Person-Centered Care - Saint Joseph Hospital
Person-Centered Care - Saint Joseph Hospital
Person-Centered Care - Saint Joseph Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Person</strong>-<strong>Centered</strong> <strong>Care</strong><br />
<strong>Saint</strong> <strong>Joseph</strong> Health System<br />
Nursing Annual Report • Fiscal Year 2010
“The needs of the spirit are as critical to health<br />
as those individual organs which make up the body.”<br />
— FLORENCE NIGHTINGALE<br />
(1820-1910)
Our integration as one at <strong>Saint</strong> <strong>Joseph</strong> Health System continued even further this year with many<br />
successful milestones along the way. Even though we are only two years old as an eight-facility system, our clinical teams are<br />
sharing best practices across the state that ultimately improve patient care in each of our communities.<br />
Our focus on improvement this year continued to elevate the standard of care from both a quality and satisfaction perspective. Our<br />
Critical Success Metrics are not just a collection of statistics and numbers, but instead are tangible and deliverable methods to reach our<br />
goal of person-centered care, which includes the categories of:<br />
• People (Workforce Development, Nursing Leadership Institute)<br />
• Quality (Service Excellence, Evidence-Based Practice)<br />
• Stewardship (Technology and System Development; <strong>Care</strong> Coordination and Patient Self-Management)<br />
• Growth (Access)<br />
As you read this publication, you will be impressed not only by the volume of initiatives that all of our nurses have implemented and<br />
accomplished, but also by their collective passion to deliver the best care possible to our patients.<br />
I am pleased to share with you the 2010 <strong>Saint</strong> <strong>Joseph</strong> Health System Nursing Annual Report, which provides an overview of our nursing<br />
team’s dedication to person-centered care, a comprehensive team approach that includes the nurse, patient, family and community.<br />
Sincerely,<br />
Gene Woods, FACHE<br />
Chief Executive Officer<br />
1
2<br />
ABBREVIATION KEY FOR DEGREES AND SPECIALTIES ABBREVIATION KEY FOR UNITS<br />
CCH Continuing <strong>Care</strong> <strong>Hospital</strong><br />
CCU Coronary <strong>Care</strong> Unit<br />
CTU Cardiac Thoracic Unit<br />
CTVU Cardiac Thoracic Vascular Unit<br />
HISSU Heart Institute Short Stay Unit<br />
ICU Intensive <strong>Care</strong> Unit<br />
L&D Labor and Delivery<br />
NICU Neonatal Intensive <strong>Care</strong> Unit<br />
PACU Post Anesthesia <strong>Care</strong> Unit<br />
PASS Pre-Admission Screening Services<br />
PRNU Prep-Recovery Nursing Unit<br />
ACHPN Advanced Certified Hospice Palliative <strong>Care</strong> Nurse<br />
ACLS-EP Advanced Cardiac Life Support - Experienced Provider<br />
ACNP Acute <strong>Care</strong> Nurse Practitioner<br />
ADN Associate Degree in Nursing<br />
APRN, NP Advanced Practice Registered Nurse, Nurse Practitioner<br />
ARNP Advanced Registered Nurse Practitioner<br />
ASN Associate of Science in Nursing<br />
BC Board Certified<br />
BSIT Bachelor of Science in Information Technology<br />
BSN Bachelor of Science in Nursing<br />
CBPN-IC Certified Breast Patient Navigator<br />
(Imaging and Cancer <strong>Care</strong>)<br />
CCM Certified Case Manager<br />
CCRN Critical <strong>Care</strong> Registered Nurse<br />
CDE Certified Diabetes Educator<br />
CDN Certified Dialysis Nurse<br />
CEN Certified Emergency Nurse<br />
CFRN Certified Flight Registered Nurse<br />
CIC Certified in Infection Control<br />
CMA Certified Medical Assistant<br />
CMSRN Certified Med/Surg Registered Nurse<br />
CNA Certified Nursing Assistant<br />
CNAA Certified in Nursing Administration, Advanced<br />
CNM Certified Nurse Midwife<br />
CNN Certified Nephrology Nurse<br />
CNOR Certified Nurse in Operating Room<br />
COHN Certified Occupational Health Nurse<br />
CPAN Certified Post Anesthesia Nurse<br />
CPN Certified Pediatric Nurse<br />
CPNP Certified Pediatric Nurse Practitioner<br />
CPST Child Passenger Safety Technician<br />
CRNA Certified Registered Nurse Anesthetist<br />
CRRN Certified Rehabilitation Registered Nurse<br />
CS Clinical Specialist<br />
CSTFA Certified Surgical Technologist/First Assistant<br />
CWOCN Certified Wound, Ostomy, Continence Nurse<br />
FNP Family Nurse Practitioner<br />
IBCLC International Board-Certified Lactation Consultant<br />
LNC Legal Nurse Consultant<br />
MBA Master’s in Business Administration<br />
MHA Master’s in Health Administration<br />
MSN Master’s of Science in Nursing<br />
NA Nursing Assistant<br />
NNP Neonatal Nurse Practitioner<br />
OCN Oncology Certified Nurse<br />
RCIS Registered Cardiac Invasive Specialist<br />
RN Registered Nurse<br />
RNC-NIC Registered Nurse Certified in Neonatal Intensive <strong>Care</strong><br />
RNC-OB Registered Nurse Certified in Obstetrics<br />
RNFA Registered Nurse First Assistant<br />
SANE Sexual Assault Nurse Examiner<br />
SWAN Nursing Assistant/Ward Secretary<br />
TNCC Trauma Nurse Core Certified<br />
UM Unit Manager<br />
US Unit Secretary<br />
TABLE OF CONTENTS<br />
Letter from Gene Woods, CEO 1<br />
Abbreviation Key 2<br />
Introduction 3<br />
<strong>Saint</strong> <strong>Joseph</strong> - Berea 11<br />
<strong>Saint</strong> <strong>Joseph</strong> - London 15<br />
<strong>Saint</strong> <strong>Joseph</strong> - Martin 19<br />
<strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling 23<br />
Flaget Memorial <strong>Hospital</strong> 27<br />
<strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong>/<strong>Saint</strong> <strong>Joseph</strong> East/<strong>Saint</strong> <strong>Joseph</strong> - Jessamine 31<br />
Living our Core Values 48<br />
PRINCIPLES OF PERSON-CENTERED CARE<br />
The ultimate goal of person-centered care is to create partnerships among health care practitioners, patients and<br />
families that will lead to the best outcomes and enhance the quality and safety of health care.<br />
The practice of person-centered care is guided by these principles:<br />
• Respect and Dignity<br />
• Information, Communication and Education<br />
• Participation<br />
• Collaboration<br />
• Physical Comfort<br />
• Emotional Support<br />
• Involvement of Family and Friends<br />
• Coordination and Integration of <strong>Care</strong><br />
—Adopted from the American <strong>Hospital</strong> Association
Fiscal year 2010 has been a great year for nursing at <strong>Saint</strong> <strong>Joseph</strong> Health System (SJHS).<br />
INTRODUCTION<br />
We would like to report on our progress toward the metrics described in our<br />
Nursing Professional Practice Model & <strong>Care</strong> Delivery System.<br />
PEOPLE<br />
To keep care person-centered: hourly<br />
rounding-nursing plan of care<br />
Hand-off of care<br />
Quality indicators<br />
Core measures<br />
Service excellence<br />
Communication boards<br />
Patient and family satisfaction<br />
STEWARDSHIP<br />
Respect for the individual patient<br />
Coordination of care<br />
Communication, information and education of care to<br />
include patient’s cultural and lifespan needs<br />
Comfort (emotional, physical and spiritual)<br />
Emotional support<br />
Family involvement (including significant others,<br />
support persons, and life partners)<br />
<strong>Care</strong> Coordination<br />
and Patient<br />
Self-Management<br />
Workforce<br />
Development<br />
Recruit and retain a qualified<br />
nursing workforce by<br />
encouraging specialty<br />
certification and<br />
continued<br />
education for our<br />
nursing staff.<br />
Technology and<br />
System Development<br />
Develop and enhance<br />
clinical information systems<br />
that support and contribute to<br />
nursing’s role in the health care<br />
delivery model.<br />
Strengthen nursing practice for<br />
the provision of safe, timely,<br />
efficient, equitable, personcentered,<br />
excuse-free,<br />
sacred and transparent<br />
care in all settings.<br />
<strong>Person</strong>-<br />
<strong>Centered</strong><br />
<strong>Care</strong><br />
Access<br />
Nursing<br />
Leadership<br />
Institute<br />
Advocate and implement<br />
strategies for access to the<br />
appropriate level of care for<br />
all patient populations. Explore<br />
use of current and future virtual<br />
care models.<br />
GROWTH<br />
NURSE<br />
PATIENT<br />
FAMILY<br />
COMMUNITY<br />
Develop and implement a core<br />
curriculum nursing leadership<br />
formation program that<br />
enhances the performance<br />
development model for<br />
all levels of nursing<br />
personnel.<br />
Service<br />
Excellence<br />
Exceed the patient, family and<br />
caregivers’ expectations in the<br />
provision of optimal patient care by<br />
building a culture of professional,<br />
courteous and respectful caregivers.<br />
Evidence-Based<br />
Practice<br />
Implement and measure key<br />
indicators to support Evidence-<br />
Based Practice through the<br />
Clinical Covenant enhancing<br />
the patient experience.<br />
QUALITY<br />
Accountability<br />
Advocacy<br />
Confidence<br />
Competence<br />
Enabling<br />
Empowerment<br />
Responsibility<br />
Relationship<br />
Stage 1: Novice<br />
Stage 2: Advanced Beginner<br />
Stage 3: Competent<br />
Stage 4: Proficient<br />
Stage 5: The Expert<br />
3
FY10 Critical Success<br />
Metrics Results<br />
PEOPLE<br />
Core Competencies Developed: Completed<br />
Achieve Voluntary RN Turnover less than 10%:<br />
Finished at 6.88%<br />
Eliminate Agency Use: As of June 30, all nursing<br />
agency has been eliminated!<br />
RNs: 1,789<br />
LPNs: 120<br />
ARNPs: 30<br />
RN Voluntary<br />
Turnover: 6.88%<br />
<strong>Saint</strong> <strong>Joseph</strong> Health System<br />
Nursing Facts<br />
SJHS Nursing Degrees – October 2010<br />
SJH/SJE/SJJ SJB SJL SJM SJMS Flaget TOTALS Percentage<br />
Associate Degree/Nursing 488 44 231 21 72 139 995 56.25%<br />
Bachelors Degree/Nursing 476 27 48 5 23 49 628 35.50%<br />
Masters Degree/Nursing 45 2 3 0 5 14 69 3.90%<br />
Other Masters Degrees 1 1 0 2 1 0 5 0.28%<br />
Diploma 68 3 0 0 1 0 72 4.07%<br />
TOTALS 1078 77 282 28 102 202 1769 100.00%<br />
4
QUALITY<br />
IMPLEMENT EVIDENCE-BASED PRACTICES<br />
All SJHS hospitals implemented Evidence-Based Practices (EBP) to include Pressure Ulcers, Surgical Never Events, Fall Prevention, <strong>Hospital</strong>-Acquired Infections, Catheter-<br />
Associated Urinary Tract Infections, Central Line-Associated Bloodstream Infections, Pain, Venous Thrombo/Embolism Prevention, and Heart Failure. There are nine EBPs<br />
with 27 bundles; all were implemented.<br />
ACHIEVE 50% REDUCTION IN HOSPITAL-ACQUIRED CONDITIONS (HAC) FOR CORE EBP<br />
This proved to be a very difficult goal. As a system, we decreased the HAC in total, but did not reach the 50% goal.<br />
DEVELOP AND IMPLEMENT THE CLINICAL COVENANT<br />
During FY10, we implemented the Clinical Covenant with three patient types: Pneumonia and Heart Failure, Orthopedic, and Critical <strong>Care</strong>. <strong>Saint</strong> <strong>Joseph</strong> - Berea developed the<br />
Pneumonia and Heart Failure team, Flaget Memorial <strong>Hospital</strong> developed the Orthopedic team and <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> developed the Critical <strong>Care</strong> team. The goal is to spread<br />
the newfound knowledge to all SJHS hospitals.<br />
The Clinical Covenant is a promise we will make to each patient that we will always do certain things and always not do certain things. The Covenant is not a guarantee but<br />
a promise to the patient that we will do all we can to give the patient the best opportunity to have a good outcome. The concept is that care at the bedside would be changed<br />
through the formation of a transactional relationship between the patient and the caregiver. The charter for all teams was to create an environment where the patient receives<br />
highly reliable, patient-centered, seamless, transparent care. This care would be evidence-based and include core measure components and safe practices from the National<br />
Quality Forum.<br />
SAINT JOSEPH HEALTH SYSTEM NURSING CERTIFICATIONS:<br />
We have 174 nationally certified nurses for SJHS, representing 10% of our RN workforce.<br />
Critical <strong>Care</strong> Registered Nurse: 27<br />
Trauma Nurse Course Certified: 21<br />
Certified Emergency Nurse: 20<br />
Sexual Assault Nurse Examiner: 14<br />
Certified Ambulatory Perianesthesia Nurse: 7<br />
Board Certified Registered Nurse: 5<br />
Certified Case Managers: 5<br />
Certified Nurse Operating Room: 5<br />
Family Nurse Practitioner, Board Certified: 5<br />
Registered Nurse Certified, Inpatient Obstetric: 5<br />
Certified Breast Navigator: 4<br />
Certified Pediatric Nurse: 4<br />
Certified Wound Ostomy Nurse: 4<br />
Adult Nurse Practitioner, Board Certified: 3<br />
Certified Bariatric Nurse: 3<br />
Certified Pediatric Emergency Nurse: 3<br />
Certified Post Anesthesia Nurse: 3<br />
Certified Hospice & Palliative <strong>Care</strong> Nurse: 2<br />
Certified Lactation Counselor: 2<br />
Certified Med/Surg Registered Nurse: 2<br />
Certified Rehabilitation Registered Nurse: 2<br />
Certified Respiratory Therapist: 2<br />
International Board Certified Lactation Consultant: 2<br />
Oncology Certified Nurse: 2<br />
Adult Nurse Specialist-Board Certified: 1<br />
Advanced Certified Hospice & Palliative Nurse: 1<br />
Board Certified Holistic Nurse: 1<br />
Certified Clinical Document Specialist: 1<br />
Certified Diabetes Educator: 1<br />
Certified Infection Control Nurse: 1<br />
Certified Nurse Administrator: 1<br />
Certified Occupational Health Nurse, Case Mgmt.: 1<br />
Certified Professional Healthcare Quality: 1<br />
Certified Radiology Nurse: 1<br />
Critical <strong>Care</strong> Registered Nurse with Cardiac Medicine Specialty: 1<br />
Fellow of the American College of Healthcare Executives: 1<br />
Gerontological Clinical Nurse Specialist-Board Certified: 1<br />
International Certified Childbirth Educator: 1<br />
Lamaze Certified Childbirth Educator: 1<br />
Legal Nurse Consultant Certified: 1<br />
Nurse Executive, Advanced Board Certified: 1<br />
Registered Cardiovascular Invasive Specialist: 1<br />
Registered Nurse Certified, Low Risk Neonatal Nursing: 1<br />
Registered Nurse Certified, Neonatal Intensive <strong>Care</strong>: 1<br />
5
All teams utilized a multidisciplinary approach to include physicians, leaders,<br />
executives, nursing and line level staff. Each of our pilot projects began their journey<br />
with a unit profile, which studied the patient population by age, diagnosis, staff<br />
composition, patient flow in the unit and patient satisfaction scores. Simultaneously,<br />
each team studied the patient flow process. These studies identified each step in<br />
detail, from the time the patient entered the system to the time of discharge, whether<br />
admitted from the Emergency Department, surgery or a medical admission. During<br />
this review, process variation and delays were identified.<br />
The teams realized some redundancy and opportunity for improvement by simply<br />
putting on paper the way “we thought” things were done on a daily basis. We also<br />
had some important “just do its” during flow charting. This was the time the rest of<br />
the hospital began to see what the group was doing, as we placed our charts on the<br />
walls and sent them on a hospital tour on display boards. With this collaboration<br />
between the Clinical Covenant teams and other stakeholders, perspectives have been<br />
broadened. This is allowing us to realize the importance of consistency in the way we<br />
work and in the way we work together, to ensure our patients’ experiences are seamless<br />
and highly reliable.<br />
CLINICAL OUTCOMES FOR CLINICAL COVENANT TEAMS<br />
<strong>Saint</strong> <strong>Joseph</strong> - Berea Pneumonia and Heart Failure Team (Pegasus)<br />
• Identified the need for education on EBP standards, NQF standards and process<br />
improvement tools, such as AIM/PDSA and Gantt Charts<br />
• Physicians were not getting timely results for the direct-admit patient for<br />
laboratory and radiology results. The orders were written routinely and as a<br />
routine many were not available in a timely manner for the physician to review on<br />
the day of admission. All laboratory and radiology orders for direct-admit patients<br />
are now ordered stat and the results are ready for the physician to review on the<br />
day of admission.<br />
• Scripting for our patients utilizing Healthy People 2010 recommendations as well<br />
as Teach Back Method<br />
• Consolidation of direct-admit process for physicians. A letter was sent to all<br />
physicians, giving them one central number to call for any direct admission.<br />
• Earlier implementation of Respiratory Bundle. The Respiratory Bundle standing<br />
orders are implemented as a bundle when patients are admitted to prevent delays<br />
in discharge.<br />
• Revised Medication Reconciliation process. Pharmacy worked with a<br />
MEDITECH resource person to revamp and streamline the process and delete<br />
redundant processes for physicians and nurses.<br />
6
• Change in admission process to prevent unwanted test results going to physicians and<br />
critical results from being missed. Patients with no primary care physician were being<br />
assigned a primary care physician in MEDITECH for the attending physician, and test<br />
results were going to that physician post-discharge.<br />
• <strong>Saint</strong> <strong>Joseph</strong> - Martin participated in this team and has taken this information and<br />
quickly spread it to its campus.<br />
Flaget Memorial Orthopedic Team (Hercules)<br />
• Identified improvement opportunity for pain management.<br />
• Developed an increased awareness of when the next dose of medication is due for the<br />
patient and the caregiver, by placing the last dose of pain medication given on the<br />
patient communication board and by adding communication boards for caregivers in<br />
discreet locations on the nursing unit with information as to when the next dose of pain<br />
medication is due for patients. The intent is to provide a system where any caregiver could<br />
let the nurse know, through a written message, that a patient was in pain without having<br />
to leave the area to find someone to notify.<br />
• Developed a method of communication that has common language and understanding<br />
between sender and receiver by scripting a consistent message being delivered to the<br />
patient regarding how to manage their pain.<br />
• Reviewed patient handbook regarding pain management to ensure scripting and written<br />
material matched.<br />
• Dedicated orthopedic rooms have been supplied with the necessary equipment so it is<br />
always in the room, to prevent delays in care when the patient arrives.<br />
• Variation with pre-op orders is being addressed by the surgeons through the development<br />
of a standard set of orthopedic admission protocols.<br />
• Pharmacy and the Post-Anesthesia <strong>Care</strong> Unit (PACU) worked together to find a way<br />
the patient’s location could be changed in the computer so orders could be faxed to<br />
pharmacy from PACU. This expedited the care of the patient on arrival to the floor by<br />
eliminating the wait time for orders to be processed by pharmacy and medication to be<br />
delivered to the unit.<br />
<strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> Critical <strong>Care</strong> Team (Leo)<br />
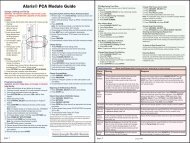
• Availability of Rapid Sequence Induction (RSI) drugs. Numerous drugs were available<br />
in the AccuDose medication cabinet, but delay occurred in obtaining each separately. An<br />
RSI kit was placed in the AccuDose to ensure a more rapid drug procurement process for<br />
emergent intubations in the unit.<br />
• Time delay in locating patient care supplies in the unit stock room. As a result, the stock<br />
system was better organized to group and categorize supplies, utilizing a color-coding<br />
system: respiratory supplies have orange tabs; urinary supplies have yellow tabs, etc.<br />
The area of search can thus be narrowed down at a glance based on the color coding.<br />
7
8<br />
• Facilitate case management for the critical care areas. The current case<br />
manager serviced two areas of the hospital: ICU South and a step-down<br />
unit. As a result, the case manager was reassigned to oversee care in<br />
two sister units: ICU South and ICU North.<br />
• Reduce the time spent in obtaining line placements,<br />
particularly deep lines, and feeding tubes. Capital money was<br />
appropriated, and an ultrasound machine was purchased for<br />
placement of lines at the bedside. The equipment is now<br />
in place and training on the machine has occurred. The<br />
critical care nurse practitioners are currently working<br />
on the development of expertise with equipment<br />
utilization during line placements. The end result in<br />
this process will be a safer line placement process,<br />
through a reduction in trips off the unit for the<br />
patient and the critical care nurse, as well as<br />
concurrent visualization during line placement.<br />
• Variability in the delivery of patient<br />
medications to ICU South. With three<br />
methods of delivery—carrier, tube system,<br />
dumbwaiter—the need to arrive at consistency<br />
was seen as a time-saving measure. The<br />
implementation of the newest PharmNet<br />
ordering system has led to the need to stabilize<br />
the changes arising from this system before<br />
suggesting changes to the delivery system.<br />
A subcommittee consisting of pharmacy,<br />
maintenance, nursing and quality has been<br />
empowered to review the existing process.<br />
• Currently developing scripting around the delivery<br />
of care, and the safe practices that they employ on<br />
a daily basis to ensure excellent patient outcomes.<br />
The areas of scripting focus are centered on the safe<br />
practices developed by the National Quality Forum<br />
(NQF). The end result of the process improvement<br />
project will be to increase the time the critical care nurse has<br />
available to spend with the patient at the bedside. This will<br />
allow the nurse to have crucial conversations with the patients<br />
and family members centered on the care that will always be<br />
delivered to the patient.
