Managing Bevacizumab-Related Toxicities in Patients with ...
Managing Bevacizumab-Related Toxicities in Patients with ...
Managing Bevacizumab-Related Toxicities in Patients with ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
HOW WE DO IT<br />
<strong>Manag<strong>in</strong>g</strong> <strong>Bevacizumab</strong>-<strong>Related</strong> <strong>Toxicities</strong><br />
<strong>in</strong> <strong>Patients</strong> <strong>with</strong> Colorectal Cancer<br />
M. Wasif Saif, MD, MBBS<br />
B<br />
evacizumab (Avast<strong>in</strong>) is the first antiangiogenic<br />
agent cl<strong>in</strong>ically proven to<br />
extend survival and <strong>in</strong> comb<strong>in</strong>ation <strong>with</strong><br />
5-fluorouracil (5-FU)–based chemotherapy<br />
has been approved by the US Food and<br />
Drug Adm<strong>in</strong>istration (FDA) for the first-l<strong>in</strong>e or<br />
second-l<strong>in</strong>e treatment of metastatic colorectal<br />
cancer (CRC).<br />
In the pivotal phase III study <strong>in</strong> the first-l<strong>in</strong>e<br />
sett<strong>in</strong>g, bevacizumab provided, a 30% <strong>in</strong>crease <strong>in</strong><br />
median overall survival (OS, 20.3 vs 15.6 months;<br />
hazard ratio [HR], 0.66; P < 0.001) and a 71%<br />
<strong>in</strong>crease <strong>in</strong> progression-free survival (PFS, 10.6<br />
vs 6.2 months; HR, 0.54; P < 0.001) when comb<strong>in</strong>ed<br />
<strong>with</strong> IFL (ir<strong>in</strong>otecan/5-FU/leucovor<strong>in</strong> [LV])<br />
versus IFL alone. 1 Cl<strong>in</strong>ical benefit, as measured by<br />
OS, was observed across all patient subgroups analyzed.<br />
Increased OS and PFS <strong>with</strong> bevacizumab<br />
added to chemotherapy have also been observed <strong>in</strong><br />
other trials <strong>in</strong> the first-l<strong>in</strong>e sett<strong>in</strong>g us<strong>in</strong>g oxali plat<strong>in</strong><br />
(Eloxat<strong>in</strong>)-based regimens 2,3 and 5-FU/LV. 4,5<br />
The Eastern Cooperative Oncology Group<br />
E3200, a randomized phase III trial, confirmed<br />
the <strong>in</strong>creased efficacy of FOLFOX4 (oxaliplat<strong>in</strong>/<br />
LV/5-FU) plus bevacizumab among patients who<br />
had experienced disease progression on first-l<strong>in</strong>e<br />
therapy. 6 <strong>Patients</strong> were randomized to be treated<br />
<strong>with</strong> FOLFOX4, FOLFOX4 plus bevacizumab<br />
(10 mg/kg every 2 weeks), or bevacizumab monotherapy.<br />
There was a significant improvement <strong>in</strong><br />
median OS <strong>with</strong> FOLFOX plus bevacizumab (12.9<br />
months) versus FOLFOX alone (10.7 months).<br />
This study confirmed the activity of bevacizumab<br />
<strong>in</strong> the second-l<strong>in</strong>e sett<strong>in</strong>g when comb<strong>in</strong>ed <strong>with</strong><br />
FOLFOX, and it provided data about the safety<br />
profile at a dose of 10 mg/kg (every 2 weeks).<br />
Manuscript submitted May 28, 2009;<br />
accepted July 7, 2009.<br />
Correspondence to: M. Wasif Saif, MD, Associate Professor,<br />
Division of Medical Oncology, Yale University School of Medic<strong>in</strong>e,<br />
333 Cedar Street, FMP 116, New Haven, CT 06520;<br />
telephone: (203) 737-1569; fax: (203) 785-3788; e-mail: wasif.<br />
saif@yale.edu<br />
J Support Oncol 2009;7:245–251<br />
© 2009 Elsevier Inc. All rights reserved.<br />
As bevacizumab is becom<strong>in</strong>g widely used <strong>in</strong><br />
general oncology practice, it is important to understand<br />
the toxicities that can arise. Currently,<br />
there are no practice guidel<strong>in</strong>es for their management.<br />
The author describes his experience <strong>in</strong><br />
adm<strong>in</strong>ister<strong>in</strong>g bevacizumab safely, and provides<br />
recommendations for toxicity management.<br />
Adverse Events of Treatment<br />
<strong>Bevacizumab</strong> offers the potential to <strong>in</strong>crease<br />
survival <strong>with</strong>out substantially alter<strong>in</strong>g the toxicity<br />
profile <strong>in</strong> the treatment of metastatic CRC. Many<br />
adverse events related to anticancer therapy were<br />
reported <strong>in</strong> the trials <strong>in</strong>volv<strong>in</strong>g bevacizumab <strong>with</strong><br />
cytotoxic chemotherapy. Because bevacizumab<br />
was used <strong>in</strong> comb<strong>in</strong>ation <strong>with</strong> other chemotherapy<br />
agents, it can be difficult to determ<strong>in</strong>e which<br />
adverse effects are solely caused by bevacizumab.<br />
However, the adverse effects associated <strong>with</strong> the<br />
chemotherapy agents are well characterized, and<br />
any new or unexpected adverse effects can thus<br />
be reasonably attributed to bevacizumab. Fortunately,<br />
bevacizumab does not have any overlapp<strong>in</strong>g<br />
hematologic or gastro<strong>in</strong>test<strong>in</strong>al (GI) toxicities<br />
<strong>with</strong> chemotherapeutic agents.<br />
Phase III/IV trials of bevacizumab <strong>in</strong> CRC have<br />
identified hypertension (grade 3/4, 1%–18%), prote<strong>in</strong>uria<br />
(grade 3, 0%–2%), wound heal<strong>in</strong>g complications<br />
(1%), GI perforation (0%–2%), arterial<br />
thromboembolism (< 1%–2%), and bleed<strong>in</strong>g<br />
(grade 3/4, < 1%–6%) as bevacizumab-associated<br />
adverse effects (Table 1). 1,5–8 The <strong>in</strong>cidence of bevacizumab-related<br />
toxicities was similar <strong>in</strong> cl<strong>in</strong>ical<br />
trials 1–6 and <strong>in</strong> community-based registry studies<br />
(BRiTE and first BEAT). 7,8 The BEAT study, conducted<br />
<strong>in</strong> 41 countries around the world, and the<br />
BRiTE registry, its US counterpart, <strong>in</strong>vestigated<br />
the use of bevacizumab <strong>in</strong> advanced CRC <strong>in</strong> comb<strong>in</strong>ation<br />
<strong>with</strong> standard chemotherapies, <strong>in</strong>clud<strong>in</strong>g<br />
oxaliplat<strong>in</strong>, ir<strong>in</strong>otecan, or 5-FU, and/or capecitab<strong>in</strong>e<br />
(Xeloda). The BEAT and BRiTE studies<br />
also evaluated the safety of bevacizumab <strong>with</strong> different<br />
chemotherapies <strong>in</strong> a broad patient popula-<br />
Dr. Saif is Director, GI<br />
Cancers Program, and<br />
Associate Professor,<br />
