br />
the last half-century, thanks in part to public health efforts such as fluoridation<br />
<strong>of</strong> drinking water and education about the benefits <strong>of</strong> fluoride toothpaste. It<br />
wasn’t long ago that the majority <strong>of</strong> Americans lost their teeth by middle age;<br />
today, most can expect to retain their natural teeth over their lifetimes.<br />
But there is significant cause for concern. A decade ago, in the first-ever<br />
Surgeon General’s report on oral health, Dr. David Satcher pointed to a “silent<br />
epidemic” <strong>of</strong> dental and oral diseases with “pr<strong>of</strong>ound disparities that affect those<br />
without the knowledge or resources to achieve good oral care.” In addition,<br />
although dental care might not seem as critical as medical care, poor oral health<br />
can cause significant problems…and can be related to health ailments outside
the mouth. Untreated, tooth decay (cavities) – the<br />
most common chronic disease in children – can<br />
cause everything from pain and difficulty eating to<br />
lost school and work time. Serious oral disorders can<br />
undermine self-esteem, inhibiting children and adults<br />
from smiling. Gum disease has recently been linked<br />
in studies to increased risk for diabetes, heart disease<br />
and stroke.<br />
And while much attention has been paid to<br />
the problem <strong>of</strong> lack <strong>of</strong> health insurance, the fact<br />
that even more are without dental coverage is <strong>of</strong>ten<br />
overlooked. Although public insurance programs<br />
such as Medicaid have increased coverage for children,<br />
dental benefits tend to be vulnerable to cuts in<br />
tough economic times. By the same token, for many<br />
low-income families struggling financially and, in<br />
some cases, lacking education about the importance<br />
<strong>of</strong> regular dental visits, dental care may be viewed<br />
as optional.<br />
“Oral health issues fit so closely with public<br />
health’s mission,” observes Andersen, “and through<br />
efforts aimed at prevention, education and addressing<br />
access issues, we have the potential to get more in<br />
return from our investment than from many other<br />
investments.”<br />
Dental public health issues haven’t been ignored<br />
at <strong>UCLA</strong>, where faculty in the <strong>School</strong> <strong>of</strong> <strong>Public</strong><br />
<strong>Health</strong> and <strong>School</strong> <strong>of</strong> Dentistry have worked – <strong>of</strong>ten<br />
together – to address some <strong>of</strong> the major concerns.<br />
One <strong>of</strong> the key efforts began in 2001 when The<br />
Robert Wood Johnson Foundation provided funding<br />
for a national demonstration program aiming to<br />
reduce dental-care access disparities. Fifteen dental<br />
schools were selected to participate in the Dental<br />
Pipeline Program, which would receive additional<br />
funding from The California Endowment. The<br />
program’s national evaluation team was based in the<br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>, with Andersen as<br />
the principal investigator and Dr. Pamela Davidson,<br />
associate pr<strong>of</strong>essor <strong>of</strong> health services at the school,<br />
as co-principal investigator. (The original project<br />
ended in 2007, but a follow-up study to measure its<br />
sustainability is ongoing.)<br />
The pipeline program was established in an<br />
effort to increase access to dental care in low-income<br />
and minority communities by recruiting more students<br />
from underrepresented minority groups to<br />
dental schools, improving dental school curricula to<br />
better prepare students to provide culturally competent<br />
care, and providing more clinical practice experiences<br />
for students in underserved communities.<br />
“If you look at the ethnicity <strong>of</strong> dentists compared to<br />
the distribution <strong>of</strong> the population, there are greater<br />
differences than in medicine,” Andersen notes. That<br />
has contributed in part to the shortage <strong>of</strong> oral health<br />
providers in minority communities, he says.<br />
Dental schools have faced significant challenges<br />
in their efforts to recruit minority students into<br />
dental careers, Andersen notes. For one, the shortage<br />
<strong>of</strong> providers in minority communities means there<br />
are few family members or friends serving as role<br />
models and mentors. Nonetheless, through steppedup<br />
efforts, including the establishment <strong>of</strong> pre-dental<br />
programs to assist students in meeting prerequisites,<br />
the pipeline program schools increased applications<br />
from underrepresented minority students by 77<br />
percent from 2003 to 2007, while enrollment <strong>of</strong><br />
underrepresented minority students increased by<br />
27 percent.<br />
Beyond the effort to increase the number <strong>of</strong><br />
minority dental providers, the pipeline program<br />
sought to revamp education and training experiences<br />
that would make all students more likely to consider<br />
careers in public health and service to underserved<br />
communities. While curricula were revised and the<br />
number <strong>of</strong> days senior dental students practiced<br />
in underserved communities increased, it’s unclear<br />
whether there was a corresponding increase in graduates<br />
going on to practice in these communities.<br />
Unfortunately, Andersen notes, dental students tend<br />
to enter practice with huge debts; thus, many who<br />
want to go into public service positions are deterred<br />
by the lower salaries and instead feel compelled to<br />
opt for private practice.<br />
The problem <strong>of</strong> disparities in utilization <strong>of</strong> dental<br />
services – particularly among children – is underscored<br />
by a recent study conducted by Dr. Nadereh<br />
Pourat, pr<strong>of</strong>essor <strong>of</strong> health services and director <strong>of</strong><br />
research for the Center for <strong>Health</strong> Policy Research,<br />
which is based in the school. Using data from the<br />
2005 California <strong>Health</strong> Interview Survey, Pourat<br />
found that nearly 25 percent <strong>of</strong> California children<br />
ages 11 and under had never seen a dentist, and<br />
that among those who had, there were significant<br />
differences by race, ethnicity and type <strong>of</strong> insurance<br />
in the amount <strong>of</strong> time between dental care visits<br />
(see page 24).<br />
Having any kind <strong>of</strong> insurance significantly<br />
increased the odds that a child would see a dentist<br />
on a regular basis, but the type <strong>of</strong> coverage mattered:<br />
54 percent <strong>of</strong> privately insured children had seen<br />
a dentist within the previous six months, vs. 27<br />
percent <strong>of</strong> publicly insured children (Medicaid or<br />
the Children’s <strong>Health</strong> Insurance Program) and 12<br />
“<strong>Public</strong> programs<br />
are designed to<br />
improve access<br />
to care for<br />
underserved<br />
populations,<br />
and our study<br />
shows that they<br />
are successful<br />
in doing so.<br />
However,<br />
they don’t close<br />
the gap.”<br />
—Dr. Nadereh Pourat<br />
5<br />
feature <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
6<br />
An analysis <strong>of</strong> children<br />
who suffer the most from<br />
dental disease suggests<br />
it’s not only children<br />
from low-income families<br />
and underserved minority<br />
groups, but also those<br />
from families with<br />
what is referred to as<br />
low oral health literacy.<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
percent <strong>of</strong> children without any coverage. Even<br />
when taking into account only those with public<br />
insurance coverage, though, the study found that<br />
Latino and African-American children went to<br />
the dentist significantly less <strong>of</strong>ten than white and<br />
Asian-American children.<br />
“<strong>Public</strong> programs are designed to improve access<br />
to care for underserved populations, and our study<br />
shows that they are successful in doing so,” Pourat<br />
says. “However, they don’t close the gap. There is<br />
more work to do in addressing disparities in dental<br />
care for children.”<br />
Pourat suspects a key factor in the persistence<br />
<strong>of</strong> these disparities is that public insurance programs<br />
reimburse dentists at a lower level than private<br />
insurance. Unlike medical care, in which managed<br />
care and group practices encourage more providers<br />
to see patients in public programs, dental care is<br />
dominated by solo practitioners in private <strong>of</strong>fices –<br />
many <strong>of</strong> whom don’t see patients with public<br />
insurance. A study conducted by Pourat and colleagues<br />
in 2003 found that only about 40 percent<br />
<strong>of</strong> California dentists accepted public-insurance<br />
patients. Coupled with the general shortage <strong>of</strong><br />
providers in low-income communities, this has<br />
posed a major barrier, and may be the reason many<br />
families choose to forgo care. Pourat has begun a<br />
new study, funded by the National Institute <strong>of</strong><br />
Dental and Crani<strong>of</strong>acial Research, to examine the<br />
impact <strong>of</strong> the local supply <strong>of</strong> oral health providers<br />
on access to care.<br />
Addressing reimbursement inequities is one<br />
<strong>of</strong> several potential solutions that Pourat and others<br />
have proposed. Another is to strengthen the safety-<br />
net system by broadening the types <strong>of</strong> dental<br />
providers – including preparing other licensed pr<strong>of</strong>essionals,<br />
such as hygienists, who can deliver primary<br />
pediatric dental care. Pourat notes that many general<br />
dentists are uncomfortable delivering care to very<br />
young children, an issue that could be addressed in<br />
dental school training with more clinical experiences<br />
involving young patients.<br />
Pourat believes more education is needed for<br />
all families about the importance <strong>of</strong> dental visits<br />
and preventive oral health care in childhood. “Many<br />
parents figure it’s not that important because their<br />
children are going to lose their primary teeth anyway,”<br />
she says. “But the reality is that when you<br />
have a poor oral health environment, the problems<br />
are likely to continue when the secondary teeth<br />
come in. Teaching children good oral hygiene can<br />
have a major impact on their oral health as adults.”<br />
An analysis <strong>of</strong> children who suffer the most from<br />
dental disease suggests it’s not only children from<br />
low-income families and underserved minority<br />
groups, but also those from families with what is<br />
referred to as low oral health literacy, says Dr. James<br />
Crall, pr<strong>of</strong>essor and chair <strong>of</strong> pediatric dentistry in<br />
the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> Dentistry and a faculty member<br />
in the <strong>UCLA</strong> Center for <strong>Health</strong>ier Children, Families<br />
and Communities, based in the <strong>School</strong> <strong>of</strong> <strong>Public</strong><br />
<strong>Health</strong>. “There are issues <strong>of</strong> culture, language, nutrition<br />
and use <strong>of</strong> health services that are amenable to<br />
public health as well as primary care approaches,”<br />
he explains.<br />
Crall has been a leader in dental public health<br />
for more than a decade. In 1997 he was appointed<br />
the first dental scholar-in-residence at the Agency for
<strong>Health</strong> Care Policy and Research and he has been actively involved in national,<br />
state and pr<strong>of</strong>essional oral health policy development ever since. From 2000<br />
to 2008 he was director <strong>of</strong> the <strong>Health</strong> Resources and Services Administration/<br />
Maternal and Child <strong>Health</strong> Bureau National Oral <strong>Health</strong> Policy Center, colocated<br />
within the Center for <strong>Health</strong>ier Children, Families and Communities.<br />
Crall also directs a pediatric dentistry leadership training program in collaboration<br />
with other members <strong>of</strong> the center’s faculty. Since 2007 he has been project<br />
director <strong>of</strong> the American Academy <strong>of</strong> Pediatric Dentistry’s Head Start Dental<br />
Home Initiative, which is building networks <strong>of</strong> providers in every state to<br />
improve access to dental services for children in Head Start programs.<br />
Crall, who was part <strong>of</strong> Andersen’s national evaluation team for the Dental<br />
Pipeline Program, believes public health efforts to address the current challenges<br />
in oral health require a combination <strong>of</strong> innovative training initiatives and community<br />
programs, along with policies that effect change in the practice environment,<br />
such as increased reimbursement and other incentives to work with underserved<br />
populations.<br />
The subspecialty area <strong>of</strong> dental public health is small, Crall notes; it will<br />
take more than dentists to make a difference. “We need to encourage more dentists<br />
to go into public health, but we also must find ways to foster collaborations<br />
with non-dentists in public health and medicine,” he says. “That’s now occurring<br />
at <strong>UCLA</strong> in a way that we haven’t seen before, and it’s a goal that has gained<br />
increasing recognition at the national level.”<br />
M.P.H. Degree Informs Her Effort to<br />
Organize American Indian Dentists<br />
Nowhere are oral health problems more severe than among American Indians. The last<br />
survey by the Indian <strong>Health</strong> Service (IHS), published in 1999, found that 87 percent <strong>of</strong><br />
American Indian children ages 6-14 and 91 percent <strong>of</strong> 15-19 year olds had a history <strong>of</strong><br />
tooth decay. Seventy-eight percent <strong>of</strong> adults ages 35-44 and 98 percent <strong>of</strong> those 55 and<br />
older had lost at least one tooth because <strong>of</strong> dental decay, gum disease or oral trauma.<br />
Dr. Ruth Bol (M.P.H. ’09), a pediatric dentist in private practice in Menifee, Calif.,<br />
who is herself American Indian, is drawing on her <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
education to organize American Indian dentists in response to the problem. Bol worked<br />
four years with the IHS (part <strong>of</strong> the U.S. <strong>Public</strong> <strong>Health</strong> Service) and became frustrated<br />
with the lack <strong>of</strong> leadership, which she believed had much to do with the scarcity <strong>of</strong><br />
American Indians among the dentists practicing on the reservations.<br />
So she worked her way up the ranks <strong>of</strong> the Society <strong>of</strong> American Indian Dentists<br />
(Bol is currently vice president), was elected to the California Dental Association board<br />
<strong>of</strong> directors and became active in the American Dental Association. Realizing the value<br />
a public health education could bring, Bol enrolled at <strong>UCLA</strong> for both her pediatric dentistry<br />
residency and M.P.H. from the <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>. With a grant she wrote in one <strong>of</strong><br />
her <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> courses, Bol secured funding from Delta Dental <strong>of</strong> California<br />
to support the Society <strong>of</strong> American Indian Dentists’ efforts to mentor American Indians<br />
before, during and after dental school. She is currently meeting with other potential<br />
funders.<br />
“The more I got involved with these big-picture issues, the more I realized there<br />
was a lot I didn’t know,” Bol says. “Getting the M.P.H. has given me credibility as well<br />
as knowledge on everything from developing and evaluating programs to writing grants.<br />
It’s provided me with the tools to work with underserved communities.”<br />
Ruth Bol, D.D.S. M.P.H. ’09<br />
7<br />
feature <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
8<br />
SHE IS<br />
WORKING WITH<br />
THE CONGOLESE<br />
TO BUILD A<br />
DISEASE<br />
SURVEILLANCE<br />
SYSTEM THAT<br />
HAS ALREADY<br />
REVEALED THE<br />
SURPRISINGLY<br />
DRAMATIC GROWTH<br />
OF HUMAN<br />
MONKEYPOX.<br />
ANNE RIMOIN:<br />
Bringing Emerging Diseases<br />
Above the Radar<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
Although her specific focus is studying the epidemiology <strong>of</strong> human<br />
monkeypox in the Democratic Republic <strong>of</strong> the Congo (DRC), Dr. Anne Rimoin also has an eye on the<br />
bigger picture: working with the Congolese government and local investigators to develop an infrastructure<br />
that will enable the Central African nation to conduct proper surveillance <strong>of</strong> all emerging infectious diseases.<br />
“To me, if you’re a researcher working in a low-resource setting, you have a moral obligation not just to<br />
collect your data and leave, but to build capacity and collaborate with the people who, by their good graces,<br />
are allowing you to do this work in their country,” she says.<br />
Over the last six years, Rimoin, assistant pr<strong>of</strong>essor <strong>of</strong> epidemiology at the school, has established a<br />
research site in central DRC that now serves as headquarters for a variety <strong>of</strong> studies <strong>of</strong> cross-species transmission<br />
<strong>of</strong> disease. Heading an all-Congolese team, Rimoin collaborates closely with the DRC Ministry <strong>of</strong><br />
<strong>Health</strong>, the Kinshasa <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> and the National Laboratory to improve disease surveillance<br />
capacity in a nation that is one <strong>of</strong> the world’s poorest, and has been devastated by civil war. “There is a long<br />
way to go – what we’ve done so far represents just a drop in the bucket – but I’m pleased just to be able<br />
to contribute as I can,” Rimoin says.<br />
Already, though, Rimoin and her Congolese collaborators have produced tangible evidence <strong>of</strong> the<br />
critical nature <strong>of</strong> building a disease surveillance infrastructure. In August, they published the first results<br />
<strong>of</strong> their human monkeypox study in the Proceedings <strong>of</strong> the National Academy <strong>of</strong> Science, showing that rates<br />
<strong>of</strong> the disease had increased by an astounding 20-fold in the DRC since 1980.