STEWARDSHIP<br />
A Case Management model of nursing has been piloted in the Lexington market.<br />
The Case Management Department has been undergoing changes over the past<br />
year to better serve our patients. The department’s name has been changed to <strong>Care</strong><br />
Coordination in order to better reflect our body of work.<br />
The changes in the care delivery model are driven by the complexity of the health<br />
care system of today. These changes are designed to assist patients on their<br />
journey across the care continuum. They support an environment of healing<br />
and wellness by focusing on excellence in patient care delivery and quality<br />
outcomes. The vision for the department is one in which the individual<br />
patient’s health care needs are met through the coordination of the many<br />
health care disciplines.<br />
The coordination of care enables us to meet the patient’s physical,<br />
mental and spiritual needs as they journey across the care continuum.<br />
In the new <strong>Care</strong> Coordination model, the care coordinators and<br />
social workers support an environment of healing grounded in our<br />
core values of reverence, integrity, compassion and excellence.<br />
In order to fulfill the vision and meet the goals of the department,<br />
the roles of the RN case managers and the social workers have to<br />
change. The care coordinator’s role has transformed by focusing on<br />
excellence in order to provide the patient with a smooth transition<br />
on to the next level of care. This excellence and transition is<br />
accomplished through the coordination and collaboration among the<br />
health care team, the patient and the patient’s family.<br />
REDUCE HEART FAILURE READMISSIONS<br />
Extensive efforts and discussion have centered on heart failure management with<br />
core measures and reduction in readmissions. In defining the problem of heart failure<br />
readmission it has been noted if the patient does not understand the discharge<br />
instruction, this leads to poor compliance with fluid and medication management.<br />
A concentrated effort with a nursing and physician committee has focused on core<br />
compliance to reduce readmissions, which includes understanding of medications.<br />
Unless contraindicated, beta blocker and ACE/ARB are indicated on discharge and<br />
long-term management. Review of readmission notes a few patients are frequently<br />
readmitted, indicating a need for a long-term non-acute program, such as a cardiac<br />
rehab or Heart Failure Clinic. Although timely retrospective review has improved<br />
core measure results, improving toward top deciles will require concurrent review. A<br />
multidisciplinary team was organized to develop a plan. Case management is focusing<br />
on length of stay; nursing is essential to improving results; an admission packet was<br />
created to collect all needed resources in one place, including the recommendation for<br />
an Evidence-Based Practice order set.<br />
It has been noted by the Institute for Healthcare Improvement that readmission occurs<br />
within seven days of discharge and post-discharge phone calls improve a patient’s<br />
understanding of patient management needs. As a pilot, <strong>Saint</strong> <strong>Joseph</strong> - London<br />
employed ARNPs as disease management leaders. The ARNP calls each patient postdischarge,<br />
and is the first contact for patients who have concerns. (Most readmission<br />
occurs within seven days of discharge.) It is expected that the discharge instructions,<br />
which consists of six indicators, will improve discharge medication management.<br />
The social worker’s role has evolved, becoming more focused and<br />
covering a broader population in order to meet the needs of our patients<br />
and their families. The social workers coordinate services for the patients<br />
as well as act as a resource to physicians, staff, patients and families for the<br />
psychosocial aspect of the patient’s care plan. They continue to serve as a<br />
bridge linking our patients and their families with community and may also<br />
provide crisis intervention and/or counseling in special situations.<br />
9
GROWTH<br />
Implemented a Med/Surg team to spread Transforming <strong>Care</strong> at the Bedside (TCAB)<br />
throughout the system. Led by Billie Turner, this team implemented bedside report on<br />
at least one unit at each site and is now spreading this to include all inpatient units.<br />
The group has collaborated with the service excellence council to design patient<br />
communication boards for patient rooms. Boards will be installed during the month<br />
of October. Patients will see consistent information on all inpatient units throughout<br />
SJHS. The team has also collaborated with the education department to offer medical/<br />
surgical specific continuing education for nurses. A two-day certification prep course<br />
and a one-day CE course are now scheduled.<br />
IMPLEMENT ED REINVENTION STRATEGIES<br />
A team was formed in January 2009, led by Kathy Stumbo and team leaders Laura<br />
LaRue, Emergency Department Director for Flaget Memorial <strong>Hospital</strong> and Marilyn<br />
Swinford, Emergency Department Director for <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> and <strong>Saint</strong> <strong>Joseph</strong><br />
- Jessamine. The team’s focus has been on sharing information, developing best practices<br />
and standardizing the ED patient experience throughout SJHS.<br />
The team has a major goal of reducing unnecessary waits and delays in the Emergency<br />
Department. Our targets are five-minute “<strong>Care</strong> Begins” and 30-minute “See a Provider”<br />
(marketed as “No Wait ER”). The initial<br />
pilot began at <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong><br />
(SJH), <strong>Saint</strong> <strong>Joseph</strong> East (SJE) and<br />
<strong>Saint</strong> <strong>Joseph</strong> - Jessamine (SJJ) with key<br />
successes due in part to the leadership of<br />
Kelly Ray at SJH, Patti Creed at SJE and<br />
Dan Andrews at SJJ. The pilot will be<br />
spread to all Kentucky facilities.<br />
satisfaction and increased ED volumes by 12% from the previous year for SJH/SJE/SJJ<br />
Emergency Departments.<br />
Patient satisfaction is a strong focus of the team. Our providers received standardized<br />
customer satisfaction training from the Physician Team Health vice president and to<br />
date our facilities have some of the highest satisfaction scores among Catholic Health<br />
Initiatives facilities, with three facilities reaching the 99th percentile. Satisfaction<br />
and spirituality of seeing the F.A.C. E. of God rings true in every ED visit (F.A.C.E.<br />
stands for Formation, Accountability, Communication and Evaluation—our service<br />
excellence best practices fall under these categories).<br />
Standardization of orientation, protocols and education are an ongoing process (led by<br />
Melinda Stumbo, <strong>Saint</strong> <strong>Joseph</strong> - Martin; Mary Lou Young, <strong>Saint</strong> <strong>Joseph</strong> - London; and<br />
Patty Sturt, <strong>Saint</strong> <strong>Joseph</strong> - Berea). The RN new graduate program is an intense fourmonth<br />
process that has resulted in successful integration of the newest members of our<br />
team into our fast-paced tertiary environment.<br />
Achieving the recognition of excellence, the SJHS Inaugural Certification in Emergency<br />
Nursing (CEN) review course was offered this year at <strong>Saint</strong> <strong>Joseph</strong> - Jessamine. Seven<br />
nurses now proudly are recognized after successfully earning the CEN.<br />
10<br />
After only four short months, “<strong>Care</strong><br />
Begins in 5 Minutes” is being met 65% of<br />
the time, with an average of four minutes<br />
for SJH, four minutes for SJJ and eight<br />
minutes for SJE. “See a Provider Within<br />
30 Minutes” is being met 60% of the time,<br />
with an average of 35 minutes for SJH,<br />
22 minutes for SJJ and 35 minutes for<br />
SJE. Our slogan “Be Safe, Be Nice, Be<br />
Quick” has resulted in high patient
The state of nursing at <strong>Saint</strong> <strong>Joseph</strong> - Berea is strong.<br />
Nurses have been heavily involved this past year in not only patient care but in community<br />
care. Recently, we recruited six pediatricians to our campus. This was a new skill set for<br />
our nurses and they took it on with great enthusiasm. Our nurses are now able to care<br />
for the whole family, from infant to senior adult.<br />
This past year also brought new Evidence-Based Practices (EBP) the nurses implemented. Huge<br />
successes were seen as the rate of hospital-acquired conditions decreased by 50%. The quality of care<br />
at <strong>Saint</strong> <strong>Joseph</strong> - Berea has been noticed and our nurses have been asked to be involved in more and<br />
more community activities, as you will see in the coming pages.<br />
Nurses are at the core of our development of a person-centered environment. As always, none of<br />
this would have happened without the dedication and commitment of all departments in the<br />
hospital. One thing we do well at <strong>Saint</strong> <strong>Joseph</strong> - Berea is work together as a family of caregivers,<br />
whether we are in nursing, the lab, radiology, respiratory, rehab, housekeeping, dietary or the<br />
many other departments that provide care to our patients either directly or indirectly every day.<br />
Each and every day is a day we come to work and fulfill our calling as nurses. This we do with<br />
our CHI and SJHS mission, vision and values in mind.<br />
With gratitude,<br />
Pat Patton, RN, MSN<br />
Chief Operating Officer/Chief Nursing Officer<br />
SAINT JOSEPH - BEREA<br />
11
Transformational Leadership<br />
During this last fiscal year, all nursing staff, rehab staff and pharmacy staff at <strong>Saint</strong> <strong>Joseph</strong> - Berea (SJB) were educated on Health Literacy and its effects on readmissions. During this<br />
two-hour class, staffs were educated on exactly what Health Literacy is, how it affects our patients and nursing staff, as well as the effect it has on readmissions. Working closely<br />
with the Madison County Health Department, the CNO taught these classes. Also during these classes, participants learned the use of the “teach back” method. In this<br />
teaching style, patients are taught certain content and then asked to repeat back or “teach back” what they have learned.<br />
The pain clinic was started in Surgery this past year. Victor McCane, RN, BSN, started this service in collaboration with Mary Turner, RN, from <strong>Saint</strong> <strong>Joseph</strong> -<br />
London. Dr. Siddiqi, board-certified in interventional pain management, comes to Berea once every two weeks to see patients and do procedures. This new<br />
service line was started effectively and efficiently due to Victor’s leadership. Frances McKeehan, RN; Clarissa Ramsay, RN; and Brenda Marcum, RN, were<br />
instrumental in making sure this service was up and running by obtaining procedural sedation classes. Victor and his nursing staff worked closely with Dr.<br />
Siddiqi and his staff to make sure patient expectations as well as quality expectations were met.<br />
Structural Empowerment<br />
In FY10 SJB received approval to move forward with our MEDITECH Clinical Documentation System. Amy Hedglin, RN, CEN,<br />
nurse informaticist, has taken the lead for this initiative. By moving forward with this initiative it will help provide better patient care in<br />
the following ways:<br />
• Improved customer satisfaction through better coordinated care and service. Information flows with fewer repetitive questions.<br />
• Increased clinician and provider satisfaction as nursing documentation will be available in real time to clinicians through the Primary<br />
<strong>Care</strong> Informatics (PCI) module.<br />
• Increased efficiency with the chart being available to all appropriate users as permitted by system availability.<br />
• Clear, concise documentation and patient history that is easily accessible in the continuation of care from department to department<br />
and visit to visit.<br />
• Mechanisms to facilitate compliance with all applicable regulations.<br />
• Assistance in the tracking of performance improvement initiatives with greater ease, and decrease in potential errors that may be<br />
caused by illegible handwriting.<br />
TOUCHING THE COMMUNITY: BEYOND OUR DOORS<br />
SJB nursing reaches out to the community through many outreach programs. These included a Go Red for Women event where blood pressures<br />
were taken; Berea Chamber of Commerce Golf Tournament at Battlefield Golf Course, where sunscreen was handed out; Berea Craft Festival at<br />
Indian Fort Theatre, where first aid was provided and health promotion and injury prevention material were provided; Berea Community School<br />
Health Fair, where information was provided regarding childhood diabetes and obesity, blood pressure checks, financial counseling, as well as<br />
other health information; Spoonbread Festival, where first aid was provided; the Kentucky Guild of Artists and Craftsman Fall Fair at Indian Fort<br />
Theatre, where first aid was provided. Our SJB nurses are in the community on a continual basis, letting the community know the benefits of using<br />
their local hometown hospital. Nurses, as well as<br />
other staff members, participated in the secondannual<br />
Get Healthy Berea event, where health<br />
promotion and injury prevention material were<br />
available for all who attended.<br />
<strong>Hospital</strong> educator Elena Baker, RN, BSN,<br />
partnered with <strong>Saint</strong> Mark Catholic School<br />
to provide monthly health-related educational<br />
presentations to children in preschool through<br />
third grade. This helped instill healthy<br />
habits in the children.<br />
12
NURSING FACTS:<br />
NUMBER OF NURSES<br />
RNs: 77<br />
LPNs: 2<br />
ARNP: 1<br />
MSNs: 2<br />
Exemplary Professional Practice<br />
The Professional Nursing Practice Model is a method for nurses who are practicing direct patient care<br />
to advance professionally. It is based on Patricia Benner’s Novice to Expert practice model and is one of<br />
patient-centered care. SJB Emergency Department is the first and only department at the hospital to<br />
have 100% staff on the Professional Nursing Practice Model.<br />
Elena Baker, RN, BSN, was instrumental in arranging pediatric in-services provided by the pediatricians<br />
for our staff nurses and respiratory therapists. By doing this, the nurses and respiratory therapists were<br />
able to ask questions directly of the pediatricians and get a better sense of how the nurses were to care<br />
for their patients.<br />
AVERAGE YEARS OF SERVICE<br />
0-5 years:<br />
48.71%<br />
6+ years:<br />
51.28%<br />
AVERAGE AGE OF NURSES<br />
21-40 years:<br />
33.33%<br />
41+ years:<br />
66.66%<br />
The ED staff and other departments were successful in SJB’s annual Chemical Stockpile Emergency<br />
Preparedness Program (CSEPP) drill. FY10 was the first year that federal investigators gave zero<br />
deficiencies to <strong>Saint</strong> <strong>Joseph</strong> - Berea’s team.<br />
BOOKS/ARTICLES<br />
Sheehy’s Emergency Nursing: Principles<br />
and Practice, chapter 42 “Toxicologic<br />
Emergencies”<br />
Author: Patty Sturt,<br />
RN, MSN, MBA, CPEN<br />
ENA: Sheehy’s Emergency Nursing,<br />
6 th edition, 2009<br />
TRIFOLD POSTERS<br />
Nurse Manager’s Review of Budget and<br />
Information and Use in Decision Making<br />
Rose Patrick, RN, MSN<br />
Patty Sturt, RN, MSN, MBA, CPEN<br />
Impact of the Clinical Ladder on Staff<br />
Satisfaction in a Community <strong>Hospital</strong><br />
Diane Bowling, RN, CEN<br />
Patty Sturt, RN, MSN, MBA, CPEN<br />
FURTHERING EDUCATION<br />
Heather Agee<br />
Beth Alcorn<br />
Elena Baker<br />
Janis Carpenter<br />
Leslie Crawford<br />
Holly Fort<br />
Amy Hedglin<br />
Charles King<br />
Teresa King<br />
Mike Miller<br />
Pat Patton<br />
Patty Sturt<br />
TURNOVER<br />
RN:<br />
6.67%<br />
Voluntary RN:<br />
2.67%<br />
Vacancy:<br />
3.60%<br />
Implementation of a Competency-Based<br />
Training Program: Impact on Staff<br />
Performance and Confidence During a<br />
Chemical Incident Drill<br />
Darcy Maupin, RN, BSN, CEN<br />
Patty Sturt, RN, MSN, MBA, CPEN<br />
13
New Knowledge Innovations and Improvements<br />
INNOVATION IN ACTION<br />
Hunter Purdy, RN, HNB-BC, was hired to create a <strong>Person</strong>-<strong>Centered</strong> Healing Environment. She<br />
worked closely with the president and CNO/COO to develop a plan to transform <strong>Saint</strong> <strong>Joseph</strong> - Berea<br />
into an Optimal Healing Environment that was person-centered. During this process we defined<br />
person-centered to include the patient and the employees, volunteers, physicians and everyone who<br />
contributes to the mission at <strong>Saint</strong> <strong>Joseph</strong> - Berea. In FY10 we began a healing therapies program,<br />
obtained funding for local art throughout the facility, and have given the inside of the facility a<br />
facelift. This work has also included involving local high school students to paint murals in two patient<br />
rooms to make them more pediatric friendly. Hunter has also worked closely with community art<br />
organizations, artists, the local farmers market and Berea College in creation of this Optimal Healing<br />
Environment. Current activities include implementing a room for renewal for all caregivers, providing<br />
therapeutic massage on-site for employees, and other self-care opportunities.<br />
In an effort to broaden the range of available programs and make more services accessible to more<br />
patients, <strong>Saint</strong> <strong>Joseph</strong> - Berea now has the availability of a Sexual Assault Nurse Examiner (SANE)<br />
service. Elena Baker, RN, BSN, SANE, is certified in forensic evidence collection and is now able<br />
to provide the service for the residents of Berea, as well as those from surrounding counties and<br />
communities. The SANE program at SJB seeks also to play an active role in the health and wellness<br />
of the local student population and would like to provide training and awareness to Berea College<br />
students, the Berea College Safety and Security Department, as well as the college faculty on sexual<br />
assault and domestic violence issues. <strong>Saint</strong> <strong>Joseph</strong> - Berea is dedicated to the healing mission of the<br />
Church, emphasizing human dignity, social justice, and the creation and maintenance of healthier<br />
communities. We are proud to continue that mission by offering this essential program to Berea and the<br />
surrounding communities we serve.<br />
CLINICAL COVENANT WORK<br />
In January 2010 we formed Team Pegasus and started down the road to implementing the Clinical<br />
Covenant at <strong>Saint</strong> <strong>Joseph</strong> - Berea. So much hard work has been done by so many dedicated and<br />
talented folks to get us to where we are today. We have been blessed to have commitment from<br />
physicians, leaders, executives, line level nursing staff, case managers, social workers, quality abstractors<br />
and other managers. The group has been focused like a laser beam and each member has held the<br />
others accountable in keeping the patient and family members at the center of every decision we made.<br />
We knew this was something different—not a project or a program—it was the right thing to do to<br />
integrate patients, caregivers and loved ones into the total care of the individual. We knew if we did this<br />
right, we could improve outcomes, reduce costs and help patient satisfaction.<br />
RESEARCH IN ACTION<br />
At SJB 30 nurses participated in the collaborative research study conducted by Loyola University<br />
Chicago and CHI that explored staff nurse perceptions in six areas of the professional practice<br />
