Intravenous anaesthetic-hypnotic drugs Propofol Pentothal ...
Intravenous anaesthetic-hypnotic drugs Propofol Pentothal ...
Intravenous anaesthetic-hypnotic drugs Propofol Pentothal ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
25/11/2010<br />
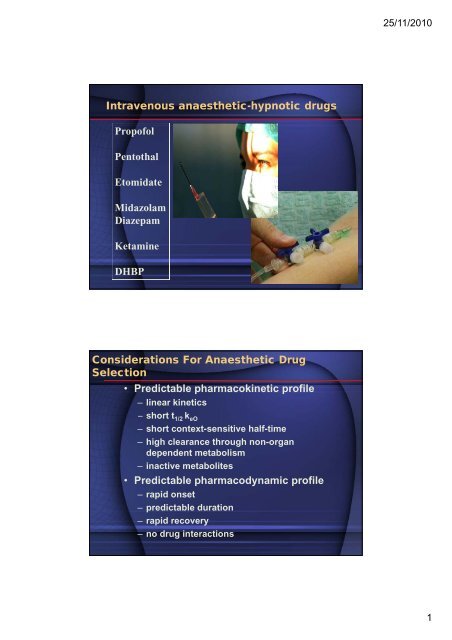
<strong>Intravenous</strong> <strong>anaesthetic</strong>-<strong>hypnotic</strong> <strong>drugs</strong><br />
<strong>Propofol</strong><br />
<strong>Pentothal</strong><br />
Etomidate<br />
Midazolam<br />
Diazepam<br />
Ketamine<br />
DHBP<br />
Considerations For Anaesthetic Drug<br />
Selection<br />
• Predictable pharmacokinetic profile<br />
– linear kinetics<br />
– short t 1/2 k eO<br />
– short context-sensitive half-time<br />
– high clearance through non-organ<br />
dependent metabolism<br />
– inactive metabolites<br />
• Predictable pharmacodynamic profile<br />
– rapid onset<br />
– predictable duration<br />
– rapid recovery<br />
– no drug interactions<br />
1
25/11/2010<br />
<strong>Intravenous</strong> drug delivery<br />
• manual infusion techniques :<br />
– bolus ( single or repeated)<br />
– constant rate infusion.<br />
– bolus + constant rate infusion.<br />
• PK/PD based infusion techniques :<br />
– open loop target controlled infusion<br />
techniques<br />
<br />
<br />
plasma target controlled delivery.<br />
effect side target controlled delivery.<br />
– closed loop infusion techniques<br />
Titration of <strong>anaesthetic</strong> depth<br />
(actual clinical practice)<br />
Inhaled <strong>anaesthetic</strong>s :<br />
VAPOR (vol%) ---- Inspired conc. ----- Endtidal conc. ----- drug<br />
effect<br />
<strong>Intravenous</strong> <strong>anaesthetic</strong>s :<br />
( “MAC” on line)<br />
Dose (mg/kg) --------????????? --------?????????? ------- drug<br />
effect<br />
(Cp50 and Cp95 not on line)<br />
2
25/11/2010<br />
Titration of <strong>anaesthetic</strong> depth<br />
(actual clinical practice)<br />
Inhaled <strong>anaesthetic</strong>s :<br />
VAPOR (vol%) ---- Inspired conc. ----- Endtidal conc. ----- drug<br />
effect<br />
<strong>Intravenous</strong> <strong>anaesthetic</strong>s :<br />
( “MAC” on line)<br />
Dose (mg/kg) --------????????? --------?????????? ------- drug<br />
effect<br />
Need for calculated (estimated) concentrations<br />
t 1/2 k e0 and time to peak effect<br />
Drug t 1/2 k e0 (min) Time to peak effect<br />
(min)<br />
<strong>Propofol</strong> 2.4 1.6 - 2.2<br />
Thiopental 1.5 1.7<br />
Midazolam 4.0 2.8<br />
Etomidate 1.5 2.0<br />
3
25/11/2010<br />
Pharmacology of iv. <strong>anaesthetic</strong>-<strong>hypnotic</strong>s<br />
CVS<br />
Drug MAP HR CO SVR Venodilation<br />
Thiopental - + - 0/+ +<br />
Diazepam 0/- -/+ 0 -/+ +<br />
Midazolam 0/- -/+ 0/- 0/- +<br />
Etomidate 0 0 0 0 0<br />
Ketamine ++ ++ + + 0<br />
<strong>Propofol</strong> - + 0 - +<br />
Drug depression of ventilation Airway resistance<br />
Thiopental ++ 0<br />
Diazepam + 0<br />
Midazolam + 0<br />
Etomidate + 0<br />
Ketamine 0 --<br />
<strong>Propofol</strong> ++ 0<br />
CNS : all : CBF , ICP , CMRO 2 <br />
ketamine : CBF , ICP , CMRO 2 <br />
γ-aminobutyric acid<br />
• a.k.a GABA<br />
• Most widespread inhibitory neurotransmitter in<br />
the CNS<br />
• Three classes of receptors<br />
• GABA A<br />
» Ligand gated ion channel<br />
» Cl - channel<br />
» Site of action of benzodiazepines, barbiturates, and<br />
propofol<br />
» Not the site of action of inhaled anesthetics<br />
• GABA B<br />
» Slow inhibitory post-synaptic potentials, regulates K +<br />
