Hospital-Associated Costs Due to Surgical Site Infection After Breast ...
Hospital-Associated Costs Due to Surgical Site Infection After Breast ...
Hospital-Associated Costs Due to Surgical Site Infection After Breast ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ORIGINAL ARTICLE<br />
<strong>Hospital</strong>-<strong>Associated</strong> <strong>Costs</strong> <strong>Due</strong> <strong>to</strong> <strong>Surgical</strong> <strong>Site</strong><br />
<strong>Infection</strong> <strong>After</strong> <strong>Breast</strong> Surgery<br />
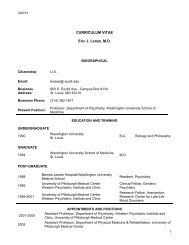
Margaret A. Olsen, PhD, MPH; Sorawuth Chu-Ongsakul, MD, MSc, MHA; Keith E. Brandt, MD;<br />
Jill R. Dietz, MD; Jennie Mayfield, BSN, MPH, CIC; Vic<strong>to</strong>ria J. Fraser, MD<br />
Objective: To determine the attributable costs associated<br />
with surgical site infection (SSI) following breast<br />
surgery.<br />
Design and Setting: Cost analysis of a retrospective<br />
cohort in a tertiary care university hospital.<br />
Patients: All persons who underwent breast surgery other<br />
than breast-conserving surgery from July 1, 1999, through<br />
June 30, 2002.<br />
Main Outcome Measures: <strong>Surgical</strong> site infection and<br />
hospital costs. <strong>Costs</strong> included all those incurred in the<br />
original surgical admission and any readmission(s) within<br />
1 year of surgery, inflation adjusted <strong>to</strong> US dollars in 2004.<br />
Results: <strong>Surgical</strong> site infection was identified in 50<br />
women during the original surgical admission or at readmission<br />
<strong>to</strong> the hospital within 1 year of surgery<br />
(N=949). The incidence of SSI was 12.4% following mastec<strong>to</strong>my<br />
with immediate implant reconstruction, 6.2% following<br />
mastec<strong>to</strong>my with immediate reconstruction using<br />
a transverse rectus abdominis myocutaneous flap, 4.4%<br />
following mastec<strong>to</strong>my only, and 1.1% following breast<br />
reduction surgery. Of the SSI cases, 96.0% were identified<br />
at readmission <strong>to</strong> the hospital. Patients with SSI had<br />
crude median costs of $16 882 compared with $6123 for<br />
uninfected patients. <strong>After</strong> adjusting for the type of surgical<br />
procedure(s), breast cancer stage, and other variables<br />
associated with significantly increased costs using<br />
feasible generalized least squares, the attributable cost of<br />
SSI after breast surgery was $4091 (95% confidence interval,<br />
$2839-$5533).<br />
Conclusions: <strong>Surgical</strong> site infection after breast cancer<br />
surgical procedures was more common than expected for<br />
clean surgery and more common than SSI after non–<br />
cancer-related breast surgical procedures. Knowledge of<br />
the attributable costs of SSI in this patient population can<br />
be used <strong>to</strong> justify infection control interventions <strong>to</strong> reduce<br />
the risk of infection.<br />
Arch Surg. 2008;143(1):53-60<br />
Author Affiliations: Division of<br />
Infectious Diseases, Department<br />
of Medicine (Drs Olsen,<br />
Chu-Ongsakul, and Fraser),<br />
and Divisions of Plastic and<br />
Reconstructive Surgery<br />
(Dr Brandt) and General<br />
Surgery (Dr Dietz), Department<br />
of Surgery, Washing<strong>to</strong>n<br />
University School of Medicine,<br />
and <strong>Infection</strong> Control<br />
Department, Barnes-Jewish<br />
<strong>Hospital</strong> (Dr Mayfield),<br />
St Louis, Missouri.<br />
Dr Chu-Ongsakul is now with<br />
the Department of Surgery,<br />
Siriraj <strong>Hospital</strong> Faculty of<br />
Medicine, Mahidol University,<br />
Bangkok, Thailand. Dr Dietz is<br />
now with the Department of<br />
General Surgery, Cleveland<br />
Clinic, Cleveland, Ohio.<br />
THE OVERALL SURGICAL SITE<br />
infection (SSI) rate following<br />
mastec<strong>to</strong>my reported <strong>to</strong><br />
the Centers for Disease<br />
Control and Prevention National<br />
Nosocomial <strong>Infection</strong>s Surveillance<br />
System from 1992 through 2004 was<br />
1.98%. 1 In contrast, SSI rates published in<br />
individual reports in the literature range<br />
See Invited Critique<br />
at end of article<br />
from 1% <strong>to</strong> 28%. <strong>Surgical</strong> site infection<br />
rates have been reported <strong>to</strong> be lowest following<br />
breast-conserving surgery, ranging<br />
from 1.5% <strong>to</strong> 10.8%. 2-8 The incidence<br />
of SSI following mastec<strong>to</strong>my ranges from<br />
2.8% <strong>to</strong> 25% in the surgical and infection<br />
control literature, 4-7,9-18 although only 2<br />
studies 4,5 report an incidence of less than<br />
5%. The SSI rate following breast cancer<br />
reconstructive surgery also seems <strong>to</strong> be<br />
relatively high (range, 6.3%-28%), based<br />
on a few reports in the literature. 10,19-22<br />
Thus, the SSI rates following breast surgery<br />
seem <strong>to</strong> be much greater than the nationally<br />
reported incidence of 2.0% and<br />
much higher than what is expected for<br />
clean surgical procedures.<br />
Given the state of fiscal constraints<br />
within the US health care system, it is important<br />
<strong>to</strong> calculate the cost-effectiveness<br />
of infection control interventions <strong>to</strong><br />
justify their use from an economic perspective.<br />
Cost-effectiveness analyses require<br />
accurate estimates for the attributable<br />
costs of hospital-acquired infections,<br />
which are lacking for SSI. To our knowledge,<br />
there is only one report in the literature<br />
describing the attributable costs of<br />
SSI following breast surgery. Reilly et al 23<br />
estimated the costs associated with SSI af-<br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
53<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.
