Oppositional Defiant Disorder, Intensive Outpatient ... - Ubhonline.com
Oppositional Defiant Disorder, Intensive Outpatient ... - Ubhonline.com
Oppositional Defiant Disorder, Intensive Outpatient ... - Ubhonline.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
OPTUM<br />
By United Behavioral Health<br />
COVERAGE<br />
DETERMINATION<br />
GUIDELINE<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of<br />
<strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD)<br />
Guideline Number: BHCDG672012<br />
Approval Date: April, 2011<br />
Revised Date: November, 2012<br />
Table of Contents:<br />
Instructions for Use 1<br />
Plan Document Language 2<br />
Indications for Coverage 2<br />
Coverage Limitations and Exclusions 10<br />
Definitions 11<br />
References 11<br />
Coding 12<br />
Product:<br />
2001 Generic UnitedHealthcare COC/SPD<br />
2007 Generic UnitedHealthcare COC/SPD<br />
2009 Generic UnitedHealthcare COC/SPD<br />
2011 Generic UnitedHealthcare COC/SPD<br />
May also be applicable to other health plans<br />
and products<br />
Related Coverage Determination<br />
Guidelines:<br />
School-Based Services<br />
Related Medical Policies:<br />
Level of Care Guidelines<br />
American Academy of Child and Adolescent<br />
Psychiatry, Practice Parameter for the<br />
Assessment and Treatment of Children and<br />
Adolescents with <strong>Oppositional</strong> <strong>Defiant</strong><br />
<strong>Disorder</strong>, 2007<br />
Association for Ambulatory Behavioral<br />
Healthcare, 2008<br />
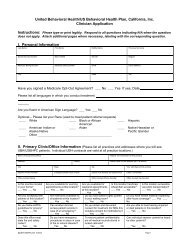
INSTRUCTIONS FOR USE<br />
This Coverage Determination Guideline provides assistance in interpreting behavioral health<br />
benefit plans that are managed by Optum. This Coverage Determination Guideline is also<br />
applicable to behavioral health benefit plans managed by Optum or U.S. Behavioral Health Plan,<br />
California.<br />
When deciding coverage, the enrollee specific document must be referenced. The terms of an<br />
enrollee’s document (e.g., Certificates of Coverage (COCs), Schedules of Benefits (SOBs), or<br />
Summary Plan Descriptions (SPDs) may differ greatly from the standard benefit plans upon which<br />
this guideline is based. In the event of a conflict, the enrollee's specific benefit document<br />
supersedes these guidelines.<br />
All reviewers must first identify enrollee eligibility, any federal or state regulatory requirements<br />
and the plan benefit coverage prior to use of this guideline. Other coverage determination<br />
guidelines and clinical guideline may apply.<br />
PLAN DOCUMENT LANGUAGE<br />
Before using this guideline, please check enrollee’s specific plan document and<br />
any federal or state mandates, if applicable.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 1 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
INDICATIONS FOR COVERAGE<br />
<br />
<br />
<br />
<br />
<br />
Key Points<br />
According to the DSM, the onset of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) typically occurs by<br />
age 8 and includes a pattern of negativistic, hostile, and defiant behavior lasting at least 6<br />
months, during which there is a presence of four or more of the following (Diagnostic and<br />
Statistical Manual of Mental <strong>Disorder</strong>s, Fourth Edition (DSM-IV-TR), 2000):<br />
o<br />
o<br />
o<br />
o<br />
o<br />
o<br />
o<br />
o<br />
Frequent loss of temper<br />
Frequent arguments with adults<br />
Often defies or refuses to <strong>com</strong>ply with adults’ requests or rules<br />
Often deliberately annoys people<br />
Often blames others for his or her mistakes or misbehavior<br />
Often touchy or easily annoyed by others<br />
Often angry and resentful<br />
Often spiteful or vindictive<br />
Establishing a definitive diagnosis requires that the related disturbance (DSM-IV-TR):<br />
o<br />
o<br />
o<br />
o<br />
Is more frequent than observed in individuals of <strong>com</strong>parable age and developmental<br />
level;<br />
Causes significant impairment in social, academic, or occupational functioning;<br />
Does not occur during the course of a Psychotic or Mood <strong>Disorder</strong>; and<br />
Does not meet the criteria for Conduct <strong>Disorder</strong> or Antisocial Personality <strong>Disorder</strong>.<br />
Differential diagnosis to rule out disorders that mask or mimic ODD in addition to the<br />
identification of <strong>com</strong>mon co-occurring conditions that may <strong>com</strong>plicate treatment such as<br />
ADHD, Substance Use <strong>Disorder</strong>s, Mood <strong>Disorder</strong>s, Anxiety <strong>Disorder</strong>s, Adjustment <strong>Disorder</strong>s<br />
