Venous Thromboembolism Prophylaxis Policy - Royal United ...
Venous Thromboembolism Prophylaxis Policy - Royal United ...
Venous Thromboembolism Prophylaxis Policy - Royal United ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Venous</strong> <strong>Thromboembolism</strong><br />
<strong>Prophylaxis</strong><br />
Reference Number: 795<br />
Author & Title:<br />
Josephine Crowe<br />
Consultant Haematologist<br />
Responsible Director:<br />
Medical Director<br />
Review Date: 23 January 2016<br />
Ratified by:<br />
Tim Craft<br />
Medical Director<br />
Date Ratified: 24 July 2014<br />
Version: 1.3<br />
Related Policies and<br />
Guidelines:<br />
• Oral Anticoagulation Guideline<br />
• <strong>Venous</strong> <strong>Thromboembolism</strong> in Pregnancy,<br />
Labour and the Puerperium<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 1 of 57
Index:<br />
1 <strong>Policy</strong> Summary _______________________________________________ 4<br />
2 <strong>Policy</strong> Statements _____________________________________________ 4<br />
3 Definition of Terms Used _______________________________________ 5<br />
4 Duties and Responsibilities _____________________________________ 5<br />
4.1 Hospital Thrombosis Committee ____________________________________ 5<br />
4.2 Admitting doctor _________________________________________________ 5<br />
4.3 Medical, nursing or pharmacy staff on wards __________________________ 5<br />
4.4 Medical, nursing or pharmacy staff on ICU ____________________________ 5<br />
5 Risk Assessment on Admission and During Stay ___________________ 6<br />
5.1 Surgical patients and patients with trauma ____________________________ 6<br />
5.2 Regional anaesthesia ______________________________________________ 7<br />
5.3 Medical patients __________________________________________________ 7<br />
5.4 Risk factors for medical and surgical patients _________________________ 7<br />
6 Information for Patients ________________________________________ 8<br />
6.1 All patients on admission __________________________________________ 8<br />
6.2 All patients on discharge ___________________________________________ 8<br />
7 Reducing the Risk of VTE <strong>Prophylaxis</strong> ____________________________ 8<br />
7.1 General Measures ________________________________________________ 8<br />
7.2 Pharmacological prophylaxis and methods ___________________________ 9<br />
7.3 Patients already on antiplatelet agents or anticoagulation on admission or<br />
needing them for treatment ___________________________________________ 10<br />
7.4 Cautions and contraindications to pharmacological thromboprophylaxis<br />
using LMWH (Dalteparin) and Rivaroxaban ______________________________ 10<br />
7.5 Mechanical thromboprophylaxis ___________________________________ 11<br />
7.6 Vena Caval Filters _______________________________________________ 13<br />
8 Procedure if <strong>Venous</strong> <strong>Thromboembolism</strong> is Suspected ______________ 13<br />
9 Hospital Acquired Thrombosis (HAT) ____________________________ 14<br />
10 Monitoring Compliance ________________________________________ 14<br />
11 Review _____________________________________________________ 14<br />
12 Training _____________________________________________________ 14<br />
References ______________________________________________________ 15<br />
Appendix 1: Guideline for the Prevention of <strong>Venous</strong> <strong>Thromboembolism</strong> in<br />
Adults ___________________________________________________ 17<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 2 of 57
Appendix 2: General Medicine Thromboprophylaxis Guideline __________ 19<br />
Appendix 2a: Stroke Thromboprophylaxis Guideline _________________ 20<br />
Appendix 2b: Palliative Care Thromboprophylaxis Guideline _____________ 22<br />
Appendix 2c:<br />
Cancer and Central Catheters Thromboprophylaxis Guideline<br />
__________________________________________________ 24<br />
Appendix 3: Pregnancy and up to 6 weeks Postpartum Thromboprophylaxis<br />
Guideline ___________________________________________________ 26<br />
Appendix 4: General Surgical Thromboprophylaxis Guideline __________ 30<br />
Appendix 4a: Vascular, Gastrointestinal, Gynaecological and Urological<br />
Surgery Thromboprophylaxis Guideline ______________________________ 33<br />
Appendix 4b: Day Surgery Thromboprophylaxis Guideline ____________ 36<br />
Appendix 5: Trauma and Orthopaedic Thromboprophylaxis Guideline _____ 38<br />
Appendix 5a: Trauma and Orthopaedic Procedure Specific<br />
Thromboprophylaxis Guideline _____________________________________ 44<br />
Appendix 5b: Trauma and Orthopaedic Major Trauma and Spinal Injury<br />
Thromboprophylaxis Guideline _____________________________________ 49<br />
Appendix 5c: Trauma and Orthopaedic Lower Limb Plaster Casts<br />
Thromboprophylaxis Guideline _____________________________________ 51<br />
Appendix 6: Critical Care Thromboprophylaxis Guideline ________________ 53<br />
Document Control Information ______________________________________ 55<br />
Ratification Assurance Statement _____________________________________ 55<br />
Consultation Schedule _______________________________________________ 56<br />
Equality Impact: (A) Assessment Screening ____________________________ 57<br />
Amendment History<br />
Issue Status Date Reason for Change Authorised<br />
1.2 Approved 17/01/2013 Recording of VTE<br />
Dr Tim Craft<br />
assessment; update<br />
reference to trust drug chart<br />
and Millennium update format<br />
1.3 Approved 24/07/2014 Align with the NICE<br />
recommendations CG92<br />
Dr Tim Craft<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 3 of 57
1 <strong>Policy</strong> Summary<br />
A significant number of people die each year as a result of hospital acquired venous<br />
thromboembolism (VTE). Many of these deaths are preventable through the use of<br />
thromboprophylaxis. The House of Commons Select Committee Report on the<br />
Prevention of <strong>Venous</strong> <strong>Thromboembolism</strong> in Hospitalised Patients Feb 2005 and The<br />
<strong>Venous</strong> <strong>Thromboembolism</strong> in Hospitalised Patients Expert Working Group have been<br />
tasked with addressing this issue. NICE Clinical Guideline 92 – “Reducing the risk of<br />
venous thromboembolism (deep vein thrombosis and pulmonary embolism) in<br />
patients admitted to hospital” January 2010, gives clear guidance regarding national<br />
standards.<br />
Patients with cancer have an approximate 7 fold increased risk of VTE, accounting<br />
for ~20% of the community presenting VTE. Cancer patients undergoing surgery<br />
have a two-fold or greater increased risk for fatal PE compared with those without<br />
cancer who are undergoing similar procedures. Patients with active cancer and<br />
particularly those with central venous lines and those receiving chemotherapy are at<br />
a significantly increased risk for VTE. In-patients with cancer must be managed<br />
according to the medical, surgical or critical care guidelines as appropriate.<br />
The appropriate use of thromboprophylaxis will:<br />
• Reduce morbidity due to VTE<br />
• Reduce mortality rates due to VTE<br />
• Reduce the cost of treatment of VTE<br />
This policy summarises best practice based on current evidence for the prevention of<br />
Hospital acquired VTE.<br />
2 <strong>Policy</strong> Statements<br />
• All inpatients must have their risk of developing VTE assessed on admission<br />
using the risk assessment tool on one of the Trust Medicines Administration<br />
Records.<br />
• All patients must have this risk assessment reviewed within 24 hours of<br />
admission and when clinical condition changes<br />
• If risk of VTE is identified and prophylaxis withheld, the reason(s) for this must<br />
be documented clearly<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 4 of 57
3 Definition of Terms Used<br />
AES<br />
DH<br />
DVT<br />
FID<br />
HAT<br />
ICE<br />
IPC<br />
LMWH<br />
NOAC<br />
PE<br />
UFH<br />
VTE<br />
Anti-Embolic Stockings<br />
Department of Health<br />
Deep Vein Thrombosis<br />
Foot Impulse Devices<br />
Hospital Acquired Thrombosis<br />
Integrated Clinical Environment<br />
Intermittent Pneumatic Compression<br />
Low Molecular Weight Heparin<br />
Novel oral anticoagulant<br />
Pulmonary Embolism<br />
Unfractionated heparin<br />
<strong>Venous</strong> <strong>Thromboembolism</strong><br />
4 Duties and Responsibilities<br />
4.1 Hospital Thrombosis Committee<br />
This comprises representatives from Medicine, Surgery, Obstetrics & Maternity,<br />
Orthopaedics, Pharmacy, Haematology and Oncology. The Committee will:<br />
• Promote best practice through local policies based on National<br />
Guidelines<br />
• Lead multi professional audit of the use of thromboprophylaxis<br />
• Promote education and training<br />
• Report quarterly to the Operational Governance Committee.<br />
4.2 Admitting doctor<br />
Responsible for completing and documenting the risk assessment and prescribing<br />
prophylaxis if indicated. Decision not to prescribe pharmaceutical prophylaxis must<br />
be documented and alternative mechanical prophylaxis recommended.<br />
4.3 Medical, nursing or pharmacy staff on wards<br />
Responsible for prescribing, checking and administering thromboprophylaxis and<br />
ensuring risk assessments are repeated by the medical staff at 24 hours and<br />
reviewed whenever the clinical situation changes.<br />
4.4 Medical, nursing or pharmacy staff on ICU<br />
Responsible for ensuring risk assessments are repeated every 24 hours and<br />
documented on medication chart.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 5 of 57
5 Risk Assessment on Admission and During Stay<br />
• All patients must have their risk of developing VTE assessed on admission<br />
and have this assessment reviewed within 24 hours of admission and if their<br />
clinical condition changes, using the risk assessment tool which is on the<br />
Trust Medicines Administration chart.<br />
