Envision Newsletter - Wills Eye
Envision Newsletter - Wills Eye
Envision Newsletter - Wills Eye
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
envision<br />
w i l l S e y e C o R n e a S e R v i C e n e w S w i n t e R 2 0 1 2<br />
High Tech Teamwork Yields Amazing Recovery:<br />
Teen Injured by Fireworks Heals Thanks to <strong>Wills</strong> <strong>Eye</strong><br />
It was a hot summer day last July,<br />
and 17-year-old Ben Spair was<br />
hanging around his backyard in<br />
New Hope, Pa., playing basketball<br />
and jumping on the trampoline<br />
with his younger brother. ey<br />
could hear neighbor kids setting off<br />
firecrackers. But the firecrackers<br />
sounded kind of small and dinky,<br />
and Ben thought he could do<br />
better. He had some bigger, louder<br />
fireworks of his own. He went into<br />
the house and returned with his<br />
firecracker: a Double Impact Mine.<br />
As Ben knelt down to touch the<br />
match to the fuse, the firework<br />
exploded in his face. He fell<br />
backwards, reeling in pain.<br />
“I knew it was bad, obviously;<br />
I couldn’t see. It hurt all over my<br />
face, burning like crazy,” Ben<br />
remembered. “I heard screaming.<br />
My mother and brother had seen it<br />
all happen.” ey guided him into<br />
the house to splash his face with<br />
water and try to assess his injuries.<br />
“His eyes were completely white,<br />
no iris, no color,” his mother,<br />
Giuliana, recounted with a shudder.<br />
“His eyelids were blackened and<br />
all of his hair was blown back. His<br />
eyelashes were gone. His eyebrows<br />
were singed off.”<br />
Doctors say that a fireworks<br />
injury to the eyes can be one of<br />
the most devastating because it is<br />
both a thermal (heat) burn and a<br />
chemical burn.<br />
e family quickly went to<br />
Doylestown Hospital for medical<br />
treatment. “ey put some kind<br />
of cool liquid on my face and it<br />
felt better, but I still couldn’t see,”<br />
Ben said. “Everything was blurry<br />
and gray.”<br />
For the next few days, the family<br />
consulted a local eye doctor, but<br />
Ben’s situation was not improving.<br />
en Ben’s dad, David, noticed<br />
blood coming from his son’s eyes.<br />
“We knew Ben needed expert help.<br />
We felt we had to see whoever was<br />
the best and we knew <strong>Wills</strong> <strong>Eye</strong> is<br />
the best,” David said. e family<br />
came to the <strong>Wills</strong> <strong>Eye</strong> Emergency<br />
Room at Jefferson late on a<br />
Saturday night, and immediately<br />
the situation improved.<br />
Photo: Roger Barone<br />
So proud of her son’s wonderful recovery, Giuliana Spair (second from left) poses with<br />
her son, Ben, and Mila Heersink, M.D. (left) and Christopher Rapuano, M.D. (right).<br />
“When I first met Ben, he could<br />
barely count fingers held in front<br />
of his face,” recalled Dr. Mila<br />
Heersink, a second-year resident at<br />
<strong>Wills</strong> <strong>Eye</strong>. “He had a devastating<br />
injury. It made me mad, because he<br />
was such a young guy. I thought he<br />
would have bad vision the rest of<br />
his life. It was a terrible feeling.”<br />
“We thank God and the<br />
doctors at <strong>Wills</strong> <strong>Eye</strong>.”<br />
Dr. Heersink explained that<br />
although the eye does have great<br />
abilities to heal itself, Ben’s injury<br />
was so severe that was not<br />
possible in his case. He had a lot<br />
of scar tissue and swelling. “Left<br />
alone, his tissues would have<br />
1<br />
envision<br />
continued on page 4
Shingles Vaccination Is Vital<br />
Recently retired Director of the <strong>Wills</strong> <strong>Eye</strong> Cornea Service<br />
Dr. Elisabeth Cohen is intimately familiar with the dangerous<br />
ocular complications that can occur when an adult contracts<br />
shingles. As a doctor, she is trained to recognize the symptoms<br />
and she knows that it’s vital to seek medical treatment as quickly<br />
as possible. at knowledge may have saved her own eyesight.<br />
About three years ago, Dr. Cohen<br />
developed shingles around her<br />
eye. It ended up affecting her<br />
cornea, retina and ultimately,<br />
her vision.<br />
“I remember the day so clearly,”<br />
