Varicose Veins Brochure - drsarma.in
Varicose Veins Brochure - drsarma.in
Varicose Veins Brochure - drsarma.in
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
THE VASCULAR DISEASE FOUNDATION<br />
The Vascular Disease Foundation is a non-profit, educational<br />
organization dedicated to reduc<strong>in</strong>g death and disability from<br />
vascular diseases and improv<strong>in</strong>g vascular health for all<br />
Americans. We are cont<strong>in</strong>ually develop<strong>in</strong>g educational<br />
<strong>in</strong>formation and other resources about vascular disease for<br />
medical professionals, the public, and for those affected by<br />
common vascular disorders. The Board of Directors of the<br />
Foundation <strong>in</strong>clude lead<strong>in</strong>g experts <strong>in</strong> vascular care, <strong>in</strong>clud<strong>in</strong>g<br />
physicians, researchers, and members of national vascular<br />
medical societies who have been active <strong>in</strong> fight<strong>in</strong>g vascular<br />
disease. The Foundation is dedicated to operat<strong>in</strong>g with m<strong>in</strong>imal<br />
overhead expenses, choos<strong>in</strong>g to apply funds to provide<br />
<strong>in</strong>formation and educational materials for the public.<br />
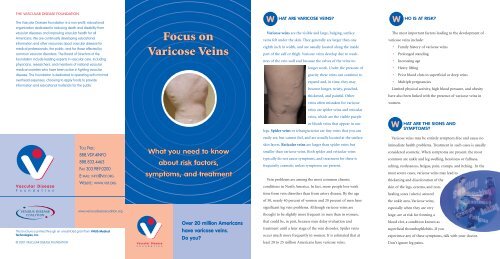
Focus on<br />
<strong>Varicose</strong> <strong>Ve<strong>in</strong>s</strong><br />
W<br />
HAT ARE VARICOSE VEINS?<br />
The<br />
<strong>Varicose</strong> ve<strong>in</strong>s are the visible and large, bulg<strong>in</strong>g, surface<br />
ve<strong>in</strong>s felt under the sk<strong>in</strong>. They generally are larger than one<br />
eighth <strong>in</strong>ch <strong>in</strong> width, and are usually located along the <strong>in</strong>side<br />
part of the calf or thigh. <strong>Varicose</strong> ve<strong>in</strong>s develop due to weakness<br />
of the ve<strong>in</strong> wall and because the valves of the ve<strong>in</strong>s no<br />
longer work. Under the pressure of<br />
gravity these ve<strong>in</strong>s can cont<strong>in</strong>ue to<br />
expand and, <strong>in</strong> time, they may<br />
become longer, twisty, pouched,<br />
W<br />
HO IS AT RISK?<br />
most important factors lead<strong>in</strong>g to the development of<br />
varicose ve<strong>in</strong>s <strong>in</strong>clude:<br />
• Family history of varicose ve<strong>in</strong>s<br />
• Prolonged stand<strong>in</strong>g<br />
• Increas<strong>in</strong>g age<br />
• Heavy lift<strong>in</strong>g<br />
• Prior blood clots <strong>in</strong> superficial or deep ve<strong>in</strong>s<br />
• Multiple pregnancies<br />
Limited physical activity, high blood pressure, and obesity<br />
thickened, and pa<strong>in</strong>ful. Other<br />
have also been l<strong>in</strong>ked with the presence of varicose ve<strong>in</strong>s <strong>in</strong><br />
ve<strong>in</strong>s often mistaken for varicose<br />
women.<br />
ve<strong>in</strong>s are spider ve<strong>in</strong>s and reticular<br />
ve<strong>in</strong>s, which are the visible purple<br />
or bluish ve<strong>in</strong>s that appear <strong>in</strong> our<br />
legs. Spider ve<strong>in</strong>s or teleangiectesias are t<strong>in</strong>y ve<strong>in</strong>s that you can<br />
W<br />
HAT ARE THE SIGNS AND<br />
SYMPTOMS?<br />
easily see, but cannot feel, and are usually located at the surface<br />
<strong>Varicose</strong> ve<strong>in</strong>s may be entirely symptom-free and cause no<br />
TOLL FREE:<br />
888.VDF.4INFO<br />
888.833.4463<br />
FAX 303.989.0200<br />
E-MAIL: INFO@VDF.ORG<br />
WEBSITE: WWW.VDF.ORG<br />
What you need to know<br />
about risk factors,<br />
symptoms, and treatment<br />
sk<strong>in</strong> layers. Reticular ve<strong>in</strong>s are larger than spider ve<strong>in</strong>s but<br />
smaller than varicose ve<strong>in</strong>s. Both spider and reticular ve<strong>in</strong>s<br />
typically do not cause symptoms, and treatment for these is<br />
