Answers to Self-Assessment Questions - ACCP
Answers to Self-Assessment Questions - ACCP
Answers to Self-Assessment Questions - ACCP
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
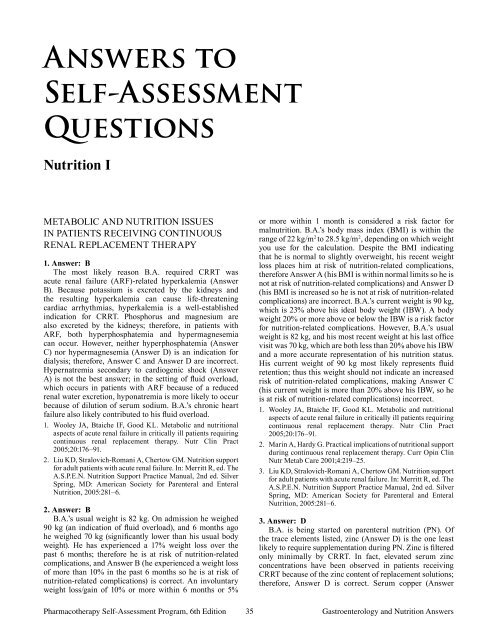
<strong>Answers</strong> <strong>to</strong><br />
<strong>Self</strong>-<strong>Assessment</strong><br />
<strong>Questions</strong><br />
Nutrition I<br />
Metabolic and Nutrition Issues<br />
in Patients Receiving Continuous<br />
Renal Replacement Therapy<br />
1. Answer: B<br />
The most likely reason B.A. required CRRT was<br />
acute renal failure (ARF)-related hyperkalemia (Answer<br />
B). Because potassium is excreted by the kidneys and<br />
the resulting hyperkalemia can cause life-threatening<br />
cardiac arrhythmias, hyperkalemia is a well-established<br />
indication for CRRT. Phosphorus and magnesium are<br />
also excreted by the kidneys; therefore, in patients with<br />
ARF, both hyperphosphatemia and hypermagnesemia<br />
can occur. However, neither hyperphosphatemia (Answer<br />
C) nor hypermagnesemia (Answer D) is an indication for<br />
dialysis; therefore, Answer C and Answer D are incorrect.<br />
Hypernatremia secondary <strong>to</strong> cardiogenic shock (Answer<br />
A) is not the best answer; in the setting of fluid overload,<br />
which occurs in patients with ARF because of a reduced<br />
renal water excretion, hyponatremia is more likely <strong>to</strong> occur<br />
because of dilution of serum sodium. B.A.’s chronic heart<br />
failure also likely contributed <strong>to</strong> his fluid overload.<br />
1. Wooley JA, Btaiche IF, Good KL. Metabolic and nutritional<br />
aspects of acute renal failure in critically ill patients requiring<br />
continuous renal replacement therapy. Nutr Clin Pract<br />
2005;20:176–91.<br />
2. Liu KD, Stralovich-Romani A, Cher<strong>to</strong>w GM. Nutrition support<br />
for adult patients with acute renal failure. In: Merritt R, ed. The<br />
A.S.P.E.N. Nutrition Support Practice Manual, 2nd ed. Silver<br />
Spring, MD: American Society for Parenteral and Enteral<br />
Nutrition, 2005:281–6.<br />
2. Answer: B<br />
B.A.’s usual weight is 82 kg. On admission he weighed<br />
90 kg (an indication of fluid overload), and 6 months ago<br />
he weighed 70 kg (significantly lower than his usual body<br />
weight). He has experienced a 17% weight loss over the<br />
past 6 months; therefore he is at risk of nutrition-related<br />
complications, and Answer B (he experienced a weight loss<br />
of more than 10% in the past 6 months so he is at risk of<br />
nutrition-related complications) is correct. An involuntary<br />
weight loss/gain of 10% or more within 6 months or 5%<br />
or more within 1 month is considered a risk fac<strong>to</strong>r for<br />
malnutrition. B.A.’s body mass index (BMI) is within the<br />
range of 22 kg/m 2 <strong>to</strong> 28.5 kg/m 2 , depending on which weight<br />
you use for the calculation. Despite the BMI indicating<br />
that he is normal <strong>to</strong> slightly overweight, his recent weight<br />
loss places him at risk of nutrition-related complications,<br />
therefore Answer A (his BMI is within normal limits so he is<br />
not at risk of nutrition-related complications) and Answer D<br />
(his BMI is increased so he is not at risk of nutrition-related<br />
complications) are incorrect. B.A.’s current weight is 90 kg,<br />
which is 23% above his ideal body weight (IBW). A body<br />
weight 20% or more above or below the IBW is a risk fac<strong>to</strong>r<br />
for nutrition-related complications. However, B.A.’s usual<br />
weight is 82 kg, and his most recent weight at his last office<br />
visit was 70 kg, which are both less than 20% above his IBW<br />
and a more accurate representation of his nutrition status.<br />
His current weight of 90 kg most likely represents fluid<br />
retention; thus this weight should not indicate an increased<br />
risk of nutrition-related complications, making Answer C<br />
(his current weight is more than 20% above his IBW, so he<br />
is at risk of nutrition-related complications) incorrect.<br />
1. Wooley JA, Btaiche IF, Good KL. Metabolic and nutritional<br />
aspects of acute renal failure in critically ill patients requiring<br />
continuous renal replacement therapy. Nutr Clin Pract<br />
2005;20:176–91.<br />
2. Marin A, Hardy G. Practical implications of nutritional support<br />
during continuous renal replacement therapy. Curr Opin Clin<br />
Nutr Metab Care 2001;4:219–25.<br />
3. Liu KD, Stralovich-Romani A, Cher<strong>to</strong>w GM. Nutrition support<br />
for adult patients with acute renal failure. In: Merritt R, ed. The<br />
A.S.P.E.N. Nutrition Support Practice Manual, 2nd ed. Silver<br />
Spring, MD: American Society for Parenteral and Enteral<br />
Nutrition, 2005:281–6.<br />
3. Answer: D<br />
B.A. is being started on parenteral nutrition (PN). Of<br />
the trace elements listed, zinc (Answer D) is the one least<br />
likely <strong>to</strong> require supplementation during PN. Zinc is filtered<br />
only minimally by CRRT. In fact, elevated serum zinc<br />
concentrations have been observed in patients receiving<br />
CRRT because of the zinc content of replacement solutions;<br />
therefore, Answer D is correct. Serum copper (Answer<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 35 Gastroenterology and Nutrition <strong>Answers</strong>
A), chromium (Answer B), and selenium (Answer C)<br />
concentrations have been reported <strong>to</strong> be decreased in patients<br />
receiving CRRT; therefore, these trace elements should be<br />
supplemented in patients receiving CRRT, making <strong>Answers</strong><br />
A, B, and C incorrect.<br />
1. Klein CJ, Moser-Veillon PB, Schweitzer A, Douglass LW,<br />
Reynolds HN, Patterson KY, et al. Magnesium, calcium,<br />
zinc, and nitrogen loss in trauma patients during continuous<br />
renal replacement therapy. JPEN J Parenter Enteral Nutr<br />
2002;26:77–92.<br />
2. Berger MM, Shenkin A, Revelly JP, Roberts E, Cayeux MC,<br />
Baines M, et al. Copper, selenium, zinc, and thiamine balances<br />
during continuous venovenous hemodiafiltration in critically<br />
ill patients. Am J Clin Nutr 2004;80:410–6.<br />
3. S<strong>to</strong>ry DA, Ronco C, Bellomo R. Trace element and vitamin<br />
concentrations and losses in critically ill patients treated<br />
with continuous venovenous hemofiltration. Crit Care Med<br />
1999;27:220–3.<br />
4. Answer: C<br />
Because of fluid overload, A.B.’s usual weight (82 kg)<br />
or his most recent preadmission weight (70 kg) should be<br />
used <strong>to</strong> calculate his caloric requirements. B.A.’s estimated<br />
caloric requirement is 25–35 kcal/kg/day. Answer C (2460<br />
kcal/day) provides 30 kcal/kg/day based on B.A.’s usual<br />
body weight (82 kg) or 35 kcal/kg/day based on his most<br />
recent preadmission weight, and is therefore the best answer.<br />
Answer A (1230 kcal/kg/day) and Answer B (1640 kcal/<br />
kg/day) provide fewer than 25 kcal/kg/day; these amounts<br />
are less than recommended for patients like B.A. Answer<br />
D (3280 kcal/kg/day) provides more than 35 kcal/kg/day,<br />
which would be an excessive daily caloric intake for B.A.<br />
leading <strong>to</strong> complications associated with overfeeding.<br />
1. Liu KD, Stralovich-Romani A, Cher<strong>to</strong>w GM. Nutrition support<br />
for adult patients with acute renal failure. In: Merritt R, ed. The<br />
A.S.P.E.N. Nutrition Support Practice Manual, 2nd ed. Silver<br />
Spring, MD: American Society for Parenteral and Enteral<br />
Nutrition, 2005:281–6.<br />
2. A.S.P.E.N. Board of Direc<strong>to</strong>rs and The Clinical Guidelines<br />
Task Force. Guidelines for the use of parenteral and enteral<br />
nutrition in adult and pediatric patients. JPEN J Parenter<br />
Enteral Nutr 2002;26S:1SA–6SA.<br />
5. Answer: C<br />
B.A. is receiving CRRT with citrate anticoagulation<br />
and has developed metabolic alkalosis. In this situation,<br />
bicarbonate administration should be decreased (Answer C);<br />
thus Answer C is the correct answer. Citrate is converted by<br />
the liver <strong>to</strong> bicarbonate and may precipitate alkalosis if the<br />
patient is not moni<strong>to</strong>red closely or if intake of other buffer<br />
solutions (bicarbonate, lactate, and acetate) is not reduced.<br />
Answer A (lactate solutions should be used <strong>to</strong> correct B.A.’s<br />
alkalosis) is incorrect because lactate-containing solutions<br />
have been shown <strong>to</strong> have a negative effect on cardiac<br />
function and mean arterial pressure. These effects would be<br />
undesirable in B.A., who has chronic heart failure and shock.<br />
Additionally, lactate is converted <strong>to</strong> bicarbonate in the liver,<br />
which would exacerbate B.A.’s alkalosis. Bicarbonatebased<br />
solutions (Answer B) are not indicated because of the<br />
potential for worsening B.A.’s alkalosis; thus Answer B is<br />
incorrect. Acetate solutions (Answer D) should not be used<br />
routinely in patients in the intensive care unit (ICU) because<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
36<br />
vasodilation and reduced myocardial contractility have<br />
been observed. These effects along with the conversion of<br />
acetate by the liver <strong>to</strong> bicarbonate may worsen the alkalosis.<br />
Therefore, Answer D is incorrect.<br />
1. Gabutti L, Marine C, Colucci G, Duchini F, Schönholzer<br />
C. Citrate anticoagulation in continuous venovenous<br />
hemodiafiltration: a metabolic challenge. Intensive Care Med<br />
2002;28:1419–25.<br />
2. Druml W. Metabolic aspects of continuous renal replacement<br />
therapies. Kidney Int Suppl 1999;72:S56–S61.<br />
6. Answer: B<br />
J.G.’s traumatic injury (Answer B) will increase her<br />
energy requirements compared with a healthy woman<br />
of her age and weight because hypermetabolism that<br />
occurs with trauma increases energy needs; thus Answer<br />
B is correct. The presence of ARF (Answer A) does not<br />
increase a patient’s basal metabolic expenditure, making<br />
Answer A is incorrect. In general, women have lower<br />
energy requirements compared with men, making Answer<br />
C (female sex) incorrect. Answer D (hypothermia from<br />
the absence of a blood warmer for the CRRT replacement<br />
solutions) is incorrect because hypothermia would induce a<br />
hypometabolic response, reducing energy needs.<br />
1. Marin A, Hardy G. Practical implications of nutritional support<br />
during continuous renal replacement therapy. Curr Opin Clin<br />
Nutr Metab Care 2001;4:219–25.<br />
2. A.S.P.E.N. Board of Direc<strong>to</strong>rs and the Clinical Guidelines<br />
Task Force. Guidelines for the use of parenteral and enteral<br />
nutrition in adult and pediatric patients. JPEN J Parenter<br />
Enteral Nutr 2002;26S:1SA–6SA.<br />
3. Uehara M, Plank LD, Hill GL. Components of energy<br />
expenditure in patients with severe sepsis and major trauma: a<br />
basis for clinical care. Crit Care Med 1999;27:1295–302.<br />
7. Answer: A<br />
J.G. is receiving CVVHD using a dialysis solution<br />
containing dextrose 2% at a rate of 1 L/hour, which will<br />
supply 480 g of dextrose per day. Because an estimated<br />
35% <strong>to</strong> 45% of dextrose in the CRRT dialysate is absorbed,<br />
168–216 g of dextrose per day would be absorbed from J.G.’s<br />
dialysate. This dextrose delivery should be accounted for<br />
in J.G.’s nutrition regimen, necessitating a decrease in the<br />
amount of dextrose administered through modalities other<br />
than CRRT. Decreasing the dextrose in the PN formulation<br />
by about 200 g/day (Answer A) is therefore the best option.<br />
Decreasing the dextrose in the PN by 480 g/day (Answer<br />
B) is incorrect because it represents 100% absorption of the<br />
dextrose being supplied through CRRT when only 35% <strong>to</strong><br />
45% is actually absorbed. Therefore, decreasing the dextrose<br />
delivery by 480 g/day would result in a caloric deficit.<br />
Answer C (increase dextrose by 200 g/day) and Answer<br />
D (increase dextrose by 480 g/day) are incorrect because<br />
dextrose in the PN formulation should be decreased, not<br />
increased, <strong>to</strong> avoid overfeeding and its inherent risks.<br />
1. Bellomo R, Martin H, Parkin G, Love J, Kearley Y, Boyce N.<br />
Continuous arteriovenous haemodiafiltration in the critically<br />
ill: influence on major nutrient balances. Intensive Care Med<br />
1991;17:399–402.<br />
2. Marin A, Hardy G. Practical implications of nutritional support<br />
during continuous renal replacement therapy. Curr Opin Clin<br />
Nutr Metab Care 2001;4:219–25.<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
8. Answer: A<br />
J.G. is receiving propofol at 11 mL/hour, which provides<br />
1.1 kcal/mL through its vehicle (10% fat emulsion). This<br />
amount of propofol will provide 290 kcal/day and 29 g of fat<br />
per day. The amount of fat emulsion in J.G.’s PN formulation<br />
must be reduced <strong>to</strong> avoid overfeeding. Decreasing the lipid<br />
emulsion by 29 g/day (Answer A) will reduce the fat intake by<br />
about the same amount of fat being provided by the propofol<br />
drip; making Answer A the best answer. Decreasing lipid<br />
emulsion by 53 g/day (Answer C) would decrease the lipid<br />
delivery by an amount that exceeds that being provided by<br />
the propofol drip, making Answer C is incorrect. Answer<br />
B (increase lipid emulsion by 29 g/day) and Answer D<br />
(increase lipid emulsion by 53 g/day) are incorrect because<br />
the lipid content should be reduced <strong>to</strong> avoid overfeeding.<br />
Once the propofol drip is discontinued, readjustment of the<br />
PN formulation will be required.<br />
1. Lowrey TS, Dunlap AW, Brown RO, Dickerson RN, Kudsk<br />
KA. Pharmacologic influence on nutrition support therapy:<br />
use of propofol in a patient receiving combined enteral and<br />
parenteral nutrition support. Nutr Clin Pract 1996;11:147–9.<br />
2. Mateu-de An<strong>to</strong>nio J, Barrachina F. Propofol infusion and<br />
nutrition support. Am J Health Syst Pharm 1997;52:2515–6.<br />
9. Answer: C<br />
Thiamine (Answer C) should be supplemented in<br />
J.G.’s PN formulation because it is lost in significant<br />
amounts during CRRT, making Answer C the correct<br />
answer. Thiamine is important in dextrose metabolism,<br />
and supplementation of 50–100 mg/day is recommended<br />
for patients receiving CRRT. Vitamin A (Answer A) and<br />
vitamin D (Answer B) are fat-soluble and are not removed<br />
<strong>to</strong> any appreciable degree during CRRT, so Answer A and<br />
Answer B are incorrect. Although vitamin C (Answer D) is<br />
lost in the CRRT filtrate, the clinical significance of this loss<br />
is unknown, and vitamin C supplementation is not currently<br />
recommended; thus Answer D is incorrect.<br />
1. Berger MM, Shenkin A, Revelly JP, Roberts E, Cayeux MC,<br />
Baines M, et al. Copper, selenium, zinc, and thiamine balances<br />
during continuous venovenous hemodiafiltration in critically<br />
ill patients. Am J Clin Nutr 2004;80:410–6.<br />
2. S<strong>to</strong>ry DA, Ronco C, Bellomo R. Trace element and vitamin<br />
concentrations and losses in critically ill patients treated<br />
with continuous venovenous hemofiltration. Crit Care Med<br />
1999;27:220–3.<br />
10. Answer: D<br />
In patients like J.G. (weight 60 kg) receiving CRRT,<br />
protein intakes of 2.5 g/kg/day have been shown <strong>to</strong><br />
optimize nitrogen balance; thus Answer D (150 g/day) is<br />
correct. Protein intakes less than 2.5 g/kg/day have been<br />
associated with serum amino acid concentrations below the<br />
reference range, whereas protein intakes of 2.5 g/kg/day<br />
are associated with a normalization of serum amino acid<br />
concentrations and a higher prevalence of positive nitrogen<br />
balance. Answer A (60 g/day), Answer B (90 g/day), and<br />
Answer C (120 g/day) provide only 1 g/kg/day, 1.5 g/kg/day,<br />
and 2 g/kg/day of protein, respectively; therefore, Answer<br />
A, Answer B, and Answer C are incorrect because the<br />
protein intake is insufficient <strong>to</strong> meet J.G.’s needs.<br />
1. Scheinkestel CD, Adams F, Mahony L, Bailey M, Davies<br />
AR, Nyulasi I, et al. Impact of increasing parenteral protein<br />
loads on amino acid levels and balance in critically ill anuric<br />
patients on continuous renal replacement therapy. Nutrition<br />
2003;19:733–40.<br />
2. Scheinkestel CD, Kar L, Marshall K, Bailey M, Davies A,<br />
Nyulasi I, et al. Prospective randomized trial <strong>to</strong> assess caloric<br />
and protein needs of critically ill, anuric, ventilated patients<br />
requiring continuous renal replacement therapy. Nutrition<br />
2003;19:909–16.<br />
11. Answer: C<br />
In patients like J.G. with ARF, there are derangements<br />
of serum amino acids. Studies have demonstrated that<br />
patients with ARF should receive an essential–nonessential<br />
amino acid combination when PN is required; thus, Answer<br />
C (essential plus nonessential amino acid combination<br />
formulation) is the correct option for J.G.’s PN formulation.<br />
Essential amino acid–only formulations (Answer A) are<br />
more costly than standard amino acid formulations and have<br />
not been shown <strong>to</strong> produce a clinical benefit; thus Answer<br />
A is incorrect. A nonessential amino acid formulation<br />
(Answer B) would put J.G. at risk of amino acid deficiencies<br />
if essential amino acids were not provided, so Answer B is<br />
incorrect. Modular protein formulations (Answer D) are not<br />
available for administration in PN formulations but are used<br />
in enteral nutrition (EN) <strong>to</strong> supplement oral intake or tube<br />
feeds; therefore, Answer D is incorrect.<br />
1. A.S.P.E.N. Board of Direc<strong>to</strong>rs and the Clinical Guidelines<br />
Task Force. Guidelines for the use of parenteral and enteral<br />
nutrition in adult and pediatric patients. JPEN J Parenter<br />
Enteral Nutr 2002;26S:1SA–6SA.<br />
2. Mirtallo JM, Schneider PJ, Mavko K, Ruberg RL, Fabri PJ.<br />
A comparison of essential and general amino acid infusions<br />
in the nutritional support of patients with compromised renal<br />