ter a variety of different surgical procedures, including<br />
breast surgery. The costs included in this study were those<br />
associated with additional hospital length of stay, outpatient<br />
and home health visits, and outpatient antibiotics.<br />
Using the <strong>to</strong>tal costs attributable <strong>to</strong> infection presented<br />
in their publication, the mean attributable costs<br />
of SSI following breast surgery equaled £359 (approximately<br />
$574 in the United States). 23 It is not clear what<br />
types of breast surgery were included in the analysis (mastec<strong>to</strong>my,<br />
breast-conserving surgery, or cosmetic surgical<br />
procedures) or what proportion of the observed SSI<br />
were diagnosed and treated solely in the outpatient setting.<br />
<strong>Infection</strong>s managed exclusively in an outpatient setting<br />
will presumably be associated with lower costs than<br />
infections requiring rehospitalization. In addition, British<br />
health care delivery and use are different from those<br />
in the United States, so the costs attributable <strong>to</strong> SSI after<br />
breast surgery determined in this study may not be comparable<br />
<strong>to</strong> the costs of SSI in the United States.<br />
Despite the publication of a number of studies describing<br />
costs associated with SSI, the magnitude of economic<br />
costs attributable <strong>to</strong> these infections is still unclear.<br />
<strong>Costs</strong> associated with SSI will likely vary depending<br />
on the type of surgical procedure. <strong>Surgical</strong> site infections<br />
following cardiothoracic or neurosurgical procedures,<br />
with the potential for severe morbidity and mortality,<br />
would presumably have the largest attributable<br />
costs, while infection following surgery not involving major<br />
organ spaces would be expected <strong>to</strong> have lower costs.<br />
This is consistent with the few adjusted estimates of SSI<br />
costs that have been reported. 23-30 We studied the hospitalassociated<br />
costs of SSI following mastec<strong>to</strong>my and breast<br />
reconstructive surgery <strong>to</strong> determine more precisely the<br />
attributable costs of SSI following these procedures.<br />
METHODS<br />
STUDY POPULATION<br />
Procedures eligible for inclusion in this study included all mastec<strong>to</strong>my<br />
and breast reconstructive surgical procedures performed<br />
at Barnes-Jewish <strong>Hospital</strong> (BJH) from July 1, 1999, through<br />
June 30, 2002. Barnes-Jewish <strong>Hospital</strong> is a 1251-bed tertiary care<br />
hospital affiliated with Washing<strong>to</strong>n University School of Medicine.<br />
International Classification of Diseases, Ninth Revision (ICD-9)<br />
procedure codes were used <strong>to</strong> identify eligible surgical admissions<br />
and outpatient surgical procedures, including breast reduction,<br />
augmentation, mastec<strong>to</strong>my, breast reconstruction with transverse<br />
rectus abdominis myocutaneous (TRAM) or other muscle<br />
flap, and insertion of a breast implant (ICD-9 procedure codes<br />
85.31-85.48, 85.7, 85.85, and 85.95). Admissions for breastconserving<br />
surgery (excisional biopsy, lumpec<strong>to</strong>my, or partial mastec<strong>to</strong>my)<br />
and mas<strong>to</strong>pexy only were also excluded, because inpatient<br />
readmission for therapy of SSI after these procedures is rare.<br />
Using these criteria, 949 admissions with breast surgery were included<br />
in the original cohort. Approval for this study was obtained<br />
from the Washing<strong>to</strong>n University School of Medicine Human<br />
Studies Committee.<br />
IDENTIFICATION OF SSI CASE PATIENTS<br />
<strong>Surgical</strong> site infections following breast surgery were identified<br />
by electronic surveillance using data from the BJH Medical<br />
Informatics database. Indica<strong>to</strong>rs suggestive of SSI included<br />
ICD-9 diagnosis codes consistent with wound infection (codes<br />
682.2, 682.3, 998.5, 998.51, 998.59, and 996.69) or breast surgery<br />
complication (codes 611.0, 996.79, 998.3, and 998.83)<br />
and/or positive microbiology wound culture results during the<br />
original surgical admission or any readmission (inpatient or outpatient<br />
surgical) within 1 year of surgery. All potential wound<br />
infections identified by electronic surveillance were verified by<br />
review of the medical records. Centers for Disease Control and<br />
Prevention–National Nosocomial <strong>Infection</strong>s Surveillance System<br />
criteria were used <strong>to</strong> define SSI. <strong>Surgical</strong> site infection required<br />
at least one of the following: purulent drainage from the<br />
incision, organisms isolated from an aseptically obtained culture,<br />
peri-incisional erythema or warmth and the incision was<br />
opened by a physician, abscess found on radiologic or his<strong>to</strong>pathologic<br />
examination, or a diagnosis of SSI by the surgeon.<br />
Only infections diagnosed during the original surgical admission<br />
or at readmission <strong>to</strong> the hospital or <strong>to</strong> outpatient surgery<br />
were included; infections diagnosed and managed solely in the<br />
outpatient setting were excluded, because by definition outpatient<br />
infections would not have associated hospital costs.<br />
VARIABLE CREATION AND DEFINITIONS<br />
Data regarding variables potentially associated with increased<br />
costs were abstracted for the cohort from the BJH Medical Informatics<br />
database. The data available for the entire cohort included<br />
ICD-9 discharge diagnosis and procedure codes, pharmacy<br />
and microbiology data, and demographic information.<br />
Preexisting comorbidities, carcinoma in situ, malignancy, and<br />
his<strong>to</strong>ry of malignancy were defined using the ICD-9 diagnosis<br />
codes assigned during the original surgical admission and the<br />
coding criteria of Deyo et al. 31 Comorbidities selected for analysis<br />
included those generally associated with increased risk of<br />
SSI (eg, diabetes mellitus) and comorbidities that may be more<br />
frequent in the population of patients with SSI and would most<br />
likely be associated with increased costs (eg, serious heart disease).<br />
In addition, frequencies were determined for all ICD-9<br />
diagnosis codes assigned <strong>to</strong> the surgical cohort; all comorbidities<br />
present in more than 1% of the cohort were included in<br />
the statistical analyses. The comorbidities analyzed included<br />
diabetes mellitus, serious heart disease (myocardial infarction<br />
or congestive heart failure), renal failure, chronic obstructive<br />
pulmonary disease, and hypertension. Diagnosis of metastatic<br />
disease was defined using ICD-9 diagnosis codes assigned during<br />
the original surgical admission and any readmission <strong>to</strong> the<br />
hospital within 1 year of surgery. Central venous catheterization<br />
was defined using ICD-9 procedure codes (code 38.93 or<br />
86.07) for the original surgical admission and any hospital readmission<br />
within 1 year of surgery. <strong>Surgical</strong> procedures performed<br />
during the original surgical admission were defined using<br />
ICD-9 procedure codes. All possible logic checks were performed<br />
for variables created from ICD-9 diagnosis and procedure<br />
codes, and discrepant results were verified using the electronic<br />
medical record.<br />
The number of ICD-9 codes assigned during the surgical admission<br />
was used as an indica<strong>to</strong>r of severity of illness rather<br />
than the Charlson comorbidity score (adapted for use with administrative<br />
data), <strong>to</strong> determine the costs associated with specific<br />
comorbidities in this population. The Charlson comorbidity<br />
score is a summary score in which weights are assigned<br />
<strong>to</strong> various comorbidities associated with mortality; because our<br />
intent was <strong>to</strong> develop a precise determination of attributable<br />
costs, we used the individual comorbidities rather than a summary<br />
score in the statistical models <strong>to</strong> calculate costs. 32 In addition,<br />
the Charlson comorbidity score includes diagnosis of<br />
any malignancy in the scoring scheme. Because we wanted <strong>to</strong><br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
54<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.
