Pre-Eclampsia
Pre-Eclampsia
Pre-Eclampsia
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
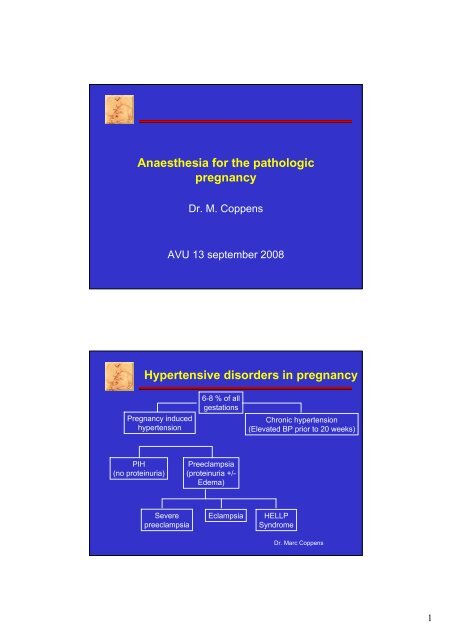
Anaesthesia for the pathologic<br />
pregnancy<br />
Dr. M. Coppens<br />
AVU 13 september 2008<br />
Hypertensive disorders in pregnancy<br />
<strong>Pre</strong>gnancy induced<br />
hypertension<br />
6-8 % of all<br />
gestations<br />
Chronic hypertension<br />
(Elevated BP prior to 20 weeks)<br />
PIH<br />
(no proteinuria)<br />
<strong>Pre</strong>eclampsia<br />
(proteinuria +/-<br />
Edema)<br />
Severe<br />
preeclampsia<br />
<strong>Eclampsia</strong><br />
HELLP<br />
Syndrome<br />
Dr. Marc Coppens<br />
1
<strong>Pre</strong>-<strong>Eclampsia</strong><br />
• Classic triad :<br />
Hypertension (>140/90)<br />
Proteinuria (>1+ or >300 mg/24h)<br />
Generalized edema (least reliable)<br />
• Hypertension and proteinuria must be present<br />
on two occasions > 6 hr apart<br />
• Rapid weight gain is supportive evidence<br />
Dr. Marc Coppens<br />
<strong>Pre</strong>-eclampsia: pathophysiology<br />
• Immunological conflict between genetic make-up of<br />
mother and baby, triggered by fœtal cells and DNA in<br />
the maternal circulation (first pregnancy or older multipara with new<br />
partner)<br />
• Focus: placenta: trophoblastic invasion<br />
• Endothelial cell dysfunction > placental ischemia<br />
• Prostacyclin/tromboxane imbalance<br />
– Vasoconstriction ↑<br />
– Platelet aggregation ↑<br />
– Uterine activity ↑<br />
– Uteroplacental blood flow ↓<br />
• Syncitine: genetic basis<br />
Dr. Marc Coppens<br />
2
Thrombocytopenia<br />
Endothelium<br />
Thrombocytes<br />
Dr. Marc Coppens<br />
Severe <strong>Pre</strong>-eclampsia:<br />
diagnostic criteria<br />
Headaches<br />
Visual disturbances<br />
Pulmonary edema<br />
Hepatic Dysfunction<br />
RUQ or epigastric pain<br />
Oliguria<br />
Elevated creatinine<br />
Proteinuria of 5 g or more in 24 h<br />
Systolic BP > 160 mmHg<br />
Diastolic BP > 110 mmHg<br />
Thrombocytopenia or hemolysis<br />
Dr. Marc Coppens<br />
3
Clinical course of pre-eclampsia<br />
Eye<br />
Arteriolar spasm amaurosis<br />
Retinal hemorrhage blindness<br />
Papilledema<br />
Transient scotoma<br />
Respiratory System<br />
Pulmonary edema<br />
ARDS<br />
Liver<br />
Subcapsular hemorrhage<br />
Hepatic rupture<br />
Hematopoietic system<br />
HELLP<br />
DIC<br />
CNS<br />
Headache<br />
Seizures – grand mal type (tonic-clonic)<br />
Intracranial hemorrhage - CVA<br />
Encephalopathy – cerebral oedema<br />
Pancreas<br />
Kidneys<br />
Uteroplacental circulation<br />
IUGR Large placental infarct<br />
Abruption<br />
Fetal compromise<br />
Fetal demise: mortality x 2<br />
Dr. Marc Coppens<br />
Cardiovascular changes<br />
• Hypovolemia<br />
• Hemoconcentration<br />
• Increased blood<br />
viscosity<br />
• Vasospasm<br />
• Interstitial oedema<br />
Hydrostat pressure ↑<br />
Vasc permeability ↑<br />
Colloid osm pressure ↓<br />
Blood volume expansion in normal<br />
pregnancy !!<br />
Focus on systolic blood pressure<br />
28 patients with stroke<br />
23 systolic P > 160<br />
3 diastolic P > 110<br />
Obstet & Gynecol 2005;246-54<br />
Dr. Marc Coppens<br />
4
<strong>Pre</strong>-eclampsia: therapy<br />
• Vasodilation<br />
• Plasma volume expansion<br />
• Anti-convulsant therapy<br />
• Correct clotting abnormalities<br />
• Delivery of the foetus<br />
Dr. Marc Coppens<br />
Magnesium sulfate<br />
• Loading dose: 4 to 6 grams in 100 ml, given<br />
IV over 15 to 20 minutes<br />
• Continuous infusion: 2 to 3 grams per hour<br />
• Monitor:<br />
– Mg levels<br />
– Reflexes: stop Mg if patellar reflexes are absent<br />
– Mental status<br />