• Inpatients must be re-assessed for risk factors at 24 hours post<br />
admission and then when clinically indicated (every 24 hours for<br />
ICU patients).<br />
• If VTE prophylaxis is withheld for any reason (e.g. bleeding risk) this<br />
must be documented clearly and alternative methods of prophylaxis<br />
prescribed.<br />
• The admitting doctor is responsible for completing the risk assessment and<br />
prescribing thromboprophylaxis. For elective patients, the risk assessment<br />
must be completed on admission, and the post-operative plan for VTE<br />
prophylaxis must be recorded in the operation note either within the health<br />
record, or on Millennium.<br />
• Extended thromboprophylaxis with low molecular weight heparin or<br />
rivaroxaban is recommended in patients with:<br />
• Elective total hip arthroplasty<br />
• Elective knee arthroplasty<br />
• Fractured neck of femur<br />
• Major cancer surgery in the abdomen or pelvis<br />
NB: It may be necessary to consider this treatment for other high risk patient<br />
groups.<br />
5.1 Surgical patients and patients with trauma<br />
Surgical patients and patients with trauma are regarded as being at increased risk of<br />
VTE if they meet one of the following criteria:<br />
• Surgical procedure with a total anaesthetic and surgical time of more than<br />
90 minutes, or 60 minutes if the surgery involves the pelvis or lower limb<br />
• Acute surgical admission with inflammatory or intra-abdominal condition<br />
• Expected significant reduction in mobility<br />
• One or more of the risk factors shown below (5.4)<br />
Surgical patients must be informed that immobility associated with continuous travel<br />
of more than 3 hours in the 4 weeks before or after surgery may increase the risk of<br />
VTE.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 6 of 57
Surgical patients on the combined oral contraceptive pill should be advised to<br />
consider stopping 4 weeks before elective surgery. Alternative contraceptive<br />
measures should be advised.<br />
Inpatients must be re-assessed for risk factors at 24 hours post admission and then<br />
when clinically indicated (every 24 hours for ICU patients).<br />
5.2 Regional anaesthesia<br />
Regional anaesthesia reduces the risk of VTE compared to general anaesthesia.<br />
The suitability of regional anaesthesia for an individual patient should be considered,<br />
in addition to any other planned method of thromboprophylaxis. If regional<br />
anaesthesia is used, the timing of the thromboprophylaxis must be planned to<br />
minimise the risk of epidural haematoma. If antiplatelet or anticoagulant agents are<br />
being used or planned, refer to the Trust guideline for guidance about safety and<br />
timing of these agents in relation to regional anaesthesia. Pharmacological or<br />
mechanical VTE prophylaxis must not be routinely offered to patients having surgery<br />
with local anaesthesia by local infiltration with no limitation of mobility.<br />
5.3 Medical patients<br />
Medical patients are regarded as being at increased risk of VTE if they<br />
• (a) Have had or are expected to have significantly reduced mobility for 3 days or<br />
more<br />
OR<br />
• (b) Are expected to have on-going reduced mobility relative to their normal state<br />
AND<br />
• Have one or more of the risk factors below<br />
5.4 Risk factors for medical and surgical patients<br />
• Active cancer or cancer treatment<br />
• Age over 60 years<br />
• Critical care admission<br />
• Dehydration<br />
• Known thrombophilia<br />
• BMI > 30 kg/m 2<br />
• Personal or first-degree relative history of VTE<br />
• One or more significant medical comorbidities (heart disease; metabolic,<br />
endocrine or respiratory pathologies; acute infectious diseases; inflammatory<br />
conditions)<br />
• HRT or oestrogen-containing contraceptive<br />
• Varicose veins with phlebitis<br />
• Pregnant or given birth within last 6 weeks<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 7 of 57
6 Information for Patients<br />
6.1 All patients on admission<br />
All patients must be given verbal and written information on admission about the<br />
risks and possible consequences of VTE, the effectiveness and possible side effects<br />
of prophylaxis and how they can reduce the risk of VTE.<br />
Since heparin is derived from animal products, consider offering synthetic<br />
alternatives to patients who have concerns about its use.<br />
6.2 All patients on discharge<br />
All patients, and their families and carers if appropriate, must be given verbal<br />
and written information on the following, as part of their discharge plan:<br />
• The signs and symptoms of DVT / PE<br />
• The correct use of extended prophylaxis (if appropriate).<br />
• The implications of not using prophylaxis (if appropriate).<br />
• The importance of seeking medical help and who to contact if deep<br />
vein thrombosis or pulmonary embolism is suspected.<br />
If discharged with prophylaxis:<br />
• The signs and symptoms of adverse events related to VTE prophylaxis<br />
• The importance of seeking help and who to contact if they have any<br />
problems using the prophylaxis<br />
7 Reducing the Risk of VTE <strong>Prophylaxis</strong><br />
7.1 General Measures<br />
Early mobilisation and leg exercises<br />
• Patients will be encouraged to mobilise as soon as possible.<br />
• Patients who are unable to mobilise will be encouraged to do regular leg<br />
exercises.<br />
Hydration<br />
• Ensure patients are adequately hydrated.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 8 of 57
7.2 Pharmacological prophylaxis and methods<br />
The choice of pharmacological thromboprophylaxis is based on local polices, clinical<br />
condition (for example) and patient preference<br />
I: Dalteparin - Low Molecular Weight Heparin (LMWH)<br />
Weight (kg)<br />
150 kg<br />
Dose<br />
2500 units SC once daily<br />
5000 units SC once daily<br />
5000 units SC twice daily<br />
7500 units SC twice daily<br />
Renal Impairment: eGFR50%. Always<br />
discuss management of these patients with a Consultant Haematologist<br />
• Osteoporosis – Heparins are associated with an increased risk of osteoporosis<br />
and bone fracture with prolonged use (>12 weeks at prophylactic doses). This<br />
risk is greater in pregnancy and older women.<br />
II: Rivaroxaban<br />
Licensed in elective hip or knee replacement. See Orthopaedic Appendices<br />
III: Anti-platelet agents<br />
Aspirin is NOT recommended as prophylaxis against VTE in any patient group.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 9 of 57
7.3 Patients already on antiplatelet agents or<br />
anticoagulation on admission or needing them for<br />
treatment<br />
• Consider offering additional mechanical or pharmacological VTE prophylaxis<br />
to patients who are having antiplatelet agents to treat other conditions and<br />
who are assessed to be at increased risk of VTE. Take into account the risk of<br />
bleeding and of comorbidities such as arterial thrombosis<br />
o If the risk of VTE outweighs the risk of bleeding, consider offering<br />
pharmacological VTE prophylaxis according to the reason for<br />
admission<br />
o If the risk of bleeding outweighs the risk of VTE, offer mechanical VTE<br />
prophylaxis<br />
• Do not offer additional pharmacological or mechanical VTE prophylaxis to<br />
patients who are taking novel oral anticoagulants (dabigatran, rivaroxaban,<br />
apixaban), or vitamin K antagonists (warfarin, phenindione) and who are<br />
within their therapeutic range, providing anticoagulant therapy is continued<br />
• Do not offer additional pharmacological or mechanical VTE prophylaxis to<br />
patients who are having treatment dose parenteral anticoagulant therapy (for<br />
example, fondaparinux, LMWH or UFH)<br />
7.4 Cautions and contraindications to pharmacological<br />
thromboprophylaxis using LMWH (Dalteparin) and<br />
Rivaroxaban<br />
This list is not exhaustive. Consider other factors in an individual patient.<br />
• Active bleeding<br />
• Acquired bleeding disorders (e.g. acute liver failure)<br />
• Concurrent use of anticoagulants known to increase bleeding risk (e.g. warfarin<br />
with INR >2)<br />
• Lumbar puncture / epidural / spinal anaesthesia within the previous 4 hours or<br />
expected within the next 12 hours<br />
• Acute stroke<br />
• Thrombocytopenia (platelets < 75 x 10 9 /L)<br />
• Uncontrolled systolic hypertension (BP ≥ 230/120 mmHg)<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 10 of 57
• Untreated inherited bleeding disorders (e.g. haemophilia or von Willebrand’s<br />
disease)<br />
• Surgery expected within the next 12-24 hours<br />
• Surgery in the past 48 hours +/- risk of clinically important bleeding<br />
• Hypersensitivity to heparin or low molecular weight heparins<br />
• History of heparin induced thrombocytopenia<br />
• Neurosurgery, spinal, eye surgery or other procedure with high bleeding risk<br />
• Renal failure<br />
o rivaroxaban: contraindicated if eGFR < 15mls/min (use<br />
unfractionated heparin 5,000 units sc twice daily)<br />
o dalteparin: contraindicated if eGFR
• Remove anti-embolism stockings daily for hygiene purposes and to inspect skin<br />
condition. In patients with a significant reduction in mobility, poor skin integrity or<br />
any sensory loss, inspect the skin two or three times per day, particularly over<br />
the heels and bony prominences<br />
Discontinue the use of anti-embolism stockings if there is marking, blistering or<br />
discolouration of the skin, particularly over the heels and bony prominences, or if<br />
the patient experiences pain or discomfort. If suitable, offer a foot impulse or<br />
intermittent pneumatic compression device as an alternative.<br />
Intermittent pneumatic compression devices (IPC), foot impulse devices (FID)<br />
or venous foot pumps<br />
• May be used as alternatives or in addition to anti-embolism stockings where<br />
appropriate in surgical inpatients<br />
• Do not offer foot impulse or intermittent pneumatic compression devices to<br />
