Pharmacy Professional - Royal Pharmaceutical Society
Pharmacy Professional - Royal Pharmaceutical Society
Pharmacy Professional - Royal Pharmaceutical Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
L E A R N I N G & D E V E L O P M E N T<br />
Produced by The <strong>Pharmaceutical</strong> Journal<br />
CONTINUING PROFESSIONAL DEVELOPMENT<br />
CONTINUING PROFESSIONAL DEVELOPMENT<br />
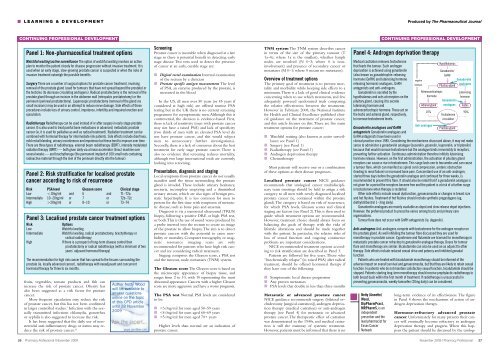
Panel 1: Non-pharmaceutical treatment options<br />
Watchful waiting/active surveillance The option of watchful waiting involves an active<br />
plan to monitor the patient closely for disease progression without invasive treatment. It is<br />
used when an early stage, slow-growing prostate cancer is suspected or when the risks of<br />
invasive treatment outweigh the possible benefits.<br />
Surgery There are a number of surgical options for prostate cancer treatment, involving<br />
removal of the prostate gland (used for tumours that have not spread beyond the prostate) or<br />
the testicles (to decrease circulating androgens). Radical prostatectomy is the removal of the<br />
prostate gland through an incision in the abdomen wall (retropubic prostatectomy) or the<br />
perineum (perineal prostatectomy). Laparosopic prostatectomy (removal of the gland via<br />
small incisions) may be used in an attempt to reduce nerve damage. Side effects of these<br />
procedures include loss of urinary control, impotence, infertility and impaired erection and<br />
ejaculation.<br />
Radiotherapy Radiotherapy can be used instead of or after surgery in early stage prostate<br />
cancer. It is also used to treat painful bone metastases in advanced, metastatic prostate<br />
cancer (ie, it is used for palliative as well as radical treatment). Radiation treatment can be<br />
combined with hormonal therapy for intermediate risk patients. Side effects include diarrhoea,<br />
mild rectal bleeding, urinary incontinence and impotence but these tend to improve over time.<br />
There are three types of radiotherapy: external beam radiotherapy (EBRT), intensity modulated<br />
radiation therapy (IMRT) — both given daily via a linear accelerator (linac) machine over<br />
several weeks — and brachytherapy (the permanent implant of 100 small rods containing<br />
radioactive material through the skin of the perineum directly into the tumour).<br />
Panel 2: Risk stratification for localised prostate<br />
cancer according to risk of recurrence<br />
Risk PSA level Gleason score Clinical stage<br />
Low 20ng/ml or 8–10 or T3–T4<br />
Panel 3: Localised prostate cancer treatment options<br />
Risk<br />
Low<br />
Intermediate<br />
High<br />
Options<br />
Watchful waiting<br />
Watchful waiting, radical prostatectomy, brachytherapy or<br />
radical radiotherapy<br />
If there is a prospect of long-term disease control then<br />
prostatectomy or radical radiotherapy (with a minimum of two<br />
years’ adjuvant hormonal therapy)<br />
The recommendation for high risk cancer that has spread to the tissues surrounding the<br />
prostate (ie, locally advanced cancer), radiotherapy with neoadjuvant and concurrent<br />
hormonal therapy for three to six months.<br />
fruits, vegetables, tomato products and fish can<br />
increase the risk of prostate cancer. Obesity has<br />
also been suggested as a risk factor for prostate<br />
cancer.<br />
More frequent ejaculation may reduce the risk<br />
of prostate cancer, but this has not been confirmed<br />
in larger controlled studies. 3 Infection with the sexually<br />
transmitted infections chlamydia, gonorrhea<br />
or syphilis is also suggested to increase the risk.<br />
It has been suggested that the daily use of nonsteroidal<br />
anti-inflammatory drugs or statins may reduce<br />
the risk of prostate cancer. 4,5<br />
Author Netty Wood<br />
will be available to<br />
answer questions<br />
online on the topic<br />
of this CPD article<br />
until 28 November<br />
2009<br />
Screening<br />
Prostate cancer is incurable when diagnosed at a late<br />
stage so there is potential benefit in detecting early<br />
stage disease. Two tests used to detect the presence<br />
of cancer at an early, curable stage are:<br />
■ Digital rectal examination Internal examination<br />
of the rectum by a clinician<br />
■ Prostate specific antigen measurement The level<br />
of PSA, an enzyme produced by the prostate, is<br />
measured in the blood<br />
In the US, all men over 50 years (or 45 years if<br />
considered at high risk) are offered routine PSA<br />
testing but in the UK there is no current screening<br />
programme for asymptomatic men.Although this is<br />
controversial, the decision is evidence-based. First,<br />
there is lack of sensitivity (men with prostate cancer<br />
may not have a raised PSA) and lack of specificity<br />
(two thirds of men with an elevated PSA level do<br />
not have prostate cancer, and this would subject<br />
men to unnecessary further investigations).<br />
Secondly, there is a lack of consensus about the best<br />
treatment for early stage prostate cancer. There is<br />
also no evidence that screening reduces mortality,<br />
although two large international trials are currently<br />
looking into screening.<br />
Presentation, diagnosis and staging<br />
Local symptoms from prostate cancer do not usually<br />
manifest until the tissue surrounding the prostate<br />
gland is invaded. These include urinary hesitancy,<br />
nocturia, incomplete emptying and a diminished<br />
urinary stream, which are also signs of benign prostatic<br />
hypertrophy. It is less common for men to<br />
present for the first time with symptoms of metastatic<br />
disease, such as bone pain and anaemia.<br />
Diagnosis is via a transrectal ultrasound (TRUS)<br />
biopsy, following a positive DRE or high PSA test,<br />
or both.This is the use of sound waves produced by<br />
a probe inserted into the rectum to create an image<br />
of the prostate to allow biopsy.The aim is to detect<br />
prostate cancers with the potential to cause morbidity<br />
or mortality. Computer tomography or magnetic<br />
resonance imaging scans are only<br />
recommended for patients who have high risk cancer<br />
and are considering radical treatment.<br />
Staging comprises the Gleason score, a PSA test<br />
and the tumour, node, metastases (TNM) system.<br />
The Gleason score The Gleason score is based on<br />
the microscopic appearance of biopsy tissue, and<br />
ranges from 2 to 10, with 10 representing the most<br />
abnormal appearance. Cancers with a higher Gleason<br />
score are more aggressive and have a worse prognosis.<br />
The PSA test Normal PSA levels are considered<br />
to be:<br />
■