– Respiratory status: stop Mg if RR is < 16 /min<br />
– Urine output: stop Mg if < 100ml/4 hr<br />
Dr. Marc Coppens<br />
5
Magnesium Levels<br />
mg/dl<br />
Normal 1.3 to 2.6<br />
Therapeutic 4 to 8<br />
Loss of patellar reflexes 8 to 10<br />
Somnolence 10 to 12<br />
Respiratory depression 12 to 17<br />
Paralysis 15 to 17<br />
Cardiac arrest 30 to 35<br />
Antidote is calcium gluconate one gram IV over 3 minutes<br />
97% excreted in urine<br />
Dr. Marc Coppens<br />
Magnesium<br />
• Effects on neuromuscular junction !<br />
– Potentiation of the action of nondepolarizing<br />
muscle relaxants<br />
reduced dose requirement<br />
longer duration of action<br />
cave ‘priming dose’<br />
– Succinylcholine and Mg ?<br />
fasciculations not seen !!<br />
Peripheral nerve stimulation<br />
Release AcChol ↓<br />
Sensitivity ↓<br />
Dr. Marc Coppens<br />
6
Magnesium<br />
• Vasodilator activity<br />
– Direct and indirect effects<br />
– Sympathetic block<br />
• Direct smooth muscle relaxation<br />
in uterus<br />
– Inhibition of catecholamine release<br />
Control of hypertension at laryngoscopy and intubation<br />
Cave hypotension with regional anesthesia<br />
Cave postpartum hemorrhage<br />
Sense of warmth at the tongue with rapid bolus<br />
Dr. Marc Coppens<br />
Management of imminent eclampsia or<br />
eclampsia<br />
• Airway, Breahting, Circulation<br />
• Left lateral position, maintain airway<br />
• Administer oxygen, check for aspiration or<br />
pulmonary oedema<br />
• MgSO 4 = therapy of choice<br />
• Vast majority of initial seizures are self-limiting<br />
• Diazepam, phenytoin not as first-line treatment<br />
Dr. Marc Coppens<br />
7
Regional anesthesia for severe pre-eclampsia:<br />
possible disadvantages<br />
• Reduced plasma volume: risk for hypotension ↑<br />
• Reduced uteroplacental perfusion > hypotension<br />
• IV fluid administration: risk for iatrogenic pulmonary<br />
oedema<br />
• More sensitive to pressor agents ( efedrine )<br />
• Incrementally dosing the epidural catheter<br />
But, …<br />
Dr. Marc Coppens<br />
Regional anesthesia for severe pre-eclampsia:<br />
CSE<br />
• Magnitude of maternal blood pressure declines<br />
similar after spinal and epidural anesthesia in severe<br />
preeclampsia Anesthesiology 1999;90:1276<br />
• Patients with severe preeclampsia experience less<br />
hypotension during spinal anesthesia for CS then<br />
healthy parturients Anest Analg 2003;97:867-72<br />
• Combined spinal epidural Reg Anesth Pain Med 2001;26:46<br />
– Low dose spinal ± epidural bolus<br />
– Rapid onset of spinal anesthesia<br />
– Especially beneficial in urgent C-section<br />
Dr. Marc Coppens<br />
8
Anti-hypertensive medication<br />
Vasodilation<br />
• Protect cerebral<br />
circulation<br />
Fœtal distress<br />
<strong>Pre</strong>-renal oliguria<br />
• Compromised perfusion<br />
Contracted intravascular<br />
volume<br />
<strong>Pre</strong>load ↓<br />
Venous return ↓<br />
CO ↓<br />
Dr. Marc Coppens<br />
Anti-hypertensive medications<br />
• Dihydralazine - Nepresol ®<br />
– Direct acting vasodilator > arteriolar<br />
– Loadingdose: 5 mg IV ( repeat/20 min, max 20 mg)<br />
– Maintenance dose: 1 mg/h Iv<br />
1 A or 25 mg in 50 ml NaCl 0.9 % - 2 ml/hr<br />
incompatible with gluc 5 % Side-effects:<br />
Tachycardia<br />
Hypotension<br />
Headache<br />
Long onset time !!<br />
Vomiting<br />
Epigastric pain<br />
Dr. Marc Coppens<br />
9
Hydralazine vs labetalol<br />
• Hydralazine was associated with<br />
– More maternal hypotension ( OR 3,29 )<br />
– More caesarean sections ( OR 1,3 )<br />
– More placental abruption ( OR 4,17 )<br />
– More maternal oliguria ( OR 4,0 )<br />
– More adverse effects on FHR ( OR 2,0 )<br />