Yale Cancer Center,<br />
Yale University School<br />
of Medic<strong>in</strong>e, New<br />
Haven, Connecticut.<br />
Vo l u m e 7, Nu m b e r 6 ■ November/December 2009<br />
www.SupportiveOncology.net<br />
245
<strong>Manag<strong>in</strong>g</strong> <strong>Bevacizumab</strong>-<strong>Related</strong> <strong>Toxicities</strong> <strong>in</strong> <strong>Patients</strong> <strong>with</strong> Colorectal Cancer<br />
Table 1<br />
Major <strong>Toxicities</strong> of <strong>Bevacizumab</strong><br />
Frequency of ADVERSE EVENTS (%)<br />
HYPERTENSION PROTEINURIA BLEEDING Gastro<strong>in</strong>test<strong>in</strong>al WOUND<br />
STUDY BEVACIZUMAB DOSE (GRADE 3) (GRADE 3) THROMBOSIS (GRADE 3/4) PERFORATION HEALING<br />
AVF2107g 1,5 5 mg/kg every 2 weeks 11 1 19 a 3 2 nR<br />
E3200 6 10 mg/kg every 2 weeks 5 1 3 (VTE) 3 1 nR<br />
1 (ATE)<br />
BRiTE 7 5 mg/kg every 2 weeks 16 b NR 2 (ATE) 2 2 1<br />
First BEAT 8 5 mg/kg every 2 weeks (5-Fu 1 nR 1 (ATE) 1 1 nR<br />
regimens) or 7.5 mg/kg every<br />
2 (VTE)<br />
3 weeks (capecitab<strong>in</strong>e regimens)<br />
5-FU = 5-fluorouracil; NR = not reported; VTE = venous thromboembolic event; ATE = arterial thromboembolic event<br />
a<br />
Thromboembolism (listed as “any thrombotic event”)<br />
b<br />
Specified as hypertension requir<strong>in</strong>g medication<br />
tion. Results from these studies show that bevacizumab’s safety<br />
profile/tolerability is consistent <strong>with</strong> the safety observations<br />
from other studies.<br />
It is also importunate to note that these toxicities are a class<br />
effect for all anti-VEGF (vascular endothelial growth factor)<br />
therapy. As the cl<strong>in</strong>ical use of bevacizumab cont<strong>in</strong>ues to <strong>in</strong>crease<br />
<strong>in</strong> the treatment of CRC as well as other malignancies,<br />
it is prudent to understand the toxicities that can arise and<br />
know how to manage them. Therefore, the discussion that follows<br />
explores these toxicities and offers management recommendations<br />
based on experience and review of the literature.<br />
Selected <strong>Bevacizumab</strong>-Associated <strong>Toxicities</strong><br />
HYPERTENSION<br />
Incidence. Grade 3 hypertension is the most common toxicity<br />
associated <strong>with</strong> bevacizumab treatment. Grade 3 hypertension<br />
is def<strong>in</strong>ed as hypertension requir<strong>in</strong>g the addition or modification<br />
of antihypertensive agents. The overall rate of grade 3<br />
hypertension <strong>in</strong> phase III/IV studies is 1%–18%. 5 Hypertension<br />
can occur at any time dur<strong>in</strong>g the course of treatment, and preexist<strong>in</strong>g<br />
hypertension does not predispose patients to grade 2/3<br />
hypertension. No deaths from bevacizumab-associated hypertension<br />
have been reported. More than 1% of patients have<br />
discont<strong>in</strong>ued bevacizumab therapy because of hypertension.<br />
Grade 4 hypertension is rare (s<strong>in</strong>gle case <strong>in</strong> breast cancer phase<br />
II study). Blood pressure is typically controlled <strong>with</strong> a s<strong>in</strong>gle<br />
antihypertensive agent.<br />
Treatment Guidel<strong>in</strong>es. <strong>Patients</strong> receiv<strong>in</strong>g bevacizumab<br />
should always be observed for the development or worsen<strong>in</strong>g of<br />
hypertension through frequent blood pressure measurements.<br />
We encourage daily home monitor<strong>in</strong>g, if possible. Blood pressure<br />
measurements should occur after the patient has been <strong>in</strong> a<br />
rest<strong>in</strong>g position for ≥ 5 m<strong>in</strong>utes. Repeat measurement of blood<br />
pressure for verification should be undertaken if the <strong>in</strong>itial<br />
read<strong>in</strong>g is ≥ 140 mm Hg systolic and/or ≥ 90 mm Hg diastolic.<br />
In most cases, a s<strong>in</strong>gle-agent antihypertensive can control<br />
hypertension. Data from the BRiTE trial showed that for patients<br />
<strong>with</strong>out basel<strong>in</strong>e hypertension, 55% needed one medication,<br />
38% needed two medications, and 8% needed three or<br />
more medications. 7<br />
The selection of an antihypertensive regimen should be left<br />
to the treat<strong>in</strong>g physician. Standard antihypertensive therapy,<br />
typically angiotens<strong>in</strong>-convert<strong>in</strong>g enzyme (ACE) <strong>in</strong>hibitors,<br />
beta-blockers, calcium channel blockers, or diuretics, can be<br />
used to control grade 3 hypertension, and bevacizumab can be<br />
cont<strong>in</strong>ued <strong>with</strong>out dose modification. We generally use ACE<br />
<strong>in</strong>hibitors, based on some aspects of the biology of VEGF <strong>in</strong>hibitors<br />
and the possibility of decreas<strong>in</strong>g the amount of prote<strong>in</strong>uria;<br />
however, standard guidel<strong>in</strong>es for the selection of antihypertensive<br />
medications are appropriate. In addition to a mechanistic<br />
rationale, diuretics should also be used cautiously to treat<br />
bevacizumab-related hypertension due to potential worsen<strong>in</strong>g<br />
of dehydration secondary to chemotherapy-<strong>in</strong>duced diarrhea.<br />
We generally practice as well as recommend assess<strong>in</strong>g hypertension<br />
and other toxicities accord<strong>in</strong>g to the National Cancer<br />
Institute–Common Toxicity Criteria (NCI–CTC) grad<strong>in</strong>g,<br />
as such an evaluation can help physicians to make a decision<br />
comparatively easily (Table 2). Several guidel<strong>in</strong>es for manag<strong>in</strong>g<br />
hypertension associated <strong>with</strong> bevacizumab follow:<br />
• <strong>Bevacizumab</strong> should not be <strong>in</strong>itiated <strong>in</strong> patients <strong>with</strong> uncontrolled<br />
hypertension.<br />
• Blood pressure should be measured at least every 2 to 3<br />
weeks <strong>in</strong> patients treated <strong>with</strong> bevacizumab.<br />
• Blood pressure monitor<strong>in</strong>g may be required at more frequent<br />
<strong>in</strong>tervals <strong>in</strong> patients who develop hypertension dur<strong>in</strong>g<br />
treatment.<br />
• Blood pressure monitor<strong>in</strong>g should cont<strong>in</strong>ue at regular<br />
