Dengue Shock Syndrome Presenting as Acute Cholecystitis - Springer
Dengue Shock Syndrome Presenting as Acute Cholecystitis - Springer
Dengue Shock Syndrome Presenting as Acute Cholecystitis - Springer
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Digestive Dise<strong>as</strong>es and Sciences, Vol. 50, No. 5 (May 2005), pp. 874–875 ( C○ 2005)<br />
DOI: 10.1007/s10620-005-2656-z<br />
CASE REPORT<br />
<strong>Dengue</strong> <strong>Shock</strong> <strong>Syndrome</strong> <strong>Presenting</strong><br />
<strong>as</strong> <strong>Acute</strong> <strong>Cholecystitis</strong><br />
Y.-M. TAN, MD, FRCS, C.-C. ONG, and A. Y. F. CHUNG, MD, FRCS<br />
KEY WORDS: dengue shock syndrome; dengue fever; cholecystitis.<br />
<strong>Dengue</strong> fever (DEF), estimated to affect 100 million people<br />
annually worldwide, may present <strong>as</strong> a mild febrile<br />
illness or <strong>as</strong> hemorrhagic fever with shock (1). However,<br />
unusual clinical presentations that mimic other common<br />
emergencies can occ<strong>as</strong>ionally occur (2). A high clinical<br />
suspicion is required to make an early diagnosis and initiate<br />
prompt treatment. If unrecognized, delay in treatment<br />
can lead to dis<strong>as</strong>trous outcomes. Here we describe an unusual<br />
clinical presentation of DF mimicking a common<br />
surgical and g<strong>as</strong>troenterology emergency.<br />
CASE REPORT<br />
A 45-year-old lady presented with a 5-day febrile illness <strong>as</strong>sociated<br />
with epig<strong>as</strong>tric discomfort radiating to the right hypochondrium.<br />
Her pain w<strong>as</strong> dull and intermittent but escalating in intensity.<br />
This w<strong>as</strong> <strong>as</strong>sociated with generalized myalgia and weakness.<br />
She had no significant medical or travel history. At presentation<br />
in the emergency room, she w<strong>as</strong> tachycardiac, with a pulse rate<br />
of 100/min and a blood pressure of 68/45. Clinically, she w<strong>as</strong><br />
flushed and dehydrated. Exquisite tenderness with guarding w<strong>as</strong><br />
elicited in the right hypochondrium, corresponding to a positive<br />
Murphy’s sign. The rest of the abdomen w<strong>as</strong> mildly distended but<br />
soft. There w<strong>as</strong> no discernible skin r<strong>as</strong>h and the rest of the systemic<br />
examination w<strong>as</strong> normal. The clinical diagnosis of acute<br />
cholecystitis with septic shock w<strong>as</strong> made.<br />
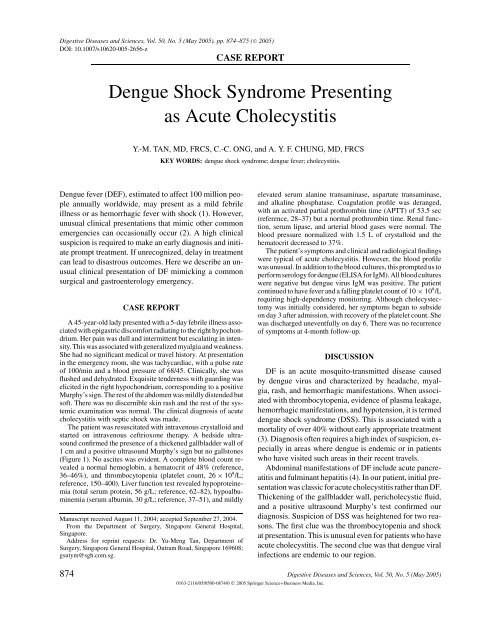
The patient w<strong>as</strong> resuscitated with intravenous crystalloid and<br />
started on intravenous ceftrioxone therapy. A bedside ultr<strong>as</strong>ound<br />
confirmed the presence of a thickened gallbladder wall of<br />
1cmand a positive ultr<strong>as</strong>ound Murphy’s sign but no gallstones<br />
(Figure 1). No <strong>as</strong>cites w<strong>as</strong> evident. A complete blood count revealed<br />
a normal hemoglobin, a hematocrit of 48% (reference,<br />
36–46%), and thrombocytopenia (platelet count, 26 × 10 9 /L;<br />
reference, 150–400). Liver function test revealed hypoproteinemia<br />
(total serum protein, 56 g/L; reference, 62–82), hypoalbuminemia<br />
(serum albumin, 30 g/L; reference, 37–51), and mildly<br />
