Scientific Presentations Summer 2009 - Dana-Farber/Harvard ...
Scientific Presentations Summer 2009 - Dana-Farber/Harvard ...
Scientific Presentations Summer 2009 - Dana-Farber/Harvard ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
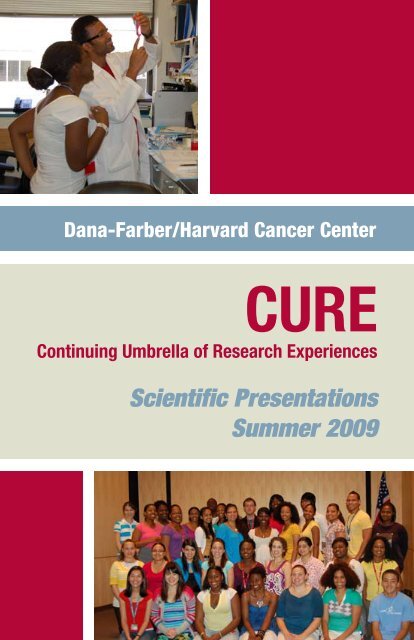
<strong>Dana</strong>-<strong>Farber</strong>/<strong>Harvard</strong> Cancer Center<br />
CURE<br />
Continuing Umbrella of Research Experiences<br />
<strong>Scientific</strong> <strong>Presentations</strong><br />
<strong>Summer</strong> <strong>2009</strong>
Launched in 2002, the Continuing Umbrella of Research<br />
Experiences (CURE) at <strong>Dana</strong>-<strong>Farber</strong>/<strong>Harvard</strong> Cancer Center<br />
is an important building block in research training initiatives.<br />
This program is designed to provide underrepresented<br />
minority high school and college students with a stimulating<br />
and rewarding hands-on research experience that encourages<br />
students to pursue education and training in the biomedical<br />
sciences and careers in basic, clinical and population sciences<br />
cancer research.
CURE <strong>Scientific</strong> <strong>Presentations</strong><br />
<strong>Dana</strong> Building, Room 1620<br />
(Smith Family Room)<br />
Wednesday, August 19, <strong>2009</strong><br />
1:00–4:00 p.m.<br />
Thursday, August 20, <strong>2009</strong><br />
1:30–5:00 p.m.<br />
Friday, August 21, <strong>2009</strong><br />
1:00–4:00 p.m.
Incidence and Predictors of a Late Prostate Cancer Recurrence Among Men Who<br />
Have No Evidence of Disease at Five Years Following a Radical Prostatectomy<br />
Abiola Ahove<br />
Mentor: Paul Nguyen, MD<br />
<strong>Scientific</strong> Advisor: Vince D’Amico, MD, PhD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute/Brigham and Women’s Hospital<br />
Background Information: Prostate cancer is the second-leading cause of cancer<br />
death in American men. A prostate-specific antigen (PSA) level >=0.2 ng/mL following<br />
radical prostatectomy is called a PSA failure and is considered to be a prostate<br />
cancer recurrence. Objective: In this study, we examined the incidence and predictors<br />
of developing a late PSA failure among men who have achieved at least five years<br />
of recurrence-free survival following a radical prostatectomy. Methods: The clinical<br />
records of 508 men who underwent radical prostatectomy for prostate cancer from<br />
1985-2000 at Brigham and Women’s Hospital and who achieved at least five years of<br />
recurrence-free survival (i.e. all PSAs
Production of ß 2<br />
M and HLA-A2 for MHC Tetramers Formation<br />
Judith Alonzo<br />
Mentor: Karen S. Anderson MD, PhD<br />
<strong>Scientific</strong> Advisors: Jaewon Choi, MS; Jun Zhou, PhD; and Jessica Wong, BA<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Background: The major histocompatibility complex (MHC) is a genomic region<br />
that plays a crucial role in the immune system of most vertebrates. MHC tetramers<br />
are proteins that monitor T-cells in the blood and bind to T-cell receptors. They are<br />
folded by binding ß 2<br />
-microglobulin (ß 2<br />
M) with HLA-A2 and antigenic peptide.<br />
MHC tetramers require refolding individual sub-units of high purity, quantity, and<br />
quality. The goal of this project is to produce high yields of ß 2<br />
M and A0201 to fold<br />
MHC tetramers with the desired peptide. Methods: Three A2 DNA constructs were<br />
tested, HLA-A2Nohis1, A2his+4, and A*0201 and one ß 2<br />
M. Culture conditions<br />
were optimized to obtain higher yields of both, ß 2<br />
M and HLA-A. Proteins were<br />
expressed in E. coli bacteria. Two methods were employed for ß 2<br />
M and HLA-A production<br />
to fold MHC tetramers, sonication and B-PER Reagent. Both techniques<br />
disrupt the cell membranes and release cell contents, including proteins. Refolding<br />
reaction and biotinylation of each protein follows. Purity is monitored on 4-20%<br />
SDS-PAGE gel. Results: HLA-A*0201 was found to work better than the other<br />
DNA constructs, giving higher yields (390.80mg for 1L culture) and more pure<br />
samples; similar results have been obtained for ß 2<br />
M but at lower yields (13.46mg for<br />
250mL culture). Currently, sonication has proven to be more suitable for large-scale<br />
protein preparation than B-PER reagent. Conclusion: A0201 was obtained in high<br />
yields and purity, as well as ß 2<br />
M. The sonication method is more efficient for Largescale<br />
protein production while B-PER reagent is more convenient for smaller sample<br />
sizes. No final conclusions can be made at this time since folding and biotinylation<br />
processes are ongoing.
Medical and Psychological Outcomes of Sibling Donors for Patients Undergoing<br />
Allogeneic Hematopoietic Stem Cell Transplantation (HSCT) at a Single Institution<br />
Bethel Belai<br />
Mentor: Leslie Lehmann, MD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Bone marrow transplant (BM) and cytokine mobilized peripheral blood stem cell<br />
(PBSC) transplantation can be curative for patients with malignant and nonmalignant<br />
hematologic diseases. Siblings are most often used as donor matches for such<br />
patients. In cases where siblings are not donor matches, unrelated donors are used<br />
as donor matches for these same patients. Much psychological assessment has been<br />
done regarding unrelated donors post-donation, but none involving sibling donors<br />
specifically. This exploratory study aims to assess the medical and psychological outcomes<br />
of sibling donors following a bone marrow harvest performed at <strong>Dana</strong>-<strong>Farber</strong><br />
Cancer Institute from January1998 through December 2008. Donor outcome was<br />
assessed at a time, 3-9 months following donation. The first part of the study is the<br />
medical element, compiled by a list of an estimated 150 sibling donors within the<br />
past 10 years, who are between 5-19 years of age. The second part is the psychological<br />
element which examines the donors mental state pre and post-donation. Assessments<br />
were performed in person, or by phone by a member of the HSCT team who did<br />
not perform the actual harvest. Donors were asked questions regarding any medical<br />
or psychological issues related to the process of serving as a donor (guardian was<br />
present for questioning unless donor was under 18 years of age and without guardian<br />
consent). Data will be gathered based on the outcome of these assessments as<br />
documented in the donor medical record.
The extracellular matrix influences mesenchymal stem cell<br />
activation toward a myofibroblast-like phenotype<br />
Melissa Bryll<br />
Mentor: Raghu Kalluri, PhD<br />
<strong>Scientific</strong> Advisor: Michael Duncan, PhD<br />
Beth Israel Deaconess Medical Center/<strong>Harvard</strong> Medical School<br />
Numerous studies suggest that mesenchymal stem cells (MSCs) have the potential<br />
to serve a therapeutic role in a variety of disease states including cancer. However,<br />
recent reports indicate that MSCs in the context of the tumour microenvironment<br />
may serve as a source of carcinoma-associated fibroblasts (CAFs). The extracellular<br />
matrix is an important component of the tumor stroma and regulates cell adhesion,<br />
survival, and proliferation. This study examines the influence of the extracellular matrix<br />
(ECM) on TGFß1- induced transition of MSCs to CAFs. We propose that distinct<br />
ECM components within the tumour microenvironment can modulate MSC<br />
activation into fibroblasts through cell-matrix adhesion events. We have conducted<br />
cell adhesion assays on matrix-coated plates to determine which matrix components<br />
effectively promote cell adhesion during MSC activation. Subsequently, immunoblotting<br />
and gene expression profiling for MSC and CAF markers of TGFß1 treated<br />
cells cultured on the ECM molecules will emphasize the extent to which the matrix<br />
influences MSC activation. We hypothesize fibronectin will have a significant effect,<br />
as it is a common component of the tumour stroma and MSCs readily adhere to it.<br />
Determining a role of the reactive stroma in MSC activation will further enhance our<br />
understanding of MSC utilization and its potential limitations in cancer therapy.
