Secondary Chondrosarcoma
Secondary Chondrosarcoma
Secondary Chondrosarcoma
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
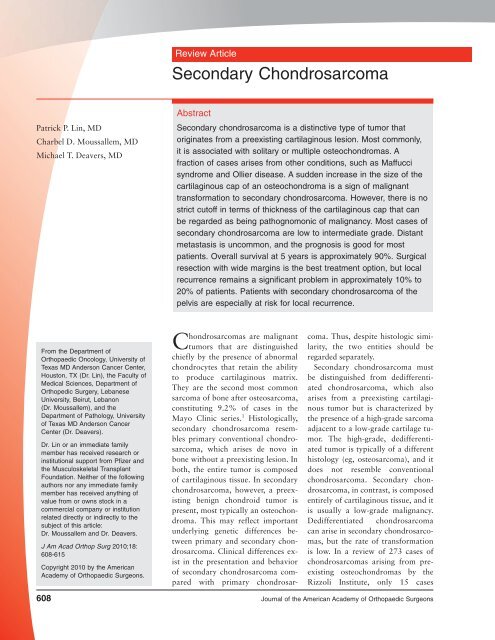
Review Article<br />
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Patrick P. Lin, MD<br />
Charbel D. Moussallem, MD<br />
Michael T. Deavers, MD<br />
Abstract<br />
<strong>Secondary</strong> chondrosarcoma is a distinctive type of tumor that<br />
originates from a preexisting cartilaginous lesion. Most commonly,<br />
it is associated with solitary or multiple osteochondromas. A<br />
fraction of cases arises from other conditions, such as Maffucci<br />
syndrome and Ollier disease. A sudden increase in the size of the<br />
cartilaginous cap of an osteochondroma is a sign of malignant<br />
transformation to secondary chondrosarcoma. However, there is no<br />
strict cutoff in terms of thickness of the cartilaginous cap that can<br />
be regarded as being pathognomonic of malignancy. Most cases of<br />
secondary chondrosarcoma are low to intermediate grade. Distant<br />
metastasis is uncommon, and the prognosis is good for most<br />
patients. Overall survival at 5 years is approximately 90%. Surgical<br />
resection with wide margins is the best treatment option, but local<br />
recurrence remains a significant problem in approximately 10% to<br />
20% of patients. Patients with secondary chondrosarcoma of the<br />
pelvis are especially at risk for local recurrence.<br />
From the Department of<br />
Orthopaedic Oncology, University of<br />
Texas MD Anderson Cancer Center,<br />
Houston, TX (Dr. Lin), the Faculty of<br />
Medical Sciences, Department of<br />
Orthopedic Surgery, Lebanese<br />
University, Beirut, Lebanon<br />
(Dr. Moussallem), and the<br />
Department of Pathology, University<br />
of Texas MD Anderson Cancer<br />
Center (Dr. Deavers).<br />
Dr. Lin or an immediate family<br />
member has received research or<br />
institutional support from Pfizer and<br />
the Musculoskeletal Transplant<br />
Foundation. Neither of the following<br />
authors nor any immediate family<br />
member has received anything of<br />
value from or owns stock in a<br />
commercial company or institution<br />
related directly or indirectly to the<br />
subject of this article:<br />
Dr. Moussallem and Dr. Deavers.<br />
J Am Acad Orthop Surg 2010;18:<br />
608-615<br />
Copyright 2010 by the American<br />
Academy of Orthopaedic Surgeons.<br />
<strong>Chondrosarcoma</strong>s are malignant<br />
tumors that are distinguished<br />
chiefly by the presence of abnormal<br />
chondrocytes that retain the ability<br />
to produce cartilaginous matrix.<br />
They are the second most common<br />
sarcoma of bone after osteosarcoma,<br />
constituting 9.2% of cases in the<br />
Mayo Clinic series. 1 Histologically,<br />
secondary chondrosarcoma resembles<br />
primary conventional chondrosarcoma,<br />
which arises de novo in<br />
bone without a preexisting lesion. In<br />
both, the entire tumor is composed<br />
of cartilaginous tissue. In secondary<br />
chondrosarcoma, however, a preexisting<br />
benign chondroid tumor is<br />
present, most typically an osteochondroma.<br />
This may reflect important<br />
underlying genetic differences between<br />
primary and secondary chondrosarcoma.<br />
Clinical differences exist<br />
in the presentation and behavior<br />
of secondary chondrosarcoma compared<br />
with primary chondrosarcoma.<br />
Thus, despite histologic similarity,<br />
the two entities should be<br />
regarded separately.<br />
<strong>Secondary</strong> chondrosarcoma must<br />
be distinguished from dedifferentiated<br />
chondrosarcoma, which also<br />
arises from a preexisting cartilaginous<br />
tumor but is characterized by<br />
the presence of a high-grade sarcoma<br />
adjacent to a low-grade cartilage tumor.<br />
The high-grade, dedifferentiated<br />
tumor is typically of a different<br />
histology (eg, osteosarcoma), and it<br />
does not resemble conventional<br />
chondrosarcoma. <strong>Secondary</strong> chondrosarcoma,<br />
in contrast, is composed<br />
entirely of cartilaginous tissue, and it<br />
is usually a low-grade malignancy.<br />
Dedifferentiated chondrosarcoma<br />
can arise in secondary chondrosarcomas,<br />
but the rate of transformation<br />
is low. In a review of 273 cases of<br />
chondrosarcomas arising from preexisting<br />
osteochondromas by the<br />