and Ca ++ conductance<br />
» Not a binding site of anesthetic <strong>drugs</strong><br />
• GABA C<br />
» Also a Cl - channel<br />
» Not a binding site of anesthetic <strong>drugs</strong><br />
4
25/11/2010<br />
GABA A Receptor<br />
• Transmembrane<br />
pentamer composed of 2<br />
α, 2 β, and 1 γ or δ<br />
subunits<br />
• Each has a binding site for<br />
GABA<br />
• Benzodiazepines<br />
• Bind a cleft of α and γ<br />
subunits<br />
• Increases frequency of<br />
channel opening<br />
• Barbiturates, (propofol)<br />
• Bind α subunit<br />
• Increase duration of<br />
channel opening<br />
• Agonist: muscimol<br />
• Antagonist: bicuculine<br />
<strong>Propofol</strong> / Characteristics (1)<br />
1. 2,6-diisopropylphenol is used for induction and<br />
maintenance of general anaesthesia.<br />
2. It is prepared as a 1% or 2% isotonic oil-in-water<br />
emulsion, which contains egg lecithin, glycerol,<br />
and soybean oil.<br />
3. Bacterial growth is inhibited by either ethylenediaminetetraacetic<br />
acid or sulfite.<br />
4. Mode of action: Increases activity at inhibitory<br />
γ-aminobutyric acid (GABA) synapses.<br />
5
25/11/2010<br />
<strong>Propofol</strong> / Pharmacokinetics (1)<br />
a. Elimination occurs primarily through hepatic metabolism<br />
to inactive metabolites.<br />
b. Context sensitive half-time (CSHT) of propofol is important.<br />
CSHT is defined as the time for a 50% decrease in the<br />
central compartment drug concentration after an infusion<br />
of specified duration.<br />
c. Induction doses rapidly produce unconsciousness<br />
(app. 30 to 45 sec), followed by rapid reawakening due<br />
to redistribution.<br />
<strong>Propofol</strong> / Pharmacodynamics (1)<br />
a. Central nervous system (CNS)<br />
1. Induction doses produce unconsciousness,<br />
whereas low doses produce<br />
conscious sedation.<br />
2. No analgesic properties.<br />
6
25/11/2010<br />
<strong>Propofol</strong> / Pharmacodynamics (2)<br />
b. Cardiovascular system<br />
1. A cardiovascular depressant.<br />
2. Produces dose-dependent decreases in<br />
arterial blood pressure and cardiac output.<br />
3. Heart rate is minimally affected, and<br />
barostatic reflex is blunted.<br />
c. Respiratory system<br />
1. Produces a dose-dependent decrease in<br />
respiratory rate and tidal volume.<br />
2. Ventilatory response to hypercarbia<br />
is diminished.<br />
<strong>Propofol</strong> / Administration (1)<br />
a. Induction: 2.0 to 2.5 mg/kg g IV.<br />
b. Sedation: 25 to 75 µg/kg/min by IV infusion is<br />
often sufficient (titrate to effect).<br />
c. Maintenance of general anesthesia:<br />
100 to 150 µg/kg/min IV (titrate to effect).<br />
d. Reduce dosages in elderly or hemodynamically<br />
compromised patients or if<br />
administered with other anesthetics.<br />
7
25/11/2010<br />
<strong>Propofol</strong> / Administration (2)<br />
e. May be diluted, if necessary, only in 5%<br />
dextrose in water to a minimum<br />
concentration of 0.2%.<br />
f. <strong>Propofol</strong> emulsion supports bacterial growth;<br />
prepare drug under sterile conditions and<br />
discard unused opened propofol after six<br />
hours to prevent inadvertent bacterial<br />
contamination.<br />
<strong>Propofol</strong> / Other effects (1)<br />
a. Venous irritation<br />
1. May cause pain during IV administration<br />
in as many as 50 to 75% of patients.<br />
2. Pain may be reduced by prior<br />
administration of opioids or the addition<br />