recalled Dr. Kristin Hammersmith,<br />
Cohen’s former partner<br />
and one of the doctors who<br />
treated her. “We were walking to<br />
the elevator and Elisabeth said she<br />
thought she had a bad mosquito<br />
bite. en we both looked at it<br />
and we knew that it wasn’t a bug<br />
bite. She had shingles and she<br />
was smart enough to start medical<br />
treatment immediately. She knew<br />
shingles could be serious.”<br />
Dr. Hammersmith explained that<br />
because Dr. Cohen identified the<br />
disease quickly – and worked in<br />
a world-renowned eye hospital–<br />
she got the fastest treatment<br />
possible. “She started taking<br />
antiviral pills an hour later. She<br />
had eye specialists treating her<br />
immediately,” Dr. Hammersmith<br />
explained. “Still, with an<br />
extraordinary level of care, she<br />
had significant vision issues due<br />
to the shingles in her eye.”<br />
Shingles generally affects only one<br />
side of the body, but can have<br />
serious consequences if it involves<br />
the trigeminal or fifth cranial<br />
nerve: the nerve responsible for<br />
sensation in the face. Dr. Cohen<br />
had shingles on her forehead and<br />
in her eye.<br />
According to the Centers for<br />
Disease Control (CDC) one<br />
out of every three people in the<br />
United States will develop<br />
shingles sometime in their life.<br />
at’s an estimated 1 million<br />
cases each year. Shingles in<br />
adults is caused by the same<br />
virus (herpes zoster) that causes<br />
chicken pox in children. If you’ve<br />
had chicken pox as a child, you<br />
may develop shingles as an adult<br />
because the virus stays inactive<br />
in the body, dormant in certain<br />
nerve cells. Doctors think that<br />
as you age, or if your immune<br />
system is weakened, the virus<br />
can reactivate, causing shingles.<br />
Because it affects nerve cells,<br />
the rash from shingles is<br />
especially painful.<br />
“It’s excruciating nerve pain,”<br />
explained cardiologist Dr. Stanley<br />
Spitzer, who said that sometimes<br />
there is pain before the rash<br />
appears on the body. “I’ve seen<br />
patients who thought they were<br />
having a heart attack, the chest<br />
pain was so intense. en, a day<br />
later, the rash broke out on their<br />
torso.” e nerve pain from<br />
shingles, called post-herpetic<br />
neuralgia, can linger for months.<br />
One of the treatments for<br />
shingles is steroids to manage<br />
2<br />
envision<br />
Dr. elisabeth Cohen<br />
Photo: Roger Barone<br />
inflammation, but steroids can<br />
lead to cataracts. “Cataracts are<br />
the clouding of the lens of the<br />
eye,” Dr. Hammersmith<br />
explained. “When you have<br />
cataracts it’s like looking through<br />
a dirty window.”<br />
During more than 50 visits to<br />
<strong>Wills</strong> <strong>Eye</strong>, Dr. Cohen was treated<br />
by Dr. Jonathan Myers, a glaucoma<br />
specialist, Dr. Joseph Maguire,<br />
a retina specialist and Drs.<br />
Hammersmith and Rapuano,<br />
cornea specialists. Unfortunately,<br />
Dr. Cohen continues to have<br />
vision issues related to her bout<br />
with shingles. She has dry eyes,<br />
corneal scarring from inflammation,<br />
some cataract clouding and<br />
retina inflammation. She had to<br />
give up practicing ophthalmology<br />
due to her vision limitations.<br />
But she has taken up the cause<br />
of educating the public to the<br />
dangers of shingles and the benefits<br />
of the vaccine.<br />
“At New York University Langone<br />
Medical Center and Bellevue<br />
Hospital in New York City, I am
doing research to increase the use of the shingles<br />
vaccine according to current national recommendations,”<br />
explained Dr. Cohen. “We’re looking at<br />
various interventions that could increase vaccination<br />
rates, including patient education, making the<br />
vaccine more readily availability in the hospital<br />
pharmacy so it can be administered by a nurse and<br />
health maintenance reminder alerts. We’re also<br />
surveying NYU primary care physicians’ knowledge<br />
and practices regarding herpes zoster and the vaccine<br />
before interventions and one year after.”<br />
Are cases of shingles on the rise? As more and more<br />