function. JPEN J Parenter Enteral Nutr 1982;6:109–13.<br />
3. Feinstein EI, Blumenkrantz MJ, Healy M, Koffler A, Silberman<br />
H, Massry SG, et al. Clinical and metabolic responses <strong>to</strong><br />
parenteral nutrition in acute renal failure: a controlled doubleblind<br />
study. Medicine 1981;60:124–37.<br />
12. Answer: B<br />
J.G. has ARF and is receiving CVVHD with citrate<br />
anticoagulation. Her condition and therapies put her at risk of<br />
both calcium and phosphorus imbalance. Close moni<strong>to</strong>ring<br />
of serum ionized calcium and phosphorus concentrations<br />
is vital; therefore, Answer B (calcium balance should be<br />
frequently assessed by moni<strong>to</strong>ring J.G.’s serum ionized<br />
calcium and serum phosphorus concentrations) is correct.<br />
The serum ionized calcium is more reliable in patients with<br />
hypoalbuminemia, which is common in ARF. Answer A<br />
(citrate anticoagulation will likely induce hypercalcemia,<br />
thus requiring a reduction in the amount of J.G.’s calcium<br />
intake) is incorrect because citrate anticoagulation would<br />
likely induce hypocalcemia because of calcium chelation by<br />
citrate. Because calcium is filtered by CRRT, hypocalcemia<br />
may develop, and the need for calcium supplementation is<br />
common in patients receiving CRRT; therefore, Answer<br />
C (hypocalcemia is rare in patients such as J.G. with ARF<br />
receiving CRRT, and calcium supplementation will not<br />
be required) is incorrect. Hyperphosphatemia is unlikely<br />
because phosphorus is removed by CRRT; however, this<br />
would not preclude correction of hypocalcemia, if necessary.<br />
Therefore, Answer D (calcium supplementation in J.G.<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 37 Gastroenterology and Nutrition <strong>Answers</strong>
should only occur if her serum phosphorus concentration is<br />
within the reference range) is incorrect.<br />
1. Wooley JA, Btaiche IF, Good KL. Metabolic and nutritional<br />
aspects of acute renal failure in critically ill patients requiring<br />
continuous renal replacement therapy. Nutr Clin Pract<br />
2005;20:176–91.<br />
2. Cubat<strong>to</strong>li L, Teruzzi M, Cormio M, Lampati L, Pesenti A.<br />
Citrate anticoagulation during CVVH in high risk bleeding<br />
patients. Int J Artif Organs 2007;30:244–52.<br />
13. Answer: D<br />
M.T.’s current metabolism is likely <strong>to</strong> be unchanged<br />
(Answer D) compared with her normal metabolic state<br />
because isolated ARF caused by nephro<strong>to</strong>xic injury does<br />
not increase energy needs, making Answer D correct.<br />
If ARF is accompanied by critical illness, then resting<br />
energy expenditure will increase. M.T. is not critically ill;<br />
therefore, Answer A (resting energy expenditure is greatly<br />
increased) is incorrect. The presence of ARF is associated<br />
with increased gluconeogenesis and increased protein<br />
catabolism; therefore, Answer B (gluconeogenesis is<br />
decreased) and Answer C (protein catabolism is decreased)<br />
are incorrect.<br />
1. Druml W. Metabolic aspects of continuous renal replacement<br />
therapies. Kidney Int Suppl 1999;72:S56–S61.<br />
2. A.S.P.E.N. Board of Direc<strong>to</strong>rs and the Clinical Guidelines Task<br />
Force. Guidelines for the use of parenteral and enteral nutrition<br />
in adult and pediatric patients. JPEN J Parenter Enteral Nutr<br />
2002;26S:1SA–6SA.<br />
14. Answer: A<br />
M.T. is not receiving dialysis; therefore, a low-electrolyte<br />
renal disease–specific enteral product (Answer A) would be<br />
the best choice for her tube feedings. If dialysis is required in<br />
the future, a high-nitrogen product (Answer D) would be an<br />
appropriate choice, but at this time, it is not the best option.<br />
An immune-enhancing product (Answer B) would not be<br />
the best choice because current evidence does not support<br />
its use in patients with ARF, and these formulations are<br />
much more expensive than standard renal disease-specific<br />
products. A calorie-dense product (Answer C) could be an<br />
option if fluid restriction is needed; however, these products<br />
are associated with gastroparesis, making other alternatives<br />
more desirable when initiating feedings.<br />
1. Wooley JA, Btaiche IF, Good KL. Metabolic and nutritional<br />
aspects of acute renal failure in critically ill patients requiring<br />
continuous renal replacement therapy. Nutr Clin Pract<br />
2005;20:176–91.<br />
2. Kapadia FN, Bhojani K, Shah B. Special issues in the patient<br />
with renal failure. Crit Care Clin 2003;19:233–51.<br />
15. Answer: A<br />
M.T.’s prealbumin and albumin concentrations must be<br />
interpreted carefully. Prealbumin is renally eliminated;<br />
thus in patients like M.T. with ARF, serum prealbumin<br />
concentrations will be falsely elevated, making Answer A<br />
(her serum prealbumin concentration is falsely elevated)<br />
the correct answer. A reasonable goal for M.T.’s serum<br />
prealbumin concentration is 30 mg/dL or higher. M.T.<br />
could be malnourished despite a normal serum prealbumin<br />
concentration because of the false elevation in serum<br />
prealbumin concentrations described previously. Therefore,<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
38<br />
Answer B (she is not malnourished because her serum<br />
prealbumin concentration is within the reference range)<br />
is incorrect. Albumin is a negative acute-phase protein<br />
that decreases in response <strong>to</strong> stress and is therefore not a<br />
good indica<strong>to</strong>r of malnutrition in the acute care setting. In<br />
addition, M.T.’s serum albumin concentration is not within<br />
the reference range. For these reasons, Answer C (she is<br />
malnourished because her serum albumin concentration<br />
is decreased) and Answer D (her serum albumin<br />
concentration is within the reference range; therefore, she is<br />
not malnourished) are incorrect.<br />
1. Liu KD, Stralovich-Romani A, Cher<strong>to</strong>w GM. Nutrition support<br />
for adult patients with acute renal failure. In: Merritt R, ed. The<br />
A.S.P.E.N. Nutrition Support Practice Manual, 2nd ed. Silver<br />
Spring, MD: American Society for Parenteral and Enteral<br />
Nutrition, 2005:281–6.<br />
2. A.S.P.E.N. Board of Direc<strong>to</strong>rs and the Clinical Guidelines<br />
Task Force. Guidelines for the use of parenteral and enteral<br />
nutrition in adult and pediatric patients. JPEN J Parenter<br />
Enteral Nutr 2002;26S:1SA–6SA.<br />
16. Answer: A<br />
M.T. has developed metabolic acidosis (Answer A)<br />
as evidenced by the low serum pH and bicarbonate<br />
concentration; thus Answer A is correct. Metabolic acidosis<br />
is common in patients with ARF because of the kidney’s<br />
decreased ability <strong>to</strong> synthesize and reabsorb bicarbonate<br />
and its impaired ability <strong>to</strong> excrete hydrogen ions. For this<br />
reason, metabolic alkalosis (Answer B) is uncommon,<br />
unless iatrogenic. Neither respira<strong>to</strong>ry acidosis (Answer C)<br />
nor respira<strong>to</strong>ry alkalosis (Answer D) is evident by the blood<br />
gas results (pCO 2<br />
35 mm Hg).<br />
1. Wooley JA, Btaiche IF, Good KL. Metabolic and nutritional<br />
aspects of acute renal failure in critically ill patients requiring<br />
continuous renal replacement therapy. Nutr Clin Pract<br />
2005;20:176–91.<br />
2. Leblanc M. Acid-base balance in acute renal failure and<br />
renal replacement therapy. Best Pract Res Clin Anaesthesiol<br />
2004;18:113–27.<br />
17. Answer: A<br />
W.G.’s renal replacement therapy has been changed<br />
from intermittent hemodialysis <strong>to</strong> CRRT. With this change,<br />
one consideration for W.G. is that while phosphorus is<br />
not removed by intermittent hemodialysis, it is removed<br />
by CRRT modalities. Therefore, W.G.’s oral phosphate<br />
binder should be discontinued (Answer A) <strong>to</strong> prevent<br />
hypophosphatemia, making Answer A the best answer.<br />
Renal vitamin formulations, which contain water-soluble<br />
vitamins, should be continued because these vitamins are<br />
removed during CRRT. Thus, Answer B (oral renal vitamin<br />
formulation should be discontinued) is incorrect. If PN<br />
becomes necessary, neither selenium (Answer C) nor zinc<br />
(Answer D) should be removed from the PN formulation.<br />
Selenium supplementation should be continued because,<br />
although selenium will accumulate in ARF, it is removed<br />
by CRRT. Although zinc concentrations have been reported<br />
<strong>to</strong> be elevated in patients with CRRT, the reported increases<br />
have been mild, and the clinical impact is unknown at this<br />
time. Therefore Answer C and Answer D are incorrect.<br />
1. Berger MM, Shenkin A, Revelly JP, Roberts E, Cayeux MC,<br />
Baines M, et al. Copper, selenium, zinc, and thiamine balances<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
during continuous venovenous hemodiafiltration in critically<br />
ill patients. Am J Clin Nutr 2004;80:410–6.<br />
2. S<strong>to</strong>ry DA, Ronco C, Bellomo R. Trace element and vitamin<br />
concentrations and losses in critically ill patients treated<br />
with continuous venovenous hemofiltration. Crit Care Med<br />
1999;27:220–3.<br />
18. Answer: D<br />
W.G.’s serum glucose concentration has been consistently<br />
elevated. The best approach for managing his hyperglycemia<br />
would be <strong>to</strong> start regular insulin by continuous intravenous<br />
infusion (Answer D); thus Answer D is correct. Using a<br />
sliding scale regimen of insulin aspart (Answer B) would<br />
be a reactive approach <strong>to</strong> hyperglycemia as opposed <strong>to</strong><br />
a proactive approach with the insulin infusion. Sliding<br />
scale insulin regimens are no longer widely used in ICUs.<br />
Although adding regular insulin <strong>to</strong> the PN formulation<br />
(Answer C) is more convenient for the nursing staff, it is<br />
not ideal for a patient like W.G. who is receiving CRRT.<br />
If insulin is in the PN formulation and CRRT is s<strong>to</strong>pped<br />
for any reason (e.g., because of filter clotting), the glucose<br />
delivery from the dialysis and replacement solutions will<br />
abruptly s<strong>to</strong>p, creating the potential for hypoglycemia unless<br />
the PN formulation is also s<strong>to</strong>pped. Similarly, administering<br />
insulin glargine subcutaneously every night (Answer A)<br />
would place the patient at risk of hypoglycemia in the event<br />
that any glucose source is discontinued.<br />
1. Wooley JA, Btaiche IF, Good KL. Metabolic and nutritional<br />
aspects of acute renal failure in critically ill patients requiring<br />
continuous renal replacement therapy. Nutr Clin Pract<br />
2005;20:176–91.<br />
2. Scheinkestel CD, Adams F, Mahony L, Bailey M, Davies<br />
AR, Nyulasi I, et al. Impact of increasing parenteral protein<br />
loads on amino acid levels and balance in critically ill anuric<br />
patients on continuous renal replacement therapy. Nutrition<br />
2003;19:733–40.<br />
19. Answer: B<br />
Various formulas are available for calculating nitrogen<br />
balance. Standard formulas have been revised <strong>to</strong> be used<br />
in patients receiving CRRT. W.G.’s nitrogen balance is<br />
negative 6.5 (-6.5) g of nitrogen (Answer B). This value can<br />
be calculated using the following equation:<br />
Nitrogen balance (g/day) = nitrogen intake (g/day) −<br />
nitrogen loss (g/day). In patients receiving CRRT, nitrogen<br />
loss (g/day) = effluent urea nitrogen loss (g/day) + amino<br />
acid losses across CRRT membrane (g/day) + urine urea<br />
nitrogen [UUN] (g/day) + insensible losses (2–4 g/day).<br />
W.G. is receiving 175 g of protein per day through his<br />
enteral formulation and additional protein supplementation.<br />
This intake provides 28 g of nitrogen per day (175 g of<br />
protein/6.25 g of protein per gram of nitrogen). The effluent<br />
urea nitrogen loss (grams per day) = <strong>to</strong>tal volume of<br />
replacement fluid (liters) + dialysate fluid (liters) + volume<br />
(liters) of parenteral volume removed from the patient over<br />
24 hours × the average urea nitrogen from the effluent<br />
sample (51 mg/dL). Convert 51 mg/dL <strong>to</strong> grams per liter<br />
by multiplying by 0.01 = 0.51 g of nitrogen per liter. Total<br />
replacement fluid plus dialysate fluid plus parenteral volume<br />
removed = 36,000 mL + 12,000 mL + 8,000 mL = 56,000<br />
mL = 56 L. Therefore, 56 L × 0.51 g of N per liter = 28.5<br />
g of nitrogen is lost as dialysate urea nitrogen. Dialysate<br />
plus replacement fluids are infusing at 2 L/hour; therefore,<br />
amino acid losses across the CRRT membrane = 2 g of N<br />
per day. Because W.G. is anuric, the UUN is omitted from<br />
the calculation. Adding 4 g of nitrogen for insensible losses<br />
gives a <strong>to</strong>tal of 34.5 g of nitrogen out. Nitrogen balance = 28<br />
g of nitrogen in – 34.5 g of nitrogen out = − 6.5 g of nitrogen.<br />
Answer A [negative 9 (−9) g of N], Answer C [negative 1.5<br />
(−1.5) g of N], and Answer D [positive 1 (+1) g of N] are<br />
incorrect based on the above calculations.<br />
1. Liu KD, Stralovich-Romani A, Cher<strong>to</strong>w GM. Nutrition support<br />
for adult patients with acute renal failure. In: Merritt R, ed. The<br />
A.S.P.E.N. Nutrition Support Practice Manual, 2nd ed. Silver<br />
Spring, MD: American Society for Parenteral and Enteral<br />
Nutrition, 2005:281–6.<br />
2. Manning EM, Shenkin A. Nutritional assessment in the<br />
critically ill. Crit Care Clin 1995;11:603–34.<br />
20. Answer: D<br />
W.G. has been converted from intermittent hemodialysis<br />
<strong>to</strong> CRRT. A high-nitrogen feeding formulation (Answer<br />
D) should be initiated because it will meet the high protein<br />
needs of this patient receiving CRRT. Also, additional<br />
protein supplementation will be needed. A low-electrolyte,<br />
renal disease–specific enteral formulation (Answer A) is not<br />
needed at this time because the low-electrolyte composition<br />
of these products is not needed during CRRT. Immuneenhancing<br />
feeding formulations (Answer B) may have a<br />
role, but currently neither clinical nor literature support is<br />
available <strong>to</strong> justify the use of these expensive formulations<br />
in patients receiving CRRT. Calorie-dense feeding<br />
formulations (Answer C) often lead <strong>to</strong> gastroparesis, which<br />
is common in patients such as W.G. who have diabetes<br />
mellitus and are receiving CRRT; thus Answer C is not the<br />
best answer.<br />
1. Wooley JA, Btaiche IF, Good KL. Metabolic and nutritional<br />
aspects of acute renal failure in critically ill patients requiring<br />
continuous renal replacement therapy. Nutr Clin Pract<br />
2005;20:176–91.<br />
2. Kapadia FN, Bhojani K, Shah B. Special issues in the<br />
patient with renal failure. Crit Care Clin 2003;19:233–5<br />
Home Parenteral Nutrition<br />
21. Answer: D<br />
A 70-year-old man was hospitalized with pancreatitis<br />
associated with biliary tract disease. Fifteen days after<br />
admission, after undergoing cholecystec<strong>to</strong>my, he is unable<br />
<strong>to</strong> <strong>to</strong>lerate oral nutrition. Two pancreatic pseudocysts were<br />
identified by ultrasound examination. The best nutrition<br />
support regimen for home nutrition support for this patient<br />
is Answer D (enteral feeding with the tip of the feeding<br />
tube located past the ligament of Treitz). There are several<br />
studies demonstrating that a nasojejunal feeding tube<br />
with the tip past the ligament of Treitz provides effective<br />
nutrition without pancreatic stimulation, which is the cause<br />
of the pain when oral feedings are attempted. Although<br />
difficult, this type of feeding can be done at home and, if<br />
it is <strong>to</strong>lerated, saves the high cost and complication rate of<br />
home PN. Answer A (PN though a central venous access<br />
device [CVAD]) is incorrect because PN is not indicated<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 39 Gastroenterology and Nutrition <strong>Answers</strong>
unless the patient does not <strong>to</strong>lerate a trial of nasojejunal<br />
feedings. Answer B (nasogastric feedings) is incorrect<br />
because nasogastric feedings empty in<strong>to</strong> the duodenum and<br />
thus stimulate the pancreas, resulting in pain. Answer C (PN<br />
through a peripheral venous catheter) is incorrect for two<br />
reasons. First, the patient has not had a trial of nasojejunal<br />
feedings, and secondly, peripheral PN is impractical at<br />
home because peripheral venous catheters often need <strong>to</strong> be<br />
replaced every 1–2 days, resulting in significant nursing<br />
effort and decreasing quality of life for the patient.<br />
1. McClave SA. Nutrition support in acute pancreatitis.<br />
Gastroenterol Clin North Am 2007;36:65–74.<br />
2. McClave SA, Chang WK, Dhaliwal R, Heyland DK. Nutrition<br />
support in acute pancreatitis: a systematic review of the<br />
literature. JPEN J Parenter Enteral Nutr 2006;30:143–56.<br />
3. ASPEN Board of Direc<strong>to</strong>rs and the Clinical Guidelines Task<br />
Force. Guidelines for the use of parenteral and enteral nutrition<br />
in adult and pediatric patients. JPEN 2002;26(1 Suppl):1SA–<br />
138SA.<br />
22. Answer: B<br />
R.C. is a 40-year-old who underwent bowel resection<br />
secondary <strong>to</strong> mesenteric artery thrombosis, leaving him<br />
with short bowel syndrome (SBS). He will require home<br />
PN probably for the rest of his life. The most appropriate<br />
access for R.C. is Answer B (a tunneled CVAD with the<br />
tip in the superior vena cava). Either an implanted line, a<br />
percutaneously inserted central catheter (PICC), or an<br />
implanted port with the tip in the superior vena cava is<br />
appropriate for all patients receiving home PN. A patient<br />
receiving home PN also needs a CVAD that is reasonably<br />
resistant <strong>to</strong> accidental dislodgement. These CVADs are<br />