Ironically, Rimoin’s group noted, one <strong>of</strong> public<br />
health’s greatest success stories opened the door for<br />
the dramatic increase. The eradication <strong>of</strong> smallpox,<br />
announced in 1980, spelled the end <strong>of</strong> a vaccination<br />
program that had also provided protective immunity<br />
against monkeypox, a related virus believed to be<br />
carried primarily by squirrels and other rodents.<br />
(Although generally less lethal than smallpox,<br />
monkeypox can cause serious symptoms, including<br />
severe eruptions on the skin, fever, headaches,<br />
swollen lymph nodes and, in some cases, blindness<br />
and death.) Particularly in rural areas, where displaced<br />
populations rely to a greater extent on bushmeat, the<br />
growing number <strong>of</strong> unvaccinated individuals over<br />
time led to a gradual increase in the rate <strong>of</strong> infection.<br />
But in the absence <strong>of</strong> any surveillance, Rimoin notes,<br />
monkeypox “fell under the radar.” (For more on the<br />
study, see page 23.)<br />
Growing up in Los Angeles, Rimoin always had<br />
positive associations with Africa. In a home adorned<br />
with African art, her father would recall fondly his<br />
research experiences working with a Pygmy population<br />
in the Central African Republic. At Middlebury<br />
College in Vermont, Rimoin earned her undergraduate<br />
degree in African History. It was only after graduating<br />
and going into the Peace Corps that she became<br />
interested in science, and particularly epidemiology.<br />
In Benin, West Africa, Rimoin spent two years as a<br />
volunteer coordinator for the guinea worm eradication<br />
effort. “It was a perfect public health program<br />
that taught me to do disease surveillance,” she says.<br />
“It really brought home the importance <strong>of</strong> using<br />
basic epidemiologic methods to solve a problem.”<br />
Upon completing the program, Rimoin enrolled<br />
at the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>, where she<br />
received her M.P.H. in 1996. For her internship<br />
she worked in Nepal doing disease surveillance for<br />
the World <strong>Health</strong> Organization’s polio eradication<br />
program. Rimoin was then hired by the WHO as a<br />
logistics <strong>of</strong>ficer, assisting in the expanded polio surveillance<br />
and eradication program in Ethiopia and<br />
Eretria. She also initiated a collaborative relationship<br />
between the WHO and the Peace Corps, including<br />
development <strong>of</strong> a program and training materials for<br />
health-oriented Peace Corps volunteers to carry out<br />
disease surveillance activities in Africa and Nepal.<br />
After completing her Ph.D. at the Johns Hopkins<br />
Bloomberg <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> in 2003, Rimoin<br />
worked as a program scientist for the National<br />
Institute <strong>of</strong> Child <strong>Health</strong> and Human Development,<br />
coordinating clinical studies in Africa. While at a<br />
meeting at the DRC Ministry <strong>of</strong> <strong>Health</strong>, she was<br />
part <strong>of</strong> a discussion in which it was noted that there<br />
had been an increase in reported cases <strong>of</strong> human<br />
monkeypox in the country. Rimoin’s interest was<br />
piqued. “It made sense to me that given the lack<br />
<strong>of</strong> infrastructure and absence <strong>of</strong> disease surveillance,<br />
if there were any significant reports <strong>of</strong> monkeypox<br />
out there it was likely a much bigger problem than<br />
anyone was anticipating,” she says. Rimoin promptly<br />
proposed to head the first epidemiologic study<br />
assessing the burden <strong>of</strong> human monkeypox in<br />
DRC, and received funding to begin setting up<br />
her program in 2004.<br />
Ever since, Rimoin and her team have been training<br />
local health workers in identifying and reporting<br />
cases as well as interviewing monkeypox patients to<br />
learn about their potential exposures. The workers<br />
collect biological samples that are transported to the<br />
project’s field station and then to Kinshasa, as well<br />
as to collaborators in the United States who conduct<br />
laboratory analyses and report back to the Congolese<br />
field workers.<br />
One reason the DRC was in such dire need<br />
<strong>of</strong> a disease surveillance program is that there are<br />
tremendous logistical challenges to implementing<br />
one. From the beginning, Rimoin’s team has faced<br />
problems such as how to collect and preserve biological<br />
specimens in settings that <strong>of</strong>ten lacked electricity,<br />
running water and refrigeration sources. A<br />
country <strong>of</strong> 900,000 square kilometers has only about<br />
300 kilometers worth <strong>of</strong> roads. Given the expense<br />
<strong>of</strong> gasoline and the DRC’s scarce economic resources,<br />
cost is never far from Rimoin’s mind. “Our supervisors<br />
have motorcycles, but for day-to-day surveillance<br />
we give our health care workers bicycles so they can<br />
take supplies from the headquarters to their village,”<br />
she says. “That can be as many as 200-300 kilometers<br />
away, but it’s a sustainable approach.”<br />
At the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>, where<br />
she has been a member <strong>of</strong> the faculty since 2004,<br />
Rimoin teaches her students the importance <strong>of</strong><br />
working with local collaborators, understanding the<br />
socio-cultural and political context in which problems<br />
occur, and designing and implementing interventions<br />
that are practical and feasible, particularly in lowresource<br />
settings. “Emerging infectious diseases are<br />
definitely out there,” she says. “You just need to<br />
identify the populations at the highest risk and<br />
make sure you’re asking the right questions or you’re<br />
going to miss important events that signal the early<br />
emergence <strong>of</strong> a disease.”<br />
Rimoin, who spends roughly a third <strong>of</strong> her time<br />
working in the field in the DRC, is committed to<br />
being there for the long haul. “My goal is sustainable<br />
research,” she says. “I am fully invested in my work<br />
in the DRC and intend to have a long relationship<br />
with my Congolese collaborators.”<br />
“It made<br />
sense to me<br />
that given<br />
the lack <strong>of</strong><br />
infrastructure<br />
and absence<br />
<strong>of</strong> disease<br />
surveillance,<br />
if there were<br />
any significant<br />
reports <strong>of</strong><br />
monkeypox<br />
out there it<br />
was likely a<br />
much bigger<br />
problem than<br />
anyone was<br />
anticipating.”<br />
—Dr. Anne Rimoin<br />
9<br />
faculty pr<strong>of</strong>ile <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
10<br />
A <strong>BROADER</strong><br />
Policies in All Sectors<br />
Make a Difference<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
AS MOMENTUM<br />
BUILDS FOR<br />
CONSIDERING THE<br />
PUBLIC <strong>HEALTH</strong><br />
EFFECTS OF<br />
DECISIONS<br />
OUTSIDE <strong>HEALTH</strong>’S<br />
TRADITIONAL<br />
PURVIEW, SPH<br />
FACULTY ARE<br />
LEADING THE WAY.<br />
Although the details were much debated during the<br />
year-long politicking over health care reform, no one would disagree that there<br />
were major health implications to the bills under consideration – and ultimately<br />
to the law passed in Congress and signed by President Obama last March.<br />
But what about debates over alternative energy, agricultural subsidies, and<br />
even extending the Bush tax cuts? Few would call these health issues…yet their<br />
potential impact on health is pr<strong>of</strong>ound. Similarly, it might seem outside <strong>of</strong><br />
health’s purview when municipalities consider mass-transit systems or major<br />
commercial developments – but whether an urban environment is conducive to<br />
safely walking and biking can go a long way toward determining the health <strong>of</strong> the<br />
local population. When public schools face massive budget reductions there is<br />
concern, rightfully, about the effects on education. But this, too, is a health issue:<br />
With physical education and other health-promoting school programs becoming<br />
vulnerable, those reductions ultimately affect obesity and children’s health. And<br />
formal education is a major determinant <strong>of</strong> longevity.<br />
Dr. Jonathan Fielding, pr<strong>of</strong>essor <strong>of</strong> health services at the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong><br />
<strong>Public</strong> <strong>Health</strong> and director <strong>of</strong> the Los Angeles County Department <strong>of</strong> <strong>Public</strong><br />
<strong>Health</strong>, is among the leaders <strong>of</strong> a growing movement to consider health impacts<br />
across a wider range <strong>of</strong> societal discussions – a movement known as <strong>Health</strong> in<br />
All Policies. “If you look at what determines health in populations, as well as<br />
disparities in health between communities, to a considerable extent it has to do<br />
with the social and physical environment – the societal underpinnings that are<br />
typically considered issues <strong>of</strong> economic development, education, transportation<br />
and housing, to name a few, but not health issues,” Fielding says.<br />
But Fielding concluded long ago that even prevention-oriented strategies by<br />
health departments to reduce health risk factors – though <strong>of</strong> great importance –<br />
fail to address major conditions that affect health in less-than-obvious ways.<br />
“We’ve gotten too used to segregating issues by sector,” he says. “We have to do<br />
a better job crossing over and working with people in other sectors to help them<br />
understand the effects <strong>of</strong> their decisions – whether it’s decisions on subsidizing<br />
high-fructose corn syrup production or decisions on how much is invested in the
11<br />
<strong>VIEWOF</strong> <strong>HEALTH</strong>:<br />
highway system as opposed to bikeable and walkable<br />
cities and mass transit-oriented development.”<br />
In the same way that <strong>Health</strong> in All Policies<br />
requires educating leaders in non-health agencies<br />
about the health consequences <strong>of</strong> decisions, it also<br />
calls for more broadly trained public health pr<strong>of</strong>essionals,<br />
contends Dr. Richard Jackson, chair and<br />
pr<strong>of</strong>essor <strong>of</strong> environmental health sciences at the<br />
school and, like Fielding, a national leader in promoting<br />
the <strong>Health</strong> in All Policies concept. “It’s clear<br />
that if you’re graduating from a school <strong>of</strong> public<br />
health, you should have at least a basic familiarity<br />
with issues such as housing, engineering and economics,”<br />
says Jackson, who has served as California’s<br />
state health <strong>of</strong>ficer and as director <strong>of</strong> the National<br />
Center for Environmental <strong>Health</strong>, part <strong>of</strong> the U.S.<br />
Centers for Disease Control and Prevention.<br />
With passage <strong>of</strong> health care reform earlier<br />
this year came tangible evidence that the voices <strong>of</strong><br />
Fielding, Jackson and other public health leaders<br />
at <strong>UCLA</strong> and elsewhere are being heard when it<br />
comes to their argument that health impacts should<br />
be considered in a broader array <strong>of</strong> policy decisions.<br />
The law created the National Prevention, <strong>Health</strong><br />
Promotion, and <strong>Public</strong> <strong>Health</strong> Council, composed<br />
<strong>of</strong> top government <strong>of</strong>ficials, to elevate and coordinate<br />
prevention activities and design a national<br />
prevention and health promotion strategy in conjunction<br />
with communities across the country.<br />
Chaired by the U.S. surgeon general, it includes<br />
the secretaries <strong>of</strong> Agriculture, Labor, <strong>Health</strong> and<br />
Human Services, Education, and Homeland Security;<br />
the administrator <strong>of</strong> the Environmental Protection<br />
Agency; the chair <strong>of</strong> the Federal Trade Commission;<br />
and the director <strong>of</strong> the National Drug Control<br />
Policy, among others.<br />
The movement is catching on at the state<br />
and local levels as well. In California, the state<br />
health department has established a <strong>Health</strong> in All<br />
Policies Task Force as part <strong>of</strong> the governor’s Strategic<br />
Growth Council. In Los Angeles County, Fielding’s<br />
department conducted a health impact assessment<br />
outlining the potential benefits <strong>of</strong> a proposed<br />
restaurant nutritional menu-labeling law in addressing<br />
the obesity epidemic. The assessment is believed<br />
to have played a key role in the passage <strong>of</strong><br />
California’s first-in-the-nation menu-labeling law<br />
in 2008, which in turn led to the inclusion <strong>of</strong><br />
menu labeling in the federal health reform law.<br />
When public schools face<br />
budget reductions, it’s also<br />
a health issue: Physical education<br />
is jeopardized, and formal education<br />
is related to longevity.<br />
cover story <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
12<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
“If you look<br />
at what<br />
determines health<br />
in populations,<br />
to a considerable<br />
extent it has<br />
to do with<br />
the societal<br />
underpinnings<br />
that are typically<br />
considered<br />
issues <strong>of</strong><br />
economic<br />
development,<br />
education,<br />
transportation<br />
and housing,<br />
to name a few,<br />
but not health<br />
issues.”<br />
