Mayo Alumni Magazine 2012 Spring - MC4409-0312 - Mayo Clinic
Mayo Alumni Magazine 2012 Spring - MC4409-0312 - Mayo Clinic
Mayo Alumni Magazine 2012 Spring - MC4409-0312 - Mayo Clinic
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Mayo</strong> <strong>Alumni</strong><br />
mayo.edu/alumni | <strong>Spring</strong> <strong>2012</strong><br />
INNOVATION INTO
<strong>Mayo</strong> <strong>Alumni</strong><br />
<strong>Spring</strong> <strong>2012</strong><br />
Features<br />
2 “Innovation Into Action”<br />
At the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association 67th Meeting in Florida,<br />
participants learned about advances in medicine, research and<br />
health care delivery systems.<br />
4 Speaker Highlights<br />
Speakers at the 67th Meeting included Daniel Brat, M.D., Ph.D.,<br />
John Woods, M.D., Ph.D., Ceci Connolly, Andre Terzic, M.D., Ph.D.,<br />
Mary Grealy, Claire Bender, M.D., and Mike Harper, M.D.<br />
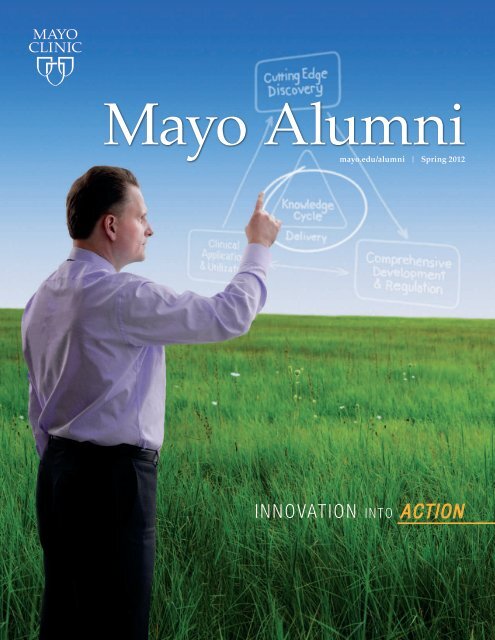
About the Cover<br />
INNOVATION INTO<br />
<strong>Mayo</strong> <strong>Clinic</strong>’s new Center for<br />
Regenerative Medicine is a prime<br />
example of turning innovation into<br />
action — the theme of the recent<br />
<strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association<br />
biennial meeting. At the meeting,<br />
Andre Terzic, M.D., Ph.D. (CV ’95)<br />
(pictured on the cover), medical<br />
director of the Center for<br />
Regenerative Medicine, spoke<br />
about how this rapidly evolving<br />
field of medicine will help repair<br />
damaged heart muscle.<br />
According to Dr. Terzic,<br />
regenerative medicine is a gamechanger.<br />
“It has the potential<br />
to offer definitive, affordable<br />
health care solutions that treat<br />
the underlying causes of diseases<br />
rather than only manage<br />
symptoms,” he says. “Our<br />
approach has the ability to turn<br />
promising laboratory discoveries<br />
into proven treatments — and<br />
make them available to patients<br />
— more effectively and efficiently<br />
than most anywhere else.”<br />
12 Awarding Excellence<br />
Award recipients at the 67th Meeting included C. Robert Stanhope,<br />
M.D., Larry Vukov, M.D., John Wheat, M.D., S. Ann Colbourne,<br />
M.D., Lee Joseph McGhan, M.B., B.Ch., and Peter Gloviczki, M.D.<br />
18 Advancing an Ideal<br />
Wyatt Decker, M.D., vice president and CEO of <strong>Mayo</strong> <strong>Clinic</strong> in Arizona,<br />
sets his sights on the future of health care.<br />
20 Twenty-five years of Caring<br />
<strong>Mayo</strong> <strong>Clinic</strong> in Florida celebrated its 25th anniversary in 2011.<br />
21 <strong>Mayo</strong> <strong>Clinic</strong> Distinguished <strong>Alumni</strong> Award<br />
2011 recipients included Richard Brubaker, M.D., Gene Hunder, M.D.,<br />
Keith Kelly, M.D., and Guillermo Ruiz-Argüelles, M.D.<br />
<strong>Mayo</strong> Update<br />
24 Board of Trustees news, obituaries<br />
<strong>Mayo</strong> <strong>Alumni</strong><br />
Print or digital?<br />
You like potato and I like potahto. No need to choose —<br />
we offer both. The print version has pass-along value,<br />
making it easy to save and share with family members<br />
and patients. The digital version has extras you won’t<br />
find elsewhere — video interviews and event clips,<br />
photo galleries and <strong>Mayo</strong> <strong>Clinic</strong> historical information.<br />
Download the free <strong>Mayo</strong> <strong>Alumni</strong> app (for iPad) in<br />
the iTunes strore. Scan the code at right to go directly<br />
to the download page. The <strong>Spring</strong> <strong>2012</strong> issue will be<br />
live and digital on May 17th.
New <strong>Mayo</strong> <strong>Clinic</strong><br />
<strong>Alumni</strong> Association president<br />
Eric Grigsby, M.D.<br />
Medical Director<br />
Napa Pain Institute<br />
Napa, Calif.<br />
Eric Grigsby, M.D. (S ’86, ANES ’88), was elected the new president of the <strong>Mayo</strong><br />
<strong>Clinic</strong> <strong>Alumni</strong> Association at the group’s biennial meeting in Jacksonville, Fla.<br />
Dr. Grigsby is founding medical director of the Napa Pain Institute and chief<br />
executive officer of Neurovations, a Napa, Calif., based company specializing in<br />
pain and neuroscience research and clinical education.<br />
A native of Knoxville, Tenn., Dr. Grigsby received an undergraduate degree<br />
from Boston University and a medical degree from Boston University Medical<br />
School. He had five years of postgraduate training in general surgery, anesthesiology<br />
and pain management at <strong>Mayo</strong> <strong>Clinic</strong> in Rochester. Currently, he is enrolled in<br />
The Duke MBA—Global Executive program through the Fuqua School of Business.<br />
Dr. Grigsby and his wife, Mary Rocca, D.M.D., operate a foundation, HealthRoots,<br />
which provides care to underserved groups, most recently in Malawi, Africa.<br />
At the recent <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association meeting, Dr. Grigsby led the<br />
organization’s board in voting unanimously to establish the <strong>Mayo</strong> International<br />
Humanitarian Endowment to support programs that provide care to underserved<br />
patient populations around the world.<br />
Dr. Grigsby succeeds Mark Laney, M.D. (PDN ’89), president and CEO of<br />
Heartland Health in St. Joseph, Mo.<br />
Eric Grigsby, M.D., in Malawi, Africa.