placed under the skin, and some have a cuff that makes them<br />
more resistant <strong>to</strong> dislodgement. Answer A (a percutaneous<br />
subclavian CVAD) is incorrect because these catheters are<br />
prone <strong>to</strong> being dislodged, which may result in significant<br />
bleeding. Answer C (a femoral CVAD with the tip located<br />
distal <strong>to</strong> the bifurcation of the iliac veins) is incorrect<br />
because femoral catheters increase the risk of infection, and<br />
most intravenous CVADs are <strong>to</strong>o short <strong>to</strong> reach the superior<br />
vena cava from a femoral approach. Answer D (a peripheral<br />
venous catheter) is incorrect because these catheters are<br />
intended for short-term use only, and R.C. will need an<br />
intravenous catheter for the rest of his life.<br />
1. ASPEN Board of Direc<strong>to</strong>rs and the Clinical Guidelines Task<br />
Force. Guidelines for the use of parenteral and enteral nutrition<br />
in adult and pediatric patients. JPEN 2002;26(1 Suppl):1SA–<br />
138SA.<br />
2. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Pract 2007;22:340–50.<br />
23. Answer: C<br />
A 45-year-old woman required a massive bowel resection<br />
and duodenocolos<strong>to</strong>my after a mo<strong>to</strong>r vehicle accident. The<br />
first step in the process of discharging a patient home on PN<br />
is <strong>to</strong> discuss the need for home PN with a discharge planner<br />
(Answer C); thus Answer C is correct. Finding a physician<br />
willing <strong>to</strong> manage the patient’s PN at home (Answer A)<br />
is incorrect. Although finding a physician experienced in<br />
home PN is desirable, if funding has not been ensured, it<br />
is unlikely that she will be able <strong>to</strong> pay for her PN. Answer<br />
B (find a home care provider <strong>to</strong> make the PN) will need <strong>to</strong><br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
40<br />
be accomplished before discharge; however, this answer is<br />
incorrect because it is not the first step in the process. The<br />
home PN provider will need funding information before<br />
accepting the patient. Training the patient and her family in<br />
CVAD care and PN administration (Answer D) is another<br />
important step in the process, but it is not the first step,<br />
making Answer D incorrect.<br />
1. Messing B, Joly F. Guidelines for management of home<br />
parenteral support in adult chronic intestinal failure patients.<br />
Gastroenterology 2006:130:S43–S51.<br />
2. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Pract 2007;22:340–50.<br />
3. Howard L. Home parenteral nutrition: survival, cost, and<br />
quality of life. Gastroenterology 2006;130:S52–S59.<br />
24. Answer: D<br />
Reimbursement for home PN by most insurance plans<br />
is provided based on the patient meeting certain criteria.<br />
Answer D (the patient is unable <strong>to</strong> maintain body mass<br />
because of intestinal failure) is the condition that most<br />
correctly identifies a patient for whom home PN will be<br />
reimbursed. Answer A (the patient is unable <strong>to</strong> maintain<br />
body mass because of malabsorption of oral nutrients) is<br />
incorrect because a trial of tube feedings with a predigested<br />
enteral formulation has not been attempted. Inability <strong>to</strong><br />
eat or refusal <strong>to</strong> have tube feedings (Answer B) is not an<br />
indication for home PN that would be reimbursed by most<br />
insurance companies, making Answer B incorrect. Answer<br />
C (inability <strong>to</strong> eat because of a terminal illness with a life<br />
expectancy of 1 month) is incorrect because a patient with<br />
a terminal illness and 1-month life expectancy is generally<br />
not considered an acceptable candidate for home PN.<br />
However, controversy does exist because some data suggest<br />
that patients in this condition may have an improved quality<br />
of life with nutrition support. Most experts in the field of<br />
nutrition support, however, feel that the risk of complications<br />
with home PN, including increased infections, may actually<br />
decrease quality of life and hasten a patient’s death.<br />
1. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Prac 2007;22:340–50.<br />
2. Kovacevich DS, Frederick A, Kelly D, Nishikawa RA, Young<br />
L. Standards for specialized nutrition support: home care<br />
patients. Nutr Clin Prac 2005;20:579–90.<br />
3. Messing B, Joly F. Guidelines for management of home<br />
parenteral support in adult chronic intestinal failure patients.<br />
Gastroenterology 2006:130:S43–S51.<br />
25. Answer: C<br />
Before a patient can be discharged <strong>to</strong> receive PN in the<br />
home, electricity, a refrigera<strong>to</strong>r, and a telephone (Answer C)<br />
must be in the home. The PN solutions will be delivered for<br />
a 7–14 day period. These solutions must be refrigerated until<br />
use. A telephone is necessary <strong>to</strong> be able <strong>to</strong> communicate<br />
with the medical provider, home health nurses, and the home<br />
PN provider. Thus, Answer C is the correct answer. Answer<br />
B (transportation <strong>to</strong> a labora<strong>to</strong>ry for weekly blood draws)<br />
is incorrect because labora<strong>to</strong>ry samples can be drawn in<br />
the home by the home care nurse. Daily nursing care in the<br />
home <strong>to</strong> initiate and discontinue the PN infusion (Answer<br />
A) is impractical and not supported by third-party payers.<br />
The patient or a caregiver must be trained <strong>to</strong> administer<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
the PN solution daily. Having a caregiver, other than the<br />
patient, <strong>to</strong> care for the CVAD and manage the PN infusion<br />
(Answer D) would be helpful for all patients, but it is not<br />
necessary before discharge because most patients can do<br />
these functions; thus Answer D is not the best answer.<br />
1. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Prac 2007;22:340–50.<br />
2. Kovacevich DS, Frederick A, Kelly D, Nishikawa RA, Young<br />
L. Standards for specialized nutrition support: home care<br />
patients. Nutr Clin Pract. 2005;20:579–9.<br />
26. Answer: B<br />
A patient with Crohn’s disease and SBS has a tunneled<br />
CVAD for home PN. She has a temperature of 104°F (40°C)<br />
for several days. The most likely cause of her fever is a<br />
CVAD-associated infection (Answer B); thus, Answer B<br />
is the correct answer. Answer A (Crohn’s disease–related<br />
hyperthermia) is possible, but in a patient receiving home<br />
PN through a CVAD, infection is more likely <strong>to</strong> explain her<br />
fever; thus, Answer A is incorrect. Answer C (a systemic<br />
viral infection) is also possible, but a CVAD-associated<br />
infection is more likely with the high fever. Answer D<br />
(hypersensitivity reaction <strong>to</strong> the fat emulsion in the PN) is<br />
incorrect because the patient has been receiving home PN<br />
for several years.<br />
1. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Prac 2007;22:340–50.<br />
2. Yildizeli B, Lacin T, Batirel HF, Yuksel M. Complications and<br />
management of long-term central venous access CVADs and<br />
ports. J Vasc Access 2004;5:174–8.<br />
27. Answer: D<br />
A 45-year-old man (weight 75 kg, height 165 cm ) with<br />
SBS (150 cm small bowel and the entire colon remaining)<br />
is receiving 2200 calories only 2 days/week. Answer D<br />
(his PN infusion should be weaned <strong>to</strong> 1 day/week) is the<br />
correct answer. He has had stable weight gain for 3 years,<br />
is well hydrated, and does not need additional hydration<br />
on the days that he does not receive a PN infusion. Thus,<br />
a trial of weaning his PN <strong>to</strong> 1 day/week is appropriate.<br />
Both Answer A (referral <strong>to</strong> an intestinal rehabilitation<br />
program) and Answer B (referral <strong>to</strong> an intestinal transplant<br />
program) are incorrect because it appears that he will be<br />
able <strong>to</strong> wean off PN without additional assistance; his bowel<br />
length is long enough, and he has been able <strong>to</strong> wean <strong>to</strong> only<br />
two PN infusions weekly. It would be desirable <strong>to</strong> attempt<br />
<strong>to</strong> wean him off PN first before referral <strong>to</strong> a rehabilitation<br />
or transplantation program. Answer C (his PN should be<br />
changed <strong>to</strong> a daily infusion of 630 kcal) is incorrect because<br />
he is doing well with hydration using his current twice<br />
weekly regimen, so there is no need <strong>to</strong> go back <strong>to</strong> a daily<br />
infusion.<br />
1. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Prac 2007;22:340–50.<br />
2. Messing B, Joly F. Guidelines for management of home<br />
parenteral support in adult chronic intestinal failure patients.<br />
Gastroenterology 2006:130:S43–S51.<br />
3. Jeppesen PB, Mortensen PB. Intestinal failure defined by<br />
measurements of intestinal energy and wet weight absorption.<br />
Gut 2000;46:701–6.<br />
28. Answer: C<br />
A 34-year-old with Crohn’s disease and SBS (25<br />
cm residual small bowel) had a dual-energy x-ray<br />
absorptiometry (DEXA) scan with T scores reported as<br />
lumbosacral spine −3.2 and right femoral neck −3.0. This<br />
patient has osteoporosis with a significant risk of fracture;<br />
thus the best treatment for her is <strong>to</strong> start pamidronate 60<br />
mg intravenously every month (Answer C). Answer A (start<br />
alendronate oral solution 7.5 mg daily) is not the best answer<br />
because alendronate in either the tablet or liquid dosage form<br />
is likely <strong>to</strong> be inadequately absorbed in this patient with<br />
severe SBS. Answer B (discontinue methylprednisolone) is<br />
incorrect because rapidly discontinuing her corticosteroid<br />
treatment is not advisable as it may result in a flare of her<br />
Crohn’s disease. Answer D (do nothing) is not the best<br />
course of action because she will require PN for her lifetime,<br />
and her osteoporosis likely will continue <strong>to</strong> worsen without<br />
treatment.<br />
1. Buchman AL, Moukarzel A. Metabolic bone disease associated<br />
with <strong>to</strong>tal parenteral nutrition. Clin Nutr 2000;19:217–31.<br />
2. Hurley DL, McMahon M. Long term parenteral nutrition and<br />
metabolic bone disease. Endocrinol Metab Clin North Am<br />
1990;19:113–31.<br />
29. Answer: A<br />
A patient receiving home PN is having difficulty aspirating<br />
blood from her CVAD for routine labora<strong>to</strong>ry testing. The<br />
CVAD flushes easily, and she reports no problems with<br />
the PN infusion. This difficulty in withdrawing blood<br />
from the CVAD likely is caused by a thrombus “flap” that<br />
allows infusion of fluid through the CVAD but obstructs<br />
the CVAD lumen when negative pressure is applied in the<br />
process of aspirating blood. Answer A (instill alteplase in<br />
the CVAD <strong>to</strong> attempt <strong>to</strong> clear the obstruction) is the correct<br />
answer. Answer B (do nothing) is incorrect because this<br />
withdrawal occlusion can progress <strong>to</strong> complete occlusion<br />
and should be addressed at this time. Answer C (instill<br />
ethanol 70% <strong>to</strong> dissolve the probable lipid occlusion) is<br />
incorrect because the most likely problem is a thrombus<br />
occlusion, not a lipid occlusion, because the catheter<br />
still flushes well. A lipid plug usually causes a complete<br />
occlusion, not just withdrawal occlusion. Answer D<br />
(have the CVAD removed) is incorrect because alteplase<br />
will likely correct the problem, avoiding CVAD removal.<br />
1. Gould JR, Carlos HW, Skinner WL. Groshong CVAD associated<br />
subclavian CVAD thrombosis. Am J Med 1993;95:419–23.<br />
2. Bern MM, Lokich JJ, Wallach SR, Bothe A Jr, Benotti PN, Arkin<br />
CF, et al. Very low doses of warfarin can prevent thrombosis in<br />
central venous CVADs. A randomized prospective trial. Ann<br />
Int Med 1990;112:4213–28.<br />
30. Answer: D<br />
The most likely cause of W.H.’s weight loss is<br />
dehydration, probably from an increase in his s<strong>to</strong>ol output.<br />
Before any changes in his therapy are made, he should be<br />
questioned <strong>to</strong> determine if his s<strong>to</strong>ol output has increased<br />
during the past week. Answer A (increase the protein and<br />
carbohydrate in his PN formulation <strong>to</strong> stimulate weight<br />
gain) and Answer B (increase the intravenous fat component<br />
of his PN formulation <strong>to</strong> stimulate weight gain) assume<br />
that his weight loss is caused by suboptimal calorie intake.<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 41 Gastroenterology and Nutrition <strong>Answers</strong>
However, a 10-kg weight loss in a 1-week period is unlikely<br />
<strong>to</strong> result from inadequate calorie intake; thus, Answer A and<br />
Answer B are incorrect. Answer C (obtain a resting energy<br />
expenditure study <strong>to</strong> determine his caloric needs) is also<br />
incorrect because it again assumes that the weight loss is<br />
caused by inadequate calorie intake. The initial intervention<br />
for W.H., given the most likely reason for the weight loss, is<br />
<strong>to</strong> provide additional intravenous fluid either by increasing<br />
his PN volume or by adding additional intravenous fluids<br />
(Answer D); thus Answer D is the correct answer. W.H.’ s<br />
weight and s<strong>to</strong>ol output should be followed daily, and the<br />
additional fluid reduced <strong>to</strong> the previous volume once W.H.’s<br />
weight has returned <strong>to</strong> his usual weight and his s<strong>to</strong>ol output<br />
has decreased <strong>to</strong> the usual volume.<br />
1. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Prac 2007;22:340–50.<br />
2. Messing B, Joly F. Guidelines for management of home<br />
parenteral support in adult chronic intestinal failure patients.<br />
Gastroenterology 2006:130:S43–S51.<br />
3. Jeppesen PB, Mortensen PB. Intestinal failure defined by<br />
measurements of intestinal energy and wet weight absorption.<br />
Gut 2000;46:701–6.<br />
31. Answer: B<br />
W.H.’s wife tells you that he has developed a tremor and<br />
is having hallucinations. These symp<strong>to</strong>ms are not normally<br />
seen in patients receiving home PN; thus Answer A (do<br />
nothing, but reassure W.H.’s wife that these symp<strong>to</strong>ms<br />
are normal) is incorrect. Hypermagnesemia can occur in<br />
patients receiving long-term home PN when receiving a<br />
trace element cocktail daily. Manganese is deposited in<br />
the basal ganglia, so hypermagnesemia results in various<br />
neurological symp<strong>to</strong>ms including those being experienced<br />
by W.H. However, other nutrient imbalances may also lead<br />
<strong>to</strong> similar symp<strong>to</strong>ms. Therefore, Answer B (have the home<br />
health nurse draw a basic metabolic panel, complete blood<br />
count, and serum manganese concentration) is the best<br />
intervention at this time, making Answer B the correct<br />
answer. Answer C (have the nurse draw a serum manganese<br />
concentration) is one of the appropriate interventions, but<br />
Answer C is not the best answer because other labora<strong>to</strong>ry<br />
tests should also be checked. Answer D (remove the<br />
trace element preparation from W.H.’s PN formulation) is<br />
incorrect. It would be premature <strong>to</strong> remove the trace elements<br />
from the PN formulation at this time. If hypermagnesemia<br />
is determined <strong>to</strong> be the cause of W.H.’s new neurological<br />
symp<strong>to</strong>ms, then the trace element preparation would have <strong>to</strong><br />
be removed, but zinc and perhaps chromium would need <strong>to</strong><br />
be added <strong>to</strong> the PN formulation <strong>to</strong> prevent a deficiency state.<br />
1. Dickerson RN. Manganese in<strong>to</strong>xication and parenteral<br />
nutrition. Nutrition 2001;17:689–93.<br />
2. Bertinet DB, Tinivella M, Balzola FA, de Francesco A, Davini<br />
O, Rizzo L, et al. Brain manganese deposition and blood levels<br />
in patients undergoing home parenteral nutrition. JPEN J<br />
Parenter Enteral Nutr 2000;24:223–7.<br />
3. Clark SF. Vitamins and trace elements. In: Gottschlick MM,<br />
DeLegge MH, Mat<strong>to</strong>x T, Mueller C, Worthing<strong>to</strong>n P, eds. The<br />
A.S.P.E.N. Nutrition Support Core Curriculum: A Case-based<br />
Approach – The Adult Patient. Silver Spring, MD: American<br />
Society for Parenteral and Enteral Nutrition, 2007, 129–59.<br />
32. Answer: A<br />
A 25-year-old woman (weight 42 kg, height 163 cm)<br />
with chronic intestinal pseudo-obstruction is admitted <strong>to</strong><br />
the hospital because of continued weight loss over the last<br />
2 years (maximum weight 60 kg). Eating causes abdominal<br />
pain, as did continuous jejunal feedings during her last<br />
hospitalization. Her symp<strong>to</strong>ms are typical of patients with<br />
chronic intestinal pseudo-obstruction. Some patients have<br />
severe small intestinal dysmotility with propulsion upward<br />
<strong>to</strong>wards the s<strong>to</strong>mach instead of downwards <strong>to</strong>ward the colon.<br />
The best plan for this patient is <strong>to</strong> plan for discharge home<br />
on PN therapy (Answer A), making Answer A the correct<br />
answer. Answer B (start high-calorie oral supplements) is<br />
incorrect because any type of oral feedings will produce<br />
the same symp<strong>to</strong>ms and will not be <strong>to</strong>lerated. Placing a<br />
transpyloric feeding tube and starting an elemental feeding<br />
formulation (Answer D) is incorrect because this therapy has<br />
already been tried and was not successful. Discharging her<br />
home with no nutrition support and waiting for her weight<br />
<strong>to</strong> decrease further (Answer C) is incorrect as she is already<br />
12 kg below her ideal weight. Further weight loss will likely<br />
