Painted Nails and Personal Narratives - Thompson Writing Program
Painted Nails and Personal Narratives - Thompson Writing Program
Painted Nails and Personal Narratives - Thompson Writing Program
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
54<br />
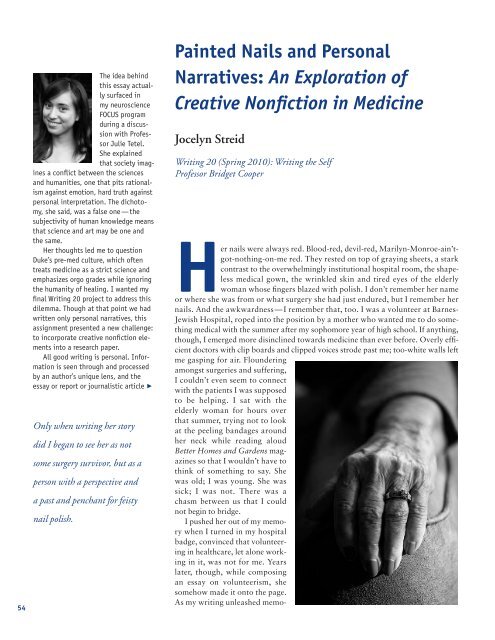
The idea behind<br />
this essay actually<br />
surfaced in<br />
my neuroscience<br />
FOCUS program<br />
during a discussion<br />
with Profes -<br />
sor Julie Tetel.<br />
She explained<br />
that society imagines<br />
a conflict between the sciences<br />
<strong>and</strong> humanities, one that pits rationalism<br />
against emotion, hard truth against<br />
personal interpretation. The dichotomy,<br />
she said, was a false one—the<br />
subjectivity of human knowledge means<br />
that science <strong>and</strong> art may be one <strong>and</strong><br />
the same.<br />
Her thoughts led me to question<br />
Duke’s pre-med culture, which often<br />
treats medicine as a strict science <strong>and</strong><br />
emphasizes orgo grades while ignoring<br />
the humanity of healing. I wanted my<br />
final <strong>Writing</strong> 20 project to address this<br />
dilemma. Though at that point we had<br />
written only personal narratives, this<br />
assignment presented a new challenge:<br />
to incorporate creative nonfiction elements<br />
into a research paper.<br />
All good writing is personal. Infor -<br />
ma tion is seen through <strong>and</strong> processed<br />
by an author’s unique lens, <strong>and</strong> the<br />
es say or report or journalistic article<br />
Only when writing her story<br />
did I began to see her as not<br />
some surgery survivor, but as a<br />
person with a perspective <strong>and</strong><br />
a past <strong>and</strong> penchant for feisty<br />
nail polish.<br />
�<br />
<strong>Painted</strong> <strong>Nails</strong> <strong>and</strong> <strong>Personal</strong><br />
<strong>Narratives</strong>: An Exploration of<br />
Creative Nonfiction in Medicine<br />
Jocelyn Streid<br />
<strong>Writing</strong> 20 (Spring 2010): <strong>Writing</strong> the Self<br />
Professor Bridget Cooper<br />
Her nails were always red. Blood-red, devil-red, Marilyn-Monroe-ain’tgot-nothing-on-me<br />
red. They rested on top of graying sheets, a stark<br />
contrast to the overwhelmingly institutional hospital room, the shapeless<br />
medical gown, the wrinkled skin <strong>and</strong> tired eyes of the elderly<br />
woman whose fingers blazed with polish. I don’t remember her name<br />
or where she was from or what surgery she had just endured, but I remember her<br />
nails. And the awkwardness — I remember that, too. I was a volunteer at Barnes-<br />
Jewish Hospital, roped into the position by a mother who wanted me to do something<br />
medical with the summer after my sophomore year of high school. If anything,<br />
though, I emerged more disinclined towards medicine than ever before. Overly efficient<br />
doctors with clip boards <strong>and</strong> clipped voices strode past me; too-white walls left<br />
me gasping for air. Floundering<br />
amongst surgeries <strong>and</strong> suffering,<br />
I couldn’t even seem to connect<br />
with the patients I was supposed<br />
to be helping. I sat with the<br />
elderly woman for hours over<br />
that summer, trying not to look<br />
at the peeling b<strong>and</strong>ages around<br />
her neck while reading aloud<br />
Better Homes <strong>and</strong> Gardens magazines<br />
so that I wouldn’t have to<br />
think of something to say. She<br />
was old; I was young. She was<br />
sick; I was not. There was a<br />
chasm between us that I could<br />
not begin to bridge.<br />
I pushed her out of my memory<br />
when I turned in my hospital<br />
badge, convinced that volunteering<br />
in healthcare, let alone working<br />
in it, was not for me. Years<br />
later, though, while composing<br />
an essay on volunteerism, she<br />
somehow made it onto the page.<br />
As my writing unleashed memo-
ies of her, something strange began to happen.<br />
I wondered if her sheets were scratchy. I<br />
imagined what she was like when she was<br />
younger. I asked myself if she felt awkward,<br />
too. I look back now on what I wrote — “she<br />
preserved her dignity by painting her nails”—<br />
<strong>and</strong> realize that only when writing her story<br />
did I began to see her as not some surgery survivor,<br />
but as a person with a perspective <strong>and</strong> a<br />
past <strong>and</strong> penchant for feisty nail polish. My<br />
words examined my response to raw emotion;<br />
through them, I learned to articulate my<br />
empathy.<br />
I wonder what would have changed if the<br />