specifically control for costs associated with tumor stage in the<br />
patients diagnosed as having in situ or invasive breast cancer<br />
in our statistical models, this was an additional rationale for<br />
not using an aggregated comorbidity score in our models <strong>to</strong> adjust<br />
for severity of illness.<br />
Pharmacy data available from the BJH Medical Informatics<br />
database were also used <strong>to</strong> define some underlying disease variables,<br />
including insulin use in the original surgical admission<br />
or within 1 year of surgery, insulin and oral hypoglycemic agents<br />
as markers of diabetes mellitus, and digoxin use as a marker of<br />
serious heart disease. These variables were compared with the<br />
comorbidity variables previously described, <strong>to</strong> verify the diagnostic<br />
variables and <strong>to</strong> assess the effect of variables created by<br />
combination of the diagnostic and pharmacy information.<br />
COST DATA<br />
Cost data for the cohort from the perspective of the hospital,<br />
including the hospital costs of the original surgical admission<br />
and hospital costs for all readmissions within 1 year of surgery,<br />
were obtained from the BJH cost accounting database<br />
(Trendstar; McKesson Corp, Alpharetta, Georgia). Eligible hospital<br />
readmissions included inpatient, same day, or ambula<strong>to</strong>ry<br />
surgery and outpatient surgery admissions. All readmission<br />
hospital costs within 1 year of surgery were included in<br />
the analyses, <strong>to</strong> hopefully capture all costs involved in the initial<br />
diagnosis and therapy of infection. Because SSI in some patients<br />
may require multiple admissions <strong>to</strong> the hospital for antibiotic<br />
or surgical treatment, we included readmission costs<br />
for all members of the cohort for a 1-year follow-up <strong>to</strong> capture<br />
these costs.<br />
The cost accounting database uses a set-down allocation<br />
method <strong>to</strong> calculate costs, which included indirect variable, direct<br />
variable, and fixed costs. All patient charge codes received<br />
during hospitalizations were recorded, and the departmental<br />
cost for each charge code calculated was based on each<br />
department’s actual cost components multiplied by the charges<br />
for that code, divided by <strong>to</strong>tal departmental charges. <strong>Costs</strong> were<br />
summed across each department <strong>to</strong> provide <strong>to</strong>tal hospital costs<br />
for each admission and were inflation adjusted <strong>to</strong> 2004 US dollars<br />
using the medical care component of the Consumer Price<br />
Index (accessed at http://www.bls.gov). Only hospitalassociated<br />
costs were included in the analysis; physician costs<br />
were not included.<br />
STATISTICAL ANALYSES<br />
The 2 test was used <strong>to</strong> compare categorical variables, and the<br />
Mann-Whitney test was used for continuous variables. Multivariate<br />
analyses <strong>to</strong> determine costs attributable <strong>to</strong> SSI were performed<br />
by ordinary least-squares and feasible generalized leastsquares<br />
(FGLS) regression, using natural log-transformed costs<br />
as the dependent variable, because of the highly skewed distribution<br />
of <strong>to</strong>tal costs. These methods can be used <strong>to</strong> estimate<br />
the costs associated with variables of interest, taking in<strong>to</strong> account<br />
variation in the occurrence of other fac<strong>to</strong>rs significantly<br />
associated with expenditures. The coefficients obtained in the<br />
FGLS model represent the mean change in the variable of interest<br />
per unit increase in X, when the other variables in the<br />
model are held constant. In this study, the change in X represents<br />
the mean difference in the natural logarithm of costs between<br />
individuals with infection and those without infection,<br />
holding all other predic<strong>to</strong>rs of costs constant.<br />
All independent variables were checked for colinearity. The<br />
models were checked for functional form misspecification using<br />
the Ramsey regression specification error test and for heteroscedasticity<br />
using the Breusch-Pagan test. 33 The <strong>to</strong>tal mortality<br />
within 1 year of surgery in the cohort was 1.5% (13/878);<br />
because it was so low, no attempt was made <strong>to</strong> adjust the FGLS<br />
models for mortality.<br />
Data for admissions in which the standardized residuals for<br />
the final model were large (3 SDs from the mean of 0) were<br />
all checked for accuracy. Because the FGLS model used the natural<br />
logarithm of costs as the dependent variable, an intermediate<br />
regression was performed <strong>to</strong> predict costs given that the<br />
dependent variable in the model was ln(costs). 33<br />
Propensity score methods were also used <strong>to</strong> determine the<br />
association between SSI and costs. 34 A nonparsimonious logistic<br />
regression model was used <strong>to</strong> obtain predicted values for<br />
SSI. Patients with SSI were then matched 1:1 with control subjects<br />
based on the propensity score. Total costs were compared<br />
between the matched pairs by the Wilcoxon signed rank<br />
test, and the mean and median differences in <strong>to</strong>tal costs were<br />
calculated. Statistical analyses were performed using commercially<br />
available software programs (SPSS, version 12.0 [SPSS<br />
Inc, Chicago, Illinois] and Stata, version 9.2 [Stata Corp, College<br />
Station, Texas]).<br />
RESULTS<br />
SSI RATES IN THE COHORT<br />
A cohort of 949 admissions in which ICD-9 procedure<br />
codes for mastec<strong>to</strong>my or breast reconstruction were assigned<br />
was established for the 2-year period of the study.<br />
Most surgical procedures (90.6%) resulted in at least an<br />
overnight hospitalization, with only 4 patients who underwent<br />
mastec<strong>to</strong>my (0.7%) discharged on the day of surgery.<br />
A <strong>to</strong>tal of 7.6% (14/185) of reduction-only surgical<br />
procedures, 50.8% (33/65) of delayed implant<br />
placement in patients with cancer, and 62.5% (15/24) of<br />
cosmetic augmentations were performed in outpatient surgery.<br />
<strong>Surgical</strong> site infection was identified in 50 patients<br />
within 1 year of surgery in this cohort (SSI rate, 5.3%).<br />
Thirteen infections (4.4%) followed mastec<strong>to</strong>my only, and<br />
22 were breast implant associated, requiring surgical removal<br />
of the implant in 18. <strong>Surgical</strong> site infection in 45<br />
patients involved the breast incision(s), 7 involved the<br />
abdominal incision in patients who had undergone TRAM<br />
reconstruction, and 1 involved the back incision in a woman<br />
who had undergone latissimus dorsi reconstruction. Three<br />
patients had SSI following TRAM reconstruction involving<br />
the breast and abdominal incisions. <strong>Surgical</strong> site infection<br />
rates were lowest following non–cancer-related<br />
surgical procedures. Rates of SSI according <strong>to</strong> the type of<br />
surgery performed are shown in Table 1.<br />
For the outcome and cost analyses, any readmissions<br />
<strong>to</strong> the hospital within 1 year of surgery, including readmissions<br />
in which eligible breast surgical procedures were<br />
performed, were included in the readmission costs associated<br />
with the original surgical admission. A <strong>to</strong>tal of<br />
61 patients had 1 or more follow-up breast surgical procedures<br />
performed within 1 year of the original surgery<br />
that were included in readmission costs, reducing the<br />
number of breast surgical admissions in the outcome cohort<br />
<strong>to</strong> 888. Ten patients had surgical admissions separated<br />
by more than 1 year; these were considered separate<br />
events. Forty patients (4.5%) included in the final<br />
breast surgical admission cohort were male; 33 males underwent<br />
subcutaneous mastec<strong>to</strong>mies or reduction mam-<br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
55<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.