and learning and developmental disabilities should be <strong>com</strong>pleted. Specifically consider<br />
whether the patient is exhibiting normal behavior according to age and stage of development<br />
(American Academy of Child and Adolescent Psychiatry (AACAP), 2007).<br />
Optum maintains that the treatment of ODD should be consistent with nationally recognized<br />
scientific evidence as available, and prevailing medical standards and clinical guidelines.<br />
Comprehensive treatment for ODD is typically treated in an outpatient setting. Members with<br />
ODD should be treated in a level of care that is least restrictive and most likely to prove safe<br />
and effective (Optum Level of Care Guidelines (LOCGs), 2012). Choice of intensive<br />
outpatient treatment is indicated for members with at least one of the following:<br />
o<br />
o<br />
o<br />
Moderate symptoms of ODD that cannot be managed in a less intensive level of<br />
care and/or a higher level of care may be required if IOP is not provided<br />
(Association for Ambulatory Mental Healthcare (AABH), 2008);<br />
Moderate impairment in the member’s psychological, social, occupational,<br />
educational, or other area of functioning has impacted the member’s ability to<br />
perform regular daily activities as <strong>com</strong>pared to baseline (AABH, 2008);<br />
The member has <strong>com</strong>pleted treatment at a higher level of care and continues to<br />
require the monitoring provided in an IOP setting (AABH, 2008).<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 2 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
o<br />
o<br />
o<br />
The member’s co-occurring medical, psychiatric and substance use conditions<br />
can be safely managed in an intensive outpatient treatment setting (AABH,<br />
2008).<br />
The member is not at imminent risk of serious harm to self or others (AABH,<br />
2008).<br />
The member or his/her support system understands and can <strong>com</strong>ply with the<br />
requirements of IOP (AABH, 2008).<br />
The goals of <strong>Intensive</strong> <strong>Outpatient</strong> treatment for ODD are to stabilize the presenting signs and<br />
symptoms to the extent that the intensity of IOP services is no longer required and the<br />
member can safely transition to outpatient care.<br />
Best practices include the following:<br />
o<br />
o<br />
o<br />
o<br />
o<br />
Assessment and Evaluation<br />
Treatment Planning<br />
Psychosocial Interventions<br />
Pharmacotherapy<br />
Treatment Discontinuation and Maintenance<br />
An intensive outpatient program (IOP) is a freestanding or hospital-based<br />
program that maintains hours of service for at least 3 hours per day, 2 or more<br />
days per week. It may be used as an initial point of entry into care, as a step up<br />
from routine outpatient services, or as a step down from acute inpatient,<br />
residential care or a partial hospital program (AABH, 2008).<br />
An IOP can be used to treat mental health conditions or can specialize in the<br />
treatment of co-occurring mental health and substance use disorders (LOCGs,<br />
2012)<br />
When supported by the benefit plan, coverage may be available for intensive<br />
outpatient programs that are provided with less intensity to members who are<br />
recovering from severe and persistent mental health conditions (LOCGs, 2012).<br />
The requested service or procedure must be reviewed against the language in<br />
the enrollee's benefit document. When the requested <strong>Intensive</strong> <strong>Outpatient</strong><br />
Treatment service or procedure is limited or excluded from the enrollee’s benefit<br />
document, or is otherwise defined differently, it is the terms of the enrollee's<br />
benefit document that prevails.<br />
Benefits include the following services provided in an intensive outpatient<br />
setting:<br />
Diagnostic evaluations and assessment<br />
Treatment planning<br />
Referral services<br />
Medication management<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 3 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
Individual, family, therapeutic group and provider-based case management<br />
services<br />
Crisis intervention<br />
Best Practices for the Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong><br />
Evaluation and Diagnosis<br />
Engagement and collaboration with the member’s parents/guardians should<br />
be considered at the time treatment begins for increased accuracy of the<br />
assessment and improved treatment out<strong>com</strong>es (American Academy of Child<br />
