Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>CHOATE</strong><br />
<strong>ROSEMARY</strong> <strong>HALL</strong><br />
DOMESTIC AND<br />
INTERNATIONAL STUDENT<br />
ACCIDENT AND SICKNESS<br />
INSURANCE PLAN<br />
2012-2013<br />
Policy Number: 2012I5A18<br />
1. This Brochure is not the insurance contract. It is a brief<br />
description of the general provisions provided under Master<br />
Policy issued to Choate Rosemary Hall and underwritten by<br />
Niagara Life and Health Insurance Company.<br />
2. Please be sure to retain this brochure as a record of your<br />
insurance benefits. No individual policies are issued. An<br />
identification card will be issued to each insured person after<br />
October 15, 2012, the Waiver deadline.<br />
THIS POLICY MEETS CONNECTICUT MINIMUM STANDARDS<br />
FOR BASIC MEDICAL/SURGICAL EXPENSE INSURANCE. IT<br />
ALSO CONTAINS ADDITIONAL BENEFITS. PLEASE READ THIS<br />
BROCHURE CAREFULLY.<br />
THIS LIMITED HEALTH BENEFITS PLAN (PLAN A) DOES NOT<br />
PROVIDE COMPREHENSVE MEDICAL COVERAGE. IT IS A<br />
BASIC OR LIMITED BENEFITS POLICY AND IS NOT INTENDED<br />
TO COVER ALL MEDICAL EXPENSES. THIS PLAN IS NOT<br />
DESIGNED TO COVER THE COSTS OF SERIOUS OR<br />
CHRONIC ILLNESS. IT CONTAINS SPECIFIC DOLLAR LIMITS<br />
THAT WILL BE PAID FOR MEDICAL SERVICES WHICH MAY<br />
NOT BE EXCEEDED. IF THE COST OF SERVICES EXCEEDS<br />
THOSE LIMITS, THE BENEFICIARY AND NOT THE INSURER IS<br />
RESPONSIBLE FOR PAYMENT OF THE EXCESS AMOUNTS.<br />
THE SPECIFIC DOLLAR LIMITS ARE AS FOLLOWS IN THE<br />
PLAN BENEFIT SECTION.<br />
Form #12-I5A18(bro/cert)<br />
ELIGIBILITY<br />
All students attending the school on a full-time basis are eligible<br />
to enroll in this Plan. This coverage is available to Domestic and<br />
International Students that travel abroad while the policy is in<br />
force.<br />
The Company maintains the right to investigate student status<br />
and attendance records to verify that Policy eligibility<br />
requirements have been met. If the Company discovers that the<br />
Policy eligibility requirements have not been met, the<br />
Company’s only obligation is refund of premium.<br />
POLICY TERM<br />
The insurance under Choate Rosemary Hall’s Student Accident<br />
and Sickness Insurance Plan for the Annual Plan is effective<br />
12:01 a.m. on September 1, 2012. You may enroll in this<br />
Insurance Program prior to the start of the School Year, or<br />
during the forty-five (45) day period beginning with the start of<br />
the first semester. This is known as the Open Enrollment<br />
Period. The Annual Plan terminates at 12:01 a.m. on<br />
September 1, 2013 or at the end of the period for which the<br />
premiums are paid.<br />
COST OF COVERAGE<br />
DOMESTIC AND INTERNATIONAL<br />
Plan A: Annual Premium (12 months) ......................... $240*<br />
Domestic Only<br />
Plan B: Accident & Sickness Insurance Plan<br />
(12 months) .................................................................. $979*<br />
Domestic & International Students – International Students are<br />
required to enroll in Plan B<br />
*Plans A and B include a $10.00 administration fee.<br />
REFUND OF PREMIUM<br />
Except for medical withdrawal due to a covered Injury or<br />
Sickness, any student withdrawing from school during the first<br />
31 days of the period for which coverage is purchased will not<br />
be covered under the Policy and a full refund of the premium<br />
will be made. Students withdrawing after such 31 days will<br />
remain covered under the Policy for the full period for which<br />
premium has been paid and no refund will be allowed.<br />
Covered Persons entering the armed forces of any country will<br />
not be covered under the Policy as of the date of such entry. A<br />
pro-rata refund of premium will be made for such person upon<br />
written request received by the Company within 90 days of<br />
withdrawal from school. Refunds for any other reason are not<br />
available.<br />
DEFINITIONS<br />
You, Your or Yours means the insured student.<br />
We, Us or Our means Niagara Life and Health Insurance<br />
Company.<br />
Accident means a sudden, unexpected and unforeseen,<br />
identifiable event causing Injury.<br />
Aggregate Maximum Benefit means the Maximum benefit We<br />
will pay for any one covered Injury or Sickness.<br />
Covered Person means You, the Student while insured under<br />
this Plan.<br />
Physician as used herein means: (a) a legally qualified<br />
physician licensed by the state in which he or she practices; or<br />
(b) a practitioner of the healing arts performing services within<br />
the scope of his or her license as specified by the laws of the<br />
state or residence of such practitioner; or (c) a certified nurse<br />
midwife while acting within the scope of that certification; or (d)<br />
a certified nurse practitioner, which means any registered nurse<br />
licensed in the state in which he or she practices who has<br />
completed a formal educational nurse practitioner program and is<br />
certified by the respective professional nursing association; or (e)<br />
a physician assistant performing services within the scope of his<br />
or her license as specified by the laws of the state of residence of<br />
such practitioner.<br />
Hospital means a facility which meets all of these tests: (a) it<br />
provides inpatient services for the care and treatment of injured<br />
and sick people; and (b) it provides room and board services and<br />
nursing services 24 hours a day; and (c) it has established<br />
facilities for diagnosis and major surgery; and (d) it is supervised<br />
by a Physician; and (e) it is run as a Hospital under the laws of the<br />
jurisdiction in which it is located. Hospital does not include a place<br />
run mainly: (a) for alcoholics or drug addicts; (b) as a<br />
convalescent home; (c) as a nursing or rest home; or (d) as a<br />
hospice facility.<br />
Hospital Confined/Confinement means a stay of 18 or more<br />
consecutive hours as a resident bed-patient in a Hospital.<br />
Loss means medical expense covered by this Plan as a result of<br />
Injury or Sickness as defined in this Plan.<br />