2 <strong>Mayo</strong> <strong>Alumni</strong><br />
InnovatIon Into Action
<strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association 67 th Meeting • September 2011 • Florida<br />
The <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association 67th meeting at <strong>Mayo</strong> <strong>Clinic</strong><br />
in Florida attracted 310 alumni and their guests from 26 states<br />
and six countries.<br />
The meeting theme, “Innovation Into Action,” did not disappoint.<br />
Participants learned about advances in medicine, research and health<br />
care delivery systems that expanded and stimulated their thinking<br />
about the future of medicine, engaged them in interactions with fellow<br />
alumni and sparked them to return home to innovate. Highlights<br />
of talks are included in the pages that follow.<br />
Visit the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association blog,<br />
alumniblog.mayo.edu,<br />
for more coverage of the 6 7<br />
th meeting.<br />
<strong>Spring</strong> <strong>2012</strong> 3
MAyO CLINIC<br />
ALUMNI ASSOCIATION<br />
67 TH MEETING<br />
2011<br />
Speaker<br />
h i g h l i g h t s<br />
The tradition of scientific presentations at <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association biennial<br />
meetings is complemented by a lecture program that highlights individuals who<br />
have expertise in medical specialties or areas of research.<br />
Raymond Pruitt Lectureship<br />
Honors Raymond Pruitt, M.D., the first dean of <strong>Mayo</strong> Medical School<br />
Lecturer demonstrates qualities admired in Dr. Pruitt — integrity,<br />
scholarship, humility and the empathy of the truly concerned<br />
Daniel Brat, M.D., Ph.D.<br />
Professor and Vice Chair,<br />
Translational Programs<br />
Department of Pathology and<br />
Laboratory Medicine<br />
Emory University School of Medicine<br />
Mechanisms of Progression in<br />
Glioblastoma: Role of Genetics,<br />
Hypoxia and Stem Cells<br />
Daniel Brat, M.D., Ph.D. (MMS ’94,<br />
PHAR ’94), reviewed his lab’s<br />
research on glioblastoma over the past<br />
decade. He uses multiple approaches,<br />
including traditional cell biology of<br />
gliomas grown in culture, animal<br />
models of disease, human specimens,<br />
and newer bioinformatics approaches<br />
that utilize molecular data sets. Dr. Brat’s<br />
main interest has been in determining<br />
the molecular switches that lead to<br />
the rapid and fatal progression of<br />
glioblastoma.<br />
Dr. Brat has focused on the<br />
emergence of necrosis, together with<br />
its severe hypoxia (low oxygen content)<br />
and angiogenesis (new vessels) since<br />
these are the two critical features that<br />
emerge and drive tumor growth in<br />
this disease.<br />
Dr. Brat emphasized his current<br />
work with the National Cancer Institute’s<br />
Cancer Genome Atlas project<br />
(TCGA), which includes a rich array<br />
of molecular data that can be probed<br />
using sophisticated bioinformatics and<br />
systems biology approaches. TCGA<br />
studies have suggested that the presence<br />
of necrosis and hypoxia lead to the<br />
activation of a specific yet small set of<br />
transcription factors (CEBP-beta and<br />
CEBP-delta) that account for the transition<br />
to an aggressive transcriptional<br />
form of glioblastoma (the mesenchymal<br />
class). They appear to be aggressive<br />
and resistant to therapy.<br />
Dr. Brat’s work also has challenged<br />
the idea that tumors become hypoxic<br />
and necrotic by simply “outgrowing<br />
their blood supply.” He has advanced<br />
the hypothesis — supported it with<br />
his own research — that blood vessels<br />
within malignant gliomas become<br />
dysfunctional and occluded, thereby<br />
leading to the rapid onset of severe<br />
hypoxia and necrosis.<br />
4 <strong>Mayo</strong> <strong>Alumni</strong>
The Doctors <strong>Mayo</strong> Society<br />
Lifetime Achievement Distinguished Lecture<br />
Established to highlight significant achievement by a <strong>Mayo</strong> alumnus/alumna<br />
John Woods, M.D., Ph.D.<br />
Emeritus Professor of Surgery<br />
College of Medicine, <strong>Mayo</strong> <strong>Clinic</strong><br />
Lessons Learned in Attitude<br />
and Integrity<br />
John Woods, M.D., Ph.D. (S ’66,<br />
PLS ’68), shared the lessons he has<br />
learned about integrity and attitude in<br />
five decades at <strong>Mayo</strong> <strong>Clinic</strong>, treating<br />
more than 20,000 surgical patients.<br />
He said his parents instilled in him<br />
the importance of integrity from the<br />
earliest age, but he still describes himself<br />
as “very much a work in progress.”<br />
“I’ve learned a lot through errors<br />
and mistakes. In fact, more from<br />
mistakes than I have through my<br />
successes,” said Dr. Woods. He also<br />
pointed out the importance of learning<br />
from others’ mistakes and the role of<br />
honesty in integrity.<br />
“As a professor, I saw how costly it<br />
was to doctors’ careers when they had<br />
discrepancies and inaccuracies in<br />
publications. It took years to recover,”<br />
he said. “I once canceled a national<br />
presentation when I discovered some<br />
errors in my statistics. Another time, I<br />
had already presented when I learned<br />
about a statistical error. I felt honorbound<br />
to correct the mistake, so I sent<br />
a letter to the attendees of the meeting,<br />
pointing out the inaccuracy and<br />
providing the correct information.”<br />
Dr. Woods described the importance<br />
of fairness as a component of integrity.<br />
“Giving recognition to others for their<br />
contributions can be a pleasurable<br />
experience and may even encourage<br />
others to contribute,” he said.<br />
He also discussed the importance<br />
of attitude. He cited the example of a<br />
patient who requested a referral to a<br />
different oncologist because the<br />
previous one lacked compassion.<br />
“Under the care of the new oncologist,<br />
the patient expressed gratitude for the<br />
warm bedside manner,” said Dr. Woods.<br />
“Attitude can be a stumbling block,<br />
and arrogance can be palpable. The<br />
physician’s attitude can make a great<br />
difference to the patient. A good<br />
bedside manner can be learned even<br />
when it is not a natural part of the<br />
physician’s armamentarium.”<br />
Dr. Woods highlighted the indomitable<br />
spirit of patients who have made<br />
significant impressions on him —<br />
patients with significant deformities<br />
who regarded the obstacles they faced<br />
as opportunities.<br />
“Many of my patients have<br />
inspired me with their memorable<br />
attitudes,” he said. “Despite many<br />
years of medical procedures and<br />
disfiguring conditions, they didn’t<br />
consider themselves handicapped. I<br />
never heard them complain. I believe<br />
their attitudes contributed to their<br />
healing and survival.<br />
“The <strong>Mayo</strong> <strong>Clinic</strong> perspective<br />
is that we should give every patient<br />
the very best. Being human, we not<br />
infrequently fail. But in my 60 years<br />
of practicing surgery — 50 of those<br />
years here at <strong>Mayo</strong> — despite failures,<br />
I continue to pray and hope to be<br />
positive in my attitude and to live<br />
with integrity.”<br />
<strong>Spring</strong> <strong>2012</strong> 5
iPad app extra<br />
Judd-Plummer Recognition Award<br />
Established to honor two early, distinguished members of <strong>Mayo</strong> <strong>Clinic</strong> medical staff —<br />
E. Starr Judd, M.D., chief of the surgical staff, and Henry Plummer, M.D., chief of the Division of Medicine<br />
Presented to an outstanding physician, surgeon, scientist or educator<br />
Ceci Connolly<br />
Senior Adviser, McKinsey Center<br />
for Health Reform<br />
Ceci Connolly led a panel discussion<br />
about efforts to transform health<br />
care delivery through the use of health<br />
care information technology. The<br />
discussion ranged from an overview<br />
of megatrends in health care and<br />
information technology to case studies<br />
about using health information<br />
technology to improve care.<br />
Panelists included:<br />
• Jamie Ferguson, Vice President,<br />
Health Information Technology<br />
Strategy and Policy, Kaiser<br />
Permanente — Discussing the<br />
work of the Care Connectivity<br />
Consortium<br />
• Christopher Chute, M.D., Dr.P.H.<br />
(EPID ’88), Professor of Medical<br />
Informatics, <strong>Mayo</strong> <strong>Clinic</strong> —<br />
Discussing work in southeast<br />
Minnesota in managing diabetes<br />
and childhood asthma through a<br />
Beacon grant<br />
Connolly is a senior adviser in the<br />
McKinsey Center for Health Reform, an<br />
independent economic research group<br />
focused on high-quality, affordable<br />
health care. She frequently advises<br />
public and private sector leaders on the<br />
implications of the Affordable Care Act,<br />
stakeholder management and crisis<br />
communications.<br />
Previously, Connolly was a<br />
nationally recognized journalist, author<br />
and television commentator. As the<br />
health policy reporter at The Washington<br />
Post, she chronicled enactment of<br />
President Obama’s Affordable Care<br />
Act and was the lead author of<br />
Landmark: The Inside Story of America’s<br />
New Health-Care Law and What It Means<br />
for Us All.<br />
• Abdul Bengali, Chair, Information<br />
Technology, <strong>Mayo</strong> <strong>Clinic</strong> —<br />
Discussing five trends in health care<br />
and information technology<br />