Table 1. <strong>Breast</strong> SSI Rates According <strong>to</strong> Type of <strong>Surgical</strong><br />
Procedure Performed<br />
Type of Surgery a<br />
No. of<br />
<strong>Breast</strong> SSIs/<br />
Total No.<br />
of Patients<br />
No. of<br />
Donor <strong>Site</strong><br />
SSIs/Total No.<br />
of Patients<br />
maplasty because of gynecomastia, while 7 underwent<br />
unilateral mastec<strong>to</strong>mies for surgical removal of a breast<br />
malignancy.<br />
CHARACTERISTICS OF PATIENTS<br />
WITH SSI AND OUTCOMES<br />
SSI<br />
Rate<br />
per<br />
Person<br />
Mastec<strong>to</strong>my only 13/296 NA 4.4<br />
Mastec<strong>to</strong>my plus immediate 15/121 NA 12.4<br />
implant b,c<br />
Mastec<strong>to</strong>my, immediate implant, 2/14 0/14 14.3<br />
plus latissimus dorsi flap d<br />
Delayed implant e,f 5/65 0/3 e 7.7<br />
Implant for augmentation g 0/24 NA NA<br />
Mastec<strong>to</strong>my plus immediate 6/162 j 7/162 j 6.2 j<br />
TRAM flap b,h,i<br />
Delayed TRAM reconstruction e 1/28 0/28 3.6<br />
Mastec<strong>to</strong>my plus latissimus dorsi 1/17 1/17 11.8<br />
flap (no implant) h<br />
Delayed latissimus dorsi flap e,k 0/10 0/10 NA<br />
Reduction surgery only l 2/185 NA 1.1<br />
Subcutaneous mastec<strong>to</strong>my<br />
because of gynecomastia<br />
0/33 NA NA<br />
Abbreviations: NA, data not applicable; SSI, surgical site infection;<br />
TRAM, transverse rectus abdominis myocutaneous.<br />
a There were 949 surgical procedures performed.<br />
b One patient had a tissue expander placed after a failed attempt at TRAM<br />
flap reconstruction.<br />
c Three patients also underwent contralateral reduction.<br />
d One patient also underwent contralateral reduction.<br />
e One patient had a delayed TRAM flap and placement of a tissue expander,<br />
and 2 patients had a delayed latissimus dorsi flap plus implant.<br />
f Three patients had contralateral reductions, and 10 patients also had<br />
nipple reconstruction.<br />
g One patient underwent contralateral reduction.<br />
h Two patients had a TRAM and latissimus dorsi flaps.<br />
i Four patients also underwent contralateral reductions.<br />
j Three patients had donor site and breast SSI.<br />
k Three patients underwent contralateral reduction.<br />
l Seven patients underwent unilateral reduction and contralateral nipple<br />
reconstruction.<br />
Characteristics identified in the surgical cohort and their<br />
associations with subsequent SSI are shown in Table 2.<br />
All of the patients with SSI following breast surgery were<br />
female, and there was no association between SSI and race,<br />
age, and malignant or metastatic breast cancer. Patients<br />
with SSI were significantly more likely <strong>to</strong> have an underlying<br />
diagnosis of diabetes mellitus, <strong>to</strong> be obese (defined<br />
by a body mass index [calculated as weight in kilograms<br />
divided by height in meters squared] 30), <strong>to</strong><br />
have undergone mastec<strong>to</strong>my or a surgical procedure involving<br />
placement of a breast implant, and <strong>to</strong> have a central<br />
venous catheter placed within 1 year of surgery (excluding<br />
catheters placed <strong>to</strong> administer antibiotics due <strong>to</strong><br />
SSI). Patients with SSI had significantly more ICD-9 diagnosis<br />
codes assigned during the breast surgical admission.<br />
<strong>Surgical</strong> site infection was significantly less likely<br />
in patients who had undergone only reduction surgery,<br />
compared with patients who had other procedures<br />
performed.<br />
Information on antibiotic prophylaxis and drain use<br />
and management for individual patients was not available,<br />
because those data were not maintained electronically.<br />
During the study period, the standard of care at our<br />
institution was <strong>to</strong> give all patients undergoing the included<br />
breast surgical procedures1gofcefazolinasprophylaxis<br />
within 1 hour before incision. In a separate analysis<br />
of a case-control subset at our institution that<br />
overlapped the period of this study, 88% of patients were<br />
given cefazolin prophylactically, with the remainder receiving<br />
vancomycin, a combination of ampicillin and sulbactam,<br />
clindamycin, or other antibiotics. Only 2% of patients<br />
in the case-control study were not given prophylactic<br />
antibiotics (M.A.O.; M. Lefta, BS; J.R.D.; K.E.B.; R. Aft,<br />
MD; R. Matthews, MPH; J.M.; and V.J.F.; unpublished<br />
data, 2006). Drains were placed routinely in the remaining<br />
breast tissue or mastec<strong>to</strong>my bed in patients who underwent<br />
mastec<strong>to</strong>my, flap reconstruction, or reduction,<br />
but were not used routinely in patients undergoing cosmetic<br />
augmentation or delayed reconstruction with an<br />
implant. Patients undergoing simple mastec<strong>to</strong>my typically<br />
had a single drain placed in the mastec<strong>to</strong>my bed,<br />
and patients undergoing modified radical mastec<strong>to</strong>my had<br />
2 drains, 1 in the mastec<strong>to</strong>my bed and 1 in the axilla. Patients<br />
undergoing reconstruction with a TRAM flap had<br />
2 drains placed in the abdomen and 1 in the reconstructed<br />
breast, and patients undergoing latissimus dorsi<br />
flap reconstruction had 1 drain placed in the back and<br />
1 in the reconstructed breast. Patients were discharged<br />
from the hospital with the drain(s) in place, and the<br />
drain(s) were generally removed between 7 and 21 days<br />
after surgery when the drainage was less than 1 ounce<br />
per 24 hours.<br />
The median time from surgery until diagnosis of SSI<br />
was 25 days (range, 2-315 days; mean [SD], 46.6 [62.0]<br />
days). Of the 50 patients with SSI, 41 (82.0%) had their<br />
infections diagnosed within 60 days of surgery. Only 2<br />
patients were diagnosed as having an SSI during the original<br />
surgical admission; almost three-quarters of infected<br />
patients (72.0%) were treated during a single readmission<br />
<strong>to</strong> the hospital (Table 3). Thirty patients with<br />
SSI (60.0%) underwent subsequent surgery because of<br />
infection: 18 involved breast implant removal, while 12<br />
involved debridement or incision and drainage of the<br />
wound in the operating room. <strong>Surgical</strong> site infections in<br />
the remaining 20 patients were treated with intravenous<br />
antibiotics with or without bedside drainage or debridement<br />
(Table 3).<br />
COSTS ASSOCIATED WITH SSI<br />
Complete cost data were not available for 4 patients, including<br />
1 with an SSI (following mastec<strong>to</strong>my plus immediate<br />
placement of an implant), resulting in a population<br />
of 884 surgical admissions available for analysis.<br />
The comparisons of the <strong>to</strong>tal costs and hospital length<br />
of stay for the surgical admission plus all readmissions<br />
within 1 year of surgery for the cohort are shown in<br />
Table 4. Patients with SSI had significantly higher hospital<br />
costs associated with surgery and during the 1-year<br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
56<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.