occur and result in another hospitalization <strong>to</strong> initiate PN.<br />
1. Messing B, Joly F. Guidelines for management of home<br />
parenteral support in adult chronic intestinal failure patients.<br />
Gastroenterology 2006:130:S43–S51.<br />
2. Kelly DA. Intestinal failure-associated liver disease: what do<br />
we know <strong>to</strong>day? Gastroenterology 2006;S70–S77.<br />
33. Answer: C<br />
A 25-year-old man (weight 50 kg, height173 cm) has been<br />
receiving home PN for 2 years after being injured in a mo<strong>to</strong>r<br />
vehicle accident. He has SBS with 20 cm of residual small<br />
intestine and 50% of his colon. His medical his<strong>to</strong>ry includes<br />
intravenous drug abuse. His recent labora<strong>to</strong>ry results include<br />
a 4-fold increase in his alkaline phosphatase (ALK), alanine<br />
aminotransferase (ALT), aspartate aminotransferase (AST),<br />
and <strong>to</strong>tal bilirubin concentrations. The most appropriate<br />
response <strong>to</strong> the elevation in this man’s liver function<br />
tests (LFTs) is <strong>to</strong> obtain hepatitis serology and conduct a<br />
detailed drug his<strong>to</strong>ry looking for drug-induced causes of<br />
his labora<strong>to</strong>ry abnormalities (Answer C), making Answer<br />
C the correct answer. Answer A (reduce the intravenous fat<br />
emulsion in his PN formulation), Answer B (reduce both<br />
the intravenous fat emulsion and dextrose components of<br />
the PN formulation), and Answer D (discontinue his home<br />
PN therapy immediately) are incorrect because the cause<br />
of the elevated the LFTs must be determined before the<br />
correct therapy can be determined. This patient has risk<br />
fac<strong>to</strong>rs for hepatitis as well as PN-induced stea<strong>to</strong>sis and<br />
cholestasis. Additionally, with this patient’s degree of SBS,<br />
discontinuing his PN is not a practical option.<br />
1. Kelly DA. Intestinal failure-associated liver disease: what do<br />
we know <strong>to</strong>day? Gastroenterology 2006;S70–S77.<br />
2. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Pract 2007;22:340–50.<br />
3. OKeefe SJ. Bacterial overgrowth and liver complications<br />
in short bowel intestinal failure patients. Gastroenterology<br />
2006;130:S67–S69.<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
42<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
34. Answer: D<br />
T.O. is obese (i.e., 300% of IBW) and is continuing <strong>to</strong><br />
gain weight with her current PN formulation, which provides<br />
29 kcal/kg/day based on her actual weight and 58 kcal/kg/<br />
day based on an adjusted body weight for obesity. Thus,<br />
Answer A (continue the current PN formulation and follow<br />
up in 1 month) is not a good option for T.O. and is incorrect.<br />
Reducing the calories delivered by the PN formulation <strong>to</strong><br />
2500 kcal/day with 150 grams of protein per day (Answer<br />
C) is an appropriate intervention, but Answer D (decreasing<br />
the PN <strong>to</strong> 2500 kcal/day, maintaining 150 grams of protein<br />
per day, and attempting slow enteral feedings, is the best<br />
answer because T.O. should be given another trial of enteral<br />
feeding. Therefore, Answer C is incorrect and Answer D is<br />
the best answer. S<strong>to</strong>pping the PN and initiating either tube<br />
or oral feedings (Answer B) is not an appropriate option for<br />
T.O.; it will fail because she does not have adequate bowel<br />
length <strong>to</strong> have sufficient nutrient absorption <strong>to</strong> discontinue<br />
the PN.<br />
1. Siepler J. Principles and strategies for moni<strong>to</strong>ring home<br />
parenteral nutrition. Nutr Clin Prac 2007;22:340–50.<br />
2. ASPEN Board of Direc<strong>to</strong>rs and the Clinical Guidelines Task<br />
Force. Guidelines for the use of parenteral and enteral nutrition<br />
in adult and pediatric patients. JPEN 2002;26(1 Suppl):1SA–<br />
138SA.<br />
3. Seres DS. Surrogate nutrition markers, malnutrition, and<br />
adequacy of nutrition support. Nutr Clin Prac 2005;20:308–13.<br />
35. Answer: C<br />
T.O. has had an increase in s<strong>to</strong>ol output for the past<br />
2 days. The s<strong>to</strong>ol is foul-smelling, and she has crampy<br />
abdominal pain but is afebrile. She is concerned that the<br />
diarrhea will soon lead <strong>to</strong> dehydration without intervention.<br />
The best therapeutic intervention for T.O. is <strong>to</strong> start<br />
metronidazole 500 mg intravenously three times/day and<br />
order intravenous replacement fluids for her s<strong>to</strong>ol losses<br />
(Answer C), making Answer C the correct answer. Simply<br />
reassuring her that her PN formulation provides adequate<br />
volume for increased s<strong>to</strong>ol losses and having her call back in<br />
2–3 days (Answer A), is incorrect because her PN provides<br />
only 3 L/day, which will not be adequate if the s<strong>to</strong>ol volume<br />
has increased significantly. Answer B (start metronidazole<br />
500 mg intravenously three times/day and order intravenous<br />
replacement fluids) is not the best answer because with the<br />
severity of her SBS and the increased s<strong>to</strong>ol output, the transit<br />
time for metronidazole taken orally will likely be <strong>to</strong>o fast <strong>to</strong><br />
allow for efficacy. Admitting T.O. <strong>to</strong> the hospital for broadspectrum<br />
intravenous antibiotics (Answer D) is incorrect<br />
because T.O.’s symp<strong>to</strong>ms suggest bacterial overgrowth,<br />
which can be treated with metronidazole alone. Unless<br />
dehydration develops, bacterial overgrowth can usually be<br />
managed without hospital admission.<br />
1. Di Stefano M, Miceli E, Missanelli A, Corazza GR. Treatment<br />
of small intestine bacterial overgrowth. Eur Rev Med<br />
Pharmacol Sci 2005;9:217–22.<br />
2. Van Citters GW, Lin HC. Management of small intestinal<br />
bacterial overgrowth. Curr Gastroenterol Rep 2005;7:317–20.<br />
3. Parrish CR, Krenitsky J, Willcutts K, Radigan AE.<br />
Gastrointestinal disease. In: Gottschlick MM, DeLegge MH,<br />
Mat<strong>to</strong>x T, Mueller C, Worthing<strong>to</strong>n P, eds. The A.S.P.E.N.<br />
Nutrition Support Core Curriculum: A Case-based Approach<br />
– The Adult Patient. Silver Spring, MD: American Society for<br />
Parenteral and Enteral Nutrition, 2007, 508–39.<br />
36. Answer: B<br />
A 70-year-old woman is admitted <strong>to</strong> the hospital because<br />
of weight loss of unknown etiology. She has diabetes<br />
mellitus and gastroparesis (diagnosed 10 years ago) and is<br />
receiving nasojejunal feedings with a polymeric formula.<br />
After 2 weeks, she is gaining weight and her prealbumin<br />
concentration has increased. She is ready for discharge but<br />
is refusing <strong>to</strong> go home on tube feedings and would rather go<br />
home on PN. She has Medicare with no secondary provider.<br />
Because she is <strong>to</strong>lerating and responding <strong>to</strong> EN, Medicare<br />
will not cover the cost of PN therapy. Therefore, Answer<br />
A (place a tunneled CVAD, initiate PN, plan for discharge<br />
on home PN) and Answer C (discharge the patient <strong>to</strong> home<br />
on peripheral PN) are not good options for this patient who<br />
likely would not be able <strong>to</strong> pay for the cost of PN therapy.<br />
Additionally, peripheral PN is not a good option for use<br />
in the home because of the need <strong>to</strong> frequently replace the<br />
peripheral infusion site. Because she came in<strong>to</strong> the hospital<br />
with unexplained weight loss, sending her back home on<br />
a oral diet with intravenous hydration is not optimal. She<br />
likely will not continue <strong>to</strong> gain weight on this regimen, and<br />
the cost of intravenous hydration will not be reimbursed by<br />
Medicare. The best option for this patient is <strong>to</strong> discuss the<br />
complications of long-term PN with her and the fact that<br />
Medicare will not cover the cost of PN therapy, and try <strong>to</strong><br />
convince her <strong>to</strong> go home with jejunos<strong>to</strong>my tube feedings<br />
(Answer B), making Answer B the correct answer.<br />
1. Messing B, Joly F. Guidelines for management of home<br />
parenteral support in adult chronic intestinal failure patients.<br />
Gastroenterology 2006:130:S43–S51.<br />
2. Howard L. Home parenteral nutrition: survival, cost, and<br />
quality of life. Gastroenterology 2006;130:S52–S59.<br />
37. Answer: D<br />
R.C.’s labora<strong>to</strong>ry reports indicate that he is dehydrated.<br />
Therefore, doing nothing (Answer A), is not an appropriate<br />
response. The best response <strong>to</strong> R.C.’s current situation is<br />
<strong>to</strong> continue the PN formulation and give lactated Ringer’s<br />
2 L followed by lactated Ringer’s replacement for his<br />
jejunos<strong>to</strong>my losses (Answer D). Increasing the PN volume<br />
<strong>to</strong> 4.5 L may help correct the existing dehydration, but it<br />
may not be adequate depending on the jejunos<strong>to</strong>my output;<br />
therefore Answer B is not the best option. Correcting the<br />
dehydration first, then replacing the losses proactively<br />
is the best approach <strong>to</strong> prevent dehydration in the future.<br />
Answer C (increase the sodium acetate in the current PN<br />
formulation <strong>to</strong>150 mEq/day) would help <strong>to</strong> acutely correct<br />
R.C.’s metabolic acidosis, but it would not correct the<br />
dehydration; thus Answer C is not the best response.<br />
1. Parrish CR, Krenitsky J, Willcutts K, Radigan AE.<br />
Gastrointestinal disease. In: Gottschlick MM, DeLegge MH,<br />
Mat<strong>to</strong>x T, Mueller C, Worthing<strong>to</strong>n P, eds. The A.S.P.E.N.<br />
Nutrition Support Core Curriculum: A Case-based Approach<br />
– The Adult Patient. Silver Spring, MD: American Society for<br />
Parenteral and Enteral Nutrition, 2007, 508–39.<br />
2. Buchman AL, Scolapio J, Fryer J. AGA technical review<br />
on short bowel syndrome and intestinal transplantation.<br />
Gastroenterology 2003;124:1111–34.<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 43 Gastroenterology and Nutrition <strong>Answers</strong>
3. Sundaram A, Koukia P, Apovian CM. Nutritional management<br />
of short bowel syndrome in adults. J Clin Gastroenterol<br />
2002;34:207–20.<br />
38. Answer: A<br />
R.C. is at high risk of developing a zinc deficiency<br />
(Answer A) because of the fact that zinc will be lost in high<br />
concentrations from the high-output jejunos<strong>to</strong>my; thus<br />
Answer A is correct. Zinc concentrations in small bowel<br />
output can be as high as 12 mg/L; thus, R.C. may be losing<br />
as much as 18 mg of zinc per day in the jejunos<strong>to</strong>my fluid.<br />
Vitamin B 12<br />
(Answer B), folic acid (Answer C), and copper<br />
(Answer D) are not substantially eliminated in the s<strong>to</strong>ol; thus<br />
R.C.’s risk of zinc deficiency is substantially higher than<br />
the risk of vitamin B 12<br />
, folic acid, or copper deficiencies,<br />
making Answer B, Answer C, and Answer D incorrect.<br />
1. Parrish CR, Krenitsky J, Willcutts K, Radigan AE.<br />
Gastrointestinal disease. In: Gottschlick MM, DeLegge MH,<br />
Mat<strong>to</strong>x T, Mueller C, Worthing<strong>to</strong>n P, eds. The A.S.P.E.N.<br />
Nutrition Support Core Curriculum: A Case-based Approach<br />
– The Adult Patient. Silver Spring, MD: American Society for<br />
Parenteral and Enteral Nutrition, 2007, 508–39.<br />
2. Buchman AL, Scolapio J, Fryer J. AGA technical review<br />
on short bowel syndrome and intestinal transplantation.<br />
Gastroenterology 2003;124:1111–34.<br />
3. Sundaram A, Koukia P, Apovian CM. Nutritional management<br />
of short bowel syndrome in adults. J Clin Gastroenterol<br />
2002;34:207–20.<br />
39. Answer: C<br />
T.C. has developed hypoglycemia (blood glucose<br />
concentration less than 60 mg/dL. The most appropriate<br />
response <strong>to</strong> hypoglycemia after discontinuing the PN when<br />
cycling in a young infant is <strong>to</strong> increase the ramp-down<br />
time; therefore, Answer C (continue <strong>to</strong> ramp up over 1<br />
hour; increase the ramp-down time <strong>to</strong> 2 hours) is the correct<br />
answer. Answer A (do nothing) is not correct. A blood<br />
glucose concentration less than 60 mg/dL can be associated<br />
with complications, including changes in neurodevelopment;<br />
therefore, allowing T.C.’s blood glucose concentration <strong>to</strong><br />
fall <strong>to</strong> 45 mg/dL after discontinuing PN is not appropriate.<br />
Answer B (increase the ramp-up time <strong>to</strong> 2 hours; continue<br />
<strong>to</strong> ramp down over 1 hour) is incorrect because the serum<br />
glucose concentration at the maximum PN infusion rate is<br />
acceptable (90 mg/dL), so no change in the ramp-up time is<br />
needed; also, this option does not address the low glucose<br />
after discontinuing the PN. Answer D (increase both the<br />
ramp-up and ramp-down times <strong>to</strong> 2 hours) could be done;<br />
however, it is not the best answer because the ramp-up time<br />
does not need <strong>to</strong> be changed.<br />
1. Kumpf VJ, Gervasio J. Complications of parenteral nutrition.<br />
In: Gottschlick MM, DeLegge MH, Mat<strong>to</strong>x T, Mueller C,<br />
Worthing<strong>to</strong>n P, eds. The A.S.P.E.N. Nutrition Support Core<br />
Curriculum: A Case-based Approach – The Adult Patient.<br />
Silver Spring, MD: American Society for Parenteral and<br />
Enteral Nutrition, 2007, 323–39.<br />
2. Bendorf K, Friesen CA, Roberts CC. Glucose response <strong>to</strong><br />
discontinuation of parenteral nutrition in patients less than 3<br />
years of age. JPEN: J Parenteral Enteral Nutr 1996;20:120–2.<br />
40. Answer: C<br />
T.C. has been receiving a standard multivitamin<br />
preparation in her PN formulation, but only zinc and<br />
chromium, because the standard trace element preparation<br />
was removed from her PN when her direct bilirubin was<br />
elevated <strong>to</strong> 4 mg/dL. She is receiving about 40% of her<br />
nutrition by the enteral route. Her direct bilirubin in clinic<br />
<strong>to</strong>day is 2.1 mg/dL, and she has a microcytic anemia. The<br />
most appropriate response would be <strong>to</strong> draw a serum iron<br />
panel and ferritin and copper concentrations (Answer C).<br />
Deficiency of both iron and copper can cause microcytic<br />
anemia. T.C. is receiving neither iron nor copper in her<br />
PN formulation; thus she is at risk for deficiency of both.<br />
Therefore, Answer C is correct. Answer A (add standard<br />
pediatric trace elements <strong>to</strong> the PN formulation daily) is<br />
incorrect because T.C.’s direct bilirubin is still elevated,<br />
indicating cholestasis; thus, copper and manganese excretion<br />
may be compromised. The trace element preparation<br />
should not be added unless a deficiency of both copper<br />
and manganese is documented. Answer B (draw a serum<br />
iron panel and ferritin, vitamin B 12<br />
, folate, and copper<br />
concentrations) is incorrect because T.C. has been receiving<br />
both vitamin B 12<br />
and folate daily in her PN formulation, and<br />
these nutrients are associated with macrocytic anemia, not<br />
microcytic anemia. Answer D (start ferrous sulfate drops<br />
orally) is not appropriate at this time because the cause of<br />
the microcytic anemia has not been determined.<br />
1. Chessman KH, Kumpf VJ. <strong>Assessment</strong> of nutrition status and<br />
nutrition requirements. In: Dipiro JT, Talber RL, Yee GC,<br />
Matzke GR, Wells BG, Posey LM, eds. Pharmacotherapy: A<br />
Pathophysiologic Approach, 7 th edition. New York: McGraw<br />
Hill Medical, 2008, 2349–66.<br />
2. Btaiche IF, Khalidi N. Parenteral nutrition-associated liver<br />
complications in children. Pharmacotherapy 2002;22:188–211.<br />
3. Btaiche IF, Khalidi N. Metabolic complications of parenteral<br />
nutrition in adults, part 2. Am J Health Syst Pharm<br />
2004;61:2050–9.<br />
Immunonutrition<br />
41. Answer: D<br />
The best EN intervention for J.B. immediately upon<br />
admission is actually no enteral feeding (Answer D) because<br />
J.B. is hemodynamically unstable and has been incompletely<br />
resuscitated; thus Answer D is correct. However,<br />
hemodynamic instability is a relative contraindication<br />
<strong>to</strong> EN, and some institutions might begin EN in a patient<br />
such as J.B. The immune-enhancing EN formulation with<br />
omega-3 polyunsaturated fatty acids (PUFAs) 8.6 g/L and<br />
antioxidants (Answer B) would be the best response only<br />
if J.B. was hemodynamically stable so that feedings could<br />
be initiated safely, so Answer B is incorrect. Answer A<br />
(immune-enhancing EN formulation with arginine 10 g/L<br />
and omega-3 PUFAs 3.6 g/L) and Answer C (immuneenhancing<br />
EN formulation with arginine 16.3 g/L, glutamine<br />
15 g/L, nucleotides 1.6 g/L, and omega-3 PUFAs 1.7 g/L) are<br />
not correct choices because each contains arginine, which<br />
has been associated with potential harm in patients with<br />
sepsis.<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
44<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
1. Consensus recommendations from the U.S. Summit on<br />
immune-enhancing enteral therapy. JPEN J Parenter Enteral<br />
Nutr 2001;25:S61–S63.<br />
2. Kudsk KA. Immunonutrition in surgery and critical care.<br />
Annu Rev Nutr 2006;26:463–79.<br />
42. Answer: B<br />
In patients like J.B. with ARDS and acute lung injury<br />
(ALI), immune-enhancing EN formulations supplemented<br />
with the omega-3 PUFAs (eicosapentaenoic acid [EPA]<br />
and g-linolenic acid [GLA]) and antioxidants have been<br />
associated with decreased mortality and improved<br />
oxygenation. The immune-enhancing EN formulation<br />
with omega-3 PUFAs 8.6 g/L and antioxidants (Answer<br />
B) contains these nutrients and is therefore the best choice.<br />
The standard EN formulation with enteral glutamine<br />