physicians I saw—the ones more interested in<br />
sodium-potassium pumps <strong>and</strong> phospholipid<br />
bilayers than the patients themselves — took<br />
the time to write something other than a medical<br />
report. The literary arts offer an underst<strong>and</strong>ing<br />
of human experience that nothing<br />
else can; they aren’t, after all, called the<br />
humanities for nothing. At the same time, the<br />
practice of healing holds its own unique<br />
insights into human life <strong>and</strong> human death.<br />
That’s why the moment after I told my college<br />
advisor that I wanted to be a doctor, I told her<br />
that I also wanted to be an English major. I’m<br />
convinced that there’s a relationship between<br />
great literature <strong>and</strong> great medicine, <strong>and</strong> that<br />
the most important type of literature a doctor<br />
can read lies at the bottom of the literary hierarchy.<br />
Creative nonfiction — sometimes condemned<br />
as inartistic <strong>and</strong> even self-aggr<strong>and</strong>izing—cultivates<br />
exactly the kind of awareness<br />
of the self <strong>and</strong> of others that the healthcare<br />
system now lacks. As I plunge into this exploration<br />
of arts both literary <strong>and</strong> medical, I’ll<br />
examine how reading the stories of others<br />
<strong>and</strong>, in turn, telling our own, promotes selfreflection,<br />
increases our capacity for em pathy,<br />
<strong>and</strong> teaches us to listen to others in a radically<br />
different way. Then, I’ll show how this precious<br />
connection between creative nonfiction<br />
<strong>and</strong> medicine is being challenged when we<br />
need it now more than ever before.<br />
The link between the humble personal essay<br />
<strong>and</strong> the towering healthcare system seems<br />
ambitious at best, delusional at worst. Yet<br />
creative nonfiction does for doctors what traditional<br />
medical training seems to miss — it<br />
gives them permission to accept their emotions.<br />
Recognizing the pull <strong>and</strong> push of our<br />
fluctuating feelings seems simple enough, but<br />
the natural mode of human beings as emotion-laden<br />
creatures grates against the ideal<br />
exalted by the medical community. Physicians<br />
are supposed to be cool, calm, collected.<br />
There’s a reason we eat up the attitude of television’s<br />
Dr. House; he exhibits exactly the sort<br />
of composure in chaos that we crave in the<br />
doctor-stoic. Yet this ethos of professionalism<br />
has morphed into an imperative of impassivity;<br />
a doctor who cries when a patient receives<br />
a heartbreaking prognosis somehow isn’t<br />
doing their job. Dr. Suzanne Poirier of the<br />
University of Illinois explains that physicians<br />
often consider emotional distress “a weakness”<br />
<strong>and</strong> consequently “hide feelings of grief, selfdoubt,<br />
<strong>and</strong> isolation” (Shapiro 142). It’s no<br />
wonder, then, that doctors suffer depression,<br />
alcoholism, <strong>and</strong> suicide at staggeringly high<br />
rates. When a cancerous concentration of bottled-up<br />
emotions metastasizes, a physician’s<br />
mental health lies ravaged in its wake (Bar -<br />
clay 1 <strong>and</strong> Siegel 593).<br />
A possible prescription? <strong>Writing</strong> creative<br />
nonfiction. It requires doctors to reflect upon<br />
rather than repress the reality of their own<br />
struggles; when pouring their stories onto<br />
paper, they cultivate a sort of emotional<br />
awareness that forces them out of their stoic<br />
shell. The pen peels away their protective covering<br />
<strong>and</strong> there they are on the page — their<br />
selves laid bare. Those brave enough to exercise<br />
this all-encompassing honesty reap the<br />
rewards, for studies have found that physicians<br />
who practice personal writing for a mere<br />
five weeks feel less insecure <strong>and</strong> more able to<br />
cope with the immense responsibility of medicine<br />
(Nevalainen 220). It’s no large leap, then,<br />
to say that personal writing makes for a more<br />
competent physician. I don’t need a medical<br />
degree to know that better mental health<br />
leads to better performance.<br />
<strong>Writing</strong> creative nonfiction, however, functions<br />
as far more than a physician’s emotional<br />
release. Unlike pushing data in a lab or studying<br />
respiration in a class, crafting personal<br />
essays cultivates an all-too elusive quality no<br />
doctor can do without: empathy. In the medical<br />
field, the word “empathy” is a bit like<br />
“diversity”— it sounds good on paper <strong>and</strong><br />
