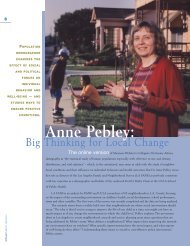
A BROADER VIEWOF HEALTH: - UCLA School of Public Health
A BROADER VIEWOF HEALTH: - UCLA School of Public Health
A BROADER VIEWOF HEALTH: - UCLA School of Public Health
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
the mouth. Untreated, tooth decay (cavities) – the<br />
most common chronic disease in children – can<br />
cause everything from pain and difficulty eating to<br />
lost school and work time. Serious oral disorders can<br />
undermine self-esteem, inhibiting children and adults<br />
from smiling. Gum disease has recently been linked<br />
in studies to increased risk for diabetes, heart disease<br />
and stroke.<br />
And while much attention has been paid to<br />
the problem <strong>of</strong> lack <strong>of</strong> health insurance, the fact<br />
that even more are without dental coverage is <strong>of</strong>ten<br />
overlooked. Although public insurance programs<br />
such as Medicaid have increased coverage for children,<br />
dental benefits tend to be vulnerable to cuts in<br />
tough economic times. By the same token, for many<br />
low-income families struggling financially and, in<br />
some cases, lacking education about the importance<br />
<strong>of</strong> regular dental visits, dental care may be viewed<br />
as optional.<br />
“Oral health issues fit so closely with public<br />
health’s mission,” observes Andersen, “and through<br />
efforts aimed at prevention, education and addressing<br />
access issues, we have the potential to get more in<br />
return from our investment than from many other<br />
investments.”<br />
Dental public health issues haven’t been ignored<br />
at <strong>UCLA</strong>, where faculty in the <strong>School</strong> <strong>of</strong> <strong>Public</strong><br />
<strong>Health</strong> and <strong>School</strong> <strong>of</strong> Dentistry have worked – <strong>of</strong>ten<br />
together – to address some <strong>of</strong> the major concerns.<br />
One <strong>of</strong> the key efforts began in 2001 when The<br />
Robert Wood Johnson Foundation provided funding<br />
for a national demonstration program aiming to<br />
reduce dental-care access disparities. Fifteen dental<br />
schools were selected to participate in the Dental<br />
Pipeline Program, which would receive additional<br />
funding from The California Endowment. The<br />
program’s national evaluation team was based in the<br />
<strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong>, with Andersen as<br />
the principal investigator and Dr. Pamela Davidson,<br />
associate pr<strong>of</strong>essor <strong>of</strong> health services at the school,<br />
as co-principal investigator. (The original project<br />
ended in 2007, but a follow-up study to measure its<br />
sustainability is ongoing.)<br />
The pipeline program was established in an<br />
effort to increase access to dental care in low-income<br />
and minority communities by recruiting more students<br />
from underrepresented minority groups to<br />
dental schools, improving dental school curricula to<br />
better prepare students to provide culturally competent<br />
care, and providing more clinical practice experiences<br />
for students in underserved communities.<br />
“If you look at the ethnicity <strong>of</strong> dentists compared to<br />
the distribution <strong>of</strong> the population, there are greater<br />
differences than in medicine,” Andersen notes. That<br />
has contributed in part to the shortage <strong>of</strong> oral health<br />
providers in minority communities, he says.<br />
Dental schools have faced significant challenges<br />
in their efforts to recruit minority students into<br />
dental careers, Andersen notes. For one, the shortage<br />
<strong>of</strong> providers in minority communities means there<br />
are few family members or friends serving as role<br />
models and mentors. Nonetheless, through steppedup<br />
efforts, including the establishment <strong>of</strong> pre-dental<br />
programs to assist students in meeting prerequisites,<br />
the pipeline program schools increased applications<br />
from underrepresented minority students by 77<br />
percent from 2003 to 2007, while enrollment <strong>of</strong><br />
underrepresented minority students increased by<br />
27 percent.<br />
Beyond the effort to increase the number <strong>of</strong><br />
minority dental providers, the pipeline program<br />
sought to revamp education and training experiences<br />
that would make all students more likely to consider<br />
careers in public health and service to underserved<br />
communities. While curricula were revised and the<br />
number <strong>of</strong> days senior dental students practiced<br />
in underserved communities increased, it’s unclear<br />
whether there was a corresponding increase in graduates<br />
going on to practice in these communities.<br />
Unfortunately, Andersen notes, dental students tend<br />
to enter practice with huge debts; thus, many who<br />
want to go into public service positions are deterred<br />
by the lower salaries and instead feel compelled to<br />
opt for private practice.<br />
The problem <strong>of</strong> disparities in utilization <strong>of</strong> dental<br />
services – particularly among children – is underscored<br />
by a recent study conducted by Dr. Nadereh<br />
Pourat, pr<strong>of</strong>essor <strong>of</strong> health services and director <strong>of</strong><br />
research for the Center for <strong>Health</strong> Policy Research,<br />
which is based in the school. Using data from the<br />
2005 California <strong>Health</strong> Interview Survey, Pourat<br />
found that nearly 25 percent <strong>of</strong> California children<br />
ages 11 and under had never seen a dentist, and<br />
that among those who had, there were significant<br />
differences by race, ethnicity and type <strong>of</strong> insurance<br />
in the amount <strong>of</strong> time between dental care visits<br />
(see page 24).<br />
Having any kind <strong>of</strong> insurance significantly<br />
increased the odds that a child would see a dentist<br />
on a regular basis, but the type <strong>of</strong> coverage mattered:<br />
54 percent <strong>of</strong> privately insured children had seen<br />
a dentist within the previous six months, vs. 27<br />
percent <strong>of</strong> publicly insured children (Medicaid or<br />
the Children’s <strong>Health</strong> Insurance Program) and 12<br />
“<strong>Public</strong> programs<br />
are designed to<br />
improve access<br />
to care for<br />
underserved<br />
populations,<br />
and our study<br />
shows that they<br />
are successful<br />
in doing so.<br />
However,<br />
they don’t close<br />
the gap.”<br />
—Dr. Nadereh Pourat<br />
5<br />
feature <strong>UCLA</strong>PUBLIC <strong>HEALTH</strong>