Fiji Health Sector Situational Analysis 2008 - Pacific Health Voices
Fiji Health Sector Situational Analysis 2008 - Pacific Health Voices
Fiji Health Sector Situational Analysis 2008 - Pacific Health Voices
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
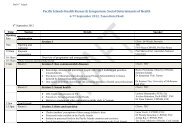
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
A SITUATIONAL ANALYSIS OF THE<br />
FIJI HEALTH SECTOR<br />
DECEMBER <strong>2008</strong><br />
1
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Table of Contents<br />
1. INTRODUCTION 1<br />
1.1. Background 1<br />
1.2. Objectives and Methodology used for this <strong>Situational</strong> <strong>Analysis</strong> 1<br />
2. THE FIJI SETTING 2<br />
2.1. <strong>Fiji</strong> - Demographic and Country overview. 2<br />
2.2. Economic and Political Situation. 3<br />
3. ORGANISATION, STAFFING AND FUNDING OF THE HEALTH SYSTEM. 4<br />
3.1. Overview of the MoH, its structure and organisation 4<br />
3.2. The Service Delivery Framework – a traditional model 4<br />
3.3. Staffing the <strong>Health</strong> System 6<br />
3.4. Financing the health system 10<br />
3.5. Planning and Managing the <strong>Health</strong> Care system, 16<br />
4. THE HEALTH OF THE PEOPLE OF FIJI. 17<br />
4.1. Key health Indicators 17<br />
4.2. Comparison with <strong>Pacific</strong> neighbours. 18<br />
4.3. Morbidity and Mortality. 18<br />
4.4. Key Lifestyle and other issues impacting on health of the people 20<br />
5. KEY ISSUES ARISING FROM THIS SITUATIONAL ANALYSIS 21<br />
5.1. Perception of the health services by the public. 22<br />
5.2. Changes in demographics and social behaviour require a rethink of the location, staffing and range of<br />
services provided by health facilities. 23<br />
5.3. Relatively Poor progress towards Achievement of <strong>Fiji</strong>’s MDGs and other designated KPIs. 25<br />
5.4. Old or non-functioning equipment impacts on service delivery 29<br />
5.5. Stock Outs of Essential drugs 30<br />
5.6. The importance of more focused planning and better use of management information systems. 31<br />
5.7. The health sector should be seen as being more than just the MoH. 32<br />
i
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
5.8. The Need for an Evidence based approach to Policy and Planning. 34<br />
6. POSSIBLE AREAS FOR ASSISTANCE BY DEVELOPMENT PARTNERS. 34<br />
6.1. Overview 34<br />
6.2. Highest Priority Areas for AusAID Support. 35<br />
6.3. Other Possible Areas for support by AusAID and other donors. 37<br />
ii
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
LIST of TABLES<br />
Table<br />
Table 1. 2004-5 survey of population by age and ethnicity 2<br />
Table 2. Distribution of <strong>Health</strong> Facilities by Division 5<br />
Table 3. Doctor and Nurse to Population Ratio by Division 2004 6<br />
Table 4. MoH Medical Cadre as at 31/10/08 7<br />
Table 5. ‘Exit’ of staff from MoH over 5 years (2003-7) 9<br />
Table 6. GDP, MoH budget and MoH budget as % of GDP, 1993-2005 11<br />
Table 7. Govt. budget, MoH allocation and budget share, MoH revenue, MoH<br />
revenue as proportion of expenditure and Per-Capita <strong>Health</strong> Expenditure 1986-<br />
2006<br />
Table 8. Pharmaceutical Budget (millions FJD) 2003-<strong>2008</strong> 12<br />
Table 9. MOH Biomedical budget allocations 2003-<strong>2008</strong> 13<br />
Table 10. Examples of main areas of support provided to the health sector<br />
through development partners<br />
Table 11. <strong>Fiji</strong>’s Key <strong>Health</strong> Indicators 17<br />
Table 12. Selected regional comparative indicators 17<br />
Table 13. The Ten major causes of Morbidity and Mortality in 2007 18<br />
Table 14. Major causes of Mortality by diagnostic group 1998-2001 and 2005 18<br />
Table 15. Major causes of Morbidity by diagnostic group 1998-2001 and 2005 18<br />
Table 16. <strong>Fiji</strong>’s MDG Targets by 2015 25<br />
Table 17. Progress towards achievement of MDGs 4 and 5 26<br />
Table 18. Trimester of First Antenatal visits 26<br />
Page<br />
12<br />
14<br />
iii
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
ACRONOMYS<br />
ADB<br />
AIDS<br />
AusAID<br />
CCF<br />
CSPF<br />
CWM<br />
EPI<br />
EU<br />
FHMR<br />
FJD<br />
FSMed<br />
FHSIP<br />
FSN<br />
DP<br />
GOA<br />
HDI<br />
HIV<br />
HMD<br />
HRH<br />
HMIS<br />
HRH<br />
IGOF<br />
IT<br />
JICA<br />
KPI<br />
MBBS<br />
MDG<br />
MCH<br />
M and E<br />
MOF& NP<br />
MMR<br />
MoH<br />
MOU<br />
NCD<br />
NGO<br />
NZAID<br />
PATIS<br />
PC &SS<br />
PDD<br />
PEP<br />
PET<br />
PIC<br />
PNG<br />
PO<br />
PPH<br />
PSC<br />
SPC<br />
SOPAC<br />
Asian Development Bank<br />
Acquired Immune deficiency Syndrome<br />
Australian Agency for International Development<br />
Consumer Council of <strong>Fiji</strong><br />
Clinical Services Planning Framework<br />
Colonial War memorial Hospital (Suva)<br />
Expanded Program on Immunisation<br />
European Union<br />
<strong>Fiji</strong> <strong>Health</strong> management Reform Project<br />
<strong>Fiji</strong> Dollar<br />
<strong>Fiji</strong> school of Medicine<br />
<strong>Fiji</strong> <strong>Health</strong> Services Improvement Program<br />
<strong>Fiji</strong> School of Nursing<br />
Gross Domestic Product<br />
Government of Australia<br />
Human Development Index of the UN<br />
Human Immunodeficiency Virus<br />
Hylanine Membrane Disease<br />
Human Resources for <strong>Health</strong><br />
<strong>Health</strong> management Information system<br />
Human Resources for <strong>Health</strong><br />
Interim Government of <strong>Fiji</strong><br />
Information Technology<br />
Japan International Cooperation Agency<br />
Key Performance Indicator<br />
Bachelor of Medicine Bachelor of Surgery<br />
Millennium Development Goals<br />
Maternal and Child <strong>Health</strong><br />
Monitoring and Evaluation<br />
Ministry of Finance and national Planning<br />
Maternal Mortality Rate<br />
Ministry of <strong>Health</strong><br />
Memorandum of Understanding<br />
Non Communicable Disease<br />
Non Government Organisation<br />
New Zealand Agency for International Development<br />
Patient Information system<br />
<strong>Pacific</strong> Counselling and Social Services<br />
Project Design Document<br />
Performance Enhancing Project<br />
Pre eclamptic toxaemia<br />
<strong>Pacific</strong> Island Country<br />
Papua New Guinea<br />
Project Officer<br />
post partum haemorrhage<br />
Public Service Commission<br />
Secretariat for the <strong>Pacific</strong> Community<br />
South <strong>Pacific</strong> Applied Geosciences Commission<br />
iv
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
TB<br />
TOR<br />
UN<br />
UNAIDS<br />
UNDP<br />
UNFPA<br />
UNICEF<br />
USP<br />
WHO<br />
Tuberculosis (the disease)<br />
Terms of Reference<br />
United National<br />
United Nations Program on HIV&AIDS<br />
United Nations Development Program<br />
United Nation Family Planning Agency<br />
United Nations Children Program<br />
University of the South <strong>Pacific</strong><br />
World <strong>Health</strong> Organisation<br />
v
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
EXECUTIVE SUMMARY<br />
Introduction<br />
The health sector remains a major pillar of Australia’s bilateral assistance to <strong>Fiji</strong>. AusAID’s<br />
current support to <strong>Fiji</strong> is given through the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> Improvement Program (FHSIP)<br />
and support for the <strong>Fiji</strong> School of Medicine (FSMed). In addition, AusAID currently provides<br />
support through a number of NGOs and a range of major regional programs in areas of<br />
HIV/AIDS; non-communicable diseases, support for equipment maintenance and biomedical<br />
engineering, visiting medical specialists and pandemic influenza preparedness.<br />
AusAID now wishes to build on the work of these programs and to move ahead with<br />
planning for a new program of support upon completion of the FHSIP. In order to make<br />
decisions on its future programs, AusAID now seeks to obtain good baseline data and<br />
analysis of the health sector situation, including progress towards achievement of the health<br />
related MDGs 4, 5, and 6.<br />
It has therefore commissioned this current situational analysis (the assessment) which will<br />
inform scoping and design of a future assistance program in health for <strong>Fiji</strong> sometime in mid-<br />
2009. The Objectives of this assessment are<br />
1. To provide a ‘snapshot’ of the current status of the health sector in <strong>Fiji</strong> from health<br />
service delivery and systems levels;<br />
2. To present and assess the state of health based on latest data and statistics, determine<br />
limitations of data and propose methodologies to enable tracking for MDGs and any<br />
future program support indicators;<br />
3. To identify opportunities and gaps for future AusAID programming, including<br />
strategic objectives and likely areas of impact.<br />
The assessment team visited <strong>Fiji</strong> from 29 th October to 18 th November. It visited health sector<br />
facilities and met with a wide range of government officials, international agencies, other<br />
development partners, training institutions and NGOs. The results of this “snapshot” mission<br />
and the issues that arose from it are presented in the report and summarised here.<br />
The Economic and Political Situation<br />
<strong>Fiji</strong> is an island nation in the south-west pacific, with an ethnically diverse population of<br />
837,271 people of whom approximately 56% are ethnic <strong>Fiji</strong>ans, 37% indo-<strong>Fiji</strong>an and the<br />
remainder consisting of other ethnic groups including Caucasian and Chinese. Its main source<br />
of revenue is from tourism, sugar, mining and agriculture. National GDP at constant price<br />
was $3.505 billion in 2000 and this has grown to $5.826 billion in 2007. The country has a<br />
relatively good infrastructure to support its development and the populations’ standard of<br />
living is declining. It is rated by UNDP Human Development Index (HDI) as being one of the<br />
medium developed countries being ranked 92 nd among a listing of 177 nations in 2006.<br />
However this represents a decline from position 46 in 1995.<br />
Despite its middle ranking status and the important role that <strong>Fiji</strong> enjoys as a regional centre,<br />
its development has been curtailed over the past 2 decades by political instability. The<br />
country has not yet attained the levels of development that were predicted for it in the early<br />
1980s. There has been widespread migration to Australia, New Zealand, the USA and more<br />
recently selective migration to the Middle East. This is particularly apparent among the<br />
educated and professional groups which <strong>Fiji</strong> can ill afford to lose. Doctors and nurses have<br />
migrated in large numbers, as shown in this report. This outward migration is having a very<br />
negative effect on the staffing of the MoH.<br />
The <strong>Health</strong> <strong>Sector</strong> in <strong>Fiji</strong><br />
vi
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
The MoH is by far the largest provider in the health sector although there is a growing private<br />
sector and a large number of NGOs some of whom now provide services to the public. Basic<br />
health care is provided to all residents through a hierarchy of village health workers, nursing<br />
stations, health centres, sub-divisional hospitals and divisional and specialized hospitals. This<br />
framework was put in place to provide ready access to all and has been functioning for many<br />
years.<br />
As stated above, this model has served the country well, but over recent years issues such as<br />
demographic and social change, improved transport and changing medical standards have<br />
meant that, while the framework is still very relevant today, the location and size of the<br />
building blocks requires review. Evidence seen at first hand during this mission indicates that<br />
some centres are overstaffed, while some are considerably understaffed. This has resulted in<br />
long waiting times at the general outpatient departments of divisional hospitals and some<br />
larger health centres. Equally important is the fact that many people are now bypassing<br />
nursing stations and health centres to go directly to divisional hospitals or other centres that<br />
are more convenient to them e.g. on a bus route or easy-access road. As a result the role of<br />
some centres may need to be re-assessed.<br />
Staffing the <strong>Health</strong> Service<br />
Within <strong>Fiji</strong>, this assessment mission found that workforce issues are of major concern to both<br />
curative and public health departments of the Ministry – although clinical areas are most<br />
acutely affected. In particular a shortage of key cadres of staff was reported to the team as<br />
being perhaps the single major issue facing the MoH – and it may worsen with the current<br />
directive by the PSC to reduce the workforce of the public sector by 10% .<br />
While there are adequate numbers of junior medical staff to fill the established positions<br />
(some would argue that these establishment levels have remained unadjusted for years despite<br />
workload increases), this assessment shows that, for all 4 levels of senior medical officers,<br />
including specialists, there is a serious shortage, with 36% of established positions being<br />
vacant.<br />
The continued shortage of specialist medical officers will, over time lead to a serious<br />
deterioration of service levels. At the divisional hospitals, waiting times for surgery are<br />
getting increasingly longer and the shortage of obstetricians and paediatricians is impacting<br />
on the care of mothers and babies. Furthermore, because of the lack of specialist medical<br />
officers and specialist nurses, the sub-divisional hospitals are functioning as little more than<br />
large health centres. Surgery, including caesarean sections, and other specialist medical<br />
services are no longer available at sub-divisional hospitals even though the hospitals may still<br />
have a functioning operating theatre and have provided these services to their communities in<br />
the past.<br />
There are shortages in other specialist areas. While there is now no shortage of generally<br />
trained nurses (there may in fact be a surplus within 2-3 years), there is a shortage of some<br />
cadres of specialist nurses, including those with specialist skills in intensive care and accident<br />
and emergency. Other areas of concern include biomedical engineering and IT support and<br />
specialist programmers.<br />
Funding the health service<br />
Financial constraints remain an ongoing problem facing the MoH. The figures presented in<br />
the report indicate that although there has been an increase in the size of health budget in<br />
recent years, the per capita health expenditure has declined from $176 in 2005 to $ 163 in<br />
<strong>2008</strong>. The MoH budget as a percentage of GDP was 2.57 in <strong>2008</strong>, representing a continuing<br />
vii
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
and steady decline from over 4 percent in 1993. It remains the lowest percentage of GDP of<br />
all countries in the <strong>Pacific</strong>.<br />
While there is some level of cost recovery, charges are very low and the amount of revenue<br />
raised is negligible. Clearly public debate is needed to establish acceptable principles of<br />
revenue collection in the context of the political and economic state of the nation. Equally<br />
important there is a need for public debate on the erosion of public health financing in <strong>Fiji</strong>,<br />
with a view to generating commitment from successive governments to incrementally<br />
increase the share of GDP allocated to health to at least that of its <strong>Pacific</strong> neighbours.<br />
There is some level of private health insurance but this is limited to those in the workforce<br />
and provides access to Suva Private Hospital and, in most cases, covers offshore referral for<br />
medical emergency.<br />
The <strong>Health</strong> of the People of <strong>Fiji</strong><br />
Key health indicators are presented in the report. <strong>Fiji</strong> made considerable progress in<br />
improving its key health indicators up to 1990, when they were seen to be excellent. During<br />
that period, life expectancy, and both maternal and infant mortality improved significantly,<br />
with MMR improving from 156.5 (per 100,000 live births) in 1970 to 53.0 in 1980 and 26.8<br />
in 1990.<br />
However since the mid 1990s, progress has stalled or deteriorated. Infant mortality rates were<br />
16.8 in 1990 but had worsened to 18.4 in 2007. Maternal mortality rates of 26.8 in 1990 had<br />
worsened to 31.1 in 2007. Both were well short of the MDGs of 5.6 for infant mortality and<br />
10.3 for maternal mortality. Clearly the MOH is not meeting these targets and data present in<br />
the full report show that under 5 mortality, infant mortality and maternal mortality are not<br />
only worse than the commitment given in the MDGs in 2000, but are considerably worse than<br />
the status in 1990.<br />
Particularly disturbing was a dramatic rises in the incidence of congenital syphilis to levels of<br />
162 cases in 5,635 lives births at the CWM hospital for the first 9 months of <strong>2008</strong>. This also<br />
serves as an endpoint indicator of an antenatal care system that needs more support.<br />
Major causes of morbidity include infection and parasitic disease (including Dengue, TB and<br />
HIV), NCD, diseases of the circulatory system; accidents and injury and diseases of the<br />
respiratory system. Major causes of mortality include diabetes and other NCDs,diseases of<br />
the circulatory system, infection and parasitic diseases, neoplasms and diseases of the<br />
respiratory system.<br />
Issues affecting the health service arising from this assessment.<br />
Apart from financial constraints and staff shortages - especially of senior level medical<br />
officers - eight other important areas were identified. These include:<br />
1. A general poor perception of the health services by the public<br />
2. Changes in demographics and social behaviour require a rethink of the location,<br />
staffing and range of services provided by health facilities.<br />
3. Relatively poor progress towards the achievement of <strong>Fiji</strong>s MDGs.<br />
4. Old or non-functioning equipment impacts on service delivery<br />
5. Stock outs of essential drugs are still occurring despite some progress over the past 12<br />
months<br />
6. There is a need for more focused planning and better use of management information<br />
systems – there appears to be a significant disconnect between the MoHs corporate<br />
plans and achievement of its KPIs<br />
viii
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
7. The health sector should be seen as being more than just the MoH – MoH should<br />
consider working more closely with its partners including the private sector, NGOs<br />
and the international agencies.<br />
8. There is a need for stronger evidence based approach to policy and planning and this<br />
will require a dedicated program or operational research<br />
Possible areas for future AusAID support.<br />
Eight possible areas of support are listed. However it is not recommended that AusAID try to<br />
address more than 3 of these areas - 1 or 2 would be preferable. In a review of the progress<br />
being made by the FHSIP that was carried out concurrently with this <strong>Situational</strong> <strong>Analysis</strong>, it<br />
was concluded that despite a number of important achievements no truly visible impact can<br />
be seen as judged by measureable progress towards the achievement of the MOHs own KPIs.<br />
In large measure this reflects the fact that the program’s activities are spread very widely,<br />
with little focus on a core set of activities.<br />
It is recommended that initial priority should be given by AusAID to assisting the MoH to<br />
achieve its MDG 4 (infant and child mortality) and MDG 5 (maternal mortality) targets.<br />
Although no design is included, the outline of a suggested approach to supporting this<br />
initiative is given in the full text.<br />
The eight areas identified for support by AusAID or other development partners are:<br />
i. Provide targeted support to the MoH to reduce its level of infant mortality (MDG 4)<br />
and maternal mortality (MDG 5).<br />
ii.<br />
iii.<br />
iv.<br />
provide support to address a limited number of the other national KPIs. These KPIs<br />
might include reduced amputation rates for diabetic sepsis (from 13% to 9%) ,<br />
elimination of drug “stock-outs “ or reduction in teenage pregnancy rates (from 16%<br />
to 8%). Obviously the choice of which of the national KPIs (listed in Annex 11)<br />
would be a matter for the Ministry.<br />
Support to review the “framework” currently in place to ensure access to health<br />
services. This should take account of changes over the last 30 years. Such a review<br />
should ask the question “what do we want the health sector to look like in 2020” and<br />
begin planning for it now.<br />