Rizzoli Institute, only 15 cases<br />
608 Journal of the American Academy of Orthopaedic Surgeons
Patrick P. Lin, MD, et al<br />
Table 1<br />
Major Series on <strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Study<br />
No. of<br />
Cases<br />
Preexisting<br />
Lesion (No.)<br />
Grade 14<br />
(No. of Cases)<br />
52 Solitary OC (21), HME (4),<br />
Coley and<br />
N/A<br />
Higinbotham 6 enchondroma (23), Ollier<br />
disease (4)<br />
Garrison et al 7 75 Solitary OC (40), HME (35) 1 (64), 2 (10), 3 (1)<br />
Hudson et al 8 15 Solitary OC (12), HME (3) 1 (11), 2 (3), 3 (1)<br />
Sun et al 12 5 Maffucci syndrome (all) 1 (1), 2 (3), N/A (1)<br />
Liuetal 9 12 Ollier disease (all) 1 (10), 2 (2)<br />
Merchan et al 10 4 HME (all) 1 (4)<br />
Wuisman<br />
45 Solitary OC (16), HME (29) 1 (30), 2 (13), 3 (2)<br />
et al 13<br />
Schaison<br />
29 Solitary OC (17), Ollier<br />
1(9),2(18),N/A(2)<br />
et al 11 disease (12)<br />
Ahmed et al 4 107 Solitary OC (61), HME (46) 1 (97), 2 (10)<br />
Altayetal 5 32 Solitary OC (14), HME (10), enchondroma<br />
(6), Ollier disease<br />
(1), Maffucci syndrome (1)<br />
1(28),2(4)<br />
HME = hereditary multiple exostosis, N/A = not available, OC = osteochondroma<br />
Table 2<br />
Risk Factors for <strong>Secondary</strong><br />
<strong>Chondrosarcoma</strong><br />
Clinical<br />
Pain<br />
Increasing size of a palpable lesion<br />
Male predominance (2:1)<br />
Location in the pelvis or hip<br />
Peak age in mid 30s<br />
Radiographic<br />
Surface irregularity<br />
Blurriness of the border<br />
Osteochondroma >5 cm<br />
Increase in size of osteochondroma<br />
Cartilage cap >2 cm<br />
Inhomogeneous mineralization of large<br />
cartilage cap<br />
Genetic<br />
Hereditary multiple exostosis (EXT1,<br />
EXT2, EXT3 mutations)<br />
Ollier disease<br />
Maffucci syndrome<br />
(5.5%) underwent dedifferentiation. 2<br />
Most cases of dedifferentiated chondrosarcomas<br />
appear to originate<br />
from central primary chondrosarcoma;<br />
it is estimated that the fraction<br />
of primary chondrosarcomas undergoing<br />
dedifferentiation may be as<br />
high as 15.4%. 3 In most cases, the<br />
prognosis of patients with dedifferentiated<br />
chondrosarcoma is dismal,<br />
which is quite unlike the prognosis<br />
of patients with secondary chondrosarcoma.<br />
<strong>Secondary</strong> chondrosarcoma is a<br />
well-recognized clinical diagnosis.<br />
However, relatively little has been<br />
published on the subject, perhaps as<br />
a result of the rarity of the condition.<br />
In a review of the literature, we<br />
found only 10 studies pertaining directly<br />
to the subject that were not<br />
case reports (Table 1).<br />
Clinical Presentation<br />
The most frequent presenting complaints<br />
with secondary chondrosarcoma<br />
are a palpable mass and pain.<br />
In many cases, the signs and symptoms<br />
are subtle, and the complaints<br />
are not severe. Large masses in the<br />
pelvis and thigh are easily hidden<br />
from patient and clinician alike. New<br />
onset of pain in a preexisting osteochondroma<br />
should alert the physician<br />
to the possibility of enlargement<br />
of the cartilaginous cap. Rarely,<br />
some tumors in the pelvis may cause<br />
urinary and bowel irregularities.<br />
A male predilection for secondary<br />
chondrosarcoma seems to be evident.<br />
Based on combined data from the<br />
published series, 63% of patients<br />
with the disease are male and 37%<br />
are female, resulting in a male:female<br />
ratio of approximately 2:1. 4-13 The<br />
mean age of persons with secondary<br />
chondrosarcoma is 34 years, which<br />
is notably younger than the average<br />
age of persons with primary conventional<br />
chondrosarcoma. 4-13 The most<br />
common site of involvement is the<br />
pelvis, followed by the proximal femur.<br />
The scapula and proximal humerus<br />
are also relatively common<br />
sites. Clinical, radiographic, and genetic<br />
features associated with secondary<br />
chondrosarcomas are summarized<br />
in Table 2.<br />
Our review of the major published<br />
series indicates that the great majority<br />
of cases arise in osteochondromas<br />
(88%), with solitary osteochondroma<br />
being slightly more common<br />
than multiple osteochondromas (ie,<br />
hereditary multiple exostosis). 4-7,11,13<br />
<strong>Secondary</strong> chondrosarcoma can also<br />
