Antiphospholipid Syndrome - Pathology
Antiphospholipid Syndrome - Pathology
Antiphospholipid Syndrome - Pathology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
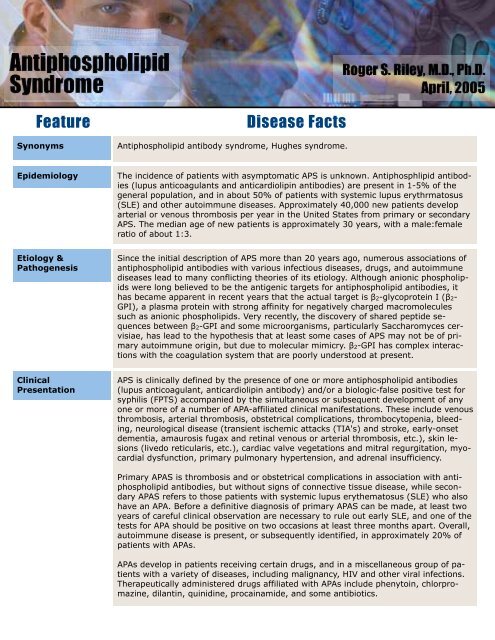
<strong>Antiphospholipid</strong> <strong>Syndrome</strong> 1<br />
<strong>Antiphospholipid</strong><br />
<strong>Syndrome</strong><br />
Feature<br />
Disease Facts<br />
Roger S. Riley, M.D., Ph.D.<br />
April, 2005<br />
Synonyms<br />
<strong>Antiphospholipid</strong> antibody syndrome, Hughes syndrome.<br />
Epidemiology<br />
The incidence of patients with asymptomatic APS is unknown. Antiphosphlipid antibodies<br />
(lupus anticoagulants and anticardiolipin antibodies) are present in 1-5% of the<br />
general population, and in about 50% of patients with systemic lupus erythrmatosus<br />
(SLE) and other autoimmune diseases. Approximately 40,000 new patients develop<br />
arterial or venous thrombosis per year in the United States from primary or secondary<br />
APS. The median age of new patients is approximately 30 years, with a male:female<br />
ratio of about 1:3.<br />
Etiology &<br />
Pathogenesis<br />
Since the initial description of APS more than 20 years ago, numerous associations of<br />
antiphospholipid antibodies with various infectious diseases, drugs, and autoimmune<br />
diseases lead to many conflicting theories of its etiology. Although anionic phospholipids<br />
were long believed to be the antigenic targets for antiphospholipid antibodies, it<br />
has became apparent in recent years that the actual target is 2-glycoprotein I (2-<br />
GPI), a plasma protein with strong affinity for negatively charged macromolecules<br />
such as anionic phospholipids. Very recently, the discovery of shared peptide sequences<br />
between 2-GPI and some microorganisms, particularly Saccharomyces cervisiae,<br />
has lead to the hypothesis that at least some cases of APS may not be of primary<br />
autoimmune origin, but due to molecular mimicry. 2-GPI has complex interactions<br />
with the coagulation system that are poorly understood at present.<br />
Clinical<br />
Presentation<br />
APS is clinically defined by the presence of one or more antiphospholipid antibodies<br />
(lupus anticoagulant, anticardiolipin antibody) and/or a biologic-false positive test for<br />
syphilis (FPTS) accompanied by the simultaneous or subsequent development of any<br />
one or more of a number of APA-affiliated clinical manifestations. These include venous<br />
thrombosis, arterial thrombosis, obstetrical complications, thrombocytopenia, bleeding,<br />
neurological disease (transient ischemic attacks (TIA's) and stroke, early-onset<br />
dementia, amaurosis fugax and retinal venous or arterial thrombosis, etc.), skin lesions<br />
(livedo reticularis, etc.), cardiac valve vegetations and mitral regurgitation, myocardial<br />
dysfunction, primary pulmonary hypertension, and adrenal insufficiency.<br />
Primary APAS is thrombosis and or obstetrical complications in association with antiphospholipid<br />
antibodies, but without signs of connective tissue disease, while secondary<br />
APAS refers to those patients with systemic lupus erythematosus (SLE) who also<br />
have an APA. Before a definitive diagnosis of primary APAS can be made, at least two<br />
years of careful clinical observation are necessary to rule out early SLE, and one of the<br />
tests for APA should be positive on two occasions at least three months apart. Overall,<br />
autoimmune disease is present, or subsequently identified, in approximately 20% of<br />
patients with APAs.<br />
APAs develop in patients receiving certain drugs, and in a miscellaneous group of patients<br />
with a variety of diseases, including malignancy, HIV and other viral infections.<br />
Therapeutically administered drugs affiliated with APAs include phenytoin, chlorpromazine,<br />
dilantin, quinidine, procainamide, and some antibiotics.