Targeting Glioma Growth<br />
Cody Cameron<br />
Mentor: Khalid Shah, PhD<br />
<strong>Scientific</strong> Advisor: Tugba Bagci, PhD<br />
Massachusetts General Hospital<br />
Glioma is a form of brain cancer which results in very sudden yet detrimental effects<br />
to the patient. Like most cancers, gliomas result from the deregulation of certain<br />
components of the cell cycle, such as proliferation. While normal cells regulate their<br />
proliferation and undergo apoptosis when damaged, glioma cells undergo uncontrolled<br />
proliferation, thereby creating neoplasms. Among other pathways, the PI3<br />
Kinase-Akt pathway is commonly mutated in gliomas resulting in uncontrolled<br />
proliferation. Over activation of PI3 Kinase leads to increased phosphorylation and<br />
thereby activation of Akt, which then leads to increased cell growth. The inhibition<br />
of activity along the PI3 Kinase pathway can achieved with a new drug, PI-103. The<br />
overall goal of the project is to test the efficacy of PI-103 alone and in combination<br />
with stem cell based pro-apoptotic therapies in both malignant and invasive glioma<br />
cells in vitro as well as in mouse models of glioma. My part in the project is to test the<br />
effect of PI-103 on the PI3 Kinase pathway components in different glioma cells in<br />
culture. Specifically, I aim to demonstrate the changes in the phosphorylation of Akt<br />
levels in response to different doses of PI-103 treatment in six established and two<br />
primary human glioma cell lines. My results will determine whether this drug will<br />
inhibit the activation of the PI3-kinase-Akt pathway in human glial cells. This should<br />
set up a clear-cut plan for in vivo experiments that will follow in culture studies and<br />
will be subsequently performed in the laboratory.
Identification of novel genes that influence virulence of vibrio cholerae<br />
Cindy Capitolin<br />
Mentor: Paula Watnick, MD, PhD<br />
<strong>Scientific</strong> Advisor: Alexandra Purdy, PhD<br />
Children’s Hospital Boston<br />
Cholera, a fatal disease characterized by severe diarrhea, is caused by a Gram-negative<br />
bacterium called Vibrio cholerae which is acquired via ingestion of contaminated food<br />
or water. Although cholera is practically non-existent in the US, it is a major concern<br />
in the developing world, particularly in countries with poor sanitation. Identification<br />
of the genes required for intestinal survival of the Vibrio cholerae bacterium will help<br />
us to understand the pathogenesis of this disease and develop new ways of treating<br />
cholera.<br />
The toxin-co regulated pilus and cholera toxin, which are responsible for the intense<br />
diarrhea that is seen in cholera, are already known to be essential for virulence of V.<br />
cholerae. We hypothesize that there are additional genes that contribute to the virulence<br />
of Vibrio cholerae. The purpose of this study is to identify these genes.<br />
The Watnick lab has developed Drosophila melanogaster as a model organism for the<br />
study of cholera. Several virulence-defective mutants were identified in a primary<br />
screen. In my study, survival assays were set up in Drosophila and the virulence defect<br />
of 8 transposon insertion mutants was confirmed. Colonization assays were then<br />
set up in order to determine the ability of each specific mutant strain to survive in<br />
and colonize the Drosophila intestine. We also isolated, amplified and sequenced the<br />
transposon insertion sites of each of these mutant strains.<br />
Thus far we have identified the transposon insertion sites of four mutant strains.<br />
These include flagellar synthesis genes, a phosphate transport system, and an uncharacterized<br />
ABC transport system. We anticipate that at the end of this project we<br />
will discover and characterize other genes that are relevant to the virulence of Vibrio<br />
cholerae.
Determination of Elafin’s role in cellular proliferation<br />
in the ovarian cancer microenvironment<br />
Amber Channer<br />
Mentor: Ronny Drapkin, MD, PhD<br />
<strong>Scientific</strong> Advisor: Adam Clauss, PhD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Ovarian cancer is a major cause of cancer-related mortality in women worldwide.<br />
Unfortunately, the lack of efficient screening methods results in the majority of patients<br />
being diagnosed with late stage ovarian cancer, when a surgical cure is highly<br />
unlikely. Although most patients with advanced stage disease initially respond to<br />
chemotherapy, the majority ultimately relapse with chemo-resistant tumors. Therefore,<br />
there is a pressing need to develop serum biomarkers for early detection. We<br />
have previously described two potential biomarkers: HE4 and Elafin. Both are located<br />
in the WAP locus on chromosome 20q13, a region frequently amplified in<br />
ovarian cancers. The FDA recently approved the HE4 ELISA test, in conjunction<br />
with CA125, to monitor patients with ovarian cancer for recurrence. Elafin is a secreted<br />
serine protease inhibitor, which has shown to specifically inhibit Elastase, a<br />
serine protease. We know that the protease function of Elastase is important to release<br />
TGF-ß and thereby active it. TGF-ß (Transforming Growth Factor) is a secreted<br />
protein that mainly functions to inhibit epithelial proliferation, tumor development<br />
and morphogenesis. During oncogenesis, TGF-ß is silenced and cannot control the<br />
cell cycle, thus enabling cells to grow uncontrollably. This work aims to characterize<br />
the role Elafin plays in the ovarian cancer microenvironment. We hypothesize that<br />
by inhibiting Elastase, Elafin prevents the release of active TGF-ß. To analyze we will<br />
transform a panel of ovarian cell-lines with either wild type Elafin, which has been<br />
previously shown to increase cellular proliferation, or two mutated forms of Elafin<br />
(M25K and M25G). The mutation of methionine to a lysine or a glycine generates<br />
a protein that no longer functions as a serine protease inhibitor. By comparing the<br />
proliferation effect of the wild type Elafin versus the mutated counterpart, we will be<br />
able to tell whether the serine protease inhibitor function of Elafin is necessary for its<br />
role in increasing cellular proliferation.
Co-crystallization of PIP2 and the FERM domain of focal adhesion kinase<br />
Douglas Chapski<br />
Mentor: Daniel Lietha, PhD<br />
<strong>Scientific</strong> Advisor: Michael Eck, MD, PhD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Focal Adhesion Kinase (FAK) is a non-receptor tyrosine kinase that plays an essential<br />
role in focal adhesions and cell migration. FAK’s overexpression in diseases such as<br />
glioblastomas and ovarian cancers suggests that it is a good target for cancer therapies.<br />
However, the mechanism of FAK regulation downstream of integrin signaling<br />
is not fully understood. Previous research indicates that phosphatidylinositol<br />
4,5-bisphosphate (PIP2) activates FAK by binding to the F2 lobe of the FERM domain.<br />
Crystallographic studies show that existing crystal packing of FERM domain<br />
crystals does not allow PIP2 to be soaked into the hypothesized binding region of the<br />
F2 lobe. Co-crystallization was attempted as an alternative method for solving the<br />
FERM+PIP2 structure, but crystals were too small for analysis. Future optimization<br />
of co-crystallization conditions and diffraction studies will give us insight on how<br />
PIP2 binds to the FERM domain, and thus how FAK gets activated. With the new<br />
crystal structure, we will be able to construct a more detailed activation pathway for<br />
FAK.
The Effect of PolyIC on Cultured Lymph Node Fibroblastic Reticular Cells<br />
Pamela Cote<br />
Mentor: Shannon J. Turley, PhD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Fibroblastic reticular cells (FRCs) in the lymph nodes (LNs) have been characterized<br />
as a subset of lymph node stromal cells (LNSCs) with a CD45-, gp38+, CD140a+,<br />
CD31- surface phenotype. These cells have also been found to express MHC Class I<br />
and II, costimulatory molecules (PD-L1, CD80) and adhesion molecules (VCAM-1,<br />
ICAM-1). Expression of these molecules may allow LNSCs to regulate T cell responses<br />
in the LNs and shape immunological tolerance. FRCs are important cells<br />
because they also secrete survival factors for memory and resting T cells in the LNs<br />
and they secrete chemokines which are necessary for the recruitment of Dendritic<br />
cells (DCs) and naïve T cells to the LNs. It has been established that certain viruses<br />
such as the Ebola virus and persistent lymphocytic choriomeningitis (LCMV) infect<br />
FRCs in the LNs which may result in immunological dysfunction and chronic infection.<br />
The purpose of this study is to ascertain whether exposure to PolyIC causes<br />
LNSCs to acquire immunostimulatory potential using flow cytometery. This study<br />
will allow us to determine if viral pathogens or viral products can cause FRCs to<br />
undergo phenotypic changes. Therefore this will allow us to establish whether FRCs<br />
continue to promote self tolerance induction or auto- reactivity of T cells during a<br />
viral infection and to ultimately recognize what important implications these cells<br />
have on immunological disorders.
Conjugating Aptamers to Nanorods Allowing for Chemotherapeutic Drug Delivery<br />
Elise Digga<br />
Mentor: Omid Farokhzad, MA, MD<br />
<strong>Scientific</strong> Advisor: Xiao Zeyu, PhD<br />
Brigham and Women’s Hospital<br />
In recent in vivo experiments, nanorods have been increasingly employed as carriers,<br />
capable of transporting chemotherapeutic drugs to targeted cancer cells. Their ability<br />
to convey the drugs is due to RNA sequences called aptamers. The entire complex<br />
consists of an aptamer attached to strands of nucleic acids, which in turn are conjugated<br />
to the nanorods. The drugs are stored between the strands of nucleic acids and<br />
released when the aptamers bind to membrane receptors specific to the malignant<br />
cells. We are currently trying to find which RNA sequence can bind to which cancer<br />
cells, using the cell lines PC3 (PSMA- prostate cancer cell), LNCaP (PSMA+ prostate<br />
cancer cell), BPH (prostate normal cell). By using FACS (fluorescence-activated cell<br />
sorter) we found an RNA sequence that binds to LNCaP, but not BPH (as expected)<br />
or PC3 due to the membrane receptor specific to LNCaP. We can cut down this<br />
sequence further to find smaller segments that will conjugate with LNCaP and by<br />
doing so will further impact drug transport studies in the future.
