Entamoeba histolytica
Entamoeba histolytica
Entamoeba histolytica
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
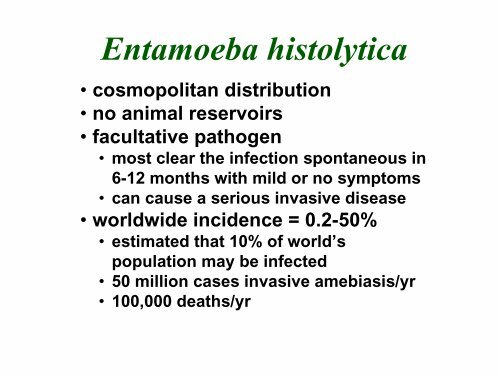
<strong>Entamoeba</strong> <strong>histolytica</strong><br />
• cosmopolitan distribution<br />
• no animal reservoirs<br />
• facultative pathogen<br />
• most clear the infection spontaneous in<br />
6-12 months with mild or no symptoms<br />
• can cause a serious invasive disease<br />
• worldwide incidence = 0.2-50%<br />
• estimated that 10% of world’s<br />
population may be infected<br />
• 50 million cases invasive amebiasis/yr<br />
• 100,000 deaths/yr
1875 Lösch correlated dysentery with amebic<br />
trophozoites<br />
1925 Brumpt proposed two species: E.<br />
dysenteriae and E. dispar<br />
1970's<br />
Facultative Pathogenicity<br />
of <strong>Entamoeba</strong> <strong>histolytica</strong><br />
biochemical differences noted between<br />
invasive and non-invasive isolates<br />
80's/90's several antigenic and DNA differences<br />
demonstrated<br />
• rRNA 2.2% sequence difference<br />
1993 Diamond and Clark proposed a new species<br />
(E. dispar) to describe non-invasive strains<br />
1997 WHO accepted two species
<strong>Entamoeba</strong> <strong>histolytica</strong><br />
Life Cycle
Excystation<br />
• cyst wall disruption<br />
• ameba emerges<br />
• nuclear division (4→8)<br />
• cytoplasmic division<br />
(8 amebala)<br />
• trophozoites colonize<br />
large intestine<br />
• feed on bacteria and<br />
debris<br />
• replicate by binary<br />
fission
Excystation<br />
• cyst wall disruption<br />
• ameba emerges<br />
• nuclear division (4→8)<br />
• cytoplasmic division<br />
(8 amebala)<br />
• trophozoites colonize<br />
large intestine<br />
• feed on bacteria and<br />
debris<br />
• replicate by binary<br />
fission
Encystation<br />
• trophozoite rounds up<br />
• secretion of cyst wall<br />
• aggregation of ribosomes<br />
(= chromatoid bodies)<br />
• 2 rounds of nuclear division<br />
(1→4 nuclei)<br />
• survive weeks to months
trophozoite<br />
immature<br />
cyst<br />
mature<br />
cyst
Pathogenesis of Amebiasis<br />
• NON-INVASIVE<br />
• ameba colony on intestinal mucosa<br />
• asymptomatic cyst passer<br />
• non-dysenteric diarrhea, abdominal<br />
cramps, other GI symptoms<br />
• INVASIVE<br />
• necrosis of mucosa → ulcers, dysentery<br />
• ulcer enlargement → dysentery, peritonitis<br />
• metastasis → extraintestinal amebiasis
• ulcers with raised borders<br />
• little inflammation between lesions
• ‘flasked-shaped ulcer’<br />
• trophozoites at boundary of necrotic<br />
and healthy tissue<br />
• trophozoites ingesting host cells<br />
• dysentery (blood and mucus in feces)
‘hematophagous’ trophozoites
Lateral and Downward Expansion<br />
of Ameba into Lamina Propria<br />
• localized sloughing<br />
• ulcers coalesce<br />
• perforation of intestinal wall
Disease Manifestations<br />
• ulcer enlargement →<br />
severe dysentery<br />
• perforation of intestinal<br />
wall → peritonitis<br />
• local abscesses<br />
• 2 o bacterial infections<br />
• occasional ameboma<br />
(=amebic granuloma)<br />
• cessation of cyst<br />
production<br />
ameboma = inflammatory thickening<br />
of intestinal wall around the abscess<br />
(can be confused with tumor)
Extraintestinal Amebiasis<br />
• metastasis via blood stream<br />
• primarily liver (portal vein)<br />
• other sites less frequent<br />
• ameba-free stools common<br />
• high antibody titers<br />
Amebic Liver Abscess<br />
• chocolate-colored ‘pus’<br />
• necrotic material<br />