<strong>Antiphospholipid</strong> <strong>Syndrome</strong> 2<br />
Feature<br />
Disease Facts<br />
Clinical<br />
Presentation<br />
(Cont’d)<br />
Rare APA patients present with acute multi-organ involvement, including signs and<br />
symptoms of encephalopathy, seizures, livedo reticularis, renal insufficiency, pulmonary<br />
failure, and multiple thrombi involving both large and small vessel occlusions.<br />
The term “catastrophic APA syndrome” and “Asherson syndrome” has been applied to<br />
this disease, which is associated with high-titered APAs and a high mortality rate.<br />
Laboratory<br />
Features<br />
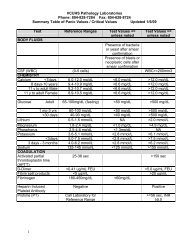
The laboratory diagnosis of a LA is based on the initial finding of an abnormal<br />
phospholipid-dependent clotting assay, followed by confirmation that a clotting inhibitor<br />
is present, and that the inhibitor is dependent on phospholipid. Unfortunately, the<br />
heterogeneous nature of LAs limits the sensitivity and specificity of individual coagulation<br />
assays for LA detection and analysis; multiple assays are usually required and<br />
there is no standard method of approach. However, the initial laboratory evaluation<br />
will usually show a prolonged activated partial thromboplastin time (aPTT) with a normal<br />
to slightly prolonged prothrombin time (PT). An aPTT mixing study is necessary to<br />
identify the cause of the elevated aPTT and establish the presence of an inhibitor.<br />
The Russell Viper Venom Time (RVVT) is the most widely used clinical laboratory assay<br />
for confirmation of the presence of a phospholipid-dependent antibody. Russell’s viper<br />
(Vipera russellii) is a large venomous snake native to India and Southeast Asia. Russell’s<br />
viper venom (RVV) causes massive thrombosis when injected in vivo. The coagulant<br />
protein of RVV is an enzyme (serine protease) which directly activates factor X in<br />
the presence of Ca ++ , bypassing the intrinsic and extrinsic pathways. The activated<br />
factor X then activates prothrombin in the presence of factor V and phospholipid.<br />
The dilute Russell Viper Venom Time (dRVVT) uses a “diluted” venom concentration<br />
and minimal phospholipid concentration to give a clotting time of 23 to 27 seconds<br />
with normal serum. Under these circumstances, the clotting time becomes very sensitive<br />
to the presence of phospholipid. LAs bind the available phospholipid, block the activation<br />
of factor II, and lead to a prolongation of the clotting time. The dRVVT is more<br />
specific for LA than the aPTT since it is not influenced by deficiencies of the contact or<br />
intrinsic pathway factors or antibodies to factors VIII, IX, or XI. The dRVVT can be<br />
used to detect LA in patient samples with a normal aPTT since phospholipid dilution<br />
increases the sensitivity of the assay. A commercially available dRVVT test reagent,<br />
(DVVtest, American Diagnostica, Inc., Greenwich, CT) combines RVV, plant phospholipid,<br />
and calcium into a single reagent. A second reagent, containing RVV, extra<br />
plant phospholipid, and calcium is usually available to “confirm” a positive result. The<br />
extra phospholipid in the confirm reagent corrects a prolonged dRVVT time in a manner<br />
analogous to platelet addition in the aPTT-based platelet neutralization procedure.<br />
Other confirmatory assays for phospholipids-dependent antibodies include the hexagonal<br />
phospholipid assay , PNP, tissue thromboplastin inhibition (TTI) assay, textarin<br />
tine, kaolin clotting time (KCT). Because of individual variability in laboratory results, a<br />
positive findings in at least two assays is recommended for diagnostic confirmation.<br />
Anti-cardiolipin antibodies are detected by ELISA assays utilizing microliter plates<br />
coated with dried cardiolipin. Bovine albumin or fetal calf serum is added to block nonspecific<br />
binding sites, serum specimens are incubated in the microtiter wells, followed<br />
by washing to remove serum and unbound immunoglobulin, and incubation with<br />
monospecific or polyvalent enzyme-labeled anti-human immunoglobulin. Affinitypurified,<br />
isotype specific ACAs and a series of international workshops in the 1980’s<br />
resulted in standardized methodology and the definition of standard units of anticardiolipin<br />
activity (GPL and MPL). One GPL or MPL unit is equivalent to one mg/mL of an<br />
affinity-purified standard IgG or IgM sample obtained from specified individuals. Later<br />
assays utilized negatively-charged phospholipids instead of cardiolipin.