environment. While the results cannot be generalized to all staff nurses at SJB, they did reveal that the<br />
hospital met or exceeded the CHI average in the areas of teamwork and leadership, and disagreement<br />
and conflict. The remaining four areas of clinical practice, general relationships and communication,<br />
internal work motivation, and cultural sensitivity are areas for examination by the nursing organization<br />
at SJB, as results were below the CHI average. <strong>Saint</strong> <strong>Joseph</strong> - Berea continues to participate in this<br />
research with the next step being managers’ awareness of employees’ perception of leadership.<br />
NATIONAL CERTIFICATIONS<br />
RECEIVED<br />
Critical <strong>Care</strong> Registered Nurses:<br />
Bernice Baird, RN<br />
Diane Snyder, RN<br />
Med/Surg Certified:<br />
Laurie Faught<br />
Certified Central Sterile Supply Tech:<br />
Wilma Masters<br />
Certified Emergency Nurses:<br />
Dixie Bryant, RN<br />
Vicki Hamilton, RN<br />
Amy Hedglin, RN<br />
Darcy Maupin, RN<br />
Certified Pediatric<br />
Emergency Nurses:<br />
Vicki Hamilton, RN<br />
Darcy Maupin, RN<br />
Patty Sturt, RN<br />
Board-Certified Holistic Nurse:<br />
Hunter Purdy, RN, HNB-BC<br />
SANE Registered Nurse:<br />
Elena Baker, RN, BSN, SANE<br />
ADVANCED DEGREES<br />
RECEIVED<br />
Pat Patton, RN, MSN: Master’s in<br />
Nursing, specializing in nursing<br />
administration, from University<br />
of Kentucky.<br />
Patty Sturt, RN, MSN: Master’s in<br />
Business Administration from<br />
Midway College.<br />
AWARDS AND RECOGNITIONS<br />
DAISY Award Recipients:<br />
Julie Hamm, RN,<br />
Med/Surg<br />
Melissa Cosby,<br />
RN, ED<br />
Sharon Clark,<br />
RN, OR<br />
EDUCATIONAL<br />
ACCOMPLISHMENTS<br />
AND MENTORING<br />
Clinical Ladder<br />
August 2010<br />
Level III<br />
Diane Bowling<br />
Melissa Cosby<br />
Darcy Maupin<br />
Mike Miller<br />
Nancy Mowbray<br />
Greta Thompson<br />
LEVEL II<br />
Vicki Hamilton<br />
Amy Hedglin<br />
Brenda Marcum<br />
Frances McKeehan<br />
Karen McKinney<br />
Ruth Prewitt<br />
LEVEL I<br />
Heather Agee<br />
Mitzi Alexander<br />
Jami Belcher<br />
Mildred Botkins<br />
Sandra Bowling<br />
Crystal Catron<br />
Leslie Crawford<br />
Laurie Faught<br />
Julie Hamm<br />
Rebekah Hamilton<br />
Mona Hanna<br />
Mary K. Johnson<br />
Stephanie Kauer<br />
Teresa King<br />
Charlene Lamb<br />
Samantha O’Neal<br />
Clarissa Ramsay<br />
Sarah Saylor<br />
Emily Shaw<br />
Diane Snyder<br />
Lori Vickers<br />
Sherry Wilson<br />
LEADERSHIP IN NURSING<br />
Pat Patton, RN, MSN: Cumberland<br />
District Director for the Kentucky<br />
Organization of Nurse Leaders<br />
(KONL)<br />
LEADERSHIP IN<br />
PROFESSIONAL<br />
ORGANIZATIONS<br />
Pat Patton, RN, MSN: Cumberland<br />
District Director for the Kentucky<br />
Organization of Nurse Leaders<br />
(KONL)<br />
Empirical Quality Outcomes<br />
• <strong>Saint</strong> <strong>Joseph</strong> - Berea maintains 100% on the AMI core measures.<br />
• Quality data submitted to CMS has been validated at a 97% success rate with only two charts falling<br />
out of the sample.<br />
• In the past year, patients have received their pneumonia vaccine 100% of the time and flu vaccine<br />
97.62% of time (one patient missed). This is a major improvement for SJB.<br />
• SJB continues to perform well in the area of patient satisfaction. In FY10 we ended in the 82nd<br />
percentile for patient satisfaction, with 78.8% of patients giving top scores for patient satisfaction.<br />
• Implemented six Evidence-Based Practices for <strong>Saint</strong> <strong>Joseph</strong> - Berea. Reduced rate of hospitalacquired<br />
conditions by 50%.<br />
14
This past year has been a journey of dreams, designs, dedication<br />
and discovery. We have been blessed to have recently opened our new facility. The talents of<br />
our nursing team were true drivers of positive change in creating our new environment.<br />
Our clinicians created our new “home” and it is phenomenal. We would be nothing<br />
without the creativity and talent of our team. Our dedication to patient care remains<br />
a driving force for us in all we do. Each of our groups is to be commended for their<br />
untiring efforts and devotion. The building is filled with innovations that are user-designed. Our<br />
team deserves kudos for continuing to give great care while juggling the demands at dual locations<br />
over an extended time frame. The challenges eased slightly with a precision patient move that was<br />
accomplished in mid-August. Yes, we really did move one patient every three minutes. Wow.<br />
While we have different challenges now, be assured that we will meet each with the same sense<br />
of care and compassion. I cannot tell you how proud I am to be on this team. The clinical staff<br />
here in London is unparalleled, in my opinion. This new facility is quite a legacy to all who<br />
created it. It is a gift and tribute to this community. We are thankful for the entire region’s<br />
support and tolerance as we worked through the multiple demands.<br />
We salute this group for their dedication in creating and transitioning into our new facility.<br />
We are delivering world-class medicine with a true hometown commitment. Please join me<br />
in congratulating the clinical team in London. We are proud to be a part of the good sisters’<br />
legacy of caring for this community.<br />
With gratitude,<br />
Peggy Green, RN, MHA<br />
Chief Operating Officer/Chief Nursing Officer<br />
SAINT JOSEPH - LONDON<br />
15
Transformational Leadership<br />
Shalan Gibbs, RN, BSN, Heart Failure Outreach Nurse, helped to design and coordinate our Heart Failure Symposium held at the London Community Center in November 2009.<br />
The Symposium featured Shalan as a speaker, as well as two of our physicians and one of our dietitians. The event also had vendors on site, prizes, a catered lunch and plenty of<br />
education for the community and clinicians that attended. This event is planned to become an annual event, each year featuring a different focus topic of some aspect of the<br />
cardiovascular system.<br />
<strong>Saint</strong> <strong>Joseph</strong> - London (SJL) received the Mission and Ministry Grant for CHF last year. With that grant funding, Shalan intercepted<br />
all heart failure patients admitted to the hospital. If the patient lived within 30 miles of the hospital, did not qualify for Home Health<br />
assistance with their heart failure, and agreed, she began to visit them at their homes. She provided physical assessments, one-onone<br />
heart failure education (or with a caregiver/family member), assistance with their medication administration, and self-care<br />
education to prevent readmission to the hospital. Patients were provided with warning signs magnets, and even scales if they<br />
needed them.<br />
Shalan Gibbs<br />
She worked in direct partnership with our Innovative Cardiac Solutions Team (who opened a patient rehabilitation<br />
program last year for cardiac patients), front line nursing staff and case managers, who are enthusiastic in educating heart<br />
failure patients about self-care and medication management of their condition. Through this collaborative effort, SJL<br />
was able to meet a very important goal on our journey to Joint Commission Advanced Heart Failure Certification:<br />
Reduce heart failure patient readmissions. We reduced them by 33%! This granted us the AHA Get with the<br />
Guidelines Bronze Award.<br />
Structural Empowerment<br />
TOUCHING THE COMMUNITY: BEYOND OUR DOORS<br />
In July, <strong>Saint</strong> <strong>Joseph</strong> - London’s Healthy Communities outreach program sponsored a Community Health Screening in Jackson County.<br />
Several nurses volunteered from SJL and worked closely with the Jackson County Health Department, White House Clinic, Manchester<br />
Memorial <strong>Hospital</strong> and volunteer cardiologists to provide blood pressure screenings, oxygen saturation measurements, finger stick<br />
glucose checks, cholesterol and other blood work to members of the Jackson County public. The nurses were from all different disciplines<br />
of health care.<br />
The Healthy Communities program also participates in a monthly clinic for the Kentucky Homeplace program, a University of Kentucky<br />
sponsored program designed to assist low-income families with their expenses of living. While these families attend this clinic, they also receive<br />
health screenings and education from nurses and physicians who volunteer from <strong>Saint</strong> <strong>Joseph</strong> - London. At the Heart Failure Clinic, people<br />
receive cholesterol screenings, vitals checks, medication assistance, detailed self-care instructions to prevent admission to the hospital, and even<br />
free scales to weigh themselves if they don’t have any. At the Diabetes Clinic, people can get their glucose checked by a volunteer nurse, foot care<br />
education, wound care education, and free testing<br />
strips and glucometers.<br />
Twice a year, our Obstetrics Department partners<br />
with Healthy Communities to host Babyfest.<br />
These events are open to the public and offer free<br />
food, educational speakers about childbirth and<br />
infant related topics, vendors, games and prizes.<br />
In FY10, we had the opportunity to help Jackson<br />
County host a Babyfest.<br />
16
NURSING FACTS:<br />
NUMBER OF NURSES<br />
RNs: 282<br />
LPNs: 27<br />
ARNPs: 6<br />
Exemplary Professional Practice<br />
HOSPITAL AWARDS<br />
2010 HealthGrades Pulmonary <strong>Care</strong> Excellence Award (5th year)<br />
2010 HealthGrades Cardiac <strong>Care</strong> Excellence Award (2nd year)<br />
2009 HealthStream Excellence Through Insight Award for<br />
Overall Employee Satisfaction and Engagement<br />
2009 HealthStream Excellence Through Insight Award for Highest Nurse Satisfaction<br />
NURSES IN ACTION<br />
Armed with education, our SANE nurses (Tracy Allen, Lori Coots, Connie Cope, Katrina Gray, Dawn<br />
Kilby, Shana Sandifer, Jamie Trett) held a Domestic Violence Vigil on the courthouse steps in October<br />
2009 to promote awareness of this too-often unnoticed killer.<br />
AVERAGE YEARS OF SERVICE<br />
0-5 years:<br />
65%<br />
6+ years:<br />
35%<br />
AVERAGE AGE OF NURSES<br />
21-40 years:<br />
62%<br />
41+ years:<br />
38%<br />
Med/Surg Director Heather Morgan, RN,<br />
BSN, was a presenter to the SJHS Medical/<br />
Surgical Reinvention Team. She presented<br />
information about bedside shift report (which<br />
we implemented in 2008) and how it improves<br />
staff communication, shortens report time, and<br />
increases patient satisfaction by including them in<br />
the health care team.<br />
Duff Holcomb, RN, from SJL Birthing Center,<br />
teaches Childbirth Classes every Tuesday and on weekends for expectant families of London. Her<br />
classes include pregnancy, warning signs during pregnancy, labor and delivery, pain relief options,<br />
Cesarean section education, post-partum and newborn care, as well as infant CPR. These classes are<br />
free to those who plan to deliver at SJL.<br />
MENTORS AND PRECEPTORS<br />
Mentor: Shelby Collins, RN, M/S; mentee: Cheryl Paul, RN<br />
Mentor: Mary Cryer, RN, M/S; mentee: Jamie Eversole, RN<br />
Mentor: Heidi Davidson, RN, M/S; mentee: Cheryl Paul, RN<br />
Mentor: Sarah Maggard, RN, M/S; mentee: Natasha Roberts, RN<br />
Mentor: Ginger Smith, RN, M/S; mentee: Karin Mathis, RN, and Cherlynn Cheak, RN<br />
CTVU preceptors: Pam Brown, RN, and Chris Griffin, RN, BSN, CCRN<br />
TURNOVER<br />
RN:<br />
11.99%<br />
Voluntary RN:<br />
7.49%<br />
17
New Knowledge Innovations and Improvements<br />
Thousands of patients in the U.S. suffering<br />
from heart attacks fail to receive critical<br />
therapy in a timely fashion, and nearly 30<br />
percent do not receive any reperfusion<br />
treatment (opening of the blocked artery)<br />
at all. As a result, the American Heart<br />
Association (AHA) created the STEMI<br />
Provider Manual. STEMI is an ST-Elevation<br />
Myocardial Infarction, the most dangerous<br />
form of a heart attack. The STEMI Provider<br />
Manual is designed to educate providers in<br />
the rapid recognition and early treatment<br />
Cath Lab Staff Nurses are now AHA STEMI Certified at SJL.<br />
strategies for patients who suffer from this<br />
type of heart attack.<br />
To ensure the <strong>Saint</strong> <strong>Joseph</strong> - London staff is trained in the recognition and treatment strategies for<br />
STEMI, all staff within the Cardiac Cath Lab have completed the manual and passed the exam. The<br />
American Heart Association recommends that patients suffering from STEMI receive reperfusion<br />
treatment within 90 minutes of entering the hospital. With an average door-to-reperfusion time of 59<br />
minutes, <strong>Saint</strong> <strong>Joseph</strong> - London consistently delivers quality care to the patients of central and eastern<br />
Kentucky.<br />
NATIONAL CERTIFICATIONS<br />
RECEIVED<br />
Cindy Angle, RN, ED: TNCC<br />
Karen Anders, RN, Hospice: CHPCN<br />
Chris Griffin, RN, CTVU: CCRN<br />
Paula Marcum, OB: IBCLC<br />
Cheryl Sasser, RN, Hospice: CHPCN<br />
ADVANCED DEGREES<br />
RECEIVED<br />
Shalan Gibbs, RN, Innov. Cardiac<br />
Solutions: BSN<br />
Carla Gilbert, RN, Infusion Svcs: BSN<br />
Paula Henson, OB CNA: ADN<br />
Sonia Jackson, Coordinator ER/Obs:<br />
BS, Management<br />
Patricia Lewis, OB Ward Clerk: ADN<br />
Leena Napier, RN, Observation: BSN<br />
AWARDS AND RECOGNITIONS DAISY Award Recipients:<br />
Karin<br />
Blankenship,<br />
RN, Med/Surg<br />
Nellie Goodin,<br />
RN, Observation<br />
Chris Griffin,<br />
RN, CTVU<br />
Melissa Walters,<br />
RN, Med/Surg<br />
Recipients of SJL’s 2010 Ambassadors of Caring Award come from various units and each was chosen by their peers<br />
who recognized their outstanding compassion shown to our patients, their families and visitors.<br />
AHA STEMI providers at SJL are Chasity Cooper, RN; Stacey Faulkner, RN; Bruce Goodrich, RN;<br />
Lena Hall, RN; Robin Harris, RN; Carmel Hensley, RN; Faith Holt, RN; Teresa Lewis, RN;<br />
JJ Parsons, RN; and Shaunnah Sizemore, RN.<br />
Empirical Quality Outcomes<br />
• SJL successfully implemented all of the required, and optional, Evidence-Based Practices—a<br />
collaborative effort among nursing, quality and leadership. We redesigned our computerized<br />
medication reconciliation form, which led to improvements in the whole process of reconciling<br />
medications and our core measures. We now have four admission/discharge nurses to help expedite<br />
the admission and discharge processes for our patients.<br />
• In June, nursing, pharmacy, materials management, education, biomedical services and IT banded<br />
together to facilitate the successful adoption of “smart pump” infusion technology. These pumps<br />
are capable of providing extra protection to patients and nurses through their “smart” technology<br />
parameters. We hope to utilize the reporting capability of these pumps to provide even safer quality<br />
care to patients.<br />
• SJL successfully implemented the LEARN system for educational requirements and elective<br />
opportunities for staff. The system contains hundreds of courses with continuing education<br />
credits attached, tracks them, and a transcript can be printed by the student at anytime. It is fully<br />
customizable and an asset to computer-based training scenarios.<br />
• With the AHA’s focus for BLS/ACLS on quality CPR, we adopted two (one adult and one infant)<br />
fully computerized BLS mannequins. They connect to a laptop loaded with specific software and can<br />
check off staff on CPR skills faster and more efficiently than ever before. Because the computer is not<br />
biased and set by internal parameters, it can ensure that CPR is done correctly every time. Learners<br />
are required to perform CPR correctly or they do not receive a card. The computerized mannequins<br />
can also be set up for “practice” mode, where someone can practice CPR with fully interactive<br />
feedback from the software—telling them immediately to slow down or speed up, or that they are<br />
giving too much breath or not enough air. Through this method, our staff will be consistently trained<br />
and practiced on quality CPR and improve overall patient survival rates after a cardiac arrest.<br />
18
I am pleased and honored to share the many accomplishments<br />
of the nursing staff and all those involved in delivery of patient care throughout the past<br />
year at <strong>Saint</strong> <strong>Joseph</strong> - Martin. Outcomes in patient care have been outstanding as we<br />
have implemented 28 Evidence-Based Practices and refined our service excellence<br />
program. Much activity also centered around expanding the continuum of care for<br />
our community as we saw the opening of a diagnostic sleep center, <strong>Saint</strong> <strong>Joseph</strong><br />
Sleep Wellness Center, and <strong>Saint</strong> <strong>Joseph</strong> Senior Renewal Center, which provides outpatient geriatric<br />
psychiatric services. We also grew our cardiology services with the addition of a full-time noninvasive<br />
cardiologist who has greatly increased the number of diagnostic procedures provided for<br />
our patients.<br />
Guided by our core values of reverence, integrity, compassion and excellence, we remain<br />
committed to achieving high quality outcomes and excellent customer satisfaction. This could<br />
not be accomplished without the dedicated, caring employees who deliver quality care on<br />
a daily basis. Our employees keep our customer satisfaction scores consistently higher than<br />
other area hospitals, maintain top performance on core measures, and have successfully<br />
implemented Evidence-Based Practices throughout the organization; but, most importantly,<br />
our employees provide such compassionate care that we often hear patients say “God is present<br />
here.” This is the impetus that inspires us daily to continue to grow our ministry at <strong>Saint</strong><br />
<strong>Joseph</strong> - Martin.<br />
With gratitude,<br />
Billie Turner, RN, MBA<br />
Chief Operating Officer/Chief Nursing Officer<br />
SAINT JOSEPH - MARTIN<br />
19
Transformational Leadership<br />
Transformational Leadership is about taking what you do well and continuing to improve upon it. <strong>Saint</strong> <strong>Joseph</strong> - Martin (SJM) always strives to deliver optimum patient care. Often<br />
this calls for transforming how we provide that care.<br />
Evidence-Based Practice (EBP) continues to be at the forefront at SJM. We were successful this year in implementing 28 EBPs as part of the CHI national initiative.<br />
Implementation of these practices resulted in a greater than 50% reduction in hospital-acquired conditions.<br />
The Med/Surg unit was restructured to include the charge nurse role. This restructuring was implemented with the goal of providing more time for direct<br />
caregivers to be at the bedside. Designated charge nurses received education and development opportunities centered around leadership and team building<br />
through change leadership training.<br />
Mary Martin, RN, infection preventionist, participated with other infection prevention specialists throughout the region in an effort to address<br />
community-acquired infection rates. The group consisted of infection control nurses and infectious<br />
disease physicians throughout eastern Kentucky.<br />
Structural Empowerment<br />
Reaching out to the community has always been an important part of the ministry at SJM.<br />
TOUCHING THE COMMUNITY: BEYOND OUR DOORS<br />
Several nurses participated in SJM’s annual Senior Health Fest. The Senior Health Fest is a<br />
community event offered to those 55 and older. Health information on numerous topics, health<br />
screenings and flu shots are provided along with food and fun. Nurses participating were Teresa<br />
Bailey, Neva Francis, Cathy Johnson, Mary Little, Mary Martin, Carol Jo May, Kim Sanders-Castle<br />