patients with a known allergy to the material of manufacture<br />
• Encourage patients on the ward who have foot impulse or intermittent pneumatic<br />
compression devices to use them for as much of the time as is possible and<br />
practical, both when in bed and when sitting in a chair.<br />
Contraindications to mechanical prophylaxis<br />
• Suspected or proven peripheral arterial disease<br />
• Peripheral arterial bypass grafting<br />
• Peripheral neuropathy or other causes of sensory impairment<br />
• Local condition in which stockings may cause damage e.g. fragile tissue paper<br />
skin, leg ulcers, dermatitis, gangrene or recent skin graft<br />
• Known allergy to material of manufacture<br />
• Cardiac failure<br />
• Massive leg oedema<br />
• Pulmonary oedema from congestive cardiac failure<br />
• Unusual leg shape or size<br />
• Major limb deformity preventing correct fit<br />
Leg or foot ulcers or wounds; use caution or clinical judgement<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 12 of 57
Intermittent pneumatic compression devices and foot impulse devices<br />
contraindications<br />
• Known allergy to material of manufacture<br />
• Known or suspected acute DVT or PE<br />
• Peripheral arterial disease<br />
• Local skin condition precluding application<br />
• Severe congestive cardiac failure<br />
• Do not apply if the legs are elevated during surgery<br />
• Pre-existing thrombophlebitis, DVT or PE<br />
• Use cautiously on an infected or insensate extremity<br />
7.6 Vena Caval Filters<br />
These must be considered for surgical patients with recent (within 1 month) or<br />
existing VTE, or who have an active malignancy and in whom mechanical<br />
prophylaxis and anticoagulation is contraindicated.<br />
8 Procedure if <strong>Venous</strong> <strong>Thromboembolism</strong> is Suspected<br />
If an inpatient already receiving thromboprophylaxis is suspected to have a DVT or<br />
PE they must be treated with a therapeutic dose of LMWH and have the<br />
appropriate radiological investigations.<br />
Refer to Acute Medicine Guidelines:<br />
Pulmonary Embolism (ACUTE 034/2014),<br />
Deep venous thrombosis (DVT) (ACUTE 027/2014)<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 13 of 57
9 Hospital Acquired Thrombosis (HAT)<br />
A hospital acquired thrombosis (DVT or PE) is defined as being a DVT or PE which<br />
has occurred within 3 months of a hospital admission.<br />
The data on these patients is collected by BIU from the diagnostic scans reported on<br />
the ICE system and the community DVT Doppler service commissioned by BANES.<br />
This information is reviewed and those incidents that are identified as possible HATs<br />
are reported on the Trust incident reporting system, Datix.<br />
A Root Cause Analysis (RCA) investigation must be completed by the patient’s<br />
initial Consultant on all patients who are suspected of having a HAT. HATs and<br />
the RCA findings must be reported to the Hospital Thrombosis Committee for<br />
review, assessment of trends across the Trust and the identification of learning<br />
and actions required to reduce identified risks.<br />
10 Monitoring Compliance<br />
The Trust-wide audit of VTE prophylaxis is mandatory.<br />
Audit data on completion of risk assessment on patients admitted to hospital<br />
is collected and reported to Trust Board every month.<br />
A review of risk assessment compliance and findings is also monitored as part of<br />
the Trust Patient Safety Improvement Programme and is reported within the Trust.<br />
11 Review<br />
This policy will be subject to a planned review every three years as part of the Trust’s<br />
<strong>Policy</strong> Review Process. It is recognised however that there may be updates required<br />
in the interim arising from amendments or release of new regulations, Codes of<br />
Practice or statutory provisions or guidance from the Department of Health or<br />
professional bodies. These updates will be made as soon as practicable to reflect<br />
and inform the Trust’s revised policy and practise.<br />
12 Training<br />
Managers are responsible for ensuring all their staff receive the type of initial and<br />
refresher training that is commensurate with their role(s).<br />
Staff must refer to the Mandatory Training Profiles available on the intranet, to<br />
identify what training in relation to venous thromboembolism prophylaxis is relevant<br />
for their role and the required frequency of update. Further information is available<br />
on the statutory and mandatory training web pages about each subject and the<br />
available training opportunities.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 14 of 57
References<br />
1. Scottish Intercollegiate Guidelines Network (SIGN), Prevention and<br />
Management of <strong>Venous</strong> <strong>Thromboembolism</strong>. 122. Dec 2010<br />
2. Report of the independent expert working group on the prevention of<br />
venous thromboembolism in hospitalised patients. Department of Health, A<br />
report to Sir Liam Donaldson, Chief Medical Officer. 2007<br />
3. Government Response to the House of Commons Health Committee<br />
report on the prevention of venous thromboembolism in Hospitalised<br />
Patients – second report of session 2004-5. July 2005.<br />
4. Collins R, Baigent C, Sandercock P, Peto RO. Antiplatelet therapy for<br />
thromboprophylaxis: the need for careful consideration of the evidence<br />
from randomised trials. Antiplatelet trialists collaboration. BMJ 1994;<br />
309; 1215-7<br />
5. NICE Clinical Guideline 92 <strong>Venous</strong> thromboembolism: reducing the risk.<br />
Reducing the risk of venous thromboembolism (deep vein thrombosis and<br />
pulmonary embolism) in patients admitted to hospital. January 2010<br />
6. All-party parliamentary thrombosis group Thrombosis: Awareness,<br />
Management and Prevention November 2007<br />
7. Kakkar AK, Coleman R et al. Prevention and Treatment of Cancer-Associated<br />
Thrombosis: A Report on a Roundtable Meeting. British Journal of Cancer vol<br />
102, supplement 1, 13 April 2010<br />
8. Haemostasis, Anticoagulation & Thrombosis (HAT) Committee, UK<br />
Clinical Pharmacy Association. UKMi Medicines Q&A 326.1: What<br />
doses of thromboprophylaxis are appropriate for adult patients at<br />
extremes of body weight? April 2010. Available from www.nelm.nhs.uk,<br />
date accessed: 21 st February, 2011.<br />
9. Templeman, E. UKMi Medicines Q&A 257.2: Should prophylactic doses of<br />
low molecular weight heparins be used in patients with renal impairment?<br />
July 2010. Available from www.nelm.nhs.uk, date accessed: 21 st February,<br />
2011.<br />
10. Ashley, C and Currie, A. Renal Drug Handbook 3 rd Edition. Dalteparin.<br />
11. Gould MK et al. Prevention of VTE in nonorthopedic surgical patients:<br />
Antithrombotic therapy and prevention of thrombosis. 9th edition: American<br />
College of Chest Physicians evidence based Clinical Practice Guidelines.<br />
Chest 2012; 141(2_suppl): e227S-e277S<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 15 of 57
12. Falck-Ytter Y et al. Prevention of VTE in orthopaedic surgical patients:<br />
Antithrombotic therapy and prevention of thrombosis. 9th edition: American<br />
College of Chest Physicians evidence based Clinical Practice Guidelines.<br />
Chest 2012; 141(2_suppl):e278S-e325S<br />
13. Kahn SR et al. Prevention of VTE in nonsurgical patients: Antithrombotic<br />
therapy and prevention of thrombosis. 9th edition: American College of Chest<br />
Physicians evidence based Clinical Practice Guidelines. Chest 2012;<br />
141(2_suppl):3195S- e226S<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 16 of 57
Appendix 1: Guideline for the Prevention of <strong>Venous</strong><br />
<strong>Thromboembolism</strong> in Adults<br />
1. All in-patients and day case surgery patients must have a documented risk<br />
assessment performed on admission leading to a clinical decision regarding<br />
appropriate measures to prevent venous thromboembolism (VTE)<br />
2. The Trust risk assessment tool on the drug chart must be used to record the risk<br />
assessment. A decision on the use or otherwise of pharmacological or<br />
mechanical prophylaxis must be clearly documented<br />
3. General preventative measures (early mobilisation, leg exercises and ensuring<br />
adequate hydration) are appropriate for all patients and are communicated on<br />
admission<br />
4. The decision on how to manage the risk of VTE will be based on an assessment<br />
of the risks of VTE against the bleeding risk of preventative treatment for each<br />
individual patient<br />
5. The risk assessment must be reviewed within 24 hours of admission.<br />
Subsequently the risk assessment must be reviewed whenever the clinical<br />
situation changes (every 24 hours for ICU patients)<br />
6. Before starting VTE prophylaxis patients and/or their families or carers must be<br />
given verbal +/- written information on their risk of VTE, the importance of VTE<br />
prophylaxis and possible side effects, the correct use of VTE prophylaxis and<br />
how they can reduce their risk of VTE (i.e. keep well hydrated, do leg exercises<br />
and mobilise if possible)<br />
7. On discharge patients and/or their families or carers must be given verbal +/-<br />
written information on:<br />
• The signs and symptoms of deep vein thrombosis and pulmonary<br />
embolism<br />
• The importance of seeking medical help and who to contact if deep vein<br />
thrombosis or pulmonary embolism is suspected<br />
• If discharged with prophylaxis:<br />
o the correct and recommended duration of use of VTE prophylaxis<br />
o how to use VTE prophylaxis correctly<br />
o the signs and symptoms of adverse events related to VTE<br />
prophylaxis<br />
o the importance of seeking help and who to contact if they have any<br />
problems using the prophylaxis<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 17 of 57
8. Ensure that patients who are discharged with anti-embolism stockings:<br />