– More maternal adverse effects<br />
– Less neonatal bradycardia<br />
BMJ 2003<br />
Dr. Marc Coppens<br />
• Labetolol - Trandate ®<br />
– α en β blocking properties<br />
– Initial oral dose of 100 mg (30 min)<br />
– IV bolus: 25-50 mg IV – max 200 mg –<br />
– infusion 20 mg/hr (max 160 mg/hr)<br />
– Short-acting<br />
– Cave bronchoconstriction (asthma)<br />
– Growth restriction > in first trimester<br />
Dr. Marc Coppens<br />
10
Anti-hypertensive medications<br />
• Nifedipine-Adalat ®<br />
– hypertensive crisis<br />
– oral administration: 10 mg<br />
– Long-acting !<br />
– Drug interaction with Magnesium ( 100.000<br />
• Platelet count indicates severity of pre-eclampsia<br />
• Trends are important !<br />
– Admission platelet count<br />
– Repeat / 4 – 6 hrs<br />
• PC continue to fall postoperatively Check PC prior to<br />
– Nadir at 29 ± 15 hrs<br />
removal of epidural<br />
– Average time to PC > 100.000 = 60 hrs catheter<br />
Dr. Marc Coppens<br />
11
<strong>Pre</strong>-eclampsia<br />
Dr. Marc Coppens<br />
Corticosteroids for HELLP<br />
• Retrospective obs. studies: improvement in<br />
lab values: Plts ↑, ALT ↓, AST ↓<br />
• Prospective randomised trials: improved<br />
outcome,lab values, BP, Urine output<br />
• More regional anesthesia: mean fall plts<br />
↓,mean platelets at delivery ↑, No with ↑ plts<br />
Dr. Marc Coppens<br />
12
Systemic analgesia<br />
Pethidine:<br />
prolonged half-life in the mother: 2.5-3 h<br />
prolonged half-life in the neonate: 18-23 h<br />
accumulation of active metabolites: 60 h<br />
subtle neonatal depression for days !<br />
Dr. Marc Coppens<br />
Remifentanil in obstetrics<br />
• Low dose: no efficacy<br />
• High dose: adverse effects<br />
– Maternal desaturation/sedation<br />
– FHR abnormalities<br />
• PCIA remifentanil<br />
– Volikas: 0.5 µ/kg bolus remi, lock out 5 min<br />
– Vs pethidine/meperidine/dolantine<br />
– Pain scores significantly less for remi<br />
– More respiratory depression for pethidine IV<br />
Dr. Marc Coppens<br />
13
Remifentanil vs pethidine<br />
bolus<br />
Lock-out<br />
infusion<br />
Blair<br />
40µ<br />
2 min<br />
Volikas<br />
0.5µ/kg<br />
2 min<br />
Roelant<br />
25µ<br />
5 min<br />
0.05 µ/kg<br />
Volmanen<br />
0.4µ/kg<br />
1 min<br />
Significant reduction in pain scores<br />
Desaturation possible ( Oxygen, monitoring, training,<br />
enough staff, sedation scores )<br />
High maternal satisfaction<br />
Less neonatal adverse events<br />
Dr. Marc Coppens<br />
Sectio preterm<br />
Dr. Marc Coppens<br />
14
Sectio preterm<br />
Difference in local anaesthetic requirements:<br />
• à term ( 38-42 w ) vs preterm ( 28-35 w )<br />
• CSE met hyperbare marcaine: 2.25 ml (11.25<br />
mgr)<br />
• <strong>Pre</strong>term: onvoldoende bij 21/25 parturienten<br />
• Onset bij preterme groep trager<br />
• À term: voldoende hoog block bij alle ptn T4<br />
• Minder hypotensie<br />
Compression of vena cava<br />
Increased sensitivity to local anesthetic<br />
Dr. Marc Coppens<br />
Remifentanil<br />
• µ opioid receptor antagonist<br />
• High potency !!!<br />
• Low onset time<br />
• Rapidly hydrolyzed<br />
• Small volume of distibution<br />
• High clearance<br />
• Does not rely on pseudocholinesterase<br />
Dr. Marc Coppens<br />
15
Remifentanil<br />
Case reports<br />
– Hemodynamic stability with CV disease<br />
– Facilitation of epid catheter placement<br />
– C section in preeclampsia and thrombocytopenia<br />
– PCA for labour<br />
– Acoustic neuroma & C section<br />
–TCI<br />
‘ the paediatricians commented on the lack of<br />
respiratory depression in view of the opioid given to<br />
the mother ‘<br />
Dr. Marc Coppens<br />