—Dr. Jonathan Fielding<br />
The idea <strong>of</strong> viewing health more broadly isn’t<br />
new – in fact, Fielding notes, in some ways <strong>Health</strong><br />
in All Policies harkens back to an earlier time for<br />
the public health field. “You would see health effects<br />
<strong>of</strong> malnutrition, or <strong>of</strong> poor housing and inadequate<br />
sanitation, and the effects <strong>of</strong> investments in other<br />
sectors on health and health disparities were obvious,”<br />
he says. The United States fell behind other<br />
parts <strong>of</strong> the developed world – particularly Europe,<br />
which has used the health impact assessment (HIA)<br />
as a widespread policy-making tool for some time.<br />
But in the last decade, the concept has gained<br />
momentum – with the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong><br />
<strong>Health</strong> playing an important leadership role.<br />
Jackson, while serving as the director <strong>of</strong> CDC’s<br />
environmental health center in the late 1990s, was<br />
among the first to advocate for including assessment<br />
<strong>of</strong> health impact in major policy deliberations.<br />
He notes that since passage <strong>of</strong> the National<br />
Environmental Policy Act in 1969, major federal<br />
projects have required environmental impact<br />
assessments; at the state level, the California<br />
Environmental Quality Act passed the following<br />
year, requiring environmental impact reports for<br />
projects with potentially significant environmental<br />
effects. Although the environmental studies that take<br />
place as part <strong>of</strong> the state and federal mandates <strong>of</strong>ten<br />
give a nod toward health impacts, thorough public<br />
health assessments for proposed policies are rare.<br />
As a result, “you can have a significant project that’s<br />
outlining what will happen to endangered species<br />
but <strong>of</strong>fering little analysis <strong>of</strong> what happens to<br />
children, old people, poor people and everyone<br />
Transportation<br />
safety issues are also<br />
community health issues:<br />
Airports present<br />
potential noise and air<br />
quality concerns for the<br />
local population.<br />
in between,” says Jackson, who is currently chairing<br />
an Institute <strong>of</strong> Medicine committee, “A Framework<br />
and Guidance for <strong>Health</strong> Impact Assessment,” on<br />
which Fielding also serves.<br />
Recent U.S. history is replete with examples <strong>of</strong><br />
major undertakings that would have benefited from<br />
advance consideration <strong>of</strong> health impacts, Jackson<br />
says, starting with the Interstate Highway System,<br />
an enormous expenditure undertaken by the federal<br />
government in the 1950s. “We know the built environment<br />
has major health impacts, from respiratory<br />
diseases and injuries to obesity and many other<br />
chronic diseases,” he says, “and yet transportation and<br />
other sister agencies are scarcely aware <strong>of</strong> them.”<br />
In 2001, Fielding brought together a group <strong>of</strong><br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> faculty to begin a<br />
joint endeavor with the Washington, D.C.-based<br />
Partnership for Prevention. With support from the<br />
Robert Wood Johnson Foundation, the <strong>UCLA</strong> <strong>Health</strong><br />
Impact Assessment Project aimed to assess the<br />
feasibility <strong>of</strong> HIAs and develop prototypes, applied<br />
to specific policies. Starting by evaluating the health<br />
impacts on the Los Angeles City Living Wage<br />
Ordinance, the group crossed traditional boundaries<br />
within public health as well as seeking out<br />
researchers in other fields. “With a lot <strong>of</strong> these issues,<br />
we don’t start with inherent expertise in the subject<br />
matter,” Fielding explains. “We need to partner with<br />
experts from other fields and use resources from<br />
other disciplines to determine how changes in different<br />
sectors positively or negatively affect health.”<br />
While the HIA tradition in Europe had emphasized<br />
bringing stakeholder communities into the<br />
process <strong>of</strong> decisions with potential health consequences,<br />
the <strong>UCLA</strong> team developed methods that<br />
are more quantitative. “We wanted to show through
<strong>Health</strong> Impact Assessment <strong>of</strong> Santa Monica Airport Teaches<br />
<strong>UCLA</strong> Pediatric Residents to Broaden View <strong>of</strong> Physician’s Role<br />
For the pediatric residents training at Ronald Reagan<br />
<strong>UCLA</strong> Medical Center, it was an unusual project – but one<br />
that reflects a recognition that social and environmental<br />
conditions are every bit as important to children’s health<br />
as what occurs in a clinical setting.<br />
In response to concerns from members <strong>of</strong> the community<br />
surrounding Santa Monica Airport, the 10 pediatric<br />
residents – part <strong>of</strong> the <strong>UCLA</strong> Community <strong>Health</strong> and<br />
Community leaders meet with <strong>of</strong>ficials to discuss concerns<br />
about potential health impacts from Santa Monica Airport.<br />
Advocacy Training (CHAT) program – conducted a health<br />
impact assessment (HIA) <strong>of</strong> the Santa Monica Airport to<br />
organize, analyze and summarize existing information on<br />
the potential health impacts <strong>of</strong> the airport’s activity related<br />
to three issues: air quality, noise and the lack <strong>of</strong> an airport<br />
buffer zone.<br />
“Pediatricians increasingly recognize that environmental<br />
health is actually closer to pediatrics than it is to<br />
adult medicine, and that we need to set environmental<br />
standards to protect kids because their exposures are<br />
much higher per pound <strong>of</strong> body weight than adults,” says<br />
Dr. Richard Jackson, chair and pr<strong>of</strong>essor <strong>of</strong> environmental<br />
health sciences at the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> and<br />
a pediatrician who has specialized in the issue <strong>of</strong> children<br />
and environmental health. Jackson, who was brought in<br />
to teach part <strong>of</strong> the course, is also a longtime proponent<br />
<strong>of</strong> the need to assess proactively the impacts on health<br />
<strong>of</strong> transportation, construction, and other major decisions.<br />
The residents conducted what’s known as a rapid<br />
non-participatory HIA over two weeks last February.<br />
Their analysis was based on reviews <strong>of</strong> relevant scientific<br />
publications; regulations and guidance relevant to airport<br />
planning and health; input from expert consultants; public<br />
comment and testimony; and participation in community<br />
forums and meetings. The group concluded, among other<br />
things, that there has been a rise in the number <strong>of</strong> jet<br />
plane operations in recent decades, potentially increasing<br />
the air and noise pollution exposure in the surrounding<br />
area. The report noted that the airport’s proximity to<br />
schools, daycare centers, parks and residential homes<br />
may pose certain health risks for children and families<br />
living in the nearby community. The HIA <strong>of</strong>fered recommendations<br />
for mitigating the potentially adverse health<br />
impacts.<br />
Whether the recommendations are acted on remains<br />
to be seen, but the effort did not go unnoticed. “It had a<br />
huge political impact,” says Ping Ho (M.P.H. ’05), a Santa<br />
Monica resident who is a member <strong>of</strong> Concerned Residents<br />
Against Airport Pollution and Friends <strong>of</strong> Sunset Park<br />
Airport Committee, two grassroots groups that have<br />
lobbied the City <strong>of</strong> Santa Monica and airport <strong>of</strong>ficials on<br />
airport-related concerns. “They showed the community<br />
and our elected <strong>of</strong>ficials that the problem is <strong>of</strong> concern to<br />
front-line medical pr<strong>of</strong>essionals, and their summary made<br />
it clear that there is sufficient science to justify the concerns<br />
<strong>of</strong> the community.” Drawing on her own education<br />
in the school’s M.P.H. for <strong>Health</strong> Pr<strong>of</strong>essionals Program<br />
in Community <strong>Health</strong> Sciences, Ho has synthesized<br />
scientific studies and written briefings for the communitybased<br />
group.<br />
“Medical practitioners haven’t been very involved<br />
in HIAs to this point,” says Brian Cole (M.P.H. ’90, Dr.P.H.<br />
’03), a researcher at the school who has been a leader in<br />
the HIA movement as part <strong>of</strong> the <strong>UCLA</strong> HIA Project, and<br />
who served as a consultant to the pediatric residents.<br />
“It was exciting to see that the pediatric training program<br />
recognized the importance <strong>of</strong> learning about some <strong>of</strong> the<br />
upstream determinants <strong>of</strong> health problems and using the<br />
HIA as a way <strong>of</strong> addressing that.”<br />
Dr. Alma Guerrero (M.P.H. ’08), an assistant clinical<br />
pr<strong>of</strong>essor <strong>of</strong> pediatrics and CHAT program faculty member,<br />
believes the pediatric residents benefited as much as the<br />
community. “What we try to instill in the residents is the<br />
importance <strong>of</strong> thinking broadly about health,” she says.<br />
“The Santa Monica Airport is near where a lot <strong>of</strong> our<br />
patients live, and it’s easy to take it for granted. By having<br />
the residents review the science and engage with the<br />
community on an important health concern, we’re encouraging<br />
them to think outside the walls <strong>of</strong> the clinic in how<br />
they define their role as physicians.”<br />
“By having<br />
the residents<br />
review the<br />
science and<br />
engage with<br />
the community<br />
on an important<br />
health concern,<br />
we are<br />
encouraging<br />
them to think<br />
outside the<br />
walls <strong>of</strong><br />
the clinic.”<br />
—Dr. Alma Guerrero<br />
13<br />
cover story <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
14<br />
“We know the<br />
built environment<br />
has major health<br />
impacts, from<br />
respiratory<br />
diseases and<br />
injuries to obesity<br />
and many other<br />
chronic diseases,<br />
and yet<br />
transportation<br />
and other sister<br />
agencies are<br />
scarcely aware<br />
<strong>of</strong> them.”<br />
—Dr. Richard Jackson<br />
our HIAs that a more systematic approach would be a valuable tool in the policy<br />
process,” says Dr. Gerald Kominski, pr<strong>of</strong>essor <strong>of</strong> health services at the school and<br />
a key member <strong>of</strong> the initial <strong>UCLA</strong> <strong>Health</strong> Impact Assessment Project team. “Our<br />
goal was to lay out the plausible downstream health effects <strong>of</strong> a variety <strong>of</strong> initiatives<br />
or laws that might be enacted, casting as broad a net as possible to show<br />
that virtually all public programs have potential health consequences.”<br />
The <strong>UCLA</strong> group also argued for bringing in an evidence base. “It’s a twostep<br />
process,” Kominski explains. “The first is analytical – mapping out the possible<br />
pathways by which a policy can affect health. But the second important step<br />
is to say whether there is scientific evidence showing that these plausible effects<br />
have been measured. And the answer is that there is a lot <strong>of</strong> literature out there.”<br />
For an HIA <strong>of</strong> California’s Proposition 49, a successful 2002 ballot initiative to<br />
significantly expand state funding <strong>of</strong> after-school programs, the <strong>UCLA</strong> researchers<br />
found substantial evidence – in the education literature – that providing targeted<br />
after-school programs for at-risk children confers secondary health benefits, from<br />
increased physical activity and improved mental health to lower rates <strong>of</strong> substance<br />
abuse, teen pregnancy and sexually transmitted diseases. Unfortunately,<br />
notes Kominski, the initiative wasn’t designed to address the challenges facing<br />
these at-risk children.<br />
In recent years, one leader in the HIA movement at <strong>UCLA</strong> and nationally<br />
has been Brian Cole (M.P.H. ’90, Dr.P.H. ’03), a researcher in the school’s<br />
Department <strong>of</strong> <strong>Health</strong> Services who was hired as the team’s original project<br />
director while he was a doctoral student in the Department <strong>of</strong> Community<br />
<strong>Health</strong> Sciences. Cole has led the effort to create the HIA Clearinghouse<br />
Learning and Information Center (www.hiaguide.org). In addition to providing<br />
a single online location for all ongoing and completed HIAs in the United States,<br />
the clearinghouse provides links to research used to inform the HIAs and presents<br />
different methods for preparing an HIA. “One <strong>of</strong> our goals is to lower the<br />
bar, particularly for smaller agencies, so that they can do these more easily,”<br />
Cole explains.<br />
Meanwhile, Cole has continued to contract with municipalities and community<br />
groups to conduct HIAs. He recently served as a consultant on an HIA <strong>of</strong> the<br />
Santa Monica Airport done by a group <strong>of</strong> pediatric residents at <strong>UCLA</strong>’s David<br />
Geffen <strong>School</strong> <strong>of</strong> Medicine (see the sidebar on page 13). With funding from the<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
Agricultural policies can<br />
affect health by, for instance,<br />
subsidizing high-fructose corn syrup –<br />
and indirectly fueling the obesity<br />
epidemic.
