Creating the Burning Platform for Change - Trinity Health
Creating the Burning Platform for Change - Trinity Health
Creating the Burning Platform for Change - Trinity Health
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
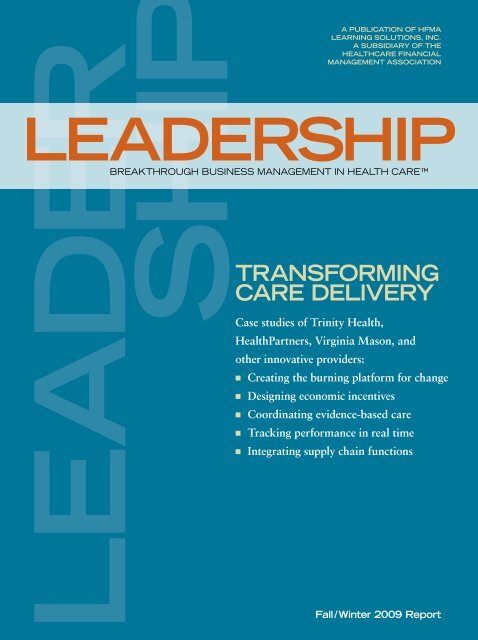
leader<br />
ship<br />
Trans<strong>for</strong>ming<br />
Care Delivery<br />
Case studies of <strong>Trinity</strong> <strong>Health</strong>,<br />
<strong>Health</strong>Partners, Virginia Mason, and<br />
o<strong>the</strong>r innovative providers:<br />
A Publication of HFMA<br />
Learning Solutions, Inc.<br />
A Subsidiary of <strong>the</strong><br />
<strong>Health</strong>care Financial<br />
Management Association<br />
leadership<br />
Breakthrough Business Management in <strong>Health</strong> Care <br />
n <strong>Creating</strong> <strong>the</strong> burning plat<strong>for</strong>m <strong>for</strong> change<br />
n Designing economic incentives<br />
n Coordinating evidence-based care<br />
n Tracking per<strong>for</strong>mance in real time<br />
n Integrating supply chain functions<br />
Fall/Winter 2009 Report
S e c t i o n 1<br />
6 LEADERSHIP | Fall/Winter 2009
<strong>Creating</strong> <strong>the</strong><br />
<strong>Burning</strong><br />
<strong>Plat<strong>for</strong>m</strong><br />
<strong>for</strong> <strong>Change</strong><br />
Forward-thinking healthcare leaders are not waiting <strong>for</strong><br />
legislation to dictate how to trans<strong>for</strong>m health care. They have<br />
a vision of <strong>the</strong> future—and <strong>the</strong>y are already headed toward it.<br />
There are many ways <strong>for</strong> healthcare organizations<br />
to move toward higher quality and greater<br />
coordination and efficiency in patient care. But<br />
all paths start from <strong>the</strong> same point: a leadership team<br />
that effectively identifies and communicates <strong>the</strong> need to<br />
radically restructure <strong>the</strong> way in which healthcare services<br />
are delivered.<br />
That trans<strong>for</strong>mation requires leaders to bring all<br />
constituencies—<strong>the</strong> governing board, physicians,<br />
clinical managers, employees, vendors, patients, and<br />
<strong>the</strong> community at large—on board with a new vision<br />
<strong>for</strong> <strong>the</strong> organization.<br />
Finding <strong>the</strong> Right <strong>Plat<strong>for</strong>m</strong><br />
Setting an example in proactive leadership, executives at<br />
Michigan-based <strong>Trinity</strong> <strong>Health</strong> launched a major technology<br />
investment and change initiative nine years ago. When<br />
<strong>the</strong>y <strong>for</strong>esaw <strong>the</strong> current financial crisis—in trends such as<br />
sharply reduced patient volumes and rising bad debt—<br />
<strong>the</strong>y moved quickly to build on <strong>the</strong>ir earlier preparations.<br />
By <strong>the</strong> time <strong>the</strong> stock market collapsed in September 2008,<br />
<strong>Trinity</strong> <strong>Health</strong> president and CEO Joseph R. Swedish was<br />
ready to launch a series of initiatives to fundamentally<br />
reinvent <strong>the</strong> system’s business, which includes 45 hospitals<br />
and 379 ambulatory facilities in seven states.<br />
“To take <strong>the</strong> organization to <strong>the</strong> next level, it was<br />
necessary to more aggressively unify and standardize<br />
our processes of care delivery, service, and support so as<br />
to reduce variation and accelerate gains,” says Swedish.<br />
The program, called “Sustaining <strong>the</strong> Ministry,”<br />
started with immediate steps, including capital<br />
spending reductions, to offset a multimillion dollar<br />
budget gap resulting from <strong>the</strong> unprecedented challenges<br />