<strong>in</strong>tervals <strong>in</strong> patients <strong>with</strong> bevacizumab-<strong>in</strong>duced or bevacizumab-exacerbated<br />
hypertension, even if they have discont<strong>in</strong>ued<br />
bevacizumab.<br />
• <strong>Bevacizumab</strong> should be suspended or permanently discont<strong>in</strong>ued<br />
if hypertension cannot be managed <strong>with</strong> standard<br />
oral antihypertensive agents. 9<br />
• <strong>Bevacizumab</strong> should be permanently discont<strong>in</strong>ued if a<br />
hypertensive crisis occurs.<br />
PROTEINURIA<br />
Incidence. Although the risk is m<strong>in</strong>imal, severe prote<strong>in</strong>uria<br />
can occur <strong>in</strong> a few patients secondary to bevacizumab. In the<br />
246 www.SupportiveOncology.net Th e Jo u r n a l o f Su p p o rt i v e On c o l o g y
Saif<br />
Table 2<br />
<strong>Bevacizumab</strong>-Associated Hypertension: Guidel<strong>in</strong>es for Dos<strong>in</strong>g and Schedule Modification<br />
Grade a DESCRIPTION MANAGEMENT<br />
Grade 1 • Asymptomatic, transient (< 24 hours) <strong>in</strong>crease <strong>in</strong> blood pressure by 20 mm Hg (diastolic) or to No action needed<br />
> 150/100 mm Hg if previously <strong>with</strong><strong>in</strong> normal limits; <strong>in</strong>tervention not <strong>in</strong>dicated<br />
• Pediatric: asymptomatic, transient (< 24 hours) <strong>in</strong>crease <strong>in</strong> blood pressure beyond upper limit<br />
of normal; <strong>in</strong>tervention not <strong>in</strong>dicated<br />
Grade 2 • Recurrent or persistent (≥ 24 hours) or symptomatic <strong>in</strong>crease by > 20 mm Hg (diastolic) or to No action needed<br />
> 150/100 mm Hg if previously <strong>with</strong><strong>in</strong> normal limits; monotherapy may be <strong>in</strong>dicated<br />
• Pediatric: recurrent or persistent (≥ 24 hours) <strong>in</strong>crease <strong>in</strong> blood pressure beyond upper limit<br />
of normal; monotherapy may be <strong>in</strong>dicated<br />
Grade 3 Requir<strong>in</strong>g more than one drug or more <strong>in</strong>tensive therapy than used previously If not controlled <strong>with</strong> medication,<br />
discont<strong>in</strong>ue bevacizumab<br />
Grade 4 Life-threaten<strong>in</strong>g consequences (eg, hypertensive crisis) Discont<strong>in</strong>ue bevacizumab<br />
a<br />
Grade based on National Cancer Institute–Common Toxicity Criteria, v 3.0<br />
Table 3<br />
<strong>Bevacizumab</strong>-Associated Prote<strong>in</strong>uria: Guidel<strong>in</strong>es for Dos<strong>in</strong>g and Schedule Modification<br />
Grade a DESCRIPTION MANAGEMENT<br />
Grade 1 ≥ 1 g of prote<strong>in</strong> or 0.15–1 g/24 h no action needed<br />
Grade 2 ≥ 2 to ≥ 3 g of prote<strong>in</strong> or > 1–3.5 g/24 h • Hold bevacizumab until prote<strong>in</strong>uria improves to ≤ 2 g of prote<strong>in</strong> per 24 hours<br />
• Discont<strong>in</strong>ue bevacizumab <strong>in</strong> a patient <strong>with</strong> > 2 g prote<strong>in</strong>uria per 24 hours that does not<br />
resolve <strong>with</strong><strong>in</strong> 3 months after hold<strong>in</strong>g bevacizumab<br />
• Workup for prote<strong>in</strong>uria, such as renal biopsy, should be considered<br />
Grade 3 ≥ 4 g of prote<strong>in</strong> or > 3.5 g/24 h Discont<strong>in</strong>ue bevacizumab<br />
Grade 4 Nephrotic syndrome Discont<strong>in</strong>ue bevacizumab<br />
a<br />
Grade based on National Cancer Institute–Common Toxicity Criteria, v 3.0<br />
randomized trial by Hurwitz et al as well as <strong>in</strong> TREE-2, the<br />
<strong>in</strong>cidence of grade 3 prote<strong>in</strong>uria was the same <strong>in</strong> both groups. 1,2<br />
Similarly, <strong>in</strong> E3200, the risk of grade 3 prote<strong>in</strong>uria was 1% or<br />
less <strong>in</strong> the groups that received FOLFOX/bevacizumab. 6 There<br />
appears to be no correlation between prote<strong>in</strong>uria and hypertension<br />
<strong>in</strong> patients treated <strong>with</strong> bevacizumab.<br />
Nephrotic syndrome did occur <strong>in</strong> 5 of 1,032 patients who<br />
were treated <strong>with</strong> bevacizumab, accord<strong>in</strong>g to data pooled from<br />
several <strong>in</strong>dustry-sponsored studies. 10 The renal dysfunction<br />
required dialysis <strong>in</strong> one patient, and a second patient <strong>with</strong><br />
nephrotic syndrome died. In the three rema<strong>in</strong><strong>in</strong>g patients, the<br />
amount of prote<strong>in</strong>uria decreased <strong>with</strong> time but did not normalize.<br />
On the other hand, no cases of nephrotic syndrome were<br />
reported among 1,960 patients <strong>in</strong> the BRiTE registry study. 7<br />
Monitor<strong>in</strong>g. There is no clear consensus on the monitor<strong>in</strong>g<br />
of prote<strong>in</strong>uria, and recommendations vary by <strong>in</strong>vestigators.<br />
However, we suggest that prote<strong>in</strong>uria be evaluated at basel<strong>in</strong>e<br />
and then monitored regularly throughout treatment.<br />
• <strong>Patients</strong> treated <strong>with</strong> bevacizumab should be monitored<br />
for prote<strong>in</strong>uria by us<strong>in</strong>g the ratio of ur<strong>in</strong>e prote<strong>in</strong> to<br />
creat<strong>in</strong><strong>in</strong>e. This <strong>in</strong>dex of prote<strong>in</strong>uria is commonly used <strong>in</strong> the<br />
nephrology literature and correlates well <strong>with</strong> 24-hour prote<strong>in</strong><br />
excretion. Us<strong>in</strong>g this ratio also avoids the <strong>in</strong>accuracies<br />
associated <strong>with</strong> dipstick ur<strong>in</strong>e assays and the <strong>in</strong>convenience<br />
of 24-hour collections.<br />
• If spot ur<strong>in</strong>e prote<strong>in</strong> tests are not available, dipstick ur<strong>in</strong>e<br />
assays at regular <strong>in</strong>tervals are useful. The frequency of test<strong>in</strong>g<br />
should be every 2–8 weeks (before each dose and/or at each restag<strong>in</strong>g),<br />
accord<strong>in</strong>g to the severity of the previous prote<strong>in</strong>uria<br />
and any other relevant risk factors or considerations.<br />
• Dipstick values 2+ or higher should be confirmed by the<br />
ratio of ur<strong>in</strong>e prote<strong>in</strong> to creat<strong>in</strong><strong>in</strong>e or 24-hour collection.<br />