Pew Charitable Trust, Cole and his <strong>UCLA</strong> <strong>School</strong><br />
<strong>of</strong> <strong>Public</strong> <strong>Health</strong> colleagues are working to ensure<br />
that health concerns are addressed in the environmental<br />
impact report for the Wilshire Corridor<br />
Transit Alternatives – the so-called Subway-to-the-<br />
Sea proposed to be built on Los Angeles’ Westside.<br />
Beyond addressing health concerns, Cole says, the<br />
<strong>UCLA</strong> group is seeking to maximize potential health<br />
benefits from the development: how, for instance,<br />
the system might be able to tap into existing pedestrian<br />
and bicycle routes to encourage people to<br />
walk and bike more. In addition, with funding from<br />
Robert Wood Johnson Active Living Research, the<br />
<strong>UCLA</strong> group is conducting rapid HIAs around<br />
physical activity in schools.<br />
HIAs related to proposed developments – from<br />
a new shopping center to a new highway or subway<br />
system – are a natural fit, Cole explains, since they<br />
can be coupled with environmental impact assessments.<br />
But he and others have also been grappling<br />
with the more challenging but no-less-important<br />
type <strong>of</strong> HIA, ones attached to policies that don’t<br />
involved bricks-and-mortar projects. “The question<br />
is how we get people thinking about the upstream<br />
determinants <strong>of</strong> public health in labor, energy or<br />
agricultural policies, for example,” Cole says.<br />
Much <strong>of</strong> the work <strong>of</strong> the <strong>UCLA</strong> HIA project<br />
has involved building the tools and evidence base<br />
for agencies to apply to these population-level HIAs.<br />
In 2008, Cole and Fielding co-wrote a white paper<br />
published by the Partnership for Prevention on how<br />
Congress and federal agencies could incorporate<br />
HIAs into large-scale policy-making (“Building<br />
<strong>Health</strong> Impact Assessment Capacity: A Strategy<br />
for Congress and Government Agencies”).<br />
Beyond the formal processes <strong>of</strong> analyzing<br />
the potential impacts <strong>of</strong> a project or policy, Cole<br />
Promoting decent,<br />
affordable housing<br />
reduces problems<br />
associated with allergens,<br />
increases community<br />
stability and improves<br />
mental health,<br />
to name a few.<br />
explains, the HIA as well as other tools can play<br />
a broader role by simply educating the public and<br />
policy-makers about the connections between decisions<br />
that are not primarily about health and their<br />
potential public health impacts.<br />
Indeed, notes Fielding, the HIA isn’t an end<br />
in itself. “The HIA is a tool for operationalizing and<br />
concretizing the <strong>Health</strong> in All Policies concept,” he<br />
says. “But it does nothing unless it’s coupled with<br />
efforts to use that information to educate those<br />
who are making policy about why they should pay<br />
more attention to the health impacts <strong>of</strong> decisions<br />
in other sectors.”<br />
Kominski points out that the <strong>Health</strong> in All<br />
Policies movement is based on a notion that has long<br />
been recognized in public health – and championed<br />
by <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> faculty including<br />
Dr. Lester Breslow, dean emeritus <strong>of</strong> the school.<br />
“In public health we know that the medical care<br />
delivery system is just one determinant <strong>of</strong> the population’s<br />
health – an important component, but a<br />
relatively small one, especially when you consider<br />
the cost,” Kominski says. “There are also social<br />
determinants <strong>of</strong> health, and we are likely to reap<br />
much greater health improvements from investments<br />
in those areas than from additional medical<br />
care expenditures.”<br />
Fielding believes many outside <strong>of</strong> public health<br />
are beginning to come around to that point <strong>of</strong> view.<br />
“When we’re spending 50-100 percent more than<br />
our developed-country trading partners and doing<br />
worse in terms <strong>of</strong> health, it becomes obvious that<br />
we can’t just work through the medical care system<br />
to improve health,” he says. “We won’t move from<br />
being 37th in the world in life expectancy until the<br />
determinants <strong>of</strong> health and health impacts <strong>of</strong> decisions<br />
become a focus <strong>of</strong> public policy at all levels.”<br />
15<br />
cover story <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
16<br />
WITH THE<br />
ONE-SIZE-FITS-ALL<br />
APPROACH A<br />
DISTANT MEMORY,<br />
EFFORTS TO<br />
CHANGE <strong>HEALTH</strong><br />
BEHAVIORS ARE<br />
RELYING ON<br />
BETTER-TARGETED<br />
MESSAGES<br />
DELIVERED IN<br />
PROACTIVE AND<br />
INNOVATIVE WAYS.<br />
Higher Education:<br />
In the short video, a young couple has just returned<br />
late one evening from a party. Obviously inebriated, they are moving toward<br />
a sexual encounter. The scene ends and in the next shot it is morning. The<br />
camera zooms in on an unopened condom at the bedside, then shows the nowsober<br />
young man and young woman, appearing regretful as they reflect on a<br />
missed opportunity.<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
“There’s an appreciation<br />
that we need to challenge<br />
our traditional ways <strong>of</strong> thinking<br />
about how to do outreach<br />
to populations.”<br />
—Dr. Beatriz Solis<br />
The frankness <strong>of</strong> the HIV-prevention message targeting youth audiences<br />
would be notable anywhere, but what’s particularly striking about this one is<br />
that it was produced by high school students for their peers – in the Republic<br />
<strong>of</strong> Senegal, a predominantly Muslim nation in western Africa. Shot using mobile<br />
digital technology, it is one <strong>of</strong> many artistically produced peer-to-peer health<br />
messages made widely available to youth in several Senegal high schools and<br />
beyond through a specially created website, www.sunukaddu.com (“our<br />
voices” in Wol<strong>of</strong>).<br />
The project, which has involved two members <strong>of</strong> the <strong>UCLA</strong> <strong>School</strong><br />
<strong>of</strong> <strong>Public</strong> <strong>Health</strong> faculty and several <strong>of</strong> their students, is one <strong>of</strong> many examples,<br />
both inside and outside the school, <strong>of</strong> innovative new approaches to health<br />
education. The days <strong>of</strong> relying on staid, top-down, one-size-fits-all messages are<br />
long gone, replaced by more dynamic, interactive communications, delivered<br />
in carefully selected settings in ways that resonate with the target audience.<br />
It’s a time <strong>of</strong> opportunity for the field <strong>of</strong> health education, says Beatriz<br />
Solis (M.P.H. ’96, Ph.D. ’07), director <strong>of</strong> healthy communities for the south
egion at The California Endowment. Solis notes,<br />
among other things, provisions in the new health<br />
care reform law call for increased education and<br />
engagement <strong>of</strong> linguistically diverse populations<br />
through community health workers. Funding for<br />
prevention that will become available under the<br />
new law will help to bolster the population-based<br />
perspective, including education. Next year will<br />
bring additional dollars to upgrade and expand<br />
community health centers and federally qualified<br />
health centers, providing new opportunities to<br />
reach populations that have traditionally been<br />
underserved by the health care system.<br />
At the same time, there has been a reexamination<br />
<strong>of</strong> traditional health education efforts.<br />
In some cases, Solis says, that has meant capitalizing<br />
on new technologies and communication<br />
approaches that enable communities to “own”<br />
their education – for example, through the use<br />
<strong>of</strong> social media in youth-oriented initiatives.<br />
In other cases, it has meant looking more broadly<br />
at social determinants <strong>of</strong> health problems and<br />
bringing in experts outside <strong>of</strong> the health arena<br />
to assist in the design and implementation <strong>of</strong><br />
initiatives.<br />
“We’re seeing much more crossing <strong>of</strong> traditional<br />
silos, as well as the building <strong>of</strong> relationships<br />
with leaders and organizations that have an ‘in’<br />
within communities and can help to build capacity,”<br />
Solis observes. “There’s an appreciation that we need<br />
to challenge our traditional ways <strong>of</strong> thinking about<br />
how to do outreach to populations.”<br />
The Senegal project was the latest in a series <strong>of</strong><br />
technical assistance and evaluation efforts by two<br />
members <strong>of</strong> the school’s Department <strong>of</strong> Community<br />
<strong>Health</strong> Sciences, Drs. Deborah Glik and Michael<br />
Prelip, to enhance digital and innovative health<br />
communication in West Africa. Funded by the<br />
Open Society Initiative for West Africa, the project’s<br />
research component asked two overarching questions:<br />
whether messages generated by youth would<br />
be more effective in changing behaviors than the<br />
more traditional government-generated messages;<br />
and whether the new media technologies currently<br />
booming in much <strong>of</strong> Africa would be effective in<br />
facilitating the desired health behavior changes.<br />
Students at three high schools in Dakar, Senegal<br />
received both content and technology training, then<br />
led clubs at their schools where students could<br />
create messages through dramatic video, song,<br />
poetry and journalistic approaches. Although the<br />
major focus was on issues around HIV (including<br />
prevention, testing and stigmatization), students<br />
were also able to bring in their own health-related<br />
topics. In addition to being posted on the website,<br />
the student-created content was entered into a<br />
contest in which peers and pr<strong>of</strong>essional artists serving<br />
as judges voted on the winners, which became<br />
part <strong>of</strong> a national campaign.<br />
In the urban center <strong>of</strong> Dakar, the adoption<br />
<strong>of</strong> new media technologies has been rapid. A<br />
post-study survey conducted by the <strong>UCLA</strong> team<br />
found that 60 percent <strong>of</strong> the students reported<br />
going online at least once a week – in many<br />
cases multiple times a day – and roughly the<br />
same proportion said they had easy access<br />
to the Internet. Two-thirds had access to<br />
mobile devices, including cell phones, and<br />
were regularly engaging in text messaging. “West<br />
Africans, like most <strong>of</strong> the developing world, are<br />
moving very quickly into these technologies,”<br />
says Prelip. “There is a great opportunity to take<br />
New Strategies for Promoting <strong>Health</strong><br />
advantage <strong>of</strong> their excitement at having access to<br />
information – especially by working with young<br />
people, who are quick adopters, to influence how<br />
they consume information about health.”<br />
The project has also provided an opportunity<br />
for <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> students to gain<br />
invaluable experience in the field. In 2008, two<br />
students then in the M.P.H. program, Philip Massey<br />
and Bozena Morawski, went to Dakar to work on<br />
the study as summer interns and published a peerreviewed<br />
paper on their findings. Another M.P.H.<br />
student, Brock Dumville, recently returned after<br />
spending 11 weeks in Dakar, working with the<br />
youth and collecting research data. “It was such<br />
a fulfilling experience,” says Dumville. “It showed<br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong><br />
<strong>Health</strong> faculty and<br />
students have worked<br />
on a project in which<br />
students at three high<br />
schools in Senegal<br />
received content and<br />
technology training, then<br />
led clubs where peers<br />
could create messages<br />
through various media<br />
approaches.<br />
17<br />
feature <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
18<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
“If you add<br />
creative artists<br />
to the mix,<br />
you get a jolt<br />
<strong>of</strong> new ideas<br />
and innovative<br />
communication<br />
methods that<br />
make everyone’s<br />
work stronger.”<br />
—Dr. David Gere<br />
me that I have the potential to use what I’ve learned<br />
in the classroom at <strong>UCLA</strong> to create a program on<br />
the ground.”<br />
Massey, now a second-year doctoral student at<br />
the school who has remained involved in the study,<br />
notes that the intervention had the desired effect.<br />
Among his group’s findings: Students in the three<br />
participating schools had nearly two times the odds<br />
<strong>of</strong> knowing a place to get tested as students in the<br />
control school, where the program was not <strong>of</strong>fered.<br />
“Although the actual number <strong>of</strong> people serving as<br />
peer mentors and creating content was small, having<br />
the contest and giving students the ability to go to<br />
the website and view the entries was hugely successful<br />
in creating widespread awareness and interest,”<br />
says Massey.<br />
Given the project’s success, there is now interest<br />
in expanding it throughout Senegal and other<br />
parts <strong>of</strong> West Africa. “For youth audiences in particular,<br />
standing up and lecturing to a group isn’t going<br />
to be the most effective approach,” says Glik. “It’s<br />
important to reach them where they are, and with<br />
messages that resonate. Using technology we can<br />
reach large numbers <strong>of</strong> people and provide opportunities<br />
for the audience to delve deeper into topics.”<br />
In India’s largest government HIV hospital, patients<br />
hear seven hours <strong>of</strong> programming each day over a<br />
public address system. The content, cycled over 14<br />
days, is all about HIV/AIDS, but it’s not what you’d<br />
expect. Through a collaboration between the <strong>UCLA</strong><br />
Art | Global <strong>Health</strong> Center and a theater troupe in<br />
Chennai, where the hospital is located, entertainment<br />
programming is used to convey everything<br />
from the basics <strong>of</strong> HIV/AIDS and treatment adherence<br />
to psychosocial issues, including coping with<br />
deeply ingrained stigma issues associated with HIV.<br />
“Are You Well? Arts in Hospitals,” one <strong>of</strong> several<br />
initiatives currently ongoing in India as part <strong>of</strong> the<br />
<strong>UCLA</strong> center’s Make Art/Stop AIDS Project, started<br />
with the theater group putting on short plays as well<br />
as epic-style theater performances and grew over<br />
several years – to the point that the head <strong>of</strong> the hospital,<br />
which was treating as many as 1,000 patients a<br />
day, asked the collaborators to deliver the entire curriculum<br />
to patients using their uniquely arts-based<br />
presentation. The program has resulted in reductions<br />
in stigma as well as improved knowledge and behavior<br />
change, including adherence to drug protocols.<br />
Another <strong>of</strong> the center’s projects finds community<br />
organizers partnering with multimedia village artists<br />
who use scroll painting, poetry and song to deliver<br />
HIV education in rural India.<br />
Dr. David Gere, associate pr<strong>of</strong>essor in <strong>UCLA</strong>’s<br />
Department <strong>of</strong> World Arts and Cultures and founding<br />
director <strong>of</strong> the <strong>UCLA</strong> Art | Global <strong>Health</strong><br />
Center – whose mission is “to unleash the transformative<br />
power <strong>of</strong> the arts to advance global health” –<br />
has attracted considerable international attention<br />
with his approach. Gere regularly teaches <strong>UCLA</strong><br />
<strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> students in his Make<br />
Art/Stop AIDS course, which is where many <strong>of</strong> the<br />
project’s idea are born, and has recently begun discussions<br />
with the school about conducting collaborative<br />
work in India.<br />
Gere stresses that public health pr<strong>of</strong>essionals,<br />
physicians and community organizers all play a vital<br />
role in fighting the AIDS epidemic. But he started
19<br />
his center out <strong>of</strong> the conviction that “if you add creative artists to the mix, you<br />