Support a culture of evidence based policy. This would be done by providing support<br />
for key operational research projects aimed at making the sector more efficient and<br />
effective.<br />
v. A program of continued capacity development in key areas. This would include<br />
management and supervision; planning, monitoring and evaluation. The Project<br />
Officer and Performance Enhancing Projects “models” introduced through the FHSIP<br />
should be continued.<br />
vi.<br />
vii.<br />
There is a need to continue to upgrade PATIS and other <strong>Health</strong> Information Systems<br />
(including training). FHSIP will continue to provide some support in this area during<br />
2009. However it is recommended that further AusAID support beyond the end of<br />
FHSIP should not be continued until there is some indication as to whether the IGOF<br />
will provide the necessary ongoing financial and specialist staffing support to enable<br />
this to be sustainable.<br />
Continued support for NGOs, who need to scale up and widen their activities.<br />
Continued donor support will enable them to do this and to play a more positive role<br />
as “partners” of the MoH.<br />
ix
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
viii.<br />
Continued support for Regional Programs, especially in the area of disease control.<br />
What is proposed here is not a new program in this area but rather that the current<br />
regional disease control activities being supported by AusAID, and especially support<br />
for NCDs and diabetes prevention and control, should be continued and even<br />
strengthened. There should be an attempt when designing regional programs to ensure<br />
that activities fit within national plans and that there is greater ownership and<br />
understanding of the programs at the senior level within individual countries.<br />
Although shortages of senior cadres of staff, and especially specialist medical officers, is<br />
identified as a major issue impacting on the quality of health care in <strong>Fiji</strong>, no specific program<br />
of AusAID support is recommended here. However FSMed will need to increase its postgraduate<br />
output to begin to address this issue, recognising that the decision on the allocation<br />
of scholarships ultimately resides with IGOF. In addition the suggested programme of<br />
targeted support to address the MDG, by the very broad nature of the suggested approach,<br />
may address staffing issues in relevant areas.<br />
A list of recommendations made throughout the report follow.<br />
x
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Recommendations<br />
Recommendation 1<br />
Continued efforts need to be made to increase the number of medical post-graduates from the<br />
FSMed. With this in mind, the IGOF should continue to allocate priority for postgraduate<br />
medical training when it allocates scholarships, either those that are internally funded or<br />
funded by its development partners.<br />
Recommendation 2<br />
The MoH should continue to work with the PSC to improve the salaries, allowances and<br />
incentives offered to specialist medical officers and specialist nurses with a view to reducing<br />
the level of outward migration and retaining their services within the <strong>Fiji</strong> health sector.<br />
Recommendation 3<br />
The MoH should consider undertaking regular surveys at the major hospitals (and other<br />
centres) to determine waiting times for patients attending at different times of the day and on<br />
different days. Concurrently, independent patient satisfaction surveys could be carried out to<br />
explore other issues such as staff attitude and drug outages. The results from such surveys<br />
could guide the implementation of a Service Improvement Program. The FHSIP should be<br />
asked to include funding for such surveys within its workplan for 2009.<br />
Recommendation 4<br />
The MoH should consider undertaking a review of the location, functions, staffing levels and<br />
operating hours of the current network of nursing stations, health centres, subdivisional and<br />
divisional hospitals to ensure that they better serve the needs of the people of <strong>Fiji</strong>. It is<br />
recognised that external assistance may be required for such a Review and development<br />
partners should look favourably on providing such support as it will offer the potential to<br />
significantly improve the efficiency of service delivery.<br />
The Clinical Services Planning Framework, developed with support of the FHSIP, should be<br />
a key tool in this exercise.<br />
Recommendation 5<br />
A carefully planned study should be undertaken of antenatal care practices in <strong>Fiji</strong>, which<br />
should include women in both urban and rural areas.<br />
Recommendation 6<br />
The MoH and its partners should consider developing “action” plans that focus specifically<br />
on reducing the levels of infant and maternal mortality. Such plans should cut across all<br />
departments of the MoH and engage with all relevant parties both within and outside of the<br />
Ministry.<br />
Recommendation: 7<br />
All options should be explored on ways to increase the level of funding made available<br />
through the national budget, and through development projects for the standardisation and<br />
procurement of essential biomedical equipment.<br />
Similarly, options should be explored on ways to increase the level of funding available for<br />
maintenance and repairs of biomedical equipment and to simplify the processes for the<br />
procurement of replacement spare parts and consumables.<br />
xi
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Recommendation 8.<br />
Recognising the very critical state of biomedical equipment procurement and repair,<br />
development partners might consider a large scale biomedical equipment project that seeks to<br />
purchase standardised equipment for the divisional hospitals in order to bring equipment up<br />
to acceptable levels. Any such project should also review the processes required for the<br />
maintenance of equipment and purchase of spare parts. Such a project should work with but<br />
be outside of the current support that AusAID is giving to strengthening biomedical<br />
engineering departments within the region.<br />
Recommendation 9<br />
Although access to essential drugs at the health facility level is improving and “stock outs”<br />
are occurring less frequently, more needs to be done, especially in the Northern Division.<br />
Any steps to improve the efficiency of drug supply should include a formal audit of the<br />
central pharmacy store , its processes and an assessment of the technical capacity of the staff<br />
to ensure that their skills match the needs of the job. FHSIP should be able to continue its<br />
support in this area during 2009, and include such an audit in its workplan<br />
Recommendation 10.<br />
The MOH should take the lead in recognising that the “health sector” consists of other<br />
partners besides the MOH.<br />
Working with outside support if necessary, it should explore ways in which it can work with<br />
these other parties, including private medical practitioners, to put in place more functional<br />
operational partnerships that better define the role of the respective partners in supporting the<br />
MOH to achieve the overall goals of the sector.<br />
It should also seek to obtain meaningful information on the range and volume of health<br />
services performed by these other parties.<br />
Recommendation 11.<br />
It is recommended that initial priority for any AusAID support beyond 2009, should be given<br />
to assisting the MoH to achieve its own MDG 4 (infant and child mortality) and MDG 5<br />
(maternal mortality) targets.<br />
Many of the issues raised in this set of recommendations are already known to the MoH.<br />
Indeed many of the recommendations take account of views expressed to the team by senior<br />
officials. However the recommendations themselves have not been discussed specifically<br />
with the Permanent Secretary and his Executive.<br />
xii
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
THE CURRENT SITUATION<br />
1. INTRODUCTION<br />
1.1. Background<br />
Australia remains committed to support <strong>Fiji</strong> to strengthen its health services. This reflects<br />
continuing support over the past decade including: community development projects in<br />
Kadavu and Taveuni (including the construction of new sub-divisional hospitals);<br />
strengthening the capacity of the National Centre for <strong>Health</strong> Promotion, support to the<br />
FSMed to introduce postgraduate medical training and more recently to strengthen the overall<br />
capacity of the School. AusAID has also sought to strengthen the capacity of the MoH to<br />
effectively manage its services and has provided support through the <strong>Fiji</strong> <strong>Health</strong> Management<br />
Reform Project (FHMRP) for management training, the introduction of the PATIS health<br />
information system (phase 1) and importantly to support the MoH plan for the<br />
decentralisation of health services.<br />
AusAID is currently providing ongoing support for the FSMed and the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong><br />
Improvement Program (FHSIP), which supports the MoH to implement its own corporate<br />
plans across a broad range of public health, curative services and administrative services.<br />
In addition, AusAID has provided support to <strong>Fiji</strong> through multilateral programs, support for a<br />
number of NGOs and a range of major regional programs in the area of HIV/AIDS, noncommunicable<br />
diseases, support for equipment maintenance and biomedical engineering,<br />
visiting medical specialists and pandemic influenza preparedness.<br />
The sector remains a major pillar of Australia’s bilateral assistance to <strong>Fiji</strong> and AusAID now<br />
wishes to move ahead with planning for a new program of support upon completion of the<br />
FHSIP project. To make decisions on its future programs, AusAID now seeks to obtain good<br />
baseline data and analysis of the health sector and of the issues that it faces in the future that<br />
may impact on the effective delivery of services. This includes the achievement of the sectors<br />
goals, including progress towards achievement of the health related MDGs 4, 5, and 6.<br />
It has therefore commissioned this <strong>Situational</strong> <strong>Analysis</strong> (the assessment), which will inform<br />
scoping and design of a future assistance program in health for <strong>Fiji</strong> sometime in mid-2009.<br />
1.2. Objectives and Methodology used for this <strong>Situational</strong> <strong>Analysis</strong><br />
The objectives for the assessment included in the TORs for the mission (see Annex 1) are as<br />
follows<br />
1. To provide a ‘snapshot’ of the current status of the health sector in <strong>Fiji</strong> from health<br />
service delivery and systems levels;<br />
2. To present and assess the state of health based on latest data and statistics, determine<br />
limitations of data and propose methodologies to enable tracking for MDGs and any<br />
future program support indicators;<br />
3. To identify opportunities and gaps for future AusAID programming, including<br />
strategic objectives and likely areas of impact. This assessment should be based on an<br />
assessment of the <strong>Fiji</strong> National <strong>Health</strong> Strategy and AusAID’s health sector programs<br />
in <strong>Fiji</strong>, including FHSIP, other bilateral, regional and donor partners’ programs.<br />
The Assessment was carried out in <strong>Fiji</strong> from 29 th October to 18 th November <strong>2008</strong> by a health<br />
development effectiveness specialist and team leader (Dr Ross Sutton); a health specialist (Dr<br />
Graham Roberts of FSMed) and a health data analyst (Mr Dharam Lingam – also of FSMed).<br />
The FSMed team members had recently commenced work on health financing and had a<br />
1
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
good level of local knowledge of the <strong>Fiji</strong> health system. Unfortunately, Dr Roberts joined the<br />
team late due to unforeseen family circumstances and could not participate in meetings<br />
during the first 5 days of the assignment.<br />
The team visited health facilities in the Central, Western and Northern Divisions. While in<br />
Suva the team met with AusAID and with officials from the MoH; CWM hospital, PSC,<br />
Ministry of Finance and National Planning (MF&NP), Consumer Council of <strong>Fiji</strong>, the FHSIP<br />
program, Attorney Generals Department, WHO, UNICEF, UNFPA, JICA and the EU. The<br />
team also met with a range of NGOs and community bodies including the <strong>Fiji</strong> College on<br />
General Practitioners (representing doctors in private practice). While in the Western and<br />
Northern Divisions the team visited a range of health facilities (nursing stations, health<br />
centres, subdivisional hospitals and divisional hospitals) and met medical and nursing staff in<br />
each facility. They also met with senior managers and their staff from the Community <strong>Health</strong><br />
and Management Services areas. The team also met with managers and staff from PC&SS<br />
(an NGO providing counselling services) in Nadi. The list of Key Persons Met is in Annex 2.<br />
Data was collected using material available in the MoH’s annual reports and department of<br />
statistics, the <strong>Fiji</strong> Islands Bureau of Statistics, MoF&NP finance circulars and <strong>Fiji</strong> Budget<br />
Estimates, PSC, Land Transport Authority and from sources contacted during this mission.<br />
The analysis sought to provide a “snapshot” of the health sector and is not considered to be a<br />
full review. As such, the actual time allocated for the assessment was relatively short. In<br />
addition the team leader also undertook a “progress check” of the current FHSIP<br />
concurrently with the assessment mission. That report is not included here.<br />
2. THE FIJI SETTING<br />
2.1. <strong>Fiji</strong> - Demographic and Country overview.<br />
<strong>Fiji</strong> is a small island state at the hub of the south-west <strong>Pacific</strong> midway between Vanuatu and<br />
the Kingdom of Tonga. The population (2007) was 837,271 comprising 475,739 ethnic<br />
<strong>Fiji</strong>ans, 313,789 Indo-<strong>Fiji</strong>ans and 47,734 of other ethnic groups. Overall, the rural population<br />
was 412, 435 and the urban 424, 846. The average annual growth rate is 0.8% (the natural<br />
increase of 1.2% minus migration) with crude growth rates being higher in the <strong>Fiji</strong>an than in<br />
the Indo-<strong>Fiji</strong>an population. Areas with noticeably increased population over the past few<br />
years are the Western Division (55,266) and Central Division, where the population of the<br />
Suva and Nausori urban and peri-urban areas has increased by 32,300. <strong>Fiji</strong>’s population by<br />
age and ethnicity is shown in table 1. Thirty nine percent of the population is less than 20.<br />
Table 1. 2004-5 survey of population by age and ethnicity<br />
Age Group <strong>Fiji</strong>an Indo-<strong>Fiji</strong>an Others Rotuman All % by Age<br />
0-4 46,068 20,519 2,567 980 70,134 8.6%<br />
5-19 143,362 96,342 8,443 3,351 251,498 30.7%<br />
20-49 184,347 170,582 13,299 4,315 372,543 45.5%<br />
50-64 40,078 44,206 3,497 1,449 89,230 10.9%<br />
65+ 17,898 14,582 1,461 607 34,548 4.2%<br />
Total 431,753 346,231 29,267 10,702 817,953 100%<br />
% by ethn’y 52.8% 42.3% 3.6% 1.3% 100%<br />
Source: 2004-05 Employment and Unemployment Survey<br />
2
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
<strong>Fiji</strong>’s Economic Exclusive Zone contains 332 islands covering a total land area of 18,333 sq<br />
km in 1.3 million sq km of the South <strong>Pacific</strong>. It is a multi-cultural and multi-religious country<br />
where different cultures meet and to some extent merge. Literacy rate is around 94%, with<br />
English being the official language and <strong>Fiji</strong>an and Hindi the languages of daily use. The 2007<br />
census indicated that 51% of the population is now urban with urban growth rate being 1.7%<br />
<strong>Fiji</strong>’s housing and employment crises are pervasive and will be compounded over time by<br />
high rates of school drop-out. As land leases expire and food costs rise, squatter settlements<br />
now number 200 with an estimated population of 100,000 people. Sixty eight percent of the<br />
workforce earns less than $7,000 per year. See Annex 3 for further information on income<br />
among different ethnic groups within <strong>Fiji</strong>.<br />
2.2. Economic and Political Situation.<br />
Main sources of revenue are tourism, sugar, mining, agriculture and bottled water. National<br />
GDP at constant price was $3.505 billion in 2000 and had grown to $5.826 billion in 2007.<br />
The country has a relatively good infrastructure to support its development but the overall<br />
standard of living is declining. It is rated on the UNDP Human Development Index (HDI) as<br />
being one of the medium developed countries, being ranked 92 nd among a listing of 177<br />
nations in 2006. However this represents a decline from position 46 in 1995. There is<br />
poverty, as reflected by the drop in ranking on the HDI, but it is not overtly apparent as seen<br />
in Africa, and some other Melanesian countries. However, poverty is increasingly becoming<br />
an issue that the present and future governments must deal with. Generally there is an<br />
adequate food supply for all although this should not imply that all have a well-balanced diet<br />
as indicated by the increasing incidence of NCDs.<br />
Despite its middle ranking status and the important role that <strong>Fiji</strong> enjoys as a regional centre,<br />
its development has been curtailed over the past 2 decades by political instability. The<br />
country has not attained the levels of development that were predicted for it in the early<br />
1980s. A series of 4 coups over the past 20 years has been a potential catalyst for an increase<br />
in migration from <strong>Fiji</strong> to Australia, New Zealand, the USA and more recently more selective<br />
migration to the Middle East. This is particularly apparent among the educated and<br />
professional groups which <strong>Fiji</strong> can ill afford to lose. Doctors and nurses have migrated in<br />
large numbers, as shown in this report.<br />
Thus <strong>Fiji</strong>’s economy has been repeatedly stressed by political changes since 1987 and<br />
subsequent fluctuations in the levels of private investment, fuelled in part by migration and<br />
the removal of preferential subsidies for sugar sold to the European Union, to reduce further<br />
by 35% in 2009. Increasing prices of oil and food imports have stressed the economy further<br />
while the decline in sugar production and in garments exports contribute more directly to<br />
poverty. The economy has become increasingly dependent on tourism, remittances from<br />
overseas, gold and forestry exports.<br />
The current Interim Government has been in place since December 2006. They have<br />
identified certain conditions to be in place prior to <strong>Fiji</strong> proceeding to a general election.<br />
These include adoption of the People’s Charter, within which Pillar 10 addresses issues of the<br />
health sector and proposes to ‘increase the proportion of GDP allocated to health by 0.5%<br />
per annum for the next 10 years to achieve a level of 7% of GDP’. The achievement of this<br />
objective would result in significantly increased funding for the health sector, yet in the<br />
current global and national economic climate achieving the increase will require continued<br />
advocacy for health developments in the face of competing demands; and the MoH to<br />
demonstrate that it uses its resources effectively.<br />
In the Reserve Bank Press Release (No. 30/<strong>2008</strong> 28 th November) the Governor of the RBF<br />
announced that “the domestic economy remained weak with growth forecast at 1.2 percent<br />
3
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
for <strong>2008</strong>, a downward revision from the earlier forecast of 1.7 percent” and that “the balance<br />
of payments was still forecast to remain under pressure, underpinned by a wide trade deficit”.<br />
In October <strong>2008</strong> inflation was at 8.5% down from a 20 year high of 9.8% in September.<br />
3. ORGANISATION, STAFFING AND FUNDING OF THE HEALTH<br />
SYSTEM.<br />
3.1. Overview of the MoH, its structure and organisation<br />
The MoH is by far the largest player in the health sector. It provides health care services<br />
directly to citizens of <strong>Fiji</strong> and to a limited extent to tourists and persons referred from within<br />
the region. The MoH also serves a role monitoring compliance of outside bodies; issues<br />
permits, provides reports and regulates the functions of professional bodies. Basic health care<br />
is provided to all residents through a hierarchy of village health workers, nursing stations,<br />
health centres, sub divisional hospitals and divisional and specialized hospitals. This<br />