Treatment Guidel<strong>in</strong>es. Aga<strong>in</strong>, we encourage oncologists to<br />
follow the NCI–CTC grad<strong>in</strong>g to assess and manage prote<strong>in</strong>uria<br />
(Table 3).<br />
WOUND HEALING<br />
Incidence. Wound heal<strong>in</strong>g complications have been described<br />
<strong>in</strong> patients who underwent primary cancer surgery<br />
<strong>with</strong><strong>in</strong> 28–60 days before start<strong>in</strong>g bevacizumab treatment and<br />
while on bevacizumab treatment. 1 Sixty-day postoperative adverse<br />
events that were recorded <strong>in</strong>cluded abnormal heal<strong>in</strong>g,<br />
wound dehiscence, delayed wound heal<strong>in</strong>g, bowel perforation,<br />
fistula, abscess, and hemorrhage. In the prelim<strong>in</strong>ary BRiTE<br />
analysis, 1% of the patients had postoperative complications. 7<br />
Treatment Guidel<strong>in</strong>es. <strong>Patients</strong> who undergo any <strong>in</strong>vasive<br />
procedure while receiv<strong>in</strong>g bevacizumab might encounter problems<br />
<strong>with</strong> wound heal<strong>in</strong>g (Table 4). 11 Therefore, any known<br />
upcom<strong>in</strong>g procedures, such as biopsies or venous access system<br />
placement, should be performed and the wound healed before<br />
<strong>in</strong>itiat<strong>in</strong>g therapy <strong>with</strong> bevacizumab.<br />
There have been limited data regard<strong>in</strong>g the safety of venous<br />
Vo l u m e 7, Nu m b e r 6 ■ November/December 2009<br />
www.SupportiveOncology.net<br />
247
<strong>Manag<strong>in</strong>g</strong> <strong>Bevacizumab</strong>-<strong>Related</strong> <strong>Toxicities</strong> <strong>in</strong> <strong>Patients</strong> <strong>with</strong> Colorectal Cancer<br />
Table 4<br />
<strong>Bevacizumab</strong>-Associated Wound Heal<strong>in</strong>g Complications (Non<strong>in</strong>fectious): Guidel<strong>in</strong>es for Dos<strong>in</strong>g<br />
and Schedule Modification<br />
Grade a DESCRIPTION MANAGEMENT<br />
Grade 1 Incisional separation of ≤ 25% of wound, no deeper than superficial fascia no action needed<br />
Grade 2 Incisional separation > 25% of wound <strong>with</strong> local care; asymptomatic hernia no action needed<br />
Grade 3 Symptomatic hernia <strong>with</strong>out evidence of strangulation; fascial disruption/dehiscence <strong>with</strong>out evisceration; Discont<strong>in</strong>ue bevacizumab<br />
primary wound closure or revision by operative <strong>in</strong>tervention <strong>in</strong>dicated; hospitalization or hyperbaric oxygen<br />
<strong>in</strong>dicated<br />
Grade 4 Symptomatic hernia <strong>with</strong> evidence of strangulation; fascial disruption <strong>with</strong> evisceration; major reconstruction Discont<strong>in</strong>ue bevacizumab<br />
flap, graft<strong>in</strong>g, resection, or amputation <strong>in</strong>dicated<br />
a<br />
Grade based on National Cancer Institute–Common Toxicity Criteria, v 3.0<br />
access catheter <strong>in</strong>sertion before bevacizumab treatment. An<br />
analysis of 534 patients who had catheters placed before treatment<br />
<strong>with</strong> bevacizumab and 5-FU or capecitab<strong>in</strong>e-based therapy<br />
showed that the risk of wound heal<strong>in</strong>g complications was<br />
low (1.1%). 12 There were no bleed<strong>in</strong>g events, and the catheterrelated<br />
thrombosis rate was 1.7% among all patients and 3.3%<br />
among those <strong>in</strong> whom the catheter was <strong>in</strong>serted <strong>with</strong><strong>in</strong> 7 days. 12<br />
In the past 2 years, we have had more than 18 patients receive<br />
bevacizumab <strong>with</strong><strong>in</strong> 24 hours after placement of a catheter, and<br />
not a s<strong>in</strong>gle complication has been witnessed to date.<br />
Further guidel<strong>in</strong>es regard<strong>in</strong>g bevacizumab-associated<br />
wound heal<strong>in</strong>g complications follow:<br />
• If a patient has been on bevacizumab, it should be held<br />
for 30–60 days before elective surgery, such as resection of metastasis<br />
or other procedures, is performed.<br />
• For emergency surgery, the patient, surgeon, and nurs<strong>in</strong>g<br />
staff should be aware of the possible risks of bevacizumab.<br />
• In general, clear communication <strong>with</strong> the surgeon is<br />
necessary, especially when a comb<strong>in</strong>ed-modality approach to<br />
care is be<strong>in</strong>g taken.<br />
GI PERFORATION<br />
Incidence. GI perforation was first observed <strong>in</strong> the pivotal<br />
phase III trial, <strong>in</strong> which six events occurred <strong>in</strong> the bevacizumab<br />
group (1.5%), compared <strong>with</strong> no events <strong>in</strong> the control group. 1<br />
S<strong>in</strong>ce then, similar rates of GI perforation have been observed<br />
<strong>in</strong> other large trials, as well as <strong>in</strong> the BRiTE study. 7<br />
The common cl<strong>in</strong>ical and radiologic manifestations of patients<br />
<strong>with</strong> GI perforations while on bevacizumab <strong>in</strong>clude subdiaphragmatic<br />
air on a kidney-ureter-bladder radiograph not<br />
Table 5<br />
Arterial Thromboembolism Events<br />
Associated <strong>with</strong> <strong>Bevacizumab</strong><br />
EVENT IFL + BEVACIZUMAB IFL + PLACEBO<br />
Cerebrovascular events 4 patients 0 patients<br />
Myocardial <strong>in</strong>farction 6 patients 3 patients<br />
Deep venous thrombosis 34 patients 19 patients<br />
Intra-abdom<strong>in</strong>al thrombosis 13 patients 5 patients<br />
IFL = ir<strong>in</strong>otecan/5-fluorouracil/leucovor<strong>in</strong><br />
requir<strong>in</strong>g surgery; a perforated stomach ulcer; colonic perforation<br />
associated <strong>with</strong> carc<strong>in</strong>omatosis or an abdom<strong>in</strong>al abscess;<br />
a small bowel obstruction, abscess, and perforated transverse<br />
colon; and bowel obstruction, ileal necrosis, and perforation.<br />
There seems to be no apparent pattern <strong>in</strong> the location of the<br />
perforation or its presentation.<br />
It is important to note that GI perforation can occur at any<br />
time while a patient is on therapy <strong>with</strong> bevacizumab. BRiTE<br />