get a jolt <strong>of</strong> new ideas and innovative communication methods that make everyone’s<br />
work stronger. A person delivering a lecture in a white coat is not the same<br />
as a puppeteer delivering what might be the same message but in a way that is<br />
easier to grasp, as well as more memorable and attention grabbing.”<br />
In the United States, for all <strong>of</strong> the messages about the health benefits <strong>of</strong> regular<br />
physical activity and risks <strong>of</strong> being sedentary, only about 20 percent <strong>of</strong> adults<br />
have made it part <strong>of</strong> their lives, and an estimated 40 percent are entirely sedentary<br />
during their leisure time. Dr. Antronette (Toni) Yancey, pr<strong>of</strong>essor <strong>of</strong> health<br />
services and co-director <strong>of</strong> the <strong>UCLA</strong> Kaiser Permanente Center for <strong>Health</strong><br />
Equity, based in the school, has begun to popularize a new approach, called<br />
Instant Recess breaks.<br />
Offered in 10-minute intervals, Instant Recess breaks are incorporated into<br />
the routine activities <strong>of</strong> workplace and other organizations, and are low-impact<br />
and moderate enough to engage the entire group rather than only its fittest<br />
members. Yancey outlines her approach in a new book, Instant Recess: Building a<br />
Fit Nation 10 Minutes at a Time (University <strong>of</strong> California Press). Grounded in<br />
science, the book is written in an engaging, lay-friendly style to reach beyond<br />
health pr<strong>of</strong>essional audiences to decision makers in corporate, education, government,<br />
sports and faith-based organizations.<br />
“In the past, we have tended to leave behind the most sedentary people,”<br />
Yancey explains. “A workplace wellness program might provide a free fitness<br />
center or <strong>of</strong>fer incentives for gym membership, but the only ones taking advantage<br />
were individuals who probably would have been active regardless. Instant<br />
Recess aims to get the most people a little bit <strong>of</strong> activity rather than getting<br />
some people a large amount.”<br />
By incorporating exercise into work and organizational settings, the Instant<br />
Recess approach seeks to overcome another traditional barrier. “For many people<br />
– especially in lower-income communities where park space is scarce and the<br />
“Jogging alone<br />
might be culturally<br />
compatible for<br />
affluent white<br />
men, but <strong>of</strong>ten it<br />
isn’t for women<br />
or ethnic minority communities.<br />
On the other hand, moving to music<br />
in a group setting tends to appeal<br />
to these groups.”<br />
—Dr. Antronette Yancey<br />
The <strong>UCLA</strong> Art |<br />
Global <strong>Health</strong> Center<br />
aims to “unleash the<br />
transformative power <strong>of</strong><br />
the arts to advance global<br />
health.” Opposite page,<br />
left: The “Medicine Man”<br />
sculpture was part <strong>of</strong> the<br />
center’s Make Art/Stop<br />
AIDS exhibition at<br />
the 2010 World AIDS<br />
Conference; right:<br />
<strong>UCLA</strong> students in an<br />
HIV-education performance<br />
for Los Angeles<br />
high school students.<br />
This page: HIV-related<br />
street theater in India.<br />
feature <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
20<br />
neighborhood might not be safe – the outside environment isn’t always conducive<br />
to physical activity,” Yancey explains. “Instant Recess can be done inside,<br />
and it doesn’t require a lot <strong>of</strong> space or a fitness room.”<br />
Beyond the commonality <strong>of</strong> being 10 minutes integrated into an organizational<br />
setting and appealing to all levels <strong>of</strong> fitness, Instant Recess breaks are<br />
meant to be adapted to culturally diverse settings. Various programs have been<br />
devised with distinct target audiences in mind, featuring different types <strong>of</strong> music<br />
and movement types. In some cases, Yancey has enlisted celebrities with close<br />
identification among certain groups to help increase interest.<br />
In all cases, the Instant Recess makes exercise a social activity. “Jogging<br />
alone might be culturally compatible for affluent white men, but <strong>of</strong>ten it isn’t<br />
for women or ethnic minority communities,” Yancey says. “On the other hand,<br />
moving to music in a group setting tends to appeal to these groups.”<br />
Dr. Antronette (Toni) Yancey has begun to popularize<br />
Instant Recess exercise breaks – <strong>of</strong>fered in 10-minute<br />
intervals and incorporated into the routine activities<br />
<strong>of</strong> workplace and other organizations. Delivered in<br />
culturally compatible formats, they are designed to<br />
appeal to everyone, not merely the fittest.<br />
<strong>Health</strong> educators have long understood the importance <strong>of</strong> knowing the target<br />
audience and tailoring messages accordingly. But in some cases, efforts haven’t<br />
been as well refined as they could be. “When your message is aimed at a population<br />
that speaks a different language, it’s not enough just to translate,” says Dr.<br />
Roshan Bastani, pr<strong>of</strong>essor <strong>of</strong> health services, associate dean for research and codirector<br />
<strong>of</strong> the <strong>UCLA</strong> Kaiser Permanente Center for <strong>Health</strong> Equity. “You need<br />
to really understand the culture and align the messages with the way people<br />
live, their family structure, and other important characteristics.”<br />
But even the most well crafted messages won’t make a difference if they<br />
don’t reach their intended target. “If you’re putting an ad in the newspaper,”<br />
says Bastani, “do you know that the community you’re trying to reach reads<br />
that newspaper – or any newspaper?” In preparing for a major study aiming to<br />
increase Hepatitis B screening in Los Angeles’ Korean community, Bastani concluded<br />
through extensive focus-group research that the best way to engage large<br />
groups <strong>of</strong> Koreans was through churches in Korean neighborhoods. “At least 95<br />
percent <strong>of</strong> Koreans in Los Angeles regularly attend church, and it’s a major part<br />
<strong>of</strong> the social fabric <strong>of</strong> the community,” Bastani explains.<br />
Bastani and colleagues also learned through the pilot work that the population<br />
was interested in receiving health-related programs at church, and was open<br />
to discussions <strong>of</strong> a topic as sensitive as Hepatitis B – a sexually transmitted virus<br />
associated with an increased risk <strong>of</strong> liver cancer. Bastani’s group has implemented<br />
a randomized controlled trial <strong>of</strong> nearly 1,500 people at Korean church<br />
sites throughout Los Angeles aiming to reduce the disproportionate burden <strong>of</strong><br />
Hepatitis B and liver cancer among Korean Americans. The trial is close to<br />
completion and preliminary findings indicate that the intervention has had its<br />
intended effect <strong>of</strong> increasing receipt <strong>of</strong> Hepatitis B testing.<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
The delivery and content <strong>of</strong> health messages can be critical to their success –<br />
and too <strong>of</strong>ten, health education efforts have fallen flat in racial/ethnic communities<br />
because they have failed to take key cultural factors into account, contends<br />
Dr. Marjorie Kagawa-Singer, pr<strong>of</strong>essor in the <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
and <strong>UCLA</strong>’s Department <strong>of</strong> Asian American Studies, whose work focuses on<br />
reducing disparities, particularly in cancer, among Asian-Americans and other<br />
populations <strong>of</strong> color.<br />
“Different initiatives might have the same goal – such as helping the<br />
population get access to health care – but the messages have to be acceptable,<br />
understandable and relevant to the particular community, using the appropriate<br />
vernacular and metaphors,” she says.<br />
As an example <strong>of</strong> where efforts have gone astray, Kagawa-Singer notes<br />
that initiatives aimed at increasing the use <strong>of</strong> mammography screening among<br />
women in the appropriate age groups have tended to emphasize a “take care <strong>of</strong>
21<br />
yourself” message that might resonate among white<br />
women but is more likely to fall on deaf ears in<br />
other communities, where a more effective<br />
approach might emphasize the importance <strong>of</strong> the<br />
woman taking care <strong>of</strong> herself so that she can fulfill<br />
her role as family caretaker. Similarly, Kagawa-Singer<br />
notes, among cancer survivors beliefs about pain can<br />
be vastly different. While the Western model focuses<br />
on relieving suffering, members <strong>of</strong> some cultures see<br />
pain as a necessary repayment for sins, and are thus<br />
less likely to seek or want relief.<br />
Kagawa-Singer ensures the cultural relevance <strong>of</strong><br />
her research by closely involving community groups<br />
at every stage. As principal investigator <strong>of</strong> the Los<br />
Angeles site <strong>of</strong> the Asian American Network for<br />
Cancer Awareness Research and Training (AAN-<br />
CART), she formed a steering council consisting <strong>of</strong><br />
representatives from 17 community-based groups<br />
serving the diverse Asian-American communities in<br />
the Los Angeles area. Kagawa-Singer’s group was<br />
recently funded for a third five-year period to continue<br />
leading the Los Angeles site <strong>of</strong> AANCART,<br />
the first cancer prevention and control research initiative<br />
targeting Asian-Americans.<br />
“In the community-based participatory research<br />
model, we don’t do anything without the input <strong>of</strong><br />
our community partners,” Kagawa-Singer explains.<br />
“The design and development <strong>of</strong> the interventions<br />
are always conducted with community people who<br />
inform us about what’s going to be most helpful and<br />
most effective. The process is longer, but it’s been<br />
very productive.”<br />
Kagawa-Singer also recently completed a project<br />
on community navigators for cancer screening.<br />
The health navigator concept has gained favor in<br />
recent years as a way to assist underserved populations<br />
in overcoming barriers to obtaining important<br />
health care services. In partnership with organizations<br />
working closely with Asian-American immigrant<br />
communities, Kagawa-Singer’s group tested a<br />
model in which trained members <strong>of</strong> those communities<br />
conduct the outreach and education, and<br />
assist women – most <strong>of</strong> whom are uninsured and<br />
non-English speaking – in everything from making<br />
and following up on appointments to providing<br />
transportation and accompanying the women to<br />
the doctor’s <strong>of</strong>fice.<br />
Navigating and properly using the health care system<br />
can be challenging for even the most educated<br />
consumers – and, Prelip asserts, the ability to do so<br />
has become more important than ever with the passage<br />
<strong>of</strong> health care reform. “If we are increasing people’s<br />
access to care, we need to make sure they are<br />
utilizing the system appropriately or we aren’t going<br />
to be able to pay for it all,” he says.<br />
Earlier this year, the U.S. Department <strong>of</strong> <strong>Health</strong><br />
and Human Services released the National Action<br />
Plan to Improve <strong>Health</strong> Literacy, aiming to make<br />
health information and services easier to understand<br />
and use. Now a <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
research team led by Prelip and Glik, in partnership<br />
with <strong>Health</strong> Net <strong>of</strong> California, has received funding<br />
from the National Institutes <strong>of</strong> <strong>Health</strong> to launch an<br />
innovative effort that uses a social-media strategy to<br />
improve the health literacy <strong>of</strong> teens.<br />
The recently launched project defines health<br />
literacy more broadly than in the past, recasting it<br />
to include health care literacy. “Rather than focusing<br />
Dr. Roshan Bastani<br />
and colleagues have<br />
designed and implemented<br />
a major study<br />
aiming to reduce the<br />
disproportionate burden<br />
<strong>of</strong> Hepatitis B and liver<br />
cancer among Korean<br />
Americans. The educational<br />
intervention is<br />
being delivered at<br />
Korean church sites<br />
throughout Los Angeles.<br />
feature <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
22<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
“For youth<br />
audiences<br />
in particular,<br />
standing up and<br />
lecturing to a<br />
group isn’t going<br />
to be the most<br />
effective<br />
approach.<br />
It’s important<br />
to reach them<br />
where they are,<br />
and with<br />
messages that<br />
resonate.”<br />
—Dr. Deborah Glik<br />
only on health information, we want our teen members<br />
also to know how and when to make appointments<br />
and get referrals, as well as their rights to<br />
services and confidentiality,” says Nancy Wongvipat<br />
Kalev (M.P.H. ’98), director <strong>of</strong> health education/<br />
cultural and linguistic services for <strong>Health</strong> Net Inc.,<br />
and one <strong>of</strong> five <strong>of</strong> the school’s alumni at <strong>Health</strong><br />
Net who are part <strong>of</strong> the study. (Others are Elaine<br />
Robinson-Frank, M.P.H. ’98; Hoa Su, M.P.H. ’98;<br />
Vinia Pangan, M.P.H. ’99; and Sharon Nessim,<br />
Dr.P.H. ’81.)<br />
The study focuses on adolescent <strong>Health</strong> Net<br />
members who are covered through public insurance<br />
programs (in California, Medi-Cal or the <strong>Health</strong>y<br />
Families Program). Many <strong>of</strong> these teens are the first<br />
in their family to have health coverage and may<br />
not know who their primary care provider is, much<br />
less take the step <strong>of</strong> making appointments for recommended<br />
adolescent well-care visits, Wongvipat<br />
Kalev explains. In many cases, she notes, this leads<br />
to emergency room visits that could have been prevented.<br />
Despite rights to confidentiality about medical<br />
care in California, some teens shy away from<br />
seeing health care providers for fear that sensitive<br />
information, such as reproductive health discussions,<br />
will be shared with their parents.<br />
The research team has developed an interactive<br />
website, www.teen2extreme.com, designed to<br />
engage teens on issues about their health as a way to<br />
improve their health care literacy. The site employs<br />
Facebook-style applications. “There are plenty <strong>of</strong><br />
fact-laden websites out there,” says Prelip. “We want<br />
this to be interactive and fun. We know that social<br />
media has become hugely popular among teens, and<br />
we’re excited to find out whether it can be used to<br />
have a desired effect on health literacy.”<br />
Over the course <strong>of</strong> a year, a series <strong>of</strong> health<br />
themes will be presented. The site will include<br />
quizzes, polls and contests, as well as encouraging<br />
participation and interactivity through blogs, live<br />
chats and opportunities to ask questions <strong>of</strong> a nurse.<br />
Users will have the opportunity to upload photos<br />
and video, and to comment on others’ postings.<br />
Embedded in the site will be information about<br />
how and when to make appointments.<br />
Teens with <strong>Health</strong> Net coverage through the<br />
public programs will be randomly assigned to either<br />
the intervention group with access to the social<br />
media website, or a control group receiving standard<br />
information provided to <strong>Health</strong> Net members.<br />
Participants will be surveyed both before and after<br />
the study to determine what effect the intervention<br />
had on their health care knowledge and behaviors,<br />
and <strong>Health</strong> Net data will be studied to weigh the<br />
intervention’s impact on utilization <strong>of</strong> services.<br />
In some ways, the project illustrates the evolving<br />
set <strong>of</strong> tools available to health educators as they<br />
develop new strategies to engage target populations<br />
in an effort to improve their health. “We were using<br />
computers 10-20 years ago, but it was mostly flat,<br />
content-driven websites,” says Glik. “Now we’re able<br />
to <strong>of</strong>fer more – links, resources and the ability to<br />
interact with people who have similar interests and<br />
concerns.”