and Adolescent Psychiatry (AACAP), 2007).<br />
Identify the precipitants for the admission/initiation of IOP treatment, current<br />
symptoms and consequences of reported symptoms/behaviors (AACAP,<br />
2007).<br />
Complete a psychiatric evaluation to include mental status, family history,<br />
functional impairments and the administration of indicated rating scales<br />
(AACAP, 2007).<br />
The assessment should focus on gathering information directly from the child<br />
as well as from the parents/guardians separately regarding the core<br />
symptoms of ODD, age of onset, duration of symptoms and degree of<br />
functional impairment (AACAP, 2007).<br />
Gather treatment information to include previous treatment, medication<br />
history and baseline level of functioning (AACAP, 2007).<br />
Evaluate family history to include parent/child relationships, parental<br />
strategies, cultural considerations, and history of abuse or neglect (AACAP,<br />
2007).<br />
o Family instability, economic stress, parental mental illness, harshly<br />
punitive behaviors, inconsistent parent practices, multiple moves, and<br />
divorce, may also contribute to the development of and exacerbate<br />
ODD symptoms (AACAP, 2007).<br />
Gather information from multiple informants using multiple methods to<br />
include:<br />
o Observational reports and clinical interviews with parents, daycare<br />
providers, teachers, family members, school professionals and selfreport<br />
(AACAP, 2007).<br />
o Rating scales for the diagnosis of ODD and for measuring behavioral<br />
progress over time. These may include the Conner’s Rating Scale-<br />
Revised (CPRS and CTRS), Achenbach Behavior Checklist: Child<br />
Behavior Checklist (CBCL, OASR), State Trait Anger Aggression<br />
Inventory (STAXI), and the Conner’s Wells Adolescent Self Report<br />
(CASS) (AACAP, 2007).<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 4 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
Evaluate the risk factors and safety of the patient including current<br />
suicide/homicide risk, patterns of aggression, violence, bullying or access to<br />
weapons (AACAP, 2007).<br />
Determine each setting where ODD symptoms are exhibited.<br />
o Children with ODD behavior in school should undergo necessary<br />
screening and/or testing in school to evaluate for possible learning<br />
disabilities. Coverage for testing is determined by the benefit plan<br />
(AACAP, 2007).<br />
Complete differential diagnosis to rule out Conduct <strong>Disorder</strong>, Mood <strong>Disorder</strong>s,<br />
Anxiety <strong>Disorder</strong>s, Adjustment <strong>Disorder</strong>s, ADHD, Substance Use <strong>Disorder</strong>s,<br />
and Medical Conditions and also consider co-occurring conditions that may<br />
warrant concurrent treatment. This should also include an evaluation of<br />
current behaviors and whether they are developmentally appropriate as<br />
<strong>com</strong>pared to expected behaviors for the child’s stage of development<br />
(AACAP, 2007).<br />
o Diagnosis may be <strong>com</strong>plicated further by relatively high rates of<br />
<strong>com</strong>orbid or overlapping of symptoms of disorders such as ADHD and<br />
Conduct <strong>Disorder</strong> and <strong>com</strong>orbidities with other medical and behavioral<br />
health conditions.<br />
o Comorbid conditions require treatment along with treatment of the<br />
ODD behaviors. If these <strong>com</strong>orbid conditions respond to treatment,<br />
then oppositional behavior may lessen or even disappear.<br />
Consider reviewing the patient’s pediatric medical history to rule out medical<br />
conditions that might better explain the symptoms or the worsening of<br />
symptoms due to medical causes, and to determine any prenatal/postnatal<br />
risk factors (AACAP, 2007).<br />
o This may include an evaluation of any prenatal risk factors to include,<br />
exposure to toxins, alcohol and poor nutrition (AACAP, 2007).<br />
Evaluate the ability of the member’s family/social supports to participate in the<br />
member’s treatment and observe parent/child interactions when possible<br />
(AACAP, 2007).<br />
Treatment Planning<br />
<br />
The treatment plan must include objectives, actions and timeframes to<br />
address all of the following:<br />
o The precipitants for treatment and the plan to improve the patient’s<br />
functioning.<br />
o A plan to improve behaviors that precipitated admission.<br />
o A plan to manage co-occurring behavioral health and medical<br />
