Consent to Examination or Treatment Policy - Halton and St Helens ...
Consent to Examination or Treatment Policy - Halton and St Helens ...
Consent to Examination or Treatment Policy - Halton and St Helens ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
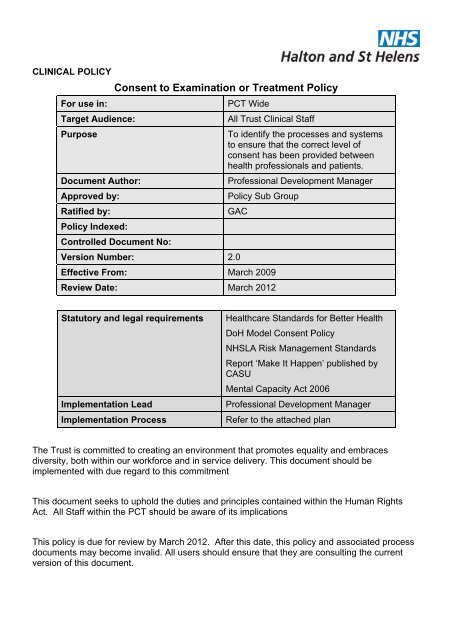
CLINICAL POLICY<br />
F<strong>or</strong> use in:<br />
Target Audience:<br />
Purpose<br />
Document Auth<strong>or</strong>:<br />
Approved by:<br />
Ratified by:<br />
<strong>Policy</strong> Indexed:<br />
<strong>Consent</strong> <strong>to</strong> <strong>Examination</strong> <strong>or</strong> <strong>Treatment</strong> <strong>Policy</strong><br />
Controlled Document No:<br />
PCT Wide<br />
All Trust Clinical <strong>St</strong>aff<br />
To identify the processes <strong>and</strong> systems<br />
<strong>to</strong> ensure that the c<strong>or</strong>rect level of<br />
consent has been provided between<br />
health professionals <strong>and</strong> patients.<br />
Professional Development Manager<br />
<strong>Policy</strong> Sub Group<br />
GAC<br />
Version Number: 2.0<br />
Effective From: March 2009<br />
Review Date: March 2012<br />
<strong>St</strong>atu<strong>to</strong>ry <strong>and</strong> legal requirements<br />
Implementation Lead<br />
Implementation Process<br />
Healthcare <strong>St</strong><strong>and</strong>ards f<strong>or</strong> Better Health<br />
DoH Model <strong>Consent</strong> <strong>Policy</strong><br />
NHSLA Risk Management <strong>St</strong><strong>and</strong>ards<br />
Rep<strong>or</strong>t ‘Make It Happen’ published by<br />
CASU<br />
Mental Capacity Act 2006<br />
Professional Development Manager<br />
Refer <strong>to</strong> the attached plan<br />
The Trust is committed <strong>to</strong> creating an environment that promotes equality <strong>and</strong> embraces<br />
diversity, both within our w<strong>or</strong>kf<strong>or</strong>ce <strong>and</strong> in service delivery. This document should be<br />
implemented with due regard <strong>to</strong> this commitment<br />
This document seeks <strong>to</strong> uphold the duties <strong>and</strong> principles contained within the Human Rights<br />
Act. All <strong>St</strong>aff within the PCT should be aware of its implications<br />
This policy is due f<strong>or</strong> review by March 2012. After this date, this policy <strong>and</strong> associated process<br />
documents may become invalid. All users should ensure that they are consulting the current<br />
version of this document.
Key individuals involved in developing the document<br />
Name<br />
Designation<br />
Linda Spooner<br />
Professional Development Manager<br />
Debbie Fairclough<br />
Assistant Chief Executive<br />
Swati Chapman<br />
Mental Capacity Lead<br />
Circulated <strong>to</strong> the following individuals f<strong>or</strong> comments<br />
Name<br />
Designation<br />
Margaret Evans<br />
Caldicott Guardian<br />
Dot Keates<br />
Head of Clinical Governance<br />
Seamus McGirr<br />
Executive Nurse<br />
Michelle Bradshaw<br />
Asst Direc<strong>to</strong>r Child & Family Health<br />
Ros Connolly<br />
Asst Direc<strong>to</strong>r Child & Family Health<br />
Barry Hut<strong>to</strong>n<br />
Asst Direc<strong>to</strong>r of Operations<br />
Fiona Bremner<br />
Divisional Manager<br />
Vicky Heilbron<br />
Divisional Manager<br />
Philip Chalmers<br />
Divisional Manager<br />
Page 2 of 64
Table of Contents<br />
Introduction ..................................................................................................................................4<br />
Purpose........................................................................................................................................4<br />
Scope...........................................................................................................................................4<br />
Objectives ....................................................................................................................................5<br />
Definitions ....................................................................................................................................5<br />
Duties <strong>and</strong> Responsibilities ..........................................................................................................7<br />
Process........................................................................................................................................8<br />
Training......................................................................................................................................17<br />
Implementation, moni<strong>to</strong>ring <strong>and</strong> review......................................................................................17<br />
Documentation...........................................................................................................................18<br />
References.................................................................................................................................19<br />
Appendix 1 .................................................................................................................................21<br />
Appendix 2 .................................................................................................................................22<br />
Appendix 3 .................................................................................................................................24<br />
Appendix 4 .................................................................................................................................31<br />
Appendix 5 .................................................................................................................................38<br />
Appendix 6 .................................................................................................................................43<br />
Appendix 7 .................................................................................................................................55<br />
Appendix 8 .................................................................................................................................56<br />
Appendix 9 .................................................................................................................................58<br />
Appendix 10 ...............................................................................................................................59<br />
Appendix 11 ...............................................................................................................................60<br />
Appendix 12 ...............................................................................................................................63<br />
Appendix 13 ...............................................................................................................................64<br />
Page 3 of 64
INTRODUCTION<br />
Patients have a fundamental legal <strong>and</strong> ethical right <strong>to</strong> determine what happens <strong>to</strong> their own<br />
bodies. Valid consent <strong>to</strong> treatment is theref<strong>or</strong>e absolutely central in all f<strong>or</strong>ms of healthcare, from<br />
providing personal care <strong>to</strong> undertaking maj<strong>or</strong> surgery. Seeking consent is also a matter of<br />
common courtesy between health professionals <strong>and</strong> patients.<br />
PURPOSE<br />
It is the responsibility of the professional providing the care <strong>to</strong> ensure that the c<strong>or</strong>rect level of<br />
consent has been provided. “<strong>Consent</strong>” is a patient’s agreement f<strong>or</strong> a health professional <strong>to</strong><br />
provide care <strong>or</strong> carry out an assessment. This policy identifies the processes <strong>and</strong> systems in<br />
operation at NHS Hal<strong>to</strong>n <strong>and</strong> <strong>St</strong> <strong>Helens</strong> that should ensure “consent” is achieved when relevant.<br />
SCOPE<br />
The requirement <strong>to</strong> obtain consent can sometimes be a complex matter. This policy outlines<br />
those occasions which may require consent <strong>and</strong> details the processes which must be<br />
undertaken in different circumstances.<br />
Patients may indicate consent non-verbally (f<strong>or</strong> example by presenting their arm f<strong>or</strong> their pulse<br />
<strong>to</strong> be taken), verbally, <strong>or</strong> in writing. F<strong>or</strong> the consent <strong>to</strong> be valid, the patient must:<br />
<br />
<br />
<br />
be competent <strong>to</strong> make the particular decision<br />
have received sufficient inf<strong>or</strong>mation <strong>to</strong> take it; <strong>and</strong><br />
not be acting under duress<br />
The context of consent can take many different f<strong>or</strong>ms, ranging from the active request by a<br />
patient f<strong>or</strong> a particular treatment (which may <strong>or</strong> may not be appropriate <strong>or</strong> available) <strong>to</strong> the<br />
passive acceptance of a health professional’s advice.<br />
In some cases, the health professional will suggest a particular f<strong>or</strong>m of treatment <strong>or</strong><br />
investigation <strong>and</strong> after discussion the patient may agree <strong>to</strong> accept it. In others, there may be a<br />
number of ways of treating a condition, <strong>and</strong> the health professional will help the patient <strong>to</strong><br />
decide between them. Some patients, especially those with chronic conditions, become very<br />
well inf<strong>or</strong>med about their illness <strong>and</strong> may actively request particular treatments. In many cases,<br />
‘seeking consent’ is better described as ‘joint decision making’. The patient <strong>and</strong> health<br />
professional need <strong>to</strong> come <strong>to</strong> an agreement on the best way f<strong>or</strong>ward, based on the patient’s<br />
values <strong>and</strong> preferences <strong>and</strong> the health professional’s clinical knowledge.<br />
Page 4 of 64
Where an adult patient lacks the mental capacity (either temp<strong>or</strong>arily <strong>or</strong> permanently) <strong>to</strong> give <strong>or</strong><br />
withhold consent f<strong>or</strong> themselves, no one else can give consent on their behalf. However,<br />
treatment may be given if it is in their best interests, as long as it has not been refused in<br />
advance in a valid <strong>and</strong> applicable advance directive. F<strong>or</strong> further details on advance directives<br />
see the Department of Health’s Reference guide <strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong> treatment<br />
(chapter 1, paragraph 19).<br />
<strong>Policy</strong> <strong>St</strong>atement<br />
This policy sets out the st<strong>and</strong>ards <strong>and</strong> procedures in NHS Hal<strong>to</strong>n <strong>and</strong> <strong>St</strong> <strong>Helens</strong>, which aim <strong>to</strong><br />
ensure that health professionals are able <strong>to</strong> comply with national guidance. While it is primarily<br />
concerned with healthcare, social care colleagues should also be aware of their obligation <strong>to</strong><br />
obtain consent bef<strong>or</strong>e providing certain f<strong>or</strong>ms of social care, e.g. Those that involve <strong>to</strong>uching<br />
the patient <strong>or</strong> client. Health professionals must also be aware of any guidance on consent<br />
issued by their own regula<strong>to</strong>ry bodies.<br />
The Department of Health has issued a range of guidance documents on consent, (see<br />
Appendix A) <strong>and</strong> these should be consulted f<strong>or</strong> details of the law <strong>and</strong> good practice<br />
requirements. ‘12 key points on consent: the law in Engl<strong>and</strong>’ has been attached in full (see<br />
Appendix B).<br />
OBJECTIVES<br />
This policy outlines the procedures <strong>and</strong> processes that have <strong>to</strong> be completed <strong>and</strong> actions that<br />
must be taken by health professionals undertaking clinical procedures that require consent.<br />
DEFINITIONS<br />
Types of <strong>Consent</strong><br />
<strong>Consent</strong> is often wrongly equated with a patient’s signature on a consent f<strong>or</strong>m. A signature on<br />
a f<strong>or</strong>m is evidence that the patient has given consent, but is not proof of valid consent. If a<br />
patient is rushed in<strong>to</strong> signing a f<strong>or</strong>m, on the basis of <strong>to</strong>o little inf<strong>or</strong>mation, the consent may not<br />
be valid, despite the signature. Patients may, if they wish, withdraw consent after they have<br />
signed a f<strong>or</strong>m: the signature is evidence of the process of consent-giving, not a binding contract.<br />
If a patient has given valid verbal consent, the fact that they are physically unable <strong>to</strong> sign the<br />
f<strong>or</strong>m is no bar <strong>to</strong> treatment.<br />
Implied <strong>Consent</strong><br />
Many examinations provided by health professional were carried out under implied consent.<br />
This is no longer considered best practice as staff should not rely on a patient’s apparent<br />
Page 5 of 64
compliance with a procedure as a f<strong>or</strong>m of consent, i.e. the fact that a patient lies down on an<br />
examination couch does not in itself indicate that the patient has unders<strong>to</strong>od what is proposed<br />
<strong>and</strong> why. F<strong>or</strong> consent <strong>to</strong> be valid, the professional must demonstrate through documentation<br />
that the patient underst<strong>and</strong>s the process, procedure, problems <strong>and</strong> outcome. If there is an<br />
alternative <strong>to</strong> this procedure, this must also be fully discussed.<br />
Verbal <strong>Consent</strong><br />
Verbal consent should be sought bef<strong>or</strong>e any procedure takes place. A clear explanation of<br />
what is <strong>to</strong> be done, any risks <strong>to</strong> consider <strong>and</strong> any alternative should be discussed with the<br />
patient. The discussion which takes place should be rec<strong>or</strong>ded in the case notes. Written<br />
evidence of consent should include how you tested that the patient unders<strong>to</strong>od what was going<br />
<strong>to</strong> be done <strong>to</strong> them; this will demonstrate that inf<strong>or</strong>med consent was given. As with all entries <strong>to</strong><br />
case notes, the date <strong>and</strong> time must be rec<strong>or</strong>ded <strong>and</strong> the entry signed.<br />
Written consent<br />
There are no legal requirements in terms of specific procedures that require written consent.<br />
However, as a matter of good practice, the General Medical Council guidance states that written<br />
consent should be obtained in cases where:<br />
<br />
<br />
<br />
<br />
<br />
The treatment is complex, <strong>or</strong> involves significant risks <strong>and</strong> /<strong>or</strong> side effects (the term ‘risk’<br />
is used throughout <strong>to</strong> refer <strong>to</strong> any adverse outcome, including those which some health<br />
professionals would describe as ‘side-effects’ <strong>or</strong> complications’)<br />
The provision of clinical care is not the primary purpose of the investigation <strong>or</strong><br />
examination<br />
There may be significant consequences f<strong>or</strong> the patient’s employment, social <strong>or</strong> personal<br />
life.<br />
The treatment is part of research programme approved by the PCT<br />
Min<strong>or</strong> surgery perf<strong>or</strong>med under local anesthesia. However, with the trend <strong>to</strong>wards m<strong>or</strong>e<br />
procedures, investigations <strong>and</strong> treatments being carried out on an outpatient <strong>or</strong> day case<br />
basis, it should also include other treatments such as certain f<strong>or</strong>ms of drug therapy,<br />
cy<strong>to</strong><strong>to</strong>xic therapy <strong>and</strong> investigations <strong>or</strong> treatments involving ionizing radiations.<br />
Legal Requirements<br />
It is rarely a legal requirement <strong>to</strong> seek written consent but it should be regarded as best practice<br />
<strong>and</strong> m<strong>and</strong>a<strong>to</strong>ry <strong>to</strong> do so if any of the circumstances indicated by the GMC Guidance (above)<br />
apply.<br />
Page 6 of 64
Mental Capacity Act 2006<br />
This policy must be read in conjunction with the PCT policy on Mental Capacity Act <strong>and</strong> the<br />
Mental Capacity Act Code of Practice. The Mental Capacity Act 2006 provides a legal<br />
framew<strong>or</strong>k f<strong>or</strong> acting <strong>and</strong> making decisions on behalf of people who lack the mental capacity <strong>to</strong><br />
make specific decisions f<strong>or</strong> them. The Act provides a statu<strong>to</strong>ry framew<strong>or</strong>k <strong>to</strong> empower <strong>and</strong><br />
protect vulnerable people who may not be able <strong>to</strong> make their own decisions. It makes it clear<br />
who can take decisions in which situations <strong>and</strong> how they should go about this. It enables people<br />
<strong>to</strong> plan ahead f<strong>or</strong> a time when they may lose capacity. There are 10 guiding principles set out in<br />
the Act that must be followed when a member of PCT is assessing the capacity of an individual<br />
<strong>to</strong> provide valid consent <strong>to</strong> treatment <strong>or</strong> refusal of treatment.<br />
DUTIES AND RESPONSIBILITIES<br />
PCT Board<br />
The Board is responsible f<strong>or</strong> ensuring that the PCT adheres <strong>to</strong> the specific Department of<br />
Health Guidance <strong>and</strong> guidelines in all areas relating <strong>to</strong> consent.<br />
Chief Executive<br />
The Chief Executive has responsibility f<strong>or</strong> meeting all statu<strong>to</strong>ry requirements <strong>and</strong> f<strong>or</strong><br />
implementing guidance issued by the Department of Health in respect of Integrated <strong>and</strong> Clinical<br />
Governance.<br />
Direc<strong>to</strong>r Clinical <strong>St</strong><strong>and</strong>ards<br />
The Direc<strong>to</strong>r of Clinical <strong>St</strong><strong>and</strong>ards is directly responsible f<strong>or</strong> ensuring that the PCT has a f<strong>or</strong>mal<br />
consent policy <strong>and</strong> that all healthcare professionals know of <strong>and</strong> apply the requirements of the<br />
policy at all times.<br />
Managers<br />
All managers have a general responsibility <strong>to</strong> ensure that staff is familiar with the requirements<br />
of all policies that apply <strong>to</strong> them. Any member of their staff who has been given particular<br />