<strong>Antiphospholipid</strong> <strong>Syndrome</strong> 3<br />
Feature<br />
Treatment<br />
Disease Facts<br />
The treatment of APS is based on the severity of clinical manifestations, particularly<br />
thrombosis, and whether the patient has the primary or secondary form of the disease.<br />
Aspirin is the cornerstone of treatment in patients without a history of thrombosis,<br />
with hydroxychloroquine added in patients with SLE. Patients with a single episode<br />
of thrombosis are at a high risk of recurrent thrombotic disease, and require lifelong<br />
anticoagulation, currently with warfarin. Pregnant women with APS are usually treated<br />
with heparin or low molecular weight heparin to prevent pregnancy loss. Other forms<br />
of treatment may include corticosteroids or intravenous immunoglobulin.<br />
Treatment<br />
Akkawat B, Chantarangkul V, Rojnuckarin<br />
P, et al: Laboratory identification<br />
of lupus anticoagulants<br />
using the combination of activated<br />
partial thromboplastin time and<br />
Russell's viper venom at two<br />
phospholipid concentrations. J<br />
Med Assoc Thai 86 Suppl 2:S451,<br />
2003<br />
Alarcon-Segovia D: The antiphospholipid<br />
story. J Rheumatol<br />
30:1893, 2003<br />
Amengual O, Atsumi T, Koike T:<br />
Antiprothombin antibodies and the<br />
diagnosis of antiphospholipid syndrome.<br />
Clin Immunol 112:144,<br />
2004<br />
Arnout J, Jankowski M: <strong>Antiphospholipid</strong><br />
syndrome. Hematol J 5<br />
Suppl 3:S1, 2004<br />
Behbehani R, Sergott RC, Savino<br />
PJ: The antiphospholipid antibody<br />
syndrome: diagnostic aspects.<br />
Curr Opin Ophthalmol 15:483,<br />
2004<br />
Bick RL: <strong>Antiphospholipid</strong> thrombosis<br />
syndromes. Hematol Oncol<br />
Clin North Am 17:115, 2003<br />
Blank M, Shoenfeld Y: Beta-2-<br />
glycoprotein-I, infections, antiphospholipid<br />
syndrome and therapeutic<br />
considerations. Clin Immunol<br />
112:190, 2004<br />
Branch DW, Khamashta MA: <strong>Antiphospholipid</strong><br />
syndrome: obstetric<br />
diagnosis, management, and controversies.<br />
Obstet Gynecol<br />
101:1333, 2003<br />
Carbillon L, Letamendia-Richard<br />
E, Lachassinne E, et al: Neonatal<br />
thrombosis associated with maternal<br />
antiphospholipid syndrome. J<br />
Pediatr Hematol Oncol 27:56,<br />
2005<br />
Cervera R, Asherson RA, Acevedo<br />
ML, et al: <strong>Antiphospholipid</strong> syndrome<br />
associated with infections:<br />
clinical and microbiological characteristics<br />
of 100 patients. Ann<br />
Rheum Dis 63:1312, 2004<br />
Chang S: More on: normal plasma<br />
mixing studies in the laboratory<br />
diagnosis of lupus anticoagulant. J<br />
Thromb Haemost 2:1480-1481,<br />
2004<br />
Chantarangkul V, Tripodi A, Clerici<br />
M, et al: Laboratory diagnosis of<br />
lupus anticoagulants--effect of<br />
residual platelets in plasma, assessed<br />
by Staclot LA and silica<br />
clotting time. Thromb Haemost<br />
87:854-858, 2002<br />
Crowther MA: <strong>Antiphospholipid</strong><br />
antibody syndrome: further evidence<br />
to guide clinical practice? J<br />
Rheumatol 31:1474, 2004<br />
de Groot PG, Derksen RH: <strong>Antiphospholipid</strong><br />
antibodies: update<br />
on detection, pathophysiology, and<br />
treatment. Curr Opin Hematol<br />
11:165, 2004<br />
de Groot PG, Derksen RH: Pathophysiology<br />
