Draft Project Charter Reduce Preventable Readmissions through ...
Draft Project Charter Reduce Preventable Readmissions through ...
Draft Project Charter Reduce Preventable Readmissions through ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
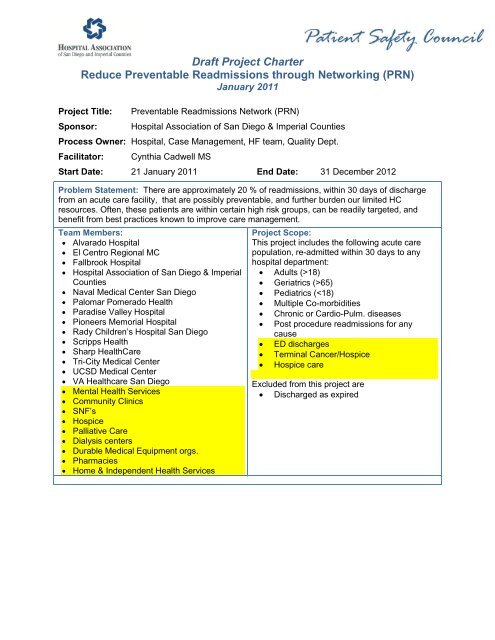
<strong>Draft</strong> <strong>Project</strong> <strong>Charter</strong><br />
<strong>Reduce</strong> <strong>Preventable</strong> <strong>Readmissions</strong> <strong>through</strong> Networking (PRN)<br />
January 2011<br />
<strong>Project</strong> Title:<br />
Sponsor:<br />
<strong>Preventable</strong> <strong>Readmissions</strong> Network (PRN)<br />
Hospital Association of San Diego & Imperial Counties<br />
Process Owner: Hospital, Case Management, HF team, Quality Dept.<br />
Facilitator:<br />
Cynthia Cadwell MS<br />
Start Date: 21 January 2011 End Date: 31 December 2012<br />
Problem Statement: There are approximately 20 % of readmissions, within 30 days of discharge<br />
from an acute care facility, that are possibly preventable, and further burden our limited HC<br />
resources. Often, these patients are within certain high risk groups, can be readily targeted, and<br />
benefit from best practices known to improve care management.<br />
Team Members:<br />
• Alvarado Hospital<br />
• El Centro Regional MC<br />
• Fallbrook Hospital<br />
• Hospital Association of San Diego & Imperial<br />
Counties<br />
• Naval Medical Center San Diego<br />
• Palomar Pomerado Health<br />
• Paradise Valley Hospital<br />
• Pioneers Memorial Hospital<br />
• Rady Children’s Hospital San Diego<br />
• Scripps Health<br />
• Sharp HealthCare<br />
• Tri-City Medical Center<br />
• UCSD Medical Center<br />
• VA Healthcare San Diego<br />
• Mental Health Services<br />
• Community Clinics<br />
• SNF’s<br />
• Hospice<br />
• Palliative Care<br />
• Dialysis centers<br />
• Durable Medical Equipment orgs.<br />
• Pharmacies<br />
• Home & Independent Health Services<br />
<strong>Project</strong> Scope:<br />
This project includes the following acute care<br />
population, re-admitted within 30 days to any<br />
hospital department:<br />
• Adults (>18)<br />
• Geriatrics (>65)<br />
• Pediatrics (
<strong>Draft</strong> <strong>Project</strong> <strong>Charter</strong><br />
<strong>Reduce</strong> <strong>Preventable</strong> <strong>Readmissions</strong> <strong>through</strong> Networking (PRN)<br />
January 2011<br />
Deliverables:<br />
• Best practices and guidelines of care<br />
• Surveillance tool(s) – to evaluate for both<br />
effective methods and readmissions tracking<br />
• Order sets; Checklists<br />
• Strategy Implementation plans<br />
• Education on processes/methods<br />
• Definitions – based on best practice<br />
• Data gathering assistance<br />
• Elevator speech<br />
• Outcomes and tools to measure outcomes<br />
Goal and Other Potential Benefits:<br />
To collaborate, utilize HIE portals as available,<br />
and apply evidenced-based project tools and<br />
organization-specific methods to reduce percent<br />
of All Cause 30 day <strong>Readmissions</strong> by at least<br />
25% by 12/31/2012, with a stretch goal of 30%<br />
by 3/31/2013 in the San Diego and Imperial<br />
County region. Optional outcomes may include<br />
percent of a significant selected population (e.g.<br />
HF, Diabetes, Depression). Furthermore,<br />
focused preventative measures with the high risk<br />
patient being discharged from the hospital will<br />
reduce healthcare costs associated with<br />
preventable readmissions and complications,<br />
and increase patient satisfaction with their care.<br />
Customer(s) and Requirements:<br />
Health care professionals and care coordinators need various tools they can adjust to their<br />
populations, to consistently execute on methods to support care transition improvement, and<br />
change acceleration strategies for rapid adoption of best practices.