frequently cosmetic unless symptoms are present.<br />
Ve<strong>in</strong> problems are among the most common chronic<br />
conditions <strong>in</strong> North America. In fact, more people lose work<br />
immediate health problems. Treatment <strong>in</strong> such cases is usually<br />
considered cosmetic. When symptoms are present, the most<br />
common are ankle and leg swell<strong>in</strong>g, heav<strong>in</strong>ess or fullness,<br />
ach<strong>in</strong>g, restlessness, fatigue, pa<strong>in</strong>, cramps, and itch<strong>in</strong>g. In the<br />
most severe cases, varicose ve<strong>in</strong>s may lead to<br />
thicken<strong>in</strong>g and discoloration of the<br />
sk<strong>in</strong> of the legs, eczema, and non-<br />
time from ve<strong>in</strong> disorders than from artery disease. By the age<br />
heal<strong>in</strong>g sores (ulcers) around<br />
of 50, nearly 40 percent of women and 20 percent of men have<br />
the ankle area. <strong>Varicose</strong> ve<strong>in</strong>s,<br />
www.venousdiseasecoaliton.org<br />
significant leg ve<strong>in</strong> problems. Although varicose ve<strong>in</strong>s are<br />
thought to be slightly more frequent <strong>in</strong> men than <strong>in</strong> women,<br />
especially when they are very<br />
large, are at risk for form<strong>in</strong>g a<br />
This brochure is pr<strong>in</strong>ted through an unrestricted grant from VNUS Medical<br />
Technologies, Inc.<br />
© 2007 VASCULAR DISEASE FOUNDATION<br />
Over 20 million Americans<br />
have varicose ve<strong>in</strong>s.<br />
Do you?<br />
that could be, <strong>in</strong> part, because men delay evaluation and<br />
treatment until a later stage of the ve<strong>in</strong> disorder. Spider ve<strong>in</strong>s<br />
occur much more frequently <strong>in</strong> women. It is estimated that at<br />
least 20 to 25 million Americans have varicose ve<strong>in</strong>s.<br />
blood clot, a condition known as<br />
superficial thrombophlebitis. If you<br />
experience any of these symptoms, talk with your doctor.<br />
Don't ignore leg pa<strong>in</strong>s.
W<br />
HAT ARE THE CAUSES?<br />
The causes of varicose ve<strong>in</strong>s are related to non-function<strong>in</strong>g<br />
ve<strong>in</strong> valves. Ve<strong>in</strong> valves are designed to allow blood to flow from<br />
the legs toward the heart aga<strong>in</strong>st gravity, while prevent<strong>in</strong>g<br />
reverse flow back down the legs. Reverse flow is called venous<br />
reflux. Ve<strong>in</strong> valves may fail to close due to either, 1) ve<strong>in</strong> wall<br />
weakness that causes the ve<strong>in</strong> to enlarge and the valves to leak;<br />
2) a history of blood clots <strong>in</strong> the ve<strong>in</strong> that damage the valves;<br />
or 3) an absence of ve<strong>in</strong> valves s<strong>in</strong>ce birth. <strong>Varicose</strong> ve<strong>in</strong>s can<br />
be hereditary, often occurr<strong>in</strong>g <strong>in</strong> several members of the same<br />
family. <strong>Varicose</strong> ve<strong>in</strong>s can also develop after trauma or <strong>in</strong>jury.<br />
Regardless of cause, defective valves cause venous blood to<br />
stagnate (pool) <strong>in</strong> the legs, lead<strong>in</strong>g to high blood pressure <strong>in</strong> the<br />
leg ve<strong>in</strong>s. This may result <strong>in</strong> further enlargement of the varicose<br />
ve<strong>in</strong>s, <strong>in</strong>creas<strong>in</strong>g the likelihood of advanced symptoms such as<br />
sk<strong>in</strong> changes and ulcers at the ankles. Reflux <strong>in</strong> the largest<br />
superficial ve<strong>in</strong>s, such as the saphenous ve<strong>in</strong>s, is often an<br />
underly<strong>in</strong>g cause of pa<strong>in</strong>ful varicose ve<strong>in</strong>s. Venous reflux is a<br />
condition that can be progressive. If left untreated, it can worsen<br />