responsibilities regarding consent should have these reflected in their w<strong>or</strong>k objectives.<br />
Clinical Executive Committee (CEC)<br />
This sub-committee of the Board is responsible f<strong>or</strong> reviewing <strong>and</strong> agreeing the processes f<strong>or</strong><br />
managing clinical risk in the <strong>or</strong>ganisation <strong>and</strong> rep<strong>or</strong>ting <strong>to</strong> the Board. CEC is directly<br />
responsible f<strong>or</strong> advising the Board on the implementation of key Department of Health<br />
Guidance such as <strong>Consent</strong>.<br />
Page 7 of 64
Healthcare Professionals<br />
It is a health professional’s own responsibility <strong>to</strong> ensure that when they require colleagues <strong>to</strong><br />
seek consent on their behalf they are confident that the colleague is competent <strong>to</strong> do so; <strong>and</strong> <strong>to</strong><br />
w<strong>or</strong>k within their own competence <strong>and</strong> not <strong>to</strong> agree <strong>to</strong> perf<strong>or</strong>m tasks which exceed that<br />
competence.<br />
PROCESS<br />
F<strong>or</strong> significant procedures i.e. commencement <strong>or</strong> course of treatment <strong>or</strong> new course of<br />
treatment / care, it is essential f<strong>or</strong> health professionals <strong>to</strong> document clearly both:<br />
<br />
<br />
A patient’s agreement <strong>to</strong> the intervention, <strong>and</strong><br />
The discussions, which led up <strong>to</strong> that agreement<br />
This may be done either through the use of a consent f<strong>or</strong>m (with further details in the patient<br />
notes if required), <strong>or</strong> through documenting in the patient’s notes that they have given verbal<br />
consent.<br />
Completed f<strong>or</strong>ms should be kept with the patient’s notes.<br />
Any changes <strong>to</strong> a f<strong>or</strong>m, made after the f<strong>or</strong>m has been signed by the patient, should be initialed<br />
<strong>and</strong> dated by both patient <strong>and</strong> health professional.<br />
It will not usually be necessary <strong>to</strong> document a patient’s consent <strong>to</strong> routine <strong>and</strong> low risk<br />
procedures, such as providing personal care <strong>or</strong> taking a blood sample. However, it would be<br />
advisable <strong>to</strong> do so if there is any reason <strong>to</strong> believe that:<br />
<br />
<br />
The consent may be disputed later, <strong>or</strong><br />
If the procedure is of particular concern <strong>to</strong> the patient (e.g. if they have declined <strong>or</strong> have<br />
become very distressed about similar care in the past).<br />
Provision of <strong>Treatment</strong><br />
The provision of inf<strong>or</strong>mation is central <strong>to</strong> the consent process. Bef<strong>or</strong>e patients can come <strong>to</strong> a<br />
decision about treatment, they need comprehensive inf<strong>or</strong>mation about their condition, possible<br />
treatments/investigations risks <strong>and</strong> benefits (including the risks/benefits of doing nothing); they<br />
also need <strong>to</strong> know whether additional procedures are likely <strong>to</strong> be necessary as part of the<br />
procedure e.g. a blood transfusion, <strong>or</strong> the removal of particular tissue.<br />
Once a decision <strong>to</strong> have a particular treatment has been made, patients need inf<strong>or</strong>mation about<br />
what will happen, where <strong>to</strong> go, how long they will be in hospital, how they will feel afterwards<br />
<strong>and</strong> so on. Patients, <strong>and</strong> those close <strong>to</strong> them, will vary in how much inf<strong>or</strong>mation they want,<br />
Page 8 of 64
anging from those who want as much detail as possible, (including details of rare risks), <strong>to</strong><br />
those who ask health professionals <strong>to</strong> make decisions f<strong>or</strong> them.<br />
Investigation<br />
Once a decision <strong>to</strong> have a particular investigation is undertaken, the patient requires inf<strong>or</strong>mation<br />
<strong>to</strong> determine what will happen with the results of the investigation should further treatment <strong>or</strong><br />
care be required. E.g. In the case of cervical screening.<br />
In the case of obtaining blood f<strong>or</strong> investigations where the outcome may have a life changing<br />
effect on not only the patient but their family, children <strong>and</strong> any other contacts e.g. in the case of<br />
testing f<strong>or</strong> a notifiable disease <strong>or</strong> if Chlamydia <strong>or</strong> HIV test is being done.<br />
There will always be an element of clinical judgment in determining what inf<strong>or</strong>mation should be<br />
given; however, the presumption must be that the patient wishes <strong>to</strong> be well inf<strong>or</strong>med about the<br />
risks <strong>and</strong> benefits of the various options. Where the patient makes it clear (verbally <strong>or</strong> nonverbally)<br />
that they do not wish <strong>to</strong> be given this level of inf<strong>or</strong>mation, this should be documented.<br />
Where the outcome may require contact tracing, full counseling must be given <strong>and</strong> consent<br />
obtained <strong>to</strong> contact trace pri<strong>or</strong> <strong>to</strong> any names being obtained from the patient. Written consent<br />
must be obtained that the patient has been fully counseled <strong>and</strong> agrees <strong>to</strong> contacts being traced.<br />
Once names have been obtained, it becomes the responsibility of the PCT <strong>to</strong> action<br />
appropriately i.e. blood investigations where the outcome may have a life changing result.<br />
When should consent be sought<br />
When a patient f<strong>or</strong>mally gives their consent <strong>to</strong> a particular intervention, this is only the endpoint<br />
of the consent process. It is helpful <strong>to</strong> see the whole process of inf<strong>or</strong>mation provision,<br />
discussion <strong>and</strong> decision making as part of ‘seeking consent’. This process may take place one<br />
stage at a time <strong>or</strong> over a series of meetings <strong>and</strong> discussions, depending on the seriousness of<br />
what is proposed <strong>and</strong> the urgency of the patient’s condition.<br />
Single stage process<br />
In many cases, it will be appropriate f<strong>or</strong> a health professional <strong>to</strong> initiate a procedure immediately<br />
after discussing it with the patient, e.g., during an ongoing episode of care a physiotherapist<br />
may suggest a particular manipulative technique, explain how it might help the patient’s<br />
condition <strong>and</strong> whether there are any significant risks. If the patient is willing f<strong>or</strong> the technique <strong>to</strong><br />
be used, they will then give their consent <strong>and</strong> the procedure can go ahead immediately. In many<br />
such cases, consent will be given verbally.<br />
If a proposed procedure carries significant risks, it will be appropriate <strong>to</strong> seek written consent.<br />
Health professionals must take in<strong>to</strong> consideration whether the patient has had sufficient chance<br />
Page 9 of 64
<strong>to</strong> abs<strong>or</strong>b the inf<strong>or</strong>mation necessary f<strong>or</strong> them <strong>to</strong> make their decision. As long as it is clear that<br />
the patient underst<strong>and</strong>s <strong>and</strong> consents, the health professional may then proceed.<br />
Processes with two <strong>or</strong> m<strong>or</strong>e stages<br />
In most cases where written consent is being sought, treatment options will generally be<br />
discussed well in advance of the actual procedure being carried out. This may be on just one<br />
occasion (either within primary care <strong>or</strong> in a hospital out-patient clinic), <strong>or</strong> it might be over a<br />
whole series of consultations with a number of different health professionals. The consent<br />
process will theref<strong>or</strong>e have at least two stages:<br />
<br />
<br />
The provision of inf<strong>or</strong>mation, discussion of options <strong>and</strong> initial (verbal) decision<br />
The confirmation that the patient still wants <strong>to</strong> go ahead<br />
The consent f<strong>or</strong>m should be used as a means of documenting the inf<strong>or</strong>mation stage(s), as well<br />
as the confirmation stage.<br />
Patients receiving elective treatment <strong>or</strong> investigations f<strong>or</strong> which written consent is appropriate<br />
should be familiar with the contents of their consent f<strong>or</strong>m bef<strong>or</strong>e they arrive f<strong>or</strong> the actual<br />
procedure. They should also receive a copy of the page documenting the decision-making<br />
process. They may be invited <strong>to</strong> sign the f<strong>or</strong>m, confirming that they wish treatment <strong>to</strong> go ahead,<br />
at any appropriate point bef<strong>or</strong>e the procedure i.e. in outpatients, at a pre-admission clinic, <strong>or</strong><br />
when they arrive f<strong>or</strong> treatment. If a f<strong>or</strong>m is signed bef<strong>or</strong>e patients arrive f<strong>or</strong> treatment a member<br />
of the healthcare team must check with the patient at this point whether they have any further<br />
concerns <strong>and</strong> whether their condition has changed. This is particularly imp<strong>or</strong>tant where there<br />
has been a significant lapse of time between the f<strong>or</strong>m being signed <strong>and</strong> the procedure.<br />
When confirming the patient’s consent <strong>and</strong> underst<strong>and</strong>ing, it is advisable <strong>to</strong> use a f<strong>or</strong>m of w<strong>or</strong>ds<br />
which requires m<strong>or</strong>e than a yes/no answer from the patient e.g. “tell me what you’re expecting<br />
<strong>to</strong> happen”, rather than “is everything all right?”<br />
While administrative arrangements will vary, it should always be remembered that f<strong>or</strong> consent <strong>to</strong><br />
be valid, the patient must feel that it would have been possible f<strong>or</strong> them <strong>to</strong> refuse, <strong>or</strong> change<br />
their mind.<br />
It will rarely be appropriate <strong>to</strong> ask a patient <strong>to</strong> sign a consent f<strong>or</strong>m after they have begun <strong>to</strong> be<br />
prepared f<strong>or</strong> treatment (e.g. when preparations are being made <strong>to</strong> administer an injection),<br />
unless this is unavoidable because of the urgency of the patient’s condition.<br />
Page 10 of 64
Who is responsible f<strong>or</strong> obtaining consent?<br />
The health professional carrying out the procedure is ultimately responsible f<strong>or</strong> ensuring that the<br />
patient is genuinely consenting <strong>to</strong> what is being done, <strong>and</strong> it is they who will be held responsible<br />
in law if this is challenged later.<br />
When verbal <strong>or</strong> non-verbal consent is being sought at the time the procedure will be carried out,<br />
this will naturally be done by the health professional responsible. However, teamw<strong>or</strong>k is a<br />
crucial part of the way the NHS operates, <strong>and</strong> where written consent is being sought, it may be<br />
appropriate f<strong>or</strong> other members of the team <strong>to</strong> participate in the process of seeking consent.<br />
Availability of consent f<strong>or</strong>ms<br />
<strong>St</strong><strong>and</strong>ard consent f<strong>or</strong>ms <strong>and</strong> f<strong>or</strong>ms f<strong>or</strong> adults who are unable <strong>to</strong> give consent (f<strong>or</strong> whatever<br />
reason) are reproduced in Appendices C-F <strong>and</strong> are available on the intranet. There are three<br />
versions of the consent f<strong>or</strong>m <strong>and</strong> a prof<strong>or</strong>ma f<strong>or</strong> completion where a patient may lack capacity<br />
<strong>or</strong> decisions are being made in the patient’s best interests.<br />
<br />
<br />
<br />
<br />
F<strong>or</strong>m 1 - f<strong>or</strong> adults <strong>or</strong> competent children, requiring anesthesia<br />
F<strong>or</strong>m 2 - f<strong>or</strong> parental consent f<strong>or</strong> a child <strong>or</strong> young person<br />
F<strong>or</strong>m 3 - f<strong>or</strong> cases where it is envisaged that the patient will remain alert throughout the<br />
procedure <strong>and</strong> no anesthetist will be involved in their care<br />
Clinical Prof<strong>or</strong>ma f<strong>or</strong> the 2 stage assessment f<strong>or</strong> mental capacity assessments <strong>and</strong><br />
best interest decisions -f<strong>or</strong> adults who are unable <strong>to</strong> consent f<strong>or</strong> investigation <strong>or</strong><br />
treatment<br />
F<strong>or</strong>m 3 may be thought m<strong>or</strong>e appropriate f<strong>or</strong> use than f<strong>or</strong>m 1 in situations where patients:<br />
<br />
<br />
<br />
Do not need <strong>to</strong> be made aware of issues surrounding general <strong>or</strong> regional anesthesia.<br />
Will not need <strong>to</strong> make any advance decisions about additional procedures (because they<br />
will be in a position <strong>to</strong> make any such decisions at the time if necessary)<br />
Are having screening which may result in the need <strong>to</strong> contact trace.<br />
Completing consent f<strong>or</strong>ms<br />
The st<strong>and</strong>ard consent f<strong>or</strong>m (F<strong>or</strong>m 1) provides space f<strong>or</strong> a health professional <strong>to</strong> provide<br />
inf<strong>or</strong>mation <strong>to</strong> patients <strong>and</strong> <strong>to</strong> sign confirming that they have done so. The health professional<br />
providing the inf<strong>or</strong>mation must be judged competent <strong>to</strong> do so, either because:<br />
<br />
They themselves carry out the procedure<br />
Page 11 of 64
They have received specialist training in advising patients about this procedure <strong>or</strong> have<br />
been assessed as competent<br />
<br />
Or are aware of their own knowledge limitations <strong>and</strong> are subject <strong>to</strong> audit<br />
Refusal of treatment<br />
If the process of seeking consent is <strong>to</strong> be a meaningful one, refusal must be one of the patient’s<br />
options. A competent adult patient is entitled <strong>to</strong> refuse any treatment, except in circumstances<br />
governed by the Mental Health Act 1983. The situation f<strong>or</strong> children is m<strong>or</strong>e complex -see the<br />
Department of Health’s ‘Seeking consent: w<strong>or</strong>king with children’ f<strong>or</strong> m<strong>or</strong>e detail. The following<br />
paragraphs apply primarily <strong>to</strong> adults.<br />
If, after discussion of possible treatment options, a patient refuses all treatment, this fact should<br />
be clearly documented in their notes.<br />
If the patient has already signed a consent f<strong>or</strong>m, but then changes their mind, the Health<br />
professional (<strong>and</strong> where possible the patient) should note this on the f<strong>or</strong>m.<br />
Where a patient has refused a particular intervention, the health professional must ensure<br />
continued provision of any other appropriate care <strong>to</strong> which consent has been given. Health<br />
professionals should also ensure that the patients realise they are free <strong>to</strong> change their mind <strong>and</strong><br />
accept treatment later if they wish <strong>to</strong> do so. Where delay may affect their treatment choices,<br />
they should be advised acc<strong>or</strong>dingly.<br />
If a patient consents <strong>to</strong> a particular procedure but refuses certain aspects of the intervention, the<br />
health professional must explain <strong>to</strong> the patient the possible consequences of their partial<br />
refusal.<br />
If health professionals genuinely believe that the procedure cannot be safely carried out under<br />
the patient’s stipulated conditions, they are not obliged <strong>to</strong> perf<strong>or</strong>m it. They must, however,<br />
continue <strong>to</strong> provide any other appropriate care. If another health professional believes that the<br />
can be carried out safely under the conditions specified by the patient, the patient’s care must<br />
be transferred on request, if at all possible.<br />
Emergencies<br />
In emergencies, the two-stage consent process (discussion of options <strong>and</strong> confirmation that the<br />
patient wishes <strong>to</strong> go ahead) will follow straight on from each other. In these circumstances, it<br />
may also be appropriate <strong>to</strong> use the patient’s notes <strong>to</strong> document any discussion <strong>and</strong> the patient’s<br />
consent, rather than using a f<strong>or</strong>m. If, at times of emergency, the patient’s situation limits the<br />
quantity of inf<strong>or</strong>mation that can be given, it should not affect its quality.<br />
Page 12 of 64
Specific areas of consent<br />
<strong>Treatment</strong> of young children – parental responsibility<br />
Only people with ‘parental responsibility’ are entitled <strong>to</strong> give consent on behalf of their children.<br />
Health professionals should be aware that not all parents have parental responsibility f<strong>or</strong> their<br />
children, e.g. unmarried fathers do not au<strong>to</strong>matically have such responsibility although they can<br />
acquire it. If there is any doubt about the status of the person with the child in respect of their<br />
parental responsibility f<strong>or</strong> that child, health professionals MUST check.<br />
Where it is not a scheduled appointment, <strong>or</strong> it is the first appointment, <strong>and</strong> a child is brought by<br />
someone who does not have parental responsibility (PR), the clinician should check directly with<br />
the person who has PR, <strong>to</strong> establish whether they consent <strong>to</strong> the treatment/have auth<strong>or</strong>ised this<br />
other person <strong>to</strong> give consent. The only exception <strong>to</strong> that would be where a child is brought f<strong>or</strong><br />
urgent/emergency treatment e.g. dental <strong>and</strong> podiatry by someone who has "care of" the child at<br />
that particular time.<br />
F<strong>or</strong> m<strong>or</strong>e inf<strong>or</strong>mation about who has parental responsibility see Appendix 8<br />
.<br />
Immunisation of younger children<br />