esearch highlights<br />
Virus Related to Smallpox Rising Sharply in Africa<br />
In the wInter <strong>of</strong> 1979 the world celebrated the end <strong>of</strong> smallpox, a highly contagious<br />
and <strong>of</strong>ten fatal viral infection estimated to have caused between 300-<br />
and 500 million deaths during the 20th century. Smallpox was defeated through<br />
an aggressive worldwide vaccination campaign – a campaign that ended in<br />
1980, with the virus having been eradicated. But a <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> healthled<br />
research team has found that the elimination<br />
<strong>of</strong> the smallpox vaccine had an unintended side<br />
effect.<br />
In the Proceedings <strong>of</strong> the National Academy<br />
<strong>of</strong> Sciences, Dr. Anne rimoin and colleagues<br />
reported that 30 years after the mass smallpox<br />
vaccination campaign ceased, rates <strong>of</strong> a related<br />
virus known as human monkeypox have increased<br />
dramatically in the rural Democratic republic <strong>of</strong><br />
Congo, with sporadic outbreaks in other African<br />
nations and even in the United States.<br />
Until 1980, rimoin notes, the smallpox vaccine<br />
provided cross-protective immunity against<br />
monkeypox, a “zoonotic orthopoxvirus,” meaning<br />
it can be passed from animals to humans.<br />
Symptoms <strong>of</strong> monkeypox in humans include<br />
severe eruptions on the skin, fever, headaches,<br />
swollen lymph nodes, possible blindness and<br />
even death. there is no treatment.<br />
once the smallpox vaccination program<br />
ended, new generations <strong>of</strong> people who were “vaccine<br />
naïve” were exposed to the monkeypox virus<br />
in the Democratic republic <strong>of</strong> Congo over time,<br />
and the number <strong>of</strong> people who became infected gradually increased. But the<br />
increase went unnoticed because the nation has little or no health infrastructure<br />
and thus no way to monitor the spread <strong>of</strong> such diseases.<br />
As a result, monkeypox was thought to be very rare. rimoin’s research<br />
shows, however, that it has become quite common.<br />
rimoin travels frequently to the Democratic republic <strong>of</strong> Congo (DrC),<br />
where she has established a research site to study and track cross-species<br />
transmission <strong>of</strong> the disease (see the pr<strong>of</strong>ile on page 8). for their recent report,<br />
rimoin and her colleagues conducted a population-based surveillance in nine<br />
health zones in the central region <strong>of</strong> the country between 2006 and 2007, gathering<br />
epidemiologic data and biological samples obtained from suspected cases.<br />
they then compared the current, cumulative incidences <strong>of</strong> infection with data<br />
gathered in similar regions from 1981 to 1986. the results were startling, showing<br />
a 20-fold increase in human monkeypox in the DrC since smallpox vaccinations<br />
were ended in 1980.<br />
Because it is unlikely that smallpox vaccinations would be resumed, rimoin<br />
is calling for improved health care education in the Democratic republic <strong>of</strong><br />
Congo and better disease surveillance. there is an urgent need to develop a<br />
strategy for reducing the risk <strong>of</strong> a wider spread <strong>of</strong> infections, she says.<br />
The results were startling, showing a 20-fold<br />
increase in human monkeypox in the Democratic<br />
Republic <strong>of</strong> Congo since smallpox vaccinations<br />
were ended in 1980.<br />
23<br />
research <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
24<br />
One in Four California Children<br />
Has Never Seen a Dentist<br />
Time Since Last Dental Visit<br />
Among California Children<br />
Younger than 11 Years <strong>of</strong> Age<br />
24% 22% 25% 26% 22% 27%<br />
5% 3%<br />
5% 7%<br />
18%<br />
17%<br />
22% 20%<br />
53% 57% 47% 47% 59% 50%<br />
Total White African-American Latino Asian-American Other<br />
Had a dental visit within past six months<br />
Had last dental visit 6-12 months ago<br />
Last dental visit was more than a year ago<br />
Never had a dental visit<br />
neArLy 25 PerCent <strong>of</strong> CALIfornIA ChILDren have never seen a dentist,<br />
and for those who have, disparities exist by race, ethnicity and type <strong>of</strong> insurance<br />
when it comes to the duration between dental care visits, according to the<br />
findings <strong>of</strong> a study by Dr. nadereh Pourat, pr<strong>of</strong>essor <strong>of</strong> health services at the<br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> health and director <strong>of</strong> research for the Center for health<br />
Policy research.<br />
for the study, published in the July issue <strong>of</strong> the journal <strong>Health</strong> Affairs,<br />
Pourat and co-author Dr. Len finocchio <strong>of</strong> the California healthCare foundation<br />
examined barriers to dental care in nearly 11,000 California children ages 11 and<br />
under using data from the 2005 California health Interview Survey, the nation’s<br />
largest state health survey, conducted by the Center for health Policy research.<br />
Among their findings: Latino and African-American children with all types <strong>of</strong><br />
insurance were less likely than Asian-American and white children to have visited<br />
the dentist in the previous six months, or even in their entire lifetime.<br />
the researchers also found that Latino and African-American children in<br />
public insurance programs, including Medicaid and the Children’s health<br />
Insurance Program (ChIP), went to the dentist less <strong>of</strong>ten than white and Asian-<br />
American children with the same insurance coverage. overall, children with private<br />
insurance saw a dentist more <strong>of</strong>ten than those in Medicaid or ChIP.<br />
“Lack <strong>of</strong> dental care continues to be a significant problem for American children,<br />
and our findings suggest that having insurance isn’t always enough,” says<br />
Pourat. “we need to address the other barriers that keep children from getting<br />
the help they need.”<br />
the authors noted that<br />
the findings raise concerns<br />
about Medicaid’s ability to<br />
address disparities in dental<br />
care access. Ultimately,<br />
3%<br />
16% 4%<br />
they argued, more strategic<br />
18%<br />
efforts are necessary to<br />
overcome systemic barriers<br />
to care, including raising<br />
reimbursement rates paid<br />
to dentists who serve the<br />
Medicaid population and<br />
increasing the number <strong>of</strong><br />
participating Medicaid<br />
providers.<br />
Despite the disparities,<br />
having any form <strong>of</strong> dental<br />
insurance significantly increased the odds <strong>of</strong> seeing a dentist on a regular basis<br />
– 54 percent <strong>of</strong> privately insured children and 27 percent <strong>of</strong> publicly insured children<br />
had seen a dentist in the last six months, compared to 12 percent <strong>of</strong> children<br />
without dental coverage.<br />
“the data tell us that Medicaid and ChIP have improved children’s ability to<br />
get dental care,” says Pourat. “however, both programs need to do more to<br />
reduce disparities.” (More on this topic can be found in the article on page 4.)<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
Same-Sex Couples in California<br />
Face Sizable <strong>Health</strong> Insurance Inequities<br />
whILe CALIfornIA IS generALLy weLCoMIng to individuals <strong>of</strong> all sexual<br />
orientations, employers in the state tend to discriminate when it comes to samesex<br />
partners and health care, according to a <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> health study.<br />
Dr. ninez Ponce and colleagues are the first to show a large gap between<br />
employer-sponsored dependent coverage received by heterosexual employees
and lesbian and gay employees. their study, whose findings were published in<br />
the journal <strong>Health</strong> Affairs, concludes that sexual-orientation disparities are<br />
greater than previously thought. Partnered gay men living in California, for example,<br />
are only 42 percent as likely as married heterosexual men to receive<br />
employer-sponsored dependent health insurance, while partnered lesbians have<br />
an even smaller chance – 28 percent – <strong>of</strong> getting coverage compared to married<br />
heterosexual women.<br />
the report used data from the California health Interview Survey. the<br />
researchers combined three years <strong>of</strong> adult surveys: 2001, 2003 and 2005. the<br />
final sample included 63,719 women and 46,535 men between the ages <strong>of</strong> 18<br />
and 64. <strong>of</strong> the sample, 51 percent <strong>of</strong> lesbians and 38 percent <strong>of</strong> gay men<br />
reported being in a partnered or married relationship, compared with 64 percent<br />
<strong>of</strong> female and 64 percent <strong>of</strong> male heterosexuals.<br />
“we found no strong evidence to suggest that California<br />
employers are discriminating in providing health insurance to gay<br />
and lesbian workers as individuals,” says Ponce, an associate<br />
pr<strong>of</strong>essor at the school. “however, we did find that employers<br />
were setting coverage rules for dependents that favored legally<br />
and heterosexually married employees.”<br />
the authors noted that most <strong>of</strong> the data were collected<br />
before full implementation <strong>of</strong> the California Insurance equality Act<br />
<strong>of</strong> 2005; they expect that the law, once fully enacted and combined<br />
with the federal Patient Protection and Affordable Care Act,<br />
may alleviate some <strong>of</strong> the disparities documented in their study.<br />
But they also noted that the way government agencies and<br />
employers define dependents, and the federal taxation <strong>of</strong> health<br />
benefits for a same-sex spouse or partner, continue to be “a relevant<br />
underlying structural determinant <strong>of</strong> whether or to what<br />
extent sexual-orientation minorities will have more equal access<br />
to employer-sponsored insurance.”<br />
Achieving universal coverage, Ponce says, "will depend in<br />
part on remedying inequalities in state and federal marriagerelated<br />
rules."<br />
Nanoparticles in Common Household Items<br />
Cause Genetic Damage in Mice<br />
tItAnIUM DIoxIDe (tIo2) nAnoPArtICLeS, found in everything from cosmetics<br />
and sunscreen to paint and vitamins, cause systemic genetic damage in<br />
mice, according to a comprehensive study conducted by researchers at <strong>UCLA</strong>’s<br />
Jonsson Comprehensive Cancer Center and <strong>School</strong> <strong>of</strong> <strong>Public</strong> health.<br />
the tio2 nanoparticles induced single- and double-strand DnA breaks and<br />
also caused chromosomal damage as well as inflammation, all <strong>of</strong> which increase<br />
the risk for cancer. the study, published in the journal Cancer Research, was the<br />
first to show that the nanoparticles had such an effect, according to Dr. robert<br />
Schiestl, a Jonsson Cancer Center scientist and pr<strong>of</strong>essor in the <strong>School</strong> <strong>of</strong> <strong>Public</strong><br />
health, who was the study’s senior author.<br />
once in the system, the tio2 nanoparticles accumulate in different organs<br />
because the body has no way to eliminate them. And because they are so small,<br />
they can go everywhere in the body, even through cells, and may interfere with<br />
sub-cellular mechanisms, Schiestl’s team noted.<br />
In the past, these tio2 nanoparticles have been considered non-toxic in that<br />
they do not incite a chemical reaction. Instead, it is surface interactions that the<br />
nanoparticles have within their environment – in this case, inside a mouse – that<br />
is causing the genetic damage, Schiestl says. they wander throughout the body<br />
causing oxidative stress, which can lead to cell death.<br />
It is a novel mechanism <strong>of</strong> toxicity, a physicochemical reaction, that these<br />
particles cause in comparison to regular chemical toxins, which are the usual<br />
subjects <strong>of</strong> toxicological research. “the novel principle is that titanium by itself is<br />
Partnered gay men living in California are only<br />
42 percent as likely as married heterosexual men<br />
to receive employer-sponsored dependent health<br />
insurance, while partnered lesbians have an even<br />
smaller chance – 28 percent – <strong>of</strong> getting coverage<br />
compared to married heterosexual women.<br />
25<br />
research <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
26<br />
chemically inert,” Schiestl explains. “however, when the particles become progressively<br />
smaller, their surface, in turn, becomes progressively bigger and in<br />
the interaction <strong>of</strong> this surface with the environment, oxidative stress is induced.<br />
given the growing use <strong>of</strong> these nanoparticles, these findings raise concern<br />
about potential health hazards associated with exposure.”<br />
the manufacture <strong>of</strong> tio2 nanoparticles is a huge industry, Schiestl notes,<br />
with production at about 2 million tons per year. In addition to paint, cosmetics,<br />
sunscreen and vitamins, the nanoparticles can be found in toothpaste, food colorants,<br />
nutritional supplements and hundreds <strong>of</strong> other personal care products.<br />
“It could be that a certain portion <strong>of</strong> spontaneous cancers are due to this<br />
exposure,” Schiestl says. “And some people could be more sensitive to nanoparticle<br />
exposure than others. I believe the toxicity <strong>of</strong> these nanoparticles has not<br />
been studied enough.”<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
Only 61 percent <strong>of</strong> home kitchens received scores<br />
that would give them an A or B grade, compared to<br />
98 percent <strong>of</strong> L.A. County restaurants. Twenty-five<br />
percent received a C, and 14 percent scored lower<br />
than the 70 percent required for a passing grade.<br />
Many Home Kitchens Not Making<br />
the Food-Safety Grade<br />
MoSt PeoPLe ASSUMe that when they are experiencing<br />
food poisoning the culprit is something they<br />
ate outside their home. But a study co-authored by a<br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> health faculty member in his<br />
role as director <strong>of</strong> the Los Angeles County<br />
Department <strong>of</strong> <strong>Public</strong> health suggests that home<br />
kitchens are more prone to causing foodborne infections<br />
than most people realize.<br />
Publishing in the Morbidity and Mortality<br />
Weekly Report <strong>of</strong> the Centers for Disease Control<br />
and Prevention, Dr. Jonathan fielding and colleagues<br />
detailed findings from a study <strong>of</strong> approximately<br />
13,000 Los Angeles County adults who<br />
voluntarily completed an online quiz on their home<br />
food-handling and preparation practices. Based on a<br />
scoring system adapted from that used for restaurant<br />
grading in the county, only 61 percent <strong>of</strong> home<br />
kitchens received scores that would give them an A<br />
or B grade, compared to 98 percent <strong>of</strong> L.A. County<br />
restaurants. twenty-five percent received a C, and 14 percent scored lower than<br />
the 70 percent required for a passing grade. “If they got below a C, I’m not sure<br />
I’d like them inviting me to dinner,” fielding says.<br />
from 1999 to 2007, foodborne diseases caused a reported 2,590 hospitalizations<br />
and 17 deaths in Los Angeles County – numbers that are considered<br />
underestimates given that not all foodborne illnesses leading to hospitalization<br />
or death are confirmed by laboratory testing.<br />
In 1998, under fielding’s leadership, Los Angeles County established<br />
numeric scores for restaurant inspections and posted grades for these inspections<br />
publicly. the initiative was credited with helping to reduce the number <strong>of</strong><br />
hospitalizations for foodborne infections by 13 percent in the first year. In 2006<br />
the county launched the voluntary home Kitchen Self-Inspection Program,<br />
which includes a quiz aiming to provide feedback and education that will promote<br />
safer food hygiene practices at home. the quiz emphasizes such food<br />