• Understand the benefits of wearing them<br />
• Understand the need for daily removal and hygiene<br />
• Are able to remove and replace them, or have someone available who will<br />
be able to do this for them<br />
• Know what problems to look for, such as skin marking, blistering or<br />
discolouration, particularly over the heels and bony prominences<br />
• Know who to contact if there is a problem<br />
9. Ensure that patients who are discharged with pharmacological and/or<br />
mechanical VTE prophylaxis are able to use it correctly, or have arrangements<br />
made for someone to be available who will be able to help them<br />
10. Notify the patient’s GP if the patient has been discharged with pharmacological<br />
and/or mechanical VTE prophylaxis to be used at home<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 18 of 57
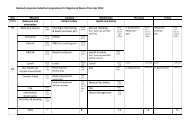
Appendix 2:<br />
Guideline<br />
General Medicine Thromboprophylaxis<br />
First assessment carried out<br />
by admitting doctor<br />
Patient has had or is expected to have<br />
significantly reduced mobility for 3 or more<br />
days (i.e. bedbound, unable to walk unaided,<br />
or likely to spend a substantial proportion of<br />
the day in bed or in a chair<br />
Yes<br />
No<br />
Patient is expected to have ongoing<br />
reduced mobility relative<br />
to normal and has one or more<br />
risk factors (box 1)<br />
No<br />
Box 1. VTE risk factors:<br />
• Active cancer or cancer treatment<br />
• Aged over 60 years<br />
• Critical care admission<br />
• Dehydration<br />
• Known thrombophilia<br />
• BMI >30 kg/m 2<br />
• Personal or first degree relative history of VTE<br />
• One or more significant medical comorbidities<br />
(heart disease; metabolic, endocrine or<br />
respiratory pathologies; acute infectious<br />
diseases; inflammatory conditions)<br />
• HRT or oestrogen-containing contraceptive<br />
• Varicose veins with phlebitis<br />
• Pregnant or given birth within 6 weeks<br />
No VTE prophylaxis needed<br />
Yes<br />
Risk of bleeding from<br />
pharmacological prophylaxis (box 2)<br />
Use LMWH. Check<br />
renal function<br />
No<br />
Prescribe dalteparin (see full guideline).<br />
If renal impairment (eGFR2)<br />
• Concurrent anticoagulant use (e.g. warfarin<br />
with INR>2)<br />
• Lumbar puncture/epidural/spinal anaesthesia<br />
within next 12 hours or previous 4 hours<br />
• Acute stroke<br />
• Platelets 230/120 mmHg<br />
• Untreated inherited bleeding disorders (e.g.<br />
haemophilia, von Willebrand’s)<br />
• Anticipated or recent procedure<br />
All VTE prophylaxis contraindicated<br />
Consider the use of anti-embolism<br />
stockings.<br />
Need to be measured and correctly fitted<br />
Wear day and night<br />
Document assessment and management<br />
Avoid dehydration<br />
Encourage mobility<br />
Give patient information leaflet<br />
Re-assess VTE and bleeding risks within 24 hours.<br />
Ensure prophylaxis is being given correctly<br />
Box 3. Contraindications to anti-embolism stockings<br />
• Suspected or proven peripheral arterial disease<br />
• Peripheral arterial bypass graft<br />
• Peripheral neuropathy or other sensory impairment<br />
• Fragile skin, dermatitis, gangrene, recent skin graft<br />
• Allergy to material<br />
• Heart failure<br />
• Severe leg oedema<br />
• Unusual leg size or shape<br />
• Major deformity preventing correct fit<br />
• Caution with venous ulcers or wounds<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 19 of 57
Appendix 2a: Stroke Thromboprophylaxis Guideline<br />
• Do NOT offer anti-embolism stockings. Use IPC graded compression system<br />
(foot pumps) until it is deemed safe for the patient to have pharmacological<br />
VTE prophylaxis<br />
• Consider LMWH if: non-haemorrhagic stroke, and risk of haemorrhagic<br />
transformation is low, and one or more of:<br />
o Major restricted mobility<br />
o Previous VTE<br />
o Dehydration<br />
o Other comorbidities (e.g. cancer)<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 20 of 57
Sequential Compression Devices<br />
for the prevention of<br />
<strong>Venous</strong> thrombo-embolism in stroke patients<br />
A Quick Reference Guide for Prescribers<br />
• Indications:<br />
• Stroke (ischaemic or haemorrhagic)<br />
• Less than 30 days from stroke onset (start use ASAP after stroke)<br />
• Immobile or requires supervision or assistance to mobilise along the<br />
ward (e.g. to the bathroom)<br />
• No contra-indication to SCD use (see below)<br />
• Contra-indications:<br />
• Dermatitis<br />
• Leg ulcers<br />
• Severe oedema<br />
• Congestive cardiac failure (causing any visible pitting oedema)<br />
• Severe peripheral vascular disease<br />
• Existing DVT<br />
• The prescription:<br />
• Prescribe “Thigh-length SCD” or “Thigh-length Flowtrons”<br />
• Mark drug chart with a continuous 24 hour loop<br />
• Also tick chart 3 times a day for skin checks<br />
• Problems to look out for:<br />
• Any skin redness / breaks<br />
• Patient discomfort from sleeves<br />
• Tubing kinked, squashed or trapped e.g. between patients’ legs<br />
• Report any of these immediately to SCD trained nursing staff and<br />
consider discontinuing SCD use (seek senior advice)<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 21 of 57
Appendix 2b: Palliative Care Thromboprophylaxis<br />
Guideline<br />
• For patients undergoing terminal care or on an end-of-life pathway do not use<br />
pharmacological or mechanical thromboprophylaxis<br />
• For patients undergoing palliative care with potentially reversible acute<br />
pathology and is at increased risk of VTE, consider using dalteparin if no<br />
contraindications<br />
• Review decisions about VTE prophylaxis for patients in palliative care daily,<br />
taking into account the views of patients, their families and/or carers and the<br />
multidisciplinary team<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 22 of 57
PATIENTS IN PALLIATIVE<br />
CARE<br />
If patient has potentially<br />
reversible acute pathology<br />
If patient in terminal care<br />
or end-of-life care pathway<br />
Consider LMWH 1 (dalteparin) if no<br />
contraindications, or UFH 2<br />
Do not routinely offer<br />
pharmacological or mechanical<br />
VTE prophylaxis<br />
Review decisions about VTE prophylaxis daily, taking into account potential risks and benefits and<br />
views of the patient, family and/or carers and multidisciplinary team<br />
1<br />
See Methods of <strong>Prophylaxis</strong><br />
2<br />
For patients with renal failure (EGFR
Appendix 2c: Cancer and Central Catheters<br />
Thromboprophylaxis Guideline<br />
Cancer patients<br />
• If the patient is having oncological treatment and is ambulant – mechanical<br />
and pharmacological thromboprophylaxis are not routinely indicated<br />
• If the patient is assessed as having additional risks for VTE use dalteparin if<br />
no contraindications<br />
Patients with central venous catheters<br />
• Do not routinely offer pharmacological or mechanical VTE prophylaxis to<br />
patients with central venous catheters who are ambulant<br />
• If the patient is high risk for VTE consider dalteparin if no contraindications<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 24 of 57
Patients with cancer<br />
Patients with central<br />
catheters<br />
Is patient having<br />
oncological treatment<br />
and ambulant?<br />
Is patient ambulant?<br />
Yes<br />
No<br />
Yes<br />
No<br />
Do not routinely offer<br />
pharmacological or mechanical<br />
VTE prophylaxis<br />
VTE risk<br />
increased?<br />
Do not routinely offer<br />
pharmacological or mechanical<br />
VTE prophylaxis<br />
VTE risk<br />
increased?<br />
Yes<br />
No<br />
Yes<br />
No<br />
Use<br />
LMWH 1 (Dalteparin) if no<br />
contraindications, or UFH 2<br />
Continue until patient no longer at<br />
increased risk of VTE<br />
Use<br />
LMWH 1 (Dalteparin) if no<br />
contraindications, or UFH 2<br />
Reasses within 24 hours of admission and whenever clinical situation changes<br />
1<br />
See Methods of <strong>Prophylaxis</strong><br />
2<br />
For patients with renal failure (eGFR
Appendix 3: Pregnancy and up to 6 weeks Postpartum<br />
Thromboprophylaxis Guideline<br />
Consider pharmacological prophylaxis for women who are pregnant or have given<br />
birth within the previous 6 weeks who are admitted to hospital but are not undergoing<br />
surgery and who have one or more of the following risk factors:<br />
• Expected to have significantly reduced mobility for 3 or more days<br />
• Active cancer or cancer treatment<br />
• Age > 35 years<br />
• Critical care admission<br />
• Dehydration<br />
• Excess blood loss or transfusion<br />
• Known thrombophilia<br />
• Obesity (pre-pregnancy or early pregnancy BMI > 30 kg /m2)<br />
• medical comorbidity (e.g. heart disease; metabolic, endocrine or respiratory<br />
pathologies; acute infectious diseases; inflammatory conditions)<br />
• Personal or first-degree relative history of VTE<br />
• Pregnancy-related risk factor (ovarian hyperstimulation, hyperemesis, multiple<br />
pregnancy, pre-eclampsia)<br />
• Varicose veins with phlebitis<br />
Consider offering combined VTE prophylaxis with mechanical methods and LMWH<br />
(or UFH for patients with renal failure) to women who are pregnant or have given<br />
birth within the previous 6 weeks who are undergoing surgery, including caesarean<br />
section.<br />
Offer mechanical and/or pharmacological VTE prophylaxis to women who are<br />
pregnant or have given birth within the previous 6 weeks only after assessing the<br />
risks and benefits and discussing these with the woman and with healthcare<br />
professionals who have knowledge of the proposed method of VTE prophylaxis<br />
during pregnancy and post-partum. Plan when to start and stop pharmacological<br />
VTE prophylaxis to minimise the risk of bleeding.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 26 of 57
Antenatal VTE risk assessment<br />
Previous VTE on warfarin<br />
VTE in current pregnancy<br />
Anti-thrombin deficiency<br />
Mechanical heart valves<br />