6 <strong>Mayo</strong> <strong>Alumni</strong>
MAyO CLINIC<br />
ALUMNI ASSOCIATION<br />
67 TH MEETING<br />
2011<br />
Research<br />
h i g h l i g h t s<br />
iPad app extra<br />
Regenerative medicine no longer ‘science fiction’<br />
<strong>Mayo</strong>’s first-of-its-kind center explores causes, cures of congenital and acquired disease<br />
Andre Terzic, M.D., Ph.D.<br />
<strong>Mayo</strong> <strong>Clinic</strong> Center for Regenerative<br />
Medicine<br />
Regenerative Medicine<br />
for Heart Repair<br />
Boosting the body’s ability to<br />
heal is the basis for regenerative<br />
medicine. This rapidly evolving<br />
field of new medicine is increasingly<br />
recognized as an important component<br />
of the practice of medicine. Regenerative<br />
medicine can use stem cells to help<br />
repair damaged heart muscle after a<br />
heart attack or even implant cells to<br />
replace those damaged by Parkinson’s<br />
disease or other chronic degenerative<br />
diseases, such as diabetes or bone and<br />
cartilage destruction.<br />
“It’s no longer science fiction,” said<br />
Andre Terzic, M.D., Ph.D. (CV ’95),<br />
medical director for the newly established<br />
<strong>Mayo</strong> <strong>Clinic</strong> Center for Regenerative<br />
Medicine. “Stem cells are unique<br />
seeds. If properly planted, guided and<br />
nurtured, they can give rise to very<br />
specific organ parts. It is now possible<br />
for stem cells to repair portions of<br />
organs and, in some cases, even help<br />
fix a diseased organ.”<br />
Dr. Terzic said a key principle in<br />
understanding regenerative medicine<br />
is to recognize how organs self-heal.<br />
“We now know that it is not just<br />
skin and liver that have a high ability<br />
to self-regenerate,” he said. “The heart<br />
and brain also have an innate capacity<br />
to heal. We don’t die with the same<br />
heart we’re born with; 50 percent or<br />
more of the heart muscle is rejuvenated<br />
during our life span.”<br />
Harnessing the body’s natural<br />
ability to heal provides a unique<br />
blueprint to address congenital and<br />
acquired diseases, according to<br />
Dr. Terzic. “As the world’s population<br />
ages — by 2025, more than 20 percent<br />
of the population in the Northern<br />
Hemisphere will be over age 60 —<br />
chronic diseases are becoming more<br />
prevalent in the population and require<br />
new solutions,” he said.<br />
Dr. Terzic added that today’s primary<br />
therapies for patient management are<br />
based on drug therapy and devices, which<br />
address symptoms rather than the root<br />
cause of a disease. “Regenerative<br />
medicine offers solutions not currently<br />
available to the medical profession and,<br />
ultimately, to patients,” he said. “It<br />
provides the opportunity to go after the<br />
causes of disease and possibly offer cures.”<br />
Regenerative medicine broadens<br />
the reach of current practices such as<br />
transplant medicine. “Rather than<br />
waiting for a donor to replace an entire<br />
organ, it’s possible to regenerate a part<br />
of the organ that is defective,” said<br />
Dr. Terzic.<br />
He shared a case study trial<br />
conducted using <strong>Mayo</strong> <strong>Clinic</strong> technology<br />
where bone marrow stem cells derived<br />
from patients were guided to become<br />
cardiac tissue, implanted in the injured<br />
heart, leading to significant long-term<br />
benefit. “These initial steps have<br />
generated broad interest worldwide,”<br />
he said.<br />
The <strong>Mayo</strong> <strong>Clinic</strong> Center for<br />
Regenerative Medicine “provides a<br />
catalyst to advance health care and<br />
address many of the questions both<br />
providers and patients may have on<br />
regenerative solutions,” said Dr. Terzic.<br />
The ability to use regenerative technologies<br />
is “becoming increasingly a<br />
reality across disciplines of medicine<br />
and surgery. Propelled by innovative<br />
science, this emerging field is poised<br />
to advance rapidly and offer tangible<br />
benefit to our patients.”<br />
<strong>Spring</strong> <strong>2012</strong> 7
MAyO CLINIC<br />
ALUMNI ASSOCIATION<br />
67 TH MEETING<br />
2011<br />
Research & Practice<br />
For answers to health care reform, pass the <strong>Mayo</strong><br />
Healthcare Leadership Council sharing private-sector innovations that benefit patients while reducing costs<br />
Mary Grealy<br />
President, Healthcare Leadership<br />
Council<br />
Washington, D.C.<br />
Innovation to Create a Health-<br />
Value Health Care System<br />
Mary Grealy, president of the<br />
Healthcare Leadership Council<br />
(HLC), told <strong>Mayo</strong> alumni: “<strong>Mayo</strong> is an<br />
example of what the health care system<br />
should be about. There’s no problem<br />
we can’t solve if we could just find a<br />
way to ‘<strong>Mayo</strong>-ize’ the entire system.<br />
There are many lessons we can learn<br />
from what <strong>Mayo</strong> has done and what<br />
is under way.”<br />
The Healthcare Leadership<br />
Council, based in Washington, D.C.,<br />
is a consortium of companies and<br />
organizations from all sectors of<br />
health care, with a shared vision of a<br />
health care system that is defined by<br />
accessibility, affordability, quality and<br />
information. <strong>Mayo</strong> <strong>Clinic</strong> is a longtime<br />
member. Former President and CEO<br />
Denis Cortese, M.D., and former<br />
CEO Robert Waller, M.D., served as<br />
president of the council.<br />
Grealy commented that while<br />
health care reform has been viewed<br />
as a battle, it’s really just a warm-up<br />
of things to come.<br />
“There is a battling over budgets in<br />
a way I have never seen before,” she said.<br />
“Deficit reduction is a primary focus and<br />
is part of the debate every day. There’s<br />
no question health care is going to play<br />
a significant role in these discussions.<br />
The question is whether the impact will<br />
be for the better or for worse.”<br />
Grealy added that potential solutions<br />
— those that involve improved quality<br />
metrics at a lower cost — will most<br />
likely be found in health care innovations<br />
put forth by the private sector.<br />
HLC published a value compendium<br />
of evidence-based innovations it has<br />
been sharing with Congress, the<br />
Institute of Medicine and the Centers<br />
for Medicare & Medicaid Services in<br />
an attempt to show how ideas that<br />
are working at institutions such as<br />
<strong>Mayo</strong> <strong>Clinic</strong> could be applied on a<br />
broader basis.<br />
She pointed to an example in<br />
the compendium: <strong>Mayo</strong>’s Total Joint<br />
Database, the most comprehensive<br />
database on joint replacements in the<br />
world, which contains information<br />
about every total joint implant<br />
performed at <strong>Mayo</strong> <strong>Clinic</strong> since 1969.<br />
Variables in total hip replacement,<br />
such as surgical technique, can affect<br />
the long-term outcome of the surgery<br />
— one of <strong>Mayo</strong>’s top reimbursement<br />
claims billed to Medicare.<br />
The Total Joint Database allows<br />
<strong>Mayo</strong> physicians to determine which<br />
surgical practices and implant models<br />
are most effective, based on historical<br />
data. Prior to surgery, information such<br />
as a patient’s level of pain and joint<br />
function is documented. During<br />
surgery, the approach, implant model<br />
and design, and fixation method are<br />
recorded. Postoperatively, patients are<br />
evaluated after one, two and five years,<br />
and then at five-year intervals.<br />
8 <strong>Mayo</strong> <strong>Alumni</strong>
iPad app extra<br />
A panel discussion moderated by Ceci Connolly (left), senior advisor of the McKinsey Center<br />
for Health Reform, included (from left) Richard Presutti, D.O. (FM ’97), Department of Family<br />
Medicine, <strong>Mayo</strong> <strong>Clinic</strong> in Florida; Sherine Gabriel, M.D. (I ’86, RHEU ’88), Division of<br />
Rheumatology, <strong>Mayo</strong> <strong>Clinic</strong> in Rochester; Robert Nesse, M.D. (FM ’80), chief executive officer,<br />
<strong>Mayo</strong> <strong>Clinic</strong> Health System; and Mary Grealy, president of the Healthcare Leadership Council.<br />
The evidence-based decision model<br />
helps increase efficiency and reduce<br />
waste. And the outcomes speak for<br />
themselves: at <strong>Mayo</strong>, the overall success<br />
rate of hip replacement at 10 years is<br />
greater than 90 percent, and there is an<br />
80 percent chance the implant will last<br />
for 20 years.<br />
“Innovation is helping patients<br />
every day,” Grealy said. “In fact, it’s<br />
happening in every sector of health care.<br />
We’re not just talking about devices<br />
and pharmaceuticals. Health care<br />
organizations like <strong>Mayo</strong> are providing<br />
innovative services, procedures, and<br />
product and information structures<br />
they have developed to make better<br />
quality health care that is more<br />
efficient.<br />
“Dr. Robert Waller has said,<br />
‘Providing quality, we can reduce the<br />
cost.’ That’s a message we continue<br />
to share.”<br />
<strong>Spring</strong> <strong>2012</strong> 9
MAyO CLINIC<br />
ALUMNI ASSOCIATION<br />
67 TH MEETING<br />
2011<br />
Education<br />
Claire Bender, M.D.<br />
Dean, <strong>Mayo</strong> School of Health Sciences<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Rochester<br />
Training Health Care Providers<br />