supplementation (Answer C) is not the best option because<br />
it does not contain omega-3 PUFAs or antioxidants. Neither<br />
Answer A (immune-enhancing EN formulation with<br />
arginine, nucleotides, and omega-3 PUFAs) nor Answer<br />
D (immune-enhancing EN formulation with arginine and<br />
omega-3 PUFAs) is best for J.B. at this time because each<br />
contains arginine, which has been associated with potential<br />
harm in patients with sepsis.<br />
1. Pontes-Arruda A, Aragao AM, Albuquerque JD. Effects of<br />
enteral feeding with eicosapentaenoic acid, gamma-linolenic<br />
acid, and antioxidants in mechanically ventilated patients with<br />
severe sepsis and septic shock. Crit Care Med 2006;34:2325–<br />
33.<br />
2. Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet<br />
P, Kazandjiev G, et al. ESPEN guidelines on enteral nutrition:<br />
intensive care. Clin Nutr 2006;25:210–23.<br />
43. Answer: C<br />
Once J.B. is started on an immune-enhancing EN<br />
formulation, the duration of therapy will have <strong>to</strong> be decided.<br />
Clinical studies indicate that the greatest benefit from these<br />
formulations in patients with ARDS is obtained when therapy<br />
is continued until the patient has been extubated (Answer<br />
C); thus, Answer C is the best answer. Patients are unlikely<br />
<strong>to</strong> benefit from any immunonutrition therapy administered<br />
for only 2 days (Answer A) or 4 days (Answer B), and there<br />
is no clinical evidence that patients with ARDS derive any<br />
further improvement in outcome if immune-enhancing<br />
diets are used after they have recovered sufficiently <strong>to</strong> be<br />
extubated. Because hospital discharge will generally occur<br />
days <strong>to</strong> weeks after extubation, discontinuing the product on<br />
discharge (Answer D) is not appropriate for the duration of<br />
J.B.’s immunonutrition therapy.<br />
1. Pontes-Arruda A, Aragao AM, Albuquerque JD. Effects of<br />
enteral feeding with eicosapentaenoic acid, gamma-linolenic<br />
acid, and antioxidants in mechanically ventilated patients with<br />
severe sepsis and septic shock. Crit Care Med 2006;34:2325–<br />
33.<br />
2. Consensus recommendations from the U.S. Summit on<br />
immune-enhancing enteral therapy. JPEN J Parenter Enteral<br />
Nutr 2001;25:S61–S63.<br />
44. Answer: C<br />
If a patient with ARDS receiving an immune-enhancing<br />
EN formulation was evaluated for immunologic and<br />
inflamma<strong>to</strong>ry markers, the result likely would reflect the<br />
increased use of omega-3 PUFAs, which is associated<br />
with a decrease in inflamma<strong>to</strong>ry media<strong>to</strong>rs and markers.<br />
Thus, the concentrations of prostaglandin E 2<br />
(Answer D)<br />
and interleukin 6 (IL-6) (Answer B) would be expected<br />
<strong>to</strong> decrease, not increase, making Answer B and Answer<br />
D incorrect. Tumor necrosis fac<strong>to</strong>r alpha concentrations<br />
(Answer C) decrease with the addition of PUFAs <strong>to</strong> the<br />
diet; thus, Answer C is correct. Although these immuneenhancing<br />
EN formulations may alter T lymphocyte<br />
function, <strong>to</strong>tal lymphocyte count would not be expected <strong>to</strong><br />
decrease (Answer A); thus Answer A is incorrect.<br />
1. Suchner U, Kuhn KS, Furst P. The scientific basis of<br />
immunonutrition. Proc Nutr Soc 2000;59:553–63.<br />
2. Pacht ER, DeMichele SJ, Nelson JL, Hart J, Wennberg AK,<br />
Gadek JE. Enteral nutrition with eicosapentaenoic acid, gammalinolenic<br />
acid, and antioxidants reduces alveolar inflamma<strong>to</strong>ry<br />
media<strong>to</strong>rs and protein influx in patients with acute respira<strong>to</strong>ry<br />
distress syndrome. Crit Care Med 2003;31:491–500.<br />
45. Answer: D<br />
The use of immune-enhancing EN formulations<br />
containing arginine, omega-3 PUFAs, and nucleotides has<br />
been shown <strong>to</strong> improve outcomes in patients after trauma.<br />
The potential benefit is greatest in patients with an injury<br />
severity score (ISS) greater than 20 or an abdominal<br />
trauma index (ATI) greater than 25. The 47-year-old<br />
woman injured in a fall with an ISS of 22 (Answer D) is<br />
the patient most likely <strong>to</strong> derive additional benefit from<br />
the use of immunonutrition. The 32-year-old man with an<br />
ISS of 12 (Answer A), the 29-year-old woman injured in an<br />
industrial accident with a ATI of 22 (Answer C), and the<br />
55-year-old woman injured in an au<strong>to</strong>mobile accident with<br />
an ATI score of 11 (Answer B) do not have markers of injury<br />
severity in the range where a benefit of immunonutrition<br />
has been shown; thus Answer A, Answer B, and Answer C<br />
are incorrect. However, use of these products would not be<br />
expected <strong>to</strong> increase complications.<br />
1. Kudsk KA, Minard G, Croce MA, Brown RO, Lowrey TS,<br />
Pritchard FE, et al. A randomized trial of isonitrogenous<br />
enteral diets after severe trauma. An immune-enhancing diet<br />
reduces septic complications. Ann Surg 1996;224:531–40;<br />
discussion 540–3.<br />
2. Consensus recommendations from the U.S. Summit on<br />
immune-enhancing enteral therapy. JPEN J Parenter Enteral<br />
Nutr 2001;25:S61–S63.<br />
46. Answer: B<br />
Improved outcomes have been demonstrated when<br />
patients with burn injuries like R.R. are given a standard<br />
EN formulation and enteral glutamine supplementation, so<br />
Answer B (begin feeding with a standard EN formulation<br />
with enteral glutamine supplementation) is the correct<br />
answer. Withholding enteral feeding for the first 48 hours<br />
after a thermal injury (Answer D) decreases the likelihood<br />
that EN will be <strong>to</strong>lerated once started; thus, Answer D is<br />
incorrect. Feeding should begin as soon as the patient is<br />
hemodynamically stable after thermal injury. Immuneenhancing<br />
EN formulations supplemented with arginine<br />
12.5, omega-3 PUFAs, and nucleotides (Answer A) or<br />
arginine (Answer C) are not associated with harm in patients<br />
with burns, but they are not recommended for routine use<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 45 Gastroenterology and Nutrition <strong>Answers</strong>
in this patient population because there is no evidence that<br />
they improve outcomes.<br />
1. Garrel D, Patenaude J, Nedelec B, Samson L, Dorais J,<br />
Champoux J, et al. Decreased mortality and infectious<br />
morbidity in adult burn patients given enteral glutamine<br />
supplements: a prospective, controlled, randomized clinical<br />
trial. Crit Care Med 2003;31:2444–9.<br />
2. Prelack K, Dylewski M, Sheridan RL. Practical guidelines for<br />
nutritional management of burn injury and recovery. Burns<br />
2007;33:14–24.<br />
47. Answer: D<br />
The medical resident would like <strong>to</strong> discuss changing<br />
R.R. <strong>to</strong> an immune-enhancing EN formulation with<br />
omega-3 PUFAs and antioxidants. The correct response <strong>to</strong><br />
this suggestion would highlight that immune-enhancing<br />
EN formulations shown <strong>to</strong> be beneficial in a specific<br />
patient population may not be associated with the same<br />
improvements in outcomes in other patient populations.<br />
The correct response is that the suggested change should<br />
not be made because an immune-enhancing EN formulation<br />
with omega-3 PUFAs 8.6 g/L and antioxidants is associated<br />
with increased survival in patients with sepsis and ARDS<br />
but has not been evaluated in patients with burns (Answer<br />
D). An immune-enhancing EN formulation with omega-3<br />
PUFAs 8.6 g/L and antioxidants has not been shown <strong>to</strong><br />
alter oxygenation in patients with burns (Answer B) or<br />
<strong>to</strong> increase survival in a nonseptic mixed medical ICU<br />
population (Answer C). Because an immune-enhancing EN<br />
formulation has not been evaluated in patients with burns,<br />
switching <strong>to</strong> an immune-enhancing product (Answer A) is<br />
incorrect.<br />
1. Garrel D, Patenaude J, Nedelec B, Samson L, Dorais J,<br />
Champoux J, et al. Decreased mortality and infectious<br />
morbidity in adult burn patients given enteral glutamine<br />
supplements: a prospective, controlled, randomized clinical<br />
trial. Crit Care Med 2003;31:2444–9.<br />
2. Prelack K, Dylewski M, Sheridan RL. Practical guidelines for<br />
nutritional management of burn injury and recovery. Burns<br />
2007;33:14–24.<br />
48. Answer: D<br />
The length of time that RR receives immunonutrition<br />
should be evidence-based. In one study that evaluated<br />
immunonutrition in patients with burns and demonstrated<br />
improved patient survival with enteral glutamine<br />
supplementation, immunonutrition was continued until<br />
complete wound healing was achieved (Answer D), making<br />
Answer D the correct answer. The other durations, until<br />
extubation (Answer C), 96 hours (Answer B), or 48 hours<br />
(Answer A), have been used as minimum therapy goals in<br />
other trials of immune-enhancing nutrients. However, in<br />
patients with burns, extending the duration of therapy until<br />
complete would healing occurs is more likely <strong>to</strong> result in<br />
additional benefit.<br />
1. Garrel D, Patenaude J, Nedelec B, Samson L, Dorais J,<br />
Champoux J, et al. Decreased mortality and infectious<br />
morbidity in adult burn patients given enteral glutamine<br />
supplements: a prospective, controlled, randomized clinical<br />
trial. Crit Care Med 2003;31:2444–9.<br />
2. Prelack K, Dylewski M, Sheridan RL. Practical guidelines for<br />
nutritional management of burn injury and recovery. Burns<br />
2007;33:14–24.<br />
49. Answer: C<br />
Clinicians should be aware that harm might result from<br />
the use of immune-enhancing EN formulations in certain<br />
patient populations. Some evidence indicates that argininecontaining<br />
immune-enhancing diets may be harmful in<br />
critically ill patients with severe sepsis. Therefore, the<br />
62-year-old man with severe sepsis and an APACHE II score<br />
of 26 (Answer C) may be harmed by an arginine-containing<br />
immune-enhancing EN formulation, making Answer C the<br />
best answer. The 32-year-old patient with a urinary tract<br />
infection after severe trauma (Answer A) is likely <strong>to</strong> benefit<br />
from an arginine-containing immune-enhancing diet, as is<br />
the 59-year-old man with gastrointestinal (GI) cancer after<br />
colonic resection (Answer B); thus Answer A and Answer<br />
B are incorrect. The 48-year-old man in the medical ICU<br />
with an APACHE II score of 12 (Answer D) is less likely<br />
<strong>to</strong> benefit from an immune-enhancing diet, but he is not<br />
in a patient population in which additional harm has been<br />
suggested.<br />
1. Ber<strong>to</strong>lini G, Iapichino G, Radrizzani D, Facchini R, Simini<br />
B, Bruzzone P, et al. Early enteral immunonutrition in<br />
patients with severe sepsis: results of an interim analysis of<br />
a randomized multicentre clinical trial. Intensive Care Med<br />
2003;29:834–40.<br />
2. Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet<br />
P, Kazandjiev G, et al. ESPEN guidelines on enteral nutrition:<br />
intensive care. Clin Nutr 2006;25:210–23.<br />
50. Answer: C<br />
Glutamine is a major energy source for enterocytes and is<br />
associated with enhanced luminal barrier function (Answer<br />
A), but this effect is not a potential advantage of parenteral<br />
glutamine compared with enteral glutamine because this<br />
effect should occur regardless of the route of administration,<br />
so Answer A is incorrect. Arginine, not glutamine, increases<br />
the production of inducible nitric oxide (NO) (Answer B);<br />
thus, neither route of glutamine administration would be<br />
expected <strong>to</strong> produce this effect, and Answer B is incorrect.<br />
Increasing the production of heat shock proteins (Answer<br />
C) is an advantage of parenteral compared with enteral<br />
glutamine administration because this effect has been<br />
more strongly associated with parenteral supplementation<br />
than enteral supplementation, making Answer C correct.<br />
Glutamine by either route would be expected <strong>to</strong> increase<br />
T-helper lymphocytes, rather than decrease them as stated<br />
in Answer D; thus, Answer D is incorrect.<br />
1. Tjader I, Berg A, Wernerman J. Exogenous glutamine—<br />
compensating a shortage? Crit Care Med 2007;35(suppl):S553–<br />
S556.<br />
2. Suchner U, Kuhn KS, Furst P. The scientific basis of<br />
immunonutrition. Proc Nutr Soc 2000;59:553–63.<br />
51. Answer: D<br />
The use of PN is often necessary because of GI<br />
in<strong>to</strong>lerance or other complications of EN or because of the<br />
presence of a contraindication <strong>to</strong> EN. The use of immuneenhancing<br />
EN is often limited by the ability of the patient <strong>to</strong><br />
<strong>to</strong>lerate an adequate volume enterally, so feeding in<strong>to</strong>lerance<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
46<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
(Answer D) occurs more often in patients receiving<br />
immunonutrition than those receiving PN, making Answer<br />
D the correct answer. Hyperglycemia (Answer A) and<br />
hypertriglyceridemia (Answer B) are both more common in<br />
patients receiving PN than in those receiving any form of<br />
EN, making Answer A and Answer B incorrect. Because of<br />
interruptions in the delivery of EN caused by GI in<strong>to</strong>lerance,<br />
the ability <strong>to</strong> deliver enough calories <strong>to</strong> overfeed a patient<br />
(Answer C) is also more likely in patients fed parenterally<br />
than enterally, making Answer C incorrect.<br />
1. Adam S, Batson S. A study of problems associated with the<br />
delivery of enteral feed in critically ill patients in five ICUs in<br />
the UK. Intensive Care Med 1997;23:261–6.<br />
2. Radrizzani D, Ber<strong>to</strong>lini G, Facchini R, Simini B, Bruzzone P,<br />
Zanforlin G, et al. Early enteral immunonutrition vs. parenteral<br />
nutrition in critically ill patients without severe sepsis: a<br />
randomized clinical trial. Intensive Care Med 2006;32:1191–8.<br />
52. Answer: B<br />
The EN formulation suggested by the physician contains<br />
arginine 2 g/L, omega-3 PUFAs 5 g/L, and antioxidants<br />
but does not supplement nucleotides; therefore, it is not the<br />
best choice for P.K.’s EN formulation, and Answer A (begin<br />
the physician’s suggested formula by nasojejunal tube) is<br />
incorrect. The best option for P.K. is an immune-enhancing<br />
EN formulation with a higher concentration of arginine and<br />
nucleotides (Answer B) because this formulation is most<br />
similar <strong>to</strong> formulations that have been shown <strong>to</strong> improve<br />
outcomes in patients with traumatic injuries; thus Answer B<br />
is correct. The use of immune-enhancing diets is appropriate<br />
in trauma patients, and those with severe injuries like P.K.<br />
(ISS 22) are more likely <strong>to</strong> benefit; thus, suggesting a<br />
standard EN formulation (Answer C) for P.K. is not the best<br />
choice, and Answer C is incorrect. No evidence exists that<br />
assesses outcomes with the use of immune-enhancing EN<br />
formulations supplemented only with omega-3 PUFAs and<br />
antioxidants in trauma patients, so Answer D (suggest an<br />
immune-enhancing EN formulation with no arginine but<br />
more omega-3 PUFAs) is also incorrect.<br />
1. Consensus recommendations from the U.S. Summit on<br />
immune-enhancing enteral therapy. JPEN J Parenter Enteral<br />
Nutr 2001;25:S61–S63.<br />
2. Kudsk KA, Minard G, Croce MA, Brown RO, Lowrey TS,<br />
Pritchard FE, et al. A randomized trial of isonitrogenous<br />
enteral diets after severe trauma. An immune-enhancing diet<br />
reduces septic complications. Ann Surg 1996;224:531–40;<br />
discussion 540–3.<br />
53. Answer: D<br />
P.K. is receiving an immune-enhancing EN formulation<br />
containing arginine 18.7 g/L, nucleotides 1.8 g/L, and<br />
omega-3 PUFAs 2.6 g/L. Clinically significant GI<br />
hemorrhage is generally viewed as a complication that can<br />
compromise GI perfusion, requiring at least temporary<br />
discontinuation of EN, including immune-enhancing diets.<br />
Therefore, Answer D (discontinue his immune-enhancing<br />
formulation) is the correct action and will decrease the<br />
likelihood of further GI-related complications. There is no<br />
evidence that indicates P.K.’s outcome will be improved by<br />
continuing his current immune-enhancing EN formulation<br />
(Answer C), providing enteral glutamine supplementation<br />
(Answer B), or switching <strong>to</strong> a standard EN formulation<br />
(Answer A); thus Answer A, Answer B, and Answer C are<br />
incorrect.<br />
1. Consensus recommendations from the U.S. Summit on<br />
immune-enhancing enteral therapy. JPEN J Parenter Enteral<br />
Nutr 2001;25:S61–S63.<br />
2. ASPEN Board of Direc<strong>to</strong>rs. Guidelines for the use of parenteral<br />
and enteral nutrition in adult and pediatric patients. JPEN J<br />
Parenter Enteral Nutr 2002;26:1SA–138SA.<br />
54. Answer: A<br />
Clinical studies of the use of immune-enhancing EN<br />
formulations containing arginine 12.5 g/L, nucleotides 1.2<br />
g/L, and omega-3 PUFAs 1.7 g/L in patients after trauma<br />
show decreased infectious complications (Answer A),<br />
making Answer A the best response <strong>to</strong> a physician asking<br />
for justification of the use of the more expensive immuneenhancing<br />
EN formulation. There is no evidence, however,<br />
indicating that this immune-enhancing EN formulation<br />
results in improved survival (Answer B) or better rates of<br />
functional recovery (Answer C), making Answer B and<br />
Answer C incorrect. Immune-enhancing EN formulations<br />
have not been associated with a decreased incidence of<br />
hyperglycemia (Answer D) compared with standard EN<br />
formulations; thus, Answer D is also incorrect.<br />
1. Kudsk KA, Minard G, Croce MA, Brown RO, Lowrey TS,<br />
