Bloodborne Pathogens Exposure Control Plan - Oakland University
Bloodborne Pathogens Exposure Control Plan - Oakland University
Bloodborne Pathogens Exposure Control Plan - Oakland University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Oakland</strong> <strong>University</strong><br />
<strong>Bloodborne</strong> <strong>Pathogens</strong><br />
<strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong><br />
MAY 1992<br />
(Revised 1993, 1994, 1996, 1999, 2000, 2001 and 2004)<br />
Office of Environmental Health and Safety<br />
Department of Risk Management and Contracting<br />
Rochester, Michigan 48309-4401<br />
(248) 370-4196
<strong>Oakland</strong> <strong>University</strong><br />
<strong>Bloodborne</strong> <strong>Pathogens</strong><br />
<strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong><br />
for<br />
DEPARTMENT: ___________________________<br />
MAY 1992<br />
[Revised 1993, 1994, 1996, 1997, 2000 and 2001]<br />
Office of Environmental Health and Safety<br />
Graham Health Center<br />
(248) 370-4196
<strong>Oakland</strong> <strong>University</strong><br />
<strong>Bloodborne</strong> <strong>Pathogens</strong> <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong><br />
TABLE OF CONTENTS<br />
1.0 About this Written <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong>................................................................................. 1<br />
1.1 The Written <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong> Includes ........................................................ 1<br />
2.0 Program Administration............................................................................................................... 2<br />
TABLE 1 - Individuals Responsible for Implementing the ECP in their Departments. ................. 3<br />
3.0 Employee <strong>Exposure</strong> Determination.............................................................................................. 4<br />
TABLE 2 - Job Classifications for which ALL employees Risk Occupational <strong>Exposure</strong>.............. 4<br />
TABLE 3 - Job Classifications for which SOME employees Risk Occupational <strong>Exposure</strong>........... 5<br />
4.0 Methods of <strong>Control</strong>ling <strong>Exposure</strong> to BBPs.................................................................................. 5<br />
4.1 Universal Precautions ............................................................................................ 5<br />
4.2 Work Practice <strong>Control</strong>s.......................................................................................... 5<br />
4.3 Engineering <strong>Control</strong>s ............................................................................................. 5<br />
TABLE 4 - Tasks Which May Present BBP <strong>Exposure</strong> and Associated PPE/Engineering Ctrls..... 6<br />
5.0 Biohazardous Waste ...................................................................................................................... 9<br />
5.1 Contaminated Sharps ............................................................................................. 9<br />
5.2 Contaminated Laundry .......................................................................................... 9<br />
5.3 Biohazard bags, hampers and sharp safes.............................................................. 9<br />
6.0 Contaminated Equipment........................................................................................................... 10<br />
7.0 Cleaning Up Spills........................................................................................................................ 10<br />
7.1 Washable Surfaces............................................................................................... 10<br />
7.2 Non-Washable Surfaces....................................................................................... 10<br />
8.0 Hepatitis B Vaccinations ............................................................................................................. 12<br />
8.1 “Pre-<strong>Exposure</strong>” Vaccinations .............................................................................. 10<br />
8.2 “Post-<strong>Exposure</strong>” Vaccinations............................................................................. 11<br />
9.0 <strong>Exposure</strong> Incident Response and Follow-up ............................................................................. 13<br />
9.1 <strong>Exposure</strong> Incident - First Response ..................................................................... 13<br />
9.2 Post-<strong>Exposure</strong> Evaluation and Follow-up ........................................................... 13<br />
10.0 Employee Training....................................................................................................................... 12<br />
10.1 When and How Often .......................................................................................... 12<br />
10.2 Who Conducts Training....................................................................................... 12<br />
10.3 Elements of Training ........................................................................................... 13<br />
11.0. Record Keeping............................................................................................................................ 13<br />
11.1 Training Records.................................................................................................. 13<br />
11.2 Medical Records .................................................................................................. 13<br />
11.3 <strong>Exposure</strong> Incident Evaluation Records................................................................ 14<br />
12.0 Conditions for Laboratories Working with HIV and Hepatitis Viruses ................................ 14<br />
12.1 Working in HIV and Hepatitis Viruses “Production Facilities” .......................... 14<br />
12.2 Working in HIV and Hepatitis Virus “Research Laboratories”........................... 15<br />
APPENDICES........................................................................................................................................... 21<br />
Blank Forms<br />
Completed Departmental Forms<br />
Universal Precautions and OSHA <strong>Bloodborne</strong> <strong>Pathogens</strong> Standard<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP Revised April 2004
1.0 ABOUT THIS WRITTEN EXPOSURE CONTROL PLAN<br />
This <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong> is intended to serve as OU’s guide to the OSHA Standard<br />
1910.1030, “Occupational <strong>Exposure</strong> to <strong>Bloodborne</strong> <strong>Pathogens</strong>”, which requires, as a central<br />
component, the development and issuance of an <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong> (ECP).<br />
The information contained in this publication is not considered a substitute for the OSH Act or<br />
any provisions of OSHA standards. It provides general guidance on the OSHA <strong>Bloodborne</strong><br />
<strong>Pathogens</strong> Standard, but should not be considered the legal authority for compliance with OSHA<br />
requirements. Rather, the reader should consult the OSHA standard in its entirety and/or OU’s<br />
Office of Environmental Health and Safety (OEHS) for specific compliance requirements.<br />
1.1 The Written <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong> includes:<br />
• Determination of employee exposure<br />
• Methods of controlling exposure, including: Universal Precautions and work practice controls<br />
• Engineering <strong>Control</strong>s and Personal Protective Equipment<br />
• Biohazardous Waste<br />
• Contaminated Equipment<br />
• Cleaning up Spills<br />
• Hepatitis B vaccination<br />
• <strong>Exposure</strong> Incident Response and Follow-up<br />
• Employee Training<br />
• Record keeping<br />
• Conditions for working with HIV or a Hepatitis virus in the laboratory<br />
Employees covered by the bloodborne pathogens standard receive an explanation of this ECP<br />
during their initial training sessions. It will also be reviewed in their annual refresher training.<br />
All employees have an opportunity to review this plan at any time during their work shifts by<br />
contacting the responsible persons identified in Table 1 (Section 2.0). If requested, those<br />
individuals will provide their employees with a copy of the ECP free of charge and within 15<br />
days of the request<br />
The responsible persons identified in Table 1 (Section 2.0) are responsible for reviewing the<br />
ECP annually, or more frequently if necessary, to identify 1) any new or modified tasks and<br />
procedures which affect occupational exposure and 2) any new or revised job classifications that<br />
present occupational exposure.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP Revised April 2004
2.0 PROGRAM ADMINISTRATION<br />
The individuals found in Table 1 below are currently responsible for the implementation of the<br />
ECP in their respective departments. These individuals are responsible to:<br />
• Maintain and provide all necessary personal protective equipment (PPE), engineering controls<br />
(e.g., sharps containers), labels, and red bags as required by the standard<br />
• Ensure that all medical actions required are performed and that appropriate employee health<br />
and OSHA records are maintained<br />
• Ensure that all training is provided and documented<br />
• Ensure that the written ECP is available to employees, OSHA, and NIOSH representatives;<br />
• Review the ECP (and request updates as necessary from the Office of EH&S) at least<br />
annually, and/or whenever necessary to include new or modified tasks and procedures.<br />
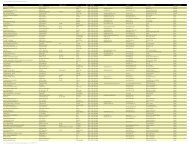
TABLE 1<br />
Individuals Responsible for Implementing ECP in their Departments<br />
Department Position(s) Employee Name(s) (as<br />
of Feb. 2005)<br />
Telephone<br />
Extension(s)<br />
Athletics<br />
Head Athletic Trainer<br />
Asst. Dir. Facilities & Ops<br />
Tom Ford<br />
Eric Stephan<br />
3189<br />
4050<br />
Biological Sciences Laboratory Manager Michael Poosch 3556<br />
Campus Cleaning Supervisors Herb Lucre, Wendy Tyrell 2168<br />
Campus Recreation<br />
Chemistry<br />
Asst. Dir., Campus Progs.<br />
Asst. Dir., Aquatics<br />
Assistant Laboratory<br />
Manager<br />
Mila Padgett<br />
Dan Plamondon<br />
4910<br />
4533<br />
Marcee Daly 2330<br />
Eye Research Institute Asst. to the Director Paulette Realy 2390<br />
Graham Health Center Coordinator Joanne Talarek 4375<br />
Grounds/Vehicle Maint. Supervisor Randy Drewry 2413<br />
Lab Animal Mgmt Svcs Manager Cliff Snitgen 4441<br />
Lowry Early Childhood Ctr Director Tiffany Wright 4100<br />
Meadow Brook Hall Facility Operations Manager Kim Zelinski 3140<br />
Electrical and Plumbing Foreman Dan Niezurawski 4438<br />
<strong>Oakland</strong> Center Asst. Director Operations Rich Zizek 3245<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 2 of 19<br />
Revised April 2004
TABLE 1<br />
Individuals Responsible for Implementing ECP in their Departments<br />
Department Position(s) Employee Name(s) (as<br />
of Feb. 2005)<br />
Telephone<br />
Extension(s)<br />
Police Department Lieutenant Mel Gilroy 3339<br />
Residence Halls<br />
Custodial & Maintenance<br />
Mgrs<br />
Frank Moss<br />
Karen Pipitone<br />
4061<br />
3570<br />
School of Education Coor of Field Svcs. Sherrill Karppinen 3083<br />
School of Health Sci<br />
School of Nursing<br />
All Sci and Res Depts.<br />
Director Exercise Science<br />
Assoc. Professor, Exer Sci<br />
Assoc. Professor, Exer Sci<br />
Program Dir., Med Lab Sci<br />
Interim Associate Dean<br />
Nursing Laboratory Mgr<br />
Admin Project Coordinator<br />
Laboratory Compliance<br />
Manager (Office of EH&S)<br />
Brian Goslin<br />
Charles Marks<br />
Robert Jarski<br />
Lynne Williams<br />
Diane Norris<br />
Patricia Ketcham<br />
Joann Burrington<br />
4140<br />
4539<br />
4191<br />
4040<br />
4484<br />
4066<br />
4065<br />
Domenico Luongo 4314<br />
3.0 EMPLOYEE EXPOSURE DETERMINATION<br />
Table 2 below identifies those OU job classifications (i.e., positions) for which ALL employees<br />
who hold those positions risk occupational exposure to <strong>Bloodborne</strong> <strong>Pathogens</strong> (without regard to<br />
the use of personal protective clothing or equipment):<br />
TABLE 2<br />
Job Classifications for which ALL* employees Risk Occupational <strong>Exposure</strong><br />
Clinical Faculty<br />
Coach<br />
Custodian<br />
Job Classification<br />
Equipment Room Attendant<br />
First Responder (Lifeguards, Facility<br />
Supervisors)<br />
Grounds keeper<br />
School of Nursing<br />
Athletics<br />
Campus Recreation<br />
Campus Cleaning<br />
Meadow Brook Hall<br />
<strong>Oakland</strong> Center<br />
Residence Halls<br />
Athletics<br />
Campus Recreation<br />
Athletics<br />
Campus Recreation<br />
Grounds Maintenance<br />
Meadow Brook Hall<br />
Department(s)<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 3 of 19<br />
Revised April 2004
TABLE 2<br />
Job Classifications for which ALL* employees Risk Occupational <strong>Exposure</strong><br />
Job Classification<br />
Department(s)<br />
Laboratory Compliance Manager (OEHS)<br />
Nursing Laboratory Manager<br />
Child Care Worker/Teacher<br />
Medical Assistant<br />
Nurse Practitioner<br />
Nurse, Registered<br />
Phlebotomist/Venipuncturist<br />
Physician<br />
Plumber<br />
Police Officer<br />
Student Intern<br />
Trainer<br />
Vehicle Maintenance Personnel<br />
All Sci and Res Depts.<br />
School of Nursing<br />
Lowry Child Care Center<br />
Graham Health Center<br />
School of Health Sciences (Med Lab Sci and Exer Sci)<br />
Graham Health Center<br />
Mechanical Maintenance<br />
Residence Halls<br />
Police Department<br />
Health Sciences (Med Lab and Exercise Sciences)<br />
School of Education<br />
School of Nursing<br />
Athletics<br />
Campus Recreation<br />
Grounds Maintenance Department<br />
* regardless of whether part- or full-time, permanent or temporary<br />
Table 3 below identifies those OU job classifications for which SOME employees who hold<br />
