(ADL) DECLINE - Primaris
(ADL) DECLINE - Primaris
(ADL) DECLINE - Primaris
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
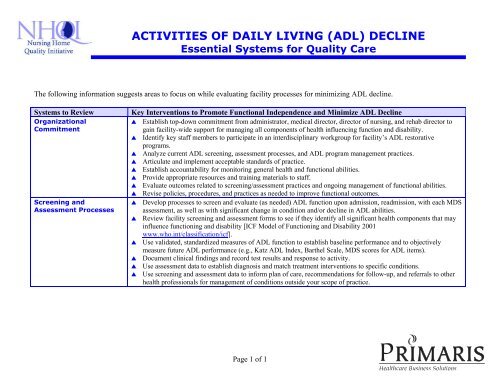
ACTIVITIES OF DAILY LIVING (<strong>ADL</strong>) <strong>DECLINE</strong><br />
Essential Systems for Quality Care<br />
The following information suggests areas to focus on while evaluating facility processes for minimizing <strong>ADL</strong> decline.<br />
Systems to Review<br />
Organizational<br />
Commitment<br />
Screening and<br />
Assessment Processes<br />
Key Interventions to Promote Functional Independence and Minimize <strong>ADL</strong> Decline<br />
Establish top-down commitment from administrator, medical director, director of nursing, and rehab director to<br />
gain facility-wide support for managing all components of health influencing function and disability.<br />
Identify key staff members to participate in an interdisciplinary workgroup for facility’s <strong>ADL</strong> restorative<br />
programs.<br />
Analyze current <strong>ADL</strong> screening, assessment processes, and <strong>ADL</strong> program management practices.<br />
Articulate and implement acceptable standards of practice.<br />
Establish accountability for monitoring general health and functional abilities.<br />
Provide appropriate resources and training materials to staff.<br />
Evaluate outcomes related to screening/assessment practices and ongoing management of functional abilities.<br />
Revise policies, procedures, and practices as needed to improve functional outcomes.<br />
Develop processes to screen and evaluate (as needed) <strong>ADL</strong> function upon admission, readmission, with each MDS<br />
assessment, as well as with significant change in condition and/or decline in <strong>ADL</strong> abilities.<br />
Review facility screening and assessment forms to see if they identify all significant health components that may<br />
influence functioning and disability [ICF Model of Functioning and Disability 2001<br />
<br />
<br />
<br />
<br />
www.who.int/classification/icf].<br />
Use validated, standardized measures of <strong>ADL</strong> function to establish baseline performance and to objectively<br />
measure future <strong>ADL</strong> performance (e.g., Katz <strong>ADL</strong> Index, Barthel Scale, MDS scores for <strong>ADL</strong> items).<br />
Document clinical findings and record test results and response to activity.<br />
Use assessment data to establish diagnosis and match treatment interventions to specific conditions.<br />
Use screening and assessment data to inform plan of care, recommendations for follow-up, and referrals to other<br />
health professionals for management of conditions outside your scope of practice.<br />
Page 1 of 1
Systems to Review<br />
Care Planning Process<br />
Interventions and<br />
Treatment Processes<br />
Key Interventions to Promote Functional Independence and Minimize <strong>ADL</strong> Decline<br />
Identify all health components impacting functional abilities.<br />
Establish a diagnosis and prognosis.<br />
Develop a plan of care that matches treatments to specific conditions.<br />
Identify interventions/treatments (i.e., functional training, training in simulated environments, exercise, device and<br />
equipment use, task adaptation, barrier accommodation or modification, safety awareness training, injury<br />
prevention/reduction training, restorative nursing program, family/caregiver training, referrals to other health<br />
professionals). Identify treatment frequency and duration.<br />
Identify caregiver to implement care plan interventions.<br />
Record expected outcomes. Record response to treatments.<br />
Review and revise care plans based on resident’s response and feedback from resident and all other team members<br />
[Guide to Physical Therapist Practice. 2 nd ed. Phys Ther. 2001;81:9-744].<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Identify and treat all health conditions that may influence functional abilities.<br />
Match treatment interventions to specific conditions. Select rehabilitation interventions appropriate to the<br />
impairment, disability, and limitation in activity or restricted ability to participate. Rehab interventions may<br />
include functional training, training in simulated environments, exercise, device and equipment use, task<br />
adaptation, barrier accommodation or modification, safety awareness training, injury prevention/reduction<br />
training, restorative nursing program, family/caregiver training, and/or referrals to other health professionals.<br />
Manage general health throughout all stages of treatment including comorbid conditions, acute illness, nutrition,<br />