Population<br />
Preventing readmission in high risk patients is possible using certain established targeting and discharge<br />
plan/transition of care modalities. Sharing implementation methods to achieve best practices among multiple<br />
providers and healthcare systems has been shown to expedite improvement. These methods can improve<br />
patient satisfaction, care quality and resource utilization.<br />
Coding based on ICD-9 and discharge DRG diagnosis 30 day readmissions and/or CMS data<br />
• May be able to track certain inter-facility readmits <strong>through</strong> SD Beacon HIE project<br />
• Providers may not be aware of ‘non PCP patient’ readmissions<br />
• Patient admitted into hospital without any accessible records<br />
• N = all patients with ‘unplanned’ readmissions within 30 days<br />
• D = all discharges<br />
Goal<br />
• <strong>Reduce</strong> the incidence of preventable readmissions into licensed care facilities across the region<br />
• Need current number – administrative data – for baseline<br />
• Each organization: 30 day ‘unplanned’ readmission rates for 2009 and 2010 as baseline; Can sort to<br />
specific DRG’s if necessary to better target high risk and high volume patients<br />
• Side goal: <strong>Reduce</strong> unnecessary resource utilization and increase bed and revenue capacity<br />
How can this project help us at our facility?<br />
• Implementation tools, ideas and methods sharing can accelerate change and impact; Improve bed and<br />
revenue capacity; Improve patient satisfaction with care<br />
Elevator Speech<br />
Recommend producing an elevator speech for each target audience.<br />
• What our project is about… improving our care ‘transition’ coordination, especially upon hospital<br />
discharge, to prevent unnecessary readmissions in our region, as well as improve patient care outcomes.<br />
• Why it is important to do… because many 30 day readmissions are preventable with appropriate<br />
intervention, yet today it occurs in approximately 20% of all cases in our region, and we are frequently over<br />
capacity at most facilities, causing patients to have care delayed.<br />
• What success will look like… increased regional capacity for planned, revenue producing and emergency<br />
hospital admissions, improved quality of care for our high risk populations, and improved resource<br />
utilization. Improved patient satisfaction scores.<br />
• What we need from you… a commitment to understand, support, and comply with best practices to<br />
prevent unnecessary readmissions, including early identification of high-risk patients, collaborating with<br />
multi-disciplinary colleagues, and providing accurate information on patient readmission rates from your<br />
facility on a quarterly basis to the region, and a monthly basis to your onsite team.<br />
Staging <strong>Project</strong><br />
Considering evidence available it’s clear what needs to be done… We need:<br />
Timeline<br />
Description<br />
March 2011 • <strong>Readmissions</strong> baseline data 2009; 2010; Quarterly progress reports<br />
• Readmission prevention campaigns<br />
• Hospital discharge order sets available in most facilities<br />
• Literature supported targets and methods<br />
May 2011 • Currently available prevention and surveillance methods, tools and resources<br />
• Facility team’s assembly and management support tools<br />
July 2011 • Change management/Implementation tools<br />
• SD Beacon’s Contribution/Alignment<br />
Sept. 2011 • 2011 <strong>Readmissions</strong> Measurement and Analysis<br />
• Stakeholder analysis<br />
Nov. 2011 • <strong>Project</strong> status evaluation<br />
• Review change management<br />
• Readjust plan, goals, etc. as needed<br />
Jan 2012 • <strong>Project</strong> plan for 2012 defined and 2011 progress report disseminated