Injury means bodily Injury due to an Accident, which is the sole<br />
cause of the Loss and results solely, directly and independently of<br />
disease, bodily infirmity or any other causes. All injuries sustained<br />
2 3
in any one Accident, including all related conditions and recurrent<br />
symptoms of these injuries are considered a single injury.<br />
Sickness means Illness, disease, and complications of<br />
pregnancy which is the sole cause of the Loss which begin after<br />
the effective date of a Covered Person’s coverage, which are not<br />
a Pre-Existing Condition. All related conditions and recurrent<br />
symptoms of the same or a similar condition will be considered<br />
the same Sickness.<br />
Medical Emergency means the unexpected onset of an Injury or<br />
Sickness which requires immediate or urgent medical attention<br />
which, if not provided, could result in a loss of life or serious<br />
permanent damage to a limb or organ or pain sufficient to warrant<br />
immediate care. A Medical Emergency does not include elective<br />
or routine care.<br />
Medically Necessary means Health care services that a physician,<br />
exercising prudent clinical judgment, would provide to a patient for<br />
the purpose of preventing, evaluating, diagnosing or treating an<br />
illness, injury, disease or its symptoms, and that are: (1) In<br />
accordance with generally accepted standards of medical<br />
practice; (2) clinically appropriate, in terms of type, frequency,<br />
extent, site and duration and considered effective for the<br />
patient's illness, injury or disease; and (3) not primarily for the<br />
convenience of the patient, physician or other health care<br />
provider and not more costly than an alternative service or<br />
sequence of services at least as likely to produce equivalent<br />
therapeutic or diagnostic results as to the diagnosis or<br />
treatment of that patient's illness, injury or disease. For the<br />
purposes of this section, "generally accepted standards of<br />
medical practice" means standards that are based on credible<br />
scientific evidence published in peer-reviewed medical literature<br />
generally recognized by the relevant medical community or<br />
otherwise consistent with the standards set forth in policy<br />
issues involving clinical judgment.<br />
Expense or Covered Charge as used herein means those<br />
charges for Medically Necessary treatment, services or supplies<br />
which are performed or given under the direction of a Physician<br />
which are: (a) not in excess of the charges of the Reasonable and<br />
Customary Expenses therefore; and (b) not in excess of the<br />
charges that would have been made in the absence of this<br />
insurance; and (c) incurred while this Plan is in force as to the<br />
Covered Person.<br />
Reasonable and Customary Charge (R&C) means the usual<br />
amount charged by a Provider for a service or supply, regardless of<br />
insurance coverage, but not more than the amount charged by most<br />
providers in the same area for a similar service.<br />
Pre-existing Condition means a Sickness or Injury for which<br />
medical care, treatment, diagnosis, or advice was received or<br />
recommended within the six months prior to the Covered<br />
Person’s effective date of coverage under the Plan. Routine<br />
follow-up care to determine whether breast cancer has reoccurred<br />
in a person who has been previously determined to be breast<br />
cancer free shall not be considered as medical advice, diagnosis,<br />
care or treatment unless evidence of breast cancer is found<br />
during or as a result of such follow-up. Genetic information shall<br />
not be treated as a condition in the absence of a diagnosis of the<br />
condition related to such information. Pregnancy shall not be<br />
considered as a Pre-Existing Condition.<br />
DESCRIPTION OF BENEFITS<br />
ACCIDENT AND SICKNESS INSURANCE PLAN<br />
DOMESTIC STUDENTS - PLAN A<br />
Plan A is designed for students whose current medical<br />
insurance has a high deductible. This insurance plan provides<br />
coverage from the first dollar of Covered Charges, at 100% of R<br />
& C Charges, up to a maximum of $5,000 per Policy Year.<br />
Accidental Dental Expense Benefit: for Dental treatment as a<br />
result of accidental Injury to sound natural teeth up to a<br />
maximum of $100 per Accident.<br />
Ambulance Expense: Up to the maximum allowable rate<br />
established by the Department of Public Health in accordance<br />
with 19a-177, as amended for Medically Necessary transportation<br />
service to or from a Hospital by an ambulance. This includes<br />
emergency transportation from the place of a covered accident to<br />
a hospital providing the necessary medical care.<br />
DOMESTIC AND INTERNATIONAL STUDENTS - PLAN B<br />
Plan B is designed for those students who have no family<br />
medical insurance. International students are required to enroll<br />
in this plan. This student plan provides coverage from the first<br />
dollar of Covered Charges, at 100% of R & C Charges, up to a<br />
maximum of $200,000 per Injury or Sickness.<br />
When a Covered Injury or Sickness requires: (a) treatment by a<br />
Physician/Surgeon; (b) hospital confinement (room and board<br />
expense should not exceed the semi-private room rate); (c)<br />
services of a licensed nurse practitioner or RN; (d) x-ray<br />
services; (e) use of operating room, anesthesia, laboratory<br />
services; (f) prescribed medicines, plaster casts, surgical<br />
dressings and other Reasonable and Customary Charges<br />
incurred for the treatment of a Covered Injury or Sickness, We<br />
will pay 100% of the Covered Charges incurred for a covered<br />
Accident or Sickness, up to a maximum of $200,000 per Injury<br />
or Sickness.<br />
Accidental Dental Expense Benefit: for Dental treatment as a<br />
result of accidental Injury to sound natural teeth up to a<br />
maximum of $650 per Injury.<br />
Ambulance Expense: Up to the maximum allowable rate<br />
established by the Department of Public Health in accordance<br />
with 19a-177, as amended for Medically Necessary transportation<br />