• usually bacteria free<br />
• lesions expand and<br />
coalesce<br />
• further metastasis, direct<br />
extension or fistula
Pulmonary Amebiasis<br />
• rarely primary<br />
• rupture of liver abscess<br />
through diaphragm<br />
• 2 o bacterial infections<br />
common<br />
• fever, cough, dyspnea,<br />
pain, vomica
Cutaneous Amebiasis<br />
• intestinal or hepatic fistula<br />
• mucosa bathed in fluids<br />
containing trophozoites<br />
• perianal ulcers<br />
• urogenital (eg, labia,<br />
vagina, penis)
Cutaneous Amebiasis<br />
• intestinal or hepatic fistula<br />
• mucosa bathed in fluids<br />
containing trophozoites<br />
• perianal ulcers<br />
• urogenital (eg, labia,<br />
vagina, penis)
Cutaneous Amebiasis<br />
• intestinal or hepatic fistula<br />
• mucosa bathed in fluids<br />
containing trophozoites<br />
• perianal ulcers<br />
• urogenital (eg, labia,<br />
vagina, penis)
Facultative Pathogenicity<br />
• 85-90% of infected individuals<br />
are asymptomatic<br />
• ~10% of the symptomatic will<br />
develop severe invasive disease
Molecular Epidemiology<br />
• molecular probes used to survey for<br />
E. dispar and E. <strong>histolytica</strong><br />
• E. dispar ~10-fold > E. <strong>histolytica</strong><br />
• discrete endemic pockets of E. <strong>histolytica</strong><br />
• many asymptomatic E.h. infections<br />
• ~10% of the E.h. infections are<br />
associated with invasive amebiasis<br />
• ~25% seropositive for E. <strong>histolytica</strong> in<br />
endemic areas
pathogenecity<br />
virulence<br />
ability to cause disease<br />
(genetic component)<br />
relative capacity to cause<br />
disease (degree of pathology)<br />
• a pathogen has an inherent ability to<br />
break host cell barriers<br />
• virulence usually correlates with ability<br />
to replicate within host<br />
• various degrees of virulence may be<br />
exhibited depending on conditions
• contact-dependent killing of epithelial cells<br />
• breakdown of tissues (extracellular matrix)<br />
• secreted proteases?<br />
• contact-dependent killing of neutrophils,<br />
leukocytes, etc.
E. <strong>histolytica</strong> vs E. dispar<br />
CRITERIA E. dispar E. <strong>histolytica</strong><br />
In Vitro Culture xenic axenic<br />
ConA Agglutination - +<br />
Complement Resistance - +<br />
Zymodemes (isoenzymes) I & III II<br />
Numerous Antigenic Differences<br />
(eg., GIAP Epitopes) 1-2 1-6<br />
Numerous DNA Sequence Differences<br />
(eg., rRNA)<br />
2.2% sequence diversity<br />
RFLP/DNA Probes<br />
B133<br />
cEH-NP1<br />
P145<br />
cEH-P1
Galactose Inhibitable Adherence Protein<br />
• trophozoites adhere to mucins, epithelial<br />
cells, leukocytes, etc<br />
• mediated by galactose-inhibitable lectin activity<br />
• lectin activity due to surface protein (GIAP)<br />
• 170 kDa heavy chain mediates binding (multigene<br />
family)<br />
• 35 kDa light chain anchor to membrane<br />
• α-GIAP Abs abrogate complement resistance<br />
• ~85% identity between Eh and Ed<br />
• Are there differences in adherence?<br />
• after contact the target cell is lysed and<br />
phagocytosed by the trophozoite
Host Cell Lysis and Phagocytosis<br />
• Amebapore<br />
• pore-forming peptide<br />
• potent anti-bacterial<br />
activity<br />
• located in vacuoles, not<br />
secreted<br />
• Eh and Ed sequences<br />
are 95% identical<br />
• Glu→Pro change<br />
breaks α-helix<br />
• Ed had 80% less<br />
activity than Eh
<strong>Entamoeba</strong> Proteases<br />
• Eh expresses and secretes higher<br />
levels of cysteine proteases<br />
• 6 cys-protease genes (ehcp1-6)<br />