VERY HIGH RISK<br />
Therapeutic enoxaparin 1mg/kg/bd<br />
or equivalent other LMWH during<br />
pregnancy and post partum<br />
warfarin<br />
Refer to combined Haem/ANC<br />
Refer to Anaesthetic ANC<br />
Single previous VTE plus<br />
thrombophilia or family history<br />
(1 st degree relative)<br />
Unprovoked/oestrogen-related<br />
Previous recurrent VTE (>1)<br />
HIGH RISK<br />
Requires antenatal prophylaxis<br />
with LMWH<br />
Refer to combined Haem/ANC<br />
Refer to Anaesthetic ANC<br />
Single previous VTE with no<br />
family history or thrombophilia<br />
Thrombophilia + no VTE<br />
Medical comorbidities, e.g. heart<br />
or lung disease, SLE, cancer,<br />
inflammatory conditions,<br />
nephrotic syndrome, sickle cell<br />
disease, intravenous drug user<br />
Surgical procedure during<br />
pregnancy, e.g. appendicectomy<br />
MODERATE RISK<br />
Consider antenatal prophylaxis<br />
with LMWH<br />
Refer to any general ANC<br />
Age > 35years<br />
Obesity (BMI > 30kg/m2)<br />
Parity > 3<br />
Smoker<br />
Gross varicose veins<br />
Current systemic infection<br />
Immobility, e.g. paraplegia,<br />
SPD, long distance travel<br />
Pre-eclampsia<br />
Dehydration/hyperemesis/<br />
OHSS<br />
Multiple pregnancy<br />
3 or more risk factors<br />
2 or more if admitted<br />
> 3 risk factors<br />
LOWER RISK<br />
Mobilisation and avoidance of<br />
dehydration<br />
KEY<br />
BMI = body mass index (based on booking weight), gross varicose veins = symptomatic, above the knee or associated with phlebitis/oedema/skin<br />
changes, immobility = > 3 days, LMWH = low-molecular weight heparin, OHSS = ovarian hyperstimulation syndrome, PPH = postpartum<br />
haemorrhage, SLE = systemic lupus erythematosus, SPD = symphysis pubis dysfunction with reduced mobility, thrombophilia = inherited or acquired,<br />
long distance travel - > 4 hours, VTE = venous thromboembolism<br />
Antenatal and postnatal prophylactic dose of LMWH<br />
Weight 170 kg = 0.6mg/kg/day enoxaparin; 75 units/kg/day daltaparin; 75 units/kg/day tinzaparin<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 27 of 57
Postnatal VTE risk assessment<br />
• Previous VTE on warfarin<br />
• Anti-thrombin deficiency<br />
• Mechanical heart valves<br />
VERY HIGH RISK<br />
• Re-warfarinize<br />
• Ensure haematology follow<br />
up is arranged<br />
• Anti-embolism stockings<br />
• Any previous VTE<br />
• Anyone requiring antenatal<br />
LMWH<br />
HIGH RISK<br />
• At least 6 weeks postnatal<br />
prophylactic LMWH and<br />
anti-embolism stockings<br />
• Caesarian section in labour<br />
• Asymptomatic<br />
thrombophilia (inherited or<br />
acquired)<br />
• BMI >40 KG/M2<br />
• Prolonged hospital<br />
admission<br />
• Medical co-morbidities e.g.<br />
heart or lung disease, SLE,<br />
cancer, inflammatory<br />
conditions, nephritic<br />
syndrome, sickle cell<br />
disease, intravenous drug<br />
user<br />
MODERATE RISK<br />
• At least 7 days postnatal<br />
prophylactic LMWH and<br />
anti-embolism stockings<br />
Note: if persisting or >3 risk<br />
factors, consider extending<br />
thromboprophylaxis with<br />
LMWH<br />
• Age > 35years<br />
• Obesity (BMI > 30kg/m2)<br />
• Parity > 3<br />
• Smoker<br />
• Elective caesarean section<br />
• Any surgical procedure in<br />
the puerperium<br />
• Gross varicose veins<br />
• Current systemic infection<br />
• Immobility, e.g. paraplegia,<br />
SPD, long distance travel<br />
• Pre-eclampsia<br />
• Mid-cavity rotational<br />
operative delivery<br />
• Prolonged labour<br />
(>24hours)<br />
• PPH > 1 litre or blood<br />
transfusion<br />
2 or more risk factors<br />
< 2 risk factors<br />
LOWER RISK<br />
• Mobilisation and avoidance of<br />
dehydration<br />
• +/- Anti-embolism stockings<br />
KEY<br />
Gross varicose veins = symptomatic, above the knee or associated with phlebitis/oedema/skin changes<br />
immobility = > 3 days<br />
Thrombophilia = inherited or acquired<br />
Long distance travel = > 4 hours<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 28 of 57
Ante-natal<br />
or postnatal<br />
weight<br />
170 kg<br />
LMWH Dose<br />
20 milligrams enoxaparin/2500 units dalteparin/3500 units tinzaparin daily<br />
40 milligrams enoxaparin/5000 units dalteparin/4500 units tinzaparin daily<br />
60 milligrams enoxaparin/7500 units dalteparin/7000 units tinzaparin daily<br />
80 milligrams enoxaparin/10000 units dalteparin/9000 units tinzaparin daily<br />
0.6 milligrams/kilograms/day enoxaparin, 75 units/kilogram/day dalteparin,<br />
75 units/kilogram/day tinzaparin<br />
For women with an identified bleeding risk e.g. von Willebrand’s disease,<br />
thrombocytopenia or severe liver disease the balance of risk and benefits should be<br />
discussed with a senior haematologist.<br />
For women who have suffered a VTE event during pregnancy, refer to the<br />
individualised postnatal care plan. If unavailable, discuss with senior haematologist<br />
at an appropriate time.<br />
For further information, refer to Thromboprophylaxis in pregnancy, labour and the<br />
pueperium policy on the RUH intranet.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 29 of 57
Appendix 4:<br />
Guideline<br />
General Surgical Thromboprophylaxis<br />
All surgery<br />
• Assess the risks and benefits of stopping pre-existing established antiplatelet<br />
therapy 1 week before surgery. Consider involving the multidisciplinary team<br />
in the assessment<br />
• Consider regional anaesthesia for individual patients, in addition to other<br />
methods of VTE prophylaxis, as it carries a lower risk of VTE than general<br />
anaesthesia. Take into account patients’ preferences, their suitability for<br />
regional anaesthesia and any other planned method of VTE prophylaxis<br />
• Advise patient to stop COCP or HRT 4 weeks prior to elective surgery; ensure<br />
using alternative contraception<br />
• If regional anaesthesia is used, plan the timing of pharmacological VTE<br />
prophylaxis to minimise the risk of epidural haematoma. If antiplatelet or<br />
anticoagulant agents are being used, or their use is planned, refer to the Trust<br />
guideline for guidance about the safety and timing of these agents in relation<br />
to the use of regional anaesthesia<br />
• Do not routinely offer pharmacological or mechanical VTE prophylaxis to<br />
patients undergoing a surgical procedure with local anaesthesia by local<br />
infiltration with no limitation of mobility<br />
• Offer VTE prophylaxis to patients undergoing surgery who are assessed to be<br />
at increased risk of VTE:<br />
• Surgical procedure with a total anaesthetic and surgical time of more than<br />
90 minutes, or 60 minutes if the surgery involves the pelvis or lower limb<br />
• Acute surgical admission with inflammatory or intra-abdominal condition<br />
• Expected significant reduction in mobility<br />
• One or more of the risk factors shown below<br />
• Active cancer or cancer treatment<br />
• Age over 60 years<br />
• Critical care admission<br />
• Dehydration<br />
• Known thrombophilia<br />
• BMI > 30 kg/m 2<br />
• Personal or first-degree relative history of VTE<br />
• One or more significant medical comorbidities (heart disease;<br />
metabolic, endocrine or respiratory pathologies; acute infectious<br />
diseases; inflammatory conditions)<br />
• HRT or oestrogen-containing contraceptive<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 30 of 57
• Varicose veins with phlebitis<br />
• Pregnant or given birth within last 6 weeks<br />
Start mechanical VTE prophylaxis on admission. Use one of:<br />
• Anti-embolism stockings (thigh or knee length)<br />
• Foot impulse devices<br />
• Intermittent pneumatic compression devices (thigh or knee<br />
length)<br />
Continue mechanical VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility.<br />
Add pharmacological VTE prophylaxis for patients who have a low risk of<br />
major bleeding, taking into account individual patient factors and according to<br />
clinical judgement. Use one of:<br />
• LMWH<br />
• UFH (for patients with renal failure)<br />
• Rivaroxaban (for elective knee/hip replacement)<br />
Continue pharmacological VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility (generally 5–7 days).<br />
Elective and Emergency patients<br />
The VTE risk assessment must be completed on admission, and the post-operative<br />
plan for VTE prophylaxis must be recorded in the operation note either within the<br />
health record or on Millennium.<br />
On admission the medical staff:<br />
• decide which thromboprophylaxis should be used<br />
• determine if any form of thromboprophylaxis is contraindicated<br />
• agree the timing of starting pharmacological thromboprophylaxis<br />
• prescribe the agreed pharmacological prophylaxis<br />
STEP 1<br />
Identify the patient’s VTE risk factors<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 31 of 57
STEP 2<br />
Identify the risk of thrombosis of the procedure:<br />
Risk group<br />
Low risk<br />
patient and<br />
procedure<br />
High risk<br />
patient or<br />
procedure<br />
Recommended Thromboprophylaxis<br />
• Mobilisation<br />
• Adequate hydration<br />
• Dalteparin<br />
• Use unfractionated heparin if eGFR
Appendix 4a: Vascular, Gastrointestinal, Gynaecological<br />
and Urological Surgery Thromboprophylaxis Guideline<br />
Vascular Surgery<br />
• Offer VTE prophylaxis to patients undergoing vascular surgery who are not<br />
having other anticoagulant therapy and are assessed to be at increased risk<br />
of VTE. If peripheral arterial disease is present, seek expert opinion before<br />
fitting anti-embolism stockings<br />
• Start mechanical VTE prophylaxis at admission. Use one of:<br />
o<br />
o<br />
o<br />
Anti-embolism stockings (thigh or knee length)<br />
Foot impulse devices<br />
Intermittent pneumatic compression devices (thigh or knee length)<br />
• Continue mechanical VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility<br />
• Add pharmacological VTE prophylaxis for patients who have a low risk of<br />
