dhjBa
dhjBa
dhjBa
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
REVIEW<br />
Retinal<br />
Insider<br />
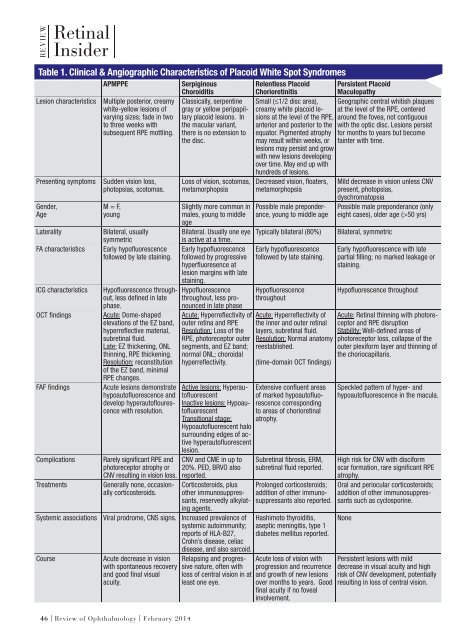
Table 1. Clinical & Angiographic Characteristics of Placoid White Spot Syndromes<br />
Lesion characteristics<br />
Presenting symptoms<br />
Gender,<br />
Age<br />
Laterality<br />
FA characteristics<br />
ICG characteristics<br />
OCT fi ndings<br />
FAF fi ndings<br />
Complications<br />
Treatments<br />
Systemic associations<br />
Course<br />
APMPPE<br />
Multiple posterior, creamy<br />
white-yellow lesions of<br />
varying sizes; fade in two<br />
to three weeks with<br />
subsequent RPE mottling.<br />
Sudden vision loss,<br />
photopsias, scotomas.<br />
M = F,<br />
young<br />
Bilateral, usually<br />
symmetric<br />
Early hypofl uorescence<br />
followed by late staining.<br />
Hypofl uorescence throughout,<br />
less defi ned in late<br />
phase.<br />
Acute: Dome-shaped<br />
elevations of the EZ band,<br />
hyperrefl ective material,<br />
subretinal fl uid.<br />
Late: EZ thickening, ONL<br />
thinning, RPE thickening.<br />
Resolution: reconstitution<br />
of the EZ band, minimal<br />
RPE changes.<br />
Acute lesions demonstrate<br />
hypoautofl uorescence and<br />
develop hyperautofl ourescence<br />
with resolution.<br />
Rarely signifi cant RPE and<br />
photoreceptor atrophy or<br />
CNV resulting in vision loss.<br />
Generally none, occasionally<br />
corticosteroids.<br />
Serpiginous<br />
Choroiditis<br />
Classically, serpentine<br />
gray or yellow peripapillary<br />
placoid lesions. In<br />
the macular variant,<br />
there is no extension to<br />
the disc.<br />
Loss of vision, scotomas,<br />
metamorphopsia<br />
Slightly more common in<br />
males, young to middle<br />
age<br />
Bilateral. Usually one eye<br />
is active at a time.<br />
Early hypofl uorescence<br />
followed by progressive<br />
hyperfl uoresence at<br />
lesion margins with late<br />
staining.<br />
Hypofl uorescence<br />
throughout, less pronounced<br />
in late phase<br />
Acute: Hyperrefl ectivity of<br />
outer retina and RPE<br />
Resolution: Loss of the<br />
RPE, photoreceptor outer<br />
segments, and EZ band;<br />
normal ONL; choroidal<br />
hyperrefl ectivity.<br />
Active lesions: Hyperautofl<br />
uorescent<br />
Inactive lesions: Hypoautofl<br />
uorescent<br />
Transitional stage:<br />
Hypoautofl uorescent halo<br />
surrounding edges of active<br />
hyperautofl uorescent<br />
lesion.<br />
CNV and CME in up to<br />
20%. PED, BRVO also<br />
reported.<br />
Corticosteroids, plus<br />
other immunosuppressants,<br />
reservedly alkylating<br />
agents.<br />
Viral prodrome, CNS signs. Increased prevalence of<br />
systemic autoimmunity;<br />
reports of HLA-B27,<br />
Crohn’s disease, celiac<br />
disease, and also sarcoid.<br />
Acute decrease in vision<br />
with spontaneous recovery<br />
and good fi nal visual<br />
acuity.<br />
Relapsing and progressive<br />
nature, often with<br />
loss of central vision in at<br />
least one eye.<br />
Relentless Placoid<br />
Chorioretinitis<br />
Small (≤1/2 disc area),<br />
creamy white placoid lesions<br />
at the level of the RPE,<br />
anterior and posterior to the<br />
equator. Pigmented atrophy<br />
may result within weeks, or<br />
lesions may persist and grow<br />
with new lesions developing<br />
over time. May end up with<br />
hundreds of lesions.<br />
Decreased vision, fl oaters,<br />
metamorphopsia<br />
Possible male preponderance,<br />
young to middle age<br />
Typically bilateral (80%)<br />
Early hypofl uorescence<br />
followed by late staining.<br />
Hypofl uorescence<br />
throughout<br />
Acute: Hyperrefl ectivity of<br />
the inner and outer retinal<br />
layers, subretinal fl uid.<br />
Resolution: Normal anatomy<br />
reestablished.<br />
(time-domain OCT fi ndings)<br />
Extensive confl uent areas<br />
of marked hypoautofl uorescence<br />
corresponding<br />
to areas of chorioretinal<br />
atrophy.<br />
Subretinal fi brosis, ERM,<br />
subretinal fl uid reported.<br />
Prolonged corticosteroids;<br />
addition of other immunosuppressants<br />
also reported.<br />
Hashimoto thyroiditis,<br />
aseptic meningitis, type 1<br />
diabetes mellitus reported.<br />
Acute loss of vision with<br />
progression and recurrence<br />
and growth of new lesions<br />
over months to years. Good<br />
fi nal acuity if no foveal<br />
involvement.<br />
Persistent Placoid<br />
Maculopathy<br />
Geographic central whitish plaques<br />
at the level of the RPE, centered<br />
around the fovea, not contiguous<br />
with the optic disc. Lesions persist<br />
for months to years but become<br />
fainter with time.<br />
Mild decrease in vision unless CNV<br />
present, photopsias,<br />
dyschromatopsia<br />
Possible male preponderance (only<br />
eight cases), older age (>50 yrs)<br />
Bilateral, symmetric<br />
Early hypofl uorescence with late<br />
partial fi lling; no marked leakage or<br />
staining.<br />
Hypofl uorescence throughout<br />
Acute: Retinal thinning with photoreceptor<br />
and RPE disruption<br />
Stability: Well-defi ned areas of<br />
photoreceptor loss, collapse of the<br />
outer plexiform layer and thinning of<br />
the chorio capillaris.<br />
Speckled pattern of hyper- and<br />
hypoautofl uorescence in the macula.<br />
High risk for CNV with disciform<br />
scar formation, rare signifi cant RPE<br />
atrophy.<br />
Oral and periocular corticosteroids;<br />
addition of other immunosuppressants<br />
such as cyclosporine.<br />
None<br />
Persistent lesions with mild<br />
decrease in visual acuity and high<br />
risk of CNV development, potentially<br />
resulting in loss of central vision.<br />
46 | Review of Ophthalmology | February 2014