and cause more advanced symptoms. In addition, blockage of<br />
the ve<strong>in</strong>s <strong>in</strong> the pelvis may severely aggravate the symptoms of<br />
varicose ve<strong>in</strong>s, requir<strong>in</strong>g separate treatment.<br />
H<br />
OW ARE VARICOSE<br />
VEINS TREATED?<br />
<strong>Varicose</strong> ve<strong>in</strong>s are always a sign of an underly<strong>in</strong>g venous<br />
<strong>in</strong>sufficiency disorder, whether symptomatic or not. If not treated,<br />
symptoms may develop, and the exisit<strong>in</strong>g venous <strong>in</strong>sufficiency<br />
signs and symptoms will worsen. Significant advances <strong>in</strong> the<br />
treatment of leg ve<strong>in</strong> problems have occurred <strong>in</strong> recent years.<br />
The treatment of varicose ve<strong>in</strong>s may be conservative, m<strong>in</strong>imally<br />
<strong>in</strong>vasive, or <strong>in</strong>vasive, depend<strong>in</strong>g on the extent of the varicosities,<br />
the symptoms of the patient, and the specific ve<strong>in</strong>s <strong>in</strong>volved.<br />
However, each treatment has some risks and downsides that<br />
should be discussed with your physician or surgeon.<br />
• Ambulatory phlebectomy is also a m<strong>in</strong>imally <strong>in</strong>vasive<br />
procedure that can be performed under local, epidural, or<br />
general anesthesia <strong>in</strong> an outpatient sett<strong>in</strong>g. <strong>Varicose</strong> ve<strong>in</strong>s<br />
are removed with small hooks through t<strong>in</strong>y sk<strong>in</strong> <strong>in</strong>cisions.<br />
Stitches are not used, and the t<strong>in</strong>y <strong>in</strong>cisions are pulled<br />
together with sterile paper-tape. Recovery is generally<br />
brief and uneventful.<br />
• Ve<strong>in</strong> stripp<strong>in</strong>g has been the traditional treatment for bad<br />
valves <strong>in</strong> the great saphenous ve<strong>in</strong>, the largest surface ve<strong>in</strong><br />
which goes down the <strong>in</strong>ner side of the leg. Usually the thigh<br />
part of the great saphenous ve<strong>in</strong> is stripped (removed). After<br />
stripp<strong>in</strong>g, multiple f<strong>in</strong>e sk<strong>in</strong> <strong>in</strong>cisions are made to allow<br />
removal of the varicose ve<strong>in</strong>s. The entire surgery is safely<br />
performed under general, epidural, or local anesthesia,<br />
typically <strong>in</strong> an outpatient sett<strong>in</strong>g, and offers long-term results.<br />
• Laser treatments use a f<strong>in</strong>e optical fiber, which is advanced<br />
through a catheter <strong>in</strong>to the saphenous ve<strong>in</strong>. Laser energy is<br />
then delivered through the fiber. The fiber makes contact<br />
with the blood and <strong>in</strong>ner wall of the ve<strong>in</strong> and, as the fiber is<br />
slowly withdrawn, the laser energy is absorbed by the blood<br />
and ve<strong>in</strong> tissue, seal<strong>in</strong>g it shut. The procedure can be performed<br />
<strong>in</strong> a doctor’s office or outpatient sett<strong>in</strong>g. Recovery<br />
time is usually fast with positive short and mid-term results.<br />
W<br />
HAT YOU CAN DO!<br />
You can’t do anyth<strong>in</strong>g about your heredity, age, or gender.<br />
However, you can help delay the development of varicose ve<strong>in</strong>s<br />
or keep them from progress<strong>in</strong>g. Some th<strong>in</strong>gs you can do:<br />
• Be active. Mov<strong>in</strong>g leg muscles keeps the blood flow<strong>in</strong>g.<br />
• Work with your doctor to keep your blood pressure under<br />
control.<br />
• To temporarily relieve symptoms, lie down and raise your<br />
legs at least six <strong>in</strong>ches above the level of your heart. Do this<br />
for at least ten m<strong>in</strong>utes a few times each day.<br />
• Strive for a normal weight.<br />