Pritchard FE, et al. A randomized trial of isonitrogenous<br />
enteral diets after severe trauma. An immune-enhancing diet<br />
reduces septic complications. Ann Surg 1996;224:531–40;<br />
discussion 540–3.<br />
2. Jacobs DG, Jacobs DO, Kudsk KA, Moore FA, Oswanski MF,<br />
Poole GV, et al; EAST Practice Management Guidelines Work<br />
Group. Practice management guidelines for nutritional support<br />
of the trauma patient. J Trauma 2004;57:660–78; discussion<br />
679.<br />
55. Answer: D<br />
The use of immune-enhancing diets in surgical patients<br />
appears <strong>to</strong> have the greatest impact in preoperative patients<br />
with preexisting malnutrition. The 58-year-old man with a<br />
12% weight loss in the past 6 months (Answer D) best meets<br />
these criteria, making Answer D correct. The 56-year-old<br />
man with a BMI of 28 kg/m 2 (Answer A) does not appear <strong>to</strong><br />
be malnourished. The 36-year-old woman with a 4% weight<br />
loss in the past 6 months (Answer B) has lost weight but<br />
not enough <strong>to</strong> be considered at risk of malnutrition-related<br />
adverse outcomes. The 52-year-old woman with a normal<br />
serum albumin concentration (Answer C) does not have<br />
evidence of significant malnutrition. Therefore, the patients<br />
in Answer A, Answer B, and Answer C are less likely <strong>to</strong><br />
benefit from an immune-enhancing diet, and these answers<br />
are incorrect.<br />
1. Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O,<br />
Soeters P, et al. ESPEN guidelines on enteral nutrition: surgery<br />
including organ transplantation. Clin Nutr 2006;25:224–44.<br />
2. Gianotti L, Braga M, Nespoli L, Radaelli G, Beneduce A,<br />
Di Carlo V. A randomized controlled trial of preoperative<br />
oral supplementation with a specialized diet in patients with<br />
gastrointestinal cancer. Gastroenterology 2002;122:1763–70.<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 47 Gastroenterology and Nutrition <strong>Answers</strong>
56. Answer: B<br />
The immune-enhancing EN formulation containing<br />
arginine 12.5 g/L, nucleotides 1.2 g/L, and omega-3 PUFAs<br />
1.7 g/L (Answer B) is the best choice for preoperative<br />
nutrition for H.H. because the evidence indicates improved<br />
outcomes in surgical patients with diets supplemented with<br />
arginine, omega-3 PUFAs, and nucleotides. The immuneenhancing<br />
formulation containing just arginine 8 g/L<br />
(Answer A) does not contain enough arginine and does<br />
not supplement omega-3 PUFAs or nucleotides; thus, it is<br />
not the best choice for H.H and Answer A is incorrect. The<br />
immune-enhancing EN formulation containing omega-3<br />
PUFAs 8.6 g/L and antioxidants (Answer C) does not<br />
contain supplemental arginine or nucleotides, making it a<br />
poor choice; thus Answer C is also incorrect. The immuneenhancing<br />
EN formulation containing arginine 5.5 g/L and<br />
omega-3 PUFAs 3.29 g/L (Answer D) contains less arginine<br />
and does not supplement nucleotides, making it a poor<br />
choice for H.H; thus Answer D is also incorrect.<br />
1. Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O,<br />
Soeters P, et al. ESPEN guidelines on enteral nutrition: surgery<br />
including organ transplantation. Clin Nutr 2006;25:224–44.<br />
2. Gianotti L, Braga M, Nespoli L, Radaelli G, Beneduce A,<br />
Di Carlo V. A randomized controlled trial of preoperative<br />
oral supplementation with a specialized diet in patients with<br />
gastrointestinal cancer. Gastroenterology 2002;122:1763–70.<br />
57. Answer: A<br />
Patients like H.H. undergoing head and neck surgeries<br />
for cancer, with a low serum albumin concentration, should<br />
receive preoperative immune-enhancing EN. Clinical<br />
studies indicate improvement in clinical outcomes when<br />
immunonutrition therapy is initiated 5 days before surgery<br />
(Answer A is correct). Neither starting 1 day before surgery<br />
(Answer B) nor 1 day after surgery (Answer C) is optimal<br />
based on current guidelines; thus Answer B and Answer<br />
C are incorrect. Waiting 5 days after surgery <strong>to</strong> begin an<br />
immune-enhancing diet (Answer D) would be waiting<br />
longer than in any of the studies that have demonstrated<br />
clinical improvement with immunonutrition, and 5 days is<br />
probably <strong>to</strong>o long <strong>to</strong> wait <strong>to</strong> expect the immune-enhancing<br />
EN formulation <strong>to</strong> confer any benefit in decreasing<br />
pos<strong>to</strong>perative complications. Therefore, Answer D is also<br />
incorrect.<br />
1. Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O,<br />
Soeters P, et al. ESPEN guidelines on enteral nutrition: surgery<br />
including organ transplantation. Clin Nutr 2006;25:224–44.<br />
2. Braga M, Gianotti L, Nespoli L, Radaelli G, Di Carlo V.<br />
Nutritional approach in malnourished surgical patients: a<br />
prospective randomized study. Arch Surg 2002;137:174–80.<br />
58. Answer: C<br />
When considering the duration of immunonutrition<br />
therapy in patients like H.H. undergoing GI surgery, both<br />
the physiologic stress of the procedure and the preoperative<br />
nutritional state are important considerations. Head<br />
and neck cancer surgery is considered very stressful,<br />
and preoperatively H.H. had a mildly decreased serum<br />
albumin concentration. Evidence suggests that continuing<br />
his preoperative feeding perioperatively would be best, so<br />
discontinuing 1 day before surgery (Answer A) is not an<br />
appropriate intervention and Answe A is incorrect. It is also<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
48<br />
unlikely that the pos<strong>to</strong>perative benefit would be maximized<br />
if immunonutrition therapy was s<strong>to</strong>pped 1 day after surgery<br />
(Answer B is incorrect), but there is no evidence addressing<br />
the effect of continuing immunonutrition therapy for 14 days<br />
after surgery (Answer D is incorrect). Available evidence<br />
suggests that immunonutrition should be continued for 5 <strong>to</strong><br />
7 days after surgery (Answer C) <strong>to</strong> optimize its benefits on<br />
pos<strong>to</strong>perative complications; thus Answer C is the correct<br />
answer.<br />
1. Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O,<br />
Soeters P, et al. ESPEN guidelines on enteral nutrition: surgery<br />
including organ transplantation. Clin Nutr 2006;25:224–44.<br />
2. Braga M, Gianotti L, Nespoli L, Radaelli G, Di Carlo V.<br />
Nutritional approach in malnourished surgical patients: a<br />
prospective randomized study. Arch Surg 2002;137:174–80.<br />
59. Answer: B<br />
H.H. and his wife seek more information regarding the<br />
benefits of using an immune-enhancing EN formulation.<br />
They should be informed that the primary benefit of<br />
immunonutrition in patients like H.H. undergoing surgery is<br />
decreased pos<strong>to</strong>perative infectious complications, including<br />
pos<strong>to</strong>perative pneumonia and surgical site infections<br />
(Answer B) and length of hospital stay; thus Answer B is<br />
correct. There is no evidence that this nutrition intervention<br />
improves the probability of survival (Answer A) or<br />
oxygenation parameters allowing more rapid removal from<br />
mechanical ventilation (Answer C); thus Answer A and<br />
Answer C are incorrect. Although an immune-enhancing<br />
diet is used <strong>to</strong> meet a patient’s caloric needs, its use should<br />
not be associated with a significantly greater weight gain<br />
perioperatively (Answer D) than the use of a standard EN<br />
formulation; thus Answer D is incorrect.<br />
1. Braga M, Gianotti L, Nespoli L, Radaelli G, Di Carlo V.<br />
Nutritional approach in malnourished surgical patients: a<br />
prospective randomized study. Arch Surg 2002;137:174–80.<br />
2. Gianotti L, Braga M, Nespoli L, Radaelli G, Beneduce A,<br />
Di Carlo V. A randomized controlled trial of preoperative<br />
oral supplementation with a specialized diet in patients with<br />
gastrointestinal cancer. Gastroenterology 2002;122:1763–70.<br />
60. Answer: A<br />
The mechanism by which arginine is associated with worse<br />
outcomes in patients with sepsis and refrac<strong>to</strong>ry hypotension<br />
is most likely the increase in NO production (Answer A)<br />
associated with arginine supplementation; thus Answer A is<br />
the correct answer. Immune-enhancing nutrients improve,<br />
rather than interfere with, gut barrier function (Answer<br />
B), are generally associated with decreases rather than<br />
increases in inflamma<strong>to</strong>ry media<strong>to</strong>r production (Answer<br />
C), and are not associated with significant decreases in <strong>to</strong>tal<br />
lymphocyte counts (Answer D); thus, Answer B, Answer C,<br />
and Answer D are incorrect.<br />
1. Suchner U, Kuhn KS, Furst P. The scientific basis of<br />
immunonutrition. Proc Nutr Soc 2000;59:553–63.<br />
2. Zhou M, Martindale RG. Arginine in the critical care setting. J<br />
Nutr 2007;137:1687S–1692S.<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
Dietary Supplements<br />
61. Answer: B<br />
Information regarding the safety and efficacy of dietary<br />
supplements must be communicated <strong>to</strong> the consumer by<br />
pharmacists. Although the Federal Trade Commission<br />
(FTC) rather than the FDA regulates advertising of dietary<br />
supplements (Answer A), this fact is not helpful <strong>to</strong> the<br />
consumer making decisions regarding whether use of such a<br />
supplement is safe and efficacious, and Answer A is incorrect.<br />
Although structure and function claims on the labels of<br />
dietary supplements must be followed by a disclaimer that<br />
the claim has not been evaluated by the FDA (Answer C),<br />
this information mainly addresses efficacy (or lack thereof)<br />
of dietary supplements rather than safety, and Answer C is<br />
incorrect. Although it is now mandated that manufacturers<br />
follow Good Manufacturing Practices (GMPs) as indicated<br />
in Answer D, these address only whether the product<br />
ingredients are consistent with the labeling and ensure that<br />
the product is free of contaminants; GMPs do not address<br />
the efficacy of dietary supplements, making Answer D<br />
incorrect. Informing the consumer that dietary supplements<br />
are regulated more like foods than conventional drugs and<br />
that they do not require premarketing approval by the FDA<br />
(Answer B) should alert them that safety and efficacy could<br />
both be issues with use of the product, making Answer B<br />
correct.<br />
1. Dietary Supplement Current Good Manufacturing Practices<br />
(CGMPs) and Interim Final Rule (IFR) Facts. U.S. Food and<br />
Drug Administration Center for Food Safety and Applied<br />
Nutrition. June 22, 2007. Available at www.cfsan.fda.gov/~dms/<br />
dscgmps6.html. Accessed April 10, 2009.<br />
2. Overview of Dietary Supplements. U.S. Food and Drug<br />
Administration Center for Food Safety and Applied Nutrition.<br />
January 3, 2001. Available at www.cfsan.fda.gov/~dms/dsoview.html#regulate.<br />
Accessed April 10, 2009.<br />
62. Answer: A<br />
The Dietary Supplement Health and Education Act<br />
(DSHEA) of 1994 defined dietary supplements <strong>to</strong> include<br />
vitamins, minerals, herbs or other botanicals, amino acids,<br />
and other dietary substances that supplement the diet by<br />
increasing <strong>to</strong>tal dietary intake. In this case, the patient’s<br />
supplements all fall in<strong>to</strong> one of these categories (folic acid<br />
and ascorbic acid [vitamin C] are vitamins, glucosamine<br />
falls under “other dietary substances,” and ginkgo and green<br />
tea extracts are herbs), making Answer A correct. Answer B<br />
does not include green tea and therefore implies that green<br />
tea extract is not regulated by DSHEA, something that would<br />
be correct if the patient were consuming commercially<br />
available green tea rather than the extract; thus, Answer B is<br />
incorrect. Answer C does not include glucosamine, implying<br />
that it is not regulated by DSHEA; this is incorrect, and<br />
Answer C is not the best answer. Even though glucosamine<br />
is not derived from an herbal source, it is a natural product<br />
that falls in the “other dietary substances” category. Folic<br />
acid in dosages greater than 0.8 mg/day was regulated as<br />
a prescription drug before DSHEA. However, since 1994,<br />
folic acid dosages greater than 0.8 mg/day are considered<br />
dietary supplements and may be sold without a prescription.<br />
Therefore, Answer D, which indicates that folic acid 1 mg is<br />
not regulated by the DSHEA, is incorrect.<br />
1. Overview of dietary supplements. U.S. Food and Drug<br />
Administration Center for Food Safety and Applied Nutrition.<br />
January 3, 2001. Available at www.cfsan.fda.gov/~dms/dsoview.html#regulate.<br />
Accessed April 10, 2009.<br />
2. FDA/CDER Drug Info. Personal communication. May 9, 2008.<br />
Mailed <strong>to</strong>/from: DRUGINFO@fda.hhs.gov. Accessed Oc<strong>to</strong>ber<br />
31, 2008.<br />
63. Answer: C<br />
Ephedra was finally removed from the market as a<br />
weight loss drug by the FDA because it was shown <strong>to</strong><br />
cause a significant risk of injury (Answer C); thus, Answer<br />
C is correct. Although the FTC can levy fines for false<br />
advertising, it cannot require that a product be removed from<br />
the market (Answer A); thus Answer A is incorrect. Under<br />
DSHEA, dietary supplements do not have <strong>to</strong> be shown <strong>to</strong><br />
be effective either before or after marketing, thus Answer<br />
B (the FDA removed ephedra from the market because of<br />
ineffectiveness) is incorrect. Ephedra can no longer be sold<br />
as a dietary supplement in the United States; thus Answer D<br />
(ephedra may still be sold as a dietary supplement but not as<br />
a nonprescription drug) is incorrect.<br />
1. Overview of dietary supplements. U.S. Food and Drug<br />
Administration Center for Food Safety and Applied Nutrition.<br />
January 3, 2001. Available at www.cfsan.fda.gov/~dms/dsoview.html#regulate.<br />
Accessed April 10, 2008.<br />
2. Federal Trade Commission. Dietary claims: an advertising<br />
guide for industry. Available at www.ftc.gov/bcp/conline/pubs/<br />
buspubs/dietsupp.shtm. Accessed April 10, 2009.<br />
64. Answer: D<br />
The GMPs apply <strong>to</strong> both domestic and foreign<br />
manufactured dietary supplements. These long-awaited rules<br />
help ensure the identity, purity, strength, and composition of<br />
dietary supplements and thus will help prevent adulterated<br />
products from reaching the market, making Answer D<br />
correct. Although the GMPs should help promote the safety<br />
of these products, the rules do not require safety testing in<br />
animals or humans (Answer A is incorrect). Similarly, the<br />
GMPs do not address efficacy, so Answer B is incorrect.<br />
No tariffs are levied on foreign products related <strong>to</strong> the GMP<br />
(Answer C is incorrect); however, implementation of these<br />
new rules will be costly, especially for small companies, and<br />
this may drive up prices of some supplements.<br />
1. U.S. Food and Drug Administration. Dietary supplement<br />
current good manufacturing practices (CGMPs) and interim<br />
final rule (IFR) facts (fact sheet). June 22, 2007. Available at<br />
www.cfsan.fda.gov/~dms/dscgmps6.html. Accessed April 10,<br />
2009.<br />
2. Current good manufacturing practice in manufacturing,<br />
packaging, labeling, or holding operations for dietary<br />
supplements, final rule (21 CFR part 111). Federal Register.<br />
June 25, 2007;72:34751. Available at www.cfsan.fda.gov/~lrd/<br />
fr07625a.html. Accessed April 10, 2009.<br />
65. Answer: B<br />
J.H., a 35-year-old obese woman with mild osteoarthritis,<br />
would like advice on using green tea for weight loss.<br />
Some clinical studies of green tea have demonstrated<br />
benefit in promoting weight loss and weight maintenance,<br />
whereas others have not. Because of the benign nature of<br />
the therapy, especially in patients without hypertension<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 49 Gastroenterology and Nutrition <strong>Answers</strong>
or cardiovascular disease, drinking green tea or taking a<br />
reliable, standardized green tea extract may be worth a try.<br />
Therefore, Answer B (taking an extract may be worth a try)<br />
is correct. Answer A (risks of adverse events with green tea<br />
outweigh the benefits) is incorrect because it indicates there<br />
are substantial adverse events with this approach, which is<br />
not the case. It appears that both the catechin and caffeine<br />
components of green tea may be important for any weight<br />
loss or maintenance benefit. Green tea generally contains an<br />
amount of caffeine considered sufficient for the beneficial<br />
effect on weight, making Answer C (she will need <strong>to</strong> both<br />
drink green tea and take an extract) incorrect. Although<br />
patients with hypertension or cardiovascular disease may be<br />
at increased risk of adverse events with green tea because<br />
of its sympathetic activity, there is no reason <strong>to</strong> believe that<br />
green tea extract would exacerbate osteoarthritis, making<br />
Answer D incorrect.<br />
1. Westerterp-Plantenga MS, Lejeune MP, Kovacs EM. Body<br />
weight loss and weight maintenance in relation <strong>to</strong> habitual<br />
caffeine intake and green tea supplementation. Obes Res<br />
2005;17:1195–204.<br />
2. Diepvens K, Westerterp KR, Westerterp-Plantenga MS.<br />
Obesity and thermogenesis related <strong>to</strong> the consumption of<br />
caffeine, ephedrine, capsaicin, and green tea. Am J Physiol<br />
Regul Integr Comp Physiol 2007;292:R77–85.<br />
3. Seeram NP, Henning SM, Niu Y, Lee R, Scheuller HS, Heber D.<br />
Catechin and caffeine content of green tea dietary supplements<br />
and correlation with antioxidant capacity. J Agric Food Chem<br />
2006;54:1599–603.<br />
66. Answer: D<br />
According <strong>to</strong> DSHEA, a dietary supplement<br />