of lidocaine to the solution; alternatively,<br />
lidocaine (0.5 mg/kg) g) may be given IV<br />
1 to 2 minutes before the propofol with a<br />
tourniquet proximal to the IV site.<br />
3. If possible, administer intravenously in<br />
a large vein.<br />
8
25/11/2010<br />
<strong>Propofol</strong> / Other effects (2)<br />
b. Postoperative nausea and vomiting occurs<br />
less frequently after a propofol-based<br />
anesthetic compared with other methods.<br />
c. Lipid disorders<br />
<strong>Propofol</strong> is a lipid emulsion and should be<br />
used cautiously in patients with disorders of<br />
lipid metabolism (e.g. hyperlipidemia, pancreatitis).<br />
Benzodiazepines / Characteristics<br />
1. For anesthetic use: midazolam, diazepam, lorazepam.<br />
2. They are often used for sedation and amnesia<br />
or as adjuncts to general anesthesia.<br />
3. Mode of action: Bind at specific receptors in the CNS<br />
and enhance the inhibitory tone of GABA receptors.<br />
9
25/11/2010<br />
Benzodiazepines / Pharmacokinetics<br />
a. Metabolized in the liver.<br />
b. Peak CNS effect occur 4 to 8 minutes after<br />
an IV dose of diazepam, and its terminal halflife<br />
is app. 20 hours. Repeated doses result<br />
in accumulation and a prolonged effect.<br />
Active metabolites of diazepam are longer<br />
lasting than the parent drug.<br />
c. Both midazolam and diazepam redistribute<br />
rapidly and similarly after bolus injections.<br />
d. Metabolism may be significantly slower in elderly<br />
patients or those with hepatic disease.<br />
Benzodiazepines / Pharmacodynamics (1)<br />
a. Central nervous system (CNS)<br />
1. Produce amnestic, anticonvulsant,<br />
<strong>hypnotic</strong>, musclerelaxant, and sedative<br />
effects in a dose-dependent manner.<br />
2. Do not produce significant analgesia.<br />
10
25/11/2010<br />
Benzodiazepines / Pharmacodynamics (2)<br />
b. Cardiovascular system<br />
1. Produce a mild systemic vasodilation and<br />
reduction in cardiac output. Heart rate is<br />
usually unchanged.<br />
2. Hemodynamic changes may be pronounced<br />
in hypovolemic patients or in those with<br />
little cardiovascular reserve, if rapidly<br />
administered in a large dose, or if<br />
administered with an opioid.<br />
Benzodiazepines / Pharmacodynamics (3)<br />
c. Respiratory system<br />
1. Produce a mild dose-dependent decrease<br />
in respiratory rate and tidal volume.<br />
2. Respiratory depression may be<br />
pronounced if administered with an<br />
opioid, in patients with pulmonary disease,<br />
or in debilitated patients.<br />
11
25/11/2010<br />
Benzodiazepines / Administration<br />
a. Sedation (incremental doses)<br />
1. Midazolam: 0.5 to 1.0 mg IV or<br />
0.07-0.1mg/kg IM. Midazolam is the only<br />
benzodiazepine that can be given reliably<br />
by the intramuscular route.<br />
2. Diazepam: 2.5 to 5.0 mg IV or orally.<br />
3. Lorazepam: 0.5 to 2.0 mg IV or orally<br />
4. Preoperative benzodiazepine<br />
administration may lead to prolonged<br />
sedation postoperatively.<br />
Benzodiazepines / Adverse effects<br />
a. Drug interactions<br />
Administration of a benzodiazepine to a patient<br />
receiving the anticonvulsant valproate may<br />
precipitate a psychotic episode.<br />
b. Pregnancy and labor<br />
1. May be associated with birth defects<br />
(cleft lip and palate) when administered<br />
during the first trimester<br />
2. Cross the placenta and may lead to a<br />
depressed neonate.<br />
12
25/11/2010<br />