Table 2. Selected Characteristics of the <strong>Breast</strong> <strong>Surgical</strong> Cohort Population and Association With SSI<br />
Characteristic<br />
Patients With SSI<br />
(n=50) a<br />
Uninfected Patients<br />
(n=838) a OR (95% CI) P Value<br />
Female sex 50 (100.0) 798 (95.2) NA .16<br />
Nonwhite race 18 (36.0) 234 (27.9) 1.5 (0.8-2.6) .22<br />
Obesity (BMI, 30) 27 (54.0) 282 (33.7) 2.3 (1.3-4.1) .003<br />
Diabetes mellitus 12 (24.0) 80 (9.5) 3.0 (1.5-6.0) .001<br />
Renal failure 2 (4.0) 7 (0.8) 4.9 (1.0-24.5) .09<br />
Chronic obstructive pulmonary disease 2 (4.0) 33 (3.9) 1.0 (0.2-4.4) .99<br />
Serious heart disease 5 (10.0) 40 (4.8) 2.2 (0.8-5.9) .10<br />
Carcinoma in situ 9 (18.0) 86 (10.3) 1.9 (0.9-4.1) .09<br />
Malignancy 31 (62.0) 460 (54.9) 1.3 (0.7-2.4) .33<br />
Malignancy plus lymph node metastases 14 (28.0) 169 (20.2) 1.5 (0.8-2.9) .18<br />
Metastatic breast cancer 0 24 (2.9) .39<br />
Mastec<strong>to</strong>my 42 (84.0) 562 (67.1) 2.6 (1.2-5.6) .01<br />
Axillary dissection 29 (58.0) 412 (49.2) 1.4 (0.8-2.5) .22<br />
Free TRAM procedure 4 (8.0) 100 (11.9) 0.6 (0.2-1.8) .40<br />
Nonmicrovascular TRAM procedure 7 (14.0) 77 (9.2) 1.6 (0.7-3.7) .31<br />
Latissimus dorsi flap 4 (8.0) 36 (4.3) 1.9 (0.6-5.7) .28<br />
Implant 22 (44.0) 165 (19.7) 3.2 (1.8-5.7) .001<br />
Bilateral surgery 17 (34.0) 306 (36.5) 0.9 (0.5-1.6) .72<br />
Reduction surgery only 2 (4.0) 164 (19.6) 0.2 (0-0.7) .006<br />
Central venous catheter 11 (22.0) 59 (7.0) 3.7 (1.8-7.6) .001<br />
Age, mean (range), y 52.5 (27-82) 51.3 (14-90) NA .41<br />
No. of ICD-9 codes assigned during<br />
surgical admission, mean (range)<br />
3 (1-8) 2 (1-9) NA .001<br />
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CI, confidence interval; ICD-9, International<br />
Classification of Diseases, Ninth Revision (ICD-9); NA, data not applicable; OR, odds ratio; SSI, surgical site infection; TRAM, transverse rectus abdominis<br />
myocutaneous.<br />
a Data are given as number (percentage) of each group unless otherwise indicated.<br />
period after surgery compared with uninfected patients,<br />
and they had a significantly longer <strong>to</strong>tal length of hospital<br />
stay (P.001 for both, Mann-Whitney test). The<br />
crude median costs attributable <strong>to</strong> SSI <strong>to</strong>taled approximately<br />
$10 750, but, as can be seen in Table 4, the range<br />
of costs for the infected and uninfected control patients<br />
was broad. The crude median length of stay attributable<br />
<strong>to</strong> SSI equaled 4.3 days, although the range of length of<br />
stay was also broad for SSI case patients and uninfected<br />
control patients (Table 4).<br />
Feasible generalized least squares was used <strong>to</strong> calculate<br />
the attributable costs of SSI in the year after breast<br />
surgery. The natural logarithm of the <strong>to</strong>tal costs was used<br />
as the dependent variable in the regression model, because<br />
of the highly skewed nature of <strong>to</strong>tal costs. The operative<br />
variables associated with significantly increased<br />
costs included the type of donor flap used <strong>to</strong> reconstruct<br />
breast tissue (free or nonmicrovascular TRAM or<br />
latissimus dorsi flap), placement of an implant immediately<br />
following mastec<strong>to</strong>my, and bilateral surgery<br />
(Table 5). The diagnosis of malignant disease was associated<br />
with significantly increased costs, and metastatic<br />
disease was associated with even greater costs (indicated<br />
by the progressively larger values for the <br />
coefficient). Correspondingly, placement of a central venous<br />
catheter, used as a proxy for chemotherapy, was associated<br />
with increased costs. The only comorbidities associated<br />
with significantly increased costs in this<br />
population were serious heart disease (acute or old myocardial<br />
infarction, congestive heart failure, or digoxin administration<br />
in the hospital in the year after surgery) and<br />
Table 3. Outcomes of SSI in 50 Patients <strong>After</strong><br />
<strong>Breast</strong> Surgery<br />
Characteristic<br />
No. (%)<br />
of Patients<br />
No. of readmissions required for therapy of SSI<br />
0 (diagnosed and treated solely during the<br />
2 (4.0)<br />
original surgical admission)<br />
1 36 (72.0)<br />
2 11 (22.0)<br />
3 1 (2.0)<br />
Type of surgery required <strong>to</strong> treat infection<br />
Removal of breast implant a 18 (36.0)<br />
Incision and drainage or debridement<br />
12 (24.0)<br />
in operating room b<br />
Treated with intravenous antibiotics only 20 (40.0)<br />
Abbreviation: SSI, surgical site infection.<br />
a One patient had the implant removed at an outside hospital because of<br />
infection and was subsequently treated at our institution with intravenous<br />
antibiotics.<br />
b Two patients with donor site SSI had abdominal mesh removed during<br />
surgery.<br />
renal failure. A diagnosis of male gynecomastia and reduction<br />
surgery in females was associated with significantly<br />
decreased costs. Controlling for the other variables<br />
in the model, costs for nonwhite persons were 7.9%<br />
higher in this breast surgical cohort compared with costs<br />
incurred by whites (Table 5). Excluding noncancer surgical<br />
procedures, diagnoses of breast cancer with lymph<br />
node metastases and metastatic breast cancer within 1<br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
57<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.