data showed that half the perforations occur after 3 months<br />
of therapy and that almost 25% occur after 6 months of treatment.<br />
Similarly, <strong>in</strong> E3200, the <strong>in</strong>cidence of bowel perforations<br />
<strong>in</strong> each bevacizumab-conta<strong>in</strong><strong>in</strong>g arm was 1%. 6<br />
Risk Factors. GI perforation is a rare but potentially lifethreaten<strong>in</strong>g<br />
toxicity of bevacizumab. Sugrue et al evaluated<br />
possible risk factors for GI perforations <strong>in</strong> patients <strong>with</strong> metastatic<br />
CRC receiv<strong>in</strong>g bevacizumab plus chemotherapy <strong>in</strong> the<br />
BRiTE study. 13 The rate of GI perforations was similar among<br />
patients <strong>with</strong> or <strong>with</strong>out a basel<strong>in</strong>e history of peptic ulcer disease<br />
(1.8% vs 1.7%), diverticulosis (1.8% vs 1.7%), or chronic<br />
use of acetylsalicylic acid (ASA) or nonsteroidal anti-<strong>in</strong>flammatory<br />
drugs (0% vs 1.7%). 9 There appeared to be a higher<br />
<strong>in</strong>cidence of GI perforations <strong>in</strong> patients <strong>with</strong> a primary tumor<br />
<strong>in</strong>tact (3.3% vs 1.4%), a recent history of sigmoidoscopy or<br />
colonoscopy (2.6% vs 1.5%), or previous adjuvant radiation<br />
therapy (2.3% vs 1.6%). However, it is necessary to confirm<br />
these prelim<strong>in</strong>ary f<strong>in</strong>d<strong>in</strong>gs <strong>with</strong> multivariate analyses.<br />
The randomized phase III study also <strong>in</strong>dicated that the risk<br />
of GI perforation is <strong>in</strong>creased among patients who have surgery<br />
<strong>with</strong><strong>in</strong> 60 days before receiv<strong>in</strong>g bevacizumab and among patients<br />
who have surgery while receiv<strong>in</strong>g bevacizumab. 1 Therefore, a high<br />
<strong>in</strong>dex of suspicion should be reserved for patients <strong>with</strong> vomit<strong>in</strong>g,<br />
constipation, and abdom<strong>in</strong>al pa<strong>in</strong>. Any concern<strong>in</strong>g symptoms<br />
should be followed by physical exam<strong>in</strong>ation and radiographic imag<strong>in</strong>g.<br />
Furthermore, the treatment team’s nurses, physicians assistants,<br />
and fellows should be educated about GI perforations <strong>in</strong><br />
these patients to promptly attend to such an emergency.<br />
Treatment Guidel<strong>in</strong>es. The use of bevacizumab before and<br />
after surgery requires a multidiscipl<strong>in</strong>ary approach, <strong>with</strong> close,<br />
clear communication between the surgeon and the oncologist.<br />
For elective operations, bevacizumab should be discont<strong>in</strong>ued<br />
at least 30–60 days before a scheduled surgery. How<br />
long to hold bevacizumab is unknown and may be related to<br />
248 www.SupportiveOncology.net Th e Jo u r n a l o f Su p p o rt i v e On c o l o g y
Saif<br />
the difference <strong>in</strong> peripheral half-life versus the tissue half-life.<br />
However, the long half-life of 20 days should be taken <strong>in</strong>to account.<br />
After surgery, bevacizumab should be held for a period<br />
of 30–60 days, and the surgical wound should be completely<br />
healed before <strong>in</strong>itiat<strong>in</strong>g treatment. This practice of ours has<br />
been adapted from cl<strong>in</strong>ical trials. In cases of emergency procedures,<br />
bevacizumab should be held and patients followed<br />
closely for complications. 14<br />
Any NCI–CTC grade of GI perforation warrants discont<strong>in</strong>uation<br />
of bevacizumab.<br />
VENOUS AND ARTERIAL THROMBOTIC EVENTS<br />
Incidence. In the randomized, double-bl<strong>in</strong>d, phase III study<br />
evaluat<strong>in</strong>g bevacizumab <strong>in</strong> comb<strong>in</strong>ation <strong>with</strong> IFL as first-l<strong>in</strong>e<br />
treatment of metastatic CRC, the <strong>in</strong>cidence of all venous and<br />
arterial thrombotic events was 19.4% <strong>in</strong> the IFL/bevacizumab<br />
group and 16.2% <strong>in</strong> the IFL plus placebo group (P = 0.26). 1<br />
The <strong>in</strong>cidence of grade 3/4 thromboembolic events <strong>in</strong> patients<br />
receiv<strong>in</strong>g IFL/bevacizumab as compared <strong>with</strong> patients receiv<strong>in</strong>g<br />
IFL plus placebo is shown <strong>in</strong> Table 5.<br />
A pooled analysis was conducted from five randomized trials<br />
(CRC, non–small-cell lung cancer [NSCLC], and breast cancer)<br />
that <strong>in</strong>cluded 1,745 patients: AVF0757g (lung), AVF0780g<br />
(CRC), AVF2119g (breast), AVF2192g (CRC), and AVF2107g<br />
(CRC). 15 The rate of arterial thromboembolic events (ATEs) <strong>in</strong><br />
the chemotherapy-only group was 1.9%, whereas the rate <strong>in</strong><br />
the bevacizumab plus chemotherapy group was 4.4%.<br />
A multivariate risk analysis identified two risk factors associated<br />
<strong>with</strong> ATE 16 : previous ATE and age > 65 years. Other<br />
risk factors might <strong>in</strong>clude hypertension and smok<strong>in</strong>g. It is notable,<br />
however, that overall, patients <strong>with</strong> these risk factors still<br />
showed substantial cl<strong>in</strong>ical benefit <strong>in</strong> the pivotal phase III trial.<br />
<strong>Patients</strong> aged ≥ 65 years had a 43% reduction <strong>in</strong> the risk of<br />
disease progression and a 39% reduction <strong>in</strong> the risk of death,<br />
and patients <strong>with</strong> a history of arterial thromboembolism had<br />
a 39% reduction <strong>in</strong> the risk of disease progression and a 62%<br />
reduction <strong>in</strong> the risk of death.<br />
Although patients aged > 65 years have an <strong>in</strong>creased risk of<br />
arterial thromboembolism, oncologists must use their own medical<br />
judgment <strong>in</strong> assess<strong>in</strong>g the overall risk/benefit of bevacizumab<br />
therapy. 16 In the pivotal bevacizumab trial, there were 271 patients<br />
aged ≥ 65 years. 1 This group of patients cont<strong>in</strong>ued to have<br />
a benefit <strong>in</strong> terms of PFS (HR, 0.57) and OS (HR, 0.61), despite<br />
the higher risk of ATEs. In addition, patients who had a history<br />
of arterial events and were aged > 65 years also had a PFS and<br />