children get vaccinated for chicken pox, that disease<br />
becomes less common. Doctors think that if<br />
children don’t contract chicken pox, adults will<br />
have fewer opportunities to boost their immunity<br />
through mild exposure to the virus.<br />
According to the CDC, the risk of shingles increases<br />
as a person ages. About half of all cases occur among<br />
men and women aged 60 and older. e CDC<br />
recommends that adults ages 60 and older be<br />
vaccinated against shingles. e shingles vaccine<br />
is FDA approved for ages 50 and older, but it is<br />
often not covered by insurance until age 60.<br />
Without insurance coverage, the vaccine costs<br />
between $200 and $250 at local pharmacies.<br />
Inspired by their colleague’s experience, Drs.<br />
Rapuano and Hammersmith and the fellows of the<br />
Cornea Service gathered data from patients, trying<br />
to determine the average age of onset of shingles<br />
around the eye. eir results confirmed their<br />
suspicion: a little over half of their shingles patients<br />
were younger than age 60. Out of a total of 112<br />
patients studied, 58 were younger than age 60;<br />
54 patients were ages 60 and older. eir research<br />
is being published in Ophthalmology, in an effort<br />
to encourage physicians to recommend shingles<br />
vaccinations to adults ages 50 and older.<br />
“We want patients to ask if they are eligible for the<br />
vaccine, and doctors to strongly recommend it to<br />
immunocompetent patients, ages 50 plus, if they<br />
are willing and able to pay for it,” said Dr. Cohen.<br />
Dr. Rapuano and his colleagues encourage their<br />
patients ages 50 and older to consult their primary<br />
care physician for more information about getting<br />
the shingles vaccine.<br />
‚ FuRTHER InFoRmATIon:<br />
<strong>Wills</strong> <strong>Eye</strong> Cornea Service study on onset of shingles:<br />
http://www.ncbi.nlm.nih.gov/pubmed/21788078<br />
Centers for Disease Control information:<br />
http://www.cdc.gov/shingles/about/index.html<br />
Ten Commandments of Contact Lens Care<br />
In 1508, Leonardo da Vinci<br />
sketched drawings and<br />
calculations of a corrective lens<br />
that could be part of the eye. In<br />
the 1800s, English astronomer<br />
Sir John Herschel came up with<br />
a glass lens that would sit directly<br />
on the eye’s surface. In 1961,<br />
Dr. Otto Wichterle, a Czech<br />
chemist, used a water-absorbing<br />
plastic to produce the world’s<br />
first soft contact lenses and in<br />
1971, Bausch and Lomb began<br />
mass production of contact<br />
lenses.<br />
Today, about 34 million people<br />
in the United States wear contact<br />
lenses; and the vast majority of<br />
them do so easily and safely. But<br />
contact lenses are so common<br />
that it leads some wearers to take<br />
them for granted and get sloppy<br />
with lens cleaning and care.<br />
Doctors will tell you how<br />
quickly vision troubles and eye<br />
complications can occur, if<br />
proper contact lens usage guidelines<br />
are not carefully followed.<br />
“We see patients several times a<br />
month<br />
who have<br />
corneal<br />
ulcers from<br />
falling<br />
asleep wearing their lenses,” said<br />
Dr. Parveen Nagra. “If a speck<br />
of dirt or dust gets behind the<br />
contact lens it will irritate the<br />
cornea all night long. If you<br />
wear contacts you have to be<br />
meticulous about care and<br />
keep them clean to avoid<br />
contamination. If your lenses<br />
continued on page 5<br />
3<br />
envision
Fireworks, continued from page 1<br />
contracted, and then the eyelashes grow inward and<br />
create havoc on the surface of the eye,” Dr. Heersink<br />
said. Because a normal cornea is clear, scar tissue<br />
clouds the cornea and obstructs vision. e doctors<br />
at <strong>Wills</strong> <strong>Eye</strong> decided to use a combination of<br />
treatments with Ben and determined that vigilant<br />
monitoring of his condition would be necessary to<br />
give him the best chance to heal.<br />
“When we first saw him, he was missing most of<br />
the surface cells, the epithelium, in both his eyes,”<br />
explained Dr. Christopher Rapuano, director of the<br />
Cornea Service. “Ben was treated aggressively with a<br />