and Melinda Stumbo.<br />
160 foster children in Floyd County had a brighter Christmas due to the SJM Angel Tree sponsored<br />
by employees.<br />
All departments were involved in fundraising activities for the 2010 Relay for Life event, resulting in<br />
a record-setting amount being raised for SJM as well as Floyd County.<br />
Food and fun were had by all during the 2010<br />
Nurses’ Week. During the celebrations several nurses<br />
were recognized for perfect attendance during 2009.<br />
Those recognized were Teresa Bailey, Sharon Bates,<br />
Carol Bentley, Neva Francis, Susan Goble, Krystal Hall,<br />
Theresa Hyden, Jessica Kidd, Tammy King, Carol Jo<br />
May, Natashia Osborne, Cindy Patton, Tina Pinson, Angie<br />
Salisbury, Sherry Slone, Melinda Stumbo and Billie Turner<br />
(pictured left).<br />
20
NURSING FACTS:<br />
NUMBER OF NURSES<br />
RNs: 48<br />
LPNs: 11<br />
Exemplary Professional Practice<br />
Recognizing the importance of expertise and professionalism, all nurses are encouraged to grow and<br />
develop in their career and assist the profession by helping others develop.<br />
Through formalized relationships with area schools of nursing, SJM nurses are afforded the opportunity<br />
to serve as preceptors and mentors for students and graduates. Carol Bentley, LPN; Lynn Goble, RN;<br />
Wanda Hall, RN; Kathy Moore, RN; and Leeda Music, RN, mentored students throughout the year.<br />
AVERAGE YEARS OF SERVICE<br />
0-5 years:<br />
41%<br />
6+ years:<br />
59%<br />
AVERAGE AGE OF NURSES<br />
21-44 years:<br />
49%<br />
45+ years:<br />
51%<br />
New Knowledge Innovations and Improvements<br />
Continuous Performance Improvement remains a high priority at SJM as we strive to always improve<br />
the quality of care provided.<br />
• Electronic documentation was expanded to include EBP requirements for Catheter Associate<br />
Urinary Tract Infection and DVT screening. Following implementation, DVT screening for<br />
inpatients improved from 78% to 95%.<br />
• The Nurse Call System was upgraded to facilitate better communication between the bedside<br />
nurse and the patient by allowing the patient to call the nurse directly, resulting in improved<br />
nursing response times.<br />
• Bedside registration was implemented in the Emergency Department.<br />
• An electronic status board for tracking EBPs and other patient care information was developed<br />
for the Med/Surg unit.<br />
• As part of the Med/Surg restructure, bedside report was initiated. This provides opportunities<br />
for better communication between nurses, safer handoffs from shift to shift, and improved<br />
communication with patients. The beside report initiative resulted in an improvement in patient<br />
satisfaction scores related to nurse communication from 85% in FY09 to 96% for FY10.<br />
• An ultrasound for bedside bladder scanning was purchased and procedures were implemented<br />
to prevent unnecessary insertion of urinary catheters.<br />
• eClinical Reference Solutions was made available for use by all clinical staff. This includes three<br />
evidence-based references encompassing more than 30 full text nursing references, 31 full text<br />
professional journals and 8,000 patient education handouts.<br />
TURNOVER<br />
RN:<br />
18%<br />
21
Empirical Quality Outcomes<br />
• Patient satisfaction remains a top priority for SJM, resulting in scores for overall satisfaction and<br />
ranking in the top 10 within CHI throughout FY10.<br />
• The Emergency Department implemented processes and mechanisms to improve the door-todoctor<br />
time and saw an 11% reduction in the time, resulting in a decrease from an average wait of 48<br />
minutes to 41 minutes. Efforts will be continued to meet the goal of 30 minutes.<br />
• The Agency for Healthcare Research and Quality Culture of Patient Safety survey was conducted<br />
with SJM receiving an “A” rating with a score of 90.3% in overall perceptions of safety.<br />
• The triennial unannounced Joint Commission survey was conducted with exceptional results of only<br />
two findings, both of which were related to the environment of care standards. There were no clinical<br />
recommendations during the survey.<br />
• The Surgery Department implemented the World Health Organization (WHO) Surgical Safety<br />
Checklist and the CHI surgical counts policy to improve surgical safety for our patients. We had 0%<br />
surgical never events.<br />
• A new wound care protocol was developed and implemented for inpatients. The protocol includes a<br />
standardized assessment, reassessment and treatment protocol.<br />
• As part of the Service Excellence program, the Surgery Department developed personalized thankyou<br />
cards that are mailed to each patient following their surgery. This and other service excellence<br />
initiatives resulted in Same Day Surgery patient satisfaction ranking 4th in CHI for FY10.<br />
• SJM continued to be involved in region 9 disaster planning activities by participation in a regional<br />
disaster drill that tested the area’s preparedness for any community-wide emergency situation.<br />
NATIONAL CERTIFICATIONS<br />
RECEIVED<br />
Carla Hayes, RN: CNOR<br />
Mary Martin, RN: CIC<br />
ADVANCED DEGREES<br />
RECEIVED<br />
Tammy King, LPN: ADN, RN<br />
AWARDS AND RECOGNITIONS<br />
Natashia Osborne, RN, was the<br />
recipient of the Waneta P.<br />
Newsome Award. This award<br />
recognizes employees who best<br />
exemplify the core values.<br />
DAISY Award Recipients:<br />
LEADERSHIP IN<br />
PROFESSIONAL<br />
ORGANIZATIONS<br />
Billie Turner, COO/CNO, member<br />
of Big Sandy Community and<br />
Technical College Advisory Board;<br />
board member of <strong>Saint</strong> Vincent’s<br />
Mission; Chair of Floyd County<br />
Relay for Life Survivorship<br />
Committee.<br />
Melinda Stumbo, RN, member<br />
Region 9 Healthcare Preparedness<br />
Planning Committee.<br />
Kay Fugate,<br />
RN, ED<br />
Theresa Hyden,<br />
RN, House<br />
Supervisor<br />
Cathy Johnson,<br />
RN, Med/Surg<br />
Natashia<br />
Osborne, RN,<br />
Surgery<br />
22<br />
Nurses (from left) Jan White, Jenny Twiss and Lisa Little and their team members in the Emergency Department<br />
implemented processes and mechanisms to improve the door-to-doctor time, resulting in a decrease from an<br />
average wait of 48 minutes to 41 minutes. Efforts will be continued to meet the goal of 30 minutes.
In this past year, our nursing team at <strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling<br />
has continued our pursuit of high quality care for our patients and community, provided<br />
by an educated and highly competent nursing staff. Our accomplishments include the<br />
implementation of numerous Evidence-Based Practices, along with our sister hospitals,<br />
initiation of changes in staffing and scheduling to be responsible stewards related<br />
to expenses and productivity, launch of the new Observation/Inpatient E.H.R.<br />
program, and successful improvements in clinical areas of patient care related to our core measures.<br />
Our progress was acknowledged when our body of work on “Transforming Cardiac <strong>Care</strong> in a Rural<br />
Setting” was honored with two awards. The first award was from Catholic Health Initiatives and<br />
was received at the annual Quality & Risk Conference in St. Louis. The second award was from<br />
the Kentucky Organization of Nurse Leaders and was received at the annual KHA Convention<br />
in Lexington in May. As we continue our work in the quality arena, we are focusing on the<br />
Orthopedic Service re-assessment as part of the Clinical Covenant, and we are participating in the<br />
ED Reinvention and Med/Surg Reinvention teams to improve care and service to all our patients.<br />
In addition to quality, our leaders and nurses are committed to Growth and Stewardship.<br />
Nursing participates in activities related to growing our business, such as physician recruitment<br />
and the development of new procedures and services. Nurses are actively engaged in planning<br />
and designing the new hospital, which will open in 2011. With regard to Stewardship, our nurses<br />
understand the need to meet productivity targets, keep overtime to a minimum, and match<br />
worked hours to volumes. I am proud to present our accomplishments in the next few pages.<br />
With gratitude,<br />
Cinda Fluke, M.Ed., BSN, NEA-BC<br />
Chief Operating Officer/Chief Nursing Officer<br />
SAINT JOSEPH - MOUNT STERLING<br />
23
Transformational Leadership<br />
<strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling (SJMS) continues to develop our leadership team through a variety of activities and opportunities. Our site visits to other health care organizations have<br />
provided us with information to update our practices, procedures, skills and equipment. Our exposure to the Master Facility Planning process has presented an opportunity to<br />
dream big, while being intentional and pragmatic in our planning for our new hospital and the patient care, service and flow we want to provide. This particular learning<br />
experience forces us to reevaluate everything; it is a detailed process both fun and demanding, as we anticipate how we will be better able to serve our community in this<br />
new space.<br />
As we continue to promote a culture of learning at SJMS, our leaders have been the role models for professional development. At this time, 100% of the nursing<br />
leadership team is BSN-prepared or enrolled in a BSN program. Three of the nursing leaders who are in BSN courses will graduate in the spring of 2011. In<br />
addition, 38% of this team is master’s degree-prepared or enrolled in a master’s degree program.<br />
As our nursing staff has witnessed their leaders’ pursuit of additional education, it has spawned a return to college for numerous employees. We have<br />
nursing assistants who are pursuing nursing degrees, LPNs returning for an RN degree, and RNs returning for a BSN. Approximately 5% of the RNs<br />
at SJMS are currently pursuing an MSN.<br />
Our hospital is a clinical site for 87 nursing students from the area nursing programs. We host nursing students six days per week, with Sunday<br />
as the only day students are not on our units. We have provided clinical rotations in all areas, allowing all our nurses the experience of helping<br />
develop new nurses into the profession. SJMS partners with Morehead State University and Maysville Community College to provide clinical<br />
opportunities for nursing students.<br />
Structural Empowerment<br />
<strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling places value on advancing nursing education. During fiscal year 2010, Edwina Melton, RN, obtained her<br />
advanced registered nurse practitioner degree and Leah English, SW, completed her registered nurse degree.<br />
SJMS nurses developed “always the best” standards, focusing on people, stewardship, quality and growth. These standards are a commitment<br />
to our patients and executive leadership to provide safe, cost-effective care to all who enter our doors. Every area of nursing developed their<br />
standards, which serve as the basis for our achievements in Perfect <strong>Care</strong> and Service Excellence.<br />
ER and Med/Surg nurses developed and led an interdisciplinary committee in order to increase communication and develop<br />
constructive relationships. This committee resulted in a positive rapport and improved flow between the participating<br />
departments, as well as improved hand-off communication and patient satisfaction.<br />
TOUCHING THE COMMUNITY: BEYOND OUR DOORS<br />
<strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling is an active participant in the Montgomery County Relay for Life. Our Relay for Life<br />
team consists of nurse managers and staff nurses. Sheila Barnes, OR nurse manager, serves as the event chair for the<br />
entire county. For several years, SJMS has played a prominent role in Relay events and activities in our community.<br />
“A Walk to Remember” is held annually in Mount Sterling, a day set aside for families to come together to<br />
acknowledge and honor a child or children lost, including losses from miscarriage, fetal death, still birth or SIDS.<br />
In October 2009, approximately 150 community members and SJMS employees participated in the event.<br />
Nurse leaders at SJMS, in collaboration with the Montgomery County Cancer Coalition, sponsor a health forum<br />
about cancer, specifically directed to women in Montgomery, Bath and Menifee Counties. This forum seeks to raise<br />
awareness and educate community members about cancer.<br />
24
Nursing Facts:<br />
NUMBER OF NURSES<br />
RNs: 102<br />
LPNs: 15<br />
ARNPs: 2<br />
Masters: 6<br />
Nurse leaders and RNs serve the community in these volunteer capacities and memberships:<br />
• Advisory Board for St. Claire Home Health • Kentucky Association for Healthcare Quality<br />
and Hospice<br />
(and NAHQ)<br />
• Bluegrass Association for Healthcare Quality • Kentucky Organization of Nurse Leaders<br />
• Board member of Montgomery County • Montgomery County Cancer Coalition<br />
Health Department<br />
• Montgomery County Chamber of Commerce<br />
• Board member of Gateway Children’s Services • Participation in community health fairs and<br />
• Church ministry in several local congregations local events<br />
• Clothing drives, bake sales and food donations • Participation in health screenings and health<br />
to local charities and churches<br />
information sessions at local schools<br />
• Frequent blood donors<br />
AVERAGE YEARS OF SERVICE<br />
0-5 years:<br />
45%<br />
6+ years:<br />
55%<br />
AVERAGE AGE OF NURSES<br />
21-40 years:<br />
47%<br />
Exemplary Professional Practice<br />
Along with the other <strong>Saint</strong> <strong>Joseph</strong> Health System hospitals, <strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling implemented<br />
all Evidence-Based Practices (EBP), with a result of reaching the targeted 50% or greater reduction in<br />
the corresponding indicators. We are proud to have received a high CRMIP score, excellent report on<br />
our Anthem scorecard, and acknowledgement from CMS that our quality program and core measures<br />
are “awesome.” This reflects the work of the whole team, coming together to work toward high quality<br />
of care, and being committed to that end.<br />
Through the work of the Med/Surg Reinvention team, we are exploring the pursuit of Heart Failure<br />
Accreditation. We are working with the Diabetic Treatment team to implement improved protocols<br />
for glycemic control for our patients. We have implemented numerous initiatives as part of the ED<br />
Reinvention team and will soon be launching the “5 and 30” program (“No Wait ER”).<br />
With facilitation by nursing and quality leaders, SJMS launched the “Treatment and Planning Team” in<br />
the Spring of 2010. This interdisciplinary team meets monthly to review selected cases, with regard to<br />
diagnosis, treatment and care planning. These fascinating cases (focus on oncology patients) offer lively<br />
discussion and have led to improved collaboration, care planning and hand-off communication.<br />
TURNOVER<br />
RN:<br />
10.23%<br />
Voluntary RN:<br />
5.68%<br />
Vacancy:<br />
4.41%<br />
41+ years:<br />
53%<br />
Our Case Management team has restructured responsibilities in order to improve in numerous areas.<br />
Length of Stay (LOS) management has resulted in a very low all-payer average LOS of 3.2 for the fiscal<br />
year. Improvements have been made in overturning denials from third-party payers and documenting<br />
medical necessity for inpatient stays.<br />
Through the efforts of our Clinical Educator, Infection Control, Pharmacy and Nursing leaders, we<br />
realized amazing success with our Flu Shot program this fiscal year, increasing from 43% compliance to<br />
73% compliance with our employees.<br />
The new <strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling facility will open in the summer of 2011.<br />
25
New Knowledge Innovations and Improvements<br />
As new physicians have come to SJMS, our services, procedures and skills have grown. Having a<br />
pulmonary intensivist has resulted in an increase of care for critically ill patients, requiring additional<br />
skills for the all-RN ICU staff. Biphasic defibrillators have replaced monophasic defibrillators on all<br />
nursing units.<br />
Over the past year, SJMS has added laparoscopic colectomies to our OR procedures, in addition to<br />
other procedures being performed by two new general surgeons. The OR staff has cross-trained in many<br />
areas in order to accommodate a growing volume with additional variety.<br />
SJMS’s Sleep Wellness Center is now hospital-run, instead of being provided by a contract service.<br />
With that change came new equipment and the availability of capnography equipment, serving both<br />
the Sleep Wellness Center, as well as inpatients with sleep disorders.<br />
Empirical Quality Outcomes<br />
Some of SJMS’s accomplishments for FY10:<br />
• Core measure scores improved for SCIP, pneumonia and heart failure<br />
• <strong>Hospital</strong>-acquired conditions decreased from prior year, from 7.75% to 3.69%<br />
• Inpatient falls decreased by 52% and there were zero falls with major injury<br />
• Median time for door-to-EKG improved from 6 minutes to 4 minutes<br />
• Mortality rate decreased for the second year in a row (2%) and there were zero Box D deaths<br />
• Zero surgical never events<br />
NATIONAL CERTIFICATIONS<br />
RECEIVED<br />
Kimberly Hamilton, RN, ED: CCM<br />
Phyllis Lucas, RN, Case<br />
Management: CWOCN<br />
Tim Winterfeld, RN, ICU: CCRN<br />
Teresa Murphy, RN, OR: CST<br />
Cinda Fluke, RN, Administration:<br />
NEA–BC<br />
ADVANCED DEGREES<br />
RECEIVED<br />
Kemberly Spencer, RN, House<br />
Administrator: MSN<br />
Edwinna Melton, RN, ED: MSN<br />
Tina O’Hair, LPN, ED: ADN<br />
Leah English, SW, Case<br />
Management: BSN<br />
AWARDS AND RECOGNITIONS<br />
In March 2010 our poster<br />
presentation for “Transforming<br />
Cardiac <strong>Care</strong> in a Rural Setting”<br />
was awarded 4th place by<br />
Catholic Health Initiatives.<br />
In May 2010 our poster presentation<br />
for “Transforming Cardiac <strong>Care</strong><br />
in a Rural Setting” was awarded<br />
1st place by the Kentucky<br />
Organization of Nurse Leaders at<br />
the KHA Convention.<br />
In October 2009 the SJMS<br />
Orthopedic Service presented<br />
a body of work at the annual<br />
tri-state quality conference and<br />
was recognized by Anthem,<br />
receiving the “Successful Practice<br />
Program” award.<br />
DAISY Award Recipients:<br />
Dana Brundon,<br />
RN, PACU<br />
Teresa Tufano,<br />
RN, Med/Surg<br />
<strong>Saint</strong> <strong>Joseph</strong> - Mount<br />
Sterling Emergency<br />
Department nurses and<br />
paramedics from the<br />
Montgomery County<br />
Fire/EMS launched a<br />
new program this year<br />
that utilizes wireless<br />
EKG technology to slash<br />
time from heart attack<br />
diagnosis to treatment.<br />
The wireless EKG technology transmits data directly to the <strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling Emergency<br />
Department from the scene, such as a patient’s home, saving valuable time for heart attack victims.<br />
In a flash, a physician in the <strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling Emergency Department can read the results<br />
to determine if a patient is suffering a heart attack, all before the patient is even transported.<br />
26<br />
<strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling’s body of work on “Transforming Cardiac <strong>Care</strong> in a Rural Setting”<br />
was honored with two awards. The first was from Catholic Health Initiatives and was received<br />
at the annual Quality & Risk Conference in St. Louis in March. The second award was from the<br />
Kentucky Organization of Nurse Leaders and was received at the annual KHA Convention in<br />
Lexington in May.