framework was put in place to provide access to all and has been functioning for many years.<br />
A more detailed discussion of this is given below at 3.2. The location of these health facilities<br />
is shown in maps at Annex 4.<br />
The Ministry underwent a process of reform commencing in 1999. Under the guidance of the<br />
GOF, and with support initially from the AusAID funded FHMRP, and later with support<br />
from the FHSIP, responsibility for much of the day-to-day operation of the health services<br />
was slowly devolved from the head office in Suva to restructured divisional offices in each of<br />
the divisions. While the head office was to retain responsibility for all policy, for national<br />
standards, for overall planning monitoring and evaluation of performance, the actual delivery<br />
of services would be the responsibility of the divisions. A feature of the divisional structure<br />
was the bringing together of public health and curative services under one Divisional Director<br />
of <strong>Health</strong> who would be in a better position to allocate resources across the two areas of<br />
health care within the divisions. This decentralisation process progressed steadily and after 5<br />
years was very widely accepted by the staff. This current assessment team heard many<br />
positive comments on the efficiency gains that were slowly being made through the process.<br />
However in <strong>2008</strong>, subsequent to IGOF concerns to more tightly control limited government<br />
resources, senior staff and management functions were re-centralised into the MoH head<br />
office in Suva under the process of “roll-back of reform”.<br />
The assessment team heard many strong views in support of the original decentralisation plan<br />
as Divisional staff were empowered to make local-level decisions that was helping them to<br />
make local improvements.<br />
Following the recentralisation a new organisation structure for the Ministry is being<br />
developed with agreement of the PSC. However this has not yet been finalised. It is thus not<br />
possible to include an official organisation chart in this report as one has not yet been agreed.<br />
However, the organisation charts for HQ and sub-divisional level were recently proposed to<br />
PSC – but have not yet been approved (they are shown at Annex 5).<br />
The situation was further complicated when, early in 2007, the MoH was combined with the<br />
Ministry of Women and Social Welfare.<br />
3.2. The Service Delivery Framework – a traditional model<br />
The model of service delivery – from nurse to health centre, to sub-divisional hospital, to<br />
divisional hospitals and ultimately to the CWM as the central referral hospital, has served <strong>Fiji</strong><br />
well. These different levels of the health system are defined in the Clinical Services Planning<br />
Framework (CSPF) as follows:<br />
4
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Village/Community <strong>Health</strong> Service: Although not formally a MoH service, the<br />
Village/Community <strong>Health</strong> Service provides an important community link for MoH<br />
health services.<br />
Nursing Station Service: This is mainly a primary health care service, provided by a<br />
solo district nurse who is on call 24 hours a day. It caters for a catchment population<br />
range of approximately 200 to 5000. The average travelling time from a nursing<br />
station to the health centre by the most commonly used mode of transport is 1 hour 20<br />
minutes<br />
<strong>Health</strong> Centre Services: This facility provides Primary <strong>Health</strong> Care Services at a<br />
‘step-up’ from the nursing station as it is the first point of medical support for a<br />
number of nursing stations, which make up a medical area. The average travelling<br />
time from a health centre to a sub-divisional hospital by the most commonly used<br />
mode of transport is 2 hours 37 minutes<br />
Sub-divisional Hospital Service: General medical practitioners, midwives, registered<br />
nurses and assistants who work across inpatient, outpatient and community settings<br />
provide this service. This service operates on an on call service and is the first point of<br />
referral from health centre level. The average travelling time from sub-divisional<br />
hospital to divisional hospital by the most commonly used mode of transport is 4<br />
hours 20 minutes.<br />
Divisional Hospital Service: This service is provided by specialists, medical and<br />
nursing staff with a full range of diagnostic and allied health support services. The<br />
divisional hospital services also serve as a teaching institution for medical and nursing<br />
students. Divisional hospitals also coordinate visiting national and international subspecialist<br />
teams in Intensive Care, Cardiology and Cardiac Surgery, Plastic Surgery<br />
(Interplast), Neurosurgery, Urology, Vascular Surgery and Paediatric Surgery, while<br />
some patients are referred for overseas medical treatment.<br />
Specialized Hospital Service: This provides only selected specialty services namely<br />
psychiatry, rehabilitation and chronic infectious disease services (TB & Leprosy).<br />
These services are based in Suva, and act as a national referral service.<br />
A more detailed description of the different levels of health facilities is at Annex 6<br />
and table 2 shows the distribution of these different levels of care by Division<br />
Table 3: Distribution of <strong>Health</strong> Facilities by Division Source CSPF 2005<br />
Institutions<br />
Divisions<br />
Central Western Northern Eastern<br />
Total<br />
Divisional Hospitals 1 1 1 - 3<br />
Specialised Hospitals 3 - - - 3<br />
Sub-divisional Hospitals 4 5 3 4 16<br />
Area Hospitals 1 - - 2 3<br />
<strong>Health</strong> Centres 21 24 19 14 78<br />
Nursing Stations 17 22 20 24 82<br />
Community Nursing Stn 5 3 1 7 17<br />
Old People’s Home 1 1 1 - 3<br />
As stated above, this model has served the country well, but over recent years demographic<br />
and social change, improved transport and changing medical standards have meant that, while<br />
the framework is still relevant today, the location and size of the building blocks requires<br />
review. Evidence to this effect was presented to the assessment team and as this issue is<br />
5
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
considered to be particularly important to the efficient operation of the health system in the<br />
future, it is discussed in more detail at section 3.3. and especially at 5.2.<br />
3.3. Staffing the <strong>Health</strong> System<br />
3.3.1. Overview<br />
This continues to be a major issue in <strong>Fiji</strong> and indeed throughout the <strong>Pacific</strong>. The serious<br />
nature of workforce issues, and especially the shortage of key staff such as specialist medical<br />
officers, is reflected in the recent creation of the <strong>Pacific</strong> Human Resources for <strong>Health</strong><br />
Alliance. The Alliance is a network of representatives from individual pacific island countries<br />
supported by regional training institutions and “interested parties” from universities and<br />
professional bodies in Australia and New Zealand. It aims to address continuing problems<br />
relating to human resource development in the <strong>Pacific</strong>. WHO currently provides the<br />
secretariat for the Alliance.<br />
Within <strong>Fiji</strong>, this assessment mission found that workforce issues are of major concern to both<br />
curative and public health departments of the Ministry– although clinical areas are most<br />
acutely affected. In particular a shortage of key cadres of staff was reported to the team as<br />
being perhaps the single major issue facing the MoH – and it may worsen with the current<br />
request to reduce the size of the public sector workforce by 10% . These Issues of the<br />
adequacy of staff establishments and the difficulties to respond to emerging needs, graduate<br />
numbers in all health cadres, emigration of health personnel, remuneration, job evaluation,<br />
performance appraisal and career progression have been discussed and disputed in the <strong>Fiji</strong><br />
health system for many years but without a concerted and coordinated response.<br />
Unfortunately outward migration appears to have been accepted as an unavoidable<br />
phenomenon, resulting in the need to train more staff to fill vacant positions. However, the<br />
provision of newly trained staff to replace experienced staff is not an adequate response.<br />
Senior staff are leaving and are being replaced by less senior level staff, thus potentially<br />
putting at risk the overall quality of the workforce. Unfortunately in the current economic<br />
climate, the potential to increase staff establishments is unlikely, although within-budget<br />
changes to the mix of staff should be possible. This will be important to establish as it will be<br />
an unavoidable outcome of the review of the current service delivery framework referred to<br />
above at 3.2 and discussed in more detail at section 5.2.<br />
3.3.2. Service Delivery Staff<br />
Table 3 shows the number of doctors and nurses employed in each division.<br />
Table 3: Doctor and Nurse to Population Ratio by Division 2004<br />
Doctors<br />
Approved Popl’n Ratio<br />
Nurses<br />
Approved Popl’n Ratio<br />
Positions<br />
Positions<br />
Central/Eastern 159 1: 2704 890 1: 439<br />
Western 121 1: 3035 539 1: 516<br />
Northern 58 1: 3104 273 1: 586<br />
NATIONAL 338 1: 2896 1702 1: 532<br />
Note: These figures include only clinical posts and not senior administrators.<br />
Medical Staff<br />
Table 5 lists total medical staff engaged within the MoH. While there are adequate numbers<br />
of more junior medical staff to fill the established positions (some would argue that these<br />
establishment levels have remained unadjusted for years despite workload increases), the<br />
table shows that for all 4 levels of senior medical officers, including specialists, there is a<br />
6
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
serious shortage, with 36% of established positions being vacant. Clearly this has major<br />
implications for the delivery and quality of health services and for the supervision of medical<br />
students and interns within the public health system.<br />
Table 4. MoH Medical Cadre as at 31/10/08<br />
Post Grade Approved<br />
Establishment<br />
7<br />
Filled<br />
Vacant<br />
Consultant Specialist MD01 35 22 13<br />
Chief Medical Officer MD02 25 18 7<br />
Principal Medical Officer MD03 44 32 12<br />
Senior Medical Officer MD04 79 46 33<br />
Medical Officer MD05 168 170 +2<br />
Medical Intern MD06 35 49 +14<br />
Medical Assistant MD07 10 10 Nil<br />
Total 396 347 49<br />
Note: the surplus in ‘filled’ intern positions is of M.O.s held against those post.<br />
Shortage of Specialists and Senior level medical staff.<br />
The continued shortage of specialist medical officers will, over time lead to a serious<br />
deterioration of service levels. At the divisional hospitals, waiting times for surgery are<br />
getting increasingly longer (although an intense campaign of extended work-hours is<br />
currently seeking to address this); and the shortage of obstetricians, gynaecologists and<br />
paediatricians is impacting on the care of mothers and babies.<br />
This shortage of specialists has been felt for some years. For example, because of the lack of<br />
specialist medical officers and specialist nurses, the subdivisional hospitals have been<br />
restricted in the range of services they provide. The assessment team was continually told that<br />
surgery, including caesarean sections, and other specialist medical services are no longer<br />
available at subdivisional hospital even though the hospitals may still have a functioning<br />
operating theatre and have provided these services to their communities in the past. As<br />
examples, the subdivisional hospitals at Kadavu and Taveuni, constructed during the past 10<br />
years with AusAID support, have fully fitted-out operating theatres but do no surgery due to a<br />
lack of qualified surgeons.<br />
One factor associated with this shortage of specialists is the constraints on the FSMed to train<br />
enough medical officers – some of whom will go on to become specialists. A second reason<br />
for the shortage is the “pull” from countries both inside and outside the region who are<br />
offering much higher salaries but also, importantly, offer more attractive working<br />
environments. A third is what many have called the “push” being placed on doctors because<br />
of the stress they experience each day because of high workloads and poor working<br />
environments (lack of equipment, drugs etc). Together factors 2 and 3 result in a large level<br />
of outward migration as discussed at 3.3.3.<br />
General medical officers and private medical practitioners.<br />
Table 4 indicates that, compared with the establishment, there is no shortage of medical<br />
officers. Indeed there may be a slight surplus. However this may need to be interpreted with<br />
some caution as many of these positions are currently filled by foreign doctors from India,<br />
Philippines, Bangladesh, Burma, Nigeria, Pakistan and China on contract with the MoH.<br />
(Previously, in the 1980s <strong>Fiji</strong> sourced its overseas trained medical officers from Australia,<br />
UK and New Zealand). The cost of engaging these contracted doctors is higher than for<br />
equivalent local doctors and it is government policy to ultimately replace these doctors with<br />
locals.
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
When reviewing the medical workforce of <strong>Fiji</strong>, it needs to also be taken into account that<br />
there are currently approximately 120 medical officers in private practice (25% of the total<br />
medical workforce). In the main these are general practitioners; few are specialists and thus<br />
they will not help address the problem raised above. However, these general practitioners are<br />
providing a wide range of consultations, including antenatal care and childhood vaccinations.<br />
They are part of the health sector although the work they do is not included in the country’s<br />
overall health sector statistics. PSC mechanisms do exist to engage these doctors on a part<br />
time or locum basis within health centres and hospitals should this be needed in selected<br />
situations. These mechanisms have been tried on a small scale and there have been some<br />
problems but equally there have been some successes. However until this matter has been<br />
more fully explored, the role and use of private general practitioners in the public sector<br />
cannot be said to have been fully addressed. Using them more effectively will give the MoH<br />
greater flexibility in regard to medical officer staffing.<br />
In other steps to help relieve the shortage of medical officers: the FSMed has increased its<br />
intake of medical students from 70 to 80, of which 70 will be from <strong>Fiji</strong>. Another new medical<br />
school (under the University of <strong>Fiji</strong>) has just commenced in Lautoka, although its viability is<br />
still to be proven, and fifteen <strong>Fiji</strong>an medical students have been selected to undertake training<br />
in Cuba where their tuition will be in Spanish. It will be another 5-6 years before a judgement<br />
can be made on the registration and value to the <strong>Fiji</strong> health system of the Cuban graduates.<br />
Nurses, allied health and paramedical staff<br />
A similar phenomenon exists in the nursing cadre, with vacancies in higher levels but<br />
surpluses (against establishment) in lower level positions. Whether the MoH actually needs<br />
more nurses will be better established by the review proposed at recommendation 4. Because<br />
of the current establishment levels, the MoH now has difficulty in employing the number of<br />
new nurses that graduate annually. Last year the graduates of the Sangam School of Nursing<br />
in Labasa were not absorbed – and it appears that some graduates from the <strong>Fiji</strong> School of<br />
Nursing (FSN) will not be absorbed in 2009.<br />
Tables listing nursing, allied health and paramedical staff are given in Annex 6<br />
While there is now no shortage of generally trained nurses at the staff nurse level, there is a<br />
shortage of some cadres of senior level nurses and importantly of specialist nurses including<br />
those with specialist skills in intensive care and accident and emergency. Nurses trained in<br />
these areas are in demand from the more developed countries. Many nurses are migrating to<br />
Australia, New Zealand and to Dubai and other destinations in the Middle East (see 3.3.3.)<br />
where high salaries are on offer. It is understood that a considerable amount of the resignation<br />
and outward migration of nurses shown in Table 8 below relates to these specialist nurses.<br />
The team was informed that in part this represents the attraction of higher salaries and<br />
working conditions but in part it is a reflection of the fact that promotion for nurses in <strong>Fiji</strong> is<br />
usually based on seniority and not necessarily on merit or special skills. As a result these<br />
specialist nurses, who in many cases have graduated in the last ten years, find that, despite<br />
their specialist skills, to get promotion they must move outside of their specialty or go<br />
overseas.<br />
Annex 6 shows that there is generally no shortage of established paramedical and allied<br />
health cadres in <strong>Fiji</strong>. Important however is the fact that there are no posts for cadres that are<br />
considered essential in many countries’ health systems – psychologist, counsellors, social<br />
workers, occupational health workers, podiatrists among others. As discussed elsewhere in<br />
this report counselling services within <strong>Fiji</strong> are now being provided by the NGO <strong>Pacific</strong><br />
Counselling and Social Services (PICASS).<br />
Other Cadres of staff.<br />
8
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
There are two other staffing areas of concern, which are in biomedical engineering and IT.<br />
The MoH has had perennial difficulty in maintaining its biomedical equipment. AusAID<br />
support has previously been provided in this area but the problems remain as discussed in<br />
section 5.4. of this report. At the root of this problem is the ongoing difficulty of recruiting<br />
biomedical engineers. There is need both to increase the establishment in this area and have<br />
biomedical engineers in each of the three main hospitals and also create attractive salary and<br />
conditions to hold such people who otherwise will be attracted to other areas such as<br />
telecommunications, and airline equipment maintenance. The costs in external maintenance,<br />
transport of equipment needing repair, downtime of equipment and importantly in<br />
deterioration of patient care because of poor equipment, far exceeds the cost of employing<br />
specialist staff. See section 5.4 for further discussion on the poor state of equipment within<br />
the health sector.<br />
Similarly there is an acute shortage of IT specialists and the level of computer literacy is<br />
often low. Although FHSIP provides funding to support a full-time IT Specialist for MoH,<br />
the need for IT staff to maintain, extend and fully utilise PATIS was apparent to the team.<br />
The limited application of PATIS may undermine its success, while those who use it find it<br />
can provide valuable information. It is apparent that the additional workload placed on nurses<br />
to enter data into PATIS is a barrier to its success, and it would be wise for MoH to allocate<br />
resources and develop people and procedures to improve data entry and the use of PATIS as a<br />
management tool (see also 5.6).<br />
3.3.3. The Problem of Resignation and Outward Migration from the MoH<br />
The importance of resignation and outward migration has already been discussed. Table 5<br />
shows the ‘exits’ of staff from the public health care system between 2003 to 2007, through<br />
resignation, retirement, death or expiry of contract, revealing a high turnover in all cadres .<br />
In these five years the equivalent of 40% of the medical and 33% of the nursing approved<br />
establishments exited the public health system.<br />
Table 5: ‘Exit’ of staff from MoH over 5 years (2003-7)<br />
Cadre 2003 2004 2005 2006 2007 Total Av.p.a.<br />
Medical Officers 29 40 37 31 23 160 32<br />
Nurses 25 64 162 216 78 545 109<br />
Paramedical 15 15 19 19 13 81 16<br />
Dental 4 4 13 10 5 36 7<br />
Pharmacy 4 3 18 8 8 41 8<br />
Total 77 126 249 284 127 863 173<br />
This issue of resignation and outward migration of senior medical and nursing staff has been<br />
discussed earlier and remains a major problem for the Ministry and for the PSC.<br />
A recent study of specialist medical officer migration (Oman 2007) ‘Should I migrate or<br />
should I remain? Professional Satisfaction and career decisions of doctors who have<br />
undertaken specialist training in <strong>Fiji</strong>’ based on 3 elements of professional growth, service<br />
