Download - American Head and Neck Society
Download - American Head and Neck Society
Download - American Head and Neck Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
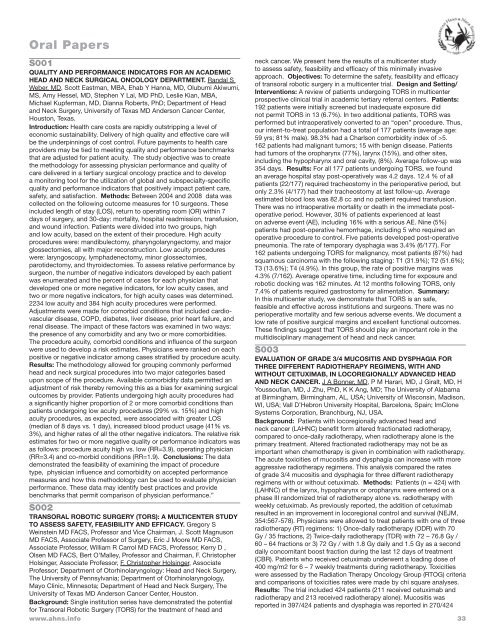
Oral Papers<br />
S001<br />
QUALITY AND PERFORMANCE INDICATORS FOR AN ACADEMIC<br />
HEAD AND NECK SURGICAL ONCOLOGY DEPARTMENT. R<strong>and</strong>al S<br />
Weber, MD, Scott Eastman, MBA, Ehab Y Hanna, MD, Olubumi Akiwumi,<br />
MS, Amy Hessel, MD, Stephen Y Lai, MD PhD, Leslie Kian, MBA,<br />
Michael Kupferman, MD, Dianna Roberts, PhD; Department of <strong>Head</strong><br />
<strong>and</strong> <strong>Neck</strong> Surgery, University of Texas MD Anderson Cancer Center,<br />
Houston, Texas.<br />
Introduction: Health care costs are rapidly outstripping a level of<br />
economic sustainability. Delivery of high quality <strong>and</strong> effective care will<br />
be the underpinnings of cost control. Future payments to health care<br />
providers may be tied to meeting quality <strong>and</strong> performance benchmarks<br />
that are adjusted for patient acuity. The study objective was to create<br />
the methodology for assessing physician performance <strong>and</strong> quality of<br />
care delivered in a tertiary surgical oncology practice <strong>and</strong> to develop<br />
a monitoring tool for the utilization of global <strong>and</strong> subspecialty-specific<br />
quality <strong>and</strong> performance indicators that positively impact patient care,<br />
safety, <strong>and</strong> satisfaction. Methods: Between 2004 <strong>and</strong> 2008 data was<br />
collected on the following outcome measures for 10 surgeons. These<br />
included length of stay (LOS), return to operating room (OR) within 7<br />
days of surgery, <strong>and</strong> 30-day: mortality, hospital readmission, transfusion,<br />
<strong>and</strong> wound infection. Patients were divided into two groups, high<br />
<strong>and</strong> low acuity, based on the extent of their procedure. High acuity<br />
procedures were: m<strong>and</strong>ibulectomy, pharyngolaryngectomy, <strong>and</strong> major<br />
glossectomies, all with major reconstruction. Low acuity procedures<br />
were: laryngoscopy, lymphadenectomy, minor glossectomies,<br />
parotidectomy, <strong>and</strong> thyroidectomies. To assess relative performance by<br />
surgeon, the number of negative indicators developed by each patient<br />
was enumerated <strong>and</strong> the percent of cases for each physician that<br />
developed one or more negative indicators, for low acuity cases, <strong>and</strong><br />
two or more negative indicators, for high acuity cases was determined.<br />
2234 low acuity <strong>and</strong> 384 high acuity procedures were performed.<br />
Adjustments were made for comorbid conditions that included cardiovascular<br />
disease, COPD, diabetes, liver disease, prior heart failure, <strong>and</strong><br />
renal disease. The impact of these factors was examined in two ways:<br />
the presence of any comorbidity <strong>and</strong> any two or more comorbidities.<br />
The procedure acuity, comorbid conditions <strong>and</strong> influence of the surgeon<br />
were used to develop a risk estimates. Physicians were ranked on each<br />
positive or negative indicator among cases stratified by procedure acuity.<br />
Results: The methodology allowed for grouping commonly performed<br />
head <strong>and</strong> neck surgical procedures into two major categories based<br />
upon scope of the procedure. Available comorbidity data permitted an<br />
adjustment of risk thereby removing this as a bias for examining surgical<br />
outcomes by provider. Patients undergoing high acuity procedures had<br />
a significantly higher proportion of 2 or more comorbid conditions than<br />