those positions risk occupational exposure to <strong>Bloodborne</strong> <strong>Pathogens</strong> (and some may not),<br />
without regard to the use of personal protective clothing and equipment:<br />
TABLE 3<br />
Job Classifications for Which SOME Employees Risk Occupational <strong>Exposure</strong><br />
Job Classification<br />
Department<br />
Directors, Managers and Supervisors All Departments listed in Table 1 (Section 2.0)<br />
“Laboratory” Personnel<br />
[Includes Faculty, Instructors (adjunct,<br />
associate, part-time, temporary or visiting), Lab<br />
Technicians, Researchers, Research Assistants,<br />
Research Technicians, PIs, Graduate Assistants,<br />
and Graduate Students]<br />
Biological Sciences<br />
Chemistry<br />
Eye Research Institute<br />
Health Sciences (Med Lab Sci and Exercise Sci)<br />
Laboratory Animal Management Services<br />
Student Employees<br />
Athletics<br />
Campus Recreation<br />
Residence Halls<br />
All laboratory sciences listed in box above<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 4 of 19<br />
Revised April 2004
4.0 METHODS OF CONTROLLING EXPOSURE TO BBPS<br />
4.1 Universal Precautions: All OU employees will utilize “Universal Precautions”:<br />
guidelines developed by the Center for Disease <strong>Control</strong> wherein all human blood or other<br />
potentially infectious body fluids are treated as if known to be infectious. A copy of<br />
these Universal Precautions is included in the Appendices of this document.<br />
4.2 Work Practice <strong>Control</strong>s: In addition to personal protective equipment and engineering<br />
controls, “work practice controls” will be used to prevent or minimize exposure to<br />
bloodborne pathogens. These include the following:<br />
• Following tasks which present exposure to BBPs, hands are always washed with soap<br />
and water immediately after removing personal protective equipment.<br />
• Following an “exposure incident” (i.e., unprotected skin or mucous membrane<br />
contact with human blood or other potentially infectious materials, OPIM), the<br />
exposed area is washed with soap and water (or, in the case eyes, flushed with an<br />
eyewash) for 15 minutes.<br />
• Contaminated needles are never recapped, but are placed instantly into sharps safes<br />
• Eating, drinking, smoking, applying cosmetics or lip balm, and/or handling contact<br />
lenses are prohibited in work areas where there is a reasonable likelihood of<br />
occupational exposure.<br />
• Food and drink shall never be kept in/on refrigerators, freezers, shelves, cabinets,<br />
counter-tops or benches where human blood or other OPIM are present.<br />
• All procedures involving blood or OPIM shall be performed in a manner as to<br />
minimize splashing, spraying, splattering, and generation of droplets.<br />
• Mouth pipetting/suctioning of blood or OPIM is prohibited.<br />
4.3 Engineering <strong>Control</strong>s<br />
4.3.1 Regulatory Overview: As of the April 18, 2001 amendments to the OSHA <strong>Bloodborne</strong><br />
<strong>Pathogens</strong> Standard (revised in conformance with the requirements of the “Needlestick<br />
Safety and Prevention Act”), the term “Engineering controls” is defined as those<br />
“appropriate, commercially available, and effective controls which isolate or remove the<br />
bloodborne pathogens hazard from the workplace”. Examples provided in the Standard<br />
include the following: 1) devices designed to reduce the risk of percutaneous exposure to<br />
bloodborne pathogens, such as blunt suture needles and plastic or mylar-wrapped glass<br />
capillary tubes; 2) safer medical devices such as sharps with engineered sharps injury<br />
protection or needleless systems; and 3) approved sharps disposal containers.<br />
These amendments further require OU to solicit input its employees responsible for<br />
direct patient care in the identification, evaluation, and selection of engineering (and<br />
work practice) controls; annually update its BBP <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong> to reflect the<br />
university has implemented any/all new developments in control technology; and<br />
establish and maintain a log of injuries from contaminated sharps (two types of log<br />
found in the Appendices of this document).<br />
4.3.2 Engineering and Personal Protective <strong>Control</strong>s used at OU: In accordance with the<br />
(original and more recent) engineering control requirements of the BBP Standard, and<br />
following several months of soliciting input from OU health care and lab research<br />
employees regarding selection of engineering controls, Table 4 below documents the<br />
specific tasks that present occupational exposure to BBPs on campus, and the associated<br />
engineering controls and personal protective equipment used in each unit on campus.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 5 of 19<br />
Revised April 2004
TABLE 4<br />
Tasks which May Present BBP <strong>Exposure</strong> and the PPE/Engineering Used to <strong>Control</strong><br />
(in alpha order by dept.)<br />
Department<br />
Tasks Which May Present<br />
Occupational <strong>Exposure</strong><br />
PPE and Engineering<br />
<strong>Control</strong>s Used<br />
Location of PPE and Engineering<br />
<strong>Control</strong>s<br />
Athletics<br />
First Aid, Lactate Testing, Uniform<br />
& towel handling/cleaning<br />
Sharps Safes, Gloves, Gggles,<br />
Biohaz bags/hampers.<br />
Training Room, Aquatic Operations<br />
Office, Equipment Room<br />
Biological Sciences<br />
Dissection of Human Eyes for<br />
Tissue Culture in 301 DHE, and<br />
Primary and SV40 Transformed<br />
Human Cells Lines used in Tissue<br />
Culture in 304B and 304C.<br />
Gloves, Masks, Goggles,<br />
Biohazard Bags and Hampers,<br />
Sharps Safes, Biohazard Signs<br />
(posted at entrances to labs),<br />
Biohazard Labels, Autoclave,<br />
and Lab coats<br />
Each and every laboratory that handles<br />
biohazardous agents contains these<br />
items (except for the autoclaves which<br />
are located centrally in 320 SEB and<br />
lab coats issued to employees)<br />
Campus Cleaning<br />
Restroom clean, trash removal, lab<br />
cleaning, GHC cleaning, cleaning<br />
up after injuries involving blood<br />
Gloves, Biohazard Bags/<br />
Hampers, Goggles, and Sharps<br />
Safes<br />
Campus Cleaning Supervisors’ Office,<br />
GHC, and Custodial Carts<br />
Campus Recreation<br />
First Aid, Lactate Testing, uniform<br />
& towel handling/cleaning, cleaning<br />
up after blood/OPIM incidents<br />
Gloves, Sharps Safes,<br />
Goggles, Biohazard<br />
Bags/Hampers<br />
Training Room, Aquatic Operations<br />
Office, Equipment Room<br />
Chemistry<br />
Purification of lymphocytes from<br />
blood of human volunteers in 208<br />
and 210 SEB.<br />
Gloves, Goggles, Sharps<br />
Safes, Gloved Laminar Flow<br />
Hood, Lab Coats, biohazard<br />
bags/boxes<br />
208 and 210 SEB (laminar flow hood<br />
in 210 SEB)<br />
Education, School of<br />
Student Interns assist with child<br />
injuries (e.g., first aid/CPR)<br />
As appropriate based on<br />
judgements of Host Facilities<br />
Host Facilities supply onsite<br />
Eye Research Institute<br />
Dissection of Human Eye Tissue<br />
and Culture in 427 DHE and<br />
Processing of Human Eye Tissue<br />
Cells in Room 419 DHE.<br />
Gloves, Goggles, Biosafety<br />
Cabinet, Biohazard<br />
Bags/Hampers, Biohazard<br />
Signs (posted at entrances to<br />
labs), Biohazard Labels<br />
Every laboratory that handles<br />
biohazardous agents contains these<br />
items<br />
Graham Health Center<br />
Drawing Blood, Handling Lab<br />
Specimens (e.g., blood, urine, etc.),<br />
Minor Office Surgeries, Office<br />
Procedures, Cleaning exam/trt rms.<br />
“BD Eclipse” blood collection<br />
needles”, Gloves, Masks,<br />
Sharps Safes, Biohazard<br />
Bags/Hampers, Goggles, Lab<br />
Coats, Gowns<br />
Exam/Treatment Rooms<br />
Grounds Maintenance<br />
-----------------------------<br />
Vehicle Maintenance<br />
Litter Pick-up, Trash Container Bag<br />
Removal, Trash Removal/<br />
--------------------------------------------<br />
Cleaning vehicles contaminated<br />
with blood or OPIM<br />
Gloves and Hand-held litter<br />
tool, Biohazard Bags/Hampers<br />
-------------------------------------<br />
Gloves, goggles<br />
BGM Building<br />
Health Sciences -<br />
Exercise Science<br />
CPR/First Aid performed by Student<br />
Interns at Host Facilities;<br />
venipuncture and finger-sticks<br />
performed in rm 207 HHS or<br />
occasionally in the field<br />
Hosts deem appropriate PPE<br />
for interns; PPE for VeniPunc<br />
includes “BD Eclipse” blood<br />
collection needles, gloves,<br />
sharp safes, goggles, lab coats<br />
and biohaz bags/hampers<br />
Host Facilities supply PPE onsite for<br />
interns; on-site PPE for venipuncture<br />
located in Room 207 HHS, or taken to<br />
field sites where tasks are being<br />
performed<br />
Health Sciences -<br />
Medical Laboratory<br />
Sciences<br />
Phlebotomy Instruction,<br />
Hematology Instruction, Clinical<br />
Analysis (instructional purposes),<br />
Washing lab glassware,<br />
Venipuncture and Urinalysis<br />
“BD Eclipse” blood collection<br />
needles, Gloves, Wrap-around<br />
Goggles, Biohazard<br />
Bags/Hampers, Biohazard<br />
Labels, Lab coats<br />
Phlebotomy Classrooms and carts, 310<br />
HHS and 373 HHS, and Lab coats<br />
issued to employees<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 6 of 19<br />
Revised April 2004
Department<br />
TABLE 4<br />
Tasks which May Present BBP <strong>Exposure</strong> and the PPE/Engineering Used to <strong>Control</strong><br />
(in alpha order by dept.)<br />
Tasks Which May Present<br />
Occupational <strong>Exposure</strong><br />
PPE and Engineering<br />
<strong>Control</strong>s Used<br />
Location of PPE and Engineering<br />
<strong>Control</strong>s<br />
Laboratory Animal<br />
Management Services<br />
(LAMS)<br />
Assisting med personnel using<br />
sharps (including surgery), handling<br />
infectious animals<br />
Gloves, Masks, Goggles,<br />
Biohazard Bags and Hampers,<br />
Sharps Safes, Biohazard Signs<br />
(posted at entrances to labs),<br />
Biohazard Labels, Autoclave,<br />
Bleach/Ethanol (for wiping<br />
down BSC2), and Lab coats<br />
Biomedical Research Support Facility<br />
Lowry Early Childhood<br />
Center<br />
First Aid, CPR, cleaning up blood,<br />
injections, and bites.<br />
Gloves, CPR Masks, Goggles,<br />
Biohazard Bags & Hampers,<br />
and Sharps Safes.<br />
Kitchen and Custodial Closet<br />
Meadow Brook Hall<br />
Cleaning Restrooms, Emptying<br />
Trash, Groundskeeping<br />
Gloves, Goggles, Sharps<br />
Safes, Biohazard<br />
Bags/Hampers<br />
Telephone Supply Room at MBH<br />
Mechanical Maint<br />
Plumbing and pipefitting in high<br />
risk areas (e.g., & restrms and labs)<br />
Gloves, Goggles<br />
Police and Support Services Bldg<br />
Nursing, School of<br />
Clinical Instruct and Patient care at<br />
off-site health care facilities<br />
Provided by off-site facilities<br />
Off-site<br />
<strong>Oakland</strong> Center<br />
Restroom clean, trash removal,<br />
Cleaning up after injuries involving<br />
blood, Trash Compaction<br />
Gloves, Masks, Goggles,<br />
Bleach, Biohazard<br />
Bags/Hampers, Sharps Safes<br />
OC Maintenance Shop and each<br />
custodial cart (except for hampers<br />
which are maintained in Shop)<br />
Police Department<br />
Accident Investigation, Treating<br />
Injured Persons, Processing Injured<br />
Victims or Injured Suspects, Subject<br />
or Vehicle Searches, Crime Scene<br />
Investigations, Evidence Processing,<br />
CPR/First Aid, Apprehending<br />
Suspects in High Risk Grps who are<br />
Resisting Arrest, Delivering Babies,<br />
Crowd <strong>Control</strong><br />
Gloves, Masks, Goggles,<br />
Biohazard Bags/Hampers,<br />
Sharps Safes, Biohazard<br />
Labels/Signs, CPR masks<br />
(with valves)<br />
Police Station and all Officer/Patrol<br />
Units have all of these items (except<br />
for biohazard labels and hampers,<br />
which are only located in the Station)<br />
Residence Halls Clean<br />
and Maintenance<br />
Trash Removal, Restroom Cleaning,<br />
Cleaning up after Injuries Involving<br />
Blood, Plumbing in high risk areas<br />
(e.g., & restrms and labs)<br />
Gloves, Biohazard Bags/<br />
Hampers, Goggles, Sharps<br />
Safes<br />
Custodial Carts and assigned rooms<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 7 of 19<br />
Revised April 2004
4.3.3 Rules Governing Engineering <strong>Control</strong>s and Personal Protective Equipment<br />
4.3.3.1 Selection: These responsible persons listed in Table 1 (Section 2.0) are required to<br />
consult with their staffs to identify what engineering controls and personal protection<br />
equipment are necessary on an ongoing basis through employee communication,<br />
observation and annual EH&S training sessions. EH&S will also help to ensure effective<br />
implementation of these recommendations.<br />
4.3.3.2 Maintenance: Sharps disposal containers are inspected, maintained and replaced by the<br />
responsible persons identified in Table 1 (Section 2.0) as needed to prevent overfilling.<br />
4.3.3.3 Training: Training in the use of the appropriate PPE for the tasks or procedures<br />
employees will perform is provided by the responsible persons (or their designees)<br />
identified in Table 1 (Section 2.0).<br />
4.3.3.4 All employees using PPE are required to observe the following precautions:<br />
• Wash hands immediately or as soon as feasible after removal of gloves or other PPE<br />
• Remove PPE after it becomes contaminated, and before leaving the work area<br />
• Used PPE may be disposed of in the red biohazard bags available in each department<br />
• Wear appropriate gloves when it can be reasonably anticipated that there may be hand<br />
contact with blood or OPIM, and when handling or touching contaminated items or<br />
surfaces; replace gloves if torn, punctured, contaminated, or if their ability to function<br />
as a barrier is compromised<br />
• Utility gloves may be decontaminated for reuse if their integrity is not compromised;<br />
discard utility gloves if they are cracking, peeling, tearing, puncturing, or deterioration<br />