conditions.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 5 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
o A plan to improve the patient’s ability to manage their condition.<br />
o A plan for reassessing the patient’s symptoms and functioning<br />
regularly.<br />
o Coordinating treatment with agencies and programs such as the<br />
school, court system or protective services with which the member has<br />
been involved; and<br />
o Preparing the member for transition from IOP treatment and the<br />
introduction of post-discharge care in the <strong>com</strong>munity.<br />
Within 48 hours of admission the provider and, whenever possible, the<br />
member should document clear, reasonable and objective treatment goals<br />
and timeframes that stem from the member’s diagnosis, and are supported by<br />
specific treatment strategies which address the member’s symptoms and the<br />
precipitant for admission (LOCGs, 2012).<br />
o The treatment plan and appropriateness of level of care should be<br />
updated every 3-5 days as new information be<strong>com</strong>es available or if<br />
the member’s status changes (LOCGs, 2012).<br />
o The treatment plan should always address co-occurring behavioral<br />
and medical conditions including substance disorders (LOCGs,<br />
2012).<br />
The treatment plan must include objectives, actions and timeframes to<br />
address all of the following (LOCGs, 2012):<br />
o Identify impairments and interventions that will maximize the patient’s<br />
quality of life.<br />
o Determine how symptom reduction and rapid stabilization will be<br />
achieved.<br />
o Determine how co-occurring behavioral health and medical conditions,<br />
if any, will be managed.<br />
o Determine how the patient’s ability to manage their condition will be<br />
improved such as by providing health education, and linking the patient<br />
with peer services and other <strong>com</strong>munity resources.<br />
o Determine how risk issues related to the patient’s presenting condition,<br />
co-occurring behavioral health or medical conditions will be managed<br />
including how the patient’s motivation will be maintained/enhanced,<br />
and collaborating with the patient to develop/revise the advance<br />
directive or relapse prevention plan.<br />
o Determine whether the patient has an advance directive, a recovery<br />
plan, and a plan for managing relapse.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 6 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
Contact the patient’s family and/or social support network, with the patient’s<br />
documented consent to regularly participate in the patient’s treatment and<br />
discharge planning when such participation is essential and clinically<br />
appropriate (LOCGs, 2012).<br />
Parents/guardians of child and adolescent patients should be contacted and<br />
should participate in the patient’s treatment unless clinically contraindicated.<br />
Optimally, the patient’s family and/or social support group should participate<br />
in treatment when the patient is a child or adolescent (LOCGs, 2012).<br />
The provider and the patient collaborate to update the treatment plan in<br />
response to changes in the patient’s condition (LOCGs, 2012).<br />
Psychosocial Interventions<br />
<br />
<br />
<br />
<br />
Psychosocial interventions should be chosen in consideration of the child’s<br />
age and developmental level. Treatments that are behaviorally based and<br />
coordinated with the family, school and any other significant others are<br />
indicated for the treatment of ODD (AACAP, 2007).<br />
Treatments often include a <strong>com</strong>bination of individual psychotherapy, family<br />
psychotherapy, pharmacotherapy and environmental intervention (e.g.,<br />
school-based interventions) (AACAP, 2007).<br />
Evidenced-based treatments for ODD include individual problem-solving skills<br />
training that is behaviorally-based and family interventions in the form of<br />
Parent Management Training (PMT) (AACAP, 2007).<br />
Children with more severe forms of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong>, and those<br />
who have co-occurring behavioral health conditions which warrant treatment<br />
may require more than one psychosocial intervention. Consider Parent<br />
Management Training (PMT) in conjunction with other behaviorally-based<br />
individual, family and/or group therapies (AACAP, 2007).<br />
o Parent Management Training or other forms of family approaches<br />
should aim to reduce reinforcement of disruptive behavior, increase<br />