Excellence in patient care at Flaget Memorial <strong>Hospital</strong> is an expectation<br />
of each person who trusts us to provide service in a time of dependency and vulnerability.<br />
Our community expects the best care and our mission impels us to provide a safe place to<br />
heal. This requires constant vigilance and a commitment to do the right thing with each<br />
patient encounter. The addition of new services and physicians to our community<br />
makes the role nurses play as the last line of defense even more imperative.<br />
To ensure patient safety remains first, Flaget Memorial <strong>Hospital</strong> engaged in the system goal of<br />
implementation of evidenced-based practices. In addition, the engagement of the nursing staff<br />
and other clinical partners at the point of care took on a new look as LEAN strategies helped us<br />
define points of delays and barriers to the patient flow and care process. The positive change in<br />
our culture is evident as staff nurses look for ways to improve processes on a daily basis and feel<br />
empowered to take an immediate action or make a needed change.<br />
After a recent obstetrical emergency, one of our staff surgical nurses came in the next day on her<br />
day off and debriefed the obstetrical nurses. The group developed a list of improvements that<br />
they presented to leadership the following Monday. The recommendations were put in place<br />
the next week. How comforting to know that departmental barriers no longer hinder us from<br />
doing what is best for the patient.<br />
Nursing continues to be the most trusted profession. The nurses and clinicians at Flaget<br />
Memorial <strong>Hospital</strong> know this trust is earned on a daily basis.<br />
With gratitude,<br />
Sue Downs, RN, MSN, BSN, CRRN<br />
Chief Operating Officer/Chief Nursing Officer<br />
FLAGET MEMORIAL HOSPITAL<br />
27
Transformational Leadership<br />
In 2008 the Flaget Memorial <strong>Hospital</strong> (FMH) leadership team began reading Jim Collins’ book Good to Great. Implementation of the key concepts throughout the hospital began<br />
with “Picking the right people first, and then figuring out where to go.” Nursing leaders collaborated with HR leaders to implement a “shadowing process” prior to hire to ensure<br />
the right persons are “on the bus.” Each potential nursing hire shadows with a nursing staff member for a minimum of four hours. Multiple persons interview the candidate<br />
and all must agree the person is the right fit. That is, the person is passionate about our healing ministry and patient safety. This process continued throughout 2010. Our<br />
voluntary RN turnover was at a record low in FY10 of 3.08%.<br />
In 2010, nurses and other caregivers committed to another concept in the book to “develop the discipline to do the right thing and to stop doing the wrong<br />
things.” Through the leadership of nurses and clinicians from multiple departments, facilitated by Cheri Davidson, RN, MSN, the journey began with<br />
detailed charts of our current processes to identify delays and barriers to patient flow and safety. This working document is posted in the units for feedback<br />
on a daily basis when problems are identified in real time. The nursing staff is empowered to make quick fixes within their respective departments.<br />
<strong>Person</strong>s are challenged to think through old processes and defend the need to continue the practice if it is not relevant to the mission.<br />
Structural Empowerment<br />
Flaget Memorial <strong>Hospital</strong>’s Nurse Council continues to use a self-governance model. The council identifies problems and works with other<br />
departments to resolve them. They approve new products and identify problems with products, such as IV start kits and upgrade of ace wrap<br />
bandages. The group provided guidance and approvals through the Evidence-Based Practice implementations. They review and approve all<br />
nursing policies and procedures to verify accuracy and reflection of concurrent practices.<br />
Bedside nurses and clinicians met each week using LEAN concepts to identify the barriers and delays in care in the ED and for the<br />
orthopedic patients admitted to our hospital. The empowerment the employees feel is evident in other areas of the hospital as we experience<br />
the breaking down of departmental silos when employees talk outside of these meetings to make a quick fix that will benefit patient care. For<br />
example, the OR and OB nurses wrapped the surgical packs that are needed during an emergency C-section with pink so anyone can easily<br />
identify what needs to be opened in an emergency.<br />
TOUCHING THE COMMUNITY: BEYOND OUR DOORS<br />
The annual Birth Center Community Baby Fair was held April 24, 2010, in Bardstown for expecting parents, parents of toddlers and anyone<br />
planning a pregnancy. Members of the Birth Center staff planned and implemented the fair. Nurses volunteered to work in the<br />
Nelson County Community Clinic, which is a free clinic with a focus on health care for the working uninsured population<br />
of Nelson County. Flaget Memorial <strong>Hospital</strong> provides and supports first-aid booths at the Bourbon Festival, Old<br />
Kentucky Home Bike Tour, Bourbon Chase, and the Bourbon City Challenge.<br />
Volunteers from the hospital participated in fundraising walks and other events associated with March of Dimes,<br />
Relay for Life, American Heart Association, Go Red for Women, and Colon Cancer Awareness. We sponsored<br />
the Relay for Life survivors’ tent in Bullitt, Marion and Nelson counties that included a hospital speaker in<br />
each county highlighting the new Cancer Center at FMH. St. Vincent DePaul food drive and back-to-school<br />
drives continued with great success. FMH sponsored “Faces of Cancer” for seven surrounding counties,<br />
highlighting the courage of survivors of cancer.<br />
Nurse volunteers active on community boards include Delisa Arnold, RN, who serves on the planning<br />
committee for the March of Dimes Tri-County walk; Jill Clark, RN, BSN, Nelson County Community<br />
Clinic Board; Cheri Davidson, RN, MSN, National League of Nursing Accreditation Commission; Sue<br />
Downs, RN, MSN, Advisory Board for St. Catherine College and president of Kentucky Organization of Nurse<br />
Leaders; Jerri Passo, RN, BSN, ambassador for American Heart Association with Go Red for Women campaign;<br />
and Rick Vancise, RN, MBA, Advisory Board for Elizabethtown Community College Nursing Program.<br />
28
Nursing Facts:<br />
NUMBER OF NURSES<br />
RNs: 202<br />
LPNs: 8<br />
ARNPs: 8<br />
MSNs: 14<br />
Exemplary Professional Practice<br />
All directors and managers completed a book review with the leadership team on StrengthsFinder.<br />
Leaders’ strengths were identified and shared in discussions with the group. The positive energy of<br />
looking at strengths instead of weaknesses continues to reap benefits.<br />
<strong>Hospital</strong> staff members also participated in opportunities for professional development and outside<br />
presentation. Nurses on inpatient units developed a poster presentation on “Inpatient Satisfaction<br />
Improvement Process” that won first place at the CHI Quality and Risk Conference in April 2010.<br />
Norma Goss, RN, BSN, presented at the conference on improving inpatient satisfaction and at the<br />
Kentucky Organization of Nurse Leaders district meeting.<br />
AVERAGE YEARS OF SERVICE<br />
0-5 years:<br />
59%<br />
6+ years:<br />
41%<br />
AVERAGE AGE OF NURSES<br />
21-44 years:<br />
48%<br />
Jerri Passo, RN, BSN, shared her personal story at Go Red for Women events in Bardstown and<br />
Lexington. Sue Downs, RN, MSN, taught a wellness class at First Christian Church in Elizabethtown,<br />
Ky., and spoke at the survivors’ meeting during Relay for Life for both Nelson and Hardin counties.<br />
EDUCATIONAL ACCOMPLISHMENTS AND MENTORING<br />
Flaget Memorial <strong>Hospital</strong> provides mentoring and preceptors for nursing students upon completion of<br />
a nursing program. Elizabethtown Community College, Galen College and <strong>Saint</strong> Catherine College<br />
use the hospital for clinical rotations.<br />
TURNOVER<br />
RN:<br />
13.85%<br />
Voluntary RN:<br />
3.08%<br />
Vacancy:<br />
5.26%<br />
45+ years:<br />
52%<br />
The hospital provided education throughout the year with an Advanced Cardiac Life Support<br />
Provider course, Cardiopulmonary Life Support Provider course, Neonatal Resuscitation Provider<br />
course, Nonviolent Crisis Intervention training program, and Pediatric Advanced Life Support<br />
Provider course. Other offerings included Assessment of the Pulmonary System III, Cardiac Rhythm<br />
Interpretation course, Hospice volunteer training, KODA workshop, Interventions to Decrease Postoperative<br />
Respiratory Complications, Identification and Application of Appropriate Patient Transfer<br />
Techniques, <strong>Care</strong> of the Post Surgical Bariatric Patient, Bariatric Surgical Procedures and Signs and<br />
Symptoms of Transfusion Reactions.<br />
Three nurse leaders participated in the AONE Aspiring Nurse Leader course sponsored by CHI. Kim<br />
Buckley, ARNP, attended the <strong>Hospital</strong>ist Boot Camp. Cheri Davidson, RN, MSN, completed a course<br />
called “LEAN for Healthcare.” Sue Downs, RN, MSN, attended the ACHE Chief Operating Officer<br />
Boot Camp.<br />
29
New Knowledge Innovations and Improvements<br />
Laura Larue, RN, BSN, MBA, worked with other hospital and emergency community leaders to train<br />
the executive team and leadership on command center operations during emergencies.<br />
The Fall Prevention Program included putting into place identification of assistive devices and patients<br />
at high risk for falls that resulted in fewer falls and a secondary outcome of a significant decline in<br />
employee injuries by 42.8% in FY09. Marlene Hardin, RN, BSN, Director of Medical Surgical Services,<br />
worked with the Med/Surg nursing staff in 2010 to focus on reduction of employee injuries on the<br />
unit. The nursing staff received education on transfers and lifting devices. More importantly the buy-in<br />
was obvious as we decreased our employee injury costs on the unit from $3,931/30 full-time employees<br />
to $323/30 full-time employees.<br />
Bariatric cases started in December of 2010. The new Flaget Center for Weight Loss Surgery required all<br />
nurses and nursing personnel to attend classes. Our first patient successfully improved her quality of life<br />
by increased mobility, controlled blood pressure without medication, and a weight loss of 80 pounds.<br />
CLINICAL COVENANT WORK<br />
About 18 months ago, the governing board for <strong>Saint</strong> <strong>Joseph</strong> Health System challenged each of the<br />
hospitals to implement a concept that few other hospitals have been successful in implementing. The<br />
concept was the Clinical Covenant. After implementation of the Clinical Covenant, care at the bedside<br />
would be changed through the formation of a transactional relationship between the patient and caregiver.<br />
NATIONAL CERTIFICATIONS<br />
RECEIVED<br />
Andrea Ames, CEN<br />
Stephanie Bradshaw, RN, Wound <strong>Care</strong><br />
Certified Nurse (WCCN)<br />
Sarah Livers, RN, Certified SANE Nurse<br />
ADVANCED DEGREES<br />
RECEIVED<br />
Laura Larue, MBA<br />
LEADERSHIP IN PROFESSIONAL<br />
ORGANIZATIONS<br />
Delisa Arnold, RN, serves on the<br />
Program Committee for KONL.<br />
Sue Downs, RN, MSN, CRRN,<br />
is president of the Kentucky<br />
Organization of Nurse Leaders<br />
(KONL).<br />
LEADERSHIP IN NURSING<br />
Delisa Arnold, RN, Director of Birth<br />
Center and Skilled Nursing Unit<br />
Susan Brown, RN, Manager of<br />
OR and PACU<br />
Cheri Davidson, RN, MSN, VP of<br />
Quality, Risk and Medical Staff<br />
Sue Downs, RN, MSN, COO/CNO<br />
Norma Goss, RN, BSN, Director of<br />
Nursing Services<br />
Marlene Hardin, RN, BSN, Manager of<br />
Medical Surgical Services<br />
Carolyn Hollingshead, RN, Manager<br />
of Pain Management<br />
Brooke Hurst, RN, BSN, Manager of<br />
Critical <strong>Care</strong> Services<br />
Laura Larue, RN, MBA, Director of<br />
Emergency Services<br />
Carrie Medley, RN, Manager of Flaget<br />
Immediate <strong>Care</strong> Clinic<br />
Pat Russman, RN, Manager of<br />
Oncology Services<br />
Rick Vancise, RN, MSN/MBA, Director<br />
of Outpatient and Projects<br />
Geri Werkman, RN, Director of<br />
Surgical Services<br />
AWARDS AND RECOGNITIONS<br />
Delisa Arnold, RN, Director of Birth<br />
Center and Skilled Nursing Unit,<br />
awarded a KONL scholarship.<br />
DAISY Award Recipients:<br />
Cheryl Bundy.<br />
RN, House<br />
Supervisor<br />
Dianne Chesser,<br />
LPN, Med/Surg<br />
Anna Culver,<br />
RN, Surgery<br />
Natalie Vancise,<br />
RN, House<br />
Supervisor<br />
30<br />
Flaget Memorial <strong>Hospital</strong> was given the honor of being the pilot hospital for this design work. In<br />
February 2010, Flaget met with <strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling, <strong>Saint</strong> <strong>Joseph</strong> - London and <strong>Saint</strong> <strong>Joseph</strong><br />
East to begin the journey. The charter of the team was to create an environment where the patient<br />
receives highly reliable, patient-centered, seamless, transparent care. The fundamental basis of this work<br />
is to promise patients that we will always do certain things and always not do certain things.<br />
Our journey is involving many different facilities and many of our departments and staff. With this<br />
collaboration between Flaget’s Ortho Clinical Covenant Team (“Hercules”) and other stakeholders,<br />
perspectives have been broadened. This is allowing us to realize the importance of consistency in the way<br />
we work and in the way we work together, to ensure our patients’ experiences are seamless and highly<br />
reliable, while at the same time improving patient safety, care and satisfaction.<br />
Empirical Quality Outcomes<br />
• The respiratory care bundle initiated in 2006 continues to show a decrease in complications and<br />
readmission rate of adults with respiratory conditions. The hospital decreased the readmission rate<br />
from 12% to 7.5% in calendar year 2009. The impact of this work was recognized nationally with<br />
the HealthGrades 5-star rating for COPD survival rates.<br />
• OB compliance to the perinatal bundle is 100%. Newborn transfer rates to a higher level of care<br />
declined by 40% from FY09 to FY10.<br />
• Skilled Nursing remained number one in patient satisfaction for subacute units in CHI. This unit<br />
continues to demonstrate outstanding care for over a decade. Nursing Home Compare, a federal<br />
website sponsored by CMS, rates the unit as a Five-Star facility (with five stars being the best).<br />
• FMH received the HealthGrades 5-star rating for Hip Fracture Repair complication rates.<br />
• BMCA continues to make a difference. The success of this is based on the nurses’ compliance<br />
with using the system. FMH nurses are committed to providing safe administration of<br />
medications; therefore, our<br />
scan rate is over 92% for all<br />
medications administered on<br />
our inpatient units. While<br />
nationally a .5/1000 doses error<br />
rate is considered acceptable,<br />
with BMCA FMH reduced our<br />
medication error rate last fiscal<br />
year to a historical low rate of<br />
.09/1000 doses.<br />
0.8<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
Flaget Memorial <strong>Hospital</strong> — Medication Errors per 1000 Doses<br />
January 2006 to June 2010<br />
BMV <strong>Hospital</strong><br />
Wide Dec 2007<br />
QUALITY EVIDENCE<br />
0<br />
• Recognition of physicians as<br />
Jan-Dec 2006 Jan-Dec 2007 Jan-Dec 2008 Jan-Dec 2008 Jan-Jun 2010<br />
internal customers is the driving force to remove barriers that would discourage the use of FMH<br />
services and impede growth. Physicians are often heard to say that our “Nursing services far surpass<br />
those in surrounding hospitals.” As a result, volumes grew in admissions by 8%, 21% in general<br />
surgery, 22% in Hospice, and 3% in ED. FMH’s surgical team continues to turn around rooms in<br />
12.7 minutes safely and efficiently, as other surgical departments struggle to get to 15 minutes.<br />
• FMH implemented 28 evidenced-based standards as part of the system initiative that resulted<br />
in a decrease of Health <strong>Care</strong> Acquired Conditions. A big thank-you to the registered nurse team<br />
leaders: Susan Brown, RN; Jill Clark, RN, BSN; Nancy Fink, RN; Brad Gagne, RN; Norma Goss,<br />
RN, BSN; Marlene Hardin, RN, BSN; Barbara Leake, RN; Jerri Passo, RN, BSN; Clara Powell,<br />
RN, BSN; and Ricky Reiter, RN, BSN. Also, a special thank-you to Bernadette Sutherland for<br />
clerical support and coordination of the project.