service to or from a Hospital by an ambulance. This includes<br />
emergency transportation from the place of a covered accident to<br />
a hospital providing the necessary medical care.<br />
REPATRIATION OF REMAINS<br />
FOR DOMESTIC AND INTERNATIONAL STUDENTS<br />
The Company will pay the reasonable covered expenses to return<br />
the Insured Person’s body to his or her home country if he or she<br />
dies. Covered expenses include expenses for embalming,<br />
cremation, coffins, and transportation. The benefit payable may not<br />
exceed $5,000.<br />
STATE MANDATED BENEFITS<br />
Mental Health Conditions Expense Benefit: We will pay benefits<br />
for mental health conditions the same as we would pay for any<br />
other sickness. "Mental Health Conditions" means mental<br />
disorders as defined in the most recent edition of the American<br />
Psychiatric Association's "Diagnostic and Statistical Manual of<br />
Mental Disorders".<br />
Mental Disorders include alcohol dependency and substance<br />
abuse, but do not include mental retardation, learning disorders,<br />
motor skills disorders, communication disorders, caffeine-related<br />
disorders, relational problems, and additional conditions that may be<br />
a focus of clinical attention, that are not otherwise defined as mental<br />
disorders in the most recent edition of the American Psychiatric<br />
Association's "Diagnostic and Statistical Manual of Mental<br />
Disorders”.<br />
In the case of benefits payable for the services of a licensed<br />
physician or psychiatrist, benefits are also payable for the same<br />
services when rendered by the following practitioners or facilities<br />
qualified and licensed in accordance with the requirements of<br />
Chapter 38A Section 488A of the Connecticut General Laws:<br />
psychologist, clinical social worker, marital and family therapist,<br />
alcohol and drug counselor, professional counselor, child guidance<br />
clinic, residential treatment facility, or nonprofit community mental<br />
health center.<br />
4 5 6
Inpatient Mental Health Conditions: If an Insured Person requires<br />
treatment for mental and nervous disorders during Hospital<br />
Confinement, We will pay the Reasonable and Customary Charge<br />
incurred on the same basis as any other Sickness.<br />
Benefits for Partial Hospitalization: Partial Hospitalization means<br />
continuous treatment consisting of not less than four hours and not<br />
more than twelve hours in any twenty-four hour period under a<br />
program based in a hospital or residential treatment facility. Two<br />
Partial Hospitalization days may be substituted for one inpatient day<br />
in a hospital or related institution.<br />
Outpatient Mental & Nervous Conditions: When the Insured<br />
Person is not hospital confined, We will pay the Reasonable and<br />
Customary Charge incurred for Outpatient Services as any other<br />
illness.<br />
Autism Spectrum Disorder Therapies: We will provide coverage<br />
for physical therapy, speech therapy and occupational therapy<br />
services for the treatment of Autism Spectrum Disorders as set forth<br />
in the most recent edition of the American Psychiatric Association’s<br />
“Diagnostic and Statistical Manual of Mental Disorders,” to the<br />
extent such services are a covered benefit for other diseases and<br />
conditions under the policy.<br />
Epidermolysis Bullosa Treatment: We will provide coverage for<br />
wound care supplies that are medically necessary for the treatment<br />
of epidermolysis bullosa and are administered under the direction of<br />
a physician.<br />
Maternity Coverage: Normal pregnancy, complications of<br />
pregnancy, resulting childbirth, miscarriage or termination of<br />
pregnancy (except for elective abortion) on the same basis as a<br />
covered Sickness. Coverage includes a minimum inpatient stay<br />
of 48 hours for a vaginal delivery and 96 hours for a caesarean<br />
delivery. If the mother and newborn are discharged prior to this<br />
timeframe, after consultation with the Physician, this Plan will<br />
cover 2 follow up visits. The first visit must be within 48 hours of<br />
discharge and the second visit within 7 days.<br />
Newborn Children: A child of the insured Student will be<br />
covered by the Policy for 31 days after the moment of birth.<br />
Coverage for a newborn child will be the same as for any other<br />
Insured Person. Coverage will include Medically Necessary<br />
care or treatment of congenital defects, birth abnormalities, or<br />
premature birth. Upon expiration of the 31 days, dependent<br />
coverage is not available under the policy.<br />
Infertility Treatment Benefits: We will pay the medically<br />
necessary expenses incurred in the diagnosis and treatment of<br />
infertility. Such treatment includes, but is not limited to the<br />
following services related to infertility:<br />
1. ovulation induction;<br />
2. intra-uterine insemination;<br />
3. in-vitro fertilization<br />
4. uterine embryo lavage;<br />
5. embryo transfer;<br />
6. gamete intra-fallopian transfer;<br />
7. zygote intra-fallopian transfer; and<br />
8. low tubal ovum transfer.<br />
Coverage under this benefit is limited:<br />
1. to a covered student until the date of the student’s 40 th<br />
birthday;<br />
2. for ovulation induction to a lifetime maximum benefit of 4<br />
cycles;<br />
3. for intrauterine insemination to a lifetime maximum benefit<br />
of 3 cycles;<br />
4. for lifetime benefits to a maximum of 2 cycles, with not<br />
more than 2 embryo implantations per cycle, for IVF,<br />
gamete intra-fallopian transfer, zygote intra-fallopian or low<br />
tubal ovum transfer, provided each such fertilization or<br />
transfer shall be credited toward the maximum as 1 cycle;<br />
5. for IVF, gamete intra-fallopian transfer, zygote intrafallopian<br />
transfer and low tubal ovum transfer, to those<br />
individuals who have been unable to conceive or produce<br />
conception or sustain a successful pregnancy through less<br />
expensive and medically viable infertility treatment or<br />
procedures covered under the policy. Nothing in this<br />