reinforcement of <strong>com</strong>pliant behavior, apply consequences for<br />
disruptive behavior and make parental response predictable and<br />
immediate (AACAP, 2007).<br />
• PMT consists of procedures in which parents are trained to<br />
change their own behaviors and thereby alter their child's<br />
problem behavior in the home.<br />
• Parental involvement in PMT is essential.<br />
o Early identification programs delivered in schools, <strong>com</strong>munity clinics<br />
and in the homes of families are re<strong>com</strong>mended. These programs<br />
target social skills, parenting, conflict resolution and anger<br />
management and have evidence to support improvement of ODD and<br />
may augment or prevent the need for further intervention. Coverage<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 7 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
for such programs may not be supported by the benefit plan (AACAP,<br />
2007).<br />
• School-based interventions may include preventive programs<br />
that focus on the development of socio-emotional skills, selfcontrol<br />
and problem solving (AACAP, 2007).<br />
o Individual approaches should be behaviorally based and geared<br />
toward the development of problem-solving skills. Behavioral<br />
interventions can aim to control aggression, modify behavior, and<br />
enhance <strong>com</strong>munication and self-awareness (AACAP, 2007).<br />
o Structured group therapy may be most helpful for adolescents focusing<br />
on <strong>com</strong>munication, problem-solving and behavior management<br />
(AACAP, 2007).<br />
o Alternative family approaches include Functional Family Therapy<br />
(FFT) and Multisystemic Therapy shown to be most effective for<br />
members with ODD and Substance Use <strong>Disorder</strong>s (AACAP, 2007).<br />
o Inoculation approaches (e.g., boot camps, shock incarceration) have<br />
been considered ineffective and even harmful especially when used in<br />
isolation from evidence-based approaches (AACAP, 2007).<br />
o Interventions should be delivered as long as clinically indicated,<br />
usually for several months with periodic “booster” sessions, reinforcing<br />
learned skills for both the member and family/guardians (AACAP,<br />
2007).<br />
Pharmacotherapy<br />
<br />
<br />
<br />
<br />
Pharmacotherapy is generally not indicated to treat ODD as a sole<br />
intervention but may be helpful as an adjunct to psychotherapy to treat<br />
aggressive symptoms and/or <strong>com</strong>orbid conditions (AACAP, 2007).<br />
Medication intervention is best introduced after a strong alliance with the<br />
member and family has been established and only after psychosocial<br />
interventions have been implemented (AACAP, 2007).<br />
If <strong>com</strong>orbid conditions are present, medications specifically targeting those<br />
conditions should be chosen however, atypical antipsychotics, mood<br />
stabilizers (e.g., divalproex and lithium), and stimulants are often<br />
prescribed in treating acute aggression in a time limited manner (AACAP,<br />
2007).<br />
Medications should only be started after a symptom baseline can be<br />
established as to not attribute positive out<strong>com</strong>es to medications rather<br />
than a stabilizing environment (AACAP, 2007).<br />
If medication use is chosen, the child in addition to the parents should<br />
agree and it should be clearly assessed whether adherence and<br />
monitoring are issues of concern (AACAP, 2007).<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 8 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
Nonresponsiveness to a specific agent should lead to a trial of another<br />
class of medication rather than the addition of other medications (AACAP,<br />
2007).<br />
Pharmacological treatments are typically short-term and/or time-limited<br />
however, prolonged treatment may be required due to usually severe and<br />
persistent ODD or ODD that co-occurs with other behavioral health<br />
conditions (AACAP, 2007).<br />
Discharge Planning and Referral Management<br />
Members in IOP may be discharged by either stepping up to a more intensive<br />
level of care when his/her condition has not improved or has worsened; or<br />
stepping down to a less intensive level of outpatient care when the member’s<br />
clinical condition improves or he/she no longer requires structured, intensive,<br />
multimodal treatment. (CMS Manual System, 2004).<br />
<br />
The discharge plan must include the anticipated discharge date and the<br />
following (LOCGs, 2012):<br />
o The next level of care, its location, and the name(s) of the<br />