occur in persons with Ollier disease<br />
(ie, multiple enchondromas) and<br />
Maffucci syndrome (ie, multiple enchondromas<br />
associated with softtissue<br />
hemangiomas). Other benign<br />
cartilaginous lesions that have been<br />
reported, although rarely to result in<br />
secondary chondrosarcoma include<br />
solitary enchondroma, synovial<br />
chondromatosis, and chondromyxoid<br />
fibroma. 6,15-20 These lesions have<br />
been noted mostly in case reports,<br />
and there may be some question<br />
whether some cases were malignant<br />
at the outset. 6,15-20<br />
October 2010, Vol 18, No 10 609
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Figure 1<br />
<strong>Secondary</strong> chondrosarcoma arising from a pelvic osteochondroma. A, Preoperative AP pelvic radiograph<br />
demonstrating a large calcified tumor arising from the iliac wing. The surfaces of the calcified areas are indistinct and<br />
not well-delineated. B, Postoperative AP pelvic radiograph following wide excision of the tumor. C, Photograph of the<br />
cut specimen after resection demonstrating a thick layer of white, glistening hyaline cartilage. The central area shows a<br />
small area of ossified bone (arrow), which represents the stalk of the preexisting osteochondroma. D, T1-weighted<br />
axial magnetic resonance image demonstrating fatty marrow in the central portion of the sessile stalk emanating from<br />
the iliac crest, indicating the presence of an ossified central portion of the original osteochondroma. E, T2-weighted<br />
axial magnetic resonance image demonstrating the thick layer of cartilaginous tumor surrounding the central ossified<br />
stalk, which appears dark. F, Gadolinium-enhanced fat-saturated T1-weighted magnetic resonance image showing a<br />
subtle speckled pattern of enhancement within the tumor.<br />
Radiologic Features<br />
Conventional radiography may offer<br />
important clues regarding the diagnosis<br />
of secondary chondrosarcoma.<br />
Osteochondromas have well-defined<br />
bony edges, including the subchondral<br />
bone of the cartilaginous cap. In<br />
contrast, secondary chondrosarcomas<br />
demonstrate irregularity or blurriness<br />
of the surface of the osteochondroma<br />
(Figure 1). A soft-tissue<br />
mass outside the osseous portion of<br />
the osteochondroma may be subtly<br />
appreciable, and this mass may exhibit<br />
scattered foci of calcification. 4,5<br />
CT and MRI are important in<br />
demonstrating the malignant features<br />
of the tumor. Most critically,<br />
they reveal an abnormally large cartilaginous<br />
cap on the osteochondroma<br />
(Figure 1, D through F). The<br />
portion of the osteochondroma that<br />
becomes malignant is the cartilaginous<br />
tissue that forms the cap of the<br />
lesion. The osseous tissue that makes<br />
up the base or stalk is not thought to<br />
610 Journal of the American Academy of Orthopaedic Surgeons
Patrick P. Lin, MD, et al<br />
undergo malignant transformation.<br />
Plain radiography may not demonstrate<br />
the cartilage cap as well as either<br />
CT or MRI do, which may lead<br />
the unwary clinician to underestimate<br />
the true size of the cap.<br />
Osteochondromas may have the<br />
appearance of an enlarged cartilage<br />
cap on T2-weighted magnetic resonance<br />
images when there is a large<br />
bursa around the cap. The fluid<br />
within the bursa appears similar to<br />
that of cartilage tissue because both<br />
entities have high water content.<br />
Gadolinium contrast is used to distinguish<br />
bursal structures from true<br />
cartilage tissue. The bursas have only<br />
rim enhancement of the bursal tissue<br />
without contrast enhancement of the<br />
fluid inside the bursa.<br />
Many clinicians believe that a cartilage<br />
cap with a thickness of 2 cm seems to be<br />
strong evidence for the presence of<br />
secondary chondrosarcoma.<br />
Some authors have stressed the importance<br />
of the character of the cartilage<br />
cap in addition to its absolute<br />
size. Ahmed et al 4 stated that “a<br />
qualitative assessment of the cartilaginous<br />
cap was more helpful than a<br />
precise measurement of cap thickness.”<br />
Irregularity of the surface of<br />
the cartilage cap correlated with the<br />
fuzzy appearance of the lesions on<br />
radiographs; this irregularity may reflect<br />
an increased invasive nature of<br />
the lesion.<br />