looks great in mission statements, but nobody<br />
really knows what it means or how to get it.<br />
Confusion is underst<strong>and</strong>able; true empathy is<br />
not nearly as easy as, say, pity. As Dr. Roy<br />
Schafer explains, to empathize is to “feel yourself<br />
into the subjective experience of another”<br />
<strong>and</strong> “identi[fy] with the other” (qtd. in Das -<br />
Gupta 452). Anyone can feel sorry for a disease<br />
victim, but it takes emotional imagination<br />
to take “aspects of the other into the<br />
self” until the “boundaries of self <strong>and</strong> other<br />
are…blurred” (Ibid). Let’s be honest; all this<br />
that emerges serves as a reflection<br />
of the writer, no matter<br />
how subtly. To merge creative<br />
nonfiction <strong>and</strong> researched argumentation,<br />
I needed to display<br />
this personal element without<br />
compromising academic credibility.<br />
It’s easier said than<br />
done, of course, <strong>and</strong> I constantly<br />
caught myself either<br />
cramming in statistic after statistic<br />
or telling anecdote after<br />
anecdote. Revising was equally<br />
confusing. One paragraph<br />
would appear too me<strong>and</strong>ering<br />
<strong>and</strong> unsupported, while the<br />
next would strike me as information-dense<br />
<strong>and</strong> textbookdry.<br />
Yet while combining the<br />
worlds of research paper <strong>and</strong><br />
nonfiction narrative sometimes<br />
seemed an unnecessary hassle,<br />
I ultimately realized that this<br />
was the only way the essay<br />
could be written; I could best<br />
argue for the synthesis of personal<br />
<strong>and</strong> academic approaches<br />
to medicine by exhibiting the<br />
same fusion in my paper. In<br />
short, I needed to argue for<br />
the importance of an individual’s<br />
story by telling a narrative<br />
of my own.<br />
There’s a relationship<br />
between great literature <strong>and</strong><br />
great medicine.<br />
55
56<br />
might sound like psychoanalyst tripe irrelevant to<br />
the practice of medicine. Is it really necessary for a<br />
doctor to “blur the boundaries” between herself <strong>and</strong><br />
her patient? The answer, according to a 2002 study,<br />
is a re sounding yes; physicians with higher levels of<br />
empathy actually have higher clinical competence<br />
during their first year after medical school (Hojat et<br />
al. 524). Another study seven years later found that a<br />
physician’s empathy can actually boost a patient’s<br />
immune system, speeding his recovery over ailments<br />
as un treatable as the common cold (Study: Doc tor’s<br />
Empathy May Help). Explanations are uncertain,<br />
but it’s all too clear that doctors need more than a<br />
brilliant MCAT score if they truly wish to serve.<br />
Empathy, however,<br />
does not come naturally<br />
to everyone, <strong>and</strong> even<br />
those gifted with oodles<br />
of it may find their abil -<br />
ity to empathize worn<br />
down in the emotional<br />
hotbed of a hospital,<br />
where stoicism provides<br />
for self-preservation in<br />
the face of human tragedy.<br />
Sterile hospital halls<br />
<strong>and</strong> sterile doctor’s in -<br />
struments encourage a<br />
sterility of emotions; con -<br />
stant exposure to death<br />
<strong>and</strong> disease practically<br />
necessitates it. Physi -<br />
cians often cope with the<br />
terror of responsibility<br />
<strong>and</strong> the inevitability of<br />
failure through “de per -<br />
sonalization of the pa -<br />
tient” (Shapiro 142). Yet<br />
a doctor who distances<br />
herself from the person<br />
she’s supposed to heal is<br />
soon dulled to the reality<br />
of human suffering; if<br />
she does not constantly<br />
renew her em pathy, she<br />
risks roboticism.<br />
<strong>Writing</strong> creative nonfiction<br />
may offer a solution.<br />
Doctors who write about where they work<br />
inevi tably write about whom they treat. Once they<br />
commit the patient’s story to paper, they gain a perspective<br />
that no medical briefing sheet could afford<br />
them. Crafting a narrative, Dr. Geoffrey Hartman of<br />
Yale explains, requires a “distinctly engaged rather<br />
than detached” writer. The doctor’s meditative lens<br />
“shield[s] the patient from being considered a passive<br />
medical object” (343). This writerly perspective<br />
A doctor who distances herself from the<br />
person she’s supposed to heal is soon<br />
dulled to the reality of human suffering;<br />
if she does not constantly renew her<br />
empathy, she risks roboticism.<br />
A doctor who writes automatically<br />
humanizes whom she heals—a character<br />