of the Future<br />
Claire Bender, M.D. (PT ’71, I ’77,<br />
R-D ’80), dean of <strong>Mayo</strong> School of<br />
Health Sciences, spoke about a new<br />
model of blended learning being<br />
employed by the School of Health<br />
Sciences to add value and efficiency<br />
to health care provider education.<br />
This model is a departure from<br />
traditional classroom-only instruction,<br />
and uses tools that include simulation<br />
and online learning. The model is<br />
being applied to three programs to<br />
study its effectiveness — clinical<br />
neurophysiology technician, histology<br />
technician and phlebotomy technician.<br />
“We are working with internationally<br />
known outside educators to ensure this<br />
model succeeds at reducing costs and<br />
provides flexible options for students<br />
while maintaining quality and integrity<br />
in our educational programming,” said<br />
Dr. Bender. “This model may provide<br />
opportunities for <strong>Mayo</strong> employees<br />
who want to go back to school and<br />
still work without giving up their<br />
employment. We are responding to<br />
the charge to innovate. We want to<br />
make a difference in health care<br />
provider education.”<br />
Mark your calendar<br />
<strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association International Scientific Education Program<br />
Course headquarters<br />
Dan Jerusalem Hotel<br />
Oct. 22-25, <strong>2012</strong><br />
Jerusalem<br />
Pre-conference tour, Jerusalem<br />
Oct. 19-22<br />
Registration materials<br />
mailed soon.<br />
Post-conference tour, northern<br />
and eastern Israel and Jordan<br />
Oct. 26- Nov. 5<br />
10 <strong>Mayo</strong> <strong>Alumni</strong>
MAyO CLINIC<br />
ALUMNI ASSOCIATION<br />
67 TH MEETING<br />
2011 Practice<br />
C. Michel (Mike) Harper Jr., M.D.<br />
Executive Dean for <strong>Clinic</strong>al Practice<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Rochester<br />
<strong>Mayo</strong> <strong>Clinic</strong>: Knowledge<br />
to Delivery<br />
Mike Harper, M.D. (I ’83, N ’86),<br />
executive dean for <strong>Clinic</strong>al<br />
Practice at <strong>Mayo</strong> <strong>Clinic</strong>, spoke about<br />
<strong>Mayo</strong> <strong>Clinic</strong>’s care process model for<br />
central venous catheters (CVC) as an<br />
example of integration and knowledge<br />
management — key factors in delivering<br />
high-quality, affordable care.<br />
“The size and complexity of our<br />
practice has resulted in best practices<br />
being less well defined and difficult<br />
to diffuse,” he said. “The risk in that<br />
environment is care that is more<br />
variable, fragmented, lower quality,<br />
less safe and more costly.”<br />
CVC protocols varied across <strong>Mayo</strong><br />
<strong>Clinic</strong>, and CVCs were identified as a<br />
source of intermittent sentinel events<br />
and higher infection rates.<br />
A work group developed a <strong>Mayo</strong><br />
standard of care for CVC, including a<br />
common protocol — called a care<br />
process model — with guidelines for<br />
education, training and credentialing.<br />
The central line care process model<br />
was codified and the information was<br />
added to Ask<strong>Mayo</strong>Expert, an online<br />
tool that provides a central repository<br />
for providers to access best practices.<br />
“When we measured the outcomes<br />
of this standardization, the result was<br />
dramatic,” said Dr. Harper. Since<br />
implementation, <strong>Mayo</strong> <strong>Clinic</strong> has had<br />
zero sentinel events related to CVC,<br />
he noted. <strong>Mayo</strong> also has seen a greater<br />
than 40 percent reduction in infection<br />
rates related to central lines.<br />
“Our core business is about generating,<br />
organizing, sharing and applying<br />
knowledge in a way that enhances<br />
high-value health care delivery,” said<br />
Dr. Harper. “Continuing to integrate<br />
and apply best practices will result in<br />
a higher standard of care.”<br />
Mark your calendar<br />
<strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association<br />
68th Meeting<br />
Sept. 25-28, 2013<br />
Rochester, Minn.<br />
<strong>Spring</strong> <strong>2012</strong> 11
MAyO CLINIC<br />
ALUMNI ASSOCIATION<br />
67 TH MEETING<br />
2011<br />
A w A r d i n g<br />
E x c E l l E n c E<br />
iPad app extra<br />
Humanitarian Award and<br />
Professional Achievement Award<br />
Presented by <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association to alumni nominated by their peers,<br />
to recognize significant contributions to humanity and to the medical profession<br />
Humanitarian Award<br />
C. Robert Stanhope, M.D.<br />
Consultant, Division of Gynecologic<br />
Surgery<br />
Department of Obstetrics and<br />
Gynecology<br />
Professor of Obstetrics and<br />
Gynecology<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Rochester<br />
Robert Stanhope, M.D. (OBG ’82),<br />
C. was awarded the 2011 <strong>Mayo</strong> <strong>Clinic</strong><br />
<strong>Alumni</strong> Association Humanitarian<br />
Award for a lifetime of dedication and<br />
devotion to helping vulnerable people<br />
in the clinic, in the community and<br />
around the world.<br />
He says his most satisfying efforts<br />
have been serving with short-term<br />
mission groups in Haiti, Mongolia,<br />
Honduras, Kenya and Guinea, West<br />
Africa. In Guinea, he is part of a team<br />
that is building obstetrical and surgical<br />
services in a medically poor region of<br />
the country.<br />
“It has been a blessing to have<br />
opportunities to serve men and women<br />
with dire medical needs in low-income<br />
and low-resource countries around the<br />
world and to be part of a compassionate,<br />
caring medical community at <strong>Mayo</strong><br />
<strong>Clinic</strong>,” he says.<br />
Dr. Stanhope is cofounder of the<br />
Good Samaritan Medical and Dental<br />
<strong>Clinic</strong>s and chair of the Rochester<br />
Medical Relief Mission Group. He has<br />
served on the boards of the Salvation<br />
Army, United Way, Gamehaven<br />
Council Boy Scouts of America,<br />
Seasons Hospice and Autumn Ridge<br />
Church. He is one of two Rochester<br />
residents to receive the Distinguished<br />
Eagle Award and also is a recipient<br />
of the Edward Henderson, M.D.,<br />
Leadership Award from the Zumbro<br />
Valley Medical Society.<br />
Dr. Stanhope was appointed to the<br />
<strong>Mayo</strong> <strong>Clinic</strong> staff in 1982 as a consultant<br />
in Gynecologic Surgery. He completed<br />
a fellowship at M.D. Anderson Hospital<br />
and Tumor Institute and a residency<br />
in obstetrics and gynecology at the<br />
University of Texas Southwestern−<br />
Parkland Memorial Hospital.<br />
Dr. Stanhope, a native of Milwaukee,<br />
received his medical degree from the<br />
Medical College of Wisconsin and<br />
undergraduate degree from the<br />
University of Wisconsin in Madison.<br />
He served in the U.S. Army, including<br />
service in Vietnam as a medical<br />
adviser. There, he built a maternity<br />
center for the wives of Vietnamese<br />
servicemen. The center was named<br />
Khu Ho Sanh Stanhope.<br />
12 <strong>Mayo</strong> <strong>Alumni</strong>
iPad app extra<br />
Humanitarian Award<br />
Larry Vukov, M.D.<br />
Consultant, Department of<br />
Emergency Medicine<br />
Associate Professor of Emergency<br />
Medicine<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Rochester<br />
Larry Vukov, M.D. (I ’80), was<br />
awarded the 2011 <strong>Mayo</strong> <strong>Clinic</strong><br />
<strong>Alumni</strong> Association Humanitarian<br />
Award for his work leading mission<br />
trips in underserved nations and for<br />
his contributions to community-based<br />
mission service for <strong>Mayo</strong> <strong>Clinic</strong><br />
patients.<br />
Every year for the last 21 years,<br />
Dr. Vukov has spent two weeks leading<br />
teams of medical and nonmedical<br />
volunteers from First Baptist Church<br />
and other churches on trips to rural<br />
Kenya to build and develop Hope<br />
Centers. These centers consist of a<br />
church, primary school, medical clinic<br />
and feeding center. Dr. Vukov has<br />
overseen the development of seven<br />
centers that educate and feed more<br />
than 2,000 children and clinics that<br />
provide health care for as many as<br />
15,000 people. The mission trips,<br />
which have included many <strong>Mayo</strong> staff,<br />
residents, students and nurses, are in<br />
conjunction with Special Ministries, an<br />
organization for which Dr. Vukov is a<br />
board member. Dr. Vukov also has led<br />
or participated in short-term mission<br />
trips to Honduras, Costa Rica, Tanzania,<br />
and Guinea, West Africa.<br />
“I am grateful to have been richly<br />
blessed with a loving and understanding<br />
wife and children, a mission-minded<br />
prayerful church, and an organization<br />
like <strong>Mayo</strong> <strong>Clinic</strong> that has provided<br />
the means and support to serve the<br />
underserved and care for those in<br />
need,” he says.<br />
Dr. Vukov was appointed to the<br />
<strong>Mayo</strong> <strong>Clinic</strong> staff in 1980 as the third<br />
member in the Section of Emergency<br />
Medicine. He completed a fellowship<br />
and residency at <strong>Mayo</strong>. A native of the<br />
Chicago area, Dr. Vukov received his<br />
medical degree from Loyola Stritch<br />
School of Medicine in Maywood, Ill.,<br />
and his undergraduate degree from<br />
North Central College in Naperville, Ill.<br />