SAINT JOSEPH HOSPITAL • SAINT JOSEPH EAST<br />
We are pleased to present the 2010 Nursing<br />
Annual Report, “<strong>Person</strong>-<strong>Centered</strong> <strong>Care</strong>.”<br />
This report reflects the previous year’s work and the many accomplishments for which<br />
all <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> (SJH), <strong>Saint</strong> <strong>Joseph</strong> East (SJE) and <strong>Saint</strong> <strong>Joseph</strong> - Jessamine<br />
(SJJ) nursing team members should take pride. The report is an excellent venue for<br />
acknowledging the tremendous effort each nurse puts forth each day to deliver<br />
collaborative and compassionate care. It also allows us to reassess our current<br />
state, determine our gaps and refocus for future opportunities and<br />
progress. In 1914 Florence Nightingale said, “Unless we are<br />
making progress in nursing, every year, every week, take my<br />
word for it, we are going back.”<br />
Throughout this annual report, there are countless illustrations of nurses<br />
demonstrating unwavering commitment to providing evidence-based, highquality,<br />
person-centered care, which is central to our mission. At the core of patientcentered<br />
care is patient safety. Patient safety continues to be a driver for numerous<br />
new ideas and changes at SJH/SJE/SJJ. Nurses have a sense of pride in fulfilling our<br />
responsibility to keep patients safe. Each day we hear testimonies from patients and families<br />
acknowledging how nurses make a difference in the lives of so many people.<br />
As we embark on another year, rapid changes in health care will challenge us<br />
daily. Expectations for efficient, high-quality, cost-effective care, along with the<br />
complexity of patient care, will require us to focus on developing future patient<br />
care delivery processes that sustain quality outcomes. Our accomplishments as<br />
portrayed in this annual report are a clear reflection of the contributions made<br />
by nurses at every level of the organization. While we reflect on our previous<br />
year’s accomplishments, we have greater expectations for our future, based on our<br />
commitment to reverence, integrity, compassion and excellence.<br />
We are proud and privileged to serve so many exceptional nurses. We salute you, we celebrate you, and<br />
we honor you for all you do. Thank you for the work you do each and every day to make SJH/SJE/SJJ<br />
all outstanding organizations.<br />
SAINT JOSEPH-JESSAMINE<br />
With gratitude,<br />
LaJava Chenault, MSN, RN<br />
VP of Nursing<br />
Christine H. Mays, MSN, RN<br />
Chief Operating Officer/Chief Nursing Executive<br />
31
Transformational Leadership<br />
Nurses are responsible for providing high-quality patient care in a culture of safety and clinical quality performance. Transformational leaders help achieve this goal. Nursing’s mission,<br />
vision, values, philosophy and strategic plan provide the framework from which all components of the nursing division are developed. Interdisciplinary teams were created to<br />
develop a shared vision for the desired performance-driven culture, guided by the behavioral attributes of our core values.<br />
<strong>Saint</strong> <strong>Joseph</strong>’s model for nursing care is person-centered care. This professional practice model aligns with our current patient care provision and shared governance<br />
practice model, and allows the patient and family an opportunity to share in the care delivery decision-making process. Patients and families work with the nursing<br />
staff to direct the care provided to the patient by sharing knowledge and providing support, creating a partnership for care. This partnership makes the patient<br />
(and family) a stakeholder in the care, which allows a more competent, tailored plan of care to ensure healthier outcomes.<br />
Both the structure and philosophy of nursing at SJH/SJE/SJJ reinforce shared decision-making. Many new councils and teams have been established<br />
this year, along with existing councils, to help improve our practice. The roles of the councils include advocacy and influence, visibility, accessibility,<br />
communication and strategic planning. The councils focus on clinical practice, quality, professional development and education, research, management<br />
and operations, and patient satisfaction. This improvement is closely linked with the increase in autonomy, especially with the frontline nursing staff.<br />
Councils include:<br />
• Clinical Patient Safety Council<br />
• Heart Failure Leadership Council<br />
• Interdisciplinary Pain Council (IPC)<br />
• Nursing Quality Council<br />
• Peri-Operative Leadership Council<br />
• Pre-Op/Post-Op <strong>Care</strong> Excellence Council<br />
• Staff-led Hiring Council<br />
• Unit-Based Quality and Practice Council<br />
• Women’s <strong>Hospital</strong> Practice Council<br />
Integrated into our person-centered nursing model and shared governance practice setting is Jean Watson’s theory of caring. Watson holds a<br />
view of the human as a valued person in and of him- or herself, to be cared for, respected, nurtured, understood and assisted. Watson’s theory is<br />
consistent with our chosen person-centered model of care. Patient-centered care is defined as:<br />
• Respect for the individual patient<br />
• Coordination of care<br />
• Communication, information and education of care to include patient’s cultural and lifespan needs<br />
• Comfort (emotional, physical, spiritual)<br />
• Emotional support<br />
• Family involvement (to include unmarried significant others, support persons and life partners)<br />
• Transition and continuity of care<br />
Structural Empowerment<br />
ANNUAL EVIDENCE-BASED PRACTICE SPRING SEMINAR<br />
<strong>Saint</strong> <strong>Joseph</strong> Health System nurses were invited to the annual Evidence-Based Practice spring seminar, “Evidence for Transformational <strong>Care</strong>,” April 23, 2010, at SJH.<br />
Special guest speaker was Jim D’Alfonso, COO & CNO for the Watson Caring Science Institute. He spoke about the Caring Theory of Jean Watson.<br />
32
Nursing Facts:<br />
NUMBER OF NURSES<br />
RNs: 1,078<br />
LPNs: 57<br />
ARNPs: 13<br />
MSNs: 45<br />
UNLOCKING CLINICAL EXCELLENCE AND PUTTING PERFECTION INTO PRACTICE<br />
Phil Beauchene, senior director with the Advisory Board Company, was the speaker on June 24, 2010,<br />
at SJH and discussed the most important unit attributes driving clinical excellence, overall strategies<br />
for pursuing those drivers of clinical excellence, detailed best practices drawn from exceptional units<br />
around the country, and zero-defect initiatives custom-fitted to unique care settings. This educational<br />
offering was open to all SJHS nurses.<br />
HEART WALK 2010<br />
More than 500 employees from SJH/SJE/SJJ and family members participated in the American<br />
Heart Association Heart Walk on April 24, 2010, at Commonwealth Stadium, all sporting red <strong>Saint</strong><br />
<strong>Joseph</strong> Heart Institute T-shirts.<br />
AVERAGE YEARS OF SERVICE<br />
0-5 years:<br />
40%<br />
6+ years:<br />
60%<br />
RELAY FOR LIFE 2010<br />
The 6th floor oncology staff at SJH led a team in the Fayette County Relay for Life June 4-5, 2010,<br />
at Lexington Christian Academy. The team held various fundraisers, including bake sales and a quilt<br />
and basket raffle, and walked laps at the event to support the American Cancer Society.<br />
AVERAGE AGE OF NURSES<br />
TURNOVER<br />
RN:<br />
11.05%<br />
Voluntary RN:<br />
7.05%<br />
Vacancy:<br />
7.8%<br />
21-40 years:<br />
45%<br />
41+ years:<br />
55%<br />
GO RED FOR WOMEN<br />
<strong>Saint</strong> <strong>Joseph</strong> Health System is the central Kentucky sponsor<br />
of the American Heart Association’s Go Red for Women<br />
program, which alerts women to their risk of cardiovascular<br />
disease. In fiscal year 2010, <strong>Saint</strong> <strong>Joseph</strong> hosted several<br />
community events to help raise awareness and encourage<br />
women to take steps to reduce their risk for cardiovascular<br />
disease. Several <strong>Saint</strong> <strong>Joseph</strong> Heart Institute nurses<br />
volunteered at these events, providing free blood pressure<br />
screenings and heart-healthy information.<br />
SURGERY ON SUNDAY (SOS)<br />
Dr. Andy Moore was named a CNN Hero for his work with the Surgery on Sunday (SOS) program<br />
in Lexington. SOS utilizes volunteer surgeons, nurses and other medical and non-medical volunteers.<br />
<strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> nurses provide a large portion of the care. Sheryl Adams, a critical care float<br />
nurse at SJH, is one of the volunteers for Surgery on Sunday.<br />
“Primarily I serve as a recovery nurse,” Sheryl said. “We start at 6 or 7 a.m., and we usually end by 1<br />
or 2 p.m. It’s hard to give up your Sunday mornings, but it’s so rewarding.” For one thing, patients are<br />
extremely grateful for the care, the nurse said. “They realize that we’re giving up our time for them. It<br />
gives you such a good feeling to be able to help them. I come from a very poor family. That makes me<br />
want to give even more.”<br />
33
HELP FOR HAITI<br />
Julia Phillips (left) is a registered nurse at SJH. Julia served in Haiti, arriving only days after the devastating earthquake hit in January. She believes<br />
it was God’s calling. “I became a nurse so I could do this kind of work anywhere in the world,” she said.<br />
She worked in makeshift hospital wards, where secluded solace was broken with chaos. She worked with international teams to provide<br />
medical, surgical and humanitarian support. Her experience is filled with poignant stories of birth, death and determination for survival.<br />
Phillips continues to receive updates about the people she cared for and has since returned in August with another Emergency<br />
Department colleague, Jana Congleton, RN, at SJJ.<br />
COMMUNITY PARTNERSHIPS FOR FITNESS<br />
Emergency Department nurses and techs provided first-aid at the inaugural Bourbon Chase, a 200-mile relay of runners<br />
covering scenic byways along the famous Kentucky Bourbon Trail and Bluegrass horse country.<br />
COMMUNITY RESOURCE CENTER<br />
Janet Morgan, RN, CBPN-IC, <strong>Saint</strong> <strong>Joseph</strong> Breast Center, was presented with a Susan G. Komen grant for the<br />
development of a Community Resource Center. This center will include books, DVDs and other materials to<br />
address breast health and care of women with breast cancer. Janet has also developed and started a Breast Cancer<br />
Survivor support group that will meet on a monthly basis in the new Community Breast Resource Center.<br />
NURSES’ CHOICE AWARD 2009<br />
Every year, nurses at SJH and SJE nominate one physician from each campus for the Nurses’ Choice Award. In December<br />
2009, nurses honored Dr. Jorge Ang (above) and Dr. Bruce Belin (above, right).<br />
The Nurses’ Choice Award recognizes physicians who display the following traits every day in their work with nurses. The criteria for<br />
selection of the physician award winner are:<br />
34<br />
• Daily demonstrates the core values of Reverence, Integrity, Compassion and Excellence, as the leader of the health care team.<br />
• Supports nurses in a collegial manner by demonstrating respect and a true spirit of collaboration with nurses in the provision of care.<br />
• Serves as a coach and teacher, whether formally or informally, to promote the advancement of nursing knowledge and practice.
NATIONAL CERTIFICATIONS RECEIVED<br />
Tammy Andrews, SJH: CEN<br />
Anne Baumgartner, SJH: ARNP - Psychiatric Board Certification<br />
Jana Congleton, SJH: CEN<br />
Betty Cornish, SJH Heart Institute Non-Invasive Manager: CCRN<br />
Rosemary Dailey, SJH: SANE Certification<br />
Jennifer Daniel, SJH: CEN<br />
Donna Doty, SJE: ASBS<br />
Jeannie Elder, SJE: ANCC<br />
Michelle Fite, SJH Cardiac Cath Lab: RCIS<br />
Chrystal Hackney, SJE/SJH/SJJ: CEN<br />
Sherry Hearley, SJE: CPAN<br />
Lona Hensley, SJH: LNC<br />
Denise Hundley, SJE: RNC-OB<br />
Davonna Hutcherson, SJE: RNC-OB<br />
Margie Isaacs, SJH: LNC<br />
Sabrina Little, SJE Cardiac Cath Lab: CCRN<br />
Brenda Lloyd, SJH HISSU: CCRN<br />
Tiffany Lowther, SJE: CNOR<br />
Jodi Manley, Heart Institute Procedure Lab: CCRN<br />
Billie May, SJH: ACHPN<br />
Janet Morgan: CBPN-IC<br />
Carol O’Connell, SJE: RNC-OB<br />
Lisa Quinn, SJH: ARNP, Family Practice Board Certification<br />
Linda Rouser, SJE: CCM<br />
Danielle Thomas, SJE: CNOR<br />
ADVANCED DEGREES RECEIVED<br />
Anne Baumgartner: ARNP<br />
Amy Blank, SJE: BSN, Eastern Kentucky University<br />
Marissa Coleman, SJE: BSN, Morehead State University<br />
Bill Currey, SJE: BA General Study Field Allied Psychology, University of Kansas<br />
Susan Fields, SJE: BSN, Eastern Kentucky University<br />
Gretchen Folk, SJE: BSN, University of Kentucky<br />
Pam Graves, SJE: BSN<br />
Sheryl Hardyman, SJH: BSN, Eastern Kentucky University<br />
Kyle Howard, SJE: BSN, University of Kentucky<br />
Margaret Howard, SJH: BSN, University of Wisconsin<br />
Samantha Jackson, SJH: BSN, University of Kentucky<br />
Amber Keath, SJH: BSN, Eastern Kentucky University<br />
Tammy Lancaster, SJE: BSN, University of Kentucky<br />
Celina Milan, SJE: BSN<br />
Michelle Moss, SJE: BSN, Eastern Kentucky University<br />
Karla Mullins, SJE: BSN, University of Tennessee<br />
Victoria Nash, SJH: BSN, South University, GA<br />
Karissa Neidig, SJE: BSN, Eastern Kentucky University<br />
Tisha Newson, SJE: BSN, IWU<br />
Lisa Quinn: ARNP<br />
Felicia Reaves, SJE: BSN<br />
Karen Scott, SJE: BSN<br />
Yvonne Sherman, SJE: BSN, University of Kentucky<br />
Karen Taylor, SJE: BSN, Eastern Kentucky University<br />
Bettina Thomas, SJE: BSN, Eastern Kentucky University<br />
Lee Trimble, SJE: BSN, Midway College<br />
Ashley Witham, SJE: BSN, Eastern Kentucky University<br />
LEADERSHIP IN PROFESSIONAL ORGANIZATIONS<br />
LaJava Chenault, MSN, RN, SJH/SJE/SJJ, executive board member National FIIL Risk Group<br />
Debbie Griffith, SJH, education coordinator for Bluegrass Chapter AACN<br />
Margaret Kramer, BSN, RN, SJH, president of Central Kentucky Staff Development Group<br />
Tiffany Lowther, SJE, appointment to board for AORN<br />
Christine H. Mays, MSN, RN, SJH/SJE/SJJ, American Cancer Society Leadership Council, Palliative<br />
<strong>Care</strong> board of directors, Camp Horsin’ Around board of directors, UK External Advisory Council<br />
PROFESSIONAL PRESENTATIONS & POSTER PRESENTATIONS<br />
• “Aspetic Technique” Department Poster • Denise Hundley, SJE, AWHONN National<br />
Presentation, Stacy Jude, RN, SJH EP Lab Conference Poster Presentation: “Because<br />
• “Clinical Orientation Re-Design” Poster<br />
One Is Too Many”<br />
Presentation: Margaret Kramer, BSN, RN, • “From Novice to Expert: Mastering the<br />
SJH/SJE Heart Institute Clinical Educator Fundamentals of Staff Development,”<br />
• “The 6 Roles of the Staff Development<br />
October 16, 2009<br />
Specialist”; Margaret Kramer, BSN, RN, • Linda Amon, SJE, new presenter of Patient<br />
SJH/SJE Heart Institute Clinical Educator Education biweekly class for Total Joint<br />
• “Women’s Heart Health”; Tammy<br />
Replacement<br />
Dail, RN, SJH, HISSU Manager, Sullivan • Poster Presentation: “National Patient Safety<br />
University May 2010<br />
Goals” <strong>Hospital</strong> Safety Poster 2nd Place<br />
• Carol O’Connell, SJE, AWHONN National winner: Tammy Dail, RN, SJH HISSU<br />
Conference Poster Presentation: “Because Manager; Erin Caldwell, RN, SJH HISSU<br />
One Is Too Many”<br />
Clinical Manager; SJH HISSU Staff<br />
• CKSDG Region Staff Development Poster • Poster Presentation: “Time Out” <strong>Hospital</strong><br />
Palooza, April 2010<br />
Safety Poster: Denise Alvey, BSN, MSN, RN,<br />
• Debbie Gibbons, SJE, certification course for SJE HISSU; Margaret Kramer, BSN, RN,<br />
“Resolve Through Sharing” for nurses and SJH/SJE Heart Institute Clinical Educator<br />
chaplains<br />
• SJHS EBP Program, April 2010<br />
• Tommie Sears, SJE, EKU College of Nursing-<br />
TB<br />
35
CERTIFIED EMERGENCY NURSE EXAMINATION (CEN)<br />
SJJ was the host site for the first system-sponsored Certification Emergency Nurse review course in May. Dan Andrews, RN, CEN, became involved in the project in early 2010. This project was a collaboration<br />
of RNs to arrive at a unified education format for Emergency Departments. <strong>Saint</strong> <strong>Joseph</strong> Health System RNs with national specialty certification served as course instructors. The inaugural course netted a large<br />
response; six RNs have attained CEN certification. This distinctive symbol marks the passion of nurses providing superior patient care and protecting the public’s health and safety.<br />
CCRN REVIEW COURSE<br />
In order to promote and encourage certification for the critical care and telemetry nurses, a CCRN review course, “Certification Exam Cram: A 2-Day Review for CCRN and PCCN Candidates,” was offered in<br />
April 2010. This program is designed for nurses preparing to take on the challenge of either the CCRN or PCCN exam. The course highlights and reinforces exam-essential concepts and should be approached as<br />
the final culmination of one’s own self-study. For the system, we have added 7 CEN nurses as a result of this course review.<br />
STUDENT NURSE PRECEPTOR LIST 2009-2010<br />
Cristy Abrams<br />
Teresa Conley<br />
Jessica Adams<br />
Alicia Cox<br />
Mitzi Alexander<br />
Teressa Cozine<br />
Lola Arnett<br />
Miranda Craft<br />
Almira Bacus<br />
Danielle Craig<br />
Ashley Baesler<br />
Donna Cruze<br />
Cassie Baker<br />
Dianna Davis<br />
Anne Baumgartner Amanda Deskins<br />
Anna Bermundo<br />
Lynette DeTinne<br />
Nikki Bermundo<br />
Donna Doty<br />
Heather Black<br />
Amy Dugan<br />
Christine Bowling<br />
Courtney Elam<br />
Cristy Callahan<br />
Earl Farler<br />
Tiffany Calvert<br />
Amber Field<br />
Teri Chasteen<br />
Susan Fields<br />
Rebecca Chesnut<br />
Shawntal Garr<br />
Carrie Clark<br />
Angela Gibson<br />
Winona Clark<br />
Pam Gill<br />
Amy Claunch<br />
Robbie Gomez<br />
Ashley Clemmons<br />
Julia Greenup<br />
Jessica Collins<br />
Amanda Hamilton<br />
April Hamilton<br />
Judy Hamilton<br />
Gwen Hammons<br />
Andrew Hancock<br />
Amy Hatton<br />
Autumn Haynes<br />
Vada Hays<br />
Joy Hoverman<br />
Sheena Hudson<br />
Dwanett Jarrells<br />
Arlene Jones<br />
Denise Jordan<br />
Mary Beth Keeton<br />
Jodi Kellman<br />
Lynette Laine<br />
Beth Leonard<br />
Pam Long<br />
Danielle Mann<br />
Donna Mann<br />
Terry May<br />
Suzanne McGill<br />
Connie Melson<br />
Shannon Melton<br />
Diane Miller<br />
Melissa Miller<br />
Cindy Napier<br />
Stephanie Niece<br />
Alesha Pennington<br />
Jodi Pernica<br />
Sherry Powell<br />
Jennie Proctor<br />
Stacey Puckett<br />
Mary Frances Regalado<br />
Jennifer Romans<br />
Kellie Rosenbalm<br />
Rubi Russell<br />
Clarissa Scott<br />
Rachel Scott<br />
Sherri Shelby<br />
Amelia Shrick<br />
Phyllis Shrout<br />
Sherry Simmons<br />
Jasmine Sims<br />
Beverly Smith<br />
Cindy Smith<br />
Glenn Standafer<br />
Beth Stearns<br />
Stacy Stephenson<br />
Debbie Stiles<br />
Amber Tarpley<br />
Kari Terando<br />