• Never wash or decontaminate disposable gloves for reuse<br />
• Wear appropriate face and eye protection when splashes, sprays, spatters, or droplets<br />
of blood or OPIM pose a hazard to the eye, nose, or mouth<br />
• Remove immediately or as soon as feasible any garment contaminated by blood or<br />
OPIM, in such a way as to avoid contact with the outer surface<br />
4.3.3.5 Exceptions to Use: If an employee decides against using personal protective equipment<br />
under rare and extraordinary circumstances (e.g., would have prevented delivery of health<br />
care or public safety services, or would have posed increased hazard to safety of<br />
employee), the employee is required to complete a PPE Use Exception Form (found in<br />
the Appendices of this document) and submit it to his/her supervisor. This form is then<br />
carefully reviewed by the employee, his/her supervisor, and the Office of EH&S to<br />
determine whether changes could be instituted to prevent such occurrences in the future.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 8 of 19<br />
Revised April 2004
5.0 Biohazardous Waste<br />
5.1 Contaminated sharps are managed as follows:<br />
• Broken glassware which may be contaminated is picked up using mechanical means,<br />
such as a brush and dust pan.<br />
• All contaminated sharps are discarded immediately or as soon as possible into “Sharps<br />
Safes”, which are available in the locations identified in Table 4 (of this Section 5.0).<br />
5.2 Contaminated laundry is managed as follows:<br />
• Sent out to those laundry facilities in the area willing and able to handle Biohazardous<br />
laundry. The Graham Health Center or EH&S can provide the name(s) of current<br />
facilities who perform this function.<br />
• Placed in leak-proof, labeled or color-coded containers before transport. Biohazard<br />
bags and hampers are available in the locations identified in Table 4.<br />
• Handled as little as possible by OU employees, and never taken home for laundering.<br />
5.3 Biohazard Bags, Hampers and Sharps Safes containing biohazardous waste are...<br />
• Maintained upright at all times<br />
• Replaced routinely and not overfilled, and<br />
• Closed prior to removal to prevent spillage or protrusion of contents during handling<br />
• Transported to the Office of EH&S when full as follows:<br />
o An "OU Medical Waste Internal Tracking Form" (Print Shop - order<br />
#001623) shall be completed for each "drop-off" (regardless of the number of<br />
containers), and brought (with the waste) to the Office of Environmental<br />
Health and Safety, in the Graham Health Center.<br />
o An individual from the Office of Environmental Health and Safety will review<br />
the manifest, keep two copies, and issue the bearer a key to the Phoenix Cage<br />
(located in the basement of the Graham Health Center).<br />
o At the time of drop-off, departments may also pick up empty biohazard<br />
hampers and/or bags from the Phoenix Cage as needed. The Biohazard<br />
hampers and bags are available at no charge; sharp safes can be ordered from<br />
most custodial/safety suppliers.<br />
o Once every two weeks, Stericycycle® shall remove the hampers/sharp safes<br />
from the Phoenix Cage, and transport them first to the BFI Medical Treatment<br />
Center in Toledo, Ohio (for high-temperature decontamination), and then to<br />
the Vienna Junction Sanitary Landfill, in Erie Michigan, for land disposal as<br />
non-hazardous waste.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 9 of 19<br />
Revised April 2004
6.0 CONTAMINATED EQUIPMENT<br />
Responsible persons identified in Table 1 (Section 2.0) will ensure warning labels are affixed to,<br />
or red bags are used for, all biohazardous waste and/or contaminated equipment. If labels are<br />
not available in the department, the responsible person may contact the Office of Environmental<br />
Health and Safety for assistance in obtaining one.<br />
Employees are to notify their supervisors and/or the Office of Environmental Health and Safety<br />
if they discover regulated waste containers, refrigerators containing blood or OPIM,<br />
contaminated equipment, etc. without proper biohazard labels.<br />
7.0 CLEANING UP SPILLS<br />
7.1 Washable Surfaces: Contaminated equipment, floors, surrounding surfaces etc. shall be<br />
cleaned up (in such a manner that spreading, splashing, etc. the material is prevented)<br />
while wearing gloves and goggles, and using a ratio of ¼⎟2½ cups of bleach for every 1<br />
gallon of water, allowing10 minutes for disinfection to occur; after which any/all<br />
contaminated waste is placed in the proper biohazard receptacles. Broken glassware<br />
must be picked up using mechanical devices ONLY such as brush/dust pan, tongs,<br />
forceps, etc.<br />
7.2 Non-Washable Surfaces (e.g., carpets): Sanitary absorbent agents shall be used (e.g.,<br />
“Zgoop”), let dry, and area vacuumed. Germicidal carpet shampoo is then applied and<br />
the area vacuumed again. Broken glassware must be picked up using mechanical devices<br />
ONLY such as brush/dust pan, tongs, forceps, etc.<br />
8.0 HEPATITIS B VACCINATION<br />
Included in new employee and annual refresher BBP exposure control training will be<br />
comprehensive information regarding hepatitis B vaccinations, including its safety, benefits,<br />
efficacy, methods of administration, and availability at no cost to the employees. Training in this<br />
regard includes, but is not limited to, the following information:<br />
8.1 Pre-<strong>Exposure</strong> Vaccinations: The hepatitis B vaccination series shall be made available<br />
at no cost to all “eligible” employees in Tables 2 and 3 (i.e.,those employees for whom<br />
exposure to BBPs is a primary function of their job descriptions ), after training and<br />
within 10 days of initial assignment.<br />
8.1.1 Contraindications to Vaccination: Vaccinations are encouraged unless:<br />
1) documentation exists that the employee has previously received the series, 2) antibody<br />
testing (i.e., a “titer”) reveals that the employee is immune, or 3) medical evaluation<br />
shows that the vaccination is contraindicated.<br />
8.1.2 Declining the Vaccination: If an employee chooses to decline vaccination, the<br />
employee must sign a “Hepatitis B Declination Form” (blank form found in the<br />
Appendices of this document). Employees who decline may request and obtain the<br />
vaccination at a later date at no cost to themselves (assuming their occupational<br />
responsibilities continue to present risk of exposure). Declination Forms are kept in the<br />
OEHS. Vaccinations are provided at OU’s Graham Health Center or the employee’s<br />
facility of choice.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 10 of 19<br />
Revised April 2004
8.1.3 Health Care Professional Written Opinion: Prior to vaccination, the Health Care<br />
Professional shall provide a written opinion, indicating that (based on consultation) the<br />
employee presents no medical contra-indications to vaccination.<br />
8.2 Post-<strong>Exposure</strong> Vaccinations: For those employees for whom exposure to BBPs<br />
(generally via first-aid/CPR activities) is a collateral function of their job descriptions<br />
(e.g., coaches, trainers, day care professionals, etc.), the hepatitis B vaccination is not<br />
offered free of charge until AFTER these employees are involved in an incident where<br />
human blood or OPIM is present (regardless of whether an exposure incident occurred);<br />
these vaccinations are highly effective if administered within 1 to 7 days of the incident.<br />
9.0 EXPOSURE INCIDENT RESPONSE AND FOLLOW-UP<br />
9.1 <strong>Exposure</strong> incident - First Response<br />
Should an “exposure incident” occur (i.e., unprotected skin, eye or mucous membrane<br />
contact human blood or OPIM), the employee shall contact the responsible person<br />
identified in Table 1 (Section 2.0) from his/her department and/or the Officeof EH&S.<br />
Following IMMEDIATE first aid (cleaning the wound with soap and water, flushing eyes<br />
or other mucous membrane for 15 minutes), this person shall perform the following<br />
activities:<br />
• Ensure that employee goes to a hospital emergency room WITHIN 2 hours of the<br />
incident in order to obtain anti-viral drugs and baseline blood testing. NOTE: If the<br />
employee does not give consent for HIV serological testing during collection of blood<br />
for baseline testing, the baseline blood sample must be preserved for ∃ 90 days; if the<br />
exposed employee elects to have the baseline sample tested during this waiting<br />
period, testing shall be performed ASAP.<br />
• Ensure that, when it is convenient and reasonable, employee documents several<br />
pieces of critical information (preferably in time to show to treating physician), using<br />
OU’s <strong>Exposure</strong> Incident Report Form (found in the Appendices of this Document).<br />
This <strong>Exposure</strong> Incident Report Form requests the following information (and shall<br />
also be used by the Office of Environmental Health and Safety to evaluate the<br />
circumstances of the incident, generate ideas for prevention, modify the ECP, etc.):<br />
o engineering controls in use at the time<br />
o work practices followed<br />
o a description of the activity that preceded the exposure incident<br />
o protective equipment or clothing that was used at the time of the incident<br />
o location of the incident<br />
o procedure being performed when the incident occurred<br />
o route of exposure<br />
• Identify and document the source individual (unless the employer can establish that<br />
identification is infeasible or prohibited by state or local law).<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 11 of 19<br />
Revised April 2004
• Obtain consent (using a consent form found in the Appendices of this document) and<br />
make arrangements to have the source individual tested as soon as possible to<br />
determine HIV, HCV, and HBV infectivity; and document that the source individual's<br />
test results were conveyed to the employee's health care provider.<br />
• Ensure that the exposed employee is provided with the source individual's test results<br />
and with information about applicable disclosure laws and regulations concerning the<br />
identity and infectious status of the source individual (e.g., confidentiality laws).<br />
9.2 Post-<strong>Exposure</strong> Evaluation and Follow-up<br />
9.2.1 Supervisory Responsibilities: Responsible persons identified in Table 1 (Section 2.0)<br />
are required to ensure that any/all health care professionals responsible for follow-up care<br />
(following an exposure incident and initial testing/treatment) are provided:<br />
• A copy of the (completed) <strong>Exposure</strong> Incident Report Form;<br />
• A copy of OSHA’s <strong>Bloodborne</strong> <strong>Pathogens</strong> Standard;<br />
• Results of the source individual's blood test (when possible); and<br />
• Relevant employee medical records, including vaccination status.<br />
9.2.2 Written Opinions: The employee should then receive a copy of Health Care<br />
Professional(s) written opinion within 15 days after completion of the evaluation.<br />
9.2.3 Follow-up Care: Any/all follow-up testing, treatment, counseling, etc. shall be funded<br />
by <strong>Oakland</strong> <strong>University</strong> (department); employees shall bear none of the cost whatsoever.<br />
10.0 EMPLOYEE TRAINING<br />
10.1 When and How Often: All employees who have occupational exposure to bloodborne<br />
pathogens receive training before they conduct any activities which could pose exposure<br />
to BBPs, and annually thereafter.<br />
10.2 Who Conducts Training: BBP <strong>Exposure</strong> <strong>Control</strong> Training for new employees and<br />
annual refresher training is conducted by responsible persons identified in Table 1<br />
(Section 2.0) or a qualified designee(s). These “trainers” were all trained and examined<br />
by representatives of Environmental Health and Safety (or a qualified designee), and<br />
have had a reasonable amount of hands-on experience understanding, applying and<br />
implementing the OSHA BBP Standard.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 12 of 19<br />
Revised April 2004
10.3 Elements of Training: Included in the training is/are the epidemiology, symptoms, and<br />
transmission of bloodborne pathogen diseases. In addition, the training program covers,<br />
at a minimum, the following elements:<br />
• copy and explanation of the standard<br />
• detailed information on HBV, HCV and HIV (signs, symptoms, treatments, etc.)<br />
• explanation of OU’s ECP and how to obtain a copy<br />
• explanation of methods to recognize tasks and other activities that may involve<br />
exposure to blood and OPIM, including what constitutes an exposure incident<br />
• explanation of the use/limitations of engineering controls, work practices and PPE<br />
• explanation of the types, uses, location, removal, handling, decontamination, and<br />
disposal of PPE<br />
• explanation of the basis for PPE selection<br />
• information on the hepatitis B vaccine, including information on its efficacy, safety,<br />
method of administration, benefits of being vaccinated, and that the vaccine will be<br />
offered free of charge<br />
• information on the appropriate actions to take and persons to contact in an emergency<br />
involving blood or OPIM<br />
• explanation of the procedure to follow if an exposure incident occurs<br />
• information on the post-exposure evaluation and follow-up that the employer is<br />
required to provide for the employee following an exposure incident<br />
• explanation of signs, labels and color coding required by the standard and used at OU<br />
• an opportunity for interactive questions and answers with the trainer.<br />
11.0 RECORD KEEPING<br />
11.1 Training Records: Training records are completed for each employee upon completion<br />
of training. These documents will be kept for at least three years in the Office of<br />
Environmental Health and Safety. Training records include for each employee a<br />