of <strong>the</strong> recession. Beyond that, however, <strong>the</strong> program<br />
is guiding <strong>Trinity</strong> <strong>Health</strong> as it redefines <strong>the</strong> model of<br />
care. “This is really our ef<strong>for</strong>t to accelerate change in<br />
<strong>the</strong> organization,” says Kedrick D. Adkins, president<br />
of integrated services at <strong>the</strong> not-<strong>for</strong>-profit Catholic<br />
health system.<br />
By “change,” Adkins means a radical departure.<br />
<strong>Trinity</strong> <strong>Health</strong> aims to trans<strong>for</strong>m itself from a traditional,<br />
hospital-centric organization that focuses primarily on<br />
acute care to a care delivery organization that delivers<br />
<strong>the</strong> full spectrum of care—ambulatory care, critical<br />
care, chronic disease care, long-term care, home care,<br />
retail-oriented care—in a coordinated, efficient manner.<br />
The vision reflects a healthcare ideal in which<br />
providers work toge<strong>the</strong>r across care sites to deliver <strong>the</strong><br />
highest-quality care in <strong>the</strong> most appropriate setting<br />
and in <strong>the</strong> most efficient manner.<br />
hfma.org/leadership | LEADERSHIP 7
The vision also makes good business sense as<br />
hospital-centric organizations watch inpatient volumes<br />
decline and outpatient numbers rise. Revenue from<br />
ambulatory care and physician practices now represent<br />
almost 50 percent of <strong>Trinity</strong> <strong>Health</strong>’s business.<br />
Fortuitously, <strong>Trinity</strong> <strong>Health</strong>’s<br />
$400 million investment nine<br />
years ago has proved crucial<br />
toward achieving <strong>the</strong> system’s<br />
new vision. The majority of <strong>the</strong><br />
dollars went toward building<br />
an electronic health record<br />
(EHR), complete with computerized<br />
physician order entry,<br />
which is now up and running<br />
at 22 system hospitals.<br />
Physicians can now access<br />
medical records and place<br />
orders from <strong>the</strong> hospital, <strong>the</strong>ir<br />
homes, <strong>the</strong>ir offices, or<br />
anywhere. Nurses are spending<br />
8 percent more time with<br />
patients, as opposed to<br />
documenting in paper records. Most important, patient<br />
safety has improved: Computer-generated alerts flag<br />
about 14,000 potential adverse drug events each year.<br />
The EHR rollout coincided with a clinical improvement<br />
ef<strong>for</strong>t aimed at adopting evidence-based care<br />
protocols. Long be<strong>for</strong>e <strong>the</strong> federal government passed<br />
legislation on comparative effectiveness research, <strong>Trinity</strong><br />
<strong>Health</strong> physicians were weighing <strong>the</strong> benefits and costs<br />
of various treatment approaches.<br />
Today, <strong>the</strong> health system has<br />
172 standard order sets in place<br />
and more than 2,500 standard<br />
The vision reflects a<br />
drugs in <strong>the</strong> <strong>for</strong>mulary.<br />
healthcare ideal in which<br />
Patients receive <strong>the</strong> greatest<br />
benefit from standardized,<br />
providers work toge<strong>the</strong>r<br />
evidenced-based care: <strong>Trinity</strong><br />
<strong>Health</strong> saw a 21 percent<br />
across care sites to deliver<br />
reduction in severity-adjusted<br />
mortality (or 2,612 fewer<br />
<strong>the</strong> highest-quality care in <strong>the</strong><br />
deaths) in 2007. Also, <strong>the</strong> health<br />
most appropriate setting and system per<strong>for</strong>ms better than <strong>the</strong><br />
national average on 97 percent<br />
in <strong>the</strong> most efficient manner. of core clinical indicators.<br />