handling practices as the need to clean and sanitize cutting boards after handling<br />
poultry, the safe handling <strong>of</strong> raw eggs, and appropriate methods for the<br />
refrigeration <strong>of</strong> cooked and uncooked foods.<br />
fielding’s group noted that the results <strong>of</strong> the quiz can’t be used to directly<br />
compare conditions in homes with those <strong>of</strong> restaurants, since they are based on<br />
self-reports rather than inspections by trained food safety pr<strong>of</strong>essionals. But<br />
given the likelihood that people more interested and conscientious about food
safety were more apt to take the quiz, the results probably understate the problem.<br />
“the findings in this report show that even among interested and motivated<br />
persons, food handling and preparation deficiencies occur frequently in the<br />
home setting,” fielding and colleagues wrote.<br />
Centralized <strong>Health</strong> Care More Cost-Effective,<br />
Offers Better Access to Preventive Services<br />
fAMILIeS froM rUrAL MexICo who receive health care from centralized<br />
clinics run by the federal government pay up to 30 percent less in out-<strong>of</strong>-pocket<br />
expenses and utilize preventive services more <strong>of</strong>ten than families who access<br />
decentralized clinics run by states, according to a study by researchers at the<br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> health. the findings were published in the September<br />
issue <strong>of</strong> the Journal <strong>of</strong> Social Science and Medicine.<br />
the findings, drawn from a comprehensive survey <strong>of</strong> 8,889 rural families<br />
from seven Mexican states conducted in 2003 by Oportunidades, Mexico's principal<br />
anti-poverty program, contradict the widely perceived notion that decentralized<br />
systems are superior, since local knowledge and<br />
resources can be more effectively used to address local needs.<br />
Since the 1990s, centralized and decentralized health care<br />
services have co-existed in 17 Mexican states without competing<br />
against one another. Because centralized and decentralized<br />
organizations rarely operate within the same country during the<br />
same time period or cater to comparable populations, Mexico’s<br />
health care system provides a rare opportunity to compare the two<br />
approaches side by side.<br />
In the study, households serviced by decentralized providers<br />
reported higher out-<strong>of</strong>-pocket health expenditures and lower utilization<br />
<strong>of</strong> preventive services, spending almost 40 percent more<br />
out <strong>of</strong> pocket and utilizing preventive care 7 percent less than<br />
households serviced by centralized providers. the households<br />
studied showed no differences in terms <strong>of</strong> age, years <strong>of</strong> schooling,<br />
family size, insurance status, employment, need and most<br />
community infrastructure measures.<br />
“the Mexican experience can be useful to other developing<br />
countries in Latin America (e.g., Chile or Brazil) and other areas<br />
<strong>of</strong> the developing world (e.g., China, Iran, turkey) where centralized<br />
governments have considered decentralization as a policy<br />
mechanism to reform their national health systems," says Dr.<br />
Arturo Vargas-Bustamante, the study’s lead investigator and an<br />
assistant pr<strong>of</strong>essor <strong>of</strong> health services at the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong><br />
<strong>Public</strong> health.<br />
Vargas-Bustamante suggests that the centralized providers have four attributes<br />
that may give them an advantage:<br />
Type <strong>of</strong> Service. Because the types <strong>of</strong> services provided to rural populations<br />
do not require a high degree <strong>of</strong> specialization and are relatively homogeneous<br />
and less sensitive to local taste and variation, centralized providers may<br />
be able <strong>of</strong>fer these services more efficiently.<br />
Quality <strong>of</strong> Care. Centralized providers have more public resources to provide<br />
better services and employ more incentives and monitoring to improve the<br />
quality <strong>of</strong> care.<br />
Experience. In the three decades since decentralization began in Mexico<br />
centralized providers may have resolved functional issues that decentralized<br />
providers may still be tackling.<br />
Local Capacity. even if local authorities are closer to their communities and<br />
are more familiar with their characteristics and limitations, they still need managerial<br />
skills to provide health services that require some level <strong>of</strong> expertise.<br />
Preventive <strong>Health</strong> Care Utilization<br />
by Type <strong>of</strong> <strong>Health</strong> Care Provider<br />
in Mexico<br />
74%<br />
72%<br />
70%<br />
68%<br />
66%<br />
64%<br />
62%<br />
60%<br />
Centralized<br />
Provider<br />
Decentralized<br />
Provider<br />
27<br />
research <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
28<br />
student pr<strong>of</strong>iles<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
“Promoting sports participation<br />
in developing countries<br />
<strong>of</strong> Africa could be a great<br />
strategy for catalyzing some<br />
<strong>of</strong> the health outcomes we<br />
want for young women.”<br />
— Myralyn "Mimi" Nartey<br />
For Former Pro Soccer Player, Future Kicks<br />
Will Promote <strong>Health</strong> Among African Girls<br />
When she Was 15, MYRALYN "MIMI" NARTEY ventured far from her family’s home<br />
in arizona to the Republic <strong>of</strong> Ghana, where her father had been raised, to play pr<strong>of</strong>essional<br />
soccer for the Ghanian women’s national team.<br />
While there, she contracted malaria. at first the team<br />
administrators and medical staff failed to appreciate the<br />
magnitude <strong>of</strong> her illness. When nartey began to deteriorate,<br />
she was taken to the nearest hospital, which she<br />
barely recognized as a medical care facility. “It felt more<br />
like an open-air marketplace,” she recalls. as she waited<br />
a seemingly interminable period to be seen, nartey saw<br />
frightened-looking women with sick babies on their backs.<br />
“They had no idea what was going on, or if they were going<br />
to be able to pay for what they needed,” she says.<br />
The experience made a huge impression. “here I was,<br />
born and raised in the United states with all the resources<br />
anyone could have, and commissioned by Ghana to play a<br />
sport – yet, I was having problems getting access to health<br />
care when I was sick,” nartey says. “It struck me that if I<br />
was having a hard time, what about everyone else in this<br />
country that was so impoverished?”<br />
With that in mind, nartey majored in environmental<br />
biology as an undergraduate at Columbia University and<br />
went on to do a fellowship in which she conducted<br />
research to develop anti-malarial drugs. Ultimately she<br />
shifted her focus to policy. she got an M.a. in Climate and<br />
society at Columbia, then came to UCLa, where she is<br />
pursuing an M.a. in african studies and a Ph.D. at the<br />
school <strong>of</strong> <strong>Public</strong> health as part <strong>of</strong> a dual-degree program. since arriving in 2006,<br />
nartey has channeled the energy she once used on the soccer field into a myriad<br />
<strong>of</strong> activities: In addition to her studies, she serves as an appointee on the student<br />
health advisory Committee and is the sPh Diversity Coordination Team co-chair, as<br />
well as co-chair <strong>of</strong> students <strong>of</strong> Color for <strong>Public</strong> health. she also has a daughter,<br />
born in February 2009.<br />
nartey continues to be interested in malaria – it is an important focus <strong>of</strong> an<br />
undergraduate seminar she has taught the last three years on the dynamics <strong>of</strong> climate<br />
and health in sub-saharan africa. But her goals have evolved. after recovering<br />
from her bout with malaria, nartey went on to a fruitful career in pr<strong>of</strong>essional<br />
soccer, representing Ghana in the 2002 FIFa african Cup <strong>of</strong> nations and 2003 FIFa<br />
Women’s World Cup. now she has her sights set on developing africa-based programs<br />
to promote participation in sports as a way <strong>of</strong> achieving better health outcomes.<br />
“The benefits <strong>of</strong> sports participation for young women are well documented<br />
in the Untied states, including delayed sexual initiation, better ability to negotiate<br />
condom use with partners, and reduced risk <strong>of</strong> gender-related violence and genderrelated<br />
medical problems,” nartey notes.<br />
Reflecting on her own soccer experience, nartey remembers the benefits<br />
accrued by her teammates, many <strong>of</strong> whom were uneducated. “They became much<br />
more confident,” she says. “It made me realize that promoting sports participation in<br />
developing countries <strong>of</strong> africa – and especially soccer, which is so woven into the<br />
cultural fabric – could be a great strategy for catalyzing some <strong>of</strong> the health outcomes<br />
we want for young women.”
M.P.H./J.D. Dual Program a Recipe for Policy Influence<br />
MoRe Than Many graduate students, ELI TOMAR has spent enough time in the<br />
thick <strong>of</strong> the policy-making process on Capitol hill to know the challenges – and in<br />
many cases, frustrations – <strong>of</strong> passing meaningful health-related legislation.<br />
Prior to embarking on his M.P.h./J.D. through a four-year concurrent degree program<br />
<strong>of</strong>fered by the UCLa school <strong>of</strong> <strong>Public</strong> health and school <strong>of</strong> Law, Tomar spent<br />
several years working in Washington, D.C. – as a congressional intern, a government<br />
relations aide for the U.s. soccer Foundation, and a legislative assistant and public<br />
policy analyst for two law firms, advocating in Congress as a registered lobbyist.<br />
“It’s easy to become disheartened when you see that even getting something<br />
passed that everyone agrees on is an uphill battle,” he says. “so <strong>of</strong>ten, opposition<br />
to a proposal is based on politics, not policy. But it’s important to understand the inertia<br />
that exists and learn how to accomplish what you can.”<br />
Tomar remains enthusiastic about the opportunity to positively affect people’s<br />
lives through legislation. In his workspace he proudly displays a copy <strong>of</strong> the<br />
Medicare Improvements for Patients and Providers act <strong>of</strong> 2008, which included<br />
provisions to expand coverage for patients with endstage<br />
renal disease as well as providing funding for<br />
patient education and prevention programs. Tomar had<br />
lobbied for the bill as part <strong>of</strong> a large coalition that<br />
included health care providers, dialysis centers and<br />
patient groups; it became law after Congress overrode<br />
a veto by then-President Bush. “These were relatively<br />
uncontroversial provisions, and yet this coalition had<br />
been trying to get them for five years,” Tomar says. “I<br />
was thrilled to see it pass.”<br />
Tomar says he knew he wanted to go to law<br />
school well before he considered getting an M.P.h.<br />
although he was exposed to health care policy as a<br />
child – his mother served as a policy director for the<br />
american hospital association – it was only after he<br />
began working with health care clients as a public<br />
policy analyst for the law firm Patton Boggs that he<br />
decided to pursue a joint-degree program.<br />
Through the M.P.h./J.D. – the first program <strong>of</strong> its<br />
kind west <strong>of</strong> the Mississippi River – Tomar is gathering<br />
credentials that will strengthen his ability to make a difference<br />
in the nation’s capital, where he plans to return<br />
after completing the four-year program. The M.P.h./<br />
J.D. is designed to prepare students to work in health<br />
law, a field that was already growing rapidly but <strong>of</strong>fers even more opportunities since<br />
the passage <strong>of</strong> health care reform. Tomar intends to resume his work in health law<br />
and policy; ultimately he would like to help shape policies as part <strong>of</strong> a think tank or<br />
as legal counsel to one <strong>of</strong> the health-related committees on Capitol hill.<br />
“With the entire nation focusing on health care, it’s an exciting time to be studying<br />
these issues,” says Tomar, who is in the school’s Department <strong>of</strong> health services.<br />
“I’m getting a different perspective on policy and a much better grasp <strong>of</strong> everything<br />
from the evaluation <strong>of</strong> programs to the economic forces behind health care, as well<br />
as management-oriented issues such as strategy and marketing. all <strong>of</strong> this is going<br />
to be extremely helpful in my future work.“<br />
“With the entire nation<br />
focusing on health care,<br />
it’s an exciting time to be<br />
studying these issues.”<br />
— Eli Tomar<br />
29<br />
students <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
30<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong><br />
contracts & grants 2009-10<br />
This section includes<br />
new contracts and grants<br />
awarded in fiscal year<br />
2009-10. Due to space<br />
limitations, only funds<br />
<strong>of</strong> $50,000 or more are<br />
listed, by principal<br />
investigator.<br />
RICHARD AMBROSE<br />
Determining Long-Term Changes in Species Abundances and<br />
Community Structure in Southern California Rocky Intertidal Habitats<br />
(Samueli Institute for Information Biology, $80,000 for 2 years)<br />
ONYEBUCHI ARAH<br />
Beyond Individual-Level Determinants: The Role <strong>of</strong> <strong>Health</strong>care<br />
System, Socioeconomic, and Environmental Factors in the Global<br />
Burden <strong>of</strong> Chronic Diseases (Netherlands Organisation for Scientific<br />
Research & Universiteit Van Amsterdam, $310,489 for 2 years)<br />
ROSHAN BASTANI<br />
Los Angeles Regional Cancer Prevention and Control Research<br />
Network (Centers for Disease Control and Prevention, $1,499,955<br />
for 5 years)<br />
RONALD BROOKMEYER<br />
Clinical and Pathological Studies in the Oldest Old: Statistical Design<br />
& Analysis (National Institute on Aging & UC Irvine, $75,822)<br />
E. RICHARD BROWN<br />
The 2009 California <strong>Health</strong> Interview Survey (County <strong>of</strong> Marin,<br />
$200,000 for 2 years; California Children & Families Commission<br />
– First 5, $1,500,000 for 2 years; California Department <strong>of</strong><br />
Managed <strong>Health</strong> Care – Office <strong>of</strong> the Patient Advocate, $251,805;<br />
The California Endowment, $1,729,643 for 2 years; California<br />
Department <strong>of</strong> Mental <strong>Health</strong>, $1,568,000; County <strong>of</strong> San Diego,<br />
$394,091 for 2 years; National Cancer Institute, $300,000); The<br />
State <strong>of</strong> <strong>Health</strong> Insurance in California Report (SHIC) (California<br />
Wellness Foundation, $175,000 for 2 years)<br />
CATHERINE CRESPI<br />
New Methods for the Design <strong>of</strong> Cancer Studies with Clustered<br />
Binary Outcomes (National Cancer Institute, $154,000 for 2 years)<br />
ROGER DETELS<br />
Multidisciplinary HIV and TB Implementation Sciences Training in<br />
China (NIH Fogarty International Center & Chinese Center for<br />
Disease Control and Prevention [China], $540,000 for 5 years);<br />
Natural History <strong>of</strong> AIDS in Homosexual Men: ARRA Supplements<br />
(National Institute <strong>of</strong> Allergy and Infectious Diseases, $1,309,694)<br />
JONATHAN FIELDING<br />
Comprehensive <strong>School</strong> Physical Activity Opportunities: Using<br />
<strong>Health</strong> Impact Assessment to Develop Accountability and<br />
Reporting Systems (Robert Wood Johnson Foundation, $99,850);<br />
<strong>UCLA</strong>/LA County HIA Demonstration and Training Project (Pew<br />
Charitable Trusts, $321,580 for 2 years)<br />
JOHN FROINES<br />
Toxicologic Pathways <strong>of</strong> Rail Yard Emission Exposure on Non-<br />
Cancer <strong>Health</strong> Impacts (British Petroleum Group, $620,480 for 2<br />
