Sepsis Mortality Reduction Project Charter - Patientsafetycouncil.org
Sepsis Mortality Reduction Project Charter - Patientsafetycouncil.org
Sepsis Mortality Reduction Project Charter - Patientsafetycouncil.org
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
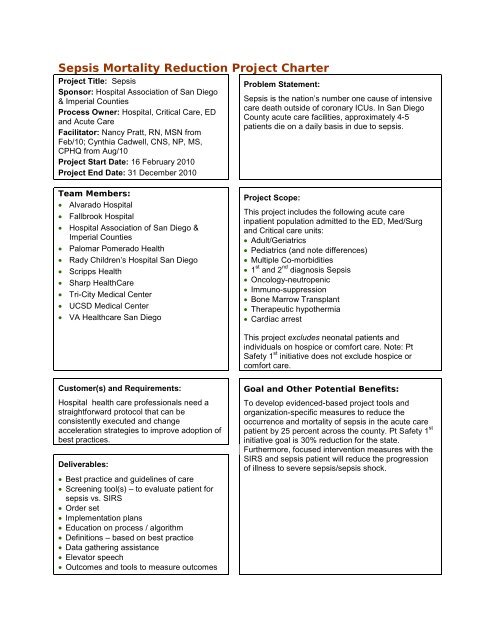
<strong>Sepsis</strong> <strong>Mortality</strong> <strong>Reduction</strong> <strong>Project</strong> <strong>Charter</strong><br />
<strong>Project</strong> Title: <strong>Sepsis</strong><br />
Sponsor: Hospital Association of San Diego<br />
& Imperial Counties<br />
Process Owner: Hospital, Critical Care, ED<br />
and Acute Care<br />
Facilitator: Nancy Pratt, RN, MSN from<br />
Feb/10; Cynthia Cadwell, CNS, NP, MS,<br />
CPHQ from Aug/10<br />
<strong>Project</strong> Start Date: 16 February 2010<br />
<strong>Project</strong> End Date: 31 December 2010<br />
Problem Statement:<br />
<strong>Sepsis</strong> is the nation’s number one cause of intensive<br />
care death outside of coronary ICUs. In San Diego<br />
County acute care facilities, approximately 4-5<br />
patients die on a daily basis in due to sepsis.<br />
Team Members:<br />
• Alvarado Hospital<br />
• Fallbrook Hospital<br />
• Hospital Association of San Diego &<br />
Imperial Counties<br />
• Palomar Pomerado Health<br />
• Rady Children’s Hospital San Diego<br />
• Scripps Health<br />
• Sharp HealthCare<br />
• Tri-City Medical Center<br />
• UCSD Medical Center<br />
• VA Healthcare San Diego<br />
<strong>Project</strong> Scope:<br />
This project includes the following acute care<br />
inpatient population admitted to the ED, Med/Surg<br />
and Critical care units:<br />
• Adult/Geriatrics<br />
• Pediatrics (and note differences)<br />
• Multiple Co-morbidities<br />
• 1 st and 2 nd diagnosis <strong>Sepsis</strong><br />
• Oncology-neutropenic<br />
• Immuno-suppression<br />
• Bone Marrow Transplant<br />
• Therapeutic hypothermia<br />
• Cardiac arrest<br />
This project excludes neonatal patients and<br />
individuals on hospice or comfort care. Note: Pt<br />
Safety 1 st initiative does not exclude hospice or<br />
comfort care.<br />
Customer(s) and Requirements:<br />
Hospital health care professionals need a<br />
straightforward protocol that can be<br />
consistently executed and change<br />
acceleration strategies to improve adoption of<br />
best practices.<br />
Deliverables:<br />
• Best practice and guidelines of care<br />
• Screening tool(s) – to evaluate patient for<br />
sepsis vs. SIRS<br />
• Order set<br />
• Implementation plans<br />
• Education on process / algorithm<br />
• Definitions – based on best practice<br />
• Data gathering assistance<br />
• Elevator speech<br />
• Outcomes and tools to measure outcomes<br />
Goal and Other Potential Benefits:<br />
To develop evidenced-based project tools and<br />
<strong>org</strong>anization-specific measures to reduce the<br />
occurrence and mortality of sepsis in the acute care<br />
patient by 25 percent across the county. Pt Safety 1 st<br />
initiative goal is 30% reduction for the state.<br />
Furthermore, focused intervention measures with the<br />
SIRS and sepsis patient will reduce the progression<br />
of illness to severe sepsis/sepsis shock.
Population<br />
• Treating SIRS can reduce patient progressing to <strong>Sepsis</strong> Shock<br />
• Coding based on MD diagnosis <strong>Sepsis</strong> (get codes for sepsis)<br />
• Most MDs state sepsis typically as severe sepsis<br />
• Providers not aware of documenting SIRS or <strong>Sepsis</strong><br />
• Patient admitted into ICU with <strong>Sepsis</strong><br />
• Y = all patients in the hospital with sepsis<br />
Any diagnosis - primary or secondary, etc.<br />
• X = mortality<br />
Goal<br />
• Reduce the incidence and mortality of sepsis in the acute care patient by 25% across the county; during<br />
the acute care hospital length of stay<br />
• Need current number – administrative data – for primary and secondary diagnosis of sepsis –<br />
what portion of patient have sepsis as secondary<br />
• Side goal: Reduce incidence of Severe <strong>Sepsis</strong>/<strong>Sepsis</strong> Shock<br />
• Each <strong>org</strong>anization: rate of SIRS, <strong>Sepsis</strong>, etc. as primary diagnosis<br />
How can this project help us at our facility?<br />
• Need implementation tools for change acceleration<br />
Elevator Speech<br />
Recommend producing an elevator speech for each target audience.<br />
• What our project is about… early identification and treatment of severe systemic infections<br />
(<strong>Sepsis</strong>) to reduce <strong>Sepsis</strong> incidence and related deaths countywide by 25 percent, as well as<br />
overall patient outcomes.<br />
• Why it is important to do… because <strong>Sepsis</strong> is treatable with appropriate and early intervention,<br />
yet today it is the number one cause of death in ICUs nationally with approximately four to five<br />
patients dying per day of <strong>Sepsis</strong> in San Diego County.<br />
• What success will look like… increased countywide compliance with evidenced-based best<br />
practices resulting in reduced incidence and mortality of sepsis with institutions realizing an<br />
overall decrease in patient hospital stay and costs.<br />
• What we need from you… a commitment to understand, support, and comply with best<br />
practices to reduce sepsis mortality including early identification of high-risk patients,<br />
collaborating with colleagues, and providing accurate classification of sepsis.<br />
Staging <strong>Project</strong><br />
Considering evidence available it’s clear what needs to be done…<br />
Timeline<br />
Description<br />
April • How to care for the patient?<br />
• Surviving <strong>Sepsis</strong> Campaign<br />
• Order set available in most facilities<br />
• Literature<br />
June • Early identification of <strong>Sepsis</strong>/Order Sets<br />
August • Finalize Toolkit<br />
• Change management/Implementation<br />
October • Measurement<br />
• Stakeholder analysis<br />
December • <strong>Project</strong> status evaluation<br />
• Review change management