and recognition. Dissatisfaction was directed primarily at the MoH and the failure to reliably<br />
provide basic medications and supplies, as well as problems of career advancement created<br />
by bottleneck from limited numbers of senior postings. Oman’s also found a ‘centrality of<br />
the professional values of service, patient welfare regardless of ability to pay’ as a very great<br />
advantage from the standpoint of the MoH’ and goes on to propose 3 intervention areas to<br />
improve retention: supporting the work of doctors, supporting professional development and<br />
career advancement and valuing and supporting doctors as members of families, extended<br />
families and communities.<br />
9
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
3.3.4. Training the Clinical Workforce<br />
There are two major clinical training institutions in <strong>Fiji</strong> – the <strong>Fiji</strong> School of Medicine and the<br />
<strong>Fiji</strong> School of Nursing. Annex 7 shows the output from these two major training institutions.<br />
It must be remembered that FSMed also serves as a regional training centre and that only<br />
60% of medical graduates are from <strong>Fiji</strong> (64% in <strong>2008</strong>).<br />
It has already been discussed that simply graduating new doctors or nurses will not address<br />
the immediate shortage of senior staff. As shown in tables 5 and Annex 8, the number of new<br />
<strong>Fiji</strong> medical graduates is almost matched by the number of doctors exiting the service.<br />
FSN and FSMed have consistently increased their intakes in response to the demonstrated<br />
needs arising from migration and high turnover – and the ever increasing need for <strong>Fiji</strong> to<br />
engage contracted foreign doctors. Unfortunately it is not possible to develop any specific<br />
“formula” to determine the number of staff that need to be trained to overcome losses. This is<br />
because the numbers leaving the services vary very significantly from year to year eg after<br />
political events such as a coup or after “recruitment drive”, by representatives from other<br />
countries eg the United Arab Emirates.<br />
Nevertheless this need to train more doctors should continue, even though data presented<br />
earlier in this report indicates that there is currently a slight surplus against establishment of<br />
the more junior levels of medical officer. This must be interpreted cautiously. There is a need<br />
to replace many of the lower level contracted foreign doctors in both <strong>Fiji</strong> and the PICs, and<br />
the need to consider contracting more senior medical staff at specialist, senior, chief and<br />
principle levels to improve the quality of health care services and also to support the training<br />
of local medical staff.<br />
Obviously the need to continue to train medical specialists through the Postgraduate Masters<br />
and Diploma level course at the FSMed should continue and indeed be given an even higher<br />
priority.<br />
Recommendation 1<br />
Continued efforts need to be made to increase the number of medical post-graduates from the<br />
FSMed, With this in mind, the IGOF should continue to allocate priority for postgraduate<br />
medical training when it allocates scholarships, either those that are internally funded or<br />
funded by its development partners.<br />
Recommendation 2<br />
The MoH should continue to work with the PSC to improve the salaries, allowances and<br />
incentives offered to specialist medical officers and specialist nurses with a view to reducing<br />
the level of outward migration and retaining their services within the <strong>Fiji</strong> health sector.<br />
3.4. Financing the health system<br />
From the outset it is important to note that the financial figures presented in this report have<br />
been vetted by the National Planning Office but there may be some discrepancies from those<br />
in the MoH accounts.<br />
3.4.1. Overview<br />
<strong>Health</strong> services in <strong>Fiji</strong> are primarily provided by government and financed almost exclusively<br />
through tax revenues. Other sources of funding for the MoH are donor assistance for service<br />
enhancements, a small cost-recovery program of user charges, a revolving drug fund account<br />
(from community pharmacies) and the government pharmacy’s bulk purchasing scheme.<br />
10
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Government allocations to the MoH vary according to policy and fiscal priorities. Developed<br />
countries spend in the order of 7% to 10% of GDP on health). <strong>Fiji</strong>’s government allocation of<br />
2.6% of GDP is the lowest among <strong>Pacific</strong> regional neighbours (UNDP 2007/<strong>2008</strong>). The<br />
Solomon Islands and Tonga allocate between 5-6% of GDP to health annually, Samoa<br />
between 4-5% and Vanuatu and Papua New Guinea over 3%. Table 6 illustrates that in <strong>Fiji</strong>,<br />
the proportion of GDP allocated to health has fluctuated around 3% but has fallen below that<br />
since the year 2000, placing pressure on the capacity to provide a quality national health care<br />
system and to continually upgrade it. This ongoing financial constraint is of major concern.<br />
The collection of fees for services provided to patients and others remains a strategy for<br />
raising revenues, but the existing fee structure allows for only a token level of cost recovery,<br />
down from 14% in 1962 to less than 1% of expenditure since 1992.<br />
Table 6. GDP, MoH budget and MoH budget as % of GDP, 1993-2005.<br />
Fiscal Year<br />
GDP ($ MOH Budget MoH Budget as %<br />
millions) (Million FJD) of GDP<br />
1993 1707.00 68.57 4.02<br />
1995 2799.00 78.11 2.79<br />
1999 3662.00 107.90 2.95<br />
2000 3505.00 124.20 3.54<br />
2003 4245.00 136.88 3.22<br />
2005 4731.00 136.88 2.89<br />
2006 5032.00 147.06 2.92<br />
2007 5079.00 142.67 2.81<br />
<strong>2008</strong> 5826.00 150.00 2.57<br />
Source: Bureau of Statistics, <strong>Fiji</strong> and <strong>Fiji</strong> Budget Estimates<br />
All services provided at outpatient departments and the general public wards are free.<br />
Inpatient services are provided free of charge unless patients choose to be admitted to ‘paying<br />
wards’ where a range of fees are charged for diagnostic services in addition to the room<br />
charges. The ‘paying ward’ fees have not been subject to review since 1982 and are very low.<br />
As an example, civil servants in <strong>Fiji</strong> pay only $0.60 cents per day for the general paying<br />
wards (4 bed per room) and $1.00 for the single bed room ‘paying wards’, while non-civil<br />
servants will pay $6.00 per day for the ‘paying wards’ and outpatients referred by a GP to a<br />
specialist clinic will pay $8.00 per consultation. We understand that the MoF&NP is<br />
currently reviewing hospital charges and that new rates may apply soon, although discussion<br />
with important stakeholders, such as the Consumer Council of <strong>Fiji</strong>, has not yet taken place.<br />
Determining a level of fees that discourages frivolous use without discouraging essential use<br />
requires careful calculation and a degree of policy expertise and action that has not been<br />
evident in health financing in <strong>Fiji</strong> to date. Policy inactivity on this issue over recent decades<br />
may reflect political caution, but in an era of sharply rising costs it has inevitably propelled<br />
<strong>Fiji</strong> towards under-funded and limited services.<br />
The MoH has not attempted to compete with the growing private sector, yet it has the<br />
opportunity to partly privatize all three Divisional Hospitals by upgrading the standard of<br />
accommodation, by raising the fees in the ‘paying wards’ and establishing cost-sharing<br />
relationships with private health insurers. It is doing this in some places such as Nadi subdivisional<br />
hospital, where services to tourists are important. This approach is now practiced<br />
widely in some countries eg Indonesia where in some provinces, such as Bali, income from<br />
private ward patients in public hospitals is considerable and contributes to supporting public<br />
services.<br />
3.4.2. National budget<br />
11
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Table 7 shows annual national budgets, health budgets and per capita expenditures from 1986<br />
to 2007. Despite the declining national budgets as a percentage of GDP (see above) there has<br />
been a relatively consistent proportion of government resources, and an increasing per capita<br />
expenditure, allocated to health.<br />
Table 7: Govt. budget, MoH allocation and budget share, MoH revenue, MoH revenue<br />
as proportion of expenditure and Per-Capita <strong>Health</strong> Expenditure 1986-2009.<br />
Fiscal<br />
Year<br />
Whole of<br />
Govt.<br />
Budget<br />
(Million<br />
MoH<br />
Budget<br />
(Million<br />
FJD)<br />
MoH Share<br />
of Govt.<br />
Budget (%)<br />
MoH<br />
Revenue<br />
(Million<br />
FJD)<br />
MoH<br />
Revenue as<br />
% of <strong>Health</strong><br />
Expenditure<br />
Per capita<br />
<strong>Health</strong><br />
Expenditure<br />
(FJD)<br />
FJD)<br />
1986 383.30 35.00 9.13 1.10 3.10 49.30<br />
1990 522.10 42.00 8.00 1.10 2.60 54.83<br />
1992 550.50 44.40 8.06 0.80 1.80 55.64<br />
1993 815.99 68.57 7.50 1.63 2.60 79.89<br />
1994 830.64 73.26 8.30 1.54 1.20 88.40<br />
2000 1,097.96 124.20 9.00 3.05 3.10 123.18<br />
2002 1,225.49 134.13 8.90 1.40 1.20 125.87<br />
2004 1,313.30 134.13 10.20 1.41 1.00 158.61<br />
2005 1,424.48 136.88 10.00 1.30 0.80 176.55<br />
2007 1,572.37 142.67 9.07 1.70 1.10 174.71<br />
<strong>2008</strong> 1,527.91 150.00 9.82 1.60 1.20 163.26<br />
2009 179.51*<br />
Source: <strong>Fiji</strong> Budget Estimates, Bureau of Statistics.<br />
* The announced 2009 budget includes an amount of FJD 27.445 million for Women and Social<br />
Welfare.<br />
Annex 9 provides further detailed information on the budget and illustrates how in the 15<br />
year period 1993-<strong>2008</strong> the population of <strong>Fiji</strong> increased by 7.3% (56,096 people), Gross<br />
Domestic Product (GDP) more than tripled, the MoH budget more than doubled, the<br />
Consumer Price Index (CPI) increased by 48 %, the MoH Salaries and Wages bill more than<br />
doubled in absolute terms and averaged 53% of the MoH budget over the period. Salaries<br />
have increased to over 60% of the annual budget in recent years.<br />
3.4.3. Breakdown in expenditure by cost centres.<br />
Annex 10 gives detailed breakdown by cost centre of the MoH budget for two successive<br />
years. This provides the reader with some indication of allocation of funds across the areas of<br />
activities. Two specific areas are highlighted here: pharmaceutical and biomedical equipment<br />
procurement costs. Both have been identified by the team and by those interviewed during<br />
this mission as being “issues of concern”<br />
Pharmaceutical Costs<br />
Much has been said of the outages of essential drugs within the health system and this is<br />
discussed in more detail at section 5.5. The figures in table 8 below indicate that despite<br />
rising costs of drugs, expenditure remained constant from 2003 until 2006. It was not until<br />
2007 that there was a meaningful increase in this area.<br />
Table 8. Pharmaceutical Budget (millions FJD) 2003-<strong>2008</strong><br />
2003 2004 2005 2006 2007 <strong>2008</strong><br />
8.032 8.032 8.032 8.032 9.5 9.5<br />
Procurement of Biomedical equipment<br />
12
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
The budget for the purchase of biomedical equipment is given in table 9 below and these<br />
show that the situation is even worse in this area – with no increase in expenditure over the<br />
past 6 years. Indeed there has been a significant decrease in <strong>2008</strong>. In large part this explains<br />
the ongoing problems now being found with the shortage of functional essential equipment.<br />
See section 5.4. for a detailed discussion of the problems occurring in this area.<br />
Table 9. MoH Biomedical budget allocations 2003-<strong>2008</strong><br />
Type of Facility 2003 2004 2005 2006 2007 <strong>2008</strong><br />
Urban Hospitals 700.000 500,000 700,000 700.000 700.000 500,000<br />
Sub divisional 700,000 700,000 700,000 700,000 700,000 500,000<br />
Hospitals<br />
H/Centre’s and 500,000 400,000 400.000 400,000 400,000 500,000<br />
nursing stations<br />
Total 1,900,000 1,600000 1,800,000 1.900000 1.800000 1.500.000<br />
3.4.4. Private insurance<br />
The feasibility of health insurance in <strong>Fiji</strong> is limited by poor economies of scale due to the<br />
high proportion of the population not formally employed, employed in low-paying jobs, or<br />
situated in remote geographical areas. <strong>Fiji</strong> has approximately 1.5 million outpatient visits and<br />
50,000 inpatient admissions annually. A government funded health insurance program such<br />
as Medicare in Australia does not appear to be feasible. While reviews of the feasibility of<br />
private health insurance schemes have been undertaken in the past, the growth in private<br />
practice may provide some justification for another review of the health insurance options<br />
available to <strong>Fiji</strong> and their potential impact on the relative rates of admissions to private and or<br />
public hospital ‘paying wards’ and redirecting some patients from the general outpatient<br />
department of the divisional hospitals to private general practitioners. At this stage prime<br />
responsibility should lie with the private health insurance companies to initiate any review.<br />
However if it is given priority by the MoH, a development partner such as AusAID or the<br />
ADB may support such a review – with a view to putting a proposal to government and the<br />
private insurance industry that takes account of the findings.<br />
3.4.5. Out of pocket expenditure<br />
National <strong>Health</strong> Accounts (NHA) show the community meeting 20% ($27 million) of all<br />
national health expenditure from its own pocket. Almost 3.5% ($4.8 million) is spent on<br />
health insurance premiums and 5.4% ($7.3 million) spent on pharmaceuticals at private<br />
providers. The true cost of health expenditure paid to private general practitioners is not<br />
reflected as there is no system in place for capturing the extent of these costs.<br />
Although out-of –pocket expenditure is high compared with other PICs it is not high by<br />
international standards. In many medium income Asian countries the private expenditure on<br />
health care is often of the order of 50%. In some countries e.g. Cambodia this may rise to as<br />
high as 80% of total health care expenditure.<br />
When all government and private costs are taken into account the total level of national<br />
expenditure on health is likely to be about 4% of GDP.<br />
3.4.6. Support from Development Partners<br />
<strong>Fiji</strong> is not a donor dependant nation, with development assistance to the health sector<br />
constituting less than 6% of the total health care budget in most years. However this may<br />
vary from year to year with some years seeing increased donor support through large<br />
infrastructure projects; the national pharmacy store, the Pasifika campus of FSMed and the<br />
new paediatric hospital being examples during the last 10 years. In terms of support for<br />
ongoing operations, AusAID is the major development assistance partner to the sector.<br />
13
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Nevertheless development partners do play an important role in supporting the health sector.<br />
This support is given through four main pathways (a) direct bilateral programs/projects (b)<br />
assistance directly to NGOs/CBOs (c) regional programs in areas such as NCDs, HIV/AIDS,<br />
pandemic preparedness and (d) donor support to the international agencies and “funds” who<br />
in turn provide assistance to the sector. While direct bilateral assistance is, in most cases,<br />
captured through the national accounts, the monetary value of much of the assistance given<br />
through other channels is not shown in the national accounts. For this reason it has not been<br />
possible for this assessment mission to put a dollar value on total value of development<br />
assistance to the sector. However an indicative assessment over a 5 year period would be of<br />
the order of $6-10 million per year. Nevertheless Table 10 below gives an indication of the<br />
nature of the support going to the sector. It should be noted that there is some double<br />
counting in this table as partners such as AusAID and NZAID may provide funds to an NGO<br />
or international agency who, in turn provides additional funds from their own resources, to<br />
help implement a program.<br />
Currently AusAID and JICA are the only development partners with bilateral programs in the<br />
health sector. NZAID has a considerable regional program, as shown in the table below; the<br />
EU has no program in the health sector at the moment. The team were told that neither<br />
NZAID or the EU have any plans to change this position. JICA will continue with its current<br />
programs (support for EPI, middle level nurse supervision training and filariasis eradication)<br />
but have not made decisions on future activities in the health sector.<br />
Despite their current plans, all development partners met during this mission did express an<br />
interest in learning of AusAID’s plans for the future. WHO and UNICEF both indicated that<br />
they will give high priority to any approach to reduce the level of infant and maternal<br />
mortality and in this regard WHO advised the team that they shortly hope to appoint a<br />
specialist MCH adviser.<br />
It is therefore possible that, subject to the design of any future program, there may be<br />
opportunities for these partners to collaborate, particularly if any new program is in an area of<br />
high priority for them such as infant and maternal mortality. Increasingly development<br />
partners and the MoH have recognised the importance of donor harmonisation – in keeping<br />
with the principles of the Paris Declaration. This harmonisation of approaches among donors<br />
is likely to produce more partnership arrangements in coming years, as it has previously been<br />
identified that to do otherwise places too great a demand on counterparts; with MoH staff<br />
being asked to defer other important tasks to conform to donor processes and timelines.<br />
Table 10. Examples of main areas of support provided to the health sector through<br />
development partners<br />
Development<br />
Partners<br />
Areas they are supporting<br />
AusAID • <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> Improvement Program (multiple projects)<br />
• Support for FSMed<br />
• support visiting specialist program<br />
• support for <strong>Pacific</strong> Human Resources for <strong>Health</strong> Alliance<br />
• FSN curriculum development<br />
• <strong>Pacific</strong> Regional Influenza Pandemic Preparedness Project<br />
(PRIPPP)<br />
• Regional NCD<br />
• Regional HIV/AIDs<br />
14
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
• Regional biomedical engineering and equipment maintenance<br />
• ADRA Australian Development Research Awards<br />
• Support for a range of NGOs including<br />
• PC&SS training of qualified counsellors<br />
• Marie stopes<br />
• <strong>Fiji</strong> Red Cross Society<br />
• <strong>Fiji</strong> network for people living with AIDS and HIV<br />
• Femlink<br />
• Consumer Council of <strong>Fiji</strong><br />
JICA • Support for Pharmacy and Consumables System<br />
• EPI Cold Chain System<br />
• Middle level nurse supervision -Protocols and Manuals etc<br />
• support for elimination of Filariasis<br />
NZ Aid • Support for tertiary health services in New Zealand<br />
• Support for a wide range of NGOs through relevant regional<br />
programs<br />
• <strong>Pacific</strong> Regional Influenza Pandemic Preparedness Project<br />
• International Planned Parenthood<br />
• <strong>Pacific</strong> Islands Aids Foundation<br />
• Marie Stopes<br />
• Foundation for Peoples of the South <strong>Pacific</strong> International<br />
• <strong>Pacific</strong> Disability Forum<br />
SPC • Adolescent reproductive health<br />
• HIV – regional coordination<br />
• Support to HIV/AIDS<br />
• PRIPPP (pandemic influenza preparedness)<br />
• NCD<br />
UNICEF • MCH/EPI<br />
• Immunizations/vaccines/ cold chain support<br />
• Promote life skills training in the community<br />
• Funding support to Peer Educators<br />
• Address non-nutritious food advertising<br />
• Promotion of Breast feeding through Baby Friendly Hospital<br />
Initiative<br />
• To increase the knowledge and understanding of sexual health<br />
issues<br />
• Integrated prevention of Mother to child transmission of HIV<br />
(PMTCT)<br />
WHO • <strong>Pacific</strong> Framework for Prevention and Control of Non<br />
Communicable Diseases (with SPC and AusAID)<br />
• Water Safety Plans (with SOPAC & AusAID)<br />
• Strengthening Specialized Clinical Services in the <strong>Pacific</strong><br />
PHRHA (with AusAID)<br />
• Communicable Diseases Surveillance<br />
