The Surgical Approach to Subaxial Cervical Spine Injuries
The Surgical Approach to Subaxial Cervical Spine Injuries
The Surgical Approach to Subaxial Cervical Spine Injuries
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Subaxial</strong> <strong>Cervical</strong> <strong>Spine</strong> <strong>Injuries</strong> • Dvorak et al<br />
2623<br />
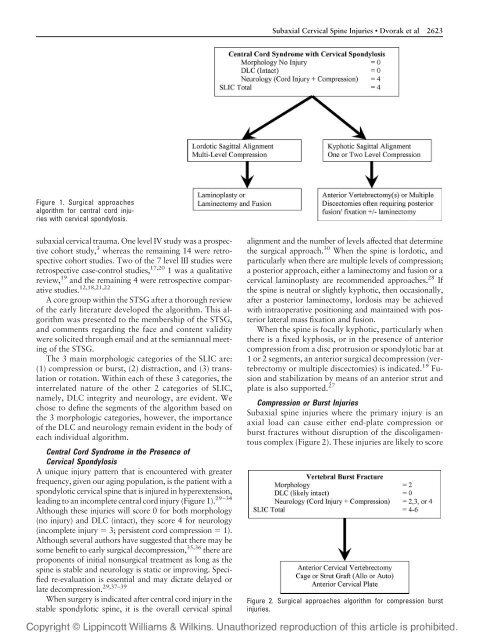
Figure 1. <strong>Surgical</strong> approaches<br />
algorithm for central cord injuries<br />
with cervical spondylosis.<br />
subaxial cervical trauma. One level IV study was a prospective<br />
cohort study, 3 whereas the remaining 14 were retrospective<br />
cohort studies. Two of the 7 level III studies were<br />
retrospective case-control studies, 17,20 1 was a qualitative<br />
review, 19 and the remaining 4 were retrospective comparative<br />
studies. 12,18,21,22<br />
A core group within the STSG after a thorough review<br />
of the early literature developed the algorithm. This algorithm<br />
was presented <strong>to</strong> the membership of the STSG,<br />
and comments regarding the face and content validity<br />
were solicited through email and at the semiannual meeting<br />
of the STSG.<br />
<strong>The</strong> 3 main morphologic categories of the SLIC are:<br />
(1) compression or burst, (2) distraction, and (3) translation<br />
or rotation. Within each of these 3 categories, the<br />
interrelated nature of the other 2 categories of SLIC,<br />
namely, DLC integrity and neurology, are evident. We<br />
chose <strong>to</strong> define the segments of the algorithm based on<br />
the 3 morphologic categories, however, the importance<br />
of the DLC and neurology remain evident in the body of<br />
each individual algorithm.<br />
Central Cord Syndrome in the Presence of<br />
<strong>Cervical</strong> Spondylosis<br />
A unique injury pattern that is encountered with greater<br />
frequency, given our aging population, is the patient with a<br />
spondylotic cervical spine that is injured in hyperextension,<br />
leading <strong>to</strong> an incomplete central cord injury (Figure 1). 29–34<br />
Although these injuries will score 0 for both morphology<br />
(no injury) and DLC (intact), they score 4 for neurology<br />
(incomplete injury 3; persistent cord compression 1).<br />
Although several authors have suggested that there may be<br />
some benefit <strong>to</strong> early surgical decompression, 35,36 there are<br />
proponents of initial nonsurgical treatment as long as the<br />
spine is stable and neurology is static or improving. Specified<br />
re-evaluation is essential and may dictate delayed or<br />
late decompression. 29,37–39<br />
When surgery is indicated after central cord injury in the<br />
stable spondylotic spine, it is the overall cervical spinal<br />
alignment and the number of levels affected that determine<br />
the surgical approach. 30 When the spine is lordotic, and<br />
particularly when there are multiple levels of compression;<br />
a posterior approach, either a laminec<strong>to</strong>my and fusion or a<br />
cervical laminoplasty are recommended approaches. 28 If<br />
the spine is neutral or slightly kyphotic, then occasionally,<br />
after a posterior laminec<strong>to</strong>my, lordosis may be achieved<br />
with intraoperative positioning and maintained with posterior<br />
lateral mass fixation and fusion.<br />
When the spine is focally kyphotic, particularly when<br />
there is a fixed kyphosis, or in the presence of anterior<br />
compression from a disc protrusion or spondylotic bar at<br />
1 or 2 segments, an anterior surgical decompression (vertebrec<strong>to</strong>my<br />
or multiple discec<strong>to</strong>mies) is indicated. 19 Fusion<br />
and stabilization by means of an anterior strut and<br />
plate is also supported. 27<br />
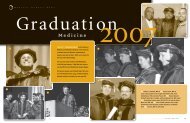
Compression or Burst <strong>Injuries</strong><br />
<strong>Subaxial</strong> spine injuries where the primary injury is an<br />
axial load can cause either end-plate compression or<br />
burst fractures without disruption of the discoligamen<strong>to</strong>us<br />
complex (Figure 2). <strong>The</strong>se injuries are likely <strong>to</strong> score<br />
Figure 2. <strong>Surgical</strong> approaches algorithm for compression burst<br />
injuries.