C. Robert Stanhope, M.D., with a Maasai<br />
patient, in Narok, Kenya, during a 2009 trip.<br />
Larry Vukov, M.D., in Tanzania, East Africa,<br />
in 1998 with a Kenyan missionary.<br />
C. Robert Stanhope, M.D., and Larry Vukov,<br />
M.D., in Guinea, West Africa, in 2009. The<br />
physician colleagues were conducting a medical<br />
clinic in a remote village near Kankan.<br />
<strong>Spring</strong> <strong>2012</strong> 13
iPad app extra<br />
Professional Achievement Award<br />
John Wheat, M.D.<br />
Professor of Community &<br />
Rural Medicine<br />
Professor of Internal Medicine<br />
University of Alabama School<br />
of Medicine, Tuscaloosa<br />
Regional Campus<br />
John Wheat, M.D. (I ’83), was awarded<br />
the 2011 <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong><br />
Association Professional Achievement<br />
Award for his work helping rural<br />
students interested in rural medicine<br />
to enter medical school and become<br />
primary care physicians with the<br />
training necessary to serve rural<br />
populations.<br />
Dr. Wheat’s focus has been on<br />
“growing our own” physicians through<br />
recruiting and training Alabamans to<br />
become primary care physicians and<br />
return to their own or other underserved<br />
rural communities in the state.<br />
He created a pipeline of programs<br />
— middle school through medical<br />
school — to help rural students prepare<br />
for and sustain their commitment to<br />
careers in rural health and medicine.<br />
Since 1993, students from every county<br />
in the state have entered this pipeline,<br />
including 471 high school students,<br />
154 Rural Medical Scholars (medical<br />
John Wheat, M.D. (center), with family medicine residents and medical students<br />
from The University of Alabama College of Community Health Sciences.<br />
students who began the program as<br />
premed graduate and senior undergraduate<br />
students) and 98 minority<br />
high school graduates. Sixty percent<br />
of medical students finishing the<br />
pipeline have entered rural practice<br />
in Alabama.<br />
“No single individual in the<br />
modern era has done more to address<br />
the shortage of primary care physicians<br />
in Alabama than Dr. Wheat,” says<br />
Holley Midgley, former executive vice<br />
president, Alabama Academy of Family<br />
Physicians. “Alabama will continue to<br />
receive the dividends from his work for<br />
many decades.”<br />
Last year, Dr. Wheat was inducted<br />
into the Alabama Healthcare Hall of<br />
Fame. He was named the 2007<br />
Distinguished Educator by the<br />
National Rural Health Association.<br />
Other recognitions include the<br />
Stueland Scholar Award from the<br />
National Farm Medicine Center,<br />
Ira L. Myers Award from the Alabama<br />
Public Health Association and a<br />
commendation from the Alabama<br />
Family Practice Rural Health Board.<br />
Dr. Wheat practices at the University<br />
of Alabama’s University Medical<br />
Center in Tuscaloosa. He completed a<br />
fellowship at the University of North<br />
Carolina at Chapel Hill, and a residency<br />
at <strong>Mayo</strong> <strong>Clinic</strong>. He received his medical<br />
degree from the University of Alabama<br />
School of Medicine and a master’s degree<br />
in public health from the University of<br />
North Carolina at Chapel Hill. His<br />
undergraduate degree is from the<br />
University of Alabama.<br />
14 <strong>Mayo</strong> <strong>Alumni</strong>
iPad app extra<br />
The Plummer Society Award for Excellence<br />
Presented by The Plummer Society to an alumnus or alumna, nominated by his or her peers, to honor excellence<br />
and unique contributions to practice, education, research or administration in Internal Medicine and subspecialties<br />
S. Ann Colbourne, M.D.<br />
Director, Division of General<br />
Internal Medicine<br />
Professor of Medicine<br />
University of Alberta, Canada<br />
Ann Colbourne, M.D. (I ’93, ADGM<br />
S. ’94), was recognized with The<br />
Plummer Society Award for Excellence<br />
for her contributions to health care<br />
delivery, policy and patient care.<br />
A professor of medicine and<br />
director of the Division of General<br />
Internal Medicine at the University<br />
of Alberta, Canada, Dr. Colbourne’s<br />
clinical passion is diabetes care, with<br />
emphasis on health promotion and<br />
disease prevention. She leads a<br />
thriving telehealth initiative for<br />
insulin pump patients in<br />
Newfoundland, Canada, and is<br />
formalizing linkage with a primary<br />
care network in Alberta to explore<br />
issues in clinical care delivery and<br />
to enhance diabetes care.<br />
Dr. Colbourne’s medical career<br />
spans the continuum from a district<br />
medical officer for four nursing stations<br />
in southeast coastal Labrador through<br />
health services leadership in policy<br />
and practice. Her internal medicine<br />
specialty practice progressed from a<br />
solo internal medicine practice in<br />
northern Newfoundland and Labrador<br />
to university-affiliated practices in<br />
St. John’s, Newfoundland, and<br />
Edmonton, Alberta.<br />
For the Alberta Health Services,<br />
Dr. Colbourne is associate zone medical<br />
director, Edmonton zone division chief<br />
and site service chief of medicine at the<br />
University of Alberta Hospital. In her<br />
provincial capacity as medical director<br />
of care transformation, Alberta Health<br />
Services, Dr. Colbourne works with<br />
clinical teams, middle managers and<br />
decision makers to transform care<br />
processes toward an interprofessional<br />
integrated plan of care for all patients<br />
and families.<br />
As physician lead for chronic<br />
disease prevention and management,<br />
Dr. Colbourne has health policy<br />
experience with the Newfoundland<br />
Labrador Ministry of Health. She<br />
also has extensive local, regional<br />
and national committee experience,<br />
including pharmacy and therapeutics,<br />
health technology assessment<br />
(Canadian Agency for Drugs and<br />
Technologies in Health), health services<br />
and quality of care.<br />
Dr. Colbourne completed a residency<br />
in Internal Medicine at <strong>Mayo</strong> <strong>Clinic</strong><br />
and received her medical degree from<br />
Memorial University in Newfoundland,<br />
Canada. She has a master’s degree<br />
from the University of Oxford in the<br />
United Kingdom, where she was a<br />
Rhodes Scholar. She has bachelor’s<br />
degrees from Memorial University<br />
and the University of Oxford. She is<br />
a fellow of the Royal College of<br />
Physicians and Surgeons and a fellow<br />
of the American College of Physicians.<br />
As part of her residency at <strong>Mayo</strong><br />
<strong>Clinic</strong>, S. Ann Colbourne, M.D.,<br />
worked on a project comparing<br />
the population of Olmsted<br />
County, Minnesota, with<br />
northern Newfoundland and<br />
Labrador, Canada. Here, in 1993,<br />
she collected samples for a<br />
measles seroprevalance study<br />
from a patient in a coastal<br />
Labrador community.<br />
<strong>Spring</strong> <strong>2012</strong> 15
The Priestley Society W. Deprez Inlow Award<br />
Presented by The Priestley Society to a general surgery resident for excellence in research<br />
On Resident Education Day in February, six general surgery residents from Arizona, Florida and Rochester compete<br />
in an academic competition. Each resident presents a research project via teleconference to staff physicians, who<br />
ask questions and rate the presentations. The resident with the highest score wins the W. Deprez Inlow Award —<br />
an all-expenses-paid trip to The Priestley Society meeting and the honor of presenting the first paper at the event.<br />
Lee Joseph McGhan, M.B., B.Ch.<br />
Resident, Division of General Surgery<br />
Department of Surgery<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Arizona<br />
L<br />
ee Joseph McGhan, M.B., B.Ch.<br />
(PRES ’09, S ’14), completed a<br />
preliminary residency in General<br />
Surgery at <strong>Mayo</strong> <strong>Clinic</strong> in Arizona and<br />
a year of research, investigating the<br />
role of the androgen receptor in<br />
triple-negative breast cancer. Currently,<br />
he is a categorical resident in General<br />
Surgery. His research interests include<br />
breast oncology, management of the<br />
axilla in breast cancer patients, staging<br />
of gastric cancer, hormone receptor<br />
expression in breast cancer, and<br />
melanoma. He plans to pursue a<br />
fellowship in surgical oncology.<br />
Dr. McGhan’s work has led to<br />
multiple oral plenary presentations<br />
at national meetings, including the<br />
American Society of Breast Surgeons<br />
and the Society for Surgery of the<br />
Alimentary Tract. He also has been<br />
accepted to present at the annual<br />
meetings of the Society of Surgical<br />
Oncology, Southwestern Surgical<br />
Congress and American College of<br />
Surgeons. His publications have been<br />
featured in journals including Annals<br />
of Surgical Oncology and Journal of<br />
Gastrointestinal Surgery.<br />
He received his bachelor of medicine<br />
and bachelor of surgery degrees from<br />
the University of Wales College of<br />
Medicine in Cardiff. He is a native of<br />
South Wales, United Kingdom.<br />
The Priestley Society is a <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association society for surgeons<br />
who trained at <strong>Mayo</strong> <strong>Clinic</strong> or who are current or former members of the<br />