“As <strong>the</strong> government and<br />
private payers move toward<br />
payment that rewards outcomes<br />
and care coordination ra<strong>the</strong>r than volume, <strong>Trinity</strong><br />
<strong>Health</strong> can leverage a full array of EHR and clinical<br />
support tools to align with physicians and create better,<br />
Managing <strong>Change</strong><br />
There is no one-size-fits-all <strong>for</strong>mula <strong>for</strong> managing change.<br />
Below are some key points.<br />
Determine <strong>the</strong> context <strong>for</strong> change. This step requires<br />
in<strong>for</strong>mation ga<strong>the</strong>ring and analysis. What is <strong>the</strong> imperative<br />
<strong>for</strong> change? Who are all <strong>the</strong> groups that need to be involved?<br />
What are <strong>the</strong> potential impediments to change?<br />
Build support <strong>for</strong> change. Early in <strong>the</strong> change process,<br />
core believers need to involve a larger group of “initial<br />
participators” who will participate in <strong>the</strong> initiative out of<br />
loyalty to <strong>the</strong> organization.<br />
Develop a motivating vision. Such a vision enables people to<br />
imagine new possibilities <strong>for</strong> <strong>the</strong> organization and <strong>for</strong><br />
<strong>the</strong>mselves as members of <strong>the</strong> organization.<br />
Articulate clear, specific, and realistic goals and strategies.<br />
Specific goals and strategies guide people as <strong>the</strong>y undertake<br />
<strong>the</strong> steps necessary to make <strong>the</strong> vision a reality.<br />
Communicate. Use all available methods of communication<br />
to get across <strong>the</strong> need <strong>for</strong> change, <strong>the</strong> vision, and <strong>the</strong><br />
change process.<br />
Identify barriers to change and develop strategies to<br />
overcome <strong>the</strong>m. Problems that are ignored and allowed to<br />
fester can breed resentment, distrust, and uncertainty.<br />
Look <strong>for</strong> <strong>the</strong> early win. By making <strong>the</strong> most out of small,<br />
early successes, managers can establish <strong>the</strong> credibility of<br />
<strong>the</strong> change initiative.<br />
Recognize participants <strong>for</strong> <strong>the</strong>ir ef<strong>for</strong>ts. Possible<br />
rewards include promotions, bonuses, praise, and notes<br />
of recognition.<br />
Source: Adapted from Organizational <strong>Change</strong>: Primer, Department of Veterans Affairs, <strong>Health</strong> Services Research and Development, 2000. For <strong>the</strong> full report,<br />
visit www.hsrd.research.va.gov/publications/primer/.<br />
8 LEADERSHIP | Fall/Winter 2009
more efficient systems of care,” says Terry O’Rourke, MD,<br />
chief clinical officer.<br />
Despite how far <strong>Trinity</strong> <strong>Health</strong> has come, it still has a<br />
lot of work to do be<strong>for</strong>e it can call itself a “care delivery<br />
organization.” Most of <strong>the</strong> progress to date has been done<br />
on <strong>the</strong> inpatient side. Now <strong>the</strong> health system is extending<br />
its EHR and clinical improvement ef<strong>for</strong>ts to ambulatory<br />
clinics and outpatient services. The work includes<br />
implementing standard EHRs and related technologies<br />
<strong>for</strong> more than 1,000 employed physicians.<br />
“EHR capabilities already support care delivery in<br />
our hospital-based outpatient service settings, and we<br />
are in <strong>the</strong> process of finalizing a strategy and approach<br />
<strong>for</strong> ambulatory clinics,” said CIO Paul Browne. “These<br />