major bleeding, taking into account individual patient factors and according to<br />
clinical judgement. Choose one of:<br />
o<br />
o<br />
LMWH<br />
UFH (for patients with eGFR < 10 ml/min)<br />
Continue pharmacological VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility (generally 5–7 days).<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 33 of 57
Gastrointestinal, Gynaecological and Urological Surgery<br />
• Offer VTE prophylaxis to patients undergoing bariatric surgery<br />
• Start mechanical VTE prophylaxis at admission. Use one of:<br />
o Anti-embolism stockings (thigh or knee length)<br />
o Foot impulse devices<br />
o Intermittent pneumatic compression devices (thigh or knee length)<br />
• Continue mechanical VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility.<br />
• Add pharmacological VTE prophylaxis for patients who have a low risk of<br />
major bleeding, taking into account individual patient factors and according to<br />
clinical judgement. Use one of:<br />
o LMWH<br />
o UFH (for patients with eGFR < 10 ml/min).<br />
• Continue pharmacological VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility (generally 5–7 days).<br />
• Extend pharmacological VTE prophylaxis to 28 days postoperatively for<br />
patients who have had major cancer surgery in the abdomen or pelvis.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 34 of 57
Patients undergoing<br />
general surgery<br />
VASCULAR<br />
SURGERY 1<br />
GASTROINTESTINAL<br />
SURGERY<br />
GYNAECOLOGY,<br />
AND UROLOGY<br />
SURGERY<br />
BARIATRIC<br />
SURGERY<br />
If VTE risk<br />
increased<br />
If VTE risk<br />
increased<br />
If VTE risk<br />
increased<br />
Start mechanical VTE prophylaxis 2 at<br />
admission.<br />
If peripheral arterial disease present, seek<br />
expert opinion before fitting anti-embolism<br />
stockings.<br />
Continue until mobility no longer significantly<br />
reduced<br />
Offer mechanical VTE<br />
prophylaxis 2 at admission.<br />
Continue until mobility no longer<br />
significantly reduced<br />
Offer mechanical VTE<br />
prophylaxis 2 at admission.<br />
Continue until mobility no<br />
longer significantly<br />
reduced<br />
If risk of major<br />
bleeding low<br />
If risk of major<br />
bleeding low<br />
If risk of major<br />
bleeding low<br />
Add:<br />
LMWH (dalteparin) or<br />
UFH 3 . Continue until<br />
mobility no longer<br />
significantly reduced<br />
(generally 5-7 days)<br />
Add:<br />
LMWH (dalteparin) or UFH 3 .<br />
Continue until mobility no longer<br />
significantly reduced (generally 5-<br />
7 days)<br />
Add:<br />
LMWH (dalteparin) or<br />
UFH 3 . Continue until<br />
mobility no longer<br />
significantly reduced<br />
(generally 5-7 days)<br />
1:<br />
Many vascular surgical patients are already having antiplatelet or<br />
anticoagulant therapy. For these patients, seek expert opinion.<br />
2:<br />
Choose any one of these:<br />
• Anti-embolitic stockings (thigh or knee length)<br />
• Foot impulse devices<br />
• Intermittent pneumatic compresssion devices (thigh or knee length)<br />
3:<br />
For patients with renal failure (eGFR
Appendix 4b: Day Surgery Thromboprophylaxis Guideline<br />
The following procedures are low risk:<br />
• Ophthalmological procedures with local anaesthetic/regional<br />
anaesthetic/sedation and not full general anaesthetic<br />
• Non-cancer ENT surgery lasting less than 90 minutes with local anaesthetic<br />
/regional anaesthetic / sedation and not full general anaesthetic<br />
• Non-cancer dental and maxillo-facial surgery lasting less than 90 minutes with<br />
local anaesthetic / regional anaesthetic / sedation and not full general<br />
anaesthetic<br />
Risk assessment to be completed on day surgery drug chart.<br />
If VTE risk high:<br />
• Start mechanical VTE prophylaxis at admission and continue mechanical<br />
thromboprophylaxis until mobility no longer significantly reduced. Use one of:<br />
o Anti-embolism stockings (thigh or knee length)<br />
o Foot impulse devices<br />
o Intermittent pneumatic compression devices (thigh or knee length)<br />
Continue mechanical VTE thromboprophylaxis until the patient no longer has<br />
significantly reduced mobility<br />
• Add pharmacological VTE prophylaxis for patients who have a low risk of<br />
major bleeding. Use LMWH (dalteparin). If the patient is expected to have<br />
significantly reduced mobility after discharge, continue pharmacological VTE<br />
prophylaxis for 5-7 days. Ensure full blood count and renal function checked<br />
prior to commencing.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 36 of 57
Patients having day surgery<br />
If VTE risk<br />
increased<br />
Start mechanical VTE<br />
prophylaxis at admission 1<br />
Continue until mobility no<br />
longer significantly reduced<br />
If risk of<br />
bleeding is<br />
low<br />
Add<br />
LMWH (dalteparin), or UFH 2.<br />
Continue until mobility no<br />
longer significantly reduced<br />
including after discharge<br />
(generally 5-7 days)<br />
1:<br />
Choose any of the following:<br />
• Anti-embolitic stockings (thigh or knee length)<br />
• Foot impulse devices<br />
• Intermittent pneumatic compression devices (thigh or knee length)<br />
2<br />
: For patients with renal failure (eGFR
Appendix 5: Trauma and Orthopaedic Thromboprophylaxis<br />
Guideline<br />
All surgery<br />
• Assess the risks and benefits of stopping pre-existing established antiplatelet<br />
therapy 1 week before surgery. Consider involving the multidisciplinary team<br />
in the assessment<br />
• Consider regional anaesthesia for individual patients, in addition to other<br />
methods of VTE prophylaxis, as it carries a lower risk of VTE than general<br />
anaesthesia. Take into account patients’ preferences, their suitability for<br />
regional anaesthesia and any other planned method of VTE prophylaxis<br />
• Advise patient to stop COCP or HRT 4 weeks prior to elective surgery; ensure<br />
using alternative contraception<br />
• If regional anaesthesia is used, plan the timing of pharmacological VTE<br />
prophylaxis to minimise the risk of epidural haematoma. If antiplatelet or<br />
anticoagulant agents are being used, or their use is planned, refer to the Trust<br />
guidelines for guidance about the safety and timing of these agents in relation<br />
to the use of regional anaesthesia<br />
• Do not routinely offer pharmacological or mechanical VTE prophylaxis to<br />
patients undergoing a surgical procedure with local anaesthesia by local<br />
infiltration with no limitation of mobility<br />
• Offer VTE prophylaxis to patients undergoing surgery who are assessed to be<br />
at increased risk of VTE:<br />
• Surgical procedure with a total anaesthetic and surgical time of more<br />
than 90 minutes, or 60 minutes if the surgery involves the pelvis or lower<br />
limb<br />
• Acute surgical admission with inflammatory or intra-abdominal condition<br />
• Expected significant reduction in mobility<br />
• One or more of the risk factors shown below<br />
• Active cancer or cancer treatment<br />
• Age over 60 years<br />
• Critical care admission<br />
• Dehydration<br />
• Known thrombophilia<br />
• BMI > 30 kg/m 2<br />
• Personal or first-degree relative history of VTE<br />
• One or more significant medical comorbidities (heart disease;<br />
metabolic, endocrine or respiratory pathologies; acute infectious<br />
diseases; inflammatory conditions)<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 38 of 57
• HRT or oestrogen-containing contraceptive<br />
• Varicose veins with phlebitis<br />
• Pregnant or given birth within last 6 weeks<br />
Document the patient’s VTE risk on the Trust drug chart. The procedure<br />
specific guidance outlines which combination of prophylaxis to use.<br />
1. Low risk patients<br />
Early mobilisation<br />
2. High risk patients<br />
• Start mechanical VTE prophylaxis at admission and continue<br />
mechanical thromboprophylaxis until mobility no longer significantly<br />
reduced. Use one of:<br />
o Anti-embolism stockings<br />
o Foot impulse devices<br />
o Intermittent pneumatic compression devices (knee length)<br />
• Total hip and knee arthroplasty patients and fractured neck of femur<br />
patients require extended pharmacological thromboprophylaxis<br />
Pharmacological prophylaxis<br />
Bleeding risk assessment: review the bleeding risk below. Pharmacological<br />
VTE prophylaxis should not be used where the bleeding risk outweighs the VTE<br />
risk. Refer to the procedure specific guidance.<br />
Active bleeding or risk of bleeding<br />
Acquired bleeding disorders (e.g. acute liver<br />
failure)<br />
Concurrent use of anticoagulants known to<br />
increase the risk of bleeding<br />
Acute stroke<br />
Thrombocytopenia (plt < 75 x 109/L)<br />
Untreated inherited bleeding disorders (e.g.<br />
haemophilia)<br />
Bleeding risks<br />
BP ≥230/120 mmHg<br />
Spinal surgery<br />
Epidural / spinal anaesthesia expected within<br />
the next 12 hours<br />
Epidural / spinal anaesthesia within the<br />
previous 4 hours<br />
Renal impairment eGFR < 30ml/min<br />
Weight < 50kg<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 39 of 57
Prescribing notes for Pharmacological Thromboprophylaxis<br />
For patients already on therapeutic anticoagulation with warfarin see intranet<br />
Periprocedural Anticoagulation Guideline<br />
For patients on clopidogrel / aspirin see Perioperative management of antiplatelet<br />
agents<br />
Dalteparin<br />
Timing Elective: 6 hours post op (18.00 /<br />
22.00)<br />
Trauma: prescribe on<br />
admission and 18.00<br />
thereafter.<br />
Ideally allow 6 hours postsurgery<br />
before administering. If<br />
surgery finishes in the afternoon<br />
delay administration until 22.00.<br />
Rivaroxaban 10mg po OD<br />
Total knee and hip arthroplasty only<br />
Administer day 3 post op at<br />
18.00.<br />
Dose<br />
adjustment<br />
Neuraxial<br />
anaesthesia<br />
- spinal<br />
Neuraxial<br />
anaesthesia -<br />
epidural<br />
Post op<br />
vomiting<br />
Weight:<br />