<strong>Mayo</strong> Department of Surgery staff. The society was named for James T.<br />
Priestley, M.D., a prominent <strong>Mayo</strong> <strong>Clinic</strong> surgeon who had significant<br />
enthusiasm for teaching residents the care of patients and the craft of surgery.<br />
The W. Deprez Inlow Award was established in 2004 by a gift from the<br />
extended family of Robert and Robbie Inlow in honor of Dr. Robert Inlow’s<br />
father, W. Deprez Inlow, M.D., who trained in surgery at <strong>Mayo</strong> <strong>Clinic</strong><br />
from 1919−1921.<br />
16 <strong>Mayo</strong> <strong>Alumni</strong>
ReMine Lecturer<br />
Presented by The Priestley Society to a speaker at the pinnacle of his or her career who represents the heart<br />
and soul of the Society, as nominated by the Executive Committee<br />
Peter Gloviczki, M.D.<br />
Consultant, Division of Vascular and<br />
Endovascular Surgery<br />
Professor of Surgery<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Rochester<br />
Peter Gloviczki, M.D. (VASS ’83,<br />
S ’87), has an extensive clinical<br />
practice that includes all areas of<br />
vascular surgery. He has a special<br />
interest in aortic, mesenteric and<br />
renovascular surgery, aortic endografts,<br />
critical limb ischemia, reconstruction of<br />
large veins, endoscopic perforator vein<br />
surgery, surgery for varicose veins and<br />
chronic venous insufficiency and<br />
lymphatic microsurgery.<br />
Dr. Gloviczki joined the <strong>Mayo</strong><br />
<strong>Clinic</strong> staff in 1989, and was chair of the<br />
Division of Vascular and Endovascular<br />
Surgery at <strong>Mayo</strong> <strong>Clinic</strong> in Rochester<br />
from 2000−2010 and director of the<br />
<strong>Mayo</strong> <strong>Clinic</strong> Gonda Vascular Center<br />
from 2002−2010. He mentored 70<br />
categorical vascular surgery fellows<br />
and 25 research fellows.<br />
Dr. Gloviczki is president-elect of<br />
the Society for Vascular Surgery and<br />
past president of the World Federation<br />
of Vascular Societies, American Venous<br />
Forum, Society for <strong>Clinic</strong>al Vascular<br />
Surgery, International Union of<br />
Angiology, Vascular Disease Foundation,<br />
American Venous Forum Foundation,<br />
Midwestern Vascular Surgical Society<br />
and Gulf Coast Vascular Society. He<br />
is editor-in-chief of Vascular and<br />
Endovascular Surgery and Perspectives<br />
in Vascular Surgery and Endovascular<br />
Therapy. He is on the editorial boards<br />
of several other journals and has<br />
co-edited multiple editions of textbooks.<br />
He has authored more than<br />
300 full-length peer-reviewed original<br />
articles and more than 150 book<br />
The ReMine Lectureship<br />
was established in 2005 to<br />
honor William J. ReMine,<br />
M.D., a gastrointestinal<br />
surgeon who practiced at<br />
<strong>Mayo</strong> <strong>Clinic</strong> in Rochester<br />
for 31 years.<br />
chapters or reviews. He has given<br />
more than 400 presentations, many at<br />
national and international meetings.<br />
He was a co-director of the <strong>Mayo</strong> <strong>Clinic</strong><br />
International Vascular Symposia,<br />
organized in Budapest and Paris.<br />
He is a fellow of the American<br />
College of Surgeons and was the sixth<br />
Carl W. Hughes Distinguished Lecturer<br />
of the Society for Military Vascular<br />
Surgery. He received the Merit Medal<br />
of the Brazilian Society of Angiology<br />
and Vascular Surgery. For his<br />
contributions to French medicine, he<br />
received the Medal of the City of Paris.<br />
Dr. Gloviczki completed a residency<br />
and fellowships at <strong>Mayo</strong> <strong>Clinic</strong>, and<br />
residencies at Hospital St. Michel and<br />
Hospital St. Joseph, both in Paris, France.<br />
He completed a fellowship in vascular<br />
surgery and a residency in general<br />
surgery at Semmelweis University in<br />
Budapest, Hungary. He received his<br />
medical degree from Semmelweis<br />
University.<br />
<strong>Spring</strong> <strong>2012</strong> 17
Advancing<br />
An Ideal<br />
In his new role as <strong>Mayo</strong>’s leader in Arizona,<br />
Wyatt Decker, M.D., is poised to help<br />
<strong>Mayo</strong> <strong>Clinic</strong> shape the future of health care.<br />
Wyatt Decker, M.D.<br />
Wyatt Decker arrived in Rochester, Minn., in 1986 to<br />
embark on a medical career. Had he not selected <strong>Mayo</strong><br />
Medical School for his education, his father — a physician<br />
himself — might have argued against his career choice.<br />
“My father felt many medical schools were focused less<br />
on the needs of the patient and more on acquiring research<br />
grants, while their doctors obsessed over building their<br />
careers,” says Dr. Decker (MMS ’90, I ’93), recounting his<br />
father’s views of increasingly selfish motivations in the field<br />
of medicine.<br />
Twenty-five years later, Dr. Decker is poised to defend<br />
and advance the ideals dear to his father’s heart. In<br />
May 2011, Dr. Decker was named vice president and CEO<br />
of <strong>Mayo</strong> <strong>Clinic</strong> in Arizona. “<strong>Mayo</strong> <strong>Clinic</strong>, as a nationally<br />
Vice President and CEO, <strong>Mayo</strong> <strong>Clinic</strong>, Arizona<br />
Consultant, Department of Emergency Medicine,<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Arizona<br />
Professor of Emergency Medicine, College<br />
of Medicine, <strong>Mayo</strong> <strong>Clinic</strong><br />
Postgraduate: M.B.A., Kellogg School of<br />
Management, Northwestern University<br />
Residency: Emergency Medicine, Denver Health<br />
and Hospitals, Denver; Internal Medicine, <strong>Mayo</strong><br />
School of Graduate Medical Education, Rochester<br />
Medical school: <strong>Mayo</strong> Medical School<br />
Undergraduate: University of California Santa Cruz<br />
18 <strong>Mayo</strong> <strong>Alumni</strong>
ecognized leader in health care, is<br />
in a position to help shape the future<br />
of how patients are cared for, how<br />
physicians and nurses are educated,<br />
and how medical research is conducted,”<br />
he says. “Combined, these influences<br />
will determine how medical care in<br />
our country is practiced.”<br />
<strong>Mayo</strong> <strong>Clinic</strong> in Arizona is shaping<br />
the way patients are cared for in many<br />
ways, including innovative e-health<br />
initiatives designed to provide <strong>Mayo</strong><br />
expertise in rural communities. The<br />
<strong>Mayo</strong> <strong>Clinic</strong> Telestroke Program, which<br />
began in 2007, connects rural hospital<br />
emergency departments with stroke<br />
specialists at the <strong>Mayo</strong> <strong>Clinic</strong> Hospital<br />
in Phoenix via telemedicine. Using a<br />
digital video camera and Internet<br />
telecommunications, vascular neurologists<br />
at <strong>Mayo</strong> <strong>Clinic</strong> perform live<br />
real-time audiovisual consultations to<br />
diagnose patients with acute strokes<br />
and prescribe clot-busting therapies<br />
(thrombolytics) immediately, before<br />
long-term disabilities develop. This<br />
program has been very effective at<br />
reducing and even eliminating longterm<br />
stroke disabilities in patients who<br />
have limited access to health care.<br />
Dr. Decker sees great opportunities<br />
for <strong>Mayo</strong> <strong>Clinic</strong> to lead the nation during<br />
the shifting political and economic<br />
landscape that is moving the United<br />
States toward a national health care<br />
system. “There’s a lot of uncertainty<br />
nationally about where the medical<br />
profession, patient care and reimbursement<br />
models are headed,” he says. “Our<br />
country has a wonderful history and<br />
culture of innovation and independence.<br />
Health care is a complex issue, and<br />
there probably is no single solution that<br />
fits for all individuals. We have many<br />
strengths in our health care here in the<br />
United States, which includes <strong>Mayo</strong><br />
<strong>Clinic</strong>. It would be a shame to implement<br />
a system that reduces health care to a<br />
mediocre level. We need to look to<br />
those organizations providing truly<br />
superb care to see how we can raise the<br />
bar across the board and provide truly<br />
outstanding medical care to all of our<br />
nation’s citizens.”<br />
Triple-Decker<br />
Dr. Decker’s career has involved<br />
working at all three <strong>Mayo</strong> <strong>Clinic</strong><br />
campuses. He developed the<br />
Emergency Medicine Residency<br />
Program at <strong>Mayo</strong> <strong>Clinic</strong> in<br />
Rochester and served as its<br />
inaugural director from 1997 to<br />
2003. He became the first chair<br />
of the Department of Emergency<br />
Medicine at <strong>Mayo</strong> <strong>Clinic</strong> in<br />
Rochester in 2000. During that<br />
eight-year tenure, he transformed<br />
care in Rochester and in Jacksonville,<br />
where he shepherded the Emergency<br />
Department at <strong>Mayo</strong> <strong>Clinic</strong> in<br />
Florida through the transition from<br />
outsourced, contracted physicians<br />
to a full-time <strong>Mayo</strong> <strong>Clinic</strong> staff<br />
model of care and into the new<br />
hospital, simultaneously serving<br />
as the department chair in Florida<br />
for three years. Today, he calls<br />
<strong>Mayo</strong> <strong>Clinic</strong> in Arizona home.<br />
<strong>Spring</strong> <strong>2012</strong> 19
1 9 8 6 - 2 0 1 1<br />