provider(s) who will deliver treatment;<br />
o The rationale for the referral;<br />
o The date and time of the first appointment for treatment as well<br />
as the first follow-up psychiatric assessment within 7 days of<br />
discharge;<br />
o The re<strong>com</strong>mended modalities of care and the frequency of each<br />
modality;<br />
o The names, dosages and frequencies of each medication, and a<br />
schedule for appropriate lab tests if pharmacotherapy is a<br />
modality of post-discharge care<br />
o Linkages with peer services and other <strong>com</strong>munity resources.<br />
o The plan to <strong>com</strong>municate all pertinent clinical information to the<br />
provider(s) responsible for post-discharge care, as well as to the<br />
member’s primary care provider as appropriate.<br />
o The plan to coordinate discharge with agencies and programs<br />
the member has been involved, when appropriate and with the<br />
member’s documented consent.<br />
o A prescription for a supply of medication sufficient to bridge the<br />
time between discharge and the scheduled follow-up psychiatric<br />
assessment.<br />
o Confirmation that the member or authorized representative<br />
understands the discharge plan.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 9 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
o Confirmation that the member or authorized representative was<br />
provided with written instruction for what to do in the event that<br />
a crisis arises prior to the first post-discharge appointment.<br />
In Some Situations Optum May Offer:<br />
Peer Review: Optum will offer a peer review to the provider when services do<br />
not appear to conform with this guideline. The purpose of a peer review is to<br />
allow the provider the opportunity to share additional or new information about<br />
the case to assist the Peer Reviewer in making a determination including,<br />
when necessary, to clarify a diagnosis.<br />
Second Opinion Evaluation: Optum facilitates obtaining a second opinion<br />
evaluation when requested by an enrollee, provider, or when Optum<br />
otherwise determines that a second opinion is necessary to make a<br />
determination, clarify a diagnosis or improve treatment planning and care for<br />
the enrollee.<br />
Referral Assistance: Optum provides assistance with accessing care when<br />
the provider and/or enrollee determine that there is not an appropriate match<br />
with the enrollee’s clinical needs and goals, or if additional providers should<br />
be involved in delivering treatment.<br />
IOP admissions require pre-service notification. Notification of a scheduled<br />
admission must occur at least five (5) business days before admission.<br />
Notification of an unscheduled admission (including Emergency admissions)<br />
should occur as soon as is reasonably possible. In the event that the Mental<br />
Health/Substance Use <strong>Disorder</strong> Designee is not notified of an IOP admission,<br />
benefits may be reduced. Check the member’s specific benefit plan document for<br />
the applicable penalty and provision for a grace period before applying a penalty<br />
for failure to notify the Mental Health/Substance Use <strong>Disorder</strong> Designee as<br />
required.<br />
Covered Health Service(s) – UnitedHealthcare 2001<br />
Those health services provided for the purpose of preventing, diagnosing or<br />
treating a sickness, injury, mental illness, substance abuse, or their symptoms. A<br />
Covered Health Service is a health care service or supply described in Section 1:<br />
What's Covered--Benefits as a Covered Health Service, which is not excluded<br />
under Section 2: What's Not Covered--Exclusions.<br />
Covered Health Service(s) – UnitedHealthcare 2007, 2009 & 2011<br />
Those health services, including services, supplies, or Pharmaceutical Products,<br />
which we determine to be all of the following:<br />
Provided for the purpose of preventing, diagnosing or treating a<br />
Sickness, Injury, mental illness, substance abuse, or their symptoms.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 10 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
Consistent with nationally recognized scientific evidence as available,<br />
and prevailing medical standards and clinical guidelines as described<br />
below.<br />
Not provided for the convenience of the Covered Person, Physician,<br />
facility or any other person.<br />
Described in this Certificate of Coverage under Section 1: Covered<br />
Health Services and in the Schedule of Benefits.<br />