F<strong>or</strong> young children not competent <strong>to</strong> give <strong>or</strong> withhold consent, such consent can be given by a<br />
person with parental responsibility, provided that person is capable of consenting <strong>to</strong> the<br />
immunisation in question <strong>and</strong> is able <strong>to</strong> communicate their decision. Where this person brings<br />
the child in response <strong>to</strong> an invitation f<strong>or</strong> immunisation, <strong>and</strong>, following an appropriate<br />
consultation presents the child f<strong>or</strong> that immunisation, these actions may be considered evidence<br />
of consent. (See appendix 8 who has parental responsibility)<br />
Immunisation in schools<br />
Where immunisations are offered in the school setting the situation differs depending on the age<br />
<strong>and</strong> competence of the individual child <strong>or</strong> young person.<br />
1. Young people aged 16 <strong>and</strong> 17 are entitled <strong>to</strong> consent <strong>to</strong> their own medical treatment.<br />
2. Younger children who underst<strong>and</strong> fully what is involved in the proposed procedure<br />
(referred <strong>to</strong> as “Fraser” <strong>or</strong> “Gillick” competent) can also give consent, although ideally<br />
their parents will be involved.<br />
3. If a person aged 16 <strong>or</strong> 17 <strong>or</strong> a ‘Fraser competent’ child refuses but the parent gives<br />
consent, it is the parent’s view that has f<strong>or</strong>ce. A court may also over-ride such a<br />
child’s refusal. However, the power <strong>to</strong> over-ride cannot be exercised in all cases –<br />
m<strong>or</strong>e detail is set out in paragraph 8 of the ‘Reference guide <strong>to</strong> consent f<strong>or</strong><br />
examination <strong>or</strong> treatment’, (see appendix 1 f<strong>or</strong> details of access <strong>to</strong> the guide)<br />
4. If a person aged 16 <strong>or</strong> 17 <strong>or</strong> a ‘Fraser competent’ child consents <strong>to</strong> treatment, a<br />
parent cannot over-ride that consent.<br />
Page 13 of 64
5. An immunisation can be administered, <strong>to</strong> a Gillick competent child who gives their<br />
consent, in the absence of parental consent. As a matter of good practice such<br />
children should be encouraged <strong>to</strong> discuss the issue with their parents, in the hope of<br />
obtaining their supp<strong>or</strong>t f<strong>or</strong> the vaccination. Parents are inf<strong>or</strong>med by way of issuing<br />
letters / leaflets of what is involved with these vaccinations <strong>and</strong> when they are<br />
planned <strong>to</strong> take place.<br />
6. There is no need f<strong>or</strong> immunisers <strong>to</strong> obtain positive parental consent <strong>to</strong> the<br />
vaccination, once that inf<strong>or</strong>mation has been provided. If however, someone with<br />
parental responsibility f<strong>or</strong> the child registers a strong objection <strong>to</strong> any vaccination<br />
proceeding, it is recommended that legal advice be sought pri<strong>or</strong> <strong>to</strong> any vaccination<br />
taking place. In the event of any complaints from those with parental responsibility,<br />
these will be dealt with by the PCT Complaints <strong>and</strong> Clinical Governance Team.<br />
7. If there are any concerns re ‘Parental Responsibility’ the Designated Nurse f<strong>or</strong><br />
Looked after Children <strong>or</strong> the Designated Nurse Child Protection should be contacted.<br />
They will inf<strong>or</strong>m staff of the necessary actions <strong>to</strong> be undertaken <strong>and</strong> the c<strong>or</strong>rect paper<br />
w<strong>or</strong>k <strong>to</strong> complete.<br />
Procedure when patients lack the capacity <strong>to</strong> give <strong>or</strong> withhold consent<br />
The st<strong>and</strong>ard consent f<strong>or</strong>ms should never be used f<strong>or</strong> adult patients unable <strong>to</strong> consent f<strong>or</strong><br />
themselves.<br />
Where an adult patient does not have the capacity <strong>to</strong> give <strong>or</strong> withhold consent <strong>to</strong> a<br />
significant intervention, the Prof<strong>or</strong>ma f<strong>or</strong> the 2 stage assessment f<strong>or</strong> mental capacity<br />
assessment <strong>and</strong> best interest decisions should be used (Appendix 6)<br />
Health Professionals should note:<br />
The assessment of the patient’s capacity<br />
Why the health professional believes the treatment <strong>to</strong> be in the patient’s best<br />
interests, <strong>and</strong><br />
The involvement of people close <strong>to</strong> the patient<br />
F<strong>or</strong> m<strong>or</strong>e min<strong>or</strong> interventions, this inf<strong>or</strong>mation should be entered in the patient’s notes<br />
An apparent lack of capacity <strong>to</strong> give <strong>or</strong> withhold consent may in fact be the result of<br />
communication difficulties rather than genuine incapacity. Health professionals should involve<br />
appropriate colleagues in making such assessments of incapacity, such as specialist learning<br />
disability teams <strong>and</strong> speech <strong>and</strong> language therapists, unless the urgency of the patient’s<br />
situation prevents this. If at all possible, the patient should be assisted <strong>to</strong> make <strong>and</strong><br />
communicate their own decision, f<strong>or</strong> example by providing inf<strong>or</strong>mation in non-verbal ways<br />
where appropriate.<br />
Page 14 of 64
Occasionally, there will not be a consensus on whether a particular treatment is in the best<br />
interests of an incapacitated adult. Where the consequences of having, <strong>or</strong> not having the<br />
treatment are potentially serious, a court declaration can be sought.<br />
Seeking consent f<strong>or</strong> anesthesia<br />
When an anesthetist is involved in a patient’s care, it is their responsibility <strong>to</strong> seek consent f<strong>or</strong><br />
anesthesia, having discussed the benefits <strong>and</strong> risks. However, in elective treatment it is not<br />
acceptable f<strong>or</strong> the patient <strong>to</strong> receive no inf<strong>or</strong>mation about anesthesia until their pre-operative<br />
visit from the anesthetist. At such a late stage the patient will not be in a position <strong>to</strong> genuinely<br />
make a decision about whether <strong>or</strong> not <strong>to</strong> undergo anesthesia. Patients should theref<strong>or</strong>e either<br />
receive a general leaflet about anesthesia at a previous visit, <strong>or</strong> have the opp<strong>or</strong>tunity <strong>to</strong> discuss<br />
anesthesia in a pre-assessment clinic.<br />
The anesthetist should ensure that the discussion with the patient, <strong>and</strong> their consent, is<br />
documented:<br />
<br />
<br />
<br />
In the anesthetic rec<strong>or</strong>d, <strong>and</strong><br />
In the patient’s notes, <strong>or</strong><br />
On the consent f<strong>or</strong>m<br />
Where the clinician providing the care is personally responsible f<strong>or</strong> anesthesia (e.g. where local<br />
anesthesia <strong>or</strong> sedation is being used), then he <strong>or</strong> she will also be responsible f<strong>or</strong> ensuring that<br />
the patient has given consent <strong>to</strong> that f<strong>or</strong>m of anesthesia.<br />
Where general anesthesia <strong>or</strong> sedation is being provided as part of dental treatment, the General<br />
Dental Council currently holds dentists responsible f<strong>or</strong> ensuring that the patient has all the<br />
necessary inf<strong>or</strong>mation. In such cases, the anesthetist <strong>and</strong> dentist will theref<strong>or</strong>e share that<br />
responsibility.<br />
Provision f<strong>or</strong> patients where English is not there first language<br />
This PCT is committed <strong>to</strong> ensuring that patients whose first language is not English receive the<br />
inf<strong>or</strong>mation they need <strong>and</strong> are able <strong>to</strong> communicate appropriately with healthcare staff. It is not<br />
appropriate <strong>to</strong> use children <strong>to</strong> interpret f<strong>or</strong> family members who do not speak English.<br />
Language Line is used by Hal<strong>to</strong>n & <strong>St</strong> <strong>Helens</strong> PCT f<strong>or</strong> interpretation service <strong>and</strong> translation of<br />
documents, the contact number is 0845 310990. Each professional using the service has been<br />
allocated a code <strong>to</strong> access the service. All new professionals can request a code from the<br />
Executive Service Manager on 01744 457306.<br />
Page 15 of 64
We also have access <strong>to</strong> Deaf Sign Language Service by <strong>St</strong> <strong>Helens</strong> Deaf Centre, they require<br />
two weeks notice 01744 23887.<br />
<strong>Consent</strong> f<strong>or</strong>ms in a variety of languages are available on the Department of Health website at<br />
www.dh.gov.uk/<strong>Policy</strong>AndGuidance/HealthAndSocialCareTopics/<strong>Consent</strong><strong>Consent</strong>Genera<br />
lInf<strong>or</strong>mation/<strong>Consent</strong>GeneralArticle/fs/en<br />
Access <strong>to</strong> health professionals between f<strong>or</strong>mal appointment<br />
After an appointment with a health professional in primary care patients will often think of further<br />
questions they would like answered bef<strong>or</strong>e they make their decision. Contact details of the<br />
health professional should be given <strong>to</strong> the patient f<strong>or</strong> further discussion if necessary.<br />
Clinical pho<strong>to</strong>graphy <strong>and</strong> conventional <strong>or</strong> digital video rec<strong>or</strong>dings<br />
Pho<strong>to</strong>graphic <strong>and</strong> video rec<strong>or</strong>dings of a patient made f<strong>or</strong> clinical purposes f<strong>or</strong>m part of<br />
that patient’s rec<strong>or</strong>d.<br />
Although consent <strong>to</strong> certain rec<strong>or</strong>dings, such as X-rays, is implicit in the patient’s consent <strong>to</strong> the<br />
procedure, health professionals should always ensure that they make clear in advance if any<br />
pho<strong>to</strong>graphic <strong>or</strong> video rec<strong>or</strong>ding will result from that procedure.<br />
Pho<strong>to</strong>graphic <strong>and</strong> video rec<strong>or</strong>dings of a patient which are made f<strong>or</strong> treating <strong>or</strong> assessing<br />
a patient must not be used f<strong>or</strong> any purpose other than the patient’s care <strong>or</strong> the audit of that<br />
care, without the express consent of the patient <strong>or</strong> a person with parental responsibility f<strong>or</strong> the<br />
patient.<br />
The one exception <strong>to</strong> this principle is set out in paragraph 3 below;<br />
To use such a rec<strong>or</strong>ding f<strong>or</strong> education, publication <strong>or</strong> research purposes, written consent must<br />
be sought, ensuring that the person giving consent is fully aware of the possible uses of the<br />
material. In particular, the person must be made aware that the health professional may not be<br />
able <strong>to</strong> control future use of the material once it has been placed in the public domain.<br />
If a child is not willing f<strong>or</strong> a rec<strong>or</strong>ding <strong>to</strong> be used, you must not use it, even if a person with<br />
parental responsibility consents.<br />
Pho<strong>to</strong>graphic <strong>and</strong> video rec<strong>or</strong>dings, made f<strong>or</strong> treating <strong>or</strong> assessing a patient <strong>and</strong> from which<br />
there is no possibility that the patient might be recognised, may be used within the clinical<br />
setting f<strong>or</strong> education <strong>or</strong> research purposes without express consent from the patient, as long as<br />
this policy is well publicised. However, express consent must be sought f<strong>or</strong> any f<strong>or</strong>m of<br />
publication.<br />
Page 16 of 64
Pho<strong>to</strong>graphic <strong>or</strong> video rec<strong>or</strong>dings of a patient made specifically f<strong>or</strong> education,<br />
publication <strong>or</strong> research purposes require written consent of the patient (<strong>or</strong> where appropriate<br />
of a person with parental responsibility) f<strong>or</strong> the rec<strong>or</strong>ding <strong>to</strong> be made <strong>and</strong> f<strong>or</strong> it <strong>to</strong> be used.<br />
Patients must know that they are free <strong>to</strong> s<strong>to</strong>p the rec<strong>or</strong>ding at any time <strong>and</strong> that they are entitled<br />
<strong>to</strong> view it if they wish, bef<strong>or</strong>e deciding whether <strong>to</strong> give consent <strong>to</strong> its use. If the patient decides<br />
that they are not happy f<strong>or</strong> any rec<strong>or</strong>ding <strong>to</strong> be used, it must be destroyed. As with rec<strong>or</strong>dings<br />
made with therapeutic intent, patients must receive full inf<strong>or</strong>mation on the possible future uses<br />
of the rec<strong>or</strong>ding, including the fact that it may not be possible <strong>to</strong> withdraw it once it is in the<br />
public domain.<br />
The situation may sometimes arise where you wish <strong>to</strong> make a rec<strong>or</strong>ding specifically f<strong>or</strong><br />
education, publication <strong>or</strong> research purposes, but the patient is temp<strong>or</strong>arily unable <strong>to</strong> give <strong>or</strong><br />
withhold consent, f<strong>or</strong> example they are unconscious. In such cases, a rec<strong>or</strong>ding may be made,<br />
but consent must be given as soon as the patient regains capacity. The rec<strong>or</strong>ding must not be<br />
used until consent has been received, <strong>and</strong> if the patient does not consent <strong>to</strong> any f<strong>or</strong>m of use,<br />
the rec<strong>or</strong>ding must be destroyed.<br />
Professional liability<br />
Doc<strong>to</strong>rs <strong>and</strong> other health professionals involved in the administration of immunisation are<br />
usually not negligent if acting within their competencies <strong>and</strong> within practice that conf<strong>or</strong>ms <strong>to</strong> that<br />
of a responsible body of medical opinion held by practitioners skilled in the field in question 1,2<br />
However, the courts are willing <strong>to</strong> be critical of a ‘responsible body’ of medical opinion <strong>and</strong> will<br />
be the final arbiters of what constitutes responsible practice.<br />
NB: This summary cannot cover all situations. F<strong>or</strong> m<strong>or</strong>e detail, please see the ‘Reference guide<br />
<strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong> treatment’, (F<strong>or</strong> details of access <strong>to</strong> the guide please see<br />
Appendix A).<br />
TRAINING<br />
The PCT will ensure that all members of staff receive the level of training necessary f<strong>or</strong> them <strong>to</strong><br />
fulfill their individual responsibilities identified in this policy.<br />
IMPLEMENTATION, MONITORING AND REVIEW<br />
The Governance Assurance Committee will moni<strong>to</strong>r the implementation of this policy. All<br />
revisions <strong>to</strong> the document must be agreed through the PCT policy approval process.<br />
Page 17 of 64
DOCUMENTATION<br />
Related policies <strong>and</strong> procedures<br />
This document should be read in conjunction with:<br />
Accident <strong>and</strong> Incident Rep<strong>or</strong>ting <strong>and</strong> Management <strong>Policy</strong><br />
Comments, Concerns <strong>and</strong> Complaints <strong>Policy</strong><br />
Confidential Code f<strong>or</strong> Rep<strong>or</strong>ting (Whistle blowing)<br />
Health <strong>and</strong> Safety <strong>Policy</strong><br />
<strong>Consent</strong> <strong>to</strong> intimate treatment <strong>and</strong> Chaperoning <strong>Policy</strong><br />
Mental Capacity Act <strong>Policy</strong><br />
Page 18 of 64
REFERENCES<br />
Reference<br />
National Health Service Litigation Auth<strong>or</strong>ity<br />
Directions 2005<br />
Relevance (whole<br />
document <strong>or</strong> section,<br />
please state)<br />
Whole<br />
Evidence Grade<br />
NHS guidance<br />
NHS Hal<strong>to</strong>n & <strong>St</strong> <strong>Helens</strong> Mental Capacity Act<br />
<strong>Policy</strong> (2006)<br />
Whole<br />
Trust policy<br />
DoH ‘Good Practice in <strong>Consent</strong>: Achieving the<br />
NHS Plan Commitment <strong>to</strong> Patient-Centred<br />
<strong>Consent</strong> Practice’ (HSC 2001/023)<br />
Whole<br />
DoH guidance<br />
DoH – Good Practice in <strong>Consent</strong><br />
Implementation Guide: <strong>Consent</strong> <strong>to</strong> <strong>Examination</strong><br />
<strong>or</strong> <strong>Treatment</strong> Nov 2001<br />
Whole<br />
DOH guidance<br />
DoH ‘ Seeking consent: W<strong>or</strong>king with children’<br />
2001<br />
Whole<br />
DoH guidance<br />
DoH ‘ Seeking consent: W<strong>or</strong>king with Older<br />
People’ 2001<br />
Whole<br />
DoH guidance<br />
DoH ‘ Seeking consent: W<strong>or</strong>king with people<br />
with learning disabilities’ 2001<br />
Whole<br />
DoH guidance<br />
DoH ‘ <strong>St</strong><strong>and</strong>ards f<strong>or</strong> Better Health’ Feb 2004 Whole DoH guidance<br />
DoH ‘ Code of Practice f<strong>or</strong> Mental Capacity Act<br />
2005<br />
General Medical Council ‘ Seeking Patient’s<br />
consent: the ethical considerations ( Nov 1998)<br />
Practice Note (Official Solici<strong>to</strong>r: Declara<strong>to</strong>ry<br />
Proceedings: Medical <strong>and</strong> Welfare Decisions f<strong>or</strong><br />
Adults Who Lack Capacity) 2006<br />
Whole<br />
Whole<br />
Whole<br />
DoH guidance<br />
GMC guidance<br />
Page 19 of 64
Relevant links<br />
The following documents have been used as guidance in compiling the policy.<br />
http://www.dh.gov.uk/<strong>Policy</strong><strong>and</strong>Guidance/HealthAndSocialCareTopics/<strong>Consent</strong>/<strong>Consent</strong>Genera<br />
lInf<strong>or</strong>mation/fs/en<br />
Page 20 of 64
APPENDIX 1<br />
Access <strong>to</strong> Useful Reference Documents<br />
1. Reference guide <strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong> treatment<br />
This provides a comprehensive summary of the current law on consent, <strong>and</strong> includes<br />
requirements of regula<strong>to</strong>ry bodies such as the General Medical Council where these are<br />
m<strong>or</strong>e stringent.<br />
Copies are available from the NHS Response Line 0541-555-455 may also be accessed on<br />
the internet at:<br />