<strong>Mayo</strong> <strong>Clinic</strong> in Florida celebrated its 25th anniversary<br />
in October. More than half a million patients from<br />
all 50 states and 143 countries have come to <strong>Mayo</strong> <strong>Clinic</strong><br />
in Florida for care.<br />
“The past 25 years have been filled with tremendous<br />
medical breakthroughs for our patients,” says William<br />
Rupp, M.D. (ONCL ’08), chief executive officer of <strong>Mayo</strong><br />
<strong>Clinic</strong> in Florida. “Our model of care combines research<br />
and education on the same campus where we provide<br />
patient care, with all three disciplines working together<br />
to develop medical innovations that ultimately save and<br />
improve our patients’ lives.”<br />
The 1986 expansion into northeast Florida marked the<br />
first time <strong>Mayo</strong> <strong>Clinic</strong> established a location outside of<br />
Rochester, Minn. Since opening its doors in Jacksonville,<br />
<strong>Mayo</strong> has grown from one four-story building to three<br />
main patient care buildings, a hospital, two research<br />
buildings and a collection of freestanding centers,<br />
administrative buildings and support facilities.<br />
<strong>Mayo</strong> <strong>Clinic</strong> in Florida started with 35 physicians<br />
and 145 support staff, and today has approximately<br />
4,900 employees and an annual impact of $1.6 billion<br />
on the Florida economy.<br />
SIGNIFICANT MILESTONES<br />
1997 Treating tremor with the first deep brain<br />
stimulation procedure<br />
1998 Discovering the first genetic cause for<br />
frontotemporal dementia<br />
1999 Identifying a new risk-factor gene for<br />
Parkinson’s disease<br />
1998 — Performing more than 3,800 organ transplants,<br />
2011 including liver, heart, lung, kidney and pancreas<br />
transplants and multi-organ procedures<br />
2001 Developing a pioneering lab model to study<br />
Alzheimer’s disease<br />
2002 Being designated a Comprehensive Cancer<br />
Center by the National Cancer Institute<br />
2008 Opening <strong>Mayo</strong> <strong>Clinic</strong> hospital on the Jacksonville<br />
campus to fully integrate inpatient and<br />
outpatient care<br />
2010 Offering the area’s first robotic surgery for<br />
less-invasive partial knee replacement surgery<br />
2011 Opening a simulation center where physicians<br />
in training can learn new skills in a risk-free<br />
environment<br />
2011 Opening the Gabriel House of Care to help<br />
transplant and cancer patients with extended-stay,<br />
affordable lodging during treatment<br />
2011 Opening a new $3.8 million, 10,000-square-foot<br />
freestanding Sleep Center<br />
20 <strong>Mayo</strong> <strong>Alumni</strong>
<strong>Mayo</strong> <strong>Clinic</strong> Distinguished <strong>Alumni</strong> Award<br />
2011 Recipients<br />
honoring ExcEllEncE in pAtiEnt cArE, rEsEArch And EducAtion<br />
T<br />
he <strong>Mayo</strong> <strong>Clinic</strong> Board of Trustees established the <strong>Mayo</strong> <strong>Clinic</strong><br />
Distinguished <strong>Alumni</strong> Award in 1981 to acknowledge and show<br />
appreciation for the exceptional contributions of <strong>Mayo</strong> alumni to the field of<br />
medicine, including medical practice, research, education and administration.<br />
Individuals who have received the award have been recognized nationally<br />
and often internationally in their fields.<br />
The 2011 <strong>Mayo</strong> <strong>Clinic</strong> Distinguished <strong>Alumni</strong> Awards were presented<br />
on Oct. 27, 2011.<br />
The 2011 Distinguished <strong>Alumni</strong> Award recipients are (from left) Keith Kelly, M.D.,<br />
Gene Hunder, M.D., Guillermo Ruiz-Argüelles, M.D., and Richard Brubaker, M.D.<br />
<strong>Spring</strong> <strong>2012</strong> 21
<strong>Mayo</strong> <strong>Clinic</strong> Distinguished <strong>Alumni</strong> Award<br />
iPad app extra<br />
Richard Brubaker, M.D.<br />
Emeritus Professor, Ophthalmology, College of Medicine, <strong>Mayo</strong> <strong>Clinic</strong><br />
Paved the way to fundamental<br />
understanding of mechanisms of<br />
ocular physiology and glaucoma<br />
The research of Richard Brubaker,<br />
M.D. (OPH ’70), revolutionized<br />
the understanding and treatment of<br />
glaucoma. His investigations on<br />
aqueous humor dynamics led to a<br />
greater understanding of normal and<br />
abnormal physiology, leading to new<br />
drugs for the treatment of glaucoma.<br />
He designed and built a scanning laser<br />
fluorophotometer to measure aqueous<br />
flow, and was able to ascertain the<br />
mechanism of function of new drug<br />
therapies because of his perfusion<br />
models and profound understanding<br />
of aqueous circulation. His invention<br />
is now standard in ocular physiology<br />
laboratories and glaucoma clinical<br />
research units around the world.<br />
<strong>Mayo</strong> <strong>Clinic</strong>, 1970−2000, consultant,<br />
Department of Ophthalmology,<br />
Professor of Ophthalmology<br />
Residency (Ophthalmology):<br />
Massachusetts Eye and Ear<br />
Infirmary<br />
Medical school: Harvard<br />
Medical School<br />
Graduate: Harvard Business<br />
School<br />
Undergraduate: Davidson<br />
College, North Carolina<br />
Native of: Georgia<br />
Gene Hunder, M.D.<br />
Emeritus Professor, Internal Medicine, College of Medicine, <strong>Mayo</strong> <strong>Clinic</strong><br />
Gene Hunder, M.D. (I ’63), is the<br />
single most-recognized and<br />
respected individual for work done<br />
in giant cell arteritis and polymyalgia<br />
rheumatica. Dr. Hunder almost singlehandedly<br />
defined the clinical spectrum<br />
of giant cell arteritis and was a major<br />
force in naming the disease. He made<br />
wide-reaching contributions to the<br />
understanding of the disease target<br />
tissues and clinical complications,<br />
and refined the therapeutic approach.<br />
Today’s work in these disorders is built<br />
on his foundations. Current Contents<br />
identifies him as one of the world’s<br />
most cited authors.<br />
Internationally recognized icon<br />
in rheumatology<br />
<strong>Mayo</strong> <strong>Clinic</strong>, 1964−1999, consultant,<br />
Division of Rheumatology,<br />
Professor of Internal Medicine<br />
Fellowship: Strong Memorial Hospital/<br />
University of Rochester Medical<br />
School, Rochester, N.y.<br />
Residency (Internal Medicine,<br />
Rheumatology): <strong>Mayo</strong> School<br />
of Graduate Medical Education<br />
Medical school: University<br />
of Minnesota Medical School,<br />
Minneapolis<br />
Graduate (M.S.): University<br />
of Minnesota, Minneapolis<br />
Undergraduate: University<br />
of Minnesota<br />
Native of: Lake City, Minn.<br />
22 <strong>Mayo</strong> <strong>Alumni</strong>
Keith Kelly, M.D.<br />
<strong>Mayo</strong> <strong>Clinic</strong> Distinguished <strong>Alumni</strong> Award<br />
iPad app extra<br />
Emeritus Professor of Surgery, College of Medicine, <strong>Mayo</strong> <strong>Clinic</strong><br />
World-renowned expert in<br />
gastrointestinal motility<br />
Keith Kelly, M.D. (PHyS ’67),<br />
is an internationally known<br />
gastrointestinal surgeon and expert<br />
in gastrointestinal motility. He was<br />
instrumental in starting much of<br />
<strong>Mayo</strong>’s clinical program on continenceproducing<br />
operations after total<br />
colectomy — first the Koch pouch and<br />
then the ileoanal anastomosis. <strong>Mayo</strong><br />
<strong>Clinic</strong> became the pre-eminent surgical<br />
center for total proctocolectomy with<br />
ileal pouch and anastomosis due to<br />
Dr. Kelly’s pioneering work. He was an<br />
NIH-funded researcher in basic science<br />
for most of his career at <strong>Mayo</strong> <strong>Clinic</strong><br />
and was recognized with the NIH<br />
Merit Award for distinguished service.<br />
<strong>Mayo</strong> <strong>Clinic</strong>, 1968−2000, consultant,<br />
Department of Surgery, Professor<br />
of Surgery<br />
Fellowship: University of<br />
Amsterdam, The Netherlands;<br />
<strong>Mayo</strong> <strong>Clinic</strong>, Rochester<br />
Residency (Surgery): University of<br />
Washington School of Medicine<br />
and Affiliated Hospitals, Seattle<br />
Medical school: University<br />
of Chicago<br />
Graduate (M.S.): University<br />
of Washington, Seattle<br />
Undergraduate: University<br />
of Illinois, Urbana<br />
Native of: Chicago<br />
Guillermo Ruiz-Argüelles, M.D.<br />
Director General, Centro de Hematologia y Medicina Interna de Puebla, <strong>Clinic</strong>a Ruiz<br />
Director, Teaching and Research Division, Laboratorios <strong>Clinic</strong>os de Puebla, <strong>Clinic</strong>a Ruiz<br />
Professor of Hematology, Universidad Popular Autónoma del Estado de Puebla and Universidad de las Americas Puebla<br />
Internationally recognized hematologist<br />
Guillermo Ruiz-Argüelles, M.D.<br />
(HEM ’83), is an internationally<br />
recognized hematologist who has<br />
made significant contributions to the<br />
management of patients with leukemia,<br />
lymphoma and aplastic anemia. He was<br />
the first scientist to show the feasibility<br />
of outpatient stem cell transplantation<br />
in hematologic malignancies —<br />
chronic myelogenous leukemia, in<br />
particular. He started a low-intensity<br />
bone marrow transplant program, with<br />
modifications designed to meet the<br />
needs of patients in developing countries<br />
with limited resources. The outcomes<br />
of the transplanted patients are<br />
comparable to the results obtained<br />
with imatinib mesylate.<br />
Fellowship (Hematology): <strong>Mayo</strong><br />