Not otherwise excluded in this Certificate of Coverage under Section 2:<br />
Exclusions and Limitations.<br />
In applying the above definition, "scientific evidence" and "prevailing medical<br />
standards" shall have the following meanings:<br />
<br />
"Scientific evidence" means the results of controlled clinical trials or<br />
other studies published in peer-reviewed, medical literature generally<br />
recognized by the relevant medical specialty <strong>com</strong>munity.<br />
"Prevailing medical standards and clinical guidelines" means nationally<br />
recognized professional standards of care including, but not limited to,<br />
national consensus statements, nationally recognized clinical<br />
guidelines, and national specialty society guidelines.<br />
Optum maintains clinical protocols for the treatment of ODD that describe the<br />
scientific evidence, prevailing medical standards and clinical guidelines<br />
supporting our determinations regarding specific services. These clinical<br />
protocols (as revised from time to time), are available to Covered Persons upon<br />
request, and to Physicians and other behavioral health care professionals on<br />
ubhonline.<br />
COVERAGE LIMITATIONS AND EXCLUSIONS<br />
Inconsistent or Inappropriate Services or Supplies – UnitedHealthcare<br />
2001, 2007, 2009 & 2011<br />
Services or supplies for the diagnosis or treatment of Mental Illness that, in the<br />
reasonable judgment of the Mental Health/Substance Use <strong>Disorder</strong>s Designee,<br />
are any of the following:<br />
<br />
<br />
<br />
Not consistent with generally accepted standards of medical practice for<br />
the treatment of such conditions.<br />
Not consistent with services backed by credible research soundly<br />
demonstrating that the services or supplies will have a measurable and<br />
beneficial health out<strong>com</strong>e, and are therefore considered experimental.<br />
Not consistent with the Mental Health/Substance Use <strong>Disorder</strong> Designee’s<br />
level of care guidelines or best practice guidelines as modified from time<br />
to time.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 11 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
Not clinically appropriate for the patient’s Mental Illness or condition based<br />
on generally accepted standards of medical practice and benchmarks.<br />
Additional Information: The lack of a specific exclusion of a service does not<br />
imply that the service is covered.<br />
The following are examples of inconsistent or inappropriate services for the<br />
treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (not an all inclusive list):<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Services that deviate from the indications for coverage summarized in the<br />
previous section such as:<br />
o A mis-match between the symptoms of <strong>Oppositional</strong> <strong>Defiant</strong><br />
<strong>Disorder</strong>, and the type and/or duration of treatment.<br />
o A treatment plan that has not been modified when there has been<br />
partial or no response to an adequate trial of treatment.<br />
Admission to IOP treatment without appropriate management of acute<br />
symptoms.<br />
Admission to IOP treatment solely as a substitute for an available lower<br />
level of care, an intensified schedule of ambulatory care, or a broadened<br />
treatment plan.<br />
Admission to IOP treatment that does not provide an adequate program of<br />
treatment.<br />
Not coordinating care when more than one practitioner is delivering<br />
treatment.<br />
Not addressing co-occurring behavioral health medical conditions<br />
including substance use disorders in the treatment plan.<br />
Services continue even though treatment goals have been <strong>com</strong>pleted.<br />
Services continue despite repeated failures to adhere with re<strong>com</strong>mended<br />
treatment despite the deployment of motivational enhancement<br />
interventions, peer support, school-based and other <strong>com</strong>munity resources.<br />
Coverage for school-based services such as screening and testing for<br />
learning disabilities and/or school delivered programs not supported by the<br />
benefit plan.<br />
Please refer to the enrollee’s benefit document for ASO plans with benefit<br />
language other than the generic benefit document language.<br />
{INCLUDE FOR ASO ONLY:<br />
For ASO plans with SPD language other than 2001 and 2007 Generic COC<br />
language,<br />
Please refer to the enrollee’s plan specific SPD for coverage.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 12 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