manufacturer may make a structure or function claim on<br />
the label as long as “This statement has not been evaluated<br />
by the FDA. This product is not intended <strong>to</strong> diagnose, treat,<br />
cure, or prevent any disease” also appears on the label. The<br />
claim that cranberry helps promote urinary tract health is<br />
clearly a function claim and is thus allowed as long as the<br />
disclaimer is present (Answer D is correct). Sometimes the<br />
distinction between structure or function claims and disease<br />
prevention or treatment claims is very difficult <strong>to</strong> determine.<br />
However, in this case, the claim would not be construed as<br />
a disease prevention claim (e.g., “helps prevent urinary tract<br />
infections”); therefore, Answer A (prevents bacteria from<br />
invading and proliferating in the urinary tract) is incorrect.<br />
If a claim is deemed <strong>to</strong> be a disease prevention or treatment<br />
claim, the product would be considered a drug and thus<br />
misbranded as a dietary supplement. Again, because this<br />
is a function claim, the cranberry would not in this case<br />
be considered a drug, making Answer B (decreases the<br />
duration of urinary tract infections) incorrect. According<br />
<strong>to</strong> the FDA, such a claim can only be made for drugs, not<br />
dietary supplements. Structure or function claims can be<br />
made based on a single ingredient within a multi-ingredient<br />
product; therefore, Answer C (decreases the severity of<br />
urinary tract infection symp<strong>to</strong>ms) is incorrect. This claim<br />
can be made if the product contains only cranberry or other<br />
substances promoting urinary health; if it contains other<br />
ingredients, it would be considered misbranded.<br />
1. Overview of dietary supplements. U.S. Food and Drug<br />
Administration Center for Food Safety and Applied Nutrition.<br />
January 3, 2001. Available at www.cfsan.fda.gov/~dms/dsoview.html#regulate.<br />
Accessed April 10, 2009.<br />
2. U.S. Food and Drug Administration. Structure/function<br />
claims. Available at www.cfsan.fda.gov/~dms/labstruc.html.<br />
Accessed April 10, 2009.<br />
67. Answer: C<br />
U.W., a 45-year-old woman who takes Saint John’s<br />
wort for depression, has been admitted <strong>to</strong> the hospital for<br />
complications related <strong>to</strong> her diabetes. In its Statement on<br />
the Use of Dietary Supplements, the American Society<br />
of Health-System Pharmacists (ASHP) discourages selfadministration<br />
of the patient’s own supply of dietary<br />
supplements during hospitalization because of lack of<br />
information regarding safety and efficacy, as well as<br />
inadequate standards for product quality. Therefore, Answer<br />
A (she may be allowed <strong>to</strong> self-administer her own supply if<br />
ordered by her physician) and Answer B (she may be allowed<br />
<strong>to</strong> self-administer her own supply after the pharmacist has<br />
verified the identity and checked for drug interactions),<br />
both of which concern self-administration of the patient’s<br />
own supply of drug, are not consistent with the ASHP<br />
recommendations and are incorrect. It is recommended that<br />
hospitals have a general policy in place regarding inpatient<br />
use of dietary supplements, but Answer D is not the best<br />
response because Saint John’s wort is not actually on the<br />
formulary but rather must be obtained for use in this patient.<br />
Answer C best follows recommendations; the pharmacy<br />
could supply the dietary supplement if Saint John’s wort<br />
is on the formulary, the physician specifically prescribes<br />
it, and the pharmacist checks the patient profile for drug<br />
interactions; thus Answer C is correct.<br />
1. American Society of Health-System Pharmacists Council on<br />
Professional Affairs. ASHP statement on the use of dietary<br />
supplements. Am J Health Syst Pharm 2004;61:1707–11.<br />
2. Bizzie KL, Witmer DR, Pin<strong>to</strong> B, Bush C, Clark J, Deffenbaugh<br />
J Jr. National survey of dietary supplement policies in acute<br />
care facilities. Am J Health Syst Pharm 2006;63:65–70.<br />
3. Cohen MH, Hrbek A, Davis RB, Schachter SC, Kemper KJ,<br />
Boyer EW, et al. Emerging credentialing practices, malpractice<br />
liability policies, and guidelines governing complementary<br />
and alternative medical practices and dietary supplement<br />
recommendations: a descriptive study of 19 integrative<br />
health care centers in the United States. Arch Intern Med<br />
2005;165:289–95.<br />
68. Answer: B<br />
The question relates <strong>to</strong> the design of a demographic<br />
survey of dietary supplement use and what aspects of the<br />
design could lead <strong>to</strong> overstating the prevalence of use.<br />
Recent surveys of the use of dietary supplements in the<br />
United States have reported a broad array of percentages of<br />
the population using these supplements, largely because of<br />
the population studied, the definition of dietary supplement,<br />
and the definition of recent use. Dietary supplements are<br />
used more commonly among women than men. Older<br />
people use them more commonly than younger people,<br />
making Answer C (excluding people older than 65 from the<br />
survey) incorrect. Answer D (oversampling of minorities<br />
with lower socioeconomic status) is also incorrect because<br />
dietary supplement use in the United States is more common<br />
in those of higher socioeconomic status and education<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
50<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
level. Exclusion of conventional vitamins and minerals<br />
from the definition of dietary supplements (Answer A)<br />
would make supplement use appear <strong>to</strong> be less common<br />
than more common, making Answer A incorrect. Because<br />
more people will have used dietary supplements within the<br />
past month than within the past week, querying about use<br />
of supplements within the past month rather than the past<br />
week (Answer B) would appear <strong>to</strong> make supplement use<br />
more common; therefore, Answer B is correct.<br />
1. Kelly JP, Kaufman DW, Kelley K, Rosenberg L, Anderson TE,<br />
Mitchell AA. Recent trends in use of herbal and other natural<br />
products. Arch Intern Med 2005;165:281–6.<br />
2. Kennedy J. Herb and supplement use in the U.S. adult<br />
population. Clin Ther 2005;27:1847–58.<br />
69. Answer: A<br />
D.L. has heard that black cohosh may alleviate some of<br />
her menopause-related symp<strong>to</strong>ms but is concerned about<br />
the risk of developing breast cancer. Although the evidence<br />
demonstrating efficacy of black cohosh in relieving vasomo<strong>to</strong>r<br />
symp<strong>to</strong>ms associated with menopause is inconsistent, it<br />
appears <strong>to</strong> be safe and may be of benefit for some women<br />
experiencing mild symp<strong>to</strong>ms. The dosages most commonly<br />
used in clinical trials were black cohosh extract standardized<br />
<strong>to</strong> the 1-mg equivalent of 27-deoxyacetein twice daily<br />
(Remifemin 20–40 mg or equivalent product twice daily).<br />
Most studies were of short duration, typically lasting a<br />
maximum of 6 months. Based on this evidence, Answer A<br />
(a cautious trial using 20–40 mg of Remifemin or equivalent<br />
twice daily for up <strong>to</strong> 6 months is unlikely <strong>to</strong> do harm) is<br />
the best response and the correct answer. A few cases have<br />
been published reporting hepa<strong>to</strong><strong>to</strong>xicity associated with the<br />
consumption of black cohosh; however, more than 2000<br />
subjects have been enrolled in clinical trials with black<br />
cohosh extract, and no reports of hepa<strong>to</strong><strong>to</strong>xicity have been<br />
published. In addition, there is currently no known plausible<br />
biologic mechanism for hepa<strong>to</strong><strong>to</strong>xic activity of black<br />
cohosh. The recommendation of the National Center for<br />
Complementary and Alternative Medicine and the National<br />
Institutes of Health Office of Dietary Supplements is on the<br />
side of caution, recommending moni<strong>to</strong>ring liver function in<br />
patients consuming black cohosh. Based on this information,<br />
Answer B (the risk of hepa<strong>to</strong><strong>to</strong>xicity with black cohosh is<br />
well established and its use should be avoided) is incorrect.<br />
Current evidence does not support the mechanistic view of<br />
black cohosh possessing estrogenic effects. Instead, research<br />
suggests that black cohosh inhibits binding of sero<strong>to</strong>nin<br />
5-hydroxytryptamine- 1A<br />
and 5-hydroxytryptamine 7<br />
, both<br />
of which are associated with the hypothalamus. Current<br />
information is inconclusive regarding black cohosh and the<br />
risk of breast cancer. It appears <strong>to</strong> be safe in women with no<br />
increased risk of breast cancer; however, current evidence is<br />
insufficient <strong>to</strong> recommend its use in women with increased<br />
risk. Therefore, Answer C (recent trials have demonstrated<br />
an estrogenic effect of black cohosh on breast tissue) is<br />
incorrect. Insufficient evidence exists <strong>to</strong> support an effect of<br />
black cohosh on cardiovascular health; therefore, Answer D<br />
(black cohosh can be recommended for primary prevention<br />
of cardiovascular disease) is also incorrect.<br />
1. National Center for Complementary and Alternative Medicine,<br />
National Institutes of Health Office of Dietary Supplements.<br />
Workshop on the safety of black cohosh in clinical studies.<br />
National Institutes of Health, Bethesda, MD. November<br />
11, 2004. Available at nccam.nih.gov/news/pastmeetings/<br />
blackcohosh_mtngsumm.htm. Accessed Oc<strong>to</strong>ber 31, 2008.<br />
2. Huntley A, Ernst E. A systematic review of the safety of black<br />
cohosh. Menopause 2003;10:58–64.<br />
3. Osmers R, Friede M, Liske E, Schnitker J, Freudenstein<br />
J, Henneicke-von Zepelin HH. Efficacy and safety of<br />
isopropanolic black cohosh extract for climacteric symp<strong>to</strong>ms.<br />
Obstet Gynecol 2005;105:1074–83.<br />
70. Answer: A<br />
D.L. decides <strong>to</strong> try black cohosh. She wants your<br />
recommendation for the most efficacious product.<br />
Remifemin black cohosh extract is the most widely studied<br />
product showing possible efficacy among products available<br />
in the United States (Answer A); therefore, Answer A is<br />
correct. Answer C (studies reporting efficacy and safety of<br />
Remifemin black cohosh extract support use of the extract<br />
for periods extending up <strong>to</strong> 1 year) is incorrect because most<br />
studies have only lasted 6 months or less. The manufacturer<br />
of Remifemin has switched between isopropanolic and<br />
ethanolic preparations and between fluid extracts and dried<br />
fluid extracts, and the package labeling has changed at least<br />
twice. These changes make it difficult <strong>to</strong> compare the results<br />
of the various trials using Remifemin; therefore, Answer B<br />
(Remifemin black cohosh extracts used in clinical studies<br />
has been consistently manufactured) is incorrect. No<br />
black cohosh product has been consistently demonstrated<br />
<strong>to</strong> increase bone density; therefore, Answer D (because<br />
Remifemin has been demonstrated <strong>to</strong> increase bone density,<br />
it should be the black cohosh product of choice) is incorrect.<br />
1. New<strong>to</strong>n KM, Reed SD, LaCroix AZ, Grothaus LC, Ehrlich K,<br />
Guiltinan J. Treatment of vasomo<strong>to</strong>r symp<strong>to</strong>ms of menopause<br />
with black cohosh, multibotanicals, soy, hormone therapy, or<br />
placebo: a randomized trial. Ann Intern Med 2006;145:869–79.<br />
2. Jellin JM, Gregory PJ, Batz F, eds. Pharmacist’s Letter/<br />
Prescriber’s Letter Natural Medicines Comprehensive<br />
Database, 9th ed. S<strong>to</strong>ck<strong>to</strong>n, CA: Therapeutic Research Faculty,<br />
2007.<br />
3. DerMarderrosian A, ed. The Review of Natural Products. St.<br />
Louis, MO: Elsevier Inc., 2005.<br />
71. Answer: C<br />
L.B., a 62-year-old man with hypertension, hyperlipidemia,<br />
and coronary artery disease, wants <strong>to</strong> take ginkgo <strong>to</strong> prevent<br />
Alzheimer’s disease. Although some studies have shown<br />
ginkgo extract <strong>to</strong> be efficacious in slowing progression and<br />
ameliorating symp<strong>to</strong>ms of Alzheimer’s dementia, the overall<br />
combined evidence of benefit in patients with cognitive<br />
impairment or dementia fails <strong>to</strong> demonstrate consistent<br />
efficacy for these disorders. Therefore, Answer B (ginkgo<br />
extract appears <strong>to</strong> be efficacious, but adverse effects and<br />
drug interactions preclude its use) and Answer D (terpene<br />
ginkgolide B is a potent inducer of cy<strong>to</strong>chrome [CYP] P450<br />
3A4 and has the potential <strong>to</strong> interact with drugs metabolized<br />
by this isozyme) are both incorrect. Ginkgo is relatively<br />
safe, and adverse effects are usually mild. Ginkgolide B<br />
is a potent inhibi<strong>to</strong>r of platelet-activating fac<strong>to</strong>r, and there<br />
is an increased risk of bleeding if the extract is taken<br />
concomitantly with antiplatelet agents, such as aspirin.<br />
Therefore, Answer C (ginkgo is generally well <strong>to</strong>lerated, but<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 51 Gastroenterology and Nutrition <strong>Answers</strong>
there is insufficient evidence <strong>to</strong> support efficacy and drug<br />
interactions are a concern for L.B.) is the correct response,<br />
and Answer A (ginkgo is free of drug interactions with<br />
L.B.’s drugs) is incorrect.<br />
1. Carlson JJ, Farquhar JW, DiNucci E, Ausserer L, Zehnder<br />
J, Miller M, et al. Safety and efficacy of a Ginkgo biloba–<br />
containing dietary supplement on cognitive function, quality<br />
of life, and platelet function in healthy, cognitively intact older<br />
adults. J Am Diet Assoc 2007;107:422–32.<br />
2. Schneider LS, DeKosky ST, Farlow MR, Tariot PN, Hoerr R,<br />
Kieser M. A randomized, double-blind, placebo-controlled<br />
trial of two doses of Ginkgo biloba extract in dementia of the<br />
Alzheimer’s type. Curr Alzheimer Res 2005;2:541–51.<br />
72. Answer: C<br />
Most published studies examining the effects of ginkgo in<br />
tinnitus lack sufficient methodology <strong>to</strong> interpret their results<br />
accurately and there is insufficient evidence that ginkgo is<br />
effective for tinnitus. Therefore, Answer A (several strong<br />
studies indicate effectiveness, but adverse effects preclude<br />
it use) and Answer D (it is well <strong>to</strong>lerated, and evidence<br />
suggests it is effective) are both incorrect. Although the first<br />
half of Answer B pertaining <strong>to</strong> efficacy is correct, ginkgo is<br />
generally well <strong>to</strong>lerated; therefore, Answer B (evidence fails<br />
<strong>to</strong> support efficacy, and adverse effects preclude its use) is<br />
incorrect. By the time a patient presents with distressing<br />
tinnitus, there is a significant psychological component<br />
present as well, which creates a strong placebo effect. This<br />
placebo effect makes it difficult <strong>to</strong> interpret results from<br />
clinical trials; therefore, Answer C (because of the strong<br />
placebo effect noted in tinnitus management, trials using<br />
ginkgo for tinnitus are difficult <strong>to</strong> interpret) is correct.<br />
1. DerMarderrosian A, ed. The Review of Natural Products. St.<br />
Louis, MO: Elsevier Inc., 2007.<br />
2. Hil<strong>to</strong>n M, Stuart E. Ginkgo biloba for tinnitus. Cochrane<br />
Database Syst Rev 2004;2:CD003852.<br />
73. Answer: A<br />
B.L. is a 66-year-old moderately obese woman with<br />
chronic, bilateral knee pain caused by moderately severe<br />
osteoarthritis. She takes acetaminophen for the pain but<br />
is interested in learning more about glucosamine. The<br />
overall response rate in the Glucosamine/chondroitin<br />
Arthritis Intervention Trial (GAIT) in participants receiving<br />
glucosamine, chondroitin, and the combined treatment<br />
was similar <strong>to</strong> that achieved with placebo. However, in a<br />
subgroup analysis of patients with moderate <strong>to</strong> severe pain<br />
at baseline, a significantly higher response rate was reported<br />
with combined therapy than with placebo. Based on this<br />
information, Answer A (patients with moderate <strong>to</strong> severe<br />
knee pain are more likely <strong>to</strong> benefit from glucosamine<br />
combined with chondroitin than patients with milder pain)<br />
is correct. The GAIT study used glucosamine hydrochloride<br />
and chondroitin sulfate, and the study was conducted under<br />
an Investigational New Drug Application filed with the FDA;<br />
therefore, the products used in this study were subject <strong>to</strong> more<br />
stringent regulations compared with other over-the-counter<br />
products. The Glucosamine Unum In Die Efficacy (GUIDE)<br />
trial used a prescription glucosamine sulfate product<br />
manufactured by the European pharmaceutical company,<br />
Rottapharm, and this product is not currently available in<br />
the United States. Because of a lack of standardization of<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
52<br />
glucosamine products in the United States, <strong>to</strong>gether with<br />
highly variable amounts of glucosamine contained in these<br />
products, extrapolation of the results from either GAIT or<br />
GUIDE cannot be recommended. Therefore, Answer B<br />
(products used in GAIT and GUIDE are similar <strong>to</strong> those<br />
available in the United States) is incorrect. The Western<br />
Ontario and McMaster University (WOMAC) and Lequesne<br />
indices were used <strong>to</strong> measure the primary outcomes in this<br />