in a story is not a sick case but rather an<br />
individual who happens to be sick.<br />
completely transforms the way physicians approach<br />
their patients. As one young doctor tells us, writing<br />
means that instead of simply looking for “material to<br />
do a patient write-up,” she searches “for material<br />
that move[s] [her] <strong>and</strong> ma[kes] [her] wonder”<br />
(Reichert et al. 260). The physician thus steps into<br />
the role of compassionate observer rather than<br />
detached scientist. In incorporating a patient’s narrative<br />
into her own, a doctor automatically humanizes<br />
whom she heals—a character in a story is not a sick<br />
case but rather an individual who happens to be sick.<br />
Writ ing, then, awakens a physician to an individual’s<br />
existence as not just a patient, but also a person.<br />
Furthermore, reading creative nonfiction holds<br />
a place in the medical<br />
field every bit as crucial<br />
as writing it. Those who<br />
want to develop compassion<br />
for the patient<br />
might as well crack open<br />
a book as well as pick<br />
up a pen. Recent studies<br />
have found that reading<br />
narratives actually stimulates<br />
areas of the brain<br />
associated with empathy;<br />
subjects scored hig h -<br />
er on various tests for<br />
compassion if they read<br />
a story rather than a dry<br />
text (Haley). To read a<br />
narrative, after all, is to<br />
put oneself in the position<br />
of another <strong>and</strong> ex -<br />
perience their lives on<br />
page after page after<br />
page—this sort of imag -<br />
inative unity is the very<br />
basis of empathy.<br />
Yet even if novels <strong>and</strong><br />
short stories fuel the de -<br />
velopment of a physician’s<br />
empathy, creative<br />
nonfiction supercharges<br />
it. The difference lies in<br />
the personal narrative’s<br />
claim to truth. We find<br />
ourselves drawn to reality<br />
television <strong>and</strong> Hollywood exposés because there<br />
is something strangely <strong>and</strong> uniquely magnetic about<br />
real people <strong>and</strong> real events. In fact, research has<br />
revealed that the brain processes information it perceives<br />
as true in a way fundamentally different from<br />
information perceived as fiction. When reading or<br />
listening to someone’s actual story, neurological re -<br />
gions associated with both the recollection of personal<br />
experiences <strong>and</strong> self-referential thought pro cesses
ecome automatically activated (Abraham 4).<br />
Simply put, the individual in the story seems<br />
real because she reminds one of oneself. If this<br />
merging of the self-<strong>and</strong>-other sounds distinctly<br />
like Dr. Schafer’s definition of empathy —<br />
that of “feel[ing] yourself into the subjective<br />
experience of another” — that’s because it is;<br />
hearing about real people causes us to see<br />
them as more relevant to ourselves. Their ex -<br />
periences bring to mind our experiences, <strong>and</strong><br />
together, identities intertwine. Thus, reading<br />
creative nonfiction allows a physician to practice<br />
relating foreign experiences to personal<br />
ones; it nurtures a habit of seeing the world<br />
through another’s eyes <strong>and</strong> encourages exactly<br />
the sort of empathy hospital wards need.<br />
The ability to empathize, however, is not<br />
the only otherwise elusive skill that creative<br />
nonfiction nurtures. Reading personal writing<br />
also teaches aspiring doctors what we all<br />
failed to learn in kindergarten: how to listen.<br />
According to Dr. J. Vannatta of the University<br />
of Oklahoma, doctors can find about eighty<br />
to eighty-five percent of the information necessary<br />
for diagnosis in patient narratives (qtd.<br />
in Smith 55). Yet the medical interview often<br />
acts as an interrogation; the doctor fires off a<br />
list of questions about cough frequency, sleep<br />
fluctuations <strong>and</strong> the intensity of a running<br />
nose on a scale from one to ten. Although<br />
such rapid-fire run-downs may diagnose common<br />
conditions, Dr. Rita Charon argues that<br />
more complicated conditions require a patient<br />
to tell his story in full. As Charon listens, she<br />
must “identify metaphors or images, tolerate<br />
ambiguity <strong>and</strong> uncertainty…identify the<br />
unspoken subtexts, <strong>and</strong> hear one story in light<br />
of others told by [the] teller” (Charon 4). The<br />
doctor must remain sensitive to nuances of<br />
the patient’s story that no check-mark list can<br />
capture. This sort of intense attention may<br />
sound superhuman, but quite frankly, it<br />