• ehcp1 and 5 are missing in Ed<br />
• 90% inhibition of ehcp5 did not affect<br />
trophozoite mediated destruction of<br />
host cell monolayers
Prevalence<br />
Epidemiologic Risk Factors<br />
• lower socioeconomic status<br />
• crowding<br />
• lack of indoor plumbing<br />
• endemic area<br />
• institutionalization<br />
• communal living<br />
• promiscuity among male<br />
homosexuals<br />
Severity<br />
Modified from Ravdin (1995) Clin. Inf. Dis. 20:1453<br />
• children, esp. neonates<br />
• pregnancy and<br />
postpartum states<br />
• corticosteroid use<br />
• malignancy<br />
• malnutrition
Clinical Syndromes<br />
Associated with Amebiasis<br />
Intestinal Disease<br />
• asymptomatic cyst passer<br />
• symptomatic nondysenteric<br />
infection<br />
• amebic dysentery<br />
• fulminant colitis<br />
! + perforation (peritonitis)<br />
• ameboma (amebic granuloma)<br />
• perianal ulceration<br />
Extraintestinal Disease<br />
• liver abscess<br />
• pleuropulmonary amebiasis<br />
• brain and other organs<br />
• cutaneous and genital diseases<br />
Intestinal Symptoms<br />
• range<br />
• mild to intense<br />
• transient to long lasting<br />
• nondysenteric<br />
• diarrhea<br />
• cramps<br />
• flatulence<br />
• nausea<br />
• dysenteric<br />
• blood/mucus in stools<br />
• cramps/pain<br />
• tenesmus<br />
• ameboma<br />
• palpable mass<br />
• obstruction
Diagnosis<br />
Intestinal<br />
• stool examination<br />
! cysts and/or trophozoites<br />
• sigmoidoscopy<br />
! lesions, aspirate, biopsy<br />
• antigen detection<br />
! <strong>histolytica</strong>/dispar<br />
Extraintestinal (hepatic)<br />
• symptoms<br />
! history of dysentery<br />
! RUQ pain<br />
! enlarged liver<br />
• serology (current or past?)<br />
• imaging (CT, MRI, ultrasound)<br />
• abscess aspiration<br />
! only select cases<br />
! reddish brown liquid<br />
! trophozoites at abscess wall
Antigen Detection Assay<br />
α-GIAP Monoclonal<br />
Antibodies<br />
mAb E.h. E.d.<br />
3F4 + +<br />
8A3 + +<br />
7F4 + -<br />
8C12 + -<br />
1G7 + -<br />
H85 + -<br />
Reactivities of mAbs against<br />
E. <strong>histolytica</strong> and E. dispar<br />
Possible Outcomes<br />
and Interpretations<br />
capture/detection mAbs<br />
3F4/8A3<br />
8C12/1G7 interpretation<br />
+ + E. <strong>histolytica</strong><br />
+ - E. dispar<br />
- + inconclusive<br />
- - negative
Diagnosis<br />
Intestinal<br />
• stool examination<br />
! cysts and/or trophozoites<br />
• sigmoidoscopy<br />
! lesions, aspirate, biopsy<br />
• antigen detection<br />
! <strong>histolytica</strong>/dispar<br />
Extraintestinal (hepatic)<br />
• symptoms<br />
! history of dysentery<br />
! RUQ pain<br />
! enlarged liver<br />
• serology (current or past?)<br />
• imaging (CT, MRI, ultrasound)<br />
• abscess aspiration<br />
! only select cases<br />
! reddish brown liquid<br />
! trophozoites at abscess wall
Treatment<br />
asymptomatic<br />
• iodoquinol or<br />
paromomycin<br />
• endemic areas?<br />
symptomatic<br />
• metronidazole or<br />
tinidazole<br />
• followed by lumenal<br />
agents<br />
drain liver abscess<br />
• only with high<br />
probability of rupture!<br />
Control and<br />
Epidemiology<br />
• avoid fecal-oral transmission<br />
• not normally associated with<br />
travelers diarrhea<br />
• > 1 month stay<br />
• institutions<br />
• mass drug treatment little<br />
affect<br />
• ↑ staff and improved housing<br />
conditions lowers prevalence<br />
• male homosexuals<br />
• 40-50% in NYC and SF during<br />
late 70’s<br />
• lower since AIDS/safe sex