Pathology<br />
The diagnosis of secondary chondrosarcoma<br />
is confirmed by histologic<br />
examination of biopsy samples. Like<br />
conventional chondrosarcoma, secondary<br />
chondrosarcoma is not always<br />
easy to diagnose, and the histologic<br />
features alone may not be<br />
sufficient to determine that a lesion<br />
has become malignant. Most secondary<br />
chondrosarcomas are low grade.<br />
The overlap in appearance between<br />
benign lesions and low-grade cartilage<br />
tumors has led to a high rate of<br />
inter- and intraobserver variability in<br />
diagnosis. 24 Critical information<br />
from the clinical history and imaging<br />
studies must be correlated with the<br />
pathologic data to render the correct<br />
diagnosis.<br />
On the pathology slides, sarcomatous<br />
transformation is usually identified<br />
by the presence of malignant<br />
chondroid tissue. Hallmarks include<br />
hypercellularity, binucleate cells,<br />
multiple cells in lacunae, atypical nuclei,<br />
and myxoid changes in the hyaline<br />
cartilage matrix (Figure 2).<br />
Thickening of the cartilage cap can<br />
be observed grossly. 23<br />
A few abnormal features may<br />
make it difficult to distinguish the<br />
cartilage of osteochondromas from<br />
low-grade chondrosarcomas on the<br />
basis of histologic findings alone,<br />
even for experienced pathologists. 25,26<br />
There may be mild nuclear atypia,<br />
slight hypercellularity, and occasional<br />
binucleate cells. In these cases,<br />
the radiographic and clinical findings<br />
are important. 27 A lesion with a thin<br />
cartilage cap that has not grown or<br />
changed for years is unlikely to have<br />
transformed into a malignant tumor.<br />
Conversely, sudden growth in a cap<br />
with marked enlargement of the cap<br />
strongly suggests the presence of<br />
chondrosarcoma, even when the histologic<br />
findings show minimal abnormalities<br />
that would be compatible<br />
only with a diagnosis of grade 1<br />
chondrosarcoma (low grade).<br />
An important feature consistent<br />
with malignancy is permeative infiltration<br />
of soft tissues and the presence<br />
of discrete nodules of cartilage<br />
in the soft tissues separated from the<br />
main tumor mass. In one study, 57%<br />
of all cases of secondary chondrosarcoma<br />
showed histologic evidence of<br />
such permeative changes on the pathology<br />
slides. 4 Medullary extension<br />
of cartilaginous tumor into bone also<br />
demonstrates invasive and malignant<br />
behavior. This may be found in up to<br />
one third of cases, and it tends to be<br />
more common in broad-based osteochondromas.<br />
13<br />
The grading of secondary chondrosarcomas<br />
is similar to that of primary<br />
chondrosarcomas and includes<br />
grade 1, low; grade 2, intermediate;<br />
and grade 3, high. 14,28 In general, increasing<br />
grade is associated with<br />
greater cellularity, number of binucleate<br />
cells, and mitoses.<br />
Most secondary chondrosarcomas<br />
are grade 1 or 2 lesions. In the pub-<br />
October 2010, Vol 18, No 10 611
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
lished data of the large series that we<br />
reviewed, more than three fourths of<br />
the cases were grade 1 tumors, and<br />
nearly all of the remaining lesions<br />
were grade 2. 4,5,7,11,13 Only 1% of<br />
cases were reported to be grade 3.<br />
Figure 2<br />
Genetics and Mutations<br />
Histologic comparison of osteochondroma and secondary chondrosarcoma.<br />
A, Cartilaginous tissue of an osteochondroma demonstrating features that<br />
recapitulate the hyaline cartilage of articular surfaces. Note the gradual<br />
enlargement of cells as they near the subchondral bone and become<br />
hypertrophic. Most cells reside in solitary lacunae, with occasional lacunae<br />
having two cells (arrowhead). The cells are relatively sparse in the abundant<br />
extracellular matrix (hematoxylin-eosin, original magnification ×40). B, Grade<br />
2 secondary chondrosarcoma demonstrating greater cellularity and less<br />
discernible organization of the chondrocytes. Lacunae with multiple cells are<br />
more common. Because cells retract from the walls of the lacunae during the<br />
fixation process, pleomorphism of cells is not easy to identify (hematoxylineosin,<br />
original magnification ×20). C, Osteochondroma under high-power<br />