Role of SCCRO/DCUN1D1 in Prostate Cancer<br />
Thao Xuan Do<br />
Mentor: Luiz Zerbini, PhD<br />
Beth Israel Deaconess Medical Center<br />
Squamous Cell Carcinoma Related Oncogene (SCCRO)/DCUN1D1 has been<br />
known to be amplified and over-expressed in up to 40% of lung, head and neck,<br />
and cervical squamous cell carcinomas, suggesting that it plays an oncogenic role<br />
in these cancers. However, the role of SCCRO/DCUN1D1 in prostate cancer is<br />
unknown. Therefore we target SCCRO/DCUN1D1 in prostate cancer cell line. By<br />
using Western Blot and PCR, we found that SCCRO/DCUN1D1 is upregulated<br />
at both the mRNA and protein level in primary and metastatic prostate cancer cell<br />
lines such as CW19, CW22, VCaP, LNCaP, DUCaP, DU145, PC3, CL1 and PREC.<br />
Knockdown of this gene in prostate cancer cell lines in vitro using RNA interference<br />
technique resulted in a decrease in proliferation rate by MTT cell proliferation assay<br />
using MTT (yellow tetrazolium salt). Suppression of SCCRO/DCUN1D1 also inhibited<br />
the migration and invasion characteristics of prostate cancer cell lines in vitro<br />
by migration/ invasion assay using BD BioCoat Matrigel Invasion Chambers. With<br />
all of the above results, we strongly believe that SCCRO/DCUN1D1 is required for<br />
the development of prostate cancer tumor.
The Growth of Malignant Plasma Cells in Zebrafish Embryos<br />
Jessica Francois<br />
Mentor: Robert I. Handin, MD<br />
<strong>Scientific</strong> Advisor: Nikhil Munshi, MD<br />
Brigham and Women’s Hospital/<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Multiple myeloma is a malignant disorder of plasma cells, which reside in the bone<br />
marrow and are the antibody-producing cells of the immune system. Our laboratory<br />
uses zebrafish embryos to study the growth of both murine and human myeloma<br />
cell lines and primary myeloma cells purified from patient bone marrow aspirates.<br />
Our objective was to determine whether zebrafish could be used to study growth<br />
characteristics of human myeloma cells. Zebrafish are an increasingly popular animal<br />
model as they are easy to breed and manipulate. Zebrafish embryos are transparent<br />
and tumor cells grow rapidly after injection. We injected 50 nl fluid containing<br />
1,000-2,000 myeloma cells suspended in matrigel into the pervitelline space of<br />
anesthetized, dechorionated zebrafish embryos 48 hours post fertilization. In some<br />
cases, unlabelled myeloma cells were injected into Tg(Fli1:GFP) fish, which express<br />
GFP in endothelial cells, to assess tumor-induced angiogenesis. The angiogenic response<br />
to tumor injection was also assessed by alkaline phosphatase staining of fixed<br />
embryos. Twenty four to forty eight hours after injection, myeloma cells induced an<br />
angiogenic response in the host with proliferation of vessels from the sub-intestinal<br />
venous (SIV) system toward the tumor. Within 2-3 days, visible growth of myeloma<br />
cells was observed. In some fish, myeloma cells grew out of the yolk sac and into<br />
vertebral bodies. In contrast, plasma cells from normal individuals or individuals<br />
with monoclonal gammopathy of uncertain significance (MGUS), a benign precursor<br />
to myeloma, did not induce angiogenesis nor form tumors. We conclude that<br />
zebrafish can be used to study the growth characteristics of human myeloma cells and<br />
may provide a convenient model to identify novel or combinations of drugs that will<br />
inhibit myeloma cell growth.
Targeting Communication Disparities with Click to Connect<br />
Charline Gay<br />
Mentor: Vish Viswanath, PhD<br />
<strong>Scientific</strong> Advisors: Sara Minsky, BA and Emily Zobel Kontos, AB, ScM<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Despite improvements in overall health of Americans, some racial/ethnic minority<br />
populations and lower socioeconomic position (SEP) individuals experience health<br />
disparities that may be attributed to inequalities in communication. The Internet has<br />
emerged as a powerful source of health information with growing penetration. Yet,<br />
limited attention has been paid to the utility and usability of websites for low literacy<br />
and low SEP individuals. In our approach to improving this communications gap,<br />
we developed an intervention (Click to Connect) focused on improving access and<br />
ability to use the Internet for low literacy and low SEP individuals. The components<br />
of the intervention include a low literacy web portal designed specifically for our<br />
audience, computer use/Internet training, and technical support. The goal of my<br />
project is to analyze and report the results of the intervention’s process data, which<br />
will aid in the assessment of the operation of the program, program strengths and<br />
weaknesses, and will allow for mid-course corrections. We hypothesize that participants<br />
will increase their usage of the Internet to seek health information over time<br />
as they acquire computer and Internet literacy skills. Each participant was asked to<br />
complete an online survey once a month to assess their Internet and computer use,<br />
their experience with the system, and a training evaluation questionnaire. In this<br />
survey, we focused on evaluating the effectiveness of the intervention in terms of<br />
the acquisition of computer and Internet literacy skills, and the effectiveness of the<br />
training component of the intervention among participants over the course of the<br />
intervention period. Qualitative and quantitative analysis was then conducted on the<br />
web portal survey results and the training evaluation.
High level baseline in language fmri<br />
Carl Glaser<br />
Mentor: Alexandra Golby, MD<br />
<strong>Scientific</strong> Advisor: Laura Rigolo<br />
Brigham and Women’s Hospital<br />
Functional Magnetic Resonance (fMRI) imaging of the brain has been widely used<br />
in research for years but is just recently becoming prominent clinically for presurgical<br />
planning of tumor resection. The use of fMRI to identify and map functional areas<br />
of the brain, those used in motor, language functions etc, has specifically gained support<br />
in the clinical field because of its non invasive nature. This surge in fMRI’s use<br />
clinically has sent researchers looking for ways to increase its effectiveness. This has<br />
resulted in investigation into the format used to administer fMRI. Currently one<br />
test used to identify areas of language activation consists of a task involving antonym<br />
generation and a baseline scan. The baseline must be obtained in order to show the<br />
change in neural activity. The baseline involves subjects fixating on a crosshair. Because<br />
of this, increased activation between scan occurs not only in the area involved<br />
in language function, it also occurs in areas such as those of working memory, attention,<br />
execution, and vision. Therefore the areas of increased activation during a<br />
language task vs. the standard baseline are not all correlated to the use of language<br />
functions. This provides the user with a wide range of data that isn’t language related.<br />
This experiment will attempt to remedy this fact by introducing a high-level<br />
baseline. This task consists of the subjects identifying whether a series of letters are<br />
uppercase or lowercase. When compared to the traditional baseline it is expected that<br />
the high level baseline will show increases in neurological activation in similar areas<br />
to the language task, excluding the language activation itself. This would then allow<br />
comparison of the language task and the high level baseline, removing all areas of<br />
similar activation from the language task results, leaving only the desired language<br />
activation.
Determining the Mechanisms of DNA Double-Strand Break in<br />
Heterochromatin & Euchromatin<br />
Raquel L. Graham<br />
Mentor: Peter O’Donovan, PhD<br />
<strong>Scientific</strong> Advisor: David Livingston, MD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Our genetic material DNA resides in a chromatin structure composed of DNA and<br />
histone proteins. There are two forms of Chromatin—heterochromatin and euchromatin.<br />
Heterochromatin is tightly compacted and transcriptionaly inactive, whereas<br />
euchromatin is less compacted and transcriptionaly active. Chromatin impacts all<br />
DNA Metabolic processes, including DNA damage and DNA repair. The DNA double-strand<br />
break [DSB] is the most toxic of various types of DNA damage because<br />
both DNA strands are damaged. There are two major categories to repair DNA DSB:<br />
homologous recombination and non-homologous endjoining. Homologous recombination<br />
is error free and non-homologous endjoining is error prone. It has been<br />
suggested that there are differences in DNA repair between heterochromatin and euchromatin.<br />
The purpose of this study is to find out whether or not there are differences<br />
in mechanisms of DNA DSB repair of heterochromatin and euchromatin. To test<br />
this hypothesis, we have developed a system that allows us to generate a single DNA<br />
DSB in a cell. The DNA DSB will be either in heterochromatin or euchromatin. We<br />
will be using an enzyme called ISce-I and female mouse embryonic fibro-blast cells<br />
[MEFs]. A restriction site will be placed in the X Chromosome of the MEFs because<br />
the female has two X Chromosomes, active X (euchromatin) and inactive X (heterochromatin).<br />
Then ISce-I will be introduced into the nucleus to generate a DNA DSB<br />
in the X Chromosome. After DNA DSB repair, genomic DNA will be extracted from<br />
cells, PCR amplified, and sequenced for the region around DSB. The sequence will<br />
tell what repair mechanism was used for DSB, i.e. homologous recombination or<br />
non-homologous endjoining. Therefore we will be able to determine whether different<br />
repair mechanisms were used between heterochromatin vs. euchromatin.
