Dr Tom Roques, Norfolk & Norwich University Hospital
Dr Tom Roques, Norfolk & Norwich University Hospital
Dr Tom Roques, Norfolk & Norwich University Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
09/01/2013<br />
What can doctors do to<br />
prevent radiotherapy<br />
errors?<br />
<strong>Tom</strong> <strong>Roques</strong><br />
Consultant Clinical Oncologist<br />
<strong>Norfolk</strong> and <strong>Norwich</strong> <strong>University</strong> <strong>Hospital</strong><br />
tom.roques@nnuh.nhs.uk<br />
BIR errors meeting September 2012<br />
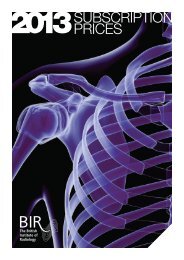
The problem - level 1<br />
Level 1 errors don’t usually involve doctors directly<br />
1
09/01/2013<br />
The problem - level 5<br />
What incidents do doctors<br />
cause?<br />
Thanks to Mark Rose, NNUH<br />
2
09/01/2013<br />
How to improve?<br />
Awareness that volume definition is an early part of a<br />
complex process<br />
Pre-planning meetings<br />
Dedicated planning and approval time in job plans<br />
(and in reality)<br />
RCR – many oncologists don’t have formal planning<br />
time in job plans. ‘Planning time…needs to be seen<br />
as equating to an operating list’<br />
Overall doctors’ role<br />
Leadership for the whole pathway<br />
A guide to understanding IR(ME)R in radiotherapy 2008<br />
3
09/01/2013<br />
WHO report<br />
Radiotherapy risk profile<br />
Systematic review of RT errors 1976-2007<br />
Published data and department incident reports<br />
Worldwide<br />
16 separate episodes affecting 3125 patients t - of<br />
whom 38 died due to overdose<br />
4
09/01/2013<br />
Radiotherapy risk profile<br />
Medical errors as a whole<br />
UK chief medical officer report 2000 suggested<br />
between 60,000 and 255,000 deaths or serious<br />
disability annually<br />
Current data - 12000 preventable hospital deaths<br />
annually in UK<br />
5
09/01/2013<br />
Why so many errors?<br />
Extremely complex hospital working - inevitability<br />
Culture – lack of learning<br />
Lack of systems<br />
Pressure on individuals<br />
Belief that clinical autonomy paramount<br />
6
09/01/2013<br />
7
09/01/2013<br />
Two main problem areas<br />
• Patient selection for treatment<br />
• Volume definition<br />
How do we choose the right<br />
treatment for the patient?<br />
Selection criteria for radiotherapy relatively vague<br />
Clinical trial selection criteria not applied in real life<br />
Rely on staging (at MDT), PS and intuition<br />
Poor at assessing functional reserve – esp in elderly<br />
8
09/01/2013<br />
Huge variation in the UK<br />
Geographical Variation in Radiotherapy Services Across the UK in 2007 and the Effect of Deprivation<br />
M.V. Williams and K.J. <strong>Dr</strong>inkwater Clinical Oncology August 2009<br />
The problem with MDTs<br />
Over-stretched<br />
- all becoming longer and there are<br />
more of them<br />
Perhaps one doctor will have met the patient<br />
The treating oncologist will almost certainly not have<br />
met the patient<br />
So decisions i based on imaging i and path, not patient<br />
t<br />
characterstics and preferences<br />
Little/no evidence to support quality of MDT decision<br />
making<br />
9
09/01/2013<br />
Performance status<br />
www.pallimed.org/2008/09/physician-patient-disagreement-about.htmlabout.html<br />
What can we do -<br />
selection?<br />
Meticulous staging to exclude those with metastases from curative<br />
RT<br />
Formal QA of MDTs - dummy patients at MDT, review of blind cases,<br />
revalidation<br />
Need to develop much better tools to select patients on basis of<br />
functional status (overall and organ specific)<br />
Good outcomes data collection by individual clinician - especially in<br />
patients with high rates of metastases<br />
Listen to others – CNSs, radiographers etc. Do they think the<br />
treatment plan is correct<br />
Collaborative oncologist discussion of NPs once seen. Pre planning<br />
meetings<br />
10
09/01/2013<br />
Volume definition<br />
11
09/01/2013<br />
• Ceci n’est nest pas une pipe<br />
Vxv| ÇËxáà Ñtá âÇ ÄâÇz vtÇvxÜ<br />
12
09/01/2013<br />
13
09/01/2013<br />
PET to improve concordance<br />
Steenbakkers et al. IJROBP 2008<br />
Radiochemotherapy +/- tirapazamine in HN cancer<br />
861 patients, 82 centres in 16 countries<br />
Diagnostic imaging and plans submitted for central<br />
review by end of week 1 of therapy (n=687).<br />
Changes recommended in 197 (29%)<br />
14
09/01/2013<br />
QA review of all plans within trial<br />
Further TMC review after trial<br />
closed of all evaluable patients<br />
(n=820)<br />
97 major errors - 24 incorrect<br />
GTV, 41 PTV not covered, 25<br />
incorrect prescription, 7<br />
prolonged treatment<br />
197 plans had major changes recommended during<br />
the study<br />
Of these 89 were implemented - all passed TMC<br />
review<br />
108 not implemented - 95 failed TMC review<br />
15
09/01/2013<br />
Conclusions<br />
GTV outlining<br />
• Main source of systematic error in RT<br />
• Have all the information you before you start –<br />
diagnostic imaging, op note, surgeon etc<br />
• View planning CT on PACS screen with the eye of a<br />
radiologist<br />
• Clinical and radiological anatomy<br />
• Never copy slices<br />
• Radiologists defining GTVs?<br />
16
09/01/2013<br />
Imaging for Oncologists<br />
• UK Royal College of Radiologists 2004<br />
17
09/01/2013<br />
CTV<br />
• Selection v delineation<br />
• Contouring atlases for<br />
standard nodal CTVs<br />
• Primary CTVs much more of<br />
an art – balance of risks<br />
CTV definition<br />
18
09/01/2013<br />
19
09/01/2013<br />
To improve volume<br />
definition<br />
Meticulous documentation of MDT discussions<br />
Pre-planning meeting - especially for selection of target<br />
volume<br />
Dedicated time for volume definition (like operating lists)<br />
Very careful review of planning CT<br />
Radiologist/surgeon input to difficult cases<br />
Review all volumes with another clinician – delineation<br />
Take part in clinical trials with QA<br />
To improve volume<br />
definition<br />
Think like a surgeon<br />
Question every bit of every contour all the time<br />
Map your recurrences very carefully<br />
Outsourcing of rarer cases?<br />
Better teaching tools (including radiation oncologists?)<br />
Always remember we are the weakest link and the biggest<br />
source of errors<br />
20
09/01/2013<br />
Conclusions<br />
• Take leadership for the whole treatment pathway<br />
• Look for the unknown unknowns<br />
• Refine tools for selecting patients for RT<br />
• GTV is a statement of fact. CTV is a statement of<br />
uncertainty.<br />
ty<br />
• We are not good at either and need help!<br />
Final picture<br />
21