years); International Forum on Disability Management (IFDM)<br />
2010 (California Department <strong>of</strong> Industrial Relations, $60,600)<br />
PATRICIA GANZ<br />
A Model Clinical Translational Research Program for Breast Cancer<br />
Survivors: A Focus on Cognitive Function after Breast Cancer<br />
Treatment (The Breast Cancer Foundation, $198,566); Reducing<br />
Breast Cancer Recurrence with Weight Loss: A Vanguard Trial<br />
(National Cancer Institute & UC San Diego, $96,417 for 4 years)<br />
BETH GLENN<br />
Sun Protection Among Children with a Family History <strong>of</strong> Melanoma<br />
(National Cancer Institute, $154,000 for 2 years)<br />
DEBORAH GLIK and MICHAEL PRELIP<br />
Adolescent <strong>Health</strong> Literacy: Improving Use <strong>of</strong> Preventive <strong>Health</strong><br />
Services (National Institute <strong>of</strong> Child <strong>Health</strong> and Human<br />
Development, $1,306,662 for 2 years)<br />
HILARY GODWIN<br />
<strong>Public</strong> <strong>Health</strong> Traineeships (DHHS/<strong>Health</strong> Resources and Services<br />
Administration, $177,392 for 3 years); SARRA – <strong>Public</strong> <strong>Health</strong><br />
Traineeship Program (DHHS/<strong>Health</strong> Resources and Services<br />
Administration, $184,319 for 3 years)<br />
NEAL HALFON<br />
The Interdisciplinary Maternal and Child <strong>Health</strong> Training Program<br />
(DHHS/<strong>Health</strong> Resources and Services Administration, $1,725,000<br />
for 5 years)<br />
GAIL HARRISON<br />
Developing the Immigrant <strong>Health</strong> Component <strong>of</strong> <strong>UCLA</strong>’s Center for<br />
Global and Immigrant <strong>Health</strong> (The California Endowment, $76,750)<br />
SHEHNAZ HUSSAIN<br />
Nucleotide Variation in the Prolactin Receptor and its Agonists and<br />
Breast Cancer Risk (Susan G. Komen Breast Cancer Foundation,<br />
$299,912 for 2 years); Molecular Epidemiology <strong>of</strong> B-Cell Activation,<br />
DNA Repair & HIV-Associated Lymphoma (National Cancer<br />
Institute, $640,376 for 5 years)<br />
MARJAN JAVANBAKHT<br />
Rectal Transmission <strong>of</strong> STIS/HIV Among Women (UC California<br />
HIV/AIDS Research Program [CHRP], $185,776 for 2 years)<br />
ROBERT KAPLAN<br />
<strong>UCLA</strong>/RAND Center for Adolescent <strong>Health</strong> Promotion – Category 1<br />
(Centers for Disease Control and Prevention, $5,180,000 for 5<br />
years); Women’s Exercise Injuries: Incidence and Risk Factors<br />
(National Institute <strong>of</strong> Arthritis & Musculoskeletal and Skin Diseases<br />
& The Cooper Institute, $74,189); Comparative Effectiveness and<br />
Outcomes Improvements (CEOI) Center (National, Heart, Lung, and<br />
Blood Institute, $3,855,398 for 2 years)<br />
LEEKA KHEIFETS<br />
Cell Phone Use and the <strong>Health</strong> <strong>of</strong> Children in the Danish National<br />
Birth 7-1-09 (National Institute <strong>of</strong> Environmental <strong>Health</strong> Sciences,<br />
$423,500 for 2 years)<br />
NOLA KENNEDY<br />
Program to Continue Training to Prevent Workplace Injuries and<br />
Illness Among Low Wage Workers in Hazardous Jobs (California<br />
Wellness Foundation, $200,000 for 3 years)<br />
GERALD KOMINSKI<br />
Pediatric Palliative Care Waiver Evaluation (CA/HHS/Department <strong>of</strong><br />
<strong>Health</strong> Services, $700,000 for 4 years)<br />
SIMIN LIU<br />
Biochemical Predictors <strong>of</strong> Type 2 DM in Women (National Institute<br />
<strong>of</strong> Diabetes, Digestive and Kidney Disease, $230,187)<br />
CAROLYN MENDEZ-LUCK<br />
Elder Caregiving in Los Angeles County: Creating a Pr<strong>of</strong>ile <strong>of</strong><br />
Caregiver <strong>Health</strong> and <strong>Health</strong> Risks (Kaiser Foundation Research<br />
Institute, $150,000 for 2 years)
SHANE QUE HEE<br />
Whole Glove Permeation/Penetration <strong>of</strong> Organic Liquids with a<br />
Dextrous Robot Hand (Centers for Disease Control and Prevention,<br />
$1,060,110 for 3 years)<br />
ANNE RIMOIN<br />
Research and Policy for Infectious Disease Dynamics (RAPIDD)<br />
(Fogarty International Center, $81,712 for 2 years); The Emergence<br />
<strong>of</strong> Human Monkeypox in Central Africa (National Institute <strong>of</strong><br />
Allergy and Infectious Diseases, $88,532); Collaborative Program<br />
Development with GVFI (USDS Agency for International<br />
Development & Global Viral Forecasting Initiative, $207,587)<br />
BEATE RITZ<br />
Sunlight Exposure & Vitamin D Metabolic Gene Variations in<br />
Parkinson’s Disease (National Institute <strong>of</strong> Environmental <strong>Health</strong><br />
Sciences, $154,000 for 2 years); Air Pollution and Childhood<br />
Cancers in California (National Institute <strong>of</strong> Environmental <strong>Health</strong><br />
Sciences, $423,095 for 2 years)<br />
HECTOR RODRIGUEZ<br />
Local <strong>Health</strong> Department Influences on the <strong>Health</strong> <strong>of</strong> Older Adults:<br />
A Statewide Evaluation (Robert Wood Johnson Foundation,<br />
$200,000 for 2 years); The Effect <strong>of</strong> Differential Item Functioning on<br />
the Measurement <strong>of</strong> Racial and Ethnic Disparities in Patients’<br />
Experiences <strong>of</strong> Ambulatory Care (Robert Wood Johnson<br />
Foundation, $75,000 for 2 years)<br />
LINDA ROSENSTOCK<br />
Diversity in <strong>Health</strong> Pr<strong>of</strong>essions (California Wellness Foundation,<br />
$150,000 for 2 years)<br />
STEVEN ROTTMAN<br />
<strong>UCLA</strong> Center for <strong>Public</strong> <strong>Health</strong> Preparedness (Centers for Disease<br />
Control and Prevention, $500,000)<br />
KIMBERLEY SHOAF<br />
<strong>Public</strong> <strong>Health</strong> Emergency Management Training and Education<br />
Academy (City <strong>of</strong> Long Beach Department <strong>of</strong> <strong>Health</strong> and Human<br />
Services, $703,000 for 1.5 years); Preparedness & Emergency<br />
Response Research Centers: A <strong>Public</strong> <strong>Health</strong> Systems Approach<br />
(Centers for Disease Control and Prevention, $4,723,148 for 4 years)<br />
PETER SINSHEIMER<br />
California Garment Care Technology Demonstration Project, Non-<br />
Toxic Dry Cleaning Incentive Program (California Environmental<br />
Protection Agency Air Resources Board, $265,000 for 2 years)<br />
STEVEN WALLACE<br />
Assessment <strong>of</strong> Local Environmental Risk Training (ALERT) (National<br />
Institute <strong>of</strong> Environmental <strong>Health</strong> Sciences, 1,000,000 for 2 years)<br />
MAY WANG<br />
Stimulus: Agent-Based Model <strong>of</strong> Individual-Level Food Choice and<br />
Physical Activity Behavior (National Institute <strong>of</strong> Diabetes and<br />
Digestive and Kidney Diseases, $860,216 for 2 years)<br />
PHYLLIS WEISS<br />
Resource Program for Policy Development and Program Evaluation<br />
for Violence Prevention Organizations (California Wellness<br />
Foundation, $150,000 for 2 years); Community Gang and Violence<br />
Reduction Strategy Planning Project (Centers for Disease Control<br />
and Prevention & The Advancement Project, $73,613)<br />
new faculty<br />
DR. YIFANG ZHU joins the faculty<br />
as assistant pr<strong>of</strong>essor in the<br />
Department <strong>of</strong> Environmental<br />
<strong>Health</strong> Sciences. Her research<br />
focuses on identifying key factors<br />
that affect human exposure to<br />
ultrafine particles on and near<br />
roadways by measuring and<br />
modeling their emissions,<br />
transport and transformation<br />
in the atmosphere, as well as into the in-cabin and<br />
indoor environments. Zhu’s studies are supported<br />
by two prestigious national awards: the National<br />
Science Foundation’s Faculty Early Career<br />
Development Award and the Walter Rosenblith<br />
New Investigator Award from the <strong>Health</strong> Effects<br />
Institute. Zhu, who was most recently an assistant<br />
pr<strong>of</strong>essor in the Environmental Engineering<br />
Department at Texas A&M University-Kingsville,<br />
received her B.S. in Environmental Engineering<br />
from Tsinghua University in China and her Ph.D.<br />
in Environmental <strong>Health</strong> Sciences from the <strong>UCLA</strong><br />
<strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>.<br />
ALSO JOINING THE FACULTY:<br />
BRIAN BRADBURY<br />
Assistant Pr<strong>of</strong>essor, Epidemiology<br />
31<br />
faculty <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
32<br />
news briefs<br />
INTERACT WITH US!<br />
You can learn about happenings at the school,<br />
participate in discussions on public health topics <strong>of</strong> the day<br />
or reconnect with former classmates and favorite faculty<br />
members through the school’s Facebook page,<br />
and follow <strong>UCLA</strong>SPH on Twitter for important updates.<br />
In addition, alumni are invited to join<br />
the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> Alumni Network<br />
on the pr<strong>of</strong>essional networking site Linkedin.<br />
SPH hosts<br />
lunchtime webinars<br />
Starting in October, the <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> began hosting a monthly<br />
series <strong>of</strong> lunchtime webinars. These lunchtime discussions, available through<br />
the school’s website, present a valuable opportunity to hear from faculty<br />
experts about some <strong>of</strong> today’s most critical public health issues. Among<br />
other things, webinar participants will learn what they can do to create healthier<br />
environments in the face <strong>of</strong> disease and environmental challenges; receive<br />
a virtual tour <strong>of</strong> the new Global Bio Lab at <strong>UCLA</strong>, a state-<strong>of</strong>-the-art facility<br />
that will vastly increase the rate at which infectious agents are submitted,<br />
tested and analyzed; hear how food marketing has vastly altered the culture<br />
<strong>of</strong> food and eating, leading to the current obesity epidemic; and see the role<br />
and impact that population health surveys have on implementing health care<br />
reform. For a schedule <strong>of</strong> upcoming webinars and to view previous webinars,<br />
please visit http://ph.ucla.edu/.<br />
curbing teen suicide<br />
motivates SPH students<br />
Ashley Roberts and Anne Sutkowi, second-year students at the <strong>School</strong> <strong>of</strong><br />
<strong>Public</strong> <strong>Health</strong>, are working with students at Olympic High <strong>School</strong> in Santa<br />
Monica as part <strong>of</strong> a health promotion and suicide prevention program they<br />
created called STRIDES. The program, inspired by research linking suicide<br />
rates and emotional health, promotes physical, mental and emotional well<br />
being through physical activity, stress relief and development <strong>of</strong> a positive<br />
self-image.<br />
During the 10-week project, Roberts and Sutkowi are working at the<br />
continuation high school with students who have faced great challenges in<br />
their home life and those who know someone who has thought about suicide<br />
or committed suicide. Twice a week they lead students in stretches and<br />
jogs on campus, hoping to help the students integrate running into their daily<br />
lives, since it is an activity that is both an individual and a team sport. Says<br />
Roberts: “We encourage them to encourage one another, but it's a solitary<br />
thing that they can do by themselves for stress relief.” The project culminates<br />
in the STRIDES 5K Run/Walk at Dockweiler Beach in November. The program<br />
was made possible by support from the Albert Schweitzer Fellowship, which<br />
assists leaders addressing the needs <strong>of</strong> underserved communities.<br />
<strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
new associate dean<br />
for global health<br />
Dr. Onyebuchi Arah, an associate pr<strong>of</strong>essor in the Department<br />
<strong>of</strong> Epidemiology, has been appointed the school’s first associate<br />
dean for global health. Arah will help implement one <strong>of</strong> the school’s<br />
strategic goals: building a world-class global health presence.<br />
Arah brings a unique perspective in both his training and his<br />
experience. A native Nigerian, he received much <strong>of</strong> his advanced<br />
academic education in Holland. As a pediatrician trained in public<br />
health, health services research, health policy and epidemiologic<br />
methods, Arah studies issues such as the role <strong>of</strong> health systems<br />
in global health and performance assessment in health care.<br />
He has been a member <strong>of</strong> the school’s faculty since 2006.<br />
special edition<br />
<strong>of</strong> alumni directory<br />
A special anniversary edition <strong>of</strong> the Alumni Directory will be<br />
produced to celebrate the <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>'s 50th<br />
Anniversary in 2011. The directory will feature contact information,<br />
photos and essays from five decades <strong>of</strong> distinguished alumni.<br />
All alumni will be soon contacted by the vendor Harris Connect<br />
to gather directory information. You may also visit www.ucla.edu/<br />
sphalumni to ensure the school has up-to-date information about<br />
you so that you will be able to reconnect with fellow alumni.<br />
school turning 50<br />
On the eve <strong>of</strong> the school’s 50th anniversary, preparations are<br />
underway for a year <strong>of</strong> celebrating five decades <strong>of</strong> innovative<br />
and high-impact research, teaching and community service.<br />
Beginning with a gala on the evening <strong>of</strong> February 2, 2011<br />
(more details on the back cover), the school will be hosting<br />
numerous events and activities throughout the year to enable<br />
all friends and supporters to participate in the celebration.<br />
Those not in Los Angeles can join in one <strong>of</strong> the lunchtime<br />
webinars (see previous page). The school will also hold a<br />
special celebration for alumni at the annual American <strong>Public</strong><br />
<strong>Health</strong> Association meeting to be held in San Francisco in<br />
November 2011.<br />
<strong>UCLA</strong>’s <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> didn’t start out as a<br />
graduate school. From 1946 to 1983, <strong>UCLA</strong> provided undergraduate<br />
instruction leading to an advanced degree in public<br />
health, which was <strong>of</strong>fered beginning in 1957. It wasn't until<br />
1961 that the University <strong>of</strong> California Regents created an<br />
independent <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> on the Westwood campus.<br />
Join us in celebrating the myriad accomplishments <strong>of</strong> alumni,<br />
students and faculty during the past 50 years, and help the<br />
school continue on the same trajectory for the next 50.<br />
DID YOU KNOW...<br />
You are a lifetime member <strong>of</strong> the<br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
Alumni Association if you are a graduate<br />
<strong>of</strong> the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
and its executive programs.<br />
If you would like more information<br />
about the activities<br />
<strong>of</strong> the <strong>Public</strong> <strong>Health</strong> Alumni Association,<br />
please call (310) 825-6464 or e-mail<br />
phaa@support.ucla.edu.<br />
33<br />
news briefs <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>
U C L A<br />
PUBLIC <strong>HEALTH</strong><br />
Nonpr<strong>of</strong>it Org.<br />
U.S. Postage<br />
PAID<br />
<strong>UCLA</strong><br />
<strong>UCLA</strong><br />
<strong>School</strong> <strong>of</strong><br />
<strong>Public</strong><br />
<strong>Health</strong><br />
<strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
Box 951772<br />
405 Hilgard Avenue<br />
Los Angeles, California 90095-1772<br />
www.ph.ucla.edu<br />
Address Service Requested<br />
The 50th Anniversary Gala <strong>of</strong> the <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
ATUL GAWANDE, M.A., M.D., M.P.H.,<br />
distinguished surgeon and bestselling author,<br />
is the featured speaker at the school’s<br />
50th Anniversary Gala.<br />
FEBRUARY 2, 2011 at 6 P.M.<br />
The Hyatt Regency Century Plaza Los Angeles<br />
To purchase tickets and for sponsorship opportunities<br />
please visit www.ph.ucla.edu/2011gala or call (310) 825-6464.