isn’t — English professors have taught it for<br />
years. The art of interpretation lies in the<br />
domain of literary scholars, but such exclusivity<br />
need not be the case. Charon argues that<br />
such “narrative knowledge” finds apt application<br />
in healthcare, for doctors exposed to the<br />
literary arts cultivate skills of careful reading<br />
that translate into skills of careful listening<br />
(10). Readers cannot interrupt an author in<br />
the midst of her essay, <strong>and</strong> a doctor cannot<br />
interject to ask if the pain was mild, moderate,<br />
or intense. Instead, the listener, like the<br />
reader, must wait, collect evidence, <strong>and</strong> un -<br />
derst<strong>and</strong> the patient’s story from the patient’s<br />
viewpoint, not her own.<br />
What does this sort of interaction look<br />
like? It’s not a specialized set of knowledge or<br />
a radically new mode of treatment—it’s a subtle<br />
kind of attention to detail that we already<br />
practice when we open a book. The difference,<br />
though, is that instead of reading an essay,<br />
we’re reading a patient. Dr. Charon tells us<br />
the story of a man who came into her office<br />
complaining of crippling abdominal cramps.<br />
Charon, however, looked beyond the textbook<br />
list of ailments. She noted the pressured way<br />
her patient spoke, saw the tension with which<br />
he gripped the examination table, <strong>and</strong> remembered<br />
his words when he said that he had<br />
endured the pain for a decade or so without<br />
once stepping into a hospital. These small<br />
signs signaled to Charon that her pa tient harbored<br />
a long-st<strong>and</strong>ing fear of the medical<br />
Hearing about real<br />
people causes us to see<br />
them as more relevant<br />
to ourselves.<br />
establishment—one that had compromised his<br />
health for years. With this knowledge in mind,<br />
she treated him with extra gentleness to ensure<br />
that her examination was “not an assault but<br />
an effort to help” (Charon 12). This is what listening<br />
to the patient means; by absorbing the<br />
man as a person with a past rather than as a<br />
hodgepodge of symptoms, she cared for his<br />
health—not only as it pertained to his immediate<br />
condition, but also as it related to his relationship<br />
with medicine as a whole.<br />
Careful listening, however, requires even<br />
more than picking up details <strong>and</strong> piecing<br />
57
58<br />
together plotlines, which again explains why<br />
creative nonfiction offers more to a physician<br />
than novels. Here too the key lies in creative<br />
nonfiction’s relationship to reality. An individual’s<br />
story is an account of subjective emotions<br />
<strong>and</strong> experiences, not a list of facts. The<br />
teller of the story lays a narrative framework<br />
over an ever-shifting collage of impressions<br />
An illness narrative, just<br />
like any narrative, cannot be<br />
objectively “True.” Those who<br />
read personal essays must sift<br />
through a complex portrayal of<br />
reality <strong>and</strong> underst<strong>and</strong> the author<br />
not through just what she says,<br />
but also how she says it.<br />
<strong>and</strong> ideas; there are a thous<strong>and</strong> ways to communicate<br />
the same events, the same symptoms,<br />
<strong>and</strong> each one gives a slightly different<br />
picture. By its very nature, then, an illness<br />
narrative, just like any narrative, cannot be<br />
objectively “True.” Those who read personal<br />
essays must sift through a complex portrayal<br />
of reality <strong>and</strong> underst<strong>and</strong> the author not<br />
through just what she says, but also how she<br />
says it. Reading creative nonfiction therefore<br />
uniquely equips doctors to deal with the everuncertain<br />
nature of truth in patient narratives.<br />
Both the essayist <strong>and</strong> patient present an<br />
underst<strong>and</strong>ing of their experiences subject to<br />
re-interpretation <strong>and</strong> revision; there is as<br />
much meaning in what they don’t mention as<br />
there is in what they do.<br />
Falsehoods <strong>and</strong> half-truths remain just as<br />
frustrating in the medical realm as they do in<br />
the literary one; a fair share of James Freys<br />
step into our hospitals. Yet the teenager who<br />
refuses to disclose his sexual history, the<br />
woman who lies about her alcohol usage, <strong>and</strong><br />
the man who exaggerates his symptoms to get<br />
a bottle of pills can’t be dealt with as easily as<br />
A Million Little Pieces. We can’t move their<br />