Rayna Thomas<br />
Heather Wallace<br />
Trish Wallace<br />
Kathleen Warner<br />
Anissa Webb<br />
Whitney Webb<br />
Therese Weinberg<br />
Debby Whitaker<br />
Amanda Wilson<br />
Vicky Wright<br />
Bev Young<br />
CONTINUING EDUCATION<br />
A total of 230 continuing education programs were offered in FY10 for nursing continuing education credit. A grand total of 1,467 nurses attended a free CE<br />
educational program during the year and a total of 961 continuing education credits were provided.<br />
36
Awards and Recognitions<br />
HEART OF SAINT JOSEPH WINNERS (NURSING)<br />
SJE: Rachel Scott<br />
SJE: Sam Griggs (deceased)<br />
2010 DAISY AWARD RECIPIENTS<br />
It is so easy to find extraordinary nurses at <strong>Saint</strong> <strong>Joseph</strong> Health System—professional nurses who exhibit extraordinary compassion in the care of their<br />
patients and families. Nominations for the DAISY Award are written by fellow RNs, patients, family members, physicians and staff. They take the time<br />
to nominate nurses because they have been, in some way, impacted by what the nurses do and who they are. Our deepest thanks to Barry Stumbo and the<br />
<strong>Saint</strong> <strong>Joseph</strong> Foundation for making this a reality for all of us!<br />
1ST<br />
QTR.<br />
Carrie Clark, RN,<br />
ICU South, SJH<br />
Angie Henley, RN,<br />
4MS, SJE<br />
Kristi McVey, RN,<br />
2 East, SJH<br />
Alesha Pennington, RN,<br />
L&D, SJE<br />
Sherri Shelby, RN,<br />
CCH, SJE<br />
Kari Terando, RN,<br />
2 East, SJH<br />
2ND<br />
QTR.<br />
Becky Alexander, RN,<br />
Cath Lab, SJH<br />
Denise Alvey, RN,<br />
HISSU, SJE<br />
Betty Evans, RN,<br />
CCH, SJH<br />
Mia Howard, RN,<br />
Women’s <strong>Care</strong>, SJE<br />
Latonya Jones, RN, 3B,<br />
SJH<br />
3RD<br />
QTR.<br />
Kathy Davis, RN,<br />
PACU, SJH<br />
Robin Payton Harrod, RN,<br />
Women’s <strong>Hospital</strong>, SJE<br />
Michele Lafave, RN,<br />
Surgery, SJH<br />
Sherri Shelby, RN,<br />
CCH, SJE<br />
Vicky Wright, RN,<br />
3 East, SJH<br />
4TH<br />
QTR.<br />
Judy Beauvier, RN,<br />
Pain Management, SJH<br />
Melissa Doss, RN,<br />
Med/Surg, SJE<br />
Mary Beth Keeton, RN,<br />
Med/Surg, SJE<br />
Ernest Morris, RN,<br />
CCH, SJH<br />
Jenny Pulliam, RN,<br />
3rd Telemetry, SJE<br />
37
NURSING EXCELLENCE AWARD<br />
Kimberley Adams, SJE Charge Nurse, Day Surgery & Block Room<br />
Carrie Barnett, SJH Staff RN<br />
Venus Bigham, SJH <strong>Care</strong> Coordinator Case Management<br />
Traci Brady, SJE Critical <strong>Care</strong> Float<br />
Charissa Burt, SJH Cardiothoracic Vascular Unit<br />
Danielle Craig, SJHS RN 2 East<br />
Melanie Donnelly, SJH Clinical Manager RN-PRNU<br />
Betty Evans, CCH/SJH Staff Nurse<br />
Earl Farler, SJH RN 3 ICU<br />
Stephanie Garcia, SJH 5A Stroke/Telemetry<br />
Miranda Gibson, SJH Clinical Manager 4A<br />
Karen Greer, SJH HISSU Staff Nurse<br />
Penny Grimes, SJE RN Endoscopy<br />
Tina Hale, SJE 7A ED Charge RN<br />
Sheryl Hardyman, SJH RN Endoscopy<br />
Miranda Hill, SJH ED Nurse<br />
Tricia Kellenbarger, SJHS RN Electrophysiology Labs<br />
Margaret Kramer, SJH & SJE Heart Institute Clinical Educator<br />
Beth Leonard, SJH RN ICU North<br />
Allison Manning, CCH - SJE Clinical Manager<br />
Sharon McCartt, SJH Clinical Documentation Specialist<br />
Celina Milan, SJE RN Surgery<br />
Lauren Mullins, SJE RN 3 Telemetry<br />
Erica Pantaliono, SJH RN Case Mgr, Charge Nurse Wound Center<br />
Shari Pearson, SJHS Staff Nurse Pre-Op & Holding<br />
Mary Ann Powers, SJH ICU South<br />
Stacey Puckett, SJJ ED Staff Nurse<br />
Tasia Rader, SJE RN 4 Medical Surgical Unit<br />
Elizabeth A. Soileau, SJH RN, Clinical I 3A Post-Op Surgery<br />
Amy Wallace, SJE Staff RN HISSU<br />
Kathleen Warner, SJH RN 3B Surgical Telemetry<br />
Shannon Woosley, SJH RN Cardiac Cath Lab<br />
Shannon Young, SJH Staff Nurse Heart Institute<br />
SPIRIT OF SAINT JOSEPH SERVANT LEADERSHIP EXCELLENCE AWARD<br />
During the summer of 2010, <strong>Saint</strong> <strong>Joseph</strong> Health System created the Spirit of<br />
<strong>Saint</strong> <strong>Joseph</strong> Servant Leadership Award. The award is to be presented to a leader<br />
who consistently demonstrates our mission and core values, and the Seven<br />
Pillars of Servant Leadership. The seven key practices of servant leaders are selfawareness,<br />
listening, changing the pyramid, developing your colleagues, coaching<br />
not controlling, unleashing the energy and intelligence of others, and foresight.<br />
Nurse nominations from SJH/SJE/SJJ include:<br />
• Debbie Bryant, Director of Nursing, <strong>Saint</strong> <strong>Joseph</strong> East<br />
• Claudia Carroll, Human Resources Senior Business Partner<br />
• Patti Creed, Unit Manager of Emergency Services, <strong>Saint</strong> <strong>Joseph</strong> East<br />
• Pat Jessen, Unit Manager for 4A General Medical Unit, <strong>Saint</strong> <strong>Joseph</strong><br />
<strong>Hospital</strong><br />
• Marilyn Swinford, Director of Emergency Services, SJH/SJJ and Patient<br />
Access<br />
• Linda Watt, Director of Surgical Services, <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong><br />
CONTRIBUTION TO NURSING PROFESSION<br />
Chris Mays, MSN, RN, COO/CNE, is one of 50 UK College of Nursing<br />
graduates being honored for her contributions to the nursing profession 2010.<br />
38
Exemplary Professional Practice<br />
MATERNITY SERVICE INITIATIVE<br />
The Maternity Service staff developed the following aim statement: to improve and enhance the safety of our perinatal population. In this<br />
effort the team discussed, educated and implemented the H1N1 flu vaccination requirement for all pregnant women who presented to<br />
L&D and were discharged from the hospital prior to or after delivery.<br />
The Maternity Staff developed and implemented an Evidence-Based Educational Competency Week on each unit to address<br />
the educational needs of the staff. They used the LEAN process to identify the high-risk, high-volume care processes used on a<br />
routine basis and developed educational tools for the competency training.<br />
PATIENT SATISFACTION<br />
<strong>Saint</strong> <strong>Joseph</strong> Health System partners with HealthStream to measure and monitor its patient satisfaction. HealthStream<br />
Research conducts patient satisfaction surveys for hundreds of hospitals in the U.S. and has a database of more than a<br />
million patient experiences. In FY10, <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong>, <strong>Saint</strong> <strong>Joseph</strong> East and <strong>Saint</strong> <strong>Joseph</strong> - Jessamine ranked<br />
high compared to other hospitals within the HealthStream national database. <strong>Saint</strong> <strong>Joseph</strong> - Jessamine ranked in<br />
the 94th percentile, <strong>Saint</strong> <strong>Joseph</strong> East ranked in the 86th percentile and <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> ranked in the 84th<br />
percentile. The goal is for all SJHS facilities, individually and as a whole, to reach the 90th percentile by 2015;<br />
<strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong>, <strong>Saint</strong> <strong>Joseph</strong> East and <strong>Saint</strong> <strong>Joseph</strong> - Jessamine are well on their way to reaching this target.<br />
These national percentiles correlate with the “Top Box” percentages outlined in the graphs below. Top Box<br />
percentages represent the percent of patients who rated the hospital a 9 or 10 (on a 10-point scale) in the overall<br />
rating of the hospital survey question (“Overall Rating of the <strong>Hospital</strong>”). In FY10, <strong>Saint</strong> <strong>Joseph</strong> East received<br />
an 81.9% Top Box rating, <strong>Saint</strong> <strong>Joseph</strong> - Jessamine received an 80.7% Top Box rating and <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong><br />
received an 80.2% Top Box rating.<br />
Also noteworthy, <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> is the only hospital in Lexington to receive HealthGrades’ Outstanding<br />
Patient Experience Award for 2010. The award from HealthGrades, the nation’s leading independent health<br />
care ratings organization, is based on an analysis of the federal government’s <strong>Hospital</strong> Consumer Assessment<br />
of Healthcare Providers and Systems survey, also known as the CAHPS® <strong>Hospital</strong> Survey, or HCAHPS. The<br />
recognition identifies those hospitals performing in the top 15 percent in the nation in patient satisfaction.<br />
39
CARE COORDINATION NEW MODEL<br />
In the new <strong>Care</strong> Coordination model, the RN <strong>Care</strong> Coordinators and social workers support an environment of healing grounded in our core values of reverence, integrity, compassion<br />
and excellence. The <strong>Care</strong> Coordinators’ role has transformed by focusing on excellence in order to provide the patient with a smooth transition to the next level of care. This excellence<br />
and transition is accomplished through the coordination and collaboration among the health care team, the patient and the patient’s family.<br />
SJHS HOSPITALS INTRODUCE KENTUCKY’S FIRST “NO WAIT” EMERGENCY ROOMS<br />
In June 2010 “No Wait ERs” were implemented at <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong>, <strong>Saint</strong> <strong>Joseph</strong> East and <strong>Saint</strong> <strong>Joseph</strong> - Jessamine. With the new process, emergency care begins<br />
within five minutes of a patient’s arrival time. A patient is seen by a nurse within five minutes of arrival; the patient is quickly seen by an ER nurse who is authorized<br />
to begin the treatment needed; and a doctor examines the patient within 30 minutes.<br />
After only four short months, the “care begins in 5 minutes” metric is being met 65% of the time, with an average of four minutes for SJH, four minutes for<br />
SJJ and eight minutes for SJE. “See a provider within 30 minutes” is being met 60% of the time with an average of 35 minutes for SJH, 22 minutes for SJJ<br />
and 35 minutes for SJE. Our slogan “Be Safe, Be Nice, Be Quick” has resulted in high patient satisfaction and increased ED volumes at 12% from the<br />
previous year for SJH/SJE/SJJ Emergency Departments.<br />
eCLINICAL REFERENCE SOLUTIONS<br />
In March 2010, Tracey McFarland, clinical educator, worked with national CHI teams to help launch eClinical Reference Solutions, a collection<br />
of three evidence-based references for nursing. Nurses can access an index of more than 900 skills, each with quick checklists, detailed step-bystep<br />
instructions (including rationales and reference links), illustrations and many with video clips for reviewing a procedure. Mosby’s Nursing<br />
Index is a journal abstract and indexing database; the index is a tool our nurses can access to perform comprehensive and systematic searches.<br />
EVIDENCE-BASED PRACTICE (EBP) INITIATIVES<br />
The following EBPs have been implemented:<br />
• Acute <strong>Care</strong> Fall Prevention<br />
• Catheter Associated Urinary Tract Infection Prevention<br />
• Central Line Associated Bloodstream Infection Prevention<br />
• Health <strong>Care</strong> Associated Infection Prevention<br />
• Heart Failure Discharge Instructions,<br />
reduce 30-day readmission<br />
• Pain Management<br />
• Pressure Ulcer Prevention<br />
• Safe Patient Handling and Movement<br />
• Surgical Never Events, WHO checklist<br />
• Venous Thromboembolism Prevention<br />
STAFF HIRING<br />
In May 2009, as part of shared governance, several nursing units formed staff-led hiring committees to independently interview and select<br />
qualified applicants for positions within the department. A committee chair and committee members volunteer to participate. The goals are to<br />
decrease turnover, increase staff satisfaction, provide an avenue for professional growth, and allow staff to become personally invested in new hires.<br />
One nurse was quoted as saying, “It feels really good to know that my opinion especially as a new nurse is so valued where I work.” One potential<br />
candidate stated, “I really love how staff nurses are so involved in your unit and I would love to be a part of that.”<br />
PRNU STAFF-LED HIRING COMMITTEE<br />
The Prep-Recovery Nursing Unit (PRNU) has 10 staff members. The attributes necessary to contribute to a great hire are determined by the team who use<br />
questions from the behavioral-based interview guide. In 2009, four staff members participated in the interview process of three candidates. Retention: there has<br />
been zero turnover year-to-date. Staff satisfaction rating in the January 2010 mini-climate assessment increased from 3.38 to 3.82 using a 1-5 scale.<br />
40
CARE BY PARENT<br />
One of the design plans for the Neonatal Intensive <strong>Care</strong> Unit (NICU) nursery included an area for parents of infants to stay and learn how to care for their infant as well as become<br />
comfortable in caring for their fragile infant prior to discharge. The new Women’s <strong>Hospital</strong> at SJE had the NICU on a different floor than the post-partum unit, so plans had to be<br />
made to incorporate an area in the NICU for <strong>Care</strong> by Parent.<br />
The <strong>Care</strong> by Parent rooms fit the needs perfectly. In looking at the space of the NICU, there was an area at the entry to the NICU, an ideal space for <strong>Care</strong> by Parent<br />
rooms located outside the doors of the NICU. Moms can socialize with other parents or take a nap, or sleep overnight on one of the sofa beds. The interaction with<br />
other families helps new parents gain confidence in the care of their infant and understand the processes in the NICU.<br />
OBSTETRICS DISCHARGE COORDINATOR<br />
The Women’s <strong>Hospital</strong> at SJE implemented a new discharge process in September 2009. The process incorporates two designated discharge coordinators,<br />
resulting in improved overall patient satisfaction, as well as increased employee satisfaction. The overall patient satisfaction scores in the Women’s<br />
Department were below the target of 71%. One of the primary dissatisfiers was inconsistency in discharge teaching. Adult learning methods were<br />
implemented to the family’s level of understanding, resulting in an individualized discharge process. The patient satisfaction scores improved in the<br />
first quarter to well over 80%.<br />
SURGICAL SERVICES HAND-OFF-OF-CARE TOOL<br />
Our Surgical Services educator developed a tool for our “hand-off-of-care” between Pre-Op, OR and PACU/Post-Op. The intent of the<br />
tool is to make certain our processes ensure patient safety. Staff was educated on the tool and process. Auditing was completed to determine<br />
compliance and weak areas were identified.<br />
In March 2010 we educated and implemented the recommended OR work practices for preventing sharp injuries and exposures: double<br />
gloving; blunt tip suture needles; sterile field neutral zone and safety scalpels, based on recommendations from the American College of<br />
Surgeons.<br />
41
Empirical Quality Outcomes<br />
On January 1, 2010, Surgical Services went live with reporting on our compliance by using the World Health Organization’s (WHO) Surgical<br />
Safety Checklist. The impetus of the checklist is to ensure we are performing the right surgery, right orientation (right or left when indicated),<br />
right patient, and that we have all items needed. We have also included some core measure items to the checklist. The checklist includes all<br />
members of the surgical team. Currently, we are consistently at 100% compliance with using the checklist.<br />
HEART FAILURE LEADERSHIP COMMITTEE<br />
Toni Gray, MSN, RN, RRT, joined SJH in January 2010 as our Heart and Vascular Institute Program Coordinator. Toni quickly<br />
assembled a team to work on heart failure (HF) management. The decision to focus a strategic alignment with the caregivers<br />
of heart failure patients and to ultimately become a certified heart failure center is the focus of the heart failure committee to<br />
better provide continuity of care.<br />
CLINICAL PATIENT SAFETY COMMITTEE<br />
Concurrent quality score and improvement plans are developed and presented to the members of the Clinical Patient<br />
Safety Committee at regularly scheduled monthly meetings. Core quality measures are reviewed with observations<br />
and actions. Focus group updates reflect the activity toward a site-based initiative. An example of a focus group<br />
update related to Rapid Response Team (RRT) was presented at the May Clinical Safety Committee by Dr. Barbara<br />
Reynolds, Chairman.<br />
Observation: the RRT focus group noticed decreased utilization of the RRT. Education in February 2010 on<br />
activation criteria and visibility of the RRT resulted in an increased utilization in March 2010. Action: The RRT<br />
committee is focused on improvement methods for deceased codes and review of the code process in its entirety.<br />
The RRT committee has also recognized the need to review resuscitation response related to compliance with<br />
advance cardiac life support guidelines. The RRT committee will coordinate physician education in the fall of<br />
2010 to adopt new American Heart advanced life support guidelines.<br />
<strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong><br />
<strong>Saint</strong> <strong>Joseph</strong> East<br />
RRT calls/1000 discharges<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Jul-09<br />
Aug-<br />
09<br />
Sep-<br />
09<br />
Oct-<br />
09<br />
Nov-<br />
09<br />
Dec-<br />
09<br />
Jan-<br />
10<br />
Feb-<br />
10<br />
Mar-<br />
10<br />
Apr-<br />
10<br />
May-<br />
10<br />
Jun-<br />
10<br />
RRT calls/1000 discharges<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Jul-09<br />
Aug-<br />
09<br />
Sep-<br />
09<br />
Oct-<br />
09<br />
Nov-<br />
09<br />
Dec-<br />
09<br />
Jan-<br />
10<br />
Feb-<br />
10<br />
Mar-<br />
10<br />
Apr-<br />
10<br />
May-<br />
10<br />
Jun-<br />
10<br />
RRT calls per 1000 discharges<br />
RRT calls per 1000 discharges<br />
NURSING QUALITY COMMITTEE<br />
The <strong>Saint</strong> <strong>Joseph</strong> Nursing Quality mission is to promote improvement in patient outcomes by engaging unit level staff.<br />
Nurses caring for patients at the point of care are in an excellent position to influence outcomes. The primary goal is the<br />
ongoing assessment and improvement of the delivery, quality and outcome of patient care. The scope and responsibility of<br />
the committee is to focus on clinical quality practices at the bedside to improve overall patient outcomes.<br />
42
THE CLOCK IS TICKING: MINUTES MATTER<br />
In an effort to continue to decrease the door-to-inflation times for the STEMI patient, it was suggested to look at the how the RRT could assist with these patients, since every minute matters. An<br />
interdepartmental bi-campus team from CCU, ICU, Cath Lab and ED met to discuss the potential collaboration. The process took six months and the outcomes continue to improve.<br />
• May: Team meeting and scope outlined; training and implementation plan developed.<br />
• June: Bi-campus RRT education offering with 98% attendance.<br />