patients undergoing low acuity procedures (29% vs. 15%) <strong>and</strong> high<br />
acuity procedures, as expected, were associated with greater LOS<br />
(median of 8 days vs. 1 day), increased blood product usage (41% vs.<br />
3%), <strong>and</strong> higher rates of all the other negative indicators. The relative risk<br />
estimates for two or more negative quality or performance indicators was<br />
as follows: procedure acuity high vs. low (RR=3.9), operating physician<br />
(RR=3.4) <strong>and</strong> co-morbid conditions (RR=1.9). Conclusions: The data<br />
demonstrated the feasibility of examining the impact of procedure<br />
type, physician influence <strong>and</strong> comorbidity on accepted performance<br />
measures <strong>and</strong> how this methodology can be used to evaluate physician<br />
performance. These data may identify best practices <strong>and</strong> provide<br />
benchmarks that permit comparison of physician performance.”<br />
S002<br />
TRANSORAL ROBOTIC SURGERY (TORS): A MULTICENTER STUDY<br />
TO ASSESS SAFETY, FEASIBILITY AND EFFICACY. Gregory S<br />
Weinstein MD FACS, Professor <strong>and</strong> Vice Chairman, J. Scott Magnuson<br />
MD FACS, Associate Professor of Surgery, Eric J Moore MD FACS,<br />
Associate Professor, William R Carrol MD FACS, Professor, Kerry D ,<br />
Olsen MD FACS, Bert O’Malley, Professor <strong>and</strong> Chairman, F. Christopher<br />
Holsinger, Associate Professor, F. Christopher Holsinger, Associate<br />
Professor; Department of Otorhinolaryngology: <strong>Head</strong> <strong>and</strong> <strong>Neck</strong> Surgery,<br />
The University of Pennsylvania; Department of Otorhinolaryngology,<br />
Mayo Clinic, Minnesota; Department of <strong>Head</strong> <strong>and</strong> <strong>Neck</strong> Surgery, The<br />
University of Texas MD Anderson Cancer Center, Houston.<br />
Background: Single institution series have demonstrated the potential<br />
for Transoral Robotic Surgery (TORS) for the treatment of head <strong>and</strong><br />
www.ahns.info<br />
neck cancer. We present here the results of a multicenter study<br />
to assess safety, feasibility <strong>and</strong> efficacy of this minimally invasive<br />
approach. Objectives: To determine the safety, feasibility <strong>and</strong> efficacy<br />
of transoral robotic surgery in a multicenter trial. Design <strong>and</strong> Setting/<br />
Interventions: A review of patients undergoing TORS in multicenter<br />
prospective clinical trial in academic tertiary referral centers. Patients:<br />
192 patients were initially screened but inadequate exposure did<br />
not permit TORS in 13 (6.7%). In two additional patients, TORS was<br />
performed but intraoperatively converted to an “open” procedure. Thus,<br />
our intent-to-treat population had a total of 177 patients (average age:<br />
59 yrs; 81% male). 98.3% had a Charlson comorbidity index of >5.<br />
162 patients had malignant tumors; 15 with benign disease. Patients<br />
had tumors of the oropharynx (77%), larynx (15%), <strong>and</strong> other sites,<br />
including the hypopharynx <strong>and</strong> oral cavity, (8%). Average follow-up was<br />
354 days. Results: For all 177 patients undergoing TORS, we found<br />
an average hospital stay post-operatively was 4.2 days. 12.4 % of all<br />
patients (22/177) required tracheostomy in the perioperative period, but<br />
only 2.3% (4/177) had their tracheostomy at last follow-up. Average<br />
estimated blood loss was 82.8 cc <strong>and</strong> no patient required transfusion.<br />
There was no intraoperative mortality or death in the immediate postoperative<br />
period. However, 30% of patients experienced at least<br />