narratives from the Autobiography to the<br />
Fiction section of the bookstore <strong>and</strong> be done<br />
with them, for no matter how misleading<br />
their stories, they still need care.<br />
How, then, can a doctor provide treatment<br />
when the truth of a patient’s condition<br />
remains shifting <strong>and</strong> uncertain? Reading creative<br />
nonfiction gives otherwise floundering<br />
doctors the skills to make sense of intensely<br />
layered information, for the stories both<br />
essayists <strong>and</strong> patients tell are in themselves<br />
telling, no matter the veracity of their claims.<br />
As oral historian Aless<strong>and</strong>ro Portelli puts it,<br />
the “psychological truth” may indeed be just<br />
as important as the factual truth (qtd. in<br />
DasGupta 450). Take, for example, medical<br />
student Yo-El Ju, whose patient lied about his<br />
symptoms <strong>and</strong> downplayed his ailments.<br />
Tests revealed prostate cancer, but when Ju<br />
confronted her patient with the diagnosis, he<br />
stormed out of the hospital denying it. Had Ju<br />
considered the psychological implications of<br />
the patient’s deception, she might have sensed<br />
that fear of disease fueled his defensive denial<br />
<strong>and</strong> may have broken the news with more tact<br />
(Smith 56). Yet she had not practiced such<br />
nuanced interpretation, <strong>and</strong> a cancer victim<br />
left the hospital untreated.<br />
Ability to underst<strong>and</strong> a patient’s story —<br />
his whole story, including what he leaves<br />
unsaid—thus carries real weight in medicine.<br />
When it comes to deciphering the meaning<br />
of an illness narrative, doctors exposed to<br />
personal essays will have an advantage over<br />
those who have read only charts <strong>and</strong> spread<br />
sheets, which are understood to be purely factual,<br />
<strong>and</strong> even over those who have read only<br />
novels, which are understood to be purely fictional.<br />
So, creative nonfiction’s inherent blending<br />
of truth <strong>and</strong> artistic liberty mirrors the<br />
nature of the patient’s story.<br />
From more honest self-reflection to more<br />
genuine compassion to more nuanced listening,<br />
those in medicine st<strong>and</strong> to gain a great<br />
deal from the study <strong>and</strong> creation of personal<br />
essays. As a pre-med English major, it’s not<br />
hard to imagine why I want to argue this<br />
point—linking writing <strong>and</strong> reading to healing
justifies my undergraduate education. But before<br />
you cast me as some overly defensive bookworm, I’d<br />
like to clarify: the purpose of this essay isn’t to rationalize<br />
my choice in majors (though it’s certainly an<br />
added bonus)—it’s to change the mentality of those<br />
who assume that a doctor’s worth is measured solely<br />
in her MCAT scores <strong>and</strong> stethoscope skills.<br />
This assumption is an increasingly common<br />
one—biology <strong>and</strong> chemistry rank as the most popular<br />
majors for medical school applicants. Such an<br />
overt bias towards the sciences was not always the<br />
case; a medical school address delivered a century<br />
ago encouraged physicians-in-training to pursue<br />
studies in not only English, but also French <strong>and</strong><br />
German literature (Williams 1067). Although re -<br />
search reveals that humanities majors make just as<br />
competent — <strong>and</strong> often, as one Journal of Medical<br />
Education study found, even more competent —<br />
physicians later in their lives, the myth prevails: science<br />
people are tougher, smarter, <strong>and</strong> ultimately better<br />
doctors (Yens 434). I stepped into a pre-medical<br />
advising meeting a few months ago <strong>and</strong> found<br />
myself met with surprise. When one friend ex -<br />
claimed “But I thought you were an English major!”<br />
I slipped into my seat, ego bruised. My medical aspirations<br />
served as a secret identity; underneath the<br />
façade of the mild-mannered bookworm lay a purpose-driven<br />
pre-med. Like a Clark Kent caught<br />
changing in a telephone booth, I felt exposed whenever<br />
my two sides showed.<br />
Yet I’m not the first to draw a link between literature<br />
<strong>and</strong> medicine. Several physicians have thrived<br />
both in the ward <strong>and</strong> at the writer’s desk, including<br />
literary giants like Chekov, William Carlos Williams,<br />
Sir Arthur Conan Doyle, <strong>and</strong> even Jurassic-Park-creator<br />
Michael Crichton (Fanning 1 <strong>and</strong> Howard 82).<br />
Even so, when the number of college students studying<br />