subdivision shall be construed to deny the coverage<br />
required by this section to any individual who foregoes a<br />
particular infertility treatment or procedure if the<br />
individual’s physician determines that such treatment or<br />
procedure is likely to be unsuccessful;<br />
6. to individuals who have maintained coverage under the<br />
policy and any of the schools’ previous policies for at least<br />
12 months.<br />
7. to require disclosure by the student seeking coverage of<br />
any previous fertility treatment or procedures which the<br />
student received under a different health insurance policy.<br />
For the purpose of this benefit, infertility means the condition<br />
of a presumably healthy individual who is unable to conceive or<br />
produce conception or sustain a successful pregnancy during a<br />
one-year period.<br />
Services provided for under this provision must be performed at<br />
facilities that conform to standards and guidelines established<br />
by the American Society of Reproductive Medicine or the<br />
Society of Reproductive Endocrinology and Infertility. The same<br />
co-payments, deductibles and benefit limits will apply to the<br />
diagnosis and treatment of infertility as those applied to other<br />
medical or surgical benefits under the Policy.<br />
Early Intervention Services– When Dependent coverage is<br />
provided under the Policy, we will pay the expenses incurred for<br />
Medically Necessary early intervention services for eligible<br />
Dependent children not to exceed $6,400 per school year.<br />
These benefits are available for Dependent children who are<br />
not eligible for Connecticut special education and related<br />
services and who are from birth to 36 months of age, inclusive.<br />
Such services are needed because a child:<br />
1. Is experiencing a significant developmental delay as<br />
measured by standardized diagnostic instruments and<br />
procedures, including informed clinical opinion, in one or<br />
more of the following areas:<br />
a. Cognitive development;<br />
b. Physical development, including vision and hearing;<br />
c. Communication development;<br />
d. Social or emotional development; or<br />
e. Adaptive skills.<br />
2. Has been diagnosed as having a physical or mental<br />
condition that has a high probability of resulting in<br />
developmental delay.<br />
No payment made under this benefit will be applied against the<br />
Aggregate Maximum Benefit per covered Sickness.<br />
Hearing Aids: We will pay the expenses incurred for the cost<br />
of hearing aids for children 18 years of age and younger. Such<br />
hearing aids will be considered durable medical equipment<br />
under this policy. The maximum benefit payable for any one<br />
child will be limited to $1,000.<br />
Cancer Screening Tests: We will pay for the charges incurred<br />
for the following cancer screening tests.<br />
1. Mammography performed according to following schedule:<br />
a. One or more mammograms per year, as<br />
recommended by a Physician, for any woman at risk<br />
for breast cancer;<br />
b. A baseline mammogram for any woman age 35 to 39,<br />
inclusive, or more frequently if recommended by the<br />
woman’s Physician;<br />
7 8 9
c. A mammogram every year for any woman who is 40<br />
years of age and older; and<br />
d. Comprehensive ultrasound screening of an entire<br />
breast or breasts if such screenings are<br />
recommended by a physician for a woman classified<br />
as category 2, 3, 4 or 5 under the breast Imaging<br />
Reporting and Data System established by the<br />
American College of Radiology.<br />
2. PAP tests for woman 18 years and older as recommended<br />
by a Physician.<br />
3. Prostate cancer screening, including digital rectal<br />
examinations and prostate-specific antigen tests for men<br />
who are symptomatic; whose biological father or brother<br />
has been diagnosed with prostate cancer, and for all men<br />
50 years of age or older.<br />
4. Colorectal Cancer Screening, including but not limited to<br />
an annual fecal occult blood test, and a colonoscopy,<br />
flexible sigmoidoscopy or radiologic imaging, in<br />
accordance with the recommendations established by the<br />
American College of Gastroenterology, after consultation<br />
with the American Cancer Society, based on the ages,<br />
family histories and frequencies provided in the<br />
recommendations.<br />
Home Health Care Expense: Expenses for covered home<br />
health care service in lieu of Hospitalization, except if<br />
diagnosed by a Physician as terminally ill with a prognosis of 6<br />
months or less to live, after a $50 deductible, 75% of the<br />
Expenses incurred, up to a maximum of 80 home health care<br />
visits in any calendar year or in any continuous period of 12<br />
months for each Covered Person. Each 4 hours of home health<br />
aide service will count as one visit. In the case of a terminally ill<br />
Covered Person, no more than $200 for medical social services<br />
for any 12-month period will be paid for covered services.<br />
Accidental Ingestion of Controlled Drugs Expense: Expenses<br />
for a Medical Emergency arising from accidental ingestion or<br />
consumption of a controlled drug limited to:<br />
• Inpatient: While Hospital Confined, Expense incurred, up to<br />
a maximum of 80% of R&C up to 30 days in any calendar<br />
year.<br />
• Outpatient: While not Hospital Confined, Expense paid at<br />
80% of R&C up to a maximum of $500 per calendar year.<br />
Chiropractic Care Expense: Services rendered by a licensed<br />
chiropractor, to the same extent coverage is provided for services<br />
rendered by a Physician, if such chiropractic services (1) treat a<br />
condition covered under this Plan and (2) are within those<br />
services a chiropractor is licensed to perform.<br />
Treatment of Leukemia, Prosthetic Devices, Surgical<br />
Removal of Tumors Expense: Surgical removal of tumors and<br />
treatment of leukemia, including outpatient chemotherapy,<br />
reconstructive surgery, cost of any non-dental prosthesis<br />
including maxillo-facial prosthesis used to replace anatomic<br />
