BSRBR|Newsletter - The British Society for Rheumatology
BSRBR|Newsletter - The British Society for Rheumatology
BSRBR|Newsletter - The British Society for Rheumatology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
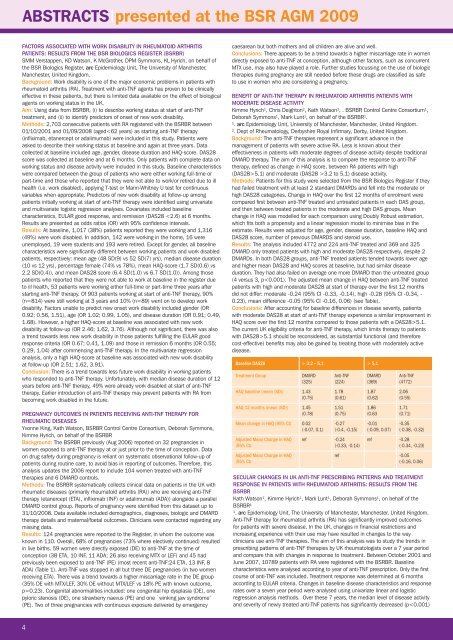
ABSTRACTS|presented at the BSR AGM 2009<br />
FACTORS ASSOCIATED WITH WORK DISABILITY IN RHEUMATOID ARTHRITIS<br />
PATIENTS: RESULTS FROM THE BSR BIOLOGICS REGISTER (BSRBR)<br />
SMM Verstappen, KD Watson, K McGrother, DPM Symmons, KL Hyrich, on behalf of<br />
the BSR Biologics Register, arc Epidemiology Unit, <strong>The</strong> University of Manchester,<br />
Manchester, United Kingdom.<br />
Background: Work disability is one of the major economic problems in patients with<br />
rheumatoid arthritis (RA). Treatment with anti-TNF agents has proven to be clinically<br />
effective in these patients, but there is limited data available on the effect of biological<br />
agents on working status in the UK.<br />
Aim: Using data from BSRBR, (i) to describe working status at start of anti-TNF<br />
treatment, and (ii) to identify predictors of onset of new work disability.<br />
Methods: 2,703 consecutive patients with RA registered with the BSRBR between<br />
01/10/2001 and 01/09/2008 (aged3.2 to 5.1) disease activity.<br />
Methods: Patients <strong>for</strong> this study were selected from the BSR Biologics Register if they<br />
had failed treatment with at least 2 standard DMARDs and fell into the moderate or<br />
high DAS28 categories. Change in HAQ over the first 12 months of enrolment were<br />
compared first between anti-TNF treated and untreated patients in each DAS group,<br />
and then between treated patients in the moderate and high DAS groups. Mean<br />
change in HAQ was modelled <strong>for</strong> each comparison using Doubly Robust estimation,<br />
which fits both a propensity and a linear regression model to minimise bias in the<br />
estimate. Results were adjusted <strong>for</strong> age, gender, disease duration, baseline HAQ and<br />
DAS28 score, number of previous DMARDS and steroid use.<br />
Results: <strong>The</strong> analysis included 4772 and 224 anti-TNF treated and 369 and 325<br />
DMARD only treated patients with high and moderate DAS28 respectively, despite 2<br />
DMARDs. In both DAS28 groups, anti-TNF treated patients tended towards lower age<br />
and higher mean DAS28 and HAQ scores at baseline, but had similar disease<br />
duration. <strong>The</strong>y had also failed on average one more DMARD than the untreated group<br />
(4 versus 3, p5.1.<br />
<strong>The</strong> current UK eligibility criteria <strong>for</strong> anti-TNF therapy, which limits therapy to patients<br />
with DAS28>5.1 should be reconsidered, as substantial functional (and there<strong>for</strong>e<br />
cost-effective) benefits may also be gained by treating those with moderately active<br />
disease.<br />
Baseline DAS28 > 3.2 – 5.1 > 5.1<br />
Treatment Group DMARD Anti-TNF DMARD Anti-TNF<br />
(325) (224) (369) (4772)<br />
HAQ baseline (mean (SD)) 1.43 1.78 1.87 2.06<br />
(0.75) (0.61) (0.62) (0.55)<br />
HAQ 12 months (mean (SD)) 1.45 1.51 1.86 1.71<br />
(0.78) (0.75) (0.63 (0.71)<br />
Mean change in HAQ (95% CI) 0.02 -0.27 -0.01 -0.35<br />
(-0.07, 0.1) (-0.4, -0.15) (-0.09, 0.07) (-0.38, -0.32)<br />
Adjusted Mean Change in HAQ ref -0.24 ref -0.28<br />
(95% CI) (-0.33, -0.14) (-0.34, -0.23)<br />
Adjusted Mean Change in HAQ ref -0.05<br />
(95% CI) (-0.16, 0.06)<br />
SECULAR CHANGES IN UK ANTI-TNF PRESCRIBING PATTERNS AND TREATMENT<br />
RESPONSE IN PATIENTS WITH RHEUMATOID ARTHRITIS: RESULTS FROM THE<br />
BSRBR<br />
Kath Watson 1 , Kimme Hyrich 1 , Mark Lunt 1 , Deborah Symmons 1 , on behalf of the<br />
BSRBR 1<br />
1<br />
. arc Epidemiology Unit, <strong>The</strong> University of Manchester, Manchester, United Kingdom.<br />
Anti-TNF therapy <strong>for</strong> rheumatoid arthritis (RA) has significantly improved outcomes<br />
<strong>for</strong> patients with severe disease. In the UK, changes in financial restrictions and<br />
increasing experience with their use may have resulted in changes to the way<br />
clinicians use anti-TNF therapies. <strong>The</strong> aim of this analysis was to study the trends in<br />
prescribing patterns of anti-TNF therapies by UK rheumatologists over a 7 year period<br />
and compare this with changes in response to treatment. Between October 2001 and<br />
June 2007, 10789 patients with RA were registered with the BSRBR. Baseline<br />
characteristics were analysed according to year of anti-TNF prescription. Only the first<br />
course of anti-TNF was included. Treatment response was determined at 6 months<br />
according to EULAR criteria. Changes in baseline disease characteristics and response<br />
rates over a seven year period were analysed using univariate linear and logistic<br />
regression analysis methods. Over these 7 years, the median level of disease activity<br />
and severity of newly treated anti-TNF patients has significantly decreased (p