humanities has declined by over fifty percent in<br />
four decades, it’s clear that the doctor-writer tradition,<br />
along with the study of literature itself, is in<br />
danger (Cohen). The wailings of English professors<br />
<strong>and</strong> Literature majors alike may sound familiar —<br />
bemoaning the state of one’s subject is as clichéd a<br />
part of the humanities tradition as quoting Shakes -<br />
peare or wearing sports coats with elbow patches.<br />
Yet as one professor points out, “people in the hu -<br />
manities…have never felt quite as much of a panic<br />
that their field is becoming irrelevant” as they do<br />
today (qtd. in Cohen).<br />
Irrelevance. Ay, there’s the rub. No one who wants<br />
to function at cocktail parties will accuse the works<br />
of Dostoevsky of worthlessness, but in an increasingly<br />
digitized, economized, <strong>and</strong> supersized world,<br />
it’s far too easy to see them as irrelevant. I hesitate<br />
when telling people I’m an English major — the<br />
phrase “cardboard box,” <strong>and</strong>, more specifically, the<br />
image of me living in it, springs far too easily to<br />
mind. No wonder, then, that those with doctoring<br />
dreams often see reading <strong>and</strong> writing as frivolous,<br />
even self-indulgent. The underst<strong>and</strong>ing is this: the<br />
mushy-gushy of literature is all very well <strong>and</strong> good,<br />
but when a surgeon hovers above your tumor,<br />
scalpel in h<strong>and</strong>, it doesn’t matter what books she<br />
reads. If my examination of creative nonfiction in<br />
medicine has accomplished anything, though, it<br />
proves that it does.<br />
And while many doctors may scoff at the idea<br />
that literature could improve their medical practice,<br />
learning how to read narratives might help their bottom<br />
lines. Eighty percent of those who file for malpractice<br />
point to problems caused by superficial or<br />
insufficient communication between their physicians<br />
<strong>and</strong> themselves (Hojat 522). If doctors were to<br />
adopt the perspectives of those they care for, they<br />
would leave their patients — not to mention their<br />
pocketbooks—in a far happier state.<br />
Nevertheless, in the face of ever more crippling<br />
malpractice insurance, the once-sacred <strong>and</strong> nowstrained<br />
relationship between doctor <strong>and</strong> patient has<br />
begun to crumble. Medical students without narrative<br />
empathy become doctors without narrative<br />
empathy, <strong>and</strong> their focus is on “curing, not caring”<br />
(De Moor 212). The “good doctor” is one who analyzes<br />
the symptoms, makes the biological connections,<br />
<strong>and</strong> defeats the disease; in the face of all this<br />
hard science, patients necessarily become numbers,<br />
subjects, goals. The public, then, accuses their doctors<br />
of being too distant, <strong>and</strong> doctors accuse the<br />
public of being too dem<strong>and</strong>ing. There is no easy<br />
solution; goodness knows that even the most powerful<br />
of personal essays will not fix the fact that scores<br />
of Americans receive subpar treatment, if they re -<br />
ceive it at all. A society’s healthcare — scientifically<br />
overwhelming, economically burdensome, <strong>and</strong> forever<br />
<strong>and</strong> ever evolving — may always remain a perpetually<br />
— <strong>and</strong> perhaps necessarily — frustrating<br />
beast. Still, improving medicine begins with the cultivation<br />
of a new philosophy of healing, one that<br />
sees the patient as an individual with a history, a<br />
heart, <strong>and</strong> most importantly, a story. Creative nonfiction<br />
will not solve all of our problems, but it certainly<br />
gives us a tool with which to start.<br />
This essay, then, is not simply a gr<strong>and</strong> justification<br />
of my classes, my major, or my nerdy libraryleech<br />
tendencies. It’s my own desperate attempt to<br />
awaken the medical (<strong>and</strong>, for that matter, pre-medical)<br />
community to the ability of the personal narrative<br />
to heal some of the rifts in modern medicine <strong>and</strong><br />
in turn provide for better care. Repairing the<br />
increasingly strained relationship between doctors<br />
<strong>and</strong> their patients does not begin with more innovative<br />
treatment techniques or more extensive medical<br />
research. After all, critics of physicians rarely claim<br />
that they have too little medical knowledge. Instead,<br />
59
60<br />
Medical students with-<br />
out narrative empathy<br />
become doctors without<br />