Table 4. Crude <strong>Costs</strong> and Length of <strong>Hospital</strong> Stay <strong>Associated</strong> With SSI in the Cohort a<br />
Cost Data<br />
LOS Data<br />
<strong>Infection</strong> Status<br />
Mean (SD), $ Median (Range), $ Mean (SD), d Median (Range), d<br />
Patients with SSI (n=49) b 19 901 (14 214) 16 882 (5198-67 763) 8.4 (7.4) 6.3 (1.4-39.3)<br />
Uninfected control patients (n=835) 9973 (10 013) 6123 (1455-120 037) 3.5 (4.4) 2.0 (0.2-47.5)<br />
Abbreviations: LOS, length of stay; SSI, surgical site infection.<br />
a The median cost and median LOS were used <strong>to</strong> calculate the crude cost ($10 759) and LOS (4.3 days) associated with SSI because of the skewed distribution<br />
of both variables.<br />
b Cost data were missing for 1 patient with an SSI.<br />
Table 5. Results of the Feasible Generalized Least-Squares Model for Determining Attributable <strong>Costs</strong> of <strong>Surgical</strong> <strong>Site</strong> <strong>Infection</strong> <strong>After</strong><br />
<strong>Breast</strong> Surgery a<br />
Variable<br />
Proportion<br />
of Patients<br />
Estimated <br />
Coefficient<br />
<strong>Surgical</strong> site infection 0.06 .45 .06 .001<br />
Free TRAM procedure 0.12 1.12 .04 .001<br />
Nonmicrovascular TRAM procedure 0.09 .82 .04 .001<br />
Latissimus dorsi flap 0.04 .50 .07 .001<br />
Implant 0.21 .14 .08 .06<br />
Mastec<strong>to</strong>my plus immediate implant 0.15 .49 .09 .001<br />
Renal failure 0.009 1.28 .18 .001<br />
Serious heart disease 0.05 .52 .09 .001<br />
Diabetes mellitus 0.10 .03 .05 .48<br />
Metastatic cancer b 0.03 .96 .11 .001<br />
Central venous catheter c 0.08 .34 .06 .001<br />
Malignancy 0.55 .12 .04 .001<br />
Bilateral surgery 0.36 .19 .04 .001<br />
Nonwhite race 0.28 .08 .03 .007<br />
Weight, mean, kg 76.90 .001 .0006 .01<br />
Reduction 0.24 −.17 .05 .002<br />
Gynecomastia 0.04 −.43 .08 .001<br />
Abbreviation: TRAM, transverse rectus abdominis myocutaneous.<br />
a Data were also adjusted for number of International Classification of Diseases, Ninth Revision, Clinical Modification codes assigned during surgical admission<br />
(using dummy variables), age, weight, mastec<strong>to</strong>my, and year of surgery. Adjusted R 2 =0.52 for the model after accounting for natural log transformation of costs.<br />
b Diagnosed during the original admission or within 1 year of surgery.<br />
c Inserted within 1 year of surgery.<br />
SE<br />
P<br />
Value<br />
year of surgery were more common in nonwhite compared<br />
with white persons (31.7% vs 25.9% for lymph node<br />
metastases [P=.13] and 6.5% vs 2.5% for metastatic breast<br />
cancer [P=.01]), suggesting that nonwhites present at a<br />
more advanced stage of cancer than do whites.<br />
The attributable cost of SSI in this cohort, adjusted<br />
for the variables previously described and others listed<br />
in Table 5, was $4091 (95% confidence interval, $2839-<br />
$5533) (in 2004 US dollars). The final model presented<br />
in Table 5 had an adjusted coefficient of determination<br />
(R 2 ) of 0.52, indicating that approximately 52% of the<br />
variation in actual costs was explained by the model.<br />
In addition <strong>to</strong> the FGLS model, <strong>to</strong>tal costs were also compared<br />
between SSI cases and controls matched based on<br />
the propensity scores. A nonparsimonious logistic regression<br />
model was developed with SSI as the dependent variable.<br />
Uninfected control patients were matched <strong>to</strong> SSI case<br />
patients based on the propensity score, with 2 SSI case patients<br />
unable <strong>to</strong> be matched. The difference in <strong>to</strong>tal costs<br />
between the matched pairs was significant (P.001, Wilcoxon<br />
signed rank test). The mean difference in <strong>to</strong>tal costs<br />
between the matched SSI and control pairs was $5700, with<br />
a median difference in costs of $3492.<br />
COMMENT<br />
Knowledge of the outcomes of breast surgery, including<br />
SSI and their associated costs, is necessary <strong>to</strong> understand<br />
the impact of these infections in a population of surgical<br />
patients. Our study, using a retrospective cohort of breast<br />
surgical patients treated at a university-affiliated tertiary care<br />
hospital, shows that SSI after breast cancer surgery is more<br />
common than would be expected for clean surgery and more<br />
common than SSI rates after similarly extensive breast surgical<br />
procedures in patients without cancer. Given the relatively<br />
high incidence of SSI after these procedures, it is important<br />
<strong>to</strong> understand their associated costs, <strong>to</strong> develop<br />
prevention strategies and make informed decisions concerning<br />
the potential cost-effectiveness of interventions designed<br />
<strong>to</strong> reduce the risk of SSI. For this reason, it is important<br />
<strong>to</strong> quantify the costs attributable <strong>to</strong> infection as<br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
58<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.
precisely as possible, <strong>to</strong> determine the true magnitude of<br />
hospital-associated costs and, ultimately, societal costs because<br />
of SSI.<br />
In this study, we used FGLS <strong>to</strong> calculate attributable hospital<br />
costs of SSI after breast surgery, controlling for differences<br />
in surgical procedures, comorbidities, stage of breast<br />
cancer, and other fac<strong>to</strong>rs associated with increased costs<br />
in this surgical population. We chose this method because<br />
it allows for the analysis of data from an entire cohort<br />
of surgical patients, in contrast <strong>to</strong> matched-pair studies<br />
in which case patients with SSI are matched <strong>to</strong> control<br />
patients without infection after surgery, resulting in analysis<br />
of only a selected subset of the control population. The<br />
inability <strong>to</strong> match some infected patients with unusual combinations<br />
of comorbidities or severe underlying illness with<br />
comparable control patients is an inherent disadvantage of<br />
the matched-pair method. The ordinary least-squares<br />
method using log-transformed costs as the dependent variable<br />
has recently been shown <strong>to</strong> accurately predict costs<br />
following coronary artery bypass graft surgery in a validation<br />
sample. 35<br />
Most published reports 36,37 addressing the costs of SSI<br />
have used a matched case-control study design, although<br />
this study design is known <strong>to</strong> result in potentially<br />
inaccurate cost estimates, because of selection bias.<br />
The estimated costs of SSI determined in studies in which<br />
some form of adjustment for patient acuity, and other<br />
fac<strong>to</strong>rs associated with increased risk of SSI, were performed,<br />
either by matching or other statistical methods,<br />
range from approximately $3400 <strong>to</strong> $17 700. The adjusted<br />
costs of SSI have been lower following general or<br />
mixed surgical procedures ($3382-$5038) 26,30 and highest<br />
following orthopedic or cardiothoracic surgery<br />
($17 708 for orthopedic SSI and $12 419-$14 211 following<br />
coronary artery bypass surgery). 27-29 These cost<br />
estimates are not necessarily comparable, even for the<br />
same type of surgery, because of differing statistical methods<br />
<strong>to</strong> determine attributable costs, different duration of<br />
follow-up after surgery, and the inclusion of different<br />
sources of cost data in the various studies.<br />