Early Detection of Morphological Changes After<br />
Massive Small Bowel Resection in Rats<br />
Winta Haile<br />
Mentor: Stanley Ashley, MD<br />
<strong>Scientific</strong> Advisor: Anita Balakrishnan, MD<br />
Brigham and Women’s Hospital<br />
Although small bowel resection incites adaptive morphological changes in remnant<br />
intestine, such changes have only been identified a week beyond resection. We aimed<br />
to determine whether these changes would occur at two days post-resection.<br />
Sprague Dawley rats were subjected to either 80% resection (n=4)or transection and<br />
reanastomosis (n=4) of the small bowel. Two days later, rats were sacrificed and sections<br />
of remaining jejunum harvested, fixed in formalin and embedded in paraffin.<br />
7um thick sections were stained with haematoxylin and eosin and used for measurement<br />
of villous height and width, crypt depth, enterocytes per crypt, enterocytes per<br />
villus, and smooth muscle thickness.<br />
I anticipate changes in morphology following resection in response to small bowel<br />
length, such as increases in villous height, crypt depth, number of enterocytes per<br />
crypt and villus, and smooth muscle thickness. If we find reproducible morphological<br />
changes in response to resection, we can use this model to identify potential specific<br />
genetic pathways regulating the adaptive response. Identifying early morphological<br />
changes and the regulating factors will allow improved treatments for patients with<br />
insufficient adaptation in short bowel syndrome.
Patient Acceptability of the Electronic Self Report<br />
Assessment Cancer Program (ESRA-C) Version 2 to Enhance<br />
Communication Between Patients and Clinicians<br />
Tanya Harrison<br />
Mentor: Donna Berry, PhD, RN, AOCN, FAAN<br />
<strong>Scientific</strong> Advisor: Barbara Halpenny, MA<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Assessing cancer symptoms and quality of life issues is essential for excellent clinical<br />
care in cancer patients. The Electronic Self Report Assessment-Cancer program<br />
(ESRA-C) version 1 was demonstrated to be an efficacious and acceptable method to<br />
cancer patients for reporting symptom and quality of life information to clinicians.<br />
ESRA-C version 2 is a further developed program that contains additional symptom<br />
questionnaires and has been used in a multi-site sample in a randomized clinical trial<br />
at two comprehensive cancer centers. The objective of this analysis is to determine<br />
if ESRA-C version 2 is as equally acceptable to patients as version 1 and whether<br />
acceptability differed in various demographics. We evaluated the average score of<br />
the five acceptability questions with response options ranging from one (not at all acceptable)<br />
to six (very much acceptable) among patients that have completed ESRA-C<br />
version 2. We also assessed demographics such as age, gender, and computer literacy.<br />
Results showed that 40% of the sample (n=65) are female, 40% are age 60 or older,<br />
and only 74% of the participants use a computer often or very often. There were no<br />
differences in acceptability of the program between men and women, patients under<br />
or over 60 years old, and frequent or non-frequent computer users. Although specific<br />
measures of acceptability varied between the two groups, the average acceptability<br />
score was lower in version 2. We conclude that ESRA-C version 2 is not as equally<br />
acceptable to patients as version 1 due to the amount of time it takes for the participants<br />
to complete the report.
Investigating the role of Esrrb and its regulation<br />
of satellite cell potential in vitro<br />
Keyauna Hoffman<br />
Mentor: Glen Rowe, PhD<br />
Beth Israel Deaconess Medical Center<br />
Estrogen related receptor beta (Esrrb) encodes for a protein that is involved in many<br />
biological processes including placental and inner ear development. Esrrb has also<br />
been reported to play a role in embryonic cell biology, their self renewal, and the<br />
potential to differentiate. However, little is known at present of the role of Esrrb in<br />
the regulation of other cell systems such as muscle biology and satellite cell’s ability<br />
to differentiate into myoblasts. We therefore wanted to determine if Esrrb played a<br />
role in the regulation of satellite cell’s potential in vitro. Satellite cells are located on<br />
the surface of myofibers and in response to muscle injury, they provide the necessary<br />
skeletal muscle growth and repair. Preliminary data from our lab has shown that elongated<br />
myotubes in culture treated with Esrrb agonist, transform into circular colonies,<br />
which morphologically resemble satellite cells. We therefore performed qPCR to<br />
determine if these circular colonies expressed markers of satellite cells or if they were<br />
simply defused myotubes. We observed a significant change in both markers of satellite<br />
cells and terminally differentiated myotubes, suggesting that the cells treated with<br />
the Esrrb agonist were indeed changing their differentiation program. In summary,<br />
our experiments suggest that Esrrb could potentionally be a regulatory factor in the<br />
satellite differentiation program. We therefore hope to determine whether these dedifferentiated<br />
myotubes can differentiate again into myotubes. In addition, we hope to<br />
perform both gain and loss of function experiments with Esrrb to determine whether<br />
it is either necessary or sufficient to regulate satellite cell differentiation. There are still<br />
many outstanding questions about Esrrb’s contribution to the adult myogenic program<br />
and how it could contribute to advances in stem cell based therapies. However,<br />
these questions are currently the focus of other ongoing studies.
Interstitial Cystitis Antiproliferative Factor Modulates MDM2,<br />
Leading to P53 Stability<br />
Nichole Jones<br />
Mentor: Jayoung Kim, PhD<br />
Children’s Hospital Boston<br />
Objectives: Interstitial cystitis (IC) Antiproliferative Factor (APF) has been reported<br />
as a sialoglycopeptide urinary biomarker of IC, a chronic syndrome of unknown<br />
etiology with variable symptoms including pelvic and or perineal pain, urinary frequency,<br />
and urgency. We previously reported that APF suppressed the proliferation<br />
rate of normal bladder epithelial cells through a mechanism that involves increased<br />
levels of p53 and activated signal pathways (Kim et al. FEBS Lett. 581:3795, 2007;<br />
Kim et al. BJU Int. 103(4):514, <strong>2009</strong>). The goal of present study is to understand<br />
the process whereby p53 expression level elicits cell growth arrest in response to APF.<br />
Methods: We performed MTT-based proliferation assay to measure APF effects on<br />
growth of T24 human bladder cells. We engineered the expression levels of p53 and<br />
the murine double minute 2 E3 ubiquitin ligase (MDM2) by transient transfection<br />
with silencing RNAs or by the use of overexpression constructs. Various biochemical<br />
experiments including Immunofluorescence Staining, western blot analysis and immunoprecipitation<br />
were used. Results: APF treatment significantly decreased protein<br />
level of MDM2 within 2 hours. Time course experiments showed that p53 level was<br />
enhanced when MDM2 expression was suppressed. Inhibition of proteasomal activity<br />
enhanced the APF-induced p53 increase. MDM2 bound to p53 and triggered<br />
ubiquitination and degradation of p53. Furthermore, APF attenuated the association<br />
of p53/MDM2 and delayed p53 degradation. Conclusions: We demonstrate that<br />
MDM2, a negative regulator of p53 expression, is functionally attenuated by APF<br />
in bladder epithelial cells. These data suggest that targeting MDM2 or p53/MDM2<br />
complex formation may be relevant in the development of novel therapeutic approaches<br />
to IC.
Exploring the Effects of Estrogen on Apoptosis<br />
Walker Keenan<br />
Mentor: Shannon Bailey, PhD<br />
<strong>Scientific</strong> Advisor: Myles Brown, MD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
The risk of a woman developing breast cancer over the course of her lifetime is 13%<br />
and 1 in 4 diagnosed cancers in 2008 was breast cancer. Anti-estrogen therapy, which<br />
prevents estrogen receptor (ER) activity, works well in ER positive breast cancer patients.<br />
Previously, our lab has determined all the binding sites for the estrogen receptor<br />
and the pro-apoptotic transcription factor p53, in the human genome. We discovered<br />
that both of these proteins share a subset of binding sites in the MCF7 breast<br />
cancer cell line. It has been determined that some of the genes near these binding<br />
sites are known to initiate apoptosis. We found that a number of these genes are differently<br />
regulated by either p53 or ER, where genes down-regulated by estrogen are<br />
up-regulated by p53 stimuli. We therefore hypothesized that estrogen inhibits apoptosis.<br />
To determine if ER can block p53-mediated apoptosis, we will treat the breast<br />
cancer cell lines, MCF7 and T47D, with apoptosis inducing drugs in the absence or<br />
presence of ß-estradiol (E2), an estrogen receptor agonist. By determining the effects<br />
of E2 on p53-mediated apoptosis, we may be able to provide a new paradigm for the<br />
discovery of more effective breast cancer treatments.
Repression Of Transcription Factor 7-Like 2 Increases Risk Of Type 2 Diabetes<br />
Tsega Meshesha<br />
Mentor: Melissa K. Thomas, MD, PhD<br />
Massachusetts General Hospital<br />
Diabetes mellitus is a disorder characterized by hyperglycemia that can occur through<br />
mechanisms such as impaired insulin secretion, insulin resistance in peripheral tissues<br />
and increased glucose output by liver. Genome-wide association studies have identified<br />
Transcription factor 7-like 2 (TCF7L2), a key element of the Wnt signaling<br />
pathway, as a genetic variant linked to a higher risk of developing type 2 diabetes.<br />
However, the mechanisms by which TCF7L2 is implicated in this disease are unknown.<br />
The objective of this study is to determine whether TCF7L2 deficiency alters<br />
pancreatic beta cell mass, function or insulin production. To address this question,<br />
we are investigating the phenotype of TCF7L2 heterozygous knockout as compared<br />
to wild-type control mice. The mice were genotyped by extracting DNA from tail<br />
biopsies. The extracted DNA was analyzed by polymerase chain reaction (PCR). To<br />
determine whether TCF7L2 deficiency alters insulin production and pancreatic architecture,<br />
pancreatic tissues from TCF7L2 heterozygote and wild-type mice were<br />
immunostained for TCF7L2, insulin, and glucagon. It is expected that if TCF7L2<br />
regulates pancreatic endocrine cell mass or hormone production, the immunostaining<br />
will reveal a change in beta and/or alpha cell mass or pancreatic hormone expression<br />
patterns when pancreatic tissue of TCF7L2 heterozygotes is compared to controls.<br />
This study may elucidate how TCF7L2 influences and/or regulates glucose levels.