150kg: 7500 units bd<br />
eGFR
Dalteparin<br />
Rivaroxaban 10mg po OD<br />
Total knee and hip arthroplasty only<br />
Drug<br />
interactions<br />
Nil<br />
Contraindications Anticoagulated (INR > 2.0 or<br />
NOAC),<br />
treatment dose LMWH, iv<br />
heparin or abnormal clotting<br />
New onset stroke<br />
Emergency<br />
surgery or<br />
procedure<br />
Discuss with haematologist on<br />
call. Consider delaying<br />
surgery or procedure for 24<br />
hours. Consider the use of<br />
protamine sulphate<br />
CYP3A4 inducers e.g. rifampicin,<br />
reduce the levels of rivaroxaban.<br />
CYP3A4 inhibitors e.g.<br />
ketaconazole, ritonavir increase the<br />
levels of rivaroxaban<br />
eGFR < 15ml/min<br />
hepatic disease associated<br />
with a coagulopathy<br />
clinically relevant bleeding<br />
risk<br />
There is no antidote to<br />
rivaroxaban.<br />
If possible delay surgery or<br />
procedure for 36 hours. If<br />
this is not possible then<br />
inform on call haematologist<br />
and proceed with surgery. If<br />
bleeding cannot be<br />
controlled, consider use of<br />
Beriplex.<br />
Extended (post discharge) prophylaxis<br />
Surgery <strong>Prophylaxis</strong> Monitoring Dose adjustment<br />
Total hip<br />
Nil<br />
arthroplasty<br />
Total knee<br />
arthroplasty<br />
Fractured neck<br />
of femur<br />
Rivaroxaban<br />
10mg PO OD<br />
for 4 weeks<br />
post-operatively<br />
Rivaroxaban<br />
10mg PO OD for 2<br />
weeks post<br />
operatively<br />
Dalteparin for 4<br />
weeks postoperatively<br />
Nil<br />
Nil<br />
Renal impairment:<br />
eGFR150kg: 7500 units twice<br />
daily<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 41 of 57
Other high risk<br />
patients: personal<br />
history of VTE,<br />
lower limb<br />
surgery requiring<br />
extended postoperative<br />
immobilisation.<br />
Dalteparin for<br />
the duration of the<br />
immobilisation<br />
Nil<br />
Renal impairment:<br />
eGFR
ELECTIVE HIP<br />
REPLACEMENT<br />
ELECTIVE KNEE<br />
REPLACEMENT<br />
At admission:<br />
Start mechanical VTE prophylaxis with any one of:<br />
• Anti-embolism stockings (knee length), used with caution<br />
• Foot impulse devices<br />
• Intermittent pneumatic compression devices (thigh or knee<br />
length)<br />
Continue until patient’s mobility no longer significantly reduced<br />
At admission:<br />
Start mechanical VTE prophylaxis with any one of:<br />
• Anti-embolism stockings (knee length), used with caution<br />
• Foot impulse devices<br />
• Intermittent pneumatic compression devices (thigh or knee<br />
length)<br />
Continue until patient’s mobility no longer significantly reduced<br />
Provided there are no contraindications, start<br />
dalteparin 6-12 hours post surgery and continue<br />
for 2 days<br />
Continue with rivaroxaban (dalteparin if<br />
contraindicated) on day 3 and continue for 28<br />
days 1<br />
Provided there are no contraindications, start<br />
dalteparin 6-12 hours post surgery and<br />
continue for 2 days<br />
Continue with rivaroxaban (dalteparin if<br />
contraindicated) on day 3 and continue for 14<br />
days<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 43 of 57
Appendix 5a: Trauma and Orthopaedic Procedure Specific<br />
Thromboprophylaxis Guideline<br />
Hip surgery prophylaxis<br />
Primary and revision THA<br />
• IPC in theatre<br />
• Early mobilisation<br />
• FID/AES (knee length)/IPC (thigh or knee length) for 48 hours postsurgery<br />
• LMWH (dalteparin) 6-12 hours post-surgery to continue until day 2<br />
• Rivaroxaban starting day 3 post op and continuing for 4 weeks. Dalteparin<br />
where rivaroxaban is contraindicated.<br />
Neck of femur fracture patients<br />
• Ensure adequate hydration<br />
• Dalteparin from day of admission continued for 4 weeks post-surgery<br />
• IPC in theatre<br />
• AES (knee length) / IPC (thigh or knee length) / FID post-surgery<br />
Hip surgery procedures < 60 minutes ie LOW risk:<br />
Hip injections<br />
Hip arthrograms<br />
All other hip surgery procedures take > 60 minutes and are high risk<br />
Knee surgery prophylaxis<br />
Arthroscopy<br />
• Early mobilisation<br />
• AES (knee length) for two weeks post-surgery +/- dalteparin<br />
perioperatively in high risk patients<br />
Ligament reconstruction surgery<br />
• Early mobilisation<br />
• Consider AES (knee length) for two weeks post-surgery<br />
High tibial osteotomy<br />
• Early mobilisation<br />
• AES (knee length) for six weeks post-surgery<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 44 of 57
UKA, TKA, revision TKA<br />
• IPC (knee length) in theatre<br />
• Early mobilisation<br />
• Dalteparin starting 6-12 hours post-surgery and continuing until day 2 post<br />
op. Start rivaroxaban day 3 post op and continue for 2 weeks. Use<br />
dalteparin throughout if rivaroxaban contraindicated<br />
Knee surgery procedures < 60 minutes i.e. LOW risk:<br />
Knee arthroscopy<br />
Ligament reconstruction surgery<br />
High tibial osteotomy<br />
All other knee surgery procedures take > 60 minutes and are high risk<br />
Foot and ankle surgery prophylaxis<br />
• Early mobilisation<br />
• Choose any one of AES (knee length)/FIDs/IPC (thigh or knee length):<br />
continue until patient fully mobile<br />
• If extended immobilisation required after surgery start<br />
thromboprophylaxis with LMWH (dalteparin) 6-12 hours post-surgery<br />
and continue until mobility restored.<br />
Foot and ankle surgery procedures
Hand surgery procedures >90 minutes i.e. HIGH risk:<br />
MCPJ replacement<br />
Total elbow replacement<br />
Total wrist replacement<br />
Complex multi finger Dupuytrens surgery<br />
All other hand surgery procedures take
HIP FRACTURE<br />
OTHER ORTHOPAEDIC<br />
SURGERY<br />
At Admission:<br />
• Start mechanical VTE prophylaxis with any one of:<br />
- anti-embolism stockings (knee length)<br />
- foot impulse devices<br />
- intermittent pneumatic compression devices (thigh or<br />
knee length)<br />
Continue until patient’s mobility no longer significantly<br />
reduced<br />
Upper Limb<br />
Surgery<br />
• Provided there are no contraindications, start<br />
LMWH (dalteparin), or UFH 1<br />
At admission:<br />
Assess patient’s<br />
risk of VTE<br />
At admission:<br />
Assess patient’s<br />
risk of VTE<br />
12 hours before surgery<br />
Stop LMWH (heparin), or<br />
UFH 1 if using.<br />
Do not routinely<br />
offer VTE<br />
prophylaxis<br />
If VTE risk<br />
increased<br />
If VTE risk<br />
increased<br />
6 – 12 hours after surgery<br />
Restart LMWH (dalteparin), or UFH 1 if using.<br />
Continue for 28 days<br />
After assessing the risks and discussing with patient:<br />
• Consider offering mechanical VTE prophylaxis with any one<br />
of the following<br />
- anti-embolism stockings (knee length)<br />
- foot impulse devices<br />
- intermittent pneumatic compression devices (thigh or knee<br />
length)<br />
Consider offering LMWH (dalteparin), or UFH 1 6 – 12 hours after<br />
surgery and continue with mechanical prophylaxis<br />
- anti-embolism stockings (knee length<br />
- foot impulse devices<br />
- intermittent pneumatic compression devices (thigh or knee<br />
length) until patient’s mobility no longer significantly reduced<br />
1:<br />
For patients with renal failure (eGFR
Patients undergoing spinal<br />
surgery<br />
If VTE risk<br />
increased<br />
Start mechanical VTE<br />
prophylaxis at admission 1<br />
Continue until mobility no<br />
longer significantly reduced<br />
If risk of<br />
major<br />
bleeding low 3<br />
YES<br />
NO<br />
Add LMWH (dalteparin), or<br />
UFH 2 and continue until<br />
mobility no longer<br />
significantly reduced<br />
(generally 5-7 days)<br />
Do not offer dalteparin or<br />
UFH 2, Continue mechanical<br />
prophylaxis and re-assess<br />
every 24 hours or if<br />
condition changes.<br />
Start pharmacological<br />
prophylaxis when safe<br />
1 Choose any of these:<br />
•<br />
Anti-embolic stockings<br />
•<br />
Foot impulse devices<br />
•<br />
Intermittent pneumatic compression devices<br />
2 For patients with renal failure (Egfr
Appendix 5b: Trauma and Orthopaedic Major Trauma and<br />
Spinal Injury Thromboprophylaxis Guideline<br />
Major trauma<br />
Offer combined VTE prophylaxis with mechanical and pharmacological<br />
methods to patients with major trauma. Regularly reassess the patient’s risks<br />
of VTE and bleeding.<br />
• Start mechanical VTE prophylaxis at admission or as early as<br />
clinically possible. Choose any one of:<br />
o Anti-embolism stockings<br />
o Foot impulse devices<br />
o Intermittent pneumatic compression devices<br />
• Continue mechanical VTE prophylaxis until the patient no longer<br />
has significantly reduced mobility<br />
If the benefits of reducing the risk of VTE outweigh the risks of bleeding and<br />
the bleeding risk has been established as low, add pharmacological VTE<br />
prophylaxis. Use one of:<br />
• LMWH<br />
• UFH (for patients with eGFR < 10 ml/min).<br />
Continue pharmacological VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility.<br />
Spinal injury<br />
Offer combined VTE prophylaxis with mechanical and pharmacological methods<br />
to patients with spinal injury. Regularly reassess the patient’s risks of VTE and<br />
bleeding.<br />
• Start mechanical VTE prophylaxis at admission or as early as clinically<br />
possible. Use one of:<br />
o anti-embolism stockings<br />
o foot impulse devices<br />
o intermittent pneumatic compression devices<br />
• Continue mechanical VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility<br />
If the benefits of reducing the risk of VTE outweigh the risks of bleeding and the<br />
bleeding risk has been established as low, add pharmacological VTE prophylaxis.<br />
Use one of:<br />
o LMWH<br />
o UFH (for patients with eGFR < 10 ml/min).<br />
Continue pharmacological VTE prophylaxis until the patient no longer has<br />
significantly reduced mobility.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 49 of 57
MAJOR TRAUMA OR<br />
SPINAL INJURY<br />
Patient<br />