Declaration Form which documents the following:<br />
• the employee name<br />
• the date of the training sessions<br />
• the contents or a summary of the training sessions<br />
• the name and qualifications of persons conducting the training<br />
• whether the employee accepted or declined the Hep B vaccination (separate Hep B<br />
Declination Form provided to all who decline).<br />
Employee training records are provided upon request to the employee or the employee's<br />
authorized representative within 15 working days. Such requests should be addressed to<br />
the Office of Environmental Health and Safety.<br />
11.2 Medical Records: Medical records are maintained for each employee with occupational<br />
exposure in accordance with 29 CFR 1910.20, "Access to Employee <strong>Exposure</strong> and<br />
Medical Records." OU’s Human Resources Department is responsible for maintenance of<br />
the required medical records for at least the duration of employment plus 30 years.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 13 of 19<br />
Revised April 2004
11.3 <strong>Exposure</strong> Incident Evaluation Records: Once an exposure incident (and the associated<br />
<strong>Exposure</strong> Incident Report Form) has been evaluated, and any Program modifications put<br />
into place, these records are maintained in the Office of Environmental Health and<br />
Safety.<br />
12.0 CONDITIONS FOR LABS WORKING WITH HIV AND HEPATITIS VIRUSES<br />
12.1 Working in HIV and Hepatitis Virus "production facilities".<br />
"Production facility" is defined by OSHA as a facility engaged in industrial-scale, largevolume<br />
or high concentration production of HIV or Hepatitis Viruses. These activities<br />
are not currently (as of this July 2000 printing) permitted at OU.<br />
12.2 Working in HIV and Hepatitis Virus “Research Laboratories” (i.e., laboratories “engaged<br />
in the culture, production, concentration, experimentation and manipulation of HIV or<br />
Hepatitis Viruses”. Does NOT apply to clinical or diagnostic laboratories engaged solely<br />
in the analysis of blood, tissues or organs).<br />
12.2.1 Minimum Requirements for laboratories engaging in HIV or Hepatitis Virus Research<br />
• Each laboratory shall contain a facility for hand washing and an eye wash facility<br />
which is readily available within the work area.<br />
• An autoclave for decontamination of regulated waste shall be available.<br />
• All regulated waste shall either be incinerated or decontaminated by a method such as<br />
autoclaving known to effectively destroy bloodborne pathogens.<br />
12.2.2 Special Practices<br />
• Lab doors shall be kept closed when work involving HIV, HBV or HCV is in progress.<br />
• Contaminated materials that are to be decontaminated at a site away from the work<br />
area shall be placed in a durable, leakproof, labeled or color-coded container that is<br />
closed before being removed form the work area.<br />
• Access to the work area shall be limited to authorized persons. Written policies and<br />
procedures shall be established whereby only persons who have been advised of the<br />
potential biohazard, who meet any specific entry requirements, and who comply with<br />
all entry and exit procedures shall be allowed to enter the work areas.<br />
• When other potentially infectious materials or infected animals are present in the work<br />
area or containment module, a hazard warning sign incorporating the universal<br />
biohazard symbol shall be posted on all access doors.<br />
• All activities involving other potentially infectious materials shall be conducted in<br />
biological safety cabinets or other physical-containment devices within the<br />
containment module; never on the open bench.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 14 of 19<br />
Revised April 2004
• Laboratory coats, gown, smocks, uniforms, or other appropriate protective clothing<br />
shall be used in the work area and animals rooms. Protective clothing shall not be<br />
worn outside of the work area and shall be decontaminated before being laundered.<br />
• Special care shall be taken to avoid skin or mucous membrane contact with other<br />
potentially infectious materials - Use gloves and goggles.<br />
• Before disposal, all waste from work areas and from animals rooms shall be<br />
decontaminated by a method, e.g., autoclaving, known to effectively destroy BBPs.<br />
• Vacuum lines shall be protected with liquid disinfectant traps and high efficiency<br />
particulate air (HEPA) filters or filters of equivalent or superior efficiency and which<br />
are checked routinely and maintained or replaced as necessary.<br />
• Hypodermic needles and syringes shall be used only for parenteral injection and<br />
aspiration of fluids from laboratory animals and diaphragm bottles. Only needlelocking<br />
syringes or disposable syringe-needle units shall be used for the injection or<br />
aspiration of other potentially infectious materials.<br />
• Extreme caution shall be used when handling needles and syringes. A needle shall not<br />
be bent, sheared, replaced in the sheath or guard, or removed from the syringe<br />
following use. The needle and syringe shall be promptly placed in a puncture-resistant<br />
container and autoclaved or decontaminated before reuse or disposal.<br />
• All spills shall be immediately contained and cleaned up by professional staff properly<br />
trained/equipped to handle potentially concentrated infectious materials.<br />
• A spill or accident that results in an exposure incident shall be immediately reported to<br />
the laboratory director or other responsible person.<br />
• Employees are required to reference the <strong>Oakland</strong> <strong>University</strong> Biosafety Manual for<br />
instructions on practices and procedures for work with HIV or Hepatitis viruses, and<br />
follow these procedures. Additionally, an application for use with any infectious<br />
agents (excluding clinical or diagnostic laboratories engaged solely in the analysis of<br />
blood, tissues or organs) must be submitted to the <strong>Oakland</strong> <strong>University</strong> Biosafety<br />
Committee; and activities may not commence until the Committee has approved the<br />
research activities in writing.<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP<br />
Page 15 of 19<br />
Revised April 2004
12.2.3 Signs<br />
The PI or laboratory supervisor shall complete and post the following sign(s) (available<br />
in the Office of EH&S) at the entrance to all HIV and/or Hepatitis virus research labs:<br />
12.2.4 Containment Equipment<br />
• Certified biological safety cabinets (Class I, II, or III) or other appropriate<br />
combinations of personal protection or physical containment devices, such as special<br />
protective clothing, respirators, centrifuge safety cups, sealed centrifuge rotors, and<br />
containment caging for animals, shall be used for all activities with OPIM that pose a<br />
threat of exposure to droplets, splashes, spills or aerosols.<br />
• Biological safety cabinets shall be certified upon installation, whenever they are<br />
moved and at least annually.<br />
12.2.5 Training Requirements.<br />
• Additional initial training for employees in HIV, HBV or HBC research laboratories<br />
shall receive the following initial training in addition to the general training described<br />
in Section 11.0.<br />
• Employees must demonstrate proficiency in standard microbiological practices and<br />
techniques and operations specific to the facility before being allowed to work with<br />
HIV, HBV or HBC.<br />
• Employees must have prior experience in the handling of human pathogens or tissue<br />
cultures before working with HIV, HBV or HCV, or ...<br />
• Employees (through their supervisors, the OEHS or the OGCSR) must arrange for a<br />
training program if/when they have no prior experience in handling human pathogens.<br />
Initial work activities shall not include the handling of infectious agents. A<br />
progression of work activities shall be assigned as techniques are learned and<br />
proficiency is developed. Employees may not participate in work activities involving<br />
infectious agents until proficiency has been demonstrated.
APPENDICES<br />
BLANK FORMS:<br />
• Sharps Injury Log (Type I for Non-Laboratories)<br />
• Sharps Injury Log (Type II for Laboratories)<br />
• Training and Hep B Declaration Form<br />
• Hep B Declination Form<br />
• Hepatitis B Vaccination - Status Form<br />
• <strong>Exposure</strong> Incident Report Form<br />
• Post-<strong>Exposure</strong> Incident Checklist<br />
• Sharps Injury Log (Type I)<br />
• Sharps Injury Log (Type II)<br />
• Blood Draw Consensus Form - Source Individual<br />
• PPE Exception Form<br />
• Research Activities Involving Direct Manipulation of <strong>Bloodborne</strong> <strong>Pathogens</strong> - Report<br />
Form<br />
COMPLETED FORMS (WHERE APPLICABLE - DEPT. SPECIFIC):<br />
• Pre-exposure Hepatitis B Vaccination - Status Form<br />
• Completed Hepatitis B Declaration/Declination Forms<br />
• <strong>Exposure</strong> Incident Report Form<br />
• Post-<strong>Exposure</strong> Incident Checklist<br />
• Blood Draw Consensus Form - Source Individual<br />
• PPE Exception Form<br />
• Research Activities Involving Direct Manipulation of <strong>Bloodborne</strong> <strong>Pathogens</strong> - Report<br />
Form<br />
UNIVERSAL PRECAUTIONS<br />
OSHA BLOODBORNE PATHOGENS STANDARD<br />
<strong>Oakland</strong> <strong>University</strong> BBP ECP Revised April 2004
<strong>Oakland</strong> <strong>University</strong><br />
Graham Health Center<br />
Sharps Injury Log<br />
Page _____<br />
Date of<br />
Incident<br />
Name of Injured<br />
Job Title of<br />
Injured<br />
Type of Needle<br />
Involved<br />
Describe how<br />
Needle stick<br />
Occurred<br />
Steps taken<br />
Immediately<br />
After Stick<br />
Steps taken to<br />
Avoid Future<br />
Needle sticks
Training Date<br />
BBP TRAINING AND HBV VACCINATION DECLARATION FORM<br />
<strong>Oakland</strong> <strong>University</strong><br />
Department ____________________________________<br />
Name Job Classification __________________________<br />
TRAINING: I hereby certify that I have received training in bloodborne pathogens exposure control. This<br />
training included providing me a copy of the BBP <strong>Exposure</strong> <strong>Control</strong> Standard, and an explanation of the<br />
following: OU’s <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong> and how to obtain a copy; details regarding transmission, signs, symptoms<br />
and prognoses of common BBP viruses (i.e., HBV, HCV and HIV); common methods to recognize tasks and other<br />
activities that may involve exposure to blood and OPIM, including what constitutes an exposure incident, the use<br />
and limitations of engineering controls, work practices and personal protective equipment (PPE); the types, uses,<br />
location, removal, handling, decontamination and disposal of PPE; the basis for PPE selection; the hepatitis b<br />
vaccine, including information on its efficacy, safety, method of administration, the benefits of being vaccinated,<br />
and that the vaccine is offered free of charge under certain circumstances; the appropriate actions to take and<br />
persons to contact in an emergency involving blood or OPIM; the procedure to follow if an exposure incident<br />
occurs, including the method of reporting the incident and the medical follow-up that will be made available;<br />
information on the post-exposure evaluation and follow-up that OU is required to provide me following an<br />
exposure incident; the signs and labels and/or color-coding required by the BBP Standard and OU. I further<br />
certify that I was provided ample opportunity for interactive questions and answers with the person(s)<br />
conducting the training session.<br />
The training was provided to me by “qualified” personnel as follows: General information regarding BBP<br />
viruses and exposure control was provided to me by OU’s Office of Environmental Health and Safety, either in<br />
person or via a handout generated by the Officeof EH&S and provided me by my supervisor. This EH&S training<br />
staff has had extensive formal training in, and experience with, interpreting and implementing the BBP Standard,<br />
and designing and providing training in this area. Site-specific information, regarding BBP exposure control in my<br />
department as it relates to the occupational activities I perform, was subsequently provided me by my supervisor<br />
(who received his/her guidance, training and handouts directly from the Office of EH&S).<br />
HEPATITIS B VACCINATION: While the HBV vaccine is well tolerated by most people, and provides<br />
significant protection against acquiring HBV-related illnesses, vaccination has some inherent risks (including, but<br />
not limited to, swelling, reddening, post injection soreness, body fatigue, headache, muscle or joint soreness), as<br />
well as some medical contra-indications (including, but not limited to, high blood pressure, allergies to yeast/mold,<br />
pregnancy), so I understand that my health care professional (in conference with myself) shall decide and document<br />
whether it is safe for me to obtain the HBV vaccination.<br />
I have read each option below and understand each of them. I have selected ONE option by placing a Τ. I also<br />
understand that I may change my mind at any time. Finally, if I select Option 2. below, I understand that I<br />
must also complete a SEPARATE Hepatitis b Declination form.<br />
1. ______ I would like to have OU pay for my HBV vaccination series; I understand that MIOSHA requires me<br />
to begin the immunization process within 10 calendar days of accepting this vaccination.<br />
2. ______I decline to have OU pay for my HBV vaccinations because (place a Τ in appropriate blank below).<br />
________ a) I have already been immunized;<br />
OR<br />
________ b) I would like OU to pay for the antibody test (i.e., “titer”) performed before deciding;<br />
OR<br />
________ c) cost of said immunization is 100% funded by another source (e.g., medical insurance); OR<br />
I understand that if I select this Option, I must also complete a separate Hepatitis B Declination Form<br />