Manuscript received August 11, 2004; accepted September 27, 2004.<br />
From the Department of Surgery, Singapore General Hospital,<br />
Singapore.<br />
Address for reprint requests: Dr. Yu-Meng Tan, Department of<br />
Surgery, Singapore General Hospital, Outram Road, Singapore 169608;<br />
gsutym@sgh.com.sg.<br />
elevated serum alanine transamin<strong>as</strong>e, <strong>as</strong>partate transamin<strong>as</strong>e,<br />
and alkaline phosphat<strong>as</strong>e. Coagulation profile w<strong>as</strong> deranged,<br />
with an activated partial prothrombin time (APTT) of 53.5 sec<br />
(reference, 28–37) but a normal prothrombin time. Renal function,<br />
serum lip<strong>as</strong>e, and arterial blood g<strong>as</strong>es were normal. The<br />
blood pressure normalized with 1.5 L of crystalloid and the<br />
hematocrit decre<strong>as</strong>ed to 37%.<br />
The patient’s symptoms and clinical and radiological findings<br />
were typical of acute cholecystitis. However, the blood profile<br />
w<strong>as</strong> unusual. In addition to the blood cultures, this prompted us to<br />
perform serology for dengue (ELISA for IgM). All blood cultures<br />
were negative but dengue virus IgM w<strong>as</strong> positive. The patient<br />
continued to have fever and a falling platelet count of 10 × 10 9 /L<br />
requiring high-dependency monitoring. Although cholecystectomy<br />
w<strong>as</strong> initially considered, her symptoms began to subside<br />
on day 3 after admission, with recovery of the platelet count. She<br />
w<strong>as</strong> discharged uneventfully on day 6. There w<strong>as</strong> no recurrence<br />
of symptoms at 4-month follow-up.<br />
DISCUSSION<br />
DF is an acute mosquito-transmitted dise<strong>as</strong>e caused<br />
by dengue virus and characterized by headache, myalgia,<br />
r<strong>as</strong>h, and hemorrhagic manifestations. When <strong>as</strong>sociated<br />
with thrombocytopenia, evidence of pl<strong>as</strong>ma leakage,<br />
hemorrhagic manifestations, and hypotension, it is termed<br />
dengue shock syndrome (DSS). This is <strong>as</strong>sociated with a<br />
mortality of over 40% without early appropriate treatment<br />
(3). Diagnosis often requires a high index of suspicion, especially<br />
in are<strong>as</strong> where dengue is endemic or in patients<br />
who have visited such are<strong>as</strong> in their recent travels.<br />
Abdominal manifestations of DF include acute pancreatitis<br />
and fulminant hepatitis (4). In our patient, initial presentation<br />
w<strong>as</strong> cl<strong>as</strong>sic for acute cholecystitis rather than DF.<br />
Thickening of the gallbladder wall, pericholecystic fluid,<br />
and a positive ultr<strong>as</strong>ound Murphy’s test confirmed our<br />
diagnosis. Suspicion of DSS w<strong>as</strong> heightened for two re<strong>as</strong>ons.<br />
The first clue w<strong>as</strong> the thrombocytopenia and shock<br />
at presentation. This is unusual even for patients who have<br />
acute cholecystitis. The second clue w<strong>as</strong> that dengue viral<br />
infections are endemic to our region.<br />
874 Digestive Dise<strong>as</strong>es and Sciences, Vol. 50, No. 5 (May 2005)<br />
0163-2116/05/0500-0874/0 C○ 2005 <strong>Springer</strong> Science+Business Media, Inc.