regime of several different lubricating and anti-inflammatory<br />
medications. We were concerned about<br />
damage to the cells that heal the surface of the eye,<br />
the limbal stem cells, and whether or not they would<br />
be able to recover. He also had physical damage to the<br />
eyelids and lashes.”<br />
Dr. Rapuano recalled that many attending and<br />
resident doctors at <strong>Wills</strong> were involved with Ben’s<br />
care. e doctors saw the teen on a daily basis, to<br />
constantly monitor his condition and adjust his<br />
medications accordingly. “We were all on the<br />
lookout for him,” Dr. Rapuano said. “It really<br />
took a team effort to frequently check the condition<br />
of his eyes, assessing if there was improvement and<br />
determining which medications he was responding<br />
to best. Monitoring his status and communication<br />
amongst the doctors who saw him were vital.”<br />
this is the ProKera ® ocular<br />
device that helped Ben Spair’s<br />
eyes recover. Doctors inserted<br />
them into his eyes, and the rings<br />
helped protect his corneas and<br />
allow for healing.<br />
In addition to<br />
the various<br />
medications, Ben<br />
was treated with<br />
ProKera®, a unique<br />
ocular-wound<br />
healing device<br />
made by Bio-<br />
Tissue, a tissue<br />
and medical<br />
device company.<br />
ProKera® is<br />
comprised of<br />
cryopreserved<br />
amniotic<br />
membrane, which has anti-inflammatory, antiscarring<br />
and wound-healing properties, clipped into<br />
a plastic ring. e rings were inserted into Ben’s eyes,<br />
like contact lenses, by Dr. Heersink and Cornea<br />
Service attending ophthalmologist Dr. Kristin<br />
Hammersmith. e ProKera® not only protects the<br />
eye with a moisturizing barrier but it helps maintain<br />
the normal anatomy of the eye as it heals. “Between<br />
the eyelid and the eye there is a small space. When<br />
the eye is injured and there is inflammation, that<br />
space is lost,” Dr. Rapuano explained. “In that<br />
condition, the eyelid can adhere to the eyeball and<br />
if left untreated the patient would have terrible<br />
infections and probably lose the eye.” e ProKera®<br />
ring helps maintain that open space and the normal<br />
anatomy of the eye, throughout the healing process.<br />
In the beginning, Ben had to come to <strong>Wills</strong> <strong>Eye</strong><br />
daily to have his condition monitored and get eye<br />
drops. e family traveled together, making the 80-<br />
mile round trip from New Hope to Center City.<br />
His need for round-the-clock care demanded a lot of<br />
his parents.<br />
“We’re religious, so we did a whole lot of praying,”<br />
Giuliana recalled. “We had to trust in Him and<br />
know that it would be OK. Many people were<br />
praying for Ben.” Ben’s doctors say that the family’s<br />
vigilance in taking good care of their son during his<br />
long healing process played a big part in his recovery.<br />
Giuliana kept a notebook to record her son’s various<br />
medication schedules.<br />
“We felt better when he was at <strong>Wills</strong>, than when he<br />
was home lying on the sofa,” David said. “We felt<br />
like he was in good hands at <strong>Wills</strong>.”<br />
Now, five months later, Ben’s recovery has astonished<br />
nearly everyone. His eyesight is 20/20 in his right<br />
eye and 20/25 in his left – more than good enough<br />
for him to read, do his homework and recently get<br />
his driver’s license. His eyes get tired more easily and<br />
he’s had to undergo surgery by Dr. Robert Penne,<br />
Chief of the Oculoplastics Service at <strong>Wills</strong> <strong>Eye</strong>, to<br />
correct some scarring of his eyelids. But other than<br />
that, he’s almost back to normal. He’s just like any<br />
other teenager, but he is one young man who will<br />
always be grateful for the gift of sight.<br />
“I was one of those kids who thought something like<br />
this could never happen to me,” Ben said. “Your<br />
eyesight is so important for everything you do.<br />
4<br />
envision
Your life can change in an instant. When I was lying<br />
on the sofa in the summer and couldn’t see, it was<br />
like being in prison. It’s just not worth taking a<br />