http://www.dh.gov.uk/<strong>Policy</strong><strong>and</strong>Guidance/HealthAndSocialCareTopics/<strong>Consent</strong>/<strong>Consent</strong>Ge<br />
neralInf<strong>or</strong>mation/fs/en.<br />
2. 12 key points on consent: the law in Engl<strong>and</strong><br />
This has been distributed widely <strong>to</strong> health professionals w<strong>or</strong>king in Engl<strong>and</strong>. This one-page<br />
document summarises those aspects of the law on consent which arise on a daily basis<br />
<strong>and</strong> is attached at Appendix B. Further copies are available from www.doh.gov.uk/consent.<br />
3. Specific guidance, inc<strong>or</strong>p<strong>or</strong>ating both the law <strong>and</strong> good practice advice, is available f<strong>or</strong><br />
health professionals w<strong>or</strong>king with children, with people with learning disabilities <strong>and</strong> with<br />
older people. Copies of these booklets are available on the Internet at<br />
www.doh.gov.uk/consent.<br />
Page 21 of 64
APPENDIX 2<br />
12 Key Points on <strong>Consent</strong>: The Law in Engl<strong>and</strong><br />
When do health professionals need consent from patients?<br />
1. Bef<strong>or</strong>e you examine, treat <strong>or</strong> care f<strong>or</strong> competent adult patients you must obtain their<br />
consent.<br />
2. Adults are always assumed <strong>to</strong> be competent unless demonstrated otherwise. If you have<br />
doubts about their competence, the question <strong>to</strong> ask is: “can this patient underst<strong>and</strong> <strong>and</strong><br />
weigh up the inf<strong>or</strong>mation needed <strong>to</strong> make this decision? Unexpected decisions do not<br />
prove the patient is incompetent, but may indicate a need f<strong>or</strong> further inf<strong>or</strong>mation <strong>or</strong><br />
explanation.<br />
3. Patients may be competent <strong>to</strong> make some health care decisions, even if they are not<br />
competent <strong>to</strong> make others.<br />
4. Giving <strong>and</strong> obtaining consent is usually a process, not a one-off event. Patients can<br />
change their minds <strong>and</strong> withdraw consent at any time. If there is any doubt, you should<br />
always check that the patient still consents <strong>to</strong> your caring f<strong>or</strong> <strong>or</strong> treating them.<br />
Can children give consent f<strong>or</strong> themselves?<br />
5. Bef<strong>or</strong>e examining, treating <strong>or</strong> caring f<strong>or</strong> a child, you must also seek consent. Young<br />
people aged 16 <strong>and</strong> 17 are presumed <strong>to</strong> have the competence <strong>to</strong> give consent f<strong>or</strong><br />
themselves. Younger children who underst<strong>and</strong> fully what is involved in the proposed<br />
procedure can also give consent (although their parents will ideally be involved). In other<br />
cases, some one with parental responsibility must give consent on the child’s behalf,<br />
unless they cannot be reached in an emergency. If a competent child consents <strong>to</strong><br />
treatment, a parent cannot over-ride that consent. Legally, a parent can consent if a<br />
competent child refuses, but it is likely that taking such a serious step will be rare.<br />
Who is the right person <strong>to</strong> seek consent?<br />
6. It is always best f<strong>or</strong> the person actually treating the patient <strong>to</strong> seek the patient’s consent.<br />
However, you may seek consent on behalf of colleagues if you are capable of perf<strong>or</strong>ming<br />
the procedure in question, <strong>or</strong> if you have been specially trained <strong>to</strong> seek consent f<strong>or</strong> that<br />
procedure.<br />
What inf<strong>or</strong>mation should be provided?<br />
7. Patients need sufficient inf<strong>or</strong>mation bef<strong>or</strong>e they can decide whether <strong>to</strong> give their consent,<br />
e.g. inf<strong>or</strong>mation about the benefits <strong>and</strong> risks of the proposed treatment, <strong>and</strong> alternative<br />
Page 22 of 64
8. <strong>Consent</strong> must be given voluntarily: not under any f<strong>or</strong>m of duress <strong>or</strong> undue influence from<br />
health professionals, family <strong>or</strong> friends.<br />
Does it matter how the patient gives consent?<br />
9. No: consent can be written, verbal <strong>or</strong> non-verbal. A signature on a consent f<strong>or</strong>m does not<br />
itself prove the consent is valid – the point of the f<strong>or</strong>m is <strong>to</strong> rec<strong>or</strong>d the patient’s decision,<br />
<strong>and</strong> also increasingly the discussions that have taken place. This inf<strong>or</strong>mation could also<br />
be rec<strong>or</strong>ded electronically on the practice clinical system.<br />
Refusal of treatment<br />
10. Competent adult patients are entitled <strong>to</strong> refuse treatment, even when it would clearly<br />
benefit their health. The only exception <strong>to</strong> this rule is where the treatment is f<strong>or</strong> a mental<br />
dis<strong>or</strong>der <strong>and</strong> the patient is detained under the Mental Health Act 1983. A competent<br />
pregnant woman may refuse any treatment, even if this would be detrimental <strong>to</strong> the fetus.<br />
Adults who are not competent <strong>to</strong> give consent<br />
11. No-one can give consent on behalf of an incompetent adult. However, you may still treat<br />
such a patient if the treatment would be in their best interests. ‘Best interests’ go wider<br />
than best medical interests, <strong>to</strong> include fac<strong>to</strong>rs such as the wishes <strong>and</strong> beliefs of the<br />
patient when competent, their current wishes, their general well being <strong>and</strong> their spiritual<br />
<strong>and</strong> religious welfare. People close <strong>to</strong> the patient may be able <strong>to</strong> give you inf<strong>or</strong>mation on<br />
some of these fac<strong>to</strong>rs. Where the patient has never been competent, relatives, carers<br />
<strong>and</strong> friends may be best placed <strong>to</strong> advise on the patient’s needs <strong>and</strong> preferences.<br />
12. If an incompetent patient has clearly indicated in the past, while competent, that they<br />
would refuse treatment in certain circumstances (an ‘advance refusal’), <strong>and</strong> those<br />
circumstances arise, you must abide by that refusal.<br />
This summary cannot cover all situations. F<strong>or</strong> m<strong>or</strong>e detail, consult the Assistant Direc<strong>to</strong>r<br />
of C<strong>or</strong>p<strong>or</strong>ate Services on 01928 593726, <strong>or</strong> Operational Direc<strong>to</strong>r of Nursing <strong>and</strong> Clinical<br />
Governance 01744 457 221 <strong>or</strong> refer <strong>to</strong> Reference guide <strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong><br />
treatment, available from the NHS Response Line 08701 555 455 <strong>and</strong> at<br />
www.doh.gov.uk/consent.<br />
Page 23 of 64
APPENDIX 3<br />
Click here <strong>to</strong> download <strong>and</strong> use the f<strong>or</strong>m <strong>and</strong> guidelines<br />
<strong>Consent</strong> F<strong>or</strong>m 1<br />
Patient agreement <strong>to</strong> investigation<br />
Or treatment<br />
Patient details (<strong>or</strong> pre-printed label)<br />
Patient’s surname/family name.………………………….<br />
Patient’s first names.……………………………………….<br />
Date of birth ………………………………………………….<br />
Responsible health professional.……………………………<br />
Job title ……………………………………………………….<br />
NHS number (<strong>or</strong> other identifier)……………………………..<br />
Male<br />
Female<br />
Special requirements ………………………………………<br />
(E.g. other language/other communication method)<br />
To be retained in patient’s notes<br />
Page 24 of 64
Patient identifier/label<br />
Name of proposed procedure <strong>or</strong> course of treatment (include brief explanation if medical<br />
term not clear) ……………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………<br />
<strong>St</strong>atement of health professional (<strong>to</strong> be filled in by health professional with appropriate<br />
knowledge of proposed procedure, as specified in consent policy)<br />
I have explained the procedure <strong>to</strong> the patient. In particular, I have explained:<br />
The intended benefits ……………………………………………………………..……….………<br />
………………………………………………………………………………………<br />
Serious <strong>or</strong> frequently occurring risks ……………………………………………...………………<br />
...…………………………………………………………………………………..<br />
Any extra procedures which may become necessary during the procedure<br />
Blood transfusion…………………………………..…….……………………<br />
Other procedure (please specify) ………………………………...……...……<br />
…………………………………………………………………………...…………<br />
I have also discussed what the procedure is likely <strong>to</strong> involve, the benefits <strong>and</strong> risks of any<br />
available alternative treatments (including no treatment) <strong>and</strong> any particular concerns of this<br />
patient.<br />
The following leaflet/tape has been provided ……………….…………………………..…<br />
This procedure will involve:<br />
General <strong>and</strong>/<strong>or</strong> regional anaesthesia local anaesthesia sedation<br />
Signed: ….……………………………………<br />
Name (PRINT) ………………………. ………<br />
Date ……………………….……….<br />
Job title …….. …………<br />
Contact details (if patient wishes <strong>to</strong> discuss options later) …..……………..<br />
Page 25 of 64
<strong>St</strong>atement of interpreter (where appropriate)<br />
I have interpreted the inf<strong>or</strong>mation above <strong>to</strong> the patient <strong>to</strong> the best of my ability <strong>and</strong> in a way in<br />
which I believe s/he can underst<strong>and</strong>.<br />
Signed ………………………….……………………. Date ………………..…………….<br />
Name (PRINT) …………………..………………………………………………………………<br />
Top copy accepted by patient: yes/no (please ring)<br />
Page 26 of 64
<strong>St</strong>atement of patient<br />
Patient identifier/label<br />
Please read this f<strong>or</strong>m carefully. If your treatment has been planned in advance, you should<br />
already have your own copy of page 2 which describes the benefits <strong>and</strong> risks of the proposed<br />
treatment. If not, you will be offered a copy now. If you have any further questions, do ask – we<br />
are here <strong>to</strong> help you. You have the right <strong>to</strong> change your mind at any time, including after you<br />
have signed this f<strong>or</strong>m.<br />
I agree <strong>to</strong> the procedure <strong>or</strong> course of treatment described on this f<strong>or</strong>m.<br />
I underst<strong>and</strong> that you cannot give me a guarantee that a particular person will perf<strong>or</strong>m the<br />
procedure. The person will, however, have appropriate experience.<br />
I underst<strong>and</strong> that I will have the opp<strong>or</strong>tunity <strong>to</strong> discuss the details of anaesthesia with an<br />
anaesthetist bef<strong>or</strong>e the procedure, unless the urgency of my situation prevents this. (This only<br />
applies <strong>to</strong> patients having general <strong>or</strong> regional anaesthesia.)<br />
I underst<strong>and</strong> that any procedure in addition <strong>to</strong> those described on this f<strong>or</strong>m will only be carried<br />
out if it is necessary <strong>to</strong> save my life <strong>or</strong> <strong>to</strong> prevent serious harm <strong>to</strong> my health.<br />
I have been <strong>to</strong>ld about additional procedures which may become necessary during my<br />
treatment. I have listed below any procedures which I do not wish <strong>to</strong> be carried out without<br />
further discussion.<br />
………………………………………………………………………………………………….……………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………<br />
Patient’s signature …………………………………… Date………………………………<br />
Name (PRINT) ………………………………………………………………………………<br />
A witness should sign below if the patient is unable <strong>to</strong> sign but has indicated his <strong>or</strong> her consent.<br />
Young people/children may also like a parent <strong>to</strong> sign here (see notes).<br />
Signature ……………………………………… Date ……………………..….……………<br />
Name (PRINT) ………………………………………………………………………………<br />
Confirmation of consent (<strong>to</strong> be completed by a health professional when the patient is<br />
admitted f<strong>or</strong> the procedure, if the patient has signed the f<strong>or</strong>m in advance)<br />
On behalf of the team treating the patient, I have confirmed with the patient that s/he has no<br />
further questions <strong>and</strong> wishes the procedure <strong>to</strong> go ahead.<br />
Page 27 of 64
Signed: …….……………………………………<br />
Name (PRINT) ………………………. ………<br />
Date... …………………….……….<br />
Job title …….. ………………….…<br />
Imp<strong>or</strong>tant notes: (tick if applicable)<br />
See also advance directive/living will (e.g. Jehovah’s Witness f<strong>or</strong>m)<br />
Patient has withdrawn consent (ask patient <strong>to</strong> sign /date here) ……………...……….<br />
Page 28 of 64
Guidance <strong>to</strong> health professionals (<strong>to</strong> be read in conjunction with consent policy)<br />
What a consent f<strong>or</strong>m is f<strong>or</strong><br />
This f<strong>or</strong>m documents the patient’s agreement <strong>to</strong> go ahead with the investigation <strong>or</strong> treatment<br />
you have proposed. It is not a legal waiver – if patients, f<strong>or</strong> example, do not receive enough<br />
inf<strong>or</strong>mation on which <strong>to</strong> base their decision, then the consent may not be valid, even though the<br />
f<strong>or</strong>m has been signed. Patients are also entitled <strong>to</strong> change their mind after signing the f<strong>or</strong>m, if<br />
they retain capacity <strong>to</strong> do so. The f<strong>or</strong>m should act as an aide-memoire <strong>to</strong> health professionals<br />
<strong>and</strong> patients, by providing a check-list of the kind of inf<strong>or</strong>mation patients should be offered, <strong>and</strong><br />
by enabling the patient <strong>to</strong> have a written rec<strong>or</strong>d of the main points discussed. In no way,<br />
however, should the written inf<strong>or</strong>mation provided f<strong>or</strong> the patient is regarded as a substitute f<strong>or</strong><br />
face-<strong>to</strong>-face discussions with the patient.<br />
The law on consent<br />
See the Department of Health’s Reference guide <strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong> treatment f<strong>or</strong> a<br />
comprehensive summary of the law on consent (also available at www.doh.gov.uk/consent).<br />
Who can give consent?<br />
Everyone aged 16 <strong>or</strong> m<strong>or</strong>e is presumed <strong>to</strong> be competent <strong>to</strong> give consent f<strong>or</strong> themselves, unless<br />
the opposite is demonstrated. If a child under the age of 16 has “sufficient underst<strong>and</strong>ing <strong>and</strong><br />
intelligence <strong>to</strong> enable him <strong>or</strong> her <strong>to</strong> underst<strong>and</strong> fully what is proposed”, then he <strong>or</strong> she will be<br />
competent <strong>to</strong> give consent f<strong>or</strong> him <strong>or</strong> herself. Young people aged 16 <strong>and</strong> 17, <strong>and</strong> legally<br />
‘competent’ younger children, may theref<strong>or</strong>e sign this f<strong>or</strong>m f<strong>or</strong> themselves, but may like a parent<br />
<strong>to</strong> countersign as well. If the child is not able <strong>to</strong> give consent f<strong>or</strong> him <strong>or</strong> herself, some-one with<br />
parental responsibility may do so on their behalf <strong>and</strong> a separate f<strong>or</strong>m is available f<strong>or</strong> this<br />
purpose. Even where a child is able <strong>to</strong> give consent f<strong>or</strong> him <strong>or</strong> herself, you should always<br />
involve those with parental responsibility in the child’s care, unless the child specifically asks<br />
you not <strong>to</strong> do so. If a patient is mentally competent <strong>to</strong> give consent but is physically unable <strong>to</strong><br />
sign a f<strong>or</strong>m, you should complete this f<strong>or</strong>m as usual, <strong>and</strong> ask an independent witness <strong>to</strong> confirm<br />
that the patient has given consent <strong>or</strong>ally <strong>or</strong> non-verbally.<br />
When NOT <strong>to</strong> use this f<strong>or</strong>m<br />
If the patient is 18 <strong>or</strong> over <strong>and</strong> is not legally competent <strong>to</strong> give consent, you should use the prof<strong>or</strong>ma f<strong>or</strong><br />
adults who are unable <strong>to</strong> consent <strong>to</strong> investigation <strong>or</strong> treatment) instead of this f<strong>or</strong>m. A patient will not be<br />
legally competent <strong>to</strong> give consent if:<br />
they are unable <strong>to</strong> comprehend <strong>and</strong> retain inf<strong>or</strong>mation material <strong>to</strong> the decision <strong>and</strong>/<strong>or</strong><br />
They are unable <strong>to</strong> weigh <strong>and</strong> use this inf<strong>or</strong>mation in coming <strong>to</strong> a decision.<br />
You should always take all reasonable steps (f<strong>or</strong> example involving m<strong>or</strong>e specialist colleagues) <strong>to</strong><br />
supp<strong>or</strong>t a patient in making their own decision, bef<strong>or</strong>e concluding that they are unable <strong>to</strong> do so.<br />
Relatives cannot be asked <strong>to</strong> sign this f<strong>or</strong>m on behalf of an adult who is not legally competent <strong>to</strong><br />
consent f<strong>or</strong> him <strong>or</strong> herself.<br />
Page 29 of 64
Inf<strong>or</strong>mation<br />
Inf<strong>or</strong>mation about what the treatment will involve, its benefits <strong>and</strong> risks (including side-effects<br />
<strong>and</strong> complications) <strong>and</strong> the alternatives <strong>to</strong> the particular procedure proposed, is crucial f<strong>or</strong><br />
patients when making up their minds. The courts have stated that patients should be <strong>to</strong>ld about<br />
‘significant risks which would affect the judgement of a reasonable patient’. ‘Significant’ has not<br />
been legally defined, but the GMC requires doc<strong>to</strong>rs <strong>to</strong> tell patients about ‘serious <strong>or</strong> frequently<br />
occurring’ risks. In addition if patients make clear they have particular concerns about certain<br />
kinds of risk, you should make sure they are inf<strong>or</strong>med about these risks, even if they are very<br />
small <strong>or</strong> rare. You should always answer questions honestly. Sometimes, patients may make it<br />