Untitled<br />
Michel Moravia<br />
Mentor: Michael F. Gurish, PhD<br />
<strong>Scientific</strong> Advisor: Tatiana G. Jones, MD, PhD<br />
Brigham and Women’s Hospital/<strong>Harvard</strong> Medical School<br />
Mast cells (MC) are found throughout the body near blood vessels and mucosal<br />
interfaces with the environment where they are thought to play a role in mast cell<br />
progenitor homing in innate immunity. The MC homes to the lungs as a committed<br />
progenitor (MCp). A recent investigation of MCp homing uncovered a role for T-bet,<br />
a transcription factor protein that regulates T cell development, as T-bet deficient<br />
mice had reduced numbers of MCp in both the intestine and the lungs (Alcaide et<br />
al, 2007). Surprisingly, the study found that T-bet expression in dendritic cells (DC)<br />
was critical to the homing of MCp to the intestine. We are extending this finding by<br />
investigating whether T-bet+ DC are also required for MCp homing to the lungs. To<br />
evaluate this, I will culture bone marrow-derived DC (BMDC) from both wild type<br />
C57BL/6 mice and T-bet knockout mice. These DC will be transferred to T-bet deficient<br />
mice to evaluate whether T-bet+ DC restores MCp homing to the lung. Two<br />
weeks after transfer, I will perform a limiting dilution assay to quantitatively assess<br />
the total numbers of MCps present in the lungs of the respective mice. This work has<br />
the potential to provide new checkpoints for applied research and drug discoveries.<br />
The use of VIA and HPV testing was favored in most studies and successful results<br />
were attained. VIA fit the criteria of being efficient compared to cytology, affordable,<br />
sensitive and not much training required although is not very specific. Colposcopy<br />
use requires a lot of training and experience in order to get the right results. HPV<br />
vaccination is costly according to most of the countries economic status, in addition,<br />
the 3 doses is problematic since in most studies many patients were lost in follow up<br />
visits.
Cervical cancer prevention in developing countries<br />
Vivian Nassali<br />
Mentor: Annekathyrn Goodman, MD<br />
<strong>Scientific</strong> Advisors: R. Sankaranarayanan, MD and Paul D. Blumenthal, MD<br />
Massachusetts General Hospital<br />
Introduction: Cervical cancer is the second most common cancer cause of death in<br />
women in undeveloped countries. The sexually transmitted viral infection, Human<br />
Papillomavirus (HPV), has been identified as the leading etiologic agent of malignant<br />
transformation of the epithelium of the lower genital tract. Specific “high risk”<br />
genital subtypes HPV 16 and 18 are highly linked with cervical cancer. It has a long<br />
pre-invasive phase called dysplasia or squamous intraepithelial lesion (SIL) that can<br />
be detected by a pelvic exam and a Pap smear. Early intervention of pre-invasive<br />
and invasive cancer could eradicate this cancer. Other screening interventions for<br />
early detection that may fit in resource poor environments have been developed.<br />
Some of the alternative strategies include; HPV testing, and Visual Inspection with<br />
Acetic acid, (VIA), HPV vaccination. Methods: We reviewed 13 of the world’s recent<br />
literature. Search terms such as “HPV high risk” “cervical Cancer” “Developing<br />
Countries” were used in search programs. We reviewed methods that are effective,<br />
acceptable, and sensitive, cost efficient as well as rapid tests that promote screen and<br />
treat approaches in some developing areas in Africa, Thailand, rural China and India.<br />
Results: The following interventions were used: VIA, HPV DNA testing, colposcopy<br />
use, as well as HPV vaccination. A total of about 55271 women took part in<br />
these different studies, their ages ranging from 24-65 years. VIA, HPV testing, cytology<br />
and vaccination showed sensitivity ranging from 67-78%,66-100,53.4%,91.6%<br />
and specificity ranging from 48-86%, 61-96%, 93%,99.7 respectively. 99.4 % acceptability<br />
by women whom where screened by VIA, method would reduce cancer<br />
by 25-30%. HPV testing requires an expert and cytology can detect CIN, CIN2<br />
CIN3 but requires infrastructure and a lab. HPV vaccination would reduce cancer<br />
by 40%. Conclusion: The use of VIA and HPV testing was favored in most studies<br />
and successful results were attained. VIA fit the criteria of being efficient compared<br />
to cytology, affordable, sensitive and not much training required although is not very<br />
specific. Colposcopy use requires a lot of training and experience in order to get the<br />
right results. HPV vaccination is costly according to most of the countries economic<br />
status, in addition, the 3 doses is problematic since in most studies many patients<br />
were lost in follow up visits.
Massively Parallel Amplification of cDNAs<br />
Ugo Nduaguba<br />
Mentors: David E. Hill, PhD and Marc Vidal, PhD<br />
<strong>Scientific</strong> Advisors: Lila Ghamsari, Elizabeth Mello, Kourosh Salehi-Ashtiani<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Primer, cloning, and sequencing costs are major obstacles in carrying out genome<br />
wide amplification and cloning of an organism’s protein coding regions. Although<br />
the advent of “next generation” sequencing technology platforms has led to decreased<br />
cost and increased throughput of DNA sequencing, the power of these methodologies<br />
cannot be fully utilized due to the lack of PCR technologies that match the<br />
throughput at which these new sequencing platforms operate cost effectively.<br />
In situ microarray synthesis of primers provides an avenue for inexpensive synthesis of<br />
primers. However, the use of such array-synthesized primers in PCR, typically generated<br />
as a complex mixture of several thousand primers, remains problematic. One of<br />
the challenges in carrying out such complex amplification reactions is that because<br />
primers are used in pools, the concentration with respect to each specific primer<br />
pair can be considerably lower than what they would be in a conventional PCR,<br />
altering the primer hybridization kinetics significantly. In order to develop a PCR<br />
protocol capable of generating hundreds of amplicons simultaneously, we have used<br />
a set of 500 primer pairs, targeting metabolic protein coding regions of Chlamydomonas<br />
reinhardtii, to determine the required amplification parameters. To compensate<br />
for the lower primer concentration, we increase the primer pool concentration by<br />
tenfold and extend the annealing time by ~15 to 30 fold (~1,000 - 2,000 seconds)<br />
for each PCR cycle. Using these modified parameters along with reverse transcribed<br />
Chlamydomonas RNA as template; we obtain gene-specific amplification products in<br />
reactions containing the 500 primer pairs. Cloning and sequencing of the obtained<br />
products verifies correct amplification of the intended targets.
Identifying Potential HLA-A*0201-restricted,<br />
Immunogenic Epitopes from Myosin VI<br />
Osamede Obanor<br />
Mentor: Simo Arredouani, PhD<br />
<strong>Scientific</strong> Advisors: Wen Yue, MD; Bin Lu, PhD; and Martin G. Sanda, MD<br />
Beth Israel Deaconess Medical Center<br />
Background: Myosin VI previously found to be overexpressed in prostate tumors<br />
and play a role in tumorigenesis, could potentially be a target for immunotherapy<br />
geared towards prostate cancers. Hypothesis: By analyzing and testing Myosin VI’s<br />
HLA-A2.1 epitopes, novel epitopes will be identified that can elicit a cytotoxic lymphocyte<br />
immune response to prostate tumors. Preliminary data: Comprehensive<br />
in-silico analysis was conducted that identified 57 novel, human prostate cancer-restricted,<br />
tumor-associated antigens (TAA). Fifteen of these TAA, including Myosin<br />
VI, were ascertained as showing prostate cancer-associated expression by Q-RTPCR<br />
of human specimens. Aims & Methods: in-silico analysis using multiple prediction<br />
algorithms was performed in order to identify novel peptides of Myosin VI that bind<br />
to human HLA-A2.1 receptors. Potential binders were then run through an in vitro<br />
HLA-A2.1 stabilization assay to determine whether they bind to the HLA-A2.1 receptor.<br />
HLA-A2.1 transgenic (HHD) mice were injected with the 5 peptides that<br />
showed significant binding, along with a constant helper peptide to test for their<br />
immunogenicity. Spleens were harvested from the immunized mice 12 days later;<br />
splenocytes were prepared and subjected to an ELISPOT testing that determined if<br />
an immune response was elicited. Results: 10 peptides from Myosin VI were chosen<br />
to go through HLA-A2.1 stabilization assay, and 5 of the 10 showed significant binding<br />
to HLA-A2.1 receptors. When the 5 peptides were injected in transgenic mice, 2<br />
showed the ability to elicit an immune response. Conclusions: 2 Myosin VI peptides<br />
were able to bind to HLA-A2.1 receptors and elicit an immune response, making<br />
them potential targets for immunotherapy.