chance playing with fireworks. I’m really grateful to<br />
the many wonderful doctors who helped me and<br />
took care of me. I’m very thankful.”<br />
“It is like a miracle,” said Giuliana. “We thank God<br />
and the doctors at <strong>Wills</strong> <strong>Eye</strong>.”<br />
Even Ben’s doctors are a bit amazed at his recovery.<br />
“It’s a much better outcome than we ever could have<br />
predicted,” said Dr. Rapuano. “All of us who saw<br />
him at the beginning were very concerned that his<br />
eyesight would never return to normal. We would all<br />
say that Ben has made an amazing recovery.”<br />
Dr. Heersink said that experienced doctors say they<br />
have one or two cases in their career that they will<br />
never forget. For her, Ben is that case. “It was so<br />
gratifying to see him getting better and better every<br />
visit,” she said. “He really is a medical miracle.”<br />
Ten Commandments,<br />
continued from page 3<br />
are contaminated, you are<br />
putting those germs right in<br />
your eye.”<br />
Dr. Nagra cautioned that<br />
although some contact lenses<br />
are approved for overnight wear,<br />
wearing them overnight<br />
significantly increases the risk of<br />
infection. “Even if you practice<br />
good lens hygiene, keeping your<br />
contacts in overnight increases<br />
the possibility of contamination<br />
and I generally recommend<br />
against it,” she said.<br />
One way to avoid many of the<br />
issues with contact lens care is to<br />
use daily disposable soft lenses.<br />
is means opening up a new<br />
package of contact lenses each<br />
morning and taking them out<br />
of your eyes and throwing<br />
them in the garbage at night.<br />
Disposable lenses can be<br />
somewhat more expensive than<br />
frequent replacement lenses that<br />
must be cleaned every night,<br />
but daily disposable lenses are<br />
generally a safer option.<br />
Here are the guidelines for safe<br />
contact lens care from the<br />
American Academy of<br />
Ophthalmology:<br />
• Before handling contact<br />
lenses, wash your hands with<br />
soap and water. Rinse and dry<br />
them with a lint-free towel.<br />
• Minimize contact between<br />
your lenses and water. is<br />
means remove your lenses<br />
before swimming.<br />
• Contact lenses should not<br />
be rinsed or stored in water–<br />
not tap water, not sterile<br />
water. Only use approved<br />
contact lens solutions for<br />
contact lens care.<br />
• During cleaning, rub your<br />
contact lens with your finger,<br />
and then rinse the lenses with<br />
solution. is “rub and rinse”<br />
method is considered by some<br />
experts to be a superior way<br />
to clean contact lenses even<br />
if the solution you use is a<br />
“no rub” variety<br />
• Rinse the contact lens case<br />
with fresh solution–not<br />
water, each time. en let the<br />
empty case air dry.<br />
• Keep the contact lens case<br />
clean and replace it regularly,<br />
every three months. e case<br />
can become a source of<br />
contamination or infection<br />
if it becomes cracked,<br />
damaged or dirty.<br />
• Do not re-use solution or<br />
mix bottles of contact lens<br />
solution.<br />
• Do not transfer solution<br />
to smaller bottles.<br />
• Do not allow the tip of the<br />
bottle to touch any surface<br />
and keep the bottle tightly<br />
closed when not in use.<br />
• People who wear contact<br />
lenses need to be examined<br />
annually, even if they are<br />
not having any problems.<br />
An annual exam gives<br />
doctors a chance to check<br />
overall eye health, update<br />
prescriptions and reinforce<br />
proper lens care.<br />
5<br />
envision
MEET THE TECHS<br />
Dana Webster<br />
Putting patients at<br />
ease when they’re<br />
anxious and in pain<br />
sounds like an<br />
impossible task,<br />
but it’s the part<br />
of her job as an<br />
ophthalmic assistant<br />
that Dana Webster<br />
likes best.<br />
“<strong>Eye</strong> problems can<br />
be very painful<br />
and our patients often have to come back for many<br />
visits,” Dana said. “e waiting room is usually full<br />
of people who are anxious, nervous and often, in<br />
pain. When they’re called back to the exam room,<br />
I try to reassure them, get them to relax a bit before<br />