Flumazenil (1)<br />
Flumazenil is a competitive antagonist t for<br />
benzodiazepine receptors in the CNS.<br />
a. Reversal of benzodiazepine-induced sedative<br />
effects occurs within 2 minutes; peak effects at<br />
app. 10 minutes.<br />
b. Flumazenil is shorter acting than the<br />
benzodiazepines it is used to antagonize.<br />
Repeated administration may be necessary due to<br />
its short duration of action.<br />
Flumazenil (2)<br />
c. Metabolized to inactive metabolites in the liver.<br />
d. Dose: 0.3 mg IV every 30 to 60 seconds<br />
(to a max. dose of 5 mg).<br />
e. Flumazenil is contraindicated in patients with<br />
tricyclic antidepressant overdose and patients<br />
receiving benzodiazepines for control of seizures or<br />
elevated intracranial pressure. Use cautiously in<br />
patients who have had long-term treatment with<br />
benzodiazepines because acute withdrawal may<br />
be precipitated.<br />
13
25/11/2010<br />
Ketamine / Characteristics<br />
1. An arylcyclohexylamine and a congener<br />
of phencyclidine (PCP).<br />
2. Ketamine is usually employed as an induction agent.<br />
3. Mode of action: Not well defined but may include<br />
antagonism at the N-methyl-D-aspartate receptor.<br />
Ketamine / Pharmacokinetics<br />
a. Metabolized in the liver to multiple metabolites,<br />
some of which are active.<br />
b. Produces unconsciousness in 30 to 60 sec after an<br />
IV induction dose; unconsciousness may last 15 to<br />
20 minutes. After IM administration, the onset of CNS<br />
effects is delayed for app. 5 minutes, with peak effect<br />
at app. 15 minutes.<br />
c. Repeated bolus doses or an infusion results in<br />
accumulation.<br />
14
25/11/2010<br />
Ketamine / Pharmacodynamics (1)<br />
a. Central nervous system (CNS)<br />
1. Produces a “dissociative” state<br />
accompanied by amnesia and profound<br />
analgesia.<br />
2. Increases cerebral blood flow, metabolic<br />
rate, and intracranial pressure.<br />
Ketamine / Pharmacodynamics (2)<br />
b. Cardiovascular system<br />
1. Increases heart rate and systemic and pulmonary<br />
artery blood pressure by causing release of<br />
endogenous catecholamines.<br />
2. Often used for induction of general anesthesia in<br />
hemodynamically compromised patients.<br />
3. May act as a myocardial depressant if<br />
administered in the presence of hypovolemia,<br />
autonomic nervous system blockade, or maximal<br />
sympathetic nervous system stimulation.<br />
15
25/11/2010<br />
Ketamine / Pharmacodynamics (3)<br />
c. Respiratory system<br />
1. Mildly depresses respiratory rate and tidal volume.<br />
2. Minimal effect on responsiveness to hypercarbia.<br />
3. Laryngeal protective reflexes tend to be<br />
maintained longer than with other intravenous<br />
anesthetics.<br />
4. Alleviates bronchospasm by a sympathomimetic<br />
effect.<br />
Ketamine / Administration<br />
a. It may be especially useful for IM induction in<br />
patients in whom IV access is not available<br />
(e.g. children). Ketamine is water soluble and may be<br />
administered either IV or IM.<br />
b. Induction dosages are 1 to 2 mg/kg IV or 5 to<br />
10 mg/kg IM (a concentrated 10% solution is available<br />
for IM use only).<br />
c. IV sedative doses may be significantly lower<br />
(e.g. 0.2 mg/kg) and should be titrated to the desired<br />
effect.<br />
16
25/11/2010<br />
Ketamine / Side effects (1)<br />
a. Oral secretions are markedly stimulated by ketamine.<br />
Coadministration of an antisialogogue<br />