magnification demonstrating cells that are fairly well-spaced in their lacunae.<br />
Slight atypia may be visible, making the distinction between benign lesions<br />
and low-grade chondrosarcoma difficult on the basis of histology alone.<br />
Certain lacunae contain two cells (hematoxylin-eosin, original magnification<br />
×400). D, Grade 1 secondary chondrosarcoma under high-power<br />
magnification demonstrating atypical features, such as the binucleate cell in<br />
the center of the field. No significant nuclear pleomorphism is present<br />
(hematoxylin-eosin, original magnification ×400).<br />
Hereditary multiple exostosis<br />
(HME), also referred to as multiple<br />
hereditary exostosis and hereditary<br />
multiple osteochondromatosis, is a<br />
rare familial disease characterized by<br />
multiple osteochondromas throughout<br />
the skeleton. The disease is inherited<br />
as an autosomal dominant condition<br />
with high penetrance. Three<br />
related genes have been implicated in<br />
the disorder, EXT1, EXT2, and<br />
EXT3, which are located on 8q24,<br />
11p13, and 19p, respectively. 29-31<br />
EXT1 and EXT2 mutations are<br />
more common and make up most<br />
cases. 32 Patients with EXT1 mutation<br />
tend to have more severe phenotypes<br />
than do patients with EXT2<br />
mutation. 32 It is not clear how the<br />
EXT genes are related to the pathophysiology<br />
of osteochondromas.<br />
Mutation of the genes usually results<br />
in truncated forms of the proteins,<br />
which are needed for the synthesis of<br />
heparan sulfate. This may secondarily<br />
impair diffusion of cellsignaling<br />
molecules. 33<br />
A genetic model for cartilaginous<br />
tumorigenesis in the setting of HME<br />
has been proposed. 34 First, inactivation<br />
of both copies of the EXT1 gene<br />
in cartilage cells is essential for the<br />
formation of osteochondroma. This<br />
typically occurs via loss of heterozygosity<br />
in sporadic cells. Cells that<br />
maintain one normal copy of the<br />
gene are apparently normal. Of note,<br />
it appears that solitary osteochondromas<br />
also develop as a result of<br />
mutation of both copies of an EXT<br />
gene, the difference being that this<br />
occurs in isolated cells and no germline<br />
mutation is inherited. Without<br />
further mutations in other genes, the<br />
lesion remains benign; most osteochondromas<br />
remain in this state and<br />
do not progress further. One or more<br />
additional mutations in other genes<br />
612 Journal of the American Academy of Orthopaedic Surgeons
is required for secondary chondrosarcomas<br />
to arise within the benign<br />
cartilaginous origin. This process is<br />
sometimes accompanied by chromosomal<br />
instability and aneuploidy, the<br />
severity of which may depend on the<br />
particular genes that are mutated.<br />
These have not been well characterized.<br />
Most secondary chondrosarcomas<br />
arise in osteochondromas; thus, it<br />
seems as though the model of tumorigenesis<br />
starting with mutation of<br />
EXT genes would apply to most of<br />
the tumors. However, this may not<br />
account for all secondary chondrosarcomas,<br />
and the genetic pathway<br />
may well be distinct in chondrosarcomas<br />
that arise in enchondromas.<br />
Ollier disease and Maffucci syndrome<br />
are characterized by multiple<br />
enchondromas dispersed through the<br />
skeleton. Maffucci syndrome is distinguished<br />
from Ollier disease by the<br />
presence of multiple soft-tissue hemangiomas,<br />
and it is less common<br />
than Ollier disease. Both diseases are<br />
known to give rise to secondary<br />
chondrosarcoma, but because of the<br />
rarity of the conditions, the rate at<br />
which malignant transformation occurs<br />
is not well-documented. Estimates<br />
range from 10% to 40% in<br />
patients with Ollier disease at longterm<br />
follow-up. 9,11,35 Some authors<br />
believe that patients with Maffucci<br />
syndrome may be at greater risk of<br />
developing malignancy; in one series,<br />
4 of 7 patients with Maffucci syndrome<br />
developed chondrosarcoma. 35<br />
However, reviews of published case<br />
reports have indicated estimates approximately<br />
15% to 20%. 12,36<br />
The genetics of Ollier disease and<br />
Maffucci syndrome differ from those<br />
of HME. Both diseases seem to arise<br />
sporadically without an obvious genetic<br />