• Outbreak response Measles, Typhoid, Dengue Fever<br />
• International <strong>Health</strong> Regulations<br />
• HIV response<br />
• <strong>Pacific</strong> Human Resources for <strong>Health</strong> Alliance (AUSAID<br />
through WHO)<br />
• FSN post-basic program development<br />
• <strong>Pacific</strong> Elimination of Filariasis<br />
FSMed • Non Communicable Diseases/ Physical Activity<br />
• Accident and Injury Prevention<br />
15
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
UNFPA • Regional Reproductive <strong>Health</strong> Training program<br />
• Increase access to condoms.(commodity security)<br />
• Men as Partners in Reproductive <strong>Health</strong> (with ILO)<br />
• Adolescent training<br />
UNAIDS • Support to NACA<br />
• World AIDS Day<br />
NGOs • AIDS Task Force <strong>Fiji</strong> (VCCT and HIV testing)<br />
• Marie Stopes International (condom social marketing VCCT and<br />
HIV testing)<br />
• PC&SS Counselling training and service provision)<br />
• International Red Cross<br />
• Foundation of the Peoples of the South <strong>Pacific</strong> (youth mental<br />
health)<br />
3.5. Planning and Managing the <strong>Health</strong> Care system,<br />
3.5.1. The Planning process.<br />
Planning at the top level of the MoH HQ and Divisions has progressed well and well<br />
documented Strategic and Corporate (annual) plans appear comprehensive. However these<br />
plans are static and do not qualify as “action” plans which seek to address the national KPIs<br />
(Annex 11 provides a list of the national KPIs).<br />
Until recently, planning processes at the divisional level have integrated curative and public<br />
heath arms of the service, but these have recently been separated again during the ‘roll-back’.<br />
Comments most frequently made to the team relate to<br />
i. the need for plans to be inclusive of the activities of partner organisations;<br />
ii.<br />
iii.<br />
iv.<br />
plans have not been well communicated down through the organisation.<br />
activity plans created at lower levels lose the strategic focus of partnering and become<br />
internal; and<br />
that the planners are generally medical staff – not professionally trained managers.<br />
While some aspects of planning are sound, much more needs to be done. (See 5.6 for a more<br />
detailed discussion of this issue, along with a discussion on the use of health information<br />
systems, including PATIS, to monitor progress of the plans).<br />
3.5.2. The slow but steady development of a pool of trained managers.<br />
Recent years has seen little change in personnel at the higher management levels of the MoH.<br />
The senior MoH staff are predominantly medically qualified and with MPH degree in which<br />
they may have been exposed to basic management training. Various training programs have<br />
been conducted over the past 10 years, especially through the FHMR project and more<br />
recently through FHSIP to supplement their management skills. Comment made to the team<br />
(and a view supported by the team) is that, of all of these management training activities, the<br />
most effective appears to be the use of ‘learning by doing’ experience established by the<br />
FHSIP project officers “ model” where project officers were given a specific project task and<br />
the responsibility to carry them out. Supportive training was provided to these people, who,<br />
on interview, appeared to have learnt much from the experience which they will carry into<br />
their careers.. The Performance Enhancing Projects” model, also introduced by FHSIP is also<br />
proving to be effective - especially at the level of senior clinicians and managers.<br />
The postgraduate diploma in health services management at FSMed has recommenced,<br />
creating the opportunity for further development of management courses and short courses<br />
16
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
for MoH staff. It is acknowledged that creative management is difficult in the IGOF system,<br />
where much of the authority is centralised into the PSC or the MoF&NP. It was often stated<br />
to the team that policies of bodies such as PSC stifle the use of many management skills<br />
learned and replace them with a set of rigid rules that deny flexibility. We gained the<br />
impression however that, while this is true, a weakness in MoH management was in the<br />
capacity to prepare convincing, factually based management submissions to present to the<br />
PSC and MoF&NP to justify requests for procedural or distributive changes e.g. changes in<br />
staff establishment numbers.<br />
The quality of management within the health sector would also be enhanced by (a) creation<br />
by the PSC of formal classifications of professional health care managers and (b) the<br />
creation of a professional grouping of health sector managers with minimum accepted<br />
qualifications and experience modelled on similar groups in Australia and New Zealand.<br />
It needs to be accepted that organisations such as the CWM and the Lautoka Hospital are<br />
among the largest operations in <strong>Fiji</strong> and would best be managed by professionally trained<br />
managers.<br />
3.5.3. <strong>Health</strong> Legislation<br />
The MoH currently administers 17 pieces of legislation. Most of this legislation is now<br />
outdated and requires revision. There are some 140 plus pieces of legislation on the calendar<br />
for revision and enactment but most of the legislation under the MoH is not yet even listed<br />
for revision. The Public <strong>Health</strong> Act, Medical and Dental Practitioners Act have been revised<br />
but not enacted.<br />
4. THE HEALTH OF THE PEOPLE OF FIJI.<br />
4.1. Key health Indicators<br />
A comprehensive set of population health indicators is presented in Table 11. Overall the<br />
figures show no real improvement in the health status of the people of <strong>Fiji</strong> over the past 5<br />
years, although there has been some small improvements in areas of post neonatal mortality<br />
and contraceptive coverage rates<br />
Table 11. <strong>Fiji</strong>’s Key <strong>Health</strong> Indicators<br />
2003 2004 2005 2006 2007<br />
Population (Census estimates) 866,099 848,647 849,361 868,488 868,107<br />
Women in CBA (15-44) 180,555 167,810 183,295 186,803 185,328<br />
Total Live Births 17,910 17,714 17,826 18,394 19,298<br />
Crude Birth Rate/1,000 Population 20.68 20.87 20.99 21.20 22.2<br />
Crude Death Rate/1,000 Population 7.06 6.63 7.02 7.1 9.8<br />
Rate of Natural Increase 1.36% 1.42% 1.4% 1.4% 1.2%<br />
0-5Mortality Rates/1000 live Births 23.73 22.52 25.81 25.8 22.4<br />
Infant Mortality Rate/1000live Births 18.87 17.84 20.76 19.5 18.4<br />
Perinatal Mortality (stillbirth and early 16.4 19.3 22.05 19.4 15.8<br />
neonatal deaths/1,000Live Births)<br />
Early Neonatal Deaths (0-7days)/1,000 live 7.54 8.13 10.43 8.0 N/A<br />
Births<br />
Neonatal Mortality (Deaths<br />
9.27 10.05 15.37 11.3 11.9<br />
0-28days) 1000 Live Births<br />
Post Neonatal Mortality (Deaths 1- 9.6 7.79 5.39 8.2 6.5<br />
12Months) 1000 Live Births<br />
Maternal Mortality Ratio/100,000live births 22.3 33.9 50.5 43.5 31.1<br />
General Fertility Rate/1,000 CBA 99.2 105.6 97.3 96.9 104.1<br />
Family Planning Coverage Rate 42.0 45.9 42.3 49.1 43.1<br />
17
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
The Millennium Development Goals.<br />
The table shows no real progress by <strong>Fiji</strong> in reducing the level of infant and to a lesser extent<br />
maternal mortality (ie MDG 4 and MDG 5), with current performance generally being lower<br />
than the baseline figures of 1990. Because of the importance of this matter both to the MOH<br />
and to the support that AusAID and other donors may provide, it is discussed in considerable<br />
detail at section 5.3. of the report.<br />
4.2. Comparison with <strong>Pacific</strong> neighbours.<br />
Table 17 presents comparative indicators for pacific states and reveals that <strong>Fiji</strong> ranks 92 on<br />
the UNDP Human Development Index, trailing behind Tonga and Samoa. <strong>Fiji</strong> exhibits<br />
double the rate of urbanisation than its neighbours; its teenage pregnancy rate (15-19) is high,<br />
partly accounted for by the young age of marriage of Indo-<strong>Fiji</strong>an females.<br />
Table 12: Selected regional comparative indicators<br />
Indicator <strong>Fiji</strong> Samoa Solomon Is Tonga Vanuatu<br />
Human Dev. Index Rank: 92 77 129 55 120<br />
% population urbanised 51 23 17 24 24<br />
Under 5 mortality rate 2006 18 28 73 24 36<br />
Life expectancy at birth 2006 69 71 63 73 70<br />
% of pop. using improved<br />
47 88 70 100 60<br />
drinking water sources 2004<br />
% of pop. using improved<br />
72 100 18 96 50<br />
adequate sanitation 2004<br />
Age specific fertility rate (15-19) 45 23 69 42 38<br />
births per 1000 women<br />
Contraceptive prevalence 44 43 7 33 28<br />
Sources: 1. UNDP Human Dev. Report 2007/08, 2. UNICEF: http://www.unicef.org/infobycountry<br />
4.3. Morbidity and Mortality.<br />
Table 13 reveals the triple burden of morbidity in <strong>Fiji</strong> as stemming from injury, infectious<br />
diseases and chronic non-communicable diseases. It also shows that non-communicable<br />
diseases account for the greatest part of mortality.<br />
Table 13. The Ten major causes of Morbidity and Mortality in 2007<br />
MORBIDITY<br />
MORTALITY<br />
No Cause No Cause<br />
1 Injury 1 Diabetes mellitus<br />
2 Influenza and pneumonia 2 Other forms of heart diseases<br />
3 Intestinal and infectious disease 3 Ischemic heart diseases<br />
4 Infection of skin and subcutaneous 4 Hypertension<br />
tissues<br />
5 Ischemic heart disease 5 Septicaemia<br />
6 Other conditions originating in the perinatal<br />
6 Cerebrovascular Disease<br />
period<br />
7 Chronic lower respiratory disease 7 Other conditions originating in the<br />
perinatal period<br />
8 Other forms of heart diseases 8 Chronic lower respiratory disease<br />
9 Hypertension 9 Renal failure<br />
10 Diabetes mellitus 10 Influenza and pneumonia<br />
Source: hospital admission<br />
Source: Death certificate<br />
Tables 14 and 15 show that the major causes of mortality in all years are disease of the<br />
circulatory system, which is reported to have increased by 14% in the past 20 years.<br />
Table 14. Major causes of Mortality by diagnostic group 1998-2001 and 2005<br />
CAUSE GROUP 1998 1999 2000 2001 2005<br />
18
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
% % % % %<br />
Disease of the Circulatory System 39.2 43.61 47.7 40.34 26.37<br />
Disease of Respiratory System N/A 7.51 6.1 8.1 8.55<br />
Infection and Parasitic Diseases 10.59 N/A 5.8 10.0 13.4<br />
Neoplasms 9.3 7.63 6.2 N/A 10.62<br />
Endocrine, Nutritional and Metabolic<br />
Disorders and Diseases of the Immune<br />
System<br />
7.27 N/A N/A 9.31 N/A<br />
Table 15 presents the major cause of morbidity for the period 1998-2001, and 2005<br />
presenting to hospitals and health centres. Infectious and parasitic diseases predominate in all<br />
years due to the high incidence of diarrhoeal disease, septicaemia and pneumonia. (Both the<br />
diseases of the Respiratory and Circulatory systems include NCDs).<br />
Table 15. Major causes of Morbidity by diagnostic group 1998-2001 and 2005<br />
CAUSE GROUP 1998<br />
%<br />
19<br />
1999<br />
%<br />
2000<br />
%<br />
2001<br />
Infection and Parasitic Disease 9.86 9.4 7.74 9.02 8.08<br />
Disease of the Respiratory system 9.14 8.6 7.74 9.02 8.08<br />
Disease of the Circulatory System 7.7 7.3 7.7 7.35 6.98<br />
Injury and Poisoning 6.82 6.9 7.4 5.9 N/A<br />
Disease of Genitourinary system 4.9 5.5 5.2 4.72 4.36<br />
Non communicable diseases (NCDs) such as diabetes, heart disease, high blood pressure<br />
and respiratory diseases have now replaced infectious and parasitic diseases as the principal<br />
causes of mortality and morbidity in <strong>Fiji</strong>. The NCD survey in 2002 showed that the<br />
prevalence of hypertension was 19.1% although this is not reflected in the table above as<br />
those patients who are “controlled” are not recorded as a new incidence. It also revealed that<br />
a third of all deaths and half of the deaths in the 40-59 years age group were due to<br />
circulatory diseases. In the year 2000 it was estimated that up to 70% of deaths in <strong>Fiji</strong> were<br />
due to NCDs (CSPF 2005). These diseases arise from the lifestyle factors of poor diet, lack of<br />
exercise, smoking, alcohol misuse and obesity. The revelation of the magnitude of NCD risk<br />
factors by the 2002 NCD STEPS survey highlighted some key reasons:<br />
• around 65% of population take one or less servings of fruits a day,<br />
• 37% currently smoke tobacco, and<br />
• there is a low rate of physical activity (25%) and<br />
• a high rate of binge drinking (77.3% of current drinkers).<br />
AusAID and other donors are providing support to <strong>Fiji</strong> to address its NCD problem through<br />
regional programs targeted at this area.<br />
Obesity: The <strong>Pacific</strong> Obesity Prevention in Communities study has recently released baseline<br />
findings for <strong>Fiji</strong> which include the statistics that “approximately one-quarter of students<br />
….were overweight (26% females; 20% males) and more than 10% were obese (12%<br />
females; 11% males)”..<br />
Diabetes: The major cause of mortality in <strong>Fiji</strong> is Diabetes. The NCD survey in 2002 showed<br />
the prevalence of Type 2 diabetes in <strong>Fiji</strong> as 16% of the adult population, up from the earlier<br />
estimate of 12% (Cornelius 2002), reportedly the third highest rate per capita of diabetes in<br />
%<br />
2005<br />
%
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
the world. One out every seven person in <strong>Fiji</strong> has diabetes. The incidence of diabetes stands<br />
at 500 new cases per year. In 2005 187 amputations were carried out in CWM and one out<br />
every 7 died.<br />
Renal Dialysis: Until recently dialysis was not available in <strong>Fiji</strong>: consequently more than 95%<br />
of kidney patients died from kidney failure because of the lack of access to dialysis and<br />
support programs. The new Dialysis Centre in Suva opened in March <strong>2008</strong>.<br />
Re-emerging and new viral diseases: <strong>Fiji</strong> is still dealing with outbreaks of re-emerging<br />
infectious and vector borne diseases (Typhoid, Tuberculosis, Leptospirosis and Dengue) and<br />
is potentially threatened by newly emerging viruses (SARS, HIV and Highly Pathogenic<br />
Avian Influenza). These threats present the risk of major socioeconomic impacts on <strong>Fiji</strong> and<br />
highlight the need for vigilance in surveillance, border control, detection capacity,<br />
investigation capacity and capacity to respond in a timely and coordinated manner.<br />
HIV & AIDS. While <strong>Fiji</strong> is still considered a low prevalence country for HIV, a rapid<br />
increase in sexually transmitted infections (STI) indicates a risk of increasing HIV<br />
prevalence. As at October <strong>2008</strong>, there have been 271 HIV-positive individuals, a large<br />
proportion of them between the ages of 20 and 29. There had been 12 new cases this year<br />
which is an improvement on the past 3 years. A significant proportion of TB patients have<br />
tested HIV positive.<br />
Dengue Fever outbreaks of have been occurring across the <strong>Pacific</strong> in the last year and <strong>Fiji</strong><br />
has had its first major outbreak for some years. Admissions to hospital continued beyond the<br />
53 cases reported in September <strong>2008</strong> to over 1531 cases in early October. Dengue fever<br />
remains a constant threat during wet periods in <strong>Fiji</strong> and constant vigilance is needed to reduce<br />
mosquito breeding sites.<br />
Nutrition: An impressive quantity and range of traditional food such as root crops, fruits and<br />
vegetables are grown throughout the country, and along with fish, and are identified as a<br />
“hidden strength” of the economy. However it is estimated that only 40% of energy needs<br />
come from locally grown food. Nutritional problems for weaning infants, undernourished<br />
children and adolescents remain. Kumar (2006) found that one third of teenage schoolgirls in<br />
the Western Division were anaemic and that many routinely miss breakfast.<br />
4.4. Key Lifestyle and other issues impacting on health of the people<br />
Lifestyle: The population of <strong>Fiji</strong> is becoming polarised between the employed and the<br />
unemployed, the former able to participate in the modern economy while the latter depend on<br />
subsistence agriculture, fishing and the sale of surplus produce. The social determinants of<br />
health, the migration to urban areas and the transition from the consumption of local produce<br />
to imported refined food items, has resulted in an increase in obesity and non-communicable<br />
diseases.<br />
It is generally believed that transition to the urban lifestyle has proceeded at a faster pace than<br />
<strong>Fiji</strong>’s neighbours. The introduction of television in the 1990s and the growth of the<br />
communications sector have connected <strong>Fiji</strong> to the lifestyles of western cultures. Secular<br />
fashion and behavioural trends are powerful influences on young people while the breakdown<br />
of traditional social controls have allowed behaviours such as binge drinking, cannabis<br />
consumption, an active nightclub scene, sexual promiscuity and commercial sex, the<br />
consumption of ‘fast foods’ and the increase in street kids and homelessness all of which are<br />
readily visible phenomenon of lifestyle change. The greatest challenge is youth<br />
unemployment. Young people of productive working age are commonly seen on the urban<br />
and suburban streets of <strong>Fiji</strong> during working hours. Protracted unemployment with little<br />
prospect of obtaining work contribute to social breakdown, violence and robbery. Other<br />
issues that impact on the health of the people are discussed below.<br />
20
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Poverty: Estimates of poverty in <strong>Fiji</strong> are that 29% of the rural population and 40% of the<br />
urban population are poor; and that poverty (35% of the overall population) is distributed<br />
across the nation. The poor often live in unsafe and overcrowded houses in under-served periurban<br />
shanty towns where exposure to pollution and other health risks are greatest. They are<br />
most likely to indulge in risky behaviours out of circumstances rather than by choice, often<br />
going hungry or eating poor quality foods, living stressful lives, indulging in personal habits<br />
such as drinking of kava and smoking tobacco to obtain comfort and to socialize.<br />
Squatting: It is estimated that by 2006 the Suva/Nausori corridor will have 15,000 squatter<br />
households with a population of 90,000-100,000 people. This will place a large strain on the<br />
entire urban infrastructure, such as water supply, sewerage, electricity, roads, traffic<br />
congestion and social services.<br />
Water and sanitation: Many of the rural water supply systems built during the colonial<br />
period are now deteriorated to the degree that village water systems are sources of diarrhoeal<br />
diseases. It is understood that UNICEF will be giving particularly priority to the availability<br />
of safe drinking water in rural areas in the coming years and that the MoH will work with<br />
SOPAC to improve <strong>Fiji</strong>’s water and sanitation systems.<br />
The cost of food: <strong>Fiji</strong> is a net importer of food and its agricultural potential for food<br />
production is largely underutilized. Much of <strong>Fiji</strong>’s arable land has been devoted to sugar<br />
production, but as land leases expire land is left fallow without any plans for further<br />
development. For <strong>Fiji</strong> to develop a viable food export sector, the quality of food produced<br />
will need to be increased to meet the expectations of recipient markets. Many of the older<br />
sugar cane leases are now lying idle and potentially there is now more arable land available<br />
for food than in recent years. This is not to say that food prices will not rise. However in the<br />
current economic climate it is simply not possible for this assessment team to make any<br />
prediction and its likely impact on health.<br />
Global warming: There have been some suggestions that global warming could cause a shift<br />
in the epidemiology of some diseases (eg: vector borne diseases such as Dengue Fever, where<br />
increased rain fall has been associated with an increase in the number of reported cases). This<br />
has relevance to <strong>Fiji</strong> as dengue fever is a major risk to the community. The IGOF does have a<br />
strong mosquito monitoring program that can detect early increases in vector numbers. It is<br />
important that this service be continued.<br />
Suicide rates for the population as a whole are reportedly 26 per 100,000 and above the world<br />
average of 16 per 100,000 (WHO), however, the rates for Indo-<strong>Fiji</strong>ans (24 per 100,000) well<br />