• Wear your prescription compression stock<strong>in</strong>gs as specified<br />
by your doctor.<br />
• See a qualified doctor who can diagnose the cause of your<br />
varicose ve<strong>in</strong>s, the sources of venous reflux <strong>in</strong> your legs, and<br />
offer a variety of treatment options.<br />
H<br />
OW ARE VARICOSE<br />
VEINS DIAGNOSED?<br />
The diagnosis of varicose ve<strong>in</strong>s is made primarily by physical<br />
exam<strong>in</strong>ation. The accuracy of physical exam<strong>in</strong>ation is further<br />
improved with the aid of a hand-held Doppler (ultrasound)<br />
<strong>in</strong>strument, which allows the exam<strong>in</strong>er to listen to the blood<br />
flow. The most accurate and detailed test is a duplex ultrasound<br />
exam, which provides an ultrasound image of the ve<strong>in</strong> to detect<br />
any blockage caused by blood clots, and to determ<strong>in</strong>e whether<br />
the ve<strong>in</strong> valves are work<strong>in</strong>g properly or have evidence of reflux.<br />
Measurement of the venous function of the leg may also be<br />
obta<strong>in</strong>ed with other tests such as plethysmography. These diagnostic<br />
tests are non-<strong>in</strong>vasive and pa<strong>in</strong>less.<br />
Here are the most common treatments:<br />
• Prescription compression stock<strong>in</strong>gs to reduce the symptoms<br />
of varicose ve<strong>in</strong>s, prevent leg swell<strong>in</strong>g, and decrease the risk of<br />
blood clots. Prescription stock<strong>in</strong>gs offer appropriate countercompression<br />
and are more effective than the over the counter<br />
stock<strong>in</strong>gs.<br />
• Sclerotherapy (<strong>in</strong>jections of the ve<strong>in</strong>s) <strong>in</strong>volves <strong>in</strong>ject<strong>in</strong>g a<br />
scleros<strong>in</strong>g solution <strong>in</strong>to spider, reticular, or varicose ve<strong>in</strong>s. This<br />
is a m<strong>in</strong>imally <strong>in</strong>vasive office procedure. This blocks the ve<strong>in</strong>s<br />
that are unsightly or not work<strong>in</strong>g well. Injection of scleros<strong>in</strong>g<br />
solutions slowly elim<strong>in</strong>ates the unsightly sk<strong>in</strong> ve<strong>in</strong>s to improve<br />
appearance. Patients typically receive multiple treatments and<br />
most see significant improvement over the course of several<br />
months of treatment.<br />
• RF treatment <strong>in</strong>volves controlled delivery of radio-frequency<br />
(RF) energy directly to a ve<strong>in</strong> wall by a small catheter caus<strong>in</strong>g<br />
collagen <strong>in</strong> the ve<strong>in</strong> wall to shr<strong>in</strong>k and the ve<strong>in</strong> to close. Once<br />
the ve<strong>in</strong> is closed, blood is naturally rerouted by the body to<br />
other healthy ve<strong>in</strong>s. Studies after RF treatment confirm fast<br />
recovery, and it may offer early advantages over surgical ve<strong>in</strong><br />
stripp<strong>in</strong>g. In mid- and some long-term studies, RF treatment<br />
has been shown to offer durable results. It can be safely<br />
performed <strong>in</strong> a doctor's office or outpatient sett<strong>in</strong>g.<br />
OTHER COMPLICATIONS: Without treatment, varicose<br />
ve<strong>in</strong>s may cause pa<strong>in</strong> or ach<strong>in</strong>g, leg swell<strong>in</strong>g, sk<strong>in</strong> color changes,<br />
hardened sk<strong>in</strong> and subcutaneous tissue (lipodermatosclerosis),<br />
and eczema. In advanced cases, breakdown of the sk<strong>in</strong> may<br />
cause bleed<strong>in</strong>g from varicose ve<strong>in</strong>s, and large varicosities may<br />
develop blood clots, a condition called superficial phlebitis or<br />
thrombophlebitis. Patients with varicose ve<strong>in</strong>s may also eventually<br />
develop chronic sk<strong>in</strong> ulceration around the ankle.