inheritance pattern. It is believed<br />
that a combination of multiple<br />
genes may be involved, but those<br />
have not been identified. One report<br />
identified two cases of a mutation<br />
(one somatic, one germline) in the<br />
gene encoding the PTH/PTHrP type I<br />
receptor. 37 It was hypothesized that<br />
the mutation could delay the differentiation<br />
of proliferating chondrocytes<br />
by constitutively activating<br />
hedgehog signaling. However, this<br />
mutation was not found consistently<br />
in other tumors upon further study. 38<br />
Prevention, Treatment,<br />
and Outcome<br />
The risk of malignant transformation<br />
of benign cartilage tumors has not been<br />
well established, and estimates vary<br />
widely. For solitary osteochondromas,<br />
the risk is most likely 5-year<br />
follow-up. 5,7,13 Patients with solitary<br />
osteochondromas tend to have a better<br />
overall prognosis, with a 5-year<br />
mortality rate of 6.5%, compared<br />
with 19.6% for patients with HME. 7<br />
Metastasis may be more apt to occur<br />
in the rare high-grade secondary<br />
chondrosarcoma. 7<br />
October 2010, Vol 18, No 10 613
<strong>Secondary</strong> <strong>Chondrosarcoma</strong><br />
Local recurrence is a significant<br />
problem for patients with secondary<br />
chondrosarcoma, and this may affect<br />
10% to 20% of patients. 4,5,13 Local<br />
control of disease is particularly important<br />
for patients with pelvic and<br />
centrally located disease. In one series,<br />
more deaths occurred from local<br />
recurrence than from distant metastasis.<br />
4 The ramifications of local recurrence<br />
on the patient’s chances for<br />
survival should not be underestimated.<br />
Local recurrence of conventional,<br />
primary low-grade chondrosarcoma<br />
has been associated with<br />
decreased survival, increased metastasis,<br />
and increased grade of tumor.<br />
44,45 Thus, an oncologically<br />
sound operation for the primary tumor<br />
with wide surgical margins is of<br />
critical importance to maximize the<br />
chances for long-term patient survival.<br />
Summary<br />
<strong>Secondary</strong> chondrosarcoma is an uncommon<br />
tumor that arises from a<br />
benign cartilaginous lesion. The tumor<br />
frequently develops in the context<br />
of a syndrome that produces<br />
multiple cartilaginous tumors, including<br />
HME, Ollier disease, and<br />
Maffucci syndrome. It appears most<br />
commonly in the pelvis and proximal<br />
femur. Several signs may alert the clinician<br />
to the possibility of malignant<br />
transformation, such as new onset of<br />
pain, sudden growth of a lesion, and<br />
radiographic changes.<br />
The size of the cartilage cap of an<br />
osteochondroma is important. MRI<br />
with gadolinium contrast may help<br />
define the thickness of the cap. Although<br />
no demarcation in size of the<br />
cap can be considered diagnostic of<br />
malignant transformation, a cap<br />
thickness of >1 cm is worrisome,<br />
particularly when there is documented<br />
growth of the cap.<br />
The overall prognosis for patients<br />
is good. Most tumors are low grade,<br />
and distant metastasis is uncommon.<br />
<strong>Secondary</strong> chondrosarcomas must be<br />
distinguished from dedifferentiated<br />
chondrosarcomas, which are very<br />
aggressive, high-grade tumors with a<br />
poor prognosis. The management of<br />
secondary chondrosarcoma relies<br />
chiefly on wide surgical excision. Inadequate<br />
surgical resection can lead<br />
to uncontrollable local recurrence,<br />
which is perhaps as likely a cause of<br />
demise as distant metastasis.<br />
References<br />
Evidence-based Medicine: Levels of<br />
evidence are described in the table of<br />
contents. In this article, references<br />
23, 30, 31, 33, 34, 37, and 38 are<br />
level III studies. References 2-18, 27-<br />
29, 32, 35, 39-42, 44, and 45 are<br />
level IV studies. References 1, 19-21,<br />
24-26, 36, and 43 are level V expert<br />
opinion.<br />
Citation numbers printed in bold<br />
type indicate references published<br />
within the past 5 years.<br />
1. Unni KK: <strong>Chondrosarcoma</strong> (primary,<br />
secondary, dedifferentiated, and clear<br />
cell), in Dahlin’s Bone Tumors: General<br />
Aspects and Data on 11,087 Cases, ed5.<br />
Philadelphia, PA, Lippincott-Raven,<br />