exceeds that of <strong>Fiji</strong>ans (4 per 100,000). The suicide rate among Indo-<strong>Fiji</strong>an females is<br />
reportedly among the highest in the world (Booth 1999). Anecdotally, these are due to family<br />
expectations of academic performance and young marriage, where the pressures associated<br />
with being a daughter-in-law are thought to contribute to stress. This situation illustrates the<br />
tensions between traditional family expectations and those of the modern world.<br />
5. KEY ISSUES ARISING FROM THIS SITUATIONAL ANALYSIS<br />
During the period of this short “snapshot” mission, a number of issues emerged that are<br />
discussed below. They include<br />
• Poor perception of the health services by the public<br />
• Changes in demographics and social behaviour require a rethink of the location,<br />
staffing and range of services provided by health facilities.<br />
• Relatively poor progress towards the achievement of <strong>Fiji</strong>s MDGs.<br />
21
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
• Old or non-functioning equipment impacts on service delivery<br />
• Stock outs of essential drugs<br />
• The importance of more focused planning and better use of management information<br />
systems<br />
• The health sector should be seen as being more than just the MoH<br />
• There is a need for evidence based approach to policy and planning<br />
In addition financial constraints and staffing issues - and especially shortages of specialist<br />
medical officers - are recognised as very important issues but these have been discussed in<br />
detail at section 3 of this report and are not discussed further here.<br />
The issues listed above are perhaps best described as “big picture” operational or structural<br />
issues. Some have a bearing on the effective functioning of the health system (e.g. shortages<br />
of equipment, drug outages; financial and workforce constraints), others relate to such issues<br />
as equitable access and highlighted the need for a review of the location and staffing of health<br />
facilities to improve access, while others might better be described as the end results of<br />
problems that are occurring within the system. This latter group includes such issues as the<br />
failure to achieve the MDGs and a poor perception of the health services by the public. They<br />
are presented here in no particular order of priority. This is because they are all very closely<br />
inter-related and addressing some will have influence on the others.<br />
No attempt has been made to in this section of the report to discuss the importance of specific<br />
diseases such as HIV/AIDs and NCDs which are clearly a problem for <strong>Fiji</strong>. They have been<br />
adequately addressed in section 3.3. above.<br />
5.1. Perception of the health services by the public.<br />
The people of <strong>Fiji</strong> appear to be increasingly critical of the health care system. This is publicly<br />
reflected in current articles in the press and the electronic media. More privately, it is<br />
reflected by comments given by patients and from health care staff to the team that patients<br />
often complain to them. Some health care staff seen during the mission indicated that they too<br />
are concerned and now use the private system for their own family’s health care needs.<br />
5.1.1. Nature of the Public Concerns<br />
Based on media reports and a small number of interviews undertaken during this mission<br />
(and confirmed by local staff), public dissatisfaction appears to lie in four key areas:<br />
• Frequently long waiting times (> 4 hours) for treatment in general outpatients<br />
departments especially at CWM hospital (Suva) and Lautoka hospital.<br />
• The often lack of the essential drugs that the doctor wishes to prescribe – which<br />
becomes more frustrating if patients have waited several hours. This situation is<br />
improving in some Divisions (see 5.5.)<br />
• The breakdown of equipment, with the doctor telling the patient that they are unable<br />
to do important tests because the necessary equipment is not working.<br />
• Patients are charged for services at a hospital when they thought that it would be free<br />
(presumably doctors had rights of private practice).<br />
These comments are also reflected in comments and formal complaints to the Consumer<br />
Council of <strong>Fiji</strong>. They receive complaints in relation to both the public and private sectors.<br />
Press releases from the Consumer Council discussing the nature of these complaints are<br />
shown in Annex 12. Unfortunately the Consumer Council have not, in the past, maintained a<br />
data base of the number of each type of complaint. Trends therefore cannot be measured.<br />
22
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
However the assessment team was informed that a new data base has been installed and that<br />
this information should be available in future years. The MoH therefore may gain benefit<br />
working closely with the Council to monitor the level and nature of complaints and compare<br />
them with their own surveys.<br />
Despite these ongoing complaints, no recent surveys of waiting times have been carried out<br />
in general outpatient departments of the larger hospitals. Nor have customer satisfaction<br />
surveys been done throughout the hospital. At the CWM, the team were advised that<br />
management of the outpatient and accident and emergency departments would welcome<br />
assistance in carrying out such surveys and asked if FHSIP would include them in their work<br />
plans for 2009. Such surveys would provide more information on the level of dissatisfaction<br />
and whether it is reflected throughout the country or more likely to be associated with<br />
services in the divisional hospitals where workloads are highest –anecdotal evidence suggests<br />
the latter.<br />
5.1.2. Continuing Complaints lead to staff dissatisfaction<br />
Importantly these ongoing complaints, and the poor recognition by the public of the work<br />
being done by health care professionals is very demoralising to staff, who often make<br />
considerable sacrifice to provide the best service possible with the resources they have been<br />
given. This view was continually repeated to the assessment team. This dedicated<br />
commitment, under difficult circumstances, with lack of any real recognition, was often cited<br />
as a major reason for staff leaving the government system – either to go into private practice<br />
or to migrate. The evidence presented to the assessment team is that the current situation is<br />
not acceptable to a wide range of staff members, as reflected in the figures given in Table 5<br />
showing high levels of staff turnover.<br />
There are three key pillars for a successful primary health care service: (a) access, (b)<br />
affordability and (c) acceptability. The current health service in <strong>Fiji</strong> does not appear to be<br />
meeting the latter. Senior staff within the MoH are aware of this and expressed the view that<br />
they would like to see this issue addressed - especially the problem of long waiting times at<br />
general outpatient departments at the larger hospitals.<br />
Recommendation 3<br />
The MoH should consider undertaking regular surveys at the major hospitals (and other<br />
centres) to determine waiting times for patients attending at different times of the day and on<br />
different days. Concurrently, independent patient satisfaction surveys could be carried out to<br />
explore other issues such as staff attitude and drug outages. The results from such surveys<br />
could guide the implementation of a Service Improvement Program. The FHSIP should be<br />
asked to include funding for such surveys within its workplan for 2009.<br />
5.2. Changes in demographics and social behaviour require a rethink of the<br />
location, staffing and range of services provided by health facilities.<br />
As discussed in section 3.2. the model currently in place in <strong>Fiji</strong> to ensure access to health<br />
services is a traditional one, based on providing easy access (usually within 1 hour) to a<br />
health facility, with provision for referral to more comprehensive services if required. The<br />
progression from community health worker to nursing station, health centres; subdivisional<br />
hospital and finally referral to a divisional hospital has served the people of <strong>Fiji</strong> well over the<br />
years – it is widely regarded in the region. It was developed to give substance to the long<br />
stated goal of providing access to a basic level of primary health care to all those living in the<br />
<strong>Fiji</strong> Islands.<br />
23
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
This model remains relevant today. However it was obvious to the assessment team that, after<br />
30- 40 years in many cases, the building blocks that go to make up this model urgently need<br />
review. This conclusion was supported by managers met by the team during this mission.<br />
There have been many changes during this period. These include (a) demographic and (b)<br />
social changes, (c) improvements in transport and (d) changes in medical practice and<br />
standards. These factors are discussed below<br />
Demographic changes. Demographic changes alone warrant a review of the location and<br />
staffing of health centres and nursing stations. Overall population in many areas has increased<br />
since most facilities were built. The 2007 census indicates that Central division population<br />
has increased 15% since 1996. Equally interesting is the fact that over the past 4 years, the<br />
annual average number of births at CWM hospital was 6,540. This represents a 10% increase<br />
over the average number of deliveries for the preceding 4 years.<br />
Importantly, there has also been a steady drift to urban areas that has accelerated in the last 2<br />
years following the termination of many sugar leases in the Western and Northern Divisions.<br />
See section 4.5 squatting.<br />
Improvements in public and private Transport. In recent years car ownership has increased<br />
and there has been an improvement in roads; bus services are now available in many areas of<br />
the country. The team heard that this has greatly influenced the mobility of patients and they<br />
are taking advantage of it. Patients are now (a) by-passing many health facilities and<br />
travelling to centres where they can see a doctor (not only a nurse) and have more chance of<br />
getting drugs and (b) some strategically placed health centres e.g. on main roads or bus<br />
routes, are receiving increased patient numbers while others have seen significantly reduced<br />
workload; However staffing levels usually remain little changed. One health centre, with a<br />
staff of one doctor/nurse practitioner and three nurses sees 10 patients per day (15-20 on days<br />
when antenatal or vaccination clinics are held) whereas in another centre one doctor saw in<br />
the order of 100 patients per day. The team was assured that such imbalance between staffing<br />
establishment and workloads is not rare. Clearly some centres have too many staff while<br />
some centres have too few. This is in stark contrast to the long waiting times being<br />
experienced in the outpatient departments of the divisional hospitals because of staff<br />
shortages.<br />
Social Changes. <strong>Fiji</strong>ans, and especially those in the larger cities, are increasingly travelling,<br />
watching television, reading magazines and using the internet. They are aware of modern<br />
trends in medical practice in other countries, especially in Australia and New Zealand where<br />
many have family members. As patients, they have increased expectations. There is an<br />
expectation that they will be seen by a doctor, have an X-ray and blood taken at the same<br />
time. They would like their health facilities to open for longer hours so that they can visit<br />
after work. There is frustration that most health facilities close at 4.00pm<br />
Patients are seeking to bypass smaller centres and go to the hospitals (where there are<br />
extended opening hours) and larger health centres where there is a doctor and other facilities.<br />
Improved transport links are making this possible. Unfortunately this results in the long<br />
waiting times at hospitals in the evening.<br />
Changing Medical standards. An increasing focus on improving the quality of medical care<br />
through the introduction of “best practice” has resulted in decisions that surgery must only be<br />
undertaken by qualified and registered specialist surgeons. This also puts increasing demands<br />
on improved diagnostic facilities. Because of the acute shortage of specialist surgeons, and<br />
the imposition of these more stringent standards, older established practices are no longer<br />
acceptable. This is especially noticeable in subdivisional hospitals where in past years<br />
considerable surgery was undertaken. Currently not one sub-divisional hospital routinely<br />
performs surgery although some occasionally host visiting surgical teams from the larger<br />
24
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
divisional hospitals or even from overseas. As stated earlier sub- divisional hospitals provide<br />
low risk antenatal and birthing care for the subdivision and are functioning as little more than<br />
larger health centres. Their operating theatres lie idle.<br />
As a result of these demographic and social changes, together with improved transport links<br />
and stricter medical standards, the current service delivery model needs review. The basic<br />
framework is appropriate, but many of the building blocks require change. Currently staff are<br />
not always being utilised effectively and patients are not receiving the level of service that<br />
they are seeking. Without change this will prove to be a barrier to meaningful improvement<br />
in the health system in <strong>Fiji</strong>.<br />
1. There is an urgent need to review the location and function of current health<br />
facilities. Some may need their role re-assessed, or be enlarged and a wider range<br />
of services offered e.g. X-ray and laboratory services. In some cases, where a<br />
decision is made to change a role, additional vehicles may be needed to provide a<br />
more comprehensive home visiting service.<br />
2. Staff establishments levels will need to be reviewed<br />
3. There may be a need for new cadres of multi-skilled staff<br />
4. In some cases opening hours will need to be extended<br />
5. possibilities should be explored for making use of private GPs to support busy<br />
centres – especially after hours or as locums<br />
6. Consideration may need to be given to closing general outpatient departments at<br />
divisional hospitals and allow them to focus on genuine accident and emergency<br />
cases<br />
7. In such cases the size, location, staffing levels, range of services and opening<br />
hours of nearby health centres will need to be reviewed. New “hyper centres” may<br />
need to be created to offer services to out-patients who are now going to the<br />
divisional hospital. These would be larger than traditional health centres, provide<br />
a wider range of services including X ray, pathology and dental treatment and be<br />
open until later, perhaps as late as 8.00pm in the evening.<br />
These changes are apparent to managers within the respective divisions. Such changes have<br />
been occurring in many countries for many years.<br />
Recommendation 4<br />
The MoH should consider undertaking a review of the location, functions, staffing levels and<br />
operating hours of the current network of nursing stations, health centres, subdivisional and<br />
divisional hospitals to ensure that they better serve the needs of the people of <strong>Fiji</strong>.<br />
It is recognised that external assistance may be required for such a Review and development<br />
partners should look favourably on providing such support as it will offer the potential to<br />
significantly improve the efficiency of service delivery.<br />
The Clinical Services Planning Framework, developed with support of the FHSIP, should be<br />
a key tool in this exercise.<br />
5.3. Relatively Poor progress towards Achievement of <strong>Fiji</strong>’s MDGs and other<br />
designated KPIs.<br />
5.3.1. The Current Position.<br />
As indicated in section 3.1. <strong>Fiji</strong> made considerable progress in improving its key health<br />
indicators during the period up to 1990, when its key indicators were seen to be excellent.<br />
During that period, life expectancy, and both maternal and infant mortality improved<br />
25
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
significantly, with MMR improving from 156.5 (per 100,000 live births) in 1970 to 53.0 in<br />
1980 and 26.8 in 1990.<br />
However since the mid 1990s, progress has stalled as shown in the table 17 below and in<br />
table 11 in Section 4.1. This is particularly disappointing in the case of <strong>Fiji</strong>s targeted<br />
Millennium Development Goals (MDGs). In 2000 <strong>Fiji</strong> committed to its people (and to the<br />
World) that by 2015 it would achieve the targets for maternal and infant mortality and for<br />
control of HIV/AIDs and tuberculosis listed below in Table 16.<br />
Table 16. <strong>Fiji</strong>’s MDG Targets by 2015<br />
Target<br />
Reduce by 2/3 between<br />
1990 and 2015 the under<br />
five mortality rate<br />
Reduce by 3/4 between<br />
1990 and 2015 the<br />
maternal mortality rate<br />
Have halted by 2015 and<br />
begun to reverse the<br />
spread of HIV/AIDS<br />
Indicator<br />
1990<br />
Baseline<br />
2015<br />
Target<br />
Under-five mortality rate per 1000 live births 27.8 9.3<br />
Infant mortality rate per 1000 live births 16.8 5.6<br />
Proportion of 1 year old immunized 86% increase<br />
Maternal mortality rate per 100,000 live births<br />
26.8 10.3<br />
HIV prevalence among 15-24 year old pregnant<br />
women 0.00% 0.00%<br />
Data in Table 17 clearly shows that the MoH is not meeting these targets and under 5<br />
mortality, infant mortality and maternal mortality are not only worse than the commitment<br />
given in the MDGs in 2000, but are considerably worse than the status in 1990. The situation<br />
has been steadily deteriorating since that time, with the exception of maternal mortality in<br />
2007 when some improvement is noticed. In relation to maternal mortality the absolute<br />
number of deaths is relatively small and 1 or 2 extra deaths can significant change the MMR.<br />
Table 17 Progress towards achievements of MDG 4 and 5<br />
Year Child (< 5 )<br />
Mortality<br />
Infant<br />
Mortality<br />
Maternal<br />
Mortality<br />
1990 Na 16.8 26.8<br />
1995 19.30 14.70 60.40<br />
2000 21.8 16.20 57.50<br />
2005 25.8 20.70 67.3<br />
2007 22.4 18.4 31.1.<br />
MDG 9.3 5.6 10.3<br />
As stated earlier HIV/AIDS cases continue to occur, although only 12 new cases were<br />
recorded so far in <strong>2008</strong>. There were approximately 80 cases of TB last year – of which 84%<br />
occurred in the Central division, The majority were pulmonary TB.<br />
Childhood Deaths<br />
The main causes of death for children under 5 and immunisation coverage rates (another<br />
target within MDG 4) are shown in Annex 14.<br />
Clearly there has been variation from year to year in the causes of childhood mortality but the<br />
disturbing feature is the very high incidence of death due to peri-natal conditions. These perinatal<br />
deaths (200-275 per year over the past 5 years) are most associated with sepsis,<br />
congenital malformations incompatible with life, gross prematurity, peri-natal asphyxia,<br />
meconium asphyxia, severe HMD and more recently, a re-emergence of congenital syphilis.<br />
In general there has been little improvement in vaccination coverage rates except for measles<br />
in 2006. In this case coverage had dropped to 68% in 2005, resulting in a large measles<br />
26
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
outbreak in the country. This became the trigger for mass immunisation program with<br />
reported coverage of 100% in 2006 but this has slipped back to 80% in 2007.<br />
Causes of maternal mortality<br />
The main causes of maternal mortality from 2001 to 2007 (and number of deaths) are also<br />
shown in Annex 14. and include ectopic pregnancy, PET/eclampsia; PPH, cardiac disease<br />
and septicaemic( puerperal infection). Of the 68 maternal deaths during the period, 55 (85%)<br />
were classified as obstetric maternal deaths and 13 (15%) were classified as incidental<br />
maternal deaths.<br />
5.3.2. Changing patterns of antenatal care<br />
It is well established that timely and professional antenatal care is a key factor in reducing<br />
both maternal and infant mortality. Advice on lifestyle and diet during pregnancy, testing for<br />
infectious diseases such as HIV and STI and a physical examination to determine the<br />
likelihood of a regular or “difficult” delivery are all vital for safe motherhood and healthy<br />
child. The team was told that antenatal practice may be changing. In previous years it was<br />
practice for women to present for their first antenatal visit during the first trimester and that<br />