Door-to-inflation times continue to meet and exceed the core measure target of under 90 minutes.<br />
Current Data: average door-to-balloon time is 68 minutes SJH, 56 minutes SJE; moving toward the goal of under 60 minutes.<br />
A few facts that encouraged us to strive to do better:<br />
• Each 30-minute delay in reperfusion with PCI increases one-year mortality 7.5%<br />
• Door-to-balloon under 60 minutes, 1% 30-day mortality; door-to-balloon under 90 minutes, 6.4% mortality<br />
DeLuca, Circulation 2004;109:1223-1225<br />
Berger, Circulation 1999;100:14-20<br />
• July/August: RRT orientation to ED and Cath Lab, SJH.<br />
• September/October: RRT orientation to ED and Cath Lab, SJE.<br />
New Knowledge Innovations and Improvements<br />
With a passion for patient- and family-centered care and a desire to impact quality outcomes and patient satisfaction scores, Lesly Arrasmith, 3A unit manager, implemented bedside shift report. Lesly describes<br />
the implementation process of bedside shift reporting on 3A:<br />
It was through the Med/Surg Reinvention team that I became more aware of bedside reporting. A unit at our sister hospital in London had begun this process. The manager had noted with<br />
an 80% compliance rate of bedside reporting that patient satisfaction had been dramatically impacted. At this time, as manager of 3A Post-Op Surgery, I was unable to impact my patient<br />
satisfaction scores to take a positive turn. I knew it was time to try something different.<br />
In March of 2010, I pulled in key staff members and clinical managers to talk of this new concept I had learned about. These were all staff with a high level of initiative. It was decided we<br />
would begin with a small cycle of change. This team was educated on asking permission to include any family/significant others present in the room in the report, introducing the oncoming<br />
nurse, what the bedside report should include in report (SBAR) format, and encouraging the patient to involve themselves in the report. A closing positive comment and introduction of the<br />
oncoming shift is always to be included. One nurse began this report on one patient at the bedside. This went well.<br />
During this report it was discovered by the patient, overhearing the allergies we had listed, that we had the allergies incorrect. What a great catch this was! This wonderful rumor spread<br />
like wildfire. Most staff was eager to be able to begin as well. The next day this same nurse got a report on her entire team at the bedside. This, too, went very smoothly. She would discuss<br />
her perceptions with the rest of the team. Such perceptions as “This will put me behind and patients will not like getting woken by report” were quickly dismissed. Because this had gone so<br />
positively and because staff was so enthusiastic about the beginning, as manager I decided we would use a “pay it forward” concept to spread this process.<br />
This “pay it forward” practice meant once a nurse received report at the beside she would educate the next shift nurse getting report on the process and then give report at the bedside as<br />
assigned. This nurse would in turn do the same thing. Within two weeks my entire unit was getting and receiving report at the bedside. During manager rounds at this time, I sought feedback<br />
about our new process. Patients and families loved that we truly were partnering with them. Patient satisfaction scores went from 59% to 71% for this quarter. This process is continued on 3A.<br />
Other units in our facility are beginning this new process at this time.<br />
— Lesly Arrasmith, Unit Manager 3A, <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong><br />
43
CLINICAL COVENANT “TEAM LEO” PROJECT, ICU SOUTH<br />
Nurses in the ICU unit at SJH, in collaboration with patient care leaders at SJH, met to discuss the current practices in the critical care areas of the hospital. A clinical covenant, Team<br />
Leo, was conceived for a process-improvement project in the spring of 2010. ICU South, a 10-bed medical/surgical critical care unit, was selected as the unit to study because of<br />
the varied patient population and the tenure of the nursing staff. The core committee team members were thus established, which include staff members from nursing and<br />
leadership of ICU South; quality improvement; pharmacy; dietary; housekeeping; respiratory therapy; case management; education; administration; Critical <strong>Care</strong><br />
Advanced Registered Nurse Practitioners; and physicians.<br />
An aim statement was established: “We aim to redesign existing processes and services, eliminate clinical waste and implement highly reliable, transparent,<br />
critical care level, person-centered care using Evidence-Based Practices. The process begins with the planned transfer or admission of the patient to the unit<br />
and ends with the patient’s discharge, transfer to another level of care or alternative care environment.”<br />
RESEARCH USE IN PRACTICE GROUP/LEVEL OF NURSE<br />
Bundles (IHI)<br />
Ventilator-Associated Pneumonia<br />
Central-Line Blood Stream Infections<br />
Perinatal<br />
All bundles implemented in practice areas<br />
affected<br />
Each initiative has an interdisciplinary<br />
team that consists of all levels of<br />
nurses<br />
Intensive Insulin Therapy Post-operative open heart patients Cardiothoracic vascular unit<br />
All levels of nurses<br />
Pain<br />
Pain education series and unit champions.<br />
Research-based pain scale utilized on nursing<br />
flow sheets<br />
Pain team consisting of all levels of nurses<br />
STEMI Program Door to discharge—all units affected STEMI team consisting of all levels of<br />
nurses<br />
Hypothermia Protocol Cardiac arrest patients arriving at the ED Hypothermia team consisting of all levels<br />
of nurses<br />
Pressure Ulcer Reduction All inpatient units Skin <strong>Care</strong> team consisting of all levels of<br />
nurses<br />
CMS Core Measures<br />
AMI<br />
HF<br />
Pneumonia<br />
SCIP<br />
Implemented in practice areas affected<br />
Each initiative has an interdisciplinary<br />
team consisting of all levels of nurses<br />
44
EVIDENCE-BASED PRACTICE (EBP)<br />
A subcommittee of the SJH nursing evidence-based committee focused on cognition and the geriatric patient. The team, comprising Debbie Kitchen, MSN, RN, CNS, and<br />
critical care staff nurses, focused on the critical care patient experiencing delirium. When a patient has delirium it means the patient cannot think clearly, has trouble<br />
paying attention and is not aware of what is going on around him/her. Causes are multifactorial; to name a few: systemic illness, polypharmacy, sleep deprivation<br />
and pain.<br />
Prevalence and incidents of developing delirium: 20-30% of all acutely hospitalized patients develop delirium; up to 60% go unrecognized; 50-80%<br />
of ventilated patients develop delirium; 20-50% of lower severity ICU patients develop delirium; and 10% remain delirious at hospital discharge.<br />
Consequences include: increased hospital length of stay, increased ICU length of stay, increased ventilator time, increased cost, increased longterm<br />
cognitive impairment, increased post-hospitalization institutionalization, and increased morbidity and mortality.<br />
The most important step in delirium management is early recognition. If delirium is not diagnosed, it is doubtful that any efforts will be<br />
made to reverse it. Once delirium is detected, efforts should focus on identifying the etiologies and correcting them. In January 2010<br />
education surrounding delirium and on performing the CAM (Confusion Assessment Method) ICU assessment tool began. The first<br />
outcome to be measured at SJH and SJE by the critical care nursing staff was if education improved nursing knowledge of delirium and<br />
use of CAM. The ICU nurses completed the delirium pre-test/post-test to compare the nurses’ baseline educational understanding of<br />
delirium prior to the in-service with knowledge gained after the in-service.<br />
Practicing the CAM-ICU tool during the in-service permitted the nurses to ask relevant questions about the tool and provided nurses<br />
with instant use of the new skills learned in the class. Overall, the educational in-service was beneficial for all ICU nurses no<br />
matter how many years of experience the nurses had within the ICU. The difference in pre-test scores between those with less than<br />
three years’ ICU experience and those with more than 10 years’ ICU experience was significant (p
46<br />
INTERDISCIPLINARY RELATIONSHIPS<br />
The Heart Failure Leadership Team for the <strong>Saint</strong> <strong>Joseph</strong> Heart Institute at <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> and<br />
<strong>Saint</strong> <strong>Joseph</strong> East formed in January 2010 to develop a program to ensure the highest quality of heart<br />
failure care to all patients. The team has developed Heart Failure Admission and Discharge orders,<br />
which incorporate Evidence-Based Practice and guidelines from AHA/ACC. The HF team is also<br />
pursuing heart failure certification by TJC and AHA “Get With the Guidelines.”<br />
RAPID RESPONSE TEAM<br />
The Rapid Response Team (RRT) consists of a critical care nurse, a respiratory therapist, a clinical<br />
pharmacist and the house administrator. The team continues to address the impact on patient care and<br />
has made changes in the RRT Standing Orders to include certain labs, EKG and IV documentation. The<br />
team also revised the lab value “triggers” for which the team members receive a page. The next step is to<br />
focus on monitoring and tracking data to identify any areas of weakness and celebrate areas of success.<br />
COLLABORATION WITH UNIVERSITY OF KENTUCKY COLLEGE OF NURSING (UKCON)<br />
Debbie Griffith, MN, CNS, collaborated with UKCON DNP candidate on a study being conducted<br />
to include SJH and SJE heart failure patients. The title of the study was “Testing a Brief Cognitive<br />
Therapy Intervention for Depressive Symptoms in Patients with Heart Failure.” The objectives of the<br />
study were:<br />
1) Participants will describe the impact of depression on morbidity/mortality in patients with<br />
heart failure. 2) Participants will be able to list two techniques taught in a brief cognitive therapy<br />
intervention (thought-stopping and affirmations). 3) Participants will describe whether or not a brief<br />
cognitive therapy intervention improves outcomes in patients with heart failure who have depressive<br />
symptoms. The results of the study, presented at the local Bluegrass Chapter of AACN, showed that<br />
the intervention patients had fewer cardiac events. Since the study has received funding to extend the<br />
dissertation study, the collaboration with UKCON will continue this fall.<br />
INTERNAL COLLABORATION<br />
2 East continues to define its role in the care of the heart failure patient and become recognized as the<br />
“Heart Failure” unit at SJH. Active ongoing collaboration is multidisciplinary, focusing on tailoring<br />
care to meet not only core measure requirements, but also the American Heart Association’s “Get With<br />
the Guidelines” recommendations.<br />
RESEARCH<br />
Celestine Trudy Gochett, Ph.D. (c), AOCNS, CCRP, received a J. Patrick Barnes Grant through the<br />
DAISY Foundation to conduct the Side Effect Index Efficacy study.<br />
Study title: The Cancer Treatment Side Effect Index: A Pilot Study of Efficacy<br />
Study status: IRB approval, funded by the J. Patrick Barnes Grant through the DAISY Foundation.<br />
Principal investigator names: Celestine Gochett, ARNP, AOCNS, CCRP;<br />
Judy Schreiber, Ph.D., RN<br />
Principal investigator credentials: Celestine Gochett, Ph.D. (c), AOCNS, CCRP<br />
Role of nurses: Assist with evaluation of the index content validity by determining<br />
patient report of the presence of 13 listed formative indicators.<br />
Study scope: Internal to a single organization.<br />
Study type: Original research; mixed method cross sectional design.
Honoring Our Daisies<br />
Congratulations to the FY10 recipients of the DAISY Award for Extraordinary<br />
Nurses throughout <strong>Saint</strong> <strong>Joseph</strong> Health System. Pictured are several recipients who<br />
attended an appreciation dinner September 7, 2010, along with nursing leaders,<br />
members of the executive team and CEO Gene Woods (front, center).<br />
47
SAINT JOSEPH - BEREA<br />
SAINT JOSEPH EAST<br />
FLAGET MEMORIAL HOSPITAL<br />
SAINT JOSEPH - MOUNT STERLING<br />
48<br />
“Thanks to all of you for the great<br />
care and kindness for my wife<br />
when we had a big car accident.<br />
The doctor, the nurses and the staff<br />
all gave their great professional<br />
effort to help her and gave us a<br />
lot of assistance and comfort. I<br />
will not forget how you did this<br />
wonderful work for us and it<br />
will always be in my testimony to<br />
others as an encouragement.”<br />
–an out-of-state Emergency<br />
Department patient<br />
“This letter is in regard to the care<br />
our mother-in-law received during<br />
her recent stay. She has been in<br />
and out of several hospitals. I have<br />
never seen a more caring, loving,<br />
kind and considerate staff. Even<br />
though she can be difficult at times,<br />
they always attended to her needs<br />
with compassion and a smile.”<br />
–a patient’s family member<br />
“During my stay, I was blessed<br />
with two of the best nurses I<br />
have ever encountered in my life,<br />
Jenny Pulliam and Melissa Doss.<br />
They explained everything clearly,<br />
researched medications and<br />
procedures, advocated to doctors<br />
on my behalf, organized labs,<br />
dressing changes and medication<br />
regiments in order to allow me<br />
to sleep as well as having the best<br />
attitudes I’ve ever witnessed in a<br />
hospital setting.”<br />
–a Med/Surg patient<br />
“My mother was at <strong>Saint</strong> <strong>Joseph</strong><br />
East recently for surgery. Following<br />
her procedure she was faced with<br />
some unexpected complications.<br />
She experienced a lot of<br />
uncontrollable pain. Mary Beth<br />
[Keeton] was my mother’s ‘light.’<br />
She was able to keep my mom calm<br />
and help her work through the<br />
pain.” –a Med/Surg patient<br />
“If you have to have a surgery,<br />
this would be the place to go...<br />
I knew that I was in competent<br />
hands. Michelle Osborne,<br />
Christy [Horton], nurses and<br />
aides both were hands-on with<br />
my care. I am much appreciative<br />
of a night nurse named Teri<br />
[Whitehouse], who I believe<br />
saved my life. The relationship<br />
with the entire staff was very<br />
meaningful and gratifying to us.”<br />
–a Surgery patient<br />
“I am writing to compliment<br />
you and your staff on the care I<br />
received while a patient on your<br />
skilled nursing unit. Your staff<br />
anticipated my needs, were always<br />
pleasant and cheerful, unlike the<br />
care I received in other hospitals.<br />
I will recommend Flaget to<br />
anyone at any time.”<br />
–an RN of 40 years, concerning her<br />
first experience as a patient at Flaget<br />
“I have traveled extensively in<br />
the U.S. and Europe and due to<br />
asthma have had many ER visits.<br />
<strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling’s<br />
ER personnel were the most<br />
conscientious, courteous and<br />
thorough of any place I’ve been<br />
for treatment. Kim Henson, Kim<br />
Hamilton, Dr. Forrester, Esther<br />
[Bloom] and Edwinna [Grayson-<br />
Melton] are the best.”<br />
–an Emergency Department patient<br />
“I would, and do, highly<br />
recommend the hospital. You<br />
could tell the concern, caring and<br />
patience from the nurses. You<br />
should be very proud of them,<br />
especially Phyllis Martin, Nathena<br />
Keeton, Teresa Tufano and Robert<br />
Bashford. Their care, personality,<br />
smiles and bedside manners should<br />
be recognized.”<br />
–a Med/Surg patient
SAINT JOSEPH HOSPITAL<br />
SAINT JOSEPH - LONDON<br />
SAINT JOSEPH - MARTIN<br />
SAINT JOSEPH - JESSAMINE<br />
“We would like to express our<br />
sincere appreciation to each person<br />
who attended to the needs of our<br />
mother. Everyone was very helpful,<br />
knowledgeable and caring in all<br />
aspects of meeting the needs of the<br />
patient and/or family. We praise<br />
your dedication and resolve in the<br />
performance of your many and<br />
varied duties.”<br />
–a 4A Medical patient<br />
“Ms. [Pam] Gill, you were working<br />
and caring for my beloved wife<br />
whose illness had progressed<br />
beyond the point of recall. Mixed<br />
with the personal tragedy of her<br />
loss was the awareness of a nurse<br />
who cared for her wonderfully<br />
and kindly, attending to her and<br />
her family with warm humanity.<br />
You were a bright light on dark<br />
days and a person whose care and<br />
skill I will never forget.”<br />
–a 4A Medical patient’s husband<br />
“Marcella [Bruner], you made a<br />
difficult time just a little easier.<br />
You always made me feel like I was<br />
just as important as all your other<br />
patients even though I know many<br />
were so very sick. I will always<br />
remember your kindness.”<br />
–a Med/Surg patient<br />
“Christy [Barger] was so very<br />
compassionate. She showed<br />
so much concern, and has a<br />
wonderful personality.<br />
She gave us hope.”<br />
–an Outpatient Surgery patient<br />
“Everyone provided excellent<br />
care, but especially Sara Craft<br />
and Sara Fitch, they could<br />
always cheer him up.”<br />
–a Med/Surg patient’s<br />
family member<br />
“Cathy Johnson, RN (Med/Surg)<br />
is a nurse who has the caring,<br />
positive attitude all nurses should<br />
have. She always has a smile no<br />
matter what the need is for the<br />
patients, visitors or co-workers.<br />
Cathy gives extraordinary service<br />
and compassionate care.<br />
She is a great nurse.”<br />
–a fellow colleague<br />
“The nurse Sherry Schwarz<br />
was great. She was helpful,<br />
courteous and polite.”<br />
–an Emergency Department patient<br />
“Ryan [Goble] was the best<br />
nurse I have honestly ever had.<br />
Please keep him or give him a<br />
raise or something!”<br />
–an Emergency Department patient<br />
“Reception and all nursing<br />
personnel were all professional<br />
and exhibited genuine care<br />
during my treatment.”<br />
–an Emergency Department patient<br />
“My nurse Stacey Puckett<br />
was really nice and took really<br />
good care of me.”<br />
–an Emergency Department patient<br />
Living Our Core Values
YOU’RE NEVER FAR FROM THE BEST CARE. ®<br />
<strong>Saint</strong> <strong>Joseph</strong> - Berea | <strong>Saint</strong> <strong>Joseph</strong> East | <strong>Saint</strong> <strong>Joseph</strong> <strong>Hospital</strong> | <strong>Saint</strong> <strong>Joseph</strong> - Jessamine<br />
<strong>Saint</strong> <strong>Joseph</strong> - London | <strong>Saint</strong> <strong>Joseph</strong> - Martin | <strong>Saint</strong> <strong>Joseph</strong> - Mount Sterling | Flaget Memorial <strong>Hospital</strong><br />
www.<strong>Saint</strong><strong>Joseph</strong>Nurses.org