Section 12 Vascular Access for Hemodialysis - American ...
Section 12 Vascular Access for Hemodialysis - American ...
Section 12 Vascular Access for Hemodialysis - American ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
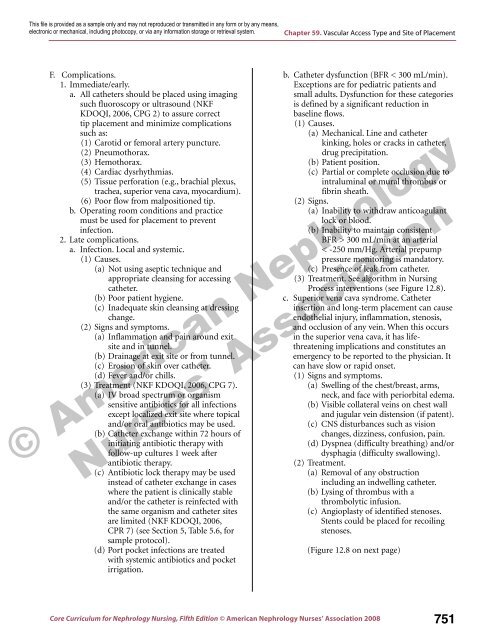
Chapter 59. <strong>Vascular</strong> <strong>Access</strong> Type and Site of Placement<br />
F. Complications.<br />
1. Immediate/early.<br />
a. All catheters should be placed using imaging<br />
such fluoroscopy or ultrasound (NKF<br />
KDOQI, 2006, CPG 2) to assure correct<br />
tip placement and minimize complications<br />
such as:<br />
(1) Carotid or femoral artery puncture.<br />
(2) Pneumothorax.<br />
(3) Hemothorax.<br />
(4) Cardiac dysrhythmias.<br />
(5) Tissue per<strong>for</strong>ation (e.g., brachial plexus,<br />
trachea, superior vena cava, myocardium).<br />
(6) Poor flow from malpositioned tip.<br />
b. Operating room conditions and practice<br />
must be used <strong>for</strong> placement to prevent<br />
infection.<br />
2. Late complications.<br />
a. Infection. Local and systemic.<br />
(1) Causes.<br />
(a) Not using aseptic technique and<br />
appropriate cleansing <strong>for</strong> accessing<br />
catheter.<br />
(b) Poor patient hygiene.<br />
(c) Inadequate skin cleansing at dressing<br />
change.<br />
(2) Signs and symptoms.<br />
(a) Inflammation and pain around exit<br />
site and in tunnel.<br />
(b) Drainage at exit site or from tunnel.<br />
(c) Erosion of skin over catheter.<br />
(d) Fever and/or chills.<br />
(3) Treatment (NKF KDOQI, 2006, CPG 7).<br />
(a) IV broad spectrum or organism<br />
sensitive antibiotics <strong>for</strong> all infections<br />
except localized exit site where topical<br />
and/or oral antibiotics may be used.<br />
(b) Catheter exchange within 72 hours of<br />
initiating antibiotic therapy with<br />
follow-up cultures 1 week after<br />
antibiotic therapy.<br />
(c) Antibiotic lock therapy may be used<br />
instead of catheter exchange in cases<br />
where the patient is clinically stable<br />
and/or the catheter is reinfected with<br />
the same organism and catheter sites<br />
are limited (NKF KDOQI, 2006,<br />
CPR 7) (see <strong>Section</strong> 5, Table 5.6, <strong>for</strong><br />
sample protocol).<br />
(d) Port pocket infections are treated<br />
with systemic antibiotics and pocket<br />
irrigation.<br />
b. Catheter dysfunction (BFR < 300 mL/min).<br />
Exceptions are <strong>for</strong> pediatric patients and<br />
small adults. Dysfunction <strong>for</strong> these categories<br />
is defined by a significant reduction in<br />
baseline flows.<br />
(1) Causes.<br />
(a) Mechanical. Line and catheter<br />
kinking, holes or cracks in catheter,<br />
drug precipitation.<br />
(b) Patient position.<br />
(c) Partial or complete occlusion due to<br />
intraluminal or mural thrombus or<br />
fibrin sheath.<br />
(2) Signs.<br />
(a) Inability to withdraw anticoagulant<br />
lock or blood.<br />
(b) Inability to maintain consistent<br />
BFR > 300 mL/min at an arterial<br />
< -250 mm/Hg. Arterial prepump<br />
pressure monitoring is mandatory.<br />
(c) Presence of leak from catheter.<br />
(3) Treatment. See algorithm in Nursing<br />
Process interventions (see Figure <strong>12</strong>.8).<br />
c. Superior vena cava syndrome. Catheter<br />
insertion and long-term placement can cause<br />
endothelial injury, inflammation, stenosis,<br />
and occlusion of any vein. When this occurs<br />
in the superior vena cava, it has lifethreatening<br />
implications and constitutes an<br />
emergency to be reported to the physician. It<br />
can have slow or rapid onset.<br />
(1) Signs and symptoms.<br />
(a) Swelling of the chest/breast, arms,<br />
neck, and face with periorbital edema.<br />
(b) Visible collateral veins on chest wall<br />
and jugular vein distension (if patent).<br />
(c) CNS disturbances such as vision<br />
changes, dizziness, confusion, pain.<br />
(d) Dyspnea (difficulty breathing) and/or<br />
dysphagia (difficulty swallowing).<br />
(2) Treatment.<br />
(a) Removal of any obstruction<br />
including an indwelling catheter.<br />
(b) Lysing of thrombus with a<br />
thrombolytic infusion.<br />
(c) Angioplasty of identified stenoses.<br />
Stents could be placed <strong>for</strong> recoiling<br />
stenoses.<br />
(Figure <strong>12</strong>.8 on next page)<br />
Core Curriculum <strong>for</strong> Nephrology Nursing, Fifth Edition © <strong>American</strong> Nephrology Nurses’ Association 2008 751