this is still current teaching in nursing school (< 12 weeks). However data presented to the<br />
team indicates that this is no longer necessarily the case and that women are presenting later<br />
for their first antenatal visit, although this may vary from area to area/hospital to hospital.<br />
Table 18 Trimester of First Antenatal visits<br />
CWMH (%) Lautoka Hospital (%)<br />
2006 2007 ) 2006 2007<br />
Trimester 1 833(17) 307(9) 370(18) 409(18)<br />
Trimester 2 2857(57) 4246(83) 1071(53) 1129(50)<br />
Trimester 3 1081(22) 493(9) 539(26) 674(30)<br />
Unbooked 167(3) 98(2) 27(1.3) 40(2)<br />
TOTAL 4988 5090 2007 2252<br />
This data for these two hospitals is subject to some margin of error as some cases may not be<br />
included although the trend is apparent. However, as discussed at 5.8, more detailed data is<br />
needed on antenatal care in <strong>Fiji</strong>.<br />
Congenital syphilis as an end-point indicator of antenatal practice.<br />
An indirect measure of the deterioration in this area is the striking increase in the number of<br />
cases of congenital syphilis among newborns. In CWM there were 132 cases in 2007 and to<br />
September <strong>2008</strong> there had been 162 cases out of 5,635 live births. In the period July-<br />
September there were 68 cases out of approx 1800 births.<br />
This high incidence of congenital syphilis is a concern in its own right but it is also an “end<br />
point indicator” of a potential quality decline in antenatal care in <strong>Fiji</strong>. More research is<br />
needed but key questions need to be asked<br />
• At what stage did mothers present for their first antenatal visit; were there follow up<br />
visits?<br />
• Was blood taken for serology at this first visit or were serology tests done at<br />
subsequent visits?<br />
• Were laboratory results relayed back to the doctor/nurse who saw the expectant<br />
mother?<br />
• Was there discussion during antenatal visits of the dangers of HIV and STI?<br />
27
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Congenital syphilis is a very preventable disease and, as stated above, it can serve as an<br />
endpoint indicator of the quality of antenatal care. It can also serve as a measure of condom<br />
use. A decline in incidence of congenital syphilis may serve as an indicator of improvement<br />
in either or both of these areas.<br />
Recommendation 5<br />
A carefully planned study should be undertaken of antenatal care practices in <strong>Fiji</strong>, which<br />
should include women in both urban and rural areas.<br />
5.3.3. Why has progress towards the achievement of MDGs 4 and 5 been so slow?<br />
The assessment team were advised by obstetricians, paediatricians, midwives and nurses that<br />
many of these infant and maternal deaths were preventable. If this is true the question must<br />
be asked “Why are these deaths still occurring and why is progress towards achievement of<br />
the MDGs 4 and 5 so slow?”?<br />
Some reasons for this have already been discussed and include poor equipment and<br />
consumables (including alcohol wipes, re-using disposable gloves etc) , shortage of specialist<br />
staff (e.g. obstetricians, paediatricians, experienced midwives, neonatal nurses), of general<br />
practitioners in rural areas; changing patterns in antenatal care as represented by women<br />
attending their first antenatal visit later in pregnancy. These represent technical/professional<br />
reasons that have contributed to slow progress towards achievement of MDGs.<br />
However, while a reduction of maternal and infant mortality are key performance indicators<br />
for the Ministry, the assessment team were informed that there is no focused plan of action in<br />
place that specifically addresses these problems. While areas within corporate plans for the<br />
public health department have relevance, as do plans for curative service department and<br />
individual hospital plans, a specific plan that addresses maternal or infant mortality must by<br />
necessity, cross both departments. The team was informed that no such focused plan exists.<br />
There is thus a need to bring more focus to these issues if the MDGs 4 and 5 are to be<br />
achieved.<br />
This must be reflected not only in stated goals or KPIs but in action plans that work to<br />
achieve these goals. Such plans need to bring to the problem the resources of both public<br />
health and curative (hospital) departments but also support of relevant NGOs, international<br />
agencies (WHO, UNICEF, UNFPA) and private medical practitioners. That is, it needs to<br />
engage the whole health sector and not just the Ministry. To a large extent this has happened<br />
in the area of HIV/AIDS, where there is a dedicated national strategic plan for HIV and the<br />
National AIDS Committee takes a cross sectoral approach. This need for more focused<br />
planning is discussed further below.<br />
5.3.4. Benefits will flow to the whole health sector.<br />
As discussed above, progress towards achieving the goals in the area of maternal and infant<br />
mortality involves improvements in both preventive health and clinical practice. It cuts across<br />
all areas of the health system. Thus any plan that targets a reduction in the levels of both<br />
infant and maternal mortality will, de-facto, go some way towards improving the health<br />
system overall. It will require improved antenatal care, improved vaccination coverage;<br />
reduction in incidence of STI, improved patient referral and transport services, fewer “stock<br />
outs” of drugs, more reliable, functioning equipment and improved cross infection control at<br />
all levels of health care.<br />
28
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
Recommendation 6.<br />
The MoH and its partners should consider developing “action” plans that focus specifically<br />
on reducing the levels of infant and maternal mortality. Such plans should cut across all<br />
departments of the MoH and engage with all relevant parties both within and outside of the<br />
Ministry.<br />
5.4. Old or non-functioning equipment impacts on service delivery<br />
A consistent problem presented to the assessment team was a shortage of essential equipment<br />
that was in good working order. The team heard that in some nursing stations and health<br />
centres, simple but essential equipment such as stethoscopes and sphygmomanometers were<br />
not functioning. In all facilities visited the team inspected essential equipment in key areas<br />
such as neonatal intensive care; obstetrics; accident and emergency; outpatient departments<br />
pathology, radiology and in health centres and nursing stations. Problems include:<br />
• Often essential equipment was very old. For example x-ray equipment in Lautoka<br />
hospital dates to 1986 (2 machines) and 1993 and 1996. The mammography machine<br />
was donated (as a second hand unit) in 1996. It is important for a successful<br />
replacement policy that the date of purchase (or date of manufacture for “second<br />
hand“ donated equipment) and the recommended replacement date should be included<br />
in the newly developed Asset Register. This should apply even for older equipment<br />
that was already in the facilities before the Registrar was put into use.<br />
• There is a shortage of funds to purchase new equipment or the processes required to<br />
purchase it were too bureaucratic even for small, inexpensive equipment. The<br />
biomedical equipment budget for the past 6 years is given in Table 9. It has not<br />
increased during the period 2003 to <strong>2008</strong>. More strikingly the percentage of funds<br />
allocated in the biomedical budget was 1.7% of the total health budget in 2003 and<br />
had declined to 1.0% in <strong>2008</strong>. To bring the <strong>2008</strong> biomedical budget back in line with<br />
the budget of 2003 would have required that an additional $ 1.05 million be allocated<br />
for procurement of biomedical equipment. Even the 2003 budget allocations are low<br />
when compared with actual needs.<br />
Repairs, maintenance and the supply of consumables are equally important. The team’s<br />
findings revealed that:<br />
• In many instances spare parts are no longer available as the type of equipment has<br />
long ceased being manufactured.<br />
• There were consistent reports of slow response from the biomedical department<br />
because they were simply overloaded with requests - the time taken was even worse<br />
for the smaller and more remote health centres<br />
• Very long delays in obtaining spare parts or vital consumables - putting essential<br />
equipment out of use for several months. This was not always a matter of the cost of<br />
the spare part - with delays often due to overly lengthy bureaucratic “processes” even<br />
for the smallest items. Examples include:<br />
o<br />
microscopes being out of use for 3-6 months because of delays in getting a<br />
bulb for the microscope lamp;<br />
o vital monitors in a neonatal intensive care unit being inoperable because of<br />
delays in getting replacement probes; with one probe being rotated between 3<br />
children even though each child should have been monitored 24/7 and<br />
importantly, with the added risk of cross infection. This is important because<br />
nosocomial infections have been a significant cause of neonatal deaths in <strong>Fiji</strong>.<br />
29
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
o in one obstetric department, the CTG (cardiotomograph) machine for<br />
monitoring foetal heart rate and maternal contractions, was new but no paper<br />
was available to record the charts so patients could not be monitored.<br />
• In many instances maintenance contracts with the supplier are relatively expensive<br />
and often no formal internal maintenance programs are in place.<br />
Recommendation: 7<br />
All options should be explored on ways to increase the level of funding made available<br />
through the national budget and through development projects for the standardisation and<br />
procurement of essential biomedical equipment. Similarly, options should be explored on<br />
ways to increase the level of funding available for maintenance and repairs of biomedical<br />
equipment and to simplify the processes for the procurement of replacement spare parts and<br />
consumables.<br />
Recommendation 8.<br />
Recognising the very critical state of biomedical equipment procurement and repair,<br />
development partners might consider a large scale biomedical equipment project that seeks to<br />
purchase standardised equipment for the divisional hospitals in order to bring equipment up<br />
to acceptable levels. Any such project should also review the processes required for the<br />
maintenance of equipment and purchase of spare parts.<br />
Such a project should work with but be outside of the current support that AusAID is giving<br />
to strengthening biomedical engineering departments within the region.<br />
5.5. Stock Outs of Essential drugs<br />
The often poor availability of essential drugs was frequently presented as a significant<br />
problem that contributed to sub-optimal patient care and to patient dissatisfaction and<br />
frustration with the system. As an extreme example the team was informed that some patients<br />
travel from Levuka (an eastern island) to CWM hospital primarily because they cannot get<br />
the necessary drugs in Levuka.<br />
Despite this concern, there is evidence that the situation is improving in most areas. The<br />
essential drug list has now been subdivided into (a) vital (b) very essential and (c) essential.<br />
Progress has been made in the past 12 months with support from FHSIP so that outages now<br />
occur very rarely in the vital drug category and on Viti Levu, where deliveries are made from<br />
the pharmacy store to the health facilities on a monthly basis, stock outs of other drugs are<br />
now occurring less frequently.<br />
However in the Northern Division, where deliveries remain on a quarterly basis, the team was<br />
informed that stock outs occur far more frequently. The team saw direct evidence of this,<br />
where only 50% of the quantities of drugs ordered by the facility had been delivered and a<br />
patient was not able to receive the necessary treatment for their hypertension. Apparently this<br />
is a regular occurrence. There is no good monitoring program in place to assess levels of<br />
drugs in the health facilities on a regular basis.<br />
There would be benefit if the FHSIP continued its work to strengthen the <strong>Fiji</strong> pharmaceutical<br />
store, including an audit of pharmacy, its processes and staff.<br />
Recommendation 9<br />
Although access to essential drugs at the health facility level is improving and “stock outs”<br />
are occurring less frequently, more needs to be done, especially in the Northern Division. It is<br />
30
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
important that a system to monitor drug “stock outs” on a weekly basis in health facilities be<br />
instituted so that in future stock outs do not occur.<br />
Any steps to improve the efficiency of drug supply should include a formal audit the central<br />
pharmacy store, its processes and an assessment of the technical capacity of the staff to<br />
ensure that their skills match the needs of the job. If the charter board agrees, FHSIP should<br />
be able to continue its support in this area during 2009, and include such an audit in its<br />
workplan.<br />
5.6. The importance of more focused planning and better use of management<br />
information systems.<br />
In a dynamic management environment, business plans are developed that target the<br />
attainment of preset goals – with indicators being selected to guide progress towards these<br />
achievements i.e. they become stepping stones. Data that measures progress is collected and<br />
analysed daily; weekly or monthly depending on the targets e.g. data to review bed<br />
occupancy rates would be collected and measured daily so that staffing levels can be adjusted<br />
to match the occupancy rates and if necessary moved between different wards of a hospital to<br />
obtain best efficiencies and best care for the patient. In such a working environment plans are<br />
dynamic and are adjusted if necessary to take account of changing circumstances e.g. shift in<br />
target population; predicted shortages in drugs; changing community needs. The key<br />
elements of such an environment are (a) plans are focused on achieving defined goals e.g.<br />
MDGs; (b) good data is collected and acted upon in a timely manner and (c) plans are not<br />
static- they are not printed once a year and stored in a drawer for the remainder of the year.<br />
During this assessment the team found that few departments use plans as management tools<br />
in a way that guides their day to day operations towards achievement of objectives; no one<br />
indicated that they revise their plans if the need arises.<br />
Unfortunately the team observed that planning and management within many areas of the<br />
MoH is more static. Plans tend to be prepared annually and not reviewed on an ongoing basis.<br />
Such plans tend to be department focused e.g. public health; curative services; corporate<br />
services. The team was told that, with the possible exception of HIV/AIDs, broad crossdepartment<br />
plans were rarely prepared. As stated in section 5.3. there are few plans that might<br />
be described as “action plans”. They are rarely linked directly to achieving key performance<br />
indicators, and there appears to be a “disconnect” between corporate plans and the actions<br />
needed to achieve preset goals (KPIs).<br />
The fact that plans did not generally recognise the need to cut across multiple departments is<br />
unlikely to apply only to the MoH – it is common in many large bureaucracies. However if<br />
there is to be a greater focus on achievement of KPIs; it should begin with a review of the<br />
planning, monitoring and evaluation processes.<br />
Currently large volumes of information are collected throughout the health sector – as<br />
reflected in the various data sets presented in section 3 of this report. However much of this<br />
data is “static”. It is collected at all levels of the health care chain sent to divisional offices<br />
and on to head office in Suva. The collated data is used in annual reports and to some extent<br />
in planning. There needs to be developed a culture of performance management and<br />
monitoring that collects the type of data that can be used to make ongoing management<br />
decisions on a day by day basis. Examples might include collecting accurate data on waiting<br />
times in general outpatient departments on a daily basis and basing staff rosters on the<br />
anticipated waiting times; taking action to address causes of individual maternal and infant<br />
deaths on a “real time” basis, based on weekly or monthly data and adjusting overall plans<br />
accordingly; recognising a concerning increase in congenital syphilis and taking action “at<br />
the root cause’ level to address the problem.<br />
31
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
As stated above there is little evidence that data is being captured in a way that enables it to<br />
be used on a daily or weekly basis to improve quality and effectiveness of the health care<br />
system. PATIS, if used widely, can be used as an effective management tool. For example the<br />
hospital pharmacy is using it routinely to measure stock levels of certain drugs among its<br />
various wards so it is in a position to reallocate drugs from one ward to another if that is<br />
needed; it can also use it to monitor for theft of drugs; and - if there is a sudden increase in<br />
the costs of drugs within a hospital PATIS, can provide information to see if the cost<br />
escalations are due to one or two expensive drugs being prescribed by a new doctor. As stated<br />
above it is being used to monitor ward occupancy and allocate staffing hours and the<br />
radiology department is using it in many ways. However it has not been widely used outside<br />
of the hospital setting and its full potential is not being felt. PATIS is potentially an important<br />
management tool but it needs “champions” who understand the benefits that a “relational data<br />
base” can provide and staff need more training on how to use it effectively.<br />
The concepts of (a) the Project Officer (PO) and (b) Performance Enhancement Projects<br />
(PEP) introduced through the FHSIP are exceptions to the principles raised in the discussion<br />
above. In both cases the PO, or responsible PEP manager, set a target and develop a plan to<br />
achieve that target. If there is need for change in that plan, those changes are made. It is the<br />
achievement of the objective and not the original plan that has been the key to success of the<br />
project officers and PEP concepts. These “models” can serve as examples to be used more<br />
widely throughout the MoH. Improvements in the use of good management information will<br />
help.<br />
This report proposes that beyond 2009. AusAID may wish to continue to support a program<br />
of capacity development in key areas (see section 6.3.). The skills needed to develo more<br />
targeted “action plans”, to use management information to monitor progress towards<br />
achieving the objectives of these plans, might well be one such area of where capacity could<br />
be further developed.<br />
5.7. The health sector should be seen as being more than just the MoH.<br />
The health “sector” within <strong>Fiji</strong> is changing. Some aspects of these changes have been<br />
discussed above at Section 5.2. However significant changes are also taking place in the<br />
nature of the “partners” within the health sector. While the MoH is by far the major provider<br />
of services, they are by no means the only provider and many other partners are now making<br />
an important contribution. It is important that the increasing role that these “partners” are<br />
playing is fully recognised. This is especially so when (a) compiling statistics on service<br />
delivery –e.g. number of services, type and location of services; (b) estimating the total cost<br />
of health services in <strong>Fiji</strong> which should include out-of- pocket expenses – estimated to be 35%<br />
of government expenditure and (c) planning to address key national targets such as the MDGs<br />
and national health KPIs.<br />
5.7.1. Other Service Providers and Partners.<br />
Apart from the MoH, other key partners of the <strong>Fiji</strong> health sector include:<br />
A large and organised private medical sector.<br />
This consists of:<br />
• more than 120 private medical practitioners– including a small number of specialist<br />
medical officers. This represents some 25% of all doctors in <strong>Fiji</strong>. Although the exact<br />
volume of their work is not certain it is estimated to be of the order of 400,000 to<br />
600,000 consultations per year (approx 80-100/doctor/week).<br />
32
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
• One established private hospital with X ray, pathology, and other support services.<br />
Several specialists working within the government service have rights of private<br />