1996, pp 71-108.<br />
2. Staals EL, Bacchini P, Mercuri M,<br />
Bertoni F: Dedifferentiated<br />
chondrosarcomas arising in preexisting<br />
osteochondromas. J Bone Joint Surg Am<br />
2007;89(5):987-993.<br />
3. Staals EL, Bacchini P, Bertoni F:<br />
Dedifferentiated central<br />
chondrosarcoma. Cancer 2006;106(12):<br />
2682-2691.<br />
4. Ahmed AR, Tan TS, Unni KK, Collins<br />
MS, Wenger DE, Sim FH: <strong>Secondary</strong><br />
chondrosarcoma in osteochondroma:<br />
Report of 107 patients. Clin Orthop<br />
Relat Res 2003;411:193-206.<br />
5. Altay M, Bayrakci K, Yildiz Y, Erekul S,<br />
Saglik Y: <strong>Secondary</strong> chondrosarcoma in<br />
cartilage bone tumors: Report of 32<br />
patients. J Orthop Sci 2007;12(5):415-<br />
423.<br />
6. Coley BL, Higinbotham NL: <strong>Secondary</strong><br />
chondrosarcoma. Ann Surg 1954;139(5):<br />
547-559.<br />
7. Garrison RC, Unni KK, McLeod RA,<br />
Pritchard DJ, Dahlin DC: <strong>Chondrosarcoma</strong><br />
arising in osteochondroma.<br />
Cancer 1982;49(9):1890-1897.<br />
8. Hudson TM, Springfield DS, Spanier SS,<br />
Enneking WF, Hamlin DJ: Benign<br />
exostoses and exostotic chondrosarcomas:<br />
Evaluation of cartilage<br />
thickness by CT. Radiology 1984;152(3):<br />
595-599.<br />
9. Liu J, Hudkins PG, Swee RG, Unni KK:<br />
Bone sarcomas associated with Ollier’s<br />
disease. Cancer 1987;59(7):1376-1385.<br />
10. Merchan EC, Sanchez-Herrera S,<br />
Gonzalez JM: <strong>Secondary</strong> chondrosarcoma:<br />
Four cases and review of the<br />
literature. Acta Orthop Belg 1993;59(1):<br />
76-80.<br />
11. Schaison F, Anract P, Coste F, De<br />
Pinieux G, Forest M, Tomeno B:<br />
<strong>Chondrosarcoma</strong> secondary to multiple<br />
cartilage diseases: Study of 29 clinical<br />
cases and review of the literature<br />
[French]. Rev Chir Orthop Reparatrice<br />
Appar Mot 1999;85(8):834-845.<br />
12. Sun TC, Swee RG, Shives TC, Unni KK:<br />
<strong>Chondrosarcoma</strong> in Maffucci’s<br />
syndrome. J Bone Joint Surg Am 1985;<br />
67(8):1214-1219.<br />
13. Wuisman PI, Jutte PC, Ozaki T:<br />
<strong>Secondary</strong> chondrosarcoma in<br />
osteochondromas: Medullary extension<br />
in 15 of 45 cases. Acta Orthop Scand<br />
1997;68(4):396-400.<br />
14. Evans HL, Ayala AG, Romsdahl MM:<br />
Prognostic factors in chondrosarcoma of<br />
bone: A clinicopathologic analysis with<br />
emphasis on histologic grading. Cancer<br />
1977;40(2):818-831.<br />
15. Atalar H, Başarir K, Uraş I, Yildiz Y,<br />
Erekul S, Sağlik Y: Chondromyxoid<br />
fibroma: An evaluation of 11 patients<br />
[Turkish]. Acta Orthop Traumatol Turc<br />
2007;41(1):31-35.<br />
16. Müller PE, Dürr HR, Nerlich A,<br />
Pellengahr C, Maier M, Jansson V:<br />
Malignant transformation of a benign<br />
enchondroma of the hand to secondary<br />
chondrosarcoma with isolated<br />
pulmonary metastasis. Acta Chir Belg<br />
2004;104(3):341-344.<br />
17. Peiper M, Zornig C: <strong>Chondrosarcoma</strong> of<br />
the thumb arising from a solitary<br />
enchondroma. Arch Orthop Trauma<br />
Surg 1997;116(4):246-248.<br />
18. Springfield DS, Gebhardt MC, McGuire<br />
MH: <strong>Chondrosarcoma</strong>: A review. Instr<br />
Course Lect 1996;45:417-424.<br />
19. Sah AP, Geller DS, Mankin HJ, et al:<br />
Malignant transformation of synovial<br />
chondromatosis of the shoulder to<br />
chondrosarcoma: A case report. J Bone<br />
Joint Surg Am 2007;89(6):1321-1328.<br />
20. Bertoni F, Bacchini P, Hogendoorn PC:<br />
614 Journal of the American Academy of Orthopaedic Surgeons
Patrick P. Lin, MD, et al<br />
<strong>Chondrosarcoma</strong>, in Fletcher CDM,<br />
Unni KK, Mertens F, eds: World Health<br />
Organization Classification of Tumours:<br />
Pathology & Genetics: Tumours of Soft<br />
Tissue and Bone. Lyon, France, IARC<br />
Press, 2002, pp 247-251.<br />
21. Huvos AG: Solitary and multiple<br />
osteochondromas and enchondromas,<br />
juxtacortical chondroma, Mafucci’s<br />
disease, in Huvos AG, ed: Bone Tumors:<br />
Diagnosis, Treatment and Prognosis.<br />
Philadelphia, PA, WB Saunders<br />
Company, 1991, pp 253-294.<br />
22. Spjut HJ, Dorfman HD, Fechner RE,<br />
Ackerman LV: Tumors of cartilaginous<br />
origin, in Firminger HI, ed: Atlas of<br />
Tumor Pathology, Second Series, Fascicle<br />
5: Tumors of Bone and Cartilage.<br />
Washington, DC, Armed Forces Institute<br />
of Pathology, 1971, pp 33-116.<br />