(e.g. glycopyrrolate) may be helpful.<br />
b. Muscle tone. May lead to random myoclonic<br />
movements, especially in response to stimulation.<br />
Muscle tone is often increased.<br />
c. Increases intracranial pressure and is relatively<br />
contraindicated in patients with head trauma or<br />
intracranial hypertension.<br />
Ketamine / Side effects (2)<br />
d. Eye movements. May lead to nystagmus, diplopia,<br />
i<br />
blepharospasm, and increased intraocular pressure:<br />
alternatives should be considered during<br />
ophthalmologic surgery.<br />
e. Anesthetic depth may be difficult to assess.<br />
Common signs of anesthetic depth<br />
(e.g. respiratory rate, blood pressure, heart rate,<br />
eye signs) are less reliable when ketamine is used.<br />
17
25/11/2010<br />
Ketamine / Side effects (3)<br />
Emotional disturbance<br />
1. Administration of ketamine may occasionally result<br />
in restlessness and agitation during emergence;<br />
hallucinations and unpleasant dreams may occur<br />
postoperatively.<br />
2. Patient characteristics associated with adverse effects<br />
include increased age, female gender, and dosages<br />
greater than 2 mg/kg.<br />
Ketamine / Side effects (4)<br />
3. The incidence (up to 30%) of these untoward<br />
sequelae may be greatly reduced with<br />
coadministration of a benzodiazepine (e.g. midazolam)<br />
or propofol.<br />
4. Children seem to be less troubled by the<br />
hallucinations than adults. Alternatives to ketamine<br />
should be considered in patients with psychiatric<br />
disorders.<br />
18
25/11/2010<br />
Etomidate / Characteristics<br />
1. It is an imidazole-containing <strong>hypnotic</strong> unrelated to<br />
other anesthetics.<br />
2. It is most commonly used as an IV induction agent<br />
for general anesthesia.<br />
3. Mode of action: Augments the inhibitory tone of<br />
GABA in the CNS.<br />
Etomidate / Pharmacokinetics<br />
a. Metabolized in the liver and by circulating<br />
esterases to inactive metabolites.<br />
b. Times to loss of consciousness and<br />
awakening after a sleep dose are similar to<br />
those of propofol.<br />
19
25/11/2010<br />
Etomidate / Pharmacodynamics (1)<br />
a. Central nervous system (CNS)<br />
1. Does not possess analgesic properties.<br />
2. Cerebral blood flow and metabolism decrease<br />
in a dose-dependent manner.<br />
b. Cardiovascular system<br />
Produces minimal changes in heart rate, blood<br />
pressure, and cardiac output; accordingly,<br />
etomidate may be a preferred agent for induction<br />
of general anesthesia in a hemodynamically<br />
compromised patient.<br />
Etomidate / Pharmacodynamics (2)<br />
c. Respiratory system<br />
Produces a dose-dependent decrease in<br />
respiratory rate and tidal volume; transient apnea<br />
may occur. The respiratory depressant effects of<br />
etomidate appear to be less than those of propofol<br />
or the barbiturates.<br />
20
25/11/2010<br />
Etomidate / Administration<br />
Available as a solution in propylene glycol.<br />
l<br />
An IV induction dose is 0.3 mg/kg.<br />
Etomidate / Side effects<br />
a. Myoclonus may occur after administration,<br />
particularly in response to stimulation.<br />
b. Nausea and vomiting occur more frequently in the<br />
postoperative period than with other anesthetic agents.<br />
c. Venous irritation may be minimized by administration<br />
into a free-flowing IV carrier infusion.<br />
d. Adrenal suppression<br />
Suppresses adrenal steroid synthesis for up to 24<br />
