Journal of Hematology - Supplements - Haematologica
Journal of Hematology - Supplements - Haematologica
Journal of Hematology - Supplements - Haematologica
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
4<br />
sources <strong>of</strong> hematopoietic stem cells include<br />
unrelated donors and autologous marrow. The<br />
results <strong>of</strong> BMT from unrelated donors demonstrate<br />
a 35% <strong>of</strong> DFS at 8 years. The search for an<br />
unrelated donor can be very long, so, when a<br />
related donor is not available, allogeneic BMT<br />
should be considered just as if chromosome<br />
alterations are present or in patients who do not<br />
respond to chemotherapy. Otherwise, transplants<br />
involving unrelated donors for AML in<br />
remission should proceed largely in the context<br />
<strong>of</strong> a clinical research protocol. 13 As far as regards<br />
autologous BMT, studies by both the Children<br />
Cancer Group and the Pediatric Oncology<br />
Group have not shown any difference in DFS<br />
between children receiving autologous transplant<br />
and those receiving continued chemotherapy<br />
(50% and 44%, respectively for the CCG<br />
study; 38% and 36% for the POG study). 12,13<br />
Allogeneic bone marrow transplantation<br />
in chronic myelogenous leukemia<br />
Allogeneic or syngenic BMT is an effective<br />
treatment for chronic myelogenous leukemia<br />
(CML); 17 the results are dependent on the phase<br />
<strong>of</strong> the disease at the time <strong>of</strong> BMT. Allogeneic<br />
grafting should ideally be performed during the<br />
chronic phase within 1 year from diagnosis, but<br />
patients in advanced phases may also be treated<br />
with this procedure on an individual basis.<br />
Children who receive a transplant during blast<br />
crisis have a 10% to 20% DFS, those in accelerated<br />
phase have a 35% to 40% DFS, and those<br />
in chronic phase have a 50 to 80% DFS. Among<br />
chronic phase patients the major factor predicting<br />
outcome is the length <strong>of</strong> time between<br />
diagnosis and transplant: 17-18 those who receive<br />
a transplant within the first year after diagnosis<br />
have a DFS <strong>of</strong> 80-85% in the first 3 years, whereas<br />
those who receive a transplant more than 2<br />
years after diagnosis have a DFS <strong>of</strong> 50-60%. 19<br />
Unrelated donor marrow transplants give<br />
results similar to those obtained from suitably<br />
matched family member donors but are usually<br />
performed in the context <strong>of</strong> clinical research protocols.<br />
Allogeneic bone marrow transplantation<br />
in myelodysplastic syndromes<br />
Myelodysplastic syndromes (MDS) (Table 4)<br />
represent a heterogeneous group <strong>of</strong> clonal alterations<br />
<strong>of</strong> hematopoiesis, having in common<br />
cytopenia, dysplasia and a predisposition to<br />
evolve in acute myeloid leukemia (20-30% <strong>of</strong><br />
cases). These disorders are typical <strong>of</strong> adult age:<br />
they represent only 2-9% <strong>of</strong> childhood hematologic<br />
malignancies; furthermore MDS <strong>of</strong> childhood<br />
appear to run a more aggressive course,<br />
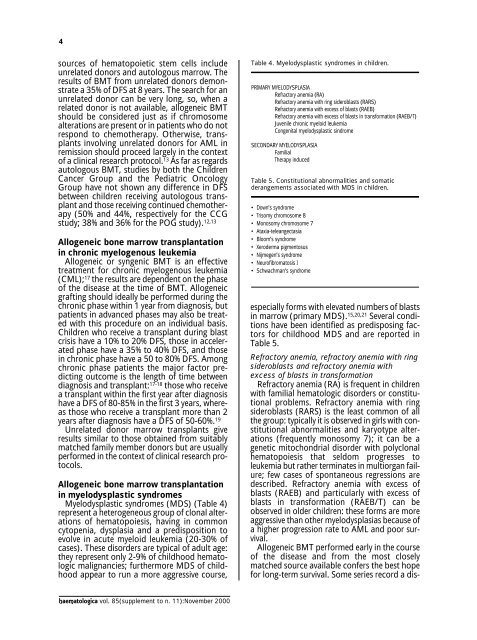
Table 4. Myelodysplastic syndromes in children.<br />
PRIMARY MYELODYSPLASIA<br />
Refractory anemia (RA)<br />
Refractory anemia with ring sideroblasts (RARS)<br />
Refractory anemia with excess <strong>of</strong> blasts (RAEB)<br />
Refractory anemia with excess <strong>of</strong> blasts in transformation (RAEB/T)<br />
Juvenile chronic myeloid leukemia<br />
Congenital myelodysplastic sindrome<br />
SECONDARY MYELODYSPLASIA<br />
Familial<br />
Therapy induced<br />
Table 5. Constitutional abnormalities and somatic<br />
derangements associated with MDS in children.<br />
• Down’s syndrome<br />
• Trisomy chromosome 8<br />
• Monosomy chromosome 7<br />
• Ataxia-teleangectasia<br />
• Bloom’s syndrome<br />
• Xeroderma pigmentosus<br />
• Nijmegen’s syndrome<br />
• Neur<strong>of</strong>ibromatosis I<br />
• Schwachman’s syndrome<br />
especially forms with elevated numbers <strong>of</strong> blasts<br />
in marrow (primary MDS). 15,20,21 Several conditions<br />
have been identified as predisposing factors<br />
for childhood MDS and are reported in<br />
Table 5.<br />
Refractory anemia, refractory anemia with ring<br />
sideroblasts and refractory anemia with<br />
excess <strong>of</strong> blasts in transformation<br />
Refractory anemia (RA) is frequent in children<br />
with familial hematologic disorders or constitutional<br />
problems. Refractory anemia with ring<br />
sideroblasts (RARS) is the least common <strong>of</strong> all<br />
the group: typically it is observed in girls with constitutional<br />
abnormalities and karyotype alterations<br />
(frequently monosomy 7); it can be a<br />
genetic mitochondrial disorder with polyclonal<br />
hematopoiesis that seldom progresses to<br />
leukemia but rather terminates in multiorgan failure;<br />
few cases <strong>of</strong> spontaneous regressions are<br />
described. Refractory anemia with excess <strong>of</strong><br />
blasts (RAEB) and particularly with excess <strong>of</strong><br />
blasts in transformation (RAEB/T) can be<br />
observed in older children: these forms are more<br />
aggressive than other myelodysplasias because <strong>of</strong><br />
a higher progression rate to AML and poor survival.<br />
Allogeneic BMT performed early in the course<br />
<strong>of</strong> the disease and from the most closely<br />
matched source available confers the best hope<br />
for long-term survival. Some series record a dis-<br />
haematologica vol. 85(supplement to n. 11):November 2000