Clinical Outcomes Review Committee Bulletin 1, April 2013
Clinical Outcomes Review Committee Bulletin 1, April 2013
Clinical Outcomes Review Committee Bulletin 1, April 2013
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
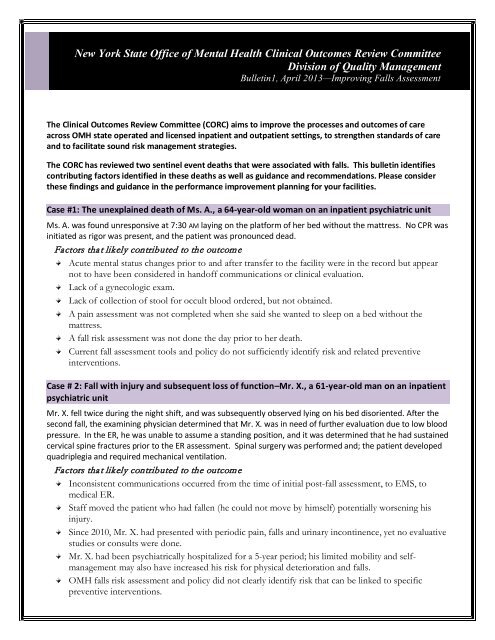
New York State Office of Mental Health <strong>Clinical</strong> <strong>Outcomes</strong> <strong>Review</strong> <strong>Committee</strong><br />
Division of Quality Management<br />
<strong>Bulletin</strong>1, <strong>April</strong> <strong>2013</strong>—Improving Falls Assessment<br />
The <strong>Clinical</strong> <strong>Outcomes</strong> <strong>Review</strong> <strong>Committee</strong> (CORC) aims to improve the processes and outcomes of care<br />
across OMH state operated and licensed inpatient and outpatient settings, to strengthen standards of care<br />
and to facilitate sound risk management strategies.<br />
The CORC has reviewed two sentinel event deaths that were associated with falls. This bulletin identifies<br />
contributing factors identified in these deaths as well as guidance and recommendations. Please consider<br />
these findings and guidance in the performance improvement planning for your facilities.<br />
Case #1: The unexplained death of Ms. A., a 64-year-old woman on an inpatient psychiatric unit<br />
Ms. A. was found unresponsive at 7:30 AM laying on the platform of her bed without the mattress. No CPR was<br />
initiated as rigor was present, and the patient was pronounced dead.<br />
Factors that likely contributed to the outcome<br />
Acute mental status changes prior to and after transfer to the facility were in the record but appear<br />
not to have been considered in handoff communications or clinical evaluation.<br />
Lack of a gynecologic exam.<br />
Lack of collection of stool for occult blood ordered, but not obtained.<br />
A pain assessment was not completed when she said she wanted to sleep on a bed without the<br />
mattress.<br />
A fall risk assessment was not done the day prior to her death.<br />
Current fall assessment tools and policy do not sufficiently identify risk and related preventive<br />
interventions.<br />
Case # 2: Fall with injury and subsequent loss of function–Mr. X., a 61-year-old man on an inpatient<br />
psychiatric unit<br />
Mr. X. fell twice during the night shift, and was subsequently observed lying on his bed disoriented. After the<br />
second fall, the examining physician determined that Mr. X. was in need of further evaluation due to low blood<br />
pressure. In the ER, he was unable to assume a standing position, and it was determined that he had sustained<br />
cervical spine fractures prior to the ER assessment. Spinal surgery was performed and; the patient developed<br />
quadriplegia and required mechanical ventilation.<br />
Factors that likely contributed to the outcome<br />
Inconsistent communications occurred from the time of initial post-fall assessment, to EMS, to<br />
medical ER.<br />
Staff moved the patient who had fallen (he could not move by himself) potentially worsening his<br />
injury.<br />
Since 2010, Mr. X. had presented with periodic pain, falls and urinary incontinence, yet no evaluative<br />
studies or consults were done.<br />
Mr. X. had been psychiatrically hospitalized for a 5-year period; his limited mobility and selfmanagement<br />
may also have increased his risk for physical deterioration and falls.<br />
OMH falls risk assessment and policy did not clearly identify risk that can be linked to specific<br />
preventive interventions.