In the present study, we calculated crude median costs<br />
attributable <strong>to</strong> SSI after breast surgical procedures equal<br />
<strong>to</strong> $10 759. <strong>After</strong> accounting for the variety of operative<br />
methods, diagnoses, and comorbidities, the adjusted attributable<br />
costs of SSI equaled $4091. We found similar<br />
results using propensity scores and calculation of median<br />
differences in costs between matched SSI cases and<br />
controls with similar propensity <strong>to</strong> develop an infection.<br />
Our cost estimates included costs incurred during<br />
the original surgical admission and all hospital readmissions<br />
within 1 year of surgery for all patients in the cohort.<br />
We included all readmission costs during a 1-year<br />
follow-up for several reasons. First, the standard definition<br />
of deep SSI used by the Centers for Disease Control<br />
and Prevention–National Nosocomial <strong>Infection</strong>s Surveillance<br />
System includes infections with onset within 1 year<br />
of surgery in patients with foreign bodies implanted during<br />
surgery. Of the patients in our cohort, 21.0% had a<br />
breast implant placed during surgery and, thus, we needed<br />
<strong>to</strong> extend the period of observation <strong>to</strong> include infections<br />
associated with implants. Second, therapy due <strong>to</strong><br />
SSI required multiple readmissions <strong>to</strong> the hospital in some<br />
patients, so we needed <strong>to</strong> include all of these readmissions<br />
<strong>to</strong> capture all costs associated with therapy due <strong>to</strong><br />
SSI. We included readmission costs for control patients<br />
<strong>to</strong> model the costs directly attributable <strong>to</strong> SSI. For example,<br />
patients with SSI may also have had complications<br />
of chemotherapy during a readmission hospitalization,<br />
so not all of the costs incurred during that<br />
readmission were directly attributable <strong>to</strong> SSI. By including<br />
all readmission costs for case patients and controls,<br />
we could use the ordinary least-squares method <strong>to</strong> model<br />
the costs attributable <strong>to</strong> each of the variables in our model.<br />
The only underlying comorbidities associated with increased<br />
costs in this patient population were serious heart<br />
disease and renal failure, most likely due <strong>to</strong> the occurrence<br />
of breast cancer in primarily elderly women. Nonwhite<br />
race was also associated with significantly increased<br />
costs in our ordinary least-squares model, possibly<br />
because of later stage at diagnosis of breast cancer in African<br />
American women compared with white women. 38 This<br />
is supported by the finding that more nonwhite persons<br />
in our cohort were diagnosed as having metastatic breast<br />
cancer within 1 year of surgery than were white persons,<br />
consistent with more advanced disease at diagnosis<br />
in nonwhite persons.<br />
Our results are consistent with the hypothesis that SSI<br />
following surgery involving major organ spaces are associated<br />
with greater costs than SSI following less extensive<br />
surgical procedures. Our calculated attributable cost of<br />
$4091 is much less than the attributable costs of SSI reported<br />
after cardiothoracic surgery 24,27,28 and orthopedic surgery,<br />
29 but much higher, however, than the value reported<br />
by Reilly et al 23 (approximately $574) in breast<br />
surgical patients. The higher attributable cost associated<br />
with SSI that we calculated may be primarily because of<br />
the inclusion of different types of surgical procedures in<br />
our study compared with that of Reilly and colleagues. We<br />
excluded breast-conserving surgery from our cohort because<br />
of the rarity of inpatient readmission for therapy due<br />
<strong>to</strong> SSI in this population at our institution (M.A.O., J.R.D.,<br />
and V.J.F., unpublished data, 2006). Reilly et al included<br />
costs incurred in the hospital and outpatient setting and,<br />
if their population included women undergoing breastconserving<br />
surgery, they may have been able <strong>to</strong> capture the<br />
outpatient costs associated with SSI following this procedure,<br />
resulting in the much lower value reported compared<br />
with our result.<br />
The attributable cost of SSI we calculated, $4091 per<br />
patient, includes only hospital-associated costs and, thus,<br />
certainly represents an underestimate of the true societal<br />
costs of serious SSI in this surgical population. Our<br />
study did not include physician costs or costs due <strong>to</strong> SSI<br />
associated with excess clinic visits, outpatient surgical<br />
procedures performed in the general or plastic surgery<br />
clinics, outpatient antibiotic use, or home health care and,<br />
thus, the <strong>to</strong>tal attributable costs we calculated represent,<br />
at best, the minimum costs associated with serious<br />
SSI resulting in readmission <strong>to</strong> the hospital or outpatient<br />
surgery.<br />
Ultimately, the goal of studying the incidence and costs<br />
associated with SSI is <strong>to</strong> develop and implement interventions<br />
<strong>to</strong> reduce the occurrence of this adverse surgical<br />
event. Potential interventions <strong>to</strong> reduce the inci-<br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
59<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.
dence of SSI in this patient population include strategies<br />
<strong>to</strong> optimize the timing and dosage of prophylactic antibiotics<br />
administered before the surgical incision, glucose<br />
control in diabetic patients, promotion of meticulous<br />
hand hygiene, and strategies <strong>to</strong> promote timely<br />
removal of drains, among others. Interventions <strong>to</strong> reduce<br />
the incidence of SSI following breast cancer surgical<br />
procedures are essential <strong>to</strong> reduce not only morbidity<br />
in these patient populations but also costs <strong>to</strong> the<br />
individuals and <strong>to</strong> society.<br />
Accepted for Publication: September 4, 2006.<br />
Correspondence: Margaret A. Olsen, PhD, MPH, Division<br />
of Infectious Diseases, Washing<strong>to</strong>n University School<br />
of Medicine, 660 S Euclid Ave, Campus Box 8051, St<br />
Louis, MO 63110 (molsen@im.wustl.edu).<br />
Author Contributions: Study concept and design: Olsen,<br />
Brandt, Dietz, and Fraser. Acquisition of data: Olsen, Chu-<br />
Ongsakul, Mayfield, and Fraser. Analysis and interpretation<br />
of data: Olsen, Chu-Ongsakul, Dietz, and Fraser. Drafting<br />
of the manuscript: Olsen and Fraser. Critical revision of<br />
the manuscript for important intellectual content: Chu-<br />
Ongsakul, Brandt, Dietz, Mayfield, and Fraser. Statistical<br />
analysis: Olsen. Obtained funding: Fraser. Administrative,<br />
technical, and material support: Chu-Ongsakul, Mayfield,<br />
and Fraser. Study supervision: Brandt, Dietz, and Fraser.<br />
Financial Disclosure: None reported.<br />
Funding/Support: This study was supported by Epicenter<br />
Prevention Program Cooperative Agreement VR8/<br />
CCU715087 from the Centers for Disease Control and<br />
Prevention (Dr Fraser).<br />
Additional Contributions: Chris<strong>to</strong>pher S. Hollenbeak,<br />
PhD, and Donald Nichols, PhD, provided insight and comments<br />
concerning the creation of the ordinary leastsquares<br />
and generalized least-squares cost models; and<br />
Bar<strong>to</strong>n Hamil<strong>to</strong>n, PhD, provided suggestions concerning<br />
