2012 Compliance: Fraud, Waste and Abuse (training - Ubhonline.com
2012 Compliance: Fraud, Waste and Abuse (training - Ubhonline.com
2012 Compliance: Fraud, Waste and Abuse (training - Ubhonline.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
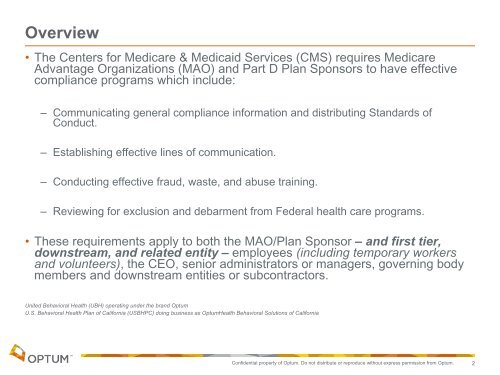
Overview<br />
• The Centers for Medicare & Medicaid Services (CMS) requires Medicare<br />
Advantage Organizations (MAO) <strong>and</strong> Part D Plan Sponsors to have effective<br />
<strong>com</strong>pliance programs which include:<br />
– Communicating general <strong>com</strong>pliance information <strong>and</strong> distributing St<strong>and</strong>ards of<br />
Conduct.<br />
– Establishing effective lines of <strong>com</strong>munication.<br />
– Conducting effective fraud, waste, <strong>and</strong> abuse <strong>training</strong>.<br />
– Reviewing for exclusion <strong>and</strong> debarment from Federal health care programs.<br />
• These requirements apply to both the MAO/Plan Sponsor – <strong>and</strong> first tier,<br />
downstream, <strong>and</strong> related entity – employees (including temporary workers<br />
<strong>and</strong> volunteers), the CEO, senior administrators or managers, governing body<br />
members <strong>and</strong> downstream entities or subcontractors.<br />
United Behavioral Health (UBH) operating under the br<strong>and</strong> Optum<br />
U.S. Behavioral Health Plan of California (USBHPC) doing business as OptumHealth Behavioral Solutions of California<br />
Confidential property of Optum. Do not distribute or reproduce without express permission from Optum.<br />
2