structures lost during treatment for head and neck tumors or<br />
additional appliances essential for the support of such<br />
prosthesis, and outpatient chemotherapy following surgical<br />
procedure in connection with the treatment of tumors. Such<br />
benefits shall be subject to the same terms and conditions<br />
applicable to all other benefits under this Plan. We will pay a<br />
Policy year benefit of: (1) $1,000 each policy year for the costs<br />
of removal of any breast implant; (2) $500 for the surgical<br />
removal of tumors; (3) $500 for reconstructive surgery; (4) $500<br />
for outpatient chemotherapy; and (5) An annual benefit of at<br />
least $350 for a wig and $300 for prosthesis, except that for<br />
purposes of the surgical removal of breast due to tumors, the<br />
policy year benefit shall be at least $300 for each breast.<br />
Hypodermic Needles or Syringes Expense: Physician<br />
prescribed hypodermic needles or syringes for the purpose of<br />
administering medications for medical conditions, provided<br />
such medications are covered under this Plan.<br />
Treatment of Inherited Metabolic Diseases and Medically<br />
Necessary Formulas: We will pay the expenses incurred for<br />
medical foods and low protein modified food products on the same<br />
basis as outpatient prescription drugs for the treatment of inherited<br />
Metabolic Diseases if the medical food or low protein modified food<br />
products are:<br />
a. Prescribed as Medically Necessary for the therapeutic<br />
treatment of inherited metabolic diseases; and<br />
b. Administered under the direction of a Physician.<br />
In so far as this benefit is concerned, the following definitions apply.<br />
Inherited metabolic disease means a disease for which a<br />
newborn screening is required under section 19a-55 (Connecticut),<br />
as amended; and cystic fibrosis<br />
Low Protein Modified Food Product means a food product that is:<br />
a. Specially formulated to have less than 1 gram of protein per<br />
serving; and<br />
b. Intended to be used under the direction of a Physician for<br />
the dietary treatment of an inherited metabolic disease.<br />
Low protein modified food product does NOT include a natural food<br />
that is naturally low in protein.<br />
Amino acid modification preparation means a product intended<br />
for the dietary treatment of an inherited metabolic disease under the<br />
direction of a physician.<br />
Specialized formula means a nutritional formula for children up to<br />
the age twelve (12) that is exempt from the general requirements for<br />
nutritional labeling under the statutory and regulatory guidelines of<br />
the federal Food and Drug Administration and is intended for use<br />
solely under medical supervision in the dietary management of<br />
specific diseases.<br />
Diabetes Treatment Expense: Treatment of insulin-dependent<br />
diabetes, insulin-using diabetes, gestational diabetes and non-<br />
Insulin using diabetes on the same basis as any other Sickness to<br />
include:<br />
1. Medically Necessary equipment, drugs and supplies, when<br />
prescribed by a Doctor.<br />
2. Diabetes outpatient self-management training, including but<br />
not limited to education and medical nutrition therapy.<br />
Benefits shall cover: (a) Initial training visits provided to an<br />
individual after the individual is initially diagnosed with the<br />
diabetes that is medically necessary for the care and<br />
management of diabetes, including but not limited to<br />
counseling in nutrition and the proper use of equipment and<br />
supplies for the treatment of diabetes, totaling a maximum of<br />
ten hours; (b) training and education that is medically<br />
necessary as a result of a subsequent diagnosis by a Doctor<br />
or a significant change in the individual’s symptoms or<br />
condition which requires modification of the individual’s<br />
program of self-management of diabetes, totaling a<br />
maximum of four hours, and (c) training and education that<br />
is medically necessary because of the development of new<br />
techniques and treatment for diabetes totaling a maximum of<br />
four hours.<br />
Treatment of Lyme Disease: We will pay the expenses incurred<br />
for the treatment of Lyme Disease. Such treatment will include:<br />
1. Not less than 30 days of intravenous antibiotic therapy or<br />
sixty days or oral antibiotic, or both, and<br />
2. Further treatment, if recommended by a board certified<br />
rheumatologist, infectious disease specialist or neurologist<br />
who is licensed in accordance with Connecticut statutes or<br />
who is licensed in another state or jurisdiction whose<br />
requirements for practicing in such capacity are substantially<br />
similar to or higher than those of Connecticut.<br />
10 11 12
Mastectomy, Reconstructive Breast Surgery or Lymph Node<br />
Dissection Expense: Benefits for such surgery will be paid under<br />
the Surgery Benefits. Coverage will be provided for at least 48 hours<br />
of inpatient care following a mastectomy or lymph node surgery.<br />
Coverage will be provided for longer periods of inpatient care if it is<br />
recommended by the patient’s treating Physician after conferring<br />
with the patient. We will also provide benefits for the reasonable<br />
costs of reconstructive surgery on each breast on which a<br />
mastectomy has been performed, and reconstructive surgery on a<br />
non-diseased breast to produce a symmetrical appearance. This<br />
benefit is subject to the same terms and conditions applicable to all<br />
other benefits under this Policy.<br />
Occupational Therapy Expense: We will pay a benefit, not to<br />
exceed 80% of Reasonable and Customary Charges, for the<br />
expenses incurred for occupational therapy received by a Covered<br />
Person as the result of a covered Accident.<br />
Care and Treatment of Insured with an Ostomy: We will pay the<br />
expenses for the care and treatment of an Insured who undergoes<br />
ostomy surgery. Such care and treatment includes coverage for<br />
Medically Necessary appliances and supplies relating to an ostomy<br />
including, but not limited to collection devices, irrigation equipment<br />