_<br />
3. _____ Based on my OU job classification (identified above), my “PRIMARY” occupational duties do not<br />
present “reasonably anticipated exposure to blood or OPIM”, and I am therefore not eligible to receive “preexposure”<br />
hepatitis b vaccination funding. I understand, however, that should I be involved in any<br />
occupational incident that involves human blood or OPIM (regardless of whether “exposure” occurs), I am<br />
then eligible to receive (at no cost) an accelerated series of hepatitis b vaccinations, which should begin<br />
within 24 hours, but up to 7 calendar days, after the incident. Note: Those who are required, encouraged<br />
and/or allowed to provide first-aid on campus as a “collateral” job responsibility (for example, athletic<br />
coaches) would select this Option.<br />
SIGNED:<br />
DATE: ______________<br />
[Requires signature of Legal Guardian if under age 18 - print words “legal guardian” next to signature if applicable]
BBP TRAINING AND HBV VACCINATION DECLARATION FORM<br />
<strong>Oakland</strong> <strong>University</strong> - School of Nursing<br />
Training Date Name __________________________________<br />
TRAINING: I hereby certify that I have received training in bloodborne pathogens exposure control. This training included<br />
providing me a copy of the BBP <strong>Exposure</strong> <strong>Control</strong> Standard, and an explanation of the following: OU’s <strong>Exposure</strong> <strong>Control</strong><br />
<strong>Plan</strong> and how to obtain a copy; details regarding transmission, signs, symptoms and prognoses of common BBP viruses (i.e.,<br />
HBV, HCV and HIV); common methods to recognize tasks and other activities that may involve exposure to blood and OPIM,<br />
including what constitutes an exposure incident, the use and limitations of engineering controls, work practices and personal<br />
protective equipment (PPE); the types, uses, location, removal, handling, decontamination and disposal of PPE; the basis for<br />
PPE selection; the hepatitis b vaccine, including information on its efficacy, safety, method of administration, the benefits of<br />
being vaccinated, and that the vaccine is offered free of charge under certain circumstances; the appropriate actions to take and<br />
persons to contact in an emergency involving blood or OPIM; the procedure to follow if an exposure incident occurs, including<br />
the method of reporting the incident and the medical follow-up that will be made available; information on the post-exposure<br />
evaluation and follow-up that OU is required to provide me following an exposure incident; the signs and labels and/or colorcoding<br />
required by the BBP Standard and OU. I further certify that I was provided ample opportunity for interactive questions<br />
and answers with the person(s) conducting the training session.<br />
The training was provided to me by “qualified” personnel as follows: General information regarding the BBP <strong>Exposure</strong><br />
<strong>Control</strong> Standard, transmission and signs/symptoms of common BBP Viruses (e.g., HBV, HCV and HIV) was provided to me by<br />
either in person, and/or via live instruction, video-tape, or handout, by a Nursing Department faculty member (in conjunction<br />
with OU’s Office of Environmental Health and Safety). The Office of EH&S training staff has had extensive formal training in,<br />
and experience with, interpreting and implementing the BBP Standard; likewise Nursing Department faculty members, based on<br />
the nature of their nursing educations, are naturally well versed in BBP <strong>Exposure</strong> <strong>Control</strong>s. I further understand that the<br />
responsibility for site-specific training (as it relates to the actual duties I perform at my site(s) of employment) is/was the<br />
responsibility of similarly qualified nursing administrators/supervisors at the facilities at which I perform these duties.<br />
HEPATITIS B VACCINATION: While the HBV vaccine is well tolerated by most people, and provides significant protection<br />
against acquiring HBV-related illnesses, vaccination has some inherent risks (including, but not limited to, swelling, reddening,<br />
post injection soreness, body fatigue, headache, muscle or joint soreness), as well as some medical contra-indications (including,<br />
but not limited to, high blood pressure, allergies to yeast/mold, pregnancy), so I understand that my health care professional (in<br />
conference with myself) shall decide and document whether it is safe for me to obtain the HBV vaccination.<br />
I have read each option below and understand each of them. I have selected ONE option by placing a Τ. I also understand that<br />
I may change my mind at any time. Finally, if I select Option 2. below, I understand that I must also complete a<br />
SEPARATE “Hepatitis b Declination Form”.<br />
1. ____I would like to have OU pay for my HBV vaccination series; I understand that MIOSHA requires me to begin the<br />
immunization process within 10 calendar days of accepting this vaccination series.<br />
2. _____I decline to have OU pay for my HBV vaccinations because (place a Τ in appropriate blank below).<br />
_____ a) I have already been immunized; OR<br />
_____ b) I would like OU to pay for the antibody test (i.e., “titer”) performed before deciding; OR<br />
_____ c) cost of said immunization is 100% funded by another source (e.g., medical insurance); OR<br />
_____ d) personal reasons<br />
I understand that if I select Option 2., I must also complete a separate Hepatitis B Declination Form:<br />
3. ______Based on my OU job classification (identified below), my occupational duties do not present “reasonably anticipated<br />
exposure to blood or OPIM”, and I am therefore not eligible to receive “pre-exposure” hepatitis b vaccination funding. I<br />
understand, however, that should I be involved in any occupational incident that involves human blood or OPIM (regardless<br />
of whether “exposure” occurs), I am then eligible to receive an accelerated series of hepatitis b vaccinations, which should<br />
begin within 24 hours (but up to 7 days) after the incident.<br />
SIGNED:<br />
Job Classification [PLEASE CHECK ONE]:<br />
_____ Learning Resources Lab Instructor<br />
_____ Clinical Instructor<br />
_____ Other (specify here) ________________________________<br />
DATE: ______________________________
HBV VACCINATION DECLINATION FORM<br />
I understand that, due to my occupational exposure to blood or other potentially infectious<br />
materials, I may be at risk of acquiring hepatitis B virus (HBV) infection. I have been given<br />
the opportunity to be vaccinated with hepatitis B vaccine, at no charge to myself. However, I<br />
decline hepatitis B vaccination at this time. I understand that my declining this vaccine, I<br />
continue to be at risk of acquiring hepatitis B, a serious disease. If in the future I continue to<br />
have occupational exposure to blood or other potentially infectious materials (OPIM) and I<br />
want to be vaccinated with hepatitis B vaccine, I can receive the vaccination series at no<br />
charge to me.<br />
Name (printed) ______________________________________<br />
Department _________________________________________<br />
Job Classification ____________________________________<br />
Signature ____________________________________________________________________________<br />
[Requires signature of Legal Guardian if under age 18 - print words “legal guardian” next to signature if applicable]<br />
Social Security Number (REQUIRED BY MIOSHA) __________________________<br />
[Wording direct from 29 CFR’s Appendix to Section 1910.1030-Hepatitis B Vaccine Declination (Mandatory)]
"PRE-EXPOSURE" HEPATITIS B VACCINATION<br />
STATUS FORM<br />
Department ______________________________________________________<br />
ELIGIBLE<br />
EMPLOYEE<br />
NAME<br />
ACCEPTED/<br />
DECLINED<br />
VACCINATION<br />
and DATE DECIDED<br />
DATES<br />
VACCINE<br />
RECEIVED<br />
#1/#2/#3<br />
ADMINISTERING<br />
HEALTH<br />
CARE FACILITY
EXPOSURE INCIDENT REPORT FORM<br />
Date of Incident<br />
Job site/location:<br />
Time of Incident _________________________<br />
Name of Employee____________________________<br />
Job Description (Description of General Duties): ________________________________________<br />
Potentially Infectious Material Involved (e.g. blood etc.) _________________________________<br />
Source of Potentially Infectious Material (e.g. needle-stick, cut, bite etc.) ____________________<br />
Circumstances Surrounding <strong>Exposure</strong> Incident (e.g. work being performed etc.) _______________<br />
_______________________________________________________________________________<br />
Route of <strong>Exposure</strong> (e.g. under-the-skin, unprotected skin, eyes, nose, mouth) _________________<br />
_______________________________________________________________________________<br />
How <strong>Exposure</strong> Occurred (e.g. equipment malfunction, human error, etc.) ____________________<br />
_______________________________________________________________________________<br />
Personal Protection Equipment Worn at Time of Incident ________________________________<br />
_______________________________________________________________________________<br />
_______________________________________________________________________________<br />
Actions Taken at Time of Incident (e.g. soap/water clean-up, reporting to supervisor etc.)<br />
_______________________________________________________________________________<br />
_______________________________________________________________________________<br />
_______________________________________________________________________________<br />
Recommendations for Avoiding Repetition: ___________________________________________<br />
_______________________________________________________________________________<br />
_______________________________________________________________________________
POST-EXPOSURE INCIDENT CHECKLIST<br />
The following steps must be taken, and information provided, in the event of an employee's exposure to<br />
blood or other potentially infectious material.<br />
Date of <strong>Exposure</strong> Incident _______________________________<br />
ACTIVITY<br />
• Contaminated area was washed with soap and water (or eyewash if the eye) for<br />
at least 15 minutes.<br />
• Employee transported to emergency room within 2 hours of incident for antiviral<br />
drugs (following washing/flushing described above).<br />
• Employee furnished with documentation regarding exposure incident.<br />
• The following documentation was forwarded to a Healthcare Professional who<br />
is evaluating employee:<br />
o <strong>Bloodborne</strong> <strong>Pathogens</strong> Standard<br />
o <strong>Exposure</strong> Incident Report<br />
o Employee’s medical records<br />
COMPLETION<br />
____________<br />
____________<br />
____________<br />
____________<br />
____________<br />
____________<br />
• Source Individual:<br />
o Identified OR it was determined that ID was not feasible (circle one)<br />
o Authorization to collect blood requested<br />
o Blood tested OR authorization refused (circle one)<br />
____________<br />
____________<br />
____________<br />
• Source individual’s blood results given to exposed employee ____________<br />
• Employee informed than any/all follow-up care shall be at no cost to him/her ____________
Authorization to Have Blood Drawn and<br />
Analyzed for Presence of Viral Infection<br />
Source Individual Consent Form<br />
1. Individual's Name<br />
Social Security Number<br />
Date of Birth<br />
2. I authorize_______________________(Name of Health Care Facility) to draw and analyze my blood<br />
for the presence of viral (i.e., HBV or HIV) infection.<br />
3. I understand that the results of this analysis shall be made available to the individual who has been<br />
exposed to my blood (in addition to his/her health care provider), and maintained in that individual's<br />
CONFIDENTIAL medical records on file at OU.<br />
4. I agree that a photocopy or facsimile of this authorization shall be as valid as the original.<br />
__________________________________________________<br />
Signed (source individual)<br />
_________________________<br />
Date<br />
____________________________________________________<br />
Parent or guardian (if individual is under 18 years of age)<br />
_________________________<br />
Date
PPE EXCEPTION FORM<br />
Name of Individual Completing Form<br />
On (date) __________________________ I voluntarily and knowingly chose against wearing<br />
Personal Protective Equipment (PPE) even though I was aware that the task I was performing<br />
introduced a risk of exposure to <strong>Bloodborne</strong> <strong>Pathogens</strong>.<br />
In my judgement, in this specific instance, obtaining/using PPE would have (check one):<br />
_____ prevented the delivery of health care or public safety services;<br />
_____ posed an increased hazard to the safety of a victim, myself or coworker(s); or<br />
______ other, explain in next paragraph.<br />
Description of task I was performing, and detailed reason for choosing against PPE:<br />
______________________________________________________________________________________<br />
__________________________________________________________________________________<br />
Suggestions for avoiding this situation in the future:<br />
_________________________________________________________________________________<br />
_________________________________________________________________________________<br />
Signed<br />
Co-Signed Employee Supervisor<br />
Date<br />
Date
RESEARCH ACTIVITIES INVOLVING DIRECT MANIPULATION OF<br />
BLOODBORNE PATHOGENS<br />
REPORT FORM<br />
Department:<br />
“MANIPULATION”<br />
PROCEDURE(S)<br />
(e.g. assay, culture,<br />
centrifuge, etc.)<br />
BLOODBORNE<br />
PATHOGENS<br />
BEING MANIPULATED<br />
LOCATION(S)<br />
PERFORMED<br />
REC’D OU<br />
BIOSAFETY<br />
COMMITTEE<br />
APPROVAL<br />
(Date and PI<br />
signature)<br />
* “Manipulation” includes, but is not limited to, culturing, assaying, centrifuging, handling, pipetting<br />
etc. of infectious organisms carried in human blood.