School of Graduate Medical<br />
Education<br />
Residency (Internal Medicine,<br />
Hematology): Instituto Nacional<br />
de la Nutricion Salvador Zubiran/<br />
Universidad Nacional Autónoma<br />
de México<br />
Medical school: Universidad<br />
Autónoma de San Louis Potosi,<br />
Mexico<br />
Undergraduate: Instituto<br />
Militarizado Orienta, Puebla, Mexico<br />
Native of: Puebla, Mexico<br />
<strong>Spring</strong> <strong>2012</strong> 23
<strong>Mayo</strong> Update<br />
Board of Trustees news<br />
The <strong>Mayo</strong> <strong>Clinic</strong> Board of Trustees<br />
welcomed a new member and<br />
re-elected another at its quarterly<br />
meeting in November.<br />
New trustee<br />
Randolph Steer, M.D., Ph.D.<br />
Independent biotechnology consultant<br />
Re-elected trustee<br />
Tom Brokaw<br />
Journalist<br />
For more information, visit<br />
http://www.mayoclinic.org/news2011-<br />
jax/6534.html.<br />
Obituaries<br />
Perren Baker, M.D. (OR ’53),<br />
died Nov. 5, 2009.<br />
Luis Bonilla, M.D. (TS-G ’95, CS ’98,<br />
S ’08, TS ’11), died Dec. 26, 2011.<br />
Mark Callahan, M.D. (I ’81, CV ’84),<br />
died Dec. 28, 2011.<br />
John Cameron, M.D. (S ’44),<br />
died Nov. 19, 2011.<br />
Franklin Ellis, M.D. (S ’46, TS ’53),<br />
died Sept. 25, 2011.<br />
Henry Helmholz Jr., M.D. (PHYS ’42),<br />
died Jan. 7, <strong>2012</strong>.<br />
Lowell Henderson, M.D. (I ’44),<br />
died Jan. 7, <strong>2012</strong>.<br />
Emerson Moffitt, M.D. (ANES ’57),<br />
died April 30, 2011.<br />
Jean Rey-Bellet, M.D. (N ’54),<br />
died Dec. 8, 2011.<br />
Burton Sandok, M.D. (N ’69),<br />
died Dec. 21, 2011.<br />
Geraldine St. Onge, M.D. (I ’70, GI ’72),<br />
died Dec. 28, 2011.<br />
David Utz, M.D. (U ’58),<br />
died Oct. 30, 2011.<br />
Horst Zincke, M.D. (U ’74),<br />
died Sept. 30, 2011.<br />
Complete obituaries and the Update section,<br />
with alumni and staff news, are available on<br />
the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association website,<br />
alumniconnections.com/olc/pub/MAYO/.<br />
Correction<br />
In the print edition of the winter issue<br />
of <strong>Mayo</strong> <strong>Alumni</strong>, the year in which<br />
Louis Wilson, M.D., died was incorrect.<br />
Dr. Wilson died in 1943.<br />
<strong>Mayo</strong> <strong>Clinic</strong> remembers Luis Bonilla, M.D., and David Hines<br />
The <strong>Mayo</strong> <strong>Clinic</strong> community was deeply saddened to learn of<br />
the loss of Luis Bonilla, M.D. (TS-G ’95, CS ’98, S ’08, TS ’11),<br />
a <strong>Mayo</strong> <strong>Clinic</strong> cardiac surgeon, and David Hines, a <strong>Mayo</strong> <strong>Clinic</strong><br />
procurement technician. They were on board a helicopter<br />
flight from <strong>Mayo</strong> <strong>Clinic</strong> in Florida, along with the pilot,<br />
E. Hoke Smith, to procure a heart for a <strong>Mayo</strong> <strong>Clinic</strong> transplant<br />
patient when the helicopter crashed. There were no survivors.<br />
“This is a great loss to <strong>Mayo</strong> <strong>Clinic</strong> and the transplant<br />
community,” says John Noseworthy, M.D. (N ’90), <strong>Mayo</strong><br />
<strong>Clinic</strong> president and CEO. “We know that our transplant<br />
procurement staff put themselves at risk each day to offer<br />
the hope of a lifesaving transplant to some of our patients in<br />
greatest need. As we mourn this tragic event, we will remember<br />
the selfless and intense dedication they brought each day to<br />
making a difference in the lives of our patients.”<br />
Luis Bonilla, M.D.<br />
David Hines<br />
24 <strong>Mayo</strong> <strong>Alumni</strong>
<strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong><br />
Association Officers<br />
Eric J. Grigsby, M.D., Napa, Calif.<br />
President<br />
Juan M. Sarmiento, M.D., Atlanta<br />
President-Elect<br />
Susheela Bala, M.D., San Bernardino, Calif.<br />
Vice President<br />
Eric S. Edell, M.D., Rochester, Minn.<br />
Secretary-Treasurer<br />
Mark Laney, M.D., St. Joseph, Mo.<br />
Past President<br />
Karen D. Herman, Rochester, Minn.<br />
Director<br />
Executive Editor — Karen Trewin<br />
Editorial Assistant — Emily DeBoom<br />
Advisory Board — Melissa Abrams, Steven Altchuler, M.D., Ph.D.,<br />
Brigitte Barrette, M.D., Karen Barrie, Eric Edell, M.D. (chair), Karen Herman,<br />
Richard Hurt, M.D., Ryan Ledebuhr, Margaret Lloyd, M.D., Lonzetta Neal, M.D.,<br />
Steven Rose, M.D., Karen Trewin, Alexandra Wolanskyj, M.D.<br />
Executive Committee<br />
Peter C. Amadio, M.D., Rochester, Minn.<br />
Sarah Y. Boostrom, M.D., Rochester, Minn.<br />
(MCR-MSGME Representative)<br />
Christopher L. Boswell, Rochester, Minn.<br />
(MMS Representative)<br />
Terrence L. Cascino, M.D., Rochester, Minn.<br />
Diane F. Jelinek, Ph.D., Rochester, Minn.<br />
Siong-Chi, Lin, M.D., Jacksonville, Fla<br />
Lonzetta Neal, M.D., Rochester, Minn.<br />
Meghan M. Painter, Rochester, Minn.<br />
(MGS Representative)<br />
Daniel L. Roberts, M.D., Scottsdale, Ariz.<br />
David K. Teegarden, M.D., Bullard, Texas<br />
Board of Directors 2011–2013<br />
Carl L. Backer, M.D., Winnetka, Ill.<br />
Douglas Chyatte, M.D., Mankato, Minn.<br />
Theresa S. Emory, M.D., Bristol, Tenn.<br />
Alan M. Freedman, M.D., Great Neck, N.Y.<br />
David L. Graham, M.D., Urbana, Ill.<br />
Jennifer Katsolis, D.O, Jacksonville, Fla.<br />
(MCF-MSGME Representative)<br />
Christopher Kramer, M.D., Scottsdale, Ariz.<br />
(MCA-MSGME Representative)<br />
Kennith F. Layton, M.D., Dallas, Texas<br />
Kevin G. Madden, M.D., Scranton, Penn.<br />
Gregory K. Mayer, M.D., Phoenix, Ariz.<br />
M. Mark Melin, M.D., St. Louis Park, Minn.<br />
Nicole W. Pelly, M.D., Seattle, Wash.<br />
Mary M. Reynolds, M.D., Golden, Colo.<br />
Scott R. Ross, D.O., Colorado <strong>Spring</strong>s, Colo.<br />
Guillermo Ruiz-Argüelles, M.D.,<br />
Puebla, Mexico<br />
Marcia J. Sparling, M.D., Vancouver, Wash.<br />
Mack H. Sullivan, M.D., West Bloomfield, Mich.<br />
Pamela B. Sylvestre, M.D., Memphis, Tenn.<br />
Karl F. Tamussino, M.D., Austria<br />
Burkhard W. Wippermann, M.D.,<br />
Hildeshiem, Germany<br />
<strong>Alumni</strong> Center<br />
507-284-2317<br />
Karen Herman, director<br />
507-538-0162<br />
Email: mayoalumni@mayo.edu<br />
Website: http://www.mayo.edu<br />
Physician Referral<br />
Arizona 800-446-2279 (toll-free)<br />
Florida 800-634-1417 (toll-free)<br />
Rochester 800-533-1564 (toll-free)<br />
mayoclinic.org/medicalprofs/<br />
Patient Transportation<br />
<strong>Mayo</strong> <strong>Clinic</strong> MedAir, <strong>Mayo</strong> One<br />
800-237-6822 (toll-free)<br />
mayomedicaltransport.com<br />
For information<br />
about alumni meetings<br />
and receptions,<br />
visit<br />
mayo.edu/alumni<br />
<strong>Alumni</strong> Philanthropy<br />
Contact: Robert W. Giere<br />
Director for <strong>Alumni</strong> Philanthropy<br />
800-297-1185<br />
tdms@mayo.edu<br />
<strong>Mayo</strong> <strong>Alumni</strong> magazine is published quarterly and mailed free of charge to<br />
physicians, scientists and medical educators who studied and/or trained at<br />
<strong>Mayo</strong> <strong>Clinic</strong>, and to <strong>Mayo</strong> consulting staff. The magazine reports on <strong>Mayo</strong> <strong>Clinic</strong><br />
alumni, staff and students, and informs readers about newsworthy activities<br />
throughout <strong>Mayo</strong> <strong>Clinic</strong>. Please send correspondence to: <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong><br />
Center, Siebens 5-33, <strong>Mayo</strong> <strong>Clinic</strong>, 200 First Street S.W., Rochester, MN 55905; or<br />
via e-mail to deboom.emily@mayo.edu; or telephone 507-284-4660; or fax<br />
507-284-8713. Send address changes to the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Center office<br />
at the preceding address or e-mail to mayoalumni@mayo.edu.<br />
<strong>Mayo</strong> <strong>Clinic</strong> is committed to creating and sustaining an environment that<br />
respects and supports diversity in staff and patient populations.<br />
<strong>MC4409</strong>rev0412
Division of Public Affairs<br />
<strong>Mayo</strong> <strong>Clinic</strong><br />
Rochester, Minnesota 55905<br />
ADDRESS SERVICE REquESTED<br />
Find <strong>Mayo</strong> <strong>Clinic</strong><br />
Facebook<br />
You Tube<br />
Twitter<br />
<strong>Mayo</strong> <strong>Clinic</strong> Proton Beam Therapy Program<br />
<strong>Mayo</strong> <strong>Clinic</strong> has taken another step toward a new era in<br />
radiation treatment with the groundbreakings for proton beam<br />
therapy programs in Rochester and Arizona. The <strong>Mayo</strong> <strong>Clinic</strong><br />
Proton Beam Therapy Program in Rochester will be located<br />
in the Richard O. Jacobson Building, which broke ground<br />
in September. The facility in Phoenix broke ground in<br />
December. The first treatment room for patients will be<br />
available in 2015.<br />
At the Arizona groundbreaking, Phoenix <strong>Mayo</strong>r-elect<br />
Greg Stanton said: “The commitment by <strong>Mayo</strong> <strong>Clinic</strong> to build<br />
this amazing new cancer treatment facility is exactly why our<br />
region must focus and redouble our commitment to health<br />
care and biosciences. This new therapy will not only save<br />
lives, it will create jobs and positive economic impact, and<br />
will continue the growth of the Phoenix area as a destination<br />
for health care delivery.”<br />
Artist’s rendering of <strong>Mayo</strong> <strong>Clinic</strong> proton beam therapy<br />
facilities in Rochester (left) and Arizona (right).