narrative empathy, <strong>and</strong><br />
their focus is on “curing,<br />
not caring.”<br />
those who distrust their doctors do so because<br />
the white coat in front of them doesn’t seem<br />
to underst<strong>and</strong> what it means to be a patient.<br />
In short, we don’t need more science in medicine—we<br />
need more humanity. This is where<br />
reading <strong>and</strong> writing creative nonfiction comes<br />
in. After all, doctors underst<strong>and</strong> individual<br />
bodies, but readers <strong>and</strong> writers underst<strong>and</strong><br />
individual consciousnesses, the souls that<br />
make us more than bags of bones <strong>and</strong> blood.<br />
Recognizing the stories of other people—real<br />
people, with painted nails <strong>and</strong> an insatiable<br />
Better Homes <strong>and</strong> Gardens obsession —<br />
encourages physicians to reflect, empathize,<br />
<strong>and</strong> listen in a way that nothing else can. I<br />
know that’s what it did for me. �<br />
Works Cited<br />
Abraham, A., <strong>and</strong> DY von Cramon. “Reality =<br />
Relevance? Insights from Spontaneous Modulations<br />
of the Brain’s Default Network when<br />
Telling Apart Reality from Fiction.” PLOS One<br />
4.3 (2009): 1-9. Print.<br />
Barclay, Laurie. “Confronting Physician<br />
Depression <strong>and</strong> Suicide: A Newsmaker Interview<br />
With Morton M. Silverman, MD.” MedScape.<br />
17 June 2003. Web. 25 Apr. 2010.<br />
Charon, Rita. “The Sources of Narrative<br />
Medicine.” Narrative Medicine: Honoring the<br />
Stories of Illness. Oxford: Oxford UP, 2006.<br />
Print.<br />
Cohen, Patricia. “In Tough Times, the Humanities<br />
Must Justify Their Worth.” The New York<br />
Times. NY Times Online, 25 Feb. 2009. Web.<br />
19 Apr. 2010.<br />
DasGupta, Sayantani. “Being John Doe<br />
Malkovich: Truth, Imagination, <strong>and</strong> Story in<br />
Medicine.”Literature <strong>and</strong> Medicine 25.2 (2006):<br />
439-462. Print.<br />
De Moor, Katrien. “The Doctor’s Role of<br />
Witness <strong>and</strong> Companion: Medical <strong>and</strong> Literary<br />
Ethics of Care in AIDS Physicians’ Memoirs.”<br />
Literature <strong>and</strong> Medicine 22.2 (2003): 208-229.<br />
Print.<br />
Fanning, Micheal. “A Doctor, Writer, <strong>and</strong> Poet.”<br />
Irish Medical Times. 29 June 2007, Lifestyle sec.<br />
Web. 19 Apr. 2010.<br />
Haley, Mick. “Socially Awkward? Hit the Books.”<br />
Globe <strong>and</strong> Mail, 10 July 2008. Web.15 Apr. 2010.<br />
Hartman, Geoffrey H. “Narrative <strong>and</strong> Beyond.”<br />
Literature <strong>and</strong> Medicine 23.2 (2004): 334-345.<br />
Print.<br />
Hojat, M., et al. “Empathy in Medical Students as<br />
Related to Academic Performance, Clinical<br />
Competence <strong>and</strong> Gender.” Medical Education<br />
36.6 (2002): 522-527. Print.<br />
Howard, Sue N. “A River of Words: The Story of<br />
William Carlos Williams.” Library Media<br />
Connections 27.5 (2009): 82. EBSCO Host.<br />
Web. 5 July 2010.<br />
Nevalainen, M.K., et al. “Facing Uncertainty as a<br />
Medical Student-A Qualitative Study of their<br />
Reflective Learning Diaries <strong>and</strong> <strong>Writing</strong>s on<br />
Specific Themes during the First Clinical Year.”<br />
Patient Education & Counseling 78.2 (2010):<br />
218-223. Print.<br />
Reichert, Julie, et al. “Narrative Medicine <strong>and</strong><br />
Emerging Clinical Practice.” Literature &<br />
Medicine 27.2 (2008)” 248-271. Print.<br />
Siegel, Bary J., <strong>and</strong> Faith T. Fitzgerald. “A Survey<br />
on the Prevalence of Alcoholism Among the<br />
Faculty <strong>and</strong> House Staff of an Academic<br />
Teaching Hospital.” Western Journal of Medicine<br />
148 (1988): 593-95. Pub Med Central. Web.<br />
24 Apr. 2010.<br />
Smith, Dinitia. “Medical <strong>Narratives</strong>: Diagnosis<br />
Goes Low Tech.” Generations 27.3 (2003):<br />
55-57. Print.<br />
Shapiro, Johanna. “Doctors in the Making:<br />
Memoirs <strong>and</strong> Medical Education.” Literature &<br />
Medicine 28.1 (2009): 138-44. Web. 25 Apr. 2010.<br />
“Study: Doctor’s Empathy May Help Cure Cold<br />
Faster.” University of Wisconsin School of<br />
Medicine <strong>and</strong> Public Health. 8 June 2009. Web.<br />
26 Apr. 2010.<br />
Williams, John. “An Introductory Address on the<br />
Training of Body <strong>and</strong> Mind for the Profession of<br />
Medicine.” The British Medical Journal, 2.2076<br />
(1900): 1065-9. Web. 25 Apr. 2010.<br />
Yens, D. P. <strong>and</strong> B. Stimmel. “Science Versus<br />
Nonscience Undergraduate Studies for Medical<br />
School—A Study of 9 Classes.” Journal of<br />
Medical Education 57.6 (1982): 429-435. Print.