"UNIVERSAL”<br />
BLOOD AND BODY FLUID<br />
PRECAUTIONS<br />
+<br />
OSHA BLOODBORNE PATHOGEN<br />
STANDARD<br />
[29 CFR 1910.1030]
Page 31 of 19
OSHA Regulations (Standards - 29 CFR)<br />
<strong>Bloodborne</strong> <strong>Pathogens</strong>. - 1910.1030<br />
Standard Number: 1910.1030<br />
Standard Title: <strong>Bloodborne</strong><br />
pathogens.<br />
SubPart Number: Z<br />
SubPart Title: Toxic and Hazardous<br />
Substances<br />
(a) Scope and Application. This<br />
section applies to all occupational<br />
exposure to blood or other potentially<br />
infectious materials as defined by<br />
paragraph (b) of this section.<br />
(b) Definitions. For purposes of this<br />
section, the following shall apply:<br />
"Assistant Secretary" means the<br />
Assistant Secretary of Labor for<br />
Occupational Safety and Health, or<br />
designated representative.<br />
"Blood" means human blood, human<br />
blood components, and products made<br />
from human blood.<br />
"<strong>Bloodborne</strong> <strong>Pathogens</strong>" means<br />
pathogenic microorganisms that are<br />
present in human blood and can cause<br />
disease in humans. These pathogens<br />
include, but are not limited to,<br />
hepatitis B virus (HBV) and human<br />
immunodeficiency virus (HIV).<br />
"Clinical Laboratory" means a<br />
workplace where diagnostic or other<br />
screening procedures are performed<br />
on blood or other potentially<br />
infectious materials.<br />
"Contaminated" means the presence<br />
or the reasonably anticipated presence<br />
of blood or other potentially infectious<br />
materials on an item or surface.<br />
"Contaminated Laundry" means<br />
laundry which has been soiled with<br />
blood or other potentially infectious<br />
materials or may contain sharps.<br />
"Contaminated Sharps" means any<br />
contaminated object that can penetrate<br />
the skin including, but not limited to,<br />
needles, scalpels, broken glass, broken<br />
capillary tubes, and exposed ends of<br />
dental wires.<br />
"Decontamination" means the use of<br />
physical or chemical means to<br />
remove, inactivate, or destroy<br />
"Source Individual" means any<br />
individual, living or dead, whose<br />
blood or other potentially infectious<br />
materials may be a source of<br />
occupational exposure to the<br />
bloodborne pathogens on a surface<br />
or item to the point where they are<br />
no longer capable of transmitting<br />
infectious particles and the surface<br />
or item is rendered safe for<br />
handling, use, or disposal.<br />
"Director" means the Director of<br />
the National Institute for<br />
Occupational Safety and Health,<br />
U.S. Department of Health and<br />
Human Services, or designated<br />
representative.<br />
"Engineering <strong>Control</strong>s" means<br />
controls (e.g., sharps disposal<br />
containers, self-sheathing needles)<br />
that isolate or remove the<br />
bloodborne pathogens hazard from<br />
the workplace.<br />
"<strong>Exposure</strong> Incident" means a<br />
specific eye, mouth, other mucous<br />
membrane, non-intact skin, or<br />
parenteral contact with blood or<br />
other potentially infectious<br />
materials that results from the<br />
performance of an employee's<br />
duties.<br />
"Handwashing Facilities" means a<br />
facility providing an adequate<br />
supply of running potable water,<br />
soap and single use towels or hot<br />
air drying machines.<br />
"Licensed Healthcare<br />
Professional" is a person whose<br />
legally permitted scope of practice<br />
allows him or her to independently<br />
perform the activities required by<br />
paragraph (f) Hepatitis B<br />
Vaccination and Post-exposure<br />
Evaluation and Follow-up.<br />
"HBV" means hepatitis B virus.<br />
"HIV" means human<br />
immunodeficiency virus.<br />
"Occupational <strong>Exposure</strong>" means<br />
reasonably anticipated skin, eye,<br />
mucous membrane, or parenteral<br />
contact with blood or other<br />
potentially infectious materials that<br />
may result from the performance of<br />
an employee's duties.<br />
employee. Examples include, but<br />
are not limited to, hospital and<br />
clinic patients; clients in<br />
institutions for the developmentally<br />
disabled; trauma victims; clients of<br />
"Other Potentially Infectious Materials"<br />
(OPIM) means (1) The following human<br />
body fluids: semen, vaginal secretions,<br />
cerebrospinal fluid, synovial fluid, pleural<br />
fluid, pericardial fluid, peritoneal fluid,<br />
amniotic fluid, saliva in dental procedures,<br />
any body fluid that is visibly contaminated<br />
with blood, and all body fluids in<br />
situations where it is difficult or<br />
impossible to differentiate between body<br />
fluids; (2) Any unfixed tissue or organ<br />
(other than intact skin) from a human<br />
(living or dead); and (3) HIV-containing<br />
cell or tissue cultures, organ cultures, and<br />
HIV- or HBV-containing culture medium<br />
or other solutions; and blood, organs, or<br />
other tissues from experimental animals<br />
infected with HIV or HBV.<br />
"Parenteral" means piercing mucous<br />
membranes or the skin barrier through<br />
such events as needlesticks, human bites,<br />
cuts, and abrasions.<br />
"Personal Protective Equipment" is<br />
specialized clothing or equipment worn by<br />
an employee for protection against a<br />
hazard. General work clothes (e.g.,<br />
uniforms, pants, shirts or blouses) not<br />
intended to function as protection against a<br />
hazard are not considered to be personal<br />
protective equipment.<br />
"Production Facility" means a facility<br />
engaged in industrial-scale, large-volume<br />
or high concen. produc. of HIV or HBV.<br />
"Regulated Waste" means liquid or semiliquid<br />
blood or other potentially infectious<br />
materials; contaminated items that would<br />
release blood or other potentially<br />
infectious materials in a liquid or semiliquid<br />
state if compressed; items that are<br />
caked with dried blood or other potentially<br />
infectious materials and are capable of<br />
releasing these materials during handling;<br />
contaminated sharps; and pathological and<br />
microbiological wastes containing blood or<br />
other potentially infectious materials.<br />
"Research Laboratory" means a laboratory<br />
producing or using research-laboratoryscale<br />
amounts of HIV or HBV. Research<br />
laboratories may produce high<br />
concentrations of HIV or HBV but not in<br />
the volume found in production facilities.<br />
drug and alcohol treatment facilities;<br />
residents of hospices and nursing homes;<br />
human remains; and individuals who<br />
donate or sell blood or blood components.
"Sterilize" means the use of a physical<br />
or chemical procedure to destroy all<br />
microbial life including highly<br />
resistant bacterial endospores.<br />
"Universal Precautions" is an<br />
approach to infection control.<br />
According to the concept of Universal<br />
Precautions, all human blood and<br />
certain human body fluids are treated<br />
as if known to be infectious for HIV,<br />
HBV, and other bloodborne<br />
pathogens.<br />
"Work Practice <strong>Control</strong>s" means<br />
controls that reduce the likelihood of<br />
exposure by altering the manner in<br />
which a task is performed (e.g.,<br />
prohibiting recapping of needles by a<br />
two-handed technique).<br />
(c) <strong>Exposure</strong> <strong>Control</strong>.<br />
(c)(1) <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong>.<br />
(c)(1)(i) Each employer having an<br />
employee(s) with occupational<br />
exposure as defined by paragraph (b)<br />
of this section shall establish a written<br />
<strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong> designed to<br />
eliminate or minimize employee<br />
exposure.<br />
(c)(1)(ii) The <strong>Exposure</strong> <strong>Control</strong> <strong>Plan</strong><br />
shall contain at least the following<br />
elements:<br />
(c)(1)(ii)(A) The exposure<br />
determination required by paragraph<br />
(c)(2),<br />
(c)(1)(ii)(B) The schedule and method<br />
of implementation for paragraphs (d)<br />
Methods of Compliance, (e) HIV and<br />
HBV Research Laboratories and<br />
Production Facilities, (f) Hepatitis B<br />
Vaccination and Post-<strong>Exposure</strong><br />
Evaluation and Follow-up, (g)<br />
Communication of Hazards to<br />
Employees, and (h) Recordkeeping, of<br />
this standard, and<br />
(c)(1)(ii)(C) The procedure for the<br />
evaluation of circumstances<br />
surrounding exposure incidents as<br />
required by paragraph (f)(3)(i) of this<br />
standard.<br />
(c)(1)(iii) Each employer shall ensure<br />
that a copy of the <strong>Exposure</strong> <strong>Control</strong><br />
<strong>Plan</strong> is accessible to employees in<br />
(d)(2)(vii)(B) Such bending,<br />
recapping or needle removal must be<br />
accomplished through the use of a<br />
mechanical device or a one-handed<br />
technique.<br />
(d)(2)(viii) Immediately or as soon as<br />
possible after use, contaminated<br />
accordance with 29 CFR<br />
1910.1020(e).<br />
(c)(1)(iv) The <strong>Exposure</strong> <strong>Control</strong><br />
<strong>Plan</strong> shall be reviewed and updated<br />
at least annually and whenever<br />
necessary to reflect new or<br />
modified tasks and procedures<br />
which affect occupational exposure<br />
and to reflect new or revised<br />
employee positions with<br />
occupational exposure.<br />
(c)(1)(v) The <strong>Exposure</strong> <strong>Control</strong><br />
<strong>Plan</strong> shall be made available to the<br />
Assistant Secretary and the<br />
Director upon request for<br />
examination and copying.<br />
(c)(2) <strong>Exposure</strong> Determination.<br />
(c)(2)(i) Each employer who has an<br />
employee(s) with occupational<br />
exposure as defined by paragraph<br />
(b) of this section shall prepare an<br />
exposure determination. This exp.<br />
determ. shall contain the following:<br />
(c)(2)(i)(A) A list of all job<br />
classifications in which all<br />
employees in those job<br />
classifications have occupational<br />
exposure;<br />
(c)(2)(i)(B) A list of job<br />
classifications in which some<br />
employees have occupational<br />
exposure, and<br />
(c)(2)(i)(C) A list of all tasks and<br />
procedures or groups of closely<br />
related tasks and procedures in<br />
which occupational exposure<br />
occurs and that are performed by<br />
employees in job classifications<br />
listed in accordance with the<br />
provisions of paragraph (c)(2)(i)(B)<br />
of this standard.<br />
(c)(2)(ii) This exposure<br />
determination shall be made<br />
without regard to the use of<br />
personal protective equipment.<br />
(d) Methods of Compliance.<br />
(d)(1) General. Universal<br />
precautions shall be observed to<br />
prevent contact with blood or other<br />
potentially infectious materials.<br />
Under circumstances in which<br />
differentiation between body fluid<br />
reusable sharps shall be placed in<br />
appropriate containers until<br />
properly reprocessed. These<br />
containers shall be:<br />
(d)(2)(viii)(A) puncture resistant;<br />
types is difficult or impossible, all body<br />
fluids shall be considered potentially<br />
infectious materials.<br />
(d)(2) Engineering and Work Practice<br />
<strong>Control</strong>s.<br />
(d)(2)(i) Engineering and work practice<br />
controls shall be used to eliminate or<br />
minimize employee exposure. Where<br />
occupational exposure remains after<br />
institution of these controls, personal<br />
protective equipment shall also be used.<br />
(d)(2)(ii) Engineering controls shall be<br />
examined and maintained or replaced on a<br />
regular schedule to ensure effectiveness.<br />
(d)(2)(iii) Employers shall provide<br />
handwashing facilities which are readily<br />
accessible to employees.<br />
(d)(2)(iv) When provision of handwashing<br />
facilities is not feasible, the employer shall<br />
provide either an appropriate antiseptic<br />
hand cleanser in conjunction with clean<br />
cloth/paper towels or antiseptic towelettes.<br />
When antiseptic hand cleansers or<br />
towelettes are used, hands shall be washed<br />
with soap and running water as soon as<br />
feasible.<br />
(d)(2)(v) Employers shall ensure that<br />
employees wash their hands immediately<br />
or as soon as feasible after removal of<br />
gloves or other personal protective<br />
equipment.<br />
(d)(2)(vi) Employers shall ensure that<br />
employees wash hands and any other skin<br />
with soap and water, or flush mucous<br />
membranes with water immediately or as<br />
soon as feasible following contact of such<br />
body areas with blood or other potentially<br />
infectious materials.<br />
(d)(2)(vii) Contaminated needles and other<br />
contaminated sharps shall not be bent,<br />
recapped, or removed except as noted in<br />
paragraphs (d)(2)(vii)(A) and<br />
(d)(2)(vii)(B) below. Shearing or breaking<br />
of contaminated needles is prohibited.<br />
(d)(2)(vii)(A) Contaminated needles and<br />
other contaminated sharps shall not be<br />
bent, recapped or removed unless the<br />
employer can demonstrate that no<br />
alternative is feasible or that such action is<br />
required by a specific medical or dental<br />
procedure.<br />
(d)(2)(viii)(B) labeled or color-coded in<br />
accordance with this standard;<br />
(d)(2)(viii)(C) leakproof on the sides and<br />
bottom; and
(d)(2)(viii)(D) in accordance with the<br />
requirements set forth in paragraph<br />
(d)(4)(ii)(E) for reusable sharps.<br />
(d)(2)(ix) Eating, drinking, smoking,<br />
applying cosmetics or lip balm, and<br />
handling contact lenses are prohibited<br />
in work areas where there is a<br />
reasonable likelihood of occupational<br />
exposure.<br />
(d)(2)(x) Food and drink shall not be<br />
kept in refrigerators, freezers, shelves,<br />
cabinets or on countertops or<br />
benchtops where blood or other<br />
potentially infectious materials are<br />
present.<br />
(d)(2)(xi) All procedures involving<br />
blood or other potentially infectious<br />
materials shall be performed in such a<br />
manner as to minimize splashing,<br />
spraying, spattering, and generation of<br />
droplets of these substances.<br />
(d)(2)(xii) Mouth pipetting/suctioning<br />
of blood or other potentially infectious<br />
materials is prohibited.<br />
(d)(2)(xiii) Specimens of blood or<br />
other potentially infectious materials<br />
shall be placed in a container which<br />
prevents leakage during collection,<br />
handling, processing, storage,<br />
transport, or shipping.<br />
(d)(2)(xiii)(A) The container for<br />
storage, transport, or shipping shall be<br />
labeled or color-coded according to<br />
paragraph (g)(1)(i) and closed prior to<br />
being stored, transported, or shipped.<br />
When a facility utilizes Universal<br />
Precautions in the handling of all<br />
specimens, the labeling/color-coding<br />
of specimens is not necessary<br />
provided containers are recognizable<br />
as containing specimens. This<br />
exemption only applies while such<br />
specimens/containers remain within<br />
the facility. Labeling or color-coding<br />
in accordance with paragraph (g)(1)(i)<br />
is required when such<br />
specimens/containers leave the<br />
facility.<br />
(d)(3)(vi) If a garment(s) is penetrated<br />
by blood or other potentially<br />
infectious materials, the garment(s)<br />
shall be removed immediately or as<br />
soon as feasible.<br />
(d)(3)(vii) All personal protective<br />
equipment shall be removed prior to<br />
leaving the work area.<br />
(d)(2)(xiii)(B) If outside<br />
contamination of the primary<br />
container occurs, the primary<br />