clear that they do not want <strong>to</strong> have any inf<strong>or</strong>mation about the options, but want you <strong>to</strong> decide on<br />
their behalf. In such circumstances, you should do your best <strong>to</strong> ensure that the patient receives<br />
at least very basic inf<strong>or</strong>mation about what is proposed. Where inf<strong>or</strong>mation is refused, you<br />
should document this on page 2 of the f<strong>or</strong>m <strong>or</strong> in the patient’s notes.<br />
Page 30 of 64
APPENDIX 4<br />
Click here <strong>to</strong> download <strong>and</strong> use the f<strong>or</strong>m <strong>and</strong> guidelines<br />
<strong>Consent</strong> F<strong>or</strong>m 2<br />
Parental agreement <strong>to</strong> investigation <strong>or</strong><br />
<strong>Treatment</strong> f<strong>or</strong> a child <strong>or</strong> young person<br />
Patient details (<strong>or</strong> pre-printed label)<br />
Patient’s surname/family name.………………………….<br />
Patient’s first names.……………………………………….<br />
Date of birth ………………………………………………….<br />
Age …………………………………………………………….<br />
Responsible health professional.……………………………<br />
Job title ……………………………………………………….<br />
NHS number (<strong>or</strong> other identifier)……………………………..<br />
Male<br />
Female<br />
Special requirements ………………………………………<br />
(E.g. other language/other communication method)<br />
To be retained in patient’s notes<br />
Page 31 of 64
Patient identifier/label<br />
Name of proposed procedure <strong>or</strong> course of treatment (include brief explanation if medical<br />
term not clear) ……………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………<br />
<strong>St</strong>atement of health professional (<strong>to</strong> be filled in by health professional with appropriate<br />
knowledge of proposed procedure, as specified in consent policy)<br />
I have explained the procedure <strong>to</strong> the child <strong>and</strong> his <strong>or</strong> her parent(s). In particular, I have<br />
explained:<br />
The intended benefits ……………………………………………………………..……….………<br />
…………………………………………………………..…………………………..……………<br />
Serious <strong>or</strong> frequently occurring risks ……………………………………………...………………<br />
...………………………………………………………………………………………….………<br />
………………………………….………………………………………………..………………<br />
Any extra procedures which may become necessary during the procedure<br />
Blood transfusion…………………………………..…….…………………………………<br />
Other procedure (please specify) ………………………………...……...…………….…..<br />
…………………………………………………………………………………………………..<br />
I have also discussed what the procedure is likely <strong>to</strong> involve, the benefits <strong>and</strong> risks of any<br />
available alternative treatments (including no treatment) <strong>and</strong> any particular concerns of this<br />
patient <strong>and</strong> his <strong>or</strong> her parents.<br />
The following leaflet/tape has been provided ……………….…………………………..<br />
This procedure will involve:<br />
General <strong>and</strong>/<strong>or</strong> regional anaesthesia local anaesthesia sedation<br />
Signed: ….……………………………………<br />
Name (PRINT) ………………………. ………<br />
Date... …………………….……….<br />
Job title …….. ………………….…<br />
Contact details (if child/parent wish <strong>to</strong> discuss options later) ……………….……………<br />
Page 32 of 64
<strong>St</strong>atement of interpreter (where appropriate)<br />
I have interpreted the inf<strong>or</strong>mation above <strong>to</strong> the child <strong>and</strong> his <strong>or</strong> her parents <strong>to</strong> the best of my<br />
ability <strong>and</strong> in a way in which I believe they can underst<strong>and</strong>.<br />
Signed ………………………….……………………. Date ………………..…………….<br />
Name (PRINT) …………………..………………………………………………………………<br />
Top copy accepted by patient: yes/no (please ring)<br />
Page 33 of 64
<strong>St</strong>atement of parent<br />
Patient identifier/label<br />
Please read this f<strong>or</strong>m carefully. If the procedure has been planned in advance, you should<br />
already have your own copy of page 2 which describes the benefits <strong>and</strong> risks of the proposed<br />
treatment. If not, you will be offered a copy now. If you have any further questions, do ask – we<br />
are here <strong>to</strong> help you <strong>and</strong> your child. You have the right <strong>to</strong> change your mind at any time,<br />
including after you have signed this f<strong>or</strong>m.<br />
I agree <strong>to</strong> the procedure <strong>or</strong> course of treatment described on this f<strong>or</strong>m <strong>and</strong> I confirm that I have<br />
‘parental responsibility’ f<strong>or</strong> this child.<br />
I underst<strong>and</strong> that you cannot give me a guarantee that a particular person will perf<strong>or</strong>m the<br />
procedure. The person will, however, have appropriate experience.<br />
I underst<strong>and</strong> that my child <strong>and</strong> I will have the opp<strong>or</strong>tunity <strong>to</strong> discuss the details of anaesthesia<br />
with an anaesthetist bef<strong>or</strong>e the procedure, unless the urgency of the situation prevents this.<br />
(This only applies <strong>to</strong> children having general <strong>or</strong> regional anaesthesia.)<br />
I underst<strong>and</strong> hat any procedure in addition <strong>to</strong> those described on this f<strong>or</strong>m will only be carried<br />
out if it is necessary <strong>to</strong> save the life of my child <strong>or</strong> <strong>to</strong> prevent serious harm <strong>to</strong> his <strong>or</strong> her health.<br />
I have been <strong>to</strong>ld about additional procedures which may become necessary during my child’s<br />
treatment. I have listed below any procedures which I do not wish <strong>to</strong> be carried out without<br />
further discussion. ……………………………………………………………………..<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………<br />
Signature …………………………………………Date……………………………………….<br />
Name (PRINT) …………………………………Relationship <strong>to</strong> child………………………<br />
Child’s agreement <strong>to</strong> treatment (if child wishes <strong>to</strong> sign)<br />
I agree <strong>to</strong> have the treatment I have been <strong>to</strong>ld about.<br />
Name ……………………………………………Signature ……………………..….……<br />
Date ………………………………………………………………………………….…….<br />
Confirmation of consent (<strong>to</strong> be completed by a health professional when the child is admitted<br />
f<strong>or</strong> the procedure, if the parent/child has signed the f<strong>or</strong>m in advance)<br />
Page 34 of 64
On behalf of the team treating the patient, I have confirmed with the child <strong>and</strong> his <strong>or</strong> her<br />
parent(s) that they have no further questions <strong>and</strong> wish the procedure <strong>to</strong> go ahead.<br />
Signed: …….……………………………………<br />
Name (PRINT) ………………………. ………<br />
Date…………………….……….<br />
Job title …….. ………………….…<br />
Imp<strong>or</strong>tant notes: (tick if applicable)<br />
See also advance directive/living will (e.g. Jehovah’s Witness f<strong>or</strong>m)<br />
Parent has withdrawn consent (ask parent <strong>to</strong> sign /date here) ……………...…<br />
Page 35 of 64
Guidance <strong>to</strong> health professionals (<strong>to</strong> be read in conjunction with consent policy)<br />
This f<strong>or</strong>m<br />
This f<strong>or</strong>m should be used <strong>to</strong> document consent <strong>to</strong> a child’s treatment, where that consent is<br />
being given by a person with parental responsibility f<strong>or</strong> the child. The term ‘parent’ has been<br />
used in this f<strong>or</strong>m as sh<strong>or</strong>th<strong>and</strong> f<strong>or</strong> ‘person with parental responsibility’. Where children are<br />
legally competent <strong>to</strong> consent f<strong>or</strong> themselves (see below), they may sign the st<strong>and</strong>ard ‘adult’<br />
consent f<strong>or</strong>m (f<strong>or</strong>m 1). There is space on that f<strong>or</strong>m f<strong>or</strong> a parent <strong>to</strong> countersign if a competent<br />
child wishes them <strong>to</strong> do so.<br />
Who can give consent?<br />
Everyone aged 16 <strong>or</strong> m<strong>or</strong>e is presumed <strong>to</strong> be competent <strong>to</strong> give consent f<strong>or</strong> themselves, unless<br />
the opposite is demonstrated. The courts have stated that if a child under the age of 16 has<br />
“sufficient underst<strong>and</strong>ing <strong>and</strong> intelligence <strong>to</strong> enable him <strong>or</strong> her <strong>to</strong> underst<strong>and</strong> fully what is<br />
proposed”, then he <strong>or</strong> she will be competent <strong>to</strong> give consent f<strong>or</strong> him <strong>or</strong> herself. If children are<br />
not able <strong>to</strong> give consent f<strong>or</strong> themselves, some-one with parental responsibility may do so on<br />
their behalf.<br />
Although children acquire rights <strong>to</strong> give consent f<strong>or</strong> themselves as they grow older, people with<br />
‘parental responsibility’ f<strong>or</strong> a child retain the right <strong>to</strong> give consent on the child’s behalf until the<br />
child reaches the age of 18. Theref<strong>or</strong>e, f<strong>or</strong> a number of years, both the child <strong>and</strong> a person with<br />
parental responsibility have the right <strong>to</strong> give consent <strong>to</strong> the child’s treatment. In law, health<br />
professionals only need the consent of one appropriate person bef<strong>or</strong>e providing treatment. This<br />
means that in the<strong>or</strong>y it is lawful <strong>to</strong> provide treatment <strong>to</strong> a child under 18 which a person with<br />
parental responsibility has auth<strong>or</strong>ised, even if the child refuses. As a matter of good practice,<br />
however, you should always seek a competent child’s consent bef<strong>or</strong>e providing treatment<br />
unless any delay involved in doing so would put the child’s life <strong>or</strong> health at risk. Younger<br />
children should also be as involved as possible in decisions about their healthcare. Further<br />
advice is given in the Department’s guidance seeking consent: w<strong>or</strong>king with children. Any<br />
differences of opinion between the child <strong>and</strong> their parents, <strong>or</strong> between parents, should be<br />
clearly documented in the patient’s notes.<br />
Parental responsibility<br />
The person(s) with parental responsibility will usually, but not invariably, be the child’s birth parents.<br />
People with parental responsibility f<strong>or</strong> a child include: the child’s mother; the child’s father if married <strong>to</strong><br />
the mother at the child’s conception, birth <strong>or</strong> later; a legally appointed guardian; the local auth<strong>or</strong>ity if the<br />
child is on a care <strong>or</strong>der; <strong>or</strong> a person named in a residence <strong>or</strong>der in respect of the child. Fathers who<br />
have never been married <strong>to</strong> the child’s mother will only have parental responsibility if they have acquired<br />
it through a court <strong>or</strong>der <strong>or</strong> parental responsibility agreement (although this may change in the future).<br />
Inf<strong>or</strong>mation<br />
Inf<strong>or</strong>mation about what the treatment will involve, its benefits <strong>and</strong> risks (including side-effects <strong>and</strong><br />
complications) <strong>and</strong> the alternatives <strong>to</strong> the particular procedure proposed, is crucial f<strong>or</strong> children <strong>and</strong> their<br />
parents when making up their minds about treatment. The courts have stated that patients should be<br />
<strong>to</strong>ld about ‘significant risks which would affect the judgement of a reasonable patient’. ‘Significant’ has<br />
not been legally defined, but the GMC requires doc<strong>to</strong>rs <strong>to</strong> tell patients about ‘serious <strong>or</strong> frequently<br />
Page 36 of 64
occurring’ risks. In addition if patients make clear they have particular concerns about certain kinds of<br />
risk, you should make sure they are inf<strong>or</strong>med about these risks, even if they are very small <strong>or</strong> rare. You<br />
should always answer questions honestly.<br />
Guidance on the law on consent<br />
See the Department of Health publications Reference guide <strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong> treatment <strong>and</strong> Seeking consent: w<strong>or</strong>king with children<br />
f<strong>or</strong> a comprehensive summary of the law on consent (also available at www.doh.gov.uk/consent).<br />
Page 37 of 64
APPENDIX 5<br />
Click here <strong>to</strong> download <strong>and</strong> use the f<strong>or</strong>m <strong>and</strong> guidelines<br />
<strong>Consent</strong> F<strong>or</strong>m 3<br />
Patient agreement <strong>to</strong> Investigation <strong>or</strong> <strong>Treatment</strong><br />
Patient details (<strong>or</strong> pre-printed label)<br />
Patient’s surname/family name………………………….<br />
Patient’s first names……………………………………….<br />
Date of birth ………………………………………………….<br />
Age …………………………………………………………….<br />
Responsible health professional.……………………………<br />
Job title ……………………………………………………….<br />
NHS number (<strong>or</strong> other identifier)……………………………..<br />
Male<br />
Female<br />
Special requirements ………………………………………<br />
(E.g. other language/other communication method)<br />
To be retained in patient’s notes<br />
Page 38 of 64
Patient/parental agreement <strong>to</strong> investigation <strong>or</strong> treatment<br />
(Procedures where consciousness not impaired)<br />
Name of procedure (include brief explanation if medical term not clear)<br />
………………………………………………………………………………………………………………<br />
…………………………………………………………………………………………<br />
<strong>St</strong>atement of health professional (<strong>to</strong> be filled in by health professional with appropriate<br />
knowledge of proposed procedure, as specified in consent policy)<br />
I have explained the procedure <strong>to</strong> the patient/parent. In particular, I have explained:<br />
The intended benefits …………………………………………………………………….…………<br />
……………………………………………………………………………………………………<br />
……………………………………………………………………………………………………<br />
Serious <strong>or</strong> frequently occurring risks:<br />
……………………………………………………….………………………………………<br />
...……………………………………………………………………………………………<br />
………………………………….…………………………………………………………………<br />
I have also discussed what the procedure is likely <strong>to</strong> involve, the benefits <strong>and</strong> risks of any<br />
available alternative treatments (including no treatment) <strong>and</strong> any particular concerns of those<br />
involved.<br />
The following leaflet/tape has been provided ……………………………………….……<br />
Signed: Date ……... ………………………………<br />
Name (PRINT) ………………………. ………. Job title ………………………………<br />
Page 39 of 64
<strong>St</strong>atement of interpreter (where appropriate)<br />
I have interpreted the inf<strong>or</strong>mation above <strong>to</strong> the patient/parent <strong>to</strong> the best of my ability <strong>and</strong> in a<br />
way in which I believe s/he/they can underst<strong>and</strong>.<br />
Signed ……………….……….Date…….…………..Name (PRINT)…………….…………………..<br />
<strong>St</strong>atement of patient/person with parental responsibility f<strong>or</strong> patient<br />
I agree <strong>to</strong> the procedure described above.<br />
I underst<strong>and</strong> that you cannot give me a guarantee that a particular person will perf<strong>or</strong>m the<br />
procedure. The person will, however, have appropriate experience.<br />
I underst<strong>and</strong> that the procedure will/will not involve local anaesthesia.<br />
Signature ……………………………………….<br />
Name (PRINT) …………………………………<br />
Date ……………………………..…<br />
Relationship <strong>to</strong> patient ……………<br />
Confirmation of consent (<strong>to</strong> be completed by a health professional when the patient is admitted f<strong>or</strong> the<br />
procedure, if the patient/parent has signed the f<strong>or</strong>m in advance)<br />
I have confirmed that the patient/parent has no further questions <strong>and</strong> wishes the procedure <strong>to</strong><br />
go ahead.<br />
Signed:<br />
Date ……... ………………<br />
Name (PRINT) ………………………..………..<br />
Job title ……………………<br />
Top copy accepted by patient: yes/no (please ring)<br />
Page 40 of 64
Guidance <strong>to</strong> health professionals (<strong>to</strong> be read in conjunction with consent policy)<br />
This f<strong>or</strong>m<br />
This f<strong>or</strong>m documents the patient’s agreement (<strong>or</strong> that of a person with parental responsibility f<strong>or</strong><br />
the patient) <strong>to</strong> go ahead with the investigation <strong>or</strong> treatment you have proposed. It is only<br />
designed f<strong>or</strong> procedures where the patient is expected <strong>to</strong> remain alert throughout <strong>and</strong><br />
where an anaesthetist is not involved in their care: f<strong>or</strong> example f<strong>or</strong> drug therapy where<br />
written consent is deemed appropriate. In other circumstances you should use either f<strong>or</strong>m 1<br />
(f<strong>or</strong> adults/competent children) <strong>or</strong> f<strong>or</strong>m 2 (parental consent f<strong>or</strong> children/young people) as<br />
appropriate.<br />
<strong>Consent</strong> f<strong>or</strong>ms are not legal waivers – if patients, f<strong>or</strong> example, do not receive enough inf<strong>or</strong>mation on<br />
which <strong>to</strong> base their decision, then the consent may not be valid, even though the f<strong>or</strong>m has been signed.<br />
Patients also have every right <strong>to</strong> change their mind after signing the f<strong>or</strong>m.<br />
Who can give consent?<br />
Everyone aged 16 <strong>or</strong> m<strong>or</strong>e is presumed <strong>to</strong> be competent <strong>to</strong> give consent f<strong>or</strong> themselves, unless<br />
the opposite is demonstrated. If a child under the age of 16 has “sufficient underst<strong>and</strong>ing <strong>and</strong><br />
intelligence <strong>to</strong> enable him <strong>or</strong> her <strong>to</strong> underst<strong>and</strong> fully what is proposed”, then he <strong>or</strong> she will be<br />
competent <strong>to</strong> give consent f<strong>or</strong> him <strong>or</strong> herself. Young people aged 16 <strong>and</strong> 17, <strong>and</strong> legally<br />
‘competent’ younger children, may theref<strong>or</strong>e sign this f<strong>or</strong>m f<strong>or</strong> themselves, if they wish. If the<br />
child is not able <strong>to</strong> give consent f<strong>or</strong> him <strong>or</strong> herself, some-one with parental responsibility may do<br />
so on their behalf. Even where a child is able <strong>to</strong> give consent f<strong>or</strong> him <strong>or</strong> herself, you should<br />