hydration, bowel and bladder function. Prevent complications of DVT, dysphagia, aspiration, skin breakdown,<br />
UTI, falls, loss of ROM, immobility, edema, adverse drug reactions, depression [Clinical Practice Guideline, Post-<br />
Stroke Rehabilitation, Quick Ref. Guide 16, AHCPR].<br />
Educate and document training provided to residents, family/caregiver, and staff regarding function, interventions,<br />
use of adaptive/assistive equipment, precautions, and safety issues.<br />
Institute restorative programs, maintenance programs, and post-discharge exercise programs to improve, maintain<br />
or prevent/minimize <strong>ADL</strong> decline.<br />
Identify and treat residents in need of skilled therapy services or restorative <strong>ADL</strong> programs.<br />
Identify and address environmental factors influencing <strong>ADL</strong> function (e.g., available equipment, assistive devices,<br />
restraint use, environmental barriers (building, furniture), attitudes, institutional support, staff knowledge/training,<br />
institutionally induced helplessness of residents, policies, family support and relationships).<br />
[ICF Model of Functioning and Disability 2001 www.who.int/classification/icf]<br />
[Morris JN, Fiatarone M, Kiely DK, Belleville-Taylor P, Murphy K, Littlehale S, Ooi WL, O’Neill E, and Doyle N.<br />
Nursing rehabilitation and exercise strategies in the nursing home. Journal of Gerontology: Medical Sciences. 1999<br />
Oct;54(10):M494-500.]<br />
Page 2 of 2
Systems to Review<br />
Monitoring and<br />
Reassessing<br />
Policies and Procedures<br />
Staff Education and<br />
Training<br />
Key Interventions to Promote Functional Independence and Minimize <strong>ADL</strong> Decline<br />
Develop documentation tools to record and monitor general health condition, significant changes, current<br />
interventions, response to interventions, duration and frequency of treatments, functional performance and<br />
capacity, amount of assistance required, adaptive techniques, assistive equipment used, progress toward goals,<br />
need for reassessment, need for referral to other health professionals.<br />
Establish ongoing channels of communication between resident, all involved health professionals, restorative<br />
aides, family, and caregivers regarding current status, progress toward goals, and related issues (e.g.,<br />
interdisciplinary team meetings, care plan meetings, family conferences, discharge planning meetings).<br />
Facility policies, procedures, and clinical practice standards are in place to screen and evaluate <strong>ADL</strong> functions at<br />
appropriate intervals.<br />
Involve all appropriate health professionals in managing residents’ health conditions.<br />
Communicate current condition and performance to designated MDS recorder, to ensure correct coding on MDS<br />
functional items.<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Measure current staff knowledge and competencies with <strong>ADL</strong> skills and all health components related to function<br />
and disability.<br />
Identify learning needs.<br />
Organize staff training to address all components of health influencing function and disability (e.g., physiological,<br />
psychological, anatomical, functional, environmental, social).<br />
Solicit training from health professionals with knowledge and skills to educate staff about various health<br />
components (i.e., physicians, nurses, therapists, dieticians, social workers, psychologists).<br />
Identify a clinical expert in the facility for <strong>ADL</strong> skills and restorative programs.<br />
Provide ongoing staff training (at least quarterly) to address all aspects of <strong>ADL</strong> management.<br />
Educate staff in documentation methods to record residents’ general condition, changes, functional performance,<br />
decline in functional abilities.<br />
Teach staff how to make referrals to other health professionals for management of significant health conditions.<br />
Incorporate training into orientation of newly hired employees regarding all components of health influencing<br />
functional abilities.<br />
Provide ongoing information to residents, families, caregivers, and staff regarding current treatment interventions,<br />
<strong>ADL</strong> programs, and how to get involved.<br />
MO-03-01-NHAD January 2003<br />
This material was prepared by <strong>Primaris</strong> under contract<br />
with the Centers for Medicare & Medicaid Services (CMS).<br />
The contents presented do not necessarily reflect CMS policy.<br />
Version 01/14/2003<br />
Page 3 of 3