they see the doctor. I like to think that I can smooth<br />
the way for patients to have a meaningful office<br />
visit,” she explained.<br />
In addition to preparing patients to see the<br />
doctor, the techs’ tasks include taking medical<br />
histories and updating current health status. A tech<br />
also performs several noninvasive diagnostic tests,<br />
including corneal topography, which maps the flat<br />
and steep areas of the cornea in colors, and autorefraction,<br />
the test that measures visual acuity and<br />
helps determine prescriptions for corrective lenses.<br />
is saves the doctors valuable exam time because<br />
the pertinent data is already entered into the<br />
computer for their review.<br />
When she’s not behind the autorefractor, Dana<br />
considers herself a homebody. She enjoys lots of<br />
different crafts and watching movies with her fiveyear-old<br />
daughter, Sara, and their black labrador,<br />
Max. e family also has a pet turtle, Tuck. Dana is<br />
an accomplished cook, who concentrates on savory<br />
foods rather than the usual baked goodies. She<br />
has tried her hand at Chinese cuisine and is now<br />
tackling Indian food. “I like following the recipes<br />
and seeing how it all turns out,” Dana said, but<br />
as any parent could guess, her daughter is not an<br />
adventurous eater. “Of course she would rather have<br />
chicken nuggets and french fries for dinner every<br />
night.”<br />
Being part of a team that works to restore people’s<br />
vision is something Dana appreciates every day.<br />
“Problems with your sight can be so overwhelming,”<br />
she said. “When you can’t see clearly it affects<br />
everything you do, every part of your life. It is so<br />
exciting when we can help patients–they have<br />
cataract surgery or get a better pair of glasses and<br />
all of a sudden they can see. ey’re excited<br />
and happy. It’s gratifying to be part of that.”<br />
Meg Nace<br />
Many of the<br />
<strong>Wills</strong> <strong>Eye</strong> Cornea<br />
Service patients<br />
have complicated<br />
vision problems or<br />
ongoing eye diseases<br />
and the technicians<br />
often help them<br />
better understand<br />
their condition.<br />
“If patients<br />
understand what is<br />
happening, not only does it empower them, but it<br />
helps them to be their own advocate,” said Meg<br />
Nace. “When patients understand all the medication<br />
options and why they have to come back to the<br />
office for another visit, it helps them have a better<br />
grasp of their own healthcare. ey can be proactive.<br />
It also helps them to have productive discussions<br />
with their doctor.”<br />
Training is a hallmark of <strong>Wills</strong> <strong>Eye</strong>’s mission and<br />
the doctors routinely teach and explain medical<br />
procedures and treatment plans, not only to the<br />
6<br />
envision
esidents and fellows, but to the techs and the<br />
patients, too. At the end of the office visit, helping<br />
explain the doctor’s instructions and making sure<br />
each patient understands his medications and<br />
instructions, are aspects of the job that Meg<br />
welcomes.<br />
“I really enjoy it when I can see it all click with<br />
the patient,” she explained. “It’s important when<br />
the patient begins to understand what the<br />
ophthalmologist orders. e doctor might say,<br />
for example, ‘warm compresses,’ but then I explain<br />
in common-sense terms why warm soaks are so<br />
important for their eyes.”<br />
Meg said that she usually sits in with the patient<br />
during the doctor’s exam, so she can be part of<br />
what is discussed. “Techs help with documentation,<br />
we read the charts and clarify what the doctors<br />
want,” she said. “Some of the treatments we can<br />
offer are life-changing. It’s very uplifting to be part<br />
of that. I like to think that we are a working team,<br />
the technicians with the doctors.”<br />
Dr. Rapuano considers the Allentown native to be<br />
a vital member of his team. “We depend on the<br />
techs to teach the patients certain procedures such<br />
as how to put drops in their eyes correctly,” he said.<br />
“e patient has time to ask any questions and the<br />