OS benefit, <strong>with</strong> HRs of 0.55 and 0.59, respectively. The data<br />
on the benefit of bevacizumab <strong>in</strong> patients aged > 65 years are<br />
important, but the <strong>in</strong>teraction of age and previous ATEs must be<br />
considered <strong>in</strong> certa<strong>in</strong> patients (eight-fold <strong>in</strong>crease <strong>in</strong> risk), and<br />
therefore therapy <strong>with</strong> bevacizumab must be <strong>in</strong>dividualized.<br />
Table 6<br />
<strong>Bevacizumab</strong>-Associated Thrombosis/Thromboembolism: Guidel<strong>in</strong>es for Dos<strong>in</strong>g and Schedule Modification<br />
Grade a DESCRIPTION MANAGEMENT<br />
Grade 1 (venous) Not applicable –<br />
Grade 2 (venous) Deep ve<strong>in</strong> thrombosis or cardiac thrombosis; No action needed<br />
<strong>in</strong>tervention (eg, anticoagulation, lysis, filter,<br />
<strong>in</strong>vasive procedure) not <strong>in</strong>dicated<br />
Grade 3 (venous) Deep ve<strong>in</strong> thrombosis or cardiac thrombosis; Withhold bevacizumab<br />
<strong>in</strong>tervention (eg, anticoagulation, lysis, filter, If the planned duration of therapeutic-dose anticoagulant therapy b<br />
<strong>in</strong>vasive procedure) <strong>in</strong>dicated<br />
is ≤ 2 weeks, bevacizumab should be <strong>with</strong>held until the period of<br />
therapeutic-dose anticoagulant therapy is over.<br />
If the planned duration of therapeutic-dose anticoagulant therapy b<br />
is > 2 weeks, bevacizumab should be <strong>with</strong>held for 2 weeks and then<br />
may be resumed dur<strong>in</strong>g the period of therapeutic-dose anticoagulant<br />
therapy as soon as all of the follow<strong>in</strong>g criteria are met:<br />
• The patient must be on a stable dose of anticoagulant medication<br />
and, if on warfar<strong>in</strong>, have an INR <strong>with</strong><strong>in</strong> the target range (usually between<br />
2 and 3) before restart<strong>in</strong>g study drug treatment<br />
• The patient has no history of grade 3/4 hemorrhagic events before<br />
restart<strong>in</strong>g bevacizumab<br />
• The patient has no evidence of tumor <strong>in</strong>vad<strong>in</strong>g or abutt<strong>in</strong>g major<br />
blood vessels on any previous CT scan<br />
Grade 4 (venous) Embolic event, <strong>in</strong>clud<strong>in</strong>g pulmonary embolism Same as for grade 3<br />
or life-threaten<strong>in</strong>g thrombus<br />
Incidentally discovered pulmonary embolus, Same as for grade 3<br />
first occurrence<br />
Symptomatic grade 4 venous thromboembolic Discont<strong>in</strong>ue bevacizumab<br />
event, first occurrence<br />
Any grade of arterial – Discont<strong>in</strong>ue bevacizumab<br />
thromboembolic event<br />
INR = <strong>in</strong>ternational normalized ratio<br />
a<br />
Grade based on National Cancer Institute–Common Toxicity Criteria, v 3.0<br />
b<br />
Def<strong>in</strong>ed as a dose titrated to ma<strong>in</strong>ta<strong>in</strong> an INR of ≥ 1.5 for warfar<strong>in</strong> or its equivalent for other anticoagulant medications<br />
Vo l u m e 7, Nu m b e r 6 ■ November/December 2009<br />
www.SupportiveOncology.net<br />
249
<strong>Manag<strong>in</strong>g</strong> <strong>Bevacizumab</strong>-<strong>Related</strong> <strong>Toxicities</strong> <strong>in</strong> <strong>Patients</strong> <strong>with</strong> Colorectal Cancer<br />
Table 7<br />
<strong>Bevacizumab</strong>-Associated Hemorrhage: Guidel<strong>in</strong>es for Dos<strong>in</strong>g and Schedule Modification<br />
Grade a DESCRIPTION MANAGEMENT<br />
Grade 1 Mild, <strong>in</strong>tervention (other than iron supplements) not <strong>in</strong>dicated no action needed<br />
Grade 2 Symptomatic and medical <strong>in</strong>tervention or m<strong>in</strong>or cauterization <strong>in</strong>dicated no action needed<br />
Grade 3 Transfusion, <strong>in</strong>terventional radiology, endoscopic, or operative <strong>in</strong>tervention <strong>in</strong>dicated; radiation therapy Discont<strong>in</strong>ue bevacizumab<br />
(ie, hemostasis of bleed<strong>in</strong>g site)<br />
a<br />
Grade based on National Cancer Institute–Common Toxicity Criteria, v 3.0<br />
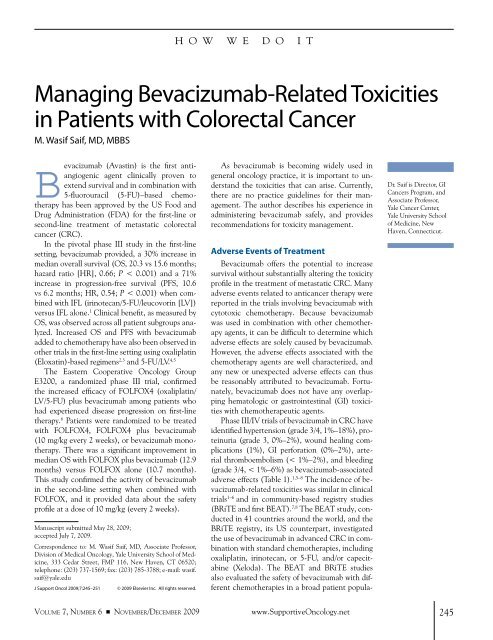
Figure 1 Fluid-Attenuated Inversion Recovery MRI<br />
Scan Taken the Day of Neurologic Symptom<br />
Development Show<strong>in</strong>g a Bilateral Occipital<br />
and Posterior Parietal Abnormality<br />
Reproduced, <strong>with</strong> permission, from Allen JA, Adlakha A, Bergethon PR.<br />
Reversible posterior leukoencephalopathy syndrome after bevacizumab/<br />
FOLFIRI regimen for metastatic colon cancer. Arch Neurol 2006;63:1475–1478<br />
Treatment Guidel<strong>in</strong>es. A high degree of suspicion should be<br />
developed <strong>in</strong> the presence of cl<strong>in</strong>ical manifestations (Table 6).<br />
<strong>Patients</strong> <strong>with</strong> a severe ATE (any grade) dur<strong>in</strong>g bevacizumab<br />
treatment should discont<strong>in</strong>ue treatment permanently.<br />
Many patients <strong>with</strong> a previous ATE are rout<strong>in</strong>ely treated <strong>with</strong><br />
low-dose ASA. When these patients entered cl<strong>in</strong>ical trials of bevacizumab,<br />
they were able to cont<strong>in</strong>ue low-dose ASA therapy<br />
<strong>with</strong>out any evidence of an <strong>in</strong>creased risk of bleed<strong>in</strong>g. 17 Because<br />
of the limited number of patients on ASA who developed a new<br />
ATE dur<strong>in</strong>g bevacizumab therapy, there are <strong>in</strong>sufficient data at<br />
this time to determ<strong>in</strong>e whether low-dose ASA reduces the risk<br />
of future events while on bevacizumab. This is an important topic<br />
for future study because of the number of patients aged > 65<br />
years who could potentially benefit from bevacizumab therapy.<br />
The use of high-dose ASA cannot be recommended because of<br />
the lack of safety data. An upcom<strong>in</strong>g trial will evaluate whether<br />
the addition of low-dose warfar<strong>in</strong> therapy can safely prevent<br />
thrombotic and thromboembolic complications.<br />
BLEEDING/HEMORRHAGE<br />
Incidence. Epistaxis was the common bleed<strong>in</strong>g event encountered<br />
<strong>in</strong> the phase II dose-f<strong>in</strong>d<strong>in</strong>g study of bevacizumab (46%,<br />