and supplies, skin barriers and skin protectors. This benefit will be<br />
payable not to exceed $2,500 per school year.<br />
Pain Management Benefit: We will pay the expenses incurred by<br />
a Covered Person for treatment by or under the management of a<br />
pain management specialist if required. We will also pay the<br />
expenses incurred for pain treatment ordered by such specialist.<br />
Such treatment may include all means necessary to make a<br />
diagnosis and develop a treatment Plan including the use of<br />
necessary medications and procedures.<br />
Hospital Dental Services: We will pay the expenses incurred for<br />
general anesthesia; nursing and related Hospital services<br />
provided in conjunction with inpatient, outpatient or one day<br />
dental services if the following conditions are met:<br />
1. The anesthesia, nursing and related Hospital services are<br />
deemed Medically Necessary by the treating dentist or oral<br />
surgeon and the Insured’s Physician; and<br />
2. The patient is either:<br />
a. Determined by a licensed dentist, in conjunction with a<br />
licensed Physician who specializes in primary care, to<br />
have a dental condition of significant dental complexity<br />
that the condition requires certain dental procedures to<br />
be performed in a Hospital; or<br />
b. A person who has a developmental disability, as<br />
determined by a licensed Physician who specializes in<br />
primary care that places the person at serious risk.<br />
c. Part B benefits will be considered a Covered Sickness<br />
the same as any other Sickness and is not subject to any<br />
dental benefit limits under this Policy.<br />
Cancer Clinical Trials: We will pay the expenses incurred for the<br />
routine patient care costs associated with cancer clinical trials. We<br />
will not pay such costs if they are eligible for reimbursement by<br />
any other entity, including the entity sponsoring the cancer clinical<br />
trial.<br />
Craniofacial Disorders: We will pay the expenses incurred for<br />
the Medically Necessary orthodontic processes and appliances<br />
for the treatment of craniofacial disorders for insured person age<br />
18 and younger. Such processes and appliances must be<br />
prescribed by a craniofacial team recognized by the American<br />
Cleft Palate – Craniofacial Association, except that no benefit will<br />
be paid for cosmetic surgery.<br />
Experimental Treatments: We will pay the expenses incurred by<br />
an Insured Person for experimental treatments, including<br />
procedures, treatments or the use of a drug as experimental if such<br />
procedure, treatment or drug, for the Sickness or condition being<br />
treated or for the diagnosis for which it is being prescribed, has<br />
successfully completed a phase III clinical trial of the Federal Food<br />
and Drug Administration. Such expenses will be paid the same as<br />
for any other Sickness under the applicable benefit provisions of this<br />
Policy, e.g. experimental surgical procedures under the surgery<br />
benefits, experimental drugs under the prescriptions benefits, etc.<br />
If an Insured Person has been diagnosed with a condition that<br />
creates a life expectancy in that person of less than two years<br />
and we have denied a benefit because we feel that it does not<br />
fit the above criteria, an Insured Person may request an<br />
expedited appeal of our decision as provided by this policy.<br />
Prescribed Drugs for Treatment of Cancer: When prescription<br />
drugs are covered under the Policy, we will pay the expenses<br />
incurred for treatment of a type of cancer for which the drug has not<br />
been approved by the Food and Drug Administration, provided the<br />
drug is recognized for treatment of the specific type of cancer in one<br />
of the following established reference compendia:<br />
1. The U.S. Pharmacopeia Drug Information Guide for Health<br />
Care Professionals (USP DI);<br />
2. The American Medical Association's Drug Evaluations (AMA<br />
DE); or<br />
3. The American Society of Hospital Pharmacist's American<br />
Hospital Formulary Service Drug Information (HAFS-DI).<br />
This benefit does NOT include coverage for any experimental or<br />
Investigational drugs or any drug which the federal Food and Drug<br />
Administration has determined to be contradicted for treatment of<br />
the specific type of cancer for which the drug has been prescribed.<br />
Neuropsychological Testing – When Dependent Coverage is<br />
part of the Insured Student’s coverage, We will provide<br />
Neuropsychological Testing for a Covered Child diagnosed<br />
with cancer on or after January 1, 2000 when ordered by a<br />
licensed physician to assess the extent of any cognitive or<br />
developmental delays in the Covered Child due to<br />
chemotherapy or radiation treatment.<br />
Isolation Care and Emergency Services– If an Insured<br />
Person requires Medically Necessary isolation care and/or<br />
emergency services that are provided by the state’s mobile field<br />
hospital We will provide coverage for the same services as for<br />
any other Sickness covered by this Policy. We will pay the<br />
same rates paid under the Medicaid program, as determined by<br />
the Connecticut Department of Social Services.<br />
Injuries Sustained While Insured Intoxicated: We will<br />
provide health care services to treat any Injury sustained while:<br />
1. Insured has an elevated blood alcohol content; or<br />
2. Insured is under the influence of intoxicating liquor or any<br />
drug or both.<br />
For the purpose of this benefit elevated blood alcohol content<br />
means a ratio of alcohol in the blood of such person that is<br />
eight-hundredths of one percent (08%) or more of alcohol by<br />
weight.<br />
CONTINUATION OF COVERAGE<br />
Any Insured Student who has been continuously covered under<br />
this Policy and prior student health insurance plans issued to<br />
Choate Rosemary Hall from one year to the next shall be covered<br />
for conditions first manifesting themselves while continuously<br />
insured, except for benefits payable under prior policies in the<br />