admitted with<br />
major trauma<br />
Patient<br />
admitted with<br />
spinal injury<br />
Start mechanical VTE prophylaxis at admission or as<br />
soon as clinically possible with any of the following:<br />
• Anti-embolic stockings (knee length)<br />
• Foot impulse devices<br />
• Intermittent pneumatic compression devices (thigh or<br />
knee length)<br />
Continue until mobility no longer significantly reduced<br />
Assess patient’s risks of<br />
VTE and bleeding<br />
If risk of VTE<br />
outweighs risk of<br />
bleeding<br />
YES<br />
Continue<br />
mechanical<br />
prophylaxis<br />
NO<br />
If bleeding<br />
risk is low<br />
Start LMWH (dalteparin) or UFH<br />
(for patients with renal failure)<br />
Continue until mobility no longer<br />
significantly reduced<br />
Regularly re-assess risks of<br />
VTE and bleeding<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 50 of 57
Appendix 5c: Trauma and Orthopaedic Lower Limb Plaster<br />
Casts Thromboprophylaxis Guideline<br />
Lower limb plaster casts<br />
If high risk for VTE start pharmacological VTE prophylaxis with LMWH (or UFH for<br />
patients with eGFR < 10 ml/min) and continue until lower limb plaster cast removal.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 51 of 57
Patient having lower limb plaster<br />
cast<br />
Assess risk of VTE<br />
If VTE risk increased<br />
Start LMWH (dalteparin), or UFH for patients with renal<br />
failure after evaluating risks and benefits and based on<br />
clinical discussion with patient.<br />
Continue until plaster cast is removed and mobility is no<br />
longer significantly reduced<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 52 of 57
Appendix 6: Critical Care Thromboprophylaxis Guideline<br />
Assess risks of VTE and bleeding on admission to critical care unit. Reassess risks<br />
of VTE and bleeding daily.<br />
Offer VTE prophylaxis to patients admitted to the critical care unit according to the<br />
reason for admission, taking into account:<br />
• Any planned interventions<br />
• The use of other therapies that may increase the risk of complications<br />
Pharmacological thromboprophylaxis<br />
LMWH – dalteparin<br />
Mechanical methods (check contraindications section 7.5)<br />
Anti-embolic stockings (AES) – thigh or knee length<br />
Use as an adjunct or alternative to pharmacological prophylaxis when<br />
there is increased risk of bleeding from heparin use due to patient or<br />
procedure related factors.<br />
Intermittent Pneumatic Compression (IPC) devices - thigh or knee<br />
length<br />
Use when pharmacological prophylaxis is contraindicated as part of<br />
speciality specific guidelines.<br />
Foot Impulse Devices<br />
Require correct use and should only be used as part of speciality specific<br />
guidelines<br />
ICU specific guidance<br />
• <strong>Prophylaxis</strong> can be introduced within 24 hours post-operatively in vascular<br />
surgery<br />
• In spinal injuries, prophylaxis can generally be commenced after 24 hours<br />
post- operatively or post-injury if the management is to be conservative:<br />
discuss with the orthopaedic team<br />
• In head injuries, prophylaxis can be commenced 24 hours post-injury provided<br />
haemostasis is achieved and surgery is not planned within the next 12 hours<br />
• Inferior vena cava filters are only indicated to prevent PE in patients with DVT<br />
who have a contraindication to anticoagulation. If possible removable filters<br />
should be used.<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 53 of 57
Patient admitted to critical care unit<br />
Assess risks of VTE and<br />
bleeding on admission to critical<br />
care unit<br />
Take into account planned<br />
interventions and other<br />
therapies that may increase<br />
risk of complications<br />
Offer mechanical 1 and/or<br />
pharmaceutical VTE<br />
prophylaxis according to<br />
reason for admission<br />
• Reassess risks of VTE and bleeding and<br />
review decisions about VTE prophylaxis<br />
daily – more frequently if clinical condition<br />
is changing rapidly<br />
• Take into account known views of the<br />
patient, family and/or carers and<br />
multidisciplinary team<br />
1. Choose any one of:<br />
• Anti-embolic stockings (thigh or knee length)<br />
• Foot impulse devices<br />
• Intermittent pneumatic compression devices (thigh or knee length)<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 54 of 57
Document Control Information<br />
Ratification Assurance Statement<br />
Dear<br />
Tim Craft<br />
Please review the following information to support the ratification of the below named<br />
document.<br />
Name of document:<br />
Name of author:<br />
<strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong><br />
Josephine Crowe<br />
Job Title:<br />
Consultant Haematologist<br />
I, the above named author confirm that:<br />
• The <strong>Policy</strong> presented for ratification meets all legislative, best practice and other<br />
guidance issued and known to me at the time of development of the <strong>Policy</strong>;<br />
• I am not aware of any omissions to the <strong>Policy</strong>, and I will bring to the attention of the<br />
Executive Director any information which may affect the validity of the <strong>Policy</strong><br />
presented as soon as this becomes known;<br />
• The <strong>Policy</strong> meets the requirements as outlined in the document entitled Trust-wide<br />
<strong>Policy</strong> for the Development and Management of Policies (v4.0);<br />
• The <strong>Policy</strong> meets the requirements of the NHSLA Risk Management Standards to<br />
achieve as a minimum level 2 compliance, where applicable;<br />
• I have undertaken appropriate and thorough consultation on this <strong>Policy</strong> and I have<br />
documented the names of those individuals who responded as part of the<br />
consultation within the document. I have also fed back to responders to the<br />
consultation on the changes made to the <strong>Policy</strong> following consultation;<br />
• I will send the <strong>Policy</strong> and signed ratification checklist to the <strong>Policy</strong> Coordinator for<br />
publication at my earliest opportunity following ratification;<br />
• I will keep this <strong>Policy</strong> under review and ensure that it is reviewed prior to the review<br />
date.<br />
Signature of Author:<br />
Name of Person<br />
Ratifying this policy:<br />
Job Title:<br />
Dr Tim Craft<br />
Medical Director<br />
Date:<br />
Signature: Date: 24 th July 2014<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 55 of 57
To the person approving this policy:<br />
Please ensure this page has been completed correctly, then print, sign and<br />
post this page only to: The <strong>Policy</strong> Coordinator, John Apley Building.<br />
The whole policy must be sent electronically to: ruh-tr.policies@nhs.net<br />
Consultation Schedule<br />
Original Document:<br />
Name and Title of Individual<br />
Date Consulted<br />
Dr Tim Craft, Deputy Medical Director 28/10/2009<br />
Dr Regina Brophy, Head Pharmacist 28/10/2009<br />
Dr. William Hubbard, Clinical Director of Medicine 28/10/2009<br />
Mr. Chris Gallegos, Clinical Director for Surgery 29/10/2009<br />
Elizabeth Beech, prescribing adviser BANES PCT 28/10/2009<br />
Name of Committee/s (if applicable)<br />
Date of<br />
Committee<br />
Hospital Thrombosis Committee 04/11/2009<br />
Clinical reference group 12/01/2010<br />
Operational Governance Committee 14/07/2010<br />
Document Revised to include Dalteparin:<br />
Name and Title of Individual<br />
Date Responded<br />
Caroline Quinn, Surgical Pharmacist 14/03/2011<br />
Gayle Wynn, Admissions Pharmacist 14/03/2011<br />
Matthew Jones, Medicines Information Pharmacist 14/03/2011<br />
Dr. Mark Mallet, Consultant Physician, Acute Medicine 14/03/2011<br />
Document Revised to clarify recording of VTE Assessment:<br />
Name of Committee/s (if applicable)<br />
Date of<br />
Committee<br />
Dr Jo Crowe, Consultant Haematologist 17/01/2013<br />
Document Revised to meet NICE guidance recommendations<br />
Name of Committee/s (if applicable)<br />
Date of<br />
Committee<br />
Dr Jo Crowe, Consultant Haematologist 17/07/2014<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 56 of 57
Equality Impact: (A) Assessment Screening<br />
To be completed when submitted to the appropriate Executive Director for<br />
consideration and approval.<br />
Person responsible for the assessment:<br />
Name:<br />
Dr Josephine Crowe<br />
Job Title:<br />
Consultant Haematologist<br />
Does the document/guidance affect one<br />
group less or more favourably than another<br />
on the basis of:<br />
Yes/No<br />
Comments<br />
Race Yes No<br />
Ethnic origins (including gypsies and travellers) Yes No<br />
Nationality Yes No<br />
Gender (including gender reassignment) Yes No<br />
Culture Yes No<br />
Religion or belief Yes No<br />
Sexual orientation Yes No<br />
Age Yes No<br />
Disability<br />
(learning disabilities, physical disability, sensory impairment and<br />
mental health problems)<br />
Yes<br />
No<br />
Is there any evidence that some groups are affected<br />
differently?<br />
Yes No<br />
If you have identified potential discrimination, are there<br />
any valid exceptions, legal and/or justifiable?<br />
Yes No<br />
Is the impact of the document/guidance likely to be<br />
negative?<br />
Yes No<br />
If so, can the impact be avoided? Yes No<br />
What alternative is there to achieving the<br />
document/guidance without the impact?<br />
Yes No<br />
Can we reduce the impact by taking different action? Yes No<br />
If you answered NO to all the above questions, the assessment is now complete, and no<br />
further action is required.<br />
If you answered YES to any of the above please complete the<br />
Equality Impact: (B) Full Analysis<br />
Document name: <strong>Venous</strong> <strong>Thromboembolism</strong> <strong>Prophylaxis</strong> Ref.: 795<br />
Issue date: 30 July 2014<br />
Status: Final<br />
Author: Josephine Crowe – Consultant Haematologist Page 57 of 57