of antiphospholipid<br />
antibodies. Neth J Med 62:267,<br />
2004<br />
de Moerloose P, Reber G: <strong>Antiphospholipid</strong><br />
antibodies: do we still<br />
need to perform anticardiolipin<br />
ELISA assays? J Thromb Haemost<br />
2:1071, 2004<br />
Derksen RH, de Groot PG: Clinical<br />
consequences of antiphospholipid<br />
antibodies. Neth J Med 62:273,<br />
2004<br />
Durrani OM, Gordon C, Murray PI:<br />
Primary anti-phospholipid antibody<br />
syndrome (APS): current concepts.<br />
Surv Ophthalmol 47:215,<br />
2002<br />
Erkan D, Lockshin MD: What is<br />
antiphospholipid syndrome? Curr<br />
Rheumatol Rep 6:451, 2004<br />
Espinosa G, Cervera R, Font J, et<br />
al: <strong>Antiphospholipid</strong> syndrome:<br />
pathogenic mechanisms. Autoimmun<br />
Rev 2:86, 2003<br />
Galli M: <strong>Antiphospholipid</strong> syndrome:<br />
association between laboratory<br />
tests and clinical practice.<br />
Pathophysiol Haemost Thromb<br />
33:249-255, 2003<br />
Galli M, Barbui T: <strong>Antiphospholipid</strong><br />
syndrome: definition and treatment.<br />
Semin Thromb Hemost<br />
29:195, 2003<br />
Gharavi AE, Wilson W, Pierangeli<br />
S: The molecular basis of antiphospholipid<br />
syndrome. Lupus<br />
12:579, 2003<br />
Grossman JM: Primary versus<br />
secondary antiphospholipid syndrome:<br />
is this lupus or not? Curr<br />
Rheumatol Rep 6:445, 2004<br />
Grover R, Kumar A: The antiphospholipid<br />
syndrome. Natl Med J<br />
India 16:311, 2003<br />
Hanly JG: <strong>Antiphospholipid</strong> syndrome:<br />
an overview. Cmaj<br />
168:1675, 2003<br />
Harris EN, Khamashta M: Anticardiolipin<br />
test and the antiphospholipid<br />
(Hughes) syndrome: 20<br />
years and counting! J Rheumatol<br />
31:2099, 2004<br />
Harris EN, Peirangeli SS, Gharavi<br />
AE: <strong>Antiphospholipid</strong> syndrome:<br />
diagnosis, pathogenesis, and<br />
management. J Med Assoc Ga<br />
91:31, 2002
<strong>Antiphospholipid</strong> <strong>Syndrome</strong> 4<br />
References<br />
(Cont’d)<br />
Harris EN, Pierangeli SS: Revisiting<br />
the anticardiolipin test and its<br />
standardization. Lupus 11:269,<br />
2002<br />
Khamashta MA, Bertolaccini ML,<br />
Hughes GR: <strong>Antiphospholipid</strong><br />
(Hughes) syndrome. Autoimmunity<br />
37:309, 2004<br />
Krillis SA: Pathogenic aspects of<br />
antiphospholipid antibodies. Autoimmun<br />
Rev 3 Suppl 1:S40, 2004<br />
Li Z, Krilis SA: Anti-beta(2)-<br />
glycoprotein I antibodies and the<br />
antiphospholipid syndrome. Autoimmun<br />
Rev 2:229, 2003<br />
Lockshin MD, Erkan D: Treatment<br />
of the antiphospholipid syndrome.<br />
N Engl J Med 349:1177, 2003<br />
Mackworth-Young CG: <strong>Antiphospholipid</strong><br />
syndrome: multiple<br />
mechanisms. Clin Exp Immunol<br />
136:393, 2004<br />
Manson JJ, Isenberg DA: <strong>Antiphospholipid</strong><br />
syndrome. Int J Biochem<br />
Cell Biol 35:1015, 2003<br />
McIntyre JA, Wagenknecht DR,<br />
Faulk WP: <strong>Antiphospholipid</strong> antibodies:<br />
discovery, definitions, detection<br />
and disease. Prog Lipid<br />
Res 42:176, 2003<br />
Meroni PL, di Simone N, Testoni C,<br />
et al: <strong>Antiphospholipid</strong> antibodies<br />
as cause of pregnancy loss. Lupus<br />
13:649, 2004<br />
Meroni PL, Tincani A: Should our<br />
approach to the anticardiolipin<br />