Assessment Process Guidance and Recommendations<br />
1. Fall Risk Assessments * should be completed on admission, after a transfer between units, at regular<br />
intervals (e.g., monthly, quarterly), when a change in status occurs, and after every fall (witnessed or<br />
unwitnessed).<br />
• Valid, reliable fall risk assessment tools such as the Morse Fall Scale and evidence-based prevention<br />
and risk reduction strategies should be used for determining fall risk, assessing patients post fall,<br />
and for intervening accordingly.<br />
2. The Pain Assessment Scale * should contain behavioral assessment.<br />
• It is critical to know the patient’s baseline level of activity and mobility, including relevant<br />
information from family/friends/service providers, for assessing behaviors and indicators of pain<br />
and discomfort.<br />
3. The Confusion Assessment Method (CAM) * is a standardized evidence-based tool that enables<br />
clinicians to identify and recognize delirium—an acute change in mental status from baseline—quickly<br />
and accurately.<br />
• It is crucial to distinguish acute cognitive changes from episodic presentations of psychiatric illness<br />
because a fluctuating mental status often signals a need for additional treatment. This can be<br />
effectively done with a standardized assessment tool.<br />
Hand-off Communication Guidance and Recommendations<br />
1. Hand off communication (nurse to nurse and doctor to doctor) must be completed at all points during<br />
transfer of care.<br />
• Well-defined screening tools * for use by the nurse and the physician can ensure that relevant<br />
information is communicated systematically at points of transfer.<br />
2. Strategies to improve inter-professional communications should be adopted (e.g., multidisciplinary<br />
rounds, medical rounds board where RNs communicate physical changes in patients’ status) and<br />
evaluated for their effectiveness.<br />
3. Doctor-to doctor communication between the psychiatric hospitals and ER must occur prior to and<br />
after ER evaluations.<br />
* Referenced Tools<br />
Fall Risk Assessment Tools<br />
Mathias S, Nayak USL, & Isaacs B. (1986). Balance in elderly patient: The “Get up and Go” Test. Archives of Physical Medicine and Rehabilitation,<br />
67, 387–389. Available online at http://www.healthcare.uiowa.edu/igec/tools/mobility/getupandgo.pdf<br />
Podsiadlo D, & Richardson S. (1991). The timed “up & go": A test of basic functional mobility for frail elderly persons. Journal of the<br />
American Geriatrics Society, 39, 142–148. Available online at<br />
http://www.saskatoonhealthregion.ca/pdf/03_Timed%20Up%20and%20Go%20procedure.pdf<br />
Morse JM. (1997). Preventing Patient Falls. Thousand Oaks, CA: Sage. Tool is available online at<br />
http://www.primaris.org/sites/default/files/resources/Restraints%20and%20Falls/falls_morse%20fall%20scale%20final.pdf<br />
Pain Assessment Tools<br />
Feldt KS. (2000). The checklist of nonverbal pain indicators (CNPI). Pain Management Nursing, 1(1), 13-21. Available online at<br />
http://www.healthcare.uiowa.edu/igec/tools/pain/nonverbalPain.pdf<br />
Horgas AL. (2003). Assessing pain in older adults with dementia. In Boltz M, series ed. Try This: Best Practices in Nursing Care for<br />
Hospitalized Older Adults with Dementia., 1(2). Hartford, CT: Hartford Institute for Geriatric Nursing. Available online at<br />
http://consultgerirn.org/uploads/File/trythis/try_this_d2.pdf<br />
Merkel SI, Voepel-Lewis T, Shayevitz JR, et al. (1997). The FLACC: A behavioral scale for scoring postoperative pain in young children.<br />
Pediatric Nurse, 23(3), 293–297. Available online at http://lane.stanford.edu/portals/cvicu/HCP_Neuro_Tab_4/FLACC_Score.pdf<br />
Hartrick CT, Kovan JP, & Shapiro S. (2003). The numeric rating scale for clinical pain measurement: A ratio measure? Pain Practice, 3(4),<br />
310–316. Available online at http://www.geriu.org/uploads/painDVD/AdditionalMaterials/ZeroToTenPainScale.pdf<br />
Wong D & Whaley L. (1986). <strong>Clinical</strong> Handbook of Pediatric Nursing, 2 nd ed, 373. St. Louis: C.V. Mosby. Available online at<br />
http://painconsortium.nih.gov/pain_scales/Wong-Baker_Faces.pdf<br />
Wary B & Collectif D. (1999). Doloplus-2, a scale for pain measurement. Soins Gerontologie, 19:25–27. Available online at<br />
http://prc.coh.org/PainNOA/Doloplus%202_Tool.pdf<br />
Confusion Assessment Method<br />
Inouye S, van Dyck C, Alessi C, et al. (1990). Clarifying confusion: The confusion assessment method. Annals of Internal Medicine, 113(12),<br />
941–948. Tool available online at http://www.ahrq.gov/legacy/research/ltc/fallpxtoolkit/fallpxtool3j.htm<br />
Handoff Communication<br />
SBAR, a standardized communication format that organizes the transfer of information under the four themes of Situation, Background;<br />
Assessment and Recommendation, was developed at Kaiser Permanente of Colorado, Evergreen. It has been endorsed by many national<br />
organizations and medical accreditation bodies. Toolkit available online at http://www.ihi.org/knowledge/Pages/Tools/SBARToolkit.aspx