will be areas of intense focus <strong>for</strong> <strong>the</strong> next several years.”<br />
<strong>Trinity</strong> <strong>Health</strong> is also reaching out to physicians to gain<br />
<strong>the</strong>ir support and cooperation in improving quality and<br />
efficiency across care sites. The health system is studying<br />
various alignment models, including physician employment<br />
and clinical service line comanagement agreements.<br />
Communicating <strong>the</strong> Vision<br />
Seattle-based Virginia Mason Medical Center’s view of<br />
<strong>the</strong> future can be summed up in <strong>the</strong> organization’s<br />
motivational vision: “To be <strong>the</strong> Quality Leader and<br />
trans<strong>for</strong>m health care.” Virginia Mason leaders seek to<br />
have zero defects in <strong>the</strong> quality and safety of care<br />
delivered to patients, and <strong>the</strong>y intend to lead all healthcare<br />
providers to share <strong>the</strong>ir vision.<br />
To move toward this goal, Virginia Mason—a<br />
336-bed hospital and a network of clinics across western<br />
Washington—uses <strong>the</strong> Virginia Mason Production<br />
System, which is adapted from <strong>the</strong> famed Toyota<br />
Production System. Virginia Mason seeks continuous<br />
improvement to eliminate defects and waste. The idea is<br />
that, by creating processes that eradicate rework and<br />
inefficiency, <strong>the</strong> health system frees up staff time and<br />
financial resources to focus on patients.<br />
To date, <strong>the</strong> positive effects on quality and costs are<br />
inspirational. Here are a few examples: Patient falls have<br />
decreased from 3.42 per 1,000 patient days to 2.92 falls<br />
MedAssist 1.2 pg color ad.pdf 12/15/08 4:50:33 PM<br />
Imagine your Revenue Cycle all in Sync…<br />
Eligibility Services<br />
Receivables Management<br />
Medical Advantage Plan<br />
Collection Services<br />
* HFMA staff and volunteers determined that this product has met specific criteria developed under <strong>the</strong> HFMA Peer Review Process. HFMA does not endorse or guaranty <strong>the</strong> use of this product.<br />
hfma.org/leadership | LEADERSHIP 9
in a single year. Inventory costs have decreased by more<br />
than $1 million through <strong>the</strong> use of supply standardization.<br />
The amount of time it takes patients to receive lab results<br />
has been reduced by more than 85 percent. Plus, <strong>the</strong><br />
health system has saved $11 million in planned capital<br />
investment by using space more efficiently.<br />
Having undertaken more than 660 continuous<br />
improvement activities in <strong>the</strong> past seven years, Virginia<br />
Mason staff members know <strong>the</strong> system’s vision and<br />
strategy <strong>for</strong> achieving it. “We have a very well developed<br />
strategic plan that all 5,000 of our employees could<br />
explain to you,” says Suzanne Anderson, senior vice<br />
president, CFO, and CIO. “Having everyone understand<br />
what we are aiming <strong>for</strong> and having <strong>the</strong> Virginia Mason<br />
Production System as our tool to get <strong>the</strong>re is what<br />
allows us to achieve <strong>the</strong> results that we are aiming <strong>for</strong>.”<br />
A triangle graphic is used to rein<strong>for</strong>ce <strong>the</strong> health<br />
system’s strategic plan at every turn (see <strong>the</strong> exhibit<br />
on this page). The graphic spells out Virginia Mason’s<br />
vision, mission, values, key strategies, and foundational<br />
elements.<br />
“As we do our work, we start meetings with this<br />
graphic so people understand that whatever we are<br />
working on at that moment ties to our strategic<br />
plan and what we are trying to accomplish,”<br />