practice to operate within the private hospital on an out-of-hours basis. Others are<br />
from FSMed or are independent private practitioners.<br />
• One small private hospital/clinic with more limited services. The team learned that a<br />
private hospital was soon to be established in Lautoka.<br />
• 49 private pharmacies staffed by 50 qualified pharmacists.<br />
A growing number of NGO service providers<br />
While in the past the core business of most health sector NGOs was training, advocacy and in<br />
special circumstances support and relief (e.g. Red Cross), this position is changing. As an<br />
example the NGO <strong>Pacific</strong> Counselling and Social Services (PC&SS) currently provides a<br />
national counselling service. It has counselling centres in Lautoka, Nadi, Suva and Labasa, an<br />
operating budget of over $800,000 and employs more than 60 staff including 36 diploma<br />
qualified counsellors. Although it has a MOU with the MoH, it receives only minimal<br />
funding from them. PC&SS provides the majority of professional counselling services in <strong>Fiji</strong><br />
- initially through specialised services to HIV positive patients and those being tested for<br />
HIV. However the range of patients is now very broad and includes hospital based<br />
counselling and social services work. PC& SS also provides training to others.<br />
Marie Stopes is another NGO that provides a wide range of services directly to the <strong>Fiji</strong><br />
public. It operates a family planning clinic in Suva staffed by a doctor and outreach clinics<br />
staffed by 2 doctors and 2 nurses. It also distributes condoms directly and through a social<br />
marketing program. Their target client base is 16-29 year olds although they do service all<br />
groups. Further the team heard of an Indo <strong>Fiji</strong>an registered nurse, recently returned from 20<br />
years in the USA, who has opened a clinic in Nadi providing free specialist services to<br />
women in the area of breast self examination, sexual health and offering a pap smear service.<br />
It is understood that she provides the services herself with the support of other local nurses.<br />
Visits by doctors from the USA may soon enable her to extend the range of services<br />
ultimately provided. The team were not able to meet with this nurse but this is mentioned<br />
here as an indication that there is the possibility of an increasing number of NGOs providing<br />
services directly to the people of <strong>Fiji</strong> in the future. Other NGOs, especially in the area of<br />
HIV/AIDS, are providing different levels of “service” to patients.<br />
The MoH will need to give consideration to developing working “Partnership Agreements”<br />
with these NGO and engage them more directly in planning of health services. This will<br />
better ensure that these NGOs contribute directly to the goals of the health sector.<br />
The International Agencies<br />
Although they are rarely involved in the direct delivery of services, they do provide high<br />
level technical expertise and can play a very important role in the planning and monitoring of<br />
progress towards the achievement of goals As .examples any focused “action plan” to address<br />
such areas as maternal and infant mortality should involve WHO, UNICEF and UNFPA as<br />
partners of the Ministry.<br />
5.7.2. The need for the MoH to engage with these other providers and partners to achieve its<br />
KPIs.<br />
There would be benefit if the MoH, working with external support if needed, could (a)<br />
explore ways in which the work of these different parties can be captured in health service<br />
statistics and (b) explore ways to best optimise the clear benefits that these other parties can<br />
bring to the health sector as a whole.<br />
33
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
In relation to engagement with the private doctors and hospitals, some issues will need to be<br />
addressed so that the public will have full confidence in the work that they do. This is not a<br />
criticism of the work of the private sector, but rather ensuring the pubic of the quality of the<br />
care they are receiving. In particular, attention should be given to addressing the need for<br />
minimum clinical standards for private doctors and guidelines for appropriate fees and<br />
issuance of formal receipts. While it would be inappropriate for MoH to actually set fees, it<br />
may be appropriate to make regulations that doctors fees must be on display in their surgery<br />
where patients can easily see them. Regarding this issue of fee levels, any move to set<br />
guidelines for fees for private doctors would, for purposes of equity, need to be extended to<br />
cover fees for doctors from the government system who have rights of private practice- and<br />
who charge patients directly for services provided within government facilities.<br />
In these areas the MoH and the <strong>Fiji</strong> College of General Practitioners may wish to work with<br />
the Royal Australian College of General Practitioners.<br />
Recommendation 10.<br />
The MOH should take the lead in recognising that the “health sector” consists of other<br />
partners besides the MOH.<br />
Working with outside support if necessary, it should explore ways in which it can work with<br />
these other parties, including private medical practitioners, to put in place more functional<br />
operational partnerships that better define the role of the respective partners in supporting the<br />
MOH to achieve the overall goals of the sector.<br />
It should also seek to obtain meaningful information on the range and volume of health<br />
services performed by these other parties.<br />
5.8. The Need for an Evidence based approach to Policy and Planning.<br />
While <strong>Fiji</strong> collects considerable and important data, as stated above, little operational<br />
research is being done to answer key questions that should guide future policy and planning<br />
decisions. Examples of 6 areas where such research is needed is given in detail at Annex 15.<br />
In summary this includes<br />
• Efficiency of Hospital outpatient departments<br />
• Change in usage patterns of health facilities<br />
• Patterns of Antenatal Care<br />
• The growing problem of congenital syphilis<br />
• Role of the private sector in <strong>Fiji</strong><br />
• The adequacy and efficiency of mercy flights ambulance and patient transport<br />
services<br />
6. POSSIBLE AREAS FOR ASSISTANCE BY DEVELOPMENT<br />
PARTNERS.<br />
6.1. Overview<br />
As part of the assessment, the team was tasked to identify opportunities and gaps for future<br />
AusAID programming – including strategic objectives and likely areas of impact. This has<br />
been done and potential areas for external assistance are listed below. In general they are<br />
34
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
targeted to address the “ issues” identified in Part B, section 4 of this <strong>Situational</strong> <strong>Analysis</strong>,<br />
although some aspects of those issues may be addressed during the final year of FHSIP .<br />
Eight possible areas of support are listed. However it is not recommended that AusAID try to<br />
address more than 3 of these areas - 1 or 2 would be preferable. In a review of the progress<br />
being made by the FHSIP that was carried out concurrently with this <strong>Situational</strong> <strong>Analysis</strong>, it<br />
was concluded that despite a number of important achievements no truly visible impact can<br />
be seen as judged by measureable progress towards the achievement of the MOHs own KPIs.<br />
In large measure this reflects the fact that the program’s activities are spread very widely,<br />
with little focus on a core set of activities.<br />
Recommendation 11.<br />
It is recommended that initial priority for any AusAID support beyond 2009, should be given<br />
to assisting the MoH to achieve its own MDG 4 (infant and child mortality) and MDG 5<br />
(maternal mortality) targets.<br />
Such a recommendation is based on three observations:<br />
1. <strong>Fiji</strong> is significantly falling behind in its objective to achieve these important targets<br />
which are a key part of the MoHs own strategic plan and represent key commitments<br />
that the IGOF has given to its people. MoH would welcome assistance from AusAID<br />
and the donor community in general to achieve these.<br />
2. A co-ordinated and focused program to address these problems would serve as a good<br />
platform for other donors to join the program and for the MoH and these development<br />
partners to embrace the <strong>Pacific</strong> Principles of donor harmonisation (based on Paris<br />
Declaration).<br />
3. The impact of efforts to improve performance in these areas will be wide – and there<br />
will likely be improvements across many area of the health sector.<br />
Similarly the assessment team believes that the second priority should be to support the MoH<br />
to address a further 1 or 2 of its national Key Performance Indicators. These might include<br />
reduced amputation rates for diabetic sepsis from 13% to 9%, elimination of drug “stockouts<br />
“ or reduction in teenage pregnancy rates from 16% to 8%. Obviously the choice of<br />
which of the 12 KPIs listed in Annex 11 would be a matter for the Ministry. The extent of<br />
any further commitment beyond addressing MDG 4 and MDG 5 would be dependent on the<br />
level of support AusAID is prepared to commit.<br />
While no detailed design is given, an approach to achieving MDG 4 and 5 is discussed below.<br />
6.2. Highest Priority Areas for AusAID Support.<br />
6.2. 1. Provide targeted support to the MoH to reduce its level of infant and maternal<br />
mortality.<br />
This would require a strong focus on these two areas and would necessitate a recognition that<br />
such support will need to be provided across the sector including relevant secondary and<br />
tertiary areas. This issue of maternal and infant mortality has been discussed in some detail at<br />
section 4.5.<br />
While it is not the purpose of this “snapshot” to design any future program, some ideas are<br />
given here, because (a) it is felt that this area should be considered to be the highest priority<br />
for any new AusAID program and (b) if that principle is accepted some steps could<br />
commence within the framework of FHSIP, which still has one further year of operation and<br />
is currently finalising it workplan for 2009.<br />
35
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
In order to progress this concept in a planned way, such a program of support might have four<br />
phases – some of which could proceed concurrently and prior to the commencement of any<br />
new formal program of support that would begin in 2010.<br />
Phase 1: preliminary research to explore in more detail the issues affecting maternal and<br />
infant mortality, including the actual causes of each maternal and infant death; obtaining the<br />
type of information outlined in section 4.5. and 4.10.<br />
Phase 2: establishment of a sector wide management structure to guide the direction of the<br />
program and its ongoing monitoring and evaluation. This phase will also identify the<br />
“partners” who will work with the MoH as it seeks to address MDGs 4 and 5. These might<br />
include UNFPA, WHO, UNICEF, relevant NGOs and also a member of the private sector -<br />
recognising that there are over 120 private general practitioners who provide some level of<br />
maternal and infant care throughout <strong>Fiji</strong>.<br />
It would be an effective management strategy to include several project officers (seconded<br />
from MoH), of the type engaged within the FHSIP. They could play a day to day role in<br />
supporting individual key areas of the program and preparing reports for the management<br />
group etc.<br />
Phase 3: the MoH, working with its partners will prepare detailed “action plans” to address<br />
both maternal and infant mortality. While the outcomes to be achieved through such plans<br />
would be the attainment of the MDGs, it will be important that the plans include “stepping<br />
stones” that can be monitored on a monthly or quarterly basis. These “stepping stones” would<br />
need to be across many issues impacting maternal and infant mortality. including such areas<br />
as improved and more timely antenatal care; equipment needs for health centres and hospitals<br />
(neonatal units etc); improved transport (e.g. ambulances) within the framework of the<br />
referral system; addressing infection control within neonatal units; possibly the location and<br />
opening hours of health centres and nursing stations and reasons why people are by passing<br />
these centres to go to hospitals; steps needed to address the problem of neonatal syphilis.<br />
These action plans would need to be dynamic and be continually reviewed by the<br />
management group.<br />
Phase 4: ongoing implementation of the “action plans”. The program budget would need to<br />
be very flexible and not all committed upfront. This is because the success of such a program<br />
will be having available funds to respond to certain needs as they arise.<br />
It would also be important to have the PSC as an active partner in such a program as it may<br />
be necessary to respond to staffing issues in creative ways – and the PSC could give guidance<br />
on ways of doing this in a way that may constitute a “trial” without setting precedents or<br />
setting changes in concrete.<br />
It cannot be stressed enough that the success of such a program or activities will lie in the<br />
concept of focus and responsiveness – of addressing the problems in a timely manner<br />
and moving ever closer to the outcomes. It may prove to be a model for addressing the<br />
MDGs in other PICs.<br />
The Format for delivery of this assistance – a project, a model similar to that used in<br />
FHSIP or a model more similar to a focused SWAp would be a matter for AusAID to<br />
determine in conjunction with the MOH.<br />
6.2.2. Addressing other national Key Performance Indicators.<br />
A similar 4 phased approach could be used to provide support to a limited number of other<br />
national KPIs. The twelve national KPIs are given in Annex 11. As stated above, a program<br />
of support in this area might address KPIs such as reduced amputation rates for diabetic<br />
36
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
sepsis (from 13% to 9%), elimination of drug “stock-outs “ or reduction in teenage<br />
pregnancy rates (from 16% to 8%). Obviously the choice of which of the 12 KPIs listed in<br />
Annex 11 would be a matter for the Ministry. As stated above it is probable that a focus on a<br />
small number of areas would more likely have positive impact on the country’s health care<br />
system.<br />
In examples 6.2.1 and 6.2.2. the impact would be obvious – achievement of, or visible<br />
progress towards, attainment of the respective KPI<br />
6.3. Other Possible Areas for support by AusAID and other donors.<br />
6.3.1. Support to review the “framework” currently in place to ensure access to health<br />
services.<br />
The reason for such a review is discussed at section 5.2. and recommendation 4 of the report.<br />
It should take account of changes over the last 30 years and should ask the question “what do<br />
we want the health sector to look like in 2020” and begin planning for it now.<br />
It should have as its outcome a more efficient service model that better meets the needs of the<br />
people and the staff for the next 20 years.<br />
6.3.2. Support a culture of evidence based policy.<br />
This would be done by providing support for key operational research projects aimed at<br />
making the sector more efficient and effective. A strong interface between FSMed and the<br />
MoH is essential to ensure that donor supported research is targeted at key areas of need.<br />
Some areas that warrant research have been listed at 4.10.<br />
Such a program of support would provide a pool of information that can guide the<br />
development of meaningful policy – that experience from other countries has shown that<br />
policies supported by carefully researched evidence, are likely to be both more effective and<br />
less wasteful of resources.<br />
6.3.3.. Support a program of continued capacity development in key areas.<br />
Throughout this report the need to build capacity in selected areas has been highlighted. This<br />
will lead to a more skilled workforce. This would include management and supervision;<br />
planning, monitoring and evaluation; and the development of skills needed to prepare strong<br />
proposals in support of needs of the Ministry.<br />
The Project Officer and Performance Enhancing Projects “models” introduced through the<br />
FHSIP should be continued. Any support for program 6.1. above (MDG 4 and 5) would<br />
include a very large element of capacity development, including support for the Project<br />
Office and Performance Enhancing Projects model, and would largely negate the need for<br />
this to be a separate program.<br />
6.3.4. Upgrade of PATIS and other <strong>Health</strong> Information Systems (including training).<br />
Considerable work has already been done to support the development and roll out of health<br />
information systems in <strong>Fiji</strong>. This includes PATIS. More is planned by FHSIP during 2009.<br />
While it is recognised that good information systems are important tools to be used by the<br />
MoH, it is recommended that further AusAID support beyond the end of FHSIP should not<br />
be continued until the MoH, MoF&NP and PSC give some indication as to whether the IGOF<br />
will provide the necessary ongoing financial and specialist staffing support to enable this to<br />
be sustainable.<br />
37
<strong>Situational</strong> <strong>Analysis</strong> of the <strong>Fiji</strong> <strong>Health</strong> <strong>Sector</strong> December <strong>2008</strong><br />
6.3.5. Continued support for NGOs.<br />
NGOs play an increasingly important role in the health sector and should be supported. This<br />
especially applies to those NGOs that are providing services directly to the community. PC<br />
and SS and Marie Stopes International are such organisations but there are others. NGOs<br />
need to scale up and widen their activities and continued donor support will enable them to<br />
do this and to play a more positive role, and have a greater impact as “partners” of the MoH.<br />
PC & SS serves as a model for such a “scale up”. As discussed earlier, it started as a small<br />
NGO providing services to HIV/AIDS patients, but with increasing demand, it worked with<br />
The Australian Institute of Professional Counsellors to train more counsellors to meet a<br />
widening need. In time it began to train its own diploma level counsellors to Australian<br />
Standards and expanded its services from the initial 1 centre to the current position where it<br />
has counselling services in Lautoka, Nadi, Suva and Labasa. It now has an MOU with the<br />
MoH and provides routine counselling services in some hospitals as well as to the<br />
community, prisons and court work. AusAID has supported PC and SS throughout this<br />
scaling up.<br />
The format for continued support to health based NGOs (eg would it come from the health<br />
sector budget or from other NGO funding sources) would be a matter for AusAID<br />
6.3.6. Continued support for Regional Programs especially in the area of disease control.<br />
The above suggestions do not propose any new program in the area of Disease Control. This<br />
is because disease control activities are currently being well supported within <strong>Fiji</strong> by a range<br />
of Regional Programs including programs targeted at NCDs; HIV/AIDs; filariasis eradication<br />
and Emerging Infectious Diseases. In addition bodies such as UNAIDS, the Global Fund, and<br />
WHO are providing valuable support in key disease control areas.<br />
What is proposed here is that those regional disease control activities being supported by<br />
AusAID, and especially support for NCDs and diabetes prevention and control, should be<br />
continued and even strengthened. There would be benefit if there was also continued input to<br />
these areas from other donors.<br />
Such programs in many ways relate to “<strong>Pacific</strong> lifestyle”, and have elements that not only<br />
impact on <strong>Fiji</strong> but on other countries in the region. They are well suited to a regional rather<br />
than a bilateral approach. However it is suggested that, as AusAID further develops its<br />
regional strategy, it ensures that activities within its regional programs are clearly consistent<br />
with an individual country’s national plans and priorities. There would be benefit in having<br />
regional MoHs “sign off” on those elements of the Program that relate to their own country to<br />
ensure better ownership and understanding of what is available to them through regional<br />
programs. The review team found there was often poor understanding at senior levels of what<br />
the development partners were doing through their regional programs and how they can<br />
become part of their own national plans.<br />
38