absence of this Policy.<br />
SUBROGATION<br />
If claims are incurred as a result of another person's<br />
negligence, the company has the right, as permitted by law, to<br />
seek reimbursement in accordance with the Policy.<br />
13 14 15
TERMINATION OF INSURANCE<br />
Benefits are payable under this Policy only for those Covered<br />
Expenses incurred while the Policy is in effect as to the Insured.<br />
No benefits are payable for expenses incurred after the date<br />
the insurance terminates for the Insured.<br />
EXCLUSIONS AND LIMITATIONS<br />
This Policy does not cover nor provide benefits for:<br />
1. Treatment, services or supplies which: are not Medically<br />
Necessary; are not prescribed by a Physician as necessary<br />
to treat a Sickness or Injury; are received without charge or<br />
legal obligation to pay; would not routinely be paid in the<br />
absence of insurance; are received from any family member.<br />
2. Expenses incurred as a result of loss due to war, or any<br />
action of war, declared or undeclared; service in the armed<br />
forces of any country.<br />
3. Injury or Sickness for which benefits are paid under any<br />
Workers Compensation or Occupational Disease law.<br />
4. Cosmetic surgery other than: Reconstructive surgery<br />
incidental to or following surgery resulting from trauma,<br />
infection, or other diseases of the involved part; or<br />
reconstructive surgery as the result of a congenital disease<br />
or anomaly as provided for dependent newborns during the<br />
first 31 days following birth.<br />
5. Riding as a passenger or otherwise in any vehicle or device<br />
for aerial navigation, except as fare-paying passenger in an<br />
aircraft operated by a commercial scheduled airline.<br />
6. Expenses incurred as a result of dental treatment, except as<br />
specifically stated.<br />
7. Eyeglasses, contact lenses, hearing aids, or prescriptions or<br />
examinations therefore, except as specifically provided<br />
under mandated benefits.<br />
8. Routine physical examinations and routine testing;<br />
preventive testing or treatment; and screening exams,<br />
except as specifically stated.<br />
9. Suicide or attempted suicide; or intentionally self-inflicted<br />
Injury, unless in conjunction with and as the result of a<br />
diagnosed Mental or Nervous Condition as defined and<br />
covered under the Policy.<br />
10. Treatment in a government Hospital, unless there is a<br />
legal obligation for the Covered Person to pay for such<br />
treatment.<br />
11. Injury sustained as the result of a motor vehicle Accident<br />
to the extent that benefits are recovered or recoverable<br />
under no-fault benefits insurance.<br />
PRE-EXISTING CONDITION LIMITATION<br />
Pre-existing Conditions are not covered for the first 12 months<br />
following a Covered Person’s Effective Date of coverage under<br />
the Policy. This limitation will not apply if:<br />
1. The Covered Person has been covered under the Policy<br />
for more than 12 months; or<br />
2. The individual seeking coverage under the Policy was<br />
previously covered under prior Creditable Coverage which<br />
was continuous to a date not less than 120 days prior to<br />
the effective date of coverage under the Policy (150 days<br />
prior to the effective date of coverage under the Policy if<br />
prior Creditable Coverage terminated due to an involuntary<br />
loss of employment) provided the Covered Person applied<br />
for coverage under the Policy within 30 days of initial<br />
eligibility.<br />
Creditable Coverage includes coverage under any of the<br />
following without a break in coverage of 120 days or more: a<br />
group health plan; health insurance coverage; Medicaid or<br />
Medicare; a State Health Benefit Risk Pool; United States<br />
military sponsored health care; Public Health Plan; the Federal<br />
Employees Health benefit plan; a medical care program of the<br />
Indian Health Service or of a tribal organization; a health plan<br />
under the Peace Corp Act. See Policy on file with the school for<br />
a full definition of Creditable Coverage.<br />
CLAIMS PROCEDURES FOR DOMESTIC AND<br />
INTERNATIONAL STUDENTS<br />
In the event of an Injury or Sickness the Insured Student<br />
should:<br />
1. If at Choate Rosemary Hall, report immediately to the<br />
Health Center so that proper treatment can be prescribed<br />
or approved, and obtain a claim form; or<br />
2. If away from Choate Rosemary Hall, or for ob/gyn<br />
treatment, consult a Physician and obtain a claim form<br />
from Willis of CT, LLC or Consolidated Health Plans or at<br />
www.chpstudent.com.<br />
3. Notify the Claims Administrator, Consolidated Health<br />
Plans, within 30 days after the date of the Injury or<br />
commencement of the Sickness, or as soon thereafter as<br />
is reasonably possible.<br />
4. Complete the claim form in full. The completed claim form<br />
should be mailed within 90 days from the date of Injury or<br />
from the date of the first medical treatment for a Sickness,<br />
or as soon as reasonably possible. Retain a copy for your<br />
records and mail a copy to the Claims Administrator,<br />
Consolidated Health Plans, at the address listed on the<br />
following page.<br />
5. Itemized medical bills must be attached to the claim form<br />
at the time of submission. Subsequent medical bills should<br />
be mailed promptly to the Claims Administrator at the<br />
address listed on the following page. No additional claim<br />
forms are needed as long as the Insured Student’s name<br />
and identification number are included on the bill. Direct all<br />
questions regarding benefits available under the Policy,<br />
claim procedures, status of a submitted claim or payment<br />
of a claim to the Claims Administrator, Consolidated<br />
Health Plans at the address below.<br />
REMEMBER THAT EACH INJURY OR SICKNESS IS A<br />
SEPARATE CONDITION AND A SEPARATE CLAIM FORM IS<br />
REQUIRED FOR EACH CONDITION.<br />
HOW TO FILE AN APPEAL<br />
Once a claim is processed and upon receipt of an Explanation<br />
of Benefits (EOB), an insured student who disagrees with how a<br />
