Techniques for Determining Cardiac Output in the Intensive Care Unit
Techniques for Determining Cardiac Output in the Intensive Care Unit
Techniques for Determining Cardiac Output in the Intensive Care Unit
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
356<br />
Mohammed & Phillips<br />
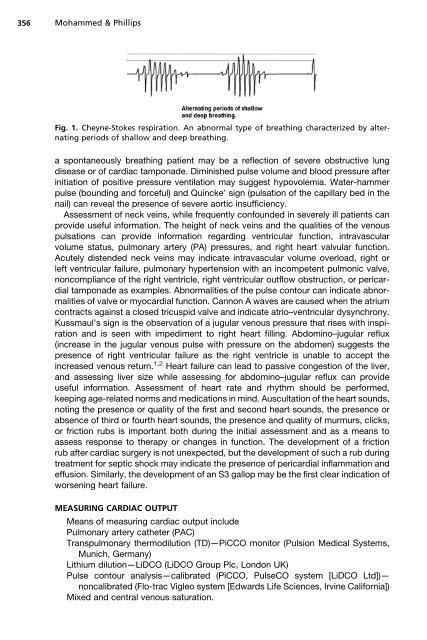
Fig. 1. Cheyne-Stokes respiration. An abnormal type of breath<strong>in</strong>g characterized by alternat<strong>in</strong>g<br />
periods of shallow and deep breath<strong>in</strong>g.<br />
a spontaneously breath<strong>in</strong>g patient may be a reflection of severe obstructive lung<br />
disease or of cardiac tamponade. Dim<strong>in</strong>ished pulse volume and blood pressure after<br />
<strong>in</strong>itiation of positive pressure ventilation may suggest hypovolemia. Water-hammer<br />
pulse (bound<strong>in</strong>g and <strong>for</strong>ceful) and Qu<strong>in</strong>cke’ sign (pulsation of <strong>the</strong> capillary bed <strong>in</strong> <strong>the</strong><br />
nail) can reveal <strong>the</strong> presence of severe aortic <strong>in</strong>sufficiency.<br />
Assessment of neck ve<strong>in</strong>s, while frequently confounded <strong>in</strong> severely ill patients can<br />
provide useful <strong>in</strong><strong>for</strong>mation. The height of neck ve<strong>in</strong>s and <strong>the</strong> qualities of <strong>the</strong> venous<br />
pulsations can provide <strong>in</strong><strong>for</strong>mation regard<strong>in</strong>g ventricular function, <strong>in</strong>travascular<br />
volume status, pulmonary artery (PA) pressures, and right heart valvular function.<br />
Acutely distended neck ve<strong>in</strong>s may <strong>in</strong>dicate <strong>in</strong>travascular volume overload, right or<br />
left ventricular failure, pulmonary hypertension with an <strong>in</strong>competent pulmonic valve,<br />
noncompliance of <strong>the</strong> right ventricle, right ventricular outflow obstruction, or pericardial<br />
tamponade as examples. Abnormalities of <strong>the</strong> pulse contour can <strong>in</strong>dicate abnormalities<br />
of valve or myocardial function. Cannon A waves are caused when <strong>the</strong> atrium<br />
contracts aga<strong>in</strong>st a closed tricuspid valve and <strong>in</strong>dicate atrio–ventricular dysynchrony.<br />
Kussmaul’s sign is <strong>the</strong> observation of a jugular venous pressure that rises with <strong>in</strong>spiration<br />
and is seen with impediment to right heart fill<strong>in</strong>g. Abdom<strong>in</strong>o–jugular reflux<br />
(<strong>in</strong>crease <strong>in</strong> <strong>the</strong> jugular venous pulse with pressure on <strong>the</strong> abdomen) suggests <strong>the</strong><br />
presence of right ventricular failure as <strong>the</strong> right ventricle is unable to accept <strong>the</strong><br />
<strong>in</strong>creased venous return. 1,2 Heart failure can lead to passive congestion of <strong>the</strong> liver,<br />
and assess<strong>in</strong>g liver size while assess<strong>in</strong>g <strong>for</strong> abdom<strong>in</strong>o–jugular reflux can provide<br />
useful <strong>in</strong><strong>for</strong>mation. Assessment of heart rate and rhythm should be per<strong>for</strong>med,<br />
keep<strong>in</strong>g age-related norms and medications <strong>in</strong> m<strong>in</strong>d. Auscultation of <strong>the</strong> heart sounds,<br />
not<strong>in</strong>g <strong>the</strong> presence or quality of <strong>the</strong> first and second heart sounds, <strong>the</strong> presence or<br />
absence of third or fourth heart sounds, <strong>the</strong> presence and quality of murmurs, clicks,<br />
or friction rubs is important both dur<strong>in</strong>g <strong>the</strong> <strong>in</strong>itial assessment and as a means to<br />
assess response to <strong>the</strong>rapy or changes <strong>in</strong> function. The development of a friction<br />
rub after cardiac surgery is not unexpected, but <strong>the</strong> development of such a rub dur<strong>in</strong>g<br />
treatment <strong>for</strong> septic shock may <strong>in</strong>dicate <strong>the</strong> presence of pericardial <strong>in</strong>flammation and<br />
effusion. Similarly, <strong>the</strong> development of an S3 gallop may be <strong>the</strong> first clear <strong>in</strong>dication of<br />
worsen<strong>in</strong>g heart failure.<br />
MEASURING CARDIAC OUTPUT<br />
Means of measur<strong>in</strong>g cardiac output <strong>in</strong>clude<br />
Pulmonary artery ca<strong>the</strong>ter (PAC)<br />
Transpulmonary <strong>the</strong>rmodilution (TD)—PiCCO monitor (Pulsion Medical Systems,<br />
Munich, Germany)<br />
Lithium dilution—LiDCO (LiDCO Group Plc, London UK)<br />
Pulse contour analysis—calibrated (PiCCO, PulseCO system [LiDCO Ltd])—<br />
noncalibrated (Flo-trac Vigleo system [Edwards Life Sciences, Irv<strong>in</strong>e Cali<strong>for</strong>nia])<br />
Mixed and central venous saturation.