The Role of TPBG in Melanoma Metastasis<br />
Barbara Owens<br />
Mentor: Lawrence N. Kwong, PhD<br />
<strong>Scientific</strong> Advisor: Lynda Chin, MD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Metastasis is the spread of cancer from its primary site to other places in the body<br />
(e.g., brain, liver). These cancer cells utilize the lymphatic and blood vessels as their<br />
means of transport to distant normal organs where they grow. In the process of trying<br />
to identify genes that play a role in regulating metastasis, we tested 50 genes expected<br />
to be tumor suppressor genes (TSG). Based on preliminary data using a 96-well Boyden<br />
chamber format, 10 significantly scoring genes were selected to be further tested.<br />
I then focused on TPBG (trophoblast glycoprotein) for validation, as results from this<br />
round of testing showed that loss of TPBG enhanced invasion through matrigel by<br />
approximately 1.8 fold using mouse melanoma cells. To evaluate and validate TPBG<br />
as a TSG, we would knock down and overexpress TPBG in both mouse and human<br />
cells. Methods of testing TPBG will include additional invasion assays, overexpressing<br />
TPBG to find a suppressive effect, and use of realtime RT PCR and western blots<br />
to determine the basal level of TPBG in cell lines with known invasive properties.<br />
This will allow us to further analyze and determine the effect of TPBG on invasion in<br />
vitro. This is an interesting discovery because the role of TPBG in melanoma has not<br />
been studied previously, and knowing which genes have this effect on cancer cells will<br />
help in the diagnosis and treatment of melanoma.
Glioblastoma Multiforme and MGMT promoter Methylation<br />
Lydia Price<br />
Mentor: Clark Chen, MD, PhD<br />
<strong>Scientific</strong> Advisor: Kimberly Ng<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Glioblastoma Multiforme (GBM) is the most common type of brain cancer. While<br />
the current standard of care for GBM patients involves surgical resection followed by<br />
radiation and temozolomide (TMZ) chemotherapy, this therapeutic strategy is only<br />
palliative, and most patients with this advanced brain disease die within two years after<br />
diagnosis. By examining 24 GBM cell lines; we hoped to determine a correlation<br />
between O-6-methylguanine-DNA Methyltransferase (MGMT) promoter methylation<br />
and MGMT expression level. MGMT is a protein that allows cells to repair<br />
the damage to their DNA in a single step, hereby permitting the cells to continue<br />
proliferation. In many cases, high levels of MGMT has been linked to resistance to<br />
radiation and chemotherapy. Thus, cells that contain low levels of MGMT may be<br />
highly sensitive to these forms of treatment. The data was collected by western blot<br />
and clonogenic assay analysis. The results of these experiments are currently pending,<br />
and further information will be available following data collection.
Role of selectins in the pathogenesis of multiple myeloma<br />
Phong Quang<br />
Mentor: Irene Ghobrial, MD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute/<strong>Harvard</strong> Medical School<br />
Introduction: Multiple-Myeloma (MM) is characterized by the disseminated involvement<br />
of the bone-marrow (BM), and its progression involves a continuous circulation<br />
of the MM cells (MMCs) in the peripheral blood and homing back to the<br />
BM. Selectins are adhesion molecules involved in the primary interaction of lymphocytes<br />
with the endothelial cells (ECs) of blood vessels. In this study we studied<br />
the role selectins in the pathogenesis of MM. Methods: We have characterized the<br />
expression of E, L and P-selectins and their ligands on MM cell lines, patient sample<br />
and plasma cells from normal subjects (NPCs). We have tested the effect of blockade<br />
of each of the selectins and selectin-ligands on the interaction of MMCs with ECs.<br />
Moreover, we tested the effect of a pan selectin inhibitor (GMI-1070) on MMCs<br />
adhesion to ECs, and trans-well (through filter) and trans-endothelial SDF1-induced<br />
migration in vitro, and characterized its effect on cytoskeletal signaling induced by<br />
the interaction of MMCs and ECs. Moreover, we have tested the effect of the inhibitor<br />
on homing of MMCs to the BM in mice using in vivo flow cytometry to detect<br />
the number of circulating cells, and in vivo confocal microscopy to directly visualize<br />
the interaction. Results: All MM cell lines and patient samples had low expression<br />
of all selectins and high expression of L and P, but not E, selectin ligands. While<br />
NPCs showed low expression of all selectins and ligands. Blockade of L and P-selectin<br />
ligands reduced the interaction of MMCs with ECs in vitro, while blockade of<br />
E-selectin ligand or any of selectins did not show any effect. The pan-selectin inhibitor<br />
reduced the interaction of MMCs with ECs in vitro, did not alter their SDF1-<br />
induced migration through filter, but reduced significantly the migration through<br />
ECs. The inhibitor inhibited the activation of FAK and ERK induced by interaction<br />
of MMCs and ECs. Moreover, the selectin inhibitor extending the circulation time of<br />
MM cells in mice, and reduced the homing of MMCs. Conclusion: We found that<br />
the overexpressed P selectin ligands in MMCs play a major role in their homing to<br />
the BM. Moreover, the pan-selectin inhibitor (GMI-1070) prevented the homing of<br />
MMCs to the BM. This provides a basis for testing the effect of the inhibitor on MM<br />
tumor progression and initiation.
High-throughput Methods for Human Interactome Network Mapping<br />
Nancy Rivera<br />
Mentors: David E. Hill, PhD and Marc Vidal, PhD<br />
<strong>Scientific</strong> Advisors: Matija Dreze and Pascal Braun, PhD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Protein-protein interactions (PPI) are of central importance to the functioning of<br />
cells. Thus, studying PPI is essential to improve our understanding of basic biology,<br />
organism development and diseases. Advancements in technology have allowed researchers<br />
to progress from studying one unique PPI at a time to global investigations<br />
of hundreds to thousands of PPI at a time. These advancements will eventually lead<br />
to a better understanding of disease processes and more rapid development of therapeutics,<br />
particularly for cancer. In order to evaluate the quality of PPI datasets, we<br />
are developing a high throughput validation system based on testing each interaction<br />
pair using multiple, distinct assays having empirically determined assay sensitivities<br />
and specifities. To calibrate each of the assays with respect to their inherent false<br />
negative and false positive rates, two reference sets of interaction pairs have been<br />
assembled. The positive reference set (PRS) is comprised of 100 well-documented<br />
pairs of interacting human proteins while a random reference set (RRS) contains 100<br />
pairs in which each partner is randomly chosen from a collection of ~15,000 individual<br />
proteins. The two reference sets are then tested in all assays to establish assay<br />
parameters. Any given interaction pair from a PPI dataset is then tested in each of<br />
the distinct assays and the results are combined to derive a “confidence score” for each<br />
interaction pair. Affinity purification assay using Glutathione S-transferase (GST)<br />
pulldowns followed by western blotting has been traditionally used for confirming<br />
PPI but overall assay sensitivity and specificity has not been established. We now are<br />
defining the assay parameters for GST pull-downs by first applying it to the PRS/<br />
RRS sets. GST pull-down results for the PRS/RRS compare favorably to those seen<br />
for other assays, albeit with some interesting differences that will be discussed.
Tumor-derived Neuropilin-2 acts as a reservoir for<br />
VEGF-A and VEGF-C and increases angiogenesis and<br />
lymphangiogenesis in a breast cancer model<br />
Jeans Santana<br />
Mentor: Diane Renee Bielenberg, PhD<br />
<strong>Scientific</strong> Advisor: Meetu Seth<br />
Children’s Hospital Boston/<strong>Harvard</strong> Medical School<br />
Background: Vascular endothelial growth factor (VEGF-A), an angiogenic factor,<br />
binds to VEGF receptor-2 (VEGFR-2) and promotes the proliferation and migration<br />
of endothelial cells (EC). Neuropilins (NRP1, NRP2), co-receptors for VEGF-<br />
A, enhance VEGF activity but lack kinase activity. Neuropilin-2 (NRP2) is expressed<br />
on EC and tumor cells and binds VEGF-A and VEGF-C (lymphangiogenic protein).<br />
Tumor cells lack VEGFR-2 and therefore cannot directly signal upon VEGF binding.<br />
Our goal is to understand the contribution of tumor-derived NRP2 toward tumor<br />
progression. We hypothesize that NRP2 will act as a reservoir for VEGF-A and<br />
VEGF-C thus increasing angiogenesis and lymphangiogenesis in breast carcinoma<br />
models. Methods: Breast carcinoma cells, MCF7MFP1, were transfected with NRP2<br />
in vitro. RT-PCR, western blot, and ELISA were used to determine the expression of<br />
endogenous VEGF ligands and receptors in these breast cancer cells. Binding assays<br />
were used to determine whether NRP2 enhanced the binding of VEGF-A or VEGF-<br />
C to the tumor cells. The tumorigenicity and metastatic potential of MCF7MFP-<br />
1NRP2 and MCF7MFP1Mock were compared by injecting the cells orthotopically<br />
into immunodeficient mice. Results: Immunoblotting confirmed the overexpression<br />
of NRP2 in MCF7MFP1NRP2 cells. RT-PCR, western blot, and ELISA showed<br />
expression of VEGF-A and VEGF-C in tumor cell lysates and conditioned medias.<br />
Expected Results: It is anticipated that these studies will demonstrate that tumor<br />
cells overexpressing NRP2 are able to bind more VEGF-A and VEGF-C than untransfected<br />
cells. These results may suggest that tumors expressing NRP2 will sequester<br />
VEGF-A and VEGF-C ligands in the tumor microenvironment and stimulate<br />
(lymph)angiogenesis.