claim was processed may appeal that decision. The student<br />
must request an appeal in writing within 60 days of the date<br />
appearing on the EOB. The appeal request must include why<br />
they disagree with the way the claim was processed. The<br />
request must include any additional information they feel<br />
supports their request for appeal, e.g. medical records,<br />
physician records, etc. Please submit all requests to the<br />
following:<br />
Consolidated Health Plans<br />
2077 Roosevelt Avenue<br />
Springfield, MA 01104<br />
The Policy is Underwritten By:<br />
Niagara Life and Health Insurance Company of Columbia, SC<br />
Policy Form: NLH-SH5-12 (CT)<br />
For a copy of the privacy notice you may:<br />
go to<br />
www.consolidatedhealth plan.com/about/hipaa<br />
or<br />
Request one from the Health Office at your School<br />
or<br />
Request one from:<br />
Commercial Travelers Mutual Insurance Company<br />
C/O Privacy Officer<br />
70 Genesee Street<br />
Utica, NY 13502<br />
16 17 18
(Please indicate the school you attend with your written request)<br />
Servicing Agent:<br />
Willis of CT, LLC<br />
185 Asylum Street, 25 th Floor<br />
Hartford, CT 06103<br />
(860) 278-1320 or (800) 843-5404, ext. 45391<br />
Claims Administered By:<br />
Consolidated Health Plans<br />
2077 Roosevelt Avenue<br />
Springfield, MA 01104<br />
(800) 633-7867<br />
www.chpstudent.com<br />
Any provision of the Policy or the brochure which is in conflict<br />
with the statutes of the state in which the Policy is issued, will<br />
be administered to conform to the requirements of the state<br />
statues.<br />
Representations of this plan must be approved by the<br />
Company.<br />
EMERGENCY MEDICAL AND TRAVEL ASSISTANCE<br />
FrontierMEDEX ACCESS services is a comprehensive<br />
program providing You with 24/7 emergency medical and travel<br />
assistance services including emergency security or political<br />
evacuation, repatriation services and other travel assistance<br />
services when you are outside Your home country or 100 or<br />
more miles away from your permanent residence.<br />
FrontierMEDEX is your key to travel security.<br />
For general inquiries regarding the travel access<br />
assistance services coverage, please call Consolidated<br />
Health Plans at 1-800-633-7867.<br />
If you have a medical, security, or travel problem, simply call<br />
FrontierMEDEX for assistance and provide your name, school<br />
name, the group number shown on your ID card, and a<br />
description of your situation. If you are in North America, call<br />
the Assistance Center toll-free at: 1-800-527-0218 or if you are<br />
in a foreign country, call collect at: 1-410-453-6330.<br />
If the condition is an emergency, you should go<br />
immediately to the nearest physician or hospital without<br />
delay and then contact the 24-hour Assistance Center.<br />
FrontierMEDEX will then take the appropriate action to<br />
assist You and monitor Your care until the situation is<br />
resolved.<br />
VISION DISCOUNT PROGRAM<br />
For Vision Discount Benefits please go to:<br />
www.chpstudent.com<br />
<strong>CHOATE</strong> <strong>ROSEMARY</strong> <strong>HALL</strong><br />
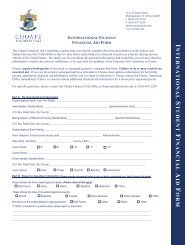
Insurance Election Form<br />
2012-2013<br />
Sickness and Accident Coverage<br />
Students Name: _____________________________________<br />
Date of Birth: _______________<br />
I understand that proof of medical insurance is required for<br />
attendance at Choate Rosemary Hall. The school Student<br />
Insurance Plan underwritten by Niagara Life and Health<br />
Insurance Company will extend from 9/1/2012 – 9/1/2013 and<br />
cover the student while attending school, at home, and while<br />
traveling.<br />
DOMESTIC & INTERNATIONAL STUDENTS<br />
I select one of the following options:<br />
Plan A (Domestic Only): Since I have viable medical<br />
insurance available for my child, I elect this plan, which is<br />
primary over my own insurance. (Please check with your<br />
insurance company to see if benefits will extend to services<br />
rendered in Connecticut. Most HMO’s and PPO Plans do not). I<br />
understand that Plan A is designed for students whose current<br />
medical insurance has a high deductible. The Policy pays<br />
covered expenses up to 100% of R&C to a maximum of<br />
$5,000 per year.<br />
Premium: $240<br />
Plan B (Domestic & International): Since I do not have a<br />
viable medical insurance Policy for my child or I have HMO<br />
coverage, I elect this plan which will serve as his/her primary<br />
insurance. The plan pays up to 100% of R&C of covered<br />
expenses incurred from injury or sickness up to a<br />
maximum of $200,000 for each incident.<br />
Premium: $979<br />
I elect to waive all of the above coverage as I am currently<br />
covered under a U.S. viable medical insurance policy. I will<br />
maintain health Insurance coverage throughout my child’s CHR<br />
career and will provide the Health Center with updated cards as<br />
necessary. Attached is a copy of both sides of my<br />
insurance card.<br />
I am covered by: _________________________________<br />
My Policy # is: ___________________________________<br />
Parent’s Signature: ___________________________________<br />
19 20
The following information is required if ELECTING a<br />
Student Insurance Plan.<br />
STUDENT INFORMATION M F<br />
Are you a U.S. Citizen? Yes No<br />
Student Name: ______________________________________<br />
Date of Birth: _______________<br />
__________________________________________________<br />
HOME Street Address<br />
__________________________________________________<br />
City, State, Zip<br />
__________________________________________________<br />
Parents Signature<br />
Please return this form with your check in the enclosed<br />
envelope by October 15, 2012 to:<br />
Consolidated Health Plans<br />
2077 Roosevelt Avenue<br />
Springfield, MA 01104<br />
OR<br />
You may enroll on-line at: www.chpstudent.com.<br />
We accept both MasterCard and Visa.<br />
For questions, please contact your servicing agent, Willis of CT,<br />
LLC at 1-800-843-5404, ext. 45391.<br />
Form EF-I5A18<br />
19 20