always involve those with parental responsibility in the child’s care, unless the child specifically<br />
asks you not <strong>to</strong> do so. If a patient is mentally competent <strong>to</strong> give consent but is physically unable<br />
<strong>to</strong> sign a f<strong>or</strong>m, you should complete this f<strong>or</strong>m as usual, <strong>and</strong> ask an independent witness <strong>to</strong><br />
confirm that the patient has given consent <strong>or</strong>ally <strong>or</strong> non-verbally.<br />
When NOT <strong>to</strong> use this f<strong>or</strong>m (see also ‘This f<strong>or</strong>m’ above)<br />
If the patient is 18 <strong>or</strong> over <strong>and</strong> is not legally competent <strong>to</strong> give consent, you should use the clinical<br />
prof<strong>or</strong>ma f<strong>or</strong> adults who are unable <strong>to</strong> consent <strong>to</strong> investigation <strong>or</strong> treatment) instead of this f<strong>or</strong>m. A<br />
patient will not be legally competent <strong>to</strong> give consent if:<br />
they are unable <strong>to</strong> comprehend <strong>and</strong> retain inf<strong>or</strong>mation material <strong>to</strong> the decision <strong>and</strong>/<strong>or</strong><br />
They are unable <strong>to</strong> weigh <strong>and</strong> use this inf<strong>or</strong>mation in coming <strong>to</strong> a decision.<br />
You should always take all reasonable steps (f<strong>or</strong> example involving m<strong>or</strong>e specialist colleagues)<br />
<strong>to</strong> supp<strong>or</strong>t a patient in making their own decision, bef<strong>or</strong>e concluding that they are unable <strong>to</strong> do<br />
so. Relatives cannot be asked <strong>to</strong> sign this f<strong>or</strong>m on behalf of an adult who is not legally<br />
competent <strong>to</strong> consent f<strong>or</strong> him <strong>or</strong> herself.<br />
Inf<strong>or</strong>mation<br />
Inf<strong>or</strong>mation about what the treatment will involve, its benefits <strong>and</strong> risks (including side-effects<br />
<strong>and</strong> complications) <strong>and</strong> the alternatives <strong>to</strong> the particular procedure proposed, is crucial f<strong>or</strong><br />
patients when making up their minds about treatment. The courts have stated that patients<br />
should be <strong>to</strong>ld about ‘significant risks which would affect the judgement of a reasonable patient’.<br />
Page 41 of 64
‘Significant’ has not been legally defined, but the GMC requires doc<strong>to</strong>rs <strong>to</strong> tell patients about<br />
‘serious <strong>or</strong> frequently occurring’ risks. In addition if patients make clear they have particular<br />
concerns about certain kinds of risk, you should make sure they are inf<strong>or</strong>med about these risks,<br />
even if they are very small <strong>or</strong> rare. You should always answer questions honestly. Sometimes,<br />
patients may make it clear that they do not want <strong>to</strong> have any inf<strong>or</strong>mation about the options, but<br />
want you <strong>to</strong> decide on their behalf. In such circumstances, you should do your best <strong>to</strong> ensure<br />
that the patient receives at least very basic inf<strong>or</strong>mation about what is proposed. Where<br />
inf<strong>or</strong>mation is refused, you should document this overleaf <strong>or</strong> in the patient’s notes.<br />
The law on consent<br />
See the Department of Health’s Reference guide <strong>to</strong> consent f<strong>or</strong> examination <strong>or</strong> treatment f<strong>or</strong> a<br />
comprehensive summary of the law on consent (also available at www.doh.gov.uk/consent<br />
Page 42 of 64
APPENDIX 6<br />
Click here <strong>to</strong> download <strong>and</strong> use the f<strong>or</strong>m <strong>and</strong> guidelines<br />
<strong>Consent</strong> F<strong>or</strong>m 4<br />
F<strong>or</strong>m f<strong>or</strong> Adults who are unable <strong>to</strong> consent<br />
To investigation <strong>or</strong> treatment<br />
Patient details (<strong>or</strong> pre-printed label)<br />
Patient’s surname/family name.………………………….<br />
Patient’s first names.……………………………………….<br />
Date of birth ………………………………………………….<br />
Age …………………………………………………………….<br />
Responsible health professional.……………………………<br />
Job title ……………………………………………………….<br />
NHS number (<strong>or</strong> other identifier)……………………………..<br />
Male<br />
Female<br />
Special requirements ………………………………………<br />
(E.g. other language/other communication method)<br />
To be retained in patient’s notes<br />
Page 43 of 64
The Mental Capacity Act 2005 – Assessment <strong>and</strong> Documentation Guidelines<br />
Context:<br />
The Mental Capacity Act 2005 (the Act) provides the legal framew<strong>or</strong>k f<strong>or</strong> acting <strong>and</strong> making<br />
decisions on behalf of individuals who lack the mental capacity <strong>to</strong> make particular decisions<br />
f<strong>or</strong> them. Everyone w<strong>or</strong>king with <strong>and</strong>/<strong>or</strong> caring f<strong>or</strong> an adult who may lack capacity <strong>to</strong> make<br />
specific decisions must comply with this Act when making decisions <strong>or</strong> acting f<strong>or</strong> that person,<br />
when the person lacks the capacity <strong>to</strong> make a particular decision f<strong>or</strong> themselves. The same<br />
rules apply whether the decisions are life-changing events <strong>or</strong> everyday matters.<br />
The whole Act is underpinned by a set of five key principles set out in Section 1 of the<br />
Act:<br />
1. A presumption of capacity – every adult has the right <strong>to</strong> make his <strong>or</strong> her own decisions<br />
<strong>and</strong> must be assumed <strong>to</strong> have capacity <strong>to</strong> do so unless it is proved otherwise;<br />
2. Individuals being supp<strong>or</strong>ted <strong>to</strong> make their own decisions – a person must be given all<br />
practicable help bef<strong>or</strong>e anyone treats them as not being able <strong>to</strong> make their own<br />
decisions;<br />
3. Unwise decisions – just because an individual makes what might be seen as an unwise<br />
decision, they should not be treated as lacking capacity <strong>to</strong> make that decision;<br />
4. Best interests – an act done <strong>or</strong> decision made under the Act f<strong>or</strong> <strong>or</strong> on behalf of a person<br />
who lacks capacity must be done in their best interests; <strong>and</strong><br />
5. Least restrictive option – anything done f<strong>or</strong> <strong>or</strong> on behalf of a person who lacks capacity<br />
should be the least restrictive of their basic rights <strong>and</strong> freedoms.<br />
Who can decide if someone lacks capacity <strong>to</strong> make a particular decision?<br />
Since the legislation was passed on the 1 st Oc<strong>to</strong>ber 2007, it is the responsibility of everyone<br />
w<strong>or</strong>king with/ caring f<strong>or</strong> adults who may lack capacity, <strong>to</strong> make sure that they have considered the<br />
issues highlighted by the Act. This covers most of the staff who w<strong>or</strong>k f<strong>or</strong> the PCT.<br />
Anyone can complete an assessment <strong>to</strong> decide if a person has the capacity <strong>to</strong> make a particular<br />
decision. It is perhaps easier, <strong>and</strong> wherever possible, should be considered best practice <strong>to</strong> complete<br />
the process as part of a clearly documented multidisciplinary process, which gathers a wide range of<br />
views <strong>and</strong> clinical opinions.<br />
It is a statu<strong>to</strong>ry requirement f<strong>or</strong> staff w<strong>or</strong>king within the framew<strong>or</strong>k of the Mental Capacity Act<br />
2005 <strong>to</strong> have regard <strong>and</strong> make reference <strong>to</strong> the Mental Capacity Code of Practice. Those staff<br />
involved in assessments should be conversant with the Code of Practice, especially Chapter 3.<br />
Why do I need <strong>to</strong> fill out the f<strong>or</strong>m attached?<br />
Page 44 of 64
The Hal<strong>to</strong>n <strong>and</strong> <strong>St</strong>. Helen’s PCT pro f<strong>or</strong>ma is designed <strong>to</strong> ensure that there is a consistent approach <strong>to</strong><br />
documenting assessments <strong>and</strong> best interest decision making processes, across Community Health<br />
Services.<br />
The pro f<strong>or</strong>ma also ensures that the c<strong>or</strong>rect process has been followed, <strong>and</strong> that this can be referred <strong>to</strong><br />
at a later date, if needed.<br />
A f<strong>or</strong>m should be completed f<strong>or</strong> each individual decision that the patient is required <strong>to</strong> make an inf<strong>or</strong>med<br />
choice around. That is, just because a person lacks the capacity <strong>to</strong> decide about one thing, we cannot<br />
assume that they lack the capacity <strong>to</strong> make all other decisions. Each decision must be treated as<br />
individual, <strong>and</strong> an assessment carried out <strong>to</strong> establish the individual’s capacity <strong>to</strong> make that specific<br />
decision.<br />
It is also imp<strong>or</strong>tant <strong>to</strong> remember that capacity can fluctuate over time, (e.g.: dementia, psychosis etc.).<br />
Things can get better as well as w<strong>or</strong>se, so it is imp<strong>or</strong>tant <strong>to</strong> revisit capacity assessments, especially if<br />
there have been any significant clinical changes.<br />
All assessments, best interest meetings, meeting with family/ carers, discussions with other<br />
professionals, <strong>and</strong> other contacts related <strong>to</strong> the Act within the patients’ care should be rec<strong>or</strong>ded within<br />
the clinical notes, as per Trust <strong>Policy</strong> on Rec<strong>or</strong>dkeeping.<br />
The pro f<strong>or</strong>ma should be completed in conjunction with the Guidance Notes <strong>and</strong> reference <strong>to</strong> the Trust’s<br />
policy on Mental Capacity Act 2005, which is available on the intranet.<br />
Sources of Inf<strong>or</strong>mation:<br />
Inf<strong>or</strong>mation about the Mental Capacity Act 2005 can be found on the website below:<br />
http://www.dca.gov.uk/menincap/legis.htm<br />
The Code of Practice is available at the website below:<br />
http://www.dca.gov.uk/legal-policy/mental-capacity/mca-cp.pdf<br />
Contacts:<br />
Debbie Fairclough (Assistant Chief Executive)<br />
debbie.fairclough@hsthpct.nhs.uk<br />
Dr. Swati Chapman (Clinical Lead Mental Capacity Act) swati.chapman@hsthpct.nhs.uk<br />
Page 45 of 64
Mental Capacity Act 2005<br />
Patient’s Name :<br />
Pro-f<strong>or</strong>ma f<strong>or</strong> the Two-<strong>St</strong>age Test <strong>to</strong> Assess Capacity<br />
DOB:<br />
Address:<br />
Contact Number:<br />
GP(Name & Address) Gender: M F<br />
NHS Number:<br />
Ethnicity/ First Language:<br />
Key Roles<br />
Next of Kin<br />
<br />
N/A<br />
Lasting/<br />
Enduring<br />
Power of<br />
At<strong>to</strong>rney (LPA<br />
<strong>or</strong> EPA)<br />
<br />
N/A<br />
Independent<br />
Mental Health<br />
Advocate<br />
(IMCA)<br />
<br />
N/A<br />
Court of<br />
Protection<br />
Deputy<br />
(CPD)<br />
<br />
N/A<br />
Name<br />
Role<br />
Address<br />
Tel<br />
Details of the decision <strong>to</strong> be made:<br />
Dated:<br />
Key Roles<br />
Person conducting<br />
assessment<br />
Supp<strong>or</strong>ting Clinician (if<br />
applicable)<br />
Manager/ supervis<strong>or</strong><br />
Other (please detail)<br />
Name<br />
Role<br />
Address<br />
Tel<br />
Page 46 of 64
Assessment of Capacity<br />
1. Does the patient have impairment <strong>or</strong> a disturbance in the functioning of the mind <strong>or</strong> brain?<br />
Yes <br />
No <br />
(See guidance note 1)<br />
Is the patient able <strong>to</strong>?<br />
Underst<strong>and</strong> the inf<strong>or</strong>mation relevant <strong>to</strong> the decision<br />
Yes <br />
No <br />
Details<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………<br />
(See guidance note 2a)<br />
Retain that inf<strong>or</strong>mation<br />
Yes <br />
(See guidance note 2b)<br />
No <br />
Details<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………<br />
Use that inf<strong>or</strong>mation as part of the decision making process, <strong>or</strong> underst<strong>and</strong> the consequences<br />
of not making a decision<br />
Yes <br />
No <br />
Details<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………<br />
Page 47 of 64
(See guidance note 2c)<br />
And/ <strong>or</strong>:<br />
Is the patient able <strong>to</strong> communicate their decision, whether by talking, using sign language <strong>or</strong><br />
any other means?<br />
Yes <br />
No <br />
Details<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………<br />
(See guidance note 2d)<br />
Other:<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………<br />
………………………………………………………………………………<br />
I consider that the patient does / does not* have capacity <strong>to</strong> make the decision detailed in this<br />
document. (*Delete as appropriate).<br />
Signed………………………….……<br />
Print name.…………….…….…….<br />
Position………………………………<br />
Date………………………………….<br />
If the individual is found <strong>to</strong> have capacity <strong>to</strong> make decision, no further action is required.<br />
Where capacity is found <strong>to</strong> be lacking, complete the Best Interest Process overleaf bef<strong>or</strong>e<br />
deciding what is in their best interest.<br />
Page 48 of 64
Mental Capacity Act 2005<br />
Best Interest Checklist<br />
Pro-f<strong>or</strong>ma f<strong>or</strong> Best Interest Process<br />
Yes no The patient has been encouraged <strong>and</strong> assisted <strong>to</strong> participate in the decision.<br />
yes no All fac<strong>to</strong>rs relevant <strong>to</strong> the decision have been considered<br />
yes no Attempts have been made <strong>to</strong> find out the views of the patient including past <strong>and</strong><br />
present wishes <strong>and</strong> feelings.<br />
yes no Decisions have not been based <strong>or</strong> influenced by the patient’s age, appearance,<br />
diagnosis <strong>or</strong> behaviour.<br />
yes no Consideration has been given <strong>to</strong> whether the patient may regain capacity, <strong>and</strong> if<br />
so, if the decision can be delayed.<br />
*F<strong>or</strong> guidance on how <strong>to</strong> apply fac<strong>to</strong>rs, see Guidance notes.<br />
People who have<br />
been contacted<br />
bef<strong>or</strong>e coming <strong>to</strong> a<br />
decision<br />
Name<br />
Person 1 Person 2 Person 3 Person 4<br />
Role/relationship <strong>to</strong><br />
patient<br />
Address<br />
Tel<br />
People who were not being consulted <strong>and</strong> the reasons why:<br />
………………………………………………………………………………………………………………………………………<br />
…………………………………………………………………………………<br />
Referral <strong>to</strong> IMCA required (NB: A referral is required by law if there are no family <strong>or</strong> friends who are able <strong>to</strong> act on<br />
the patient’s behalf):<br />
Yes No Referral date: ……………………………………………………………<br />
Details of best interest decision made:<br />
………………………………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………………………………<br />
………………………………………………………………………………………………………………………………………<br />
Signed………………………….……<br />
Print name: …………….…….…….<br />
Position………………………………<br />
Date………………………………….<br />
Page 49 of 64
Mental Capacity Act 2005- Clinical Guidance Notes;<br />
To be used in conjunction with the Mental Capacity Act Prof<strong>or</strong>ma f<strong>or</strong> Hal<strong>to</strong>n <strong>and</strong> <strong>St</strong>. Helen’s PCT<br />
Community Health Services.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
1. Examples of an impairment <strong>or</strong> disturbance in the functioning of the mind <strong>or</strong> brain<br />
may include the following:<br />
conditions associated with some f<strong>or</strong>ms of mental illness<br />
dementia<br />
significant learning disabilities<br />
the long-term effects of brain damage<br />
physical <strong>or</strong> medical conditions that cause confusion, drowsiness <strong>or</strong> loss of consciousness<br />
delirium<br />
concussion following a head injury, <strong>and</strong><br />
the symp<strong>to</strong>ms of alcohol <strong>or</strong> drug use.<br />
2. F<strong>or</strong> a person <strong>to</strong> lack capacity <strong>to</strong> make a decision, the Act says their impairment <strong>or</strong> disturbance must affect<br />
their ability <strong>to</strong> make the specific decision when they need <strong>to</strong>. But first people must be given all practical <strong>and</strong><br />
appropriate supp<strong>or</strong>t <strong>to</strong> help them make the decision f<strong>or</strong> themselves. <strong>St</strong>age 2 can only apply if all practical<br />
<strong>and</strong> appropriate supp<strong>or</strong>t <strong>to</strong> help the person make the decision has failed. See Guidance Note 3 f<strong>or</strong><br />
guidance on ways of helping people <strong>to</strong> make their own decisions.<br />
2a. It is imp<strong>or</strong>tant not <strong>to</strong> assess a person’s underst<strong>and</strong>ing bef<strong>or</strong>e they have been given relevant inf<strong>or</strong>mation<br />
about a decision. Every eff<strong>or</strong>t must be made <strong>to</strong> provide inf<strong>or</strong>mation in a way that is most appropriate <strong>to</strong><br />
help the person <strong>to</strong> underst<strong>and</strong>. Quick <strong>or</strong> inadequate explanations are not acceptable unless the situation is<br />
urgent (see chapter 3 f<strong>or</strong> some practical steps). Relevant inf<strong>or</strong>mation includes:<br />
<br />
<br />
<br />
<br />
<br />
The nature of the decision<br />
The reason why the decision is needed, <strong>and</strong><br />
The likely effects of deciding one way <strong>or</strong> another, <strong>or</strong> making no decision at all.<br />
Take time <strong>to</strong> explain anything that might help the person make a decision. It is imp<strong>or</strong>tant that<br />
they have access <strong>to</strong> all the inf<strong>or</strong>mation they need <strong>to</strong> make an inf<strong>or</strong>med decision.<br />
Try not <strong>to</strong> give m<strong>or</strong>e detail than the person needs – this might confuse them. In some cases, a<br />
simple, broad explanation will be enough. But it must not miss out imp<strong>or</strong>tant inf<strong>or</strong>mation.<br />
What are the risks <strong>and</strong> benefits? Describe any f<strong>or</strong>eseeable consequences of making the<br />