techs make sure the patients understand everything<br />
before they leave the office.”<br />
Meg feels that the office staff is a very close-knit<br />
group that has strong feelings for the patients. “We<br />
see people with complicated vision problems who<br />
need to have many, many appointments with the<br />
doctors and we get to know them and their<br />
families,” she said. “When we ask about their<br />
children or how their gardens are, we really mean it<br />
because we know them. We build relationships.”<br />
Don’t Suffer Alone:<br />
Dry <strong>Eye</strong> Support Group<br />
Coming Soon<br />
For people with dry eye syndrome, every day can feel<br />
like a dusty, allergic day. the eyes burn or itch and<br />
often don’t produce sufficient tears. the pain is<br />
constant and irritation comes with every blink.<br />
“it’s like an itch that won’t go away,” says certified<br />
ophthalmic assistant Carrie larrivee, who will be<br />
facilitating a dry eye support group in the future.<br />
What is dry eye syndrome?<br />
Dry eye syndrome is a fairly common medical<br />
condition. tears are made up of three layers: lipids<br />
(oily), water, and mucus. the oily layer helps prevent<br />
evaporation of water, while the mucus helps spread<br />
tears evenly over the surface of the cornea. if the<br />
tears evaporate too quickly or do not spread, dry eye<br />
symptoms can develop. the most common form of<br />
dry eye is from an inadequate amount of water from<br />
decreased tear production. this is known as<br />
keratoconjunctivitis sicca or KCS. Problems with<br />
the lipid layer created by oil glands in the eyelids<br />
are also common and often accompany decreased<br />
tear production. these can be caused by eyelid<br />
inflammation, blepharitis.<br />
Who is at risk?<br />
Dry eye syndrome is an unfortunate side effect of<br />
common medications including antihistamines,<br />
blood pressure drugs and antidepressants. exposure<br />
to environmental irritants like smoke or air conditioning<br />
increases one’s risk, as does wearing contact lenses<br />
or having had refractive eye surgery. Dry eye syndrome<br />
affects women more than men, because the<br />
hormonal changes of pregnancy and menopause<br />
are thought to be contributing factors. increasing<br />
age is another risk factor. in some cases, the cause<br />
of dry eye syndrome is unknown.<br />
What can we do?<br />
the Cornea Service at wills is working to establish<br />
a Dry eye Support Group so KCS patients can come<br />
together for emotional support and to exchange<br />
information. it will be a chance to learn which<br />
medications have worked for others and share<br />
thoughts on everything from pain-management<br />
techniques to dietary tips for maintaining water<br />
intake. For this type of chronic condition, doctors<br />
have found that a supportive, discussion group can<br />
be helpful to patients. we are seeking philanthropic<br />
support for this initiative and will keep you updated.<br />
7<br />
envision
Cornea Service<br />
840 Walnut Street, Suite 920<br />
Philadelphia, PA 19107-5109<br />
non-profit<br />
organization<br />
U.S. poStage<br />
paid<br />
philadelphia, pa<br />
permit no. 2081<br />
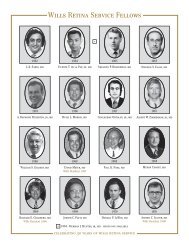
Doctors of the Cornea Service at <strong>Wills</strong> <strong>Eye</strong> Institute<br />
Photo: Jack Scully<br />
Get to know the faces behind the ophthalmoscope. Pictured are (front row<br />
from left) Parveen nagra, M.D., Kristin Hammersmith, M.D., Christopher<br />
Rapuano, M.D., Peter laibson, M.D., Brandon ayres, M.D., (back row from left)<br />
Melvin Roat, M.D., Brad Feldman, M.D., Colleen Halfpenny, M.D., Sadeer<br />
Hannush, M.D., and irving Raber, M.D.<br />
Christopher J. Rapuano, M.D.<br />
Director, Cornea Service<br />
Kristin M. Hammersmith, M.D.<br />
Director, Corneal Fellowship Program<br />
Brandon D. Ayres, M.D.<br />
Brad Feldman, M.D.<br />
Elad Feldman, M.D.<br />
Colleen Halfpenny, M.D.<br />
Sadeer Hannush, M.D.<br />
Jennifer Kim, M.D.<br />
Parveen K. Nagra, M.D.<br />
Jayrag Patel, M.D.<br />
Irving M. Raber, M.D.<br />
Melvin Roat, M.D.<br />
Sara Rapuano, Administrator,<br />
Cornea Service<br />
Ellen Scolnic, Writer<br />
Phone: 215-928-3180<br />
www.cornealdocs.com