study. The importance of addressing the implications of<br />
using differing measures of primary outcomes in clinical<br />
trials when evaluating response rates is unders<strong>to</strong>od. The<br />
WOMAC index appears <strong>to</strong> be more sensitive than the<br />
Lequesne index. Therefore, Answer C (they demonstrate<br />
comparable validity, reliability, and responsiveness <strong>to</strong><br />
glucosamine) is incorrect. Although most of the published<br />
trials examining the use of glucosamine in patients with<br />
osteoarthritis indicate it is generally well <strong>to</strong>lerated with a<br />
safety profile significantly superior <strong>to</strong> nonsteroidal antiinflamma<strong>to</strong>ry<br />
drugs (NSAIDs), most of these trials have<br />
been short, lasting 6 months or less. Long-term safety<br />
information beyond 6 months cannot be ascertained at this<br />
time, making Answer D (the long-term safety profile is<br />
superior <strong>to</strong> NSAIDs) incorrect.<br />
1. Gentell-Bonnassies S, Le Claire P, Mezieres M, Ayral X,<br />
Dougados M. Comparison of the responsiveness of symp<strong>to</strong>matic<br />
outcome measures in knee osteoarthritis. Arthritis Care Res<br />
2000;13:280–5.<br />
2. Clegg DO, Reda DJ, Harris CL, Klein MA, O’Dell JR, Hooper<br />
MM, et al. Glucosamine, chondroitin sulfate, and the two in<br />
combination for painful knee osteoarthritis. N Engl J Med<br />
2006;354:795–808.<br />
3. Herrero-Beaumont G, Ivorra JA, Del Carmen Trabado M,<br />
Blanco FJ, Beni<strong>to</strong> P, Martin-Mola E, et al. Glucosamine sulfate<br />
in the treatment of knee osteoarthritis symp<strong>to</strong>ms: a randomized,<br />
double-blind, placebo-controlled study using acetaminophen<br />
as a side compara<strong>to</strong>r. Arthritis Rheum 2007;56:555–67.<br />
74. Answer: B<br />
The Glucosamine/chondroitin Arthritis Intervention<br />
Trial used a robust study design (a randomized, doubleblind,<br />
placebo- and celecoxib-controlled multicenter<br />
design); however, the study design cannot correct for a<br />
higher-than-expected placebo response and lower-thanexpected<br />
celecoxib response. In addition, inclusion of<br />
patients with mild symp<strong>to</strong>ms may have resulted in less<br />
sensitivity <strong>to</strong> the outcome measures. Therefore, Answer<br />
A (they are of minimal concern in this trial because of<br />
the robustness of the study design) is incorrect. The high<br />
placebo response rate, <strong>to</strong>gether with the lower-than-expected<br />
celecoxib response rate, may limit the ability <strong>to</strong> detect true<br />
treatment benefits, thus increasing the risk of mistakenly<br />
failing <strong>to</strong> reject the null hypothesis when the alternative<br />
hypothesis is true (a type II error); therefore, Answer B<br />
(may mask true response rates <strong>to</strong> glucosamine, increasing<br />
the risk of a type II error) is correct. Type I errors (Answer<br />
C) occur when a true null hypothesis is rejected; therefore,<br />
Answer C is incorrect. Although the authors did perform<br />
a power analysis, readers should realize that statistical<br />
power depends on the statistically significant criterion (a<br />
= 0.017 for comparisons of glucosamine, chondroitin, and<br />
combined-treatment group with placebo, with an overall a<br />
= 0.05), the effect size, and the sensitivity of the data. The<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition
claimed effect size in GAIT was an absolute increase of<br />
15% in the response rate compared with placebo, assuming<br />
a 35% response rate in the placebo group. The much larger<br />
placebo response reported in GAIT would make it more<br />
difficult <strong>to</strong> detect the effect size. Therefore, Answer D (there<br />
is minimal concern in this trial because of the successful<br />
use of a power analysis) is incorrect.<br />
1. Towheed TE, Maxwell L, Anastassiades TP, Shea B, Houpt<br />
J. Robinson V, et al. Glucosamine therapy for treating<br />
osteoarthritis. Cochrane Database Syst Rev 2005;2:CD002946.<br />
2. Guller U, DeLong E. Interpreting statistics in medical literature:<br />
a vade mecum for surgeons. J Am Coll Surg 2004;198:441–58.<br />
75. Answer: C<br />
T.G. is a 49-year-old man with hypercholesterolemia<br />
being treated with a<strong>to</strong>rvastatin. He is interested in obtaining<br />
information regarding the use of policosanol. Although early<br />
studies of Cuban sugar cane policosanol showed promising<br />
results in lipid-lowering effects, recent studies have not<br />
substantiated these results. In a double-blind, placebocontrolled<br />
trial, adding policosanol <strong>to</strong> a<strong>to</strong>rvastatin (Answer<br />
A) showed no better lipid-lowering effect than a<strong>to</strong>rvastatin<br />
alone. Other recent studies of policosanol have demonstrated<br />
that results with its use are no better than placebo in reducing<br />
low-density lipoprotein cholesterol (LDL-C). Therefore,<br />
Answer B (replacement of a<strong>to</strong>rvastatin with policosanol<br />
would result in similar lowering of LDL-C) is incorrect.<br />
The advice that policosanol should not be expected <strong>to</strong> lower<br />
LDL-C is based on its lack of efficacy (Answer C), making<br />
Answer C the correct response. Policosanol is relatively<br />
free of adverse events such as elevated liver function<br />
tests or elevated creatine phosphokinase, making Answer<br />
D (it has the potential <strong>to</strong> elevate creatine phosphokinase<br />
concentrations) incorrect.<br />
1. Cubeddu LX, Cubeddu RJ, Heimowitz T, Restrepo B,<br />
Lamas GA, Weinberg GB. Comparative lipid-lowering<br />
effects of policosanol and a<strong>to</strong>rvastatin: a randomized,<br />
parallel, double-blind, placebo-controlled trial. Am Heart J<br />
2006;152:982.e1–5.<br />
2. Berthold HK, Unverdorben S, Degenhardt R, Bulitta<br />
M, Gouni-Berhold I. Effect of policosanol on lipid values<br />
among patients with hypercholesterolemia or combined<br />
hyperlipidemia: a randomized controlled trial. JAMA<br />
2006;295:2262–9.<br />
76. Answer: D<br />
C.D. is a 32-year-old moderately obese woman who is<br />
seeking advice on the use of Saint John’s wort for postpartum<br />
depression. Although recent literature does not indicate<br />
a significant interaction between hypericum and oral<br />
contraceptives, the potential for such an interaction cannot<br />
be excluded; therefore, Answer A (current evidence fails<br />
<strong>to</strong> substantiate significant drug interactions between Saint<br />
John’s wort and oral contraceptives) is incorrect. Lovastatin<br />
undergoes similar metabolism compared with simvastatin,<br />
with CYP P450 3A4 playing a major part in its metabolism,<br />
as well as being a potential substrate for P-glycoprotein.<br />
Therefore, a significant interaction with hypericum is likely,<br />
which may result in significantly reduced bioavailability of<br />
lovastatin. Therefore, Answer B (significant interactions<br />
with Saint John’s wort and lovastatin are unlikely) is<br />
incorrect. Because C.D. is described <strong>to</strong> be suffering from<br />
major depression (i.e., postpartum depression), Answer C<br />
(recent evidence suggests benefit of hypericum extracts in<br />
patients with mild <strong>to</strong> moderate depression and is therefore a<br />
viable option for C.D.) is incorrect. Although older studies<br />
have suggested a benefit of hypericum compared with<br />
placebo for the treatment of major depression, more recent,<br />
methodologically robust studies fail <strong>to</strong> support these results.<br />
Although the consensus continues <strong>to</strong> indicate its efficacy in<br />
the treatment of symp<strong>to</strong>ms associated with mild <strong>to</strong> moderate<br />
depression, more studies are needed <strong>to</strong> further ascertain<br />
its role in the treatment of major depression. Therefore,<br />
Answer D (recent data suggest Saint John’s wort is no<br />
more efficacious than placebo for the treatment of major<br />
depression such as C.D. is experiencing) is correct because<br />
C.D. appears <strong>to</strong> meet criteria for major depression.<br />
1. Madabushi R, Frank B, Drewelow B, Derendorf H, Butterweck<br />
V. Hyperforin in St. John’s wort drug interactions. Eur J Clin<br />
Pharmacol 2006;62:225–33.<br />
2. Whitten DL, Myers P, Hawrelak A, Wolhmuth H. The effect<br />
of St. John’s wort extracts on CYP3A: a systematic review of<br />
prospective clinical trials. Br J Clin Pharmacol 2006;62:512–<br />
26.<br />
3. Hypericum Depression Trial Study Group. Effect of Hypericum<br />
perforatum (St. John’s wort) in major depressive disorder: a<br />
randomized controlled trial. JAMA 2002;287:1807–14.<br />
4. Fava M, Alpert J, Nierenberg AA, Mischoulon D, Ot<strong>to</strong> MW,<br />
Zajecka J, et al. A double-blind, randomized trial of St. John’s<br />
wort, fluoxetine, and placebo in major depressive disorder. J<br />
Clin Psychopharmacol 2005;25:441–7.<br />
77. Answer: D<br />
Equol is an isoflavone formed by bacterial intestinal<br />
metabolism of the soy isoflavone daidzein. Equol has<br />
greater affinity for the estrogen recep<strong>to</strong>r than daidzein, and<br />
activity at the estrogen recep<strong>to</strong>r is believed <strong>to</strong> be important<br />
for the activity of soy in cardioprevention and for relief of<br />
menopausal symp<strong>to</strong>ms. Only about one-third of non-Asian<br />
people can form equol from daidzein, so it is plausible<br />
that these populations may derive less benefit from soy<br />
isoflavones compared with Asian populations in which a<br />
higher percentage of the constituency are equol formers.<br />
Thus, Answer A (most Americans are equol formers) is<br />
incorrect. Although soy food supplementation has resulted<br />
in blood pressure lowering in hypertensive patients in some<br />
studies, this result has not been consistent across studies.<br />
Thus Answer B (blood pressure reduction is expected with<br />
soy isoflavones) is incorrect. The lipid-lowering effects of<br />
soy have been found <strong>to</strong> be more modest in recent studies<br />
compared with older studies. These recent effects of a 3%<br />
<strong>to</strong> 5% reduction in LDL-C are lower than those typically<br />
seen with statin agents, making Answer C (the effects are<br />
similar) an incorrect answer. The most compelling reason<br />
for incorporating more soy in<strong>to</strong> the animal protein–rich<br />
American diet is that this will tend <strong>to</strong> decrease dietary<br />
saturated fat and cholesterol (Answer D); thus Answer D is<br />
the correct answer.<br />
1. Reynolds K, Chin A, Lees KA, Nguyen A, Bujnowski D, He J.<br />
A meta-analysis of the effect of soy protein supplementation on<br />
serum lipids. Am J Cardiol 2006;98:633–40.<br />
2. Nettle<strong>to</strong>n JA, Greany KA, Thomas W, Wangen KE, Adlercreutz<br />
H, Kurzer MS. The effect of soy consumption on the urinary<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition 53 Gastroenterology and Nutrition <strong>Answers</strong>
2:16-hydroxyestrone ratio in postmenopausal women depends<br />
on equol production status but is not influenced by probiotic<br />
consumption. J Nutr 2005;135:603–8.<br />
78. Answer: C<br />
A patient who has been taking green tea extract for weight<br />
loss is complaining that the product is not working for her.<br />
The weight loss effects of green tea and green tea extract<br />
are believed <strong>to</strong> be related <strong>to</strong> their caffeine and catechin<br />
content. Therefore, Answer A (the product contains <strong>to</strong>o<br />
much catechin relative <strong>to</strong> the caffeine content) is incorrect.<br />
Guarana or mate could be found in combination with green<br />
tea extract in some weight loss products. Although these<br />
combinations might be expected <strong>to</strong> increase the adverse<br />
effect potential of the product, natural sources of caffeine,<br />
guarana, and mate would be expected <strong>to</strong> potentiate the<br />
effects of green tea extract on weight loss rather counteract<br />
them (Answer B); thus Answer B is incorrect. Habitually<br />
high consumption of caffeine can accentuate weight loss<br />
during green tea therapy, whereas habitually high caffeine<br />
consumption is a risk fac<strong>to</strong>r for weight regain after weight<br />
loss. Thus, Answer C (habitually low caffeine consumption<br />
may attenuate the effect of the green tea extract) is correct.<br />
The antiangiogenic effect of green tea extracts may attenuate<br />
the growth of new adipose tissue (Answer D); however, this<br />
effect would not explain why the patient is not losing weight<br />
while taking the extract, making Answer D incorrect.<br />
1. Cooper R, Morre J, Morre DM. Medicinal benefits of green<br />
tea. Part I. Review of noncancer health benefits. J Altern Comp<br />
Med 2005:11:521–8.<br />
2. Westerterp-Plantenga MS, Lejeune MP, Kovacs EM. Body<br />
weight loss and weight maintenance in relation <strong>to</strong> habitual<br />
caffeine intake and green tea supplementation. Obes Res<br />
2005;13:1195–204.<br />
79. Answer: A<br />
T.K. is a 52-year-old, overweight, postmenopausal<br />
woman seeking advice regarding incorporating more soy<br />
in<strong>to</strong> her diet. In T.K., who consumes a high animal protein/<br />
high-fat diet, the incorporation of several servings of soyderived<br />
foods daily (taken in place of animal-derived foods)<br />
likely would result in a diet more in line with the saturated fat<br />
and cholesterol content suggested in the Dietary Guidelines<br />
for Americans. Such a diet could thus help reduce her<br />
LDL-C. Although not all studies of soy show benefit in<br />
LDL-C lowering or alleviation of vasomo<strong>to</strong>r symp<strong>to</strong>ms<br />
of menopause, some studies do show benefit. Therefore,<br />
Answer A (incorporating several servings of soy per day<br />
could modestly help her vasomo<strong>to</strong>r symp<strong>to</strong>ms and lower<br />
LDL-C) is the correct answer. Answer B (consumption<br />
of three <strong>to</strong> five servings of soy-derived foods per week)<br />
would not supply the 30 g of soy protein per day necessary<br />
<strong>to</strong> contribute <strong>to</strong> enough weight loss <strong>to</strong> improve the blood<br />
lipid profile or alleviate vasomo<strong>to</strong>r symp<strong>to</strong>ms. Therefore,<br />
Answer B is incorrect. Answer C, which states erroneously<br />
that several servings per day are unlikely <strong>to</strong> result in any<br />
health benefit but may increase her risk of endometrial<br />
cancer, is incorrect. Answer D (risks of several servings per<br />
week include a greater chance of developing endometrial<br />
hyperplasia or breast cancer and would outweigh any benefit)<br />
postulates a connection between a modest consumption of<br />
soy and detrimental effects on endometrial and breast tissue<br />
that is highly unlikely; therefore, Answer D is incorrect.<br />
1. Lethaby AE, Brown J, Marjoribanks J, Kronenberg F,<br />
Roberts H, Eden J. Phy<strong>to</strong>estrogens for vasomo<strong>to</strong>r menopausal<br />
symp<strong>to</strong>ms. Cochrane Database of Systematic Reviews<br />
2007;4:CD001395.<br />
2. St-Onge MP, Claps N, Wolper C, Heymsfield SB.<br />
Supplementation with soy-protein–rich foods does not enhance<br />
weight loss. J Am Diet Assoc 2007;107:500–5.<br />
3. Reynolds K, Chin A, Lees KA, Nguyen A, Bujnowski D, He J.<br />
A meta-analysis of the effect of soy protein supplementation on<br />
serum lipids. Am J Cardiol 2006;98:633–40.<br />
4. Taku K, Umegaki K, Sa<strong>to</strong> Y, Taki Y, Endoh K, Watanabe S.<br />
Soy isoflavones lower serum <strong>to</strong>tal and LDL cholesterol in<br />
humans: a meta-analysis of 11 randomized controlled trials.<br />
Am J Clin Nutr 2007;85:1148–56.<br />
80. Answer: C<br />
A meta-analysis included five studies that evaluated the<br />
effect of soy isoflavone on LDL-C concentrations. Data<br />
from the studies are summarized in the following table:<br />
LDL-C<br />
Concentrations<br />
(mmol/L) with High<br />
Isoflavone Intake<br />
LDL-C<br />
Concentrations<br />
(mmol/L) with Low<br />
Isoflavone Intake<br />
Weighted Mean<br />
Difference<br />
(95% confidence<br />
interval)<br />
3.83 3.85 −0.02 (−0.32, 0.28)<br />
3.83 3.80 0.03 (−0.29, 0.35)<br />
2.14 2.31 −0.17 (−0.31, −0.03)<br />
2.86 2.87 −0.01 (−0.29, 0.27)<br />
3.01 3.22 −0.21 (−0.35, −0.07)<br />
Total<br />
−0.14 (−0.23, −0.06)<br />
With these types of data, a 95% confidence interval that<br />
crosses on both sides of 0 means that there is no statistical<br />
difference between treatment groups. Because the<br />
aggregated weighted mean difference for all of the studies<br />
in this meta-analysis was –0.23 <strong>to</strong> –0.06, it did not cross 0,<br />
indicating a benefit for one of the therapies over the other.<br />
Thus, Answer D (has no statistically significant effect on<br />
LDL-C) is incorrect. Answer A (raises the effect of soy<br />
isoflavone intake on LDL-C in a statistically significant<br />
fashion) is incorrect. Results from four of the five studies<br />
showed lower LDL-C concentrations with high isoflavone<br />
intake compared with low isoflavone intake; therefore, the<br />
aggregated value represents a benefit for high isoflavone<br />
intake (Answer C, lowers LDL-C in a statistically significant<br />
fashion) rather than a detrimental effect (Answer B, raises<br />
LDL-C in a non-statistically significant fashion), making<br />
Answer C correct and Answer B incorrect.<br />
1. Zhuo XG, Melby MK, Watanabe S. Soy isoflavone intake<br />
lowers serum LDL cholesterol: a meta-analysis of 8 randomized<br />
controlled trials in humans. J Nutr 2004;134:2395–400.<br />
2. Guller U, DeLong E. Interpreting statistics in medical literature:<br />
a vade mecum for surgeons. J Am Coll Surg 2003;198:441–58.<br />
Gastroenterology and Nutrition <strong>Answers</strong><br />
54<br />
Pharmacotherapy <strong>Self</strong>-<strong>Assessment</strong> Program, 6th Edition