The Potential Role of Pituitary Tumor Transforming Gene 1 in<br />
Breast Cancer Development and Progression<br />
Bhaumika Shah<br />
Mentor: Towia Libermann, PhD<br />
Beth Israel Deaconess Medical Center<br />
Breast cancer is the most common cause of cancer in women and the second most<br />
common cause of cancer death in women in the U.S. While Pituitary Tumor-Transforming<br />
Gene 1 (PTTG1) has been recognized as an oncogene in the context of<br />
several types of tumors and a single nucleotide polymorphism in the PTTG1 gene<br />
has been linked to breast cancer development, no further studies into the potential<br />
role of PTTG1 in breast cancer have been pursued. Our preliminary analysis of<br />
genomic data sets link PTTG1 overexpression to recurrence and poor outcome in<br />
breast cancer patients and provide the basis for our innovative study that PTTG1<br />
is a novel breast cancer oncogene that plays an essential role in breast cancer development,<br />
progression and aggressiveness. We analyzed a variety of publicly available<br />
breast cancer microarray datasets for correlation between high expression of PTTG1<br />
and survival. Kaplan Meier curve analysis demonstrated that high PTTG1 expression<br />
strongly correlated with poor survival. The purpose of this study is to determine the<br />
potential role of PTTG1 in breast cancer development and progression as it relates to<br />
poor outcome. The potential biological relevance of the PTTG1 gene in breast cancer<br />
will be assessed by evaluating its mRNA (real time PCR) and protein expression levels<br />
(Western Blot) in breast cancer tissue and cell lines. We will also verify if PTTG1 promotes<br />
breast cancer survival or if the blockage of PTTG1 gene expression can induce<br />
cell death in breast cancer cells through RNA interference. The preliminary results<br />
display that the PTTG1 is upregulated at both mRNA and protein levels in breast<br />
cancer cell lines. For mRNA levels, about 60% of breast cancer tissue samples were<br />
upregulated from the PTTG1. There were high expression levels for both the PTTG1<br />
mRNA and protein levels in the MDA453 cell line. siRNA will be introduced into<br />
these breast cancer cell lines to verify the effect of PTTG1 blockage on breast cancer<br />
proliferation and apoptosis. We anticipate that PTTG1 overexpression is required for<br />
breast cancer progression and metastasis.
Genetic Characterization of a New Leukemia Cell Line<br />
Bethlehem Solomon<br />
Mentor: David Sweetser, MD, PhD<br />
Massachusetts General Hospital<br />
Cancer derives from sequential mutations in a cell. This is especially documented in<br />
leukemia. Our lab is studying a specific type of leukemia known as acute myeloid leukemia<br />
(AML). The most common type of AML has a balanced translocation between<br />
chromosome 8 and 21, which creates a fusion gene called AML1-ETO. Although<br />
this step creates a preleukemic state, it needs other mutations to become a full-blown<br />
leukemia. The most common additional mutation seen with AML1-ETO is a partial<br />
deletion on the long arm of chromosome 9, del(9q). Our lab has studied leukemia<br />
cells from patients with t(8;21) and del(9q). However, there currently is no cell line<br />
that grows in culture with t(8;21) and del(9q). It would be helpful to be able to study<br />
these cells in a culture to examine their biochemistry and drug sensitivity. We obtained<br />
an immortalized cell line that started with umbilical cord blood samples that<br />
had AML1-ETO introduced into them and from initial analysis appeared to have<br />
subsequently spontaneously deleted a portion of chromosome 9. Thus, the purpose<br />
of this project is to verify and precisely map the chromosomal deletion in this cell<br />
line.<br />
We hypothesize that there will be a similar del(9q) deletion and similar gene expression<br />
patterns in this cell line as compared to patient AML samples. PCR were used<br />
to allelotype this cell line to compare it to a control cell line in order to precisely map<br />
the deletion. We anticipate to map a large commonly deleted region (CDR) in these<br />
cells that compares to the CDR in the AML samples. More precise mapping and<br />
gene expression analysis by quantitative RT-PCR is also underway. We project that<br />
the outcome of this project will be validation of a new cell line that will be useful in<br />
evaluating new drugs that might be used to treat leukemia.
The Role of PTEN and SHIP1 in Efferocytosis of<br />
Apoptotic Neutrophils By Macrophages<br />
Yunwei Sun<br />
Mentors: Hongbo R. Luo, PhD<br />
<strong>Scientific</strong> Advisor: Subhanjan Mondal, PhD<br />
Children’s Hospital Boston<br />
Neutrophils are the most abundant and shortest-lived cells of the immune system<br />
Substantial daily turnover of neutrophils occurs through spontaneous apoptosis followed<br />
by clearance by macrophages. Defects in the clearance mechanism cause increased<br />
necrotic cells in circulation, which may lead to generation of self antibodies<br />
and may cause autoimmune diseases such as systemic lupus erythmatorus (SLE).<br />
Phosphatidylinositol 3-kinase (PI3K) is important for efferocytosis,the engulfment<br />
of apoptotic cells by phagocytes. Inhibition of PI3K reduces efferocytosis efficiency.<br />
Phosphatidylinositol-3,4,5-triphosphate (PtdIns(3,4,5)P3), a product of PI3K, localizes<br />
in the phagocytic cup during efferocytosis. After engulfment, PtdIns(3,4,5)P3 is<br />
converted to PtdIns(3,4)P2 by phosphatase SHIP1 or to PtdIns(4,5)P2 by PTEN.<br />
The focus of this study is to determine whether PTEN and SHIP1 localize to the<br />
phagocytic cup in macrophagesduring engulfment of neutrophils. This will lead to a<br />
greater understanding of the roles of PTEN/SHIP1 in efferocytosis.<br />
A phagocytosis assay with immunostaining was performed by labeling apoptotic<br />
neutrophils (isolated from mice) with snarf-1 and by transfecting RAW 264.7 macrophages<br />
with GFP conjugated PTEN or SHIP1. Western blots were also used to<br />
analyze PTEN and SHIP1 protein levels.<br />
It was found that PTEN is not enriched in the phagocytic cup and is globally distributed<br />
throughout macrophages. Therefore, it can be inferred that the little amount<br />
of PTEN is enough for the converting PtdIns(3,4,5)P3 to PtdIns(4,5)P2. Ship1 is<br />
found to be enriched at the phagocytic cup indicating that it is involved in the conversion<br />
of PtdIns(3,4,5)P3 to PtdIns(3,4)P2.
Optimizing HA Immunopurification Strategies Using Click Chemistry<br />
Maria N. Tomar, BS<br />
Mentor: Jarrod A. Marto, PhD<br />
<strong>Scientific</strong> Advisors: Scott B. Ficarro, PhD and Guillaume Adelmant, PhD<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Insight into many cellular processes requires an understanding of protein-protein<br />
interaction networks. These networks can be established by purification of protein<br />
complexes followed by their component analysis by mass spectrometry. Tandem affinity<br />
purification (TAP), which relies on antibodies (Abs) to affinity tags (i.e. flag and<br />
HA), is a valuable technique to purify protein complexes from cells and organisms,<br />
yielding greater purity than using only one affinity label. Although this combination<br />
has been successfully used by many laboratories, the elution from the HA Ab poses<br />
a challenge for MS based experiments due to the high concentration of HA peptide<br />
required for elution. Although protein precipitation or MWCO membranes can be<br />
used to remove HA peptide prior to MS analysis, they typically lead to sample losses<br />
and are therefore not desirable. To circumvent this problem, we are synthesizing two<br />
HA peptide analogues and their corresponding scavenger resins that should allow a<br />
quantitative removal of the HA peptide using click chemistry, an approach that exploits<br />
the fast, selective reactions that occur between azide and alkyne or phosphine<br />
functional groups. So far, alkyne and azide functionalized HA peptides have been<br />
synthesized, along with an intermediate required to produce the azide capture resin.<br />
Synthesis of other reagents is underway, and when complete, we will assess removal<br />
of HA peptide from protein extracts.
Patient-Provider Communication Regarding<br />
Self-Reported Insomnia in Cancer Care<br />
Bianca Valcarce<br />
Mentor: Donna Berry, PhD, RN, AOCN, FAAN<br />
<strong>Scientific</strong> Advisor: Barbara Halpenny, MA<br />
<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Sleep problems experienced by patients with cancer are often caused by the anxiety<br />
and stress of a cancer diagnosis, plus multiple bio-physiological factors. The disturbance<br />
in sleep patterns often develops into serious insomnia, requiring attention and<br />
intervention from the oncology provider. Insomnia has been associated with cognitive<br />
dysfunction, changes in ability to work, a decline in quality of life, as well as<br />
alterations to bodily functions. The symptom should be a concern of clinicians and<br />
should be openly and routinely communicated in cancer care. The purpose of this<br />
analysis is to illustrate the nature of the discussions between patients and their clinicians<br />
regarding patient-reported insomnia during the course of treatment. A secondary<br />
analysis of data collected in the larger Electronic Self Report Assessment- Cancer<br />
(ESRA-C) trial will be performed. In particular, patient self-report of insomnia will<br />
be evaluated and corresponding audio-recordings of clinic visits will be content-analyzed.<br />
Out of the 590 patients who had their clinic visits audio-recording during<br />
the ESRA-C study, 120 reported serious insomnia. Only 81 patients, however, had<br />
the insomnia issues discussed during the clinic visit. Content-analysis of these audio<br />
recordings is ongoing. We expect that the nature of the conversations will vary from<br />
case to case, including clinician abrupt initiation of another topic without addressing<br />
the issue of insomnia, pharmacologic and non-pharmacologic interventions.