Placental transfer<br />
Anesthesiology, 1998<br />
• Elective C section with epidural anesthesia<br />
and concomitant IV infusion of remifentanil (<br />
0,1 µg/kg/min ) - 16 patients<br />
• Increase, decrease or bolus according clinical<br />
judgment<br />
• Blood samples: ABG, remifentanil,<br />
remifentanil acid<br />
– maternal arterial<br />
– umbilical venous<br />
– umbilical arterial<br />
Dr. Marc Coppens<br />
16
Placental transfer<br />
Maternal<br />
• blood pressure<br />
• heart rate<br />
• O 2 Sat<br />
• Pain score<br />
• Sedation score<br />
Neonatal<br />
• Apgar<br />
• Nacs<br />
Dr. Marc Coppens<br />
Placental transfer<br />
• UV:MA ratio suggests a significant placental<br />
transfer<br />
• UA:UV ratio suggests rapid metabolism and<br />
rapid redistribution<br />
Dr. Marc Coppens<br />
17
Placental transfer<br />
• Mean clearance:<br />
93.1 ml/min<br />
kg<br />
• Non obstetric patients: 41.2 ml/min<br />
kg<br />
• Physiologic changes of pregnancy<br />
– Larger blood volume<br />
– Increased cardiac output<br />
– Increased renal perfusion<br />
– Altered volume of distribution<br />
– Lower plasma protein concentration<br />
– Increase in nonspecific esterase activity<br />
Dr. Marc Coppens<br />
Placental transfer<br />
• No adverse neonatal effects !<br />
• Slightly increased UV P CO2 values ~ maternal<br />
P CO2<br />
Dr. Marc Coppens<br />
18
Placental transfer<br />
Dr. Marc Coppens<br />
SURGERY & ANAESTHESIA<br />
in <strong>Pre</strong>gnancy<br />
• 0.5% - 2% of gravidae undergo surgery<br />
• <strong>Pre</strong>-term labour and fetal loss are major risks<br />
• Pulmonary oedema is a major risk<br />
• Teratogenesis a minor risk<br />
• Regional is better than general<br />
• Consider delivery first if > 28-30 weeks<br />
• Safe Anaesthesia is based on sound<br />
understanding and application of pregnancy,<br />
physiology and pharmacology<br />
0.3 % amb non ob surgery<br />
Dr. Marc Coppens<br />
19
Types of SURGERY in <strong>Pre</strong>gnancy<br />
1. Surgery associated with <strong>Pre</strong>gnancy:<br />
Cervical Cerclage<br />
Ovarian torsions, cysts, etc.<br />
Fetal surgery<br />
2. Surgery unrelated to <strong>Pre</strong>gnancy:<br />
Severe Trauma<br />
Acute abdomen<br />
Neurosurgery (life-threatening)<br />
Cardiothoracic (decompensating)<br />
Dr. Marc Coppens<br />
• Avoid maternal hypoxaemia, reduction in<br />
placental perfusion: intrauterine asphyxia<br />
• Maintenance of maternal pregnant<br />
physiology:avoid hypotension, hypohypercapnia<br />
• Consider direct and indirect toxic effects of<br />
anaesthetic drugs upon the feto-placental unit<br />
Dr. Marc Coppens<br />
20
Respiratory:<br />
• ↑ VO 2 ; ↑ Minute Ventilation; ↓ pCO 2 ; ↓ FRC<br />
• Mucosal hyperaemia<br />
• ↑ risk of difficult intubation<br />
• ↑ risk of pulmonary aspiration<br />
Aspiration prophylaxis:<br />
Zantac<br />
Primperan<br />
Na-citrate<br />
Dr. Marc Coppens<br />
Cardiovascular<br />
• ↑ CO; ↑ Blood Volume (100ml/kg); ↓ PCV<br />
• Aortocaval compression (> 20 weeks)<br />
• ↑ in baroreceptor responsiveness<br />
• ↓ vascular responsiveness<br />
• ↑ risk of thrombosis<br />
Dr. Marc Coppens<br />
21
Avoiding hypotension<br />
• Prophylactic Phenylephrine Infusion for<br />
<strong>Pre</strong>venting Hypotension During Spinal<br />
Anesthesia for Cesarean Delivery:<br />
100 µ/min<br />
no adverse effects on neonate<br />
• The full left lateral position reduces the<br />
incidence of early hypotension compared with<br />
the tilted supine position with tilt, and makes it<br />
easier to treat.<br />
Dr. Marc Coppens<br />
Neurological:<br />
• ↓ MAC gaseous/volatile drugs: sensitivity<br />
• ↓ Dose requirements of LAs<br />