DEFINITIONS<br />
Diagnostic and Statistical Manual of the American Psychiatric Association<br />
(DSM) A manual produced by the American Psychiatric Association which<br />
provides the diagnostic criteria for mental health and substance use disorders,<br />
and other problems that may be the focus of clinical attention. Unless otherwise<br />
noted, the current edition of the DSM applies.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Program An intensive outpatient program (IOP) is a<br />
freestanding or hospital-based program that maintains hours of service for at<br />
least 3 hours per day, 2 or more days per week. It may be used as an initial point<br />
of entry into care, as a step up from routine outpatient services, or as a step<br />
down from acute inpatient, residential care or a partial hospital program.<br />
Mental Illness Those mental health or psychiatric diagnostic categories that are<br />
listed in the current Diagnostic and Statistical Manual of the American Psychiatric<br />
Association, unless those services are specifically excluded under the Policy.<br />
<strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) According to the DSM, the essential<br />
feature of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> is pattern of negativistic, hostile, and<br />
defiant behavior lasting at least 6 months, during which there is a presence of<br />
four or more of the following:<br />
Frequent loss of temper, frequent arguments with adults, often defies or refuses<br />
to <strong>com</strong>ply with adults’ requests or rules, often deliberately annoys people, often<br />
blames others for his or her mistakes or misbehavior, often touchy or easily<br />
annoyed by others, often angry and resentful, often spiteful or vindictive.<br />
REFERENCES<br />
1. Generic UnitedHealthcare Certificate of Coverage, 2001<br />
2. Generic UnitedHealthcare Certificate of Coverage, 2007<br />
3. Generic UnitedHealthcare Certificate of Coverage, 2009<br />
4. Generic UnitedHealthcare Certificate of Coverage, 2011<br />
5. American Academy of Child and Adolescent Psychiatry, Practice Parameter<br />
for the Assessment and Treatment of Children and Adolescents with<br />
<strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong>, 2007.<br />
6. American Academy of Child and Adolescent Psychiatry, <strong>Oppositional</strong> <strong>Defiant</strong><br />
<strong>Disorder</strong>s Resources, 2011.<br />
7. Association for Ambulatory Mental Healthcare, Standards and Guidelines for<br />
Partial Hospital and <strong>Intensive</strong> <strong>Outpatient</strong> Treatment Programs, 2008.<br />
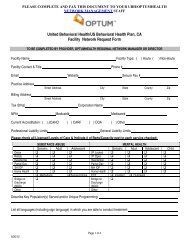
CODING<br />
The Current Procedural Terminology (CPT) codes and HCPCS codes listed in this guideline are<br />
for reference purposes only. Listing of a service code in this guideline does not imply that the<br />
service described by this code is a covered or non-covered health service. Coverage is<br />
determined by the benefit document.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 13 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates
Limited to specific CPT and HCPCS codes?<br />
x YES □ NO<br />
H0015<br />
S9480<br />
<strong>Intensive</strong> outpatient (treatment program that<br />
operates at least 3 hours/day and at least 3<br />
days/week and is based on an individualized<br />
treatment plan), including assessment,<br />
counseling; crisis intervention, and activity<br />
therapy.<br />
<strong>Intensive</strong> outpatient psychiatric services, per<br />
diem<br />
Limited to specific diagnosis codes?<br />
x YES □ NO<br />
313.81 <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong><br />
Limited to place of service (POS)?<br />
x YES □ NO<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Program<br />
Limited to specific provider type?<br />
□ YES x NO<br />
Limited to specific revenue codes?<br />
□ YES x NO<br />
HISTORY<br />
Revision Date Name Revision Notes<br />
12/2/12 L. Urban Version 2-Final<br />
The enrollee's specific benefit documents supersede these guidelines and are used to make coverage determinations.<br />
These Coverage Determination Guidelines are believed to be current as of the date noted.<br />
<strong>Intensive</strong> <strong>Outpatient</strong> Treatment of <strong>Oppositional</strong> <strong>Defiant</strong> <strong>Disorder</strong> (ODD) Page 14 of 14<br />
Coverage Determination Guideline<br />
Confidential and Proprietary, © Optum 2012<br />
Optum is a brand used by United Behavioral Health and its affiliates