DENGUE SHOCK SYNDROME PRESENTING AS ACUTE CHOLECYSTITIS<br />
Fig 1. Ultr<strong>as</strong>ound showing thickening of the gallbladder wall but no gallstones, suggestive of<br />
acalculous cholecystitis.<br />
Ultr<strong>as</strong>ound examination failed to reveal any calculi and<br />
our patient w<strong>as</strong> diagnosed with the acalculous variant of<br />
cholecystitis. The etiology of acalculous cholecystitis in<br />
DF is not clear. In DSS, the underlying pathophysiological<br />
mechanism results from endothelial damage and incre<strong>as</strong>ed<br />
v<strong>as</strong>cular permeability. Local inflammation of the<br />
gallbladder can be attributed to “pl<strong>as</strong>ma leakage” leading<br />
to wall thickening and hypotension leading to ischemia of<br />
the gallbladder. Direct viral involvement of the gallbladder<br />
may also contribute to this unusual presentation. A search<br />
of the English literature showed only one previous report<br />
of cholecystitis and DF (5). In that report, the patient w<strong>as</strong><br />
not <strong>as</strong> acutely ill and/or in shock. With conservative treatment,<br />
the patient recovered uneventfully. Our patient similarly<br />
had acalculous cholecystitis but presented in shock<br />
with DSS. Definitive treatment for patients with acalculous<br />
cholecystitis from other causes is cholecystectomy<br />
(6). This is because of the high incidence of complications<br />
like gangrene, perforation, and abscess formation. However,<br />
we chose to manage our patient conservatively, due<br />
to the severe thrombocytopenia, and to monitor closely for<br />
any complications. Cholecystectomy in this patient would<br />
have been fraught with danger due to bleeding intraoperatively<br />
or postoperatively. Moreover, her symptoms began<br />
to settle by the third day. This conservative approach w<strong>as</strong><br />
justified, <strong>as</strong> acalculous cholecystitis in the background of<br />
DF appears to be a self-limiting event.<br />
REFERENCES<br />
1. Rigau-Perz JG, Clark GG, Griber DJ, Reiter P, Sanders EJ, Vorndam<br />
AV: <strong>Dengue</strong> and dengue hemorrhagic fever. Lancet 352:971–977,<br />
1998<br />
2. George R, Liam CK, Chua CT, Lam SK, Pang T, Geethan R: Unusual<br />
clinical manifestations of dengue virus infection. Southe<strong>as</strong>t Asian J<br />
Trop Med Public Health 19:585–590, 1988<br />
3. Gibbons RV, Vaughn DW: <strong>Dengue</strong>: an escalating problem. BMJ<br />
324:1563–1566, 2002<br />
4. Nimmanitya P, Thisyakorn U, Hemsrichart V: <strong>Dengue</strong> hemorrhagic<br />
fever with unusual manifestations. Southe<strong>as</strong>t Asian J Trop Med Public<br />
Health 18:398–406, 1987<br />
5. Sood A, Midha V, Sood N, Kaushal V: Acalculous cholecystitis<br />
<strong>as</strong> an atypical presentation of dengue fever. Am J G<strong>as</strong>troenterol<br />
95(11):3316–3317, 2000<br />
6. Kalliaf<strong>as</strong> S, Zeigler DW, Flancbaum L, Choban PS: <strong>Acute</strong> acalculous<br />
cholecystitis: incidence, risk factors, diagnosis, and outcome. Am<br />
Surg 64(5):471–475, 1998<br />
Digestive Dise<strong>as</strong>es and Sciences, Vol. 50, No. 5 (May 2005) 875