• ↑ Dose requirements others. e.g. SCh<br />
Gastrointestinal:<br />
• ↑ gastric volume<br />
Cave unconscious sedation !<br />
• ↓ gastric pH<br />
• ↓ lower oesophageal sphincter tone<br />
Rapid sequence induction !!<br />
Dr. Marc Coppens<br />
22
Anaesthesia techniques:<br />
MAINTAIN NORMOXIA, NORMOCARBIA<br />
Regional: ↓ fetal drug exposure (spinal, CSE)<br />
less<br />
blood loss, airway simplified,<br />
tocolysis more complicated, better<br />
analgesia, ↓ DVT risk<br />
General:<br />
Total control, simple tocolysis<br />
Sevoflurane produces dose-dependent depression of uterine muscle<br />
contractility. At concentrations of 3.5 MAC and above, uterine activity was<br />
virtually abolished.<br />
Dr. Marc Coppens<br />
Anaesthesia & Gestation:<br />
Non-viable fetus: Follow general principles.<br />
Assess coagulopathy, uterine rupture<br />
1 st Trimester: Avoid surgery if possible.<br />
Assess fetal viability and status.<br />
Nausea, vomiting common.<br />
After 6-8 weeks, pregnancy physiology is<br />
well established.<br />
Dr. Marc Coppens<br />
23
Anaesthesia & Gestation:<br />
2 nd Trimester: ‘Best’ time for surgery.<br />
Uterine displacement beyond 18-20 weeks.<br />
Aspiration prophylaxis, intubate.<br />
Minimise uterine manipulation.<br />
Careful with ketamine, etc.<br />
Tocolysis usually required.<br />
Thromboprophylaxis advisable.<br />
Dr. Marc Coppens<br />
Anaesthesia & Gestation:<br />
3 rd Trimester:<br />
CONSIDER DELIVERY FIRST<br />
Uterine displacement.<br />
Aspiration prophylaxis, intubate.<br />
Minimise uterine manipulation.<br />
Care with ketamine. Avoid NSAIDs.<br />
Tocolytics often required.<br />
Thromboprophylaxis.<br />
Steroids (< 34 weeks).<br />
Dr. Marc Coppens<br />
24
Inhalation<br />
• Chloroform: hepatic failure<br />
• Ether & cyclopropane: explosion<br />
• Halothane: headache, exhaustion, …<br />
• 1967: adverse reproductive effects<br />
• Halothane in rats: aberrant skeletal<br />
development after 12 h exposure<br />
• Fink: rats exposed to high concentrations of<br />
nitrous oxide: more skeletal abno<br />
Prolonged exposure to trace concentrations<br />
Single or repeated high dose exposure<br />
Dr. Marc Coppens<br />
Inhalational anaesthetics<br />
• No mutagenic effects ( N 2 O, E,I,D,S )<br />
• No carcinogenic effects<br />
• N 2 O is the only inhaled anaesthetic that has<br />
been convincingly shown to be directly<br />
teratogenic in experimental animals<br />
• Interference with DNA synthesis (methionine<br />
synthethase)<br />
• Consensus: any teratogenic effects caused<br />
by changes in physiology !<br />
Dr. Marc Coppens<br />
25
Inhalational anaesthetics<br />
• No data to suggest that waste anaesthetic<br />
gases are a danger to those women working<br />
in a scavenged environment who are<br />
contemplating pregnancy or who are already<br />
pregnant<br />
• Scavenging of waste anaesthetic gases<br />
should be performed in whatever location an<br />
inhaled anaestetic is used<br />
Dr. Marc Coppens<br />
• NSAID’s: avoid in 3th trimester: premature<br />
closure of ductus<br />
• Aspirine/NSAID’s: gastroschisis, mild cardiac<br />
defects, orofacial defects<br />
• BZD: oral cleft<br />
• Paracetamol is safe<br />
• NMB drugs: high molecular weight, do not<br />
reach fetal circulation<br />
Dr. Marc Coppens<br />
26
Fetal monitoring<br />
Fetal heart rate variability decreased !<br />
Ideally + external tocography !!<br />
Dr. Marc Coppens<br />
EFFECTIVE TOCOLYTIC DRUGS<br />
• General (Volatile) Anaesthetics<br />
• Oxytocin antagonists (ATOSIBAN)<br />
• Calcium antagonists (esp Mg ++ )<br />
• Nitric Oxide donors (GTN)<br />
• Beta-2 Sympathomimetics<br />