container shall be placed within a<br />
second container which prevents<br />
leakage during handling,<br />
processing, storage, transport, or<br />
shipping and is labeled or colorcoded<br />
according to the<br />
requirements of this standard.<br />
(d)(2)(xiii)(C) If the specimen<br />
could puncture the primary<br />
container, the primary container<br />
shall be placed within a secondary<br />
container which is punctureresistant<br />
in addition to the above<br />
characteristics.<br />
(d)(2)(xiv) Equipment which may<br />
become contaminated with blood or<br />
other potentially infectious<br />
materials shall be examined prior to<br />
servicing or shipping and shall be<br />
decontaminated as necessary,<br />
unless the employer can<br />
demonstrate that decontamination<br />
of such equipment or portions of<br />
such equipment is not feasible.<br />
(d)(2)(xiv)(A) A readily observable<br />
label in accordance with paragraph<br />
(g)(1)(i)(H) shall be attached to the<br />
equipment stating which portions<br />
remain contaminated.<br />
(d)(2)(xiv)(B) The employer shall<br />
ensure that this information is<br />
conveyed to all affected employees,<br />
the servicing representative, and/or<br />
the manufacturer, as appropriate,<br />
prior to handling, servicing, or<br />
shipping so that appropriate<br />
precautions will be taken.<br />
(d)(3) Personal Protective<br />
Equipment.<br />
(d)(3)(i) Provision. When there is<br />
occupational exposure, the<br />
employer shall provide, at no cost<br />
to the employee, appropriate<br />
personal protective equipment such<br />
as, but not limited to, gloves,<br />
gowns, laboratory coats, face<br />
shields or masks and eye<br />
(d)(3)(viii) When personal<br />
protective equipment is removed it<br />
shall be placed in an appropriately<br />
designated area or container for<br />
storage, washing, decontamination<br />
or disposal.<br />
(d)(3)(ix) Gloves. Gloves shall be<br />
worn when it can be reasonably<br />
anticipated that the employee may<br />
protection, and mouthpieces, resuscitation<br />
bags, pocket masks, or other ventilation<br />
devices. Personal protective equipment<br />
will be considered "appropriate" only if it<br />
does not permit blood or other potentially<br />
infectious materials to pass through to or<br />
reach the employee's work clothes, street<br />
clothes, undergarments, skin, eyes, mouth,<br />
or other mucous membranes under normal<br />
conditions of use and for the duration of<br />
time which the protective equipment will<br />
be used.<br />
(d)(3)(ii) Use. The employer shall ensure<br />
that the employee uses appropriate<br />
personal protective equipment unless the<br />
employer shows that the employee<br />
temporarily and briefly declined to use<br />
personal protective equipment when, under<br />
rare and extraordinary circumstances, it<br />
was the employee's professional judgment<br />
that in the specific instance its use would<br />
have prevented the delivery of health care<br />
or public safety services or would have<br />
posed an increased hazard to the safety of<br />
the worker or co-worker. When the<br />
employee makes this judgement, the<br />
circumstances shall be investigated and<br />
documented in order to determine whether<br />
changes can be instituted to prevent such<br />
occurrences in the future.<br />
(d)(3)(iii) Accessibility. The employer<br />
shall ensure that appropriate personal<br />
protective equipment in the appropriate<br />
sizes is readily accessible at the worksite<br />
or is issued to employees. Hypoallergenic<br />
gloves, glove liners, powderless gloves, or<br />
other similar alternatives shall be readily<br />
accessible to those employees who are<br />
allergic to the gloves normally provided.<br />
(d)(3)(iv) Cleaning, Laundering, and<br />
Disposal. The employer shall clean,<br />
launder, and dispose of personal protective<br />
equipment required by paragraphs (d) and<br />
(e) of this standard, at no cost to the<br />
employee<br />
(d)(3)(v) Repair and Replacement. The<br />
employer shall repair or replace personal<br />
protective equipment as needed to<br />
maintain its effectiveness, at no cost to the<br />
employee.<br />
have hand contact with blood, other<br />
potentially infectious materials, mucous<br />
membranes, and non-intact skin; when<br />
performing vascular access procedures<br />
except as specified in paragraph<br />
(d)(3)(ix)(D); and when handling or<br />
touching contaminated items or surfaces.<br />
(d)(3)(ix)(A) Disposable (single use)<br />
gloves such as surgical or examination
gloves, shall be replaced as soon as<br />
practical when contaminated or as<br />
soon as feasible if they are torn,<br />
punctured, or when their ability to<br />
function as a barrier is compromised.<br />
(d)(3)(ix)(B) Disposable (single use)<br />
gloves shall not be washed or<br />
decontaminated for re-use.<br />
(d)(3)(ix)(C) Utility gloves may be<br />
decontaminated for re-use if the<br />
integrity of the glove is not<br />
compromised. However, they must be<br />
discarded if they are cracked, peeling,<br />
torn, punctured, or exhibit other signs<br />
of deterioration or when their ability<br />
to function as a barrier is<br />
compromised.<br />
(d)(3)(ix)(D) If an employer in a<br />
volunteer blood donation center<br />
judges that routine gloving for all<br />
phlebotomies is not necessary then the<br />
employer shall:<br />
(d)(3)(ix)(D)(1) Periodically<br />
reevaluate this policy;<br />
(d)(3)(ix)(D)(2) Make gloves<br />
available to all employees who wish<br />
to use them for phlebotomy;<br />
(d)(3)(ix)(D)(3) Not discourage the<br />
use of gloves for phlebotomy; and<br />
(d)(3)(ix)(D)(4) Require that gloves<br />
be used for phlebotomy in the<br />
following circumstances:<br />
[i] When the employee has cuts,<br />
scratches, or other breaks in his or her<br />
skin;<br />
[ii] When the employee judges that<br />
hand contamination with blood may<br />
occur, for example, when performing<br />
phlebotomy on an uncooperative<br />
source individual; and<br />
[iii] When the employee is receiving<br />
training in phlebotomy.<br />
(d)(3)(x) Masks, Eye Protection, and<br />
Face Shields. Masks in combination<br />
with eye protection devices, such as<br />
[b] Puncture resistant;<br />
[c] Leakproof on sides and bottom;<br />
and<br />
[d] Labeled or color-coded in<br />
accordance with paragraph (g)(1)(i) of<br />
this standard.<br />
(d)(4)(iii)(A)(2) During use,<br />
containers for contaminated sharps<br />
shall be:<br />
[a] Easily accessible to personnel and<br />
located as close as is feasible to the<br />
goggles or glasses with solid side<br />
shields, or chin-length face shields,<br />
shall be worn whenever splashes,<br />
spray, spatter, or droplets of blood<br />
or other potentially infectious<br />
materials may be generated and<br />
eye, nose, or mouth contamination<br />
can be reasonably anticipated.<br />
(d)(3)(xi) Gowns, Aprons, and<br />
Other Protective Body Clothing.<br />
Appropriate protective clothing<br />
such as, but not limited to, gowns,<br />
aprons, lab coats, clinic jackets, or<br />
similar outer garments shall be<br />
worn in occupational exposure<br />
situations. The type and<br />
characteristics will depend upon the<br />
task and degree of exposure<br />
anticipated.<br />
(d)(3)(xii) Surgical caps or hoods<br />
and/or shoe covers or boots shall be<br />
worn in instances when gross<br />
contamination can reasonably be<br />
anticipated (e.g., autopsies,<br />
orthopaedic surgery).<br />
(d)(4) Housekeeping.<br />
(d)(4)(i) General. Employers shall<br />
ensure that the worksite is<br />
maintained in a clean and sanitary<br />
condition. The employer shall<br />
determine and implement an<br />
appropriate written schedule for<br />
cleaning and method of<br />
decontamination based upon the<br />
location within the facility, type of<br />
surface to be cleaned, type of soil<br />
present, and tasks or procedures<br />
being performed in the area.<br />
(d)(4)(ii) All equipment and<br />
environmental and working<br />
surfaces shall be cleaned and<br />
decontaminated after contact with<br />
blood or other potentially infectious<br />
materials.<br />
(d)(4)(ii)(A) Contaminated work<br />
surfaces shall be decontaminated<br />
with an appropriate disinfectant<br />
immediate area where sharps are<br />
used or can be reasonably<br />
anticipated to be found (e.g.,<br />
laundries);<br />
[b] Maintained upright throughout<br />
use; and<br />
[c] Replaced routinely and not be<br />
allowed to overfill.<br />
(d)(4)(iii)(A)(3) When moving<br />
containers of contaminated sharps<br />
from the area of use, the containers<br />
shall be:<br />
after completion of procedures;<br />
immediately or as soon as feasible when<br />
surfaces are overtly contaminated or after<br />
any spill of blood or other potentially<br />
infectious materials; and at the end of the<br />
work shift if the surface may have become<br />
contaminated since the last cleaning.<br />
(d)(4)(ii)(B) Protective coverings, such as<br />
plastic wrap, aluminum foil, or<br />
imperviously-backed absorbent paper used<br />
to cover equipment and environmental<br />
surfaces, shall be removed and replaced as<br />
soon as feasible when they become overtly<br />
contaminated or at the end of the workshift<br />
if they may have become contaminated<br />
during the shift.<br />
(d)(4)(ii)(C) All bins, pails, cans, and<br />
similar receptacles intended for reuse<br />
which have a reasonable likelihood for<br />
becoming contaminated with blood or<br />
other potentially infectious materials shall<br />
be inspected and decontaminated on a<br />
regularly scheduled basis and cleaned and<br />
decontaminated immediately or as soon as<br />
feasible upon visible contamination.<br />
(d)(4)(ii)(D) Broken glassware which may<br />
be contaminated shall not be picked up<br />
directly with the hands. It shall be cleaned<br />
up using mechanical means, such as a<br />
brush and dust pan, tongs, or forceps.<br />
(d)(4)(ii)(E) Reusable sharps that are<br />
contaminated with blood or other<br />
potentially infectious materials shall not be<br />
stored or processed in a manner that<br />
requires employees to reach by hand into<br />
the containers where these sharps have<br />
been placed.<br />
(d)(4)(iii) Regulated Waste.<br />
(d)(4)(iii)(A) Contaminated Sharps<br />
Discarding and Containment.<br />
(d)(4)(iii)(A)(1) Contaminated sharps shall<br />
be discarded immediately or as soon as<br />
feasible in containers that are:<br />
[a] Closable;<br />
[a] Closed immediately prior to removal or<br />
replacement to prevent spillage or<br />
protrusion of contents during handling,<br />
storage, transport, or shipping;<br />
[b] Placed in a secondary container if<br />
leakage is possible. The second container<br />
shall be:<br />
[i] Closable;<br />
[ii] Constructed to contain all contents and<br />
prevent leakage during handling, storage,<br />
transport, or shipping; and
[iii] Labeled or color-coded according<br />
to paragraph (g)(1)(i) of this standard.<br />
(d)(4)(iii)(A)(4) Reusable containers<br />
shall not be opened, emptied, or<br />
cleaned manually or in any other<br />
manner which would expose<br />
employees to the risk of percutaneous<br />
injury.<br />
(d)(4)(iii)(B) Other Regulated Waste<br />
Containment.<br />
(d)(4)(iii)(B)(1) Regulated waste shall<br />
be<br />
placed in containers which are:<br />
[a] Closable;<br />
[b] Constructed to contain all contents<br />
and prevent leakage of fluids during<br />
handling, storage, transport or<br />
shipping;<br />
[c] Labeled or color-coded in<br />
accordance with paragraph (g)(1)(i)<br />
this standard; and<br />
[d] Closed prior to removal to prevent<br />
spillage or protrusion of contents<br />
during handling, storage, transport, or<br />
shipping.<br />
(d)(4)(iii)(B)(2) If outside<br />
contamination of the regulated waste<br />
container occurs, it shall be placed in<br />
a second container. The second<br />
container shall be:<br />
[a] Closable;<br />
[b] Constructed to contain all contents<br />
and prevent leakage of fluids during<br />
handling, storage, transport or<br />
shipping;<br />
[c] Labeled or color-coded in<br />
accordance with paragraph (g)(1)(i) of<br />
this standard; and<br />
[d] Closed prior to removal to prevent<br />
spillage or protrusion of contents<br />
during handling, storage, transport, or<br />
shipping.<br />
(d)(4)(iii)(C) Disposal of all regulated<br />
waste shall be in accordance with<br />
applicable regulations of the United<br />
States, States and Territories, and<br />
political subdivisions of States and<br />
Territories.<br />
(d)(4)(iv) Laundry.<br />
(d)(4)(iv)(A) Contaminated laundry<br />
shall be handled as little as possible<br />
with a minimum of agitation.<br />
(d)(4)(iv)(A)(1) Contaminated<br />
laundry shall be bagged or<br />
containerized at the location where it<br />
was used and shall not be sorted or<br />
rinsed in the location of use.<br />
(d)(4)(iv)(A)(2) Contaminated<br />
laundry shall be placed and<br />
transported in bags or containers<br />
labeled or color-coded in<br />
accordance with paragraph (g)(1)(i)<br />
of this standard. When a facility<br />
utilizes Universal Precautions in<br />
the handling of all soiled laundry,<br />
alternative labeling or color-coding<br />
is sufficient if it permits all<br />
employees to recognize the<br />
containers as requiring compliance<br />
with Universal Precautions.<br />
(d)(4)(iv)(A)(3) Whenever<br />
contaminated laundry is wet and<br />
presents a reasonable likelihood of<br />
soak-through of or leakage from the<br />
bag or container, the laundry shall<br />
be placed and transported in bags<br />
or containers which prevent soakthrough<br />
and/or leakage of fluids to<br />
the exterior.<br />
(d)(4)(iv)(B) The employer shall<br />
ensure that employees who have<br />
contact with contaminated laundry<br />
wear protective gloves and other<br />
appropriate personal protective<br />
equipment.<br />
(d)(4)(iv)(C) When a facility ships<br />
contaminated laundry off-site to a<br />
second facility which does not<br />
utilize Universal Precautions in the<br />
handling of all laundry, the facility<br />
generating the contaminated<br />
laundry must place such laundry in<br />
bags or containers which are<br />
labeled or color-coded in<br />
accordance with paragraph<br />
(g)(1)(i).<br />
(e) HIV and HBV Research<br />
Laboratories and Production<br />
Facilities.<br />
(e)(1) This paragraph applies to<br />
research laboratories and<br />
production facilities engaged in the<br />
culture, production, concentration,<br />
experimentation, and manipulation<br />
of HIV and HBV. It does not apply<br />
to clinical or diagnostic laboratories<br />
engaged solely in the analysis of<br />
blood, tissues, or organs. These<br />
requirements apply in addition to<br />
the other requirements of the<br />
standard.<br />
(e)(2) Research laboratories and<br />
production facilities shall meet the<br />
following criteria:<br />
(e)(2)(i) Standard Microbiological<br />
Practices. All regulated waste shall<br />
either be incinerated or<br />
decontaminated by a method such as<br />
autoclaving known to effectively destroy<br />
bloodborne pathogens.<br />
(e)(2)(ii) Special Practices<br />
(e)(2)(ii)(A) Laboratory doors shall be kept<br />
closed when work involving HIV or HBV<br />
is in progress.<br />
(e)(2)(ii)(B) Contaminated materials that<br />
are to be decontaminated at a site away<br />
from the work area shall be placed in a<br />
durable, leakproof, labeled or color-coded<br />
container that is closed before being<br />
removed from the work area.