hours (probably an effect of little clinical significance).<br />
Repeated doses or infusions are not recommended<br />
because of the risk of significant adrenal suppression.<br />
21
25/11/2010<br />
Barbiturates / Characteristics<br />
1. For anesthetic use: thiopental, methohexital.<br />
2. These medications, like propofol, rapidly<br />
produce unconsciousness (app. 30 to 45 sec)<br />
followed by rapid reawakening due to<br />
redistribution.<br />
3. Barbiturates are very alkaline (pH>10) and<br />
are usually prepared as dilute solutions<br />
(1.0 to 2.5%) for IV administration.<br />
i ti<br />
4. Mode of action<br />
Barbiturates occupy receptors adjacent to<br />
GABA receptors in the CNS and augment the<br />
inhibitory tone of GABA.<br />
Barbiturates / Pharmacokinetics<br />
a. Metabolism to inactive metabolites occurs in the liver.<br />
b. Produce unconsciousness in one arm-tobrain<br />
circulation time (app. 30 sec).<br />
c. Recovery from an induction dose occurs<br />
quickly (app. 5 to 10 minutes) as a result of<br />
high lipid solubility and rapid redistribution<br />
into muscle and organs with high blood flow.<br />
d. Multiple doses or a prolonged infusion may<br />
produce prolonged sedation or unconsciousness.<br />
The CSHT of these <strong>drugs</strong> are long,<br />
even after short infusions.<br />
22
25/11/2010<br />
Barbiturates / Pharmacodynamics (1)<br />
a. Central nervous system (CNS)<br />
1. Produce unconsciousness but cause<br />
hyperalgesia in sub<strong>hypnotic</strong> doses.<br />
2. Produce a dose-dependent decrease in<br />
cerebral metabolism and blood flow and,<br />
at high doses, may produce an isoelectric<br />
electroencephalogram.<br />
Barbiturates / Pharmacodynamics (2)<br />
b. Cardiovascular system<br />
1. Decrease arterial blood pressure and<br />
cardiac output in a dose-dependent<br />
manner.<br />
2. May increase heart rate via baroceptor<br />
reflexes.<br />
c. Respiratory system<br />
Produce a dose-dependent decrease<br />
in respiratory rate and tidal volume.<br />
Apnea may result for 30 to 90 sec after<br />
a sleep dose.<br />
23
25/11/2010<br />
Barbiturates / Administration<br />
a. Thiopental and thiamylal: 3 to 5 mg/kg IV.<br />
b. Methohexital: 1 to 2 mg/kg IV or<br />
25 to 30 mg/kg per rectum<br />
c. Reduce doses in sick, elderly, or<br />
hypovolemic patients.<br />
Barbiturates / Side effects (1)<br />
a. Allergy<br />
Do not administer to patients with history of<br />
allergy to any barbiturate. bit t Anaphylactic and<br />
anaphylactoid reactions occur rarely.<br />
b. Porphyria<br />
1. Absolutely contraindicated in patients with<br />
acute intermittent porphyria, variegate<br />
porphyria, and hereditary coproporphyria.<br />
2. Barbiturates induce the enzyme δ-aminolevulinic<br />
acid synthetase, the rate-limiting<br />
step in porphyrin synthesis, and may<br />
precipitate an acute attack.<br />
24
25/11/2010<br />
Barbiturates / Side effects (2)<br />
c. Venous irritation and tissue damage<br />
1. May cause pain at the site of administration<br />
because of venous irritation.<br />
2. Infiltration of intraarterial administration of a<br />
barbiturate may cause severe pain, tissue<br />
damage, and necrosis due to its high alkalinity.<br />
If intraarterial administration occurs,<br />
heparinization and regional sympathetic blockade<br />
may be helpful in treatment.<br />
d. Myoclonus and hiccoughing are often associated<br />
with the administration of methohexital.<br />
25