• Prostaglandin inhibitors (< 30/40)<br />
• Combination therapies<br />
• (Local Anaesthetics)<br />
• (Ethanol)<br />
Dr. Marc Coppens<br />
27
ACUTE TOCOLYSIS - PRACTICALITIES<br />
General Anaesthesia:<br />
• Titrate volatile agent to effect while monitoring<br />
mother, fetus, uterine tone and contractility.<br />
• 1.5 – 2.0 MAC usually required. ( isoflurane,<br />
sevoflurane)<br />
• MAINTAIN TOCOLYSIS POST-OP.<br />
Dr. Marc Coppens<br />
ACUTE TOCOLYSIS - PRACTICALITIES<br />
Regional Anaesthesia:<br />
• Magnesium Sulfate (4 – 6G + infusion)<br />
• Terbutaline 250mcg bolus<br />
• GTN boluses 3 – 4 mcg / kg<br />
(Atosiban)<br />
• MAINTAIN TOCOLYSIS POST-OP<br />
Dr. Marc Coppens<br />
28
Dr. Marc Coppens<br />
SUMMARY<br />
• <strong>Pre</strong>-term labour is greatest concern, and tocolytics<br />
needed<br />
• Expert planning and team work needed<br />
• Anaesthesia is safe, conditions that necessitate surgery<br />
and surgery itself, is more important<br />
• Reassure mother about drugs and anaesthesia<br />
• Follow basic principles of obstetric anaesthesia<br />
• Good post-op analgesia and fetal / uterine monitoring<br />
• Consider delivery if fetus is viable and > 28 weeks<br />
Dr. Marc Coppens<br />
29
The obstetric patient with cardiac<br />
disease<br />
Dr. Marc Coppens<br />
• Understanding the defect and the physiologic<br />
effects of pregnancy on hemodynamics<br />
– No inappropriate advice against pregnancy<br />
– Identifying those patients with unacceptable high<br />
risk (contraception)<br />
– Optimal perinatal care in co-operation with<br />
relevant specialities<br />
– Good communication with the on-call teams<br />
Dr. Marc Coppens<br />
30
Dr. Marc Coppens<br />
Anticoagulation<br />
• Heparin does not cross the placenta<br />
– No adverse effects on fetal development<br />
– But maternal thrombocytopenia and osteoporosis<br />
• Oral anticoagulants:<br />
– Readily crosses the placenta<br />
– Fetal warfarin syndrome: hydrocephalus,<br />
microcephaly, growth retardation, ophtalmic<br />
abnormalities<br />
Dr. Marc Coppens<br />
31
• Vaginal delivery has been favoured<br />
– Induction of labour but, …<br />
Reversal of anticoagulation<br />
Side effects of drugs used to induce labour<br />
Labour and vaginal delivery associated with profound<br />
haemodynamic changes:<br />
1st stage: CO ↑ 10%<br />
uterine contraction: autotransfusion of 500 ml<br />
2nd stage: CO ↑ 50%<br />
immediately postpartum: autotransfusion<br />
Dr. Marc Coppens<br />
Regional analgesia<br />
– Anticoagulation ?!<br />
– Minimizes cardiovascular changes during labour<br />
– Consider orthosympathic blockade<br />
– Use dilute local anaesthetic/opioid solutions<br />
– Consider CSE for C-section<br />
Dr. Marc Coppens<br />
32
C-section<br />
bupi<br />
sal<br />
bupi<br />
sal<br />
c<br />
sal<br />
Test<br />
pinprick<br />
ether<br />
ethylchloride<br />
Low-dose CSE plus EVE<br />
Dr. Marc Coppens<br />
Aorto-caval compression<br />
Anest Analg 2003;97:256-8<br />
To avoid any detrimental<br />
effect on maternal<br />
cardiac output the<br />
pregnant patient would<br />
ideally be kept in the full<br />
lateral position<br />
When it is necessary to lay<br />
the woman on the back<br />
tilting her to the left is<br />
preferable<br />
Even more important in<br />
compromised patients<br />
Dr. Marc Coppens<br />
33
Phenylephrine<br />
• Excellent efficacy to maintain maternal blood<br />
pressure during spinal anesthesia for C-<br />
section<br />
• Less fetal acidosis compared to ephedrine<br />
• Good hemodynamics in the cardiovascular<br />
impaired patients<br />
Dr. Marc Coppens<br />
Peripartum hemorrhage<br />
Dr. Marc Coppens<br />
34
Postpartum hemorrhage<br />