says Anderson.<br />
For example, a current initiative aimed<br />
at improving <strong>the</strong> discharge process in <strong>the</strong><br />
emergency department (ED) addresses<br />
Virginia Mason’s “service” strategy,<br />
which seeks to “create an extraordinary<br />
patient experience.”<br />
Virginia Mason leaders use<br />
this simple graphic to<br />
continually communicate<br />
and sum up <strong>the</strong> health<br />
system’s vision and<br />
strategic plan.<br />
Strong<br />
Economics<br />
People<br />
We attract<br />
and develop<br />
<strong>the</strong> best team<br />
Patient<br />
Vision<br />
To be <strong>the</strong> Quality Leader<br />
and trans<strong>for</strong>m health care<br />
Mission<br />
To improve <strong>the</strong> health and<br />
well-being of <strong>the</strong> patients we serve<br />
Values<br />
Teamwork | Integrity | Excellence | Service<br />
Virginia Mason Team Medicine ® Foundational Elements<br />
Responsible<br />
Governance<br />
We relentlessly<br />
pursue <strong>the</strong><br />
highest quality<br />
outcomes of care<br />
Integrated<br />
In<strong>for</strong>mation<br />
Systems<br />
Source: Virginia Mason Medical Center. Reprinted with permission.<br />
Strategies<br />
Quality Service Innovation<br />
We create an<br />
extraordinary<br />
patient experience<br />
Education<br />
Virginia Mason Production System<br />
The initiative also ties into one of <strong>the</strong> plan’s foundational<br />
elements—strong economics—since a more efficient<br />
discharge process would help increase patient throughout.<br />
Fur<strong>the</strong>r, it ties to <strong>the</strong> “people” component of <strong>the</strong><br />
strategic plan because a less crowded ED reduces <strong>the</strong><br />
frustration that staff members experience when <strong>the</strong>y<br />
work in a harried ED.<br />
“Elements of this initiative tie into each one of <strong>the</strong><br />
pieces of our strategic plan,” says Anderson. “If you<br />
have staff people involved in <strong>the</strong> work, it is important<br />
<strong>for</strong> <strong>the</strong>m to understand <strong>the</strong> bigger picture.”<br />
Catching <strong>the</strong> Momentum<br />
The leaders of <strong>Trinity</strong> <strong>Health</strong> see <strong>the</strong> current healthcare<br />
landscape in historic terms—and <strong>the</strong>y are using this<br />
momentum to stoke a trans<strong>for</strong>mative change process.<br />
“We say our business model is experiencing a<br />
tectonic shift,” says Adkins, pointing out that delivering<br />
hospital-centric health care is no longer sufficient to<br />
fulfill <strong>Trinity</strong> <strong>Health</strong>’s mission. “We have to realign our<br />
business, change many of our processes, and reposition<br />
ourselves to reflect how we see healthcare trans<strong>for</strong>mation.”<br />
But it’s also important to get it right, says Andrea<br />
Walsh, executive vice president of <strong>Health</strong>Partners,<br />
<strong>the</strong> integrated healthcare system in Minneapolis.<br />
One of <strong>the</strong> biggest leadership challenges in<br />
health care is balancing <strong>the</strong> need <strong>for</strong> urgent<br />
change with a well thought-out strategy.<br />
“We need to figure out that right balance<br />
of taking <strong>the</strong> time to do it right with<br />
<strong>the</strong> recognition that we do not have<br />
a lot of time.” n<br />
We foster a<br />
culture of learning<br />
and innovation<br />
Research<br />
Virginia Mason<br />
Foundation<br />
10 LEADERSHIP | Fall/Winter 2009<br />
Republished with permission from <strong>the</strong> Fall/Winter 2009 Leadership Special Report, copyright 2009, HFMA Learning Solutions, Inc., www.hfma.org/leadership