CDK8 overexpression as a possible regulator of ß-catenin<br />
localization in colon cancer<br />
Lise Wagnac<br />
Mentor: William Hahn, MD, PhD<br />
<strong>Scientific</strong> Advisor: Xiaoxing Wang, PhD<br />
Broad Institute/<strong>Dana</strong>-<strong>Farber</strong> Cancer Institute<br />
Colon cancer is the third most common cancer in the United States and also the<br />
second leading cause of cancer deaths. Despite the vast efforts that have been made<br />
to make colon cancer more understandable, only a few molecularly targeted therapies<br />
have entered clinical practice. A lack of therapeutic approaches exist that target<br />
specific molecular pathways responsible for the development of tumors adds to the<br />
difficulty of treating colon cancer. In the case of colon cancer, aberrant activation<br />
of Wnt/ß-catenin signaling and successive up-regulation of ß-catenin transcriptional<br />
response is a critical event for its development. Upon activation of Wnt ligand/receptor<br />
complex, ß-catenin proteins become stabilized and enter the nucleus. By several<br />
research groups, it has been demonstrated that if ß-catenin is aberrantly activated,<br />
it remains in the nucleus and functions as an oncogene. Recent work has identified<br />
Cyclin-Dependent Kinase 8 (CDK8) as a regulator of ß-catenin signaling in colon<br />
cancer. However, the mechanism of regulation is not entirely clear. Since nuclear<br />
accumulation of ß-catenin is critical for its biological function, we propose to determine<br />
whether CDK8 overexpression affects ß-catenin subcellular localization. We<br />
will investigate localization of ß-catenin in colon cancer cell lines with various level<br />
of CDK8 expression using both immunofluorescence and biochemical fractionation<br />
approaches. To assess if the localization of ß-catenin is specifically a result of CDK8<br />
expression, we will introduce shRNA against CDK8 and CDK8 kinase mutants into<br />
the cells and evaluate if the ß-catenin localization is altered. We hypothesize that<br />
ß-catenin will accumulate under CDK8 overexpression and prove that CDK8 does<br />
have a correlation with ß-catenin localization. This will aid us in understanding the<br />
biology of ß-catenin in signaling pathway in colon cancer and lead to new ideas for<br />
potential cancer therapeutic targets.
Validation of an anti-Dkk1 monoclonal antibody for<br />
the treatment of bone disease in multiple myeloma<br />
Cienna Wesley<br />
Mentor: Noopur Raje, MD<br />
<strong>Scientific</strong> Advisors: Samantha Pozzi, MD and Sonia Vallet, MD<br />
Massachusetts General Hospital<br />
Multiple Myeloma (MM) is a cancer of the bone marrow caused by a proliferation of<br />
malignant plasma cells. MM plasma cells interfere with bone remodeling, acting on<br />
osteoblasts (OB) (bone producing cells) and the osteoclasts (OC) (bone resorption<br />
cells) creating an imbalance in their number and function resulting in the development<br />
of osteolytic lesions, typical of the disease. Increased serum concentration of<br />
Dkk1, an inhibitor of the Wnt pathway essential for osteoblastogenesis, has been<br />
observed in MM patients. It correlates with osteolytic lesions and inhibits the activity<br />
of OB in MM patients. It is our hypothesis that targeting this serum protein will<br />
enable us to restore bone homeostasis in MM and thus prevent bone disease. We will<br />
test this hypothesis by using a novel anti-Dkk1 monoclonal antibody with the goal<br />
of decreasing bone disease in MM.<br />
We have previously identified its effects on OB. Here I will focus on effects of anti-<br />
DKK1 on OC. OC were generated from bone marrow mononuclear cells derived<br />
from MM patients. After 2-3 weeks of culture, cells were fixed and stained for Tartrate<br />
Resistant Acid Phosphatase (TRAP) characteristic of OC and counted. Our<br />
data demonstrates a reduction of OC number in the treated samples compared with<br />
control. We will next test whether OC function is impacted as well. These experiments<br />
will highlight the effects of anti-DKK1 on the OC in MM.
Nerve Regeneration II<br />
Further Studies on the Mechanisms of Mst3b Function<br />
Sherry Wu<br />
Mentor: Nina Irwin, PhD<br />
Children’s Hospital Boston<br />
Axon outgrowth is necessary for wiring the brain during development and repairing<br />
nerve damage following injury. I have previously shown that two proteins that<br />
are each part of protein complexes and are critical for axon outgrowth, Mst3b and<br />
RGS12, bind in response to growth factors to form a large protein complex. This<br />
summer, to learn more about their roles in a signal transduction pathway leading<br />
to axon outgrowth, I will complete experiments in which RNAi and mutated proteins<br />
will be used to analyze the mechanisms by which Mst3b and RGS12 regulate<br />
outgrowth. In addition, Nina Irwin has recently shown that Mst3b can be cleaved<br />
by caspase. I will examine the effects of caspase cleavage on the activity of Mst3b in<br />
COS-7 cells by transfection with plasmids expressing wild-type, cleaved, or uncleavable<br />
Mst3b; and immunoprecipitating Mst3b from cell lysates to measure differences<br />
in kinase activity. I will study the role of caspase cleavage in the regulation of axon<br />
growth in response to growth factor by transfecting embryonic day 18 (E18) neurons<br />
with plasmids expressing wild-type, cleaved, or uncleavable Mst3b; and co-expressing<br />
Mst3b siRNA to block endogenous Mst3b expression. Interestingly, caspase cleavage<br />
removes the nuclear export signal in Mst3b, but retains the nuclear import signal.<br />
Thus, I hypothesize that cleaved Mst3b will be found in the nucleus. I will test this<br />
hypothesis by a localization assay using fluorescent microscopy of E18 neurons transfected<br />
with plasmids expressing wild-type, cleaved, or uncleavable EGFP/Mst3b. In<br />
summary, I expect that following the addition of growth factors, caspase cleavage allows<br />
nuclear localization of the Mst3b and RGS12 protein complex, which I predict<br />
to be necessary for axon outgrowth to occur.
Alumni Notable Achievements<br />
This past year a CURE student:<br />
• Completed their second year at Chicago Medical School.<br />
• Presented a scientific poster at the Annual Biomedical Research Conference for<br />
Minority Students.<br />
• Won the 2008 Annual Biomedical Research Conference for Minority Students<br />
award in Cell Biology Oral presentation.<br />
• Was a Tufts <strong>Summer</strong> Scholar.<br />
• Enrolled in the MED Prep program at UNC Chapel Hill.<br />
• Presented research at the National McNair Scholars Research Conference.<br />
• Participated in Project Success <strong>2009</strong>.<br />
• Was employed in the Vidal lab at <strong>Dana</strong>-<strong>Farber</strong> Cancer Institute.<br />
• Won the <strong>Harvard</strong> Vanguard Scholarship.<br />
• Received the Gardener’s Award for Research in Science.<br />
• Obtained a scholarship from Genzyme.<br />
• Was awarded 1st Place in the Massachusetts State Science and Engineering Fair<br />
2007 and was a finalist in the Intel International Science and Engineering Fair<br />
(ISEF) 2007.<br />
• Was inducted as a member of National Honors Society 2008.<br />
• Received the Gateway to Research Scholarship from the American Foundation<br />
for Pharmaceutical Education.<br />
• Traveled to Brazil to conduct cancer research.<br />
• Attended one of these conferences: the National Conference for Undergraduate<br />
Researchers, American Association of Cancer Research Conference, or the<br />
Biomedical Science Careers Program.<br />
• Presented a poster or an oral presentation at the New England Science<br />
Symposium.<br />
• Finished their first year at Boston Medical School.
<strong>Dana</strong>-<strong>Farber</strong>/<strong>Harvard</strong> Cancer Center’s Continuing Umbrella of Research Experiences<br />
(CURE) wishes to acknowledge and thank the CURE Advisory Committee,<br />
mentors, scientific advisors, lecturers, and supporters for expanding the academic<br />
and career horizons of our students.<br />
Many thanks to the following organizations:<br />
• Amgen<br />
• Biogen/Idec<br />
• The Friends of <strong>Dana</strong>-<strong>Farber</strong><br />
• National Cancer Institute<br />
• University of Massachusetts Bridges to Baccalaureate program<br />
• <strong>Dana</strong>-<strong>Farber</strong> Cancer Institute’s Workforce Development<br />
A special thanks to:<br />
• Tracy Callahan<br />
• Hachung Chung<br />
• Nicole Cohen<br />
• Kirsten Fertuck<br />
• Girija Goyal<br />
• Carla Hawkins<br />
• Petra Loesch<br />
• Iqbal Massodi<br />
• Narie Storer<br />
• Venus Swearingen<br />
• Michael Verzi<br />
• Janghee Woo<br />
• Adrienne Yanez
©<br />
NCI<br />
CCC<br />
DANA-FARBER/HARVARD CANCER CENTER<br />
A Comprehensive Cancer Center<br />
Designated by the National Cancer Institute