Normal blood loss:<br />
vaginal: 500 ml / 24 hrs<br />
abdominal:1000 ml / 24 hrs<br />
4 T’s<br />
Tone<br />
Trauma<br />
Tissue<br />
Thrombi<br />
n<br />
Specific Cause<br />
Atonic uterus<br />
Cervical,vaginal,<br />
Perineal, uterine<br />
inversion, ruptured uterus<br />
Retained placenta<br />
Invasive placenta<br />
coagulopathies<br />
Relative<br />
frequenc<br />
70 % y<br />
20 %<br />
10 %<br />
1 %<br />
Dr. Marc Coppens<br />
Postpartum hemorrhage:<br />
uterine atony<br />
• Most common cause of serious blood loss !!<br />
• 15 % of cardiac output to gravid uterus<br />
• Management<br />
– Fluid resuscitation<br />
–Oxygen<br />
– Uterine massage<br />
– Uterotonics<br />
Dr. Marc Coppens<br />
35
Postpartum hemorrhage:<br />
uterine atony<br />
• High parity<br />
• Dysfunctional labor<br />
• Uterine distention<br />
– Multiple gestation<br />
– Polyhydramnios<br />
– Macrosomia<br />
• Retained placenta<br />
• Infection: chorioamnionitis<br />
• Medication<br />
– Prolonged oxytocin use<br />
– Tocolytic agents<br />
– Inhalational anesthetics<br />
Dr. Marc Coppens<br />
Uterotonics<br />
• Oxytocin: bolus 5 U<br />
– Stimulation of upper uterine segment (rhytm)<br />
– Vasodilator<br />
– Cave hypotension, water intoxication<br />
– IM or dilute IV infusion<br />
– 10 units/500 ml ( max 80 mU/min)<br />
Dr. Marc Coppens<br />
36
Synto: bolus vs infusion<br />
Dr. Marc Coppens<br />
Adverse effects<br />
Dr. Marc Coppens<br />
37
Uterotonics: methergine<br />
• Sustained increase in uterine tone<br />
Tetanic contraction of upper and lower uterine segment<br />
• IM 0.2 mg IM<br />
• Peripheral vasoconstriction and hypertension<br />
• Coronary vasospasm ( stess-test in cardiology )<br />
Dr. Marc Coppens<br />
Uterotonics<br />
• 15-methyl prostaglandin F2α or carboprost<br />
• Prostin ® /15M<br />
– Intramyometrially<br />
– Intramuscularly<br />
– 0.25 mgr up to 2 mgr<br />
• Systemic and pulmonary vasoconstriction<br />
– Cave accidental IV infusion<br />
– Rapid uptake by uterine venous sinuses<br />
– Severe systemic and pulmonary hypertension<br />
– Severe bronchospasm<br />
Dr. Marc Coppens<br />
38
Misoprostol<br />
Dr. Marc Coppens<br />
Postpartum hemorrhage:<br />
retained placenta<br />
• Occurs in 1% of deliveries<br />
• Anesthetic management<br />
– Uterine relaxation:<br />
• Nitroglycerin: 100 µgr<br />
• Onset time: 30-45 sec<br />
• Duration: 60-90 sec<br />
– Analgesia:<br />
• Epidural<br />
• Spinal<br />
• > 1 MAC Inhalatie<br />
Careful dosing !!!<br />
Hypovolemia<br />
Manual removal<br />
Dr. Marc Coppens<br />
39
Placenta previa<br />
• Abnormal implantation of placenta<br />
• <strong>Pre</strong>natal ultrasonographic diagnosis: anterior or posterior<br />
• More common with prior C section<br />
• Painless vaginal bleeding thirth trimester<br />
• Blood loss – placental surface area ↓<br />
Dr. Marc Coppens<br />
Placenta accreta<br />
• Abnormal attachment of placenta to uterine<br />
wall<br />
• Risk factors<br />
– Placenta praevia<br />
• No previous CS: 0.5%<br />
• 1 previous CS: 24%<br />
• 2 previous CS: 50%<br />
• ≥ 4 previous CS: 67%<br />
Dr. Marc Coppens<br />
40
Placenta accreta<br />
• Risk factors:<br />
– Multiparity<br />
– <strong>Pre</strong>vious CS<br />
– Advanced maternal age<br />
– <strong>Pre</strong>vious dilatation and curettage<br />
Dr. Marc Coppens<br />
Dr. Marc Coppens<br />
41
Abruptio placentae<br />
• Bleeding into the decidua<br />
basalis leads to separation of<br />
the placenta.<br />
• Hematoma formation further<br />
separates the placenta from<br />
the uterine wall, causing<br />
compression of these<br />
structures and compromise of<br />
blood supply to the fetus.<br />