decision, <strong>and</strong> of not making any decision at all.<br />
<br />
<br />
<br />
Explain the effects the decision might have on the person <strong>and</strong> those close <strong>to</strong> them – including<br />
the people involved in their care.<br />
If they have a choice, give them the same inf<strong>or</strong>mation in a balanced way f<strong>or</strong> all the options.<br />
F<strong>or</strong> some types of decisions, it may be imp<strong>or</strong>tant <strong>to</strong> give access <strong>to</strong> advice from elsewhere. This<br />
may be independent <strong>or</strong> specialist advice (f<strong>or</strong> example, from a medical practitioner <strong>or</strong> a financial<br />
<strong>or</strong> legal adviser). But it might simply be advice from trusted friends <strong>or</strong> relatives.<br />
2b. The person must be able <strong>to</strong> hold the inf<strong>or</strong>mation in their mind long enough <strong>to</strong> use it <strong>to</strong> make an effective<br />
decision. But section 3(3) of the Code of Practice states that people who can only retain inf<strong>or</strong>mation f<strong>or</strong> a<br />
sh<strong>or</strong>t while must not au<strong>to</strong>matically be assumed <strong>to</strong> lack the capacity <strong>to</strong> decide – it depends on what is<br />
necessary f<strong>or</strong> the decision in question. Items such as notebooks, pho<strong>to</strong>graphs, posters, videos <strong>and</strong> voice<br />
rec<strong>or</strong>ders can help people rec<strong>or</strong>d <strong>and</strong> retain inf<strong>or</strong>mation<br />
Page 50 of 64
Suggested Assessment of Ability <strong>to</strong> Retain Inf<strong>or</strong>mation:<br />
<br />
<br />
<br />
<br />
Present inf<strong>or</strong>mation <strong>and</strong> ask questions as above in 2a of the Guidance Notes<br />
Ask same questions after 5 minutes; note responses f<strong>or</strong> inconsistencies.<br />
Facilitate mem<strong>or</strong>y with aids such as writing things down, pictures etc.<br />
Ask same questions over three consecutive days <strong>to</strong> see if responses are cognisant <strong>and</strong> consistent.<br />
2c. F<strong>or</strong> someone <strong>to</strong> have capacity, they must have the ability <strong>to</strong> weigh up inf<strong>or</strong>mation <strong>and</strong> use it <strong>to</strong> arrive at a<br />
decision. Sometimes people can underst<strong>and</strong> inf<strong>or</strong>mation but an impairment <strong>or</strong> disturbance s<strong>to</strong>ps them<br />
using it. In other cases, the impairment <strong>or</strong> disturbance leads <strong>to</strong> a person making a specific decision without<br />
underst<strong>and</strong>ing <strong>or</strong> using the inf<strong>or</strong>mation they have been given.<br />
Some Suggested Questions <strong>to</strong> Assess Level of Underst<strong>and</strong>ing:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Can you tell me about ……? (the decision).<br />
What do you think is going <strong>to</strong> happen?<br />
What do you think would happen if you did not do x <strong>or</strong> y/ move in<strong>to</strong> a home/ tell someone something/<br />
get the treatment etc.? (results of not deciding either way)<br />
What are the benefits/ positive outcomes of doing this?<br />
What negative consequences are there?<br />
Are you okay with this happening?<br />
What are your wishes?<br />
2d. To help someone make a decision f<strong>or</strong> themselves, all possible <strong>and</strong> appropriate means of communication<br />
should be tried.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Ask people who know the person well about the best f<strong>or</strong>m of communication (try speaking <strong>to</strong> family<br />
members, carers, day centre staff <strong>or</strong> supp<strong>or</strong>t w<strong>or</strong>kers). They may also know somebody the person<br />
can communicate with easily, <strong>or</strong> the time when it is best <strong>to</strong> communicate with them.<br />
Use simple language.<br />
Where appropriate, use pictures, objects <strong>or</strong> illustrations <strong>to</strong> demonstrate ideas.<br />
Speak at the right volume <strong>and</strong> speed, with appropriate w<strong>or</strong>ds <strong>and</strong> sentence structure. It may be<br />
helpful <strong>to</strong> pause <strong>to</strong> check underst<strong>and</strong>ing <strong>or</strong> show that a choice is available.<br />
Break down difficult inf<strong>or</strong>mation in<strong>to</strong> smaller points that are easy <strong>to</strong> underst<strong>and</strong>. Allow the person<br />
time <strong>to</strong> consider <strong>and</strong> underst<strong>and</strong> each point bef<strong>or</strong>e continuing.<br />
It may be necessary <strong>to</strong> repeat inf<strong>or</strong>mation <strong>or</strong> go back over a point several times.<br />
Be aware of cultural, ethnic <strong>or</strong> religious fac<strong>to</strong>rs that shape a person’s way of thinking, behaviour <strong>or</strong><br />
communication. F<strong>or</strong> example, in some cultures it is imp<strong>or</strong>tant <strong>to</strong> involve the community in decisionmaking.<br />
Some religious beliefs (f<strong>or</strong> example, those of Jehovah’s Witnesses <strong>or</strong> Christian Scientists)<br />
may influence the person’s approach <strong>to</strong> medical treatment <strong>and</strong> inf<strong>or</strong>mation about treatment<br />
decisions.<br />
Page 51 of 64
If necessary, consider using a professional language interpreter. Even if a person communicated in<br />
English <strong>or</strong> Welsh in the past, they may have lost some verbal skills (f<strong>or</strong> example, because of<br />
dementia). They may now prefer <strong>to</strong> communicate in their first language. It is often m<strong>or</strong>e appropriate<br />
<strong>to</strong> use a professional interpreter rather than <strong>to</strong> use family members.<br />
Would an advocate (someone who can supp<strong>or</strong>t <strong>and</strong> represent the person) improve communication in<br />
the current situation? (See chapters 10 <strong>and</strong> 15 f<strong>or</strong> m<strong>or</strong>e inf<strong>or</strong>mation about advocates.)<br />
Suggested Communication Checklist:<br />
<br />
<br />
<br />
<br />
<br />
In what way does the individual communicate?<br />
In what way does s/he communicate an affirmative response?<br />
In what way does s/he indicate a negative response?<br />
In what way do they signal their preferences?<br />
In what way can the inf<strong>or</strong>mation be presented <strong>to</strong> facilitate maximum comprehension?<br />
3. One of the key principles of the Act is that any act done f<strong>or</strong>, <strong>or</strong> any decision made on behalf of a person<br />
who lacks capacity must be done, <strong>or</strong> made, in that person’s best interests. That is the same whether the person<br />
making the decision <strong>or</strong> acting is a family carer, a paid care w<strong>or</strong>ker, an at<strong>to</strong>rney, a court-appointed deputy, <strong>or</strong> a<br />
healthcare professional, <strong>and</strong> whether the decision is a min<strong>or</strong> issue – like what <strong>to</strong> wear – <strong>or</strong> a maj<strong>or</strong> issue, like<br />
whether <strong>to</strong> provide particular healthcare. As long as these acts <strong>or</strong> decisions are in the best interests of the person<br />
who lacks capacity <strong>to</strong> make the decision f<strong>or</strong> themselves <strong>or</strong> <strong>to</strong> consent <strong>to</strong> acts concerned with their care <strong>or</strong><br />
treatment, then the decision-maker <strong>or</strong> carer will be protected from liability.<br />
3a. A person trying <strong>to</strong> w<strong>or</strong>k out the best interests of a person who lacks capacity <strong>to</strong> make a particular decision<br />
(‘lacks capacity’) should:<br />
a. Encourage participation<br />
Do whatever is possible <strong>to</strong> permit <strong>and</strong> encourage the person <strong>to</strong> take part, <strong>or</strong> <strong>to</strong> improve their ability <strong>to</strong> take part, in<br />
making the decision.<br />
b. Identify all relevant circumstances<br />
Try <strong>to</strong> identify all the things that the person who lacks capacity would take<br />
in<strong>to</strong> account if they were making the decision <strong>or</strong> acting f<strong>or</strong> themselves.<br />
c. Find out the person’s views<br />
Try <strong>to</strong> find out the views of the person, who lacks capacity, including:<br />
i. The person’s past <strong>and</strong> present wishes <strong>and</strong> feelings – these may have been expressed<br />
verbally, in writing <strong>or</strong> through behaviour <strong>or</strong> habits.<br />
ii.<br />
iii.<br />
Any beliefs <strong>and</strong> values (e.g. religious, cultural, m<strong>or</strong>al <strong>or</strong> political) that would be likely <strong>to</strong><br />
influence the decision in question.<br />
Any other fac<strong>to</strong>rs the person themselves would be likely <strong>to</strong> consider if they were making the<br />
decision <strong>or</strong> acting f<strong>or</strong> themselves.<br />
Page 52 of 64
d. Avoid discrimination<br />
Do not make assumptions about someone’s best interests simply on the basis of the person’s age, appearance,<br />
condition <strong>or</strong> behaviour.<br />
e. Assess whether the person might regain capacity<br />
Consider whether the person is likely <strong>to</strong> regain capacity (e.g. after receiving medical treatment). If so, can the<br />
decision wait until then?<br />
f. If the decision concerns life-sustaining treatment<br />
Not be motivated in any way by a desire <strong>to</strong> bring about the person’s death. They should not make assumptions<br />
about the person’s quality of life.<br />
g. Consult others<br />
If it is practical <strong>and</strong> appropriate <strong>to</strong> do so, consult other people f<strong>or</strong> their views about the person’s best interests <strong>and</strong><br />
<strong>to</strong> see if they have any inf<strong>or</strong>mation about the person’s wishes <strong>and</strong> feelings, beliefs <strong>and</strong> values. In particular, try <strong>to</strong><br />
consult:<br />
<br />
<br />
<br />
<br />
<br />
anyone previously named by the person as someone <strong>to</strong> be consulted on either the decision in<br />
question <strong>or</strong> on similar issues<br />
anyone engaged in caring f<strong>or</strong> the person<br />
close relatives, friends <strong>or</strong> others who take an interest in the person’s welfare<br />
any at<strong>to</strong>rney appointed under a Lasting Power of At<strong>to</strong>rney <strong>or</strong> Enduring Power of At<strong>to</strong>rney made by the<br />
person<br />
any deputy appointed by the Court of Protection <strong>to</strong> make decisions f<strong>or</strong> the person.<br />
F<strong>or</strong> decisions about maj<strong>or</strong> medical treatment <strong>or</strong> where the person should live <strong>and</strong> where there is no-one who fits<br />
in<strong>to</strong> any of the above categ<strong>or</strong>ies, an Independent Mental Capacity Advocate (IMCA) must be consulted. When<br />
consulting, remember that the person who lacks the capacity <strong>to</strong> make the decision <strong>or</strong> act f<strong>or</strong> themselves still has a<br />
right <strong>to</strong> keep their affairs private – so it would not be right <strong>to</strong> share every piece of inf<strong>or</strong>mation with everyone.<br />
h. Avoid restricting the person’s rights<br />
<br />
<br />
See if there are other options that may be less restrictive of the person’s rights.<br />
Weigh up all of these fac<strong>to</strong>rs in <strong>or</strong>der <strong>to</strong> w<strong>or</strong>k out what is in the person’s best interests.<br />
3b. To help someone make a decision f<strong>or</strong> themselves, check the following points:<br />
a. Providing relevant inf<strong>or</strong>mation<br />
<br />
<br />
Does the person have all the relevant inf<strong>or</strong>mation they need <strong>to</strong> make a particular decision?<br />
If they have a choice, have they been given inf<strong>or</strong>mation on all the alternatives?<br />
Page 53 of 64
. Communicating in an appropriate way<br />
<br />
<br />
<br />
Could inf<strong>or</strong>mation be explained <strong>or</strong> presented in a way that is easier f<strong>or</strong> the person <strong>to</strong> underst<strong>and</strong> (f<strong>or</strong><br />
example, by using simple language <strong>or</strong> visual aids)?<br />
Have different methods of communication been expl<strong>or</strong>ed if required, including non-verbal communication?<br />
Could anyone else help with communication (f<strong>or</strong> example, a family member, supp<strong>or</strong>t w<strong>or</strong>ker, interpreter,<br />
speech <strong>and</strong> language therapist <strong>or</strong> advocate)?<br />
c. Making the person feel at ease<br />
<br />
<br />
<br />
Are there particular times of day when the person’s underst<strong>and</strong>ing is better?<br />
Are there particular locations where they may feel m<strong>or</strong>e at ease?<br />
Could the decision be put off <strong>to</strong> see whether the person can make the decision at a later time when<br />
circumstances are right f<strong>or</strong> them?<br />
d. Supp<strong>or</strong>ting the person<br />
<br />
Can anyone else help <strong>or</strong> supp<strong>or</strong>t the person <strong>to</strong> make choices <strong>or</strong> express a view?<br />
4. There are two circumstances when the best interest principle will not apply:<br />
a. The first is where someone has previously made an advance decision <strong>to</strong> refuse medical treatment<br />
while they had the capacity <strong>to</strong> do so. Their advance decision should be respected when they lack<br />
capacity, even if others think that the decision <strong>to</strong> refuse treatment is not in their best interests.<br />
b. The second concerns the involvement in research, in certain circumstances, of someone lacking<br />
capacity <strong>to</strong> consent.<br />
Page 54 of 64
APPENDIX 7<br />
How <strong>to</strong> seek a court declaration<br />
you are unable <strong>to</strong> gain consent<br />
(A court <strong>or</strong>der may be needed if the patient’s<br />
ability <strong>to</strong> give consent is in doubt)<br />
Ensure that all negotiations <strong>and</strong> discussions with<br />
the patient have been documented <strong>and</strong> signed<br />
preferably in the presence of a witness<br />
Is the treatment needed immediately? If yes, is it<br />
out of hours?<br />
Yes<br />
No<br />
The on-call Manager<br />
contact Direc<strong>to</strong>r on Call<br />
<strong>to</strong> ring Hal<strong>to</strong>n <strong>and</strong> <strong>St</strong><br />
<strong>Helens</strong> PCT legal<br />
advis<strong>or</strong>s f<strong>or</strong> immediate<br />
advice<br />
Contact PCT Legal<br />
Adviser. They will<br />
gain access <strong>to</strong> legal<br />
advice<br />
Page 55 of 64
APPENDIX 8<br />
Who has parental responsibility?<br />
1. Mothers au<strong>to</strong>matically have parental responsibility f<strong>or</strong> their children. Fathers also have<br />
parental responsibility:<br />
<br />
<br />
if they were married <strong>to</strong> the mother when the child was conceived <strong>or</strong> b<strong>or</strong>n, <strong>or</strong><br />
if they married her later.<br />
2. By law, unmarried fathers do not au<strong>to</strong>matically have parental responsibility.<br />
3. Pri<strong>or</strong> <strong>to</strong> 1 December 2003, they could only obtain this by:<br />
<br />
<br />
<br />
Parental Responsibility Order granted by the court.<br />
Residence Order granted by the court.<br />
M<strong>or</strong>e than one person can have parental responsibility if a Residence Order is<br />
granted, e.g. <strong>to</strong> a stepfather <strong>or</strong> other family relative with a Residence Order.<br />
Parental Responsibility Agreement.<br />
This must be signed by both parents, their signatures witnessed by an Officer of the Court<br />
<strong>or</strong> a Magistrate <strong>and</strong> the f<strong>or</strong>m sent <strong>to</strong> the Principal Registry of the High court f<strong>or</strong> registration<br />
after which it becomes effective.<br />
4. Since 1 December 2003, an unmarried father who is the natural father of the child can<br />
also acquire parental responsibility if he is named as the father on the child’s birth<br />
certificate.<br />
5. Although the consent of one person with parental responsibility f<strong>or</strong> a child is usually<br />
sufficient f<strong>or</strong> immunisation purposes (see section 2(7) Children Act 1989), if it appears that<br />
one parent agrees <strong>to</strong> immunisation but the other disagrees, further discussions with both<br />
parents are advised bef<strong>or</strong>e proceeding.<br />
6. The person with parental responsibility does not necessarily need <strong>to</strong> be present at the<br />
time an immunisation is given. Although a person may not abdicate <strong>or</strong> transfer parental<br />
responsibility, they may arrange f<strong>or</strong> some <strong>or</strong> all of it <strong>to</strong> be met by one <strong>or</strong> m<strong>or</strong>e persons<br />
acting on their behalf (section 2(9) Children Act 1989). There is no requirement f<strong>or</strong> such<br />
arrangements <strong>to</strong> be made in writing.<br />
7. Children may be brought f<strong>or</strong> immunisation by a person without parental responsibility, e.g.<br />
a gr<strong>and</strong>parent <strong>or</strong> child-minder. In this situation, the health professional would need <strong>to</strong> be<br />
satisfied that the circumstances indicate that that person has the necessary auth<strong>or</strong>ity, f<strong>or</strong><br />
example:<br />
Page 56 of 64
the person with parental responsibility has consented in advance <strong>to</strong> the immunisation<br />
(i.e. they received all the relevant inf<strong>or</strong>mation in advance <strong>and</strong> arranged f<strong>or</strong> the other<br />
person <strong>to</strong> bring the child <strong>to</strong> the appointment)<br />
the person with parental responsibility has arranged f<strong>or</strong> this other person <strong>to</strong> provide<br />
the necessary consent (i.e. they asked the other person <strong>to</strong> take the child <strong>to</strong> the<br />
appointment, <strong>to</strong> consider any further inf<strong>or</strong>mation given by the health professional, <strong>and</strong><br />
then <strong>to</strong> agree <strong>to</strong> immunisation if appropriate)<br />