5 mg/kg; 53%, 10 mg/kg, compared <strong>with</strong> FU/LV (11%). Most<br />
epistaxis events were transient (< 5 m<strong>in</strong>utes). Although three<br />
patients <strong>in</strong> the 10-mg/kg arm had grade 3/4 bleed<strong>in</strong>g, the relationship<br />
to the bevacizumab dose was unclear. No grade 3/4<br />
bleed<strong>in</strong>g occurred <strong>in</strong> the 5-mg/kg group or <strong>in</strong> the control group.<br />
In the phase III pivotal trial, there was not a significantly<br />
<strong>in</strong>creased risk of grade 3/4 bleed<strong>in</strong>g <strong>with</strong> the addition of bevacizumab<br />
(5 mg/kg) to chemotherapy. 1 In E3200, which used<br />
the 10-mg/kg dose of bevacizumab, there was only a marg<strong>in</strong>al<br />
<strong>in</strong>crease <strong>in</strong> bleed<strong>in</strong>g of 1%, compared <strong>with</strong> < 1% for the control<br />
arm <strong>with</strong>out bevacizumab. However, <strong>in</strong> the first BEAT study,<br />
although the <strong>in</strong>cidence of serious bleed<strong>in</strong>g events was only<br />
1.3%, there were eight deaths from bleed<strong>in</strong>g (three of these patients<br />
also had GI perforation). 8 The BRiTE data registered a<br />
2.2% rate of serious bleed<strong>in</strong>g events.<br />
A notable toxicity <strong>in</strong> the E4599 NSCLC study was the occurrence<br />
of two deaths from hemoptysis, prompt<strong>in</strong>g the exclusion<br />
of patients <strong>with</strong> a history of significant hemoptysis and centrally<br />
located squamous cell tumors from receiv<strong>in</strong>g bevacizumab. 18<br />
Treatment Guidel<strong>in</strong>es. Among patients <strong>with</strong> colon cancer who<br />
experience grade 3 hemorrhage while receiv<strong>in</strong>g full-dose anticoagulation<br />
(<strong>with</strong><strong>in</strong> the therapeutic range or <strong>in</strong>creased range), bevacizumab<br />
should be discont<strong>in</strong>ued (Table 7). For patients <strong>with</strong><br />
grade 3 hemorrhage who are not receiv<strong>in</strong>g full-dose anticoagulation,<br />
bevacizumab should be held until the bleed<strong>in</strong>g has resolved,<br />
there is no coagulation disorder that would <strong>in</strong>crease the<br />
risk of subsequent bleed<strong>in</strong>g, and there is no anatomic or pathologic<br />
condition that <strong>in</strong>creases the risk of hemorrhage. If the patient<br />
experiences a repeat grade 3 or a new grade 4 hemorrhagic<br />
event, bevacizumab should be permanently discont<strong>in</strong>ued.<br />
REVERSIBLE POSTERIOR<br />
LEUKOENCEPHALOPATHY SYNDROME<br />
Incidence and Diagnosis. The prescrib<strong>in</strong>g <strong>in</strong>formation for bevacizumab<br />
has been updated to <strong>in</strong>clude warn<strong>in</strong>gs regard<strong>in</strong>g a rare<br />
bra<strong>in</strong>-capillary leak syndrome called reversible posterior leuko-<br />
250 www.SupportiveOncology.net Th e Jo u r n a l o f Su p p o rt i v e On c o l o g y
Saif<br />
encephalopathy syndrome (RPLS). Cl<strong>in</strong>ical studies and postmarket<strong>in</strong>g<br />
data reveal that RPLS occurs at a rate of < 0.1%. 19<br />
Signs and symptoms of RPLS <strong>in</strong>clude headache, seizure, lethargy,<br />
confusion, bl<strong>in</strong>dness, and hypertension. It is hypothesized<br />
that <strong>in</strong> these patients, bevacizumab might have <strong>in</strong>duced vasospasm<br />
that coupled <strong>with</strong> hypertension led to RPLS.<br />
The diagnosis of RPLS is made by cl<strong>in</strong>ical and radiologic<br />
f<strong>in</strong>d<strong>in</strong>gs. MRI reveals patchy areas of <strong>in</strong>creased fluid-attenuated<br />
<strong>in</strong>version recovery signal <strong>in</strong>tensity <strong>in</strong> the bra<strong>in</strong>, as shown <strong>in</strong><br />
Figure 1, consistent <strong>with</strong> RPLS. Cl<strong>in</strong>icians should be aware of<br />
this potential complication and should control blood pressure<br />
strictly dur<strong>in</strong>g and after bevacizumab <strong>in</strong>fusion.<br />
Treatment Guidel<strong>in</strong>es. <strong>Bevacizumab</strong> should be discont<strong>in</strong>ued <strong>in</strong><br />
patients <strong>with</strong> MRI-confirmed RPLS, and hypertension should be<br />
treated if necessary. Controll<strong>in</strong>g hypertension and discont<strong>in</strong>u<strong>in</strong>g<br />
the offend<strong>in</strong>g agent appear to help reverse the complication.<br />
Conclusion<br />
<strong>Bevacizumab</strong>, the first FDA-approved VEGF-targeted<br />
agent, significantly <strong>in</strong>creases PFS and OS (first-l<strong>in</strong>e and<br />
second-l<strong>in</strong>e) <strong>in</strong> comb<strong>in</strong>ation <strong>with</strong> standard chemotherapy<br />
regimens <strong>in</strong> patients <strong>with</strong> metastatic CRC. Phase II/III trials<br />
have demonstrated the efficacy of bevacizumab <strong>in</strong> comb<strong>in</strong>ation<br />
<strong>with</strong> 5-FU/LV, IFL, FOLFOX, FOLFIRI (5-FU/LV/<br />
ir<strong>in</strong>otecan), CAPOX (capecitab<strong>in</strong>e/oxaliplat<strong>in</strong>), and cetuximab<br />
(Erbitux)/bevacizumab. The efficacy and toxicity of<br />
bevacizumab have primarily been evaluated <strong>in</strong> patients<br />
<strong>with</strong> advanced disease, and the prelim<strong>in</strong>ary results of the<br />
National Surgical Adjuvant Breast and Bowel Project C08<br />
study <strong>in</strong> adjvant treatment of stage II and III CRC showed<br />
no unexpected side effects. However, long-term follow-up<br />
cont<strong>in</strong>ues.<br />
As current trials mature, safety data will be clarified further,<br />
and specific guidel<strong>in</strong>es for the management of bevacizumabrelated<br />
toxicities will become more detailed. As the use of<br />
bevacizumab <strong>in</strong>creases, more <strong>in</strong>formation will be necessary to<br />
identify specific factors plac<strong>in</strong>g patients at higher risk of complications.<br />
The key to adm<strong>in</strong>ister<strong>in</strong>g bevacizumab treatment<br />
safely will be through education of patients, nurses, and other<br />
healthcare providers.<br />
Conflicts of <strong>in</strong>terest: Dr. Saif is on the speakers bureau of Genentech.<br />
References<br />