on adverse event (AE), including 16% with a serious AE. Nine (5%)<br />
patients had post-operative hemorrhage, including 5 who required an<br />
operative procedure to control. Five patients developed post-operative<br />
pneumonia. The rate of temporary dysphagia was 3.4% (6/177). For<br />
162 patients undergoing TORS for malignancy, most patients (87%) had<br />
squamous carcinoma with the following staging: T1 (31.9%); T2 (51.6%);<br />
T3 (13.6%); T4 (4.9%). In this group, the rate of positive margins was<br />
4.3% (7/162). Average operative time, including time for exposure <strong>and</strong><br />
robotic docking was 162 minutes. At 12 months following TORS, only<br />
7.4% of patients required gastrostomy for alimentation. Summary:<br />
In this multicenter study, we demonstrate that TORS is an safe,<br />
feasible <strong>and</strong> effective across institutions <strong>and</strong> surgeons. There was no<br />
perioperative mortality <strong>and</strong> few serious adverse events. We document a<br />
low rate of positive surgical margins <strong>and</strong> excellent functional outcomes.<br />
These findings suggest that TORS should play an important role in the<br />
multidisciplinary management of head <strong>and</strong> neck cancer.<br />
S003<br />
EVALUATION OF GRADE 3/4 MUCOSITIS AND DYSPHAGIA FOR<br />
THREE DIFFERENT RADIOTHERAPY REGIMENS, WITH AND<br />
WITHOUT CETUXIMAB, IN LOCOREGIONALLY ADVANCED HEAD<br />
AND NECK CANCER. J A Bonner, MD, P M Harari, MD, J Giralt, MD, H<br />
Youssoufian, MD, J Zhu, PhD, K K Ang, MD; The University of Alabama<br />
at Birmingham, Birmingham, AL, USA; University of Wisconsin, Madison,<br />
WI, USA; Vall D’Hebron University Hospital, Barcelona, Spain; ImClone<br />
Systems Corporation, Branchburg, NJ, USA.<br />
Background: Patients with locoregionally advanced head <strong>and</strong><br />
neck cancer (LAHNC) benefit form altered fractionated radiotherapy,<br />
compared to once-daily radiotherapy, when radiotherapy alone is the<br />
primary treatment. Altered fractionated radiotherapy may not be as<br />
important when chemotherapy is given in combination with radiotherapy.<br />
The acute toxicities of mucositis <strong>and</strong> dysphagia can increase with more<br />
aggressive radiotherapy regimens. This analysis compared the rates<br />
of grade 3/4 mucositis <strong>and</strong> dysphagia for three different radiotherapy<br />
regimens with or without cetuximab. Methods: Patients (n = 424) with<br />
(LAHNC) of the larynx, hypopharynx or oropharynx were entered on a<br />
phase III r<strong>and</strong>omized trial of radiotherapy alone vs. radiotherapy with<br />
weekly cetuximab. As previously reported, the addition of cetuximab<br />
resulted in an improvement in locoregional control <strong>and</strong> survival (NEJM,<br />
354:567-578). Physicians were allowed to treat patients with one of three<br />
radiotherapy (RT) regimens: 1) Once-daily radiotherapy (ODR) with 70<br />
Gy / 35 fractions, 2) Twice-daily radiotherapy (TDR) with 72 – 76.8 Gy /<br />
60 – 64 fractions or 3) 72 Gy / with 1.8 Gy daily <strong>and</strong> 1.5 Gy as a second<br />
daily concomitant boost fraction during the last 12 days of treatment<br />
(CBR). Patients who received cetuximab underwent a loading dose of<br />
400 mg/m2 for 6 – 7 weekly treatments during radiotherapy. Toxicities<br />
were assessed by the Radiation Therapy Oncology Group (RTOG) criteria<br />
<strong>and</strong> comparisons of toxicities rates were made by chi square analyses.<br />
Results: The trial included 424 patients (211 received cetuximab <strong>and</strong><br />
radiotherapy <strong>and</strong> 213 received radiotherapy alone). Mucositis was<br />
reported in 397/424 patients <strong>and</strong> dysphagia was reported in 270/424<br />
33