If the child attends with an adult without parental responsibility f<strong>or</strong> the first scheduled<br />
immunisation appointment <strong>or</strong> unscheduled further appointments, it is imp<strong>or</strong>tant f<strong>or</strong> the<br />
immuniser <strong>to</strong> check that the parent <strong>or</strong> person with parental responsibility has given<br />
their consent. This can be either in writing <strong>or</strong> by a telephone call <strong>to</strong> the parent <strong>to</strong><br />
confirm the position. It should then be documented in the rec<strong>or</strong>d.<br />
Alternatively, there may be evidence that the person with parental responsibility:<br />
<br />
<br />
did not agree <strong>to</strong> the immunisation (e.g. the notes indicate that the parent(s) may have<br />
negative views on immunisation) <strong>or</strong><br />
did not agree that the person bringing the child could give the necessary consent<br />
(e.g. suggestion of disagreements between the parents on medical matters)<br />
In these exceptional circumstances, it may be necessary <strong>to</strong> contact the person with<br />
parental responsibility bef<strong>or</strong>e proceeding.<br />
8. A person giving consent on behalf of a child may change his <strong>or</strong> her mind <strong>and</strong> withdraw<br />
consent at any time. Where consent is either refused <strong>or</strong> withdrawn, this decision must be<br />
documented.<br />
9. It is the duty of each healthcare professional <strong>to</strong> communicate effectively <strong>and</strong> share such<br />
knowledge <strong>and</strong> inf<strong>or</strong>mation with other members of the primary health care team.<br />
Page 57 of 64
APPENDIX 9<br />
Advance refusals of treatment<br />
Patients may have a “living will” <strong>or</strong> “advance directive” specifying how they would like <strong>to</strong> be<br />
treated in the case of future incapacity. While professionals cannot be required by such<br />
directives <strong>to</strong> provide particular treatments (which might be appropriate), case law is now clear<br />
that an advance refusal of treatment which is valid <strong>and</strong> applicable <strong>to</strong> subsequent circumstances<br />
in which they patient lacks capacity is legally binding. An advance refusal is valid if made<br />
voluntarily by an appropriately inf<strong>or</strong>med person with capacity. Failure <strong>to</strong> respect such an<br />
advance refusal can result in legal action against the practitioner.<br />
If there is doubt about the validity of an advance refusal a rule should be sought from the court.<br />
It is not legally necessary f<strong>or</strong> the refusal <strong>to</strong> be made in writing <strong>or</strong> f<strong>or</strong>mally witnessed, although<br />
such measures add evidentiary weight <strong>to</strong> the validity of the refusal. A health professional may<br />
not over-ride a valid <strong>and</strong> applicable advance refusal of the on the grounds of the professional’s<br />
personal conscientious objection <strong>to</strong> such a refusal.<br />
Although the issue has not yet come bef<strong>or</strong>e a court, it has been suggested that as a matter of<br />
public policy individuals should not be able <strong>to</strong> refuse in advance, measures which are essential<br />
<strong>to</strong> keep a patient comf<strong>or</strong>table. 12 This is sometimes referred <strong>to</strong> as “basic” <strong>or</strong> “essential care, <strong>and</strong><br />
includes keeping the patient warm <strong>and</strong> clean <strong>and</strong> free from distressing symp<strong>to</strong>ms such as<br />
breathlessness, vomiting, <strong>and</strong> severe pain. However, some patients may prefer <strong>to</strong> <strong>to</strong>lerate<br />
some discomf<strong>or</strong>t if this means they remain m<strong>or</strong>e alert <strong>and</strong> able <strong>to</strong> respond <strong>to</strong> family <strong>and</strong> friends.<br />
However, although basic/essential care would include the offer of <strong>or</strong>al nutrition <strong>and</strong> hydration, it<br />
would not cover f<strong>or</strong>ce feeding an individual <strong>or</strong> the use of artificial nutrition <strong>and</strong> hydration. The<br />
courts have recognised that a competent individual has the right <strong>to</strong> choose <strong>to</strong> go on a “hunger<br />
strike”, although this may be qualified if the person has a mental dis<strong>or</strong>der. Towards the end of<br />
such a period an individual is likely <strong>to</strong> lose capacity (become incompetent) <strong>and</strong> the courts have<br />
stated that if the individual has, whilst competent, expressed the desire <strong>to</strong> refuse until death<br />
supervenes, the person cannot be f<strong>or</strong>ce fed <strong>or</strong> fed artificially when incompetent. If the patient is<br />
refusing food as a result of mental dis<strong>or</strong>der <strong>and</strong> is detained under the Mental Health Act 1983,<br />
different considerations may apply <strong>and</strong> m<strong>or</strong>e specialist guidance should be consulted.<br />
Reference:<br />
12 British Medical Association, Advance statements about medical treatment (1995) BMA<br />
Publishing Group: London<br />
Page 58 of 64
APPENDIX 10<br />
Useful Contact Details<br />
Debbie Fairclough Assistant Direc<strong>to</strong>r C<strong>or</strong>p<strong>or</strong>ate Services 01928 593726<br />
Legal Advis<strong>or</strong><br />
Margaret Evans Caldicott Guardian 01744 457 221<br />
Swati Chapman Mental Capacity Act Lead 01928 582955<br />
Helen Smith Head Safeguarding Adults 01744 621821<br />
Charlie Whelan Designated Nurse Child Protection (H) 0151 495 5017<br />
Ann Dunne Designated Nurse Child Protection (<strong>St</strong>H) 01744 627576<br />
Linda Spooner Professional Development Mgr 01928 593640<br />
Dot Keates Head Clinical Governance 01744 621822<br />
Page 59 of 64
APPENDIX 11<br />
Mental Capacity Act<br />
There are 10 guiding principles set out in the Act that must be followed when a member of the<br />
PCT is assessing the capacity of an individual <strong>to</strong> provide valid consent <strong>to</strong> treatment <strong>or</strong> refusal of<br />
treatment.<br />
Principle 1: “A person must be assumed <strong>to</strong> have capacity unless it is established that he<br />
lacks capacity” (Mental Capacity Act, Section 1 (2). there must be clear proof that a person<br />
lacks capacity about the particular decision they are being required <strong>to</strong> make. People may need<br />
help <strong>to</strong> make the decision <strong>or</strong> <strong>to</strong> communicate it – but this does not mean that they lack the<br />
capacity <strong>to</strong> make the decision.<br />
Principle 2: “A person is not <strong>to</strong> be treated as unable <strong>to</strong> make a decision unless all<br />
practicable steps <strong>to</strong> help him <strong>to</strong> do so have been taken without success” (Mental<br />
Capacity Act, Section 1 (3)). This is a proactive duty on those who w<strong>or</strong>k with a person who<br />
may be thought <strong>to</strong> lack capacity <strong>to</strong> make a particular decision - they must ensure that all<br />
possible steps must be taken <strong>to</strong> assist the person <strong>to</strong> make the decision. Where complex<br />
decisions are being taken, relating <strong>to</strong> a person’s accommodation <strong>or</strong> treatment (including the<br />
giving of medication), these steps should be clearly described in the person’s case notes, with a<br />
rec<strong>or</strong>d of their success <strong>or</strong> failure <strong>and</strong> the reasons f<strong>or</strong> this. These rec<strong>or</strong>ds should be signed <strong>and</strong><br />
dated by the staff member concerned <strong>and</strong> should be specifically countersigned by the manager<br />
of the team/service.<br />
The kind of supp<strong>or</strong>t a person needs will depend on their circumstances. It may include:<br />
using a different f<strong>or</strong>m of communication (such as non-verbal communication)<br />
providing inf<strong>or</strong>mation in a m<strong>or</strong>e accessible f<strong>or</strong>m (such as pho<strong>to</strong>graphs, drawing <strong>or</strong> tapes)<br />
treating a medical condition which may affect a person’s capacity<br />
having a structured programme <strong>to</strong> improve a person’s capacity <strong>to</strong> make particular<br />
decisions.<br />
This principle aims <strong>to</strong> s<strong>to</strong>p people being au<strong>to</strong>matically considered as lacking capacity <strong>to</strong> make<br />
particular decisions. If they play as big a role as possible in decision-making, this will help<br />
prevent unnecessary interventions in their lives.<br />
Principle 3: “A person is not <strong>to</strong> be treated as unable <strong>to</strong> make a decision merely because<br />
he makes an unwise decision” (Mental Capacity Act, Section 1 (4). This can be one of the<br />
most difficult areas f<strong>or</strong> families, carers <strong>and</strong> professionals alike. The Mental Capacity Act Code of<br />
Practice (page 24) is clear, however:<br />
Page 60 of 64
“Everybody has their own values, beliefs, preferences <strong>and</strong> attitudes. A person should not be<br />
assumed <strong>to</strong> lack the capacity <strong>to</strong> make a decision just because other people think their decision<br />
is unwise. This applies even if family members, friends <strong>or</strong> healthcare <strong>or</strong> social care staff are<br />
unhappy with a decision”.<br />
However, as with other aspects of the Act, the key issue is the context of the decision-making.<br />
An unwise decision in itself may not indicate a lack of capacity, but it may be a trigger a fuller<br />
examination of the person’s capacity <strong>to</strong> make a specific decision, <strong>or</strong> indeed of the inf<strong>or</strong>mation<br />
that person may need in <strong>or</strong>der <strong>to</strong> come <strong>to</strong> a fully inf<strong>or</strong>med decision f<strong>or</strong> themselves.<br />
Principle 4: “An act done, <strong>or</strong> decision made, under the Mental Capacity Act f<strong>or</strong> <strong>or</strong> on<br />
behalf of a person who lacks capacity must be done, <strong>or</strong> made, in his best interests”<br />
(Mental Capacity Act, Section 1 (5)). This applies whoever is making the decision, <strong>and</strong><br />
whether the decision is a min<strong>or</strong> <strong>or</strong> a maj<strong>or</strong> one. It covers all aspects of financial, personal<br />
welfare <strong>and</strong> healthcare decision making <strong>and</strong> actions.<br />
To ensure best interests are addressed throughout, the Code of Practice (pages 65-66)<br />
identifies a series of steps that should be taken by someone who is making a decision <strong>or</strong> taking<br />
an action:<br />
encourage the person <strong>to</strong> take part in – <strong>or</strong> improve their ability <strong>to</strong> take part in – making the<br />
decision<br />
find out the person’s views – including past <strong>and</strong> present wishes <strong>and</strong> feelings, <strong>and</strong> taking in<strong>to</strong><br />
account any of the person’s beliefs <strong>or</strong> values, <strong>or</strong> any other fac<strong>to</strong>rs the person themselves<br />
would take in<strong>to</strong> account, when making the decision<br />
avoid discrimination – do not make assumptions about a person’s best interests simply on<br />
the basis of their age, appearance, condition <strong>or</strong> behaviour<br />
assess whether the person might regain capacity – <strong>and</strong> if so, consider whether the decision<br />
can be delayed<br />
consult others, where practical <strong>and</strong> appropriate – particularly someone previously named by<br />
the person as someone <strong>to</strong> be consulted, anyone providing care f<strong>or</strong> the person, close<br />
relatives <strong>and</strong> others who take a close interest in the person’s welfare, a person with Lasting<br />
<strong>or</strong> Enduring power of At<strong>to</strong>rney, <strong>and</strong> any deputy appointed by the Court of Protection<br />
avoid restricting the person’s rights<br />
where the decision concerns life-sustaining treatment, do not be motivated in any way by a<br />
desire <strong>to</strong> bring about the person’s death, through assumptions about their quality of life.<br />
Principle 5: “Bef<strong>or</strong>e the act is done, <strong>or</strong> the decision is made, regard must be had <strong>to</strong><br />
whether the purpose f<strong>or</strong> which it is needed can be effectively achieved in a way that is<br />
less restrictive of the person’s rights <strong>and</strong> freedom of action” (Mental Capacity Act,<br />
Section 1 (6)). This consideration – finding the least restrictive alternative, whilst continuing <strong>to</strong><br />
consider the person’s best interests – includes considering whether there is a need <strong>to</strong> act <strong>or</strong><br />
make a decision at all.<br />
Page 61 of 64
ASSESSING CAPACITY<br />
General issues: Mental capacity is the ability <strong>to</strong> make a decision, ranging from a min<strong>or</strong><br />
decision that affects daily life only, <strong>to</strong> a m<strong>or</strong>e significant decision with much wider implications,<br />
including a decision that may have legal consequences f<strong>or</strong> themselves <strong>or</strong> others. The starting<br />
point is always <strong>to</strong> assume that a person has capacity <strong>to</strong> make a specific decision, although<br />
possibly with health <strong>or</strong> supp<strong>or</strong>t.<br />
F<strong>or</strong> the purposes of the Act, a person lacks capacity if at the time of the decision <strong>to</strong> be made:<br />
<br />
<br />
they have an impairment <strong>or</strong> disturbance that affects the way their brain <strong>or</strong> mind w<strong>or</strong>ks <strong>and</strong><br />
this impairment <strong>or</strong> disturbance means that they cannot make a specific decision<br />
Hence the decision about a person’s capacity is based on their ability <strong>to</strong> make a specific<br />
decision at the time it needs <strong>to</strong> be made, <strong>and</strong> not their ability <strong>to</strong> make decisions in<br />
general.<br />
Who should conduct assessments of capacity? Under the Mental Capacity Act, a decision<br />
about one person’s capacity can be made by anyone who follows the criteria f<strong>or</strong> assessing this<br />
– it is no longer the specific responsibility of a psychiatrist <strong>or</strong> other doc<strong>to</strong>r. This will usually be<br />
the person most directly connected with the individual at the time the decision has <strong>to</strong> be made.<br />
This will particularly be the case f<strong>or</strong> day <strong>to</strong> day decisions.<br />
Page 62 of 64
APPENDIX 12<br />
EQUALITY IMPACT ASSESSMENT TOOL<br />
To be completed <strong>and</strong> attached <strong>to</strong> any c<strong>or</strong>p<strong>or</strong>ate document when submitted <strong>to</strong> the appropriate<br />
committee f<strong>or</strong> consideration <strong>and</strong> approval.<br />
1. Does the policy/guidance affect one group less <strong>or</strong><br />
m<strong>or</strong>e favourably than another on the basis of:<br />
Yes/No<br />
Race No<br />
Ethnic <strong>or</strong>igins (including gypsies <strong>and</strong> travellers) No<br />
Nationality No<br />
Gender No<br />
Culture No<br />
Religion <strong>or</strong> belief No<br />
<br />
Sexual <strong>or</strong>ientation including lesbian, gay <strong>and</strong><br />
bisexual people<br />
Age No<br />
<br />
Disability - learning disabilities, physical disability,<br />
sens<strong>or</strong>y impairment <strong>and</strong> mental health problems<br />
2. Is there any evidence that some groups are<br />
affected differently?<br />
3. If you have identified potential discrimination, are<br />
there any exceptions valid, legal <strong>and</strong>/<strong>or</strong><br />
justifiable?<br />
4. Is the impact of the policy/guidance likely <strong>to</strong> be<br />
negative?<br />
5. If so can the impact be avoided? N/A<br />
6. What alternative are there <strong>to</strong> achieving the<br />
policy/guidance without the impact?<br />
7. Can we reduce the impact by taking different<br />
action?<br />
No<br />
No<br />
No<br />
No<br />
No<br />
N/A<br />
N/A<br />
Comments<br />
If you have identified a potential discrimina<strong>to</strong>ry impact of this c<strong>or</strong>p<strong>or</strong>ate document, please refer it<br />
<strong>to</strong> [insert name of appropriate person], <strong>to</strong>gether with any suggestions as <strong>to</strong> the action required<br />
<strong>to</strong> avoid/reduce this impact. F<strong>or</strong> advice in respect of answering the above questions, please<br />
contact [insert name of appropriate person <strong>and</strong> contact details].<br />
Page 63 of 64
APPENDIX 13<br />
DISSEMINATION PLAN<br />
Title of document:<br />
<strong>Consent</strong> <strong>Policy</strong><br />
Dissemination Lead: (Print name <strong>and</strong><br />
contact details)<br />
Date finalised: March 2009<br />
Previous document already being used?<br />
delete as appropriate)<br />
Yes/No (Please<br />
Linda Spooner<br />
If yes, in what f<strong>or</strong>mat <strong>and</strong> where?<br />
On intranet <strong>and</strong> paper copies<br />
Proposed action <strong>to</strong> retrieve out-of-date<br />
copies of the document:<br />
To inf<strong>or</strong>m all services updated document <strong>and</strong> <strong>to</strong> put new<br />
document on Document P<strong>or</strong>tal<br />
To be disseminated <strong>to</strong>:<br />
Who will<br />
disseminate<br />
it<br />
Timescale<br />
(Date)<br />
<strong>St</strong>atus<br />
Paper<br />
<strong>or</strong><br />
Electronic<br />
Heads of Service L Spooner April 2009 Electronic<br />
Comments<br />
TRAINING PLAN<br />
Event (Please provide details of where <strong>and</strong> training dates available <strong>to</strong><br />
educate staff about this policy)<br />
Timescale Owner <strong>St</strong>atus<br />
<strong>Consent</strong> Training<br />
2 April<br />
8 July<br />
8 Oc<strong>to</strong>ber<br />
Training Plan Lead (Please provide details of staff who will be responsible<br />
f<strong>or</strong> overseeing this training)<br />
Linda Spooner<br />
Additional inf<strong>or</strong>mation (Please provide details of any processes in place<br />
<strong>to</strong> supp<strong>or</strong>t implementation)<br />
Denotes: Action not yet taken <strong>or</strong> deadline f<strong>or</strong> action not met. Action plan <strong>to</strong> address this must be provided.<br />
Denotes: Action partially implemented.<br />
Denotes: Action complete.<br />
Page 64 of 64