assay change 20 years after its<br />
discovery? J Thromb Haemost<br />
2:1074, 2004<br />
Merrill JT: Diagnosis of the antiphospholipid<br />
syndrome: how far to<br />
go? Curr Rheumatol Rep 6:469,<br />
2004<br />
Nash MJ, Camilleri RS, Kunka S,<br />
et al: The anticardiolipin assay is<br />
required for sensitive screening for<br />
antiphospholipid antibodies. J<br />
Thromb Haemost 2:1077, 2004<br />
Obermoser G, Bitterlich W, Kunz F,<br />
et al: Clinical significance of anticardiolipin<br />
and anti-beta2-<br />
glycoprotein I antibodies. Int Arch<br />
Allergy Immunol 135:148, 2004<br />
Park KW: The antiphospholipid<br />
syndrome. Int Anesthesiol Clin<br />
42:45, 2004<br />
Passam F, Krilis S: Laboratory<br />
tests for the antiphospholipid syndrome:<br />
current concepts. <strong>Pathology</strong><br />
36:129, 2004<br />
Pechlaner C, Wiedermann CJ:<br />
<strong>Antiphospholipid</strong> testing and outcome.<br />
Arch Intern Med 164:1701;<br />
author reply 1701, 2004<br />
Rand JH: The antiphospholipid<br />
syndrome. Annu Rev Med 54:409,<br />
2003<br />
Rand JH: Molecular pathogenesis<br />
of the antiphospholipid syndrome.<br />
Circ Res 90:29, 2002<br />
Roubey RA: <strong>Antiphospholipid</strong> antibodies:<br />
immunological aspects.<br />
Clin Immunol 112:127, 2004<br />
Sebire NJ, Backos M, El Gaddal S,<br />
et al: Placental pathology, antiphospholipid<br />
antibodies, and pregnancy<br />
outcome in recurrent miscarriage<br />
patients. Obstet Gynecol<br />
101:258, 2003<br />
Sheehan TL: A guide to Hughes'<br />
syndrome. Nurs Times 99:24,<br />
2003<br />
Shoenfeld Y: Anti-phospholipid<br />
syndrome from a systemic disease<br />
toward the infectious etiology. Rev<br />
Med Interne 25 Suppl 1:S10, 2004<br />
Shoenfeld Y: Etiology and pathogenetic<br />
mechanisms of the antiphospholipid<br />
syndrome unraveled.<br />
Trends Immunol 24:2, 2003<br />
Shoenfeld Y, Blank M: The infectious<br />
etiology of the antiphospholipid<br />
syndrome (APS). Autoimmun<br />
Rev 3 Suppl 1:S32, 2004<br />
Sibilia J: <strong>Antiphospholipid</strong> syndrome:<br />
why and how should we<br />
make the diagnosis? Joint Bone<br />
Spine 70:97, 2003<br />
Smikle M, Wharfe G, Fletcher H, et<br />
al: Anticardiolipin, other antiphospholipid<br />
antibody tests and diagnosis<br />
of the antiphospholipid syndrome.<br />
Hum Antibodies 12:63,<br />
2003<br />
Triplett DA: Lupus anticoagulants:<br />
diagnosis and management. Curr<br />
Hematol Rep 2:271-272, 2003<br />
Tripodi A, Chantarangkul V, Clerici<br />
M, et al: Laboratory diagnosis of<br />
lupus anticoagulants for patients<br />
on oral anticoagulant treatment.<br />
Performance of dilute Russell viper<br />
venom test and silica clotting time<br />
in comparison with Staclot LA.<br />
Thromb Haemost 88:583, 2002<br />
Tripodi A, Biasiolo A, Chantarangkul<br />
V, et al: Lupus anticoagulant<br />
(LA) testing: performance of clinical<br />
laboratories assessed by a<br />
national survey using lyophilized<br />
affinity-purified immunoglobulin<br />
with LA activity. Clin Chem<br />
49:1608-1614, 2003<br />
Wisloff F, Jacobsen EM, Liestol S:<br />
Laboratory diagnosis of the antiphospholipid<br />
syndrome. Thromb<br />
Res 108:263, 2002<br />
Wu C, Kalunian K: Treatment of<br />
the antiphospholipid antibody syndrome.<br />
Curr Rheumatol Rep<br />
6:463, 2004