PubMed ID <strong>in</strong> brackets<br />
1. Hurwitz H, Fehrenbacher L, Novotny W, et<br />
al. <strong>Bevacizumab</strong> plus ir<strong>in</strong>otecan, fluorouracil, and<br />
leucovor<strong>in</strong> for metastatic colorectal cancer. N Engl J<br />
Med 2004;350:2335–2342.[15175435]<br />
2. Hochster HS, Hart LL, Ramanathan RK,<br />
Ha<strong>in</strong>sworth JD, Hedrick EE, Childs BH. Safety and<br />
efficacy of oxaliplat<strong>in</strong>/fluoropyrimid<strong>in</strong>e regimens<br />
<strong>with</strong> or <strong>with</strong>out bevacizumab as first-l<strong>in</strong>e treatment<br />
of metastatic colorectal cancer: f<strong>in</strong>al analysis of the<br />
TREE study. J Cl<strong>in</strong> Oncol 2006;24(18S):3510.<br />
3. Saltz L, Clarke S, Diaz-Rubio E, et al.<br />
<strong>Bevacizumab</strong> (Bev) <strong>in</strong> comb<strong>in</strong>ation <strong>with</strong> XELOX or<br />
FOLFOX4: updated efficacy results from XELOX-1/<br />
NO16966, a randomized phase III trial <strong>in</strong> firstl<strong>in</strong>e<br />
metastatic colorectal cancer. J Cl<strong>in</strong> Oncol<br />
2007;25(18S):4028.<br />
4. Kabb<strong>in</strong>avar FF, Hambleton J, Mass RD, Hurwitz<br />
HI, Bergsland E, Sarkar S. Comb<strong>in</strong>ed analysis of efficacy:<br />
the addition of bevacizumab to fluorouracil/leucovor<strong>in</strong><br />
improves survival for patients <strong>with</strong> metastatic<br />
colorectal cancer. J Cl<strong>in</strong> Oncol 2005;23:3706–3712.<br />
[15867200]<br />
5. Hurwitz HI, Fehrenbacher L, Ha<strong>in</strong>sworth JD, et<br />
al. <strong>Bevacizumab</strong> <strong>in</strong> comb<strong>in</strong>ation <strong>with</strong> fluorouracil and<br />
leucovor<strong>in</strong>: an active regimen for first-l<strong>in</strong>e metastatic<br />
colorectal cancer. J Cl<strong>in</strong> Oncol 2005;23:3502–3508.<br />
[15908660]<br />
6. Giantonio BJ, Catalano PJ, Meropol NJ, et al.<br />
High-dose bevacizumab improves survival when<br />
comb<strong>in</strong>ed <strong>with</strong> FOLFOX4 <strong>in</strong> previously treated advanced<br />
colorectal cancer: results from the Eastern<br />
Cooperative Oncology Group (ECOG) study E3200. J<br />
Cl<strong>in</strong> Oncol 2005;23(16S):2.<br />
7. Hedrick E, Kozloff M, Ha<strong>in</strong>sworth J, et al. Safety<br />
of bevacizumab plus chemotherapy as first-l<strong>in</strong>e treatment<br />
of patients <strong>with</strong> metastatic colorectal cancer:<br />
updated results from a large observational registry <strong>in</strong><br />
the US (BRiTE). J Cl<strong>in</strong> Oncol 2006;24(18S):3536.<br />
8. Van Cutsem E, Michael M, Berry S, et al.<br />
Prelim<strong>in</strong>ary safety of bevacizumab <strong>with</strong> first-l<strong>in</strong>e<br />
FOLFOX, CAPOX, FOLFIRI, and capecitab<strong>in</strong>e for<br />
mCRC: first BEAT trial. 2006 Gastro<strong>in</strong>test<strong>in</strong>al Cancers<br />
Symposium. Abstract 250.<br />
9. Saif MW, Mehra R. Incidence and management<br />
of bevacizumab-related toxicities <strong>in</strong> colorectal cancer.<br />
Expert Op<strong>in</strong> Drug Saf 2006;5:553–566.[16774493]<br />
10. Avast<strong>in</strong> (bevacizumab) prescrib<strong>in</strong>g <strong>in</strong>formation.<br />
South San Francisco, CA: Genentech; 2006.<br />
11. Scappaticci F, Fehrenbacher L, Cartwright<br />
T, et al. Lack of effect of bevacizumab on wound<br />
heal<strong>in</strong>g/bleed<strong>in</strong>g complications when given 28-60<br />
days follow<strong>in</strong>g primary cancer surgery. J Cl<strong>in</strong> Oncol<br />
2004;22(14S):3530.<br />
12. Berry S, Michael M, Kretzschmar A, et al.<br />
Lack of effect of start<strong>in</strong>g bevacizumab shortly after<br />
venous access device implantation on wound heal<strong>in</strong>g/bleed<strong>in</strong>g<br />
complications: prelim<strong>in</strong>ary results from<br />
first BEAT. 2006 Gastro<strong>in</strong>test<strong>in</strong>al Cancers Symposium.<br />
Abstract 245.<br />
13. Sugrue M, Kozloff M, Ha<strong>in</strong>sworth J, et al.<br />
Risk factors for gastro<strong>in</strong>test<strong>in</strong>al perforations <strong>in</strong><br />
patients <strong>with</strong> metastatic colorectal cancer receiv<strong>in</strong>g<br />
bevacizumab plus chemotherapy. J Cl<strong>in</strong> Oncol<br />
2006;24(18S):3535.<br />
14. Saif MW, Elfiky A, Salem RR. Gastro<strong>in</strong>test<strong>in</strong>al<br />
perforation due to bevacizumab <strong>in</strong> colorectal cancer.<br />
Ann Surg Oncol 2007;14:1860–1869.[17356952]<br />
15. Gray R, Giantonio BJ, O’Dwyer PJ, et al.<br />
The safety of add<strong>in</strong>g angiogenesis <strong>in</strong>hibition <strong>in</strong>to<br />
treatment for colorectal, breast, and lung cancer:<br />
the Eastern Cooperative Oncology Group’s (ECOG)<br />
experience <strong>with</strong> bevacizumab (anti-VEGF). Proc Am<br />
Soc Cl<strong>in</strong> Oncol 2003;22:825.<br />
16. Skill<strong>in</strong>gs JR, Johnson DH, Miller K, et al.<br />
Arterial thromboembolic events (ATEs) <strong>in</strong> a pooled<br />
analysis of 5 randomized, controlled trials (RCTs) of<br />
bevacizumab (BV) <strong>with</strong> chemotherapy. J Cl<strong>in</strong> Oncol<br />
2005;23(16S):3019.<br />
17. Hambleton J, Skill<strong>in</strong>gs J, Kabb<strong>in</strong>avar F, et al.<br />
Safety of low-dose aspir<strong>in</strong> (ASA) <strong>in</strong> a pooled analysis<br />
of 3 randomized, controlled trials (RCTs) of bevacizumab<br />
(BV) <strong>with</strong> chemotherapy (CT) <strong>in</strong> patients (pts)<br />
<strong>with</strong> metastatic colorectal cancer (mCRC). J Cl<strong>in</strong> Oncol<br />
2005;23(16S):3554.<br />
18. Sandler AB, Gray R, Brahmer J, et al. Randomized<br />
phase II/III trial of paclitaxel plus carboplat<strong>in</strong> <strong>with</strong> or<br />
<strong>with</strong>out bevacizumab (NSC #704865) <strong>in</strong> patients <strong>with</strong><br />
advanced non-squamous non-small cell lung cancer<br />
(NSCLC): an Eastern Cooperative Oncology Group<br />
(ECOG) trial - E4599. J Cl<strong>in</strong> Oncol 2005;23(16S):4.<br />
19. Ozcan C, Wong SJ, Hari P. Reversible posterior<br />
leukoencephalopathy syndrome and bevacizumab.<br />
N Engl J Med 2006;354:980–982.[16514715]<br />
Vo l u m e 7, Nu m b e r 6 ■ November/December 2009<br />
www.SupportiveOncology.net<br />
251