(e)(2)(ii)(C) Access to the work area shall be limited to authorized persons. Written policies and<br />
procedures shall be established whereby only persons who have been advised of the potential<br />
biohazard, who meet any specific entry requirements, and who comply with all entry and exit<br />
procedures shall be allowed to enter the work areas and animal rooms.<br />
(e)(2)(ii)(D) When other potentially infectious materials or infected animals are present in the work<br />
area or containment module, a hazard warning sign incorporating the universal biohazard symbol shall<br />
be posted on all access doors. The hazard warning sign shall comply with paragraph (g)(1)(ii) of this<br />
standard.<br />
(e)(2)(ii)(E) All activities involving other potentially infectious materials shall be conducted in<br />
biological safety cabinets or other physical-containment devices within the containment module. No<br />
work with these other potentially infectious materials shall be conducted on the open bench<br />
(e)(2)(ii)(F) Laboratory coats, gowns, smocks, uniforms, or other appropriate protective clothing shall<br />
be used in the work area and animal rooms. Protective clothing shall not be worn outside of the work<br />
area and shall be decontaminated before being laundered.<br />
(e)(2)(ii)(G) Special care shall be taken to avoid skin contact with other potentially infectious<br />
materials. Gloves shall be worn when handling infected animals and when making hand contact with<br />
other potentially infectious materials is unavoidable.<br />
(e)(2)(ii)(H) Before disposal all waste from work areas and from animal rooms shall either be<br />
incinerated or decontaminated by a method such as autoclaving known to effectively destroy<br />
bloodborne pathogens.<br />
(e)(2)(ii)(I) Vacuum lines shall be protected with liquid disinfectant traps and high-efficiency<br />
particulate air (HEPA) filters or filters of equivalent or superior efficiency and which are checked<br />
routinely and maintained or replaced as necessary.<br />
(e)(2)(ii)(J) Hypodermic needles and syringes shall be used only for parenteral injection and<br />
aspiration of fluids from laboratory animals and diaphragm bottles. Only needle-locking syringes or<br />
disposable syringe-needle units (i.e., the needle is integral to the syringe) shall be used for the<br />
injection or aspiration of other potentially infectious materials. Extreme caution shall be used when<br />
handling needles and syringes. A needle shall not be bent, sheared, replaced in the sheath or guard, or<br />
removed from the syringe following use. The needle and syringe shall be promptly placed in a<br />
puncture-resistant container and autoclaved or decontaminated before reuse or disposal.<br />
(e)(2)(ii)(K) All spills shall be immediately contained and cleaned up by appropriate professional staff<br />
or others properly trained and equipped to work with potentially concentrated infectious materials.<br />
(e)(2)(ii)(L) A spill or accident that results in an exposure incident shall be immediately reported to<br />
the laboratory director or other responsible person.<br />
(e)(2)(ii)(M) A biosafety manual shall be prepared or adopted and periodically reviewed and updated<br />
at least annually or more often if necessary. Personnel shall be advised of potential hazards, shall be<br />
required to read instructions on practices and procedures, and shall be required to follow them.<br />
(e)(2)(iii) Containment Equipment.<br />
(e)(2)(iii)(A) Certified biological safety cabinets (Class I, II, or III) or other appropriate combinations<br />
of personal protection or physical containment devices, such as special protective clothing, respirators,<br />
centrifuge safety cups, sealed centrifuge rotors, and containment caging for animals, shall be used for<br />
all activities with other potentially infectious materials that pose a threat of exposure to droplets,<br />
splashes, spills, or aerosols.<br />
(e)(2)(iii)(B) Biological safety cabinets shall be certified when installed, whenever they are moved<br />
and at least annually.<br />
(e)(3) HIV and HBV research laboratories shall meet the following criteria:<br />
(e)(3)(i) Each laboratory shall contain a facility for hand washing and an eye wash facility which is<br />
readily available within the work area.<br />
(e)(3)(ii) An autoclave for decontamination of regulated waste shall be available.
(e)(4) HIV and HBV production facilities shall meet the following criteria:<br />
(e)(4)(i) The work areas shall be separated from areas that are open to unrestricted traffic flow within<br />
the building. Passage through two sets of doors shall be the basic requirement for entry into the work<br />
area from access corridors or other contiguous areas. Physical separation of the high-containment<br />
work area from access corridors or other areas or activities may also be provided by a double-doored<br />
clothes-change room (showers may be included), airlock, or other access facility that requires passing<br />
through two sets of doors before entering the work area.<br />
(e)(4)(ii) The surfaces of doors, walls, floors and ceilings in the work area shall be water resistant so<br />
that they can be easily cleaned. Penetrations in these surfaces shall be sealed or capable of being<br />
sealed to facilitate decontamination.<br />
(e)(4)(iii) Each work area shall contain a sink for washing hands and a readily available eye wash<br />
facility. The sink shall be foot, elbow, or automatically operated and shall be located near the exit door<br />
of the work area.<br />
(e)(4)(iv) Access doors to the work area or containment module shall be self-closing.<br />
(e)(4)(v) An autoclave for decontamination of regulated waste shall be available within or as near as<br />
possible to the work area.<br />
(e)(4)(vi) A ducted exhaust-air ventilation system shall be provided. This system shall create<br />
directional airflow that draws air into the work area through the entry area. The exhaust air shall not<br />
be recirculated to any other area of the building, shall be discharged to the outside, and shall be<br />
dispersed away from occupied areas and air intakes. The proper direction of the airflow shall be<br />
verified (i.e., into the work area).<br />
(e)(5) Training Requirements. Additional training requirements for employees in HIV and HBV<br />
research laboratories and HIV and HBV production facilities are specified in paragraph (g)(2)(ix).<br />
(f) Hepatitis B Vaccination and Post-exposure Evaluation and Follow-up.<br />
(f)(1) General.<br />
(f)(1)(i) The employer shall make available the hepatitis B vaccine and vaccination series to all<br />
employees who have occupational exposure, and post-exposure evaluation and follow-up to all<br />
employees who have had an exposure incident.<br />
(f)(1)(ii) The employer shall ensure that all medical evaluations and procedures including the hepatitis<br />
B vaccine and vaccination series and post-exposure evaluation and follow-up, including prophylaxis,<br />
are:<br />
(f)(1)(ii)(A) Made available at no cost to the employee;<br />
(f)(1)(ii)(B) Made available to the employee at a reasonable time and place;<br />
(f)(1)(ii)(C) Performed by or under the supervision of a licensed physician or by or under the<br />
supervision of another licensed healthcare professional; and<br />
(f)(1)(ii)(D) Provided according to recommendations of the U.S. Public Health Service current at the<br />
time these evaluations and procedures take place, except as specified by this paragraph (f).<br />
(f)(1)(iii) The employer shall ensure that all laboratory tests are conducted by an accredited laboratory<br />
at no cost to the employee.<br />
(f)(2) Hepatitis B Vaccination.<br />
(f)(2)(i) Hepatitis B vaccination shall be made available after the employee has received the training<br />
required in paragraph (g)(2)(vii)(I) and within 10 working days of initial assignment to all employees<br />
who have occupational exposure unless the employee has previously received the complete hepatitis B<br />
vaccination series, antibody testing has revealed that the employee is immune, or the vaccine is<br />
contraindicated for medical reasons.<br />
(f)(2)(ii) The employer shall not make participation in a prescreening program a prerequisite for<br />
receiving hepatitis B vaccination.
(f)(2)(iii) If the employee initially declines hepatitis B vaccination but at a later date while still<br />
covered under the standard decides to accept the vaccination, the employer shall make available<br />
hepatitis B vaccination at that time.<br />
(f)(2)(iv) The employer shall assure that employees who decline to accept hepatitis B vaccination<br />
offered by the employer sign the statement in Appendix A.<br />
(f)(2)(v) If a routine booster dose(s) of hepatitis B vaccine is recommended by the U.S. Public Health<br />
Service at a future date, such booster dose(s) shall be made available in accordance with section<br />
(f)(1)(ii).<br />
(f)(3) Post-exposure Evaluation and Follow-up. Following a report of an exposure incident, the<br />
employer shall make immediately available to the exposed employee a confidential medical<br />
evaluation and follow-up, including at least the following elements:<br />
(f)(3)(i) Documentation of the route(s) of exposure, and the circumstances under which the exposure<br />
incident occurred;<br />
(f)(3)(ii) Identification and documentation of the source individual, unless the employer can establish<br />
that identification is infeasible or prohibited by state or local law;<br />
(f)(3)(ii)(A) The source individual's blood shall be tested as soon as feasible and after consent is<br />
obtained in order to determine HBV and HIV infectivity. If consent is not obtained, the employer shall<br />
establish that legally required consent cannot be obtained. When the source individual's consent is not<br />
required by law, the source individual's blood, if available, shall be tested and the results documented.<br />
(f)(3)(ii)(B) When the source individual is already known to be infected with HBV or HIV, testing for<br />
the source individual's known HBV or HIV status need not be repeated.<br />
(f)(3)(ii)(C) Results of the source individual's testing shall be made available to the exposed<br />
employee, and the employee shall be informed of applicable laws and regulations concerning<br />
disclosure of the identity and infectious status of the source individual.<br />
(f)(3)(iii) Collection and testing of blood for HBV and HIV serological status;<br />
(f)(3)(iii)(A) The exposed employee's blood shall be collected as soon as feasible and tested after<br />
consent is obtained.<br />
(f)(3)(iii)(B) If the employee consents to baseline blood collection, but does not give consent at that<br />
time for HIV serologic testing, the sample shall be preserved for at least 90 days. If, within 90 days of<br />
the exposure incident, the employee elects to have the baseline sample tested, such testing shall be<br />
done as soon as feasible.<br />
(f)(3)(iv) Post-exposure prophylaxis, when medically indicated, as recommended by the U.S. Public<br />
Health Service;<br />
(f)(3)(v) Counseling; and<br />
(f)(3)(vi) Evaluation of reported illnesses.<br />
(f)(4) Information Provided to the Healthcare Professional.<br />
(f)(4)(i) The employer shall ensure that the healthcare professional responsible for the employee's<br />
Hepatitis B vaccination is provided a copy of this regulation.<br />
(f)(4)(ii) The employer shall ensure that the healthcare professional evaluating an employee after an<br />
exposure incident is provided the following information:<br />
(f)(4)(ii)(A) A copy of this regulation;<br />
(f)(4)(ii)(B) A description of the exposed employee's duties as they relate to the exposure incident;<br />
(f)(4)(ii)(C) Documentation of the route(s) of exposure and circumstances under which exposure<br />
occurred;<br />
(f)(4)(ii)(D) Results of the source individual's blood testing, if available; and<br />
(f)(4)(ii)(E) All medical records relevant to the appropriate treatment of the employee including<br />
vaccination status which are the employer's responsibility to maintain.
(f)(5) Healthcare Professional's Written Opinion. The employer shall obtain and provide the<br />
employee with a copy of the evaluating healthcare professional's written opinion within 15 days of the<br />
completion of the evaluation.<br />
(f)(5)(i) The healthcare professional's written opinion for Hepatitis B vaccination shall be limited to<br />
whether Hepatitis B vaccination is indicated for an employee, and if the employee has received such<br />
vaccination.<br />
(f)(5)(ii) The healthcare professional's written opinion for post-exposure evaluation and follow-up<br />
shall be limited to the following information:<br />
(f)(5)(ii)(A) That the employee has been informed of the results of the evaluation; and<br />
(f)(5)(ii)(B) That the employee has been told about any medical conditions resulting from exposure to<br />
blood or other potentially infectious materials which require further evaluation or treatment.<br />
(f)(5)(iii) All other findings or diagnoses shall remain confidential and shall not be included in the<br />
written report.<br />
(f)(6) Medical Recordkeeping. Medical records required by this standard shall be maintained in<br />
accordance with paragraph (h)(1) of this section.<br />
(g) Communication of Hazards to Employees.<br />
(g)(1) Labels and Signs.<br />
(g)(1)(i) Labels.<br />
(g)(1)(i)(A) Warning labels shall be affixed to containers of regulated waste, refrigerators and freezers<br />
containing blood or other potentially infectious material; and other containers used to store, transport<br />
or ship blood or other potentially infectious materials, except as provided in paragraph (g)(1)(i)(E), (F)<br />
and (G).