23. Forest M: Osteochondroma, in Forest<br />
M, Tomeno B, Vanel D, eds: Orthopedic<br />
Surgical Pathology: Diagnosis of Tumors<br />
and Pseudotumoral Lesions of Bone and<br />
Joints. Edinburgh, Scotland, Churchill<br />
Livingstone, 1998, pp 117-190.<br />
24. Eefting D, Schrage YM, Geirnaerdt MJ,<br />
et al: Assessment of interobserver<br />
variability and histologic parameters to<br />
improve reliability in classification and<br />
grading of central cartilaginous tumors.<br />
Am J Surg Pathol 2009;33(1):50-57.<br />
25. Flemming DJ, Murphey MD:<br />
Enchondroma and chondrosarcoma.<br />
Semin Musculoskelet Radiol 2000;4(1):<br />
59-71.<br />
26. Campanacci M: Multiple chondromas<br />
(chondromatosis, Ollier’s disease,<br />
Maffucci’s syndrome), in Campanacci<br />
M: Bone and Soft Tissue Tumors, ed2.<br />
New York, NY, Springer, 1999, pp 235-<br />
245.<br />
27. Mirra JM: The osteochondroma, solitary<br />
and multiple, in Mirra JM, ed: Bone<br />
Tumors: Diagnosis and Treatment.<br />
Philadelphia, PA, JB Lippincott, 1980,<br />
pp 520-532.<br />
28. O’Neal LW, Ackerman LV: <strong>Chondrosarcoma</strong><br />
of bone. Cancer 1952;5(3):551-<br />
577.<br />
29. Cook A, Raskind W, Blanton SH, et al:<br />
Genetic heterogeneity in families with<br />
hereditary multiple exostoses. Am J Hum<br />
Genet 1993;53(1):71-79.<br />
30. Wu YQ, Heutink P, de Vries BB, et al:<br />
Assignment of a second locus for<br />
multiple exostoses to the pericentromeric<br />
region of chromosome 11. Hum Mol<br />
Genet 1994;3(1):167-171.<br />
31. Le Merrer M, Legeai-Mallet L, Jeannin<br />
PM, et al: A gene for hereditary multiple<br />
exostoses maps to chromosome 19p.<br />
Hum Mol Genet 1994;3(5):717-722.<br />
32. Porter DE, Lonie L, Fraser M, et al:<br />
Severity of disease and risk of malignant<br />
change in hereditary multiple exostoses:<br />
A genotype-phenotype study. J Bone<br />
Joint Surg Br 2004;86(7):1041-1046.<br />
33. Wuyts W, Van Hul W, De Boulle K,<br />
et al: Mutations in the EXT1 and EXT2<br />
genes in hereditary multiple exostoses.<br />
Am J Hum Genet 1998;62(2):346-354.<br />
34. Bovée JV, Cleton-Jansen AM, Wuyts W,<br />
et al: EXT-mutation analysis and loss of<br />
heterozygosity in sporadic and hereditary<br />
osteochondromas and secondary<br />
chondrosarcomas. Am J Hum Genet<br />
1999;65(3):689-698.<br />
35. Schwartz HS, Zimmerman NB, Simon<br />
MA, Wroble RR, Millar EA, Bonfiglio<br />
M: The malignant potential of<br />
enchondromatosis. J Bone Joint Surg Am<br />
1987;69(2):269-274.<br />
36. Lewis RJ, Ketcham AS: Maffucci’s<br />
syndrome: Functional and neoplastic<br />
significance. Case report and review of<br />
the literature. J Bone Joint Surg Am<br />
1973;55(7):1465-1479.<br />
37. Hopyan S, Gokgoz N, Poon R, et al: A<br />
mutant PTH/PTHrP type I receptor in<br />
enchondromatosis. Nat Genet 2002;<br />
30(3):306-310.<br />
38. Rozeman LB, Sangiorgi L, Briaire-de<br />
Bruijn IH, et al: Enchondromatosis<br />
(Ollier disease, Maffucci syndrome) is<br />
not caused by the PTHR1 mutation<br />
p.R150C. Hum Mutat 2004;24(6):466-<br />
473.<br />
39. Florez B, Mönckeberg J, Castillo G,<br />
Beguiristain J: Solitary osteochondroma<br />
long-term follow-up. J Pediatr Orthop B<br />
2008;17(2):91-94.<br />
40. Schmale GA, Conrad EU III, Raskind<br />
WH: The natural history of hereditary<br />
multiple exostoses. J Bone Joint Surg Am<br />
1994;76(7):986-992.<br />
41. Wicklund CL, Pauli RM, Johnston D,<br />
Hecht JT: Natural history study of<br />
hereditary multiple exostoses. Am J Med<br />
Genet 1995;55(1):43-46.<br />
42. Murphey MD, Choi JJ, Kransdorf MJ,<br />
Flemming DJ, Gannon FH: Imaging of<br />
osteochondroma: Variants and<br />
complications with radiologic-pathologic<br />
correlation. Radiographics 2000;20(5):<br />
1407-1434.<br />
43. Pierz KA, Womer RB, Dormans JP:<br />
Pediatric bone tumors: Osteosarcoma<br />
ewing’s sarcoma, and chondrosarcoma<br />
associated with multiple hereditary<br />
osteochondromatosis. J Pediatr Orthop<br />
2001;21(3):412-418.<br />
44. Schwab JH, Wenger D, Unni K, Sim FH:<br />
Does local recurrence impact survival in<br />
low-grade chondrosarcoma of the long<br />
bones? Clin Orthop Relat Res 2007;462:<br />
175-180.<br />
45. Weber KL, Pring ME, Sim FH:<br />
Treatment and outcome of recurrent<br />
pelvic chondrosarcoma. Clin Orthop<br />
Relat Res 2002;397:19-28.<br />
October 2010, Vol 18, No 10 615