• Revealed hemorrhage = solutio<br />
Dr. Marc Coppens<br />
<strong>Pre</strong>term labor<br />
• <strong>Pre</strong>term delivery = birth before 37 weeks gestation<br />
• <strong>Pre</strong>term labor = uterine contractions prior to 37 w<br />
cervical effacement and dilation<br />
• PROM = premature rupture of membranes<br />
Rupture one hour or more prior to onset of labor<br />
• PPROM = preterm premature rupture of membranes<br />
premature rupture of membranes at less than 37 w<br />
Dr. Marc Coppens<br />
42
PPROM : complications<br />
• Fetal complications<br />
– Infection<br />
– <strong>Pre</strong>maturity<br />
• Maternal complications<br />
– Chorioamnionitis<br />
– Endomyometritis<br />
– Operative intervention<br />
Dr. Marc Coppens<br />
Corticosteroids in PTL<br />
• Effectively reduce RDS, IVH,and infant<br />
mortality at 24-34 weeks gestation<br />
• Criteria: 24-34 weeks gestation +<br />
– No contraindication to 24-48 h delay in delivery<br />
– No contraindication to steroids<br />
• Betamethasone 12 mg IM, 2 doses, 24 h<br />
apart<br />
• Dexamethasone 6 mg IM, 4 doses, 12 hours<br />
apart<br />
Dr. Marc Coppens<br />
43
Tocolytic agents<br />
• « buying time » for<br />
– Steroid induced maturity of fetal lungs<br />
– Maternal transfer to MIC (maternal intensive care)<br />
• Terbutaline<br />
• Ritodrine = <strong>Pre</strong>par ®<br />
Dr. Marc Coppens<br />
<strong>Pre</strong>par<br />
• Beta 1 -agonist side effects<br />
Shortness of breath<br />
Hypotension<br />
Cardiac arrhytmias<br />
• Hypokalemia is one of the most common side effects<br />
– Increase in plasma insulin<br />
– Stimulation of cellular intake of potassium<br />
After cessation: decrease in insulin might produce a rebound<br />
release of intracellular potassium<br />
Hyperkalemia<br />
Max 90-150 minutes after cessation<br />
Dr. Marc Coppens<br />
44
Venous thromboembolism<br />
• Virchow’s triade:<br />
– Increased pro-coagulant factors and reduced fibrinolysis<br />
– Venous flow is altered<br />
– Trauma to venous system ( vaginal delivery, cesarean)<br />
• Reduction in blood flow velocity<br />
– 2nd trimester, nadir at 34 weeks, 6 weeks postpartum<br />
– Common femoral vein<br />
Diameter increases ( 9.1 to 12.7 mm)<br />
Flow velocity falls ( 14.8 to 4.5 cm/second)<br />
> Cesarean section !!!<br />
> DVT:in 85 % of cases left leg<br />
Dr. Marc Coppens<br />
Risk factors of VTE<br />
• Age > 35<br />
• Weight > 80 kg<br />
• Multiparity<br />
• Family history of VTE<br />
• Deficiencies:<br />
– Antithrombin<br />
– Protein C<br />
– Protein S<br />
• Gene variants:<br />
– Factor V Leiden<br />
– Prothrombin<br />
• Lupus anticoagulant<br />
Dr. Marc Coppens<br />
45
Basic Literature<br />
• The role of the anaesthetist in the<br />
management of the pre-eclamptic patient.<br />
Dyer, Current Opinion in Anaesthesiology<br />
2007,20: 168-174<br />
• First trimester anesthesia exposure and fetal<br />
outcome. A review. Allaert, Acta<br />
Anaesthesiologica Belgica 2007, vol 58, 2, pg<br />
119<br />
Dr. Marc Coppens<br />
Suggested reading<br />
• Severe cardiac disease in pregnancy, part I:<br />
impact of congenital and acquired cardiac<br />
diseases during pregnancy. Van Mook:<br />
Current Opinion in Critical Care 2005,<br />
11:430-434<br />
• Severe cardiac disease in pregnancy, part II:<br />
impact of congenital and acquired cardiac<br />
diseases during pregnancy. Van Mook:<br />
Current Opinion in Critical Care 2005,<br />
11:435-448<br />
Dr. Marc Coppens<br />
46
Suggested reading<br />
• Options for systemic labour analgesia. Evron<br />
Current Opinion in Anaesthesiology, 2007,<br />
20:181-185;<br />
Dr. Marc Coppens<br />
47