the use of propensity score methods.<br />
REFERENCES<br />
1. National Nosocomial <strong>Infection</strong>s Surveillance System. National Nosocomial <strong>Infection</strong>s<br />
Surveillance (NNIS) System Report, data summary from January 1992 through<br />
June 2004, issued Oc<strong>to</strong>ber 2004. Am J Infect Control. 2004;32(8):470-485.<br />
2. Seltzer MH. Partial mastec<strong>to</strong>my and limited axillary dissection performed as same<br />
day surgical procedure in the treatment of breast cancer. Int Surg. 1995;80<br />
(1):79-81.<br />
3. Keidan RD, Hoffman JP, Weese JL, et al. Delayed breast abscesses after lumpec<strong>to</strong>my<br />
and radiation therapy. Am Surg. 1990;56(7):440-444.<br />
4. Tejler G, Aspegren K. Complications and hospital stay after surgery for breast<br />
cancer: a prospective study of 385 patients. Br J Surg. 1985;72(7):542-544.<br />
5. Platt R, Zucker JR, Zaleznik DF, et al. Prophylaxis against wound infection following<br />
herniorrhaphy or breast surgery. J Infect Dis. 1992;166(3):556-560.<br />
6. Rotstein C, Ferguson R, Cummings KM, Piedmonte MR, Lucey J, Banish A.<br />
Determinants of clean surgical wound infections for breast procedures at an oncology<br />
center. Infect Control Hosp Epidemiol. 1992;13(4):207-214.<br />
7. Tran CL, Langer S, Broderick-Villa G, DiFronzo LA. Does reoperation predispose<br />
<strong>to</strong> pos<strong>to</strong>perative wound infection in women undergoing operation for breast cancer?<br />
Am Surg. 2003;69(10):852-856.<br />
8. Bertin ML, Crowe J, Gordon SM. Determinants of surgical site infection after breast<br />
surgery. Am J Infect Control. 1998;26(1):61-65.<br />
9. Chen J, Gutkin Z, Bawnik J. Pos<strong>to</strong>perative infections in breast surgery. J Hosp<br />
Infect. 1991;17(1):61-65.<br />
10. Vin<strong>to</strong>n AL, Traverso LW, Zehring RD. Immediate breast reconstruction following<br />
mastec<strong>to</strong>my is as safe as mastec<strong>to</strong>my alone. Arch Surg. 1990;125(10):<br />
1303-1308.<br />
11. Morimo<strong>to</strong> K, Kinoshita H. Once-daily use of ofloxacin for prophylaxis in breast<br />
cancer surgery. Chemotherapy. 1998;44(2):135-141.<br />
12. Broadwater JR, Edwards MJ, Kuglen C, Hor<strong>to</strong>bagyi GN, Ames FC, Balch CM.<br />
Mastec<strong>to</strong>my following preoperative chemotherapy: strict operative criteria control<br />
operative morbidity. Ann Surg. 1991;213(2):126-129.<br />
13. Beatty JD, Robinson GV, Zaia JA, et al. A prospective analysis of nosocomial wound<br />
infection after mastec<strong>to</strong>my. Arch Surg. 1983;118(12):1421-1424.<br />
14. Lipshy KA, Neifeld JP, Boyle RM, et al. Complications of mastec<strong>to</strong>my and their<br />
relationship <strong>to</strong> biopsy technique. Ann Surg Oncol. 1996;3(3):290-294.<br />
15. Nie<strong>to</strong> A, Lozano M, Moro MT, Keller J, Carralafuente C. Determinants of wound<br />
infections after surgery for breast cancer. Zentralbl Gynakol. 2002;124(8-9):<br />
429-433.<br />
16. Hayes JA, Bryan RM. Wound healing following mastec<strong>to</strong>my. AustNZJSurg.<br />
1984;54(1):25-27.<br />
17. Badr el Din A, Coibion M, Guenier C, et al. Local pos<strong>to</strong>perative morbidity following<br />
pre-operative irradiation in locally advanced breast cancer. Eur J Surg Oncol.<br />
1989;15(6):486-489.<br />
18. Say CC, Donegan W. A biostatistical evaluation of complications from mastec<strong>to</strong>my.<br />
Surg Gynecol Obstet. 1974;138(3):370-376.<br />
19. Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastec<strong>to</strong>my<br />
breast reconstruction: two-year results of the Michigan <strong>Breast</strong> Reconstruction<br />
Outcome Study. Plast Reconstr Surg. 2002;109(7):2265-2274.<br />
20. Vandeweyer E, Deraemaecker R, Nogaret JM, Hertens D. Immediate breast reconstruction<br />
with implants and adjuvant chemotherapy: a good option? Acta Chir<br />
Belg. 2003;103(1):98-101.<br />
21. Van Geel AN, Contant CM, Wai RT, Schmitz PI, Eggermont AM, Menke-<br />
Pluijmers MM. Mastec<strong>to</strong>my by inverted drip incision and immediate reconstruction:<br />
data from 510 cases. Ann Surg Oncol. 2003;10(4):389-395.<br />
22. Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications<br />
following breast reconstruction with expanders and implants. Plast Reconstr Surg.<br />
2003;112(2):467-476.<br />
23. Reilly J, Twaddle S, McIn<strong>to</strong>sh J, Kean L. An economic analysis of surgical wound<br />
infection. J Hosp Infect. 2001;49(4):245-249.<br />
24. Boyce JM, Potter-Bynoe G, Dziobek L. <strong>Hospital</strong> reimbursement patterns among<br />
patients with surgical wound infections following open heart surgery. Infect Control<br />
Hosp Epidemiol. 1990;11(2):89-93.<br />
25. Zoutman D, McDonald S, Vethanayagan D. Total and attributable costs of surgicalwound<br />
infections at a Canadian tertiary-care center. Infect Control Hosp Epidemiol.<br />
1998;19(4):254-259.<br />
26. Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sex<strong>to</strong>n DJ. The impact of surgicalsite<br />
infections in the 1990s: attributable mortality, excess length of hospitalization,<br />
and extra costs. Infect Control Hosp Epidemiol. 1999;20(11):725-730.<br />
27. Jenney AWJ, Harring<strong>to</strong>n GA, Russo PL, Spelman DW. Cost of surgical site infections<br />
following coronary artery bypass surgery. ANZ J Surg. 2001;71(11):<br />
662-664.<br />
28. Hollenbeak CS, Murphy D, Dunagan WC, Fraser VJ. Nonrandom selection and<br />
the attributable cost of surgical-site infections. Infect Control Hosp Epidemiol.<br />
2002;23(4):177-182.<br />
29. Whitehouse JD, Friedman D, Kirkland KS, Richardson WJ, Sex<strong>to</strong>n DJ. The impact<br />
of surgical-site infections following orthopedic surgery at a community hospital<br />
and a university hospital: adverse quality of life, excess length of stay, and<br />
extra cost. Infect Control Hosp Epidemiol. 2002;23(4):183-189.<br />
30. Perencevich EN, Sands KE, Cosgrove SE, Guadagnoli E, Meara E, Platt R. Health<br />
and economic impact of surgical site infections diagnosed after hospital discharge.<br />
Emerg Infect Dis. 2003;9(2):196-203.<br />
31. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with<br />
ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619.<br />
32. Charlson ME, Pompei P, Ales K, MacKenzie CR. A new method of classifying prognostic<br />
comorbidity in longitudinal studies: development and validation. J Chronic<br />
Dis. 1987;40(5):373-383.<br />
33. Wooldridge JM. Introduc<strong>to</strong>ry Econometrics: A Modern Approach. Mason, OH:<br />
Thomson Learning; 2003.<br />
34. Rubin DB. Estimating causal effects from large data sets using propensity scores.<br />
Ann Intern Med. 1997;127(8, pt 2):757-763.<br />
35. Austin PC, Ghali WA, Tu JV. A comparison of several regression models for analysing<br />
cost of CABG surgery. Stat Med. 2003;22(17):2799-2815.<br />
36. Smith HL. Matching with multiple controls <strong>to</strong> estimate treatment effects in observational<br />
studies. Sociol Methodol. 1997;27:325-353.<br />
37. Ming K, Rosenbaum PR. Substantial gains in bias reduction from matching with<br />
a variable number of controls. Biometrics. 2000;56(1):118-124.<br />
38. Ghafoor A, Jemal A, Ward E, Cokkinides V, Smith R, Thun M. Trends in breast<br />
cancer by race and ethnicity. CA Cancer J Clin. 2003;53(6):342-355.<br />
(REPRINTED) ARCH SURG/ VOL 143 (NO. 1), JAN 2008 WWW.ARCHSURG.COM<br />
60<br />
Downloaded from www.archsurg.com at Washing<strong>to</strong>n University - St Louis, on January 21, 2008<br />
©2008 American Medical Association. All rights reserved.